annual report
2019/2020
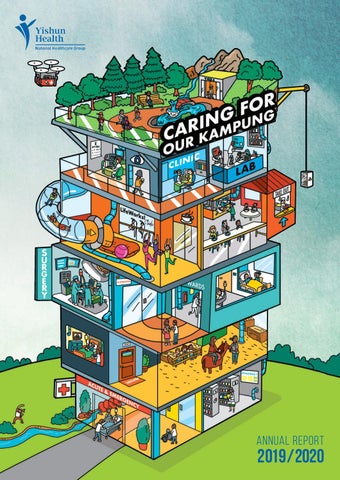
CARING FOR OUR KAMPUNG
CARING FOR OUR KAMPUNG At Yishun Health, we believe that we are better when we work together. By integrating our strengths and capabilities, we are greater than the sum of our individual parts. This collaborative approach means moving beyond the confines of our medical specialties, services and institutions to
13
LIVING WELL
29
LIVING WITH ILLNESS
37
CRISIS AND COMPLEX CARE
develop holistic ‘one care plans’ for our patients and residents. Therein lies the meaning of our ‘vertical kampung’, a visual representation of a forward-looking, future-ready ecosystem of care that will allow us to meet the healthcare needs of tomorrow. Anchored upon a model of unified and personcentred care, we integrate clinical processes across acute and emergency care to the management of chronic conditions and intermediate care needs. This spectrum of care also extends to the wider community in the form of various community health programmes, ageing-in-place and end-of-life care. This teamwork not only flows within our processes as a hospital; it also connects us with the everyday lives of the people whom we serve. In building this community of care, our ‘kampung’ works closely to leverage the knowledge, strengths and partnerships of our healthcare professionals, our patients and their caregivers, and our partners in the community. And while we maintain the old-school spirit of gotong royong, our network is enabled and supported by modern-day systems, technology, infrastructure and innovative practices rooted in our kaizen culture of continuous improvement. Flowing through this vertical kampung is a river, a symbolic illustration of the ‘River of Life’ — our blueprint to care for our patients and residents through all stages of their life, health conditions and needs. It also signifies our commitment to navigate forward as one Yishun Health team in Caring For Our Kampung.
2
49
LIVING WITH FRAILTY
57
LEAVING WELL
73
AWARDS AND RECOGNITION
79
OUR People
PUBLISHER Yishun He alth is a network o f medical institution s and health fac ilities in th e north of S ingapore, under the Na Healthcare tional G comprises roup. It Admiralty
entre, Medical C Puat k Khoo Tec Yishun d n a l Hospita It y Hospital. Communit ity n u m m co es also includ s such as extension ampung. K Wellness
E D ITO R S
U TO R S C O N T R IB s Variou
Sabrina N g Sharon N g Hannah W ong Albert Fo o
63
RESEARCH AND EDUCATION
nts departme s s ro c a ealth Yishun H
www.ktph.com.sg/about-us/media/publications aha@ktph.com.sg A Publication by Yishun Health Corporate Communications Designed by ThinkFarm Pte Ltd
3
CARING FOR OUR KAMPUNG
VISION
Adding years of healthy life
MISSION
Provide good quality, affordable and hassle-free healthcare with science, love and wisdom
CARE PHILOSOPHY
Care that is good enough for our own mothers without making special arrangements
WE ARE NHG The Nati onal Hea lthcare G leader in roup (NH public he G) is a althcare recognis in Singap ed at ho ore, me and a of its me broad fo dical exp r the quali ertise an ty provided d facilitie through s . Care is a n in tegrated six prima network ry care p of olyclinics tertiary h , acute c ospitals, a re a n d n ational s and busin pecialty ess divis c e n tr es ions. Tog a rich leg ether, th acy of m ey bring e d ic al expert philosop ise to ou hy of inte r grated p atient-ce ntred ca re. NHG’s vis ion is ‘Ad d in g Years of This visio Healthy n goes b Life’. e yo n d m sick to th erely hea e more d ling the ifficult an d infinite ly more
4
d illness an reventing p f o ith k s W . g ta f life rewardin quality o d n re a h lt e a rovid ca g he aims to p preservin G H N , s , s ff le eam 00 sta essible, s c some 18,0 c . a , ic tr c effe tive tient-cen and costte a that is pa ri p ro pp ensive, a compreh r Central ystem fo S h lt a e H rtner and egional HG to pa As the R N r fo l a nity , it is vit , co m m u Singapore eholders k ta s tions. h is it n te w orga a re a lf e collabora w ntary milies , and volu ts, their fa advisors n e ti a p r tegrated r with ou deliver in Togethe to in im a e that help givers, w rammes g ro p and care d . n d es a concerne re servic Life to all healthca y h lt a e H ears of Adding Y
A MESSAGE FROM THE GROUP CEO, NHG Since its early days in Alexandra Hospital, Yishun Health has had a driving goal of providing hassle-free person-centred care, a vision that has always been aligned with that of the National Healthcare Group (NHG). For us, the shared mission of ‘Adding Years of Healthy Life’ is more than just treating sickness when it occurs, but taking a holistic and comprehensive approach to prevent illness, preserve health, as well as maintain and restore quality of life. This is the basis of our ‘River of Life’ framework, where we move upstream and focus on proactive and preventive care that can meet the different needs of our population. By considering the determinants of health, we are able to shape our care delivery according to the needs of our population across five segments of care: Living Well, Living with Illness, Crisis and Complex Care, Living with Frailty, and Leaving Well.
Yishun Health’s Unified Care Model (UCM) is a key area of work that complements the River of Life framework, enabling the shift towards proactive self-management through capability building and community development. By building an ecosystem of care that encompasses service provision, collaboration with community partners, and healthy lifestyle activation of the population, Yishun Health supports and enables residents to manage their own health. This means patients are able to tap on public healthcare at the right point, resulting in lower costs for both themselves and the healthcare provider. Such moves mark a transformation from the early days of episodic hospital-centric care. Today, Yishun Health — together with its fellow NHG institutions — strive to meaningfully engage our community and build purposeful relationships with the patients and population to add years of healthy life.
This is done through greater integration of health and social services, and the development of targeted programmes and timely interventions to support our population through the different stages of their life. In particular, the River of Life framework will put healthcare organisations in better stead to address three important issues — Pre-Disease, Chronic Disease, and Frailty — and work to mitigate the impact of each one.
Prof Philip Choo
Group Chief Executive Officer NHG
5
CARING FOR OUR KAMPUNG
A MESSAGE FROM THE CEO
As a healthcare organisation, Yishun Health is cognisant of the challenging reality of healthcare. Apart from an ageing population, the rising burden of chronic disease, and escalating healthcare costs, we must also address the increasingly complex patient journeys that arise from poor lifestyle habits, lack of access to care, multiple co-morbidities, socio-economic issues, and more. Across the globe, healthcare systems are searching for ways to move seemingly intractable ‘rocks’ that disrupt the flow of care. This takes more than simply offering ‘more’ healthcare. Instead, we must shift our focus to identify key leverage points and pull our strengths together to create fulcrums of meaningful change. At Yishun Health, we are doing this through a concerted effort of care integration: our Unified Care Model (UCM). A united vision of care The UCM is central to Yishun Health’s — and NHG’s — thrust of moving upstream to care for our patients in the ‘River of Life’ to achieve the 6
‘Three Beyonds’ set out by MOH: from Hospital to Community, from Healthcare to Health, from Quality to Value. It also represents our aspiration to co-create with our staff and communities the highest form of integrated care. This care is person- and community-centred, and built upon collective strengths and shared goals, trust and relationships. We envision that all residents have a ‘One Care Plan’ that offers hassle-free access to dignified, safe, and value-driven care throughout the stages of their healthcare needs — from enabling them to live fit and healthy lifestyles and confidently managing their chronic conditions to spending their senior years in comfort and dignity. This model of care requires us to bring together all our skilled individuals and departments across Khoo Teck Puat Hospital (KTPH), Yishun Community Hospital (YCH), Admiralty Medical Centre (AdMC), and the Population Health & Community Transformation (PHCT) teams to form a shared vision and — through collective wisdom — co-create and implement new service models.
Creating levers to unclog the flow of care I am proud to share that many programmes and clinical pathways are already in place to enable us to deliver more unified care. Much of this work has been reviewing and revising our workflows. But more importantly, it has been about driving even more patient-ownership by physicians. By amplifying our ethos of care, instilling empathy, passion, ownership and teamwork into our culture, we are able to optimise care plans and unclog the flow for more streamlined care.
Together, we are working to bridge gaps in care, leverage resources and strengths, and collaborate as one Yishun Health so that — regardless of whether our patient is on the campus or in the community — our healthcare teams readily cross boundaries to deliver seamless, timely and integrated right-sited care, so that we can truly care for our kampung.
Mrs Chew Kwee Tiang Chief Executive Officer Yishun Health
In this Annual Report, you will read about some of the ways we have: • Reduced unnecessary admissions via an Ambulatory Emergency Care Service (page 40) • Smoothened the flow of patient and care processes within Yishun Health with our Integrated Medical Clinics (IMCs) (page 31) • Improved discharge processes and linkages for seamless care transitions in programmes such as the Ageing-in-Place Community Care Teams (AIP-CCT) (page 51) In addition to these improvements, we expanded a successful pilot that optimises patient transfers and referrals between KTPH and YCH. Leveraging collective efforts to care Apart from improving our internal processes, clinical pathways, and transitional care plans, we have also strengthened our engagement with our community, empowering them to self-manage and be active participants in their own health. It is seen in our PHCT teams, who take an Asset-Based Community Development approach to drive sustainable neighbourhoodbased engagement. This is — and always has been — a focus for us at Yishun Health. Supporting us in our efforts to drive better care coordination is one of our newest pilots, the Tele-health and Integrated Network (ThINk) Centre service. ThINk aims to further propel the focus of care from hospital to community. Plans are in place to pull together different pieces — client engagement, patient activation, and supported self-management — for more integrated care, even without visiting the hospital. 7
CARING FOR OUR KAMPUNG
CARING FOR OUR RESIDENTS IN THE NORTH LEGEND
Healthcare Institution
3 4 1 2
MARSILING-YEW TEE
Community Nurse Post
SEMBAWANG Share a Pot®
Healthcare Institution
Wellness Kampung
1. Admiralty Medical Centre 676 Woodlands Dr 71
Community Nurse Post
*Other Share a Pot® locations not shown in the map: 1. Starlight RC Café Corner 718 Tampines St 72 2. Church of St Vincent de Paul 301 Yio Chu Kang Rd 3. Tembusu Senior Activity Centre 3 Eunos Cres 4. Agape Village 7A Lor 8 Toa Payoh 5. Anglican Senior Centre (Tampines) 117 Tampines St 11 6. Evergreen Circle Seniors Activity Centre 827A Tampines St 81 7. Meeting Point @ 128 128 Lor 1 Toa Payoh 8. Blk 139 Residents’ Lounge 139 Petir Rd 9. Sree Narayana Care Centre @ Pek Kio CC 21 Gloucester Rd 10. Kebun Baru Community Club 113 Ang Kio Ave 4 11. Jalan Besar Bendemeer RC 22 Boon Keng Rd 12. THK Bedok Radiance Senior Activity Centre 12 Bedok South Ave 2 13. Goodlife! @ Telok Blangah 7 Telok Blangah Cres 14. West Spring Secondary @ Fei Yue Senior Activity Centre 634B Senja Rd 15. Chong Hua Tong Tou Teck Hwee 232, 234 Tampines St 21 16. Carelight Wellness Centre 141 Bedok Reservoir Rd 17. Thye Hua Kwan Senior Activity Centre @ Cassia 52 Cassia Cres
8
1. NTUC Health Active Ageing Hub 676 Woodlands Dr 71 2. Sunlove Senior Activity Centre @ Golden Saffron 764B Woodlands Circle 3. Sembawang Zone K RC 588C Montreal Dr 4. Sembawang Zone J RC 793 Woodlands Ave 6 5. ACE The Place Community Centre 120 Woodlands Ave 1 6. Care Corner Senior Activity Centre 569A Champions Way 7. Sembawang Zone H RC 770 Woodlands Dr 60 8. TOUCH Senior Activity Centre 513 Wellington Circle
MARSILING-YEW TEE Community Nurse Post 1. Sunlove Senior Activity Centre (Marsiling) 3 Marsiling Rd 2. NTUC Silver COVE Marsiling 180B Marsiling Rd 3. Marsiling Zone 7 RC 206 Marsiling Dr
Share a Pot® 4. Woodlands Secondary @ Marsiling Zone 3 RC 123 Marsiling Rise
Share a Pot® 6. Care Corner Senior Activity Centre 569A Champions Way 9. Woodgrove Zone 1 RC 521 Woodlands Dr 14 10. Covenant Evangelical Free Church (Woodlands) 90 Woodlands Dr 16 11. Singapore Anglican Community Services Centre @ Floral Spring 426A Yishun Ave 11 12. Covenant Evangelical Free Church (Woodlands) & Admiralty Primary School @ Woodlands Galaxy CC 31 Woodlands Ave 6 13. Canberra Secondary @ Blossom Seeds SAC 105 Canberra St 14. Victory Family Centre 55 Sembawang Dr 15. Anglican Senior Centre (Woodlands) & DBS 572 Woodlands Ave 1
14 8
7
2
4
1
13
3
SEMBAWANG 13
9
12 10 15
10
3
4
6
8
6 5
12
1
5
NEE SOON
7
9
11 2
11
NEE SOON Healthcare Institution 1. Khoo Teck Puat Hospital 90 Yishun Central 2. Yishun Community Hospital 2 Yishun Central 2
Community Nurse Post 3. Wellness Kampung @ 115 (Chong Pang) 115 Yishun Ring Rd 4. Wellness Kampung @ 765 (Nee Soon Central) 765 Yishun St 72 5. Wellness Kampung @ 260 (Nee Soon East) 260 Yishun St 22 6. Thye Hua Kwan Chong Pang Social Service Hub 131 Yishun St 11 7. Wellness For Life @ Nee Soon South 839 Yishun St 81 8. Nee Soon East Community Club 1 Yishun Ave 9 9. Yishun Clover RC 398 Yishun Ring Rd 10. TOUCH Senior Activity Centre 162 Yishun St 11 11. TOUCH Senior Activity Centre 436 Yishun Ave 11
Share a Pot® 3. Wellness Kampung @ 115 (Chong Pang) 115 Yishun Ring Rd 4. Wellness Kampung @ 765 (Nee Soon Central) 765 Yishun St 72 5. Wellness Kampung @ 260 (Nee Soon East) 260 Yishun St 22 6. Thye Hua Kwan Chong Pang Social Service Hub 131 Yishun St 11 12. Sree Narayana Mission Home (Singapore) 12 Yishun Ave 5 13. Church of Our Lady Star of the Sea 10 Yishun St 22
Wellness Kampung 3. Wellness Kampung @ 115 (Chong Pang) 115 Yishun Ring Rd 4. Wellness Kampung @ 765 (Nee Soon Central) 765 Yishun St 72 5. Wellness Kampung @ 260 (Nee Soon East) 260 Yishun St 22
9
CARING FOR OUR KAMPUNG
B OA RD C O M MIT T EE
Mr Robert Chew
Mr Tow Heng Tan
S E NIO R M ANAGEM ENT
10
Mrs Chew Kwee Tiang
A/Prof Pek Wee Yang
Ms Yen Tan
Chief Executive Officer
Chairman, Medical Board
Chief Operating Officer
Dr Wong Sweet Fun
A/Prof Terence Tang
A/Prof Wong Moh Sim
Chief Transformation Officer; Deputy Chairman, Medical Board (Population Health); Clinical Director, Population Health & Community Transformation
Chief Clinical Informatics Officer; Deputy Chairman, Medical Board (Clinical Informatics, Innovation & Patient Engagement)
Deputy Chairman, Medical Board (Clinical Quality & Manpower Development)
Prof James Best
Ms Shirley Heng Chief Nurse
Prof Philip Choo
Mrs Chew Kwee Tiang
Ms Magdalene Chai
Mr Roger Leong
Chief Human Resource Officer
Chief Financial Officer
A/Prof Phoa Lee Lan
A/Prof Tan Kok Yang
Dr Lee Kok Keng
Dr Bin Wern Hsien
Deputy Chairman, Medical Board (Care Integration & Clinical Standards)
Deputy Chairman, Medical Board (Service Development)
Medical Director, Yishun Community Hospital
Medical Director, Admiralty Medical Centre
11
CARING FOR OUR KAMPUNG
HEADS OF DEPARTMENTS khoo teck puat hospital Dr Sanjay Patel Dr Bin Wern Hsien Dr Patrick Lim Dr Wu Loo Cheng A/Prof S Tavintharan Prof Wilfred Peh A/Prof Phoa Lee Lan A/Prof Tan Kok Yang A/Prof Angeline Seah Dr Siew Chee Weng A/Prof Wong Moh Sim A/Prof Yip Chee Chew Dr Sandeep Uppal Dr James Tan Dr Goh Kah Hong Dr Teoh Chin Sim Dr Molly Eng A/Prof Lim Su Chi A/Prof Edwin Seet Ms Teresa Foong Ms Supadhara Ramaiyah Ms Jenny Goh Ms Ng Lih Yen Ms Chow Pek Yee Ms Chelsea Law Mr Albert Foo Dr Ng Yeuk Fan Mr Donald Wai Ms Fatimah Moideen Kutty Ms Cheong Choy Fong Mr Liew Phey Bong
Head and Senior Consultant, Acute and Emergency Care Centre Head and Senior Consultant, Anaesthesia Head and Consultant, Cardiology Head and Senior Consultant, Dental Surgery Clinical Director and Senior Consultant, Diabetes Centre Head and Senior Consultant, Diagnostic Radiology Head and Senior Consultant, General Medicine Head and Senior Consultant, General Surgery Head and Senior Consultant, Geriatric Medicine Head and Consultant, Family and Community Medicine Head and Consultant, Laboratory Medicine Head and Senior Consultant, Ophthalmology and Visual Sciences Education Director, Education Development Office Head and Senior Consultant, Otolaryngology (ENT), Head and Neck Surgery Head and Senior Consultant, Orthopaedic Surgery Head and Senior Consultant, Psychological Medicine Clinical Director and Senior Consultant, Sports Medicine Centre Head and Senior Consultant, Urology Clinical Director and Senior Consultant, Clinical Research Unit Clinical Director and Senior Consultant, Office of Clinical Governance Deputy Director, Allied Health Services and Pharmacy Head and Senior Principal Clinical Psychologist, Psychology Service Head and Senior Principal Clinical Pharmacist, Pharmacy Deputy Head and Principal Medical Social Worker, Medical Social Service Head and Senior Principal Physiotherapist, Rehabilitation Services Head and Principal Dietitian, Nutrition and Dietetics Principal Podiatrist, Podiatry Head and Deputy Director, Corporate Communications Director, Corporate Development Director, Hospital Planning and Infrastructure Director, Operations Admin Director, Quality and Risk Management Yishun Health IT Director
Yishun Community Hospital Mdm Chua Gek Choo Ms Chua Ee Cheng Ms Chan Sue Mei Ms Low Suat Fern Mr Adon Chan Hock Kiong
Director, Nursing Head and Principal Medical Social Worker, Medical Social Service Deputy Head and Principal Dietitian, Nutrition and Dietetics Deputy Head and Principal Pharmacist, Pharmacy Deputy Head and Principal Physiotherapist, Rehabilitation Services
population health & community Transformation Ms Low Beng Hoi Mr Bastari Irwan
Director, Nursing Director, Population Health & Community Transformation
We would like to thank the following for their contribution: A/Prof Edwin Seet Head and Senior Consultant, Anaesthesia (until 31 Dec 2019)
12
LIVING WELL
LIVING WELL
EDUCATING AND EMPOWERING OUR COMMUNITY TOWARDS WELLNESS
A Café Supported Self-Management (SSM) session in action. 14
Although she has several chronic illnesses and used to be quite reserved, Mdm Norjahan has nevertheless taken part in several of Yishun Health’s Café Supported Self-Management (SSM) sessions, and even shared her experiences with participants. This did not use to be the case. Previously, the 70-year-old — who has diabetes, high blood pressure, high cholesterol, as well as a left hip fracture — would often stay alone at home with her cats. However, when she was introduced to the friendly and welcoming nurses at her nearby Community Nurse Post (CNP) in 2018, she began to open up about her conditions and limitations. Through regular conversations with and gentle encouragement from Senior Staff Nurse Wen Chao, Mdm Norjahan learnt how to monitor her glucose level and blood pressure, recognise normal readings, and manage her medications. Within three months, she became more independent in monitoring her vital signs and giving herself insulin injections. She made healthy lifestyle changes, such as avoiding sweetened beverages and opting for plain water; she even achieved her goal of doing 30 minutes of muscle-strengthening exercises every morning to prevent falls. Importantly, Mdm Norjahan has access to help whenever she needs it — and actively seeks advice from the community nurse when her readings are abnormal or when she is unwell. Building a healthy community is more than ‘doing’ for others. In fact, Yishun Health’s philosophy on community health is not about deferring to the expertise of medical professionals, but empowering patients, their families, caregivers and even neighbours to play a role in care. Over and above building the infrastructure, the Population Health & Community Transformation (PHCT) team has developed programmes to improve rapport between our Community Care Teams and residents, as well as among residents themselves. Making use of available resources, abilities, networks and services, this model of care shifts from telling to listening, and instructing to interacting. It also moves away from solely giving help to empowering patients to help themselves, stepping in only when necessary. This participatory model builds resilience, gives the community autonomy, and puts health ownership into the hands of people. This has meant immersing teams in the local community and getting to know them over the years through formal and informal means, such as our CNPs, Wellness Kampungs, and more. Through various interactions, our teams have
unearthed ‘hidden treasures’ — unseen strengths, assets, connections, resources and skill sets that can be leveraged to transform neighbourhoods at a collective and systemic level. Since expanding our reach in 2018, residents have started their own community gardens, offered free haircuts, and organised flea markets. This inspiring evolution of our efforts to truly engage, empower and enable our community is the fruition of our Asset-Based Community Development (ABCD) approach.
Empowered individuals, participatory neighbours, resilient communities We believe that everyone is an agent of change — all they need are the tools and support to make this happen. To this end, Yishun Health has built a strong community health network, which forms our foundation of care. Working upstream to focus on health promotion and disease prevention keeps people out of the hospital and living well in their communities. From helping to enabling self-help The PHCT team continues its mission to work with residents and partners to build a sustainable community-based care ecosystem in the North, and support residents there to live well throughout their life stages. The approach is based on ABCD. Since 2016, the team has progressively incorporated the ABCD principles into the way they interact with residents in the community. Under ABCD, the focus is on what is strong (asset-based), not what is wrong (deficitbased). This way, they identify and mobilise underrecognised assets in the community to promote sustainable community-driven development. The ABCD philosophy starts with identifying what residents can do on their own, followed by how their family, friends and neighbours can help, and finally how service providers can serve as a safety net.
WHAT IS THE ABCD APPROACH?
What can you do by yourself?
What can you do with a little help from the people around you?
What do you need us or other agencies to do for you?
15
LIVING WELL
Mr Cormac Russell (second from right), who shared on ABCD with staff, in discussion with fellow panellists at the PHCT Forum.
ABCD gained renewed attention in 2018 through our partnership with South Central Community Family Service Centre and Ang Mo Kio Family Service Centre (AMKFSC). Mr Cormac Russell, Managing Director of Nurture Development and Faculty Member of the ABCD Institute, trained 30 PHCT staff in ABCD principles in February 2019. He also shared an overview of ABCD with staff and partners at the annual forum. Following this, PHCT ran a series of workshops in collaboration with AMKFSC for 55 PHCT staff, together with seven other staff from departments such as Pharmacy, Diabetes Centre, Nutrition & Dietetics, Corporate Communications, and Finance. Additional workshops are being organised under this training programme to reach more staff. As part of the ABCD efforts, PHCT also partners national agencies such as Health Promotion Board, SportsSG, Silver Generation Office, and 16
local agencies such as grassroots organisations, Intermediate and Long-Term Care operators, social agencies, and primary care services. Beyond these, they also work closely with nontraditional organisations such as schools, social enterprises, as well as arts and religious groups. These community partners play an important role in building supported-self managed communities. Together, PHCT builds layers of support that incorporate social and family connections (such as neighbours and relatives) with formal services to address the behavioural, environmental, social and economic factors that contribute to health and well-being. This helps people gain the capability, capacity and confidence to manage their own health. As many residents do not know the extent of health and care services available to them, PHCT also links residents with the appropriate services as needed.
Our partners: • Tzu Chi Humanistic Youth Centre • SHINE Children and Youth Services • Vibrance @ Yishun • Campus Impact • Yishun Town Secondary School • National Civil Defence Cadet Corps • SATA CommHealth • Feiyue Family Service Centre • Christ Church Secondary School Apart from these, PHCT also continues to develop greater capability of self-management in the community — through CNPs and Wellness Kampungs as well as other programmes — moving beyond education to teaching residents to take charge of their health, take ownership of their community, and work together to address gaps and needs. Community Nurse Posts Operating in the community since 2012, PHCT’s CNPs encourage residents with chronic conditions, such as hypertension and diabetes, to monitor their health more regularly. Nurses demonstrate and guide residents on the use of blood pressure monitors or glucometers, teach residents to recognise normal readings, and provide self-management tips. Residents are encouraged to take their own measurements at home and record their own readings prior to their CNP visits. They can also practise taking their own measurements at the CNP. Mobile Community Nurse Posts Mobile CNP brings community care nursing to neighbourhood spaces near wet markets, parks and town councils so as to reach out to more residents, especially to those who are not living near existing CNPs or have difficulty travelling.
CNP IMPACT IN FY2019
13 CNPs + 1 Mobile CNP Yishun and Sembawang
1,624 residents
6 CNPs Woodlands and Marsiling
471 residents
TOTAL HOME VISITS IN FY2019: 341
Travelling to different spaces each week helps the team to ‘discover’ new at-risk residents who would otherwise fall through the cracks. In FY2019,
432 new residents were seen at the mobile CNPs, and 10% subsequently visited existing CNPs. Café Supported Self-Management To take self-management to a new level at the CNP, Café SSM was piloted in November 2019. It offers a safe space for residents who have longterm health conditions, such as Mdm Norjahan, to participate in meaningful conversations on how to better manage or improve their health, and encourage the community to build support networks that can provide mutual support and care. During each hour-long session, residents pool their collective wisdom and resources for peer learning and support. They even set their own healthcare goals and review them weekly, keeping themselves accountable for their own health. Café SSM runs weekly for an average of 10 sessions. In FY2019, 28 participants participated in five Café SSM runs across four CNPs. Their feedback was that they not only gained friendship and knowledge, but many of them also saw improvement in their condition, and were more motivated to maintain good lifestyle habits. Wellness Kampung: our community living room The Wellness Kampung was one of the first steps taken to build a participatory community for Yishun Health. Started in 2017, the network of three wellness and care centres in Chong Pang, Nee Soon Central and Nee Soon East turn void decks into social places where residents meet, bond and support each other. In these spaces, healthcare professionals would also become visible and accessible resources in the community.
