

IMPROVING MATERNAL HEALTH

in taking care of the legal, so you can take care of the patients.
We've been serving the legal needs of the Arkansas healthcare industry for more than 120 years.
• Medical Malpractice Defense
• Healthcare Transactions & Employment Agreements
• Government Relations & Administrative Proceedings
• Licensing, Privileging & Peer Review
• Labor & Employment Concerns
• HIPAA Privacy & Security
• Stark I and II & Anti-Kickback Statutes
• Medicare/Medicaid & Insurance Reimbursement
• Telehealth & Remote Healthcare
• Long-Term Care & Skilled-Nursing Defense
• Defense of Claims Against Pharmacies & Pharmacists
Your Arkansas Healthcare Law Team WE BELIEVE




IMPROVING MATERNAL HEALTH

ARKANSAS HOSPITALS
Arkansas Hospitals is published by The Arkansas Hospital Association 419 Natural Resources Drive | Little Rock, AR 72205
To advertise, please contact Brooke Wallace magazine@arkhospitals.org
Becca Bona, Editor in Chief
Nancy Robertson, Senior Editor & Contributing Writer
Katie Hassell, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-elect
Michelle Krause, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Rogers / At-Large
Chris Barber, Jonesboro
Connie Castleberry, Camden
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
Tommy Hobbs, Clarksville
Charlotte Jackson, Searcy
Eric Pianalto, Rogers
Brian Thomas, Pine Bluff
Matt Troup, Conway

Cody Walker, North Little Rock
EXECUTIVE TEAM
Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO




Improving Maternal Outcomes in Arkansas
The U.S. has the poorest record on maternal outcomes of the world’s high-income nations, and in the area of maternal health, Arkansas consistently ranks last or almost last among the 50 states. More must be done to increase access to care and to provide for the prenatal, safe delivery, and postpartum needs of Arkansas moms.
Pregnant people trust their local hospitals to provide safe maternal health care. Across Arkansas, hospitals are doing all they can, not only to serve the medical needs of their communities and offer emergency care and services, but also to provide care at each stage of pregnancy.
Yet Arkansas’s maternal health crisis continues.
We all recognize that hospitals can’t solve this crisis alone. Increasingly, the cost of providing care is not covered by reimbursements from Medicaid and private-pay insurers. There are hospitals in our state, especially in rural areas, which are finding it fiscally impossible to maintain dedicated labor and delivery units as reimbursement rates remain locked and OB/GYN physicians leave their rural care practices.
The Arkansas Hospital Association (AHA) is working with the legislature and with the Department of Human Services (DHS) and its Department of Medicaid Services to develop new policies addressing these reimbursement roadblocks.
In the past, hospitals could sometimes shift gains from more profitable service lines to help cover the costs of maintaining their labor and delivery units. This is increasingly rare as reimbursement rates for all service lines remain stagnant while costs in every division of health care are rising dramatically.
No community can survive with only one provider of obstetrical care, and many rural OB/GYN physicians are leaving for larger cities where they can share coverage of their patients. We are working to address recruiting challenges that communities, particularly those in rural areas, experience when seeking to draw OB physicians and other trained professionals.
The legislature, DHS, hospitals, and the AHA are looking for solutions to

stop the downward spiral affecting maternal health in Arkansas: OBs need to be associated with hospitals that can provide maternal health services. Hospitals cannot continue to fund maternal health services when reimbursement rates from Medicaid Services and private-pay insurers are not adequate to cover costs. And communities cannot recruit OB physicians if there are not hospitals nearby that can support maternal health units.
During the upcoming legislative session, we’ll be working with legislators to address these challenges. And we are continually working with DHS in our joint endeavor to meet the medical needs of Arkansans, whether they’re in our most rural communities, in metro areas, or someplace in between.
To specifically help our hospitals, this issue of Arkansas Hospitals offers hands-on resources for improving and maintaining maternal health units, and we offer an in-depth look at the new DHS maternal health report, “Healthy Moms, Healthy Babies.”
The AHA is front and center in the fight to improve maternal outcomes in Arkansas. You can count on us to be your voice with legislators as we make hospitals’ needs known, and we continue our work daily with hospitals as they seek to provide the best care possible for all of the patients of Arkansas.

Bo Ryall President and CEO Arkansas Hospital Association










AFMC – A Trusted Resource for Arkansas Providers.




With 50+ years of experience and expertise, our dedicated team has a successful history of delivering exceptional value to Arkansas providers.
• Contact Center Services: Assisting Clients with Access to Care
• Data Sciences: Better Data for Better Health Care



• Outreach Services: A Lifeline to the Provider Community
• Practice Transformation: Your Guide to Value Based Care Success
• Security Risk Analysis: Because Patient Trust Starts with Secure Data
• Event Planning Services: Memorable Events, Minus The Stress
Visit afmc.org to find out more.

Let us help you plan your next conference, meeting, or community event – contact us to reserve your spot! Visit afmc.org/events for more information. Host Your Next Event in
Style at the
District Event Center
Conveniently located in downtown Little Rock, our newly renovated event space offers free parking, seating for up to 100 attendees, a state-of-the-art A/V system, virtual conferencing options, and a fully equipped catering kitchen.
A Solid Resource
It feels like only yesterday that I was introduced to you as Editor in Chief of Arkansas Hospitals magazine. It’s been my honor to work with each of you as, together, we tackled health care challenges in Arkansas, illustrating their impact through articles from and about our member hospitals and offering ideas and resources from experts in the field.
Nancy Robertson, our Senior Editor, has been my partner in sharing these stories. Nancy’s association with the magazine spans the past 20 years. Many of you have worked with her and come to rely upon her writing and editing skills. Nancy recently announced her retirement; this is her final issue of the magazine. I am witness to her joy in writing our leadership profiles, working with national experts and Arkansas contributors, and the fulfillment she feels in helping our hospitals gain resources and insight through the pages of Arkansas Hospitals
This is also my last issue of the magazine. As I move on to another role in the health care field, I am happy to introduce you to Becca Bona, AHA’s new Director of Communications and Editor in Chief of Arkansas Hospitals. Becca brings a fresh perspective and is dedicated to continuing the magazine’s legacy of relevant storytelling and advocacy.
Thank you for the privilege of serving you and for your trust in me over the years.
AAshley Warren Editor in Chief

s I step into my role as Director of Communications for the Arkansas Hospital Association, I want to recognize the exceptional work of my predecessor, Ashley Warren. Her leadership continued Arkansas Hospitals’ long tradition of bringing to light articles that matter most to hospital leaders, clinicians, health care advocates, volunteers, and AHA members across the state.
This issue of the magazine is dedicated to a critical topic: improving maternal health. Arkansas faces one of the highest maternal mortality rates in the nation, but through innovation, collaboration, and advocacy, change is happening. We examine the “Healthy Moms, Healthy Babies” report by Governor Sarah Huckabee Sanders’s Strategic Committee for Maternal Health and provide links to maternal health resources from the American Hospital Association. Additionally, we introduce the Arkansas Perinatal Quality Collaborative and highlight how two Arkansas hospital systems are addressing today’s maternal health challenges.
I look forward to partnering with you, our readers, as we present stories of the resilience, ingenuity, and commitment that define Arkansas health care. Thank you for your continued support of this publication and the vital work it represents.
Becca Bona Incoming Editor in Chief


2025 Calendar

JANUARY
January 9
Arkansas Hospital Auxiliary Association (AHAA) Board Meeting
AHA Headquarters
January 10
AHA Board Meeting
AHA Headquarters
January 15
AHA Services Webinar “Navigating the Healthcare Affordability Maze” Hosted by AblePay Virtual Event
January 21
340B Quarterly Meeting Virtual Event
FEBRUARY
February 14
AHA Board Meeting
AHA Headquarters
February 19

AHA Services Webinar “The Nursing Residency Program” Hosted by Vizient Virtual Event
MARCH
March 13
Arkansas Hospital Auxiliary Association (AHAA) Board Meeting AHA Headquarters
March 14
AHA Board Meeting
AHA Headquarters
Register for AHA Events Online!


Employees of AHA member hospitals can now log in to www.arkhospitals.org and register for events online.

Joyner Kersee

PAM BROWN HONORED BY Great 100 Nurses Foundation
The Arkansas Hospital Association (AHA) is proud to announce that Pamela Brown, RN, BSN, CPHQ, CPPS, the association’s Vice President of Quality and Patient Safety, has been recognized by the Great 100 Nurses Foundation as one of this year’s Great 100 Registered Nurses in Arkansas. This prestigious award celebrates her exceptional dedication to the nursing profession, her commitment to patient care, and her role in mentoring future health care professionals.
The Great 100 Nurses Foundation, established to recognize and celebrate nursing excellence, honors nurses who demonstrate concern for humanity, dedication to their profession, and a commitment to mentoring others. Brown exemplifies these qualities through her tireless work at the AHA and her ongoing efforts to enhance patient safety and quality of care across the state.
"Pam’s recognition by the Great 100 Nurses Foundation is a testament to her unwavering dedication to improving health care in Arkansas," says Bo Ryall, President and CEO of the Arkansas Hospital Association. "Her leadership and her passion for patient safety and quality are truly inspiring, and we are incredibly proud to have her as part of our team."
With 37 years of experience in the nursing field, Brown has been instrumental in advancing quality and patient safety initiatives at the AHA. Her contributions have significantly impacted the health care landscape in Arkansas, ensuring that hospitals and health care providers can access the information and resources they need to deliver the highest standard of care to their patients.
The Great 100 Nurses Foundation honored Brown and the other distinguished nurses at the annual celebration event on October 8, 2024, in Little Rock. This event brings together health care professionals, community leaders, and families to celebrate the achievements and contributions of these outstanding nurses.

