

SPRINGING INTO ACTION
WE BELIEVE
in taking care of the legal, so you can take care of the patients.

We've been serving the legal needs of the Arkansas healthcare industry for more than 120 years.
• Medical Malpractice Defense
• Healthcare Transactions & Employment Agreements
• Government Relations & Administrative Proceedings
• Licensing, Privileging & Peer Review
• Labor & Employment Concerns
• HIPAA Privacy & Security
• Stark I and II & Anti-Kickback Statutes
• Medicare/Medicaid & Insurance Reimbursement
• Telehealth & Remote Healthcare
• Long-Term Care & Skilled-Nursing Defense
• Defense of Claims Against Pharmacies & Pharmacists
Your Arkansas Healthcare Law Team


What does it mean to be taken care of?
At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and to help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.

Nancy
Pam
Ashley
Mike Spain,
Roland R.
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-Elect
Michelle Krause, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Rogers / At-Large
Chris Barber, Jonesboro
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
Bob Honeycutt, Russellville
James Magee, Piggott
Guy Patteson, Jonesboro
Gary Paxson, Batesville
Eric Pianalto, Rogers
Douglas Ross, Hot Springs
Neta Sue Stamps, Berryville
Michael Stewart, Benton
Brian Thomas, Pine Bluff
Tina Creel / President of AHA Services, Inc.



Active Involvement
The Arkansas Hospital Association’s (AHA) mission is to safeguard hospitals’ operational effectiveness in advancing the health and well-being of their communities. Supporting our hospitals in the areas of health care quality and patient safety is one of the most important ways we do this.
More than a decade ago, the AHA established our Department of Quality and Patient Safety under the able leadership of Pamela Brown. Pam and her team strategize constantly with our hospitals as they seek to provide each patient with the best outcome possible, identifying and diminishing the possibility of avoidable harm, and delivering the highest possible quality of care.
We are dedicating this issue of Arkansas Hospitals to health care quality and patient safety. Inside, you’ll find articles contributed by experts at the local, state, and national levels, and you'll get an inside look at how the AHA works with our hospitals to create sustainable cultures of safety.
Beyond providing assistance to our hospitals through our Quality Department, the AHA directly advocates for legislation that will help our hospitals improve health care quality. In fact, we’ll soon be heading to Washington, D.C., for the annual meeting of the American Hospital Association to do just that.
Each year, our association sponsors a private luncheon with our senators, congresspeople, and their staff members. This year, I’m specifically looking forward to probing our congressional delegation on the area of health care spending.

We know – and they know – that workforce shortages, severe government underpayment for Medicare and Medicaid care services, and the continually rising costs of providing care are choking hospitals financially. Many Arkansas hospitals are struggling to keep their doors open. With drastic cuts to health care programming now under serious consideration by Congress, we will be asking the delegation to hold firm and avoid cuts that will negatively affect hospital budgets.
Taking Arkansas hospitals’ concerns and local stories directly to Senators Boozman and Cotton and Representatives Crawford, Hill, Womack, and Westerman (and their staff members) drives home the impact that Washington actions have at the local level.
We ask that you, our hospital leaders and stakeholders, accompany us to Washington, D.C. for the American Hospital Association’s annual meeting and our congressional luncheon. To help defray the costs of registration, travel, and lodging, the AHA is offering a $2,500 stipend to hospital leaders who make this education- and advocacyoriented trip to Washington with us. You can contact Lyndsey Dumas or me to learn more about this incentive.
In this issue of the magazine, you’ll also find an update on our state’s 340B program. Arkansas was the first state to pass 340B legislation regarding contract pharmacies’ specific involvement in the program, and other states are now following our lead and turning to us for guidance as we seek to protect this vital participation.
Whether it’s helping to protect the 340B drug program, helping to carry Arkansas hospitals’ message directly to our congressional members, or honing your hospital’s quality and patient safety programming to create the best possible culture of safety, I urge you to stay involved.
Arkansas’s patients, and our hospitals, depend on you.




The Big Picture
The best thing about my role as the association’s Director of Communications is that I get the chance to work directly, every day, with every department at the AHA.
In any given week, I might produce a handout with talking points that support our advocacy agenda, an email campaign inviting members to attend a Quality Forum, a data-driven report that helps hospital leaders communicate with legislators and stakeholders about the economic impact of hospitals, a directory of AHA Services vendors, and a website promoting our annual meeting.
This constant variety in my work not only holds my attention – it also gives me a unique perspective on how all the work we’re doing overlaps and interlocks. Where some might see a vast array of diverse projects, I see the totality of our work as greater and more profoundly meaningful than the sum of its parts.
As we pulled together this issue of Arkansas Hospitals , which is focused on all the best and latest initiatives in the world of health care quality and patient safety, I realized that the AHA Quality Team's work has a similarly complex impact on all the most fundamental aspects of hospital care. Reporting and making data-driven improvements, bedside systems to enhance patient outcomes, and compliance with the requirements of payors – these (and so many more efforts in quality and patient safety) are all crucially important to the mission of hospitals and to their long-term financial viability.

In these pages, you’ll learn more about Arkansas hospitals’ commitment to continuously improving patient experiences and outcomes. You’ll get reacquainted with the AHA Quality Team and how they serve our hospitals, and you’ll find out about some exciting new opportunities the AHA is adding to our quality program.
We’ve also included an article highlighting a recent ruling in ongoing 340B litigation: Arkansas’s 340B Nondiscrimination Act has been upheld by the 8th Circuit Court of Appeals. This decision directly affects Arkansas patients and hospitals’ ability to deliver high-quality health care in our state.
Sometimes, it’s useful to shift perspective from the “big picture” vantage point of the entire quality “umbrella” and, instead, zoom in. The quality and patient safety interventions being developed and implemented by Arkansas hospitals often require them to take a very detailed, granular focus – where checklists, protocols, and formulas abound. Being fully “zoomed in” is often a matter of life or death in our hospitals, and we’re proud to showcase a few of our member hospitals’ efforts in this edition focused on quality and patient safety.
Whether we’re looking at health care in general, quality and patient safety in particular, or the details involved in every health care professional’s daily work, our viewpoints matter. The “big picture” of health care in Arkansas is far greater than the sum of all the work of thousands of individuals. Our purpose is what animates that work: delivering the best possible care for our fellow Arkansans.
2024 Spring Calendar
APRIL
April 14-16
American Hospital Association
2024 Annual Meeting Washington, D.C.
April 17
AHA Healthcare Cybersecurity Alliance Meeting
Virtual event
April 19
Arkansas Association for Medical Staff Services (ArkAMSS)
2024 Spring Conference
AHA Classroom
April 23
340B Quarterly Meeting
Virtual event
April 25
AHA Quality Forum
Virtual event
April 25-26
Society for Arkansas Healthcare Purchasing and Materials Management (SAHPMM)
2024 Annual Meeting and Trade Show
DoubleTree by Hilton Hot Springs
MAY
May 1
Quarterly CAH Leadership Meeting
AHA Classroom
May 9
AHAA Board Meeting
AHA Board Room
May 14-15
2024 Emergency Preparedness Forum
Wyndham Riverfront Little Rock, NLR

May 15
AHA Healthcare Cybersecurity Alliance Meeting
Virtual event
May 16
AHA Quality Forum
Virtual event
JUNE
June 6
Arkansas Hospital Association Workers’ Comp Self-Insured Trust (AHAWCSIT) Board Meeting
Virtual event
June 13
AHA Quality Forum
Virtual event
June 19-21
2024 AHERT Leadership Conference
The Peabody Memphis
June 19
AHA Board Meeting in conjunction with the 2024 AHERT Leadership Conference
The Peabody Memphis
June 26
AHA Healthcare Cybersecurity Alliance Meeting
Virtual event
The Solar Eclipse and Patient Safety Preparations in Arkansas
By Danyelle McNeill, Arkansas Department of HealthOn April 8, 2024, a total solar eclipse will take place in the skies over North America. Nearly two-thirds of Arkansas (53 of 75 counties) will be in the path of totality, or the track of the moon’s shadow across the Earth’s surface that totally blocks the sun.
The path of the April 8 eclipse will impact Texas, Oklahoma, Arkansas, Missouri, Illinois, Kentucky, Indiana, Ohio, Pennsylvania, New York, Vermont, New Hampshire, and Maine. Small sections of Tennessee and Michigan will also experience moments of totality, and all of the states involved will also experience periods of partial eclipse.
As a result of this infrequent phenomenon, millions of people are expected to visit Arkansas to witness the eclipse, and many of our state’s communities will be holding eclipseviewing festivals, as well.
PREPARING FOR A MASSIVE INFLUX
A large, sudden influx of out-of-state visitors could create safety issues for Arkansans and create challenges for the organizations that serve and protect them. For more than a year, the Arkansas Department of Health (ADH) has been working with multiple state agencies and partners to plan for such safety concerns. For example, highways may become congested, cell phone towers may become overtaxed and hamper communications, and a surge of patients could impact hospital emergency rooms.
To begin their preparations for the April 8 eclipse, ADH and the Arkansas Department of Emergency Management reviewed after-action reports from states that experienced the total solar eclipse of 2017, hoping to learn what challenges they faced, what strategies were most effective, and what they learned from the experience.
Joe Martin, director of the ADH’s Office of Preparedness and Emergency Response Systems (OPERS), explains the organization’s specific preparatory work with health care facilities in Arkansas: “OPERS has made eclipse planning a high priority. We are working to help Arkansas hospitals and emergency medical
services (EMS) prepare for this event as efficiently as possible. With the prospect of delayed response times and possible surge events, we are involving [Arkansas health care entities] in the statewide preparation for potential impacts [the eclipse and its many observers may bring] to our state and their facilities.”
WORKGROUP PREPARATIONS
The ADH is holding monthly workgroup meetings in the lead up to the eclipse. The workgroup includes the Arkansas Hospital Association, the Arkansas Ambulance Association, EMS partners, hospital partners, and other community members. The workgroup drafted a joint letter to hospitals and EMS agencies with important things to consider as they undertake their preparations.
During the event, the ADH will staff its emergency operations center (EOC) to monitor the situation.
The ADH’s Environmental Health program recommends that event organizers secure permits for food vendors and follow rules for mass gatherings. These rules for mass gatherings, available on the department's website, provide a comprehensive guide to obtaining contact information for first responders and wrecker services; planning travel routes; making parking arrangements; managing waste disposal; identifying potable water sources; locating potential spaces for med-flight landings; and advising communities on identifying accessible manholes for RV waste disposal.
Ultimately, the eclipse is an incredible educational and economic opportunity for communities across the state.

“The 2024 solar eclipse will be an important and enjoyable event for Arkansas,” Martin says. “The Department of Health wants to ensure that our citizens and tourists can safely enjoy their time here in our state.”
Danyelle McNeill serves as the Public Information Officer for the Arkansas Department of Health’s Office of Health Communications.
HOSPITAL NEWSMAKERS

Governor Sarah
signed
Executive Order March 6 regarding Arkansas’s high maternal mortality rate. Among other interventions, the Executive Order creates the Arkansas Strategic Committee for Maternal Health, a statewide plan for improving education about and access to health care available to women in the state. The initiative also includes plans for a pilot program to be launched in five counties (Crittenden, Garland, Phillips, Polk and Scott), with the intention to "increase the percentage of women who access prenatal care in the first trimester and reduce incidences of women who receive no prenatal care prior to delivery.”
AHA President and CEO, Bo Ryall, and AHA Executive Vice President, Jodiane Tritt, were guest speakers at a recent State of Healthcare Breakfast, an event hosted by the Harrison Regional Chamber of Commerce and North Arkansas Regional Medical Center (NARMC). NARMC CEO Sammie Cribbs Roberson also spoke to the group. The gathering brought together Harrison's community leaders to learn more about the critical challenges currently impacting our state and local hospitals – and how those challenges can affect local and regional economies.
The Arkansas Children’s Hospital (ACH) Neonatal Intensive Care Unit has received a Gold-Level Beacon Award for Excellence from the American Association of Critical-Care Nurses. It is one of only 11 NICUs in the nation to achieve this honor.
Progressive Health of Helena is the new name for Helena Regional Medical Center and its related clinics. The hospital has recently been granted Rural Emergency Hospital status.
Michael Wood, PT, DPT, is the new CEO at Mena Regional Health System. He has been with the system since 2017, previously serving as Interim CEO, Director of Inpatient Rehab, and Director of Outpatient Therapy Services. He earned his Bachelor of Science in Health Professions and Related Clinical Sciences and his Doctor of Physical Therapy degrees from the University of Central Arkansas.


