Matters of your Heart
A guide in handling your heart attack



Heart attacks are often thought of as a sudden, pressure-like chest pain that takes a person by complete surprise. But heart attacks can have early warning signs, and often result from heart disease that builds up over time.
To prevent a heart attack, you need to know the risk factors that can lead to heart disease.
To survive a heart attack, you need to know the early warning signs.
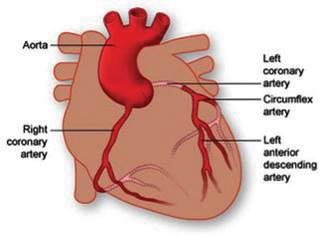
A heart attack occurs when a coronary artery suddenly becomes blocked, stopping the flow of blood to the heart muscle and damaging it. All or part of the heart muscle become cut off from its oxygen supply. Left without oxygen, the heart muscle is injured.
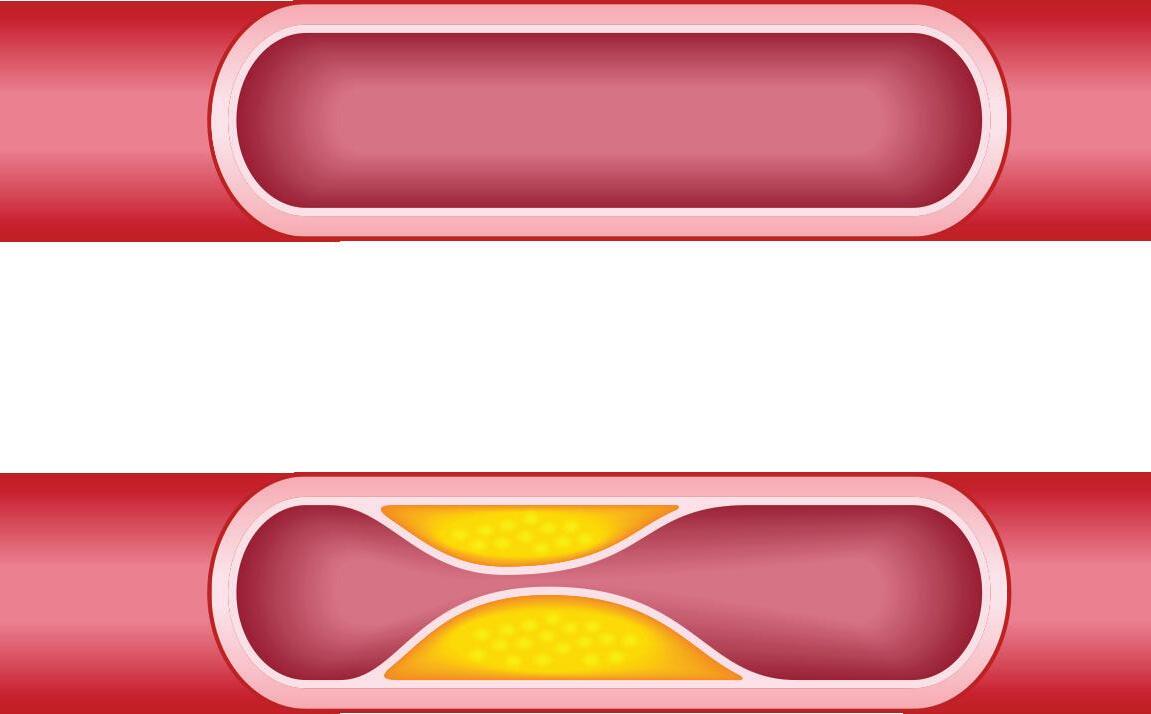
Coronary artery disease (CAD) is the leading cause of heart attacks. CAD is a condition in which coronary arteries (the major blood vessels that supply the heart with blood) get clogged up with deposits of cholesterol. These deposits are called plaques.
During a heart attack, one of the plaques ruptures (bursts), causing a blood clot to develop at the site of the rupture. The clot may then block the supply of blood running through the coronary artery, triggering a heart attack.