Pamela Brown, RN, BSN, CPHQ, CPPS
HOSPITAL NEWSMAKERS

Howard Memorial Hospital recently celebrated its 75th anniversary serving Nashville and the southwest Arkansas area. Included in the event were tributes to the hospital’s recognition as one of the Top 100 Critical Access Hospitals in America (Chartis Center for Rural Health) and being recognized by Becker’s Healthcare as one of the nation’s top 350 cleanest hospitals.
The University of Arkansas for Medical Sciences (UAMS) is the recipient of a federal grant that will provide up to $2.4 million over the next four years to reduce the high rates of maternal and infant deaths in Arkansas’s Delta region. The initial grant from the U.S. Department of Health and Human Services is for $600,000 for one year and can be renewed for up to four years. The grant will fund a combination of education, training, outreach, and preventive health services focusing on the Helena-West Helena, Lake Village, and Pine Bluff areas.
The UAMS Historical Research Center recently opened a new collection, “Making a Difference: The M. Joycelyn Elders, MD Collection,” which is a digital collection documenting the career of U.S. Surgeon General Dr. Joycelyn Elders. Elders, who serves as an emeritus professor of pediatrics and distinguished professor of public health at UAMS, served as U.S. Surgeon General from 1993-1994, and was the first African American, the second female, and the first Arkansan appointed to the post.
Becker’s Healthcare has named four Arkansas Hospital Association member hospitals to its Top 350 Cleanest Hospitals in America list. AHA member hospitals earning the award are Howard Memorial Hospital (Nashville), Magnolia Hospital (Magnolia), North Arkansas Regional Medical Center (Harrison), and the VA Medical Center (Fayetteville).
The UAMS Winthrop P. Rockefeller Cancer Institute has been designated as a Center of Excellence by the Myelosdysplastic Syndromes (MDS) Foundation, making it Arkansas’s only medical center to become part of the foundation’s referral network of the top bone marrow disorder treatment centers in the world.

Howard Memorial Hospital celebrated its 75th anniversary and its ranking among the Top 100 Critical Access Hospitals in the United States with a special event September 20. Visiting after the program were (from left) Bill Craig, CFO; Shelby Frachiseur, Director of Human Resources; Chris Stuard, CNO; Stacy Harberson, COO; Dr. John Hearnsberger, CEO; Beth Schooley, Director of PI/Compliance/Risk Management; and Sandy Webb, Administrative Director. (Photo courtesy of Southwest Arkansas Radio)
UAMS recently opened a new historical collection chronicling the life and career of U.S. Surgeon General Joycelyn Elders, MD.

North Arkansas Regional Medical Center has been awarded a $398,346 Rural EMS Training Grant from the Substance Abuse and Mental Health Services Administration (SAMHSA). The two-year grant will support recruitment and training of Emergency Medical Services personnel with a focus on addressing substance use disorders and co-occurring disorders in Boone and Newton counties and the surrounding area.
St. Bernards Medical Center has earned Arkansas’s first “Pediatric Ready” status for emergency care provided at nonpediatric hospitals, achieving “Gold Tier Recognition” from the Arkansas Department of Health. The St. Bernards emergency department applied for and received the designation through the Arkansas Emergency Medical Services for Children State Partnership program. The hospital honored its pediatric emergency team and celebrated its newest designation with a ceremony on October 2.
Mercy Fort Smith held its third annual Inclusive Hiring Event in celebration of National Disability Employment Awareness Month on October 7. The event focused on job candidates with disabilities and featured an accessible and accommodative interview space where candidates could learn about Mercy’s opportunities, as well as additional information on resources for individuals who experience barriers to employment due to a disability.
The North Arkansas Regional Medical Center team is receiving a SAMHSA grant that will help enhance EMS training focused on substance use disorders.

The Regional Policy Board 7 of the American Hospital Association held its fall 2024 meeting at the Capital Hotel in Little Rock September 19-20. Arkansas Hospital Association President and CEO Bo Ryall represented Arkansas at the meeting, alongside Troy Wells ( Baptist Health ) and Marcy Doderer (Arkansas Children's). Topics covered in the two-day meeting included a briefing on the activities of the Coalition to Strengthen America’s Healthcare, the aftermath of the Change cyberattack, policy and advocacy next steps on health plan accountability, the impact of drug shortages and potential solutions, access to maternity care in rural areas, and other challenges.
Wadley Regional Medical Center-Hope is now operating as Southwest Arkansas Regional Medical Center. The hospital was saved from closure through a joint effort of the City of Hope, Hempstead County, and Pafford Medical Services. The hospital was previously operated by Steward Health Care.
Angie Longing, MHSM, BSN, RN, NE-BC, is the new president of CHI St. Vincent Morrilton. She will additionally continue to serve in her ongoing role as Senior Vice President and Chief Nurse Executive for the CHI St. Vincent system. She is a board-certified nurse executive and was honored with the prestigious DAISY Lifetime Achievement Award earlier this year.
The Mercy Hospital System is working with the Alice L. Walton Foundation, the Cleveland Clinic, and the Heartland Whole Health Institute in a 30-year, $700 million affiliation agreement that includes creating a cardiovascular center of excellence in Rogers.
College-educated Black women are 5.2 times more likely to die from pregnancy-related issues than the same educational attainment and 1.6 times higher than the rate for white women with less than a
IMPROVING Maternal Health in Arkansas
Top Causes of Pregnancyassociated Mortality, 2022 Timing of Pregnancy-related
Maternal health is under the microscope as, again this year, the United States continues to have the highest rate of maternal mortality of any of the world’s high-income nations. Among the 50 states, Arkansas has one of the highest rates of maternal mortality, and many of these deaths are preventable.
Improving access to care is seen as a monumental step in the effort to boost maternal health outcomes in Arkansas. Addressing maternal health needs is a top priority for Arkansas leaders not only in the field of health care, but also for Governor Sarah Huckabee Sanders, the Arkansas legislature, and a number of non-governmental organizations.
Source:
We offer this special section on Improving Maternal Health in Arkansas for the use of our hospitals and health care organizations. You’ll find a look at the new “Healthy Moms, Healthy Babies” report by Governor Sanders’s Strategic Committee for Maternal Health; an introduction to the Arkansas Perinatal Quality Collaborative, a new resource-sharing initiative; and what two Arkansas hospital systems are doing to address and improve maternal and infant health. In addition, you can link to Maternal Health Initiative resources from the American Hospital Association at the QR code below.
Core Principles for Improving Maternal and Infant
We hope that this special section offers not only insight into the gravity of Arkansas’s maternal health challenges but also offers concrete resources that every hospital and health care facility can utilize in the effort to improve maternal health in our state.
Source: Journal of the American Medical Association
Source: Centers for Disease Control and Prevention of pregnancy-related deaths are
Source: Centers for Disease Control and Prevention women annually are affected by severe maternal morbidity — unexpected and lifethreatening complications from childbirth

Examine quality and outcomes to guide strategy Apply an equity lens Involve patients and community in their own care
Healthy Moms, Healthy Babies Report Offers Recommendations
Submitted by the Arkansas Department of Human Services
Strategic Committee for Maternal Health delivers report with recommendations to improve care for pregnant women, new moms, and babies.
The Strategic Committee for Maternal Health delivered its report, “Healthy Moms, Healthy Babies,” to Arkansas Governor Sarah Huckabee Sanders in September outlining recommended new policies, programs, and approaches aimed at improving health outcomes for pregnant women, new moms, and babies.
Governor Sanders established the committee and initiated a six-month timeline to consider potential reforms when she signed the Executive Order to Support Moms, Protect Babies, and Improve Maternal Health on March 6, 2024. More than 100 stakeholders representing dozens of organizations across the state met to develop the recommendations contained in the report.
“As the first mom to lead Arkansas, maternal health is personal,” Governor Sanders says. “I’m not interested in headline-grabbing policies or duplicative government programs that don’t actually change maternal health outcomes. Instead, this committee pursued a comprehensive, coordinated approach that will help healthier moms have healthier babies. I’m grateful to all the stakeholders who participated in this discussion, and I look forward to continuing our work to turn these ideas into action.”
PARTNERS COME TOGETHER
The Strategic Committee for Maternal Health included representatives from the Arkansas Department of Human Services (DHS), the Arkansas Department of Health (ADH), the Arkansas Department of Education, and the Arkansas Surgeon General.
“We are incredibly grateful that so many partners came together to consider obstacles to maternal and postpartum care that exist in our state today, and to align around this set of meaningful solutions which promise to make a real and positive difference in our state,” says DHS Secretary Kristi Putnam. “We will act on these changes as quickly as possible because we know they have the potential to improve the health of countless women and babies, and to save lives.”
The committee worked with stakeholders and divided into four subgroups, each of which provided recommendations within their respective focus areas: Data, Reporting, and Technology; Education and Outreach; Clinical and Practice Improvements; and Health Care Access and Medicaid.
The Data, Reporting, and Technology subgroup developed recommendations aimed at addressing technological deficiencies and needs, including data collection, data reporting, and software, and they discussed potential new tools that could improve maternal health.
The Education and Outreach subgroup developed recommendations aimed at improving health care access for moms by modernizing public health education for pregnant women and new mothers across multiple channels.
The Clinical and Practice Improvements subgroup worked to find ways to improve access and maternal health outcomes by enhancing financial incentives, improving care delivery, and modernizing the maternal health workforce.
The Health Care Access and Medicaid subgroup aimed to ensure pregnant women and new mothers have clear and convenient access to coverage and care.
“Medicaid pays for more than half of the pregnancies in our state, so it’s critical that we optimize the system so that care is available and encouraged every step of the way before, during, and after birth,” says Janet Mann, DHS Deputy Secretary of Programs and





Greenfield,
State Medicaid Director. “These recommendations put in place significant changes that will remove barriers, improve care, and lead to better health outcomes.”
Dr. William “Sam” Greenfield, ADH Medical Director for Family Health, serves on the Strategic Committee for Maternal Health, and says the recommendations are a positive step toward improving maternal health across the state.
“I am encouraged to see so many people from different sectors come together to address this issue,” he says. “As Chair of the Arkansas Maternal Mortality Review Committee, I can attest that the challenges surrounding maternal health are complex. This is a significant step that addresses specific findings and needs in Arkansas. I am supportive of these recommendations and look forward to the role enactment will play in improving health outcomes for mothers in our state.”
Recommendations in the report include:
• Developing a dashboard reporting key maternal health indicators.
• Evaluating Medicaid reimbursement rates.
• Implementing presumptive eligibility for Medicaid-eligible pregnant women.
• Creating a pathway for Medicaid provider types and reimbursements for both doulas and community health workers.
• Expanding the number of obstetrics and gynecology residencies in Arkansas.
• Developing a maternal health education and advertising campaign.
“As someone who has spent her career taking care of Arkansas women, I am inspired by the many conversations this committee started and the actions we will take as a result,” says Dr. Kay Chandler, Arkansas Surgeon General. “It will take efforts from many different groups across the state to move the needle, and I believe we’ve put together a road map to make that happen.”
ALREADY UNDERWAY
The report also details several activities that have already been completed or are underway, including holding stakeholder meetings in five pilot counties that have high rates of women receiving no prenatal care, developing a Transforming Maternal Health (TMaH) Model grant application, and reviewing several key Medicaid processes tied to maternal care.
Dr. Kay Chandler, Arkansas Surgeon General
Renee Mallory, Arkansas Secretary of Health
Kristi Putnam, Secretary, Arkansas Department of Human Services
Janet Mann, Deputy Secretary of Programs and State Medicaid Director, Department of Human Services
Dr. William
Medical Director for Family Health, Arkansas Department of Health
It will take efforts from many different groups across the state to move the needle, and I believe we've put together a road map to make that happen.

