































































































































































































































































CUSTOM: FOOT ORTHOTICS • AFO’S • RICHIES
At Hersco, our first priority is to fabricate custom orthotics accurately and precisely. We have mastered the art of accepting scans and 3D printing to deliver better orthotics for your patients and the environment. 3D printing is not only environmentally friendly, but allows us to specify modifications that were not possible before.


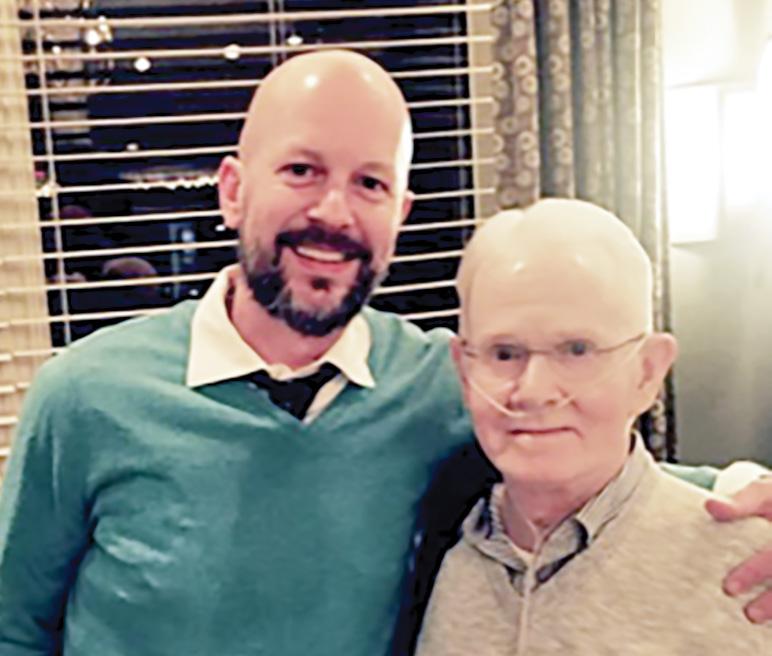
Jason Tanner, CPO, leaned on his hand skills to create a “once-in-a-lifetime” solution—a combination orthosis/ prosthesis—to replace a deteriorating device for a 74-year-old patient with osteogenesis imperfecta.

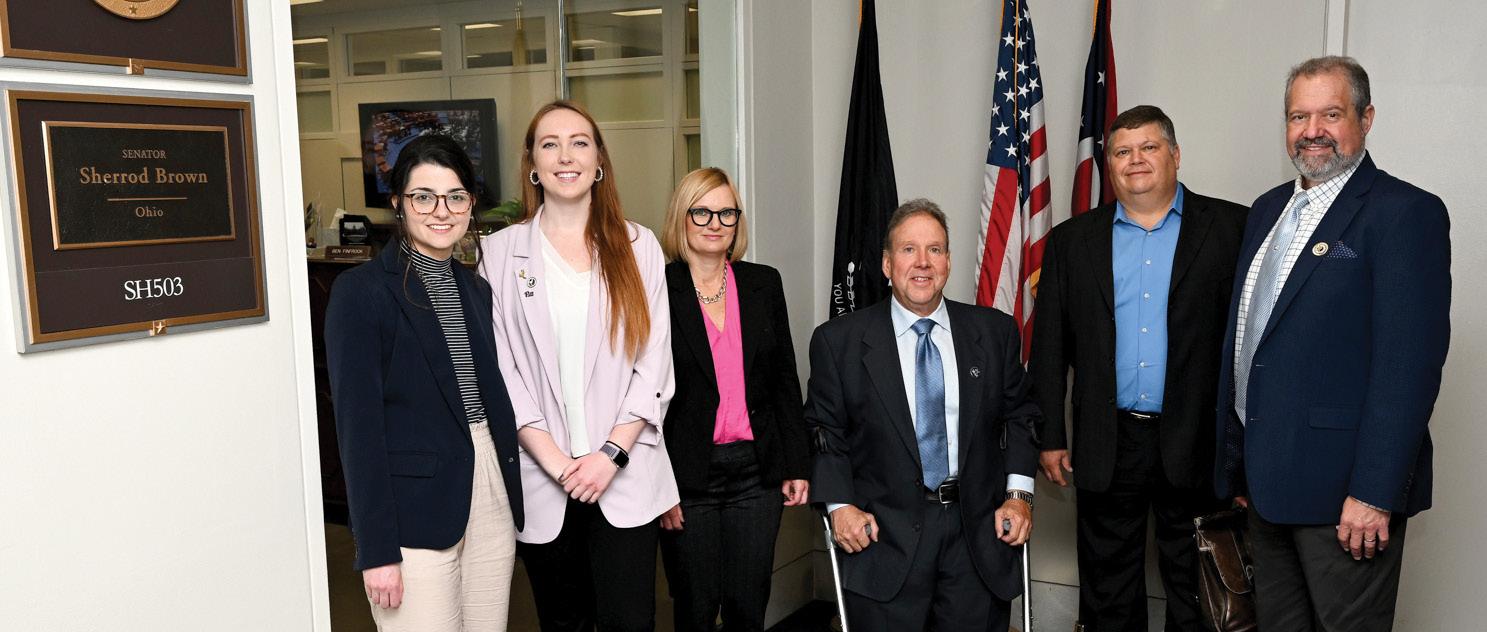
The 2023 AOPA Policy Forum convened advocacyminded O&P stakeholders from across the country to meet with legislators and promote the Medicare O&P Patient-Centered Care Act.
It’s time for O&P stakeholders to eschew outdated ways of speaking about O&P and embrace an updated lexicon that fosters acceptance of clinicians as true allied health professionals.

 By MICHAEL COLEMAN
By MICHAEL COLEMAN


Greetings to all! For the past 24 years, the world of O&P, including AOPA’s membership of incredibly hard-working, compassionate people, has brought me a sense of belonging, a sense of connectedness, and a sense of purpose. That’s usually how serving others makes us feel.
I’d like to invite you to serve—to serve your patients beyond the exam room—by volunteering on an AOPA committee. We need your expertise to continue to do the work for the O&P profession. I’d love nothing more than for you to feel the sense of belonging, connectedness, and purpose. How do you volunteer? The first step is to sign up and get involved.
AOPA’s annual Call for Volunteers opens this month. I encourage each and every one of you to look at the list of opportunities and then apply for the one(s) that you are most interested in, where you feel you can make an impact.
I will use my journey as an example of how to get involved. I am an attorney, a business owner, an educator, and a mother. I am motivated by the thought of doing good work. No one asked me to get involved; I felt compelled to do so. I realized early on that I could use my legal background to do nonprofit legislative advocacy work at the state and federal levels not only with AOPA, but also with Minnesota Society of Orthotists, Prosthetists, & Pedorthists and Wiggle Your Toes, an amputee nonprofit. Serving one organization fueled my passion to serve others. Owning and running an O&P office is commendable work, but serving those in need of O&P care beyond the exam room is where I found purpose.
How did I begin this journey? I started by attending the AOPA Policy Forums and quickly found myself on the State Reps Committee. Then I was asked to join the AOPA Board of Directors to fill the small business 1-5 facility seat. What an incredible honor! This led to service on the National Assembly Planning Committee, Government Relations Committee, VISN Network, and the O&P Alliance. I don’t think words can accurately express how rewarding serving on these committees has been for me. You have the opportunity to work with other O&P professionals from across the states to help drive the organization’s direction and help the staff execute exciting new initiatives—not to mention share your day-to-day experience so that others in the membership and profession can benefit. You get to do good work.
Being a member of AOPA is important, because together we find strength in numbers and can fight the external forces that provide barriers to our delivery of O&P care. But taking the next step to volunteer to serve on a committee and share your expertise is what truly helps advance the profession. AOPA is the organization to help address legislative and policy issues at the state and federal levels. AOPA is the organization to preserve the integrity and viability of our profession. AOPA is the organization to provide you with the tools you need to run your business so your focus can be on providing quality patient care. Serving on a committee, you do all this and more.
I would love for every one of our members to feel the belonging, connectedness, and purpose that comes with working together to serve others. There is no doubt in my mind that it is our shared vision and connectedness that helps us move our profession forward. Let’s continue to do this good work together. Please consider sharing your time and talents by answering the Call for Volunteers and serving on a committee.
I look forward to working with you!
Very truly yours,
 Teri Kuffel, JD
Teri Kuffel, JD, is president of AOPA.
Teri Kuffel, JD
Teri Kuffel, JD, is president of AOPA.
OFFICERS
President
Teri Kuffel, JD
Arise Orthotics & Prosthetics, Spring Lake Park, MN
President-Elect
Mitchell Dobson, CPO, FAAOP Hanger Clinic, Austin, TX
Vice President
Jeffrey M. Brandt, CPO Brandt Ventures, Exton, PA
Immediate Past President
Dave McGill Össur Americas, Foothill Ranch, CA
Treasurer Rick Riley Bakersfield, CA
Executive Director/Secretary
Eve Lee, MBA, CAE AOPA, Alexandria, VA
DIRECTORS
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Elizabeth Ginzel, MHA, CPO Össur, Fort Worth, TX
Kimberly Hanson, CPRH Ottobock, Austin, TX
John “Mo” Kenney, CPO, FAAOP Kenney Orthopedics, Lexington, KY
James Kingsley Hanger Clinic, Oakbrook Terrace, IL
Lesleigh Sisson, CFo, CFm Prosthetic Center of Excellence, Las Vegas, NV

Linda Wise Fillauer Companies, Chattanooga, TN
Shane Wurdeman, MSPO, PhD, CP, FAAOP(D) Research Chair Hanger Clinic, Houston Medical Center, Houston, TX
A world where orthotic and prosthetic care transforms lives.

AOPA staff and volunteers are committed to our mission of being a trusted partner, advocating for and serving the orthotic and prosthetic community by:
• Fostering relationships with decision makers to ensure equitable access.
• Providing education that promotes professional excellence.
• Supporting research that informs innovative care.
• Advancing equality to strengthen the orthotic and prosthetic profession and improve the lives of patients.
A world where orthotic and prosthetic care transforms lives.
330 John Carlyle St., Ste. 200, Alexandria, VA 22314
AOPA Main Number: 571-431-0876 | AOPA Fax: 571-431-0899 | AOPAnet.org
Eve Lee, MBA, CAE, executive director, 571-431-0807, elee@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Sam Miller, manager, state and federal advocacy, 571-431-0814, smiller@AOPAnet.org
Susannah Engdahl, PhD, manager, health policy and research, 571-431-0843, sengdahl@AOPAnet.org
Tina Carlson, CMP, senior director, education and meetings, 571-431-0808, tcarlson@AOPAnet.org
Kelly O’Neill, CEM, senior manager of meetings and exhibition, 571-431-0852, kelly.oneill@AOPAnet.org
Kristen Bean, digital meetings specialist, 571-431-0876, kbean@AOPAnet.org
Joy Burwell, director of communications and membership, 571-431-0817, jburwell@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Nicole Ver Kuilen, manager of public engagement, 571-431-0836, nverkuilen@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
Eve Lee, MBA, CAE, executive director/publisher, 571-431-0807, elee@AOPAnet.org
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
Christine Umbrell, editorial/production associate and contributing writer, 703-662-5828, cumbrell@contentcommunicators.com
PUBLISHER EVE LEE, MBA, CAE
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
O&P Almanac (ISSN: 1061-4621) is published monthly, except for combined issues in June/July and November/ December, by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
Postmaster: Send address changes to: O&P Almanac, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2023 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
Engage the profession today. Reach AOPA’s membership with more than 10,694 subscribers. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net
Learn more at bit.ly/23AlmanacMediaKit







Seeking to demonstrate the benefits of multiarticulating prosthetic hands, researchers from Queen Elizabeth University Hospital in Glasgow compared patient-reported and functional measures in unilateral prosthetic users transitioning from bodypowered or traditional myoelectric prostheses to multiarticulating hands.
The researchers conducted a retrospective cohort analysis of 20 patients for whom they had access to complete data sets of patient-reported and functional measures—both before and six months after provision of the device. The research team studied patients’ outcome measures using several tools, including the DASH test, the Southampton Hand Assessment Procedure Index of Function, the


health-related quality of life index, the Trinity Amputation and Prosthesis Experience Scales satisfaction, and the box-and-block test.
Results indicated improvements among those using the multiarticulating hand, including an 8-unit mean reduction in the DASH test; a 9.5-unit improvement in the Southampton Index; a 4-point improvement in Trinity Scales satisfaction; and the ability to transfer 3.3 more blocks in the box-and-block test. “The evidence clearly supports continued provision of multiarticulating hands to this group of moderate users,” reported the researchers. “The more function the user achieves, the less of a disability they perceive to have.” The study was published April in Prosthetics and Orthotics International
Based on the latest work injury statistics, amputation is the most expensive type of work injury, with an average cost of $118,837 per work injury.