2,752 registered residents
29
supported self-management groups
437
residents ‘leaders’
To drive participation, we encourage residents to co-create with us. They have contributed to the programming, environment, operations — even the name ‘Wellness Kampung’ was crowdsourced! The 10 guiding principles regulating the use of the space to establish norms of reciprocity were also developed by our residents. On 26 September 2019, the Wellness Kampung was one of 12 international awardees of the Human City Design Award. The Human City Design Award recognises outstanding and creative projects in sustainable social design 17
LIVING WELL
Our Wellness Kampung initiative getting recognition at the 2019 Human City Design Award.
to overcome the effects of human alienation, materialism and environmental changes. The Wellness Kampung was selected for the way it addresses the major global challenge of ageing populations and how it innovatively connected a community-building process to the creation of support networks and meeting places. Horsing around for happiness Studies show that connecting with animals is beneficial for social-emotional well-being. Based on the positive experiences of past beneficiaries (e.g. nursing home residents, at-risk youths), PHCT partnered Equal-Ark and Nee Soon East Community Centre to start Wednesdays with Horses, the first equine-assisted therapy programme held in a HDB estate. Held at a sheltered basketball court beside Oasis Waterpark, horses assist persons with special needs to develop confidence, self-awareness and life skills. Residents rallied to contribute to the programme, assisting with logistics, promotion and participant support. PHCT also connected the project to their network of partners so that more residents could benefit from it. 18
Eating together to build bonds Share a Pot was launched in 2015 to leverage the Asian cultural norm of communal eating — and using the opportunity to address frailty and isolation, as well as encourage vulnerable elderly to socialise, exercise and eat better. The programme includes group exercises, regular basic functional assessments, and a nutritious pot of soup. This simple concept invites volunteer groups and organisations to take ownership of the programme in their local neighbourhoods, with support from the programme team. Share a Pot has become a platform for neighbours to get to know and look out for one another. Regular Share a Pot sessions are held at 32 community locations island-wide, including Wellness Kampung centres, senior activity centres, religious organisations, and nursing homes. Today, there are 1,758 registered participants and 242 senior volunteers. Students from Admiralty Primary School, Canberra Secondary School, West Spring Secondary School, and Woodlands Secondary School also contribute their time to the programme, forging intergenerational bonds with their seniors.
The main lobby at KTPH is one of the six touchpoints of Heart Zone @ Yishun.
Heart Zone in the North Heart Zone @ Yishun was officially launched on 2 May 2019. Heart Zone is a joint initiative effort by Yishun Health, the Public Transport Council, Land Transport Authority, and SMRT Trains that aims to encourage commuters to assist patients and visitors going to KTPH and YCH from Yishun MRT Station. Heart Zone @ Yishun comprises six touchpoints identified with distinct posters. The posters at these touchpoints, such as the Yishun MRT Station and KTPH main lobby, urge people to offer help to patients or visitors who need help getting to the hospital, accessing nearby shuttle service areas, or finding their way to bus stops. The move helps residents look out for those in need and build stronger community ties.
Prevention and proactive action Our upstream programmes, such as health screening and health coaching, take a proactive approach to health, picking up risk factors and chronic diseases so that early intervention can take place. This can prevent chronic illnesses from developing in the first place, or lower their severity and prevent complications. Our screenings are coupled with initiatives to help residents make sense of the information on their blood pressure, cholesterol, and blood sugar levels. Where needed, they are linked to the services, treatment and resources they need to become educated and empowered to take responsibility for their health. 19
LIVING WELL
Chronic disease health screening: sustaining our reach Since 2013, KTPH has worked with the People’s Association Active Ageing Committees to bring chronic disease health screening to the residents at communal places such as the wet markets and community centres.
2,027 residents screened
727
of whom were reviewed and supported by GP partners
Screenings for seniors-at-risk Project Silver Screen was launched nationally in 2018 to promote early detection of functional decline through opportunistic and scheduled screening of vision, hearing and oral health in seniors, targeting Singaporeans aged 60 years old and above. In FY2019, a total of 4,826 residents were screened.
Residents with abnormal results receive appropriate follow-up by neighbourhood GPs and Community Nurses. They are also offered other lifestyle intervention programmes, such as CHAMP (Coaching for Health Action and Management Programme) and Skills for Life@Community. In July 2019, Yishun Health conducted localised health screening for the underprivileged residents in the Chong Pang and Gambas neighbourhoods by partnering Touch Senior Activity Centre, Nee Soon Spring CC, and Floral Spring Resident’s Committee.
Taking action after screening Health screening is only one part of our healthpromoting efforts. More importantly, we must address the root causes. To this end, PHCT runs lifestyle intervention programmes, targeting individuals who are at risk of chronic disease. Skills for Life! @ Community and CHAMP programmes encourage participants to adopt health-promoting actions:
This benefited 62 residents who would, under normal circumstances, be unreached; 18 of these residents met the criteria for newly diagnosed chronic disease and were referred to our partners — Shenton Medical Group and OneCare Medical — in clinics located close to their home for early attention and management.
1. No free sugar 2. Wholegrain substitution 3. 150 minutes of physical activity every week 4. Half a plate of vegetables at every meal
HEARING
VISION
PHCT partnered NUHS Mobile Hearing Clinic to review seniors with abnormal hearing results at various Community Centres in the North. Since May 2019, an audiologist from KTPH has assessed seniors at the AdMC Ear, Nose and Throat clinic twice weekly for their suitability for hearing aids.
PHCT collaborated with KTPH’s Ophthalmology and Visual Sciences Department to offer optometrist follow-up in the community at Kampung Admiralty Active Ageing Hub and Wellness Kampung @ 115.
DENTAL
PHCT worked with NTUC Unity Denticare Mobile Dental Clinic for scaling, polishing, extraction and fillings. Those requiring dentures were referred to NTUC Unity Denticare dental clinics.
Where needed, residents could get a direct referral to SOCs to allow audiologists and optometrists to assess seniors who require SOC intervention. With this arrangement, seniors enjoy their entitled subsidy for specialist care with less hassle.
20
TYPE OF FUNCTIONAL SCREENING
PARTICIPANTS WITH ABNORMAL RESULTS
PARTICIPANTS FOLLOWED UP
Hearing
2,368
987
Vision
638
455
Dental
813
401
These programmes are considered ‘health action coaching’ because only consistent and persistent action in the right direction brings about the change that we want. In health action coaching, our coaches do not tackle health queries with just health education; neither do they just promote good health. Instead, they focus the conversations on the concrete actions taken by those whom they coach, the positive outcomes they can see when they are successful, and the challenges that they face in their well-intended plans. Small wins are encouraged, big wins celebrated. This helps participants gain confidence and motivation. SKILLS FOR LIFE! @ COMMUNITY
CHAMP
19 runs
109 runs
345 participants
1,066 participants
In FY2019, Skills for Life! @ Community expanded its outreach to partner religious organisations. Culturally sensitive content was co-developed to be relevant and acceptable to communities served by Sri Senpaga Vinayagar Temple, Central Sikh Temple, and AlMuttaqin Mosque. “In July 2019, during a routine visit to the doctor, I discovered that I had severe hypertension. It made me realise that I had taken my physical health for granted for too long, and my blood pressure was a big warning sign. I paid little attention to my diet and rarely exercised. At the time, I weighed 80kg, my heaviest ever. I thought about the consequences of my poor health on my family and decided to enrol in a six-month weight management programme at Khoo Teck Puat Hospital. Thanks to the sound advice and comprehensive support, I managed to bring my weight down to 67kg. I was pleasantly surprised because, for 20 years, my weight has never gone below 75kg! More importantly, my blood pressure improved, my recurring back pain also disappeared, and I am very happy with the overall outcome.” — Victor Seet, 41
Driving health literacy and action in our community Health begins at home and within the community. This is why we undertake many outreach efforts beyond our organisation to engage both residents and our medical colleagues. We take a proactive role to care for our population in the North through a wide spectrum of ways to improve their overall social, physical and even emotional well-being. Addressing ‘diabesity’ AdMC Diabetes Centre organised its ‘Diabetes and Metabolic Symposium 2019: Diabesity Revisited — A Primary Care Focus!’ at Sheraton Towers Singapore on 6 April 2019. Targeted at healthcare professionals, it was well-attended by approximately 300 GPs, nurses and allied health professionals. The transdisciplinary team, comprising doctors, dietitians and psychologists, discussed the rising challenge of diabesity — which refers to the strong association between diabetes and obesity — its complications, the risk stratification, and management options. Participants then attended various breakout sessions on nutrition, psychology, therapeutics and surgery for more in-depth learning. World Diabetes Day 2019: A family effort Yishun Health, together with Active Ageing SG, marked World Diabetes Day and Active Ageing Day on 9 November 2019 at Kampung Admiralty Community Plaza with activities, awareness and
Yishun Health marked World Diabetes Day 2019 with a health fair. 21
LIVING WELL
education in a Diabetes Health Fair organised by Yishun Health. The fair, dubbed ‘The Family & Diabetes’, reinforced Yishun Health’s five pillars of diabetes management: Diet, Exercise, Support, Monitoring and Medication (DESMM). More specifically, the programme emphasised the importance of inter-generational family support in combating diabetes. Gathering to drive healthy seniors and healthy eyes
A combined community event was held at Kampung Admiralty on 5 October 2019 to celebrate a Geriatric Health Carnival and mark Age-related Macular Diseases (AMD) Week. Organised by Yishun Health’s Ophthalmology & Visual Sciences (OVS) and Geriatric Medicine departments, the event’s objective was to engage, educate and empower our senior residents to adopt and lead a healthy lifestyle, preparing them for the transition into their silver years. With the same vision of encouraging these seniors to age healthily and gracefully, OVS provided eye screenings to detect macular diseases. To make the day fun, informative and participatory, the event included fitness and cooking demonstrations, as well as educational exhibition booths on topics such as falls and dementia.
seminar aimed to educate participants on various practical ways of self-care, finding joy in their role, and reassuring them that they are not alone in their caregiving journey. The programme covered lighthearted tips on eating joyfully as well as deeper conversations on Advance Care Planning — all in a safe and comfortable space where they could learn, and show and receive support from one another. Putting the focus on pressure injury
Caring for caregivers
The Caregivers Seminar held on 5 October 2019 was attended by 110 caregivers. Organised by Yishun Health’s Patient Experience Office, the 22
Yishun Health’s Pressure Injury Workgroup commemorated World Wide Pressure Injury Prevention Day with a line-up of programmes. This year’s Stop Pressure Injury Seminar, held on 29 November 2019, was targeted at professional caregivers and clinical staff to create awareness on medical device-related pressure injuries, with a focus on prevention.
Communicate to connect
pain, heart failure, high blood pressure, and heart blockages. Beyond informative sharing sessions by cardiologists, there was also a multidisciplinary aspect to the event. For a holistic approach, the Nutrition & Dietetics (N&D) department, Pharmacy and Rehabilitation Services also set up educational booths to raise awareness on how to maintain good heart health. Steps towards elder foot care
On 2 November 2019, our Speech Therapists marked Speech Therapy Day with ‘Communication, Our Key to Connection’, a meaningful volunteering outreach event in the community. The day brought together 43 speech therapists across NHG for a day of activities with nursing home residents at Sree Narayana Mission Home and Lee Ah Mooi Nursing Home. They organised games and facilitated the creation of memory books, a helpful way for persons with dementia to preserve cherished memories and past experiences. They also took the opportunity to hold an educational talk for nursing home staff on speech therapy and strategies to facilitate communication. Helping to raise self-care for heart health Yishun Health’s Cardiology department’s first Cardiology Symposium, held on 6 April 2019, was attended by more than 300 members of the public. The event was aimed at increasing the public’s awareness and knowledge of various cardiac conditions, such as heart attack, chest
Our Podiatry team celebrated Podiatry Day on 16 April 2019, focusing on nail and skin management in the geriatric population and persons with diabetes. They highlighted issues and conditions such as calluses and corns, warts, and bacterial and fungal infections. In addition to public education, the team supported colleagues in raising skills in foot care, with a workshop for Healthcare Assistants and Geriatric Nurses. Participants were taught how to safely trim the nails for elderly persons with foot conditions, and how to manage nail and skin issues in people with diabetes.
Participants at Yishun Health's inaugural Cardiology Symposium trying out some simple exercises. 23
LIVING WELL
Participants of the Mini Medical School's series on cancer awareness.
When cells don’t die More than 300 participants attended the Mini Medical School’s (MMS) ‘When Cells Don’t Die’ series on cancer awareness. Over the course of three Saturday mornings in August 2019, students from all walks of life gathered to learn about cancer formation and treatment strategies. Providing inspiration were MMS ‘valedictorians’ — cancer survivors who took to the stage to share their cancer journeys with the audience. MMS ‘graduates’ also received certificates of attendance after completing the entire series. This event was complemented by educational and informative booths, and also the launch of Letters to the Stars, a book of letters written by attendees of the 2018 session to departed loved ones. Staying in the pink of health
Some 300 participants attended the Breast Cancer Awareness Public Forum at the KTPH Auditorium on 28 September 2019. The event covered a wide range of topics — some conducted in English, some in Mandarin — on the prevention and management of the condition. It was organised by the General Surgery department, in collaboration with Rehabilitation Services, Psychology Service, N&D, and Food Services. 24
Expanding stroke awareness and prevention
A Stroke Carnival was held on 12 November 2019 to commemorate Stroke Awareness Day. Stroke is the fourth leading cause of death in Singapore, and one in four people hospitalised for stroke is under 60 years old. Organised by the Acute Stroke Unit Workgroup, the event aimed to educate staff and public on how to identify the risk factors for stroke, and the importance of eating healthily and in moderation, exercise and keeping fit, and training the brain to maintain health and wellness. Doctors gave talks on stroke prevention, and there were health screening booths to encourage people to get their check-ups done. More than 200 people visited the interactive educational booths, attended the healthy cooking demonstration helmed by KTPH’s chef and dietitian, and took part in a mass Zumba workout. Tackling youth mental health Recognising the growing mental health needs among youths in the local population, KTPH’s Psychological Medicine (Psy Med) department embarked on a pilot collaboration with Republic Polytechnic (RP) in 2019 to proactively extend mental health service access to the youth, especially those studying in Institutes of Higher Learning.
School-based mental health screening assessments mean students referred by school counsellors can be seen in a more familiar environment less loaded with stigma. Such on-site assessments allow for more holistic assessments and management by taking into account the situations and places they manifest. These screening assessments are also conducted by psychiatrists, allowing students and caregivers to directly address concerns about the conditions and treatments, improving understanding and motivation to seek follow-up care. Together, these reduce: • Barriers to mental health assessments for youths at risk of developing mental health conditions, so as to facilitate early diagnosis • Treatment gaps through early right-siting of care Between May 2019 and January 2020, a total of 13 sessions were conducted and 21 students were reviewed. From available data, 70% of assessed students required and were referred for follow-up care with mental health services. Of these, 50% opted to seek follow-up care at KTPH; 75% of these students were seen in KTPH by the same psychiatrist who had performed the initial assessment for continuity of care. Following this successful pilot, RP has awarded a contract to the team at Psy Med to continue providing this service in Academic Year 2020.
Fan-active about health Health is about taking action in our daily lives to build good habits. To this end, we organise events, develop programmes and services, as well as form partnerships to encourage our community to embrace an active lifestyle. Active Hub The first Active Health Lab within a Medical Centre was launched on 25 May 2019 at AdMC. The firstof-its-kind facility, a collaboration between SportSG and Yishun Health, is aimed at helping residents in the North take ownership of their fitness. The holistic community space offers access to fitness monitoring tools, programmes and activities. Uniquely, the Active Health Lab can initiate referrals to doctors, as well
25
LIVING WELL
as from AdMC physiotherapists to Active Health, integrating the medical and physical aspects of a patient’s overall health. For our patients, this means they can transition from medical care to self-care by being empowered and equipped with skills to own their health and wellness proactively. Sedentary no more!
Taking action to help people overcome a sedentary lifestyle and make better food choices, the Integrated Care for Obesity and Diabetes team organised ‘Don’t Wait to Lose Weight’, a weight management forum in collaboration with Rehabilitation Services, Psychological Medicine and N&D. Held on 19 October 2019 at the KTPH Learning Centre, participants were encouraged to take charge and adopt healthier lifestyles and dietary habits. A selection of workshops, educational booths, cooking demonstrations, and talks gave a holistic and balanced view on weight management. These included practical tips on
exercising effectively and overcoming emotional barriers, adopting healthier dietary habits, and gaining an understanding of the various medical approaches in their journey to weight loss. To drive the message home, patients from the KTPH Weight Management Programme shared personal stories and testimonies of their struggles, perseverance, and small victories over personal health issues with guidance from the KTPH team. The strength to tackle daily life Yishun Health’s Sports Medicine Centre held their annual public forum on 2 November 2019, introducing the more than 200 participants to the ‘what’, ‘why’ and ‘how’ of functional strength. Titled ‘Functional Strength: Improving Function Through Strength’, the day-long event featured speakers who shared their expertise across the different aspects of strength training, such as Olympic Weightlifting, Powerlifting, and Strongman. Beyond explanations on the different styles and their benefits, three other speakers spoke about common injuries and preventive drills, and advocated for proper techniques for safe, effective, and injury-free training. The three strength training experts also displayed their prowess in their respective sports, and involved participants in learning several movements such as the snatch, squats and deadlifts.
Participants at the Sports Med Forum trying out the ‘snatch’ movement as demonstrated by the speaker. 26
Active-ating our community FY2019 was a year of change and progress for KTPH’s Sports Medicine Centre as they continued to provide quality sports medicine care to their patients and the community. The Centre organised a number of community events. One of these was a series of monthly Chinese Medicine Public Talks at AdMC, which concluded on 8 June 2019. Sports Medicine Centre acupuncturists, Melissa Ong and Amanda Chua, shared how acupuncture could help with digestion issues, diabetes, lower-back pain, knee pain, as well as stroke rehabilitation. There was a good mix of English and Mandarin sessions from March to June, allowing more than 200 members of the public to learn more about the benefits of acupuncture. Our Sports Medicine team was also invited by Sembawang Community Sports Club to give talks during their Sports Fiesta, held at Kampung Admiralty on 8 June. Dr Shauna Sim, Resident Physician, shared about keeping fit and preventing sports injuries, while our acupuncturist Amanda shared how acupuncture could help with knee and lower-back pain. Beyond their clinical work and health literacy advocacy, the Sports Medicine Centre also focuses on professional growth and undergraduate and postgraduate medical education. The team welcomed their second trainee in 2019. Various SMC doctors hold teaching appointments in the Yong Loo Lin and Lee Kong Chian Schools of Medicine and the Graduate Diploma in Sports Medicine. They also directed and hosted the inaugural AACES Pain Medicine Ultrasound and MSK Ultrasound courses. Sports Medicine Centre doctors have also made their mark in the community. Many senior doctors hold key positions within standing committees of the Singapore National Olympic Council, Anti-Doping Singapore, and Republic Polytechnic. The team actively provides medical coverage for several sports events, including the SMBC Singapore Open, Singapore Powerlifting Open and Invitational in January, April and September 2019 respectively, as well as the
ASEAN Schools Games in Semarang, Central Java, in July 2019, and SEA Games in December 2019. Other notable highlights: • A new Sports Medicine Service at AdMC that includes an acupuncture arm, which recorded an increasing load of patients through the second and third quarters of 2019 • The growth of the musculoskeletal ultrasoundguided intervention service, with the addition of a new ultrasound machine • A $233,000 MOH Traditional Chinese Medicine Research Grant in a joint effort with the Departments of Geriatric Medicine and Orthopaedic Surgery for post-operative work in hip-fracture patients • A cross-cluster research collaboration with the National University Heart Centre on profiling the hearts of athletes 27
LIVING WELL
The good life: clean, green and healthy! Our pioneering vision of building a ‘Hospital in a Garden, Garden in a Hospital’ is about developing not just a healthcare institution, but a healing environment. It speaks to our mission of holistic wellness — not just the health we have in our physical being, but also in our mind and spirit. This wellness extends to the cleanliness and beauty in our environment. This is what drives our ongoing commitment to build and nurture a sustainable environment, and corporate and social responsibility. Standing up for sustainability KTPH, in partnership with Health Care Without Harm and Global Green and Healthy Hospitals Network, organised and hosted the 5th Green Hospitals Asian Conference, from 8–10 October 2019.
The three-day conference, themed ‘Towards a Sustainable, Climate-resilient Asian Healthcare’ and held for the first time in Singapore, welcomed more than 200 healthcare and sustainability professionals and experts from 25 countries. It was graced by Er Dr Lee Bee Wah, Chairman of the Government Parliamentary Committee for the Environment and 28
Water Resources, and Member of Parliament for Nee Soon GRC. In her opening speech, CEO Mrs Chew Kwee Tiang shared Yishun Health’s long-standing commitment to sustainability as an integral part of our healthpromoting mission. She said that Yishun Health has continued to emphasise the importance of being a health-promoting and environmentally sustainable hospital through the years, despite the changing healthcare landscape. Gladys Wong, Senior Principal Dietitian, N&D, talked about food and waste, and promoted Meatless Mondays. In a separate session, Mr Jerry Ong, Senior Vice President, CPG Consultants — who was involved in designing and building both KTPH and YCH — shared various guiding principles that make up a green building. COO Ms Yen Tan also took the time to share Yishun Health leadership’s culture of sustainability in the campus. Guest-of-Honour Er Dr Lee launched the book Seeking Sustainability — The Khoo Teck Puat Hospital Experience. The event closed with commitments from participants and international representatives to improve sustainability efforts. For KTPH, we pledged to further reduce the plastics and non-biodegradables used in our hospital by looking at more environmentally friendly medical consumables. In addition, we also aimed to reduce our energy consumption by 5%. This will be done through increasing our solar power generation capacity and upgrading our facilities to be more energy efficient.
LIVING WITH ILLNESS
LIVING WITH ILLNESS
MANAGING CHRONIC ILLNESS AS A TEAM Mr Arjan once had more than 16 active appointments for his multiple chronic illnesses. It was no wonder he often felt lost and confused. Under an organisationwide effort to streamline care under a Unified Care Model, Mr Arjan was enrolled in one of our new Integrated Medical Clinics (IMCs).
He underwent a review with Dr Ang Yan Hoon and Senior Care Coordinator Audrey Tan to make his care more efficient. They discovered that as many as four of his appointments were for eye specialists at different institutions. Taking the time to understand his medical issues, concerns and capabilities for
Second from left: Audrey Tan, Senior Care Coordinator, Dr Ang Yan Hoon, Senior Consultant, and Low Suat Fern, Principal Pharmacist, consulting with a patient. 30
self-management, Dr Ang reduced his appointments from 16 to seven. The Ageing-In-Place Community Care Team (AIP-CCT) was roped in to do home visits and further reconcile his medication regime of more than 20 drugs and supplements. Today, Mr Arjan is supported with reminders, advice and guidance over text, phone and emails. This has enabled him to better navigate the healthcare system and access community resources. Having Dr Ang act as his Primary Doctor has also made him more reassured and motivated to make the lifestyle changes needed to keep him living his best life, even with chronic illness. Many chronic and lifestyle diseases are multifactorial — and it makes sense to address them in a comprehensive and sustained way. Yishun Health’s team-based and integrated approach to managing disease addresses the medical, functional, emotional and social aspects of chronic disease for more effective and long-term outcomes. One in four Singaporeans above the age of 40 suffers from at least one chronic disease, be it diabetes, high blood pressure, high cholesterol or stroke. Termed ‘lifestyle diseases’ — because the risks increase with poor lifestyle and habits such as diet, inactivity, excessive stress, smoking and excess weight — they are linked to poor long-term health, disability and premature death. This underscores the importance of not only preventing chronic illness, but managing it well so that patients with existing chronic conditions can stay healthy, active and lead meaningful lives for as long as possible.
Holistic team-based management To transform care and unify it in a way that is truly person-centric, we have strived to use a Unified Care Model that puts patients at the centre of care, connecting them with holistic, transdisciplinary care. In our current healthcare system, patients living with multiple chronic diseases are typically seen at multiple
IMC
PHYSICIAN
specialist outpatient clinics (SOCs), primary care clinics, and polyclinics. While this meets the definition of multidisciplinary care — as many healthcare professionals are involved to tackle different aspects of care — it does not translate to a hassle-free or effective experience for patients. Instead, what happens is that different providers provide multiple care plans, resulting in duplication, inconvenience and added cost. It becomes challenging for patients such as Mr Arjan to understand and participate in their own care. More significantly, it can lead to gaps in care. Unaddressed functional, psychosocial and behavioural factors can then exacerbate the situation, and patients and caregivers become unable to cope. This results in frequent relapses, multiple acute hospital admissions, poor outcomes, disability and poor well-being, and high financial and social costs. Integrated Medical Clinics One way we have done this is through developing our IMCs, the first of which was started in October 2018. It aims to develop a model of relationshipbased shared care whereby patients are managed by a single physician-led team of healthcare professionals. This team takes ownership of the patient’s care; assesses and coordinates his needs across medical, functional and psycho-social domains; and develops and implements a One Care Plan for each patient in consultation with different medical specialists. It is estimated that this three-year pilot will achieve a reduction in healthcare utilisation per year by complex patients, which will result in reduction in healthcare costs. These patients are expected to have better clinical outcomes. Patients and caregivers will also have more confidence and competence in managing their health at home. There are currently a total of five IMC Care teams at Geriatric Medicine, Cardiology, Renal, and Diabetes Clinic, with 129 patients receiving active follow-up.
FIRST ENROLMENT NO. OF PATIENTS ENROLLED
Geriatric 1
Dr Ang Yan Hoon
5 Oct 2018
53
Geriatric 2
Dr Foong Yin-Lin & A/Prof Terence Tang
27 Mar 2019
29
Cardiology
Dr Dinna Soon & Dr Ling Lee Fong
28 Jan 2019
13
Renal
Dr Lim Eng Kuang
9 Sep 2019
12
Diabetes
A/Prof Tavintharan Subramaniam
19 Nov 2019
22 31
LIVING WITH ILLNESS A united effort against diabetes Diabetes is a disease that is multi-faceted — not only in its origins and risk profile, but also its complications. Between 1990 and 2017, overweight and obesity rose from Singapore’s eighth leading risk factor to its fifth. Disabilityadjusted life years (DALYs) caused by overweight and obesity rose 141% during that time. In 2017, overweight and obesity contributed to 6.4% of Singapore’s DALYs, up from 3.9% in 1990. This is why Yishun Health takes a multi-pronged approach to the disease across its campus, driving diabetes care that is person-centred, seamless and sustained. Diabetes care with partners Taking a One Care Plan approach, the Diabetes Centre at AdMC takes a relationship-based, integrated shared-care plan in managing diabetes. This means not just seeing patients, but also leveraging a network of primary care physicians to sustain care. Importantly, patients are equipped with the knowledge and skills to sustain good diabetes care in their daily lives. The goal is to enable them to live well with illness, slow down the progression of the disease, and, in doing so, reduce the risk of complications. • The Diabetes Centre streamlines access to specialist diabetes care • Treatment is customised to each patient • Patients are expected to play an active role in their care, including tracking their blood sugar and more • Patients with stable illness can easily seek care from partner GPs/Polyclinics, and all information is tracked under the One Care Plan for visibility • A structured framework of criteria and thresholds ensure that patients can be appropriately referred to specialists when necessary Integrated Care for Obesity and Diabetes The Integrated Care for Obesity and Diabetes (ICOD) programme tackles excess weight and diabetes in a multidisciplinary way. A holistic care team supports and empowers patients in achieving their goals. After developing and fine-tuning the workflow in the SOC in 2019, ICOD went on to streamline the inpatient workflow for patients undergoing bariatric surgery. Project Corner C, with space and facilities dedicated to the care and needs of bariatric patients, was developed together with specialty nurses in Ward A61. This allows for a more integrated and streamlined flow of outpatient to inpatient for those undergoing Bariatric & Metabolic surgery. 32
2.6% 5.2% 5.2%
On the clinical front, a total of 77 Bariatric Operations performed
87% Primary Operations Revisional Operations
Intragastric Balloon Procedures Body Contouring Operations
30-day readmission rate was 3.9% — three out of 77 cases — all of which were Clavien-Dindo Class III complications; average Total Weight Loss was 27.7% after one year post-op
There were a total of 27 patients (35%) with diabetes or pre-diabetes. After one year post-op, 96% were off medications or on reduced doses, of which 16 (59%) with diabetes went into remission by six months post-op, and seven (26%) with newly diagnosed diabetes never required to start medications postoperatively. Diabetic Foot Service Diabetic foot conditions are often very complex and require the management of many different disciplines, such as General Medicine, Orthopaedics, and General Surgery. Traditionally, the problem is difficult to manage because of the lack of clarity and ownership, leading to poor patient outcomes and high lower limb major amputation rate. The Podiatry team addressed the problem by working closely with the various disciplines in the set-up and refinement of the Diabetic Foot Service (DFS). This takes a multidisciplinary approach to patient care to ensure better screening to pick up problems earlier, address potential serious wounds promptly, and reduce complications. There has been a 35% on-year reduction in major limb amputation rates since its start in 2019. Furthermore, DFS managed to improve the quality of life of our patients with diabetes.