Other completed activities tied to improving maternal health detailed in the report include:
• Participating in and planning a Month of May women's health event at the State Capitol.
• Partnering with the University of Arkansas for Medical Sciences (UAMS) on a pilot project to place mobile maternal units in certain counties.
• Educating rural hospitals about the UAMS Obstetrics helpline.
• Participating in panel discussions with multiple agencies and partners to improve and expand maternal health education, awareness, and ongoing policy reforms.
• Discussing with RootED ways to assist rural schools with funding to support the placement of a resource counselor in the school to interact with students and connect them to resources and future educational and workforce options.
“We are proud to present these strategies and recommendations,” says Renee Mallory, Arkansas Secretary of Health. “This report is the result of many meetings and listening sessions with stakeholders across the state. While we’ve already begun this important work, we look forward to continuing to enact solutions to improve the health and wellbeing of moms and babies in Arkansas.”
The full report with complete details is available at humanservices.arkansas.gov/u/maternalhealth/


Scan this code for the full report.
OrthoExperts
YOUR PARTNERS IN CARE




Missional Prenatal Care at St. Bernards
By Mitchell Nail
About a decade ago, health care providers at St. Bernards Medical Center in Jonesboro noticed a troubling trend. More than one in eight women who delivered babies at the hospital had received little to no prenatal care.
Dana Lands, St. Bernards Nursing Director for Women’s and Children’s Services, describes the situation.
“We were seeing tragic maternal health outcomes,” Lands says. “These women would arrive at our emergency department without any record of seeing an OB or receiving any type of prenatal care. Knowing that we lived in a region with some of the worst maternal health outcomes in the nation, it sparked an ongoing conversation of what we could do to change our community.”
Those conversations turned into listening sessions. Patients explained that they could not afford to go to any of the clinics that demanded money upfront. Others needed to file for Arkansas Medicaid, but the complicated process left them confused and frustrated.
Unsure how to remedy the situation, the team returned to its mission, which began in 1900 with courageous Olivetan Benedictine Sisters who selflessly cared for malaria fever patients with nowhere to turn. That mission, “To provide Christ-like healing to the community through education, treatment, and health services,” prioritizes meeting needs above all else, letting the other pieces fall into place. Through this lens, it sparked a vision.
“St. Bernards stepped in and said, ‘We’re going to open a clinic where you can receive prenatal care, regardless of your ability to pay,’” says Lands.
Trusting that the mission was worth the effort, St. Bernards opened its first Pregnancy Clinic on April 13, 2016.
Dr. Whitney Rich, St. Bernards Pregnancy Clinic physician, with one of her clinc patients.
FINISHING STRONG IS OUR FOUNDATION
Add to your charitable fund at Arkansas Community Foundation or contact us to get one started. The Foundation has a vision for communities in Arkansas – to become the places your kids will want to raise their kids. As 2024 comes to an end, we want to thank all the Arkansans who shared our vision this year and invested in our communities through their contributions.
A big issue for our patients was that they didn't have the transportation, the time off work, or a babysitter to come to the doctor. We needed to move beyond Jonesboro
ST. BERNARDS
PREGNANCY CLINIC
The initial clinic opened in a multispecialty health care building in downtown Jonesboro, operating near a traditional St. Bernards women’s health clinic. As volume in the pregnancy clinic blossomed, however, it soon became clear that it needed more space.
In August of 2020, St. Bernards Pregnancy Clinic moved into a shared, standalone facility near the industrial park of the city. The extra room allowed the clinic to offer more to expectant mothers.
“We’ve expanded our services twice at that clinic,” Lands says. “We added more providers, exam rooms, and space in the back of the building. We moved our outpatient lactation clinic as well as our ANGELS (Antenatal and Neonatal Guidelines, Education and Learning System) telemedicine partnership with UAMS into that space. Most importantly, we can see more patients.”


In addition to help from retired OB physicians, the clinic recently hired a staff physician, Dr. Whitney Rich. It also employs three nurse practitioners and a social worker, and it collaborates with St. Bernards Behavioral Health providers to identify and treat substance abuse and perinatal depression. The clinic regularly hosts postpartum depression support groups, and women from all socioeconomic tiers participate.
In April of 2024, the clinic celebrated receiving more than $60,000 in grants from the Blue & You Foundation and the Arkansas Department of Finance and Administration’s Pregnancy Help Organization. These funds
helped it purchase car seats, safe sleep environments, and educational materials. Clinic workers distribute these necessities to women at no charge.
MOVING BEYOND JONESBORO
St. Bernards Medical Center serves as a major referral hospital for 23 counties in northeast Arkansas and Southeast Missouri. Despite the success of the Jonesboro clinic, women outside of Craighead County still had trouble accessing prenatal care, finding themselves in the hospital’s emergency department without having seen a doctor.
“A big issue for our patients was that they didn’t have the transportation, the time off work, or a babysitter to come to the doctor,” Lands says. “We needed to move beyond Jonesboro.”
Through a close management partnership with Lawrence Memorial Hospital in Walnut Ridge, St. Bernards opened a specialty clinic within the hospital in July of 2023. This clinic brought many new health services to Lawrence County, including prenatal care.
In October of 2024, St. Bernards expanded the services eastward, using space within another specialty clinic to offer prenatal care in Osceola. Meanwhile, a short month later, the health care system began offering prenatal services in Jackson County through its Newport Family Medical Clinic.
Emily McGee, St. Bernards Vice President of Nursing and Women’s and Children’s Services, says she, herself, lives an hour from the hospital. That
LEARN MORE
commute helps her see the importance of reaching women where they are.
“If I worked where I live, I would have to take a day or a half day off work, simply to go to the doctor,” McGee said. “Even if they have reliable transportation, pregnant women cannot afford to do that eight to twelve times throughout a pregnancy. It depletes whatever limited resources they have.”
MISSIONAL RESULTS
To say the pregnancy clinics keep growing understates their importance. In October of 2024, they saw more than 700 patient visits – nearly 40 encounters per their days of operation. In addition, Lands and other care teams estimate they will deliver more than 75 babies in December 2024 from these clinics. At that pace, the clinics would yield about 900 births each year. In other words, the availability of these clinics allows approximately 900 to 1,000 babies to get healthier starts, and their moms are empowered physically, mentally, emotionally, and spiritually to care for their children.
Lands says these results go back to the St. Bernards mission.
“Our community encompasses many rural areas and many counties. When you think about our mission ‘to provide Christlike healing,’ it's for every patient, no matter what language they speak, no matter their ability to drive to a clinic, or their need to ride a Medicaid van. It doesn’t matter if they have the money to pay up front. What matters is these clinics are a prime example of our mission –caring for those who have nowhere else to turn.”

Mitchell Nail serves as the Media Relations Manager for St. Bernards Healthcare.




Top: St. Bernards holds a ribbon cutting for prenatal services at its Newport Family Practice Clinic. Left: A view of the high-risk ANGELS telemedicine exam room. Right: Dana Lands speaks at the Osceola Clinic grand opening. Bottom: St. Bernards holds a ribbon cutting ceremony for its prenatal services in Osceola.

The Arkansas Perinatal Quality Collaborative
By Dr. Jennifer Callaghan-Koru
Alone, we can do so little. Together, we can do so much. The Arkansas legislature has prioritized initiatives to improve health outcomes for mothers and their babies. This much-needed focus – Arkansas has one of the highest maternal mortality rates in the nation – will undoubtedly bring about change statewide. With support, structure, and collaborative expertise from the Arkansas Perinatal Quality Collaborative (ARPQC), birthing hospitals can shift from working independently from one another to joining a network of experts, policymakers, and teams collaborating to improve maternal health in Arkansas.
WHAT IS THE ARPQC?
State perinatal quality collaboratives (PQCs) are one of the national strategies proven to improve maternal health outcomes, and almost all states now have functional PQCs. Dr. William Greenfield, Medical Director with the Arkansas Department of Health (ADH), and I worked together to secure funding for the Arkansas PQC, applying for and receiving grants from the Centers for Disease Control and Prevention (CDC) and Health Resources and Services Administration (HRSA).
The ARPQC is a state-based network of health care teams, facilities, policymakers, patients, and experts working together to improve the quality of maternal health care in Arkansas. With the launch of the ARPQC, Arkansas joined a national movement to prevent maternal morbidity and mortality and reduce disparities in maternal outcomes.
DATA-DRIVEN SUPPORT FOR PARTICIPATING HOSPITALS
The ARPQC is a support system for 33 participating hospitals (all but one of the state's birthing hospitals), offering datadriven, evidence-based initiatives to improve maternal and neonatal outcomes guided by quality improvement methods and implementation science. We also collaborate with the UAMS High-Risk Pregnancy Program to combine quality improvement efforts. A real collaborative spirit has developed among participating hospitals as they share their innovative practices and help solve each other's challenges.
The ARPQC offers a variety of beneficial supports to health care facilities and clinicians, including evidence-based tools, quality improvement best practices, and actionable health care data.
While we primarily collaborate with facilities and providers, we believe patients are essential in health care decisionmaking. Patients deserve to be empowered to choose the best care for them and advocate for themselves during pregnancy, birth, and the postpartum period. We provide information to support patient decision-making on our website, including a map of birthing hospitals with detailed information about each hospital's services and information sheets related to our initiatives.
CURRENT MATERNAL HEALTH INITIATIVES
ARPQC identifies health care processes that can be improved to enhance health outcomes for mothers and babies. We examine state data and collect input from participating hospitals to select initiative topics. We are currently focusing on three maternal health initiatives, with more to come soon.
Our first initiative with birthing hospitals is focused on the safe reduction of primary cesarean birth. Unnecessary cesarean birth increases the risks of maternal complications and health care costs. The initiative will run for another 12 months, and we'll start a new topic by July 2025. In partnership with ADH's Infectious Disease Branch, we have also begun a "sprint" initiative on preventing congenital syphilis that will run from January through June 2025. We are introducing the materials in November and asking hospitals to sign participation agreements before the end of the year. The focus will be on screening all mothers for syphilis at delivery and ensuring coordination with ADH for reporting and treatment of positive cases.
We also have a simulation training initiative for emergency departments to ensure they are prepared to identify and manage serious obstetric complications. The obstetric emergency preparedness initiative offers training on pregnancyrelated hypertension and eclampsia. By the end of the year, we will also introduce training on precipitous birth and obstetric hemorrhage.
HOW TO PARTICIPATE IN THE ARPQC
Birthing hospitals must sign a participation agreement to participate in the collaborative, which formalizes their commitment to collaborative quality improvement through the ARPQC.
All participating hospitals attend monthly calls to learn from experts and share their experiences, successes, and challenges. We also encourage non-birthing hospitals, particularly those in rural areas, to participate in the obstetric emergency preparedness simulations by hosting training at their facility.
CONTACT THE ARPQC
To contact the ARPQC, use the contact form on our website: arpqc.org/contact. Clinicians at birthing hospitals interested in getting involved can also connect with the nurse and physician champions for their facility – these are the unit leaders who work with the ARPQC to improve their hospital.
Arkansas birthing hospitals are working hard to implement initiatives to improve maternal health. Collaboration and support from the Arkansas Perinatal Quality Collaborative will allow participating hospitals to leverage evidence-based, data-driven care strategies for mothers and their babies. Having a team of experts, policymakers, and clinically experienced personnel to share challenges and identify solutions is instrumental in reducing maternal morbidity and mortality statewide.


