E X P L O R I N G N O N - I N V A S I V E O P T I O N S
A I M A T M E L A N O M A P U B L I C A T I O N
SPOT CHECK
FOR MELANOMA
Melanoma is a potentially fatal disease that is largely preventable. AIM at Melanoma raises awareness of preventive measures; provides support for patients, caregivers, and survivors; and funds critical research all to end melanoma in our lifetime. AIM is dedicated to fighting the world’s deadliest skin cancer, melanoma.


AIMATMELANOMA.ORG
CONT ENTS
PAGE 1
INTRO
PAGE 2
THE BENEFITS OF EARLY DETECTION OF MELANOMA
PAGE 3
RISK FACTORS FOR MELANOMA
PAGE 4
PERSONAL RISK FACTORS
PAGE 5-6
RISKY SPOTS
PAGE 7
EVALUATION OF SUSPICIOUS SPOTS
PAGE 8-9
NON- INVASIVE OPTIONS
PAGE 10
NON-INVASIVE GENETIC STICKER
PAGE 11
HOW DOES THE NON-INVASIVE GENETIC STICKER WORK?
PAGE 12
HOW IS THE NON-INVASIVE GENETIC STICKER TEST PERFORMED?
PAGE 13
HOW MUCH DOES THE NON-INVASIVE GENETIC STICKER COST?
PAGE 14
ADVOCATE FOR YOURSELF
PAGE 15
QUESTIONS TO ASK YOUR DOCTOR ABOUT MOLES OR SPOTS THAT ARE CONCERNING

PAGE 16
RESOURCES

When you see your doctor for a skin check or seek care for a lesion that is suspicious for melanoma, the evaluation process can be mysterious and scary. How does your doctor recognize melanoma? Is a biopsy always necessary? How sure can your doctor be in the diagnosis? But if you understand the process and the lesion evaluation tools that are available, you can alleviate some of the fear and be an active participant in your own care.
This e-magazine provides an overview of the different ways suspicious pigmented lesions can be evaluated, with a special focus on the potential role for non-invasive tests, including the noninvasive genetic sticker test.

Melanoma is a particularly dangerous form of skin cancer that can spread quickly to other sites of the body To detect a melanoma early, before it has had the chance to spread, you and your healthcare team should monitor your skin on a regular basis

This e-magazine provides you with information about:
The benefits of early detection of melanoma
Risk factors for melanoma
How spots are evaluated to determine if they are suspicious for melanoma (biopsy as well as non-invasive tests)
The non-invasive genetic sticker test
How to advocate for yourself
It’s important that you are able to advocate for yourself and your skin care If you are at risk for melanoma, you deserve to have professionals monitor your skin carefully, using the best tools available to look for melanoma and other skin cancers so that those cancers can be identified and treated as early as possible
INTRO
page |1
THE BENEFITS OF EARLY DETECTION OF MELANOMA
The skin is the largest and most exposed organ in the body. More people are diagnosed with skin cancer every year in the United States than all other cancers combined. Therefore, it’s important to monitor your skin for cancer, especially melanoma. While melanoma is rare accounting for only 1% of skin cancers it causes a large proportion of the deaths from skin cancer.

Why is melanoma so deadly? Because it can easily and quickly spread (metastasize) to other organs. Melanoma experts stage (figure out the extent of) melanoma based on how thick it is, whether it is ulcerated, and how much it has spread. In Stage I and Stage II melanoma, depth and ulceration are the two important factors.
When melanoma metastasizes (spreads), it is harder to treat and can be deadly. For instance, when melanoma is localized (Stage 0, I, or II), the five-year survival rate is 99.5%, meaning more than 99 out of 100 people will be alive five years after diagnosis. The five-year survival rate drops to 71% for people with Stage III melanoma (called “regional” disease because it has spread, but not too far), and 32% for people with Stage IV melanoma (called “distant” disease because it has spread to distant sites in the body).
The good news is that the earlier melanoma is found, the better the chance of achieving good outcomes. Many localized melanomas can be cut out and effectively cured by surgery. That’s why finding melanoma at its earliest stages is critical when it is most curable. You need a plan to evaluate your skin