White River Health Behavioral Health in Batesville has been recognized as Inpatient Program of the Year by Signet Health, as a part of the first-ever Signet Excellence in Advocacy Awards. The award is presented to recognize a hospital program that demonstrates excellence throughout the year and achieves exceptional overall program performance.
ACH has been designated as a Level 1 Pediatric Trauma Center by the American College of Surgeons. It is the state’s only Level 1 Trauma Center for Pediatrics, and this year’s designation is the organization’s third reverification.
Megan Bonney, MHA, is the new President of CHI St. Vincent North. She previously served as the CHI St. Vincent Director of Orthopedics and Cardiovascular Services and has served various roles with the CHI St. Vincent System since 2015. She earned her Master of Health Administration from Cornell University and her bachelor’s degree from the University of Rochester.
The University of Arkansas for Medical Sciences (UAMS) has been designated by the American College of Surgeons as the state’s only adult Level 1 Trauma Center, a distinction it has held, and for which it has been reverified, for seven years.
UAMS announced establishment of its eighth institute, the Institute for Community Health Innovation, effective March 1. The Institute will work with communities across Arkansas to conduct community-based research and deploy communitydriven programs to improve health outcomes in rural and medically underserved areas of the state. The Institute, which will be based in Northwest Arkansas, will have staff and offices across the state, including in Batesville, El Dorado, Fort Smith, Helena-West Helena, Jonesboro, Lake Village, Little Rock, Magnolia, Pine Bluff, and Texarkana.
Washington Regional Medical Center has earned renewal of its designation as an Antimicrobial Stewardship Center of Excellence (CoE) by the Infectious Diseases Society of America. This designation is considered the industry’s gold standard in antimicrobial stewardship. Washington Regional first achieved CoE status in 2018.
Mena Regional Health System is transitioning from a Prospective Payment System facility to a Critical Access Hospital. The transition will occur over the next several months to allow for uninterrupted health services.
Fulton County Hospital has reached a longterm agreement to become part of the Baxter Health system. Baxter Health will continue management of the hospital until the longterm agreement launches January 1, 2025.

Phase II funding will bring new services to the CARTI Cancer Center in El Dorado.
CARTI has secured seven million dollars in funding to finalize Phase II development of its $19 million comprehensive cancer center in El Dorado. Phase II will bring radiation oncology and imaging services, including mammography, CT, and MRI, to the facility.
Share your hospital's news with us by sending to Ashley Warren, Director of Communications, awarren@arkhospitals.org
The Hospital Quality Umbrella
By Pamela Brown, RN, BSN, CPHQ Vice President of Quality and Patient Safety, Arkansas Hospital AssociationQuality and patient safety is an umbrella under which numerous assessment, education, compliance, and goal-setting programs come together to improve patient care in America’s hospitals. Long a mainstay of the Arkansas Hospital Association’s (AHA) hospital-centered focus, the movement is roaring back both nationally and at the local level in 2024.
Not that it ever was put on a back burner, but COVID-19 shifted the way we think about hospital quality and the measures we will take to safeguard our patients' health.
In fact, during the long days of the pandemic, hospital quality and patient safety was of critical importance in every hour of every day to patients, medical professionals, hospital workers, and hospital administrators alike – more so than ever.
As the emergent nature of COVID has evolved into a lower-level, yet ever-present, threat, so has the nation's approach to health care quality evolved in the wake of the shock the pandemic gave to our field.
In this issue of Arkansas Hospitals , we are
highlighting some of the programs and priorities that hospitals will see emerge and/or persist in the quality field this year and into the future.
QUALITY’S MANY FACETS
Health care’s approach to quality and patient safety has many facets. There are national priorities, there are priorities set at the state level, and there are goals and priorities that individual Arkansas hospitals set for themselves. In each of these areas, the AHA’s Quality Team works daily to serve the hospitals and patients of our state.
Whether taking a long view of hospital quality or working specifically on an individual quality improvement project, quality and patient safety as addressed by the Arkansas Hospital Association includes a wide range of policymaking, compliance, and patient care services.
The AHA's Quality Team is made up of nurses – with an array of expertise and experience, both bedside and supervisory, in areas like critical care and

infection prevention – and administrative staff, who help streamline our efforts so that we can do more, more effectively. We are dedicated to helping our member hospitals achieve their goals of continuous improvement.
2024’S NATIONAL QUALITY PRIORITIES
National priorities in the quality and patient safety realm are determined by policies and regulations resulting from enacted legislation.
Based upon this legislation, the Centers for Medicare & Medicaid Services (CMS) sets its National Quality Strategy, which is designed to promote quality outcomes, safety, equity, and accessibility for all individuals. CMS sets Quality Assessment & Patient Improvement (QAPI) Conditions of Participation (CoP) guidelines that health care organizations must meet in order to participate in the Medicare and Medicaid programs. The AHA's Quality Team helps our member hospitals meet and stay cognizant of these QAPI CoPs, tailoring programs and education to each hospital’s needs. The overarching goal of QAPI CoPs is to help hospitals deliver safe, quality patient care and prevent adverse events and patient harm.
Also involved at the national level are the Centers for Disease Control and Prevention and other public health agencies, which recommend national public health initiatives, strategies, and action plans designed to address the nation’s most pressing health problems. Again, the AHA Quality Team steps in to help our member hospitals participate in and benefit from these public health initiatives.
Specific national priorities for 2024 include reducing the numbers of hospital acquired conditions, reducing readmissions, identifying health disparities, analyzing social determinants of health in localized populations, increasing patient and family engagement in the health setting, and improving the patient experience.
AHA’S FOCUS ON HOSPITAL NEEDS
The AHA Quality Team’s work is process-oriented. We help hospitals initiate improvement goals, and we then conduct gap analyses to examine opportunities for improvement that exist between today’s baseline and the future point where goals are met.
We provide our hospitals with technical assistance designed to help them improve their approaches to and use of evidence-based practices, and we offer a variety of forums where quality professionals can learn together and from one another.
We keep our hospitals updated on regulatory changes under which their own quality assurance and compliance efforts will be measured, and we assist our member hospitals with meeting their data submission requirements at the state and federal levels.
Besides the four-member Quality Team, other areas of the AHA staff work toward assisting our hospitals’ quality efforts:
AHA Analytics provides necessary data and research to support hospitals’ work to improve quality and patient safety at the local level.
AHA Education provides webinars and inperson teaching/training events that help hospital staff members sharpen their quality and patient safety skills.
AHA Advocacy conveys our hospitals’ concerns and policy positions to decision-makers in Washington, D.C., and Little Rock, assuring that the local hospital voice is heard by legislators when policies are debated.
AHA Communications provides resources and tools for staying in touch with cutting-edge strategies in-play at both the national and state levels.
AHA Services, Inc., offers group-rate pricing for those goods and services hospitals require to keep their quality and patient safety efforts on target and in focus.
YOUR HOSPITAL’S GUIDE TO QUALITY AND PATIENT SAFETY IMPROVEMENT
We hope this edition of Arkansas Hospitals magazine will serve as a guide to the many areas of health care quality that fall under the quality and patient safety umbrella. we want you to have access to current movements in Arkansas hospital quality and the ability to tap into strategies and initiatives that can improve care for your patients and their families. Please feel free to contact the AHA Quality Team for assistance in reaching your hospital’s quality improvement goals. We are here to serve you.
The AHA Quality Team
PAMELA BROWN, RN, BSN, CPHQ, Vice President of Quality and Patient Safety
Pam earned her BSN in Nursing at the University of Central Arkansas and has served as Vice President of Quality and Patient Safety at the AHA for more than 12 years. Prior to that, she served as Associate Vice President of Quality Programs at AFMC for four years after serving that organization for seven years as the Manager of Hospital Quality Projects. Her 42 years as a nurse has given her experience in hospitals, home health agencies, and long-term acute care from the bedside to leadership roles.
CINDY CRUMP, MBA-HM, BSN, RN, Quality Specialist
Cindy earned her MBA in Health Care Management from Western Governors University and her BSN in Nursing at the University of Arkansas at Little Rock. She has served as a Quality Specialist at the AHA for nearly six years. Prior to that, her nursing career included service as Director of Quality and Patient Safety/Patient Safety Officer for Mercy Hospital Northwest Arkansas for nearly five years, as ICU Director/Project Manager/Quality Coordinator at Siloam Springs Regional Hospital for three years, and at Saline Memorial Hospital for 11 years as an Intensive Care Nurse and Wound Care Center Manager.
NIKKI WALLACE, MS, BSN, RN, Quality Specialist
Nikki earned her master’s degree in Patient Safety Leadership from the University of Illinois Chicago and her BSN in Nursing from the University of Arkansas at Little Rock. She has served as a Quality Specialist at the AHA for more than eight years, and prior to that she served as an Infection Preventionist at Jefferson Regional Medical Center for more than 10 years. She also served for a time as an RN with Arkansas Hospice.
CINDY HARRIS, Administrative Assistant
Cindy has served as Administrative Assistant in the AHA’s Quality and Patient Safety Department for 12 years, and prior to that served as an administrative assistant at AFMC for many years.








Hospitals Are Leading the Way to Advance Patient Safety
By Rick Pollack, American Hospital AssociationPatient safety and top-notch patient care have always been the twin guide stars of our field.
Hospitals and health systems have led the way in making bold changes to drive improvement in outcomes for decades, and we know that the dramatic improvements we have seen since the landmark 1999 Institute of Medicine report are a direct result of that leadership.

