COMMUNITY

in taking care of the legal, so you can take care of the patients.
We've been serving the legal needs of the Arkansas healthcare industry for more than 120 years.
• Medical Malpractice Defense
• Healthcare Transactions & Employment Agreements
• Government Relations & Administrative Proceedings
• Licensing, Privileging & Peer Review
• Labor & Employment Concerns
• HIPAA Privacy & Security
• Stark I and II & Anti-Kickback Statutes
• Medicare/Medicaid & Insurance Reimbursement
• Telehealth & Remote Healthcare
• Long-Term Care & Skilled-Nursing Defense
• Defense of Claims Against Pharmacies & Pharmacists
Your Arkansas Healthcare Law Team WE BELIEVE





COMMUNITY INVOLVEMENT

ARKANSAS
HOSPITALS
Arkansas
To advertise, please contact Brooke Wallace
Ashley Warren, Editor in Chief
Nancy Robertson, Senior Editor & Contributing Writer
Katie Hassell, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-Elect
Michelle Krause, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Rogers / At-Large
Chris Barber, Jonesboro
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
James Magee, Piggott
Guy Patteson, Jonesboro
Gary Paxson, Batesville
Eric Pianalto, Rogers
Douglas Ross, Hot Springs
Neta Sue Stamps, Berryville
Brian Thomas, Pine Bluff
EXECUTIVE TEAM
Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO



•
•
•
•
•



Ripple Effects
Summertime trips to the lake are a big part of my life, but the visits have new meaning when looking through the eyes of my children. Splash right in and enjoy the cool water on a hot, hot day. Try to catch a dragonfly as it glides over the water. Drop a rock into a pool, and watch the ripples spread.
In the world of health care, we often talk about “ripple effects.” Every hospital affects its community in a multitude of ways, rippling from inside the hospital, outward to the community, and beyond.
There are community health “ripples” that start within the hospital walls, as patients and families receive nurturing care, and then move outside the hospital, as wellness programs engage the people living in the communities we serve and help them look at personal health through new eyes.
There are economic “ripples”: A hospital pays its workers, who spend their wages in the community. Groceries are purchased, mortgages are paid, car payments are delivered – then the grocery stores, car dealerships, and banks and lending institutions in turn invest back into their communities.
And, of course, hospitals make their own purchases, expanding the ripple effect. Capital spending on new construction, the purchase of new equipment and supplies, stocking of the hospital’s kitchen and pharmacy and gift shop – the ripples keep expanding outward.
At the Arkansas Hospital Association, we see these ripples from another perspective. We not only see the cultural and economic impacts hospitals have on their communities, we see the collective positive impact hospitals have on the overall health of Arkansans. And, as an association, we advocate for the hospitals of Arkansas, seeking to increase their viability and extend their impact even further.

This edition of Arkansas Hospitals takes a look at a number of innovative community outreach programs hospitals are creating across the state. Hospitals large and small are meeting the needs of various segments of the population, one patient and family at a time. Our hope is that your own hospital can take these inventive solutions and adapt them to your unique community’s needs.
In this edition, we also present The AHA Guide to Hospital Statistics, our annual look at the data side of hospitals’ impact on their communities and on our state. When you combine Hospital Statistics with our newly released 2024 Economic Impact Report , you get a remarkable view of how foundational hospitals are to Arkansas’s health, well-being, economic viability, and cultural growth.
As summertime outdoor temperatures heat up and you, yourself, consider jumping into a pool or lake to cool life’s stresses, think about the ripples in the water. Let them remind you that your work, every day, has positive effects that ripple outward and have impacts greater than you may ever see or know.

Ashley Warren Editor in Chief

JULY
July 10
2024 Summer Calendar
Provision of Care in a Safe Environment:
Update on Patient Rights and Suicide Prevention Webinar
July 11
Arkansas Hospital Auxiliary Association (AHAA) meeting
AHA Headquarters
July 16
340B Quarterly Meeting
Virtual Event
July 17
What Physicians Want
Hosted by Jackson Physician Search
AHASI Webinar
July 17
AHA Healthcare
Cybersecurity Alliance
Virtual Event
July 18
Quality Forum
Shared Governance: Empowering the Front Lines
Virtual event
AUGUST
August 1-2
AHA Board Retreat
Location TBD

August 14-16
2024 Mid-South CAH & Rural Hospital Conference
The Peabody Memphis, TN
August 21
AHA Healthcare Cybersecurity Alliance Virtual Event
August 22 Quality Forum Virtual Event
SEPTEMBER
September 12
Arkansas Hospital Auxiliary Association (AHAA) meeting AHA Headquarters
Employees of AHA member hospitals can now log in to www.arkhospitals.org and register for events online.
September 13
AHA Board Meeting Virtual Event
September 18
AHA Healthcare Cybersecurity Alliance Virtual event
September 19
2024 Arkansas Hospital Association Workers’ Comp Self-Insured Trust (AHAWCSIT) Annual Education Conference
AHA Classroom
September 19
Quality Forum
Virtual Event
September 20
Arkansas Association for Healthcare Engineering (AAHE) Fall Conference
Location TBD

LEADERSHIP WORKSHOP
(4.5 Continuing Education Hours Applied for)
Patrick Houlahan, Founder and CEO of Strategic Leadership Consultants, LLC, Former United States Marine Corps “Top Gun” Fighter Pilot
Learn how to apply TOPGUN pilot tools and techniques when leading your own highperformance teams.
KEYNOTE ADDRESS

HOT TOPICS:
• Health Equity Belongs to Everybody

October 30-31
Little Rock Marriott • 3 Statehouse Plaza
Mike Massimino, Professor of Mechanical Engineering, Columbia University; Senior Advisor for Space Programs at the Intrepid Sea, Air & Space Museum; Former NASA Astronaut
How to remember that we are making the world a better place through our work.

• When Good Isn’t Good Enough: How Unconscious Bias Harms Patients…Despite Our Good Intentions
• Consumer Behavior in a World of Memes, GIFs, and Trends
• It’s All in the Delivery (Communication Training)
• Leading Like Taylor Swift
Approval is pending for continuing education credits for ACHE, Legal, Nursing, Quality, and Risk Management. Brochure and Registration
Mike Massimino
Patrick Houlahan
HOSPITAL NEWSMAKERS
Mercy NWA recently sponsored the inaugural Wellness Festival at Crystal Bridges and The Momentary, joining community partners in celebrating the connection between art, nature, and well-being. The engagement featured insightful dialogues, including Dr. Sonal Bhakta's conversation with Olivia Walton and filmmaker Tonya Lewis Lee. Senior leaders and local physicians participated in a thought-provoking discussion on AI's role in advancing whole health. And if that wasn't enough, musical artist Jewel provided comments and a performance that attendees found moving. We look forward to continuing our commitment to community well-being.
Senior leaders and area physicians participated in Mercy NWA's inaugural Wellness Festival. From left, Kerry Bommarito, Vice President of Enterprise Data Science; Sonal Bhakta, Chief Medical Officer, Mercy NW Arkansas Communities; Joe Kelly, Executive Vice President and Business Development Officer; Dr. John Mohart, President, Community Operations; Dr. Megan Busch, Mercy Family Medicine Physician; Byron Yount, Chief Data and AI Officer.

Fulton County Hospital is now operating under its new name, Baxter Health Fulton County Hospital. Full integration of the hospital into the Baxter Health system will take place in January of next year.

A
CHI St. Vincent Hot Springs, together with Hot Springs National Park, is hosting “Hike to Health,” a new seasonal wellness opportunity for the public. The free program will allow the public to learn more about Hot Springs and its national parks, while exercising and engaging with CHI St. Vincent health professionals. The first event was held this spring, and other events are scheduled through the fall.
Robert Rupp, MHA, is the new CEO of Forrest City Medical Cent er. He has served hospitals in Texas, Oklahoma, Louisiana, and Arkansas, including Harris Hospital, Helena Regional Medical Center, and the Medical Center of South Arkansas.
St. Bernards Medical Center recently celebrated a ribbon cutting for its new $7 million surgery department expansion, opening three new surgical suites and shell space for a fourth.
roll-out of the hospital's new name included t-shirts for staff members reading "Baxter Health Fulton County Hospital."
Jefferson Regional has opened its new rehabilitation and behavioral health specialty hospital in White Hall. The 87,000 square foot facility houses 76 beds and is unique in the state in this combination of patient services.
Specialists at Arkansas Children’s Research Institute and the University of Arkansas for Medical Sciences will use a $3.2 million award from the National Institutes of Health to lay the foundation for a new treatment that could transform quality of life for children with lymphatic malformations. This research is supported by the National Heart, Lung and Blood Institute of the National Institutes of Health.
Arkansas Children's Hospital’s (ACH) nationally ranked Cancer and Blood Disorders program has earned full accreditation from the Foundation for the Accreditation of Cellular Therapy (FACT) for performing bone marrow transplants and cellular therapy. The full accreditation recognizes the hospital's dedication to providing high-quality care and adhering to rigorous standards. By meeting the stringent requirements set forth by FACT, ACH has demonstrated its ability to deliver comprehensive and cutting-edge treatment options to pediatric patients.
Rustin Morse, MD, MM M, has been named Senior Vice President and Chief Administrator of Arkansas Children’s Northwest . He most recently served as Chief Medical Officer of Nationwide Children’s Hospital in Columbus, Ohio.
Baptist Healt h, in support of the University of Arkansas for Medical Sciences' (UAMS) Milk Bank, has opened a milk depot at its medical center in Fort Smith. The Fort Smith Baptist Health Milk Depot is a designated space for individuals to donate milk, which will be sent to the UAMS Milk Bank for screening, pasteurization, and nutritional analysis. After processing, milk will be sent, according to need, to hospitals throughout Arkansas.
Casey Willis, MBA, RHIT, CPPS, is the new CEO for Saint Mary’s Regional Health System. She previously served as Chief Operating Officer at National Park Medical Center and Associate Administrator at North Alabama Medical Center. She earned her master’s degree in business administration from Martin Methodist College and her undergraduate degree in management and human relations from Trevecca Nazarene University.
The Washington Regional Environmental Services Department received special recognition during Patient Experience Week. Pictured below, the EVS team members clean and disinfect approximately 750,000 square feet each day to ensure that the hospital is ready for patients, visitors, and staff.

AHA Awards Call for Nominations:
The AHA is now accepting nominations for the 2024 AHA Awards, which will honor outstanding and innovative CEOs, trustees, community advocates, nurses, physicians, and bright, young executives! The Arkansas Hospital Association’s 2024 Annual Meeting Awards Luncheon – on Thursday, October 31, at the Little Rock Marriott – will feature presentations of the A. Allen Weintraub Memorial Award; Distinguished Service Award; C. E. Melville Young Administrator of the Year Award, recognized by the ACHE of Arkansas (formerly Arkansas Health Executives Forum); and the Diamond Awards, cosponsored by the Arkansas Society for Healthcare Marketing and Public Relations. In addition, the American College of Healthcare Executives (ACHE) Regent’s Awards will be presented during the Awards Luncheon this year. To learn more and to submit nominations, you may scan the QR code at right.

Washington Regional EVS Team
COMMUNITY INVOLVEMENT: Ideas from Arkansas Hospitals
In Arkansas and across the U.S., patients and communities rely on the wide range of critical health care services that only hospitals and health systems can provide, including 24/7 emergency and other higher-acuity care. Hospitals also work with their community partners to develop and deploy tailored programs that advance health and wellness in every part of the state.
Arkansas’s hospitals and health care workers continually stand strong for their communities, and they play a vital role in our society to keep communities healthy.
We hope you will enjoy reading about the many community-oriented projects Arkansas hospitals have created, and perhaps you will be able to adopt or adapt some of these ideas for use in your own community setting.
The Arkansas Hospital Association sincerely thanks all of the hospitals across the state who are sharing their community outreach ideas in these pages.
If you have Community Outreach projects your hospital would like to share, please contact Ashley Warren, awarren@arkhospitals.org.
RESOURCES FOR TELLING YOUR HOSPITAL STORY
If you would like help in developing presentations that tell your hospital story, please visit aha.org/tellingthehospitalstory , where you’ll find a toolkit from the American Hospital Association that includes case studies, presentation slides, social media ideas, photos and logos you can adapt to your needs, and more.



Scan this QR Code to get the resources.
Community Outreach’s Mission Serves Those in Need, Where They Need It
By Matt Dishongh
Arkansans face many barriers to health care for a wide variety of reasons. These include, among others, ready access to care, income challenges, transportation challenges, and access to wellness education.
Baptist Health's statewide Community Outreach team is passionate about helping people remove these barriers in pursuit of living their most healthy lives. Baptist Health exists to provide quality patient-centered services, promote and protect the voluntary not-for-profit health care system, provide quality health education, and respond to the changing health needs of the residents of Arkansas with Christian compassion and personal concern.
The Community Outreach team delivers on this mission outside the hospital walls in a wide variety of ways. Targeted outreach groups include people who are underserved, underinsured, under-resourced, or groups with focused needs, such as low-income expectant and new parents, seniors who are not receiving the care they need, and the growing unsheltered population.
This outreach team meets these underserved populations where they are, identifies resources and services particular to their needs, and either delivers those services or directs them to others who can help.
The team's goal is to serve more Arkansans, improve the health of Arkansas communities, partner with other community organizations, and expand Baptist Health’s healing ministry.
The team originates programs for children and youth, builds community coalitions, provides community education, sponsors support groups, offers community wellness centers, and is a source for free health screenings and health fairs, school initiatives, partnerships, and in-kind donations with which Community Outreach has been involved over many years.
“Baptist Health’s mission is to care for all individuals in the community who need our assistance,” says Teresa Conner, System Director of Community Outreach. “Whether they need our programs only one time or many times, [caring for those who need help] is important to our team.”
COMMUNITY WELLNESS CENTERS
Among its many duties, the Community Outreach team offers non-emergent health care services through its community wellness centers and mobile

Community education dietitian Samantha Stadter teaches participants about healthy eating in this cooking class for adults.
UAMS Serving Patients in Their Communities
By Kate Franks
When many Arkansans think of the University of Arkansas for Medical Sciences (UAMS), the image that comes to mind is of a clinic near their home, a community event, or a mobile health unit serving their hometown rather than the hospital and clinics in the heart of Little Rock.
“We created UAMS Health in October 2019, and since then UAMS has grown to become a health system that extends our clinical programs beyond the physical walls in Little Rock to patients across Arkansas,” says Michelle Krause, MD, MPH, Senior Vice Chancellor for UAMS Health and Chief Executive Officer for UAMS Medical Center. “We have had regional program sites across Arkansas for decades, but the UAMS Health clinical umbrella allows us to dramatically increase patient care across the state.
“The COVID pandemic highlighted the need for our support in rural communities, and as soon as vaccines became available, we sent teams out to offer support to small towns across Arkansas. The relationships we formed through these efforts established a foundation for more outreach programs, ranging from breast cancer screenings, prenatal classes and diabetes education to culinary medicine events and the creation of the Institute for Community Health Innovation earlier this year. We look forward to partnering with the Institute’s community-based research efforts to deploy community-driven programs that will improve both quality of life and life expectancy in medically underserved regions of Arkansas.”
UAMS MAMMOVAN AND MOBILE HEALTH
The Mammovan is one of the oldest examples of UAMS’s community outreach, traveling around the state since early 2010. More than 17,000 Arkansas women have been screened at these mobile mammography units in the past 14 years. The three-room, handicap-accessible unit is outfitted with advanced 3D digital mammography equipment and staffed by certified mammography technologists.
“Many of the women we serve are uninsured or underinsured, and most of them don’t have easy access to mammography services,” says Gwendolyn Bryant-Smith, MD, director of the Breast Center at the UAMS Winthrop P. Rockefeller Cancer Institute and Chief of Breast Imaging. “A Mammovan visit to their community is often their only opportunity to have this important screening for breast cancer. Many women now know about the Mammovan and watch for us to come to their community for annual screenings.”