Stage 0 (in situ): Melanoma that is confined to just the upper layer of the skin the epidermis
Stage I: Local melanoma that extends into the dermis up to 1 mm in depth regardless of ulceration status or up to 2 mm in depth if not ulcerated
Stage II: Local melanoma that is generally deeper than Stage I melanoma: either more than 1 mm and up to 2 mm if ulcerated or more than 2 mm in depth regardless of ulceration status
Stage III: Melanoma that spreads to the regional lymph nodes or to the region between the primary melanoma and those lymph nodes
Stage IV: Melanoma that spreads beyond the regional lymph nodes to distant sites (e g , to the lungs, brain, etc )
"It is critical to find melanoma at its earliest stages —when it is most curable. You need a plan to evaluate your skin."
Orit Markowitz, MD, FAAD Assistant Professor of Dermatology
Icahn School of Medicine at Mount Sinai
page |2
RISK FACTORS FOR MELANOMA

Because early detection of melanoma is important, it’s critical to look for it. Everyone should check their skin and have it checked by a health care professional. We all have skin that is exposed to the sun, so we are all at risk for skin cancer. And some of us have an increased risk compared to the general public. It’s important to know your risk so you and your healthcare provider can develop a plan for monitoring your skin that is appropriate for you.
You can think of risk in two ways your overall personal risk for melanoma as well as the risk posed by the spots themselves.

page |3
PERSONAL RISK FACTORS
A wide array of factors increase your chances of developing melanoma. These include your exposure to ultraviolet (UV) light, your skin type, your genetics, and your medical history.


Features that put you at risk for melanoma include:
High levels of UV sun exposure, including a history of sunburns

Lots of moles
Tanning bed use
Fair skin that burns easily

Family history of skin cancer
Personal history of skin cancer
Weakened immune system
Being aware of your risk factors and communicating them to your health care provider can help you make more informed health care decisions. Your health care provider can look at your skin at your regular visits. People at high risk for melanoma should be monitored by a dermatologist.
page |4
RISKY SPOTS
Your plan to check your skin should include self-checks that you can perform at home as well as regular screenings by a qualified health care professional. Self-checks involve being familiar with your skin and monitoring suspicious spots. Some of the hallmark features to look for include the ABCDEs of melanoma.
While the ABCDEs are helpful when evaluating a spot, it’s also important to trust your judgment for any spot that is concerning. Your spot does not need to have all five of the ABCDE features to be suspicious. A spot with just one of these features might warrant an appointment with your healthcare provider. Additionally, you should be on the lookout for any new or changing spots that don’t look like your other moles. If you find such a spot, schedule an appointment with a healthcare provider who has experience with melanoma.
Are there specific circumstances in which your concern for spots should be heightened? Yes. Your personal history matters. For example, a new spot that appears on your skin is more concerning as you get older or if you have a history of skin cancer. If you have had an organ transplant or are taking immunosuppressive drugs, you should also be on the lookout for new spots on your skin. Immunosuppressive drugs make it easier for cancer to evade the immune system, increasing the risk for skin cancer. It’s important to have a conversation with your healthcare provider about the recommended strategy for monitoring your skin based on your risk profile.
Melanomas are frequently asymmetrical: the shape of one half does not match the other.

Melanomas frequently have uneven or irregular borders (ragged or notched edges).


Melanomas often contain multiple shades of brown or black but can sometimes be mixed with white, gray, blue, or red. Some melanomas will show a loss of color in a preexisting mole or in the area surrounding the mole.

B C D
Melanomas are often larger than 6 mm (1/4 inch) in diameter. However, with increased awareness about early detection, about 30% of melanomas are found when they are less than 6 mm in diameter
Melanomas typically have shown some evidence of change in the months prior to diagnosis. Look for any change.

A
E
page |5
DON'T FORGET THE "UGLY DUCKLING"

An “Ugly Duckling” is a mole or lesion that is unlike the others on your skin. It might be a lighter colored or darker colored mole or lesion than the others around it, or it might be a larger or smaller mole or lesion than others around it. If you have an Ugly Duckling, show it to your healthcare provider and keep your eyes out for other different-looking moles and lesions.

page |6
EVALUATION OF SUSPICIOUS SPOTS
When a spot is suspicious, your healthcare provider will often perform a skin biopsy to determine if the spot is cancerous. In this surgical procedure, a piece (or all) of the spot is cut out and is processed. A specialist will look at the processed material under the microscope to see if it looks like melanoma.


A pathologic examination of a biopsy sample is considered the gold standard for the diagnosis of melanoma; however:
A biopsy can be overused due to an abundance of caution. A biopsy is a procedure that is needed to make a diagnosis of melanoma, but most lesions that are biopsied due to concern that they could be melanoma will turn out to be benign (noncancerous).
Biopsies increase the risk of bleeding, scarring, and infection. Not all areas can be easily biopsied because of the way the skin lies or because of risk of bleeding (e.g., the scalp, side of the nose, or the shin).

