ISSUE 2 : Apr–jun 2025


ISSUE 2 : Apr–jun 2025


10 COVER STORY
Matters of the Heart: Transforming Cardiac Care
92-year-old Mr Wee shares how his apprehension became assurance under the Cardiology team’s care
4
8
A roundup of KTPH and YCH appearances in the media
16 SPOTLIGHT
Into the MIST: Advancing Urological Care
KTPH’s Urology department is transforming treatment options for patients, making advanced urological care more accessible
20 EAT WELL
Eat Your Way into Strength
Eat better to prevent muscle loss as we age
Part 2 of 2

22 LIVE WELL
A Lifelong Quest for Scientific Truth
A/Prof Lim Su Chi’s passion for research and purpose for medicine keep him young at heart
In this second instalment of our series on KTPH’s efforts in enhancing patient care and partnering patients in the pursuit of health, we showcase how innovations in cardiac care are helping patients recover better and live well. This is exemplified through the journey of an inspiring 92-year-old who reminds us that age is no barrier to an active, healthy life.
After 14 years of bringing inspiring stories and health knowledge to you, our dear readers, this chapter of aha magazine will be coming to a close, with this being our last issue. Thank you for all your encouraging feedback over the years that have inspired us to put our best into each issue! Don’t worry, this is ‘see you again’, not ‘goodbye’! Sign up using this QR code to receive our future articles digitally!

26 5 THINGS ABOUT… Wound Care
Taking care of wounds correctly prevents scarring and reduces infection risks
28 DAILY DOSE
Need Help with Knee Pain?
Understand knee pain to take steps toward better mobility
30 MAKAN TIME
Spaghetti Aglio Olio with Anchovies and Salmon
This dish provides 40% of the daily nutritional
We are a network of medical institutions and health facilities of the National Healthcare Group in the north of Singapore. We care for patients in Khoo Teck Puat Hospital, Yishun Community Hospital, and our community extension, Admiralty Medical Centre.
Benny Tan
Nur Amalina
Hannah Wong
Jack Lau
Sharon Ng
Albert Foo
The editorial committee — made up of clinical, nursing, allied health, and administrative heads of department — advises aha’s direction.
A/Prof Tan Kok Yang
Fatimah Moideen Kutty
Shirley Heng
Teresa Foong
www.ktph.com.sg/ about-us/media/publications aha@ktph.com.sg

THINKFARM PTE LTD www.thinkfarm.sg
MANAGING DIRECTOR
Christopher Tay
CONTRIBUTING EDITOR
Sheralyn Tay
HEAD, CREATIVE Lee Lily
HEAD, CLIENT RELATIONSHIP
Jessie Kek
CONTRIBUTORS
Justin Loh, Yong Ruey Teng
ha is the official quarterly publication of Khoo Teck Puat Hospital (Co. Reg. No. 200717564H) and is produced by ThinkFarm Pte Ltd. All rights to this publication are reserved and no part may be reproduced without the express written consent of the publishers. While every effort has been made to ensure that the information in this newsletter is accurate and up to date, the editorial team will not be responsible for errors due to information received. Opinions expressed are that of the writers and do not necessarily represent the views and opinions of the publishers. Printed by Mainland Press Pte Ltd. MCI (P) 054/06/2024
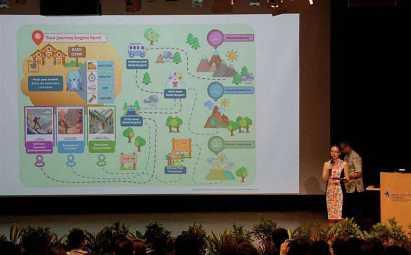
From artificial intelligence predicting patient needs and virtual reality-based medical training to robotic assistants in the surgical theatre. Science fiction was brought to life at our inaugural One Improvement Festival 2025.
Held from 17 to 21 February, the week-long festival showcased the future of healthcare and a thrilling glimpse into healthcare’s AI-powered future – all intending to foster a culture of continuous improvement. The festival kicked off with external educational visits and on-site learning opportunities, providing diverse experiences for participants, and culminated in a vibrant celebration at the KTPH auditorium on 19 February.
The festival saw the launch of CHI@KTPH & YCH, a collaboration between Khoo Teck Puat Hospital (KTPH), Yishun Community Hospital (YCH), and the Centre for Healthcare Innovation (CHI). This initiative brings together expertise across institutions to strengthen capabilities, foster innovation, and support meaningful improvements in patient care. CHI@ KTPH & YCH will explore areas like AI-


driven analytics, virtual reality training, and robotics-assisted surgery to enhance care and efficiency.
The highlight of the event was the award ceremony, where we

celebrated individuals and teams for their exceptional work in improving quality and safety, processes and service delivery. Awards were also given out to staff to recognise their



contributions to KTPH and YCH in its innovations and patient care.
The festival foyer buzzed with excitement as attendees explored interactive booths showcasing NHG’s Health Empowered by AI Launchpad (HEAL) initiative, experienced the CHI Virtual Reality Lab, and discovered the VELYS robot assistant that enhances surgical precision in joint replacement procedures.
As part of the festival, our colleagues visited various innovation partners, learning about emerging technologies focused on healthcare challenges at Nanyang Polytechnic, cutting-edge automation solutions in food technology employed at SATS, and advanced automotive manufacturing processes and electric vehicle development at the Hyundai Motor Group Innovation Centre Singapore.
The One Improvement Festival 2025 has set the stage for a year of innovation and continuous



Through months of planning and coordination, the One Improvement Festival organising committee successfully curated meaningful innovation experiences for all staff
improvement at KTPH and YCH. Staff are encouraged to embrace the spirit of innovation in their daily work, continuously imagine new
possibilities for better patient care, collaborate across disciplines and institutions, and create solutions that make a tangible impact.