Designed to assist prosthetists in assessing prosthetic alignment, a new computational protocol that incorporates machine learning techniques has been created by Colombian researchers.
The research team recruited 16 subjects with transfemoral amputation to validate the protocol. They performed four misalignments and one nominal alignment, and recorded 11 prosthetic limb ground-reaction force parameters. The researchers leveraged a support vector machine with a Gaussian kernel radial basis function and a Bayesian regularization neural network, which were trained to predict the alignment condition and the magnitude and angle required to align the prosthesis correctly.
In a new study, two-thirds of patients who would have required amputation due to chronic limb-threatening ischemia (CLTI)— an extreme form of peripheral artery disease—kept their limbs after undergoing a new procedure called LimFlow. Approximately 20% of CLTI patients are diagnosed with “no-option” CLTI each year, usually resulting in amputation.
Two prosthetists validated the protocol, which was found to correct poor alignment within 0.51 degrees and recover 94% of the angles needed to correct prosthetic misalignment. The research team recommended that the protocol be used as a tool to help prosthetists during alignment processes to help decrease the incidence of gait deviations and musculoskeletal diseases associated with misalignments. The study was published May in Gait & Posture
The new transcatheter arterialization procedure enables doctors to take an artery ahead of the point of blockage in CLTI patients and connect it to an unblocked vein in the lower leg using a stent graft, then reduce the flow in that vein to send blood to the foot. Among participants in the study, the outpatient procedure was performed successfully in 104 out of 105 individuals with CLTI. Participants had a mean age of 70; 30% were female; and 43% were Black, Hispanic, or Latino.
Six months postprocedure, 66% of study participants had avoided amputation. “We found that transcatheter arterialization of the deep veins was safe and could be performed successfully in patients with CLTI and no conventional surgical or endovascular revascularization treatment options,” reported the researchers. The study was published March 30 in New England Journal of Medicine
Fifty veterans with lower-limb amputation took part in a recent study on phantom limb pain conducted by a team of researchers from the Minneapolis Veterans Healthcare System and University of Minnesota.
The research team surveyed veterans via phone calls. Participants were an average of 15 years postamputation, and 80% reported experiencing phantom limb pain. According to the researchers, there was high variability in the experience of phantom limb pain; most patients displayed acceptance and resilience regarding the pain;


and most of the veterans had tried common nondrug treatments for phantom limb pain—with none endorsed as highly effective.
“Phantom limb pain can have a profound impact on daily functioning … and continues to be a major clinical challenge without clear shared clinical guidelines or best practices,” the researchers concluded. They encourage future work on engaging end users in the development and design of novel nondrug interventions. The study was published April in Journal of Pain Research
In the U.S., overall prices grew by 6% in February 2023 from the previous year, while prices for medical care increased only 2.3% —an unusual finding as health prices historically outpace prices in the rest of the economy.

CMS finalized a 3.32% pay bump to Medicare Advantage plans for 2024 and will phase in changes to risk adjustment over three years.

When searching for healthcare providers, nearly two-thirds (61%) turn to online research—and 80% of consumers who browse websites conduct two or more online searches, according to findings from Kyruus’s sixth annual survey of healthcare consumers. The survey sought to capture healthcare consumers’ preferences for searching for, selecting, and accessing care.
Patients are increasingly willing to complete healthcare-related tasks online: 40% prefer to book appointments online, with 55% of millennials and 46% of Gen Xers preferring online scheduling. In addition, more than 90% of consumers demonstrate an
interest in digital self-service options for pre-appointment check-ins and payments, according to the survey.
Today’s consumers take cost into account when making healthcare decisions, according to Kyruus: 87% consider cost when choosing providers, and 68% are more likely to schedule an appointment when they are informed of expected out-of-pocket expenses ahead of time. More than 80% of consumers also prioritize insurance acceptance, clinical expertise, provider/facility reputation, and appointment availability when choosing healthcare providers.

The Range of Motion Project (ROMP) and the Research Committee of the U.S. member society of the International Society for Prosthetics and Orthotics (USISPO) are collaborating to disseminate their research-related work in Central America. ROMP and USISPO are offering two opportunities for master’s or doctorate student projects: dissemination of the
The current version of the Advance Beneficiary Notice of Noncoverage (ABN) form was approved in 2020 and expires June 30, 2023. Last month, the Office of Management and Budget approved and released a new ABN form, CMS-R-13.

The revised form contains no substantial changes in content or in directions for use; however, the expiration date has been updated. Use of the revised ABN will be mandatory June 30, 2023. To verify you are using the most recent version of the ABN on or after June 30, check the expiration date on the bottom left corner of the form; it should be “01/31/2026.”
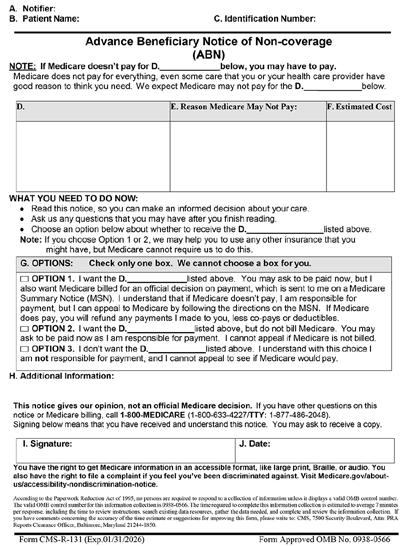
Visit cms.gov/Medicare/Medicare-General-Information/BNI/ABN to access the new ABN form with instructions.
TAPES Spanish formal translation process, and ROMP communitybased rehabilitation data analysis and dissemination.
These opportunities could enable current graduate-level O&P students to complete a professional activity, a directed study, or other possible degree requirements. For details, contact USISPOresearch@gmail.com




Rudolf (Rudy) B. Becker III, a former AOPA president, passed away April 30 at the age of 73 at his home in Bloomfield Hills, Michigan. Becker was a champion for the profession and leaves a lasting legacy.
Becker was born in Detroit to Lucille and Otto Becker. He earned a bachelor’s degree from University of Hartford in Connecticut, a master’s degree in zoology from University of Nebraska, and a juris doctorate from Tulane University School of Law. In 1977, Becker returned to Detroit to help run the family business. He served as president and chief executive officer of Becker Orthopedic Appliance Co. from 1980 to 2023. Under his guidance, the company founded Becker Metal Works in 1986.
Becker was highly involved with AOPA for decades, serving as president in 1994-1995. He represented AOPA on the O&P National Office Board, including serving as chair. He was a driving force in the creation of Capitol Connection and was a proponent of the O&P PAC. A supporter of research and higher education, he donated $10,000 to create the Otto and Lucille Becker Award, named after his parents and awarded annually to the best orthotic abstract submitted for a poster presentation by a student or resident. In 2011, Becker was honored with AOPA’s Lifetime Achievement Award.
Becker enjoyed spending time with his family, fly fishing, sports cars, fine dining, and music. He is survived by his wife of 52 years Carolyn M. Becker; his oldest son Rudy Jr.; his daughter Kristin; and his son Tom, as well as five grandchildren.
Pete Stoy, formerly the president and chief operating officer (COO) at Hanger Inc., has assumed the role of Hanger’s chief executive officer (CEO). Stoy also will serve on Hanger’s Board of Directors.

Stoy’s appointment was announced in January as part of a multiyear succession plan and follows the retirement of Vinit Asar, who held the CEO position for more than a decade. Asar will serve as executive chairman of Hanger’s board.
“I am pleased to pass the torch to Pete Stoy,” said Asar. “Having led large-scale teams across commercial, operational, supply chain, and finance functions, Pete brings a balanced skillset and perspective, and is well-positioned to lead Hanger in its achievement of long-term growth.”

Since Stoy joined Hanger as COO in November 2020, he has contributed to several growth initiatives, operational efficiencies, and business improvements.
“We have an incredible company with an important purpose that is focused on helping others, and it is truly the honor of a lifetime to lead this organization and great team,” said Stoy. “Hanger is uniquely positioned to grow and thrive in today’s complex healthcare environment, and I look forward to continuing to build on our firm foundation, further strengthening Hanger as the leading O&P company in the world.”
Stoy has more than 20 years of healthcare experience with leadership in large, complex organizations, and holds a designation as a Fellow of the American College of Healthcare Executives. Prior to joining Hanger, Stoy held positions at Sodexo, McKesson, and Cardinal Health.
ARCH Medical Solutions Corp. (ARCH) announced the acquisition of American Prosthetic Components (APC) of Green Bay, Wisconsin. APC produces high-quality modular prosthetic components that are designed and engineered to meet or surpass ISO 10328 standards and are manufactured in a range of materials. With this acquisition, ARCH Medical Solutions expands its capabilities into prosthetic components and strengthens its position in the medical device contract manufacturing market.
“We are excited to have APC join the ARCH Medical Solutions group of companies, adding an important group of products that play a critical role in enabling affected patients to enjoy increased mobility and enhanced lifestyles,” said Paul Barck, divisional president of ARCH Medical Solutions.
As part of the ARCH family, APC President and CEO Jeff Braun foresees growth and a more defined future for employees and customers. “This is the appropriate time to partner with a larger company that can offer ongoing financial stability as well as additional resources and financing to support our continued growth,” said Braun, who will remain the company’s president.
The Board of Certification/Accreditation (BOC) has been awarded a Bronze Stevie® Award for Sales & Customer Service in the new “Best Customer Engagement Initiative” category. This new category recognizes organizations distinguishing themselves through customer engagement initiatives creating a positive customer experience and increasing customer loyalty.
“We’re proud to be recognized for the customer service that is such a strong part of our BOC culture and valued by our customers,” said BOC’s president and CEO, Judi Knott, MA, MBA, CAE. “As a repeat Stevie Award winner for the past decade, we’re proud to be an authentic leader in customer service.”
The Pedorthic Footcare Association has launched a redesigned website, pedorthics.org. The site features improved navigation, enhanced content for the public and referral sources, and a “Find the Credentialed Pedorthist” search engine.


