for anyone touched by cancer
Artificial sweeteners’ connection to liver cancer
Colonoscopy Q&A
Navigating prostate cancer
5 marijuana considerations
She is a new person page
BROUGHT TO YOU BY THE


for anyone touched by cancer
Artificial sweeteners’ connection to liver cancer
Colonoscopy Q&A
Navigating prostate cancer
5 marijuana considerations
She is a new person page
BROUGHT TO YOU BY THE

Upstate will be offering cancer care to residents of Madison and Oneida counties in a new, larger and convenient location, starting in September.

The state-of-the-art, comprehensive center at 5548 E. Main Street in Verona is easily accessible from the New York State Thruway (Exit 33), Route 31 or Route 365. It’s just 15 minutes from the existing Oneida center, which will transfer services to Verona.

The best cancer care involves more than one doctor. Upstate Cancer Center at Verona continues Upstate’s tradition of offering multidisciplinary care with a team of nationally renowned experts, including board-certified surgeons, medical oncologists, radiation oncologists and other specialists, who consult together to manage each patient’s specific treatment. The center features the latest cancer-fighting technology and access to clinical trials not available elsewhere in the region.
In addition to 15 infusion chairs, 15 exam rooms and two rooms for minor procedures, the center has an on-site pharmacy, plus sophisticated machines for diagnosis and treatment:

Computerized tomography, known as CT or CAT scans, can show a tumor’s shape, size and location, or the blood vessels feeding the tumor, without cutting into the patient.
A CT simulator is a 3D treatment planning system that allows radiation oncologists to design the safest and most effective treatment for each patient before radiotherapy beings.
A linear accelerator aims several types of external beam radiation at cancer tumors with pinpoint accuracy, meant to spare nearby healthy tissues.
Magnetic resonance imaging, or MRI, can sometimes show doctors if a tumor is cancerous, or if a known cancer has spread to other parts of the body. It may also help a doctor plan surgery or radiation therapy.
PET CT is an advanced nuclear imaging technique that enables doctors to examine abnormalities at the cellular level. It combines positron emission tomography, or PET, scans with computerized tomography.
Varian TrueBeam radiotherapy delivers precise dosages of radiotherapy quickly – and synchronized with the patient’s breathing pattern. u

Many people see two outcomes for someone in cancer treatment, says Sophie Friedman. Either the person dies, or the person gets better, and their life returns to normal.
Especially for those who face cancer treatment as young adults the way she did, there is no normal to go back to, she points out.
Friedman, 32, of Fayetteville is a librarian and archivist by training, with a master’s degree in library and information science. She returned to Central New York during the pandemic and embarked on a new career as a project manager with a tech company.
Her cancer began as a quarter-sized blue mark on her arm, almost like a bruise, except it wasn’t flat. It did not hurt, but she could move the mass beneath the skin. A primary care doctor told her not to worry — which she tried to abide by — and to return in six months if the mark was still there. A month later she decided to have it reevaluated. Something about it felt off.
An ultrasound image of the mass revealed it to be a complex cyst, meaning it was comprised of tissue and blood. The doctor offered two options. She could have a magnetic resonance imaging scan and a biopsy to find out what the mass was made of. Or she could have it surgically removed.
Friedman opted for surgery, which was done in February 2022. Lab testing showed the mass was Ewing sarcoma, which usually is found in children and adolescents. A diagnosis in someone in their 30s was rare. “Friedman’s surgeon referred her to Upstate orthopedic oncology surgeon Timothy Damron, MD, an expert in cancers that occur in the limbs.
After six rounds of chemotherapy, she underwent a second surgery to remove more tissue. Then she had an additional eight rounds of chemo, sometimes requiring hospitalization. Her chemo was a regimen including five medications. She began connecting with other young adult cancer survivors on social media and decided to share her experiences on Instagram and TikTok.