Besides clinical improvements, the team also started a new insole inventory management system to improve productivity. Deploying the 5S methodology, the new process has saved 17.3 hours a year, freeing the team to focus on more meaningful patient care work.
Smarter blood glucose monitoring The Clinical Research Unit (CRU) introduced the Augmented Glucose Monitoring (AGM) Programme in partnership with AdMC in October 2019 to improve diabetes care through strategic periodic continuous blood glucose monitoring. Leveraging smart technology, the programme comprises intermittent scan flash glucose monitoring that is cheaper and more user-friendly than conventional continuous glucose monitoring. Users simply use an adhesive sensor skin patch and the flash glucose monitoring scanner to take a reading — this means no more repeated finger pricking. Complementing this advancement is a scalable AGM toolkit to guide community residents and professionals to better manage diabetes in the community. The toolkit consists of a pictorial guide and a food diary. Two groups of patients with diabetes have been selected for this programme, identified because their susceptibility to large glucose fluctuations predisposes them to complications: • Older diabetic patients with poor glycaemic control and greater risk of hospital admissions. The CRU’s prior research had found that patients aged over 60 years with poor diabetes control had significantly higher HbA1c variability than those with better diabetes control in the same age group.
The AGM toolkit.
• Muslim patients who fast during Ramadan can run the risk of acute metabolic emergencies. Anticipating risks and teaching patients to manage them proactively can mediate the risks during the fasting period. Under this programme, community nurses review flash glucose readings during home visits or at the CNPs. The readings give almost immediate feedback to patients on their daily food and activity choices and help them to adjust their lifestyles. Their primary doctors use the readings in clinical decision-making such as medication adjustment. To date, 25 residents have been enrolled into the pilot.
Eye diseases, we see you! With a rising elderly population, as well as the complications related to chronic illnesses such as diabetes and vascular disease, the focus is increasingly on eye health. More than just treating eye disease when they arise, it has become imperative to move the care upstream so as to detect problems in the early stages. At Yishun Health, the Ophthalmology and Visual Sciences (OVS) department has long taken a concerted approach to holistically address eye care across the spectrum, particularly at the community level, in a bid to speed up early detection. At the clinical level, OVS has also continued to raise the efficiency of care delivery so that it is safer, more productive and, ultimately, better for patients. G-CARE: Glaucoma Community-based Augmented Review and Empowerment In 2017, OVS, PHCT, and the Operation Admin department launched Community & Home Eye Screening Services (CHESS), a collaborative effort to address the gap in eye screening for the vulnerable population.
CHESS / L1 FiLCES L2 SeLECT L3 KTPH AdMC First-level Community Eye Screening
Second-level Eye Care Team
Specialist Outpatient Clinic visit for treatment and management
Trained Nurses & Healthcare Assistants from PHCT
Trained Optometrists
Ophthalmologists
Volunteers from Wellness Kampung & NTUC Health Tele-consult with Ophthalmologists based in KTPH / AdMC
33
LIVING WITH ILLNESS
Since April 2019, OVS has enhanced CHESS by adding on the G-CARE programme. The team, which learnt from similar programmes in Sydney, Australia, as part of the Human Manpower Development Programme, adapted G-CARE for local application. G-CARE adds screenings at the First-level Community Eye Screening (FiLCES) and Second-level Eye Consultation Team (SeLECT) to hone in on glaucoma, which is often asymptomatic in early to moderate stages.
PILOT OUTCOMES Detection of glaucoma-associated abnormalities:
3.8%
8.3%
Projected cost-to-patient outcomes:
$10–$39
increased savings in avoided polyclinic or SOC visits
Projected direct medical cost savings:
$7,012–$12,504
/ patient
Projected hospital manpower cost savings:
$75,000
/ year through use of ophthalmologist-extenders (OEs)
SHORT-TERM BENEFITS
LONG-TERM BENEFITS
Greater access to community eye care
Reduced healthcare costs
Improved management of uncomplicated eye conditions in the community, obviating hospital referrals
Right-siting of eye care
Early detection of eye conditions, especially glaucoma
Lower manpower costs
Timelier treatment and improved outcomes
Promoting community eye care by OEs
One Pack Wonder One Pack Wonder is a collaborative project that improves operational efficiency in the packing of kits used for intravitreal (IVT) injection, allowing nurses to allocate their resources to more important matters, such as patient care. An IVT injection is an outpatient day surgery procedure where medication is injected into the eye to treat age-related macular degeneration, diabetic eye disease, and retina problems to slow down vision loss. To prepare for each procedure, a kit requiring about 14 individual consumable items is needed. About 50 kits are pre-packed every Saturday by two eye clinic nurses for use over the following week. It takes about two hours to pre-pack these 50 sets. To raise efficiency and also identify a more cost-effective alternative, OVS worked with the Materials Management department to outsource the packaging of IVT consumables. 34
A look at the contents of the One Pack Wonder.
PRE-PACKED IVT SET ONE PACK WONDER (TO-BE) (AS-IS)
SAVINGS
Operational cost
$27.55
$3.15
$24.40 (89% savings)
IVT packing time
4m 48s
0s
4m 48s (100% savings)
Preparation time
1m 39s
37s
1m 2s per procedure (62.6% savings)
Annual cost savings: $58,560
Man-hour savings: 249 hours
Time savings can be allocated to 260 more cases/year
Project REMOVE OVS has greatly enhanced and streamlined cataract surgery at Yishun Health, making it safer, quicker and more convenient for patients. As part of efforts to further improve, REMOVE (Removal of Eye Medications for Value-add and Efficiency) — a collaboration between OVS, SOC and Day Surgery Centre (DSC) — was introduced in May 2019 as part of the well-established Lean Cataract Surgery Care Path. Typically, patients undergoing cataract surgery are asked to use Prophylactic Preoperative Antibiotic Eye Drops (PPADs) for three days prior to surgery as a means of reducing infection of the surgical site. However, this requirement leads to: • Inconvenience for patients as they need to visit the pharmacy and wait to collect PPAD after their clinic consult • Decreased productivity and multiple levels of engagement. OVS has to educate patients on the use of PPAD, the pharmacy has to dispense the drops, and DSC has to contact patients to remind them to start PPAD • Potential rescheduling of surgery as patients
sometimes forget to use the PPAD • An increased risk of drug-related adverse reaction or allergy due to the use of multiple eye drops • Over-prescription as there are already existing intra- and postoperative protocols to reduce the risk of infection Reviewing medical literature to assess the efficacy of PPAD and whether it is essential as a preoperative step, the team found that PPAD is not crucial to reduce postoperative eye infection. During a onemonth pilot, two senior surgeons operated on patients who forgot to use PPAD. No complications were reported. Based on the results obtained during the pilot period, REMOVE was rolled out to all cataract surgeries, except for special cases. Exclusions include patients who are immunocompromised, undergoing IVT injections, and who have a history of severe eye infections. Between December 2018 and December 2019, a total of 1,982 cataract surgeries were performed without PPAD, with no reports of postoperative eye infection.
REMOVE FOR BETTER, FASTER, CHEAPER AND SAFER CARE
AS-IS
Patient visits Eye Clinic
Patient listed for cataract surgery
Patient is informed to use preoperative antibiotics eye drops
Patient proceeds to cataract surgery
Patient collects eye drops from pharmacy
Did patient use eye drops?
YES
NO
Patient to use eye drops 3 days before surgery
Cancellation of surgery 35
LIVING WITH ILLNESS
REMOVE FOR BETTER, FASTER, CHEAPER AND SAFER CARE
TO-BE
Patient visits Eye Clinic
Patient listed for cataract surgery
Patient proceeds to cataract surgery
RESULTS BE
TT
ER S FA
Cancellation rate reduced due to removal of PPAD
SOC, DSC and Pharmacy can spend their resources on other matters
TE
R
No additional trip to Pharmacy
1,982 HOURS SAVED Transdisciplinary Urology Care 2019 was a pivotal year for the Department of Urology as they embarked on expanding and deepening its services. Minimally Invasive Surgery for Uro-oncology This minimally invasive surgery (MIS) has been a focus of care, emphasising its continual improvement in functional outcomes without compromising oncological outcomes. In all, 24 patients benefited from MIS upper tract (kidney/ureter) cancer surgery in 2019. With increasing diagnoses of incidental small kidney tumours due to abdominal scanning for unrelated problems, there is a rising demand for laparoscopic partial nephrectomy. From 2018 to 2019, the department performed 23 such procedures and referred several others for ablative procedures by Interventional Radiology. Consultants Dr Shum Cheuk Fan and Dr Raymond Chung demonstrated and shared the transdisciplinary nature of this unique oncological problem at a clinicalpathological conference on 1 November 2019. Pelvic oncology Patients with locally advanced bowel, bladder and prostate cancer suffer from significant morbidity. With the ageing population and higher life expectancy, the demand for this service is expected to increase. A collaborative surgical effort between Colorectal Surgery, Urology, and the Early Recovery After Surgery (ERAS) teams optimised the oncological and functional outcome for these complex cases. In 2019, three such cases were identified to be suitable for this collaboration. 36
CH
EA
PE
R
Patients no longer need to buy PPAD
SA
FE
R
No ocular allergy, side-effects or toxicity
$1,684.70 SAVED Genito-urinary reconstruction Occurring in 0.6% of men, urethral stricture disease is a relatively common condition that is conventionally treated by endoscopic incision or dilatation, followed by debilitating regular selfdilatation. The team is now able to offer buccal mucosa graft reconstruction of urethral strictures (BMG urethroplasty), resulting in improved satisfaction and reduced risk of recurrence. To date, two patients have undergone BMG urethroplasty with excellent outcomes. For penile and scrotal cancers, and diseases that involve significant degree of skin loss, close transdisciplinary collaboration between the extirpative Urological surgeon, the Plastic Reconstructive surgeon, and the wound nursing team has achieved optimal holistic functional and cosmetic outcomes. Other minimally invasive therapies Going forward, the department aims to provide more non- and minimally invasive procedures. This includes low-intensity extracorporeal shockwave therapy for the treatment of erectile dysfunction, Peyronie’s Disease, and Chronic Pelvic Pain Syndrome. Medical education The team continues to be highly involved in Resident, Medical Student, GP and Nursing education. They participated actively in the local urological conference (UroFair) in April 2019, held a GP symposium on 20 July 2019, and offered three urology nursing courses in 2019.
CRISIS AND COMPLEX CARE
CRISIS AND COMPLEX CARE
INNOVATING TO IMPROVE PATIENT OUTCOMES When Mdm Yap had an intestinal obstruction that necessitated emergency laparotomy surgery, it was an anxious time for her and her family. The 79-year-old has multiple co-morbidities, including Alzheimer’s disease. One night after the operation, Mdm Yap’s anxiety heightened when she did not see her daughter, Agnes — her main caregiver — and began shouting and crying inconsolably in the ward. To alleviate Mdm Yap’s anxiety, and as part of the emergency surgery pathway, a geriatrician attended to her promptly to adjust her mood medications. The nurse manager of the ward, at the request of Agnes, also shifted her to a bed nearer the window to help her be more comfortable. These efforts calmed Mdm Yap, and she made an uneventful recovery back to her baseline functions. Today, she remains well and is on regular follow-up with both her geriatrician and surgeon in KTPH. For Agnes, the level of care her mother received was exemplary — not only in clinical terms of her acute care needs. Quite apart from the successful operation, it was the patience, understanding and person-centred care that made the crucial difference. She noted that her surgeons, Dr Clement Chia and Dr Marc Ong, made efforts to allay the family’s anxieties, and showed great understanding and patience towards their worries about Mdm Yap’s ability to 38
withstand the operation. Nurse Clinician Chen Yanyan also ensured Mdm Yap was cared for and comfortable. Agnes appreciated the team’s holistic, humanistic approach, which viewed her mother as not just a patient and a medical crisis, but as a person with specific social, emotional and psychological needs.
Care beyond the crisis When it comes to acute medical issues such as stroke, trauma, broken bones, and heart attack, there is more to care than life-saving surgery or treatment. The care goals for those who require immediate or acute care include not only attending swiftly to the immediate medical problems, but more importantly, seeing to the restoration of health, function and quality of life.
General Surgery and Geriatric Medicine clinicians from the ELAP team (From L-R): Dr Jerry Goo, Senior Consultant; Dr Clement Chia, Consultant; Dr Marc Ong, Consultant; Dr Grace Lim, Associate Consultant; Dr Priscilla Ng, Associate Consultant.
Yishun Health takes a holistic and transdisciplinary approach to support patients in their recovery through pre- as well as postoperative plans. This involves early, accurate diagnoses and prompt interventions. This is important to address and resolve medical issues before complications develop. This is crucial as the healthcare landscape moves to better address rising challenges, such as the growing burden of chronic disease, a rapidly ageing population, and its concomitant rise in agerelated conditions. Crisis and complex care at Yishun Health is about coming together as a team and improving longterm outcomes. We ensure that we can add value through the work we do as a healthcare organisation, delivering the best possible
outcomes for our patients at the most affordable cost, while also considering their physical, emotional, functional and even social well-being. To ensure this, Yishun Health uses models, such as the Optimal Care Index (OCI), to push for value-based care over and beyond the objective and immediate measure of success posttreatment. OCI is a novel holistic index that incorporates a patient’s function, cost and experience into the traditional clinical model. It is a composite score that divides patient outcomes (measured using the Patient Value Compass score) by the total cost. Ultimately, it is about helping patients adapt to living well with their conditions and regain as much independence as possible so that they can live their lives to the full. 39
CRISIS AND COMPLEX CARE Raising the level of emergency care In line with our philosophy of raising the bar on acute care while also taking a longer-term, wholeof-person approach, the Acute and Emergency Care Centre (A&E) continually innovates to offer better holistic care. Ambulatory Emergency Care Service Patients with acute medical conditions often need urgent clinical review, diagnostic tests, medication administration, and subsequent ongoing clinical reviews. However, many do not strictly need to be warded for these procedures. Unfortunately, financial and insurance incentives, coupled with the lack of alternative options for acute emergency care, usually result in a hospital stay.
To reduce the need for unnecessary admission, the A&E piloted a concept adapted from the United Kingdom. The Ambulatory Emergency Care (AEC) service admits patients to the A&E’s Extended Treatment and Diagnostic Unit for a few hours. This allows them to get the tests, treatment and opinions they need. The patient then gets discharged and can return the next morning for a review by the medical team and repeat tests or medicine titration, if needed. The consultation charge of this review is absorbed into the initial inpatient cost, minimising out-of-pocket costs, which the patient can pay with MediSave. This way, patients get fast and definitive care while still being at home with their families, and avoid the risks and costs of a hospital stay. A five-month pilot of AEC for patients with conditions such as very high blood pressure and anaemia resulted in: • 128 avoided admissions • An average savings of $419 in hospital bills for subsidised patients • 1.2 fewer days in hospital Projected over a year, AEC can potentially save 423 inpatient bed days and $274,950 for these two conditions. The team hopes to expand the diagnostic inclusion criteria and open the service to other medical specialties. Refining acute and emergency for seniors Before the implementation of the Geriatric Emergency Medicine (GEM) project, geriatric patients who visited the A&E were treated the same way as other non-geriatric patients despite more complex-care circumstances.
The AEC team ensures that everyone is kept up-to-date on their patients' progress with regular team huddles.
Geriatric patients are now given priority triage and taken care of by GEM nurses trained to perform geriatric assessments and identify complex care needs. Besides being evaluated for acute medical management, all elderly patients are given frailty and confusion assessments. With a holistic picture of each elderly patient, a more comprehensive pathway of care can be implemented, which will continue either in the inpatient or community setting.
After she collapsed at home and briefly lost consciousness in January 2020 in the dawn hours, Mdm Loh presented at the A&E, where she had a CT scan that revealed a small tumour in her brain. Instead of being admitted, the AEC team identified her as suitable for discharge home the same day after expedited tests and specialist opinions. She was admitted to the AEC Unit at 2.30pm and, after a review by specialists, was sent home on the same day at 7pm, with specialist follow-ups planned. This saved her from a hospital stay as well as admission fees. “All the doctors were caring, very efficient in their job scopes,” she shared. “It saved me an admission that could have kept me in the hospital for a few days. I really appreciate the calls to follow up after my discharge.”
40
This enables the team to create more effective discharge care plans for patients. To cater to the follow-up care needs of GEM patients, dedicated slots have been created for direct referrals, as well as an early review clinic and Community Care Teams. A pathway for direct transfer to YCH is now also in place for patients who require intermediate care and/or rehabilitation.
Working with Corporate Development, the outcomes of ELC on patients were studied using the OCI, and compared to delayed laparoscopic cholecystectomy, which is typically performed up to six weeks later. A comparison study of 254 patients found that this Acute Surgical Care Model (ASCM) transformed the delivery of care of AC and showed excellent clinical outcomes.
Medical Home services run by AIP-CCT works with the A&E to identify patients whose care needs could be met by their enhanced services, avoiding acute admissions.
At the heart of person-centred care
GEM outcomes: • 392 referrals • Avoided admissions • Early follow-ups Using the Optimal Care Index to measure outcomes for acute cholecystitis Acute cholecystitis (AC) is an inflammation of the gall bladder that occurs when a gallstone obstructs one of its ducts. It is a condition requiring surgery, and is one of the most common surgical emergencies. At Yishun Health, the Department of General Surgery implemented early laparoscopic cholecystectomy (ELC), offered by the A&E’s Emergency Surgery and Trauma (ESAT) service — a dedicated surgical unit.
Cardiovascular disease is one of the leading causes of poor health, disability and death in Singapore and across the world. While advancements in treatments and drugs are vastly improving the survival rates of cardiac events, there are many challenges in long-term care and management, particularly in compliance with upstream risk factors, such as diet, smoking and exercise. The goal is thus to transform overall care in an integrated-team approach, and achieve outcomes based on the Patient Value Compass. Heart failure project A hassle-free end-to-end heart failure (HF) care pathway was developed to tackle the poor prognosis typically associated with HF. Consisting of Cardiologists, Case Managers, Advanced Practice Nurses (APN), Cardiac Pharmacists, Allied Health Professionals, and Operations Admin, the integrated transdisciplinary HF Unit was formed to:
Some members of the Acute Cholecystitis team at their poster presentation in Poland. 41
CRISIS AND COMPLEX CARE
CLINICAL OUTCOME
Conversion Rate
Emergency Readmission to General Surgery (GS) within 30 days ASCM
300
10%
1.7%
250
6%
200
4%
150
2.3%
2% Pre-ASCM
Operation Duration (mins)
11.0%
12%
9.8%
Pre-ASCM
ASCM
Mean=139
Mean=121
100 50
0%
Pre-ASCM
0
ASCM
FUNCTIONAL OUTCOME
EXPERIENCE OUTCOME
Patients Ambulating by Post-op Day (POD) < 1
Patient Satisfaction Score
80% 60% 40% 20% 0%
58.80%
Pre-ASCM
87.60%
EARLY LAPAROSCOPIC CHOLECYSTECTOMY (ELC)
74.80%
86.10%
Pre-ASCM
ASCM = ACUTE SURGICAL CARE MODEL
ASCM
ASCM
COSTS-TO-PATIENT OUTCOME Early Laparoscopic Cholecystectomy Rates
100% 58.5%
50%
41.5%
0%
Hospital Length of Stay (days)
15.7%
40
84.3%
30 20
Pre-ASCM
ASCM
10
Interval (delayed LC) - elective Index (early LC) - emergency
ASCM Pre-ASCM Mean=5.5
Mean=4.8
0
OPTIMAL CARE INDEX
COSTS-TO-DELIVER OUTCOME Pre-ASCM
Pre-ASCM
ASCM
OCI per $1,000 spent
OCI per $1,000 spent
=
90.3 = 10,607 * 1,000 = +8.5
$10,164 $10,607
ASCM Cost difference not significant
42
46.2 10,164 * 1,000 = +4.5
• Reduce avoidable readmissions • Improve clinical and functional outcomes of patients upon discharge • Provide high-quality cardiac care while keeping costs affordable to patients An early post-discharge review clinic run by APNs was set up, and patients could access direct phone contact with a Case Manager for post-discharge queries. This continuity of care improved early interventions and reduced A&E readmissions. In 2018, there was a 30.8% improvement in functional class outcomes at the point of discharge compared to the same functional measurement during the point of admission. Many patients also reported increased satisfaction in the perception of health benefits as they encountered less disruption in their daily lives, such as work schedules, while also receiving support to manage their HF condition.
The presence of APN Case Managers also improved anticipatory care through advocating for preventative measures, such as vaccinations against pneumonia and influenza, as well as the implantation of devices for long-term HF management. These measures resulted in better survival, functional capacity, and quality of life. Between 2018 and 2019: • Three-fold increase in vaccinations • Rate of Implantable Cardioverter Defibrillator or Cardiac Resynchronisation Therapy devices increased from 0% to 42% In 2019, 94% of patients (336) on the HF pathway received nurse education to self-manage exacerbated symptoms, leading to: • Greater ownership of health and well-being • Collaborative approach to health
The Heart Failure team with their poster presentation. 43
CRISIS AND COMPLEX CARE
HEART FAILURE UNIT
CASES DELAYED DUE TO HDU BEDS REQUIRED
UNPLANNED READMISSIONS WITHIN 30 DAYS OF DISCHARGE 2016 9.96%
2019 7.17%
< National target of 13%
EARLY MEDICATION INITIATION AND REVIEW COVERAGE IN 2019
510 patients (99.8% of patients)
INPATIENT MORTALITY RATES Pre-2017 2%
2017–2019 0%
Driving radial access for acute coronary syndrome Patients who have undergone percutaneous coronary intervention (PCI), such as an angioplasty or stent surgery, via their femoral artery — located in the upper leg — typically require high dependency unit (HDU) monitoring for their wound and heart rhythm. However, this procedure has a higher risk of wound complications, including retroperitoneal bleeds and large haematomas. At Yishun Health, interventional cardiologists have moved towards a predominantly radial access via the arm and adopted snuff-box/distal radial access for suitable end-stage renal failure patients. This reduces complications associated with the femoral approach; patients are also able to move and walk earlier.
2017
2018
2019
278
226
159
Total PCI via femoral and radial access
1,053
1,159
1,138
Decreased femoral access PCI (%)
26.4%
19.4%
14.0%
Femoral access PCI
Since implementation of the Non-ST-elevation myocardial infarction (NSTEMI) pathway, patients have been moved to Wards B65 and B66, reducing the use of HDU and Critical Care Unit (CCU) beds. This is despite an increasing number of patients presenting with myocardial infarction. The number of patients who need to be transferred back to the CCU also reduced, from 17 patients in 2018 to 13 patients in 2019. Overall, these initiatives have significantly reduced the case delay and improved patient access to definitive care earlier despite higher volumes and increased utilisation of the lab. 44
2017
2017
2018
2019
34
66
89
9
LDL cost-savings project Since 2018, the move towards monitoring lowdensity lipoprotein (LDL) instead of a full lipid panel has continued to translate to savings for patients. A total of 10,359 LDL tests were conducted between April 2018 and March 2020, translating to significant savings for patients. Expansion of the Device Implantation service His bundle, left bundle, and right bundle pacing are emerging techniques that deliver physiological electrical activation of the heart. There is a growing body of evidence to support these forms of pacing as best practice. Favourable clinical outcomes include a reduction in heart failure arising from standard right ventricular apical or septal pacing. In order to innovate, the Arrhythmia team reviewed the scientific data, explored the implant technology with different vendors, and completed a pilot assessment of implantation in KTPH patients. They established the appropriate indications, selected the appropriate equipment, introduced correct laboratory procedure and post-implantation checks, and confirmed early safety and efficacy. The team now has a platform to expand physiological pacing to all cases, affording patients the published clinical benefits.
Adding value and compassion to colorectal surgery Over the years, the Colorectal Service at KTPH has developed a team that provides high-quality, compassionate, and individually tailored patient care for all colorectal conditions, including colorectal cancer. The focus of the service is to provide value-based care with core ‘value pools’ that have the greatest impact on outcomes, spending, and patient experience — this aligns with MOH’s ‘value-consciousness’. The Clinical Quality Index (CQI), a quality tool, has been developed by a national value-based healthcare workgroup under MOH for colorectal cancer to compare and benchmark clinical outcomes and costs across restructured hospitals. Using Yishun Health’s OCI, the team drives value not just by raising the level of surgery, but also by • Improving screening uptake in targeted populations • Refining referral protocols for symptomatic patients • Ensuring efficient use of their endoscopy capacity • Involving multidisciplinary teams • Providing timely and effective emergency surgical care • Consistent provision of palliative care
CQI: CLINICAL OUTCOMES AND COST: 2018
• Enforcing standardised follow-up protocols and tracking results
KTPH CQI (%)
National Average CQI (%)
Anterior Resection
79.1
57.6
Type of Procedure
COLORECTAL SERVICE AT KTPH: STATISTICS 2019
Patients seen at SOC
11,656
Colonoscopies performed
3,164
Right Hemicolectomy
61.1
53.8
FIT+* patients screened
1,800
Left Hemicolectomy
60.0
62.5
Surgeries performed
1,041
Major surgeries performed
CQI for colorectal cancer: for CQI to be 100%, all five of the following criteria must be met: 1) Post-op length of stay <5/6days; 2) 30-day complication rate; 3) 30-day return-to-OT rate; 4) 30-day readmission rate; 5) Inpatient mortality rate.
210
* Faecal Immunochemical Test (FIT) positive The team has pioneered the establishment of key surgical service lines, such as the Geriatric Surgical Service, and enhanced recovery protocols in the region. These care systems have enabled the service to achieve enhanced value in terms of better patient health outcomes and higher productivity by reducing average length of stay and increasing manpower productivity.