(From left) Graduates of the April 2024 UAMS Community Health Worker Training and Apprenticeship Program Abby Solis-Linares, Ursula Galvez, Lizbeth Hoyle, Angela DiDomenico and Manuel Mercado. Graduates not pictured are Guada Campos and Jasmine Miller.
UAMS Health currently has four mobile health units that offer group and individual prenatal care to improve maternal health outcomes in areas of the state designated as rural health deserts. CenteringPregnancy®, used by UAMS Health to deliver group prenatal care, includes group learning and sharing along with regular checkups with a health care provider. Topics covered in the 10 group sessions include nutrition during pregnancy, mental health, infant safety, newborn care, and breastfeeding.
“Our mobile health clinics give us the ability to meet the patient where they are – literally,” says Kelly Conroy, Senior Director for Community Programs in the UAMS Institute for Community Health Innovation. “The ability to deliver prenatal care in some of the most rural and medically underserved areas of Arkansas helps improve the health outcomes of pregnant women, babies, and families by bringing care and support to where it is most needed.”
COMMUNITY HE ALTH WORKER TRAINING
Almost 90 participants from 21 counties have enrolled in the UAMS Institute for Community Health Innovation’s statewide Community Health Worker Training and Apprenticeship Program, which provides 80 hours of core training to new and experienced community health workers to give them tools to better support local communities.

The UAMS Institute for Community Health Innovation’s mobile health units travel anywhere in the state, wherever care is needed most. Free services include blood pressure, cholesterol, and diabetes screenings, colorectal cancer screening kits, COVID-19 and flu vaccinations, health insurance enrollment, referrals to prenatal care, and connection to ongoing medical care.
Seven new Community Health Workers graduated from the institute’s one-year training program in April. They each completed an additional 80 hours of supplemental training, 2,000 hours of on-the-job training, and demonstrated skills in 21 core competencies, such as providing culturally appropriate health education, connecting individuals to resources, and expanding health literacy.
During the pandemic, the institute trained and deployed more than 150 Community Health Workers to 40 counties across Arkansas, and more than 350 Community Health Workers statewide are affiliated with the institution. UAMS was also instrumental in advocating for "Community Health Worker" to become an officially recognized state title, which Arkansas added in July 2023.
“Here at UAMS-East in HelenaWest Helena, we are fortunate to
have a Community Health Worker and Nurse Educator who help recruit pediatric patients to our clinic,” says Area Director Stephanie Loveless, MPH. “They play an incredibly important role in the care team, working closely with patients to ensure they get the support and resources they need as followup to clinic visits. They advocate for patients and help them navigate private and government insurance options, therapy resources, nutrition, and fitness coaching, and provide health education for diabetes, heart health, and other complicated conditions.”
PARTNERSHIP WITH EASTERSEALS
A partnership with Easterseals Arkansas is another example of how UAMS serves the community beyond the walls of traditional clinics. Clinical staff from the UAMS Health Neighborhood
St. Bernards Healthcare Community Benefit Programs Keep Communities Healthy
By Mitchell Nail
Kathy Murray of Paragould felt drained in early 2023. Her energy vanished, and she struggled to complete daily tasks.
“I just could not function,” Kathy recalls, believing previous colon and shoulder issues could be possible health culprits. “You kind of think, ‘Well, maybe I’m just not getting over that yet.’”
Kathy’s niece, Mackenzie, an employee of St. Bernards Healthcare, encouraged her aunt to attend a free healthscreening event her organization had planned for February. The screenings, part of free community wellness events that St. Bernards conducts each month, had a heart focus to correspond with American Heart Month. There, Kathy received carotid artery and calcium score screenings, as well as a slew of free blood panels and other important health measurements.
Kathy’s calcium score detected abnormally high levels of plaque, and she immediately scheduled an appointment with a cardiologist. She needed a coronary angiogram, which found four nearly complete blockages. Kathy underwent successful bypass surgery in April 2023 before entering a cardiac rehabilitation program at St. Bernards. Today, Kathy has regained much of her energy, and she is able to enjoy life with her children and seven grandchildren.
“Sometimes we don’t think about our own health,” Kathy says, “and I honestly don’t believe I would be here now if I had not gone to that screening.”
Through her story, Kathy shares a similar experience with millions of people. These individuals have improved their health and quality of life, even saved their own lives, by taking part in local Community Benefit programs hosted across Arkansas and throughout the United States.
COMMUNITY BENEFITS AT ST. BERNARDS HEALTHCARE
St. Bernards Healthcare has a service area of 23 counties in northeast Arkansas and southeast Missouri. This service area incorporates more than 620,000 persons, and the health care system’s headquarters in Craighead County places it squarely within the most populous county in the region.

St. Bernards Heart Day, 2024.
On average, St. Bernards’ Community Benefit program serves nearly 300,000 people each year. Three-fourths of the benefit reaches disadvantaged community members, and the program itself goes well beyond unpaid costs and charity care. Its highlights include regular free health screenings and education, as well as system donations and robust volunteerism.
For example, the aforementioned wellness screenings provide a $150 value to each attendee plus additional health emphases depending upon the time of year. This year, St. Bernards has already hosted events that focus on heart, colorectal, dermatological, and children’s health. It plans to target the health of seniors, men, women, and other populations later this year.
St. Bernards Value Based/Population Health Director Josh Jenkins helps lead the system’s Community Benefit efforts. He describes the program as an organized extension of the good work that St. Bernards team members already do.
“The purpose of community benefit is to improve the health of the communities we serve,” Jenkins says. “We improve access and promote medical knowledge, keeping our community members healthy and living independently.”
Jenkins says that St. Bernards focuses its resources to have the largest impacts.
“The more community benefit we provide, the fewer hospitalizations we have, and the more preventive care we promote,” he adds.
Using a dedicated team, St. Bernards has gradually evolved its Community Benefit program to find new ways of providing
care. This model reaches community members where they are, keeping them out of the hospital and preventing readmissions should they need hospital care.
Jenkins describes the creativity needed to create a healthy program. He says partnerships within St. Bernards and within the community play pivotal roles.
“Because we’re constantly identifying our highest risk populations,” he says, “we often ask, ‘How can we bring in other organizations to have larger impacts?’”
CONGREGATIONAL WELLNESS
One of St. Bernards’ newest and strongest partnerships involves local churches. The health care system’s Congregational Wellness program collaborates with area congregations to improve a community’s overall health. Regardless of hospital affiliation or church denomination, St. Bernards helps church members navigate challenging health care environments. The system believes that spiritual, physical, mental, and emotional health work together for overall wellness. In response, its program targets health awareness and education as well as disease prevention.
Jenkins says the Congregational Wellness team approaches each of its church partners with the premise of keeping congregations and community members healthy.
“Local churches have deep roots throughout the community, and these partnerships help us identify and address disparities through a shared vision of healing,” he says.


St. Bernards Mobile Mammography Unit.
St. Bernards sports medicine athletic trainers and physical therapists at Jonesboro High School.
IMPROVING MATERNAL AND NEWBORN OUTCOMES
St. Bernards has led a concerted effort to combat challenging maternal and newborn outcomes. Eight years ago, it opened a dedicated prenatal and postpartum clinic, designed to serve all pregnant women regardless of their insurance status or ability to pay.
These services, provided at St. Bernards Pregnancy Clinic in Jonesboro, began in a shared four-story medical building. Demand grew quickly, however, and the parking situation for pregnant moms often proved tricky. In 2021, the clinic moved to a forward-facing facility, helping its clients better access maternal services. Two years later, it began providing care in Walnut Ridge, and it plans to expand its reach to Osceola and Marion later this year.
Dana Lands, St. Bernards Nursing Director for Women’s and Children’s Services, says nearly half of the babies delivered at St. Bernards Medical Center connect to the hospital through the Pregnancy Clinic.
“This clinic truly is the mission of St. Bernards, ‘to provide Christ-like healing to the community,’” Lands says. “We have changed the perception of where our situation is to where we’re going.”
Even more, St. Bernards received approval from the Arkansas Life360 HOME Program earlier this year. This program provides home-based care support to women with high-risk pregnancies during gestation and up to two years postpartum. St. Bernards will serve as the first Life360 HOME program in Arkansas, continuing the organization’s efforts to improve birth outcomes.
HELPING WITH FOOD AND HOUSING INSECURITY
At St. Bernards Medical Center, its Transitions of Care department recently began identifying patients who experience food or housing insecurity. Rather than discharging these individuals with unmet needs, the department established an Angel Backpack program that includes essential items and food. It also provides tents for patients without housing who have no other means of shelter.
St. Bernards employees have generously donated to the backpack program, and employees with food insecurity even benefit from the additional help.
MORE OUTREACH PROGRAMMING
• Mammograms: St. Bernards has a dedicated mobile mammography unit that travels to outlying areas. This Class A vehicle logs thousands of miles each year, offering the latest mammography technology for women who have trouble accessing St. Bernards’ Imaging Center in Jonesboro. Through generous donations, uninsured and underinsured women receive needed imaging services, including their yearly breast cancer screenings.
• Internal Medicine Residency Clinic: St. Bernards’ Internal Medicine Residency Program trains 24 internal medicine resident physicians each year. These physicians and their physician preceptors operate a dedicated clinic that accepts any patient, with or without insurance. Doing so gives community members a place to go for primary care services, regardless of their ability to pay, while also giving resident physicians practical, real-world experience.
• Student Pre-Participation Evaluations: Each spring, St. Bernards provides free physical evaluations to area students entering the 7th through 12th grades. The evaluations include free EKG testing for students in the 9th grade and above.
• Certified Athletic Trainers: St. Bernards provides certified athletic trainers to area schools in two counties, helping offset costs that schools incur in keeping their student-athletes healthy.
• Education Classes: St. Bernards offers education on diabetes, nutrition, exercise, heart health, cancer, mental wellness, birthing, breastfeeding, stroke awareness and much more. In addition, it certifies individuals to perform CPR and use AEDs while training high school students to babysit children in an official capacity.
• Support Groups: St. Bernards regularly hosts free and confidential support groups for persons experiencing grief, cancer diagnoses, behavioral and mental challenges, and more. This list, a small glimpse of the system’s total outreach programs, highlights the impacts of concerted community benefit efforts. Collectively, when these programs succeed, they provide better, preventive care models over traditional, intervening medicine. In addition, they drive down health care costs that burden communities at large. Addressing a community’s needs proactively and adequately helps the community thrive. Its healthier members live longer and have a better quality of life.
Jenkins says it best. “The more we serve our community, the better it is for everyone.”

Mitchell Nail serves as Media Relations Manager for St. Bernards Healthcare.







HOSPITAL STATISTICS 2024

ARKANSAS HOSPITAL ASSOCIATION 2024 HOSPITAL STATISTICS
25 Maternal Health in Arkansas, by the Numbers
26 Arkansas Hospitals 2024, by the Numbers
27 Arkansas Hospital Association Member Organizations by Type, 2024
28 AHA Members by City, Type, Size, and Services
30 Statewide Hospital Financial and Utilization Indicators, 2018-2022
31 Arkansas Hospitals Receiving Local Tax Support, 2024
32 Key Financial Indicators: Arkansas and Surrounding States, 2022
33 Comparative Financial Indicators: U.S. Community Hospitals
34 Hospital Access by County
35 AHA-Member Organizations by Congressional District
36 AHA Members by Control and System Affiliation
38 Inpatient and Emergency Department Discharges by Payer, 2022
Uninsured Inpatient Admissions and Costs, 2011-2022
39 Hospital Uncompensated Care Costs, 2018-2022
Top 20 Inpatient DRGs, 2022
40 Arkansas Hospitals Locator Map, 2024
Hospital Statistics uses the latest data available, and this year includes utilization and financial data reflecting the first-year post-public health emergency declaration for the COVID-19 pandemic. When comparing 2022-2023 data to previous years, it is important to remember that hospitals experienced massive disruptions in 2020-21. Reductions in revenue due to deferred and delayed care, expenditures related to pandemic preparedness and response, supply chain issues, staffing shortages, and several major surges associated with COVID-19 during previous years can bias trends seen in the current year’s data. Additionally, federal and state COVID-19 relief funding that provided some much-needed assistance is no longer available to hospitals, and repayment requirements (if applicable) will continue over the next few years. Financial and utilization measures included are reported based on hospital fiscal year, and not all 2022 data reflect the same 12-month period for each hospital. This year’s edition of Hospital Statistics reflects a full year’s view of hospital operations post-public health emergency declaration for the COVID-19 pandemic, and year-over-year changes in measures should be interpreted with caution.
MATERNAL HEALTH IN ARKANSAS, BY THE NUMBERS
In 2023, 35,161 births were recorded in Arkansas. Arkansas ranks highest in the nation in maternal mortality, with 43.5 maternal deaths per 100,000 births. Currently, expectant mothers in Arkansas are served by 35 hospitals licensed to provide labor and delivery services.
BIRTHING HOSPITALS BY HOSPITAL REGION
ARKANSAS BIRTHS BY COUNTY OF RESIDENCE, WITH HOSPITAL LOCATIONS