But hospitals and health systems are continually striving to raise the bar on patient safety. As innovative medicines and technologies bring new hope to the patients and communities we serve, the hospital field is relentlessly assessing, reassessing and improving our approaches to maximize the safety of care.
To support and advance those efforts, the American Hospital Association recently launched a new Patient Safety Initiative that seeks to energize all the work already underway and reaffirm hospital and health system leadership and commitment to patient safety.
Through the initiative we seek to:
• Provide hospitals with tools and data to advance patient safety.
• Give hospitals a platform and resources to tell their improvement stories.
• Highlight and resource successful local innovations to national scale.
• Inform public policy discussions about the most effective policy steps to support, spread, and sustain safety improvement.
With significant input from patient safety leaders at hospitals and health systems and other groups, the
CEOinitiative will center on three foundational elements of patient safety improvement:
• Culture of Safety from board to bedside, fostering board and senior leadership strategies to continually support safer care delivery.
• Health Equity, which focuses on ensuring that all patients receive safe care regardless of their race/ethnicity, gender, preferred language, and health-related social needs.
• Workforce Safety, which focuses on helping ensure that health care’s most vital resource –the workforce – practices in a safe environment that supports workers’ physical and emotional well-being.
This hospital- and health system-driven initiative will help hospitals further their commitment to advancing their work on these three topics. As part of the initiative, we’re establishing new collaboratives that will share strategies and resources to support hospitals in addressing these three important areas.
At the same time, we are working closely with data partners to explore how to share more real-time, nationally aggregated insights into the continuous improvement in patient safety outcomes we are seeing across the country.
As our health care system continues to evolve, one thing remains steadfast for America’s hospitals and health systems: We are committed to providing patients with safe, high-quality, effective, equitable, and person-centered care.
Please visit our webpage (https://www.aha.org/ aha-patient-safety-initiative ) to learn more about these efforts and how to participate. We’ll continue to share tools that help build a culture of patient safety; best practices in care delivery and other critical safety topics; and strategies so that hospitals can learn from each other’s experiences in improving safety.
AHA Patient Safety Initiative
All hospitals and health systems strive to deliver safe, high-quality care to every patient they serve. The hospital field has led the way in making bold changes to drive improvement in outcomes for decades, and the dramatic improvements we have seen since the landmark 1999 Institute of Medicine report are a direct result of that leadership.
In recent years the unprecedented strain of battling COVID-19 and its aftershocks made it significantly more challenging for hospitals and health systems as they worked to advance safety and quality. The key to improving care is the field’s continuous collaboration and innovation to drive safety forward. That’s why the AHA launched a national initiative to reaffirm hospital and health system leadership and commitment to patient safety.
Goals of Initiative
Provide hospitals with tools and data to advance patient safety
Give hospitals a platform and resources to tell their improvement stories
Highlight and resource successful local innovations to national scale
Focus Areas For 2024
Foster a culture of safety from the board room to the bedside
Identify and address inequities in safety
What You Can Do
Inform public policy discussions about the most effective policy steps to support, spread and sustain safety improvement
Enhance workforce safety
Sign up your hospital or health system to participate in the initiative
Share your successful efforts with the AHA so that we can highlight and scale them nationally
Tell your own story to your community about how you are working to advance safety.
The Health Equity Journey – A Perspective
By Pamela Brown, RN, BSN, CPHQ, Vice President of Quality and Patient Safety, Arkansas Hospital AssociationThere is a strong, new emphasis on health equity in America. From federal regulatory agencies like the Centers for Medicare and Medicaid Services (CMS) to accrediting bodies like The Joint Commission to associations like the American Hospital Association and the American Medical Association to state-oriented groups like the Arkansas Hospital Association – health equity is taking a new position of importance and is affecting every health care professional and organization in the nation.
What motivated this push?
One painful lesson our nation learned during the COVID-19 pandemic: Severe inequities in access to and quality of health care exist in our country, and people who do not have access to quality care suffer with poorer health than those who enjoy ready access.
The realization that addressing health equity could have extremely positive effects on the nation’s overall health – and the economics of health care – is a significant catalyst.
The resulting new regulations, rules, expectations, and standards of practice are creating a real buzz in health care organizations, both nationally and in our state.
Health equity is an important component of health care, and it’s going to cause each of us to re-think our approaches to the delivery of health care. This is new territory, and we are all learning as we go.
The most important message I have to offer to the hospitals of Arkansas is that we are here – with you and for you. As you and your hospital teams pursue your health equity journey, we urge you to reach out to the AHA Quality Team for assistance.


The 2023-2024 LAMMICO Patient Safety Award and Grant topic is falls prevention. Learn more about this grant at lammico.com/grant. Applications are due May 31, 2024.

QUALITY AND PATIENT SAFETY
Bringing Health Care Quality Home to Arkansas: AHA’s 2024 Quality Advisory Council
By Pamela Brown, RN, BSN, CPHQBelieving that collaboration will improve Arkansas’s quality and patient safety movement, the Arkansas Hospital Association (AHA) has formed the AHA Quality Advisory Council to represent the voice of AHA member hospitals regarding hospital needs and challenges in the areas of patient safety and health care quality improvement.
The Quality Advisory Council is a multidisciplinary team of stakeholders representing AHA member


hospitals. Members are committed to patient safety and quality, supportive of collaboration, and involved in advancing the AHA’s quality and patient safety goals.
One important Council objective is to make recommendations to the AHA leadership regarding quality and patient and safety priorities in support of our mission: to safeguard hospitals’ operational effectiveness in advancing the health and well-being of their communities.
SCOPE AND RESPONSIBILITIES
The new AHA Quality Advisory Council includes 16 members representing six of the AHA’s seven regions. The Council's responsibilities include:
• Providing vision and strategic direction for quality improvement initiatives.
• Providing oversight and recommendations on patient safety and quality issues.
• Facilitating collaboration and the organizational sharing of best practices.
TJC's National Patient Safety Goals
The Joint Commission’s 2024 National Patient Safety Goals went into effect January 1, and they include eight major categories for hospitals’ focus in the current year.
Each year, the Joint Commission forms its National Patient Safety Goals after gathering information about emerging patient safety issues from widely recognized experts and health care stakeholders. The Joint Commission then tailors these goals to needs in the areas of ambulatory health care, assisted living community care, behavioral health care and human services, critical access hospital care, home care, hospital care, laboratory functions, nursing care center health care, and office-based surgical care.
Joint Commission goals often align with other national patient safety standards, and they are designed to promote effective patient safety interventions to improve health care quality and reduce harm.
The 2024 Joint Commission National Patient Safety Goals for Hospitals and Critical Access Hospitals include:
• Identify patients correctly. Use at least two ways to identify patients. For example, use the patient’s name and date of birth. This is done to make sure that each patient gets the correct medicine and treatment.
• Improve staff communication. Get important test results to the right staff person on time.
• Use medicines safely.
º Before a procedure, label medicines that are not labeled: for example, medicines in syringes, cups, and basins. Do this in the area where medicines and supplies are set up.
º Take extra care with patients who take medicines to thin their blood.
º Record and pass along correct information about a patient’s medicines. Find out what medicines the patient is taking. Compare those medicines
• Providing recommendations and/ or advisement on health policy, legislation, and regulations.
• Supporting the mission and vision of the Arkansas Hospital Association.
A PROMISING START
The Quality Advisory Council’s first meeting was held March 1.

Stephanie Welch, Executive Director of Quality at White River Medical Center, was elected Chair, and Kayla Beamon, Chief Nursing Officer at Arkansas Care Hospital of Jonesboro, was elected Chair-Elect. Melissa Reny, Quality Manager of Stone County Medical Center, was elected Secretary. Other members of the Council include:
Christy Whatley, Market Vice President of Quality and Professional Services, CHI St. Vincent Health; Amanda Novak, MD, Vice President of Quality and Safety, Baptist Health; Lavanda Gangluff, Director of Quality, Baptist Health; Thea Rosenbaum, MD, Chief Quality and Transformation Officer, UAMS; Sherry Clements, Director of Quality, Encompass Health Sherwood; Tammy Penka, Director of Quality, Baxter Health; Janice Pryor, Chief Quality Officer, Progressive Health of Helena REH; Karen Pettit, Director of Quality, Regulatory, and Risk Management, St. Bernards Medical Center; Stephanie Taylor, Associate
to new medicines given to the patient. Give the patient written information about the medicines they need to take. Tell the patient it is important to bring their up-to-date list of medicines every time they visit a doctor.
• Use alarms safely. Make improvements to ensure that alarms on medical equipment are heard and responded to on time.
• Prevent infection. Use the hand cleaning guidelines from the Centers for Disease Control and Prevention or the World Health Organization. Set goals for improving hand cleaning.
• Identify patient safety risks. Reduce the risk for suicide.
• Improve health care equity. Improving health care equity is a quality and patient safety priority. For example, health care disparities in the patient population are identified and a written plan describes ways to improve health care equity.
• Prevent mistakes in surgery.
º Make sure that the correct surgery is done on the correct patient and at the correct place on the patient’s body.
Administrator, NEA Baptist; Anthony Williams, MD, Vice President and Chief Quality Officer, Washington Regional; Donna Boehm, Chief Nursing Officer, North Arkansas Regional Medical Center; Erin Bolton, Director of Quality, Jefferson Regional; Dee Rogers, Director of Quality, Risk, and Compliance, Magnolia Regional Medical Center.
The group will develop an annual work plan based on what they determine to be the Council's priorities for 2024, and they will make recommendations to AHA to address these priorities. The group plans to meet bimonthly.
Pamela Brown, RN, BSN, CPHQ, is the is the Arkansas Hospital Association’s Vice President for Quality and Patient Safety.
º Mark the correct place on the patient’s body where the surgery is to be done.
º Pause before the surgery to make sure that a mistake is not being made.
More detailed information about The Joint Commission’s National Patient Safety Goals for 2024 can be found at https://www.jointcommission.org/ standards/national-patient-safety-goals/

The Growing Threat of Antimicrobial Resistance
By Nikki Wallace, MS, BSN, RNFor decades now, health care professionals –especially those involved with quality improvement and patient safety – have voiced concern about the over-prescribing of antibiotics and the subsequent development of resistance to these antibiotics.
Whether we call it antibiotic resistance or antimicrobial resistance (AMR), the result is the same: When antibiotics are over-prescribed, germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. As the Centers for Disease Control and Prevention (CDC) tell us, “Resistant infections can be difficult, and sometimes impossible, to treat.”
A PUBLIC HEALTH NIGHTMARE
AMR presents one of today’s most daunting threats to public health. New requirements for reporting antimicrobial use and resistance (AUR) data for the electronic health record reporting period went into effect January 1 of this year, with the hope of tracking AMR, gathering data regarding AUR, and using the resulting data to help inform improvement efforts.
AUR data are useful for identifying improvement opportunities and guiding antimicrobial stewardship activities at the local hospital level. The new reporting requirements include eligible hospitals and critical
access hospitals, and they include the submission of both antimicrobial use and antimicrobial resistance data.
PROVIDERS ARE KEY
Health care providers have, for several years, been identified as the key to preventing infections through the improvement of their antimicrobial prescribing practices. When these providers learn the patterns of resistance in their hospitals and communities, they can create needed changes in prescribing practices to make a real difference in reducing/ preventing antimicrobial resistance.
According to the CDC, providers are the front line in fighting AMR. Suggesting ways for providers to be alert and take action include:
• Be aware of infections and resistance patterns in your facility and community.

Antibiotic Stewardship in Arkansas
Buddy Newton, MD, FACP, FIDSA, Director of Antibiotic Stewardship at Washington Regional Medical Center in Fayetteville and Mandy Langston, PharmD, Pharmacy Director at Stone County Medical Center in Mountain View, presented information on their Antibiotic Stewardship Programs (ASP) at the Arkansas Hospital Association’s January Quality Forum.
Dr. Newton’s presentation focused on new reporting requirements and how Standardized
Antimicrobial Administration Ratio (SAAR) data can be used to identify and fill gaps in individual hospitals’ ASPs. [SAAR is a ratio comparing observed, or reported, antimicrobial use to the antimicrobial use predicted by a referent, or baseline, population.]
SAAR categories include:
• Broad Spectrum Hospital Organisms.
• MRSA.
• Broad Spectrum Community Organisms.
• Ensure you are notified by the lab immediately when antimicrobial-resistant pathogens are identified in your patients.
• Inform patients and families if they have an antimicrobial-resistant infection.
• Know when to report cases and submit resistant isolates to the health department to identify unusual resistance or treatment failures.
A GLOBAL THREAT
AMR is not just a challenge in the U.S. Globally, it has been identified as one of the top 10 global public health threats facing humanity.
The World Health Organization estimates that by 2050, more than 10 million deaths could occur annually due to AMR, and that AMR’s economic toll could, within the next six years, result in a global drop of GDP of at least $3.4 trillion annually (USD), pushing 24 million more people into extreme poverty.
WHY ANTIBIOTIC STEWARDSHIP MATTERS