Risk factors for CAD, many of which are related to each other, are:
• Smoking
• High cholesterol level
• High blood pressure
• Diabetes mellitus
• Being overweight or obese
• Lack of exercise
• Family history of heart disease
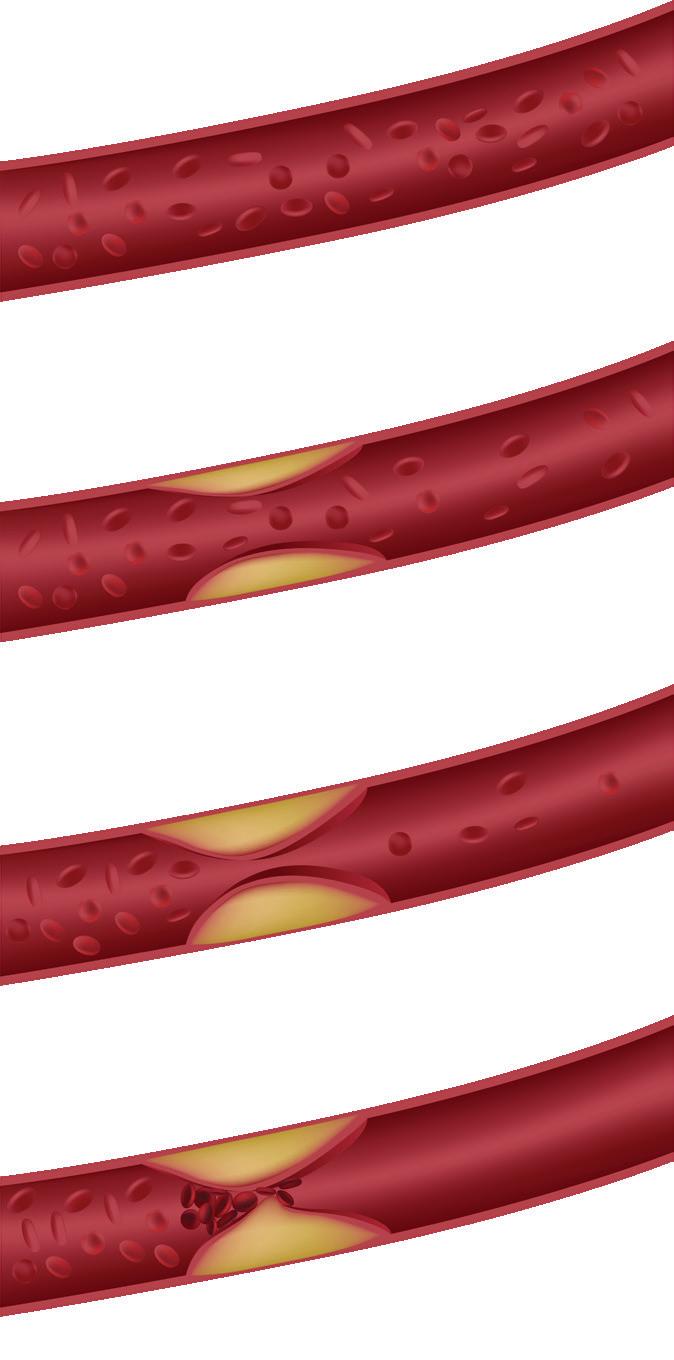
causing blood clots to form around the rupture, blocking the artery
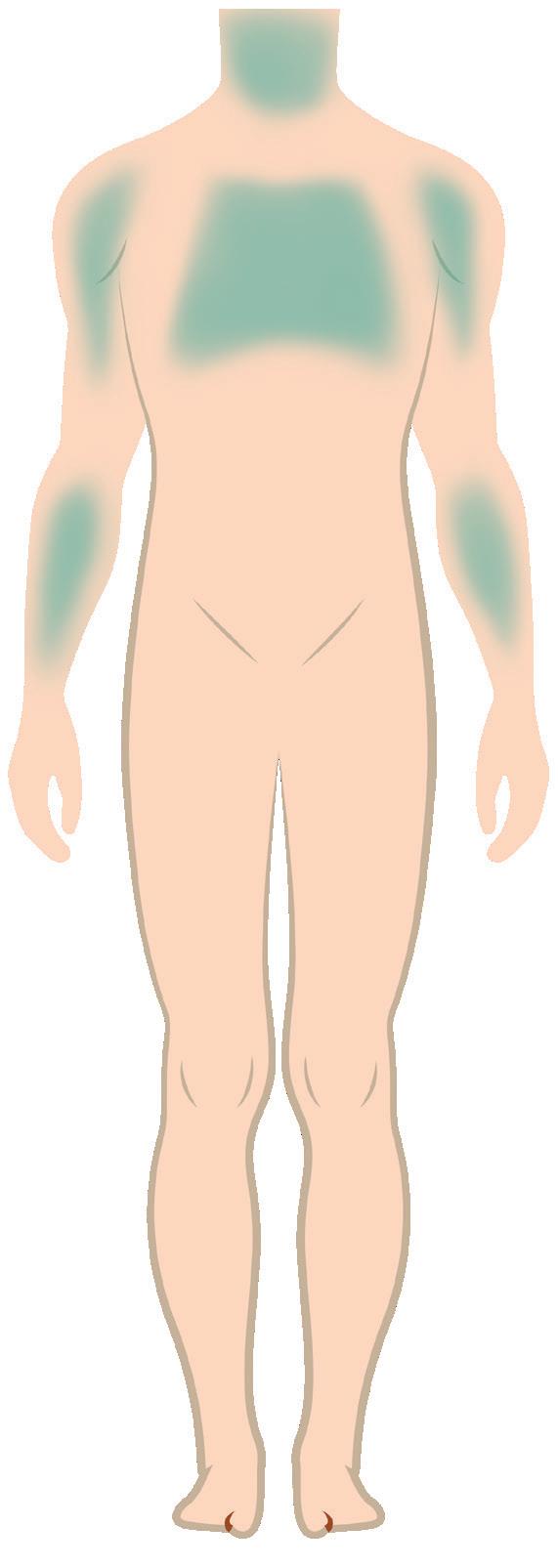
If you have any one of the symptoms described below that lasts for more than 5 minutes, seek emergency treatment (call 995) without delay. The following symptoms could be signs of a heart attack:
• Chest pain
• Discomfort in the centre of the chest, such as:
• heaviness
• tightness
• pressure
• aching
• burning
• numbness
• fullness or squeezing feeling that lasts for more than a few minutes or goes away and comes back. This can sometimes be mistaken as indigestion or heartburn.
• pain or discomfort in other areas of the upper body including the arms, left shoulder, back, neck, jaw, or stomach.
• Difficulty in breathing or shortness of breath
• Sweating or “cold sweat”
• Fullness, indigestion, or choking feeling (may feel like “heartburn”)
• Nausea or vomiting
• Light-headedness, dizziness, extreme weakness or anxiety
• Rapid or irregular heart beats
Once the emergency care team arrives, they will ask you about your symptoms and begin to evaluate you. The diagnosis of the heart attack is based on your symptoms, electrocardiogram (ECG) and the results of your blood tests.