WORKFORCE CHALLENGES
In 2024, 49 of Arkansas’s 75 counties do not have a hospital that provides residents with birthing services. On average, expectant mothers will travel 17.2 minutes to their nearest birthing hospital, but in some of the state’s most rural areas, the travel time to a birthing hospital can reach 65 minutes. Hospitals’ ability to provide birthing services is dependent upon the availability of highly qualified staffing resources. Arkansas is among the states where OB/GYN services are becoming more limited, due to a shortage of physicians licensed to provide OB/GYN services. Currently, 353 physicians* are licensed to provide OB/GYN services in Arkansas, and there are 48 licensed nurse midwives who are able to provide a continuum of care services for pregnant and postpartum women. In 2024, 42 Arkansas counties have no licensed OB/GYN services available to their residents.
47 27 40 $18.05 BILLION
ARKANSAS HOSPITALS 2024 BY
THE NUMBERS
Hospitals of all types are located in cities, towns, and communities throughout Arkansas.
Hospitals and other health care organizations are members of the Arkansas Hospital Association
Community hospitals have fewer than 100 acute care beds.
Hospitals are designated by the federal government as critical access hospitals, having no more than 25 acute care beds.
Counties are served by a single hospital. Twenty of those counties are served by a single critical access hospital.
Is contributed by hospitals toward Arkansas’s economy, through the impacts of well-paid, consistent employment, purchases of goods and services, and construction and capital spending.
Of Arkansas workers are employed by hospitals or other health care organizations
Arkansas counties and cities believe their hospitals to be important enough that people in those areas have voted to provide local tax support for the hospital.
Arkansas counties – more than 25% of all counties in the state – do not have a local community hospital.
Of AHA member organizations are charitable, not-for-profit organizations, while 25% are operated by private, for-profit companies, and 12% are public hospitals owned and operated by a city, county, state, or federal government.
Hospitals offer labor and delivery services for birthing mothers in Arkansas.
Arkansans sought inpatient or outpatient care from the state’s hospitals each day in 2022, on average, for illnesses, injuries, and other conditions that require medical attention.
Newborns were delivered in Arkansas hospitals in 2023. Nearly 40% of those births were covered by Medicaid.
ARKANSAS HOSPITAL ASSOCIATION
MEMBER ORGANIZATIONS BY TYPE, 2024
General Med-Surg Hospitals (43)
Arkansas Methodist Medical Center
Baptist Health-Fort Smith
Baptist Health-Van Buren
Baptist Health Medical Center-Conway
Baptist Health Medical Center -Drew County
Baptist Health Medical Center -Hot Spring County
Baptist Health Medical Center -Little Rock
Baptist Health Medical Center -North Little Rock
Baptist Health Medical Center-Stuttgart
Baptist Memorial Hospital - Crittenden
Baxter Health
Chambers Memorial Hospital
CHI St. Vincent - Hot Springs
CHI St. Vincent - Infirmary
CHI St. Vincent - North
Conway Regional Health System
Forrest City Medical Center
Great River Medical Center
Jefferson Regional
Johnson Regional Medical Center
Levi Hospital
Magnolia Regional Medical Center
Mena Regional Health System
Mercy Hospital Fort Smith
Mercy Hospital Northwest Arkansas
National Park Medical Center
NEA Baptist Memorial Hospital
North Arkansas Regional Medical Center
Northwest Health Physicians' Specialty Hospital
Northwest Medical Center - Bentonville
Northwest Medical Center - Springdale
Ouachita County Medical Center
Saint Mary's Regional Medical Center
Saline Memorial Hospital
Siloam Springs Regional Hospital
South Arkansas Regional Hospital
St. Bernards Medical Center
UAMS Medical Center
Unity Health - Jacksonville
Unity Health - Newport
Unity Health - Searcy
Washington Regional Medical System
White River Health System
Critical Access Hospitals (27)
Ashley County Medical Center
Baptist Health Medical Center
- Arkadelphia
Baptist Health Medical Center
- Heber Springs
Baxter Health Fulton County Hospital
Bradley County Medical Center
CHI St. Vincent - Morrilton
Chicot Memorial Medical Center
CrossRidge Community Hospital
Dallas County Medical Center
Dardanelle Regional Medical Center
Delta Health System
DeWitt Hospital and Nursing Home
Howard Memorial Hospital
Izard Regional Hospital
Lawrence Memorial Hospital
Little River Medical Center
McGehee Hospital
Mercy Hospital Berryville
Mercy Hospital Booneville
Mercy Hospital Ozark
Mercy Hospital Paris
Mercy Hospital Waldron
Ozark Health Medical Center
Ozarks Community Hospital
Piggott Health System
Sevier County Medical Center
Stone County Medical Center
Rural Emergency Hospitals (4)
Eureka Springs Hospital
Progressive Health – Helena
South Mississippi County Regional Medical Center
St. Bernards Medical Center – Five Rivers
Inpatient Rehab Hospital (6)
Baptist Health Rehabilitation Institute
CHI St. Vincent Hot Springs Rehabilitation Hospital
CHI St. Vincent Sherwood Rehabilitation Hospital
Conway Regional Rehabilitation Hospital
Encompass Health Rehabilitation Hospital
Mercy Rehabilitation Hospital Fort Smith
Inpatient Psych Hospitals (11)
Arkansas State Hospital
Conway Behavioral Health
Methodist Behavioral Hospital
Perimeter Behavioral Hospital of West Memphis
Pinnacle Pointe Behavioral Healthcare System
Rivendell Behavioral Health Services
Riverview Behavioral Health
Springwoods Behavioral Health Hospital
The BridgeWay
Valley Behavioral Health System
Vantage Point of NWA
Veterans Affairs Hospitals (2)
Central Arkansas Veterans Healthcare System
Veterans Health Care System of the Ozarks
Long Term Care Hospitals (4)
Advanced Care Hospital of White County
Arkansas Continued Care Hospital of Jonesboro
Baptist Health Extended Care Hospital
Cornerstone Specialty Hospitals
- Little Rock
Special Focus (3)
Arkansas Children's Hospital
Arkansas Children's Northwest
Willow Creek Women's Hospital
Out-of-State, Border City Hospitals (2)
CHRISTUS St. Michael Health System
Regional One Health
Non-Hospital Facilities (3)
19th Medical Group
Arkansas Hospice
CARTI
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
CITY HOSPITAL
ARKADELPHIA BAPTIST HEALTH MEDICAL CENTER-ARKADELPHIA
ASHDOWN LITTLE RIVER MEDICAL CENTER MEDICAL-SURGICAL
BARLING VALLEY BEHAVIORAL HEALTH SYSTEM
BATESVILLE WHITE RIVER HEALTH
BENTON RIVENDELL BEHAVIORAL HEALTH SERVICES PSYCHIATRIC
BENTON SALINE MEMORIAL HOSPITAL
BENTONVILLE NORTHWEST MEDICAL CENTER – BENTONVILLE
BERRYVILLE MERCY HOSPITAL BERRYVILLE
BLYTHEVILLE GREAT RIVER MEDICAL CENTER
BOONEVILLE MERCY HOSPITAL BOONEVILLE
CALICO ROCK IZARD REGIONAL HOSPITAL
CAMDEN OUACHITA COUNTY MEDICAL CENTER
CLARKSVILLE JOHNSON REGIONAL MEDICAL CENTER
CLINTON OZARK HEALTH MEDICAL CENTER
CONWAY BAPTIST HEALTH MEDICAL CENTER-CONWAY
CONWAY CONWAY BEHAVIORAL HEALTH
CONWAY CONWAY REGIONAL HEALTH SYSTEM
CONWAY CONWAY REGIONAL REHABILITATION HOSPITAL REHABILITATION 26 REHAB
CROSSETT ASHLEY COUNTY MEDICAL CENTER
DANVILLE CHAMBERS MEMORIAL HOSPITAL
DARDANELLE DARDANELLE REGIONAL MEDICAL CENTER
DE QUEEN SEVIER COUNTY MEDICAL CENTER MEDICAL-SURGICAL 15
DEWITT DEWITT HOSPITAL & NURSING HOME
DUMAS DELTA MEMORIAL HOSPITAL
EL DORADO SOUTH ARKANSAS REGIONAL HOSPITAL
EUREKA SPRINGS EUREKA SPRINGS HOSPITAL
FAYETTEVILLE ENCOMPASS HEALTH REHABILITATION HOSPITAL, A PARTNER OF WASHINGTON REGIONAL REHABILITATION 80 REHAB
FAYETTEVILLE NORTHWEST HEALTH PHYSICIANS’ SPECIALTY HOSPITAL MEDICAL-SURGICAL 20
FAYETTEVILLE SPRINGWOODS BEHAVIORAL HEALTH HOSPITAL PSYCHIATRIC 80
FAYETTEVILLE VANTAGE POINT OF NWA
FAYETTEVILLE VETERANS HEALTH CARE SYSTEM OF THE OZARKS VETERANS AFFAIRS 73 PSYCH
FAYETTEVILLE WASHINGTON REGIONAL MEDICAL SYSTEM MEDICAL-SURGICAL 425 LEVEL II OB/HH/PALL
FORDYCE DALLAS COUNTY MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB
FORREST CITY FORREST CITY MEDICAL CENTER
FORT SMITH BAPTIST HEALTH-FORT SMITH MEDICAL-SURGICAL 492 PSYCH/HH
FORT SMITH MERCY HOSPITAL FORT SMITH MEDICAL-SURGICAL 336 LEVEL III REHAB/HH
FORT SMITH MERCY REHABILITATION HOSPITAL FORT SMITH REHABILITATION 50 REHAB
GRAVETTE OZARKS COMMUNITY HOSPITAL
HARRISON NORTH ARKANSAS REGIONAL MEDICAL CENTER
25 SB
HEBER SPRINGS BAPTIST HEALTH MEDICAL CENTER-HEBER SPRINGS MEDICAL-SURGICAL 25 SB/HH
HELENA PROGRESSIVE HEALTH - HELENA MEDICAL-SURGICAL HH
HOT SPRINGS CHI ST. VINCENT HOT SPRINGS MEDICAL-SURGICAL 282 LEVEL II OB/PSYCH/REHAB/HH
HOT SPRINGS CHI ST. VINCENT HOT SPRINGS REHABILITATION HOSPITAL REHABILITATION 48 REHAB
HOT SPRINGS LEVI HOSPITAL
HOT
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
CITY HOSPITAL
LITTLE ROCK BAPTIST HEALTH EXTENDED CARE HOSPITAL LONG TERM CARE 36 PALL
LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-LITTLE ROCK
LITTLE ROCK BAPTIST HEALTH REHABILITATION INSTITUTE REHABILITATION 120 PALL
LITTLE ROCK CARTI OP CANCER CENTER
LITTLE ROCK CENTRAL ARKANSAS VETERANS HEALTHCARE SYSTEM VETERANS AFFAIRS 505 PSYCH/REHAB/HH/PALL/LTC
LITTLE ROCK CHI ST. VINCENT INFIRMARY
LITTLE ROCK CORNERSTONE SPECIALITY HOSPITALS LITTLE ROCK LONG TERM CARE 40
LITTLE ROCK PINNACLE POINTE BEHAVIORAL HEALTHCARE SYSTEM PSYCHIATRIC 127 PSYCH
LITTLE ROCK UAMS MEDICAL CENTER
MAGNOLIA MAGNOLIA REGIONAL MEDICAL CENTER
MALVERN BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY
MAUMELLE METHODIST BEHAVIORAL HOSPITAL
MCGEHEE MCGEHEE HOSPITAL
MEMPHIS, TN REGIONAL ONE HEALTH
MENA MENA REGIONAL HEALTH SYSTEM
MONTICELLO BAPTIST HEALTH MEDICAL CENTER-DREW COUNTY
MORRILTON CHI ST. VINCENT MORRILTON
MOUNTAIN HOME BAXTER HEALTH
MOUNTAIN VIEW STONE COUNTY MEDICAL CENTER
NASHVILLE HOWARD MEMORIAL HOSPITAL
NEWPORT UNITY HEALTH - NEWPORT
NORTH LITTLE ROCK, HOT SPRINGS, RUSSELLVILLE ARKANSAS HOSPICE
INPATIENT HOSPICE 24 PALL
NORTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-NORTH LITTLE ROCK MEDICAL-SURGICAL 225 LEVEL III OB/REHAB/PALL
NORTH LITTLE ROCK THE BRIDGEWAY PSYCHIATRIC 127 PSYCH
OSCEOLA SMC REGIONAL MEDICAL CENTER MEDICAL-SURGICAL
OZARK MERCY HOSPITAL OZARK
PARAGOULD ARKANSAS METHODIST MEDICAL CENTER
PARIS MERCY HOSPITAL PARIS
PIGGOTT PIGGOTT HEALTH SYSTEM
PINE BLUFF JEFFERSON REGIONAL
POCAHONTAS ST. BERNARDS FIVE RIVERS
ROGERS MERCY HOSPITAL NORTHWEST ARKANSAS
HH
ROGERS MERCY REHABILITATION SERVICES - NORTHWEST ARKANSAS REHABILITATION 36 REHAB
RUSSELLVILLE SAINT MARY’S REGIONAL MEDICAL CENTER
SALEM BAXTER HEALTH FULTON COUNTY HOSPITAL
SEARCY ADVANCED CARE HOSPITAL OF WHITE COUNTY LONG TERM CARE
SEARCY UNITY HEALTH - SEARCY
SHERWOOD CHI ST. VINCENT NORTH
SHERWOOD CHI ST. VINCENT SHERWOOD REHABILITATION HOSPITAL
SILOAM SPRINGS SILOAM SPRINGS REGIONAL HOSPITAL
SPRINGDALE ARKANSAS CHILDREN’S NORTHWEST
SPRINGDALE NORTHWEST MEDICAL CENTER - SPRINGDALE
STUTTGART BAPTIST HEALTH
TEXARKANA RIVERVIEW BEHAVIORAL
TEXARKANA,
VAN BUREN BAPTIST HEALTH-VAN BUREN
(PED)
WEST MEMPHIS BAPTIST MEMORIAL HOSPITAL-CRITTENDEN
WEST
STATEWIDE HOSPITAL
AND UTILIZATION INDICATORS, 2018 - 2022
INDICATOR
BEDS AVAILABLE
ADMISSIONS
PATIENT DAYS
AVERAGE LENGTH OF STAY
NON-EMERGENCY OP VISITS
OUTPATIENT VISITS
NON-EMERGENCY AS A % OF TOTAL OP VISITS
ADJUSTED PATIENT DAYS
OCCUPANCY RATE
INPATIENT SURGERIES
OUTPATIENT SURGERIES
TOTAL SURGERIES
OUTPATIENT AS % OF TOTAL SURGERIES
TOTAL FULL-TIME EQUIVALENT EMPLOYEES
FULL-TIME EQUIVALENT EMPLOYEES PER ADJUSTED
OCCUPIED BED
GROSS REVENUE, INPATIENT
GROSS REVENUE, OUTPATIENT
GROSS PATIENT REVENUE
BAD DEBTS
CHARITY
MEDICARE, MEDICAID, & OTHER PAYER WRITEOFFS
TOTAL DEDUCTIONS
NET PATIENT REVENUE
OTHER OPERATING REVENUE
NONOPERATING REVENUE
TOTAL NET REVENUE
PAYROLL EXPENSE
TOTAL EXPENSE
PATIENT REVENUE MARGIN
TOTAL MARGIN
CHARGE PER ADJUSTED INPATIENT DAY
PAYMENT PER ADJUSTED INPATIENT DAY
EXPENSE PER ADJUSTED INPATIENT DAY
PAYROLL PER ADJUSTED INPATIENT DAY
PAYROLL AS % OF TOTAL EXPENSE
BAD DEBT AND CHARITY AS % OF TOTAL CHARGE
TOTAL DEDUCTIONS AS % OF TOTAL CHARGE
OUTPATIENT REVENUE AS % TOTAL PATIENT REVENUE
ADMISSIONS PER BED
PATIENT DAYS PER 1,000 POPULATION
ADMISSIONS PER 1,000 POPULATION
POPULATION (000'S)
$13,777,391,679
$15,450,146,464
$29,227,538,143
$502,016,281
$358,871,422
$20,647,010,804
$21,507,898,507
7,719,639,636
$395,516,849
$44,821,792
$8,159,978,277
$2,989,469,225
$7,797,448,234
$14,814,502,613
$17,025,641,576
$31,840,144,189
$509,174,368
$442,315,671
$22,702,507,161
$23,653,997,200
$8,186,146,989
$433,117,737
$145,788,360
$8,765,053,086
$3,040,326,208
$8,049,927,966 1.66% 8.16%
$7,445.97
$1,914.37
$1,882.51
$14,965,703,755
$16,733,703,930
$31,699,407,685
$503,958,456
$499,580,152
$22,706,699,474
$23,710,238,082
$7,989,169,603
$760,697,334
$164,859,866
$8,914,726,803
$3,122,035,492
$8,206,104,259 -2.72%
$17,185,062,486 $18,570,833,303 $35,755,895,789 $512,576,407 $574,072,837 $25,738,880,672
$26,825,529,916 $8,930,365,873 $919,369,130 $246,467,868 $10,096,202,871 $3,542,564,965 $9,161,715,585 -2.59% 9.26%
3.36 $16,766,340,537 $19,010,965,594 $35,777,306,131 $468,830,369 $466,432,386 $25,758,657,460 $26,693,920,215 $9,083,385,916 $1,143,477,147 ($5,690,890) $10,221,172,173 3,844,177,083 $10,093,617,469 -11.12% 1.25% $8,033.36 $2,039.56 $2,266.40 $863.16
ARKANSAS HOSPITALS
RECEIVING LOCAL TAX SUPPORT, 2024
INDICATOR
ASHLEY COUNTY MEDICAL CENTER
BAPTIST HEALTH MEDICAL CENTER-DREW COUNTY
BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY
BAPTIST HEALTH MEDICAL CENTER-STUTTGART
BAXTER HEALTH FULTON COUNTY HOSPITAL
BRADLEY COUNTY MEDICAL CENTER
CHI ST. VINCENT MORRILTON
CHICOT MEMORIAL MEDICAL CENTER
CROSSRIDGE COMMUNITY HOSPITAL
DALLAS COUNTY MEDICAL CENTER
DELTA HEALTH SYSTEM
DEWITT HOSPITAL & NURSING HOME
GREAT RIVER MEDICAL CENTER
JOHNSON REGIONAL MEDICAL CENTER
LAWRENCE MEMORIAL HOSPITAL
LITTLE
MAGNOLIA REGIONAL MEDICAL CENTER (A)
MAGNOLIA REGIONAL MEDICAL CENTER (B)
MCGEHEE HOSPITAL
MERCY HOSPITAL BOONEVILLE
MERCY HOSPITAL OZARK
MERCY HOSPITAL PARIS
OUACHITA COUNTY MEDICAL CENTER
OZARK HEALTH MEDICAL CENTER
PIGGOTT COMMUNITY HOSPITAL
SMC REGIONAL MEDICAL CENTER
ST. BERNARDS FIVE RIVERS
NA=Information not available
Source: Self-reported information provided to the Arkansas Hospital Association
$649,000 $670,000 $1,600,000 $2,300,000 $310,000 $1,200,000 $1,000,000 $1,100,000 $2,500,000 $840,000 $840,000 $850,000 $2,439,800 $65,000 $1,900,000 $834,000 $2,600,000 $540,000 $600,000 $360,000 $350,000
$150,000 $360,000 $829,300 $800,000
KEY FINANCIAL INDICATORS:
ARKANSAS AND SURROUNDING STATES, 2022
Texas
Tennessee
$476,634,436,780
$102,614,520,924
$381,415,598,693 $95,218,838,087 $92,809,526,734 30,334,335
$79,804,803,898
$71,093,509,255 $27,035,340,159 $28,519,881,907 10,396,864 ($1,484,541,748) ($142.79) -5.49% $2,000,313,405 $515,771,657 1.78%
Mississippi
Louisiana $70,303,754,603
Arkansas
$35,777,306,131
$26,693,920,215 $9,083,385,916 $10,093,617,469 4,453,594 ($1,010,231,553) ($226.84) -11.12%
Hospitals charged this amount for the inpatient and outpatient care they provided in 2022: But patients and payer groups didn't pay the full amount of billed charges for various reasons. Government programs like Medicare and Medicaid, workers' comp programs, and others never pay the full hospital bill. Managed care plans and other insurers typically pay discounted amounts only, and individual patients often can't afford to pay some or any of the out-of-pocket costs related to their hospital bills. For those reasons, hospitals had to forfeit this much of their billed charges: As a result, actual payments to hospitals were: At the same time, hospitals spent this much providing patient care services… …to patients needing care for this many adjusted patient days while being served. So the revenue excess (loss) was: In other words, hospitals made (or lost) this much on each of the equivalent days of care they provided to inpatients and outpatients: Yielding a "patient service" margin of:
In addition, hospitals also received revenues from normal, day-today operations from services other than health care provided to patients, such as COVID relief dollars, space rental, cafeteria and gift shop sales, and operating gains: Which raised total operating income to:
As a result, the "operating margin" rose to:
Hospitals also collected other types of revenue from sources including contributions, tax appropriations, and investments. Those amounted to: That resulted in total funds available to reinvest in new equipment, update facilities, expand programs and repay debt equaling: For a return on investment totaling:
COMPARATIVE FINANCIAL INDICATORS: U.S. COMMUNITY HOSPITALS
1. DISTRICT
2.
3.
4.
5.
6.
13.
14.
15.
16.
17.
18. OKLAHOMA
19. MINNESOTA
20. KANSAS
21. KENTUCKY
22. VIRGINIA
23. GEORGIA
24. ILLINOIS
25. TENNESSEE
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
48.
49.
AVERAGE PAYMENT PER HOSPITAL STAY ($)
NORTH DAKOTA
OREGON
NEBRASKA MARYLAND MONTANA
NEW JERSEY INDIANA
NEW
U.S.
VERMONT
MASSACHUSETTS
CONNECTICUT
PENNSYLVANIA
WISCONSIN
OHIO
OREGON
COLORADO
IDAHO
DELAWARE
MARYLAND
VERMONT
ALASKA
NEBRASKA
CONNECTICUT
NEW
MONTANA
UTAH
NEW JERSEY
U.S.
PENNSYLVANIA
INDIANA
SOUTH DAKOTA
OHIO
WISCONSIN
ILLINOIS
WYOMING
MICHIGAN
MISSOURI
TEXAS
KANSAS
RHODE
ARIZONA
GEORGIA
VIRGINIA
WSC
WEST
NORTH
HOSPITAL ACCESS BY COUNTY