Some people may want to avoid biopsies. If you have diabetes or a bleeding disorder, you may be concerned about complications. If you have anxiety about the cutting procedure, you may wish for an alternative.
Sometimes, biopsies can miss some melanomas or diagnose some noncancerous spots as melanomas. Why does this happen? First, a biopsy and pathologic examination often look at only a piece of the spot, so it’s possible that the part of the spot that contains the melanoma is not evaluated. Secondly, not all specialists reviewing the specimens agree on what is a melanoma and what is not. That’s one reason a second opinion can be helpful when you have your pathology read.
page |7
NONINVASIVE OPTIONS

As mentioned previously, not all spots are biopsy worthy, but when there is doubt, some practitioners don’t have any other option but to cut the spot to test it. In reality, most spots fall along a continuum in terms of how suspicious they are (Figure 1). Some moles are so bland and normal looking that an experienced provider can immediately determine that they have no risk for melanoma and therefore are not biopsy worthy. At the other end of the spectrum, some spots are so clearly melanoma (e.g., the image marked “high risk” below that has all the ABCDE features), they will definitely require a biopsy. The challenging cases are those in the middle zone they seem to be potentially suspicious to the eye, but it’s unclear how high the melanoma risk is. So providers often biopsy these out of an abundance of caution. However, if the provider has the right non-invasive tools, s/he can often get a better assessment of these middle-ground cases without cutting.
Figure 1. Spectrum of risk for melanoma based on visualization and genetic testing of spots. The diagram also addresses the use of non-invasive testing for spots that are suspicious but not clearly melanoma upon visual examination.
As mentioned in the below Figure, your provider may be able to use a range of non-invasive tools to evaluate your spot(s).

FIGURE 1
page |8
Some of the non-invasive tools your provider may use to evaluate your suspicious spots.
These tools can help your provider decide which of your spots are high risk enough that they warrant a biopsy. It’s helpful to ask your provider if they have these tools and whether they can be used for any of your spots.

Dermoscopy is a technique in which the healthcare provider gently presses a handheld device called a dermatoscope against the suspicious lesion. Kind of like a specialized lighted magnifying glass, the dermatoscope allows the healthcare provider to look below the skin's surface for specific colors and patterns that would be consistent with melanoma or other skin cancers
Photography can be used to obtain close follow-up of a spot to see if it is changing or getting more suspicious. Photography can be used as part of dermoscopy as well, which provides a precise picture to examine over time
Mole mapping creates a comprehensive guide of all the moles or spots on someone's body. The spots are followed over time and photographed to look for subtle changes. This tool is often used for people with a lot of moles or who have a high risk of skin cancer



Reflectance confocal microscopy is a technique in which the provider uses laser light at an infrared wavelength to get a horizontal view of the layers of skin It produces an image similar to that observed from a biopsy
The non-invasive genetic sticker is a sticker applied to the skin that measures the presence of genes that are considered markers of melanoma (PRAME, LINC, and TERT)


page |9
NON-INVASIVE GENETIC STICKER


The non-invasive genetic sticker samples spots for the expression (production) of melanoma markers called LINC and PRAME. You can think of these genes as biomarkers for melanoma. When these two genes are positive, 93% of those spots are confirmed as melanoma when a biopsy is performed. An additional genetic test that analyzes another melanoma gene called TERT can be used after the two-gene test to increase testing sensitivity to pick up melanomas.
The non-invasive genetic sticker test has a 99% negative predictive value, which means that if the test is negative, the probability that you don’t have melanoma is 99% Therefore, if this non-invasive test is negative, you can be reasonably confident that you do not have melanoma and that a biopsy is unnecessary This result can bring peace of mind and allow you to avoid an unnecessary biopsy .

"I find the non-invasive genetic sticker helpful for patients in whom I want more information about a concerning spot but want to avoid an unnecessary biopsy, if possible."
– Laura K. Ferris, MD, PhD, Professor of Dermatology at the University of Pittsburgh
page |10
PHOTO COURTESY OF DERMTECH
HOW DOES THE NON-INVASIVE GENETIC STICKER WORK?