Dr. Jennifer Callaghan-Koru is an Associate Professor at the University of Arkansas for Medical Sciences (UAMS), with appointments in the Departments of Internal Medicine and Obstetrics and Gynecology and is a core faculty member of the UAMS Center for Implementation Research. Dr. Callaghan-Koru co-founded the Arkansas Perinatal Quality Collaborative and serves as its Director of Evaluation. She received doctoral and Master of Health Sciences degrees from the Johns Hopkins Bloomberg School of Public Health. She completed the National Institutes of Health's (NIH) Training Institute for Dissemination and Implementation Research in Health. Her research is focused on improving maternal and child health by applying implementation science methods to support quality improvement and innovative service delivery. NIH, the Health Resources and Services Administration, the U.S. Centers for Disease Control and Prevention, and the United States Agency for International Development have funded Dr. Callaghan-Koru's work. She is the Primary Investigator (PI)/Co-PI of $20 million in active research and program grants, including a hybrid effectiveness-implementation trial of enhanced postpartum care delivered through telehealth, funded by the Patient-Centered Outcomes Research Institute.
Full Circle Moments
By Nancy Robertson

“From a young age, I knew that I wanted to pursue a career in health care,” says Cody Walker, President of Baptist Health Medical Center-North Little Rock. “It just took me longer than some to figure out that health care leadership was to be a part of that path,” he grins.
While still in high school, Walker attended a health sciences academy sponsored by the school and supported by area health care entities. It presented a chance for exposure to a realm of health care career choices, and it solidified his desire to seek a career in the health care field.
“I had the chance to shadow a physical therapist, a pharmacist, a cardiologist, and nurses in varying supportive and leadership roles,” he says. “Those collective experiences strengthened my desire to enter the health care field.”
He attended Ouachita Baptist University with physical therapy as a possible career goal, so he turned his studies to kinesiology. “I wanted to be certain I was making the right career choice, so while still an undergraduate I worked at the ER in Arkadelphia as an ambulance dispatcher,”
he says. “That job exposed me to the vast number of nursing careers available as I observed, and got to know, CRNAs, RNs, LPNs, and nurse practitioners. Nursing really appealed to me, so after graduating I went back for a second bachelor’s degree in nursing, which I earned through an accelerated program at Samford University in Birmingham, Alabama.”
He says nursing was not his original plan, but it became his early career path. “I worked as an RN on the Critical Care Unit of Brookwood Baptist Medical Center in Birmingham, determined to be the best nurse I could be. As so often happens, if you apply yourself and prove to be good at your position, you’re likely to be promoted. I was named Charge Nurse of the CCU, then Manager of the Surgical Intensive Care Unit, then Director of Critical Care at Brookwood.
“During that time, I found that leading teams was my real strength, and I decided to pursue a Master of Science degree in Health Systems Administration/Management from Samford.”
Cody Walker, President, Baptist Health Medical Center-North Little Rock
There's no silver bullet when it comes to meeting the needs of pregnancy. We are trying to develop a comprehensive set of alternatives that can expand access to care and encourage people, no matter their income, to seek prenatal care and achieve healthy deliveries.

Walker credits an untamed curiosity for learning as key to his management philosophy. “I have always questioned how things work, how we can find a better way of doing things, how we can find answers to hard questions, and, in health care, how we can improve patient care,” he says.
Leadership roles at Brookwood Baptist Health included serving in several service line administrative roles, which eventually led to C-suite positions with Brookwood and hospitals within its hospital system. “I worked in Birmingham for 10 years, then had a chance to return to Arkansas just before COVID hit,” he says. He became the Vice President of Hospital Operations at Baptist Health Medical Center in Little Rock in January 2020.
“I spent the first two months of 2020 reconnecting with Arkansas,” he says, “and then we received news of a new virus that was causing alarm.” COVID-19’s arrival on the west coast of the U.S. in March began an unforgettable period in health care, the ramifications of which we are still experiencing today.
“The pandemic helped align those of us in health care with what really matters,” Walker says. “We had to hyperfocus on simultaneously keeping our staff safe, keeping our patients safe, and keeping our communities safe. It brought extreme clarity to each of us, and it helped us concentrate on our values as health care professionals.”
With COVID’s arrival in Arkansas, Walker helped to navigate several components of the COVID response for the Baptist system. That involved managing vaccine distribution, creating mechanisms for drive-through testing, and establishing (in coordination with the Arkansas Department of Health) one of the state’s first in-hospital testing labs – one that would soon process tests for entities around the state.
“I really got into the weeds on COVID testing,” he says. “We were on the front lines of acute response as we took a lead on testing in Arkansas. The team effort was truly remarkable. I believe I’ll look back on that period as one of the most edifying of my career, and certainly a highlight of the way people in health care work together for the greater
Baptist Health's Rose City Clinic.


Solutions Designed for Healthcare Providers and Organizations
Achieve your goals with world–class people solutions
Gallagher believes quality healthcare comes from strong support and sound counsel. Our healthcare practice is built on the timeless principles of doing what’s right for our clients and creating innovative solutions to meet your unique challenges.
Chris Newkirk Area Vice President Chris_Newkirk@ajg.com (501) 485 3082 Connect with us
© 2024 Arthur J. Gallagher & Co. | GBSUS46326



45 YEARS OF HEALTHY GROWTH



good. It was what we did moment by moment that mattered, and health care teams always meet the moment!”
He quoted April Rinne, who says that uncertainty equals opportunity in its purest form. “The Baptist Health team saw that extreme level of uncertainty as an opportunity to step up for the state. Our work came more into the public eye during that time, but it’s what we’ve always done behind the scenes. As health care has done throughout the course of history, we found ways to make a positive difference that could carry us into the future. It carries over every day in the way we do business post-COVID.”
He says that what he learned during the pandemic informs his work as President of Baptist Health Medical Center-North Little Rock today. “Our response during COVID was a reflection of the Baptist Health system culture,” he says. “We constantly seek ways to advance the health of Arkansans by improving the way health care is delivered.”
When asked about the challenges Arkansas faces in the area of maternal health today, he points to that same culture of care innovation and describes programming that the Baptist Health system and his own hospital are implementing.
Baptist Health is an early adopter of the Life360/ARHOME effort in the state. He says that Baptist Health is addressing maternal health by seeking to reduce the state’s maternal and infant morbidity and mortality rates while also addressing health-related social needs for high-risk, low-income mothers.
Baptist’s maternal health program lines include community outreach pregnancy wellness centers, the Baptist Health Pregnancy Clinic in Little Rock (and another coming in early 2025 to North Little Rock), the ARHOME Home Visiting Program, and the Maternal Navigation Program. “There’s a great need for developing new solutions in the area of maternal health,” he says. “These programs are designed to help meet our area’s maternal health needs.”
RANDY ROGERS Sr. Benefits Consultant
CHRIS NEWKIRK Area Vice President
LEADERSHIP Q/A WITH CODY WALKER
What is the best advice you were ever given? “You become like the people you hang around.” -Dad
What would you be doing if you weren’t in health care? Talk show host. I’d want Jimmy Fallon’s job.
What do you like to do in your down time? If it’s above 55 and sunny, I’m outside with my family. If it’s above 85, I’m in the water with my family.
What’s on your desk right now?
Hand sanitizer, Arkansas Business , Harvard Business Review , my notebook, and coffee.
What are you reading? (non-work-related material) A biography of Steve Jobs.