COVID-19 remains a health threat in the United States, with more than 14,000 new cases reported during the week of April 12, 2023, according to the Centers for Disease Control and Prevention. However, the worst of the pandemic appears to be behind us. Whether due to increased vaccination rates, herd immunity, treatment advances, a combination of these, or other factors, society appears to have found a way to exist in a world with COVID-19. The federal government announced that it will end the COVID-19 public health emergency (PHE) effective May 11, 2023.

COVID-19 was officially declared a PHE Jan. 27, 2020, and the PHE was renewed every 90 days as required by law until the Department of Health and Human Services made the decision to officially end the order May 11, 2023. The declaration of any PHE creates flexibilities that allow federally funded and operated health systems, such as Medicare and Medicaid, to alter or waive policy requirements in the interest of ensuring maximum access to healthcare services.
The COVID-19 PHE impacted many Medicare and Medicaid beneficiaries—and the delivery of O&P care to those patients. This month’s Reimbursement Page examines how the PHE impacted O&P care, and how the end of the PHE will affect your patients and your O&P practice.
The federal government announced that it will end the COVID-19 public health emergency (PHE) effective May 11, 2023.


One of the most significant flexibilities of the COVID-19 PHE was the relaxation of eligibility requirements to qualify for Medicaid coverage, along with regulations that prevented states from disqualifying and disenrolling Medicaid beneficiaries.
According to the Kaiser Family Foundation, Medicaid enrollment grew to 92.3 million individuals during the COVID-19 PHE, an increase of 29.8% from pre-COVID enrollment levels.
As a result of provisions of the Consolidated Appropriations Act, 2023, that reinstated states’ ability to requalify Medicaid beneficiaries on a regular basis and the subsequent end of the PHE, many patients that may have qualified for Medicaid coverage during the PHE may no longer qualify under the newly reinstated enrollment criteria. Many states have passed laws to prevent a hard cutoff of Medicaid benefits, but these laws are not permanent fixes, and many Medicaid beneficiaries will eventually lose their Medicaid benefits.
O&P companies may want to invest resources to ensure that there have not been changes to their patients’ insurance coverage, including Medicaid coverage, as a result of the PHE’s end.

In March 2020, the durable medical equipment Medicare administrative contractors (DME MACs) issued a joint article indicating that, based on guidance from CMS, certain policy requirements would be waived for the duration of the COVID-19 PHE. These

included the suspension of certain faceto-face visit requirements, the waiver of clinical indications of coverage for certain Local Coverage Determinations (LCDs) and National Coverage Determinations (NCDs), and the relaxation of requirements in some LCDs and NCDs that certain Medicare services be provided by specific physician specialties. The instructions that accompanied the joint DME MAC publication indicated that any claims where one of the COVID19 PHE-based waivers applied should be submitted with a CR modifier.
The CR modifier is used to indicate that a claim was impacted by a specific disaster or catastrophe; it has been used in the past to allow flexibilities in areas impacted by natural disasters such as hurricanes or tornados. COVID-19 impacted the entire globe and the PHE declaration impacted the Medicare population, so the CR modifier was the logical choice to identify Medicare claims impacted by COVID-19.
O&P LCDs were not included in the waivers of policy requirements; however, the suspension of face-to-face visit requirements with prescribing physicians during the COVID-19 PHE allowed for the expansion of telehealth services as a viable means of establishing medical necessity of O&P services. O&P claims that normally required
in-person interaction with a physician were considered for coverage as long as they were submitted with a CR modifier.
After May 11, 2023, the CR modifier should no longer be applied to claims impacted by COVID-19.
Telemedicine was an area of major growth during the COVID-19 PHE. Although telehealth was not a new concept, providers were required to adhere to very specific, often restrictive requirements that could make the delivery of healthcare services via telemedicine challenging prior to 2020. Dedicated telehealth sites, secure two-way communication, and burdensome documentation requirements often outweighed any potential advantages that the use of telemedicine provided.
Under the COVID-19 PHE, the requirements for telemedicine were relaxed to allow for increased access to medical professionals without potential exposure to infection through face-to-face interaction. Advances in technology through services such as Zoom and Microsoft Teams proved that telemedicine was an effective method for providing healthcare services.
As the COVID-19 PHE began to wind down, the future of telemedicine entered
the forefront of discussion. Almost everyone agreed that telemedicine had proven to be an effective means of delivering healthcare during the pandemic, and there was no interest in returning to the restrictive pre-COVID telemedicine requirements. Congress addressed this issue temporarily by extending the telehealth rules that were in place during the PHE through the end of 2024—but additional legislation will be required to make any changes permanent. It appears that telemedicine is here to stay, even if the path forward is not fully clear.
The COVID-19 PHE remained in effect continuously from its initial declaration in January 2020 until its end May 11, 2023, but healthcare practices have gradually returned to normal. The official end of the PHE should represent a transition—more than a sudden change—but it is important to understand what the end of the PHE actually means for your business. While the impact to your business may be limited, not understanding what will change could be costly.
Joe McTernan is director of health policy and advocacy at AOPA. Reach him at jmcternan@AOPAnet.org





O&P stakeholders traveled to Capitol Hill to advocate for patients and the profession
More than 100 O&P advocates from 32 states convened May 10-11 at the 2023


Policy Forum in Washington, DC, with a purpose: educate lawmakers about the newly revamped Medicare O&P Patient-Centered Care Act. O&P business owners, managers, clinicians, educators, and students joined forces to discuss advocacy basics, strategize for one-on-one congressional visits, and meet up with legislators and their staff

The first day of the Policy Forum featured sessions highlighting successes from the So Kids Can Move initiative, “Lobbying 101,” and a detailed explanation of the current Medicare O&P Patient-Centered Care Act. On the second day, participants ventured to the Capitol to visit their individual senators and representatives or staff members to share their stories and deliver their “ask”: that the legislators sign on to cosponsor the bill. The bill would ensure patient protection from fraud and abuse by prohibiting “drop shipping” of custom-fabricated orthoses and all prostheses; include certified/licensed orthotists and prosthetists in the exemption from competitive bidding contracts that currently exists for physicians and therapists; and eliminate the default five-year reasonable useful lifetime restriction on replacement of orthoses. These provisions are designed to ensure beneficiary access to patient-centered clinical O&P care.


This year’s Policy Forum resulted in an impressive 138 legislative meetings: 79 with representatives or their offices and 59 with senators or their offices. Participants appreciated the opportunity to make connections with lawmakers, explain the value of O&P clinicians as care providers, and increase awareness of the Medicare O&P Patient-Centered Care Act. Look for details about the legislation in the June/July issue of O&P Almanac




Every day, O&P providers see evidence of the important connection between patient mobility and their mental health and well-being. Consider this example from Erin O’Brien, CPO, FAAOP, clinician and clinical education specialist at Hanger Clinic: A patient who was very active as an EMT contracted MRSA from a cut on his foot; he thought his career and hobbies would be over after becoming a below-knee amputee. “The patient was hesitant to go back to work because he was worried about being able to care for his own patients with his new mobility challenges,” O’Brien recalls.
Fast forward to a new prosthesis and clinical care and support from the Hanger Clinic team, who talked through his goals and assured him that going back to his job and hobbies was absolutely in the realm of possibilities. “We tracked his mobility and well-being over the next several months, and we saw a clear relationship: As his prosthetic mobility improved, his well-being increased,” says O’Brien. “He enrolled in EMT school to get recertified and reengaged in his favorite hobbies, which made him a more confident, outgoing version of himself.”
Stories like O’Brien’s, demonstrating the link between mobility and well-being, are common at O&P facilities across the country. As more researchers and clinicians track and study patient outcomes after receiving a prosthesis, evidence of
what O&P professionals already know is growing: Returning patients to mobility and function can improve both their physical and mental health.
A brand new advisory from the U.S. surgeon general’s published this month draws national attention to the link between “social connection” and health. The advisory defines social connection as “a continuum of the size and diversity of one’s social network and roles, the functions these relationships serve, and their positive or negative qualities.” Understanding how social connection impacts well-being is important for the O&P community to understand because returning patients to mobility can improve patients’ ability and willingness to continue and expand their social connections.
According to the advisory, the loneliness that comes from isolation and disconnection harms both individual and societal health and is associated with a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. “The mortality impact of being socially disconnected is similar to that caused by smoking up to 15 cigarettes per day,” according to Surgeon General Vivek Murthy, MD, author of the advisory. Loneliness and social isolation increase the risk for premature death by 26% and 29%, respectively.
f O&P clinicians have long understood that, as prosthetic mobility improves, so, too, do patient well-being and mental health. New research helps explain those connections.
f An advisory from the U.S. surgeon general draws attention to the link between “social connection” and health, underscoring the need to return patients to mobility to help prevent isolation and loneliness.
f A recent study of veterans with traumatic amputation found that higher physical functioning scores were associated with better quality of life, and lower scores were associated with screening positive for PTSD or depression.
f Another study shows that prosthetic use may be associated with well-being among individuals with amputation secondary to dysvascular disease and diabetes.
f Other studies demonstrate that more advanced devices, such as those with microprocessor technology, may improve mobility and boost well-being.
Social connection can be negatively impacted by several individual factors, including chronic disease, mental health, and physical health. And while new technologies have increased the prevalence of virtual communications and online interactions, they also may reduce the quality of physical interactions, according to the advisory. “Evidence across scientific disciplines converges on the conclusion that socially connected people live longer,” notes Murthy.
The advisory urges Americans to “make the same investments in addressing social connection that we have made in addressing tobacco use, obesity, and the addiction crisis.” The publication also calls on the U.S. health sector to train healthcare providers on the physical and mental health benefits of social connection, and to recognize the risks associated with social disconnection.
In an O&P-specific quality-of-life study published last year, researchers analyzed the link between mental health and mobility among veterans. A research team from Leidos and the Naval Health Research Center, led by Susan Eskridge, PhD, studied patient-reported outcomes of physical functional status, posttraumatic stress disorder (PTSD), depression, and quality of life among service members after combat-related lower-extremity amputation.
Eskridge’s team found that higher physical functioning scores were associated with better quality of life, and lower physical functioning scores were associated with screening positive for PTSD or depression. “A significant relationship was observed between mean physical functioning scores and amputation level with a negative PTSD or depression screen only,” reported the authors in their published journal article. “Those with bilateral amputation reported lower physical functioning.”
Poor mental health was found to be associated with poor physical function and mobility. Eskridge’s team noted that screening positive for PTSD or depression was associated with worsened self-reported physical function, “and may outweigh the impact of amputation severity on physical functioning.” They concluded that both physical and mental health must be considered for successful rehabilitation postamputation.
“Good mental health is crucial to optimal functioning, as presence of adverse mental-health symptoms may exacerbate physical functional limitations among those with combat-related amputations,” the researchers noted. “Assessing variables related to adverse mentalhealth symptoms and ultimate physical functioning outcomes is critical for clinicians to optimize rehabilitative strategies and outcomes.”

The surgeon general’s advisory discusses the importance of social connection in both preventing and managing diabetes: “Social disconnection (poor structural social support and living alone in men, low emotional support in women, and not having a current partner in women older than 70) has been linked to an increased
risk for the development of type 2 diabetes.” Among those who already have diabetes, “social connection has been associated with better self-rated health and disease management,” according to the report. “Diabetic outcomes may be better among people who are more socially connected due to better diabetic management behaviors and patient self-care such as medication adherence, physical activity, diet, and foot care.”
The surgeon general’s analyses align with findings from Hanger Clinic’s MAAT 6 study on “Mobility, Satisfaction, and Quality of Life Among Long-Term Dysvascular/Diabetic Prosthesis Users.” In a cross-sectional analysis, Hanger’s clinical research team, led by Shane Wurdeman, PhD, CP, FAAOP(D), Phillip Stevens, MEd, CPO, FAAOP, and James Campbell, PhD, CO, FAAOP, studied outcomes of individuals with amputation secondary to dysvascular disease and diabetes and discovered that prosthetic use—which can keep individuals socially connected—was associated with well-being. Individuals from this population who continue to participate in prosthetic rehabilitation appear to experience levels of mobility, satisfaction, and quality of life seven years after amputation, comparable to that reported in the first six months postamputation.