As more and more microbes mutate and become resistant to antibiotics, decreasing antibiotic use (antibiotic stewardship) is a known weapon in improving patient safety and hospital care quality.
To remind ourselves of the importance of antibiotic stewardship, it’s good to remember that:
• It decreases antimicrobial resistance.
• It decreases the incidence of C. diff infections.
• It improves dosing in renal-impaired patients.
• It improves infection cure rates.
• It decreases mortality rates.
• It saves on hospital costs.
More information on the new CMS reporting objectives and measures is available at https://www. cms.gov/files/document/cy-2024-antimicrobial-useand-resistance-surveillance-specification-sheet.pdf
IMPROVING ARKANSAS’S PATIENT OUTCOMES
Arkansas hospitals have implemented measures to improve antibiotic stewardship for many years as they focus on improving patient outcomes.
The Arkansas Hospital Association Quality Team recently partnered with an acute care hospital and a critical access hospital for sharing best practices in a forum with their peers (see sidebar below).
The CDC recognizes the complex nature of variables that impact improving antibiotic stewardship, such as the type of facility addressing challenges, and has developed resources for a variety of health care settings.
The expertise of different types of facilities in Arkansas are appreciated as we realize that we all have the common goal of fighting antimicrobial resistance. The collaboration with peers to share expertise across the state and the conversations that surround this topic are important as we all seek to decrease this global threat.
For access to the recent AHA Quality Forum presentation on this topic, you may contact Nikki Wallace, nwallace@arkhospitals.org.
Nikki Wallace, MS, BSN, RN, is a Quality Specialist with the Arkansas Hospital Association.
• CDI.
• Narrow Spectrum Beta-lactams.
• Antifungals.
His presentation included tables outlining a way to quantify how antibiotic use reductions can realistically help a hospital meet its SAAR goals.
In short, he says, “Every day and every dose matters!”
Mandy Langston’s presentation demonstrated how to implement facility-specific guidelines at
a Critical Access Hospital. She included tips on how to implement CDC core elements in a small hospital, how to tailor national guidelines to rural patient populations, and how to develop and distribute education, adherence, and facilityspecific treatment guidelines. She also explained how pharmacy-driven interventions can help lower antibiotic use in the hospital setting, and how use of National Healthcare Safety Network (NHSN) data can assist hospitals in meeting their ABS improvement goals.
The New Kid in Town: Patient Experience Collaboration
By Cindy Crump, MBA-HM, BSN, RNWhen it comes to patient and family engagement (PFE) as a subset of health care quality and patient safety, a new focus is shining a light on the patient experience.
Patient Experience Collaboratives are now being scheduled in Arkansas at least twice yearly, and they are designed to heighten focus on how to best engage patient experience leaders and patient/family member advocates, bringing them together to help improve patient care from both the hospital’s and the patient’s perspectives.
Some topics of focus continue to be:
• Improving communication.
• Utilizing HCAHPS surveying and data.

• Developing performance Improvement projects.
• Building patient and family advisors into hospital operations, including widening the use of Patient
Saline Health System Starts Program
By DeAnn Thomas, Saline Memorial HospitalIn partnership with Evergreen Healthcare Partners, Saline Memorial Hospital launched StepOne Service, a program to help those battling addiction, on Monday, January 8.
As the first phase in the recovery process, StepOne Service is a hospital-based, acute withdrawal management service for adults who are in the impending or early stage of withdrawal from alcohol and/or opioids.
“During our bi-annual community needs assessments, addressing substance abuse disorder is nearly always identified as one of the most critical health care needs for this area,” says Saline Memorial Hospital CEO Michael Stewart.
“We have been working diligently to address this need and believe this is in the first step toward providing hope and support for those battling addiction.”
The process starts with the patient calling 501.288.9292 or visiting SalineMemorial.org/StepOne

and Family Advisory Councils and seating patient advisors dedicated to PFE on hospital governing boards.
• Addressing diversity, equity, and inclusion (DE&I) in all areas of the hospital [including how to expand diversity on Patient/ Family Advisory Council committees, using data to drive DE&I and health equity in patient care, hosting and/or collaborating on community events for diverse populations, using social drivers of health to focus outreach].

• Utilizing systems of award and recognition for staff that go above and beyond for patients and their families, i.e., the Daisy Awards, and to encourage patient safety, i.e., Good Catch Awards.
Arkansas’s Patient and Family Advisory Council continues to meet monthly, and this year it will put an emphasis on the Patient Experience Collaboratives. The AHA Quality Team and AHA Analytics are currently working on a platform for sharing and hosting all activities related to quality and patient safety, including PFE and the patient experience through the
Circle app. This will allow expansion of message board/ thread conversations, promote sharing of resources, alert people to upcoming events, allow sharing of best practices and experiences among peers, and improve real-time communication between all those dedicated to improving the patient experience.
To learn more about involvement with the Patient Experience Collaboratives, please contact me at ccrump@arkhospitals.org.
Cindy Crump, MBA-HM, BSN, RN is a Quality Specialist with the Arkansas Hospital Association’s Quality Team.
Aimed at Addressing Addiction
to request a pre-screening. If the patient meets the criteria, they will be scheduled for admission to the hospital’s medical-surgical unit.
“This service is not for everyone,” says Bryan Jensen, co-founder and CEO of Evergreen Healthcare partners. “Patients seeking this treatment must meet medical criteria, be in the early stages of withdrawal, and be properly motivated for their recovery.”
Once a patient is admitted, the hospitalists and nurses at Saline Memorial Hospital provide round-theclock medical care using protocol-specific medications to reduce the severity of withdrawal symptoms. Treatment lasts on average about three days for opioid withdrawal and about five days for alcohol withdrawal.
“From admission to discharge, we have a clinical care team specially trained to work with withdrawal patients,” Stewart says. “Once we address their medical needs, these patients can focus on the next steps of their recovery.”
The clinical team will work with patients on a longterm care plan to guide the patient from their discharge from the hospital to their continuing treatment at the next, appropriate facility or program. The care team will keep working with the patient for up to six months after discharge.
“After withdrawal treatment, it is important for patients to continue on with some form of addiction treatment to learn coping strategies for maintaining sustained sobriety,” Jensen says. “StepOne Service will assist patients in finding the next appropriate treatment center so they can get the life skills and relapse prevention training they need.”
QUALITY AND PATIENT SAFETY
UAMS Inpatient Sepsis Protocol Will be
Arkansas will be represented in a Best Practices Poster Presentation at the upcoming CMS Quality Conference in Baltimore, Maryland, April 8-10!
The University of Arkansas for Medical Sciences (UAMS), in collaboration with Healthcare Improvement Quality Contractor TMF Health Quality Institute and the Arkansas Hospital Association, will have its work in reducing the 30-day sepsis mortality rate showcased through a poster presentation outlining UAMS’s new clinical pathway standard.
The hospital achieved a 25% relative improvement
hospital’s sepsis mortality rate. This was in the early part of 2021, when most meetings were still virtual due to COVID-19 pandemic precautions.
RH: As the only Level One Trauma Center in the state, UAMS receives the sickest of the sick from hospitals around the state, and as a result we have a much higher acuity level than other academic teaching hospitals. We did analyses to look for areas where process improvements might help improve patient outcomes, and we determined that patients with sepsis presented such an opportunity. We constantly work to improve protocols with the goal of achieving better outcomes for our patients.
We wanted to make certain everyone understood the signs of sepsis and the ways to keep everyone on the care team informed and ready to act if sepsis was suspected or identified.
rate (RIR) in sepsis mortality and a 51% RIR for post-operative sepsis after developing an inpatient sepsis pathway, then implementing the pathway and collecting data over a nearly two-year period October 2021 through August 2023.
Arkansas Hospitals talked with UAMS Quality Director Robbie Hemmer and Process Improvement Analyst Sarah Merlos about the two-year study documenting the improvement effort and the dramatic improvement in sepsis mortality achieved.
AH: How did this sepsis improvement project come about?
SM: Our UAMS Mortality Reduction Team identified sepsis as an area of opportunity for improvement, and we began meeting to formulate a plan to reduce our
SM: We brought a multidisciplinary group together to work on the new inpatient sepsis protocol. Utilizing a successful sepsis identification protocol already in place in our Emergency Department, we set out to develop a protocol that could be used in the inpatient setting system-wide to identify and improve the treatment of sepsis.
AH: What groups were a part of this multidisciplinary team?
SM: Our Process Improvement group, the Quality team, Critical Care physicians and the MedicalSurgical nursing team were involved. Another group involved was the Clinical Documentation team, which could help us create electronic health record (EHR) code to help in the identification of possible sepsis. Dr. Aaron Wenger, Director of the Integrated Medicine Service Line, was the champion for this effort.
RH: Sepsis was certainly being identified and treated on our inpatient units, but we did not have a standard protocol set for use throughout the hospital system. That was the purpose of this multidisciplinary team: to create a sepsis protocol that would be aided by EHR alerts and develop treatment bundles that would be applied consistently on our inpatient floors.
SM: The result of this work, which took approximately six months, was to set standards
QUALITY AND PATIENT SAFETY
CONTINUED FROM PREVIOUS PAGE
the one- and three-hour bundles, when combined with ongoing sepsis education, has generated these drastic improvements. These methods are now being modeled with other hospital acquired infections, such as central line-associated blood stream Infections, across the hospital system. Data on the hospital’s current sepsis case rate is reported daily in staff meetings, physician grand rounds, and unit-specific safety huddles.
AH: It has been two years since the Inpatient Sepsis Pathway went live. What are your thoughts about the protocol’s success and the recognition this program will receive at the upcoming CMS Quality Conference?
SM: It has been amazing to be a part of this system-wide effort. It is a rarity to implement such a house-wide protocol, and it’s really gratifying to be a part of this effort! Dr. Wenger, the project’s sponsor, says, “I am very proud of the work UAMS has done to improve our sepsis outcomes. I really appreciate the contributions from our quality department, our nursing staff and leadership, and the many physicians who have contributed to this progress. Sepsis is one of the most common causes of death for hospitalized patients, so it seemed like a natural place for us to focus when looking to improve our overall mortality scores. I definitely think the two have gone hand in hand. Optimum sepsis care requires the input of many different members of our team, and I think the progress we have made through this initiative can serve, really already is serving, as a template for us to make the same kind of progress on other critical quality metrics. Communication is the foundation of safe, effective hospital care, and I’m really happy to be part of a team that emphasizes that.”
RH: We’re all really proud of this work, and we’re honored to have Arkansas’s quality efforts presented at the national conference. We appreciate TMF’s heavy lifting in the creation of the actual poster. But more than the recognition, it’s a pride we all feel in the way we are caring for our patients in Arkansas. What we are doing with the Inpatient Sepsis Pathway can be replicated by others and will increase the health of patients across the state of Arkansas.
Patient Care and
By Carvin Brown, Executive Director, Our Blood InstituteBlood transfusion is an indispensable component of health care. It contributes to saving millions of lives each year in both routine and emergency situations and dramatically improves the life expectancy and quality of life for patients with a variety of acute and chronic conditions.
Community blood centers like Our Blood Institute (OBI) play a pivotal role in ensuring a steady and reliable supply of blood to local hospital partners for medical treatments, surgeries, and emergency situations. OBI is the nonprofit blood supplier for patients at more than 200 hospitals, medical facilities, and air ambulances across Arkansas, Oklahoma, and Texas. OBI’s blood supply is drawn solely from generous residents across all three states.
Despite ongoing efforts to encourage voluntary blood donations, blood donation patterns often show seasonal variations. During holidays, vacations, or extreme weather conditions, the number of voluntary donors tends to decrease. This fluctuation can strain available blood reserves, prompting blood centers like OBI to appeal for donations to ensure a stable supply throughout the year.

Community Blood Centers
ALLEVIATING DIPS IN INVENTORY
OBI had robust blood collections through the fall of 2023 until Christmas, but saw a post-holiday inventory dip, followed by extreme weather during the first two weeks of January. Prevailing winter weather continued to significantly disrupt blood collections, so an official blood emergency appeal was launched on January 16. At the start of the appeal, inventory was lower than desired for some types of blood, in particular O negative, which is the type essential to help trauma patients, premature babies, and cancer patients.
Thankfully, OBI was able to meet all patient and hospital needs throughout the month, and the emergency appeal ended on January 29. OBI saw tremendous support for those two weeks of the appeal – from the media, from the community, and especially from valued hospital partners.