Hassle-free integrated care for emergency laparotomy Emergency laparotomy (ELAP) is commonly performed as life-saving surgery for patients with acute abdominal catastrophic conditions, such as bowel obstruction and perforation. They have higher risk of mortality and post-surgical complications of up to five times greater compared to high-risk elective surgery. A big challenge is that
PATIENT FLOW EMERGENCY LAPAROTOMY STEP 1
Preoperative treatment and procedures at the A&E Care Centre A&E Doctor, General Surgery Doctor
STEP 2
STEP 3
Postoperative care and recovery in the general ward, HD Unit or ICU Geriatrician, Physiotherapist, Dietitian
Emergency surgery in the operating theatre Consultant Surgeon, Anaesthetist
STEP 4
Post-discharge care and follow-up in the community Community Care Team
45
CRISIS AND COMPLEX CARE
CLINICAL OUTCOME Patients with Post-operative Complications Clavien III-V
30-Day Mortality
5.3%
19.1%
ELAP
Pre-ELAP
12.3%
EMERGENCY LAPAROTOMY (ELAP)
3.1%
Specialists Presence in OT
Consultant Surgeon Consultant Anaesthetist
92.1
Pre-ELAP
ELAP
Patients >65 years old reviewed by a Geriatrician
92.6%
58.6% 45.1%
30.9%
15.0%
Pre-ELAP
ELAP
Pre-ELAP
ELAP
FUNCTIONAL OUTCOME Patients Ambulating by Post-op Day (POD) 2
EXPERIENCE OUTCOME
Perceived Well-being
Patient Satisfaction Score 87.52%
89.0%
46.7%
30.0% 86.48%
87.4%
Pre-ELAP
ELAP
Pre-ELAP
ELAP
Pre-ELAP
ELAP
COSTS-TO-PATIENT OUTCOME Gross Bill Size (SGD$)
Average Length of Stay (days)
$32,128
15.6 days
$27,947
14.2 days
Pre-ELAP
ELAP
Pre-ELAP
ELAP
OPTIMAL CARE INDEX Pre-ELAP
ELAP
OCI per $1,000 spent
OCI per $1,000 spent
23.7 = 32,128 * 1,000 = +0.7
46
=
46.8 * 1,000 = +1.7 27,947
patients undergoing this surgery are often older people with complex medical issues, and require varying types of care from many parts of the hospital within a limited period time. To circumvent these challenges, KTPH redesigned and introduced an integrated emergency laparotomy pathway in 2019 to streamline and standardise best-practice care processes to ensure delivery of consistent perioperative care. This transdisciplinary, hassle-free laparotomy pathway, which includes timely geriatrician input, has helped improve clinical outcomes and value delivered to patients. ELAP implements both Yishun Health’s Patient Value Compass Score and OCI to quantify the impact. ELAP has resulted in: • Higher proportions of patients who receive better preoperative assessment • Increased specialist presence in surgery and holistic geriatric management in the general ward • Improved transdisciplinary teamwork satisfaction, efficiency and positive synergy
Driving Neurosurgery towards the future Apart from taking care of patients with head injuries, brain tumours, as well as neurovascular and spine pathologies, the Neurosurgery team has a strong focus on clinical research, and translating research and technology to improve patient care. In collaboration with educational institutes in Singapore, the team is investigating new methods of reconstructive surgery with the use of 3D printing to offer better outcomes to trauma patients. On top of that, they are leveraging technology to push out telemedicine as a way to enable faster and more efficient patient care while protecting patients’ data security. On top of teleconsults, patients may soon be able to obtain online prescriptions, medical certificates, and even make online payments in the near future. Another exciting area of research is a partnership with the National University of Singapore to look at using modified stem cells for the treatment of brain cancer. So far, in-vivo experiments and animal models have yielded promising results.
Enhanced recovery after Total Knee Replacement With the ageing of an active population, the management of degenerative joint disease has become even more challenging as patients are no longer content with a sedentary lifestyle. A Total Knee Replacement (TKR) can restore a
patient's mobility, enabling him to participate in social and recreational activities. However, this procedure has traditionally been associated with significant downtime due to pain, stiffness and a prolonged hospital stay. With this in mind, a transdisciplinary team of doctors — including orthopaedic surgeons, anaesthetists and geriatricians — physiotherapists and administrators was formed to look into how we can improve the recovery process of patients undergoing knee replacement surgery. A standardised workflow — comprising preoperative exercise and education rehabilitation classes, effective multi-modal pain management strategies, modern anaesthetic techniques, and accelerated postoperative rehabilitation — means that patients can now look forward to a pain-free joint replacement process that has them walking as soon as the day after surgery. The protocol for TKR has also allowed patients to return home earlier, with 40% of patients discharged just one day after surgery, and reduced overall length of stay among kneereplacement patients by 1.4 days. This allows patients to recover and recuperate in their own homes, thus reducing the demand on hospital beds. In addition, these improvements were accomplished with fewer complication rates and an improved OCI. Looking forward, the team will look at working with community rehab partners so that patients are further optimised pre and post joint replacement surgery.
Expanding the realm of possibilities The KTPH Plastic, Reconstructive and Aesthetic Surgery Service epitomises the concept of transdisciplinary team-based care. Close collaboration with various specialties within Yishun Health has become the norm, transforming and enabling surgeons to tackle more challenging and complex cases with the knowledge that reconstruction is an available option. The wide-ranging collaboration has allowed them to expand their services to include: • General Plastic and Reconstructive Services with General Surgery and Urology teams • Body Contouring procedures for post-bariatric surgery patients after massive weight loss • Combined Plastic Surgery-Podiatry clinic services for diabetic foot reconstruction patients • Facial Trauma services • Aesthetic and Cosmetic Plastic Surgery 47
CRISIS AND COMPLEX CARE
The Plastic Surgery team was part of a transdiciplinary care team that took care of a patient who underwent a successful reconstuctive surgery of her abdominal wall.
The cornerstone of Plastic Surgery is adding quality years of life to patients, enhancing both physical as well as psychosocial well-being. Their reconstructive procedures have allowed them to: • Salvage limbs otherwise destined for amputation • Surgically clear cancers and infections that were not possible without reconstruction • Restore patients’ self-image and confidence, especially for breast reconstruction and post-bariatric reconstructions • Drive earlier healing of complex wounds, allowing earlier return to function • Better scarring and cosmesis Additionally, the team has continued to train and nurture the next generation of doctors and plastic surgery specialists, conducting many in-house workshops, including a flap dissection cadaver workshop and a rib fixation cadaver workshop. They also frequently engage their trainees and young doctors to learn in both the operating theatre as well as the outpatient setting. 48
The Plastic Surgery team organised a flap dissection cadaver workshop for the next generation of doctors and plastic surgery specialists.
LIVING WITH FRAILTY
LIVING WITH FRAILTY
A PERSON-CENTRED APPROACH TO GERIATRIC CARE
Members of the Ageing-in-Place Medical Home team (From Lâ&#x20AC;&#x201C;R): Ernie Yanty Bte Borhanudin, Senior Staff Nurse; Jason Tan Jing Sheng, Senior Staff Nurse; Dr Foong Yi-Lin, Senior Staff Physician; Kng Han Nee, Senior Staff Nurse; Dr Boh Toon Li, Consultant.
When she developed a urinary problem, 94-year-old Mdm Yue sought care at the KTPH A&E Care Centre. In a typical scenario, it would have involved a sevenday stay in order to receive intravenous (IV) antibiotics. Instead, under a new initiative for frail elderly, she was fitted with an indwelling catheter and discharged. 50
She was then treated in the comfort of her home by our Community Care Team under the Medical Home (AIP-MH) programme. Nurses visited Mdm Yue at home to deliver the three-day course of antibiotics and monitored her recovery. She was soon better and discharged from the programme after nine days.
Mdm Yue’s daughter was grateful that her mother could avoid a hospital stay but yet receive ‘hospitallevel’ treatment in the comfort and convenience of her own home. Having access to 24-hour phone support and weekend visits conducted by the AIPMH team gave her the assurance that her mother was well taken care of. Compared to $1,470 for a hospital stay, the bill for Mdm Yue came up to $540. This was a win-win situation — greater affordability for our patients, and more hospital beds freed up for acute cases. AIP-MH is just one of the many services delivered under Yishun Health's Ageing-in-Place Community Care Team (AIP-CCT) programmes. They underscore Yishun Health’s strong belief in person-centred care, which is especially sharpened when it comes to taking care of seniors. Geriatric care is not just about addressing biomedical issues, but personhood, too — someone’s personal history, values and preferences. In fact, over and above medical needs, psychological and social aspects as well as quality of life often take centre stage. This ensures that the person — not just patient — is always at the centre of care. In FY2019, we worked to address the ongoing challenge of frailty. Frailty poses a complex problem; this segment of patients requires intense levels of care, yet sometimes responds poorly to medical treatment. The hospital environment is not always the ideal place for the physically and cognitively frail. To enhance care standards for this vulnerable group of patients, there was a concerted effort to understand and tackle frailty as an organisation. Together with the Geriatric Education and Research Institute (GERI), a multidisciplinary hospital-level workgroup was convened in 2019 to develop a united nomenclature and conceptualisation of persons at risk using a Clinical Frailty Score. This understanding has been the keystone in not only improving care in the inpatient setting, but, more importantly, building a robust care and support system to provide multifaceted, multidisciplinary care that keeps patients such as Mdm Yue out of the hospital and well cared for in their homes and community.
Connecting patients to quality, right-sited care Yishun Health formulates services to match the needs of frail patients, delay progression of frailty, and guide curative treatment at an intensity suited to their needs. Ageing-in-Place Community Care Teams Patients, especially older ones, often prefer to be at home and in the community rather than in the hospital wards. With the right support at home, patients are able to achieve a good quality of life. They and their caregivers also gain more independence, agency and self-efficacy. Established in 2011, AIP-CCT supports, at their respective homes, patients with complex medical and psychosocial issues, and older patients at risk of hospital re-admissions. These nurse-led Community Care Teams, which are supported by multidisciplinary healthcare professionals, visit patients who are unwell but stable and require longer holistic care within community settings after their discharge from hospital. AIP-CCT also provides support for quality, end-of-life care (turn to page 59 to read about the palliative aspects of care). In FY2019, AIP-CCT expanded its spectrum of home healthcare services to better serve the heterogeneous needs of patients: • Hospital-to-home services were extended beyond the previous six-month cap for patients who have chronic relapsing or recurrent symptoms. • Early supported discharges offer rehabilitation at home to patients who require active rehabilitation (e.g. stroke, hip fracture, post-surgical patients) as an alternative to a community hospital stay. • A new discharge to assess pathway allows medically stable patients from the A&E or Extended Diagnostic Treatment Unit (EDTU) to return home for functional or psychosocial assessments (see page 40 to read about Ambulatory Emergency Care Service). • Medical Home, which provides treatments previously only available in hospitals to homes (read more on page 60).
AIP-CCT HOSPITAL-TO-HOME SERVICES (INCLUDING PHONE FOLLOW-UP SERVICES) APRIL–SEPTEMBER 2019
TOTAL EPISODES: 3,247 / TOTAL UNIQUE PATIENTS: 2,958 180 days pre-intervention
180 days post-intervention
Reduction
KTPH Admissions
2,300
1,389
911 (-40%)
Length of Stay (Days)
17,292
10,950
A&E Visits
2,697
1,706
6,342 (-37%) 991 (-37%) 51
LIVING WITH FRAILTY
NUTRITION & DIETETICS The Department of Nutrition and Dietetics works with teams across Yishun Health, playing an essential role in care plans and supporting the team-based holistic management of patients. To drive seamless and integrated care, the team has streamlined the e-documentation of medical nutrition notes to improve the workflow of information and continuity of care within the campus. This has helped greatly in their numerous collaborations, which include: • A transition feeding guide developed to empower ward nurses in managing patients’ nutrition care while transitioning from tube feeding to oral diet. • A hepato-pancreato-biliary project that provides cohesive and seamless transdisciplinary care from diagnosis through to surgery and recovery for patients requiring major liver/pancreas surgery. This has led to lower postoperative complication rates, lower average length of hospital stays, and inpatient cost savings. • Working with our renal nurse coordinators and National Kidney Foundation (NKF) in the Know Right, Start Right programme. This raises patients' dietary knowledge to prevent urgent dialysis and delay kidney function deterioration among chronic kidney disease patients, while ensuring optimal nutrition intake. This has helped caregivers become more aware of how to care and support their loved ones, and improved patients’ understanding of their diet. • Setting up a Frailty Class with physiotherapists to teach pre-frail elderly how to eat healthily for bone health, as well as improve the nutrition status and decrease sarcopenia. • Initiating the Nutrition Optimisation and Support in Hospital (NOSH) pilot in partnership with nurses and health care assistants in December 2019, with the goal to attenuate malnutrition rates in an acute hospital. The pilot was successful, and work is underway to expand NOSH hospital-wide. • Working with Speech Therapists and Food
Keeping seniors mobile in the community Community mobility — being able to walk or use public transport to get around — is essential to health and well-being. It means being able to go to the market, join in social activities, and safely get around with more confidence. One aspect of community mobility is getting in and out of cars or taxis safely, especially for patients using wheelchairs. To help educate patients and caregivers on car transfers, Yishun Health Occupational Therapists (OTs) have been using a model taxi as part of rehabilitation sessions. Located 52
Services to review and improve textured modified food for patients with dysphagia in accordance with the new IDDSI (International Dysphagia Diet Standardisation Initiative) guidelines. Trainings and audits were conducted by speech therapists, while dietitians worked closely with Food Services to ensure quality and consistency of the food. • Promoting healthy cooking and developing recipes involving eight ingredients or fewer together with Food Services and Lifeworks in our monthly cooking demo for staff. These recipes were also contributed to aha magazine. The team has also engaged our community through awareness and educational efforts across many platforms, including newspaper and magazine articles, TV and radio broadcasts, social media, and public events. Driving dietetics research Apart from day-to-day clinical work and supporting patients in their nutritional needs and goals, the team continued to look at ways to innovate and cater to future challenges. In FY2019, they tapped on the Enterprise SG Grant and collaborated with Faesol and Singapore Institute of Technology to develop a locally sustainable thickening agent for dysphagia patients. Senior Principal Dietitian Gladys Wong initiated the idea of 3D Food Printing with Nanyang Technological University (NTU) and, together with NTU as CoPrincipal Investigator, secured S$99,600 funding from National Additive Manufacturing Innovation Cluster (NAMIC) to explore research potentials in a two-year project entitled “3D Food Printing for Elderly and Patients with Chewing Difficulties and/ or Dysphagia”, which ended on 1 October 2019. The results were promising and led to an expansion of the research team at Singapore University of Technology and Design (SUTD). Together with KTPH and NTU, SUTD secured further funding worth S$649,600 from both NAMIC and SUTD to explore “Enabling Digital Gastronomy for 3D Food Printing” from 8 November 2019 to 8 July 2021.
at the Tower D basement 2 car park, this model car offers a safe and supervised way to practise and learn how to conduct car transfers tailored to a person’s specific impairments and precautions. Here, they can find the most suitable method to make car transfers easier. This may include the use of assistive devices such as transfer boards. It also lets patients and caregivers familiarise themselves with the sequence of movements and become comfortable with putting away wheelchairs. The sessions also facilitate conversations among OTs, patients and their families on alternative ways of engaging in community mobility.
nurses and North West CDC. These student volunteers then conduct fortnightly home visits in a bid to bridge generational and healthcare gaps. More than 1,000 student volunteers from secondary schools and universities work in tandem with our community nurses, doctors and allied health providers, helping to increase the frequency of home care visits. Through building rapport, the seniors are encouraged to take better care of themselves. It goes beyond the medical factors and looks after the seniors’ social life, behaviours and environmental settings. PlayKaki: sports for all
Patients with impairments and their caregivers learn how to conduct car transfers safely according to their specific needs with this model car, located in the basement car park of Tower D.
Celebrating a milestone as Tri-Generational HomeCare @ North West turns five.
Engaging the community to drive ageing-in-place We have formulated community-driven services in the Yishun Health healthcare landscape to match the needs of frail patients, delay progression of frailty, and guide curative treatment at an intensity suited to their needs. Tri-Generational HomeCare @ North West turns 5! PHCT's Tri-Generational HomeCare @ North West celebrated its fifth anniversary on 16 November 2019. To mark the occasion, the KTPH Auditorium was abuzz with about 90 people, made up of PHCT’s partners, including its student volunteers and alumni, North West Community Development Council (CDC), and representatives from Tan Tock Seng Hospital and Singapore General Hospital (SGH). This milestone is a reflection of PHCT’s good and sustainable work in caring for our senior residents. Today, TriGen is even expanding beyond the North — National University Health System and SGH have joined the family, expanding support to seniors living in other parts of Singapore. TriGen is a student-led initiative that extends social and health advocacy support to at-risk seniors who do not have close-knit families in their homes. Led by NUS student volunteers from the Medicine, Nursing, Pharmacy, and Social Work faculties, students under this programme go through basic healthcare, caregiving and befriending training by our community
Tri-Generational student volunteers, supervised by a nurse, extending support to an at-risk senior.
Adapted sports, like any other sports, provide physical, cognitive and emotional benefits. It acts as a common ground, building an inclusive community to optimise each patient’s abilities beyond their illness. A previous initiative to introduce adapted sports met with some barriers, including declining participation of patients and volunteers. Thus, PlayKaki was conceptualised to better engage patients in adapted sports. Since January 2019, Rehabilitation Services has collaborated with Yishun Health's Volunteer Management Team to create a safe space for people of different abilities to interact and experience inclusivity through sports. In July 2019, PlayKaki began as a novel, volunteer-led programme 53
LIVING WITH FRAILTY
for others. It even initiated a discussion that led them to befriend and provide social support to other stroke patients in the ward. This has been very encouraging, and the team hopes that such a ground-up initiative and the synergy from it can be replicated to create a self-sustaining stroke community in the North.
Enhancing the patient experience
An adaptative bowling game being played during a PlayKaki session.
with adapted bowling. It achieved better patient engagement through sports, with 97.7% patients expressing interest in participating in future sessions. This was achieved by empowering passionate community volunteers to facilitate adapted sports through specific training, and constructing an environment beyond therapy such that patients can look past their disability and discover the best versions of their abilities. PlayKaki volunteers are diverse and include persons with disabilities; this gives a deeper meaning and significance to the programme’s inclusivity. Feedback from the volunteers found high volunteer engagement with an average score of 82.2% on the Utrecht Work Engagement Scale. Supporting recovery process of stroke survivors Developing and maintaining a healthy lifestyle to prevent stroke recurrence can be a challenging and uphill task for stroke survivors. Social support in the recovery process can empower stroke survivors to manage life after stroke — coping with new disabilities and multiple lifestyle adjustments. With this in mind, the Medical Social Service (MSS) team developed a Stroke Survivor Support Group (SSSG), in collaboration with Singapore National Stroke Association, to help patients overcome challenges in their post-stroke recovery process. The SSSG programme provides coaching to increase confidence and ownership in survivors through six sessions on, respectively: • Stroke and Symptoms • Risk Factors • Healthy Lifestyle • Exercise • Emotional Management • Recap and Community Resources To maintain its relevance and impact, the sessions are reviewed to ensure consistency in knowledge and skills. Participants have benefited not only from gained knowledge and skills, but also friendship, empowerment, self-acceptance, and compassion 54
Yishun Health has built senior-specific clinical pathways and programmes that seek to better support elderly and frail patients with multiple, poorly managed conditions or life-limiting illnesses. Facilitating stroke recovery by Therapy Assistants The Rehabilitation Services team started a Therapy Assistant (TA)-led group therapy initiative for Acute Stroke Unit patients in March 2019 to improve the functional recovery and psychosocial well-being after acute stroke. After suffering an acute stroke, patients often have a wide range of impairments, including physical impairments as well as low mood and depression due to changes in their functional status. This can lead to decreased engagement and participation, which can negatively impact functional recovery. Typically, group therapy for stroke patients is conducted in community hospitals during their longer stays. However, this weekly initiative moves up the process to the beginning of the rehabilitation journey. Suitable patients are selected by physiotherapists based on a strict set of inclusion criteria, which includes medical stability and functional mobility. Guided by handover notes provided, the TAs and trained volunteers run the 45-minute sessions, which comprise up to six patients. This early rehabilitation approach has been positively received by patients. It also has the benefit of helping to upskill TAs, train community volunteers, and improve outcomes for patients who have complex needs.
A training session for TAs who are going to lead group therapy for stroke patients.
Let’s Eat Together: building bodies and bonds
The ‘Let's Eat Together’ initiative encourages communal dining among elderly patients.
Elderly patients are at high risk of low food intake during hospitalisation. Typically, eating alone, in bed, or being fed under time constraints can have negative effects on their appetite, mood and sense of independence. Studies have shown promising results on food intake in the elderly when they eat with others. This person-centred care approach offers a positive and pleasant social environment that potentially improves patients’ oral intake, well-being and independence in the acute care ward. To this end, the ‘Let's Eat Together’ initiative introduced communal dining at Ward D87 to create a pleasant social eating environment. The ward team identifies patients who are suitable and encourages them to sit out of bed to have lunch together with other patients in a more social and interactive ambience.
Impact on patients: • More motivated to feed independently • Reinforces sense of self-efficacy and maximises abilities • Enhances the dining experience, mood, and improves food intake • Greater sense of purpose and control, which improves well-being • Facilitates functional and overall recovery as well as early discharge A more liberating inpatient stay Bed rails are a barrier to mobility and associated with functional decline. They also induce patients with dementia to climb over the rails. The absence of a selection criteria to identify patients who are suitable to be mobilised, coupled with staff’s fear of a patient’s falls risk and misalignment of care practices have resulted in bed rails being raised all the time. As such, the Rehabilitation Services team set out to attain better quality patient care by establishing a balance between fall prevention and promotion of patients’ autonomy, mobility and dignity in acute care wards. A total of 15 patients were recruited in the intervention group, and seven patients in the control group.The Clinical Frailty Scale (CFS) was utilised to guide the appropriate use of bed rails. Patients with CFS score ≤4 had their bed rails lowered daily from 7am–8pm. Physical function was assessed on admission and discharge. There was no falls incidence in either the intervention group or the control group (bed rails raised). Importantly, there was a modest increase in physical function compared to patients in the
30S CHAIR STAND TEST
12
10 8 6 4 2 0
CONTROL
INTERVENTION
Patients in the bed rails intervention group showed a greater improvement in the total repetitions achieved within 30s than the control group.
Change in performance (%)
Change in performance (%)
LOWERED BED RAILS PROJECT TIMED UP AND GO 0 -1 -2 -3 -4 -5 -6 -7
CONTROL
INTERVENTION
Patients in the control group had greater decline in gait speed than patients in the intervention group.
55
LIVING WITH FRAILTY
Visiting Expert Dr Karl Tomm (in blue shirt), from the Calgary Family Therapy Centre, conducted training for staff and community partners of our Family Counselling Service.
control group. Subsequently, the team hopes to implement an induction programme for all ward staff regarding the use of CFS to assess patients and guide them on the appropriate use of bed rails. Ward physiotherapists will continue to train nursing staff on the use of walking aids and assistance during mobilisation.
provided by psychiatrists and psychologists. Referrals are made by in-house psychiatrists and psychologists with patient consent. Patient and family members are invited to the family sessions, and a systemic approach is used to assess the familiesâ&#x20AC;&#x2122; interaction patterns and stressors, as well as their strengths and resources.
Improving dysphagia management The Dental department worked with Speech Therapists (STs) in a Six Vitals project to train and improve knowledge of STs in the oral care of patients with dysphagia. The training included recognition of oral conditions and their timely referrals. It culminated in a poster at the 17th Singapore Health and Biomedical Congress in 2019, which won the Best Poster Award in the category of Health Professions Education (see page 75).
Through compassion and curiosity, the sessions seek to understand their situations and challenges, and enable them to feel understood and empowered to work on their family issues. This generative and collaborative process highlights and enhances the familyâ&#x20AC;&#x2122;s strengths, and helps them to connect better with each other while encouraging them to utilise their own innate resources to resolve difficulties.
Partnering colleagues in Geriatric Medicine, a Clinical Practice Improvement Programme was also set up to improve oral cleanliness in geriatric patients of Ward B65. The objective was to identify patients with poor oral hygiene and increased risk of developing aspiration pneumonia. There are follow-up plans to roll out the initiative to other wards. Family counselling to work out issues In February 2019, MSS set up a Family Counselling Service in collaboration with the Department of Psychological Medicine to assist patients with family issues. Complex family dynamics contribute to or play a part in perpetuating poor mental health, and is something that individual counselling cannot adequately address. Family counselling is a bid to address issues in a comprehensive way, and complements treatment 56
An average of 17 sessions are conducted across two half-day clinic sessions a week as well as clinic sessions in a month. Each hourlong session cost $40 for subsidised patients, and can be assisted by MediFund. It has since benefited 26 families. In the first quarter of 2020, the team started using outcome monitoring tools to measure family satisfaction and improvement of well-being. With the changes to clinic operations due to the onset of the COVID-19 pandemic, in-person sessions were reduced; secure video conferencing technology was used instead for family sessions. The team was trained by Visiting Expert Dr Karl Tomm, of Calgary Family Therapy Centre (CFTC). He provided annual week-long trainings to KTPH staff and our community partners from 2017 to 2019. Dr Cheang Ka Man, Dr Goh Kah Hong and Medical Social Worker Suzanna Lee also did their HMDP training in family therapy at CFTC in Canada.
LEAVING WELL
LEAVING WELL
PROVIDING A QUALITY END-OF-LIFE
The Programme IMPACT team (From L-R) Wong Sue May, Senior Staff Nurse; Dr Tan Shu Zhen, Resident Physician; and Thilagavathy D/O Muthusamy, Senior Staff Nurse; speaking to a patientâ&#x20AC;&#x2122;s next-of-kin (in purple) at their home. 58
Since May 2018, Mdm H has been cared for by the Ageing in Place-Community Care Team (AIP-CCT) for complex medical needs and frailty. She had been frequently admitted to hospital due to diabetes, heart failure, kidney failure, respiratory issues, and multi-level compression vertebral fractures. With the expansion of AIP-CCT services and the introduction of the Medical Home (AIP-MH) programme, she has been supported through her ups and downs, reducing admissions to the hospital. When she was given an end-of-life six-month prognosis in April 2019, Mdm H was referred to the Integrated Management & PAlliative Care for the Terminally Ill non-cancer patients (IMPACT) Programme. Through Advance Care Planning conversations, the care team learned that Mdm H hoped to stay at home, where she could continue to enjoy eating, watching TV, and playing mahjong with her family. She also wished to pass away at home with conservative management and symptom relief. Through regular home visits and telephone calls, the team of doctors, nurses and occupational therapists managed Mdm H’s symptoms and trained her family in the area of comfort-care support. On 1 July 2019, Mdm H experienced fluid overload and a urinary tract infection, but was reluctant to be admitted to hospital. For eight days, the AIP-MH team visited her daily to administer IV diuretics and was on standby 24/7 to give advice on urgent care. After her condition stabilised, Programme IMPACT continued to support Mdm H up until her eventual death on 27 August 2019. Mdm H’s daughter expressed her appreciation to AIP-MH and Programme IMPACT for extending comfort and care to her mother in her final days. The team had helped to fulfil her mother’s wishes for a peaceful last journey at home, surrounded by her family members. Yishun Health’s mission to provide quality healthcare spans the spectrum of care along the River of Life. It extends from early prevention and swift diagnosis to holistic management and person-centred treatments. It also encompasses the delivery of compassionate care at journey’s end. Ensuring comfort and dignity during the final stages of life-limiting illnesses when curative treatments no longer work involves a different type of care that is less medicalised. While medications, treatments and procedures may still carry on, the focus is on providing relief from any symptoms, physical pain and mental stress that may arise from serious illness. More importantly, this form of care strives to keep patients in the familiar surroundings of home and among loved ones. Not only does this add to the quality of life for patients, it also reduces the
financial and time burden on family members. By creating a supportive network of care, and enabling caregivers with the skills and resources, patients can continue to receive appropriate levels of care that keep them out of the hospital. The Cognition 6th Vital Sign (6th VS) initiative conceived last year has not only shaped our care delivery for the frail elderly, it also extends to our end-of-life care to ensure dignity and personhood at every stage of a person’s journey. Guided by these principles, Yishun Health has rolled out various initiatives to offer continuity of care while also optimising existing services and support. We also continue to strengthen the palliative care landscape through capacity-building programmes so as to ensure that community partners are equipped to provide support.