“At first I didn’t share a lot, but the more I shared, the more I felt empowered, and the more I felt like I was advocating for myself and other people,” she explains. “Not only was I connecting with other people in similar circumstances, but I was also educating the people in my life who knew nothing about this.”
She never photographed the blue mark, which people on social media constantly ask to see. She has a fairly extensive scar there now. She considers herself lucky. Ewing sarcoma usually occurs in the bone and requires amputation or bone replacement surgery. Her tumor was confined to soft tissue. It was so close to the surface that Damron did not have to remove muscle or do a skin graft.
Her active treatment is over. She’s technically a survivor. But it’s a tough role. She wrestles with fear of recurrence, fear of a secondary cancer, survivor’s guilt, side effects now and longer-term side effects, physical and mental exhaustion, depression, anxiety and more.



“It’s awful. I won’t lie,” Friedman says. “In some ways, this posttreatment era is harder in a psychological and emotional sense than going through treatment.”
Weeks after Friedman’s treatment ended, her cat, Posey, was diagnosed with small cell lymphoma affecting her gastrointestinal tract. The cat is on a special diet now. She also has a vitamin injection every week and a chemo pill every other day. Friedman frets about giving Posey drugs so similar to the ones she had to take.

Survivorship feels impossible for her, some days. Some days she’s anxious. Some days she’s depressed. She does have days where she feels normal, where she doesn’t think about cancer. Friedman is grateful her treatment worked, that she’s in remission. She would like people to understand that for young adult cancer survivors, there’s no going back to a previous life before cancer.
“Our lives are changed forever. We are new people,” she says. u
Maybe you’ve seen Upstate’s big blue mobile mammography van. It travels throughout Central New York, a rolling billboard of sorts that urges women to get screened for breast cancer.
The so-called “mammo van” is especially meaningful to Kimberly Copeland, 43, of Verona.
She turned 40 during the pandemic and scheduled her first mammogram for September 2021, when the 45-foot van was stationed at

Vernon Town Hall, near where she worked as a property manager.
“The ladies on the mammo van, they were fantastic,” she remembers. “They made me feel incredibly comfortable.” Her mammogram was on a Monday. Results came two days later: A mass was discovered that warranted further imaging.
Copeland came to the Upstate campus in downtown Syracuse for the additional imaging and biopsy. When her gynecologist in Oneida
received the lab report, she told Copeland she needed an oncologist. “I said I really like the Upstate people,” and she made an appointment.
Surgery to remove both breasts took place in December 2021 with breast surgeon Lisa Lai, MD, and plastic surgeon Prashant Upadhyaya, MD. Then Copeland had chemotherapy from February through April 2022.
“They saved my life,” she says, crediting Upstate providers, “and it all started with the mammo van.” u
Organizations and businesses throughout Central New York can apply to host Upstate Mobile Mammography by contacting program manager Wendy Hunt at 315-492-3353. Make appointments or learn about upcoming screening events at upstate.edu/noexcuses

Vince Lumia’s hobby always involved music, either through his blues band, Modern Mudd, or karaoke singing, or disc jockeying. And he enjoys giving back by working various benefits.
He was the volunteer DJ when the Upstate Cancer Center celebrated National Cancer Survivors Day last year at the Rosamond Gifford Zoo at Burnet Park.