When OBI asked for extra help to rebuild the blood supply, local hospitals stepped up and showed outstanding support. These partners helped lift OBI out of blood inventory difficulties and restore the customary security and reliability to local transfusion care.
HOSPITALS AS PARTNERS
A sincere thank you goes out to all OBI hospital partners for their very visible modeling of dedication to excellence and commitment to patient care. OBI recognizes that partner hospitals share motivation to keep blood flowing to the patients and caregivers relying upon it, and the OBI team is now hard at work to guarantee that appeals result in a sustained blood supply for these partners.
However, there is no substitute for close collaboration to wisely steward resources and take
best care of patients. To maintain the blood supply and meet the medical needs of the community without interruption, OBI humbly requests readers of this magazine to take part in hospital blood drives and encourage colleagues and family members of patients to do the same.
While the post-holiday January inventory emergency has waned, other holidays and spring break vacations are already with us. Please educate employees on the importance of blood donation, and remind people you know how to donate consistently, regardless of the time of year. Advocating for blood donations is not a sign of failure, but an initiative-taking measure to ensure a robust and responsive blood supply system for all.
Community participation is paramount in meeting the constant demand for blood, especially during emergencies and unforeseen situations. By understanding the need, hospital partners can contribute to the well-being of their communities and continue being an essential part of a lifesaving endeavor.
QUALITY AND PATIENT SAFETY
AAHQ Invites Your Participation!
By Cindy HarrisThe Arkansas Association for Healthcare Quality (AAHQ) is a professional organization affiliated with the Arkansas Hospital Association. Its members are made up of health care quality professionals serving in many capacities across diverse medical settings. AAHQ members serve Arkansas Hospital Association member organizations and their associated service lines.
AAHQ members are active in many disciplines of the hospital quality movement. These include nurses, physicians, pharmacists, and other allied professionals who are active in quality and performance improvement, risk management, patient safety, case management, data analysis, infection control, and health information.
The organization has been active since its inception in 1982. Its leadership team includes hospital quality professionals who not only serve as group officers, but also as directors of teams including groups for Protocol, Communications, Professional Development, Membership Services, Finance, and External Relations.
As a member, you will join the group in working to emphasize the significant contribution of quality in the health care arena, increase
the diversity of the profession, and enhance the leadership skills of tomorrow’s role models. AAHQ’s mission is to engage health care quality professionals to improve care and patient safety in Arkansas. Its vision is to be recognized as the vital resource for Arkansas health care quality, patient safety, and leadership professionals.
Membership in AAHQ offers numerous additional benefits, including:
• Statewide networking with other Quality professionals.
• The ability to earn continuing education hours in the areas of Nursing and CPHQ (Certified Professional in Healthcare Quality).
• Access to the organization’s newsletter, which focuses on Quality, Patient Safety, and other professional matters.
• Access to professional development and leadership opportunities.
• Planned office hours and journal club sessions new in 2024.
For more information or to join AAHQ, you may call Cindy Harris at 501-224-7878, email charris@ arkhospitals.org, or visit the AAHQ website at https://www.arkahq.org/ membership/
2024 AAHQ LEADERSHIP TEAM
PRESIDENT
Teresa Jeffus UAMS
PRESIDENT-ELECT
Devin Terry UAMS
PAST PRESIDENT
Chelsey Davidson
Conway Regional Health System
SECRETARY
Kristi Toblesky
American Data Network
PROTOCOL TEAM
Erin Bolton
Jefferson Regional
PROFESSIONAL DEVELOPMENT/ EXTERNAL RELATIONS TEAMS
Justin Villines
ADH-SHARE
Christi Whatley
St. Vincent Health
COMMUNICATIONS TEAM
Joel Anderson
Jefferson Regional
FINANCE TEAM
Trey McCorkindale UAMS
MEMBERSHIP SERVICES TEAM
Tim Copeland
Unity Health
AT-LARGE
Amanda Wyatt Hutto TMF
AT-LARGE
Shanda Guenther
SCP Health

APIC: Hand in Glove with Quality and Patient Safety
By Nikki Wallace, MH, BSN, RNMany Arkansas health care professionals working in the areas of quality and patient safety belong to organizations that specifically support their work.
HospitalToolkit:Resource
The Association for Professionals in Infection Control and Epidemiology (APIC) is one such organization, and as a longtime member and board member of APIC’s Arkansas chapter, I’d like to share some of its goals and how it helps me in my career as a nurse devoted to improving hospital care quality.
MISSION AND VISION
The national APIC organizational vision is: A safer world through the prevention of infection. This vision correlates directly with the Arkansas Hospital Association’s (AHA) Quality Team goal of working closely with member hospital care teams to prevent patient harm, save lives, and reduce health care costs without compromising on quality.
APIC Arkansas’s mission is to be a knowledgeable resource for the people of Arkansas. Our goal is to promote excellence in the principles and practice of infection prevention in health care facilities and the community through education, communication, networking, and public awareness.
We believe that infection prevention is key to meeting quality and patient safety goals no matter the focus: national, state, and local level, and
even the local hospital level. Infection prevention impacts every aspect of health care, from day-today practices to responding to global emergencies.
APIC supports infection preventionists (IPs) as they lead efforts to:
• Prevent health care-associated infections.
• Conduct surveillance activities.
• Promote interdisciplinary collaboration.
• Provide education.
• Develop policies and procedures based on evidence-based practices.
• Coordinate with related groups in the areas of public health, data reporting and analysis, and real-time observation of IP practices.
SHARING EXPERTISE
Sharing expertise locally, nationally, and internationally is a priority for APIC Arkansas. Teams of IPs, including Arkansas IPs from Mercy Hospital Booneville, Mercy Hospital Waldron, and Mercy Hospital Northwest Arkansas, recently published articles in the American Journal of Infection Control. These are titled “Development of Infection Prevention Program Standards for Critical Access Hospitals” and “Implementation of an Electronic Hand Hygiene Monitoring System: Learnings on How to Maximize the Investment.”
I’m proud that the AHA has, for several years, partnered with the national APIC team to support our Arkansas IPs. We are continuing this practice in 2024, seeking to provide the IP community with needed resources as we all work to improve health care quality and dedicate ourselves to the safety of Arkansas patients.
Infection prevention impacts every aspect of health care, from day-to-day practices to responding to global emergencies.
A Passion for Quality and Safety
By Nancy RobertsonDouglas Ross, MD, President of CHI St. Vincent Hot Springs, embodies the unusual combination of physician and hospital administrator. Now in his fifth year as CEO of the hospital where he has served since completing his medical residency program more than 20 years ago, he says that his role as administrator increases the opportunity to pursue clinical excellence.
He first knew he wanted to become a physician when he was just a boy. His mother, a nurse, inspired his career choice at an incredibly young age, and he has never looked back.
Born in Michigan, Dr. Ross moved to Arkansas when in the 9th grade and says he is proud to call Arkansas home.
He took a path less-traveled in his undergraduate pre-med training, earning his Bachelor of Chemical Engineering degree from the University of Arkansas at Fayetteville. “I took this non-traditional pre-med track because I loved math and science,” he says. “Engineers are taught analytical ways to solve problems. This process-oriented approach lends itself naturally to the practice of medicine, and I believe the foundation in chemical engineering has served me well throughout my career.”
Ross attended the University of Arkansas for Medical Sciences Medical School, and he completed his residency in Emergency Medicine at the University of South Carolina.
“When I finished residency, I headed straight back to Arkansas where, in 2003, I joined [what was then known as] Mercy Hospital Hot Springs as an emergency room physician,” he says. “I thought I would be an ER doc for life. I loved the variety of conditions we saw and treated – and the varying age ranges of our patients.
“Work as an ER physician gave me the opportunity to learn about people, their motivations, what makes them tick. It taught me how to work with them to achieve their goals,” he says. It also brought about the skill and ability to be flexible in his approach to work and life.
 Douglas Ross, MD
Douglas Ross, MD
LEADERSHIP CALLS
“My first taste of leadership came when I served as Chief Resident during my days in South Carolina,” he says. “Later, while serving as an ER physician at what had evolved to be CHI St. Vincent Hot Springs, I was asked to serve as Medical Director for the ER Department. That role was about half clinical and half administrative, and one of my major assigned projects was to help our hospital make the transition from paper records to the EPIC electronic medical record system. Today, that may seem like a natural progression of records-keeping, but during the days when the U.S. was making this transition, the physical scale and mental adjustments of the changeover were huge.
“We knew, at the time, that the culture change involved in the switch to EMR was a big deal,” he says, “but only now are we seeing the full scope of benefits in the areas of quality, patient safety, and revenue cycle.”
Leaders of the St. Vincent System identified Ross’s leadership capabilities as he led his hospital
through this transition. Likewise, his work in guiding this project also gave him the realization that leading through change was a gift he could offer.
In 2018, the CHI St. Vincent System named him Chief Medical Officer over all of the system’s hospitals in Arkansas, and in 2019 he was offered the role of President of CHI St. Vincent Hot Springs. “I find this role very fulfilling,” he says. “It offers me a chance not only to interact with our team of professionals here at the hospital but also to engage with the public and community as we seek to provide the best of patient care to the area communities we serve.”
A PASSION FOR QUALITY AND PATIENT SAFETY
“I am incredibly passionate about quality and patient safety,” he says. “COVID-19 brought a new perspective to our efforts in those areas. With the passing of the public health emergency that emerged with COVID-19, we have added knowledge gained during the pandemic to our pursuit of zero harm.”
Zero harm is a health care quality aspirational goal. It can be achieved through thorough care team buy-in of an organization’s culture of safety, and can potentially lead to zero complications of care, zero patient safety events, zero health care-acquired conditions, zero falls, etc. The Joint Commission also identifies it as creating a culture of zero harm to employees and visitors – and zero lost opportunities to provide exemplary care.
Ross says he is pleased to see health care moving toward full transparency in reporting of patient safety events. “We cannot keep these types of events secret,” he says. “How can we learn from these events if we do not bring





them into the open? We must communicate quickly and clearly when these incidents occur, opening up to patients, their families, and our staff so that we can identify paths to improvement and the prevention of future patient harm. We must develop a rigor around these principles, and we must be transparent so that, together, we can learn and progress on our journey to zero harm.”
CHI St. Vincent Hot Springs’s recent acceptance into the Forum for Shared Governance is evidence of the hospital’s dedication to improving quality and patient safety. The Forum is an international organization of 41 hospitals that operate under a shared-governance model of management, highlighting nurse autonomy and empowerment as methods of improving patient outcomes.