Home-based care, comfort and support Yishun Health provides comprehensive care and support to patients and their families that see to their medical, physical, psychosocial and spiritual needs for the end-of-life, as well as concurrently with curative care in both inpatient and outpatient settings. Making a meaningful IMPACT on end-of-life care In the case of Mdm H, as her prognosis worsened, her care team transitioned her from the AIP-MH programme to Programme IMPACT. It was started in September 2018. The home care team — comprising palliative medicine physicians, palliative-trained nurses, medical social workers and counsellors — provides regular home visits and phone consultations. The goal is to improve the quality of life for patients through providing symptom relief as well as psychological, social and spiritual support to them and their families. The team works in close collaborations with cardiac, renal, respiratory and other medical organ specialists to fill the gap for patients with end-stage organ failure of the heart, kidney or lung. In FY2019, 30 patients were enrolled into the service, and more than 835 home visits were carried out by the team. Palliative care in the community Beyond delivering home-based care to patients with complex medical and psychosocial issues, the AIP-CCT programme takes care of patients with life-limiting illness as well. Such palliative care services to patients at home seek to relieve their symptoms and improve their quality of life. This allows AIP-CCT to deliver person-centred care that enables patients to age comfortably 59
LEAVING WELL
AIP-CCT HOSPITAL-TO-HOME SERVICES APRIL–SEPTEMBER 2019
TOTAL EPISODES: 216 / TOTAL UNIQUE PATIENTS: 208
KTPH Admissions Length of Stay (Days) A&E Visits
Reduction
180 days pre-intervention
180 days post-intervention
188
79
109 (-58%)
2,043
821
1,222 (-60%)
196
89
107 (-55%)
in place after discharge, and avoid the stress of unnecessary hospitalisation. Receiving medical care at home In 2019, AIP-CCT started a new initiative to support patients with medical needs at home. The initiative — a collaboration between Family and Community Medicine Department and PHCT led by Dr Wong Sweet Fun and Dr Ang Yan Hoon — is for selected patients presenting at the A&E and Acute Geriatric Assessment Unit as well as AIP-CCT patients. Patients include those who are Activities of Daily Living (ADL)dependent with heart failure, fluid overload, cellulitis, urinary tract infection, and gouty flare.
AIP-MH, together with caregivers, adopts a multidisciplinary patient-care approach over a short course of seven to 10 days with a mix of home visits and round-the-clock phone support through weekends and public holidays. It provides hospital-level care to the home, such as intravenous antibiotics, physiotherapy, or nursing treatment previously only available in hospitals. Receiving treatment in an exclusive environment reduces the likelihood of acquiring cross infections, or errors due to wrong-patient identification, especially for frail elderly patients who are not able to communicate. It is also especially beneficial for patients with cognitive impairment as it minimises any change of physical environment and caregivers. The familiarity of moving around and using toilet and bath environments already tailored to their routines reduces confusion, falls, incontinence, or incontinence-associated dermatitis and pressure injury; while a good night’s sleep in their own beds without disturbance at night reduces delirium and promotes healing. While the AIP-MH service did not reduce hospital length of stay or readmission to acute hospital, the average cost of providing such care was $2,484 per patient, 19% less than an average of $3,081 per patient in the inpatient group. The average bill size to an AIP-MH patient was also 60% smaller ($384) than that of the inpatient counterpart ($961). Enabling and empowering our community partners Programmes such as GeriCare have been made possible through the Shared Care Partnership Office (SCPO), which was established to integrate patient care as they transition from community to hospital, and back from hospital to the community.
60
A personhood-based approach to dementia care Dementia is a complex problem that requires a holistic approach. To help our staff better understand the disease and care for patients with delirium and dementia, we held a series of monthly courses under our 6th VS initiative. As of January 2020, more than 450 ground staff in Yishun Health have undergone the training. Assessment of the Knowledge, Attitudes and Practice of staff post-training showed a statistically significant improvement in average scores. As classroom training was suspended during the COVID-19 pandemic, an e-learning programme with self-assessment MCQs was developed and will be implemented. Beyond courses, the 6th VS initiative was also applied to our A&E, where a triage protocol was implemented. Cognitively compromised patients are now prioritised for admission into the CAre for the Mentally Infirm Elder (CAMIE) ward, failing
which they are channelled into geriatric wards, which have the extra staffing capacity and training to provide specialised care for this group of patients with high care needs. Furthermore, a 6th VS consult team provided assistance to patients who exhibited challenging behaviours, such as agitation, refusal of care, or other combative conduct. A six-month review showed that 6th VS intervention resulted in improved patient outcomes compared to those without it â&#x20AC;&#x201D; with shorter average length of stay, as well as reduced 30-day readmission rates and 30-day A&E visits. In December 2020, a multidisciplinary team of 10 nurses, a therapist and a doctor from our geriatric wards participated in a four-day in-house training course on Humanitude. This is a personcentred care methodology that emphasises care techniques and strategies that draw on the innate and residual abilities of vulnerable and dependent
Aunty Doreen (in wheelchair) was one of our patients whom participants worked with during the sessions. Initially fearful of even standing, she was eventually convinced to take a walk after our staff employed Humanitude communication tools to engage and interact with her.
61
LEAVING WELL
older people to secure their well-being and quality of life. The techniques stress the four pillars of human connection — gaze, touch, speech and verticality (upright position) — which are also techniques that help socialise newborns into human relationships. These elements are also the very elements often missing in the lives of cognitively compromised seniors. Reinstating these in the lives of these seniors, including those deemed to be beyond help, is aimed at restoring — to varying degrees — well-being. During the course, participants witnessed the profound effects of Humanitude. A patient who persistently refused to stand because she was fearful of falling was cajoled into standing and even walking. Another patient with advanced dementia who was intermittently screaming was soothed into a gentle slumber with caresses and lullabies. It is hoped that, in the coming FY, more staff can be trained in Humanitude to enhance the well-being of our seniors and help staff rekindle greater meaning and joy in their work.
SCPO strives to ensure that patients have their own primary-care physician. This ensures that patients are supported for common acute ailments, and the management of long-term conditions. To this end, SCPO partners GPs, polyclinics and Family Medicine Clinics. In FY2019, the team matched 243 medically stable Specialist Outpatient Clinic (SOC) patients to their preferred primary care physicians for continued care in the community under the Outpatient to Community programme. Depending on clinical complexity, patients are either discharged to or have their care comanaged between the specialist and the primary care physician. Partnership Officers also take the opportunity to educate patients to take ownership of their health and practise self-management. SCPO connects GPs to community resources such 62
as Community Nurse Posts for chronic disease monitoring, education and coaching between doctor visits. This arrangement helps to improve the management of patients’ conditions while optimising the use of GP resources. When allied health services are required, Northern GPs can send their patients directly to AdMC for a same-day appointment, which drives greater convenience for patients and early investigation and treatments. Yishun Health also organises Continuing Medical Education (CME) events to help medical professionals such as GPs to keep abreast of the latest developments in medical care. At the events, GPs, Family Physicians and Specialists exchange expertise to improve the way they care for and manage their patients. In FY2019, 14 CMEs were conducted for more than 1,000 doctors. SCPO has expanded its reach beyond primary care and works with community partners — including nursing homes (for initiatives such as GeriCare) and community care service providers — to create a community-based care ecosystem. Enhancing nursing home access to specialist geriatric care The GeriCare programme was conceptualised in 2010 with the purpose of enhancing the quality of care and therefore the quality of life of residents of nursing homes. It leverages technology to provide access to specialist care to nursing home residents of eight nursing homes in Singapore. Using telemedicine, it provides clinical care support to the nursing homes’ nurses and doctors, while training and supervising the homes’ nurses in geriatric and palliative nursing care. Under GeriCare, members of a team of clinical educators and geriatricians are on call daily from 9am to 5pm to advise on semi-urgent cases. Nursing home residents can also be referred directly for admission to KTPH via teleconsults without having to go through the A&E. A virtual specialist outpatient clinic In March 2019, GeriCare started TeleSOC, which enables consultations on geriatric issues to occur via video so that patients need not visit the hospital for appointments. This also allows clinicians to review the patients earlier, enabling timely intervention to prevent and anticipate deterioration where possible. In FY2019, the team served 32 patients. In addition to setting up the physical structure and process for conducting TeleSOC, they also trained the geriatric medicine SOC nurses, and developed standard work instructions and workflows to carry out TeleSOC in alignment with the National Telemedicine Guidelines and in compliance with PDPA.
RESEARCH AND EDUCATION
RESEARCH AND EDUCATION
DRIVING KNOWLEDGE, MAKING A DIFFERENCE Building research capacity as well as developing capabilities form the driving force of our mission to provide quality, affordable and integrated team-based healthcare. As such, above and beyond ensuring that our clinical operations run smoothly, we invest in people and time to identify gaps, conduct research, and drive quality improvements so that we can tackle important healthcare issues and challenges. We also equip our healthcare professionals with the skills and knowledge to strengthen our ability to rise up and meet long-term needs.
64
The Alexandra Health Fund (AHF) drives a large proportion of Yishun Health’s research work. In FY2018, it supported 17 key programmes directed at improving the quality of life of our patients. AHF was incorporated as a Company Limited by Guarantee and a registered charity under the Charities Act in September 2014. It has since benefited over 300 patients annually with financial assistance. It helps patients to live independently in the community through support services such as transportation and home care, medical equipment, consumables, and medical treatment across Yishun Health. Such initiatives consistent with AHF objectives are aligned to Yishun Health’s key focus to build ‘health resilience’. This means keeping the population well through health promotion, illness prevention, as well as empowered self-care and crisis management. AHF supports Yishun Health's UCM, and funds programmes that encourage the community to manage their own health independently. These programmes may target complex patients transitioning from or entering acute to communitycare settings, patients with chronic diseases who can be better managed by primary care physicians and supported by our community nursing teams, and residents living in the community to support each other. In FY2019, AHF awarded new grants to: • Two scholarships for nurse leaders • IDEAL: The Inspiring Diabetes Enablement and Active Living programme promotes diabetes self-management by addressing the daily challenges patients face • Diabetes and metabolism research, ‘Life journey with diabetes (and beyond): the next league’ • A dance community interest group and a song community interest group to increase the engagement of community-based interventions for residents with respiratory-related illness. These activities can help manage symptoms of breathlessness and prevent falls among seniors • Clinically relevant research projects that contribute directly to improved patient care, enhanced clinical research capabilities, and demonstrate potential in translating basic discoveries into the prevention, diagnosis, treatment and cure of diseases • YCH to fund pressure-relieving mattresses • The Living Well Fund for patients in palliative care to fulfil their wishes and live with dignity
Educating the next generation of medical leaders The Education Development Office (EDO) oversees and coordinates the delivery of pre-employment clinical training. These include pre-professional
AS OF MARCH 2020, AHF HAS $168 MILLION IN ITS COFFERS
$200,000
Yishun Health’s Nursing Leaders Scholarship
$150,000
AdMC Diabetes Programme
$47,000
General donations (including Giving.sg)
$11,000
Yishun Health’s Human Resource Development (KTPH surplus)
education programmes for students reading medicine, nursing and allied health, as well as graduate medical education for residents and postgraduate year 1 (PGY1) programmes. The EDO team also ran a wellness programme on mindfulness, conducted by the Psychological Medicine department, for educators and students to manage burnout. Through experiential learning, participants were taught to be more emotionally aware, attuned to signs and symptoms of burnout, and learn how to manage accordingly. Inter-professional education workshop Inter-professional education is paramount in developing effective and functioning medical teams that are able to navigate the complex healthcare
PRE-PROFESSIONAL EDUCATION PROGRAMMES 11 months of training with an aggregate of more than 12,000, 22,000 and 1,500 student-days for medical, nursing, and allied health respectively. GRADUATE MEDICAL EDUCATION 254 residents were posted to Yishun Health and aggregated about 837 training months’ training for up to 165 PGY1s at 55 trainees per rotation.
65
RESEARCH AND EDUCATION
context. Recognising this, EDO and Rehabilitation Services brought together doctors and therapists in a well-received workshop for nurses on Respiratory Care in an Acute and Community Setting. Medical Hub for Faculty and Medical Students Mooted by Dr Toh Hong Chuen, Head and Senior Consultant, A&E, KTPH, and Associate Dean, Yong Loo Lin School of Medicine, NUS, this one-stop seamless portal is scheduled to commence in late 2020. It was developed for the medical faculty and medical undergraduates to support teaching and learning. The medical administrative team for this project was led by Dr Ong Chye Sun, Deputy Director, EDO. Training@YH The EDO’s Graduate Medical Education team and Yishun Health’s HR department co-developed training@YH, an online portal to capture mandatory courses for residents and PGY1s. This provides real-time updates of courses attended, including certifications, expiry dates, and exemptions. This also allows clinical departments to monitor and track course attendances. This replaces the laborious manual tracking by individual departments, and facilitates access by the junior doctors rotated to other departments. Residency programme in plastic surgery Yishun Health has been accredited as a participating institution for plastic surgery. The first enrolment of medical residents began in July 2020. This takes the total number of graduate medical training programmes to 35.
THANK YOU, MEDICAL EDUCATORS!
On 20 September 2019, EDO organised the annual Teachers’ Appreciation Day to commend and honour teachers and clinical education leads in medical, nursing, pharmacy, and allied health, as well as the heads of departments, for their commitment and support in delivering high-quality medical education to develop future medical leaders. A/Prof Yip Chee Chew, Education Director, announced the integration of Residency Programme Office into EDO, and the re-organisation of EDO into three units: Pre-Professional Education, Graduate Medication Education, and Education Development. This will optimise resources and manpower utilisation, and better align EDO with the working structure and philosophy of the NHG Education Office.
66
Elevating care through science Yishun Health’s clinician scientists, doctors and other healthcare professionals are committed to seizing every opportunity to delve into research that improves care for patients. From understanding the basis of disease and finding better ways to diagnose them, to enhancing the ways we deliver interventions, we collaborate to have more effective methods for disease prevention, treatment and management. Definitive early diagnosis and treatment for familial high cholesterol A/Prof Subramaniam Tavintharan Familial hypercholesterolemia (FH) is a genetic disease that impairs the body’s ability to remove ‘bad’ low density lipoprotein (LDL) cholesterol from the blood. Compared to people in the general population, individuals with FH have up to 20 times increased risk of having heart disease and stroke at an earlier age (before the age of 50 years). To emphasise the seriousness and severity of FH, people with FH have more than seven times the risk of developing coronary heart disease for the same level of LDL-cholesterol as those without FH. Children of parents with FH have a 50% chance of inheriting the disease. FH is under-diagnosed and under-treated. The true prevalence of FH in Singapore is unknown. One reason for this is that there is no standardised method of identifying and diagnosing individuals with FH in Singapore. Recent global data suggests that approximately one in every 200–300 people could suffer from FH. Extrapolated to our Singapore population, we could have up to 27,500 individuals in Singapore with FH. The need for a local structured screening and treatment strategy led A/Prof Tavintharan to set-up the FH-Case identification, Assessment and Reduction in adverse Events (FHCARE) collaboration. Comprised of teams from Endocrinology, Cardiology and Clinical Research Unit, the group aims to establish a standardised method to screen FH, set up a FH registry, and improve early diagnosis and care. In 2018, FHCARE was the first to identify a spectrum of DNA mutations that can provide a definitive diagnosis of FH in Singapore. The results were published in the highly esteemed scientific journal Atherosclerosis. The identification of these DNA mutations allow physicians to accurately diagnose and treat patients with FH early. For their research contributions, FHCARE was awarded the 2019 NHG Award for Outstanding Research Impact.
A/Prof Subramaniam Tavintharan (in blue shirt) and his FHCARE Team.
With these progressions, FH is gaining greater awareness among public healthcare professionals across all Singapore’s healthcare clusters. FHCARE has established many collaborations with other healthcare institutions in Singapore in order to build a Singapore registry for FH. Such disease registries are useful to understand the long-term consequences of care pathway and events for people with FH and their family members. The team will also continue to partner global leaders in FH to contribute and learn from each other’s national experience in FH management. Determining the best type of CPR during emergency transport to hospital Dr Desmond Mao Renhao In urban settings worldwide, where high-rise living is the norm, the survival rates of out-of-hospital cardiac arrests (OHCA) can differ, depending on which floor the patients live on. In fact, OHCAs at a higher floor are associated with lower survival rates, which may be due to the compromised quality of CPR that is given in an elevator during transport. Providing a higher rate of adequate compressions contributes to higher-quality CPRs and higher survival rates. While on HMDP in Taiwan, Dr Desmond Mao ran a simulation study to compare the quality of three forms of response for OHCAs that involve confined elevator transport: • Conventional CPR (C-CPR) Using hands-only compressions without the need to apply a device • Active compression decompression (ACD): Using a mechanical piston device to compress the chest, minimising time where there is no compression on the chest wall • Load-distribution band CPR: Another mechanical device wrapped around the patient’s chest that rhythmically tightens to compress the entire chest
The study was conducted over seven days, between December 2017 and February 2018, at the National Taiwan University Hospital (NTUH) in Taipei with 12 paramedic teams. A total of 144 simulation runs with 48 runs in each arm were completed. The simulation showed that: • C-CPR took the shortest amount of time to move patients down the elevator • ACD delivered the least amount of time without compressions • ACD gave the best compression depth regardless of the position of the patient (lying down or sitting up) The study revealed that, in situations where CPR is required in an elevator, usage of the ACD mechanical device can minimise deterioration of CPR quality. What makes teamwork work? Pearlyn Goh, Cheng Ling Jie, Chin Guey Fong, Liaw Sok Ying With Singapore facing an ageing population, demand for healthcare services is on the rise; concomitantly, a heavier workload inflates the risk of errors and lapses. Studies from abroad suggest that effective nursing teamwork has the potential to offset these shortcomings. Despite the benefits, little is known about nursing teamwork in Singapore. A cross-sectional, descriptive exploratory design was adopted to investigate factors influencing teamwork among nurses in a general ward setting. The Nursing Teamwork Survey (NTS) was distributed to 248 general inpatient ward nurses in a tertiary hospital. The NTS encompassed five subscales: Team Leadership, Team Orientation, Backup, Trust, and Shared Mental Model (SMM). Nurses reported positively (3.65 out of 5) on teamwork among nurses, with SMM and Team Orientation being the highest and lowest scoring 67
RESEARCH AND EDUCATION
subscales respectively. Previous studies conducted also showed similar findings. Other factors — such as qualification level, years of working experience, job staffing adequacy, and job satisfaction — were found to influence nursing teamwork. Based on these findings, it is recommended that nursing management could promote teamwork by: • Implementing teamwork training in the workplace • Cultivating a feedback-friendly environment • Looking into staff-mix ratio and regular work schedule • Incorporating intra-professional teamwork and delegation into the school curriculum This study offers preliminary insight into nursing teamwork and its influencing factors in the clinical areas, and demonstrates that effective nursing teamwork brings about positive patient and nursing outcomes. Enhancing oral care for patients with dysphagia Clarisse Look, Chloe Ang, Chong Boon Keng, Idayu Binte Eusoff Sahab, Sophia Yee, Wong Kuan Yee It is well established that poor oral care is a significant risk factor for aspiration pneumonia. Poor oral care results in colonisation of pathogenic bacteria in the oral cavity. Subsequently, these pathogens could enter the lower airway, increasing the risk of developing pneumonia. As patients with dysphagia have an increased likelihood of aspirating, speech therapists (STs) have a professional interest in reducing the risk of dysphagia-related aspiration pneumonia. STs are also in a position to detect oral diseases and enhance the oral health of patients with dysphagia. However, levels of understanding, experiences and practices differ among the STs.
as well as the development of guidelines to define their role in oral care for patients with dysphagia. This will facilitate the adoption of an interdisciplinary team approach to develop a holistic oral care programme. Discovering the links and risks of obstructive sleep apnoea and postoperative heart attacks A/Prof Edwin Seet Chuen Ping and OSA Investigators People with obstructive sleep apnoea (OSA) have breathing that stops repeatedly during sleep due to their throat muscles intermittently relaxing and blocking their upper airway. Long-term population studies have demonstrated that OSA is associated with an increased risk of myocardial ischaemia, heart failure, stroke, and even death. However, it is uncertain if undiagnosed OSA affects outcomes during the 30-day period after surgery. A prospective multinational cohort study was conducted in five countries with more than 1,200 patients over the age of 45 who had at least one cardiac risk factor. In KTPH, the effort was led by A/Prof Edwin Seet Chuen Ping, from the Anaesthesia Department. It was found that severe unrecognised OSA was associated with postoperative cardiovascular complications and even 30-day mortality. Another novel aspect discovered by the investigators was that low oxygen saturation (<80%) predicted adverse outcomes. The Singapore site has been supported by the SIGI and SIGII grants since 2012, and the results were published in the highly regarded Journal of the American Medical Association in 2019.
A team of STs, dentists and an oral health therapist sought to explore the knowledge, attitudes and practices with regard to oral care among STs in Yishun Health. In June 2019, 18 STs completed an online questionnaire, which included questions on these three areas. This questionnaire was developed by the team based on previously published literature and clinical experience. The findings indicated that STs in Yishun Health have a fair amount of knowledge pertaining to oral care (average 66.9%). Although STs strongly agreed that oral care is important for patients’ clinical outcomes, there was a lack of consensus regarding their role in oral care provision and education. Key barriers to performing oral care included lack of knowledge, uncooperative patients, and inadequate time. As a result, only half of the STs incorporate oral care provision and education frequently in their daily work. This study underscores the usefulness of more oral care education and training for speech therapists, 68
A/Prof Edwin Seet investigated links between obstructive sleep apnoea and post-operative heart attacks.
The study suggests that severe unrecognised OSA puts surgical patients at risk of adverse cardiovascular outcomes. Based on this, the same researchers will look at possible interventions to avoid complications in susceptible OSA patients.
Clinical improvements: an ongoing journey
Investigating the correlation between pulse pressure and cognition Dr Serena Low and SMART2D Investigators Stiffness of the artery is a known risk factor for cognitive impairment. Measuring the pulse pressure is one way of determining the stiffness of arteries. Pulse pressure is calculated as the difference between systolic and diastolic blood pressures. An increase in pulse pressure over time reflects increased arterial stiffness.
A prescription for speed and safety Prescribing a controlled drug (CD) has always been done manually, requiring doctors to write the full prescription, including the patient’s name and address; name, strength and formulation of CD spelt out completely; quantity to dispense written in both words and numerals. Pharmacists often have to continuously follow-up with doctors to write these labourious prescriptions. Yishun Health’s Pharmacy team, together with the Office of Clinical Informatics, was able to implement electronic prescription for CDs in February 2020. The system maintains the legal requirements of a CD prescription and is secured with double authentication to safeguard against fraudulent prescriptions.
To elucidate the effects of arterial stiffness on cognition, patients recruited into the SMART2D study underwent a comprehensive battery of cognitive tests and blood pressure measurements. Analysis of the results showed that a wide pulse pressure, rather than elevation of blood pressure and steady vascular blood flow, was negatively correlated with cognitive performance. This was observed not just globally but also in subdomains of immediate memory, visuospatial/construction, language and attention. The association was independent of demographics, education, clinical covariates, and presence of Apolipoprotein E (APOE) e4 allele. Similar findings were observed in both younger (<60 years old) and older age groups (≥60 years old). Pulse wave velocity (which estimates arterial stiffness), systolic blood pressure, and diastolic blood pressure were correlated with one domain each — attention, language and visuospatial/ construction respectively. The potential mechanisms for the association between the pulsatile component of blood pressure and cognitive function could be due to: • Interference with local blood flow with transitory ischaemia of brain tissue • Oxidative stress that disrupts blood-brain barrier • Structural change in the microcirculation, with resultant decrease in vasodilatory reserve This decreased cognitive performance puts patients at higher risk for dementia. Preserved cognitive function is important for diabetes selfcare and management (e.g. medication adherence and doctor-patient communication). Therefore, if future studies confirm this relationship as causal, pulse pressure may become a treatment target for the prevention of cognitive impairment among people with diabetes.
From making the dispensing of medication safer and more efficient to improving the accuracy of tests, we continually innovate to elevate our processes and operations.
Medicine: signed, sealed, delivered! As we move into the era of e-commerce, the Outpatient Pharmacy has implemented a new home delivery service for a more seamless and convenient patient experience. Patients can place orders with the Outpatient Pharmacy by calling in, using the KTPH website, or using the HealthHub mobile application. The average turnaround time for a home delivery process is one to two working days. In March 2020, uptake for home deliveries increased by 2.5 times. To cope with the load, productivity measures were introduced to make order sheets faster to fill with automated text and order generation. The automation of the Excel file enables staff to reduce transcribing and transferring information, increasing overall efficiency. This new file allows multiple staff to input delivery information at the same time, enabling the Home Delivery Team to cope with the increased demand for the service. Your medication, ready for pickup Medi-Box is a fast, convenient and simple way of collecting medications. Located at Tower C, Level 1, beside the pharmacy, Medi-Box utilises secured and temperature-controlled lockers to ensure that medications are properly stored at all times. Patients, caregivers and staff may place their medication orders by dropping them off, calling in, using the KTPH website or the HealthHub mobile application. Medications can be collected one working day afterwards at their own convenience. An initial 24 lockers were installed on 6 June 2019 and underwent rigorous user testing to ensure a smooth and hassle-free collection process. 69
RESEARCH AND EDUCATION
Stringent software security testing was also conducted to ensure that confidential patient information remained secure at all times. To enable all patients to utilise Medi-Box, the user interface was translated to the four national languages: English, Mandarin, Malay and Tamil. A brochure with simple text and pictorials was used to guide patients in the collection of their medications. Since July 2019, Medi-Box has been serving patients and staff 24 hours a day, 7 days a week. To date, Medi-Box has served more than 1,200 individuals. An instrumental upgrade for dental care In FY2019, the Dental department continued to strengthen ties and collaborations between institutions and within the hospital in a journey of continuous improvement. One of these was the Dental Sterilisation and Organisation for Recall and Traceability (DSORT), a multi-stakeholder initiative to address the need for a system to record the sterility of instruments, to trace the instruments, and to track their usage to the specific patient. This has led to the: • Renovation and improvement of the instrument reprocessing infrastructure to separate the dirty and clean areas • Creation of an instrument inventory to label every instrument with a unique identifier • Development of a software to track instruments, sterility expiry dates, and an automated systemwide recall of non-sterile instruments 70
Laboratory Medicine: achieving precision, speed and safety The Department of Laboratory Medicine (Lab) passed two major inspections in 2019: re-accreditation by the College of American Pathologists (CAP) in April, and — together with Yishun Health — the Ministry of Health (MOH) licensing inspection in October. Apart from these routine inspections, the Department has continued to elevate its processes. Better turnaround for thalassaemia screening The Lab evaluated the performance of a method using lateral flow immunochromatography against the current conventional method that uses microscopic examination. A major component of thalassaemia screening is a microscopic examination to look for Haemoglobin H (HbH) inclusions, which indicate alpha thalassaemia. The extended preparation and screening time of HbH, however, takes 30 minutes for positive samples and between 60–120 minutes for negative samples, forming a bottleneck in the panel. Today, the swap to lateral flow immunochromatography has resulted in a significant improvement of more than 98% in average turnaround time. The average turn-around-time post-implementation is now 1.7 days/sample, with a 95th percentile at 3.2 days. Enhancing e-Traceline e-Traceline was enhanced to include the requisition and management of blood derivatives. In January
The Medi-Box is a convenient way for patients to pick up their medications when they are ready.