Another view of the Baptist Health Rose City Clinic.
The pregnancy clinics are designed to increase access to care and assure that high-risk moms receive the care they need, regardless of their ability to pay for such care.
“Our goal is to create a robust family medicine/obstetric residency program that will expand the number of physicians with specific training in the area of pregnancy,” he says. Arkansas is among the states needing more physicians with training in prenatal, delivery, and post-natal care to serve in rural markets. “We aim to train physicians who are willing to move to rural areas for their practices – areas where, historically, it is hard to place physicians with specific OB/GYN training. A new fellowship program will bring these family medicine/ obstetric residents to North Little Rock for clinical training, and it will be headquartered in our clinic on JFK Boulevard. We plan to launch that fellowship in the fall of 2025, though our clinic is now open and staffed to see new patients.” This new clinic will also address women’s needs in the areas of cancer genetics and cancer treatment, taking it beyond the singular focus on maternal health.
“We are also excited about encouraging the use of Baptist’s mobile phone app, “Hello Pregnancy.” This app brings 24/7 access to education, resources, and a provider chat feature that moves patient education out to rural, as well as metro, areas,” he says.
Another new venture assigning a hospitalist specific to maternal care – a laborist – was launched at Baptist Health-North Little Rock in October. This program employs board-certified OB/GYNs who serve as in-hospital providers for moms presenting in the ER with imminent delivery or pregnancy concerns. “This ER-specific availability provides moms who are not receiving prenatal care and do

not have their own OB/GYN with a physician who can immediately assess their pregnancy-related needs.”
Arkansas is changing its health care scene to better meet maternal care needs, and it is expanding from the current “norm” of OB/GYN care to include family medicine physicians trained in pregnancy care, midwives, and doulas who can help with health care access and safe prenatal and delivery care. “Though these roles have historically existed, the pendulum is now swinging to bring them back into the fold as accepted alternative maternal care providers,” Walker says. “There’s no silver bullet when it comes to meeting the needs of pregnancy. We are trying to develop a comprehensive set of alternatives that can expand access to care and encourage people, no matter their income, to seek prenatal care and achieve healthy deliveries.”
Walker says he is honored to be involved with the North Little Rock community, whether as an active
member of the North Little Rock Chamber, partnering with Mayor Hartwick’s office to assure health equity in the Rose City area, or sponsoring North Little Rock High School’s Health Sciences Academy to assist students in their pursuit of a career in health care. “Young people today are out there wondering which career in health care might be a good match for them,” he says. “Our hospital management team offers in-classroom education and shadowing of health care professionals to help introduce and encourage a career in health care. We’re seeking to ‘give back’ beyond the ‘normal’ hospital and health care services that are expected.
“In reality, this partnership with the health sciences academy brings me full circle to where my career in health care took root,” he says. “This is our second year participating with the students, and we hope we’re helping to build the health care workforce of the future – something that’s much needed in today’s world.”

The Comprehensive Women's Clinic is located on JFK Boulevard.

Here’s What I Want You to Know
By David Mantz, CEO, Dallas County Medical Center
Every hospital staff plans for mass casualty emergencies, but when one comes, will you truly be ready?
My small community of Fordyce, Arkansas experienced a mass shooting on June 21, 2024. It was a hot summer morning, and I remember being glad that it was Friday.
At 11:41 a.m., our Health Information Manager entered my office and said a shooting was happening at our community’s only grocery store, The Mad Butcher. At 11:42 our Physical Therapy Director called and said she could hear gunfire. At 11:43, I called my wife to be certain she was at home, and I asked her to stay there.
I ran to the entrance of our ER and found that we had four patients entering at the same time. One person had a chest wound and had driven himself to the hospital, then collapsed. One was in a wheelchair and had leg wounds. One, a police officer, had been shot in the arms, chest, and face, and the fourth was coming in with severe facial and head wounds.
I locked the lobby door and called for Maintenance and our Disaster Preparedness Director to help with the coming crowd and cover the ambulance entrance to make sure the wounded could enter. Since our normal on-duty ED staff is one physician, two RNs and one tech, I realized we needed help.
Two men express their emotion in the parking lot of The Mad Butcher following the shooting.





In the next 25 minutes, we received a total of 13 patients. Two were dead upon arrival. One of those was a coworker, a beloved young nurse who worked in our Rural Health Clinic. She was off-duty and at the grocery store. She witnessed a person being shot and then had an opportunity to exit the building. Instead, she stayed to comfort the injured woman and was, herself, shot and killed a few moments later.
Most of our staff personally knew the victims they were treating. Because we had no ready communication with the scene of the shooting, we did not know when the flow of patients would stop. Ambulance transports were being managed from the scene.
During the next 15 minutes, one physician who was not on duty rushed from home to help. Three clinic APRNs sped to the ER to offer their assistance.
Altogether, we triaged and treated 13 patients, some of whom, understandably, needed extensive wound care. Because we are such a small hospital, we held some of those needing treatment in our inpatient wing. Volunteers from nearby medical facilities, including EMS teams from six surrounding towns, immediately came to help. And, very importantly, our Behavioral Medicine team came in to help our ER team and the victims’ families begin to deal with the mental trauma we were all experiencing.
HELICOPTERS NEEDED
Do you know how inter-group communication will work if you need helicopters for transport to larger facilities? If you are a small Critical Access Hospital (CAH), have you drilled with local emergency managers on the protocols of who’s in charge, and do all of the other players know exactly what should happen?
At the end of the day, our tiny hospital with four Emergency Department beds triaged and cared for 13 people – our very own –who all came in over the short course of 25 minutes.
We needed two helicopters for the transport of shooting victims. When I called Trauma Communications, I was told they were not managing the helicopter transports, but that the transports were being managed at the scene. And we still had no direct communication with emergency managers at the scene itself.
I was able to text our EMS director but was not able to patch through to the on-scene communications network. We had an emergency radio, but it was a hand-held device and though a part of the Arkansas Wireless Information Network (AWIN) system being used that day by on-scene trauma delivery teams, the radio had no signal inside of our building and was of no use.
Our EMS director diverted one helicopter to the hospital, and one to the high school football field. Patients were then airlifted quickly.
OUR LITTLE TOWN
Fordyce is a typical “Friday Night Lights” town. With a population of 4,300, we are home to the “Redbugs” and are known as the birthplace of football coaching great Paul “Bear” Bryant. We are a diverse and close-knit community. Our town is typical of many whose large source of employment – in our case, a wood mill – disappeared with a plant shutdown, and with that, our economy has significantly weakened.
Dallas County Medical Center is a Critical Access Hospital serving Fordyce and the surrounding areas. We employ two physicians and five APRNs. One of those APRNs is dedicated to behavioral health care.
We make it a priority to plan for the unexpected. In the 13 months prior to the shooting, the issue of hospital campus security was front-andcenter. Experts assessed our facility and made security recommendations. This included a new, secure, exterior door entry system. On order were the doors, locks, and badge entry-only keypads. 34 interior and exterior surveillance cameras had been installed. An enterprise-wide panic button system activated by employee’s cell phones was put in
FORDYCE SHOOTING
Number of Deaths: 4
Callie Weems, 23
Roy Sturgis, 50
Shirley Taylor, 62
Ellen Shrum, 81
Number of Surviving Injured: 11
8 Civilians, aged 20-65
2 Law Enforcement Officers
1 Suspect
MENTAL HEALTH CONSIDERATIONS
Our little community of Fordyce, located in rural south-central Arkansas, offers a range of mental health care services to area residents. Our hospital, Dallas County Medical Center, employs an APRN specific to psychiatric medication management, and we established a Behavioral Health Program on our campus a year and a half ago to facilitate senior intensive outpatient psychiatric services including offering meals and group activities.
Pinnacle Pointe previously sponsored an on-site presence in our community, but now serves established patients via telehealth care and in the schools. We are currently seeking a grant that would allow us to remodel a portion of one of our rural health clinics to accommodate both individual and group therapy being integrated into our primary care programs.
When the mass shooting occurred, our community was understandably devastated. We opened four days of free counseling to everyone in our community immediately following the shooting, yet more is needed to meet the needs of our community and the surrounding region.
But of extreme concern to me, as hospital CEO, is the mental health care of our hospital employees. They not only experienced the trauma of receiving shooting victims en masse, they found themselves treating friends and family members who received extensive injuries from gunfire. One of those killed was our co-worker, Callie Weems, who was brought in by a Sheriff’s vehicle but was dead upon arrival. There are no words that can convey the depth of that trauma.
We immediately put into place counseling services specifically for our employees. In the months since the shooting, we have been actively working to thwart the stigma against “needing” mental health care. Our mantra has become, “Mental Health Care is Health Care.” I am seeing a counselor, and it’s my choice to make this known to our staff and coworkers, hoping that this open acknowledgment encourages others to continue seeking the care they need. Together, we’re working on developing coping mechanisms and dealing with the anxiety that manifests after such massive mental trauma.
place. We trained in the plain language emergency communication method for health care emergencies. We planned special campus orientation programs for law enforcement officers, and we had a total campus mapping and labeling of all rooms in process. All of these security measures were scheduled to be fully live five weeks after the shooting. None of these would have helped us on that fateful day.
We had drilled and practiced with law enforcement and emergency management teams for a variety of potential emergency situations. But the mass casualty incident exposed chinks in our armor that have now been addressed.
AWIN is a statewide digital communications system designed to provide a reliable way for first responders to communicate. It’s used by law enforcement, fire departments, 911 services, health care organizations, and other agencies involved in the emergency management realm. It’s designed to allow agencies to coordinate communications and share resources in the midst of a regional emergency. Many Arkansas hospitals do not have AWIN radios or base stations, so they can potentially be left out of on-scene emergency communications. Dallas County Medical Center experienced this dark reality on the day of the shooting. Today, we have installed an AWIN base station and roof antenna at the hospital itself.
Another consideration is how your facility can meet the needs of nonambulance trauma arrivals. Of the 13 wounded patients that arrived at our hospital that day, only one arrived by EMS. This converted our team from an Emergency Department mindset and skillset to a First Responder mindset. Ask yourself: Do you have adequate stretchers available? Are they in good
working order? How long has it been since you checked the condition of your stock of stretchers? Are they outdated? We found that we did not have adequate stretcher capabilities for trauma patients arriving in multiples rather than one-at-atime. We did not have enough stretchers to meet numerous patients arriving on foot or in personal vehicles and who were collapsing on the sidewalk outside the hospital. We had wheelchairs, but many of these victims could not sit up on their own.
Policy discussions need to determine what will be allowed when trained and untrained medical volunteers respond in any emergency. How will you legally employ their help? Do you have an emergency contact list? Do you have a way to send a mass message to all employees, both those on and off duty?
THE AFTERMATH
During the four days after the shooting, our hospital team and the entire community were in a state of shock. Though public unity and an outpouring of support from other communities was amazing, we realized that mental health support was desperately needed.
Our first action was to organize four days of free counselling services for our team and members of the public. This was led by our behavioral health staff and included many non-employee counselors from the area.
To help our grieving community, a prayer vigil was organized, and 350 people attended. Substantial funds were donated for the shooting victims and their families. A local bank donated funds to cover funeral expenses for the four community members who were killed in the shooting. A group made crosses with hearts on them to commemorate each of the shooting victims, and people were encouraged to write messages on them for the victims and their families.




On that June day, 13
From top: The Mad Butcher’s roadside signage says it all. Memorials display messages for the victims and their families, written by fellow Fordyce citizens. The Dallas County Medical Center’s Emergency Department normally can treat four people concurrently.
shooting victims were treated within a 25-minute time span. This overhead shot shows the route from the grocery store, site of the shooting, to the hospital. The grocery store is located near the top, center, and the route to the hospital is denoted in yellow.