Today, at 56, Lumia lives with metastatic colon cancer.
“When people find out you have cancer, the first thing they say is, ‘Oh, I’m so sorry.’ I try to explain to them, it’s not as bad as you think,” Lumia says. Cancer forces you to appreciate every moment, he explains, “and I can’t say I’ve always lived that way.”
He and his wife, Sherri Lumia, live on the North Side of Syracuse and have three adult
sons, three adult sons, in Syracuse, Oswego and Raleigh, NC.
They have three grandchildren. They’ve been married 35 years, and Lumia says each year seems like it’s the best.
He was 47 when his doctor sent him for a colonoscopy. He had noticed blood in his stool. “They found a polyp that was too big to snip,” he says. He would need surgery to remove it.
In preparing for that surgery, Lumia went for an imaging scan, which pinpointed the colon cancer but also revealed a tumor on his kidney. Lumia would also need surgery to remove that.
Which was more urgent? The colorectal surgeon and the urologist each believed they needed to operate first; then Lumia would recover for six months before undergoing the second surgery.
What about doing both surgeries at the same time? Lumia asked.
Colorectal surgeon Jiri Bem, MD, and urologist Gennady Bratslavsky, MD, combined their work into a single operation. Both cancers were removed, and Lumia remembers singing two weeks after his surgery.
He regularly went for follow-up blood tests and imaging scans.
“I was fine until the last visit of my fifth year. You know, the one before you’re home free,” Lumia says. “For almost five years, I was cancer-free.”
Cells from his colon cancer were found to have spread to his liver. He underwent chemotherapy and, later, surgery. Today his oncologist, Bernard Poiesz, MD, helps guide further treatment. u
Commonly used sweeteners can cause cancer in the liver, according to Upstate research published recently in the journal Nature Metabolism. The work also shows that medication may prevent the growth of this cancer.
“We should avoid using sugar alcohols such as erythritol and sorbitol as sweeteners,” says Andras Perl, MD, PhD. “They are causing liver cancer, there’s no doubt.”
Erythritol is added to many sugar substitutes, such as stevia, Truvia and other products. Sorbitol sweetens products like chewing gum, ice cream and mints.

Because it is a naturally occurring compound, erythritol is “generally recognized as safe” by the federal Food and Drug Administration, but the quantities used in foods are generally much higher than the body typically creates, Perl says. “Normally the level in the body is very low, undetectable.”
He is a rheumatologist and a SUNY distinguished professor who also oversees a laboratory at Upstate.
Perl designed a study of liver cirrhosis that progresses to liver cancer in mice with a genetic mutation that is also found in humans. Previously, his team of scientists determined mice with a specific mutation were much more likely to develop cancer.
Researchers found that sugar alcohols accumulated in subjects with the genetic defect, which caused a lack of the enzyme transaldolase, known as TAL. Subjects that were missing TAL had a 216-fold increase of erythritol.
The production of sugar alcohols depends on another enzyme, aldose reductase, Perl explains. He says medication can inhibit that enzyme, and “when you block the formation of the sugar alcohol, there’s no cancer.”
His study focused on sugar alcohols created by the body, but they are chemically identical to the sugar alcohols found in many popular sweeteners on the market.
“When we treat cancer cells with sweeteners, it causes the proliferation of cancer cells. They grow much more rapidly,” Perl describes. “In contrast, when we treat cancer cells with inhibitors of aldose reductase, it blocks their proliferation.”
Perl says this is the first study to show the link between sugar alcohols and liver cancer. The next step is to study the rates of cancer in patients who consume sweeteners containing sugar alcohols.
In the meantime, he says this data is strong enough for people to consider avoiding sweeteners that contain erythritol and sorbitol. “These studies are quite definitive that these sweeteners cause cancer.” u
Aclinical trial led by Upstate radiation oncologist Jeffrey Bogart, MD, may have major implications for the treatment of small cell lung cancers.

Patients in Bogart’s trial had similar outcomes and long-term survival rates regardless of whether they were treated with once-a-day or twice-a-day radiotherapy.
With more than 700 participants, the trial was the largest ever performed in limited-stage small cell lung cancer. Data was collected from 2008 to 2019 from patients at Upstate and other cancer centers throughout the United States. Results were published in the Journal of Clinical Oncology, which Bogart describes as “a well-regarded high impact oncology publication.”
A twice-a-day regime had been the standard recommendation for patients with limited-stage small cell lung cancer, but many patients have trouble coming to the hospital for radiotherapy two times
a day for three weeks. Only 15 percent of patients nationwide opt for twice-daily treatments, instead choosing a higher dose of radiation given once a day over seven weeks, not knowing whether it will be as effective.