“Working within the Forum’s guidelines, we engage our doctors, nurses, and co-workers in designing processes for maximizing patient safety,” Ross says. “It’s a collaborative model that thoroughly involves our frontline coworkers in developing the structure of care. When our staff feel like they’re integral to the process, they become, and stay more, engaged. Actually, our method marries engagement with solid process improvements. We’re immensely proud of our progress, and again, this is all a part of our journey to zero harm.”
The hospital has also earned the Leapfrog Group’s highest rating in Patient Safety for the past three years running. This rating reflects the hospital’s ability to protect patients and their families from errors, injuries, accidents, and infection.
ENGAGEMENT IN ACTION
Hospitals have long been working to reduce the number of hospital-acquired infections, or HAIs. The list of HAIs includes central lineassociated blood stream infections (CLABSI), surgical site infections, catheter-associated urinary tract infections (CAUTI), and ventilatorassociated pneumonia, among others.
The caregivers at CHI St. Vincent Hot Springs, working on their journey to zero harm – at first considered an impossibility by many on the medical staff – have employed safety bundles and evidence-based practices to develop safer modes of venous access and have significantly reduced the rate of CLABSIs. “We have gone, in recent years, from a rate of about one infection per month to achieving 700+ days without a CLABSI,” Ross says. “This is due solely to our co-workers’ buy-in and their belief in, engagement with, and employment of the safety bundles and processes that, together, we put into place.”
And gains are being made in other areas, as well. “Whether we’re working to reduce HAIs, falls, or other harms, the process is all the same,” he says. “When we are dedicated to and engaged with the process, we are able to record some of the highest quality and patient safety scores in the state.”
“Once we have designed our process, the next step is to remain vigilant and to keep every co-worker engaged,” he continues. “At our hospital, we hold facility-wide safety huddles each morning where we celebrate successes on our various units, emphasize our commitment to a culture of safety and to the patient experience, and give individual recognition to those co-workers who catch harms before they can happen.
“At the unit level, where the real implementation occurs, we hold safety huddles at every shift change and try to take a 360 degree look at the safety processes involving each of our patients. This is all a part of the engagement that remains vital for maintaining our safety record, and at the heart of it is dedication to providing the safest care possible for our patients and their families.”
NEW PROGRAMS
INCREASE ACCESS TO CARE
Ross is particularly excited about two new programs his hospital has developed to increase access to care for patients previously
living in care deserts or in situations where access was difficult.
One of these programs is working with a grant from the federal government to increase maternal and neonatal care in 10 communities served by CHI St. Vincent Hot Springs.
“We’re one of four hospital systems in the U.S. to work within this grant,” he explains, “and our goal is improving maternal and fetal outcomes in rural Arkansas. Again, utilizing evidence-based pre-natal care methods, we hope to greatly improve the health outcomes of mothers and their babies by bringing easy access to care directly to them in and around the communities of De Queen, Nashville, Murfreesboro, Glenwood, Mt. Ida, Fordyce, Bearden, Hampton, Amity, and Magnolia. Our providers travel to these communities and see patients there, in specially designed clinical settings, one or two days a week. Our goal is to provide convenient local access to prenatal and postnatal care that previously our patients might have had to drive hours to achieve.”
The other program involves working with the Morehouse University School of Medicine’s Internal Medicine Residency Program to bring a diverse and culturally sensitive group of medical residents to central and southwest Arkansas. “Our goal is, frankly, to work with Morehouse to bring more culturally diverse medical residents to our state with the hope that they’ll decide to stay and practice medicine here as their careers unfold,” Ross says. “We believe this collaboration will bring a more diverse group of Internal Medicine residents to the state, and it will improve our provider base for the future.”
ARKANSAS HOSPITAL ASSOCIATION BOARD WORK
Ross is one of the newer members of the Arkansas Hospital Association’s Board of Directors, and as such, sees his work as helping to promote the spread of best practices and the journey to zero harm throughout the state. “I want to learn from other hospital leaders, and I believe our work on the Board can facilitate the sharing of best practices,” he says. “The journey to zero harm is for all Arkansans, and our work on the Board can help promote this journey for our member hospitals. We believe in working with health systems locally to keep access to care as convenient as possible. We realize that developing effective strategies around access to care is going to help all Arkansans in the future. Keeping quality and patient safety as a shared passion will have an incredible impact on health care in our state.”
Leadership Profile Q/A with Douglas Ross, MD
What’s on your music playlist?
Classic Rock: Pink Floyd and Led Zeppelin, to name a couple.
Do you have a favorite movie? Why do you like it?
“Hacksaw Ridge.” A true story, the courage and faith of Desmond Doss on that ridge in WWII was unbelievable.
Who is someone you greatly admire, and why?
I admire my wife, Jenny. She is the kindest and most genuine person I have ever met. She has been a fantastic mother to our kids, and she is my best friend.
What would you be doing if you weren’t in health care?
That’s easy! I would own a farm. I love tending to animals and growing things. It is very peaceful for me.
What do you like to do in your down time?
Anything outside. I love to hike, golf, and spend time on the lake.
What are you reading? (non-work-related material)
The Bible. I spend time in God’s word every day. It is my strength and anchor.

A Brief History of the 340B Drug Program Dispute in Arkansas, and Why it Matters
By Jodiane Tritt and Tina Creel, Arkansas Hospital AssociationIn a big win for Arkansas hospitals, federally qualified health centers, pharmacies, and patients, on Tuesday, March 12, 2024, the United States Court of Appeals for the Eighth Circuit affirmed the ruling of the United States District Court for the Eastern District of Arkansas: Arkansas Act 1103, “The 340B Nondiscrimination Act,” is not pre-empted by Section 340B of the Public Health Service Act or the Federal Food, Drug, and Cosmetic Act’s Risk Evaluation and Mitigation Strategies Program.
For more than 30 years, the 340B Drug Pricing Program, administered by the Health Resources and Services Administration (HRSA), has provided financial help to hospitals serving vulnerable communities. The program benefits are designed to be used not only to reduce the price of outpatient pharmaceuticals for patients, but also to allow hospitals (and certain other health care organizations) to stretch scarce resources to expand health services to the patients and communities they serve.
The program gets its name because Section 340B of the Public Health Service Act requires pharmaceutical manufacturers participating in Medicare and Medicaid to sell outpatient drugs at discounted prices to certain health care organizations – known in the federal statute as “covered entities” – that care for many uninsured and low-income patients.
These covered entities include HRSAsupported health centers and several types of hospitals, including Critical Access Hospitals, Sole Community Hospitals, Children’s Hospitals, Rural Referral Centers, and public and nonprofit Disproportionate Share Hospitals that serve lowincome and indigent populations.
In Arkansas, 31 of our 75 counties have no 340B hospitals. Also, most of our 340B hospitals are
prohibited from owning a retail pharmacy permit under Arkansas law. In order to capture benefits of the program, covered entities must rely on extensive partnerships with community pharmacies to dispense 340B drugs to our patients.
[There are four hospitals (Jefferson Regional, Baptist Hospital-Little Rock, UAMS, and Arkansas Children’s Hospital in Little Rock) that were grandfathered into the Arkansas state law prohibiting not-for-profit and governmental hospitals from attaining a retail pharmacy permit.] This, of course, makes contract pharmacies even more important to the provision of 340B drugs for covered entities in Arkansas.
A BRIEF LEGAL HISTORY
Act 1103 of 2021
In 2020, drug manufacturers began implementing distribution policies that limited or prohibited covered entities from contracting with outside pharmacies for the dispensation of 340B drugs to patients. Some manufacturers sent notice to hospitals that only one contract pharmacy would be permitted to receive and dispense 340B drugs. Some required that the covered entity provide proprietary information to the pharmaceutical manufacturer before the manufacturer would allow contract pharmacies to receive and dispense 340B drugs. These manufacturer-imposed restrictions –and others – were designed to reduce the benefits of the 340B program to patients and covered entities, and to keep drug manufacturer profits high.
Complying with these restrictions caused covered entities dependent on contract pharmacies to become unable to serve patients in need.
Led by strong members of the Arkansas Legislature, two associations representing covered entities – the Arkansas Hospital Association
and the Community Health Centers of Arkansas – collaborated with the Arkansas Pharmacists Association (representing contract pharmacies) to pass Arkansas Act 1103 of 2021, the 340B Nondiscrimination Act.
In short, Act 1103 of 2021 prohibits manufacturers from putting restrictions on covered entities’ use of contract pharmacies.
Act 1103 provides, among other things, that a pharmaceutical manufacturer may not prohibit a pharmacy from contracting or participating with an entity (authorized to participate in 340B drug pricing) by denying access to drugs manufactured by the pharmaceutical manufacturer.
Act 1103 also provides that pharmaceutical manufacturers shall not deny or prohibit 340B drug pricing for an Arkansas-based community pharmacy that receives drugs purchased under a 340B drug pricing arrangement with an entity authorized to participate in 340B drug pricing.
There are a few other important provisions, too.
• A payor, or payor’s intermediary, or a PBM, MUST:
º Inform a patient that the patient is not required to use mail-order; have the patient sign a waiver allowing a mail-order if one is used.
º Allow a patient the freedom to use any pharmacy or provider the patient chooses.
• A payor, or payor’s intermediary, or a PBM, must NOT:
º Transfer the 340B benefit from covered entities to other parties (like PBMs, private insurers, or managed care organizations).
º Refuse to cover 340B drugs or prohibit pharmacies in the 340B program from participating in an insurer’s network.
º Lower reimbursement or impose separate terms upon pharmacies based on participation in the 340B program.
º Require a pharmacy to reverse, resubmit, or clarify a 340B drugpricing claim after the initial







adjudication unless these actions are in the normal course of pharmacy business and not related to the 340B program.
º Require a billing modifier to indicate that the drug or claim is a 340B claim unless the claim is billed to the fee-for-service Medicaid program.
º Modify a patient’s copayment on the basis of a pharmacy’s participation in the 340B program.
The Act gives enforcement authority to the Arkansas Insurance Department.
P h RMA BALKS
The day after the law became effective, Pharmaceutical Research and Manufacturers of America (PhRMA) filed a complaint to the Arkansas Insurance Department asserting that the Insurance Department did not have authority to enforce the law. The Insurance Department then followed its administrative procedure and set up and conducted a hearing for the complaint. Following the hearing, PhRMA filed a complaint in federal court.
PhRMA asserted two main claims – both of which are constitutional challenges:
That Act 1103 is preempted by federal law (stating that the state did not have jurisdiction, as 340B is a federal program).
That the law violates the Dormant Commerce Clause, which gives Congress broad authority to regulate interstate commerce and restricts states from impairing it.
One of our hospitals – Piggott Community Hospital – and the Community Health Center Association (which represents Federally Qualified Health Centers) joined the Arkansas Insurance Commissioner in the case.
Judge Billy Roy Wilson ruled in Arkansas’s favor at the district level. PhRMA appealed to the 8th Circuit Court of Appeals.
The American Hospital Association, 340B Health, and our Arkansas Hospital Association joined together in an amicus brief filed at the appellate level. Our message: Arkansas’s 340B Nondiscrimination Act does not conflict with federal law, but rather it supports Congress’s goal in enacting the 340B program. The Arkansas law prohibits discriminatory policies against 340B providers in the state, including drug company policies that restrict provider access to 340B discounts through community and specialty pharmacy partners. Our brief defends Act 1103 against a constitutional challenge brought by PhRMA.
Oral arguments were held on September 20, 2023.
CONTINUING OUR FIGHT TO UPHOLD THE LAW
Instead of following Act 1103, pharmaceutical manufacturers have continued to restrict distribution of 340B drugs, which is causing major financial hardship on Arkansas covered entities and on patients. Covered entities are filing complaints with the Arkansas Insurance Department, consistent with the Act. The drug manufacturers are requesting that the Arkansas Insurance Department enter into regulatory settlement agreements with them instead of enforcing the law and fining the manufacturers for their injurious behavior.
In early February 2024, the Arkansas Hospital Association, in a letter to the Arkansas Insurance Department, requested that every provision of Act 1103 of 2021 be upheld as individual pharmacy manufacturers seek to thwart the distribution of 340B drugs by contract pharmacies.
THE EIGHTH CIRCUIT AGREES WITH US
On March 12, Judge Michael J. Melloy wrote in the Court’s opinion: “Pharmacy has traditionally been regulated at the state level, and we must assume that absent a strong showing that Congress intended pre-emption, state statutes that impact health and welfare are not pre-empted. (Pharm. Care Mgmt. Ass’n, 18 F.4th at 972.) For these reasons, we conclude that in enacting Section 340B, Congress did not intend to pre-empt the field.”
Further, the opinion states, “Act 1103 does not create an obstacle for pharmaceutical manufacturers to comply with 340B, rather it does the opposite: Act 1103 assists in fulfilling the purpose of 340B. In arguing otherwise, PhRMA presents no evidence of an obstacle. Instead, PhRMA raises the same arguments it raised with field pre-emption. We reject these same arguments again here.”
NEXT STEPS
We will continue to urge the Department to enforce the law as it is written as we stand with Arkansas hospitals and other covered entities and – most importantly – the patients of Arkansas.
JODIANE TRITT, JD, serves as Executive Vice President of the Arkansas Hospital Association. Tina Creel is the association’s Vice President of Member Services and President of AHA Services, Inc.
Now Is the Time to Protect 340B
The 340B drug pricing program is critical to ensuring patients with low incomes and those living in rural areas can access the care they need. The growing number of drug companies restricting access to 340B pricing through community and specialty pharmacies undermines safety-net hospitals and harms their ability to care for patients in need. Patients are losing access to needed services, switching their prescriptions to less-effective medications, and experiencing worsened health outcomes.
Now is the time to protect 340B because…
340B Protects Underserved and Rural Patients
Patients have better access to comprehensive health care and support services because of 340B. This is especially true for patients with low incomes, members of historically underserved communities, and those who are uninsured, underinsured, or reliant on public health programs that underpay for care.
340B Provides Crucial Resources to Tackle Challenges
Hospitals are treating unprecedented levels of patient illness amid high inflation, increased labor costs, and other factors. These challenges have hit especially hard for 340B hospitals, which have extremely tight operating margins. 340B resources help hospitals maintain needed care in this environment.
340B Is a Lifeline for Rural Hospitals
340B enables rural community hospitals and critical access hospitals in remote areas of the nation to continue serving their communities. These rural hospitals are more likely to report that the savings they receive through participation in 340B help keep their doors open.
340B Supports Patient Care Without Burdening Taxpayers
Increased access to health care through 340B comes from drug company profits, not American taxpayers. This critical contribution to the health care safety net enables 340B hospitals to reach more people in need, especially patients in public health programs
340B Helps Restrain Drug Price Increases
Congress designed 340B to require deeper discounts when drug companies repeatedly raise prices faster than the inflation rate. When allowed to work as intended, these penalties influence drugmakers to restrain price hikes on both 340B and non-340B drugs, producing billions of dollars of cost savings.
340B Strengthens Local Communities
340B savings enable investments in a health care safety net for communities that are under increasing economic stress. In every state and nearly every congressional district, 340B hospitals maintain health services and support that make their communities better places to live and work.
At a time when American families and safety-net hospitals are facing critical economic and health access barriers, 340B continues to provide crucial resources for overcoming these problems.