Making mental health care easily accessible – always a consideration in small, rural communities – was a priority before the shooting and a necessity after. Besides offering free mental health counseling to community members, a trained grief-management therapy dog was brought in for hospital staff by a volunteer agency. Dealing with the death of their co-worker has been especially traumatic to hospital staff. Just one day with the therapy dog helped to melt some of those tightly-held traumatic feelings for our staff. (Please see Mental Health Considerations sidebar.)



Our grocery store was, necessarily, closed for a number of days after the shooting. The community came together to help those who do not have ready transportation or the funds to purchase food and necessities, like diapers, from surrounding communities. Community members established collection boxes for food and household necessities. Our grocery store donated and distributed baby formula to the community, and made their normal deliveries of dairy products, fruit, and bread available to all. Volunteers determined who, within the community, needed food and household products and developed a distribution network. In this time of great crisis, caring for one another was paramount and people just figured it out. We saw the best in one another at work.
WHAT I WANT YOU TO KNOW
Every health care leader and team member takes emergency preparation seriously. We consider how to make our buildings secure and the processes we will follow if an emergency occurs.
Mitchell, Williams, Selig, Gates & Woodyard, P.L.L.C
Jeffrey H. Thomas, Managing Director
We do dry runs, drills, and practices both internally and with our emergency management partners in the community and the region. We try to think everything through, from potential cyber-attacks on our IT systems to mass casualty events linked to shootings or weather or vehicular accidents.
When a lone shooter, also a resident of our area, opened fire in our town’s only grocery store late on a hot June Friday morning, friends and neighbors were injured and killed. At the end of the day, our tiny hospital with four Emergency Department beds triaged and cared for 13 people – our very own – who all came in over the short course of 25 minutes. Offduty and neighboring community medical staff immediately came to offer assistance. We responded well, but we have amended some practices and capabilities in the wake of this devastating occurrence.
We have learned that no matter how well you have prepared, weaknesses will appear. People will find ways to criticize after the fact, but you must stand strong in the knowledge that when the emergency came to your door, you responded well. Be proud of the planning efforts you put in place in advance, and know that you will learn from deficits you can discover only in the midst of the crisis.
Train, drill, practice. Stay involved with community planning. Take what you’ve learned and use it to connect the dots to other community needs and insert what you’ve learned into your processes. Secure your facilities so that you can deter a shooting like this from happening on your campus. But please, don’t ever think that these things can’t happen in your little town. This is what I want each of you to know.



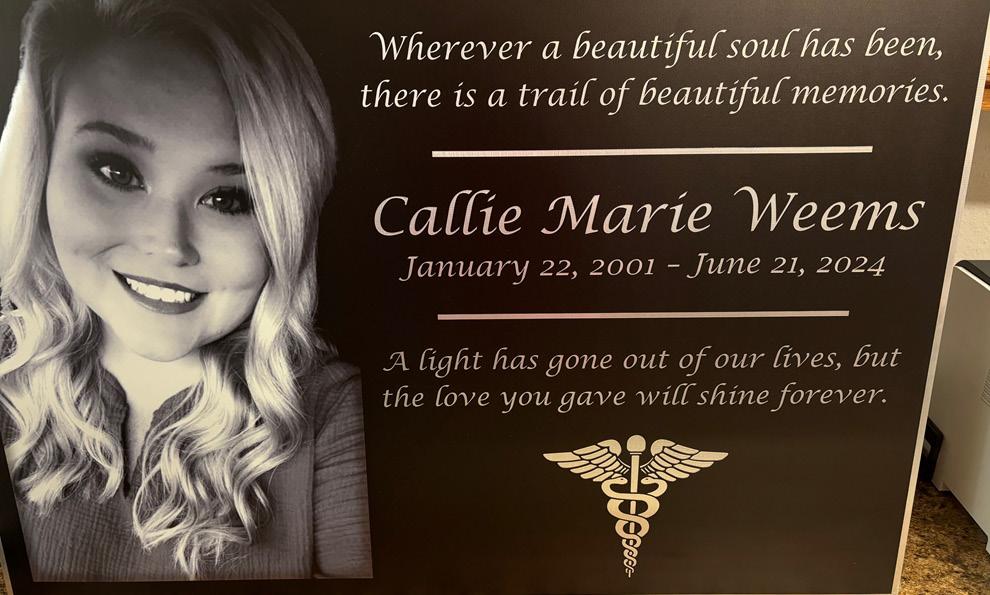
From top: Employees of The Mad Butcher started the #We Are Fordyce Strong movement. Here, they’re pictured outside of the grocery store. The movement is still growing six months after the tragic shootings. 350 Fordyce community members came together for a remembrance and prayer vigil following the shooting incident. A plaque celebrating the life of co-worker Callie Weems now graces the halls of the Family Medical Clinic.

New Food Pantry Addresses Health Disparities through Proactive Medicine: Nutrition
By Courtney Crawford
When it comes to food, Lawrence County offers a tale of abundance versus access.
According to the U.S. Department of Agriculture, the county yields about $240 million in crops, livestock, and poultry products each year, more than 20% higher than the average Arkansas county. Still, despite the abundant presence of raw agricultural goods, many county residents simply cannot find or afford ready-to-consume, nutritious food.
Looking at Arkansas as a whole, recent USDA data reveals that nearly 19% of the state’s 3 million persons experience low or very low food security, the worst rates in the nation. The problem is getting worse, too. In fact, the federal agency recently cited “statistically significant increases… from the periods 2018-2020 to 2021-2023.”1
On a micro level, Lawrence Healthcare in Walnut Ridge noticed this trend well before USDA released its findings. After a year of digging into local social determinants of health, the system learned that nearly half of its surrounding residents struggle with food, with many uncertain about their next meal. Compounding the problem, Lawrence County has one full-service grocery store, challenging residents to not only find food but also access healthy options.
This realization sparked a vision: a community food pantry that provides proactive medicine through healthy nutrition. The new Lawrence Healthcare Community Food Pantry opened its doors on October 22, 2024, representing a powerful effort to improve the health and quality of life for county residents. As food insecurity limits choices and forces families to make difficult decisions between essentials like food, rent, and utility bills, the pantry can alleviate some of these pressures while also promoting health equity.
Creating the pantry took over a year. It began with renovating a long-neglected building beside Lawrence Memorial Hospital. Maintenance crews transformed the dilapidated storage structure into a modern food pantry. They outfitted it with essential technology like CoolBot ® storage, which allows for safe refrigeration of meats, poultry, and produce. It now provides a welcoming space that serves the community at large. In fact, the opening distribution day on November 4 met an immediate need, serving 84 households and 307 persons in total.
Stocking the pantry and maintaining its operations requires a network of partnerships with local businesses and nonprofits. Lawrence Healthcare relies heavily upon close partnerships with the Food Bank of Northeast Arkansas,
A ribbon-cutting ceremony was held for Lawrence Healthcare’s new food pantry October 22.
a major source of food and grants. In addition, a growing list of local businesses, like Peco Foods, Inc., Birdsong Peanuts, and First National Bank of Commerce, provide ongoing donations and support.
Volunteers are central to operating the pantry. Every month, approximately 100 dedicated community members help with hands-on work, including shelving, sorting, and portioning food into distribution bags. Twice monthly – on the first Monday from 9 to 11 a.m. and the third Monday from 4 to 7 p.m. – teams of 10 to 15 volunteers assist with the actual food distribution.
The approach to operating the pantry emphasizes dignity and respect. Unlike some food assistance programs, Lawrence Healthcare does not require proof of income, recognizing that residents may struggle with temporary or hidden challenges. The system has a goal to treat each recipient with the same kindness, care, and respect afforded our patients.
The focus remains on providing healthy options to foster better health outcomes. The pantry offers simple, accessible recipes to accompany staple ingredients like tuna and rice. These extras enable residents to prepare healthy meals with the foods they receive.
The food pantry also aligns with broader efforts to improve food access and promote health across Lawrence County. With the help of a Delta Regional Authority grant, Lawrence Healthcare is working in partnership with the City of Walnut Ridge and the Lawrence County Chamber of Commerce to reestablish a farmers market. This market, anticipated to open in the spring, will allow SNAP recipients to access fresh produce, a significant step in a county that has not had a farmers market in over a decade. Lawrence Healthcare is also collaborating with Williams Baptist University and local farmers to supply the market and expand the availability of fresh, nutritious foods.
This pantry initiative is one of three targeted health improvement areas that Lawrence Healthcare commits to addressing: lack of transportation, poor health literacy, and limited access to healthy food. Improving these focus areas creates a more equitable health care environment for all residents, where basic needs are met, and no one compromises their health because of hunger.
Health care organizations have the power to go beyond traditional medicine and address the root causes of health disparities, such as poor nutrition. Lawrence Healthcare has created a model that can inspire other communities facing similar challenges. Its pantry provides more than a source of food – it offers a lifeline, a symbol of community, and a tool for creating a healthier, more equitable Lawrence County.

Lawrence Healthcare has created a model that can inspire other communities...



From top counterclockwise: Pantry volunteers gather for work during the pantry’s first week in operation. Walnut Ridge High School pantry volunteers help to fill bags and stock shelves. Cars were lined up to receive bags of nutritious food on the first pantry distribution day, November 4.
Endnote 1. USDA Economic Research Service, “Household Food Security in the United States in 2023,” https:// www.ers.usda.gov/publications/pub-details/?pubid=109895
Courtney P. Crawford serves as the Community Relations Director for Lawrence Healthcare.