SEARCY
AHA-MEMBER ORGANIZATIONS BY CONGRESSIONAL DISTRICT
1st Congressional District
Arkansas Continued Care Hospital of Jonesboro
Arkansas Methodist Medical Center
Baptist Health Medical Center-Stuttgart
Baptist Memorial Hospital-Crittenden
Baxter Health
Baxter Health Fulton County Hospital
Chicot Memorial Medical Center
CrossRidge Community Hospital
Delta Memorial Hospital
DeWitt Hospital & Nursing Home
Forrest City Medical Center
Great River Medical Center
Izard Regional Hospital
Lawrence Memorial Health Foundation, Inc.
McGehee Hospital
NEA Baptist Memorial Hospital
North Arkansas Regional Medical Center
Perimeter Behavioral Hospital of West Memphis
Piggott Community Hospital
Progressive Health - Helena
SMC Regional Medical Center
St. Bernards Five Rivers
St. Bernards Medical Center
Stone County Medical Center
Unity Health - Newport
White River Health System
Total = 26
2nd Congressional District
19th Medical Group
Advanced Care Hospital of White County
Arkansas Children's Hospital
Arkansas Hospice
Arkansas State Hospital
Baptist Health Extended Care Hospital
Baptist Health Medical Center-Conway
Baptist Health Medical Center-Heber Springs
Baptist Health Medical Center-Little Rock
Baptist Health Medical Center-North Little Rock
Baptist Health Rehabilitation Institute
CARTI
Central Arkansas Veterans Healthcare System
CHI St. Vincent Infirmary
CHI St. Vincent Morrilton
CHI St. Vincent North
CHI St. Vincent Sherwood Rehabilitation
Hospital, a Partner of Encompass Health
Conway Behavioral Health
Conway Regional Health System
Conway Regional Rehabilitation Hospital
Cornerstone Specialty Hospitals Little Rock
Methodist Behavioral Hospital
Ozark Health Medical Center
Pinnacle Pointe Behavioral Healthcare System
Rivendell Behavioral Health Services
Saline Memorial Hospital
The BridgeWay
UAMS Medical Center
Unity Health - Jacksonville
Unity Health - Searcy
Total = 30