ECG is a device used to record the electrical activity of the heart. It can help to tell how much damage has happened to your heart muscle and where it has occurred. In addition, your heart rate and rhythm can be monitored. You will also be connected with leads (wires) to a bedside monitor for continuous monitoring of your heart rate and rhythm.
Blood tests are necessary to determine the size of the heart attack and approximately when the heart attack started. As the heart muscles are injured, their contents – including the biochemical markers – are released into your bloodstream. Blood may be drawn to measure levels of biochemical markers. Those biochemical markers are called cardiac enzymes.

Echo is an ultrasound scan of the heart. It can be used during and after a heart attack to determine how the heart is pumping and identify areas that are not pumping normally. The echo also detects any injuries to the heart structure that could have occurred during the heart attack.

Cardiac catheterisation (also called cardiac cath) is an invasive imaging procedure that allows your doctor to:
• Evaluate or confirm the presence of blocked / narrowed arteries
• Determine the need for further treatment (such as ballooning and stenting procedures or coronary artery bypass surgery, CABG)
It may be performed urgently after a heart attack if medication failed to relieve the symptoms or if you are suffering from a large heart attack.
During a cardiac catheterisation, a long, narrow tube called a catheter is inserted into a blood vessel in your leg or arm. The catheter is guided through the blood vessel to the coronary arteries with the aid of a special X-ray machine. This is followed by injecting a contrast material (dye) so that it can be visualised in the X-ray.