Organised by KTPH’s Clinical Research Unit, the Research & Innovation Day - held as part of the One Improvement Festival –brought together over 200 staff members to explore new frontiers in healthcare research on 21 February.
The event, themed ‘Research & Innovation for Better Care – Onwards to New Frontiers’, showcased our commitment to enhancing patient care through innovative approaches.
In his welcome address, CEO Prof Chua Hong Choon highlighted KTPH’s partnership with NTU and Lee Kong Chian
School of Medicine to develop a robust Academic Health System that fosters education and research. Prof Benjamin Seet, NHG Group Chairman Medical Board (Research), noted that 2024 was an outstanding year for research at NHG, marked by significant collaborative grants and recognition of clinician-scientists.
The event also featured a keynote address by Prof Joseph Sung, NTU Senior Vice President (Health & Life Sciences) and LKCMedicine Dean. He emphasised the importance of research-driven hospitals and encouraged identification of

knowledge gaps and collaboration.
A panel discussion followed, where the research and innovation leaders of NHG and LKCMedicine discussed how research collaboration between our two institutions has enhanced patient care. They also addressed the challenges of balancing research and clinical duties.
The day was also a celebration of our research achievements, with an exhibition showcasing various projects, studies and work, inspiring attendees to contribute to improving healthcare outcomes through research and innovation.

From milestones to everyday moments, connect with us online for regular updates, inspiring achievements and a touch of fun.
Scan below to connect!






FACEBOOK INSTAGRAM TIKTOK LINKEDIN
Khoo Teck Puat Hospital • Yishun Community Hospital
For years, Han Xueli struggled to manage her high cholesterol despite following a strict diet and medication regimen. The answer came when she discovered she has Familial Hypercholesterolemia (FH), a genetic condition that causes abnormally high cholesterol levels from birth and significantly increases the risk of heart disease. Unlike lifestyle-
Scan to learn more about FH and genetic testing.

related high cholesterol, FH runs in families - when one member has it, their relatives face a 50% chance of sharing the condition.
Through genetic testing at Khoo Teck Puat Hospital’s FHCARE programme, led by Dr Sharon Pek, Han received her diagnosis, enabling better management of her cardiovascular health.

Two of Khoo Teck Puat Hospital’s innovative non-drug therapies – the “Garden by the Bed” project, which brings nature to patients’ bedsides, and the “Crochet for a Good Cause” staff volunteer group, which crafts knockers for post-mastectomy breast cancer patients – were featured in a Lianhe Zaobao interactive article.
The feature highlighted how local hospitals are using creative approaches to enhance patients’ mental well-being during physical recovery. These personalised therapeutic initiatives are part of a broader holistic healing movement, bringing warmth and hope to patients.

Scan to learn more about these inspiring initiatives across Singapore’s hospitals.

Late-life depression affects about 5.5% of Singapore’s elderly population, yet many suffer in silence. While commonly associated with sadness, it often manifests differently in seniors – through memory loss, withdrawal from activities or physical illnesses. The condition frequently goes undiagnosed as symptoms can mimic normal ageing.
In this commentary, A/Prof Ng Chong Jin, head and senior consultant of the geriatric medicine department at Khoo Teck Puat Hospital, explains how families can recognise the signs and support elderly loved ones to ensure they receive the help they need.
Scan to learn more about the risk factors for late-life depression.


Launched in 2019, KTPH@Home brings acute medical care to patients in the comfort of their own homes, empowering both patients and caregivers to take a more active role in the recovery process.
Follow us on Facebook & Instagram! f @khooteckpuathospital
Join us as we follow Irfan, one of our dedicated KTPH@Home nurses, on his daily rounds to see how hospital-level care can be delivered right to your doorstep.

Scan to watch the video.

When it comes to matters of the heart, timely intervention and the right care approach can make all the difference. At KTPH’s Cardiology department, enhanced care pathways and innovative monitoring solutions are helping patients recover faster and live better, while building partnerships that last beyond the hospital stay.
At 92, Mr Wee Sek Kay maintains an impressive fitness routine, hitting the gym three times a week for hour-long sessions that would tire many people half his age. But this wasn’t always guaranteed. Last September, during one of his regular workouts, he noticed something wasn’t quite right.
“Every time I went on the treadmill or cycling, I became unusually short of breath,” he recalls. He knew something was amiss as someone who has always been highly attuned to
his body’s performance. A visit to his family doctor led to an immediate referral to KTPH’s Acute & Emergency Care, where tests revealed cardiac irregularities.
Under the care of Head and Senior Consultant Dr Patrick Lim and the cardiology team, Mr Wee underwent an angiogram that revealed several blocked arteries requiring stents. “The team was so cheerful and encouraging,” he shares. “When you first have heart problems, you think the worst. But their positive attitude made a real difference – I felt I was in good hands.”