COMMUNITY OUTREACH: Arkansas Hospitals Share Their Successes
A Day to Remember Celebrating 75 Years of Excellence at AMMC
By Tiffany Lidisky, Director of Marketing, Arkansas Methodist Medical Center
On October 16, 2024, Arkansas Methodist Medical Center (AMMC) commemorated its 75th anniversary with a celebration capturing its enduring legacy and community spirit. The day was filled with joy, reflection, and camaraderie, as the community honored the hospital’s past while looking toward a promising future.
The day began with distribution of free employee polos bearing a special 75th-anniversary logo. A group employee photo in front of the hospital building followed, with staff proudly wearing their new polos – a great display of unity and pride.
AMMC employees were treated to a complimentary lunch catered by a variety of food trucks. Free drinks were generously provided by Pepsi, and a refreshing sno-cone truck courtesy of Centennial Bank added to the festive atmosphere. As the afternoon unfolded, employees were treated to specialty drinks courtesy of 7 Brew Coffee.
The anniversary celebration concluded with a community gathering bringing together past and retired employees for


a heartfelt homecoming. Current CEO Brad Bloemer warmly welcomed everyone, while Pastor Dane Womack provided an uplifting invocation. Dr. Larry Lawson, a retired general surgeon renowned for his years of dedication to AMMC, and past Chief Nursing Officer Debra Vassar each offered inspiring words that resonated with all attendees.
Mayor Josh Agee signed a proclamation declaring October 16 as AMMC Day in the city of Paragould. Tori Thompson, Director of The Foundation, described the hospital’s significant impact on the community and highlighted The Foundation's fundraising efforts. She also shared the exciting news that AMMC is to receive a $509,000 grant from the Delta Regional Authority for new MRI equipment, an investment that will enhance the hospital’s capacity to deliver high-quality care.
Adding to the celebration was a historical display offered by the AMMC Auxiliary, featuring photos and scrapbooks chronicling AMMC’s long history. Those attending were carried through time, revisiting key milestones defining AMMC’s history and legacy. To round off this memorable anniversary celebration, guests enjoyed a selection of refreshments, light snacks, and a beautifully decorated cake. The day helped employees and community citizens alike reflect upon AMMC’s rich history and its unwavering dedication to providing exceptional health care. In our next 75 years, our hospital intends to continue serving as a beacon of health, hope, and healing, committed to lighting the way for a healthy community.

Left: Some of the AMMC staff sporting special 75th anniversary polo shirts gathered outside the hospital for photos.
Above: AMMC staff and community members enjoyed looking through a historical display featuring hospital milestones.

2024 AHA Annual Meeting
The AHA Annual Meeting was held October 30-31, 2024 at the Little Rock Marriott. Hospital leaders gathered to advance their skills, network with colleagues and peers, and reconnect with the sense of purpose that guides their work. The AHA would like to thank everyone who attended the event, as well as our amazing sponsors – without whom these annual meetings would not be possible.
On day one of the conference, attendees learned from Patrick Houlahan, a former United States Marine Corps “Top Gun” Fighter Pilot, the tools and techniques to adopt to propel their commitment and performance to new heights. Day two blasted off with a keynote presentation by Mike Massimino, a former NASA astronaut who serviced and repaired the Hubble space telescope. His message encouraged never losing sight of how our work is meaningful in a big-picture sense. Experts in an array of specialties presented in the afternoon on topics from health equity to new media. A panel of CEOs from Arkansas hospitals spoke on financial sustainability, with a focus on creating realistic plans of action.
Planning for next year’s meeting is already underway; it will be held October 15-16, 2025, at the Little Rock Marriott.

Prior to the keynote presentation, AHA PAC contributors, hospital CEOs, and Affiliated Group presidents were invited to meet Mike Massimino in a short meet-and-greet session, where they received a personalized, autographed copy of his latest book.
Former NASA astronaut Mike Massimino enchanted a rapt audience as he delivered the keynote address at the 2024 AHA Annual Meeting in October.

AUXILIARY HONORS ADMINISTRATORS
Hospital volunteers joined the festivities on Thursday morning for the keynote session, which also featured the fun and funky tunes of the Rodney Block Collective. When the auxilians arrive, it really brings up the energy in the room! We all celebrated together as they presented awards to administrators who go above and beyond in their hospitals not only for staff, patients, and patients’ loved ones but also for their volunteers. This year’s recipients were Darren Caldwell, FACHE, of Mercy Hospital Berryville, and Michael Givens, FACHE, of St. Bernards Medical Center in Jonesboro.

Above: Darren Caldwell, Mercy Hospital Berryville, and Michael Givens, St. Bernards Medical Center, Jonesboro, received Administrator of the Year awards from the Arkansas Hospital Auxiliary Association (AHAA). Auxiliary members joined AHA Annual Meeting attendees for the October 31 keynote address.
Right: AHAA President Neta Sue Stamps receives recognition for her service from AHA Board Chair Larry Shackelford.



2024 AWARD WINNERS
A. Allen Weintraub Memorial Award
Gary Sparks, CrossRidge Community Hospital, Wynne
C.E. Melville Young Administrator of the Year
Jeremy Capps, CEO, Delta Health System, Dumas
ACHE Regents Award: Senior-Level Career Executive
Matthew Troup, FACHE, President and CEO, Conway Regional Health System, Conway
ACHE Regents Award: Early Career Healthcare Executive
Tobias Pugsley, VP of Marketing & Communications, Baxter Health, Mountain Home
Distinguished Service Award
Donna Norris, RN, Dumas
Distinguished Service Award
Callie Weems, RN, Fordyce

Larry Shackelford presents Jeremy Capps with his award as C.E. Melville Young Administrator of the Year.





From top clock wise: Greg Crain presents Tobias Pugsley with the ACHE Regents Early Career Healthcare Executive award for 2024. Greg Crain presents Matt Troup with the ACHE Regents Senior-Level Career Executive award for 2024. Chris Barber (left), CEO of St. Bernards Healthcare, awards Gary Sparks (right), retired administrator of CrossRidge Community Hospital, with the 2024 A. Allen Weintraub Memorial Award, AHA’s most distinguished award, that each year honors a hospital administrator for contributions to their hospitals and communities. Jeremy Capps, CEO, Delta Health System, presents Donna Norris, RN, OR Director of the Delta Health System, with her 2024 Distinguished Service Award.
Callie Weems, a young nurse who died while giving aid to a fellow shooting victim at a mass shooting in Fordyce, Arkansas, was honored with a distinguished service award. Holding her photo is Cory McMahon, APRN, alongside BrieAnn Coston, LPN, who were co-workers of Callie’s. David Mantz, CEO of Dallas County Medical Center, where Callie was employed, accepted the award on her behalf and is pictured at right.

2024 DIAMOND AWARDS
The AHA Diamond Awards recognize excellence and encourage improvement in the quality, efficacy, and impact of health care marketing and public relations endeavors in the state of Arkansas.
Recipients of the Arkansas Hospital Association’s 2024 Diamond Awards were honored during the Arkansas Hospital Association’s 2024 Annual Meeting at the Little Rock Marriott on October 31, 2024.
The competition, co-sponsored by the Arkansas Society for Healthcare Marketing and Public Relations, is designed to recognize excellence in hospital public relations and marketing. Diamond Awards and Certificates of Excellence were possible in four divisions (hospitals with 0-25 beds, hospitals with 26-99 beds, hospitals with 100-249 beds, and hospitals with 250 or more beds) in 10 categories. The competition drew 81 entries.
Judging for each entry was based on goals and objectives, audience to whom directed, reasons for choosing the format, frequency and quantity, portions that were created internally/externally, results/evaluation, and total budget. Only one Diamond Award was awarded in each category, per division (bed size).
THE DIAMOND AWARD-WINNING ORGANIZATIONS FOR 2024 ARE:
ARKANSAS HOSPICE, NORTH LITTLE ROCK
ARKANSAS METHODIST MEDICAL CENTER, PARAGOULD
BAPTIST HEALTH, LITTLE ROCK
BAXTER HEALTH, MOUNTAIN HOME
CARTI, LITTLE ROCK
CHI ST. VINCENT, LITTLE ROCK
CONWAY REGIONAL HEALTH SYSTEM, CONWAY
CROSSRIDGE COMMUNITY HOSPITAL, WYNNE
DELTA HEALTH SYSTEM, DUMAS
HOWARD MEMORIAL HOSPITAL, NASHVILLE
JEFFERSON REGIONAL, PINE BLUFF
MENA REGIONAL HEALTH SYSTEM, MENA
NORTH ARKANSAS REGIONAL MEDICAL CENTER, HARRISON
OZARK HEALTH MEDICAL CENTER, CLINTON
ST. BERNARDS FIVE RIVERS, POCAHONTAS
ST. BERNARDS HEALTHCARE, JONESBORO
UAMS MEDICAL CENTER, LITTLE ROCK
UNITY HEALTH, JACKSONVILLE
WHITE RIVER HEALTH, BATESVILLE
THANK YOU TO OUR SPONSORS!
We thank our sponsors for their support of the AHA’s Annual Meeting. Many of our sponsors’ representatives joined us for this year’s event, where they learned more about the special challenges our hospitals are facing and were able to speak with hospital leaders face-to-face to help them discern whether their products or services are right for their facilities. Our sponsors offer valuable services to member hospitals, and we remain grateful for their partnership. This year’s sponsors, supporters, and contributors include:
DIAMOND LEVEL
AHA Services
Arkansas Blue Cross Blue Shield
Nabholz
Qualivis
SILVER LEVEL
ACHE of Arkansas
AHA Connectivity Consortium/ Federal Funding Group
Bernhard
CorroHealth
Engelkes Felts and Barnhard, LTD
Jorie Healthcare
Mitchell Williams Law Firm
SUNRx
SUPPORTERS
CareSource PASSE
Cromwell Architects Engineers, Inc.
Geiger
Hyve Health
Mainstream Technologies, Inc.
Medical Information Technology, Inc. (Meditech)
NewGen Emergency Medicine
CONTRIBUTORS
Arkansas Association of Hospital Trustees
AHA Workers Compensation Self-Insured Trust
PLATINUM LEVEL
AblePay Health
Cadence Insurance, a Gallagher Company
Clark Contractors, LLC FORVIS, LLP
Friday, Eldredge & Clark, LLP
Gallagher
Prime Capital Investment Advisors Qualivis
GOLD LEVEL
AFMC
Arkansas Regional Organ Recovery Agency (ARORA)
ChartSpan HSS, Inc.
Jackson Physician Search
MASA MTS
State Health Alliance for Records Exchange (SHARE)
Vizient, Inc.