Bogart’s trial showed no statistical difference in survival rates and outcomes.
Now that patients and doctors know both regimens can be associated with good outcomes, he says they have a real choice, “understanding that there may be some differences in side effects or their ability to complete the longer therapy.”
The next step in assessing the benefit of this treatment protocol is to look at subpopulations, for example, based on gender or age, says Bogart, who is a professor and chair of radiation oncology.
“The goal over time is to get away from the one-size-fits-all approach to offer better, more personalized therapy. The findings of this study move us in that direction.” u
Patients with small cell lung cancer (lower left) who came for radiation treatment (above) once daily were shown to have similar outcomes to those coming twice daily. Twice daily is difficult for many patients.
ABOUT 30,000 PEOPLE ARE DIAGNOSED WITH SMALL CELL LUNG CANCER EACH YEAR. THAT TYPE OF CANCER, WHICH IS TREATED WITH CHEMOTHERAPY AND RADIATION, ACCOUNTS FOR ABOUT 15 TO 20 PERCENT OF ALL LUNG CANCER PATIENTS, SAYS JEFFREY BOGART, MD, WHO CHAIRS UPSTATE’S DEPARTMENT OF RADIATION ONCOLOGY.
The typical adult colon, or large intestine, is 5 or 6 feet long. The last portion is called the rectum. A colonoscopy allows a doctor to look at the inside of the entire colon. Some polyps discovered during a colonoscopy can be removed immediately, by snipping them with a wire loop from inside the surgeon’s scope.
Many patients who are diagnosed with colon or rectal cancers have no symptoms. Some have vague complaints of abdominal pain, changes in bowel habits or blood in the stool, reports Upstate colorectal surgeon Kristina Go, MD.
Colorectal cancer is the second leading cause of cancer death in the United States. When it’s caught early, it can often be cured, she says.
Rates of colorectal cancer in people under 50 have doubled since 1990. That’s why men and women are now recommended to begin screening at age 45 — and even earlier if they have a family history of the disease.
Go answers five common questions related to colonoscopy, below:
Q.
A. I really want to look at the inner lining of the colon, called the mucosa. In order for a patient to have a clean colon, they literally need to flush out any kind of solid and liquid waste so that we can see the clean inside area.
A. In a normal colon, the inside lining is nice and smooth, and you can see the underlying blood vessels, and it can even look pretty shiny during a colonoscopy.
When I see a polyp, they usually look like little bumps, or they can almost look like little mushrooms. Polyps are abnormal clumps of cells. They can have the potential to grow into a cancer — which is why we get very excited about doing colonoscopies, to prevent them from turning into cancer — but you have some polyps that never turn into a cancer.
Experience and expertise can let us know which polyps look more suspicious.
A. It depends on the individual, and sometimes it can even be variable within the same person. On average, in a non-constipated patient, that transit time solely through the colon can take about 30 to 40 hours, and even going to 72 to 100 hours can still be considered normal. It can be variable in the same patient, based on how much physical activity they’ve had in the day, what kinds of foods they’ve had and whether they were more processed foods or more fluid and more whole grains.
And from patient to patient, it can also depend on any kind of medicines or underlying medical conditions they might have.
A. The osmotic laxatives doctors prescribe before colonoscopies are designed to hydrate and soften stool to unblock your system without harsh gastrointestinal side effects. Most patients are not fond of the taste, especially since they may have to swallow 64 ounces of prep fluid.
To help you drink that prep: Place your prep on ice. Drink it through a straw. Suck on lemon slices or sugar-free menthol candy
In the week prior to your screening test, avoid high-fiber foods — no leafy green vegetables, no beans, no fiber supplements — exactly the opposite advice I tell my patients for their colon health. After the colonoscopy, you should return to a high-fiber diet.
A. Stool-based tests that look for blood in your GI tract are pretty good at detecting cancers, but they provide no information about polyps. If you get a positive result from these tests, you’ll need a colonoscopy.
“Virtual” colonoscopy is a test that requires the same bowel prep. Then, instead of a camera scope in your colon, your colon is inflated with air, and you’re asked to move into several positions while computerized tomography images (CT, or CAT, scans) are made. Any polyps that are detected cannot be removed using this method, and if the doctor sees anything of concern, you’ll need a colonoscopy. u