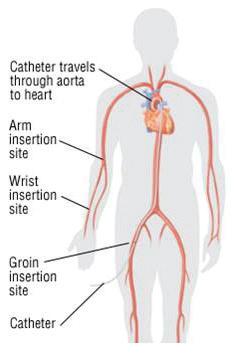
You may be given a mild sedative, but you will be awake and conscious during the entire procedure. The doctor will use a local anesthetic to numb the catheter insertion site. The procedure itself generally takes 30 minutes, but it may take longer (1 to 3 hours) if the ballooning and / or stenting procedure (Percutaneous Coronary Intervention) is performed after cardiac catheterisation.
Cardiac catheterisation is not considered a surgical procedure because there is no large incision to open the chest, and the recovery time is much shorter than that of a surgery.
Heart attack is treated using any one or a combination of the following methods:
1. Percutaneous Coronary Intervention (PCI)
2. Coronary Artery Bypass Surgery (CABG)
3. Medication
Percutaneous Coronary Intervention (also called coronary angioplasty) is a non-surgical treatment used to open narrowed coronary arteries to improve blood flow to the heart.
PCI can be performed during a diagnostic cardiac catheterisation when a blockage is identified, or it may be scheduled after a catheterisation has confirmed the presence of coronary artery disease.
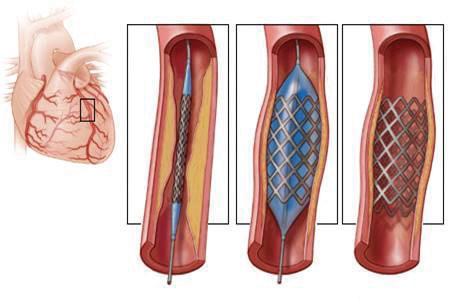
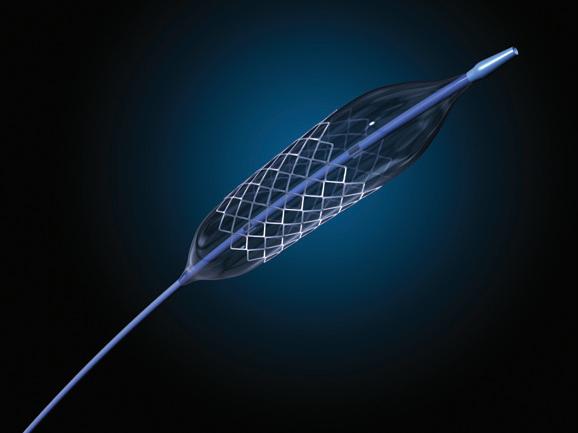
This procedure uses a flexible tube with a balloon at the tip. The tube is inserted into the affected coronary artery through your leg or arm.
Once in place, the balloon is inflated and it compresses the plaque against the artery walls (balloon angioplasty). The artery is widened and blood flow is improved. Often, a stent made of wire mesh, acting as a scaffold, will be inserted to keep the artery open.
Stents are metal mesh tubes inserted during angioplasty. Stents help prevent re-narrowing of the artery (restenosis). Without the use of stents, about 40 to 50 percent of arteries can become blocked again.
Difference between Bare Metal Stent (BMS) vs Drug-eluting Stent (DES)
There are two kinds of stents: bare-metal stents and drug-eluting stents. Bare-metal stents do not have special coating. They act as simple scaffolding to prop open blood vessels after they are widened with balloon angioplasty. As the artery heals, tissue grows around the stent holding it in place. However, sometimes an overgrowth of this scar tissue in the arterial lining increases the risk that the artery will become blocked again. Therefore, it is important not to miss your medication.
Drug-eluting stents are coated with medication that is slowly released overtime to help prevent the growth of scar tissue in the artery lining. This will reduce the risk of re-narrowing of the artery. However, depending on your condition, your doctor will select the stent that is most appropriate for you. People who have undergone PCI with or without stent placement will need to take 2 types of blood thinning medication (dual antiplatelet therapy - DAPT):
1. Aspirin - usually for life
2. Clopidogrel, Ticagrelor or Prasugrel — up to 1 year in duration
It is very important to follow your medication schedule as stopping medication early greatly increases the risk of the stent becoming blocked suddenly and causing another heart attack. Your doctor will advise you on the duration of dual antiplatelet therapy. Should you require surgery or invasive procedures, inform your cardiologist before stopping your medication.
