Angle-based Minimally Invasive Glaucoma Surgery (MIGS)
What is Angle-based Minimally Invasive Glaucoma Surgery (MIGS)?
Angle-based MIGS are procedures which enhance the natural outflow pathway of the eye, or the “angle” (Figure 1), where eye fluid normally drains out. This helps to reduce eye pressure.

These surgeries involve either the implanting of devices, or the removal of tissue from the angle of the eye.
In general, angle-based MIGS may not be as effective in reducing eye pressure as compared to traditional glaucoma surgeries or other forms of MIGS. However, they are less invasive procedures and also have a better safety profile. In addition, no anti-scarring medications are needed for these surgeries. Hence, there is no risk of side effects associated with these medications.
These surgeries may be performed alone, or in combination with cataract surgery. Your doctor will discuss the most suitable implant for your condition with you. Some examples of angle-based MIGS include the following:
iStent Inject
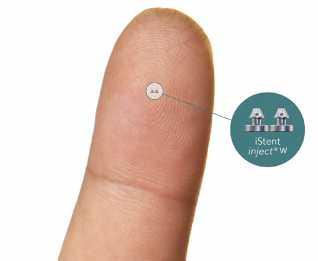
The iStent Inject system contains two stents which are 0.3mm long and made of lightweight titanium. The iStent Inject implants are inserted into the Schlemm’s canal, which is the natural drainage canal of the eye. It treats glaucoma by reducing the eye pressure by improving the drainage of fluid from the eye.
Hydrus Microstent
The Hydrus Microstent is a crescentshaped, implantable microstent made of nitinol (a metal alloy of nickel and titanium). Roughly the size of an eyelash, it is inserted into the Schlemm’s canal, which is the natural drainage canal of the eye. It treats glaucoma by reducing the eye pressure by improving the drainage of fluid from the eye.

iTrack Advance
The iTrack Advance is a device that enters the eye through a small cut at the edge of the cornea (the eye’s clear outer layer). It is an illuminated device used to dilate the drainage channel, called the Schlemm’s channel, and fluid collector channels. This procedure helps to reestablish the function of the eye’s natural drainage system. This is an implant-free procedure and hence not prone to problems of dislodged or blocked implants.
Why do I need this procedure?
Glaucoma is a disease of the optic nerve where the eye pressure is too high for the eye to remain healthy. If untreated, blindness can result from damage of the optic nerve. To lower the eye pressure, eye drop medications or a laser can be used. But when those measures are inadequate to lower eye pressure, it is sometimes necessary to undergo surgery.
If you are on glaucoma eyedrop medications and are undergoing cataract surgery, you may also be advised to undergo this procedure together with your cataract surgery, as this may help to reduce both your eye pressure and the number of glaucoma medications after surgery.
As with all glaucoma treatment, this surgery cannot cure glaucoma. It will not reverse any damage or vision loss already caused by glaucoma and is aimed at preventing your glaucoma from getting worse.
What precautions do I need to take?
Before surgery:
• Continue your glaucoma medications up to the day of surgery
• If you are on anti-platelet or anti-coagulant medication, you may have to stop these prior to surgery. Your doctor will advise you accordingly
After surgery:
• Use your eyedrops and other medications as instructed and attend eye reviews with your doctor as arranged
• Use an eye shield while sleeping for 3 weeks after surgery
• Avoid eye exposure to tap water for 3 weeks after surgery
• Avoid strenuous activities for 2 months after surgery
• Do not go swimming unless your doctor has informed you it is safe to do so
How is the procedure performed?
• The procedure is performed as a day surgery
• Usually, either local or regional anesthesia will be used to keep you comfortable. You will be lying on the operating table for 30 to 45 mins whilst the surgery is performed. The duration of the surgery will depend on which procedure you are undergoing and whether o you are undergoing cataract surgery in the same operation
• After the surgery, you will be monitored for 1 to 2 hours before being discharged home.
What are the risks and complications of the procedure?
Angle-based MIGS are less invasive procedures compared to traditional glaucoma surgeries and have been shown to have a better safety profile. However, the following are some examples of risks and complications which may still occur:
• Infection: Rare but treatable. However, severe infections may result in permanent visual loss
• Bleeding: In the front or rarely, at the back of the eye. Usually resolves with eye medications
• Low eye pressure: Less likely
• High eye pressure and glaucoma progression
• Wound leak
• Damage to the iris (muscle which controls pupil size)
• Cornea abrasion, swelling or decompensation
• Cataract formation, if not performed together with cataract surgery
• Loss of all remaining vision (“wipe-out”): Rare
• Droopy eyelid (ptosis)
• Inflammation
• Eye redness and discomfort
• Operation failure requiring further treatment in the form of eyedrops, laser or further surgery
• Device-related problems
• Malpositioning: Usually, no further procedures will be required
• Blockage by iris: Sometimes, further laser treatment may be required
• Dislocation or dislodgement: Very rare. Further surgery may be required
• Operation failure requiring further treatment
• Anaesthesia risk
• General anaesthesia –heart attack, stroke
• Regional anaesthesia –globe perforation, optic nerve injury, bleeding
What can I expect after the procedure?
• You can expect to be followedup closely for the first few weeks after surgery
• Your quality of vision may reduce or fluctuate for the first month, before stabilising. You may experience some eye discomfort and mild pain for a few days, but this should subside over a few days or weeks
• You will be given steroid and antibiotic eye drops to apply at home for approximately one month. The need for additional glaucoma eye drops will be advised by your doctor
• In general, after angle-based MIGS, you may expect a lower eye pressure. Your doctor may also reduce the number of longterm glaucoma eyedrops you are applying
• Your glaucoma condition may stabilise after the surgery
• However, depending on the condition of the eye, your recovery and the severity of your glaucoma, you may be required to restart one or more glaucoma eyedrops long-term
What are the other options?
• Conservative management with glaucoma eyedrop medications
• Laser procedures for glaucoma e.g. selective laser trabeculoplasty
• Other minimally invasive glaucoma surgical procedures
• Conventional glaucoma surgery, including trabeculectomy and tube implants
What will happen if I do not undergo the procedure?
• There is a risk of progressive vision loss or blindness if your eye pressure is not well controlled
• If you are on glaucoma medications and you are undergoing cataract surgery without this procedure, you may be required to continue the use of the glaucoma medications even after your cataract surgery
DISCLAIMER: This information sheet mentions some of the more common or important risks of surgery/ procedure. This list is NOT meant to be, and CANNOT be exhaustive.
Affix Patient Label
Name :
NRIC :
DOB :
Race :
Sex :
Case No :

This brochure was developed together with NHG Eye Institute partners.
Yishun Health is a network of medical institutions and health facilities of the National Healthcare Group in the north of Singapore. It comprises Khoo Teck Puat Hospital, Yishun Community Hospital and community extensions such as Admiralty Medical Centre and Wellness Kampung. Khoo Teck Puat Hospital • (65) 6555 8000 • www.ktph.com.sg Yishun Community Hospital • (65) 6807 8800 • www.yishuncommunityhospital.com.sg
The information is correct at the time of printing and subject to revision without further notice.