“This is an interesting population,” explains Stevens, director, clinical and scientific affairs. “When you look at the vascular literature on individuals that require amputation, it can be pretty discouraging. Mortality rates are high, revision amputation rates are high, and return to ambulation rates are low. We also know that quality-of-life values tend to be lower among those with vascular disease.
“And yet we see a subset of this population succeed regularly in our clinics,” Stevens says. “MAAT 6 demonstrated that not all those who undergo dysvascular amputation are destined for a gradual decline in mobility and well-being. Rather, we found that those from this population who have enough health and motivation to continue to use a prosthesis are quite stable with respect to mobility, quality of life, and well-being—some of them as much as five to seven years postamputation.”
Other diabetes-focused research demonstrates the importance of examining gender disparities to ensure women’s mental health needs are being addressed. In a new study published in April in Disability and Rehabilitation, researchers explored the differences in prosthesis prescription among veterans who had undergone amputation due to diabetes or peripheral artery disease. Researchers at the VA Puget Sound Healthcare System conducted a retrospective cohort study to determine gender disparities and potential factors that modify prosthesis prescription practices. Led by David C. Norvell, PhD, the research team studied the records of more than 2,800 veterans who had undergone a first major unilateral amputation due to diabetes or peripheral artery disease.


The first study in Hanger’s MAAT research series, published in Prosthetics and Orthotics International in 2017, was groundbreaking in establishing a link between mobility and quality of life and satisfaction among individuals who use lower-limb prostheses. Researchers from Hanger’s Department of Clinical and Scientific Affairs conducted a retrospective chart review of the Prosthetic Limb Users Survey of Mobility and the Prosthesis Evaluation Questionnaire—Well-Being subsection. The analysis of more than 500 patient records demonstrated that mobility was positively correlated with qualify of life and general satisfaction.
“In today’s healthcare system, we are always looking for what I would characterize as ‘common currencies,’ or constructs that everyone involved in an individual’s care would value; things
The researchers found that men more commonly received a prosthesis prescription, and received it earlier than women: 59% of men and 45% of women received prosthesis prescriptions. The disparity was most extreme among women who had been diagnosed with a major depressive order—this population was least likely to receive a prosthesis prescription, and thus least likely to return to mobility. Among the subgroup of veterans with a diagnosis of major depressive disorder, the odds of men receiving a prosthesis over women was more than three times. “Both disparities will have a significant, negative impact on women’s functional and quality-of-life outcomes,” according to the researchers.
The researchers recommended that women who undergo transfemoral amputation, and are deemed prosthesis candidates, should be considered for earlier prosthesis prescription and rehabilitation. They also recommended that providers identify patients at greater risk of depression early, and consider targeted interventions to address depression during the preoperative and immediate postoperative phases. “The identification of gender-specific needs that might contribute both to depression and to other healthcare disparities for women with amputation is an important area for future investigation,” they noted.
Ensuring patients receive the most appropriate O&P devices can also impact patients’ quality of life and increase their likelihood to make social connections. This may be particularly true for lowerlimb prosthesis users who are fit with microprocessor technology that facilitates increased mobility.
For example, in Hanger’s MAAT 7 study, published in the American Journal of Physical Medicine & Rehabilitation last year, and the CASTLE 1 study (Creating Adjusted Scores Targeting Mobility Empowerment), which has been accepted in Disability and
that are valued by the patient, the referral source, the treating clinician and the pay source,” explains Phillip M. Stevens, MEd, CPO, FAAOP, director, clinical and scientific affairs, and one of the study authors. “We see the idea of ‘well-being,’ or an aggregated assessment of quality of life and general satisfaction, as one of these common currencies. So, the question then becomes, ‘Can we influence it, and if so, how?’ Once we understand the relationship between well-being and mobility, we recognize the opportunity to enhance the one by improving the other,” he says.
“That finding was foundational to all of our subsequent research in this area, because it clarified that when we do something that improves mobility, we’re also impacting this overarching construct of well-being.”
Rehabilitation and is pending publication, the Hanger clinical and scientific affairs team found a connection between age and mobility with respect to amputation level and etiology. Additionally, in CASTLE 1’s “Determination of Normative Mobility Scores After Lower Limb Amputation for Each Year of Adulthood,” the team found a relationship between microprocessor knee use among patients and increased long-term mobility, particularly among older patients.
“We mapped the average prosthetic mobility of transfemoral prosthesis users by age, and as you might expect, we see this gradual decline in mobility with aging,” says Stevens. “We see this with traumatic amputation, but it’s even more striking with dysvascular amputation.
“However, when we break those populations down by prosthetic knee type, we see two very divergent lines. Those with nonmicroprocessor knees decline with aging as we would expect, but access to a microprocessor knee bends that curve in a very striking, meaningful way,” says Stevens. “It begins when the patients studied are in their early 50s, but the divergence becomes more and more striking through their 60s and early 70s. Those with microprocessor knees stay within a standard deviation of average mobility values, while those with nonmicroprocessor knees do not.”
The team found similar correlations when considering prosthetic foot selection. “When we control for things like amputation etiology and K level, and adjust for things like comorbid health, body mass index, and amputation level,” Stevens explains, “we see clear improvements in prosthetic mobility with the use of modern prosthetic componentry like microprocessors, shock and torque absorbers, and hydraulic ankles.”
“Recognizing that prosthetic mobility is modifiable for many patients, we start to recognize that so is well-being,” he says. “We can impact quality of life in a meaningful way when we enhance prosthetic mobility.”
Evidence that return to function correlates with well-being also exists for the upper-limb loss population, according to another recent article published by Hanger’s clinical and scientific research team. “We looked at a number of variables that we felt might correlate to quality of life for this population,” Stevens explains. “Factors like bimanual function and prosthesis satisfaction values correlate quite strongly with well-being. Factors like time since amputation, or daily wearing schedules, do not
“Our data suggests that patients who are pleased with the prosthesis and are able to perform bimanual activities when they need to tend to report higher levels of well-being,” Stevens says. “That capability with a prosthesis appears to be much more important than how often they wear it, or how long they’ve lived with an amputation. It really speaks of the importance of designing a prosthesis that enables a patient to perform the activities that are most important in their daily activities.”
Going forward, clinicians will need to stay educated on new research studies related to mobility for patient well-being. The good news is that most practitioners already understand this concept— and a recent survey demonstrates that O&P professionals want to do more to help patients improve their mental health.
Researchers at Adapttech conducted a questionnaire among healthcare professionals, including CPOs, physicians, occupational therapists, O&P residents, and rehabilitation clinic owners. They asked participants about patient mobility outcomes, daily professional practice, and their views on patients’ mental health. Results were shared via poster presentation during the AOPA National Assembly in September.
“The study found that prosthetists understand mental health as an important factor in prosthetic rehabilitation. They recognize that patients who struggle with mental health issues may have a more challenging time adjusting to their prosthetic device and may require more support during the rehabilitation process,” says Bruna Rolo, a former Adapttech employee and author of the poster presentation. “Prosthetists also acknowledge that mental health issues can impact a patient’s motivation and willingness to engage in the rehabilitation process, which can ultimately affect the patient’s outcomes.”
Prosthetists believe that addressing mental health concerns should be an integral part of rehabilitation, according to the survey results. “They emphasized the need for a holistic approach that considers the patient’s mental and emotional well-being as well as their physical needs,” says Rolo. Prosthetists suggested that mental health counseling, support groups, and other interventions aimed at improving mental well-being should be incorporated into the rehabilitation process.
Some O&P facilities already embrace strategies to monitor mobility indicators among patients for several reasons, according to Rolo: Monitoring mobility offers prosthetists access to valuable information about patients’ physical and functional capabilities and allows them to track patients’ progress. Prosthetists also can monitor
patients’ mobility to identify potential issues or complications early on, and evaluate the effectiveness of the rehabilitation plan.
However, “traditional methods of monitoring mobility indicators, such as observation and self-report, have limitations and may not provide a complete picture of the patient’s mobility,” says Rolo. She suggests the O&P profession finds or creates more tools to monitor mobility indicators accurately and objectively. “For example, wearable sensors and other technological devices can provide more detailed and accurate data on the patient’s mobility, allowing prosthetists to make more informed decisions about the patient’s rehabilitation plan and prosthetic device.”
“Prosthetic rehabilitation is not just about physical rehabilitation but also about mental rehabilitation,” adds Rolo. “It’s crucial to consider the patient’s mental health when planning and analyzing the recovery process. By addressing any mental health issues that may arise during the rehabilitation process, patients can achieve their maximum potential and lead fulfilling lives.”
Christine Umbrell is a contributing writer to O&P Almanac
Reach her at cumbrell@contentcommunicators.com
The following research is referenced in this article:
• England DL, Miller TA, Stevens PM, Campbell JH, Wurdeman SR. Mobility Analysis of AmpuTees (MAAT 7): Normative Mobility Values for Lower Limb Prosthesis Users of Varying Age, Etiology, and Amputation Level. Am J Phys Med Rehabil. 2022;101(9):850-858. doi:10.1097/ PHM.0000000000001925
• Eskridge SL, Watrous JR, McCabe CT, Clouser MC, Galarneau MR. The relationship between self-reported physical functioning, mental health, and quality of life in Service members after combat-related lower extremity amputation. Disabil Rehabil. 2022;44(13):3189-3195. doi:10.1080/09638288.2020.1863481
• Norvell DC, Turner AP, Morgenroth DC, et al. The effect of depression on prosthesis prescription in men and women who have undergone a lower limb amputation [published online ahead of print, 2023 Apr 10]. Disabil Rehabil. 2023;1-8. doi:10.1080/09638288.2023.2192976
• Rolo Dos Santos B, Carvalho V. Patient outcomes and mental health—poster presentation. Publications—Adapttech.
September 28, 2022. Accessed May 1, 2023. https://static1. squarespace.com/static/63daa1a4657ea066fb886b6f/t/63fde76c2aea1f6e975082a0/1677584236446/Patient_Outcomes_and_Mental_ Health.pdf.
• Wurdeman SR, Stevens PM, Campbell JH. Mobility Analysis of AmpuTees (MAAT I): Quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet Orthot Int. 2018;42(5):498-503. doi:10.1177/0309364617736089
• Wurdeman SR, Stevens PM, Campbell JH. Mobility Analysis of AmpuTees (MAAT 6): Mobility, Satisfaction, and Quality of Life among Long-Term Dysvascular/Diabetic Prosthesis Users—Results of a Cross-Sectional Analysis. J Prosthet Orthot. 2021;33(3):161-167. doi:10.1097/JPO.0000000000000304
f The O&P profession has evolved through advances in education and clinical training, but there has been a delay in gaining recognition and acceptance as allied health professionals.
f Some of the outdated language associated with O&P does not reflect the high levels of education and expertise that prosthetists and orthotists are now attaining.
f At times, clinicians use language that is device-centric as opposed to patient-centric, which may diminish the perception of the importance of O&P care.
f The disconnect between payors’ perceptions of O&P and the high-level, sophisticated care that O&P professionals provide may negatively impact reimbursement rates.
f Effecting change in O&P will require using appropriate clinical terminology with patients, payors, and referral sources.
The O&P profession is constantly evolving and improving, but some of the key words and phrases used to describe it aren’t keeping up—prompting a push to update O&P’s vocabulary in a way that will boost respect and compensation for certified professionals.