Coronary bypass surgery is an open heart surgery. It restores blood flow to your heart muscle by diverting the flow of blood around the blocked artery.
Healthy blood vessels are taken from your leg, arm or chest abdomen and connects it to the other arteries in your heart so that blood bypasses the diseased or blocked area. After a coronary bypass surgery, blood flow to your heart will improve. Coronary bypass surgery is just one option to treat heart disease.
Coronary bypass surgery improves symptoms, such as chest pain and shortness of breath due to poor blood flow to the heart. In some situations, coronary bypass surgery may improve your heart function and reduce your risk of dying of heart disease.




































Treatment of coronary artery disease is aimed at controlling symptoms and slowing or stopping the progression of disease. In many cases, if the blockage is not severely limiting blood flow, medication may be the first line of treatment.
The medication you are prescribed are specific to you and your heart problem. It is important to know:
• The names and strength of your medication
• What they are for
• How often and at what times to take your medication
Your doctor or pharmacist should review your medication with you. Keep a list of your medication and bring them to each of your doctor visits. You can obtain the list of your medication from your pharmacist. If you have questions about your medication, ask your doctor or pharmacist.
Please always monitor for drug allergy or adverse reactions when you are taking medication that are new to you. Signs of drug allergy include swelling around the eyes, facial area, tongue or lips, difficulty in breathing and / or generalised rash all over the body. Please seek medical attention immediately if you experience any of the above.

The following medication are commonly prescribed.
Aspirin
Clopidogrel
Prasugrel
Ticagrelor
Reduce the risk of blood clot formation by preventing blood platelets from sticking together and causing another heart attack.

Lower blood pressure and make the heart beat more slowly and with less force, thus reducing the stress on the heart.
Helps to prevent / treat irregular heart rhythms and / or chest pain (angina).
Prevent future heart attacks and improve survival after heart attacks.
All antiplatelets can increase the risk of bleeding.
Nausea, stomach upset or heartburn. Always take aspirin after food to minimise these gastrointestinal side effects.
Prasugrel may cause diarrhea.
Ticagrelor can cause back pain, diarrhea, nausea, fatigue and headache.
Seek immediate medical attention if you experience bleeding symptoms e.g. unusual bruising, black tarry stools or blood in the urine. Do not stop your medication on your own.
If you cut / injure yourself, apply continuous pressure for 10 to 15 minutes. If bleeding does not stop, seek immediate medical attention.
Inform your healthcare provider or dentist if you are going for any surgery or dental procedure.
Other painkillers that contain NSAIDs (e.g. ibuprofen and naproxen) may cause bleeding problems when taken in combination with your antiplatelets. Consult your doctor or pharmacist before taking them.
Dizziness or light-headedness is common when you start taking a beta blocker or after an increase in dosage of your beta-blocker. However this is transient and can be minimised by rising slowly from a sitting or lying position.
Tiredness is usually temporary as your body needs time to adjust to the lower heart rate. Avoid doing intensive exercise or work when tired.
Other side effects include cold hands and feet, headache, nightmares, difficulty sleeping, nausea, heartburn, diarrhea or constipation, decreased libido.
Inform your doctor or pharmacist if side effects are severe or affecting your daily activity.
Take and record your blood pressure and heart rate daily. If your heart rate is slower than 50 beats per minute, contact your healthcare provider before taking your beta-blocker that day.
Angiotensin-Converting Enzyme Inhibitors (ACEI)
Enalapril
Lisinopril
Captopril
Perindopril
Expand blood vessels and improve blood flow, thus reducing blood pressure.
Enable the heart to pump against a lower resistance and thus reduce the workload of the heart.
Prevent “stiffening” of the heart muscle.
Improve survival in patients with heart failure and minimise kidney damage in people with diabetes.