The genetic sticker is a pain-free adhesive that is applied directly to the area of concern for 10 to 20 seconds It samples the genetic material shed from the melanocytes that give the spot its color The sticker gently collects skin cells off the top layer of the skin within minutes, and the sample is then sent to a laboratory that measures the expression of PRAME and LINC If

WHEN IS T GENETIC
If you have a spot th criteria but is not obvio health care provider).
If you have a mole in your shin) or where th (e.g., your face).
If you have diabetes, p and/or are taking drug would make taking a bi If you have a personal phobic, concerned abo to be evaluated)
The test helps determine suspicious for melanoma instances in which it might However, there are also ti to your healthcare provide case.
. page |11
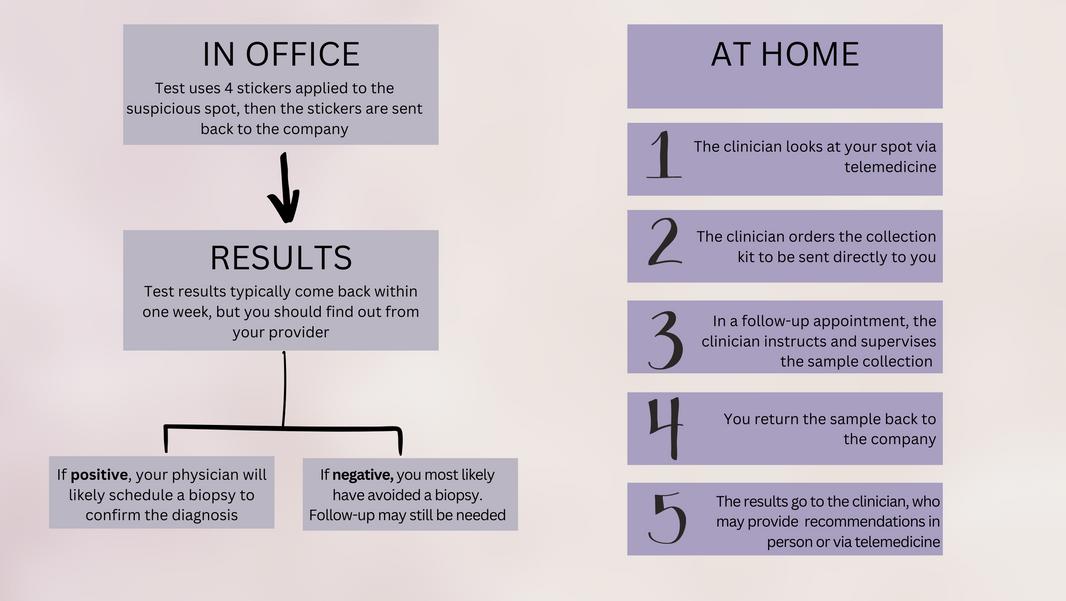
HOW IS THE NON-INVASIVE GENETIC STICKER TEST PERFORMED?
The Figure below illustrates the in-office and telemedicine strategies for using the sticker .
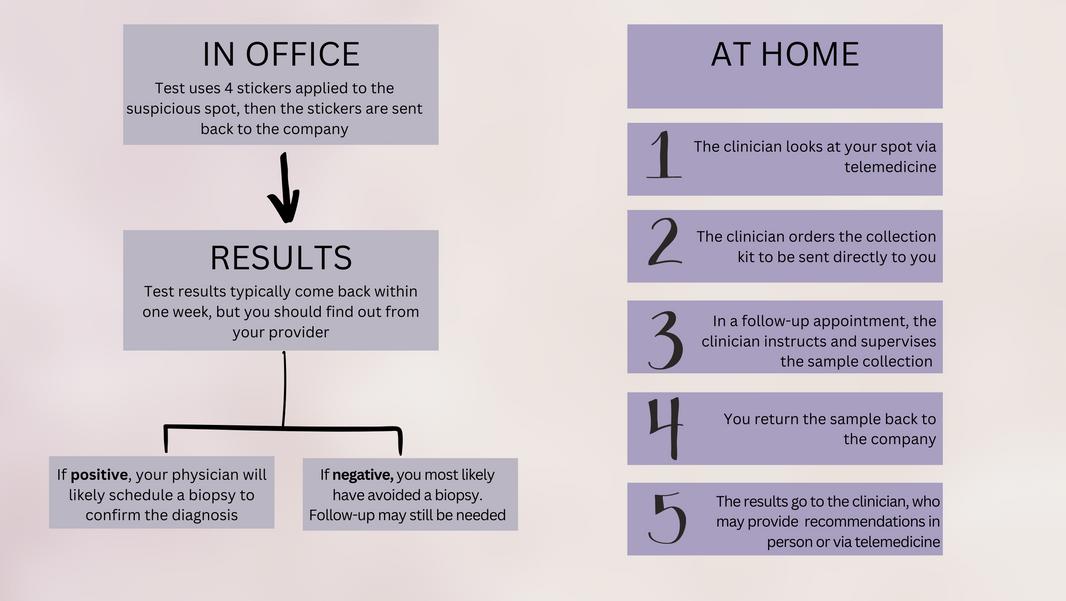
WHAT’S THE BEST APPROACH FOR USING THE TEST?
An in-person visit is preferred so the health care provider can directly look at your skin on a regular basis or to follow up on a suspicious spot. But you can also initiate an appointment to evaluate a spot you are concerned about via telemedicine. Whether in-person or online, it is critical to share any skin concerns with a clinician. Talking with your provider and getting tested is always beneficial since a negative test will help ease any worry about potential melanoma and a positive test will aid in catching the melanoma early.