Some O&P experts and associated healthcare professionals say outdated ways of speaking about O&P often don’t reflect the high levels of education and expertise that prosthetists and orthotists are now attaining. This inconsistency leads to the undervaluing of their work by some payors, referral sources, and the public.
Alan Davis, MD, an orthopedic surgeon at the Cleveland Clinic, specializes in foot and ankle procedures and works closely with O&P clinicians to help his patients obtain the best outcomes. Davis says that, historically, these professionals have not been given credit for providing clinical care to patients. “That’s really what they do, so the perception is wrong,” Davis says. “Their value to patient care is misperceived, and it needs to be reframed, and the value of this clinical care needs to be changed. Providing clinical care to other human beings is a big responsibility and should be looked at as such.”
The O&P profession has evolved to become a highly educated healthcare specialty—and it’s time for the lexicon to catch up
O&P has “a bit of an identity crisis,” says Joe McTernan, director of health policy and advocacy at AOPA, which stems from its proud history of craftsmanship compared to the modern reality of O&P: Individuals now entering the field are generally much more highly educated, due to the O&P master’s degree requirement, than practitioners were just 20 years ago.
“Over time, we’ve evolved through advances in education and advances in clinical training, and we’ve really become part of the broad allied health community,” McTernan says. “But there’s been a delay in getting that acceptance as true allied health professionals, whether it’s from the insurance companies or referral sources. I also think it’s also created a bit of a bad taste in people’s mouth because they feel that they’re not respected.”
Shane Wurdeman, PhD, CP, FAAOP(D), is director of clinical research at Hanger and a former O&P technician who has co-authored more than 40 peer-reviewed manuscripts and 100 conference abstracts on O&P rehabilitation, giving him deep familiarity with the industry’s lexicon. Wurdeman says changing perceptions of O&P starts with “changing the language.” A lack of precision in the way O&P providers describe their work diminishes the perception of its importance, leaving some insurers, and even the public, with the impression that they are simply “device dispensers,” as opposed to highly skilled healthcare providers.
“We repeatedly use language that is very device-centric as opposed to patient-centric,” Wurdeman says, “and because our language is so old, I don’t even know if we’re aware of how device-centric a lot of things we say really are.”
At the 2023 AOPA Policy Forum, Peter Thomas, JD, managing partner at Powers Pyles Sutter & Verville, who has nearly 30 years of experience providing counsel and advocacy services to the O&P profession, explained that O&P is referred to as a supplier in payor circles. “Under the Medicare statute, the word ‘provider’ actually defines hospitals. It defines institutions,” he explained. The word “supplier” means “a physician or other practitioner, a facility, or other entity other than a provider of services that furnishes items of service under this title. Physicians, PTs and OTs, prosthetists and orthotists, [and] durable medical equipment suppliers are all suppliers under the Medicare program.
“The answer to me is to continue to define our services as professional services, as clinical services, the way PTs, OTs, and physicians do.”
Clinicians should be more thoughtful in the words they choose, Wurdeman suggests. For example, rather than saying they provided a patient with a C-leg or other device, clinicians could say they provided them with orthotic or prosthetic care, or helped rehabilitate them through use of a prosthesis.
“Otherwise, all you’ve done is basically reaffirm that you’ve only dispensed a device,” Wurdeman says. “Do we want the emphasis on the patient or on the technology? Our devices and technology are the instruments for what we do, not what we do. If we keep going
down this road, we’re not going to be recognized as healthcare providers; we’re going to become [viewed as] a commodity.”
Some language used to describe devices themselves also is antiquated, Wurdeman says, and at odds with the goal of securing approvals and appropriate payments from insurers and payors. O&P practitioners frequently describe a device provided to patients as representing the “latest and greatest” technology, including devices containing microprocessor technology. But Ottobock’s game-changing and now widely used C-leg microprocessor-controlled knee (MPK) was first introduced into O&P in 1999—nearly a quarter-century ago. “You never see someone talk about a vehicle from 1999 and describe it as ‘advanced,’” Wurdeman says.
Such characterizations of long-existing technology can clog pathways to truly groundbreaking innovation and stifle payor acceptance of newer, and potentially more effective, modern technologies. “We’ve fallen into the trap of thinking the way we get these [devices] to be more available is by creating this awareness that this is the latest and greatest, which conflicts, however, with those in the payor community that aren’t willing to give the option,” Wurdeman says. Healthcare payors will often resist shelling out money for “cutting-edge” technology because it doesn’t have a demonstrable history of long-term efficacy and effectiveness.
Wurdeman and other O&P professionals say that simple words that are part of O&P foundational vocabulary are falling out of favor in the 21st century.
For example, some O&P professionals discourage use of the word “stump” in reference to the remaining legs or arms of “amputees”— another word that some believe has outlived its usefulness (and should be replaced by the term “individuals with limb loss,” which is person-first language). Instead, they suggest the term “residual limb.” If patients want to refer to their own residual limb as a “stump,” that’s their preference and there is no compelling reason to discourage them from doing so. But many O&P experts now advise against the word’s use in clinical settings despite its longstanding acceptance in the profession. “We have to get away from the word ‘stump’ because the connotation there is it’s not functional; it doesn’t do anything—and a limb is very functional,” Wurdeman says. “It can do a lot; it just needs to be equipped with the right tool.”
“Our devices and technology are the instruments for what we do, not what we do. If we keep going down this road, we’re not going to be recognized as healthcare providers.”
—Shane Wurdeman, PhD, CP, FAAOP(D)
Similarly, the words “brace” and “splint” commonly used to describe orthoses—and used interchangeably within other areas of healthcare—somehow imply less dynamism than an “orthosis.” “A brace is something that is not moving and is stabilizing, whereas an orthosis is allowing and promoting healthy movement,” Wurdeman says.
Effecting change in O&P starts with the basics, says McTernan, and that means using appropriate clinical terminology with patients, payors, and referral sources. McTernan often sees O&P professionals who should know better referring to an “orthosis,” which is a noun, as an “orthotic,” which is an adjective. The same is true for a “prosthesis” (noun) and “prosthetic” (adjective).
“I hear it all the time,” McTernan says. “You can have a prosthetic leg. You can have a prosthetic device. You could have a prosthetic arm. But it’s a prosthesis when you’re referring to it as a noun,” he explains. “If we can encourage our own folks—our clinicians, our administrators who are working in the profession—to use the right terminology, I think it will be beneficial.”
A nuanced, careful lexicon also is important when it comes to billing. The disconnect between the payors’ perceptions of O&P and the high-level, sophisticated care that O&P professionals provide serves to depress reimbursement rates. “The payors have gotten away with not compensating this profession for what their value is to patient care,” Davis says. “Historically, the payors have gotten away with under-paying, underestimating, and under-respecting this profession. And if you’re a payor, why would you want to change that? They’re running a business, too. So, the bottom line is that they’re going to try to stick to their historical mindset because that is what allows them to pay less money.”
But the reality is that O&P providers can help patients avoid surgical procedures, and help them heal and avoid pain, which is an exceptional service not only to the healthcare industry, but to humanity. And it should be rewarded as such. “They really should be considered part of the team of healthcare providers, rather than mere technicians,” Davis says.
McTernan says administrators, billers, and even clinicians should avoid talking about their patient care in terms of providing comfort or convenience. “If you’re providing something, it has to have a critical value in order for it to be reimbursed,” he says. “And it’s not about comfort. It’s not about convenience. It’s not about feeling better. It’s about: How is it helping to restore function? It’s all about showing why something is medically necessary. You’ll want to talk about how you’re going to restore function or perhaps even reduce cost down the road.”
With respect to billing, it’s also important to maintain records that contain wording consistent with the verbiage in the records of prescribing physicians for each patient. McTernan says it raises red
flags when—to use a rather extreme example—a physician’s records describe a patient as elderly, frail, and wheelchair-bound, and the prosthetist’s records characterize the patient as living an active lifestyle that requires an advanced, expensive prosthesis.
“The insurance company will … ask questions about those inconsistencies, so you want to identify those and address them beforehand,” McTernan explains. “Once you have inconsistency, the insurance company is going to look to the physician’s record, not the [O&P] provider’s. You want to make sure there is corroboration and consistency between the prescribing physician and the orthotist or prosthetist.”
David McGill, vice president of legal affairs and reimbursement at Össur and immediate past-president of AOPA, has extensive experience dealing with coding, regulatory, and reimbursement issues affecting the O&P industry, and he says O&P professionals have been trying to finetune the industry’s lexicon for decades. Some even wrestle with whether to refer to O&P as an industry or a profession. (It’s both, of course.)
“It’s very common, especially if you work at a larger company that isn’t directly involved in patient care, to sort of orient yourself around the language of corporate America, or just the corporate world. And corporations talk about industries, and they talk about end users of products,” McGill says. “Patient-care organizations tend to talk about the profession that they’re a part of, and the patients that they serve. It’s not necessarily an intentional effort to somehow undercut the work that’s being done; it just reflects the unique perspectives that different players in this space bring to the table.”
A widespread lack of understanding about holistic O&P, even among some in the healthcare industry, is a barrier to broader respect and better billing returns. “The entire reimbursement system is built around only being able to bill for the delivery of a device, and there is little understanding that payments for the device include all the necessary follow-up care and treatment for some period until the patient’s condition clinically changes down the road,” McGill says. “The system that we operate in, in some ways reinforces the kinds of conclusions that we don’t want reinforced, but there’s not a lot you can do about that easily.”
Perhaps the most efficient path to change is insisting that O&P professionals respect themselves and their work and speak about it in terms that ascribe value appropriate for the profound difference they make in their patients’ lives, McTernan says.
“Our biggest responsibility as professionals is making sure that we are our own proponents,” he says, “and making sure that folks are aware that this profession exists and are aware of all of the training, education, and clinical expertise that goes into making sure patients have the best outcomes.”
“Our biggest responsibility as professionals is making sure that we are our own proponents.”
—Joe McTernan