3rd Congressional District
Arkansas Children’s Northwest
Baptist Health-Fort Smith
Baptist Health-Van Buren
Encompass Health Rehabilitation Hospital, a Partner of Washington Regional
Eureka Springs Hospital
Mercy Hospital Berryville
Mercy Hospital Fort Smith
Mercy Hospital Northwest Arkansas
Mercy Rehabilitation Hospital Fort Smith
Northwest Health Physicians’ Specialty Hospital
Northwest Medical Center Bentonville
Northwest Medical Center Springdale
Ozarks Community Hospital
Siloam Springs Regional Hospital
Springwoods Behavioral Health Hospital
Valley Behavioral Health System
Vantage Point of NWA
Veterans Health Care System of the Ozarks
Washington Regional Medical System
Willow Creek Women’s Hospital
Total = 20
Additional AHA Member
Hospitals Include:
CHRISTUS St. Michael Health System, Texarkana, TX
Regional One Health, Memphis, TN
4th Congressional District
Ashley County Medical Center
Baptist Health Medical Center-Arkadelphia
Baptist Health Medical Center- Drew County
Baptist Health Medical Center-Hot Spring County
Bradley County Medical Center
Chambers Memorial Hospital
CHI St. Vincent Hot Springs
CHI St. Vincent Hot Springs Rehab Hospital, a Partner of Encompass Health
Dallas County Medical Center
Dardanelle Regional Medical Center
Howard Memorial Hospital
Jefferson Regional
Johnson Regional Medical Center
Levi Hospital
Little River Medical Center, Inc.
Magnolia Regional Medical Center
Mena Regional Health System
Mercy Hospital Booneville
Mercy Hospital Ozark
Mercy Hospital Paris
Mercy Hospital Waldron
National Park Medical Center
Ouachita County Medical Center
Riverview Behavioral Health
Saint Mary's Regional Medical Center
Sevier County Medical Center
South Arkansas Regional Hospital
Total = 27
19TH MEDICAL GROUP
AHA MEMBERS BY CONTROL AND SYSTEM AFFILIATION
ADVANCED CARE HOSPITAL OF WHITE COUNTY
ARKANSAS CHILDREN'S HOSPITAL
ARKANSAS CHILDREN'S NORTHWEST
ARKANSAS CONTINUED CARE HOSPITAL OF JONESBORO
ARKANSAS HOSPICE
ARKANSAS METHODIST MEDICAL CENTER
ARKANSAS STATE HOSPITAL
ASHLEY COUNTY MEDICAL CENTER
BAPTIST HEALTH EXTENDED CARE HOSPITAL
BAPTIST HEALTH MEDICAL CENTER-ARKADELPHIA
BAPTIST HEALTH MEDICAL CENTER-CONWAY
BAPTIST HEALTH MEDICAL CENTER-DREW COUNTY
BAPTIST HEALTH MEDICAL CENTER-HEBER SPRINGS
BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY
BAPTIST HEALTH MEDICAL CENTER-LITTLE ROCK
BAPTIST HEALTH MEDICAL CENTER-N. LITTLE ROCK
BAPTIST HEALTH MEDICAL CENTER-STUTTGART
BAPTIST HEALTH REHABILITATION INSTITUTE
BAPTIST HEALTH-FORT SMITH
BAPTIST HEALTH-VAN BUREN
BAPTIST MEMORIAL HOSPITAL-CRITTENDEN
BAXTER HEALTH
BAXTER HEALTH FULTON COUNTY HOSPITAL
BRADLEY COUNTY MEDICAL CENTER
CARTI
CENTRAL ARKANSAS VETERANS HEALTHCARE SYSTEM
CHAMBERS MEMORIAL HOSPITAL
CHI ST. VINCENT HOT SPRINGS
CHI ST. VINCENT HOT SPRINGS REHABILITATION HOSPITAL
CHI ST. VINCENT INFIRMARY
CHI ST. VINCENT MORRILTON
CHI ST. VINCENT NORTH
CHI ST. VINCENT SHERWOOD REHABILITATION HOSPITAL
CHICOT MEMORIAL MEDICAL CENTER
CHRISTUS ST. MICHAEL HEALTH SYSTEM
CONWAY BEHAVIORAL HEALTH
CONWAY REGIONAL HEALTH SYSTEM
CONWAY REGIONAL REHABILITATION HOSPITAL
CORNERSTONE SPECIALITY HOSPITALS LITTLE ROCK
CROSSRIDGE COMMUNITY HOSPITAL
DALLAS COUNTY MEDICAL CENTER
DARDANELLE REGIONAL MEDICAL CENTER
DELTA MEMORIAL HOSPITAL
DEWITT HOSPITAL & NURSING HOME
ENCOMPASS HEALTH REHABILITATION HOSPITAL, A PARTNER OF WASHINGTON REGIONAL
EUREKA SPRINGS HOSPITAL
FORREST CITY MEDICAL CENTER
GREAT RIVER MEDICAL CENTER
HOWARD MEMORIAL HOSPITAL
IZARD REGIONAL HOSPITAL
LTCH
CHILDREN'S
CHILDREN'S
LTCH
INPATIENT HOSPICE
RURAL/RRC
IP PSYCH
CAH LTCH
CAH
URBAN
RURAL/SCH
CAH
RURAL/MDH
URBAN
URBAN
RURAL/MDH IRF
URBAN
URBAN
URBAN
RURAL/SCH/RRC CAH
CAH
URBAN/IP PSYCH/LTCH/ IRF/HOSP
RURAL/SCH
URBAN/RRC IRF
URBAN CAH
URBAN IRF CAH
URBAN (TX) IP PSYCH
URBAN
RURAL/SCH
RURAL/SCH/RRC
U.S. DEPARTMENT OF DEFENSE
UNITY HEALTH
ARKANSAS CHILDREN'S
ARKANSAS CHILDREN'S
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
STATE
LOCAL BOARD
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST MEMORIAL HEALTHCARE CORP.
LOCAL BOARD
COUNTY
LOCAL BOARD
LOCAL BOARD
U.S. DEPARTMENT OF VETERANS AFFAIRS
LOCAL BOARD
COMMONSPIRIT HEALTH
ENCOMPASS HEALTH
COMMONSPIRIT HEALTH
COMMONSPIRIT HEALTH
COMMONSPIRIT HEALTH
ENCOMPASS HEALTH
LOCAL BOARD
CHRISTUS HEALTH
ACADIA HEALTHCARE
CONWAY REGIONAL HEALTH SYSTEM
CONWAY REGIONAL HEALTH SYSTEM
SCIONHEALTH
ST. BERNARDS HEALTH SYSTEM
COUNTY
CONWAY REGIONAL HEALTH SYSTEM
LOCAL BOARD
LOCAL BOARD
ENCOMPASS HEALTH
EUREKA SPRINGS HOSPITAL COMMISSION
QUORUM HEALTH
COUNTY
LOCAL BOARD
LOCAL BOARD
SEARCY LITTLE ROCK
LITTLE ROCK
N. LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
MEMPHIS, TN
LITTLE ROCK
LITTLE ROCK/NLR
CHICAGO, IL
BIRMINGHAM, AL
CHICAGO, IL
CHICAGO, IL
CHICAGO, IL
BIRMINGHAM, AL
IRVING, TX
FRANKLIN, TN CONWAY
CONWAY
LOUISVILLE, KY JONESBORO
CONWAY
BIRMINGHAM, AL
EUREKA SPRINGS, AR
FRANKLIN, TN
JEFFERSON REGIONAL
JOHNSON REGIONAL MEDICAL CENTER
LAWRENCE MEMORIAL HOSPITAL
LEVI HOSPITAL
LITTLE RIVER MEDICAL CENTER
MAGNOLIA REGIONAL MEDICAL CENTER
MCGEHEE HOSPITAL
MENA REGIONAL HEALTH SYSTEM
MERCY HOSPITAL BERRYVILLE
MERCY HOSPITAL BOONEVILLE
MERCY HOSPITAL FORT SMITH
MERCY HOSPITAL NORTHWEST ARKANSAS
MERCY HOSPITAL OZARK
MERCY HOSPITAL PARIS
MERCY HOSPITAL WALDRON
MERCY REHABILITATION HOSPITAL FORT SMITH
MERCY REHABILITATION SERVICES - NORTHWEST AR
METHODIST BEHAVIORAL HOSPITAL
NATIONAL PARK MEDICAL CENTER
NEA BAPTIST MEMORIAL HOSPITAL
NORTH ARKANSAS REGIONAL MEDICAL CENTER
NORTHWEST HEALTH PHYSICIANS' SPECIALTY HOSPITAL
NORTHWEST MEDICAL CENTER - BENTONVILLE
NORTHWEST MEDICAL CENTER - SPRINGDALE
OUACHITA COUNTY MEDICAL CENTER
OZARK HEALTH MEDICAL CENTER
OZARKS COMMUNITY HOSPITAL
PERIMETER BEHAVIORAL HOSPITAL OF WEST MEMPHIS
PIGGOTT HEALTH SYSTEM
PINNACLE POINTE BEHAVIORAL HEALTHCARE SYSTEM
PROGRESSIVE HEALTH - HELENA
REGIONAL ONE HEALTH
RIVENDELL BEHAVIORAL HEALTH SERVICES
RIVERVIEW BEHAVIORAL HEALTH
SAINT MARY'S REGIONAL MEDICAL CENTER
SALINE MEMORIAL HOSPITAL
SEVIER COUNTY MEDICAL CENTER
SILOAM SPRINGS REGIONAL HOSPITAL
SMC REGIONAL MEDICAL CENTER
SOUTH ARKANSAS REGIONAL HOSPITAL
SPRINGWOODS BEHAVIORAL HEALTH HOSPITAL
ST. BERNARDS FIVE RIVERS
ST. BERNARDS MEDICAL CENTER
STONE COUNTY MEDICAL CENTER
THE BRIDGEWAY
UAMS MEDICAL CENTER
UNITY HEALTH - SEARCY
UNITY HEALTH - JACKSONVILLE
UNITY HEALTH - NEWPORT
VALLEY BEHAVIORAL HEALTH SYSTEM
VANTAGE POINT OF NWA
VETERANS HEALTH CARE SYSTEM OF THE OZARKS
WASHINGTON REGIONAL MEDICAL SYSTEM
WHITE RIVER HEALTH
WILLOW CREEK WOMEN'S HOSPITAL
URBAN/SCH
RURAL/MDH
CAH
URBAN
CAH
RURAL/SCH
CAH
RURAL/SCH
CAH
CAH
URBAN
URBAN
CAH
CAH
CAH
IRF
IRF
IP PSYCH
URBAN/RRC
RRC
RURAL/SCH/RRC
URBAN
URBAN
URBAN
RURAL/SCH
CAH
CAH
IP PSYCH
CAH
IP PSYCH
REH
URBAN (TN)
IP PSYCH
IP PSYCH
RURAL/RRC
URBAN
RURAL
URBAN
REH
RURAL/SCH
IP PSYCH
REH
URBAN/RRC
CAH
IP PSYCH
URBAN
RURAL/SCH/RRC
URBAN
CAH
IP PSYCH
IP PSYCH
RURAL
RURAL/SCH/RRC
URBAN
LOCAL BOARD
LOCAL BOARD
ST. BERNARDS HEALTH SYSTEM
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
CITY
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
MERCY HEALTH SYSTEM
LIFEPOINT
LIFEPOINT
METHODIST FAMILY HEALTH
LIFEPOINT
BAPTIST MEMORIAL HEALTHCARE CORP.
LOCAL BOARD
COMMUNITY HEALTH SYSTEMS
COMMUNITY HEALTH SYSTEMS
COMMUNITY HEALTH SYSTEMS
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
WOODRIDGE BEHAVIORAL CARE
CITY
UNIVERSAL HEALTH SERVICES
PROGRESSIVE HEALTH
REGIONAL ONE HEALTH
UNIVERSAL HEALTH SERVICES
ACADIA HEALTHCARE
LIFEPOINT
LIFEPOINT
COUNTY
COMMUNITY HEALTH SYSTEMS
COUNTY
LOCAL BOARD
UNIVERSAL HEALTH SERVICES
ST. BERNARDS HEALTH SYSTEM
ST. BERNARDS HEALTH SYSTEM
WHITE RIVER HEALTH SYSTEM
UNIVERSAL HEALTH SERVICES
STATE
UNITY HEALTH
UNITY HEALTH
UNITY HEALTH
ACADIA HEALTHCARE
ACADIA HEALTHCARE
U.S. DEPARTMENT OF VETERANS AFFAIRS
LOCAL BOARD
WHITE RIVER HEALTH SYSTEM
COMMUNITY HEALTH SYSTEMS
JONESBORO
ST. LOUIS, MO
ST. LOUIS, MO
ST. LOUIS, MO
ST. LOUIS, MO
ST. LOUIS, MO
ST. LOUIS, MO
ST. LOUIS, MO
BRENTWOOD, TN
BRENTWOOD, TN
LITTLE ROCK
BRENTWOOD, TN MEMPHIS, TN
FRANKLIN, TN
FRANKLIN, TN
FRANKLIN, TN
JACKSON, TN
KING OF PRUSSIA, PA
OXFORD, MS
MEMPHIS, TN
KING OF PRUSSIA, PA
FRANKLIN, TN
BRENTWOOD, TN
BRENTWOOD, TN
FRANKLIN, TN
KING OF PRUSSIA, PA
JONESBORO
JONESBORO
BATESVILLE
KING OF PRUSSIA, PA
SEARCY
SEARCY
SEARCY
FRANKLIN, TN
FRANKLIN, TN
BATESVILLE
FRANKLIN, TN
HOSPITAL UNCOMPENSATED CARE COSTS, 2018-2022
GROSS REVENUES (BILLED CHARGES)
$29,227,538,143
$31,840,144,189
$31,699,407,685
$35,755,895,789
$35,777,306,131
TOTAL UNCOLLECTED AMOUNTS DUE
$21,507,898,507
$23,653,997,200
$23,710,238,082
$26,825,529,916
$26,693,920,215
NET REVENUES (AMOUNT COLLECTED)
$7,719,639,636
$8,186,146,989
$7,989,169,603
$8,930,365,873
$9,083,385,916
$395,516,849
$433,117,737
$760,697,334
$919,369,130
$1,143,477,147
GROSS+ OTHER REVENUE
$29,623,054,992
$32,273,261,926
$32,460,105,019
$36,675,264,919
$36,920,783,278
TOTAL OPERATING COSTS
$7,797,448,234
$8,049,927,966
$8,206,104,259
$9,161,715,585
$10,093,617,469
$502,016,281
$509,174,368
$503,958,456
$512,576,407
$468,830,369
$358,871,422
$442,315,671
$499,580,152
$574,072,837
$466,432,386
$860,887,703
$951,490,039
$1,003,538,608
$1,086,649,244
$935,262,755
$212,015,528
$222,318,771
$238,120,014
$256,264,830.53
$243,811,319.81
Source: American Hospital Association, Hospital Statistics 2022
TOP 20 INPATIENT DRG s , 2022
DIAGNOSIS-RELATED GROUP
885 - PSYCHOSES
795 - NORMAL NEWBORN
807 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W/O CC/MCC
871 - SEPTICEMIA W/O MV 96+ HOURS W MCC
794 - NEONATE W OTHER SIGNIFICANT PROBLEMS
291 - HEART FAILURE & SHOCK W MCC
177 - RESPIRATORY INFECTIONS & INFLAMMATIONS W MCC
788 - CESAREAN SECTION W/O STERILIZATION W/O CC/MCC
189 - PULMONARY EDEMA & RESPIRATORY FAILURE
193 - SIMPLE PNEUMONIA & PLEURISY W MCC
897 - ALCOHOL/DRUG ABUSE/DEPENDENCE W/O REHABILITATION THERAPY W/O MCC
392 - ESOPHAGITIS, GASTROENT & MISC DIGEST DISORDERS W/O MCC
872 - SEPTICEMIA W/O MV 96+ HOURS W/O MCC
057 - DEGENERATIVE NERVOUS SYSTEM DISORDERS W/O MCC
806 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W CC
621 - O.R. PROCEDURES FOR OBESITY W/O CC/MCC
641 - NUTRITIONAL & MISC METABOLIC DISORDERS W/O MCC
683 - RENAL FAILURE W CC
682 - RENAL FAILURE W MCC
690 - KIDNEY & URINARY TRACT INFECTIONS W/O MCC
TOTAL CHARGES
681,816,501.38
118,191,989.21
272,365,090.12
846,529,029.38
83,571,241.23
301,545,908.54
384,006,699.65
144,841,005.80 209,161,799.92 200,424,676.19
83,675,934.90
87,317,566.02
106,723,487.92
142,135,303.76
55,284,713.59
171,199,869.13
59,427,235.29
75,591,055.15
124,018,514.10 63,334,930.28
Source: Arkansas Department of Health, Hospital Discharge Program, 2022
Arkansas Hospitals, 2024
INNOVATING FOR IMPROVEMENT
By Nancy Robertson

Michael Wood is one of a small group of hospital CEOs who was born in the hospital where he now serves. “Coming home to Mena and working at Mena Regional Health System is a full-circle moment for me,” he says.
Wood earned his Doctor of Physical Therapy degree at the University of Central Arkansas after completing his undergraduate work at the Conway college. His wife, Jennifer, is a pediatric DPT, and suggested after their graduation that they start their careers in Florida.
“One of my mentors at UCA was a professor who taught us the business side of running a practice,” Wood says. “He connected us with professional colleagues in Florida who owned and ran physical therapy clinics in the Gainesville and Ocala area, and so we made the move.”
Wood recalls their location in Florida as breathtaking. “We lived in the part of Florida that is horse country, with rolling hills and deep, crystal clear springs. You could see right down to the bottom of the springs and see the water bubbling up through the sand.”
After five years in the Sunshine State, Wood says he was becoming more and more dissatisfied with the way health care is delivered in the U.S. “In clinics and on a regional basis, we were trying new things and making a wonderful difference in our patients’ lives, but we weren’t able to make that same difference in the health care delivery system,” he says. “I wanted to find a way to help fix health care from the inside.”
The Woods moved back to Mena, where Michael began working as the hospital’s Director of Outpatient
Therapy Services. Soon thereafter, his role expanded to include leadership of inpatient rehab, as well. “Therapy is a small piece of the bigger health care puzzle,” he says, “but instinctively I knew we needed clinically minded people to work from the inside to effect change in the larger web of U.S. health care delivery.”

A FERTILE ENVIRONMENT
Mena Regional Health System operates a locally controlled hospital serving a rural population. Wood considers these aspects of the facility a plus. He also appreciates that the hospital’s small-town location allows caregivers to get to know patients and their families. “When you know the families you’re working with, it allows more leeway to understand and meet their particular needs,” he says.
Wood joined Mena Regional’s executive team in 2019, working closely with then-CEO Jay Quebedeaux, whom he considers to be a mentor. “We were constantly trying out new ideas to help improve the delivery of health care at our hospital,” he says. “Our particular hospital’s independence allows us to innovate … to try new things and make changes quickly.”
When Quebedeaux accepted a new role at Baptist Health Medical Center-Hot Spring County, Wood continued to serve on the executive team under the new CEO, Robert Rupp.
Upon Rupp’s departure, Wood was named interim CEO for the Mena System. He accepted the position of the system’s CEO in January of this year.
“In addition to my relationship with Jay, I have been blessed with a great mentor in Scott Peak, CEO of Chambers Memorial, whom I have known personally for most of my life,” Wood says. “The Arkansas health care community has been incredibly supportive and giving of both time and knowledge any time I have reached out to any of my fellow hospital CEOs.”
CONTINUOUS INNOVATION
The nationwide staffing shortage is one of the health care delivery challenges Wood sees as most pressing. As such, it was one of his first focuses in the quest to improve patient care from within the hospital itself.
“We began to determine how we could improve the staffing situation right at home,” he says. “Our first priority was to make certain every one of our staff members are working at what we call ‘the top of their licenses.’ That means that, for instance, RNs are spending most of their time assessing patients and providing interventions while care extenders such as patient care technicians are helping patients with activities of daily living. Because the nation’s staffing challenges affect even small, rural hospitals, we are diligent about helping our staff make the best use of their expertise and experience.”
During the pandemic, Mena Regional found it necessary to fill staff needs with traveling nurses, as did many hospitals in the U.S.
“One of our most recent accomplishments is reducing our number of travelers from 21 to seven,” Wood says, “which results in significant cost savings. Our teams are coming up with more creative ways in utilizing existing staff, and working to the top of their licenses is a part of this.”
He sees his role as “getting the right people in the right seat on the right bus,” making certain that staff expertise is utilized to its fullest extent. “One of my main focuses and
Michael and Jennifer Wood with their daughters Lexi, Ellie, and Ava.
LEADERSHIP Q/A WITH MICHAEL WOOD
What’s on your music playlist?
My wife and three young daughters control much of the music in our house, so right now we listen to a lot of Taylor Swift, the “Sing 2” soundtrack, and all things Kidz Bop. But my song of choice on repeat right now is probably “Good Day” by Forrest Frank.
Who is someone you greatly admire, and why?
I admire my wife for being selfless in her pursuit of our family and for raising three strong, independent, and beautiful girls. I could not do what I do without her.
What would you be doing if you weren’t in health care?
I joke all the time that I would be living in a van down by the river, but honestly, I can’t imagine a world where I wasn’t involved in health care to one degree or another.
What do you like to do in your down time?
I like spending time with my family hiking, camping, riding bikes, and swimming.
What is the most valuable lesson COVID taught you?
Relationships matter, and we are stronger together. COVID isolation was a huge detriment to our youth, our elderly, and everyone in between. We are still seeing those negative effects today.
jobs as CEO is to ensure we continuously look for ways to improve communication,” Wood says. “We are constantly listening to our staff, patients, and community members, working together to deliver the best possible health care.”
Another change underway at the hospital is bringing more service lines in-house, rather than having third-party contractors fill care needs. “This allows us, again, to work more personally with our patients and build the trusting relationships that are so important in health care.”
The innovations are making a fiscal difference in hospital operations. Wood says that the facility’s operating margin is currently 10% better than last year at this time.
But perhaps the biggest change is Mena Regional's planned switch to operation as a Critical Access Hospital, changing from its current status as a Prospective Payment System hospital. “The Centers for Medicare and Medicaid Services (CMS), as well as other government and commercial payers, are trying to move more patient care to outpatient, rather than inpatient, services. Our decision to change our hospital designation allows us to continue to operate 25 acute care inpatient beds while maintaining 10 beds each for rehab and geriatric psych patients. This change of designation is our solution for working within the system to best fit our community’s needs.”
COMMUNITY OUTREACH
Mena Regional, like so many Arkansas hospitals, has created a variety of community outreach programs suited specifically to regional needs.
One of Wood’s favorite programs is the Teddy Bear Clinic, offered each year to area first graders. “When a first-grade class visits the hospital, it becomes the keeper of a teddy bear that is ‘sick’ and needs care in the hospital setting. The children follow their teddy bear through the emergency room to X-ray, to rehab and physical therapy. They even visit our labor and delivery group while on their teddy bear hospital tour. Time has proven that this helps our community’s kids