Mr Wee maintains a balanced routine of cardio, strength training, and his signature hour-long stretching routine
Mr Wee’s experience reflects the Cardiology department’s commitment to treating heart conditions and ensuring patients can return to their daily lives as quickly as possible. “We constantly seek ways to improve patient flow and reduce hospital stays while maintaining the highest standards of care,” explains Dr Lim.
One significant advancement has been the introduction of sameday discharge for eligible patients.

“The team was so cheerful and encouraging. When you first have heart problems, you think the worst. But their positive attitude made a real difference – I felt I was in good hands.”
Mr Wee Sek Kay
Common signs of heart problems to watch for:



Chest pain or discomfort lasting more than 15 minutes
Unexplained shortness of breath Unusual fatigue during normal activities
Note: Women and diabetic patients may experience different symptoms
Pain in arms, neck, or jaw
Seek immediate medical attention if you experience these symptoms, especially if you have:
Family history of heart disease
Remember, early intervention can make a significant difference in outcomes!
“Our role extends beyond performing procedures. We work with patients to understand their goals and help them achieve the best possible quality of life.”
Dr Patrick Lim Head and Senior Consultant cardiology, KTPH
Those undergoing planned procedures, such as angioplasty or pacemaker generator replacements, can often return home on the same day, in contrast to the previous standard of two to three days in hospital.
The department has also embraced technology to enhance post-procedure care. Patients with cardiac devices may be offered remote monitoring services, where their devices sync with transmitters that send data directly to the care team. “This allows us to detect any issues early and reduce unnecessary clinic visits,” Dr Lim explains. “If we spot any concerning

patterns, we can proactively contact patients to come in earlier for a review.”
For Mr Wee, the care he received went beyond just treating his heart condition.
The team supported his desire to return to an active lifestyle, guiding him to resume his exercise routine
safely. Starting with light activities, he gradually built his fitness back to his previous level. “Three months later, I’m back to about 80% of my usual routine,” he says proudly.
This partnership approach to care is central to the department’s philosophy. “Our role extends beyond performing procedures,” says Dr Lim. “We work with patients to understand their goals and help
them achieve the best possible quality of life.”
This focus on patient well-being has led to enhanced rehabilitation programmes and closer collaboration with primary care providers, ensuring continuity of care even after patients leave the hospital. The department is also working to expand its network of care partners, making it easier for patients to access cardiac services closer to home.
Today, Mr Wee continues his thriceweekly gym sessions. He maintains a balanced routine of cardio, strength training, and his signature hour-long stretching routine –a habit from his tennis coaching days that has served him well. His story serves as inspiration that with the right medical care and personal determination, age need not be a barrier to an active life.
“Listen to your body, and don’t delay seeking medical help when something feels wrong,” he advises. “With good doctors and a positive attitude, you can overcome many health challenges.”
As healthcare continues to evolve, KTPH’s Cardiology department remains committed to enhancing care delivery through innovation while maintaining what matters most – the human touch that helps patients feel supported on their journey to recovery.
Started in 2012, KTPH’s Cardiovascular Centre (CVC) has been at the forefront of cardiac care in northern Singapore. What began as a mission to provide accessible, high-quality cardiac services has grown into a comprehensive centre of excellence, operating around the clock to serve patients experiencing heart emergencies.
The centre has seen remarkable growth; the number of cardiac procedures rose from 14,887 in 2019 to over 17,000 in 2024. This 14% increase reflects not just Singapore’s ageing population’s growing needs but also the community’s trust in the CVC’s services.
To keep up with demand, CVC recently upgraded its facilities with a new angiography system in its newly renovated Angiogram Suites. This advanced technology represents a significant step in cardiac care and patient safety, providing crystal-clear, real-time images while minimising radiation exposure. The system’s faster image acquisition means procedures can be completed more quickly, reducing the time patients spend on the treatment table. The new system integrates seamlessly with the CVC’s existing infrastructure, ensuring it can continue to deliver efficient, high-quality care to more patients well into the future.
Importantly, the CVC’s 24/7 emergency angioplasty service means heart attacks are treated quickly – because in cardiac emergencies, every minute counts.
To find out more about our Cardiology department and non-invasive tests that can be done for your heart, scan this QR code:


Beyond the general urology capabilities of the KTPH Urology department, patients receive care from specialists trained specifically in their condition
KTPH’s Urology department is transforming treatment options for patients, making advanced urological care more accessible, even for those previously considered high-risk, through innovative minimally invasive procedures and a comprehensive team-based approach.
For 85-year-old Mr Chen*, what began as a memorable family holiday turned into an unexpected medical emergency when he suddenly found himself unable to pass urine. Unknown to him, he had developed benign prostatic hyperplasia (BPH) – a common condition where the prostate gland becomes enlarged. For him, the condition caused his prostate to press against his urinary tract, restricting urine flow.
After requiring an urgent catheter insertion abroad and cutting his journey short, Mr Chen returned to Singapore to face a challenging situation: his enlarged prostate needed treatment, but his heart condition made him a high-risk candidate for traditional surgery under general anaesthesia.
His surgeon, Dr Lau Weida, Head and Senior Consultant, Urology, notes that such a scenario is common. “About 20% of our patients first come to us during a crisis, rather than through regular clinic visits for
early symptoms,” he says. “Many brush off urinary problems as a normal part of ageing, but this can lead to emergency situations that are more complicated to manage.”
Fortunately for Mr Chen, recent advancements in Minimally Invasive Surgical Therapy (MIST) at KTPH’s Urology department offered him a solution that would have been impossible just a few years ago. Under local anaesthesia and light sedation, he underwent water vapour ablation therapy. This procedure uses precisely controlled steam to reduce prostate tissue, which reduces pressure on the urinary tract and allows the channel to reopen.