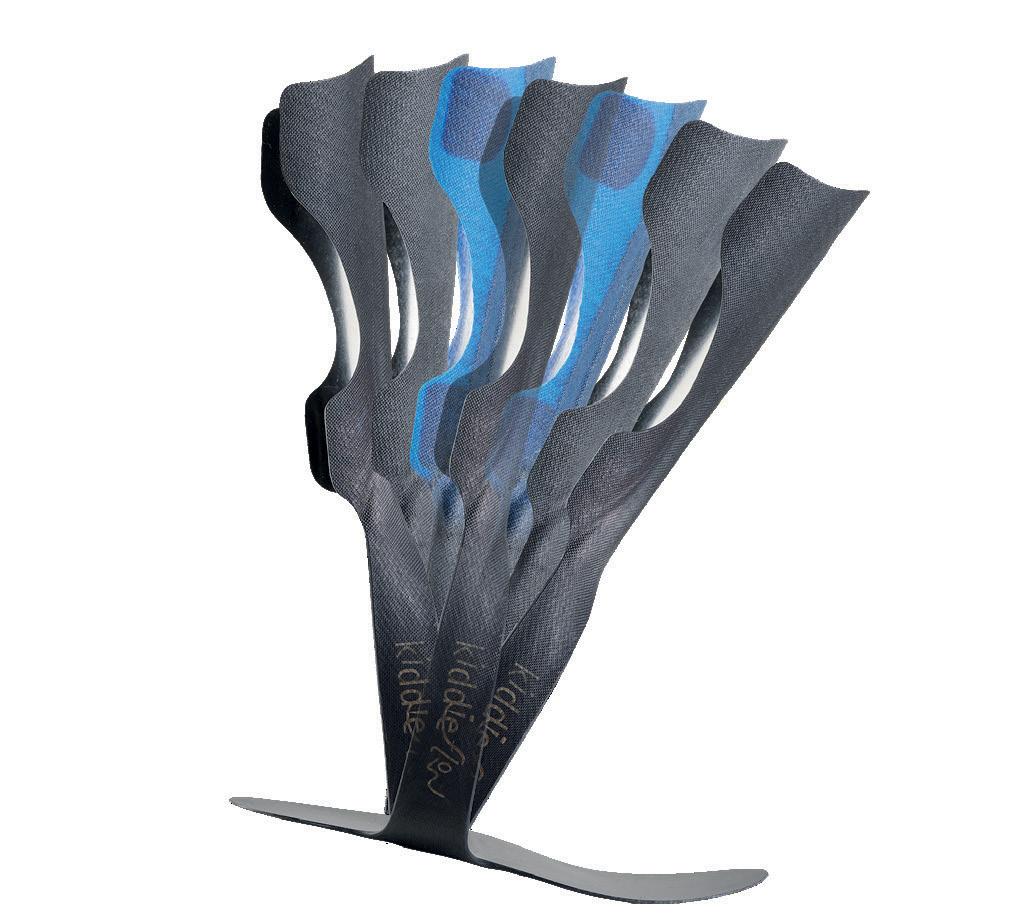
Soar through life with the Aviator. This new, lightweight foot is designed to provide high energy return, comfort, and vertical shock absorption in every step. Combining flexible Intelliweave® composites with dynamic carbon fiber, the sleek Aviator uses a hybrid material approach in its springs. These features o er superior range of motion to accommodate a wide range of activities and users. When life gets turbulent, the Aviator can help you stay the course.

PDAC APPROVED!



















More new products are coming soon! Connect with College Park for updates. www.college-park.com/aviator















issue
As a business owner and clinician, Jason Tanner, CPO, often faces one-of-a-kind problems— and he enjoys working with his hands to create helpful solutions. That’s exactly what happened when 74-year-old Randy Fisher approached Tanner about creating a replacement device for his 50-yearold knee-ankle-foot orthosis (KAFO).

Tanner, owner of Ark Valley Orthotics & Prosthetics in Wichita, Kansas, since 2008, embraced the challenge: He agreed to design a KAFO that would fit Fisher’s unique needs. Fisher was born with osteogenesis imperfecta, sometimes known as “brittle bone disease,” a genetic disorder in which bones fracture easily, often with no obvious cause or minimal injury—and he required a KAFO to ambulate.
Tanner began his undergraduate education studying physical therapy—but made the switch to O&P his freshman year after he recognized the blend of art and science that is a hallmark of the profession. “I had always liked building things and working

with my hands, and O&P seemed like the perfect combination of the medical aspect of helping people and building devices.” He worked as an O&P technician his first few years of college before pursuing his CPO credentials—and eventually purchasing Ark Valley.
Tanner embraces modern technology, but he keeps most fabrication in-house. A fabrication lab occupies the back half of the facility and is designed with windows so that patients and families can watch the process. “Part of the reason I got into the profession is that I like to build things myself,” he explains.
That mindset served Tanner well when Fisher walked into his office requiring a “once-in-a-lifetime” solution that Tanner had only seen in textbooks. “What makes this unique is that he has osteogenesis imperfecta, and he’s had 26 fractures” over the course of his life; 12 of them affected his right leg. Many of those fractures occurred when Fisher was young, impacting the growth plates and preventing growth of his right foot and leg, which is shorter than his left leg, according to Tanner.
In each
of O&P Almanac, the Transformations column features the success story of an O&P clinician who has worked with an inspiring or challenging patient. This month, we speak with Jason Tanner, CPO, who created a replacement “prosthosis” for a patient with osteogenesis imperfecta.Jason Tanner, CPO
As a child, Fisher started with shoe lifts on his right shoe. But as his leg height discrepancy became more noticeable, and his right foot remained smaller than his left foot, his orthotist suggested making a brace that would give the appearance of wearing a pair of matching shoes while also accounting for his leg length discrepancy. Fisher was fit with a device of that design in middle school and again in his early 20s. His last hip-kneeankle-foot orthosis (HKAFO) served him well for half a century. “It’s a combination of an orthosis and a prosthesis,” explains Tanner. “Because his right leg is 8 inches shorter, his leg is in a regular brace, then beneath

that, there’s an exoskeletal prosthesis with a SACH foot, that fits into a shoe and allows him to wear matching shoes.”


Over the years, Fisher relied on his brace to successfully navigate an active life as a reporter, and he also played wheelchair basketball. The “hip” part of his HKAFO eventually broke off, but Fisher found he didn’t need it. He made occasional repairs to the brace on an as-needed basis.
By last year, Fisher’s KAFO had deteriorated to the point where he was “looking to get it repaired or made new,” recalls Tanner. He visited a few O&P facilities to compare options. Fisher eventually chose Ark Valley
to make his new KAFO, telling Tanner he felt most comfortable with the team there; he was grateful the device would be built in-house rather than sent out for central fabrication.
For Tanner, the first step in designing a replacement device was to study the prosthosis that had been so successful for Fisher over the years. At that point, the leather on the original device had disintegrated in several places. Tanner could see the stainless-steel upright had been broken, patched, and welded together.




“Our first dilemma was trying to find a shoe.” Fisher’s old device had a straight-last shoe, to fit a very small foot. Fisher hoped to find a shoe very similar to his previous surgical-opening type shoe. After searching and navigating supply chain delays, Tanner located a viable replacement—a straightlast shoe from Markell. “Getting shoe sizes was difficult, but now he has a better fitting shoe” with more room for his foot and toes.
Next, Tanner took a cast. Because Fisher’s ankle and foot had recently swollen, due to an unrelated medical condition, he could no longer fit properly in the old device, so he left the device at Tanner’s facility to use as a reference.
Tanner managed the fabrication process in stages, beginning with the metalwork. He studied both the mold and Fisher’s old device to design the metal parts. Because he was providing a brace for a patient who had used the same device for so many years, Tanner sought to replicate much of the original design. “My experience is that, many times, it is better to duplicate what patients are used to, rather than to try and change them into something completely different after all these years,” he explains.
The stirrup and calf band needed to be silver-soldered to the stainless-steel uprights, according to Tanner, but he was able to convince Fisher that aluminum would be preferable for the thigh bands, resulting in a lighter weight device. Given his tibial bowing and rotation, Tanner molded the leatherwork to Fisher’s unique shape and size. “His knee center is

way off, his shin is bowed, and it’s actually rotated so the foot’s twisted off in another direction.”
After completing the metalwork, Tanner added the molded leather lacers and assembled the KAFO in a temporary fashion. The foot block was composed of wooden two-by-fours that he glued together, then he used his planer to ensure the correct thickness for the leg length discrepancy. “I had to leave wood sections removable to access the stirrup and the ankle block, so I could adjust the alignment,” he says. “These pieces were screwed together for the trial fitting.”
Tanner also made some changes to how Fisher’s foot is positioned in the KAFO. “The dilemma was getting pants” to fit over Fisher’s foot at the top of the prosthetic section of his device; Tanner plantarflexed the ankle and pointed the foot down, so it didn’t stick out as much as was the case in his old device. “We effectively made the foot length shorter by plantarflexing the ankle.”
Tanner sent Fisher home with the temporary device to test it for a few weeks. When Fisher returned, he reported that the device was great, except his anterior tibial crest was a bit red. “I gave him the option of adding some padding, letting it mold over time to his shape, or expediting the molding process by wearing the lacer after getting it wet,” says Tanner. Fisher opted for some padding to be left removable for use as needed.
In addition, as Tanner watched him walk with the device, he thought the foot needed
to be everted and outset more than his original device had allowed. Tanner made the change, then let Fisher try it again, with the padding in place over the shin. Fisher tested it again at home, then “he dropped it off a few weeks later for us to finish up the device.” At that point, Tanner glued the foot block together and his technician laminated the device. He delivered the final product to Fisher in April.
Fisher is grateful to have a new KAFO to use when he needs to ambulate, and he appreciates both the craftsmanship that went into its design and the comfort it provides him, says Tanner. “When you have someone who’s worn something for so long, they don’t necessarily want something that’s different—they just want what they have, but in a new form. And that’s what we tried to do: We gave him what he always had, but not worn out.”
Tanner says they discussed more radical changes, such as forgoing leather, “but the reason he has the leather lacer is because he’s at increased risk for fracturing” due to the underlying osteogenesis imperfecta. The leather “basically works like a cast, or fracture brace, to support the bones between the joints to keep the bones from further fracturing. That’s why it’s a wraparound system, and not an open system.”

Given the unique design of the prosthosis, Tanner completed most of the work himself, working nights and weekends outside of regular office hours, “because I wanted to make sure I gave it that TLC that it needed,” Tanner says. “My technicians helped—they formed some of the leather, and after I got the ankle block shaped, they did the lamination. The exoskeletal part was a bit of a challenge. I literally took two-by-fours to build the exoskeletal block, then carved it out to fit the curved contours of the sole of the shoe after removing the heel. After connecting the wood to the shoe, I had to figure out the plantarflexion. Next was to create the block to house the stirrup and uprights that I had

welded and soldered together. After this, I built an ankle block with a T-nut to attach the SACH foot. Once I had all of these pieces, I had to attach all of them together while getting the correct height and alignment for the leg length.”




The work Tanner put in is “something that not everyone can do anymore” because most O&P facilities use thermoplastics and laminations. “I had never brazed stainless steel; I contoured the stainless steel and then brazed it together. I had to make a stirrup—it’s more of a fabrication wonder.”
“If you figure the amount of time and materials I put into this, my rate of pay was very little, compared to what I usually make,” says Tanner. “But I love what I do, and I love the craftsmanship of making something unique.”
DO YOU HAVE A TRANSFORMATIVE PATIENT-CARE EXPERIENCE YOU’D LIKE TO SHARE WITH O&P ALMANAC READERS? Contact Editor Josephine Rossi, jrossi@contentcommunicators.com, with your story to be considered for an upcoming profile.