STEP 1 PLACE
ORDER
• Scan QR code OR use HealthHub App OR visit the link below • https://eservices.healthhub.sg/p ublic/MedicationRefill/ktphhome
(FBC). The appearance of IG in the peripheral blood indicates an early-stage response to infection, and helps in the rapid discrimination of bacterial from viral infections.
• Enter order details
STEP 2
SCHE D UL E
D E L IVERY
(2 working days in advance) • Select delivery date • Choose preferred time slot
STEP 3 PAY
ONL INE
• Via VISA/Mastercard OR • PayNow
2020, the Blood Derivatives module was created and deployed in SCM and e-Traceline. This initiative, which was derived from the electronic ordering module for Blood and Blood Products, was a collaboration of the Blood Bank, Nursing, and the SCM team. Prior to this, blood derivatives (5% and 20% albumin and intravenous immunoglobulin) were ordered in SCM as medication, and required verification from the Pharmacist in the iPharm system. The derivatives, however, are stored in Blood Bank. When there are subsequent orders or order cancellations for a particular patient, nurses had to resort to manual processing. With the introduction of the Blood Derivatives module, SCM orders for blood derivatives are received directly in e-Traceline, eliminating the verification requirement from the Pharmacist. The orders are also reflected on the Blood Bank Andon Board, and are managed the same way as blood and blood product orders in e-Traceline, including administration. This creates a complete electronic loop from ordering the derivative, releasing of the product, receipt at the requesting location and, lastly, administration to the patient. A return process is also incorporated into the system for the management of unused derivatives. Shortening the time taken to detect early infection In August 2019, the Haematology section started reporting immature granulocytes (IG) in the white blood cell differential count for full blood count
Before the automated reporting of IG, the presence of these cells is flagged in the analyser and verified by Lab staff via microscopic review of the blood film. Since it is a manual analysis, this procedure is labour-intensive, time-consuming and very subjective. On a daily basis, around 160 FBC samples require slide review because of flagged abnormalities, including the presence of IG. The three-month post-implementation assessment showed a decrease of 4%, or an average of 22 slides, in the number of slides requiring review. When measured in time saved, this is equivalent to a decrease of 1.5 hours a day, or up to 547 hours annually, in time spent for Lab staff performing microscopic review. The fight against an emergent threat Candida auris (C. auris) is an emerging fungus that has caused outbreaks in healthcare settings, and presents a serious global health threat. It is capable of causing serious infections, and is generally resistant to multiple antifungal drugs commonly used to treat Candida infections. To complicate matters, the organism is difficult to identify with standard laboratory methods, and misidentifications may lead to inappropriate management. Early identification of C. auris is important so that precautions can be taken to stop its spread. As of 1 January 2020, the Microbiology Section is fully capable of identifying C. auris from clinical specimens and, specifically, from screening samples. The protocol is based on chromogenic medium culture, supplemented by selective broth culture for added sensitivity. Identification is achieved with a high level of confidence using the MALDI-TOF Mass Spectrometry system, and biochemical kit-based testing as a backup measure. The Lab also has reference laboratory testing for rarer strains with unusual phenotypes that confound routine identification. A joint-initiative to tackle prosthetic joint infections The Lab worked closely with key staff from Orthopaedic Surgery to address prosthetic joint infections (PJIs). PJIs are often difficult to diagnose and treat, and prolonged culture and specialised procedures may be required 71
RESEARCH AND EDUCATION
to successfully isolate causative pathogen(s). Less common and more fastidious organisms, such as Cutibacterium acnes, may be involved in the pathogenesis of these infections. A comprehensive protocol for specialised workup of these difficult but highly important specimens has been implemented since 1 May 2019. Special ordering procedures and prolonged incubation has ensured a broader set of media to enhance recovery. Reducing Brucella infection risk Brucella species are globally important zoonotic bacterial pathogens, but not found commonly in Singapore. Nevertheless, it is important to recognise this pathogen early as the cultured form is highly infectious and a well-known cause of laboratory-acquired infection. When one of our patients was identified with Brucella tissue infection, the Lab initiated a review of their protocols, changed their biological safety infrastructure, and improved identification procedures for this unusual organism. Owing to the highly hazardous nature of the bacterium, specialised extraction procedures are necessary to inactivate the organism sufficiently to render it safer to process in the Biosafety Level 2 laboratory. More accurate ‘fingerprints’ (mass spectrometric profiles) were also added to enhance the identification of organisms belonging to this genus. These procedures were fully implemented by 1 October 2019. Rolling out meningococcal vaccination To enhance staff safety in our laboratory, the 72
Lab worked with Health for Life and Pharmacy to offer improved meningococcal vaccination for Microbiology staff. Like Brucella, Neisseria meningitidis is a very significant cause of serious laboratory-acquired infection, and is even more commonly isolated in the local setting. The team improved the initial meningococcal vaccination programme with added coverage for serogroup B. With the introduction of new and effective vaccines against this variant, which causes approximately half our clinical menginococcal disease locally, we started offering both vaccination against serogroup B as well as booster immunisations against the other four serogroups covered by the previous vaccine. This enhancement in immunisation for laboratory staff was implemented in June 2019.
Medical Technologists are often hidden behind the scenes and their microscopes, churning out timely lab test results so that doctors can make accurate diagnoses. During Medical Laboratory Professionals Week, which was held from 22–26 April 2019, the Laboratory Medicine team highlighted their work to the public in an exhibition at the KTPH lobby. As part of their outreach, they conducted tours for colleagues, introducing them to the laboratory and the different areas of work. The week also saw interested students coming by to find out more about pursuing this as a career.
AWARDS AND RECOGNITION
AWARDS & RECOGNITION
PRIZED MOMENTS AND MILESTONES
Our two winners at the Public Sector Transformation Awards — A/Prof Yip Chee Chew (left) and Mdm Chua Gek Choo (right) — flanking Yishun Health CEO Mrs Chew Kwee Tiang.
As healthcare workers, hearing a heartfelt ‘thank you’ is all it takes to make a day’s work worthwhile. While not the sole focus of our work, these awards validate Yishun Health’s DNA of continuous improvement. Being recognised by peers and the sector can elicit pride and satisfaction, and boost our commitment to quality care and healthcare transformation.
Our Public Sector Transformation Awards stars Two of our own were feted at the 2019 Public Sector Transformation Awards — both of them leaders, 74
mentors and inspirations for all of us at Yishun Health. The Public Sector Transformation Awards is conferred by the Public Service Division of the Prime Minister’s Office, and honours individuals and public agencies for work and organisational excellence. Exemplary Leader Award Mdm Chua Gek Choo, Director, Nursing, YCH Mdm Chua received the Exemplary Leader Award for her incredible impact on nursing in Yishun Health. Though small in stature, she is well known and loved for her energetic personality, dedication and tenacity in addressing challenges
big and small. For more than four decades, she has undertaken many roles, including Deputy Director of Nursing and the Team Lead in KTPH’s Inpatient Planning Committee. Exemplary Innovator Award A/Prof Yip Chee Chew, Head and Senior Consultant, Department of Ophthalmology and Visual Sciences (OVS), KTPH; and Education Director, Education Development Office, KTPH Known as Yishun Health’s ‘Man of Ideas’, A/Prof Yip has a passion for developing improved patient care models and initiating quality improvement projects. He applies his Six Sigma Lean Black Belt expertise towards collaborative efforts to improve patient care, increase productivity, and reduce healthcare costs.
A win for being ‘innovative & progressive’ Yishun Health won two awards at the Asian Hospital Management Awards (AHMA), held on 12 September 2019. AHMA is a prestigious award in the Asia Pacific that recognises and honours hospitals that take innovative and progressive approaches to improve healthcare in the region. AdMC received a Gold Award under the Facility Management and Financial Improvement Project Category, and the Community & Home Eye Screening Service (CHESS) won an Excellence Award under the Community Involvement Project category. They were picked from a nomination pool of more than 500 entries from 17 countries.
National recognition at the Singapore Health & Biomedical Congress KTPH bagged a total of 12 awards at the 17th Singapore Health & Biomedical Congress (SHBC) Scientific Competition, organised by NHG. SHBC is a platform to recognise healthcare professionals, research scientists, academics and industry experts for their hard work, and for them to share and discuss strategies for the advancement of the healthcare landscape. Among the 12 given to KTPH, five were Gold Awards and were presented to four of our colleagues in October 2019: Singapore Clinician Investigator Award Dr Serena Low, Consultant, Clinical Research Unit SHBC Best Poster Awards (Basic Science/ Translational Research, and Clinical Research) Dr Angela Moh, Senior Research Officer, Clinical Research Unit
(Left to right) Mr Donald Wai, Ms Karve Anuja, and A/Prof Yip Chee Chew smiling with their awards from AHMA.
SHBC Best Poster Award (Health Professions Education) Clarisse Look, Senior Speech Therapist, Rehabilitation Services Care Centre Singapore Young Investigator Award (Clinical Research) Dr Desmond Mao, Consultant, Acute & Emergency Care Centre This year’s SHBC also included the inaugural NHG Research Awards, held to acknowledge quality research work that has led to good clinical outcomes. Yishun Health’s Department of Anaesthesia received the Outstanding Research Culture Award; the Outstanding Research Impact Award went to the team behind Familial Hypercholesterolemia: Case Identification, Assessment and Reduction in Adverse Events, led by A/Prof Subramaniam Tavintharan, Clinical Director and Senior Consultant, Diabetes Centre.
Yishun Health's Familial Hypercholesterolemia research team posing with their trophies for Outstanding Research Impact at SHBC. 75
AWARDS & RECOGNITION Making an impact on HEALTH Yishun Health brought home the Singapore HEALTH Award (Merit) on 4 October 2019 in acknowledgement of the stewardship in championing healthy living practices and programmes for employees, partners and the community. This biennial award recognises organisations for their health promotion programmes, ensuring effectiveness for their employees.
The KTPH Dementia team, together with their partners Lien Foundation and Alzheimer’s Disease Association (ADA), were lauded for Forget Us Not (FUN), an initiative to create public awareness about dementia. They won the Singapore Patient Engagement Initiative Award, which recognises teams for their outstanding patient engagement projects or initiatives that enhance care delivery and overall well-being of public, patients and caregivers. FUN was launched by KTPH and Lien Foundation in early 2016 to train as many people as possible to support persons with dementia and help them lead active, engaged lives for as long as they can. The first dementia-friendly community in Singapore started in Yishun that year. In 2017, ADA joined as a key partner.
The KTPH Dementia Team were lauded at the Singapore Patient Conference for their FUN initiative.
A FUN and meaningful impact on building a dementia-friendly community The 7th annual Singapore Patient Conference was held on 25 October 2019 under the theme ‘Building a Community of Carers’. It was held in conjunction with the Singapore Patient Action Awards.
To date, close to 29,000 Dementia Friends across the island have been trained, and 158 organisations have come on board the programme. They include enterprises and entities from a diverse spectrum — civic and religious groups, voluntary welfare organisations and schools, F&B and retail businesses, manufacturers and essential service providers, banks and public transport companies, and statutory boards and government agencies. With the combined efforts of the team, dementia-friendly communities have also been established in Bishan East-Thomson, Kebun Baru, Ang Mo Kio, and Toa Payoh.
Honouring our outstanding healthcare professionals The Yishun Health Awards Ceremony, held on 19 November 2019, celebrated the achievements and
A/Prof Chin Thaim Wai holding his trophy for the Distinguished Senior Clinician Award at Yishun Health Awards. 76
contributions of colleagues who have contributed to the growth of the organisation. In particular, many long-serving staff have been integral in the restructuring and rebuilding of Alexandra Hospital, as well as the move to KTPH. In acknowledgement of his contributions in clinical, education and research practice as a veteran surgeon, A/Prof Chin Thaim Wai, Senior Consultant, Orthopaedic Surgery, was conferred the highest accolade: the MOH Distinguished Senior Clinician Award. Long-serving Yishun Health staff were also recognised for their loyalty and dedication. Two of them, Loh Patsy and Esther Yap, received their 50-Year Long Service Award! COO Ms Yen Tan also marked her 20th year of service. In addition, the NHG Outstanding Citizenship Award went to Ms Low Beng Hoi, Director, Nursing, PHCT. Jenny Goh (right) receiving the Ann Wee NUS Social Work Alumni Award from Mrs Ann Wee herself!
Our first Annual Report as Yishun Health — published in 2018 — clinched an Award of Excellence for design and layout at the Better together 31st Annual Apex Awards 2019 for Publication Excellence, a US-based competition that attracted more than 1,200 entries worldwide. The winning FY2017/2018 Annual Report was themed ‘Better Together’. Using hand-drawn illustrations, we created the cover, chapter dividers and infographics to showcase how healthcare is a team effort, and how Yishun Health integrates care across the spectrum of needs and empowers the community to stay healthy. This is the second year running that our Annual Reports have been recognised at the Apex Awards. annual report 2017/2018
Syaiful Hakimnudin Bin Sa’adon (right) receiving his Distinguished Toastmaster Award.
For being there when it mattered
Toasting our public-speaking maestros
Yishun Health’s Deputy Head, Medical Social Service (MSS), Jenny Goh, received the Ann Wee NUS Social Work Alumni Award on 13 September 2019. Jenny, who is also Principal Medical Social Worker and Manager, MSS, KTPH, has worked for 20 years as a social worker. In her acceptance speech, she paid tribute to social work pioneers and shared stories about her favourite interactions with patients and caregivers. Named after Mrs Ann Wee — a pioneer social work educator and the longestserving Head of NUS’ Department of Social Work — the award recognises NUS Social Work alumni who have made major contributions to social work education and practice.
Yishun Health’s Toastmasters Club bagged a number of awards at the 2019 Achievers Nite on 21 June, an event organised by Toastmasters International Singapore. Syaiful Hakimnudin Bin Sa’adon, Radiographer, Diagnostic Radiography, and Vice President (Education) of the Toastmasters Club, was awarded the Distinguished Toastmaster (DTM) Award, the highest accolade Toastmasters International bestows. DTM Award recognises a superior level of achievement in both communication and leadership. Syaiful also received the Triple Crown Award together with Tony Yang, Senior Manager, Facilities Management, and Secretary of the Toastmasters Club. This award is presented to those who have achieved three or more awards within a Toastmasters year. 77
AWARDS & RECOGNITION Left: The Yishun Health contingent showing off their moves at the Purple Parade. Below: CHRO Ms Magdalene Chai receiving a Certificate of Recognition at the Enabling Employer Awards on behalf of Yishun Health. Bottom: Volunteer Irene Tay presenting a prize-winning pumpkin from YCH.
Growing an inclusive organisation Since 2006, Yishun Health has championed an inclusive workforce and hired persons with disabilities. We have strengthened our efforts over the years. In 2017, we began working with SG Enable on the School-To-Work programme to provide internship opportunities and assist graduates from Special Education schools to transition into the workforce. Working with job coaches from MINDS, we structure and customise training according to special needs. Apart from providing step-by-step pictorial guides, staff are also trained to interact and work with special-needs graduates appropriately. Interns are also supported with ‘buddies’ and trained supervisors. On 26 July 2019, Yishun Health was accorded the Certificate of Recognition at the 5th Enabling Employers Awards for providing employment opportunities for people with intellectual disability, autism, physical disability, or hearing/visual impairment.
A prize for our Purple Parade contingent Yishun Health was named one of the top 10 best contingents during the Purple Parade’s appreciation event, held on 21 November 2019. The Yishun Health contingent was one of 242 organisations that participated in this year’s parade, which supports inclusion and celebrates the abilities of the special needs community in Singapore. This win was made possible through the support, creativity and energy of Yishun Health’s staff, friends and family, volunteers from YCH’s Fun Fit Club and patient sitter programme, as well as our Corporate Social Responsibility partners: Villa Francis Home for the Aged, Singapore Christian Home, and Sree Narayana Mission Home. Besides underscoring the strong ties between Yishun Health and its community partners, the win also reflects the solidarity exemplified by everyone towards this worthy cause. 78
Giving back matters! Yishun Health was conferred the Charity Gold Award at the annual Community Chest Awards Ceremony, held at the Istana on 9 October 2019. This award recognises organisations with employees on SHARE for their high donation rate to Community Chest. Yishun Health attained an 80–89% staff participation rate, underscoring the caring and generous hearts of Yishun Health staff.
Not just lush and beautiful, but award-winning also! KTPH and YCH won several awards at the 2019 Community Garden Edibles Competition. The annual event, organised by National Parks, was part of the Community Garden Festival. KTPH won in the Heaviest Pumpkin category with its 5.9kg champion, while YCH’s 5.4kg pumpkin won third place. Both institutions also brought home multiple consolation prizes for wintermelon, papaya, luffa, and long beans. These awards recognise the effort, skill and dedication of our gardening volunteers who tend our rooftop gardens. Besides nurturing plants, volunteers also run weekly horticulture therapy sessions for patients in KTPH and YCH.
OUR PEOPLE
OUR PEOPLE
ONE PEOPLE, ONE VISION, ONE YISHUN HEALTH The tenacity, commitment and effort we put in as an organisation to care for our kampung is more than about setting a mission statement, but the result of ongoing engagement and investment in our people. Our people form the heart of Yishun Health. Guided by a strong and united vision, as well as passion and courage, we deploy multiple ways to nurture the Yishun Health culture of care, and equip each and every one with the insights, tools and knowledge that inspire ownership and action to make a difference. Setting our compass for greatness Like a ship setting course for brave new worlds, we have set our sights on our journey of transforming care. Apart from mapping our way forward, we take extra measures to frequently recalibrate and reinvigorate ourselves.
80
We held four Townhalls and Vision Alignments in FY2019. These form an essential platform to disseminate our messaging and share best practices. It is a time for us to gain clarity and be lifted by the energies of each other through our unifying quest to do what is best for the patients, people and community we serve. Nurturing collective leadership across our healthcare family At the end-of-year Townhall in November 2019, Prof Philip Choo, Group CEO, NHG, provided some key updates of each NHG institution and outlined
future plans. Referencing the three waves of Frailty, Chronic Disease and Pre-Disease, Prof Philip stressed the compounding effect of each wave as it hits us, and the importance of moving upstream to invest and focus on preventive care.
Developing meaningful careers Human capital development is central to our success as an organisation. To this end, we are committed to continuous learning, strong HR practices that engage and foster organisational pride, as well as build platforms to connect and collaborate. Building a future-ready workforce Yishun Health awarded close to 100 in-service sponsorships and scholarships to staff in FY2019. These educational initiatives and clinical attachments enable our staff to upgrade their competencies and prepare for the future through local and overseas programmes. In addition, Yishun Health also invited visiting experts from overseas to share with our departments on work that benefits our patients and residents. Building our pipeline of talent Our first cohort of Management Associates (MA) graduated from the challenging and fulfilling twoyear programme in July 2020. Each MA underwent three postings to learn about episodic care, lifelong care and shared services, and was part of departmental and organisational projects. The Healthcare Management Associate Programme was started in 2018, and Yishun Health has enrolled its third cohort as of July 2020. Going digital: future-proofing our organisation Digitalisation has always been a strategic training thrust for Yishun Health. In September 2019, we conducted a staff survey to assess perceptions of digitalisation’s impact on healthcare, and how training services could be shaped accordingly. This led to a Basic Digital Literacy workshop and modular programmes on Smart Healthcare. For general outreach, two Learning Lunchtime sessions were organised on ‘Data-Driven Healthcare: How Big Data is transforming the industry’, held in December 2019, and ‘Story-telling in an Age of Data’, in January 2020. For educators and trainers, learning technology workshops were also organised. These included micro-course development (NTUC ULeap) and e-course design and development (Articulate Storyline 3TM), both held in November 2019. We also added a digital presence to our longstanding Wednesday Learning Lunchtime Book Reviews. The National Library Board was invited to set up e-Reads @ Yishun Health. This online service is offered on a jumbo touchscreen placed at the Auditorium Foyer, showcasing a curated book collection of titles featured at our Lunchtime
The e-Reads @ Yishun Health booth lets staff browse a curated catalogue of e-books and borrow them on the spot.
The Clinicians' Course Tracking portal.
Sessions. Staff can tap, browse and immediately borrow e-books and resources using their digital handheld devices. Added to this, a customised Clinicians’ Course Tracking portal — built in collaboration with Medical Affairs — was launched for clinicians and HODs. This allows them to browse core and compulsory courses, and view key training hours for their units. It aggregates data from various online learning systems, and provides a one-stop access portal for easy visualisation of course records. Online learning, meeting and collaboration: the new way forward The COVID-19 pandemic accelerated our deployment and adoption of virtual technologies. The team at Human Resource Development (HRD) boosted digital learning offerings, making available more corporate courses that had previously been offered only on a classroom basis. Micro-courses from reputable training vendors were also sourced in areas such as leadership, personal effectiveness, mental health, and resilience to support staff during this period. A Training Trainers initiative was a high-value move to encourage colleagues who had undergone training to produce online learning events. A threepart ‘Activate Virtual Learning’ tutorial series was produced wholly in-house by HRD, aimed at our 100 staff facilitators, course developers, and educators. 81
OUR PEOPLE
Our staff facilitators for the course, '7 Habits of HIghly Effective People'.
Team Conversations is an initiative that offers a safe space for staff to express their real feelings about the workplace.
These covered the spectrum of existing online training tools in Yishun Health, including courses on using Zoom effectively.
The strengths affirm and validate each department’s unique identity. In addressing areas for improvement, a ground-up approach was designed to enable empowerment and autonomy, leading to sharedaction planning. One of the collective leadership concepts of ‘offers and requests’ was introduced. Here, staff take the lead in offering support for proposed initiatives and request for assistance from colleagues or head of department. These conversations encourage staff to share their thoughts and ideas, and builds an engaged workforce.
The Speak Up for Safety programme was also one of the first courses to be identified for online conversion. This core course emphasises patient safety through a conversational protocol and establishes clear levels of accountability. Approval was obtained from training provider, Cognitive Institute, to allow the re-adaptation of its teaching materials for live Zoom-based facilitation. HRD worked with inhouse certified facilitators to provide training through virtual facilitated sessions using several features in Zoom to engage learners. HRD also introduced a larger range of online courses on soft skills from established leaders, including topics such as personal effectiveness, customer service, time management, productivity, big data, and analytics. Building a Community of Practice for effective habits In FY2019, staff who had gone through the ‘7 Habits of Highly Effective People’ course and become facilitators gathered for its third Community of Practice (CoP) on 17 October 2019. That day, they welcomed three new facilitators. During the CoP, the group exchanged knowledge on best practices and facilitation experiences, and new elements in the offerings by FranklinCovey.
An ongoing quest to do better We build on our culture of quality improvement with ongoing efforts to support improvement and ideas. The value question — and why it matters On 26 April 2019, Yishun Health held the first Quality Convention (QC) of 2019. ‘Adding Value to Quality: How do we get there?’ was a timely event that touched on how to deliver more meaningful outcomes to patients. The guest speakers were Ms Gillian Tee and Ms Lily Phang, the co-founders of Homage, which provides on-demand caregiving for the elderly in Singapore. They spoke on tackling challenges, such as an ageing population and rising healthcare
To further improve take-up, the course is now available as one of our self-paced courses. These self-paced courses have defined guidelines on training hours and establishing self-paced learning after a mutual agreement with supervisors. Authentic department engagement HRD facilitated an Employee Climate Survey follow-up, known as Team Conversations. This session offers a safe space for staff and their head of department to take part in authentic and genuine conversations about the department’s strengths as well as opportunities for continued improvement. 82
Signing their publicity poster at our inaugural Quality Convention were the co-founders of Homage.
costs, and how to deliver value to their patients through technology and mobile applications. More importantly, they focused on what dignified care means from the patient’s point of view, and the importance of covering the wide range of complex functional, emotional and social needs. Taking ownership of risks for better patient care On 13 September 2019, a second QC was held, and themed ‘Risk Management Strategies in an Acute Hospital’. The guest speaker was Ms Ann D Gaffey, President, Healthcare Risk and Safety Strategies, LLC. While the idea of risk sounds negative, Ms Gaffey emphasised that it is inherent in all we do as a hospital; when managed well, it can lead to good outcomes. She highlighted that everyone has a role in risk management, be it doctors, nurses or administrators. Along these lines, accountability and speaking up for safety plays an important role in risk management. This QC also featured the first debate on the motion, ‘Working in Silos Makes Us Lose the Big Picture’. The lively and highly entertaining session was won by the proposition.
An entertaining debate session in progress at Yishun Health's second Quality Convention.
Yishun Community Hospital’s first Quality Day YCH hosted its first Quality Day on 8 November 2019. The central theme of this inaugural event was ‘Safer Transition of Care’. This is a critical aspect of a patient’s care journey, especially as the healthcare system undergoes transformative efforts to go “Beyond Hospital to Community” and “Beyond Quality to Value”. A care transition — a continuous process in which a patient’s care shifts from being provided in one setting to another setting, and between healthcare practitioners — can pose a risk to not only patients, but also caregivers, families and healthcare providers. The event brought intermediate and long-term care partners together, where they could learn about the potential areas of risk and discuss strategies to mitigate potential issues during times of transition in the patient care journey. In his opening address, Prof Pang Weng Sun, Dy Group CEO (Population Health), NHG, emphasised the importance of engaging community partners continually in order to create a well-integrated healthcare system. A/Prof Tai Hwei Yee, Group Chief Quality Officer, NHG, delivered a keynote
The leaders of YCH at their inaugural Quality Day.
The ribbon-cutting ceremony to launch the 2019 Patient Safety Month. 83
OUR PEOPLE
address focused on the value of care transitions and the repercussions of poorly executed care transitions. Empowering our staff to be safety advocates 1 July 2019 marked our inaugural Patient Safety Month. Organised by the Patient Safety Month Committee, this campaign seeks to educate the public on pressure injuries, infection control, falls prevention, and medication safety.
OUR SAFETY COMMITMENT
Strive to uphold the highest standards in patient care
Advocate for patient safety every day
Fully support clinical quality projects
Educate patients, caregivers, the public and our staff on ways to protect patients from harm caused by pressure injuries, falls, poor hygiene practices, and poor medication compliance
that help us continue providing quality healthcare
For staff, workgroups from Pressure Injury, Falls Prevention, Infection Control, and Medication Safety organised its focus areas. The month was also a timely reminder to never compromise on our safety commitment. During the closing ceremony, CEO Mrs Chew Kwee Tiang highlighted safety as critical in a time when the number of frail elderly are rising. It is even more essential for families and healthcare teams to partner each other in ensuring patient safety. A/Prof Pek Wee Yang, Chairman, Medical Board (CMB), also emphasised how it is possible for everyone to embrace patient safety as a priority. All hands on deck for hand hygiene Yishun Health held its Patient Safety Briefing and Hand Hygiene Day on 17 May 2019. A/Prof Wong
Moh Sim, Dy CMB (Clinical Quality & Manpower Development), urged staff to take ownership of building a just culture of safety, and know that open and honest reporting for patientsâ&#x20AC;&#x2122; safety is supported by the organisation. Joining her was A/Prof Edwin Seet, Senior Consultant, Anaesthesia, who emphasised the need to be vigilant in ensuring high hygiene standards. He called for more careful checks in our day-to-day work in caring for our patients. Hearteningly, Dr Chris Willis, Chairperson of the Infection Control Committee and Senior Consultant, General Medicine, noted that Yishun Healthâ&#x20AC;&#x2122;s compliance to hand hygiene has been steadily improving over the years, but we should never become complacent. The event ended with prizes being handed out to teams with outstanding handhygiene compliance.