THE



Prostate cancer screening usually starts when a man is in his 40s or 50s. It’s done through a blood test that measures for prostate specific antigen, or PSA. That’s an enzyme in the prostate that gets released into the bloodstream.
A man’s PSA level may fluctuate, and a high number does not necessarily mean cancer. A benign enlargement of the prostate, or an infection, can affect the PSA level.
“If we didn’t have prostate specific antigen, we’d be missing a lot of early cancers, and
we would only detect those that are already advanced,” says Gustavo de la Roza, MD. He is a professor and vice chair of pathology and the director of anatomic pathology at Upstate.
The prostate, part of the male reproductive system, is located just below the bladder and in front of the rectum. It produces the fluid that makes up part of the semen. Generally the prostate increases in size as a man ages. About one in eight men will be diagnosed with prostate cancer, which most commonly occurs in men 65 and older.
Prostate cancer is diagnosed through a biopsy of tissue from the prostate. A pathologist looks at the cells through a microscope. Cancer cells are larger, grow in a haphazard pattern and have certain distinguishing features.
A decade ago, when prostate biopsies included samples from six areas of the prostate, cancers were sometimes missed. De la Roza says modern prostate biopsies include samples from at least a dozen areas, including the periphery of the prostate, where cancer is more likely to be detected, so fewer cancers are missed.

Upstate urologists offer image-guided biopsies, also known as fusion biopsies. It’s a method of targeting a specific lesion in the prostate using ultrasound and magnetic resonance imaging.
The size of the tumor does not predict a prognosis. The Gleason score and tumor staging do.
The Gleason score — a 1 to 10 grade created in the 1960s by a doctor in Minnesota — remains the most reliable grading system, de la Roza says. It ranks cancers from least aggressive to most aggressive and weighs the risk of the cancer returning after surgery. Basically, the lower the Gleason score, the better.
Clinical staging uses medical images including MRIs and ultrasound.
The Gleason score, the staging, and the PSA levels combine to help urologists determine what treatment options are best for each patient.
A man who is diagnosed with a prostate cancer that is not aggressive or causing symptoms may opt for active surveillance, an aspect of care that de la Roza says has seen great advancements in recent years.
“It’s not just waiting for something to happen,” he explains. “You are actually actively watching the PSA and deciding when to biopsy again — and that is critical.” He says men in active surveillance receive regular PSA tests and may also undergo imaging and repeat biopsies. “If done this way, the likelihood of missing cancer is much lower.”
When prostate cancer is removed through surgery, pathologists like de la Roza examine tissue samples and report whether the cancer was confined to the prostate, spread to surrounding tissues or traveled to distant areas of the body.
This is called TNM staging —T stands for tumor, N for nodes and M for metastases — and it is used worldwide among medical providers who take care of cancer patients. u
Cancer cells are larger and more haphazard in appearance. Most prostate cancers arise from epithelial cells.

Two generic types of cells — stromal and epithelial — exist in healthy prostate tissue. The stroma includes smooth muscle cells, vascular cells, nerve cells and immune cell components. Some types of epithelial cells can acquire genetic mutations that transform them into cancer.


Cancer experts trumpet a 65% reduction in cervical cancer among 20- to 24-year-old women from 2012 to 2019. They were among the first group of 11- and 12-year-olds to receive vaccination against the human papillomavirus, or HPV.
HPV is the most frequent sexually transmitted infection in the United States. (Yes, more common than herpes or gonorrhea.) Without the protection of immunization, many individuals will acquire this infection at some point, says Manika Suryadevara, MD, a pediatric infectious disease specialist at Upstate.
More than 100 types of HPV exist, with more than 40 affecting the genital area, she says. The virus can cause genital warts, throat cancer, cervical cancer or other genital cancers.
HPV infection often occurs with no symptoms, so many people won’t know they’ve been infected.
The body’s immune system may be able to clear the virus, or the virus may quietly persist for years before developing a cancer.
Upstate gynecologist Allison Roy, MD, says sometimes the body clears the infection, but “we know that the longer the HPV stays around in the cervical cells, the more likely it is to cause dysplastic changes, or the precancerous changes that then go on to develop a cancer.”
Pediatricians offer the HPV vaccine to adolescents along with tetanus, meningitis and other standard vaccines. Suryadevara says, “By vaccinating boys and girls, you are protecting both genders from developing HPV-associated cancers later in life.”