HSS Rebranding as Tarian
AHA Services announces the rebranding of our endorsed business partner, HSS, to Tarian.
Tarian’s Risk, Consulting, and Training division will continue to provide essential services to your organization, including workplace violence training, active shooter training, and risk assessments.
These programs are vital in ensuring the safety and security of our hospitals and their staff members, as well as being a key component in achieving compliance with annual regulatory initiatives.
We present here the current training and support packages offered to AHA member hospitals by Tarian. Seth Karnes remains your contact for scheduling training or consulting sessions. His contact information can be found at the end of the support package listing.
ANNUAL TRAINING & SUPPORT PACKAGES
Tarian offers a number of training options that allow for hospital-wide training, compliance initiatives, and quarterly in-person training touchpoints from expert trainers throughout the year.
Option A
Workplace Violence & Active Shooter Annual Training w/ Consultation
– Over a twelve-month period, Tarian will provide:
• TEAM® Essentials eLearning course (unlimited user access on customer’s LMS)
• One (1) TEAM® Advanced Training Day
• One (1) Active Shooter Seminar Training Day
• One (1) Active Shooter Exercise Training Day
Option B
• One (1) Active Shooter Tabletop Exercise
• Annual Workplace Violence Policy Review
• Annual Active Shooter/Active Threat Policy Review
• Annual Physical Risk and Security Assessment
Workplace Violence & Active Shooter Annual Training
– Over a twelve-month period, Tarian will provide:
• TEAM® Essentials eLearning course (unlimited user access on customer’s LMS)
• One (1) TEAM® Advanced Training Day
Option C
Workplace Violence Annual Training Support
– Over a twelve-month period, Tarian will provide:
• One (1) Active Shooter Seminar Training Day
• One (1) Active Shooter Exercise Training Day
• One (1) Active Shooter Tabletop Exercise
• TEAM® Essentials eLearning course (unlimited user access on customer’s LMS)
• Four (4) TEAM® Advanced Training Days
• Annual Workplace Violence Policy Review
Option D
Active Shooter Annual Training Support
– Over a twelve-month period, Tarian will provide:
• One (1) Active Shooter Seminar Training Day
• One (1) Active Shooter Exercise Training Day
• One (1) Active Shooter Tabletop Exercise
• Annual Active Shooter/Active Threat Policy Review
WORKPLACE VIOLENCE TRAINING
TEAM ® Essentials – Recognizing and Managing Aggression teaches hospital staff to recognize and safely manage factors and hazards that can escalate to aggression or violence in patients, visitors, and co-workers. Tarian will place the TEAM® Essentials eLearning one-hour course directly onto the customer’s Learning Management System (“LMS”) and grant the Client unlimited annual user access to the course.
TEAM ® Advanced – Protecting Patients and Yourself teaches hospital staff who have completed the Essentials course the strategies and techniques they can use to protect patients and themselves in case of physical attack. Staff will build relationships and teamwork in the group interactions of an instructorled session. Tarian will provide one instructor who will conduct up to four sessions per 9-hour training.
ACTIVE SHOOTER TRAINING
Active Shooter Training Seminar – The Active Shooter Seminar increases awareness among all staff and prescribes actions they should take in the event of an active shooter incident. The Active Shooter Training Seminar is a 60-minute didactic presentation with room staging and real-world lessons learned. Tarian will provide one instructor who will conduct up to six sessions per 9-hour training.
Active Shooter Practical Exercise – The Active Shooter Practical Exercise is a 45-minute exercise that provides participants a hands-on opportunity to practice the learned training concepts and further
foster preparedness of staff members. Tarian utilizes a scenario-based exercise model for the offering. Tarian will be responsible for the design, development, conducting, and reporting of the exercise to include exercise controllers and a senior instructor who will also act as the aggressor during the practical exercises. Multiple exercise offerings will be provided to maximize staff participation within the organization and minimize loss of productivity. Tarian will provide three personnel who will conduct up to six sessions per 9-hour training.
Active
Shooter Incident Management
Team Tabletop
Exercise – The Active Shooter Tabletop Exercise is led by two Tarian personnel and is a 2-3-hour course designed to emphasize training concepts and give the organization’s Incident Command Team and/or leadership the invaluable opportunity to test response capabilities through discussion and a scenario-driven exercise.
RISK ASSESSMENT
Our experts provide actionable and practical recommendations, serving frontline staff to senior leadership. A Tarian evaluator will provide the following deliverables:
• Review of exterior grounds and physical security measures.
• Analysis of passive and active security measures within the environment.
• Area Crime Report analysis.
• Cultural review and interviews with clinical staff and leadership.
• Access control, cameras, systems integration review.
• Delivery of useable documentation, digital or otherwise, for executive analysis.

Seth K. Karnes Sr. Director, RCT

Putting the Success in Your Succession Planning
By Kay Kendall
Having an Emergency Preparedness Plan (EPP) is a requirement for every hospital or health care system. Over time, the concept of an EPP has expanded to include precautions against and recovery from threats unheard of decades ago, such as pandemics, active shooters, and cybersecurity attacks. But have you considered expanding your EPP further to include succession planning?
The loss or unexpected departure of a CEO (or other key senior executive) can be catastrophic for any organization, but particularly one devoted to health care. Consider the following: Research studies have found that when a President/CEO departs an acute care hospital, four additional senior executives are likely to follow that leader out the door within one year, thereby resulting in a crucial loss of organizational momentum and severed relationships with key internal and external stakeholders.1
In a recent white paper published by McKinsey & Company’s Strategy & Corporate Finance practice, researchers noted, “We estimate that 10 years ago, CEOs and top teams typically focused on four or five critical issues at any one point in time; today, the number is double that.” The rate of change, emergence of disruptive technologies,
expanding globalization, and increasing complexity in the business environment all speak to the challenge of creating and sustaining an organization that thrives.
McKinsey cites a key personal attribute needed by hospital leadership: the ability to address leadership development as a core capability that focuses on current and future leaders.
Putting into place succession planning led by the CEO and board is a critical step toward building organizational resilience. This planning also shows up in multiple areas of the Baldrige Excellence Framework, beginning with Senior Leadership, then Governance, Career Development and Succession Planning (under Workforce), and the core value and concept of “Focus on Success and Innovation.”
WHY LEADERS DON’T ENGAGE IN SUCCESSION PLANNING
A Deloitte research study notes that, “While 86% of leaders believe leadership succession planning is an ‘urgent’ or ‘important’ priority, only 14% believe they do it well.” There are many reasons responsible for this real or perceived gap in effectiveness.
And what of those who avoid succession planning altogether?
Some leaders fear that placing others in documented succession planning roles will appear as favoritism. Others fear it may instill complacency in those who feel their career path is secure, or cause disharmony within the leadership team. Still others apparently don’t want to confront their own job vulnerability or their own mortality. Some have never seen effective succession planning in practice and, thereby, don’t give it due consideration. And some boards simply don’t view succession planning as a critical element of good governance.
TO INFORM OR NOT TO INFORM
There are differing views as to whether potential candidates should be informed that they are included in an organization’s succession plans, but almost all agree that it needs to be made clear that no succession plan guarantees being moved into a position should it become vacant.
I personally favor having frank discussions with people listed on a succession plan for several reasons:
• One, it allows you to determine if the person has any interest in the role. (My stepdaughter was a fabulous individual contributor in several organizations, and her bosses constantly tried to promote her into management. She wanted no part of that, so it would have been senseless to put her on a leadership succession plan.)
• Two, it allows you to discuss developmental assignments and further individuals’ formal education.
• Three, it can define a mentorship to help the person grow into the role.
• Finally, it may help with retention by assuring the candidate that he/ she is well regarded and that the organization sees a bigger future for them.
I was once lured away by another organization to a vice president's position reporting directly to the CEO. My then-current boss was furious and blurted out, “Didn’t you know you were on two different succession plans, including my own?!” No, I hadn’t known, because succession planning in that organization was shrouded in secrecy, strictly guarded by a select few human resource executives.
WHERE TO START
A simple internet search for “succession planning” yields many white papers, research studies, best practices and even templates. You’ll find processes for identifying high potential employees, how to plan for filling positions “now,” “in 2-3 years,” and “in 3-5 years.” Tips are also offered for succession planning where no internal candidates currently possess the requisite skills and experience, and for positions for which an external search will be required.
I’m also an advocate for expanding the scope of succession planning beyond executive and senior management positions. In many health care organizations (and other types of organizations) where specialized skills, accreditations, and licensures are required, there may be a significant amount of time and investment needed to prepare viable candidates to fill key positions. And some regulatory agencies add new positions that must be planned for prior to the implementation of the regulation, such as the role of Infection Prevention and Control Officer in health care in 2022 by The Joint Commission and CDC.
Finally, boards themselves should have succession plans to account for term limits as well as unexpected vacancies. There are similarly available resources to be found on the internet to guide boards in this endeavor.
ORGANIZATIONAL UPHEAVAL
The loss of a CEO or other senior leader has a ripple effect throughout the organization. Employees at all levels wonder what this loss may mean for the viability of the organization. Will it go bankrupt? Will it be sold? Workforce productivity can also be affected as employees worry about their continued job security. Will there be layoffs? Will my department be outsourced? What will happen to that raise I counted on?
The company which I left after recruitment from another organization had five presidents in 13 months in my division alone, the last one being named only an “Acting President.” One of my colleagues on the senior leadership team once said to me, “Every day I come in and just try not to spook the herd.”
As a leader, you owe it to yourself, your colleagues, your workforce, and your customers to treat succession planning as one of your most important responsibilities. It is, indeed, a vital part of your EPP. And the right time to make your plan is now.

Endnote
1. Cohen, K. R., PhD, The Synergy Organization, “Best Practices for Developing Effective and Enduring Board/ CEO Relationships,” Monograph, American Hospital Association-Center for Healthcare Governance, Chicago, 2008.

The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 25 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.

Better Health for Mothers and Babies Initiative
Improving maternal and infant health in the U.S. is a priority for the AHA and our member hospitals and health systems While the field has made progress, we are continuing to work toward more equitable outcomes.

Maternal Mortality Rates in the U.S. Racial and Ethnic Disparities in Maternal Mortality
Source:
College-educated Black women are 5.2 times more likely to die from pregnancy-related issues than white women with the same educational attainment and 1.6 times higher than the rate for white women with less than a high school diploma.
Source: Centers for Disease Control and Prevention
Top Causes of Pregnancyassociated Mortality, 2022
Timing of Pregnancy-related Deaths
Source:
Core Principles for Improving Maternal and Infant Health
Examine quality and outcomes data to guide strategy Apply an equity lens
Involve patients and community in their own care Engage and diversify workforce

What does it mean to be taken care of?
At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and to help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.




WE BUILDPlaces for Healing
For over 75 years, Nabholz has upheld our purpose: Grow our people. Serve our clients. Build our communities. Our extensive work on healthcare facility projects aligns with just that by giving medical professionals and the surrounding communities the tools they need to succeed.