“While traditional prostate surgery requires general anaesthesia and carries risks of bleeding, this new approach allows us to treat even high-risk patients safely,” Dr Lau explains. In some cases, the procedure can even be done with just a local anaesthetic without sedation.
*Name changed for privacy.
And because it is minimally invasive, the operation and recovery time are shorter. Patients can also usually go home the day of the procedure.
The department’s adoption of MIST represents a significant leap forward in urological care. Since 2021, they have performed over 60 such procedures using two main approaches: water vapour ablation and prostatic urethral lift.
The latter involves placing small implants that lift and hold the enlarged prostate tissue away from the urethra, creating a clear channel for urination. These techniques
“Many brush off urinary problems as a normal part of ageing, but this can lead to emergency situations that are more complicated to manage.”
DR LAU WEIDA HEAD AND SENIOR CONSULTANT, UROLOGY, KTPH
have shown remarkable success, with 80-90% of patients able to discontinue their medications completely after treatment.
For Mr Chen, though it took about two months before he could be catheter-free, he felt it was worth the wait. “He understood that healing would take time,” Dr Lau shares.
“The important thing was that we could offer him a safe treatment option that worked with his medical conditions, not against them.”
These new treatment options are transforming care not just for elderly or high-risk patients but also for younger individuals seeking alternatives to long-term medication.

Traditional medications for prostate conditions often come with unwanted side effects, from postural hypotension (a form of low blood pressure) to sexual dysfunction.
“Younger, well-educated patients often come to us specifically seeking alternatives to chronic medication,” Dr Lau notes. “They prefer a one-time procedure with minimal downtime that can free them from daily medications and their side effects.”
The department’s outcomes support this approach: in the three years they have performed these procedures, only one patient has required retreatment – a testament to the durability of these new techniques.
The Urology department’s growth extends beyond prostate treatments.
The team has developed several subspecialty services, each led by consultants with advanced overseas training. These include:
• Female urology services for urinary incontinence and recurrent urinary tract infections
• Complex stone management using advanced techniques
• Urethral reconstruction surgery
• Men’s health services including erectile dysfunction treatments
• Advanced treatments for chronic pelvic pain
“What sets us apart is our teambased, consultant-led practice,” Dr Lau explains. “While we maintain general urology capabilities, we ensure patients receive care from specialists trained specifically in their condition. Our internal referral system means patients get the right care from the right physician.”
The department also emphasises holistic care through collaboration with other specialties. For instance, they
Urinary symptoms fall into three main categories:
Storage Symptoms
• Frequent urination
• Urgency (inability to hold urine)
• Increased nighttime urination
Voiding Symptoms
• Weak urine stream
• Difficulty starting urination
• Sensation of incomplete bladder emptying
Red Flag Symptoms
• Burning sensation during urination
• Urinary leakage
• Complete inability to pass urine
• Blood in urine
Early recognition and treatment of storage and voiding symptoms can help prevent crisis situations.
work closely with geriatricians for older patients, renal physicians and dietitians for stone prevention, and other relevant specialists to ensure comprehensive treatment plans.
As the department continues to grow, it remains focused on bringing innovative solutions to complex urological problems. “We’re seeing excellent outcomes with these new approaches,” Dr Lau says. “Our data shows patients require shorter hospital stays and low readmission rates.”
For patients like Mr Chen, these advances mean more than just medical success – they represent a chance to maintain quality of life despite complex medical conditions. “When we can offer safe, effective treatments to patients who previously had limited options,” Dr Lau reflects, “That’s when we know we’re making a real difference.”
To find out more about our urology services, scan this QR code:

Muscle loss can occur with ageing, especially if one leads a sedentary life. Ensuring that we get enough protein in our diet and continuing to be active can help to slow down the process.

In
consultation
with
Chow Pek Yee, Head and Principal Dietitian, Nutrition & Dietetics