The latest numbers from the American Cancer Society seem to show the vaccine is effective. u
Infants typically are vaccinated against the hepatitis B virus, which can be acquired through sexual transmission or contaminated blood products and leads to liver cancer.






















As marijuana becomes easier to obtain legally in New York state, more patients with cancer may turn to the drug to augment their treatment. Upstate radiation oncologist Karna Sura, MD — who has sometimes prescribed medical marijuana — goes over a few things to consider:

• While it has a reputation for creating euphoric feelings, marijuana can quell nausea and vomiting and stimulate the appetite. It may also help alleviate neuropathic (nerve-related) pain.
• Dispensaries have strict regulations, and their products are labeled with what percentage of cannabidiol, or CBD, and tetrahydrocannabinol, or THC, and other compounds they contain.
• Marijuana does not have to be smoked. Dispensaries typically have a variety of options, including powders and lozenges or other types of edibles.
• Purchases are cash only, and nothing is covered by health insurers, regardless of whether you have a prescription.
• Patients may fear addiction, although Sura says that is usually not a problem. “I counsel them to say that we want to put you on this to get you better so that you can do your normal activities, but then we will try to take it away, over time, so that you won’t be addicted.”
Sura is optimistic that more research will be done so that doctors will know which dosages to recommend and which types of products work better for which symptoms. u
How can you make today a more contented and peaceful day?
Kaushal Nanavati, MD, recommends belly breathing. He’s the director of integrative medicine at Upstate and the assistant dean of wellness.
For proper belly breathing, when you breathe in, the belly pushes out; when you exhale, the belly comes back in. And, you go slowly.
“Take a nice, deep inhaling breath, the longest inhale possible,” he coaches, “and take even longer to breathe out. Slowly, slowly, slowly.”
Taking time to breathe slowly and deeply helps break your pattern of thinking.
“As we start to get anxious, the emotions spiral. In our brain, the prefrontal cortex, which helps us with some of our logic, doesn’t get a chance to get activated,” Nanavati describes.
“When we take a deep breath, and we calm ourselves, that part of our brain can get engaged again. That helps us to use reason and logic and be able to think, ‘OK, in this situation, what is in my control?’
“We have good science behind this,” Nanavati says. “We know that with 10 minutes of nice, deep breathing”:

• Levels of cortisol, the stress hormone, drop. This not only helps reduce stress but can help prevent immune systems from weakening. Lower levels of cortisol also help control blood sugar and inflammation in the body.
Cortisol can also affect blood pressure.
• Levels of adrenalin, the “fight or flight” hormone, drop, which helps reduce anxious feelings.
• Levels of the hormone melatonin rise. This can help with sleep and in boosting the immune system.
• Levels of the chemical serotonin rise. This can enhance mood and help with gut motility (digestion).
• Levels of the chemical messenger dopamine rise, increasing our sensation of pleasure.
Researchers at Harvard University studied people who did belly breathing an average of
27 minutes per session, Nanavati says. Medical images of their brains revealed changes in density and blood flow over the course of eight weeks, which he says indicates focused breathing had a cellular impact.
Nanavati reminds people that “at any given moment, regardless of what we’re facing within us, we have potential to make a choice. That choice can be as simple as taking a nice slow, deep breath, which actually does have a calming effect.
“And that allows us to focus better and to redefine our purpose.” u

To date, no randomized controlled trials show that sugar causes cancer, says Katie Krawczyk, registered dietitian nutritionist at the Upstate Cancer Center. However, an indirect link exists between sugar and cancer. Eating a lot of high-sugar foods, such as cakes, cookies and sweetened beverages, can contribute to excess caloric intake. This may lead to weight gain and excess body fat.
Research has shown that being overweight or obese increases the risk of 11 types
of cancers, including colorectal, postmenopausal breast, ovarian and pancreatic cancer.
It is recommended to reduce added sugars, such as table sugar, honey, agave and maple syrup, Krawczyk says. Instead, consume nutrient-dense, high-fiber, complex carbohydrates, such as fruit, vegetables and whole grains, such as quinoa, wholewheat pasta and brown rice. u
Registered dietitian nutritionist Katie Krawczyk says this simple, creative take on ice cream, with no added sugars, can satisfy a sweet tooth.
INGREDIENTS:
4 bananas, peeled
PREPARATION:
Cut the peeled bananas into 2- to 3-inch chunks and place them in a freezer bag in the freezer for at least 6 hours. Remove and blend in a blender until smooth. Serve immediately or freeze in an airtight container for at least 2 hours. Scoop and serve.
NUTRITIONAL INFORMATION:
Each of 4 servings contains 110 calories, 1 gram protein, 28 grams carbohydrate, 15 grams naturally occurring sugar, 3 grams fiber and 450 milligrams potassium.
Impacting patient care, education, research and community health and well-being through charitable giving.