page |12
HOW MUCH DOES THE NONINVASIVE GENETIC STICKER COST?


Steps have been taken to make sure the cost of the test is not a barrier More often than not, patients pay $75 or less out of pocket for the non-invasive genetic sticker If you have commercial insurance, a claim separate from your doctor’s claim will be submitted to your insurance company If your insurance company doesn’t cover the entirety, the manufacturer of the test may be able to help you address costs Additionally, there are other options that can be explored to help cover costs for those who are uninsured. Talk with your health care provider.

"I was excited to learn about the non-invasive genetic sticker and had no reservations about trying it."
– Monica, non-invasive genetic sticker patient
page |13
.
ADVOCATE FOR YOURSELF
Although you should be your own advocate when it comes to your skin, you should not feel like the responsibility to monitor it is all on you. Your healthcare provider can help guide you in this process. For some patients with increased risk of skin cancer, regular examinations with a dermatologist can be an important part of the plan.

If you are seeing a new dermatologist, find out what tools s/he has for evaluating your spots. If you have an established dermatologist, be sure to ask about non-invasive options as well. Make sure to discuss any worries you have about your skin. You have a right to know all the options available to assess your spots and determine if they are high risk for melanoma You are a partner in your care

page |14
QUESTIONS TO ASK YOUR
DOCTOR ABOUT MOLES OR SPOTS THAT ARE CONCERNING
If your health care provider says you have a spot that is concerning:

Why are you concerned about this particular mole or spot? Do you have any tools to evaluate this spot without cutting me? If so, which ones?
Am I a candidate for the non-invasive genetic sticker test? Why or why not?
If the non-invasive genetic sticker test is an available option:

Is it possible that the sticker will not sample enough material to do the test? What happens then?
How soon will your office get the results?
How do you communicate the results to me?
What can I expect next if the results are negative? If they are positive?
page |15
RESOURCES
o AIMatMelanoma.MelanomaRiskFactors. AccessedNovember3,2022.
o
AmericanAcademyofDermatology.Skincancer: everyone’satrisk.AccessedNovember3,2022.

o
BaumanCA,EmaryP,DamenT,DixonH. Melanomainsitu:acasereportfromthepatient’s perspective.JCanChiroprAssoc.2018;62(1):56-61.
o
FerrisLK,GeramiP,SkelseyMK,etal.Real-world performanceandutilityofanoninvasivegene expressionassaytoevaluatemelanomariskin pigmentedlesions.MelanomaRes. 2018;28(5):478-482.
doi:10.1097/CMR.0000000000000478
o
GeramiP,AlsobrookJPII,PalmerTJ,RobinHS. Developmentofanovelnoninvasiveadhesive patchtestfortheevaluationofpigmentedlesions oftheskin.JAmAcadDermatol.2014;71(2):P237244.doi:10.1016/j.jaad.2014.04.042
o
NationalCancerInstituteSurveillance, Epidemiology,andEndResultsProgram.Cancer StatFacts:MelanomaoftheSkin.
o
ShahA,HyngstromJ,FlorellSR,GrossmanD.Use ofthepigmentedlesionassaytorapidlyscreena patientwithnumerousclinicallyatypical pigmentedlesions.JAADCaseRep. 2019;5(12):1048-1050.
doi:10.1016/j.jdcr.2019.10.004
Thank you, Laura K Ferris, MD, PhD, Professor of Dermatology, University of Pittsburgh, and Orit Markowitz, MD, Assistant Professor of Dermatology, Icahn School of Medicine at Mount Sinai, for their review of this material

page |16
BY
BEING DILIGENT IN
THE
AND EARLY DETECTION OF MELANOMA AND OTHER SKIN CANCERS, YOU GIVE YOURSELF THE BEST CHANCE FOR GOOD HEALTH.

PREVENTION
page |17

page |18