For Job Seekers: Job searching is easy with the pane-view job search page. Set up job alerts, upload your resume or create an anonymous career profile that leads employers to you.
For Employers:
Reach 4,500+ O&P professionals through the Job Flash™ email. Ensure high visibility for your open positions through this highly engaging email.
For more information on recruitment options, contact Customer Service at clientserv@communitybrands.com or (727) 497-6565

OWNERS:
LOCATION: Lexington, Kentucky
HISTORY: 33 years
When Maurice Adkins and prosthetist Jim McClanahan, CP, LP, first met in Lexington, Kentucky, it was to fit Adkins with a prosthesis. Like Adkins, McClanahan was a transfemoral amputee, so the two shared much in common. Adkins traveled in the coal business, but when he was in town, he and McClanahan would get together—at first to adjust Adkins’s prosthesis. Over time, the two developed a friendship, says Adkins’s son, Shayne.
“They used to talk about opening their own practice one day, with my dad taking care of the business side and Jim heading patient care,” says Shayne. “They knew they could create a clinic through the eyes of an amputee, because as amputees themselves, they knew what [would make] patients comfortable and what they appreciated.” In 1990, Adkins and Jim McClanahan launched Hi-Tech Artificial Limbs in Lexington, now called Integrity Prosthetics.
Shayne Adkins, now a certified and licensed prosthetist, began his internship in 1996 after graduating from the University of Kentucky; obtained his postgraduate degree in prosthetics from Northwestern University; and completed his residency at his father’s facility. Now president, Adkins is in his 27th year at Integrity. Both his father and McClanahan have passed on, and Adkins’s current business partner is McClanahan’s widow, Tori.
Integrity began as a small, single-location facility, and it has intentionally remained so. “Our entire goal was to create a family of employees who would make patients feel they were joining the family when they came here,” says Adkins. “We met that goal, and today, patients I saw as kids are coming in with their own kids trailing along. We’ve shared birthday parties, fishing trips, golf tournaments, and other events with our patients. Our patients know that this is the place where they will be taken care of and loved.”
Integrity does little advertising and no major marketing to referral sources, because patient loyalty and word of mouth remain so strong. Adkins is the sole practitioner at Integrity. Additional staff members include his wife, Melissa Adkins, who is on the administrative team; DeRon Cunliffe, CTP, CPA,
who has been at Integrity as a prosthetic assistant for 32 years; and Jason Smith, CTP, CPA, a technician at Integrity for 30 years.


Like many prosthetic facilities, most of Integrity’s limb loss patients have diabetes, although Adkins also works with patients who have amputations due to trauma or cancer, as well as children of all ages. “One thing I am very proud of is our longstanding relationship with the Lexington [Department of Veterans Affairs]. For three decades we have provided care for people we consider our heroes,” he says. “It is a great honor to work with military amputees, and I’ve formed close friendships with many of them.”
While Adkins often uses high-tech components, including microprocessor knees, feet, and ankles and myoelectric upper-limb prostheses, he is reluctant to adopt scanning and CAD/CAM for fabricating sockets. “All of our custom work is made in our own lab, by our own people, with their own hands on it,” he says. “This [strategy] fits well with the type of atmosphere we’re trying to create—devices made on site by the faces our patients know.”
One of Adkins’ favorite patient success stories is that of a decorated Marine who stepped on an IED and lost his vision and both of his legs. “With the prostheses we created for him, he’s become an inspirational speaker and a motivator for University of Kentucky football and basketball teams; he’s been to the Oval Office; and he competes in Spartan races and obstacle races and plays golf.”
After nearly 30 years in prosthetics, Adkins is feeling the urge to mentor a new generation of prosthetists. Integrity is working toward becoming a residency site. “I really enjoy teaching classes at local universities and rehab hospitals, and if anything, my passion has grown to pass along everything I’ve learned and am still learning.”

Adkins’ son, Josh, will begin his second summer of internship at Integrity in June. The family tradition continues.
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
100% dynamic AFO
No skin contact
Symmetrical design that fits left and right shoes
Conforms to eneven grounds and slopes
Lace clip technology that allows fast installation from shoe to shoe












Included lace clips
Warranty on plastic and\or carbon fiber par ts
insurance coverage such as VA, Medicare and MedicAid
HCPCS PDAC approved
Turbomedusa.com
2 years
3 years
See through design that is almost invisible when worn

25% lighter**
18% more dorsi-flexion power**
35% more medio-lateral strength**
2 years
Designed for patients with reduced dexterit y and hand mobility such as stroke patients
Unique front suppor t design
Easy rear entry thanks to revolutionary frontal design
Magnetized velcro strap is easily attached with one hand




25% more medio-lateral stability**

COMPANY: Invent Medical OWNERS: Family owned and operated
LOCATIONS: Philadelphia, Germany, and Czech Republic
HISTORY: 32 years

Invent Medical originated in the Czech Republic in 1991, founded by Jiri Rosicky, the company’s chief executive officer, and his brother-in-law, Milan Pustka. Both founders had expertise as mechanical engineers and studied to become orthotist/ prosthetists. At first, the company provided traditional O&P central fabrication and clinical services, as well as distribution for companies such as Össur and Fior-Gentz, but it soon moved to computer-aided design and manufacturing (CAD/CAM).
Since 2010, the company has been working with 3D printing, says Jiri’s son, Jan Rosicky, Invent Medical’s business development director. “We run a large O&P clinical facility in the Czech Republic, and we saw firsthand the limitations of traditional fabrication,” Jan Rosicky explains. “We wanted to create something better for our own patients, so we tested all kinds of 3D printers, 3D scanners, materials, and postprocessing to develop the next generation” of devices.

Invent Medical currently has offices in Philadelphia, Germany, and the Czech Republic. Eight manufacturing sites situated around the world provide local fabrication, “from Mexico to Singapore and everything in between,” Rosicky says. The company’s 75-member team includes CPOs, technicians, mechanical engineers, product designers, and software engineers, as well as marketing, sales, and administrative staff.
Invent works with O&P clinicians as their digital fabricator. The company’s first 3D-printed product was a cranial orthosis, and it continues to be Invent’s flagship offering. The company’s 3D-printed helmets are thin, lightweight, and breathable, according to Rosicky. “These attributes reduce sweating and skin issues by up to 90%, which is a huge benefit—especially for our customers in countries like Brazil and Singapore,” he says. “The smart design of the devices allows practitioners to save about 50% of clinical time, because adjustments are easier and checkups are less frequent.”
The company has expanded to offer Piro 3D-printed supramalleolar orthoses and ankle-foot orthoses (AFOs), now their fastest growing product line. “The main benefit is that they are thin, so they beautifully fit into shoes,” says Rosicky. “We’ve seen widespread
acceptance of the device, so compliance is up, and even the gait pattern is more natural. The smaller the patient is, the more they appreciate that it is so unobtrusive.”

Using a combination of nylon and flexible material, Invent created advanced designs that are soft and malleable on bony prominences to relieve pressure points, according to Rosicky. “They respond to the anatomy to prevent problems.”
The company also prints a below-knee prosthetic socket for adults, which has a soft brim and soft inner pads to prevent pressure. “We tested this device with CPOs who are amputees themselves,” who offered positive feedback, Rosicky says.
Invent Medical’s customers are clinicians, and the company works with more than 400 O&P clinics and hospitals in 40 countries. Clinicians provide 3D scans and additional information through the online portal; Invent produces the final, warrantied products.
It takes about five years to bring a new product to market, according to Rosicky. “We go through 3 million cycles to make sure our AFOs don’t fail,” he notes. “Then we actually test these products with our own patients in-house for about three years, and then work with early-adopter customers to perfect the product and get feedback before the official launch.”
Sustainability is an important aspect of the company’s operations. Rosicky says, “With HP 3D printing, all the material we don’t use we can repurpose and use again. Also, unlike most, we use a plant-based, fully renewable material.”
Over the next three to five years, Rosicky expects that all cranial orthoses will be produced by 3D printing, and that many more—but not all—devices will benefit from the 3D-printing technology. “3D printing is just a tool. However, if paired with the right design and process, it can add significant value,” he says. “Our goal is to responsibly drive this change and democratize accessibility to 3D printing and a new generation of devices. We follow our mission: Together, helping through innovation.”
The Invent Medical team members Invent Medical offers a variety of products, including ankle-foot orthoses and cranial remolding helmets.













The American Orthotic & Prosthetic Association (AOPA) has opened its annual call for volunteers and we need your talent. Employees of all AOPA member companies are invited to serve on one of AOPA’s Committees and/or Workgroups.






















APPLICATION DEADLINE:




Terms of service are two-years and begin December 1, 2023.

QUESTIONS? Contact Betty Leppin at bleppin@AOPAnet.org or 571-431-0810.



Are you thinking about a career change? Is your company looking to hire? Visit AOPA’s online Career Center! With dedicated pages for job seekers and employers, the Career Center is the perfect place to make O&P career matches.
The Career Center also features a Career Planning Portal to assist job seekers in their searches. Visit today at jobs.aopanet.org !
Stay up to speed on all of the rules and regulations for 2023— join AOPA’s regulatory staff and guest speakers for the 2023 monthly webinar series. Webinars provide relevant content and the opportunity to earn 1.5 continuing education credits each month. They are a great way to promote team building, providing an opportunity for your staff to come together and refresh their skills. One registration provides access for five staff members at your office location. (Contact Kristen Bean at kbean@AOPAnet.org to register more than one person from your facility— maximum of five per facility.)
New this year, and in response to feedback on preferred ways to access the webinars, all 2023 webinars will be available on demand (asynchronous) instead of live. Topics will be announced at the beginning of the month, and the webinars will be automatically delivered to AOPAversity accounts by the end of the month—then remain available. The

NuTech Synergies
1800 Gordon Road
Jamestown, OH 45335-9730
937-510-2220
Mark Ford
Supplier Startup
popular Clinician’s Corner session will be featured in several webinars.
The full-year series is $790 for AOPA members—a great value at 12 for the price of 10! Nonmembers may purchase the series for $1,999. Individual webinars may be purchased at $79 for AOPA members and $199 for nonmembers.
Register for the series at My AOPA Connection. You also may register for single topics.
Note that AOPA experts and guest speakers will be available to answer questions should they arise after you view the webinar. Contact AOPA’s experts with suggested webinar topics or questions: Email jmcternan@aopanet.org or dbernard@aopanet.org
Orthopaedic Associates of Michigan
555 Midtowne Street NE
Grand Rapids, MI 49503-5729
616-459-7101
oamichigan.com
Courtney Arnett, CO
Patient-Care Facility
Orthopaedic Associates of Michigan
1111 Leffingwell Avenue NE Grand Rapids, MI 49525 616-459-7101
oamichigan.com
Patient-Care Facility Affiliate
Orthotica
29 Star Flower Row Riverhead, NY 11901
888-895-1305
orthotica.com
Peter Karolidis
Supplier Startup
The officers and directors of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
Contact Bob Heiman at bob.rhmedia@comcast.net
KiddieFLOW™, Allard USA’s extension to our pediatric AFO line, was introduced in response to clinician requests for an orthosis with more foot plate flexibility. KiddieFLOW allows for better control of foot positioning in late swing, which aids in stability during stance. FLOW models offer increased ROM in the sagittal plane and a smoother transition (flow) throughout the gait cycle.

For more information, contact customer service at 888-678-6548 or info@allardusa.com and request your free Teddy Bear Tape Measure!
The world does revolve around you. The Orbit foot was designed to provide smooth rotation and rollover. College Park’s unique, built-in torsion feature has integrated energy return, which may improve comfort for golf, baseball, tennis, and more! The durable Orbit offers an incredibly low profile and total rotation range of 40 degrees. This foot also incorporates College Park’s composite expertise in a carbon fiber design, helping to provide a dynamic response during low- to high-impact activities.
To learn more or request a demo, please visit college-park.com/orbit

ESP created the Flexi family of suspension sleeves as a comfortable, durable, and cost-effective alternative to traditional suspension sleeves. Preflexed at 43 degrees for maximum comfort and natural unrestricted movement.