The Negative Impact of Medical Credit Cards and Patient Interest Charges
From AblePay
The Consumer Financial Protection Bureau (CFPB), U.S. Department of Health and Human Services (HHS), and U.S. Department of Treasury (Treasury) launched an inquiry into high-cost specialty financial products, such as medical credit cards and installment loans, that are pushed on patients to pay for routine medical care, and which drive up health care costs and medical debt.
The request for information builds on CFPB research on medical payment products and medical billing and collections, in addition to other actions by the CFPB and federal agencies to relieve the burden of medical debt and collections practices.
The three agencies seek information about the prevalence of these products, patients’ experiences with them, and health care providers’ incentives to offer these highcost products to patients, which may include avoiding the insurance claims process and financial assistance programs. The CFPB will use public input as it considers ways to address patient harm caused by these specialty financial products.
Learn more about CFPB research at consumerfinance.gov, searching for the article entitled:
CFPB, U.S. Department of Health and Human Services, and U.S. Department of Treasury Launch Inquiry into Costly Credit Cards and Loans Pushed on Patients for Health Care Costs | Consumer Financial

ABLEPAY – AHA SERVICES’ ENDORSED BUSINESS PARTNER

AHA Services’ endorsed vendor, AblePay, is the “antithesis” to the concerns highlighted above. AblePay (based out of Allentown, Pennsylvania) is addressing the affordability gap by helping patients with savings on out-of-pocket expenses (up to 13%), savings over time, or extended terms with 0% interest, while also providing advocacy services if a patient has a question on a bill.
Their solution is rapidly expanding across the country by helping both providers and their patients. AblePay is significantly changing the financial landscape for providers and their patients, and we are excited to share case study results from a Pennsylvania-based system that utilizes the AblePay program.
EPHRAIM MCDOWELL HEALTH CASE STUDY: IMPROVING REVENUES AND PATIENT RELATIONSHIPS WITH ABLEPAY

Ephraim McDowell Health serves patients in six counties in Central Kentucky through three hospitals (two of which are critical access hospitals) and 48 outpatient centers. They employ more than 1,700 people and have $282M in annual net revenue.
With revenues declining and the cost of collecting patient out-ofpocket responsibility steadily rising, Ephraim McDowell Health was in search of a way to improve their patient post-insurance collections.
Ephraim McDowell selected AblePay’s unique process to increase revenue and decrease the cost of collections while also enhancing the experience for their patients.
By assuming all payment risks, AblePay not only eliminated the unpredictability of patient payments, but also all of the associated costs. This positively impacted the health system while patients benefited from the savings, flexible payment options, a convenient payment portal, and billing advocacy provided by AblePay.
The results of the Ephraim case study with AblePay included:
• 106% increase in collection rate compared to their historical collection rate.
• 48% increase in revenue per patient.
• 46.2% of patients that enrolled in AblePay paid zero on prior bills.
• The number of days to collect decreased from 107 days to 14 days for AblePay members.





LEHIGH VALLEY HEALTH NETWORK CASE STUDY: CHANGING PATIENT PAYMENT BEHAVIOR WITH ABLEPAY
The Lehigh Valley Health Network (LVHN) serves the citizens of the greater Lehigh Valley, and the system includes 13 hospitals, 320+ outpatient centers, 20,000+ employees, and $3.2B in annual revenue. LVHN chose AblePay’s unique program to increase its revenue on balance after insurance and decrease their cost of collections, while also enhancing the experience for their patients in the communities they serve.
Faced with considerable rising patient out-of-pocket costs, LVHN embarked on a new strategy to efficiently collect patient balances. The objective of this approach was to enhance revenue, while at the same time reducing collection expenses.
In pursuit of these objectives, LVHN decided to embrace the cutting-edge solution provided by AblePay. By assuming full responsibility for payment risks, AblePay not only eliminated the uncertainties of collections but also removed all related expenses.



Patients benefited from cost savings, flexible payment choices, a user-friendly payment portal, and the billing advocacy services offered by AblePay.
The results of the LVHN case study with AblePay included:
• 47.3% increase in collection rate compared to LVHN’s historical collection rate.
• 43% increase in revenue per patient.
• 16.7% increase in new revenue for AblePay patients at LVHN facilities.
• A decrease in days to collect from 97 days to 14 days for AblePay members.
• A Net Promoter Score (NPS) of 89 for LVHN patients that joined AblePay.
You can view a recent Becker’s Webinar with both AblePay and the Lehigh Valley Health Network: https://vimeo.com/825193077
To find out more on how AblePay can work for your organization, please contact Tina Creel at 501.224.7878, tcreel@arkhospitals.org, or Ryan Werling at ryan.werling@ablepayhealth.com.
Hospitals: The Intersection Between Health Care and Hospitality
By Kay KendallAccording to the U.S. Bureau of Labor Statistics, the average employee turnover rate across all industries is between 12-15%, with the average across hospitals significantly higher at roughly 23%.
Yet some hospitality businesses, such as quick service restaurants, routinely experience 150% annual staff turnover. And another sector of the hospitality field, the hotel and motel industry, reports a turnover rate of nearly 74% even after the industry occupancy rate has rebounded since the dire days of the COVID-19 pandemic.
Recent studies examine the reasons behind such high turnover rates among hospitality employees. These studies may offer insights to health care leaders desperately seeking to boost employee retention rates in their hospitals.
SIGNALS FROM THE HOSPITALITY SECTOR
A white paper recently published by Scout Logic [ https://www.scoutlogicscreening.com/blog/ what-causesemployee-turnover-in-hospitality/ ] posits the top nine reasons why hospitality
employees are leaving their jobs:
• The seasonal nature of the industry, accompanied by frequent layoffs and mass hires.
• Low wages.
• Toxic workplace culture.
• Inability to work remotely.
• Long hours.
• Inflexible schedules.
• Poor communication.
• “Landing pad” syndrome, where people can hop from one temporary job to another.
NO OPPORTUNITY FOR GROWTH
Some of these causes of turnover in the hospitality industry sound similar to wellestablished challenges experienced in the health care environment, don’t they?
Using the hospitality field’s “Top Nine” may help hospital leaders in the quest for retention. Not all may apply to health care’s challenges, but the areas of culture, scheduling, and communication are certainly within your control as a leader.

RE-THINKING SOLUTIONS
Culture – What’s the culture like in your organization? Do you reinforce a patientcentered focus? Do you “round” on your employees, as well as your patients, to get to know them as people? Do you ensure that they have the training, tools, and supplies they need to do their jobs well? Do you actively remove real or perceived barriers to performing work efficiently? Do you provide real-time recognition? Do you promote teamwork? Do you empower your employees in such a way that they take intelligent risks in the interests of your patients? If a mistake is made, do you use that as a teachable moment rather than as a mechanism to reprimand and shame?
Long hours and inflexible schedules both lead to burnout. They can also severely limit an employee’s ability to take advantage of educational opportunities that could lead to personal development and career growth. Health care employees’ schedules can make work-life balance challenging, whether for parents of young children, caregivers of older adults, or employees managing family members who have disabilities. Does your organization explore every opportunity to organize scheduling with employees’ needs as a part of the equation?
Poor communication can create an expensive flaw in organizations, but it offers opportunities for surprisingly inexpensive fixes. Many best practices can be learned from health care and hospitality organizations that expanded and innovated communication techniques during the pandemic.
EXEMPLARY CUSTOMER SERVICE: HOSPITALITY AND HOSPITALS
To date, the Ritz-Carlton is the only hotel system to win the prestigious Malcolm Baldrige National Quality Award, and it did so not only once, but twice. Horst Schulze, the group’s former cofounder and president, and other senior executives readily share their techniques.
One of the foundational elements of providing the Ritz-Carlton’s legendary customer service is building respect for



COACH'S PLAYBOOK
their employees, reflected in the credo: “Ladies and gentlemen serving ladies and gentlemen.” The Ritz presents a model of service that health care organizations have the opportunity to exemplify in every interaction with patients and with one another.
And the Ritz-Carlton, like many health care organizations, incorporates daily morning huddles into practice in each of its hotels. This practice allows every employee worldwide across the corporation to hear the same message detailing the previous day’s occupancy and revenue, daily projections, and a discussion highlighting one of the corporation’s 12 service standards.

CUSTOMER SERVICE STANDARDS: WHAT IF?
I rarely hear about customer service standards in the health care industry, and even more rarely do I see them executed with such discipline and reinforcement as at the Ritz-Carlton. What are these standards, and how might they become a part of your hospital’s daily practice? As you read this list of values, ask yourself how it might equate with your organization’s practices.
Service Values: I Am Proud To Be Ritz-Carlton
1. I build strong relationships and create RitzCarlton guests for life.
2. I am always responsive to the expressed and unexpressed wishes and needs of our guests.
3. I am empowered to create unique, memorable, and personal experiences for our guests.
4. I understand my role in achieving the Key Success Factors, embracing Community Footprints and creating The Ritz-Carlton Mystique.
5. I continuously seek opportunities to innovate and improve the Ritz-Carlton experience.
6. I own and immediately resolve guest problems.