Angiotensin II Receptor Blockers (ARBs)
Losartan
Valsartan
Telmisartan
Irbesartan
The ARBs help as the same way as the ACEIs.
It is usually prescribed to substitute ACEIs if you are unable to take an ACEI.
Dizziness or lightheadedness is common after the first few doses or when dose is increased. However this is transient and can be minimised by rising slowly from a sitting or lying position.
Persistent dry cough. Use hard candy (sugarless) to help moisten your throat and control the cough. If coughing prevents you from sleeping at night, is intolerable or severe, contact your cardiologist or pharmacist in-charge.
Hyperkalemia (too much potassium in the body) — signs of hyperkalemia include confusion; irregular heartbeat, numbness or tingling in hands, feet, or lips, shortness of breath or difficulty breathing, heaviness in legs.
The side effects are similar to ACEIs except ARBs are not as highly associated with dry cough.
You will need to have your blood pressure and kidney function checked regularly.
ACE inhibitor medication can cause the body to retain potassium. While taking an ACE inhibitor or ARB, avoid salt substitutes that contain potassium, like Pan salt® or Lo-salt®.
Contact your healthcare provider immediately if you experience swelling of your neck, face, tongue or lips.
NSAIDs like ibuprofen or naproxen may cause sodium and water retention, and decrease the effect of ACE inhibitors. Check with your doctor or pharmacist before taking any anti-inflammatory medication.
Simvastatin
Atorvastatin
Rosuvastatin
Lower low-density lipoprotein or LDL (”bad”) cholesterol and triglycerides, raise HDL (”good”) cholesterol.
Lowering LDL prevents fatty material from building up on the walls of your coronary arteries. This in turns helps to reduce the chances of a recurrent heart attack.
Long-acting Isosorbide Mononitrate CR Isosorbide Dinitrate
Quick-acting Sublingual Glyceryl Trinitrate (GTN) Tablets Spray
Dilate the heart arteries and veins throughout the body. This increases blood flow to the heart, relieving chest pain or discomfort (angina), and reducing the heart’s workload
Long-acting nitrates may be used for long-term prevention of chest pain during daily activities. Quick-acting GTN tablets and spray are quick-acting and help to relieve sudden discomfort.
Generally well-tolerated
Muscle aches, nausea, vomiting, diarrhea and abdominal pain. These side effects are usually mild and transient. You may try taking your statin after your dinner to minimise gastric upset.
Other rare but serious side effects include severe muscle aches, tea-colored urine, or yellowing of the eyes and the skin (jaundice). If you experience the above, please seek immediate medical attention.
Generally should be taken at night at dinnertime or bedtime.
Avoid taking grapefruit or its juice in large amounts as some statins (e.g. simvastatin) as it increases the risk of side effects.
Avoid alcohol as it may increase the risk of liver damage when taking statins.
Seek immediate medical attention if you experience general muscle aches.
Headache
Flushing
Lowers blood pressure and thus cause dizziness.
How to take quick-acting GTN tablet / spray
Place the GTN tablet under your tongue. Leave it there until it dissolves. If you accidentally swallow the tablet, take another.
The medicine won’t work if it is swallowed.
GTN Spray - Spray under your tongue by pushing the spray canister button. Close your mouth right away.
Take one tablet or spray dose. If after 5 minutes the chest pain is not better or gets worse, call 995 immediately.
Inform your doctor or pharmacist if side effects are severe or affecting your daily activity.
Do not take the erection-enhancing medicine sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis) if you are taking a nitrate. Combining these two drugs can cause a life-threatening drop in blood pressure.
Carry sublingual GTN everywhere you go.
Once the container of GTN tablets is opened, GTN tablets must be replaced every 8 weeks. GTN spray can be kept and used until expiry date.
What you can expect when you return home
Returning home after a heart attack can be frightening. This section talks about early recovery, including:
• activity
• feelings
• diet
• sexual activity
Keep in mind it may take up to two months for your heart to heal.
You may feel tired or weak during the first week after you return home. This may be due to damage to your heart muscle, prolonged bed rest you had in the hospital or side effects from the medication.
• Getting back into a normal routine will help in faster recovery. You should be able to take care of all your personal hygiene (bathing, shaving, dressing).