Above, left and right: First-graders attend the Teddy Bear Clinic, where their bear is x-rayed and treated with the best of care. Below, area sixth graders come to the hospital to learn about future careers in health care service.
YOUR PARTNERS IN JOINT CARE AT

OrthoArkansas provides your patients with comprehensive orthopedic services all under one roof. From imaging and treatment to physical therapy, patients receive expert care from fellowship-trained physicians, with the guidance of our Care Navigator program, ensuring a seamless and personalized care experience. Our Care Navigators are dedicated to coordinating every aspect of your patient's journey, providing support and expertise at every step. Refer your joint patients to your partners in care—OrthoArkansas.

Emergency Preparedness as Community Outreach
By Lyndsey Dumas
One community outreach effort every hospital in Arkansas supports is preparation for community safety in a time of crisis. Whether a public health emergency like COVID-19, a toxic chemical spill, an explosion, an accident involving multiple vehicles or a vehicle of mass transit, or a weather-related incident, Arkansas’s emergency preparedness coalitions work in the background to assure that disaster response can occur at a moment’s notice.
Arkansas is divided into seven regions, each represented by its own Healthcare Emergency Preparedness Coalition: Metropolitan, Arkansas Valley, North Central, Northeast, Northwest, Southeast, and Southwest.
The seven Healthcare Coalitions (HCCs) serve facilities in all 75 Arkansas counties under the authority of the Arkansas Department of Health (ADH) and the Healthcare Preparedness Program (HPP), a grant program of the Administration for Strategic Preparedness and Response (ASPR), which is a division of the U.S. Department of Health & Human Services (HHS).
“These coalitions and partnerships coordinate efforts to prepare health care delivery systems for disasters and emergencies,” says Stephen Brown, NREMT, HPP Manager in the Arkansas Department of Health’s Office of
Preparedness and Emergency Response Systems. “They establish methods for efficient patient movement, maintain situational awareness, and promote resource-sharing among various health care entities.”
ARKANSAS’S HPP PROGRAM
The HPP program in Arkansas is guided by a leadership team that includes a Program Manager, Grant Coordinator, Medical Director, two co-leads from each coalition, Coalition Secretary, Coalition Readiness Response Coordinators (RRCs), coalition clinical advisors, and coalition members.
Each region has its own leadership team, made up of two regional leaders, one secretary, at least one clinical advisor, and one RRC.
These leaders meet twice a year, once in the fall and once in the spring, to provide updates on what has taken place in each region, share best practices and lessons learned during emergency response, and to plan for the HPP grant’s next budget year.
“HPP funding supports training and exercises that equip HCC members to manage real emergencies,” Brown explains. “Each HCC must consist of four core member
Regular drills help responders keep their skills sharp. Here, setting up a mobile hospital is practiced.
organizations: acute care hospitals, public health agencies, emergency medical services, and emergency management agencies. Additional health care and private organizations are encouraged and invited to join their regional coalitions.”
HEALTHCARE COALITIONS
The regional HCCs are collaborative networks of health care organizations and their respective public and private sector response partners. The HCCs serve as multi-agency coordinating groups to assist with preparedness, response, recovery, and mitigation activities related to health care organization disaster operations.
Each HCC plans, organizes, equips, trains, exercises, and evaluates emergency response for a variety of disaster scenarios and possibilities. If your community has hosted a mock disaster preparedness drill, you may have seen some of this planning, exercising, and evaluation activity in person.
During disaster response, the regional coalition leaders, RRCs, and coalition members provide multi-agency coordination in helping health care organizations face an unfolding crisis. This coordination may include either a response role as part of a multi-agency coordination group assisting with incident management (area command or unified command), or an active role in guiding decisions regarding support to individual health care organizations.
“Our work is vital,” says Emily Johnson, Arkansas Valley HCC Co-Leader and Mercy Clinic Manager at Mercy Hospital Fort Smith. “We assist our member facilities by supplying support when they need it. For example, if they are short on essential PPE (masks, gloves, gowns, etc.) we have supplies that we can provide. If we don’t have what they need, we assist by reaching out to our contacts to help find the resources they need.”
The leadership of each coalition strives to communicate the importance of emergency preparedness, Johnson says. “We send updates about upcoming issues facing our state/region, hold drills and meetings, and assist coalition members with fund request processes so they can purchase equipment that will make their facility more prepared and stronger [in disaster readiness].”
For example, the North Central region recently purchased a multi-use communications/morgue trailer. The trailer can be used for emergency communications, as it is equipped with a dispatch console. This allows on-site dispatching of law enforcement, fire, EMS, and Survival Flight ground and air units, as well as the ability to be used as a secure communications command center.
If needed as a mobile morgue, the trailer has significant cooling equipment. When not being used as a mobile morgue, the cooling equipment allows the trailer to double as a mobile clinic or vaccination distribution site, a cooling chamber for patients suffering from heat exhaustion, or a transportation and storage unit for vaccines and PPE.
WHAT IS THE HEALTHCARE PREPAREDNESS PROGRAM?
ASPR’s HPP provides leadership and funding through cooperative agreements to states, territories, and eligible major metropolitan areas to increase the ability of HPP funding recipients to plan for and respond to large-scale emergencies and disasters. The HPP is the primary source of federal funding for health care system preparedness and response and, in collaboration with state and local health departments, prepares health care delivery systems to save lives through the development of health care coalitions (HCCs).
HCCs bring together individual health care and response organizations in a defined geographic area, such as acute care hospitals, emergency medical service (EMS) providers, emergency management agencies, and public health agencies, to prepare health care delivery systems to respond to emergencies and disasters. HCCs collaborate to ensure each member has what it needs to respond to emergencies and other events, including medical equipment and supplies, real-time information, communication systems, and educated and trained health care personnel in the event of an emergency.



Solutions Designed for Healthcare Providers and Organizations
Achieve your goals with world–class people solutions



©



RELATIONSHIPS ARE EVERYTHING
Members of the HCC are representatives from hospitals, emergency management professionals, public health workers, advanced higher education (university and college experts), skilled long-term care facilities, law enforcement, fire departments, EMS, coroners, funeral directors, and other identified partners as designated by the 18 CMS provider types. They work together to prepare each facility and region for efficient response to emergency situations.
“Many times, members do not see or understand the RRC function until they require services,” says Andrew Hradesky, RRC for the North Central region. He explains that strong relationships form the foundation for each region’s preparedness activities. When a disaster strikes, coalition members contact their regional co-leaders, who then immediately contact their RRCs. This is when the constant planning, communication-building, and drilling pay off.
Successful disaster response coordination doesn’t happen on its own. The secret lies in constant training and preparation. Hradesky says his mantra is “’Exercise, Exercise, and Exercise!’ This includes communication, communication, and more communication, and then some training. Lead by example and lead by showing. This includes continuous relationship building, on-site visits, plan reviews, encouraging LEPC attendance within the county, and attendance at any annual EP forums across the state.”
Though most people take it for granted that health care facilities and others will respond quickly and efficiently in the face of a disaster, they may not realize the extensive training, preparation, and coordination that happens in the background, allowing emergency response to occur seamlessly.
Safeguarding the local community in the event of a disaster is always on the minds of hospital professionals in Arkansas. Emergency preparedness is a quiet, but mighty, example of community outreach that is in place in every hospital every single day.

Lyndsey Dumas serves as the Vice President of Education for the Arkansas Hospital Association.
RANDY ROGERS
CHRIS NEWKIRK
Saline Health System
Creating New Ways to Engage Our Communities
By DeAnn Thomas
Saline Health System engages with Benton and the surrounding communities with a creative combination of outreach programs each year. “One of the main goals of our outreach events is to demonstrate our level of care and commitment to this community,” says Char Boulch, Chief Nursing Officer. “We aren’t just fulfilling obligations; we truly want to make a difference in improving the overall quality of life here in Saline County and the surrounding areas. Interacting with people at events helps deepen our relationships with them so that they feel more confident in the care that we provide.”
BEAUTIFUL BEGINNINGS BABY FAIR
One of the most beloved new offerings is the Beautiful Beginnings Baby Fair held each spring. It’s an opportunity to bring parents, parents-to-be, and families together in

one place to learn about labor and delivery services from local obstetricians, and infant and newborn care from area pediatricians. Giving young parents the opportunity to meet and talk with the physicians who will be helping with their labor and delivery – and, later, caring for their children – is a popular aspect of the fair.
Beautiful Beginnings is really like a huge baby shower, and it offers an environment where it’s safe to ask questions of the experts, learn about area vendors who can offer products helpful to new parents, and celebrate the joy families bring to the community. Besides the classes that are offered, there’s a wealth of vendors and educational groups that cater to expectant families. And, of course, there are fun activities for kids and adults alike.
A food truck provides snacks and drinks, and kids’ activities include such things as a Build-a-Bear workshop (complete with adding the new bear’s “heart”) and a bubble house.
Adults enjoy the Baby Boot Camp Challenge, where new parents and parents-to-be can practice nurse-guided skills like diapering, safe sleep habits, and safe care habits. The Boot Camp allows parents to quell their fears and ask oneon-one questions of the nurses who help with the session.
And everyone enjoys the Maternity-to-Toddler Fashion Show, where community residents serve as the models and walk the runway.
“Our community has a lot to offer for growing families,” says Brynn Doddridge, Director of Women & Infant Services. “We’re excited to get to highlight all the different resources that are available.”
BOSOM BUDDIES BASH
Another popular outreach event is the annual Bosom Buddies Bash, held in the fall. This weekday event – to be held Tuesday, October 22 this year – celebrates the friendships of women and encourages friends to come together to receive their yearly mammograms and learn more about breast health – all while getting a little pampering on the side.
Kids and parents-to-be were invited to Build-A-Bear, adding a special, loving heart inside.
Washington Regional Meeting Specific Community Needs
By Brooke Morgan
Since its beginnings as a county hospital in 1950, Washington Regional Medical System has grown into the largest health care system in Northwest Arkansas with a 425-bed medical center, five Centers of Excellence and 45 clinic locations. Washington Regional’s mission is to improve the health of people in the communities it serves through high quality, compassionate care and wellness education. “As a locally governed, nonprofit health care system, community outreach is a large part of that mission,” Washington Regional President and CEO Larry Shackelford says.
To help meet the needs of the community, Washington Regional has developed outreach programs and partnerships designed to meet specific needs, including post-hospital care for unhoused patients, support for isolated seniors, and resources for those with cancer.
RECUPERATIVE CARE FOR THE UNHOUSED
Northwest Arkansas, like other regions, has seen an increase in the number of people experiencing homelessness. Doctors often face a difficult choice for patients who are unhoused. Many may need continued care after leaving the hospital but lack a safe place to go. The result is patients either choose to leave without getting the continued care they need or face extended stays in the hospital. “It would not be uncommon to see patients in our hospital for 20, 30, or 40 days that could have been discharged four days into their stay if they had a safe place to go,” Shackelford explains. “Our hospitalists saw a need for a place for those patients to receive care after being discharged.”
Members of Washington Regional’s hospital medicine group, including Drs. Michael Bolding, Jonna Dyer, Trey Becton, Jon McCowan, and Dustin Temple, partnered with New Beginnings, a nonprofit organization that works with chronically unsheltered people, to create A Place to Heal. The program provides respite care for patients who need post-

hospitalization services after discharge, such as physical therapy, wound care, or IV antibiotics. Hospitalists from Washington Regional regularly check on patients. The program is the first of its kind in the state.
“A lot of times, those experiencing homelessness will leave the hospital against medical advice for social reasons,” Dr. Michael Bolding says. “With this program, you could say, ‘I advise against you leaving, but if you do decide to do that, here's a place for you to go.’ Just knowing that I can discharge a patient from the hospital and know that I or one of my colleagues are personally going to go check on them at A Place to Heal provides peace of mind.”
A Place to Heal provides respite care for unhoused patients who need post-hospitalization services after being discharged.
FOUNDATION SUPPORTS SENIORS AND CANCER PATIENTS
The Washington Regional Medical Foundation’s two outreach programs – Senior Support in Action and the J.B. Hunt Transport Services Cancer Support Home – also serve community members in need. Senior Support in Action connects socially isolated seniors in Benton and Washington counties to their community through volunteer support. Volunteers can provide friendly visits, transportation for appointments or errands, chore assistance, and deliveries including food, household items, and hygiene products from the Senior Support in Action Pantry. Last year, Senior Support in Action served 68 clients, provided 1,058 nonmedical services, 152 trips to essential errands and appointments, 228 deliveries, and logged 11,616 miles while serving clients.
In 2023, Senior Support in Action introduced the Bridging & Belonging initiative. This grant-funded initiative gives Senior Support in Action clients and volunteers an opportunity to spend time together in the community while fostering a sense of belonging. Last year alone, 113 clients, volunteers, and guests participated in Bridging & Belonging activities. More information about Senior Support in Action can be found at wregional.com/ssia.
The J.B. Hunt Transport Services Cancer Support Home provides hope and comfort to those on a cancer journey. Located in a serene 4.4-acre setting near the Washington Regional Medical Center campus and many cancer treatment facilities, the 9,000-square-foot Cancer Support Home offers eight overnight guestroom suites and home-like amenities, a salon-style boutique with private dressing rooms, and a consultation room. In addition to those services, the Cancer Support Home provides breast health navigation services and early detection screenings. All services are offered at no cost, and clients do not have to be a Washington Regional patient to receive services.
“We cannot make cancer and all its burdens go away,” says Nancy Cozart, Washington Regional Medical Foundation executive director. “However, the programs and services at the Cancer Support Home are designed to eliminate barriers to care and provide support for an individual’s emotional, social, and financial well-being while walking on a cancer journey.”
Last year, the Cancer Support Home provided 1,420 nights of lodging, 1,285 boutique items including wigs and mastectomy supplies, and health education, information, and referrals for 2,356 clients. According to the National Cancer Institute, social support programs such as those provided at the Cancer Support Home can improve a patient’s quality of life and chances for survival. To learn more about the Cancer Support Home, visit wregional.com/csh.
As a community health system, the work Washington Regional does outside its hospital, clinics and other facilities is an important part of caring for others. “Our values include treating others as we would want to be treated,” Shackelford says. “By finding ways to meet the needs of our neighbors, these outreach programs help us live out those values while achieving our mission.”