Did you know that from age 40, we could be losing up to 8% of our muscle mass every decade? Even more concerning is that this rate may double after age 70. This natural age-related decline in muscle mass, strength and function is called sarcopenia.
While this is a normal part of ageing, certain factors can accelerate muscle loss. These include:
• Chronic diseases: Conditions such as diabetes, heart disease, and chronic obstructive pulmonary disease (COPD)
• Malnutrition: Those who are undernourished or have inadequate protein intake are at higher risk
• Inflammatory conditions: Diseases that cause chronic inflammation, like rheumatoid arthritis
• Hormones: Changes in hormone levels, particularly testosterone and oestrogen
• Sedentary lifestyle: Lack of physical activity can lead to muscle atrophy
The good news is that there are ways to maintain muscle mass and strength as we age. The key lies in two main areas: proper nutrition and regular physical activity.
Protein is the building block of muscles. As we age, our bodies may become less efficient at using protein, so we need to consume more of it.
Aim for three servings of protein-rich foods daily, with one serving being any of these:
• 1 palm-sized piece of lean meat, fish or
• 5-6 pieces of medium-sized prawns (90g)
• 1 palm-sized piece of lean meat,
• 3 eggs (150g)
• 5-6 pieces of medium-sized prawns
• 2 glasses of low-fat milk or soy milk (500ml)
• 3 eggs (150g)
• 1 bowl of shelled edamame (200g)
• 2 glasses of low-fat milk or soy
1 palm-sized piece of lean meat, fish or poultry (90g-100g)
2 glasses of low-fat milk or soy milk (500ml)
5-6 pieces of medium-sized prawns (90g)
1 bowl of shelled edamame (200g)
1 cup of mixed nuts trail mix (150g)
3 eggs (150g)
• 1 cup of mixed nuts trail mix (150g)
• 1 bowl of shelled edamame (200g)
• 4 pieces of tempeh (90g-100g)
• 1 cup of mixed nuts trail mix (150g)
• 2 small blocks of tofu (150g)
• 4 pieces of tempeh (90g-100g)
• 2 small blocks of tofu (150g)
• 1 palm-sized piece of lean meat, fish or poultry (90g-100g)
• 5-6 pieces of medium-sized prawns (90g)
• 3 eggs (150g)
4 pieces of tempeh (90g-100g)
• 1 palm-sized piece of lean meat,
• 5-6 pieces of medium-sized prawns
• 2 glasses of low-fat milk or soy milk (500ml)
• 3 eggs (150g)
• 1 bowl of shelled edamame (200g)
• 2 glasses of low-fat milk or soy
• 1 cup of mixed nuts trail mix (150g)
• 1 bowl of shelled edamame (200g)
• 4 pieces of tempeh (90g-100g)
• 1 cup of mixed nuts trail mix (150g)
• 2 small blocks of tofu (150g)
2 small blocks of tofu (150g)
• 4 pieces of tempeh (90g-100g)
• 2 small blocks of tofu (150g)
Try to include protein-rich foods in every meal! For example, add an egg to your breakfast, include some chicken or fish at lunch, and have a serving of tofu or lean meat with dinner. Spreading your protein intake throughout the day helps maximise muscle growth and maintenance.
• Decreased strength
• Difficulty performing daily activities
• Slower walking speed
• Poor balance
• Frequent falls
• Unintentional weight loss
• Increased fatigue
Physical activity, especially strength or resistance training, is crucial for maintaining muscle mass. Simple exercises you can begin with at home include:
• Squats while holding onto a chair
• Wall push-ups
• Standing up from a chair repeatedly
• Climbing stairs
• Walking with hand weights
Even daily activities like gardening, carrying groceries, or playing with grandchildren can help maintain some muscle strength. Remember, it’s never too late to start taking care
of your muscles. Small changes in your diet and activity levels can make a big difference in maintaining strength and independence as you age.
If you notice increasing difficulty with daily activities, have been eating less than usual in the last two weeks, or have lost weight unintentionally, speak to your doctor. They can assess your muscle strength and recommend appropriate exercises or interventions.
Senior Consultant Associate Professor
Lim Su Chi reflects on how his enduring curiosity and passion for research have kept him young at heart, while his purpose-driven approach to medicine helps him maintain perspective in life.
With a gentle demeanour and thoughtful manner, A/Prof Lim Su Chi speaks about his life’s work with the quiet yet evident enthusiasm of someone discovering something new. A/Prof Lim is one of the National Healthcare Group’s prominent clinician-scientists and heads KTPH’s Clinical Research Unit as Clinical Director.
His eyes light up on his serene and ageless face as he describes

aspects of his life’s work in diabetes research. He likens it to ‘watching a drama series’, pointing out that there’s always another episode, another discovery, another mystery to solve.
This childlike curiosity has been a driving force throughout his career and partly led him to make an unusual decision 20 years ago despite being
an established consultant.
With 16 years of medical practice already under his belt, he found himself at a career crossroads.
“I asked myself, am I going to do the same thing over the next 10 to 20 years?” he recalls.
At the time, medicine was at an exciting juncture. With developments like the Human Genome Project, it was evolving towards more personalised care.
“The stars were aligned,” he says, explaining how technological
Diabetes is, in many ways, a good model for us to understand how complex health problems can be addressed. And in fact, some people say that if you can tame diabetes, you can tame a lot of complex diseases.
A/Prof Lim Su Chi Clinical director, Clinical research, KTPH
advances were opening new possibilities in healthcare.
This led him to pursue a PhD while maintaining his clinical practice – an arduous journey that took six long years. His decision came at a time when there was
no established pathway for clinical investigators, so he had to pursue both his studies and clinical work concurrently, working late nights, weekends and public holidays.
“It was a lot of self-navigation,” he notes, adding with characteristic
humility that he could not have done it without support from his supervisors, peers and family.
A/Prof Lim describes his interpretation of PhD as standing for “People, Host, and Dream”. People represent the connections made along the way, while Host signifies the supportive environment and community that enabled his growth, and Dream embodies the vision that drove him forward.
A/Prof Lim’s inspiring PhD pursuit was not just borne of intellectual curiosity. After all, the constant pursuit of knowledge contributes to improved patient care.
“We are custodians of scientific


truth,” he states, emphasising how good science translates to better healthcare outcomes.
This was particularly evident during the COVID-19 pandemic, which he says, “compressed into three years the importance of good science.” Pulling together as a scientific community drives medical advancements by leaps and bounds – this effort can be seen in countless achievements. Just look at the Human Genome Project, he says. Back then, it took 200 scientists, 10 years and USD3 billion to sequence one human genome.
“Today, you can do it in three days, with one scientist for USD600.”
As an endocrinologist with a profound interest in type 2
For doctors, or most people in healthcare, hard work becomes bearable very quickly once we see meaning and hope in what we’re doing.
diabetes, A/Prof Lim hopes that a steadfast pursuit of scientific truth can unveil the mysteries of metabolic disease, which he notes has “become one of the biggest health challenges of the modern age.” Over two decades, he has not only pioneered research pathways but also actively encouraged others to engage in scientific inquiry. His own extensive research
has provided crucial insights for Singapore’s fight against diabetes.
One key finding revealed that Singaporeans tend to develop diabetes at a much lower BMI than Western counterparts – typically around BMI 27, compared to BMI 30 in Western populations. His wide-ranging work with cohort studies uncovered another significant discovery: that different