• Pace yourself. Spread your activities throughout the day. If you become tired, rest and schedule unfinished activities for another day.
• You may climb stairs at home as part of your daily activity, unless your doctor has told you not to. Try to arrange your activities so that you do not have to climb up and down stairs several times during the day.
• Walk every day as prescribed by your doctor. A regular walking programme is a good way to regain your energy
• When you feel stronger, you may return to light household chores, such as folding clothes, cooking, light gardening, dusting and washing dishes.
• Do not lift, push or pull very heavy objects until your doctor tells you that you may do so.
• Your doctor will advise you when you can return to work (usually 2 to 4 weeks after your heart attack), drive a car and begin more vigorous activity.
About one in four patients feel depressed, angry and afraid after a heart attack. These are normal responses that usually go away with time, as you get back to your regular activities. To help relieve the emotional blues:
• Do not stay in bed all day.
• Get out and walk daily. This will help you maintain a healthy mind and body.
• Resume hobbies and social activities you enjoy.
• Share your feelings with your family, a friend, a clergyman, or support group.
• Get a good night’s sleep. Lack of sleep can cause you to feel tired or irritable. Be careful not to nap too much during the day, or you will not be able to sleep at night.
• Limit visits with friends and family at first, to avoid feeling over-tired. Increase these activities gradually, depending on how you feel. With time, these visits can be helpful to lift your spirits.
• Join a cardiac rehabilitation programme. It not only provides you with a guided activity and education programme but will also offer a network of emotional support.
• If you do not feel your emotions improving or are feeling depressed, call your doctor. Medication and counseling can help you through this period.
Eating a heart healthy diet is essential to prevent future complications of heart disease.
1. Cut down on total fats, especially saturated fats and trans fats. Replace your intake of saturated fats with unsaturated fats. Example: switch your vegetable oil to heart-friendly oils such as canola, sunflower, corn or olive oil.
2. Limit excessive intake of dietary cholesterol. Example: internal organs, seafood and egg yolk.
3. Increase your dietary fibre, especially soluble fibre. Example: oats, wholegrains, brown rice, legumes, fruits and vegetables.
4. Reduce your intake of refined sugars. Example: from sweetened beverages, cakes and pastries.
5. Limit salt intake. Example: ask for less sauces and gravy, avoid preparing food with excessive salt, stocks and sauces.
6. Reduce alcohol intake.
Sexual activity can usually be resumed shortly after leaving the hospital. The amount of energy it requires to perform intercourse is similar to climbing about one or two flights of stairs or walking about one-half mile (0.8 km) at a brisk pace. If you cannot perform these activities without getting chest pain, shortness of breath, or becoming over-tired, please discuss this with your doctor before resuming sexual activity.
How you can prevent heart attacks from reoccurring
The goal after your heart attack is to keep your heart healthy and reduce your risks, to prevent future damage to your heart.
1. Take your medication
2. Cardiac rehabilitation
3. Change your lifestyle
4. See your doctor for regular heart checkups
1. Take your medication
Medication are prescribed after a heart attack to:
• prevent future blood clots especially after an operation (CABG or PCI)
• lessen the work of your heart and improve your heart’s performance and recovery
• lower cholesterol level
It is important that you take your medication as instructed. Your doctor or nurse should review your medication with you. Keep a list of your medication and bring them to each visit to your doctor.
2. Cardiac rehabilitation
After a heart attack, a cardiac rehabilitation programme provides a medically supervised setting to help you recover from your heart attack, learn about your heart disease, and learn strategies to change your lifestyle to prevent further progression of your disease.
Cardiac rehabilitation (rehab) has many benefits. It can:
• Reduce your overall risk of dying, the risk of future heart problems, and the risk of dying from a heart attack**
• Decrease pain and the need for medicines to treat heart or chest pain
• Lessen the chances of readmission to the hospital or emergency room for a heart problem
• Improve your overall health by reducing your risk factors for heart problems
• Improve your quality of life and make it easier for you to work, resume social activities and exercise
Going to cardiac rehab regularly can also reduce stress, improve your ability to move around, and help you stay independent.