Teams with outstanding hand-hygiene compliance getting the recognition they deserve. 84
A happy & healthy Yishun Health family
The Yishun Health Senior Management and Heads of Departments took their vaccination shots on 6 May 2019 in a concerted effort to model the way.
Keeping staff fit and advocating active and healthy living, the WorkLife team continued to bring daily fitness classes during lunchtime and evenings to the campus for staff convenience. More than 1,000 staff have participated in cardio kickboxing, K-pop fitness, muay thai, pilates, yoga and zumba (above, left). The team also organised non-fitness-oriented courses, such as terrarium making (above, right).
ACTIVE Day 2019, held on 1 November 2019, reiterated our philosophy of a holistic culture of health with a series of yoga, pilates and zumba classes as well as other workshops to engage staff. 85
OUR PEOPLE
The FY2019 League saw more than 500 staff competing in badminton, basketball, bowling, futsal and captain’s ball, with hundreds of supporters cheering them on. The closest match was between the A&E team and Diagnostic Radiology department. Both teams vied for the Championship title, which concluded with an exciting tie!
Our 2019 Fitness Challenge recorded a high rate of participation (80%), with 74 departments achieving a 100% participation rate. To reinforce the message of staying healthy at work, the WorkLife Team collaborated with Rehabilitation Services to come up with an eight-week series of fitness workshops. Participants learnt better form, technique and injury prevention in areas such as push-ups, sit-ups, sit & reach, the 1.6km walk and 2.4km run.
Yishun Health’s Safety & Security Week 2019, themed ‘Stay Engaged, Stay Safe’, reinforced safety and preparedness messages through safety talks and exercises. 86
We held our Volunteer Appreciation Lunch on 2 November 2019 at the Nee Soon Central Community Centre for some 187 volunteers from more than 18 volunteer groups. The event acknowledged their hard work, support and contributions in caring for our patients.
The Health For Life clinic gets a name makeover!
Now called the Staff and Occupational Health Clinic (SOHC), Yishun Health’s Health For Life (HFL) clinic got a new address in addition to its new name, moving from C58 to C26 in June 2019. SOHC will continue to focus on managing acute conditions in a general-practice setting, occupational hazards connected to work in a hospital environment, health promotion via selected evidence-based health screening, and vaccinations and pre-employment screening with targeted occupational advice. Making space to connect within Yishun Health’s Human Resource WorkLife! team continuously collaborates with the Psychological Medicine department and Medical Social Services in the PsychoSocial Committee to guide and promote psychological support for staff within Yishun Health. In FY2019, one of the key initiatives to promote psychological well-being was Heart Space. Heart Space focuses on providing bite-sized learning opportunities to empower staff to enhance mental well-being. In FY2019, the committee organised talks on self-compassion, burnout, the social brain, and conflict resolution. There were also monthly meditation sessions. Another key initiative was the launch of the complimentary Staff Counselling Service in September 2019. This service offers professional
counselling to staff requiring support in handling work and personal issues. To help staff de-stress while at work, various events and activities were held. These included terrarium-making and lunchtime talks. PALS to lean on During the peak periods of the COVID-19 pandemic, the Peers Around Lending Support (PALS) programme ramped up its outreach. Launched in 2008 and run by clinical psychologists, the programme offers systematic staff support. In response to heightened stress during the crisis, PALS developed a Pandemic Support and Advocacy Plan to help staff transition smoothly between peacetime and pandemic periods. Various PALS initiatives offer specific support to nurses, junior doctors, as well as staff in general. It involves groups sessions, meditation sessions, a 24/7 helpline, email, and educational materials. Where needed, additional counselling, psychiatric or psychological support is offered. A gentle nudge towards cultivating mindfulness In April 2019, KTPH’s Psychology Service was awarded a Culture of Health grant to pilot programmes for a culture of health in the workplace. This led to the Mindful Moments initiative. The key to good mental health is possessing self-awareness of the need for rest and recharge. Mindfulness is one way to regain energy and joy through restorative practice. It is an effective and easy way to rest mentally, improve mental clarity, 87
OUR PEOPLE
and develop positive thinking, thereby building resilience. Mindful Moments seeks to create a culture of positive mental wellness through: • Education: knowledge and information about mindfulness and compassion • Empowerment: experiential mindful can-do moments
• Engagement: encourage and motivate people to continue with regular mindfulness practice Building on our existing health-promoting initiatives that use visual reminders, the initiative created experiential opportunities throughout the hospital to nudge people to take a mental break.
‘TAKE A MINDFUL MOMENT’ CAMPAIGN
A series of stickers were designed to encourage mindfulness at different times of the day.
Celebrating as one kampung
Yishun Health staff gathered on 26 June 2019 to celebrate Hari Raya Aidilfitri with their Muslim colleagues, and to learn the roots and rhythm of Malay culture.
More than 200 staff gathered in their festive attire to form a vibrant sea of colours as we marked Deepavali on 11 November 2019 with cultural dancing and joyous music. There was also a surprise flash mob, gamely led by Chief Financial Officer Mr Roger Leong. 88
Yishun Health’s Corporate Social Responsibility (CSR) Committee organised a Christmas Light-Up on 11 December 2019 to spread the festive cheer to our CSR partners. Residents from our four nursing home partners — All Saints Home, Singapore Christian Home, Villa Francis Home and Sree Narayana Mission — gathered at the KTPH Learning Centre together with staff to celebrate the joyous occasion. (below)
Nurses Day 2019 was a call for nurses to Dream, Dare, and Do — a testament to the soul of nursing, and the need for tenacity, conviction and courage to take on the hard tasks, ask the hard questions, and speak up even when it is difficult to do so. The theme was a call to action, to rally our individual and collective strengths towards better, safer and more accessible person-centred care. On 25 July 2019, as part of the Nurses’ Day pre-event activities, a Promenade Walk around Yishun Pond was organised for the nurses, followed by a session of Laughter Yoga. There was also the Nurses’ Day exhibition, which showcased personal stories from our nurses. (above)
Held on 22 October 2019 was the much-anticipated Staff Appreciation, which was all about ‘Everyday Superheroes on a Mission’. During the launch, staff were treated to a series of activities and meals, and were acknowledged for their hard work and effort in finding ways to implement initiatives for patients’ well-being. CEO Mrs Chew also took the time to share heart-warming anecdotes of our people who have been re-trained to assume different roles, affirming Yishun Health’s commitment to contribute to the growth and development of each individual staff member. 89
GREEN REPORT CARD
FA U NA AND FL O R A
Dragonflies & Damselflies
Butterflies
99 SPECIES
Fruit Trees
50
Birds
Fishes
100 SPECIES
31 SPECIES
88 SPECIES
Medicinal Plants
Flowering Plants
Vegetables
SPECIES
SPECIES
SPECIES
102 SPECIES
52
51
UT IL IT IES
Electricity
42,132,040 KWH (increased by 2% from 41,189,501kWh)
115,718 M
3
(increased by 1% from 114,382m3)
NEWater Consumption
226, 077 M
3
(decreased by 3% from 234,061m3)
Gas
General Waste
Recyclable Waste
(decreased by 2% from 617,079kWh)
(increased by 1% from 2,326 tons)
(increased by 49% from 172 tons)
602, 722 KWH 90
Potable Water Consumption
2, 356 TONS
257 TONS
OPERATIONAL HIGHLIGHTS
K H O O T EC K PUAT HO SP ITAL
Beds in Service
Bed Occupancy
Total Inpatient Days
Average Length of Stay
(Decreased by 4% from 92%)
(Decreased by 4% from 220,300)
(Increased by 4% from 5.3 days)
(Decreased by 3% from 375,705)
A&E Attendances
Inpatient Admissions
Total Surgeries
Day Surgeries
Inpatient Surgeries
(Decreased by 0.1% from 133,980)
(Decreased by 7% from 41,722)
659
133,848
88%
38,913
211,524
49,000
(Decreased by 4% from 51,234)
5.5 DAYS
31,838
(Decreased by 6% from 33,810)
Outpatient Attendances
364,161
17,162
(Decreased by 2% from 17,424)
YISHUN COMMUNITY HOSPITAL
Beds in Service
Bed Occupancy
Total Inpatient Days
Average Length of Stay
Inpatient Admissions
(Decreased by 13% from 258)
(Decreased by 1% from 79%)
(Decreased by 8% from 74,232)
(Decreased by 3.5% from 25.9)
(Decreased by 5% from 2,834)
224
78%
68,176
25 DAYS
2,692
ADMIRALTY MEDICAL CENTRE
Outpatient Attendances
29,078
(Increased by 11% from 26,254)
Day Surgeries
1,947
(Decreased by 7% from 2,089)
91
AWARDS APR 2019 HEALTHCARE HUMANITY AWARDS Open Category • Dr Ramaswamy Akhileswaran, Senior Consultant, Geriatric Medicine, KTPH • Dr Chua Kong Yeow John, Senior Staff Physician, Acute and Emergency Care Centre, KTPH • Manjit Kaur, Senior Nurse Manager, Ward B55, KTPH • Noor Aiyshah Binte Abdul Raman, Senior Assistant Nurse, Isolation Ward, KTPH Caregiver Category • Mr Daniel Ho, Caregiver, KTPH MAY 2019 NHG RECOGNITION AND DEVELOPMENT AWARDS Lee Foundation-NHG Lifetime Achievement Award • Prof Pang Weng Sun, Deputy Group Chief Executive Officer (Population Health), NHG; Senior Consultant, Geriatric Medicine, KTPH NHG Distinguished Senior Clinician Award • A/Prof Chin Thaim Wai, Senior Consultant, Orthopaedic Surgery, KTPH NHG Distinguished Achievement Award • A/Prof Lim Su Chi, Senior Consultant, General Medicine, KTPH NHG Outstanding Citizenship Award • Low Beng Hoi, Director, Nursing, PHCT • Dr Wong Sweet Fun, Chief Transformation Officer; Deputy Chairman, Medical Board (Population Health); Clinical Director, PHCT, Yishun Health NHG Young Achiever Award • Dr Geraldine Cheong Pei Chin, Consultant, Anaesthesia, KTPH • Sharon Toh Fong Mei, Principal Occupational Therapist, Rehabilitation Services, YCH • Phyllis Tan Xiuzhuang, Nurse Manager, Ward D98, YCH • Debbie Do Nguyen Ngoc Thuy, Senior Pharmacist, Pharmacy, KTPH NHG Team Recognition Award (Gold) • Excellence Through Collaboration, Multidisciplinary Trauma Team, KTPH NHG Team Recognition Award (Silver) • Less is for More: Lean Cataract Surgery Care Path, Ophthalmology & Visual Sciences, KTPH NHG Team Recognition Award (Bronze) • Campus Flow and Care Integration Team, Yishun Health 92
JUN 2019 TOASTMASTERS AWARDS Distinguished Toastmaster Award • Syaiful Hakimnudin Bin Sa’adon, Radiographer, Diagnostic Radiography, KTPH Triple Crown • Syaiful Hakimnudin Bin Sa’adon, Radiographer, Diagnostic Radiography, KTPH • Tony Yang, Senior Manager, Facilities Management, KTPH Select Distinguished Club Award • Yishun Health Toastmasters Club JUL 2019 NURSES’ MERIT AWARD 2019 • Yu Lee Hoon, Senior Nurse Clinician, Inpatient Wards, KTPH • Joyce Lee, Nurse Manager, Cardiovascular Centre, KTPH • Fan Xiulan, Assistant Nurse Clinician, Peri-Ops, KTPH • Kathy Lam, Nurse Educator, Nursing Administration, YCH • Koh Pei Pei, Assistant Nurse Clinician, Ward A82, KTPH • Chan Hoi Sum, Nurse Manager, Ward B96, KTPH • Siti Nor Ilyana Binte Kamsol, Nurse Clinician, Acute and Emergency Care Centre, KTPH PUBLIC SECTOR TRANSFORMATION AWARDS 2019 Exemplary Innovator Award • A/Prof Yip Chee Chew, Head & Senior Consultant, Ophthalmology & Visual Sciences, KTPH; Education Director, EDO, KTPH Exemplary Leader Award • Chua Gek Choo, Director, Nursing Administration, YCH 5TH ENABLING EMPLOYERS AWARDS • Certificate of Recognition Yishun Health AUG 2019 NATIONAL DAY AWARDS The Public Administration Medal (Bronze) • Yen Tan, Chief Operating Officer, Yishun Health The Commendation Medal • Audrey Saw Guat Lin, Deputy Director, Nursing, KTPH • Angeline Ng Phui Heng, Deputy Director, Allied Health Services The Public Service Medal • Dr Teoh Chin Sim, Senior Consultant, Sports Medicine, KTPH • Ip Kit Ling, Senior Manager, Patient Experience Office, KTPH The Efficiency Medal • Guo Hui, Senior Nurse Manager, Ward B85, KTPH • Ng Siew Fong, Senior Nurse Manager, Ward B105, KTPH • Chin Guey Fong, Senior Nurse Clinician, Nursing Administration, KTPH • Foo Meow Ling, Nurse Clinician, Infection Control, KTPH • Koh Pei Pei, Assistant Nurse Clinician, Ward A82, KTPH
• Benjamin Tan Boon Cheng, Assistant Nurse Clinician, Nursing Administration, YCH • Gong Zhixiao, Senior Staff Nurse, Ward B55, KTPH • Janice Wong Wai Keng, Principal Medical Technologist, Cardiovascular Centre, KTPH • Nya Lee Hoon, Manager, Human Resource, KTPH • Low Teck Yee, Manager, Human Resource, KTPH • Yap Bee Kiat, Manager, Finance & Accounting, KTPH • Chok Kim Hua, Executive, Finance & Accounting, KTPH The Long Service Medal • A/Prof Terence Tang, Chief Clinical Informatics Officer and Deputy CMB (Clinical Informatics, Innovation & Patient Engagement), Yishun Health • Dr Ang Yan Hoon, Senior Consultant, Geriatric Medicine, KTPH • Dr Liow Pei Hsiang, Senior Consultant, Psychological Medicine, KTPH • Jessie Tan Joon Cheen, Senior Nurse Clinician, APN and Specialty Nurse, KTPH • Loh Pey Lin, Nurse Clinician, Acute and Emergency Care Centre, KTPH • Maligah D/O Krishnan, Senior Staff Nurse, Acute and Emergency Care Centre, KTPH • Teresa Foong, Deputy Director, Allied Health Services and Pharmacy, Yishun Health; Head and Senior Principal Clinical Psychologist, Psychology Service, KTPH • Janice Wong Wai Keng, Principal Medical Technologist, Cardiovascular Centre, KTPH • Faridah Binte Asik, Project Coordinator, Operation Administration, KTPH 31ST ANNUAL APEX AWARDS 2019 FOR PUBLICATION EXCELLENCE Award of Excellence • Yishun Health Annual Report 2018/2019 SINGAPORE HEALTHCARE MANAGEMENT 2019 Patient Experience Category Merit Award • Let’s Eat Together Initiative SEP 2019 NHG TEACHING EXCELLENCE AWARDS NHG Education Leaders Award • A/Prof Yip Chee Chew, Head & Senior Consultant, Ophthalmology & Visual Sciences, KTPH; Education Director, EDO, KTPH • Lee Yoke Kee, Senior Nurse Educator, Nursing Administration, KTPH NHG Teaching Award for Senior Doctors • Dr Toh Hong Chuen, Senior Consultant, Acute and Emergency Care Centre, KTPH
• Dr Lekha Gopal, Senior Consultant, Ophthalmology & Visual Sciences, KTPH • Dr Leong Chuo Ren, Senior Consultant, General Surgery, KTPH • Dr Jerry Goo Tiong Thye, Senior Consultant, General Surgery, KTPH • Dr Christie Lyndsay Mei Janet, Associate Consultant, Acute and Emergency Care Centre, KTPH • Dr Marc Ong Weijie, Associate Consultant, General Surgery, KTPH • Dr Clement Chia Luck Khng, Associate Consultant, General Surgery, KTPH NHG Teaching Award for Junior Doctors • Dr Sangtam Tiakumzuk, Registrar, Ophthalmology & Visual Sciences, KTPH • Dr Surinderjit Singh Satwant Singh, Clinical Associate, Orthopaedic Surgery, KTPH NHG Inter-Professional Teaching Award • Dr Khemlani Mansha Hari, Senior Consultant, Geriatric Medicine, KTPH • Foo Meow Ling, Nurse Clinician, Infection Control, KTPH • Nor Syafawati Binte Juma’at, Assistant Nurse Clinician, Nursing Administration, KTPH NHG Outstanding Nurse Teachers Award • Kathy Lam Sie Mien, Nurse Educator, Nursing Administration, YCH • Catherine Hu Youqin, Nurse Educator, Nursing Administration, KTPH • Alberto Albert Kim Christian Panado, Senior Staff Nurse, Acute and Emergency Care Centre, KTPH • Fatin Fairuz Binte Abdul Haddy, Senior Staff Nurse, Ward B106, KTPH • Aisyah Binte Nasir, Senior Staff Nurse, Ward B86, KTPH NHG Teaching Award for Allied Health Senior Educators • Khoo Sue Anne, Principal Clinical Psychologist, Psychology Service, KTPH • Mabel Yum Po Shan, Principal Clinical Psychologist, Psychology Service, KTPH • Eunice Yap Yu Ming, Principal Clinical Psychologist, Psychology Service, KTPH • Phoenix Tong Po Yu, Principal Physiotherapist, Rehabilitation Services, KTPH • Thng Chew Khim, Senior Radiographer, Diagnostic Radiology, KTPH NHG Teaching Award for Allied Heath Educators • Giang Thuy Anh, Senior Occupational Therapist, Rehabilitation Services, KTPH • Sunny Tan Boon Chai, Senior Physiotherapist, Rehabilitation Services, KTPH • Jeanette Lee Ming Yan, Senior Speech Therapist, Rehabilitation Services, KTPH
NHG Teaching Award for Pharmacy Senior Preceptors • Heng Jian Wei, Senior Pharmacist, Pharmacy, KTPH NHG Teaching Award for Nursing Preceptors • Angeline Aw Run Qi, Senior Staff Nurse, Ward B106, KTPH • Ngee Shi Wei, Senior Staff Nurse, Ward B106, KTPH • Ramanathan S/O Perumal, Senior Staff Nurse, Ward B65, KTPH • Tan Rodchell San Miguel, Senior Staff Nurse, Ward D67, YCH • Aisyah Binte Rahamat, Staff Nurse, Ward B105, KTPH ASIAN HOSPITAL MANAGEMENT AWARDS Gold Award, Facility Management and Financial Improvement Project • A Health-Promoting Medical Facility, AdMC Excellence Award, Community Involvement Project • Community & Home Eye Screening Service (CHESS), Ophthalmology & Visual Sciences, KTPH ANN WEE NUS SOCIAL WORK ALUMNI AWARD • Jenny Goh, Deputy Head, Medical Social Service, Yishun Health; Principal Medical Social Worker, Medical Social Service, KTPH HUMAN CITY DESIGN AWARDS Human City Design Award • Wellness Kampung, PHCT, Yishun Health OCT 2019 SINGAPORE HEALTH AWARD 2019 Singapore HEALTH Award (Merit) • Yishun Health COMMUNITY CHEST AWARDS Charity Gold Award • Yishun Health SINGAPORE PATIENT ACTION AWARDS Singapore Patient Engagement Initiative Award • Forget Us Not (FUN), KTPH Dementia Team, Lien Foundation, and Alzheimer’s Disease Association (ADA) 17TH SINGAPORE HEALTH & BIOMEDICAL CONGRESS Singapore Clinician Investigator Award (Gold) • Dr Serena Low, Consultant, Clinical Research Unit, KTPH SHBC Best Poster Award (Allied Health) (Silver) • Dr Shao Yi-Ming, Assistant Manager, Clinical Research Unit, KTPH SHBC Best Poster Award (Allied Health) (Merit) • Wee Guan Lim, Senior Medical Technologist, Laboratory Medicine, KTPH
SHBC Best Poster Awards (Basic Science/Translational Research) (Gold) • Dr Angela Moh, Senior Research Officer, Clinical Research Unit, KTPH SHBC Best Poster Awards (Basic Science/Translational Research) (Merit) • Dr Serena Low, Consultant, Clinical Research Unit, KTPH SHBC Best Poster Awards (Clinical Research) (Gold) • Dr Angela Moh, Senior Research Office, Clinical Research Unit, KTPH SHBC Best Poster Award (Health Professions Education) • Clarisse Look, Senior Speech Therapist, Rehabilitation Services, KTPH SHBC Best Poster Award (Health Services Research) (Merit) • Dr Deborah Ng, Senior Staff Physician, General Surgery, KTPH SHBC Best Poster Award (Nursing) (Merit) • Jocelyn Loke, Senior Staff Nurse, GeriCare@North, KTPH Singapore Young Investigator Award (Clinical Research) (Gold) • Dr Desmond Mao, Consultant, Acute and Emergency Care Centre, KTPH Singapore Young Investigator Award (Clinical Research) (Bronze) • Dr Ang Su Fen, Senior Research Officer, Clinical Research Unit, KTPH Singapore Allied Health Award (Bronze) • Wang Jiexun, Senior Biostatistician, Clinical Research Unit, KTPH Singapore Nursing Award (Silver) • Cheng Ling Jie, Staff Nurse, Ward D87, KTPH NOV 2019 COMMUNITY GARDEN EDIBLES COMPETITION • Heaviest Pumpkin (1st Place) Khoo Teck Puat Hospital • Heaviest Pumpkin (3rd Place) Yishun Community Hospital MOH DISTINGUISHED SENIOR CLINICIAN AWARD • A/Prof Chin Thaim Wai, Senior Consultant, Orthopaedic Surgery, KTPH JAN 2020 PUBLIC SECTOR TRANSFORMATION AWARDS 2020 Exemplary Leader Award • Dr Wong Sweet Fun, Chief Transformation Officer; Deputy Chairman, Medical Board (Population Health); Clinical Director, PHCT, Yishun Health 93
JOURNAL PUBLICATIONS
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO.