KTPH’s Clinical Research Unit has led illuminating research in the fields of diabetes, obesity and familial hypercholesterolemia
regions of Singapore showed subtle but important differences in nutritional practices between nearby communities, highlighting the need for targeted interventions.
Such findings reveal the nuances of cultural, ethnic and even socio-economic factors on disease progression – deepening the way clinicians develop care plans for their patients.
Such understanding sheds light on the deeply multi-factorial puzzle that is diabetes. He says, “Diabetes is, in many ways, a good model for us to understand how complex health problems can be addressed. And in fact, some people say that if you can tame diabetes, you can tame a lot of complex diseases.” His forays into the mysteries of our metabolism may also hold the key to understanding how and why we age – and why it is often accelerated in those with metabolic disease.
A/Prof Lim has an air of youthfulness about him – not just in his countenance, but also in his boundless curiosity and passion for patient care.
As a mentor to younger clinicianscientists, A/Prof Lim emphasises that age is not a determining factor. “What’s important is not so much the chronological age,” he explains, observing how some septuagenarian doctors remain passionate, while young doctors sometimes lose their curiosity.
To him, it is important to be young at heart and mind through purpose. A/Prof Lim shares wisdom from a former boss: “For doctors, or most people in healthcare, hard work becomes bearable very quickly once we see meaning and hope in what we’re doing.”
This purpose-driven perspective has guided him through decades
of medical practice and research and maintained his enthusiasm to overcome challenges.
He believes healthcare professionals have a ‘birthright’ to pursue research excellence alongside clinical practice.
“The two are linked together,” he explains, “You need both to combine and conquer.”
And ultimately research isn’t just about academic achievement and medical excellence. To A/Prof Lim, it is about improving care and making a difference in people’s lives.
To find out about current studies and participate in them, scan this QR code:

Be it a wound from a small cut, a scrape or a blister, proper care not only prevents scarring and helps healing but also reduces the risk of infection – especially in people with diabetes.


In consultation with
Gimilie Valerio and Isabella Chua Xue Bing, Senior Staff Nurses, Advanced Practice Nurses & Specialty Nurses, KTPH
Keep the wound clean to prevent infection. Begin by washing the area with mild soap and water. Avoid harsh scrubbing to prevent further damage. You can then flush it with normal saline to remove dirt and bacteria. Avoid using rubbing alcohol or medicated oil, as these can damage healthy tissue. Pat the area dry with a clean towel or gauze.
Cover the wound with clean gauze or plaster to protect it from further injury and contamination. Refrain from scratching or picking at the wound, as this can disrupt the healing process and increase the risk of infection. Ensure that dressings are not too tight and change it when it becomes wet or soiled.
3
Do not let the wound dry out completely. Maintaining a moist (but not wet) wound environment promotes healing and reduces scarring. Cover the wound with the appropriate wound product to aid healing. However, do avoid submerging a wound in water when bathing or showering.


Observe the wound for signs and symptoms of infection. If there is redness, swelling, pus or pain, or if you develop a fever, seek medical advice or attention. For wounds on swollen arms or legs, try to keep them elevated where possible. This can help reduce swelling and improve circulation, which promotes faster healing. 4
Proper nutrition plays a crucial role in wound healing. Ensure you are eating a balanced diet rich in vitamins, particularly Vitamins A and C, which help in tissue repair and immune function. Protein intake is also essential for wound recovery. Unless advised otherwise by a medical professional, drink plenty of water too as proper hydration supports cell function, helping to promote faster and more effective healing. If you smoke, consider quitting as tobacco can impair circulation and reduce oxygen supply to the wound area, slowing down the healing process.

Knee pain is one of the most common joint complaints that can significantly impact daily activities and quality of life. Understand its causes and available treatments so you can take steps toward better knee health and mobility!

In consultation with Dr Sim Wei Ping, Consultant, Orthopaedic Surgery, KTPH
Our knees do so much for us. They bear our weight and help us walk, run, jump, sit and more! With all the work they do, it is no wonder that our knees can sometimes hurt. Sometimes, knee pain is temporary — caused by a simple strain or overuse. For some, knee pain can be chronic. And it’s not just an age-related problem — knee pain can affect people of all ages, from athletes to seniors.
Osteoarthritis is the most common cause of chronic knee pain. This occurs when the protective cartilage in the knee joint gradually wears down. This condition often develops with age, but can also be influenced by body weight, previous injuries, and genetics. The breakdown of joint cartilage and underlying bone changes leads to inflammation, causing pain and stiffness.
Injuries such as ligament tears (like the anterior cruciate ligament or ACL) and meniscus tears can occur to anyone. These injuries not only cause immediate pain but may also increase the risk of developing osteoarthritis later in life.
Overuse conditions , such as runner’s knee (patellofemoral pain syndrome) or tendinitis, typically develop from repetitive stress on the knee joint. These conditions are common among athletes and people whose activities involve frequent knee movements.