Psychologists say a “flashbulb memory” is a vivid, detailed snapshot of a consequential moment. For the Radel family of New Hartford, that moment was Aug. 26, 2021. That’s when they heard the words “Hodgkin lymphoma” applied to their otherwise healthy 17-year-old son, Luke.
Priorities shifted in an instant. College visits were replaced with chemo treatments. Senior portraits gave way to PET imaging scans. Instead of cross-country practices, Luke focused on clinical trials.
“When your child’s future is on the line, the questions are innumerous regarding treatment, symptoms, side effects, longterm effects — the list goes on. We were (and are) so grateful for the obvious skill and consideration the entire team at Upstate gave to our questions and to Luke’s treatment,” says Mary Radel, Luke’s mother. She had her own battle with lymphoma as a teenager.
She says the family relied on a supportive network of family and friends, along with the pediatric cancer care specialists at the Upstate Golisano Children’s Hospital — and the families they bonded with that were on similar journeys.

“Once you have slept by your child’s hospital bedside, you share a common experience that can be hard to describe, difficult to endure, impossible to forget,” Patrick Radel says.
Luke finished chemotherapy Feb. 4, 2022, and celebrated by ringing the bell at the Upstate Cancer Center. He’s a student at Syracuse University now.
“Just because I finished my battle with cancer in the medical sense does not mean that my struggle is over. Far from it,” he writes on a blog about his experience.


“In the 365 days since my bell-ringing moment, I’ve come to understand that the fight has only just begun.

“All my scans have been clear since May 2022, and my quarterly checkups with the fantastic oncology team at Upstate have all been positive. I am incredibly blessed to have made it one year out from the end of treatment, still in remission.”
The Radel family wanted to give back, by helping to improve the sleeping arrangements for parents staying overnight in the hospital with their child. They established the #LimeforLuke Pediatric Cancer Fund at the Upstate Foundation, because lime is the symbolic color for lymphoma awareness. Money collected will be used to make a child’s hospital room a more comfortable place for family members to rest and restore themselves as they provide reassurance to their child through the night.
A gift of gratitude is a meaningful way to express appreciation to caregivers and help patients during their time of great need. To donate, contact the Upstate Foundation at 315-464-4416 or go to upstatefoundation.org/donate


Emma Mollapour’s introduction to painting came when she was 2. “My parents, they put a canvas in front of me, and they covered my hands with paint,” she recalls. Mollapour, 11, has been painting ever since, though now she uses brushes more than her hands. She also likes sketching and watercolors.

Several of Mollapour’s works were on display at the Upstate Cancer Center during



the Kids Against Cancer event. One rectangle featured stars and stripes. A big green square held pine cones. An even larger blue square was the backdrop for red berries in the shape of a heart.
“The heart is my favorite shape,” she explains. “I really love love.”
Mollapour is glad to spread some happiness with her art. She’s a sixth grader who plans to become an actress. She appears as Maya on the local WCNY-TV/PBS series The


Reading League’s “Reading Buddies Season 2,” a fun, foundational series for kids about learning to read. Her parents are Upstate cancer scientists Mehdi Mollapour, PhD, and Dimitra Bourboulia, PhD.
Kids Against Cancer is a charitable organization that was founded in 1983 to provide holiday spirit to children hospitalized for cancer treatment. u


Emma Mollapour, 11, shows some of her artworks that were displayed for a Kids Against Cancer event at the Upstate Cancer Center. She used red berries to make a giant heart, left, and notes, “The heart is my favorite shape. I really love love.”