94
Acute & Emergency
Desmond Mao Renhao
Effect of Vertical Location on Survival Outcomes for Out-of-Hospital Cardiac Arrest in Singapore
Resuscitation
139
24 – 32
Acute & Emergency
Desmond Mao Renhao
Inter-Hospital Variations in Resuscitation Processes and Outcomes of Out-of-Hospital Cardiac Arrests in Singapore
Journal of Emergency and Critical Care Medicine
3
21 – 30
Acute & Emergency
Desmond Mao Renhao
Effectiveness of a Community Based Out-of-Hospital Cardiac Arrest (OHCA) Interventional Bundle: Results of a Pilot Study
Resuscitation
146
220 – 228
Acute & Emergency
Desmond Mao Renhao
Emergency Medical Dispatch Services Across Pan-Asian Countries: A Web-Based Survey
BMC Emergency Medicine
20
1 – 8
Anaesthesia
Edwin Seet
Association of Unrecognized Obstructive Sleep Apnea With Postoperative Cardiovascular Events in Patients Undergoing Major Noncardiac Surgery
Journal of the American Medical Association
321 (18)
1788 – 1798
Anaesthesia
Edwin Seet, Chandra Mohan Kumar
Letter to the Editor: In Response
Anesthesia & Analgesia
128 (4)
e58 – e59
Anaesthesia
Bin Wern Hsien, Ashutosh Joshi, Edwin Seet
Use of King Vision® Videolaryngoscope for Nasotracheal Intubation: A Prospective Observational Study
Journal of Clinical Anesthesia
58
3–4
Anaesthesia
Li Woan Wui, Daniel Lee Jin Keat, Kang Min Li, Venkatesan Kumaresh, Jerry Goo
A Comprehensive Analysis of Traumatic Rib Fractures in an Acute General Hospital in Singapore
Journal of Emergencies, Trauma, and Shock
12 (2)
145 – 149
Anaesthesia
Naville Chia
Singapore Spice: Sedation Practices in Intensive Care Evaluation in Singapore – A Prospective Cohort Study of the Public Healthcare System
Singapore Medical Journal
61 (1)
19 – 23
Anaesthesia
Edwin Seet, Chandra Mohan Kumar
Perioperative Considerations and Anesthesia Management in Patients With Obstructive Sleep Apnea Undergoing Ophthalmic Surgery
Journal of Cataract 45 (7) & Refractive Surgery
1026 – 1031
Anaesthesia
Chandra Mohan Kumar, Edwin Seet
Peri-Operative Considerations for Sedation-Analgesia During Cataract Surgery: A Narrative Review
Anaesthesia
74 (12)
1601 – 1610
Anaesthesia
Joselo Macachor
The Block Room
Academy of Regional Anaesthesia
–
15 – 17
Anaesthesia
Ashutosh Joshi
Lateral Femoral Cutaneous Nerve
Ultrasound for Interventional Pain Management
–
121 – 129
Anaesthesia
Edwin Seet, Wang Jiexun
Factors Predicting One-Year Post-Surgical Mortality Amongst Older Asian Patients Undergoing Moderate to Major Non-Cardiac Surgery – A Retrospective Cohort Study
BMC Surgery
20 (1)
11
Anaesthesia
Chandra Mohan Kumar
Review of Anaesthetic Management for Cataract Surgery in Transplant Recipients
Anaesthesia and Intensive Care
48 (1)
25 – 35
Anaesthesia
Chandra Mohan Kumar, Edwin Seet
Measuring Endotracheal Tube Intracuff Pressure: No Room for Complacency
Journal of Clinical Monitoring and Computing
–
1–8
Anaesthesia
Yvonne Wong Chiong Ling
Sellick Maneuver Assisted Real-Time to Achieve Target Force Range in Simulated Environment – A Prospective Observational Cross-Sectional Study on Manikin
PLOS ONE
15 (2)
–
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO. Anaesthesia
Sanjay Bajaj
Scope of Hand Surgery Using Surgeon Administered Local/Regional Anaesthesia
Annals of Plastic Surgery
83 (3)
278 – 284
Anaesthesia / Ophthalmology and Visual Sciences
Chandra Mohan Kumar, Lekha Gopal, Edwin Seet
Choosing Anaesthesia Option for Cataract Surgery in Patients With Dementia
Journal of Anaesthesiology and Clinical Pharmacology
35
81 – 84
Cardiology
Michael Liang Mao-Chen
Prognostic Implications of Left Ventricular Global Longitudinal Strain in Patients With Bicuspid Aortic Valve Disease and Preserved Left Ventricular Ejection Fraction
European Heart Journal – Cardiovascular Imaging
21 (7)
759 – 767
Clinical Research Unit
Serena Low Kiat Mun, Xiao Zhang, Wang Jiexun, Yeoh Lee Ying, Allen Liu Yan Lun, Ang Su Fen, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Impact of Haemoglobin A1c Trajectories on Chronic Kidney Disease Progression in Type 2 Diabetes
Nephrology
24 (10)
1026 – 1032
Clinical Research Unit
Liu Jianjun, Sylvia Liu, Resham Lal Gurung, Keven Ang, Sum Chee Fang, Subramaniam Tavintharan, Lim Su Chi
Arterial Stiffness Modulates the Association of Resting Heart Rate With Rapid Renal Function Decline in Individuals With Type 2 Diabetes Mellitus
Arteriosclerosis, Thrombosis, and Vascular Biology
39 (11)
2437 – 2444
Clinical Research Unit
Angela Moh Mei Chung, Wang Jiexun, Clara Tan, Ang Su Fen, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Association Between Gain in Adiposity and Diabetic Kidney Disease Worsening in Type 2 Diabetes is Mediated by Deteriorating Glycaemic Control: A 3-year Follow-up Analysis
Diabetes Research and Clinical Practice
157
107812
Clinical Research Unit
Serena Low Kiat Mun, Ang Su Fen, Angela Moh Mei Chung, Wang Jiexun, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
The Prevalence of Sarcopenic Obesity and Its Association With Cognitive Performance in Type 2 Diabetes in Singapore
Clinical Nutrition
39 (7)
2274 – 2281
Clinical Research Subramaniam Tavintharan Unit
Does Balance Confidence Improve in Tandem With Balance Performance? A Longitudinal Study in Diabetic Patients
Archives of Physical Medicine and Rehabilitation
100 (10)
e64
Clinical Research Angela Moh Mei Chung, Serena Low Kiat Mun, Unit Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Role of Endothelium-Independent Microcirculation Vasodilation in the Relationship Between Visceral Adiposity and Reduced Cognitive Performance in Older Adults With Type 2 Diabetes
27 (4)
e012609
Clinical Research Unit
Angela Moh Mei Chung, Sharon Pek Li Ting, Liu Jianjun, Wang Jiexun, Subramaniam Tavintharan, Keven Ang, Sum Chee Fang, Lim Su Chi
Plasma Osteoprotegerin as a Biomarker of Poor Glycaemic Control That Predicts Progression of Albuminuria in Type 2 Diabetes Mellitus: A 3-Year Longitudinal Cohort Study
Diabetes Research and Clinical Practice
161
107992
Clinical Research Unit
Angela Moh Mei Chung, Serena Low Kiat Mun, Wang Jiexun, Ang Su Fen, Clara Tan, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Association of Traditional and Novel Measures of Central Obesity With Cognitive Performance in Older Multi-Ethnic Asians With Type 2 Diabetes
Clinical Obesity
10 (2)
e12352
Clinical Research Unit
Angela Moh Mei Chung, Ang Su Fen, Wang Jiexun, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Association Between Lower Extremity Skeletal Muscle Mass and Impaired Cognitive Function in Type 2 Diabetes
Scientific Reports
10
2956
95
JOURNAL PUBLICATIONS
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO. Clinical Research Unit
Clara Tan, Ang Su Fen, Lim Su Chi
Response to Multiple GlucoseLowering Agents in a Sib-Pair With a Novel HNF1a (MODY3) Variant
European Journal of Human Genetics
28
518 – 520
Clinical Research Unit
Sharon Pek Li Ting, Lim Su Chi, Keven Ang, Sum Chee Fang, Subramaniam Tavintharan
Endothelin-1 Predicts Incident Diabetic Peripheral Neuropathy in Type 2 Diabetes: A Cohort Study
European Journal of Endocrinology
182 (4)
429 – 438
Clinical Research Unit
Liu Jianjun, Sylvia Liu, Resham Lal Gurung, Lim Su Chi
Association of Urine Haptoglobin With Risk of All-Cause and CauseSpecific Mortality in Individuals With Type 2 Diabetes: A Transethnic Collaborative Work
Diabetes Care
43 (8)
625 – 633
Clinical Research Unit
Resham Lal Gurung, M Yiamunaa, Sylvia Liu, Liu Jianjun, Clara Chan, Keven Ang, Sum Chee Fang, Subramaniam Tavintharan, Lim Su Chi
Association of Haptoglobin Phenotype With Incident Acute Myocardial Infarction in Chinese Patients With Type 2 Diabetes
Cardiovascular Diabetology
18
1–9
Clinical Research Unit
Sylvia Liu, Liu Jianjun, Resham Lal Gurung, Clara Chan, Darren Yeo, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Clinical Determinants of Diabetes Progression in Multiethnic Asians With Type 2 Diabetes – A 3 Year Prospective Cohort Study
Annals, Academy of Medicine, Singapore
48 (7)
217 – 223
Clinical Research Unit
Subramaniam Tavintharan
Short-Term Strength and Balance Training Does Not Improve Quality of Life but Improves Functional Status in Individuals With Diabetic Peripheral Neuropathy: A Randomised Controlled Trial
Diabetologia
62 (12)
2200 – 2210
Clinical Research Unit
Angela Moh Mei Chung, Sum Chee Fang, Subramaniam Tavintharan, Keven Ang, Lim Su Chi
Gain in Adiposity Over 3 Years is Associated With Progressive Renal Decline in Multi-Ethnic South-East Asians With Type 2 Diabetes
Journal of Diabetes
11 (4)
316 – 325
Clinical Research Unit
Liu Jianjun, Sylvia Liu, Resham Lal Gurung, Clara Chan, Keven Ang, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi
Relationship Between Fasting Plasma Glucagon Level and Renal Function – A Cross Sectional Study in Type 2 Diabetes
Journal of the Endocrine Society
Clinical Research Unit / Anaesthesia
Claude Renaud, Wang Jiexun
Faculty Use of Active Learning in Postgraduate Nephrology Education: A Mixed Methods Study
Kidney Medicine
1 (3)
115 – 123
Clinical Research Unit / Family & Community Medicine
Serena Low Kiat Mun, Jonathon Khoo Kay Chin, Wang Jiexun, Bastari Irwan, Sum Chee Fang, Subramaniam Tavintharan, Lim Su Chi
Development of a Metabolic Syndrome Severity Score and Its Association With Incident Diabetes in an Asian Population – Results From a Longitudinal Cohort in Singapore
Endocrine
65
73 – 80
Medical Costs Associated With Chronic Kidney Disease Progression in Type 2 Diabetes
Nephrology
24 (5)
534 – 541
Association of Central Arterial Stiffness With Presence and Severity of Diabetic Retinopathy in Asians With Type 2 Diabetes
Diabetes and Vascular Disease Research
16 (6)
498 – 505
Clinical Research Serena Low Kiat Mun, Lim Su Chi, Xiao Zhang, Unit / General Wang Jiexun, Darren Yeo, Medicine Yeoh Lee Ying, Allen Liu Yan Lun, Subramaniam Tavintharan, Sum Chee Fang Clinical Research Unit / Ophthalmology and Visual Sciences
96
Xiao Zhang, Lim Su Chi, Subramaniam Tavintharan, Yeoh Lee Ying, Sum Chee Fang, Keven Ang, Darren Yeo, Serena Low Kiat Mun, Kumari Neelam
273 – 283
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO. Clinical Research Unit / Diabetes Centre / Ophthalmology and Visual Sciences
Xiao Zhang, Sharon Pek Li Ting, Subramaniam Tavintharan, Sum Chee Fang, Lim Su Chi, Keven Ang, Darren Yeo, Yip Chee Chew, Kumari Neelam
Leucine-Rich a-2-Glycoprotein Predicts Proliferative Diabetic Retinopathy in Type 2 Diabetes
Journal of Diabetes and its Complications
33 (9)
651 – 656
Diagnostic Radiology
Ashish Chawla
Sonographic Assessment of Musculoskeletal Causes of Calf Pain and Swelling
Emergency Radiology
26
349 – 359
Diagnostic Radiology
Ashish Chawla
Watch What You Swallow! – A Rare Cause of Not So Rare Entity Presenting to the Emergency Room
Journal of Gastrointestinal and Abdominal Radiology
2
49 – 52
Diagnostic Radiology
Ashish Chawla, Wilfred Peh Chin Guan
Reply To: Underestimating the Impact of Erect Abdominal Radiographs
Journal of Medical Radiation Sciences
66 (2)
146
Diagnostic Radiology
Manickam Subramanian, Dinesh Chincure
Clinics in Diagnostic Imaging (199)
Singapore Medical Journal
60 (9)
487 – 490
Diagnostic Radiology
Chin Teck Yew, Chou Hong, Wilfred Peh Chin Guan
The Acutely Injured Elbow
Radiologic Clinics of North America
57 (5)
911 – 930
Diagnostic Radiology
Sumer Shikhare Nrupendra, Wilfred Peh Chin Guan
Pyogenic Spondylodiscitis
Musculoskeletal Imaging Volume 2
87 – 90
Diagnostic Radiology
Wilfred Peh Chin Guan
Osteomyelitis of Long and Short Bones
Musculoskeletal Imaging Volume 2
91 – 96
Diagnostic Radiology
Wilfred Peh Chin Guan
Septic Arthritis
Musculoskeletal Imaging Volume 2
97 – 101
Diagnostic Radiology
Wilfred Peh Chin Guan
Soft Tissue Injections
Musculoskeletal Imaging Volume 2
102 – 108
Diagnostic Radiology
Wilfred Peh Chin Guan
Imaging of the Shoulder Bankart Lesion and Its Variants
Nepalese Journal of Radiology
9 (1)
33 – 39
Diagnostic Radiology
Geoiphy George Pulickal, Dinesh Singh, Rahul Lohan, Ashish Chawla
Dual-Source Dual-Energy CT in Submandibular Sialolithiasis: Reliability and Radiation Burden
American Journal of Roentgenology
213 (6)
1291 – 1296
Diagnostic Radiology
Geoiphy Pulickal
Conductive Hearing Loss With a “Dry Middle Ear Cleft” – A Comprehensive Pictorial Review With CT
European Journal of Radiology
110
74 – 80
Diagnostic Radiology
Sivasubramanian Srinivasan, Ashish Chawla
Patterns and Signs in Thoracic Imaging
Thoracic Imaging Basic to Advanced
1 – 29
Diagnostic Radiology
Ashish Chawla
Imaging of Large and Small Airways
Thoracic Imaging Basic to Advanced
31 – 64
Diagnostic Radiology
Ashish Chawla
Imaging of Cystic Lung Diseases
Thoracic Imaging Basic to Advanced
65– 83
Diagnostic Radiology
Ashish Chawla
Imaging of Pulmonary Nodules
Thoracic Imaging Basic to Advanced
85 – 100
Diagnostic Radiology
Sumer Shikhare Nrupendra
Imaging of Thoracic Malignancies
Thoracic Imaging Basic to Advanced
101 – 146
Diagnostic Radiology
Dinesh Singh
Imaging of Pulmonary Infections
Thoracic Imaging Basic to Advanced
147 – 172
Diagnostic Radiology
Rahul Lohan
Imaging of ICU Patients
Thoracic Imaging Basic to Advanced
173 – 194
Diagnostic Radiology
Ashish Chawla, Lim Tze Chwan
Imaging of the Mediastinum
Thoracic Imaging Basic to Advanced
195 – 234
Diagnostic Radiology
Ashish Chawla
Imaging of Pulmonary Artery
Thoracic Imaging Basic to Advanced
235 – 267
97
JOURNAL PUBLICATIONS
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO.
98
Diagnostic Radiology
Raymond Chung
Imaging of the Aorta
Thoracic Imaging Basic to Advanced
269 – 293
Diagnostic Radiology
Pratik Mukherjee, Lim Tze Chwan, Ashish Chawla
Imaging of the Esophagus
Thoracic Imaging Basic to Advanced
295 – 324
Diagnostic Radiology
Dinesh Singh
Imaging of Chest Wall and Pleura
Thoracic Imaging Basic to Advanced
325 – 360
Diagnostic Radiology
Ashish Chawla
Imaging of Interstitial Lung Diseases
Thoracic Imaging Basic to Advanced
361 – 423
Diagnostic Radiology
Ashish Chawla
Imaging of Miscellaneous Diseases
Thoracic Imaging Basic to Advanced
425 – 455
Diagnostic Radiology
Ashish Chawla, Sumer Shikhare Nrupendra, Lim Tze Chwan, Wilfred Peh Chin Guan
Computer Vision Syndrome: Darkness Under the Shadow of Light
Canadian Association of Radiologists Journal
70 (1)
5–9
Diagnostic Radiology
Trishna Shimpi Ramesh, Sumer Shikhare Nrupendra, Raymond Chung, Wilfred Peh Chin Guan
Imaging of Gastrointestinal and Abdominal Emergencies in Binge Drinking
Canadian Association of Radiologists Journal
70 (1)
52 – 61
Diagnostic Radiology
Sivasubramanian Srinivasan
Commentary: Noncardiac Uses of Chest Ultrasonography Other Than Pleural Effusion
Indian Journal of Radiology and Imaging
29 (1)
98
Diagnostic Radiology
Wilfred Peh Chin Guan
The Role of Magnetic Resonance Imaging in the Evaluation of Scaphoid Fractures
Journal of Medical Radiation Sciences
66 (1)
3–4
Pharmacy / Jessica Goh Hui Fe, General Medicine Ooi Say Tat, (Infectious Lee Siok Ying Diseases)
Optimizing Vancomycin Dosing in Chronic Kidney Disease by Deriving and Implementing a WebBased Tool Using a Population Pharmacokinetics Analysis
Frontiers in Pharmacology
10
1 – 11
General Surgery
Daniel Lee Jin Keat, Tan Kok Yang
Frailty in Surgical Preoperative Evaluation and Postoperative Recovery
Current Geriatrics Reports
8
87 – 96
General Surgery
Lim Woan Wui, Daniel Lee Jin Keat, Kang Min Li, Jerry Goo Tiong Thye
A Comprehensive Analysis of Traumatic Rib Fractures in an Acute General Hospital in Singapore
Journal of Emergencies, Trauma, and Shock
12 (2)
145 – 149
General Surgery
Clement Chia Luck Khng, Anil Dinkar Rao, Reyaz Moiz Singaporewalla
Assessing Adequacy of Informed Consent for Elective Surgery by Student-Administered Interview
ANZ Journal of Surgery
89 (6)
677 – 682
General Surgery
Surendra Kumar Mantoo
Multifocal Small Bowel Adenocarcinoma Mimicking Crohn’s Disease
Gastrointestinal Endoscopy
90 (4)
691 – 693
General Surgery
Clement Chia Luck Khng, Daniel Lee Jin Keat, Anil Dinkar Rao, Lim Woan Wui, Tan Kok Yang, Jerry Goo Tiong Thye
Early Laparoscopic Cholecystectomy by a Dedicated Emergency Surgical Unit Confers Excellent Outcomes in Acute Cholecystitis Presenting Beyond 72 Hours
ANZ Journal of Surgery
89 (11)
1446 – 1450
General Surgery
Jerry Goo Tiong Thye
The Price of Personal Mobility: Burden of Injury and Mortality From Personal Mobility Devices in Singapore – A Nationwide Cohort Study
BMC Public Health
19
880
General Surgery
Ng Zhi Xu
Is Anticoagulation for Venous Thromboembolism Safe for Asian Elective Neurosurgical Patients? – A Single Centre Study
ANZ Journal of Surgery
89 (7-8)
919 – 924
General Surgery
Eugene Yang Weiren
Cranial Infections
Oxford Textbook of Neurosurgery
–
–
General Surgery / General Medicine
Tan Man Hong, Clement Chia Luck Khng, Vikram Janardan Sonawane, Reyaz Moiz Singaporewalla
Rare Case of an Adrenal Tumor: Phaeochromocytoma with Concomitant Hypercortisolism
Journal of Surgery & 3 (1) Clinical Practice
1–3
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO. Geriatric Medicine
Rachel Cheong Chin Yee, Than Htun Aung, Pang Wee Yang, Ng Chong Jin, Philip Yap Lin Kiat
Isolated Complete Unilateral Ptosis With Intact Extraocular Eye Movements
Age & Ageing
48 (4)
596 – 597
Geriatric Medicine
Philip Yap Lin Kiat
A 3-Item Screening Scale for Caregiver Burden in Dementia Caregiving: Scale Development and Score Mapping to the 22-Item Zarit Burden Interview
Journal of the American Medical Directors Association
20 (5)
629 – 633
Geriatric Medicine
Philip Yap Lin Kiat
Symptom Clusters of Subjective Cognitive Decline Amongst Cognitively Normal Older Persons and Their Utilities in Predicting Objective Cognitive Performance: Structural Equation Modelling
European Journal of Neurology
26 (9)
1153 – 1160
Geriatric Medicine
Philip Yap Lin Kiat
The Optimal Short Version of the Zarit Burden Interview for Dementia Caregivers: Diagnostic Utility and Externally Validated Cutoffs
Aging & Mental Health
23 (6)
706 – 710
Geriatric Medicine
Giang Thuy Anh, Philip Yap Lin Kiat
The Effectiveness of Horticultural Therapy on Older Adults: A Systematic Review
Journal of the American Medical Directors Association
20 (10)
1351.e1 – 1351.e11
Geriatric Medicine
Philip Yap Lin Kiat
Validity and Utility of the Center for Epidemiological Studies Depression Scale for Detecting Depression in Family Caregivers of Persons With Dementia
Dementia and Geriatric Cognitive Disorders
47 (4-6)
323 – 334
Geriatric Medicine
Philip Yap Lin Kiat
Comparing the Effects of Grief and Burden on Caregiver Depression in Dementia Caregiving: A Longitudinal Path Analysis Over 2.5 Years
Journal of the American Medical Directors Association
20 (8)
977 – 983
Geriatric Medicine
Philip Yap Lin Kiat, Rachel Cheong Chin Yee
Deep but Not Periventricular White Matter Disease is a Marker for Frailty in Older Patients With Early Alzheimer’s Disease
Advances in Geriatric Medicine and Research
–
1 – 10
Geriatric Medicine
Philip Yap Lin Kiat
The Three Dimensions of Caregiver Grief in Dementia Caregiving: Validity and Utility of the Subscales of the MarwitMeuser Caregiver Grief Inventory
International Journal of Geriatric Psychiatry
35 (2)
213 – 222
Geriatric Medicine
Philip Yap Lin Kiat, Ang Yan Hoon
Dyadic Approach to Post-Stroke Hospitalizations: Role of Caregiver and Patient Characteristics
BMC Neurology
19
267
Geriatric Medicine
Khoo Sue Ann, Chan Sue Mei, Philip Yap Lin Kiat
Assessment of Sarcopenia Among Community-Dwelling At-Risk Frail Adults Aged 65 Years and Older Who Received Multidomain Lifestyle Interventions: A Secondary Analysis of a Randomized Clinical Trial
JAMA Network Open
2 (10)
e1913346
Geriatric Medicine
Ang Yan Hoon, Wong Chek Hooi
From Hospital to Home: Impact of Transitional Care on Cost, Hospitalisation and Mortality
Annals, Academy of Medicine, Singapore
48 (10)
333 – 337
Geriatric Medicine
Rachel Cheong Chin Yee
Risk Factors of Progression to Frailty: Findings From the Singapore Longitudinal Ageing Study
The Journal of Nutrition, Health & Aging
24 (1)
98 – 106
Geriatric Medicine
Wong Chek Hooi, Jagadish Ullal Mallya
Cognitive Appraisal and Knowledge as Risk Factors for High Fear of Falling in Older and Middle-Aged Adults in Singapore
Innovation in Aging
3
S473
Geriatric Medicine
Wong Chek Hooi, Jagadish Ullal Mallya
Indoor and Real-Life Outdoor Gait Speed and Its Association on Geographic Lifespace and Outdoor Mobility
Innovation in Aging
3
S472 – S473
99
JOURNAL PUBLICATIONS
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO.
100
Geriatric Medicine
Philip Yap Lin Kiat
A Brief, 6-Item Scale for Caregiver Grief in Dementia Caregiving
Gerontologist
60 (1)
e1 – e10
Geriatric Medicine
Wong Chek Hooi, Jagadish Ullal Mallya
111 Disparities Between Actual and Perceived Fall Risk Affect Participation in 5 Fall Prevention Interventions
Age and Ageing
48
iv18 – iv27
Geriatric Medicine
Wong Chek Hooi, Jagadish Ullal Mallya
135 Gendered Differences in Effect of Falls-Related Threat Appraisal on Attitudes Towards Exercise Amongst Community-Dwelling Older Singaporeans
Age and Ageing
48
iv28 – iv33
Geriatric Medicine
Wong Chek Hooi, Jagadish Ullal Mallya
136 Barriers to Discussing Fall Prevention With Healthcare Professionals Amongst Community-Dwelling Singaporean Older Adults
Age and Ageing
48
iv28 – iv33
Laboratory Medicine
Rama Narayana Deepak
One Hypervirulent Clone, Sequence Type 283, Accounts for a Large Proportion of Invasive Streptococcus Agalactiae Isolated From Humans and Diseased Tilapia in Southeast Asia
PLOS Neglected Tropical Diseases
13 (6)
e0007421
Laboratory Medicine
Rama Narayana Deepak
Antecedent Carbapenem Exposure as a Risk Factor for Non-CarbapenemaseProducing CarbapenemResistant Enterobacteriaceae and Carbapenemase-Producing Enterobacteriacea
Antimicrobial Agents and Chemotherapy
63 (10)
e00845 – 19
Nursing Research Unit
Cheng Ling Jie
A Systematic Review and MetaAnalysis: Vinegar Consumption on Glycaemic Control in Adults With Type 2 Diabetes Mellitus
Journal of Advanced Nursing
76 (2)
459 – 474
Nursing Research Unit
Mok Wen Qi, Chin Guey Fong, Yap Suk Foon
A Cross Sectional Survey on Nurses’ Second Victim Experience and Quality of Support Resources in Singapore
Journal of Nursing Management
28 (2)
286 – 293
Ophthalmology and Visual Science
Jason Lee Kian Seng
Optimizing Esthetic Outcomes in Graded Full-Thickness Anterior Blepharotomy for Graves’ Ophthalmopathy
257
1303 – 1308
Ophthalmology and Visual Sciences
Bindu Rajesh
Safety of 6000 Intravitreal Dexamethasone Implants
Graefe’s Archive for Clinical and Experimental Ophthalmology British Journal of Ophthalmology
104 (1)
39 – 46
Ophthalmology and Visual Sciences
Sangtam Tiakumzuk, Anoop Thomas
Young’s Modulus Determination of Normal and Glaucomatous Human Iris
Investigative Ophthalmology & Visual Science
60 (7)
2690 – 2695
Ophthalmology and Visual Sciences
Kumari Neelam
Singapore Chinese Eye Study: Key Findings From Baseline Examination and the Rationale, Methodology of the 6-Year Follow-Up Series
British Journal of Ophthalmology
104 (5)
610 – 615
Ophthalmology and Visual Sciences
Kumari Neelam
The Association Between Body Composition Using Dual Energy X-Ray Absorptiometry and Type 2 Diabetes: A Systematic Review and Metanalysis of Observational Studies
Scientific Reports
9
12634
Ophthalmology and Visual Sciences
Bashajan Sowkathali, Hnin Hnin Oo
Concurrent Presence of Retinal Hemorrhages in the Setting of Acute Vogt-Koyanagi-Harada Syndrome – An Unusual Presentation
Journal of Ophthalmic Inflammation and Infection
10
12
Ophthalmology and Visual Sciences
Kumari Neelam
Cataract Surgery and 6-Year Incidence of AMD in Multiethnic Asian Cohort
Asia-Pacific Journal of Ophthalmology
9 (2)
130 – 136
PAGE DEPARTMENT AUTHORS TITLE OF PAPER JOURNAL VOLUME NO. Ophthalmology and Visual Sciences
Philip Francis Stanley, Lai Foon Wan, Rostihar Abdul Karim
A Randomized Prospective Placebo-Controlled Study of the Effects of Lavender Aromatherapy on Preoperative Anxiety in Cataract Surgery Patients
Journal of PeriAnaesthesia Nursing
35 (4)
403 – 406
Ophthalmology and Visual Sciences
Sangtam Tiakumzuk, Anoop Thomas, Philemon Huang
Phacoemulsification Vs Phacoemulsification With MicroBypass Stent Implantation in Primary Angle Closure and Primary Angle Closure Glaucoma: A Randomised Single-Masked Clinical Study
Clinical & Experimental Ophthalmology
48 (4)
450 – 461
Ophthalmology and Visual Sciences
Sangtam Tiakumzuk
Outcome & Complications of Combined Modified Deep Sclerectomy and Trabeculectomy for Surgical Management of Glaucoma: A Pilot Study
Clinical Ophthalmology
14
795 – 803
Orthopaedic Surgery
Timothy Teo Wei Wen
Ossification of the Yellow Ligament BioMedicine in the Cervical Spine – An Unusual Location
9 (2)
14
Orthopaedic Surgery
Shauna Christine Sim, Alvin Tan, Sirisena Udawattage Dinesh Chaminda
Partial Patella Tendon Tear in a Middle-Aged Man With No Previous Knee Injuries: A Non-Surgical Approach
Annals, Academy of Medicine, Singapore
48 (8)
268 – 273
Orthopaedic Surgery
Kelvin Lor Kah Ho, Toon Dong Hao
Buttress Plate Fixation of Coronoid Process Fractures via a Medial Approach
Chinese Journal of Traumatology
22 (5)
255 – 260
Orthopaedic Surgery
Antony Xavier Rex Premchand
Epidemiology of Inpatient Tibia Fractures in Singapore – A Single Centre Experience
Chinese Journal of Traumatology
22 (2)
99 – 102
Orthopaedic Surgery
Sirisena Udawattage Dinesh Chaminda
Scoping Review and International Multi-Centre Cohort Study Investigating Teaching, Knowledge and Beliefs Regarding Physical Activity as a Health Intervention Among Medical Students: A Comparison Between Singapore and UK
Singapore Medical Journal
60 (12)
642 – 651
Pharmacy
Hobart Owen Ng Tsai
Pharmacological Review of Anticoagulants
Anticoagulation Drugs – The Current State of the Art
–
–
Pharmacy
Doreen Tan Su-Yin
CYP2C19 Phenotype in South-East Asian Acute Coronary Syndrome Patients and Impact on Major Adverse Cardiovascular Events
Journal of Clinical Pharmacy and Therapeutics
45 (1)
52 – 58
Pharmacy
Doreen Tan Su-Yin
Patients’ and Caregivers’ Attitudes The Journals of Towards Deprescibing in Singapore Gerontology: Series A
Pharmacy / Cardiology
Doreen Tan Su-Yin, Kim Ji Heon, Syed Saqib Imran
Switching from Ticagrelor to Clopidogrel in Asian patients with ST-Elevated Myocardial Infarction – A Time Dependent Analysis Study
Acta Cardiologica Sinica (The Official Journal of the Taiwan Society of Cardiology)
36 (1)
8 – 15
Psychological Medicine
Soh Keng Chuan, Lim Wei Shyan, Cheang Ka Man, Chan Keen Loong
Stigma Towards Alcohol Use Disorder: Comparing Healthcare Workers With the General Population
General Hospital Psychiatry
58
39 – 44
Psychological Medicine
Lim Wei Shyan
Maximizing Efficacy of Positive Psychological Interventions: Developing Positive Interventions for Use in Eastern Cultures
Positive Psychological Intervention Design and Protocols for Multi-Cultural Contexts
1–8
277 – 295
101
ADMIRALTY MEDICAL CENTRE 676 Woodlands Drive 71 #03-01 Kampung Admiralty Singapore 730676 www.admiraltymedicalcentre.com.sg
KHOO TECK PUAT HOSPITAL 90 Yishun Central Singapore 768828 www.ktph.com.sg
YISHUN COMMUNITY HOSPITAL 2 Yishun Central 2 Singapore 768024 www.yishuncommunityhospital.com.sg
WELLNESS KAMPUNG 115 Chong Pang 115 Yishun Ring Road #01-495 Singapore 760115 260 Nee Soon East 260 Yishun Street 22 #01-87 Singapore 760260 765 Nee Soon Central 765 Yishun Street 72 #01-366 Singapore 760765