Treatment of knee pain depends on its cause and severity.
Medication:
Non-steroidal anti-inflammatory drugs (NSAIDs) and topical treatments like creams and gels can help reduce pain and inflammation.
Rehabilitation through physiotherapy and exercise:
Strengthening the muscles supporting the knee can help reduce the load on the joint. This not only aids in pain relief but can also serve as surgery preparation, should an operation be needed in the future.
Surgical options: When conservative treatments become inadequate, your doctor may recommend surgical options like a knee replacement. This can significantly improve quality of life. Surgery has been shown to:
• Reduce chronic pain
• Improve knee motion, physical mobility, and daily function
• Correct leg alignment
• Enable the return to daily activities
The most common surgical option is a Total Knee Replacement. This involves replacing the whole knee joint with prosthetic components made of surgical-grade metal alloys and plastic. It is typically recommended for
Injections: For more persistent pain, doctors may recommend injections as an adjunct. Viscosupplementation or steroids through a gel injection into the knee can help reduce inflammation. Another option involves injections targeting the sensory nerves around the knee. If there is good relief, this can be extended to a radiofrequency treatment for longer lasting results.

patients with widespread knee damage. As an alternative, Partial (Half) Knee Replacement is suitable for people whose knees only have partial damage. This less invasive option preserves more of the natural knee tissue and allows a faster recovery time. This surgery has a smaller incision, involves less blood loss, and provides a more natural knee movement.
In some instances, knee pain may improve with rest and home care. However, consult a doctor if you experience:
• Severe pain or swelling not improved with self-medication or rest
• Inability to bear weight on the affected leg
• Significant reduction in range of motion
• Impairment of daily function/activities due to pain
• Significant deformity of the knee joint
Seeking early treatment often means better outcomes and may help prevent the progression of knee conditions. Your doctor can evaluate your condition and recommend the most appropriate treatment plan.
Modern knee replacements are built to last; though longevity varies on factors like physical condition, activity level, and body weight. With modern advances in surgical technology, knee replacement surgery is more precise than ever before. This will allow surgeons to restore your knee to as close to its pre-disease state as possible, thereby improving function and satisfaction.
Our knee replacement journey has significantly improved over the years. Prior to surgery, we provide comprehensive classes to ensure you are fully prepared. Thanks to our enhanced recovery protocols, you can look forward to walking soon after the procedure, supported by our dedicated therapy teams. We believe in personalised solutions because everyone is unique. Our approach is to tailor the techniques to meet your specific needs. Scan this QR code to find out more!


This recipe, rich in calcium, protein and vitamins, provides 40% of your daily nutritional needs for strong bones!
Serves 2
• 200g whole-grain spaghetti
• 200g salmon fillet, skin removed and cut into chunks
• 4 anchovy fillets, finely chopped
• 4 cloves garlic, thinly sliced
• 2 tablespoons extra virgin olive oil
• 1 teaspoon red pepper flakes
• 2 tablespoons fresh parsley, chopped
• 1/2 lemon, juiced
• Black pepper to taste
1. Cook spaghetti in a large pot of salted water according to package instructions until al dente. Reserve 1/2 cup pasta water before draining.
2. While pasta cooks, heat 1 tablespoon olive oil in a large pan over medium heat.
3. Add salmon chunks and cook for 3-4 minutes until just done. Remove and set aside.
4. In the same pan, add remaining olive oil, garlic, and anchovies. Cook on low heat until the garlic is golden and anchovies dissolve.
5. Add red pepper flakes and cook for 30 seconds.
6. Add cooked pasta to the pan along with a few tablespoons of pasta water. Toss well to combine.
7. Slowly add in the cooked salmon, parsley, and lemon juice. Add more pasta water for desired consistency.
8. Season with black pepper and serve immediately.

Recipe provided by Nge Aik Tee, Executive Chef, Food Services, KTPH, in consultation with Nutrition & Dietetics, KTPH

NUTRITIONAL INFORMATION (PER SERVING)


Your frequently asked questions about fall risk answered by KTPH’s Falls and Balance Clinic.
In consultation with

Su Su Senior Consultant

Sook Gin Assistant Nurse Clinician
I’m caring for my elderly mother. She has high blood pressure and other chronic illnesses. How can I tell if she’s at risk of falling and should a medical professional assess her fall risk?
As your mother has high blood pressure, she may be taking medication with side effects that may lead to falls, such as giddiness and low blood pressure. Some other indicators include:
• Difficulty maintaining balance while walking or standing
• Taking small, shuffling steps
• Holding onto furniture while moving around
• Recent changes in medications which may lead to dizziness and drowsiness
• Vision or hearing problems
• A history of previous falls
• Multiple chronic conditions like diabetes, arthritis, and high blood pressure
If you notice any of these signs, it is important to have your mother assessed by healthcare professionals.