Baxter Health
Safe Haven Baby Box, New Food Pantry

Baxter Health is the second hospital in Arkansas to join with Safe Haven Baby Boxes to provide a safe drop-off location for the babies of struggling mothers who can no longer provide for their newborn child.
The drop-box, which is located on the east side of Baxter Health’s hospital campus in Mountain Home, is connected to one of the hospital’s break rooms, ensuring that it will be monitored 24/7.
The Safe Haven Baby Box provides a discreet and anonymous way for mothers to leave their babies safely. The box is equipped with an alarm system that immediately notifies the hospital staff when a baby is left in the box. The hospital staff then rushes to the box to retrieve and care for the baby.
The new drop-box was created through the joint efforts of Safe Haven Baby Boxes, Baxter Health, members of the Mountain Home Chamber of Commerce 2022 Leadership Program, Baxter Health Foundation, Informed Choices Women’s Center, The Knights of Columbus, and St. Peter the Fisherman Catholic Church. The partnership aims to provide a safe and secure environment for mothers to legally leave their babies if they are not able to take care of them.
The installation of the Safe Haven Baby Box at Baxter Health is a testament to the hospital and their partners’ dedication to serving the community. It also shows the prioritization of the welfare of the mothers and the babies in their care.
NEW FOOD PANTRY
Brooke Morgan serves as Director of Content Marketing for the Washington Regional Medical System.
Baxter Health recently started a hospital food pantry as part of our Health Equity team. Employees donate food and money to stock a food pantry for underprivileged patients being discharged with a need for food in the home. In addition, the hospital provides a food and hunger resource guide that serves as a reference for people needing access to local food pantries. The guide lists pantry locations, hours of service, and any stipulations required to receive food services.

Parents who feel they must give up their newborns for any reason can do so safely and anonymously at the Safe Haven Baby Box at Baxter Health.
The J.B. Hunt Transport Services Cancer Support Home provides hope and comfort to those on a cancer journey with services offered at no charge.
Left: Senior Support in Action brings senior citizens and volunteers together. Here, a Bridging and Belonging event brings isolated seniors out into the community to enjoy interactions at the zoo.
White River Health
Working for Healthier Communities
By Sheila Mace
Community hospitals are an integral part of the cities and towns across Arkansas. Since 1976, White River Health’s (WRH) mission has been to improve the health of residents in the communities it is privileged to serve.
Hospitals impact health in the delivery of quality health care and community involvement. For example, sports physicals, the Children's Health Carnival, Camp WRMC, health fairs, the Health First Women's Health Expo, and cancer screening events are ways the hospital serves and connects with the community.
COMMUNITY ENGAGEMENT DIVISION ESTABLISHED
In 2019, WRH embarked on a journey to create healthier communities outside the delivery of medical care using an intentional, relational, and strategic approach. The Community Engagement Division consolidated community outreach efforts and focused on projects that improve access to care, promote physical activity and wellness, foster community partnerships, and provide employees with opportunities for service. WRH partners with local schools, colleges and universities, social services, and the business community to achieve our mission of creating healthier communities through education and outreach.
The Community Engagement Division also includes WRH Marketing, Foundation, and Volunteer Services. These departments are a natural fit to create a collaborative team to coordinate activities across WRH’s service area.

BECOMING A TRUSTED RESOURCE
The COVID pandemic required a shift in strategy. The group teamed with WRH Marketing to proactively manage information using social media and become a trusted, local source of information. The Marketing and Community Engagement team coordinated leaders, physician champions, residents, and other staff to voice public service announcements, record videos on managing mental health, explain treatments, and coordinate vaccination clinics. The community engagement team became a trusted partner with community organizations and a hub for coordinating employee community service.
WORKING WITH CHILDREN
The emphasis on community engagement in education is intentional. Helping children learn the
benefits of good nutrition and physical activity leads to healthier families and healthier communities. By reaching out to students, these programs reach parents, grandparents, and extended family members. WRH understands that teaching healthy behaviors creates a foundation and students need tools to implement what they are learning. The WRH annual 5K is a family friendly event benefiting area school food pantries. Schools are on the front lines of addressing food insecurity in the local communities. The event has raised more than $60,000 to address food insecurity while encouraging physical activity.
An important part of community engagement in the schools is fostering an interest in health care careers. Projects such as the Scrub Club expose students to careers in health care and connect the dots of good nutrition and physical activity to good health. Health care professionals from the Internal Medicine Residency program, nursing, and ancillary services create hands-on activities for students. The program also
White River Health's Cave City Scrub Club.
provides opportunities for service and to connect with the community outside a clinical setting. The experience is rewarding for students and staff and builds trust between health care workers and young patients.
IMPROVING ACCESS TO CARE
Improving access to care is an important part of the community engagement strategy. Traditional medical clinics may be in locations or have hours of operation that are inconvenient for patients and their families. Access to care can reduce use of the Emergency Department for non-emergency care and encourage earlier intervention in chronic disease management.
In the Batesville School District, WRH partners with the district to offer schoolbased clinics at each campus using telemedicine. Nurses are equipped with the technology and training to facilitate telemedicine visits with a WRH APRN. Parents can participate in the visit in person or remotely. This care is available to district personnel as well.
WORKING WITH COLLEGES
WRH has long been a partner in postsecondary education. Continuing this tradition, WRH partners closely with post-secondary education to develop new clinical degrees to close the gap where there is a shortage of health care workers and support students with clinical rotations, scholarships, and employment opportunities.
At Lyon College, WRH provides practical patient care experience to pre-professional students through our Health Coach Program. In the program, students learn about health care operations from WRH leaders. Students benefit from one-on-one
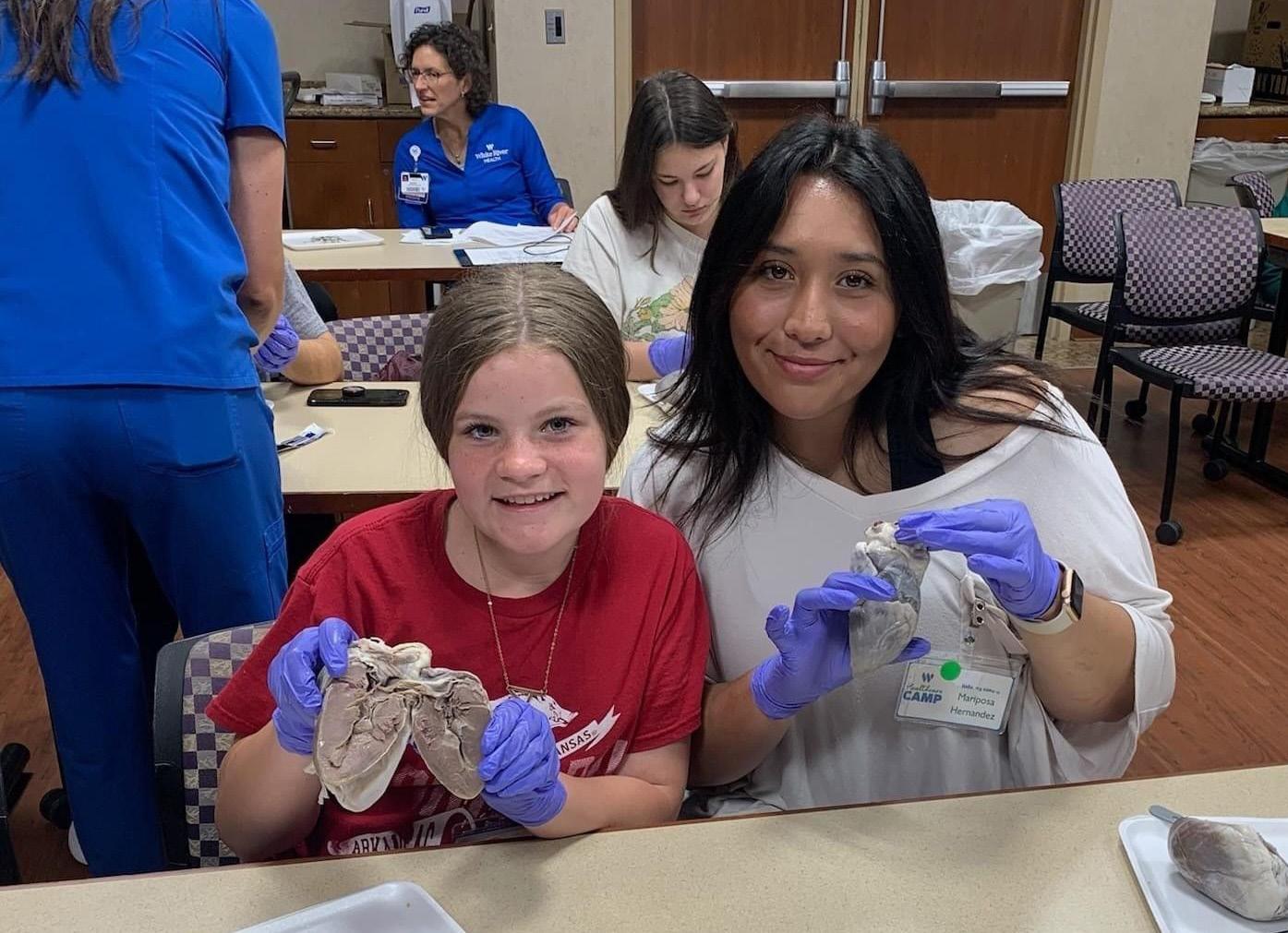
interaction with patients as they learn about chronic disease management and how economic, cultural, and social experiences can impact health and wellbeing in vulnerable populations. WRH is a partner in the development of a Bachelor of Science in Nursing degree at Lyon and looks forward to employing the nurses graduating from the program.
ENGAGING THE BUSINESS COMMUNITY
WRH Community Engagement in the business community focuses on relationships with fellow employers to address workforce needs in the community. Outreach efforts include basic first aid, CPR, and Narcan training for employers. Setting up flu shot clinics, mammography screenings, and wellness visits are services that improve health, reduce absenteeism for illness, and improve productivity.
Partnering with the business community is a way for leaders from across the community to come together and develop programs to move communities forward.
COMMUNITY DEVELOPMENT
The WRH team is active in local, regional, and state community development initiatives, partnering with communities and organizations on grants, short- and long-term development projects, and community strategic planning.
It is an honor to serve on the Batesville Area Chamber of Commerce, Spring River Chamber of Commerce, Hometown Health Coalition, Arkansas Behavioral Health Integrated Network, and others. The Community Engagement division allows WRH to be a partner with organizations doing extraordinary work for residents in the communities the hospital is privileged to serve. The results are clear: Healthier communities are created through intentional, relational, strategic community engagement.

Sheila Mace serves as the Marketing Department's Public Relations & Foundation Development Coordinator for White River Health.
White River Health's Health Camp, 2023.
Mercy Hospitals Arkansas
Enhancing Health Care Access in Arkansas
By Mardi Taylor and Nate Kuester
The mission of Mercy’s healing ministry extends far beyond the walls of its hospitals. With a commitment to serving communities, Mercy addresses the unique health needs of the people it cares for. Comprehensive outreach programs across Mercy communities in Northwest Arkansas and Fort Smith and critical access hospitals in Berryville, Booneville, Ozark, Paris, and Waldron exemplify this dedication.
Father Paul Fetsko, Vice President of Mission for Mercy Arkansas Communities, says care provided through Mercy extends beyond basic health care.
“It’s about taking care of all of a person’s needs, including their most basic needs,” he says. “Mercy’s mission includes providing compassionate care and exceptional service, and our outreach projects are designed to do just that.”
COMMUNITY HEALTH WORKER (CHW) PROGRAM: A BEACON OF HOPE
A cornerstone of Mercy’s outreach efforts is the Community Health Worker (CHW) program. Corina Huston, director of community health and access, says, “Mercy’s CHWs are true advocates, bridging the gap between patients and health care providers. They empower patients to navigate our health care system, understand their needs, and access necessary resources.”
Mercy Hospital Northwest Arkansas employs five CHWs: two in the emergency department, two in clinics and one serving Berryville exclusively. Fort Smith is home to four CHWs: one covering all critical care hospitals/clinics, one in the emergency department, one in the clinic, and one who splits time between the emergency department and Riverview Hope Campus, a homeless shelter that features a Mercy primary care clinic. The CHW program fosters relationships with community partners to provide essential services such as food assistance, transportation, and financial support.
In the past year, CHWs in Northwest Arkansas alone assisted 3,171 patients, connecting them with critical health care services and support. “We help patients understand that they can visit primary care or urgent care for nonemergency issues, which is often more cost effective,” Huston says.
FORT SMITH COMMUNITY HEALTH COUNCIL
The Fort Smith Community Health Council, a collaboration among Mercy Fort Smith, community members, and other local nonprofits, aims “to provide and continually advance the health and well-being of individuals and communities by addressing the social, economic and environmental determinants of health equity,” (from the Council’s mission statement).
Established in 2016 through the Robert Woods Johnson Foundation, the council advises and supports health care needs for Sebastian County residents. The council collaborates with Mercy Fort Smith and other health care organizations on Community Health Improvement Plan (CHIP) assessments every few years. Key areas of focus have included foster care, access to care, nutrition, mental health, obesity, and smoking/vaping.

Mercy Hope Campus sponsors an outreach flu clinic for its homeless shelter patients.
The council also promotes health care initiatives in the River Valley, including local health fairs, prescription drug takeback events, and more. Mercy often hosts these events, and co-workers frequently serve as volunteers.
VESTIDO ROJO: CELEBRATING HISPANIC WOMEN’S HEALTH
One of Mercy’s standout community events is the Vestido Rojo, a day dedicated to promoting health awareness among Hispanic women. This event, in collaboration with the American Heart Association, provides vital health information, screenings, and resources to a population that faces significant barriers to health care access.
“Vestido Rojo is about celebrating and empowering Hispanic women by giving them the tools and knowledge they need to take control of their health,” Huston explains. “We offer free health screenings, educational workshops and a supportive community atmosphere.”
Seven hundred Hispanic women participated in the most recent event, with Mercy providing 236 health screenings, including lipid, HbA1c, blood pressure, and atherosclerotic cardiovascular disease (ASCVD) risk scores. Additionally, 28 Mercy staff members volunteered their time to assist with screenings, exemplifying Mercy’s strong commitment to community health.