7. I create a work environment of teamwork and lateral service so that the needs of our guests and each other are met.
8. I have the opportunity to continuously learn and grow.
9. I am involved in the planning of the work that affects me.
10. I am proud of my professional appearance, language, and behavior.
11. I protect the privacy and security of our guests, my fellow employees, and the company’s confidential information and assets.
12.I am responsible for uncompromising levels of cleanliness and creating a safe and accident-free environment.
It seems that with thoughtful creativity, these Ritz-Carlton values could be adapted and adopted by most health care organizations. This would require education, reinforcement, and role modeling, but the yield in retention and patient experience could be astounding.
ARE YOU UP TO THE CHALLENGE?
As a hospital leader, you have an advantage over the hospitality industry. Your commitment to communicating your organization’s mission, vision, and values to every employee is likely already in place. By doing so, you urge your employees to commit to a common purpose. Many studies on employee engagement reveal what a powerful driver of engagement that connection is.
Most health care employees went into their profession with a desire to make a difference in the lives of others. It’s time for us to rekindle that flame, reinforce our respect for employees and encourage their respect for one another and the patients they serve, and recognize their contributions. This is a critical goal for all senior leaders in health care, and your hospital’s quality and patient safety, employee retention, and patient experience metrics could all improve in the balance when you weave hospitality’s customer service focus into your organization’s fabric of serving.
The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 24 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.
Maternal Mortality and Morbidity in Arkansas in a Post-Covid World
Shaneca Smith, BSN, RN, CNOR(E)There’s no escaping the barrage of articles – and even primetime TV medical dramas – focused on illuminating the U.S. crisis in maternal mortality and morbidity.
Though already a challenge pre-COVID, maternal health care in the U.S. experienced unprecedented challenges with the rise of COVID-19, causing even more devastating maternal outcomes.
The Centers for Disease Control and Prevention (CDC) reports that maternal mortality rose significantly from 2020-21 for all racial and ethnic groups. However, Black women continue to experience remarkably higher maternal mortality and morbidity rates than white and Hispanic women. In 2021, there were approximately 1,205 maternalrelated deaths in the U.S., and the maternal mortality rate rose from 23.8 deaths per 100,000 live births in 2020 to 32.9 deaths per 100,000 live births in 2021.
MATERNITY CARE DESERTS
The aftermath of COVID also produced an increasing number of maternity care deserts as hospital maternity units began diverting services or closing. In 2020, Arkansas offered pregnant patients access to 39 delivery facilities. As of January 2024, that number has dropped to 35.
SOME POSITIVE ADVANCEMENTS
Despite lingering gaps in Arkansans’ access to maternal health care, some notable advancements are occurring. In 2022, Arkansas became the 48 th state to join the Alliance for Innovation on Maternal Health (AIM). This designation positions Arkansas to partner with other states in developing and implementing maternal safety bundles.
Groups such as AFMC’s Medicaid Quality Improvement (MQI) team and the UAMS HighRisk Pregnancy Program continue to promote the implementation of safety bundles and recognition of perinatal warning signs.

In late 2022, Arkansas also established its first Perinatal Quality Collaborative, focusing on reducing primary cesarean deliveries. This five-year project is funded by a $1.2 million federal funding award and is a joint project of the University of Arkansas for Medical Sciences and the Arkansas Department of Health. Funding was granted by the CDC Division of Reproductive Health, part of the U.S. Department of Health and Human Services.
For the past five years, Arkansas has been reviewing and working toward prevention of maternal deaths through its Maternal Mortality Review Committee (AMMRC), established through legislation and developed with guidance from the CDC.
The AMMRC is a group of professionals who work together to improve maternal outcomes by examining factors that affect maternal morbidity and mortality. Through extensive research, the AMMRC verified 35 pregnancy-related deaths per
100,000 live births in Arkansas from 2018-2020, with potentially 92% being preventable.
To combat preventable deaths, the AMMRC makes recommendations for the prevention of future maternal deaths in Arkansas. Its December 2023 Legislative Report executive summary contains a brief overview and detailed recommendations. The recommendations are designed to address the diverse needs within a health care system. This includes, but is not limited to, government officials, providers, community leaders, patients, and families.
We all have a part in reviewing these recommendations and assisting in their application. The 2023 Report can be found here: https://www.healthy.arkansas.gov
ADDRESSING MATERNAL DISPARITIES
Lastly, increasing maternal disparities have fostered a necessity to empower communities, support grassroots efforts, and dignify the efforts of partners like the Ujima Maternity Network and The Arkansas Birthing Project. These organizations establish impactful connections and have proven strategies to meet our birthing communities and their families where they are and produce viable changes.
Though COVID exacerbated maternal hardships and generated several new barriers, it ushered in promising efforts toward reducing maternal mortality. Now is the time to act on those endeavors and change Arkansas’s narrative from tragedy to triumph.
SHANECA SMITH, BSN, RN, CNOR(E) serves as Manager, Quality at AFMC. A certified registered nurse for more than 16 years, she works in the area of quality improvement and is a co-facilitator of process improvement measures working with health care organizations and community-based programming.
REFERENCES
AFMC (2023). Maternal Mortality and PostDelivery Warning Signs. https://medicaid.afmc. org/medicaid-quality-improvement/maternalmortality
Alliance for Innovation of Maternal Health
https://saferbirth.org/
Arkansas Maternal Mortality Review Committee (2023). https://www.healthy.arkansas.gov/ programs-services/topics/arkansas-maternalmortality-review-committee
Arkansas Perinatal Quality Collaborative (2023). https://news.uams.edu/2023/08/30/uamsled-arkansas-perinatal-quality-collaborativelaunches-with-support-of-33-hospitals-takesaim-at-reducing-c-sections/#:~:text=The%20 ARPQC%20will%20equip%20 health,especially%20in%20low%2Drisk%20 pregnancies
Centers for Disease Control and Prevention, National Center for Health Statistics (NCHS), National Vital Statistics System, “Maternal deaths and mortality rates: Each state, the District of Columbia, United States, 2018-2021”
Hoyert D. Centers for Disease Control and Prevention, National Center for Health Statistics. Maternal mortality in the United States, 2021. Mar 2023. https://www.cdc.gov/ nchs/data/hestat/maternal-mortality/2021/ maternal-mortality-rates-2021.pdf
The Arkansas Birthing Project (2023). https:// www.arkansasbirthingproject.org/ Ujima Maternity Network (2023). https://www. ujimamaternitynetwork.org/
US Government Accountability Office. Maternal health outcomes worsened, and disparities persisted during the pandemic. Oct 2022. https://www.gao.gov/assets/gao-23105871.pdf
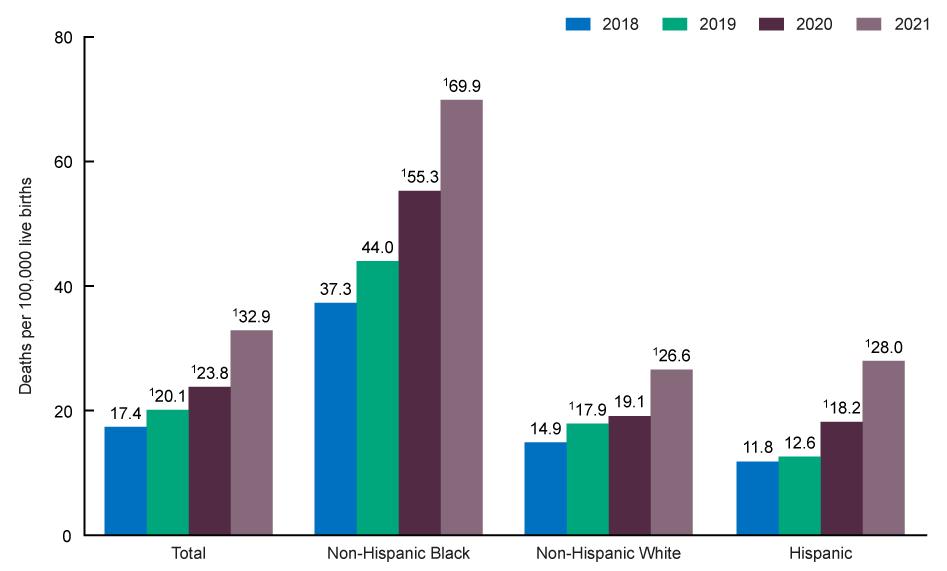
Addressing Maternal Mortality at the Grassroots Level
Two organizations in Arkansas are specifically addressing the disparities in maternal health care experienced by Black mothers-to-be. These organizations help with education, mentoring, caregiving, and monitoring during pregnancy and up to one year following a baby’s birth.
The Ujima Maternity Network addresses the Black maternal and infant health crisis in the state of Arkansas experienced by expectant Black mothers and their families. Established in 2018, the Ujima Maternity Network brings together Black birth workers and maternal advocates who are dedicated to making positive impacts within the birthing community to help ensure Black mothers survive and thrive during their pregnancy, birth, and postpartum experiences with advocacy, support, and safety. Its birthing community includes skilled birth workers, including Black midwives, doulas, and lactation consultants located throughout the state of Arkansas. Its goal is to aid in the reduction of Black maternal and infant mortality in the state of Arkansas. (ujimamaternitynetwork.org)
The Arkansas Birthing Project is a communitybased organization serving pregnant women and their families who need health care and social support to improve the chances of their babies being born healthy. The Project provides support to communities and organizations in Arkansas who would like to begin their own local Birthing Projects. This volunteer effort is designed to encourage better birth outcomes by providing practical support to women during pregnancy and for one year after the birth of the baby. The program allows women who understand and are able to function within their perspective communities to serve as a link between women who need services and those who provide them. (arkansasbirthingproject.org)

What Do IPs Do?
IPs promote a culture of safety and impact the health of patients, workers, staff, and community members. Their advocacy and work extend throughout the organization and the community.
HEALTHCARE QUALITY
• Performance improvement
• Incorporating evidence-based research into practice
HEALTHCAREASSOCIATED INFECTIONS
• Hand hygiene
• Medical devices
• Surgical procedures
• Antimicrobial stewardship
• Diagnostic stewardship
• Standard and transmission-based precautions
EPIDEMIOLOGY
• Surveillance and reporting
• Technology and innovation
LEADERSHIP
• Change agents for process improvement
• Subject matter experts promoting evidencebased guidelines and science
SAFETY ADVOCACY
Promote a culture of safety for patients, staff, workers, and community members
EMERGENCY MANAGEMENT
• Response to new and emerging pathogens
• Pandemic preparedness
• Outbreak response
• Environmental disaster response
EDUCATION
• Team members
• Patients
• Community
ENVIRONMENT OF CARE
• Air and water quality
• Construction safety
• Cleaning, disinfection, sterilization
• Product evaluation


Take the pain out of in-person, hybrid, and virtual events
Take the pain out of in-person, hybrid, and virtual events
At AFMC, we make events a breeze. From meetings and workshops to professional medical symposiums, we have the expertise to ensure your events run smoothly. Let us take care of the registration, marketing, A/V, and technical support so you can focus on what matters most — hosting a top-notch event.
AFMC is your event solution.
Let AFMC put our decades of experience to work for you. Whether you need support for virtual meetings, hybrid conferences, or other live-streaming options, AFMC is your trusted source.
Take the first step toward pain-free event planning. Visit afmc.org/VirtualEvents to find out more.
LOOKING
FORWARD TO THE NEXT 75 YEARS OF
building places for healing


For the past 75 years, we’ve completed projects of all types and sizes for healthcare facilities — delivering high quality work to fulfill our client’s vision and needs.
UAMS trusted Nabholz to construct the Orthopaedic and Spine Hospital, a new ground-up facility for orthopaedic and spine patients. The project utilized the fast-track construction delivery method and we delivered the 156,000-square-foot facility in 23 months. Now Arkansas is properly equipped to treat orthopaedic and spine patients with the highest quality of care.
LOOKING FORWARD SINCE 1949
1.877.NABHOLZ | nabholz.com