** Studies show that individuals who had undergone cardiac rehabilitation reduced all-cause mortality (risk of dying) by 27%, cardiac death (heart-related death) by 31%
3. Change your lifestyle
There is no cure for coronary artery disease. In order to prevent the progression of this disease, you must follow your doctor’s advice and make necessary lifestyle changes:
a. Stop smoking
The toxins in cigarettes narrow and damage heart arteries. This makes smokers more vulnerable to CAD. Compared with nonsmokers, people who smoke 20 or more cigarettes a day are 60 to 90 percent more likely to develop CAD and have a heart attack.
Even small amounts of tobacco can be harmful. If you smoke only one cigarette a day, you are still 30 percent more likely to develop CAD than a non-smoker. Do obtain an appointment with our Smoking Cessation Clinic for assistance by calling the hospital hotline.
b. Lower high blood cholesterol / diet
A high-fat diet can contribute to increased fat in your blood. Follow a low-fat, low-cholesterol eating plan. When proper eating does not control cholesterol levels, medication is prescribed.
c. Control high blood pressure
Poorly controlled blood pressure can weaken the coronary arteries, making them more vulnerable to CAD. The higher your blood pressure, the greater your risk of CAD and heart attacks. A healthy diet, exercise, medication and low salt intake can help control high blood pressure.
d. Maintain tight diabetes control
The increased levels of blood glucose associated with diabetes can damage the coronary arteries, making them more vulnerable to CAD. It is estimated that people with diabetes are two to five times more likely to develop CAD than the general population. If you have diabetes, it is important to control high blood sugar through diet, exercise, and medication.
e. Follow a regular exercise plan
Lack of exercise may double a person’s risk of developing and subsequently dying from cardiovascular disease. This is because a person who leads a sedentary lifestyle is more likely to become overweight and / or have high blood pressure, diabetes, and high LDL cholesterol. All these factors adversely affect one’s heart health.
A regular exercise programme helps you regain or maintain your energy level, lower cholesterol, manage weight, control diabetes and relieve stress. Check with your doctor first before beginning an exercise programme.
f. Achieve and maintain your ideal body weight
Obesity is defined as being very overweight. When you are very overweight, your heart has to do more work, and you are at increased risk of high blood pressure, high cholesterol levels and diabetes. A healthy diet and exercise programme aimed at weight loss can help improve your health.
Controls stress and anger
Uncontrolled stress or anger is linked to increased coronary artery disease risk. You may need to learn skills such as time management and relaxation to help lower your stress levels.
4. See you doctor for regular heart check-ups
You will be given a follow-up appointment with your doctor after your discharge. Do not miss your appointment. If you have rescheduled your appointment, please ensure you have enough medication. You can call the hospital hotline or the Cardiac Clinic at C53 to obtain a prescription. Do give us at least 3 days to process.
What should you do if you have chest pain or a suspected heart attack?
If you feel discomfort, pressure, heaviness or pain in the chest, back, jaw, throat or arm similar to your heart attack.
You must:
• Stop your activity. Sit down and rest.
• If you have GTN, place 1 GTN tablet under your tongue and let it dissolve, or spray the GTN under your tongue.
• Wait 5 minutes.
• If you are still experiencing angina after 5 minutes, call 995 to get emergency help. DO NOT DELAY.
• Do not drive yourself to the hospital. In many cases, the emergency personnel can begin to give you heart-saving care right away.
• To prevent damage to your heart muscle, do not delay seeking medical treatment.
Sudden cardiac arrest is the unexpected loss of heart function, breathing and consciousness. The heart pump stopped pumping blood to the rest of the body.
Sudden cardiac arrest is a medical emergency. If not treated immediately, it causes cardiac death. With fast, appropriate medical care, survival is possible. Administering cardiopulmonary resuscitation (CPR) can improve the chances of survival until emergency personnel arrive.
Patients with history of heart attack have higher risk of such events therefore family member are encouraged to learn about CPR.
There are such courses conducted in Singapore Heart Foundation. You can visit their website for more information: www.myheart.org.sg
Khoo Teck Puat Hospital • (65) 6555 8000 • www.ktph.com.sg
Yishun Community Hospital • (65) 6807 8800 • www.yishuncommunityhospital.com.sg
The information is correct at the time of printing and subject to revision without further notice.