(Continued on page 58)
45 YEARS
OF HEALTHY GROWTH



Conway Regional
WALKING TOWARD WELLNESS: Wellness Walk and Talk
By Lauren Norris

The Conway Regional Wellness Walk and Talk program represents an ongoing effort to engage the community in accessible health and wellness activities. Held at the scenic Tucker Creek trail adjacent to the Conway Regional Health and Fitness Center, this initiative combines health education with physical activity in a community setting.
During each session, participants gather to receive valuable health tips from experts on topics such as heart health or stress management, before embarking on a walk along the trail or indoor walking track. This approach not only promotes physical activity but also fosters community interaction and education in a relaxed environment.
Recent walks include a minority health walk with Kuna Okong, MD, a mental health walk with Thad Hardin, MD, and a breast cancer awareness walk with Kala Slaton, MD.
The Wellness Walk and Talk program is designed to be inclusive, catering to individuals of all ages and fitness levels. The act of walking itself is a simple, yet effective, way to improve overall health, offering benefits such as weight management, reduced risk of chronic diseases, and enhanced mental wellbeing. The American Heart Association and the Centers for Disease Control and Prevention endorse 10,000 steps per day to ward off disease and stay fit.
Each walk serves as a practical demonstration of easy steps individuals can take towards a healthier lifestyle, emphasizing the importance of regular physical activity. The program also serves as a unique opportunity for participants to discuss personal health goals and challenges with professionals, making wellness more attainable and personalized.
While the program is still growing and evolving, it embodies Conway Regional’s commitment to making health resources accessible to everyone. By providing a platform for regular physical activity and expert health advice, the program aims to strengthen community ties and encourage a healthier lifestyle among participants.
This initiative is part of Conway Regional's broader mission to ensure that all community members can lead healthier lives, reflecting the hospital's dedication to wellness and preventive care.

PATIENT CLOTHING CLOSET: OUTREACH FROM WITHIN
At Mercy Hospital Fort Smith, patients often do not have clothing available to them when they are discharged. That’s where the patient clothing closet comes in.
Patients’ needs are identified by their care team, whose members then match patients up with items from the closet. The closet is stocked with brand new men’s and women’s socks and underwear, sweatpants, and T-shirts in sizes small through 3X. Toiletries such as toothbrushes, soap, and other items are also available.
“We are making an effort to honor patients’ dignity by not discharging them in paper scrubs,” says Hayley Howard, manager of strategic initiatives at Mercy Fort Smith. “The patient clothes closet fits into Mercy’s mission because we are acknowledging someone in need and providing clothing to them in a situation where they otherwise wouldn’t have any.”
Mercy Health Foundation’s Women With a Mission provides funding for the closet, but donations of new items are always welcome. In February, Mercy coworkers took part in a drive where items were purchased for the closet from an Amazon wish list. Additional clothing drives are in the works.

Dr. Kuna Okong speaks to a group about minority health before they set off together on their Wellness Walk and Talk session.
Clothing for patients in need is collected through Mercy Fort Smith Clothes Closet drives.
Lauren Norris serves as Director of Marketing for the Conway Regional Health System.
ADDRESSING RURAL NEEDS
Another vital aspect of Mercy’s outreach is its rural programming. In Berryville, the “People Helping People” program, supported by local foundations, identifies patients needing medication assistance. These efforts ensure that patients receive their first month of medications following their discharge free-of-charge, and arrangements for their future medication needs are addressed, enabling them to stay on track with their treatment plans. Huston says, “Through our programs, we offer medications at reduced or no cost, often delivering them directly to patients’ homes.”
In rural areas such as Booneville and Waldron, community input is a vital part of Mercy’s ability to recognize residents’ biggest needs and find ways to address them. Rural coalitions help conduct frequent Community Health Needs Assessments (CHNA), similar to those done through the Fort Smith Community Health Council for the larger Fort Smith area.
In May 2022, Mercy Hospital Booneville completed a comprehensive CHNA, which considered input from the county health department, community members, members of medically underserved, low-income, and minority populations, and various community organizations representing the broad interests of the communities of Booneville and Magazine. Health care priorities as determined by the 2022 assessment include mental health, substance use, and transportation for health care services.
In Waldron, the Scott County Health and Education Coalition’s mission statement is “to give hope and provide education and resources to build and maintain a healthy Scott County.” Its key focus areas are similar to those in Booneville and include substance abuse, mental health, and transportation for health care services.
IMPACT ON THE COMMUNITY
The impact of these programs is profound. In the past year, CHWs alone have touched the lives of thousands of patients, providing access to critical health care services. The Vestido Rojo event engaged 700 participants, fostering greater community health awareness.
“The most significant benefit of our CHWs is their ability to advocate for both the patients and our clinical staff,” Huston notes. “They spend quality time with patients, helping them understand health care and empowering them to ask essential questions.”
As Mercy continues to expand and enhance its outreach efforts, the dedication and compassion of its team remain unwavering. Mercy Arkansas is proud to lead these initiatives, ensuring that quality health care is accessible to all.

Mardi Taylor serves as Senior Communications Coordinator for Mercy Fort Smith.
Nate Kuester serves as Mercy Northwest Arkansas’s Senior Media Relations and Communications Specialist.
LIVING IN A HOUSE OF CARDS – DEALING WITH ACES IN OUR LIVES

Hospitals and Community Outreach
By Kay Kendall
Hospitals play a key role in a community, often serving as one of its largest employers. Hospital quality and services are included as a factor in the relocation of industry headquarters, plants, or service centers to new communities. Families also want to know the kinds of health care services that would be available to them should they choose to relocate to a new home. An often-overlooked contribution that hospitals make to the fabric of a community’s culture is their role in community outreach.
The Baldrige Excellence Framework has a related core value around societal contributions in all three versions of the criteria, but the health care version ties it to community health. This makes perfect sense since health care organizations have core competencies in areas that can contribute to community health.
The description of the value emphasizes the need for organizations to go beyond meeting regulatory requirements
and minimal compliance. “Such leadership and support might include efforts to determine and address societal determinants for health and to provide both charity care and investment in your local community and beyond. … It might also involve being a role model for addressing socially important issues, such as diversity, equity, and inclusion; practicing resource conservation; reducing your carbon footprint; performing community service and charity; improving health care industry practices; and sharing nonproprietary information.”1
MORE THAN COMMUNITY NEEDS ASSESSMENTS
While most hospitals are required to conduct a Community Needs Assessment every three years, many hospitals and health systems keep their fingers on the pulse of emerging needs and those that arise in the interim.
This was evident with the rapid pivot that we saw in health care with the advent of the COVID-19 pandemic. From providing personal protective equipment (PPE), to offering drivethrough rapid testing, to staffing vaccination clinics, hospitals served a critical role in various aspects of community outreach in addition to more traditional outreach such as high blood pressure screening, diabetes clinics, and caregiver support groups.
COMMUNITY OUTREACH AND BRAND AWARENESS
One aspect of community outreach that cannot be overstated is the impact it has on brand awareness, particularly in a crowded health care market.
Ryan Owens, Texas-based Methodist Health System Assistant Vice President, Public Relations says, “North Texas is a very competitive health care market that is rapidly growing. We focus on putting on events, frequently featuring physicians, on a variety of topics that will educate the public and also attract new patients to Methodist hospitals.”
Lexy Young, Methodist Dallas Center’s Director, Community and Public Relations, adds, “We also look to support events that raise awareness of some of the diseases we treat in our facilities. At Methodist Dallas, for example, we sponsor the annual pancreatic cancer walk with a robust team of physicians and other caregivers who walk, playing an active role so the community knows that Methodist cares.”
While many activities are coordinated at the system level, often creative ideas are generated at the local level and sponsored by individual hospitals.
For instance, Richardson is a thriving community with a clear focus on the arts. Methodist Richardson is a sponsor the annual Wildflower Arts and Music Festival where thousands of people attend. In another, related innovative approach, the hospital features the work of local artists in several well-traveled hallways throughout the facility, giving that particular hospital another venue to showcase local artists’ work.
NEW WAYS TO VIEW COMMUNITY OUTREACH
Charity care is also a vital part of hospitals’ community outreach. “Last year alone, Methodist Health Systems provided $182 million in unreimbursed charity care,” Owens says. In addition, its Golden Cross Clinic gathers and distributes donations of toiletries and other personal care items at the same time the system provides affordable or no-cost care.
I recently read about hospitals in rural Mississippi that have come up with another way to provide community outreach in an area where health disparities abound. Delta GREENS –short for Growing a Resilient, Enriching, Equitable, Nourishing food System –aims to establish a local food economy in the Mississippi Delta. The project is a collaboration between the Friedman
Notes 1 Baldrige Performance Excellence Program. 2023—2024 Baldrige Excellence Framework® (Health Care): Proven Leadership and Management Practices for High Performance. Gaithersburg, M.D.: U.S. Department of Commerce, National Institute of Standards and Technology. https://www.nist.gov/baldrige.
2 https://www.modernhealthcare.com/community-health-centers/food-is-medicine-clinical-trial-mississippi-delta?adobe_mc=MCMID%3 D83705919885430923662983505848559429748%7CMCORGID%3D138FFF2554E6E7220A4C98C6%2540AdobeOrg%7CTS%3D17156 24653&CSAuthResp=1%3A%3A303103%3A7461%3A24%3Asuccess%3A07089A102075B09AC245C1829D120D84
School of Nutrition Science and Policy at Tufts University, the Reuben V. Anderson Institute for Social Justice at Tougaloo College, Delta Health Center and the Center for Science in the Public Interest.2 This win-win model helps local farmers sell their crops of healthy fruits and vegetables to health care systems that “prescribe” them to patients with diabetes and certain forms of cancer. What does your hospital do for community outreach? Can you engage your staff in generating creative ideas that might particularly resonate with your unique community needs and interests? The Methodist Health System’s Public Relations Department launched a robust online content hub, ShineOnlineHealth.com, where collaborations with physicians and other caregivers create timely health articles and highlight patient success stories. (https://shineonlinehealth.com/) Could you follow their lead?


The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement.
As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 24 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com

COMMUNITY OUTREACH: The Impact of Giving on Personal Health and Company Well-Being
By Chad Rodgers, MD
“Philanthropy” translates to “love of humanity." Most people think of philanthropy as large monetary donations to nonprofit organizations such as the arts, humanitarian needs, or specific health-related causes.
However, philanthropy can include more than just money; it often involves giving of yourself with your time and your talents. These efforts not only benefit the recipient but also benefit the giver. The adage, "It is better to give than receive," especially rings true when discussing health benefits. We can all be philanthropists in our own way and receive the benefits of giving.
PARTNERING WITH COMMUNITIES
AFMC has been serving Arkansans and the health care community for fifty years. Our mission is to promote and inspire innovation in health, wellness, and technology through partnerships in our communities. We began as a peer review organization but have grown into a multi-faceted company with more than 300 employees.
As a company focusing on wellness and health improvement, we understand and observe how most
determinants of health care outcomes occur outside of hospitals and clinics, in the communities where we work, live, and play. We are an Arkansas-based company with people living and working in every county in the state and beyond!
AFMC has "HEART" values, which include honesty, excellence, accountability, respect, and teamwork. The heart represents the core function of keeping the body going and highlights the importance of keeping that heart healthy. The wellness and well-being of employees and their communities are at the core of that "HEART."
There are many health benefits to giving and being involved in one's community. Research has shown that it can lower your blood pressure, improve your mental health, promote the development of motor skills, and, as a result, promote a long and happy life.
For the benefit of our employees and the communities they serve, AFMC has supported many nonprofit organizations and educational organizations throughout the years that support our mission. We provide education and evaluation services to reach our goal of “healthy people, healthy businesses, healthy communities."
Team AFMC paddles in the 2023 River Cities Dragon Boat Festival race, raising over $2,400 to benefit the Children’s Protection Center.
AFMC CARES
Expanding on our history of giving, AFMC has implemented a company-wide program, AFMC CARES (Community, Advocacy, Resources, Education, Services). To maximize our impact on people, businesses, and communities, we organized our philanthropic efforts into a giving program that promotes employee personal giving and involvement and corporate giving and involvement. By ensuring that our giving aligns with our mission, "HEART” values, and contract obligations, we can prioritize our giving for the maximal benefit of our customers and the people served.
One component of AFMC CARES includes a matching program where employees can give to a nonprofit of their choice in their community, and AFMC will match up to a pre-determined amount per employee per year.
In addition to that, AFMC employees are encouraged to give their time to nonprofit organizations and other volunteer activities in their hometowns, including coaching their child’s sports team, being involved in civic and faith-based activities, and becoming involved with community initiatives.
Employees are encouraged to share their "philanthropic" choices on our intranet, "The Social Hub." This promotes good morale and camaraderie among our employees and lets their co-workers know what interests are important to them. It is also an excellent way for employees to build their network in the community and increase social awareness.
Our corporate giving includes some long-held relationships with other health care entities. Through our work for Arkansas Medicaid, AFMC can support health education conferences and events related to our work for the state, benefitting providers and beneficiaries. AFMC often provides additional support for meetings and events that align with other AFMC work and priorities through financial support, education, and resources. A good example includes our effort to increase awareness of Adverse Childhood Experiences and the importance of resilience. Our staff's expertise is shared with health care providers, educators, and community members. AFMC staff members have participated in many healthrelated walks and fundraising events.

Many of our employees give their time and expertise to boards and commissions, nonprofit organizations, and to many programs throughout the state of Arkansas. Programs sponsored by the state are directly related to our work at AFMC. They are primarily health-related and provide professional growth opportunities for our employees.
AFMC CARES was established to meet the needs of the company, its employees, our customers, and the people we serve. Through these philanthropic efforts, we hope to give back to the state in which we live, work, and play. And we hope to promote a healthier future for all.

Chad Rodgers, MD, FAAP , serves as Chief Medical Officer for AFMC. AFMC is a private, nonprofit organization focused on improving health and health care through trusted, committed private and public partnerships. Founded on AFMC's mission, our experienced and dedicated leadership team and staff have delivered value to our customers and partners for over 50 years. To learn more about AFMC, visit www.afmc.org.

The AFMC HEARTbeats walked in the recent American Heart Association Heart Walk, raising $1,174 for the Heart Association.


What does it mean to be taken care of?
At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and to help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.
LOOKING FORWARD TO THE NEXT 75 YEARS OF
building places for healing


For the past 75 years, we’ve completed projects of all types and sizes for healthcare facilities — delivering high quality work to fulfill our client’s vision and needs.
When Conway Regional Health System wanted to add a new 24-bed intensive care unit, they enlisted Nabholz’ help. The new ICU features 330-square-foot patient rooms and cutting-edge equipment, ensuring patients receive the highest quality care.
CRHS, Intensive Care Unit