Rou Senior Staff Nurse

At KTPH, we have a multidisciplinary team that will develop a customised prevention plan that takes into account your mother’s unique circumstances and needs. They will evaluate her fall risk by checking on her:
• Walking speed
• Ability to stand up from a seated position
• Balance when standing unsupported in various positions
• Previous fall history
• Living environment safety
• Vision problems
• Chronic health conditions
• Cognitive function
The team will also assess if your mother’s medications cause dizziness and unsteadiness. If you notice any of these signs, inform her doctor about her symptoms to adjust the dosage safely.
Don’t wait for a fall before seeking help – being proactive about fall prevention is key to keeping your loved ones safe and mobile.
Are falls as serious as they seem? What changes can I make to my home to prevent falls?
Falls can lead to serious injuries such as fractures, traumatic brain injuries, muscle breakdown and even pneumonia. Research shows that about one in four seniors aged 65 and above – excluding those living in nursing homes – will have at least one fall each year. A 2020 study published in the Singapore Medical Journal revealed that falls accounted for nearly all emergency trauma cases involving the elderly.
Making your home safer is one of the best ways to prevent falls. Read more tips on home modifications to consider on page 30.
My father insists he doesn’t need a walking aid, even though he’s becoming unsteady. How can I convince him?
Many older adults resist using walking aids because they see them as a sign of losing independence. Help your father understand that mobility aids promote independence, allowing him to move around safely and confidently. Share that many falls can lead to serious injuries that could result in a real loss of independence. Have him assessed by a physiotherapist who can:
• Recommend the most suitable type of walking aid
• Ensure the aid is properly fitted
• Teach him how to use the aid correctly
• Demonstrate how the aid can help him maintain his active lifestyle

I keep encouraging my grandfather to exercise more, but I’m also concerned if it is safe for him, especially since he had a minor fall a while ago and is reluctant to go out now.
Fear of falling is a concern among seniors who have experienced a fall. This fear can lead to decreased activity levels and social isolation, which may lead to a decrease in the senior’s ability to perform everyday activities and increase the risk of falls
This is exactly why staying active is so important and why you should continue to encourage your grandfather! Regular exercise is one of the best ways to prevent falls. Exercise helps improve:
• Balance
• Muscle strength
• Flexibility
• Coordination
• Overall mobility

Help him rebuild his confidence gradually through guided exercises and activities. Look for low-impact exercise programmes specifically designed for seniors, such as tai chi , chair yoga, water exercises, supervised strength training, and balance exercises. Remind him that staying active is not just about preventing falls –it’s about maintaining his independence and quality of life.
Always consult a healthcare provider before starting any new exercise programme to ensure it is appropriate for his fitness level and health conditions.
Scan this QR code for more information on the specialist outpatient care available for the elderly.


As we age, making our homes safer becomes crucial to help prevent accidents and reduce fall risk. Through simple home modifications and arrangements, we can help our seniors to live safely, actively and independently.


WLee Ruoyu Cara, Senior Occupational Therapist
anting to remain in one’s own home as we grow older is common among seniors. However, natural age-related changes in mobility, vision, and balance, along with various medical conditions, can make navigating even familiar spaces challenging.
Thoughtful home modifications can help create a safer environment that supports independent living while reducing the risk of falls and accidents.
Begin by evaluating how one’s daily activities flow through a living space. Wherever possible, incorporate


universal design principles that work for everyone, regardless of ability. For example, having level access at toilet entrances benefits both able-bodied individuals as well as those using mobility aids.
1 Rearrange furniture to create wider pathways, especially for walking aids
2 Remove unnecessary items and declutter regularly
3 Ensure frequently used items are within easy reach
4 Check furniture heights for comfortable and safe use
5 Install removable ramps with non-slip surfaces at entrance steps
6 Lower or eliminate curbs where possible
Install grab bars and handrails strategically throughout the home. Consider adding them where they will come in most handy.
1 Place vertical grab bars near steps and level changes
2 Install horizontal bars in bathrooms near toilets and in shower areas
3 Add handrails along both sides of staircases
To ensure that they are safe and useful, ensure all support fixtures are properly anchored and weight-tested. You may even consider using contrasting colours for better visibility. Remember to keep grab bars clear of items like towels or toiletries that might interfere with their use.

Slips and falls are some of the most significant risks. Reduce fall risk with these measures:
1 Install non-slip mats to cover the entire bathroom floor, not just small areas
2 Remove or secure loose rugs and carpets with proper anchoring
3 Use anti-slip and coloured tape on stairs and level changes
4 Keep floors dry and clean up spills immediately
5 Consider non-slip flooring options during renovations
6 Install proper drainage in wet areas
7 Organise and secure loose electrical cords and telephone wires using cable ties or cable management systems

Improve lighting throughout the home to improve visibility:
1 Install brighter bulbs in frequently used areas
2 Add motion-sensor lights in hallways and bathrooms
3 Use night lights in bedrooms and along paths to bathrooms
4 Ensure stairways are

well-lit from both the top and bottom
5 Add task lighting in work areas like kitchen counters
6 Use contrasting colours to highlight changes in floor levels
For tech-savvy seniors, smart home features can enhance safety. These can make activities of daily living more convenient and increase safety. Consider:
1 Voice-activated lighting control
2 Automated medication reminders
3 Smart doorbell with video capabilities
4 Fall detection devices and/or emergency response systems
5 Automated appliance shut-off features
6 Motion-sensor water taps

You may also consider having an occupational therapist assess your home. They are trained to identify specific risk areas based on individual needs and can recommend appropriate modifications and adaptive equipment. Importantly, they can provide training on the safe use of modifications, and review and update safety measures should the need arise.