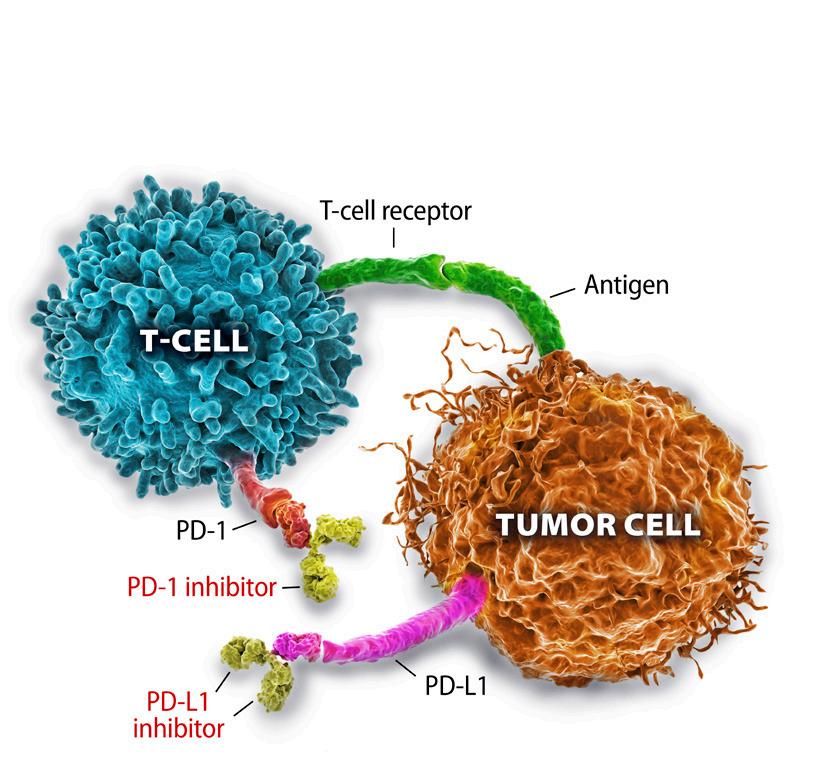
You may have seen advertisements for Keytruda and OPDIVO. These are nonchemotherapy options for treating cancer called immune checkpoint inhibitors. These two, plus several other checkpoint inhibitors, show tremendous promise.
Over a period of six months, these patients received the medication every three weeks. The caregivers at Memorial Sloan Kettering Cancer Center anticipated they would need chemotherapy, radiation and surgery— but they all had a complete response. Merima Ramovic, DO, from the Upstate Cancer Center explains that means there is no evidence of cancer after treatment with the immune checkpoint therapy.
Immune checkpoint inhibitors are a class of medications engineered to enable the body’s immune system to recognize the cancer cells and kill them. Cancer cells can find ways to turn off the immune system, and these drugs can prevent this from happening. Ramovic notes that these medications are generally well-tolerated by patients with relatively little impact on the quality of life in most cases. However, they cannot be used in patients with autoimmune conditions. Rarely, they can cause the immune system to go on a hyperdrive, causing autoimmune reactions as side effects.
Ramovic adds that this class of drugs has had utility in other cancers, including lung cancer and gynecological cancers. The National Comprehensive Cancer Network guidelines recommends checkpoint therapy use in several cancers. u
The immune system relies on immune checkpoints to prevent an immune response from being so strong that it destroys healthy cells in the body. Proteins on the surface of immune cells, called T cells, seek to connect with partner proteins on other cells, including tumor cells. When these proteins bind, they send an “off” signal to the T cells. This can prevent the immune system from destroying the cancer.
Immune checkpoint inhibitors are immunotherapy drugs that block checkpoint proteins from binding with their partner proteins, by blocking either the protein on the T cell or the tumor cell. This can prevent an “off” signal from being sent, allowing the T cells to kill cancer cells.
Source: National Cancer Institute