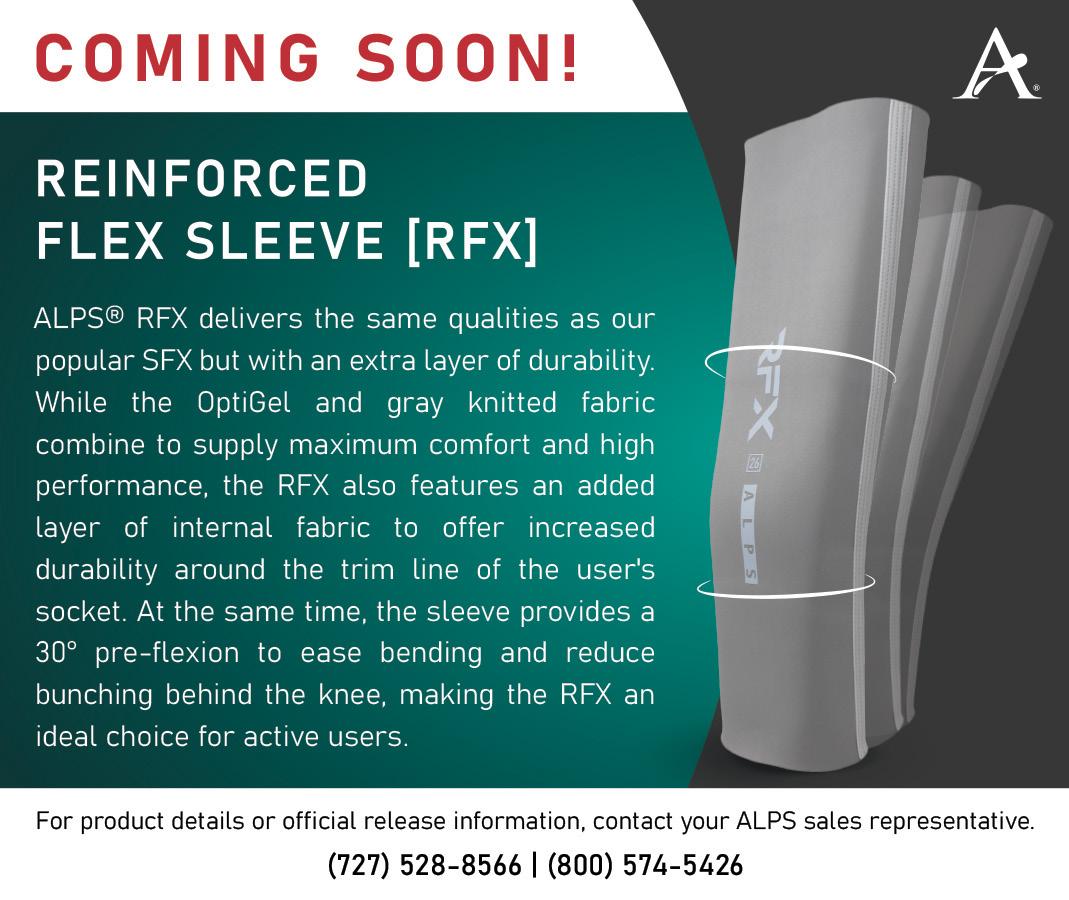
For more information, call ESP LLC at 888-932-7377 or visit wearesp.com
Hersco is delighted to offer HP’s advanced 3D-printing technology for custom orthotics. 3D printing has unique design capabilities not possible with other methods—reducing landfill waste by 90%! The accuracy of 3D is unparalleled, specs exceed direct-milled polypro, and manual plaster fabrication. Among the benefits: a 90% reduction in landfill waste, many new design possibilities for posting, and the ability to vary thickness and flexibility across the shell. The PA-11 polymer is a biobased renewable material that has been tested and proven in research and industry.

Call today, 800-301-8275, for a free sample.
It’s all about function. We are the manufacturers of durable prosthetic devices specifically for finger and partial-hand amputations. Our aim is to positively impact our wearers’ lives by providing high-quality finger prostheses. We offer four devices: MCPDriver (shown in rose gold), PIPDriver, ThumbDriver, and our newest device, the GripLock Finger. Our devices help to restore length, pinch, grasp, stability, and protection for sensitive residuum. Robust device engineering and their ability to withstand harsh environments help get people back to performing activities of daily living, and back to work. All are available in a dozen color coatings to match our wearers’ preferences and styles. To learn more, visit npdevices.com

The Varos Adjustable Socket is designed to benefit transfemoral amputees starting in the rehabilitation phase as well as later during treatment with the final prosthesis. Varos is adjustable by the user to account for volume fluctuations and everyday activities (sitting, driving a car) at any time and any place. Combined with the Kenevo, your patients can have everyday confidence, right from the start!
For more information, visit shop.ottobock.us

The multiarticulating hand you know and love with improved functionality—the bebionic hand! We’ve redesigned some of the most vulnerable and delicate components of the bebionic hand to improve overall durability and reduce service burden. The improved bebionic features a novel automotive coating in pearl white and matte black for a modern and sleek finish. Improved stand-by time to experience function all day long. Field serviceable interchangeable modular fingers for quick repair turn around for user-focused assistance, giving you greater clinical impact and control.
For more information, visit shop.ottobock.us


Patients with a transfemoral amputation place high importance on being able to complete functional tasks and activities of daily living. An independent study found that after 30 days of at-home use, patients identified five functional tasks as easier to complete with the PROTEOR QUATTRO MPK compared to their typical MPK. On average, subjects rated the following complex tasks statistically significantly easier with the QUATTRO: Walking backwards, walking sideways, walking over an obstacle of six inches in height, kneeling on their prosthetic knee, standing up, and swinging a golf club. Read more about this study here: freedomquattro.com/clinical-evidence

Turbomed has extended its line of AFOs to include three models: Xtern Classic, Summit, and Frontier. The Xterns will allow running, walking, and even hiking as long and far as you want without discomfort. Their unique design acts as an exoskeleton to the impaired limb, keeps the foot at 90 degrees, and provides the user with unparalleled levels of function.
The Xtern Summit is lighter than the Classic, has more dorsiflexion power, and features a see-through design. The Xtern Frontier was designed for patients with reduced hand dexterity and requiring front leg support. Visit turbomedusa.com, and think outside the shoe!
A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P. Scan
Contact Bob Heiman at bob.rhmedia@comcast.net
June 1–30
ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at abcop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org or visit abcop.org/contact-us
June 23–24
PrimeFare East. Nashville Renaissance Hotel and Conference Center. In-person meeting. Contact Cathie Pruitt at 901-359-3936, pruittprimecare@gmail.com; or Jane Edwards at 901-487-6770, jledwards88@att.net. For more information, visit primecareop.com

June 30
Deadline for Applications To Volunteer for an AOPA Workgroup or Committee. Visit aopanet.org/volunteer or contact Betty Leppin at bleppin@aopanet.org, 571-431-0810.
July 27–29
Alabama Prosthetic & Orthotic Association Meeting. Birmingham, AL. Visit alabamapoa.org

August 24–26
Texas Society of Orthotic & Prosthetic Professionals Meeting. San Antonio. Visit txsop.org.
September 6–9
AOPA National Assembly. Indianapolis. For more information, visit aopanet.org
November 8–10
New Jersey AAOP Annual Meeting. Harran’s Resort, Atlantic City, NJ. Visit njaaop.org

Full-year series: AOPA member $790; Nonmember $1,999
Individual webinar: AOPA member $79: Nonmember $199 Register for the series at My AOPA Connection www.bocusa.org
Advertise O&P events for maximum exposure with O&P Almanac Contact Bob Heiman at bob@rhmedia.comcast.net or learn more at bit.ly/23AlmanacMediaKit. Announcement and payment may also be sent to O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 223340711 or emailed to jburwell@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
ORTHOTIC, PROSTHETIC AND PEDORTHIC EDUCATION AND CE CREDITS FROM THE ORGANIZATION THAT KNOWS O&P.
Each month, State By State features news from O&P professionals about the most important state and local issues affecting their businesses and the patients they serve. This section includes information about medical policy updates, fee schedule adjustments, state association announcements, and more. These reports are accurate at press time, but constantly evolve. For up-to-date information about what is happening in your state, visit the Co-OP at AOPAnet.org/resources/co-op
The New York legislature has introduced a second insurance fairness bill, Senate Bill (SB) 6039. Like Assembly Bill 4395, SB 6039 requires that individual, group, and inpatient plans in the state provide coverage for prosthetic devices that are intended for medically necessary rehabilitative and habilitative services as required by the Affordable
Care Act’s Essential Health Benefits. However, SB 6039 specifies that the bill would only affect policies that also cover durable medical equipment (DME), and that coverage for prosthetics must be equivalent to the coverage provided for DME. In addition, specific language in SB 6039 prohibits denials of coverage if an enrollee’s physician determines a device is medically necessary.
O&P advocates in several states are making progress in their quest for improved coverage of O&P devices for children
In Arkansas, House Bill (HB) 1252, which mandates coverage of one additional prosthetic device for “athletics or recreation” (amended to be limited to K3 and K4 functional levels) and one additional prosthetic device for “showering or bathing,” has passed the House and Senate with the help of Francois Van Der Watt, CPO, LPO; Frank Snell, CPO, LPO, FAAOP; and the Arkansas State Orthotics and Prosthetics Association. The bill now awaits the governor’s signature to be enacted into law.
In Colorado, HB 1136, which mandates coverage for an additional activity-specific prosthesis for enrollees in commercial plans of all ages, has passed the House Health and Insurance Committee and will now move to the House Appropriations Committee. On March 1, advocates with the Rocky Mountain Orthotic and Prosthetic Coalition participated in Colorado’s Disability Rights Day at the Colorado State Capitol, where they met with legislators to gather support for the cause.

In Illinois, Senate Bill (SB) 2195, which mandates coverage of activity-specific orthoses and prostheses in commercial health
SB 797, which would implement insurance fairness for O&P devices in private group and individual health insurance plans in the state, has passed the Senate and will now move to the House. The bill was supported in part by testimony from O&P patients and providers in the state, as well as AOPA’s manager of public engagement, Nicole Ver Kuilen.
House Bill (HB) 626 and identical companion bill SB 673, introduced earlier this year, would mandate that private plans in the state offer coverage for prosthetic devices that is at least equivalent to Medicare. The bills are identical to SB 2140 and HB 2214, which were introduced during last year’s legislative session.
For more information on these and other state developments, visit the AOPA Co-OP or contact Sam Miller at smiller@AOPAnet.org
plans for enrollees of all ages, has passed the Senate with the assistance of the Illinois Society of Orthotists and Prosthetists. SB 2195 will now move to the House.
In Indiana, HB 1433 has passed the House and its first Senate committee due to efforts from the Indiana Association of Orthotics and Prosthetics. HB 1433 requires that Indiana Medicaid cover an orthotic or prosthetic device that meets both ADL and physical activity needs for patients 18 and under; mandates orthotics coverage in Indiana Medicaid; and increases the Indiana Medicaid fee schedule to 100% of Medicare.
In New Mexico, HB 131, which prohibits insurers from discriminating or conducting unfair trade practices upon the basis of disability (including limb loss and limb difference) in the provision of everyday and activity-specific O&P devices, was signed into law by Gov. Michelle Lujan Grisham with the help of Kyle Stepp, Laura and Callaway Lewis, and other advocates in the state. The bill will take effect Jan. 1, 2024.
• Basic business acumen
• Practical knowledge to apply immediately to your work
• Techniques for developing better business practices


• How to think about improving your company’s returns



To complete the certificate program, you must register and complete one core course and one elective course from each of the four areas of learning within a four-year period
OF LEARNING CORE ELECTIVES



O&P
MANAGEMENT Increase
knowledge and skills to better manage multiple, individual, and team priorities.
HEALTHCARE SALES AND MARKETING Learn the functions of marketing along with a variety of tools and approaches to personal selling along with the many digital marketing tools available. 5
Healthcare
A dynamic companion for every step.
Designed for motivated patients with higher mobility, the NEW Dynion mechanical knee is an ideal companion for independent, self-determined users who are ready to push their goals to the next level.


Scan for more!
