2023 STATISTICS ISSUE

Summer 2023
BUILDING BRIDGES

YOUR CHILD’S HEALTH IS A BIG DEAL. Arkansas Children’s is the state’s only health system built just for kids. By working within the communities we serve, it’s our mission to make children better today and healthier tomorrow. We are Champions for Children where they live, learn and play. archildrens.org | 501-430-3142 Our Promise: Unprecedented Child Health. Defined and Delivered.

3 ARKANSAS HOSPITALS | SUMMER 2023


4 SUMMER 2023 | ARKANSAS HOSPITALS
Arkansas Hospitals is published by The Arkansas Hospital Association


419 Natural Resources Drive | Little Rock, AR 72205
To advertise, please contact Brooke Wallace magazine@arkhospitals.org
Ashley Warren, Editor in Chief
Nancy Robertson, Senior Editor & Contributing Writer
Mike Spain, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Ron Peterson, Mountain Home / Chairman
Larry Shackelford, Fayetteville / Chairman-Elect
Peggy Abbott, Camden / Treasurer
Chris Barber, Jonesboro / Past-Chairman
Ryan Gehrig, Fort Smith / Director, At-Large
Greg Crain, Little Rock
Barry Davis, Paragould
David Deaton, Clinton

Phil Gilmore, Crossett
James Magee, Piggott
Guy Patteson, Jonesboro
Gary Paxson, Batesville
Eric Pianalto, Rogers
Robert Rupp, Mena
Judy Shaffer, Mountain Home
Brian Thomas, Pine Bluff
Debra Wright, Nashville
EXECUTIVE TEAM
Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO
DISTRIBUTION:
5 ARKANSAS HOSPITALS | SUMMER 2023
FEATURES 14 Addressing Social Determinants of Health 22 Healthy People 2030 31 2023 Hospital Statistics Guide 56 Adverse Childhood Experiences 60 Medicaid Unwinding IN EVERY ISSUE 7 President’s Message 9 Editor’s Letter 10 Event Calendar 12 Hospital Newsmakers 24 Leader Profile: Dr. Michelle Krause 50 AHA Services Presents 52 Coach’s Playbook SUMMER 2023
BUILDING BRIDGES
Arkansas Hospitals is distributed quarterly to hospital executives, managers and trustees throughout the United States; to physicians, state legislators, the congressional delegation, and other friends of the hospitals of Arkansas. Arkansas Hospitals is produced quarterly by Central Arkansas Media. Periodicals postage paid at Little Rock, AR and additional mailing offices. The contents of Arkansas Hospitals are copyrighted, and material contained herein may not be copied or reproduced in any manner without the written permission of the Arkansas Hospital Association. Articles in Arkansas Hospitals should not be considered specific advice, as individual circumstances vary. Products and services advertised in the magazine are not necessarily endorsed by the Arkansas Hospital Association. To advertise, email magazine@arkhospitals.org.
Plus, enjoy earning on your business checking account!

6 SUMMER 2023 | ARKANSAS HOSPITALS
Determination
In late April, hospital leaders from across the state joined the AHA staff at the 2023 Annual Membership Meeting of the American Hospital Association with the mission of carrying the concerns of Arkansas’s hospitals directly to Washington, D.C.
In meetings with Senator John Boozman and Representative French Hill – and staff members from the offices of Senator Tom Cotton and Representatives Rick Crawford, Steve Womack, and Bruce Westerman –our group provided a clear-eyed assessment of Arkansas hospital finances and other issues, including ways to grow the health care workforce and evidence of the detrimental impact of delayed Medicare Managed Care payments on our hospitals.
Our congressmen and their staffers listened carefully to and showed an understanding of Arkansas hospitals’ issues, and we appreciated their acknowledgement of the difficulties hospitals everywhere are facing.
We would particularly like to thank Senator Boozman for co-sponsoring the Physicians for Underserved Areas Act, legislation that would update the Graduate Medical Education (GME) distribution process to allow medical residency programs in areas with physician shortages a greater chance of gaining available residency slots following a hospital closure elsewhere in the country. We also appreciate his sponsorship of the the Resident Education Deferred Interest (REDI) Act that would allow medical and dental students to pause student loan interest accrual and principal loan payment while serving in their residencies or internships.
Hospitals in Arkansas faced workforce challenges even before the COVID-19 pandemic, but the situation is now alarming. Projected shortfalls in the numbers of health care professionals pose a significant threat to the health and wellness of our communities and, frankly, to the

stability of our state. We must not take our excellent health care workforce for granted. This problem will not be solved quickly or by hospitals alone, but we owe it to the coming generations to take aggressive action to meet this challenge. Updating the GME distribution process is a first step on this journey.
Also at the Annual Meeting, Michael Stewart, CEO of Saline Health System, did an excellent job representing the state of Arkansas during his panel presentation titled “Pressure Points: The Financial Future of the Field and Impact on Patients.” He and other panel members discussed policyrelevant research on the financial pressures facing hospitals as they fight to care for their communities, and they pinpointed policy and regulatory burdens that add to these pressures. The panel explored key considerations related to short-term reforms and long-term strategies that address the financial sustainability of the health care field. Thank you, Michael, for a job well done!
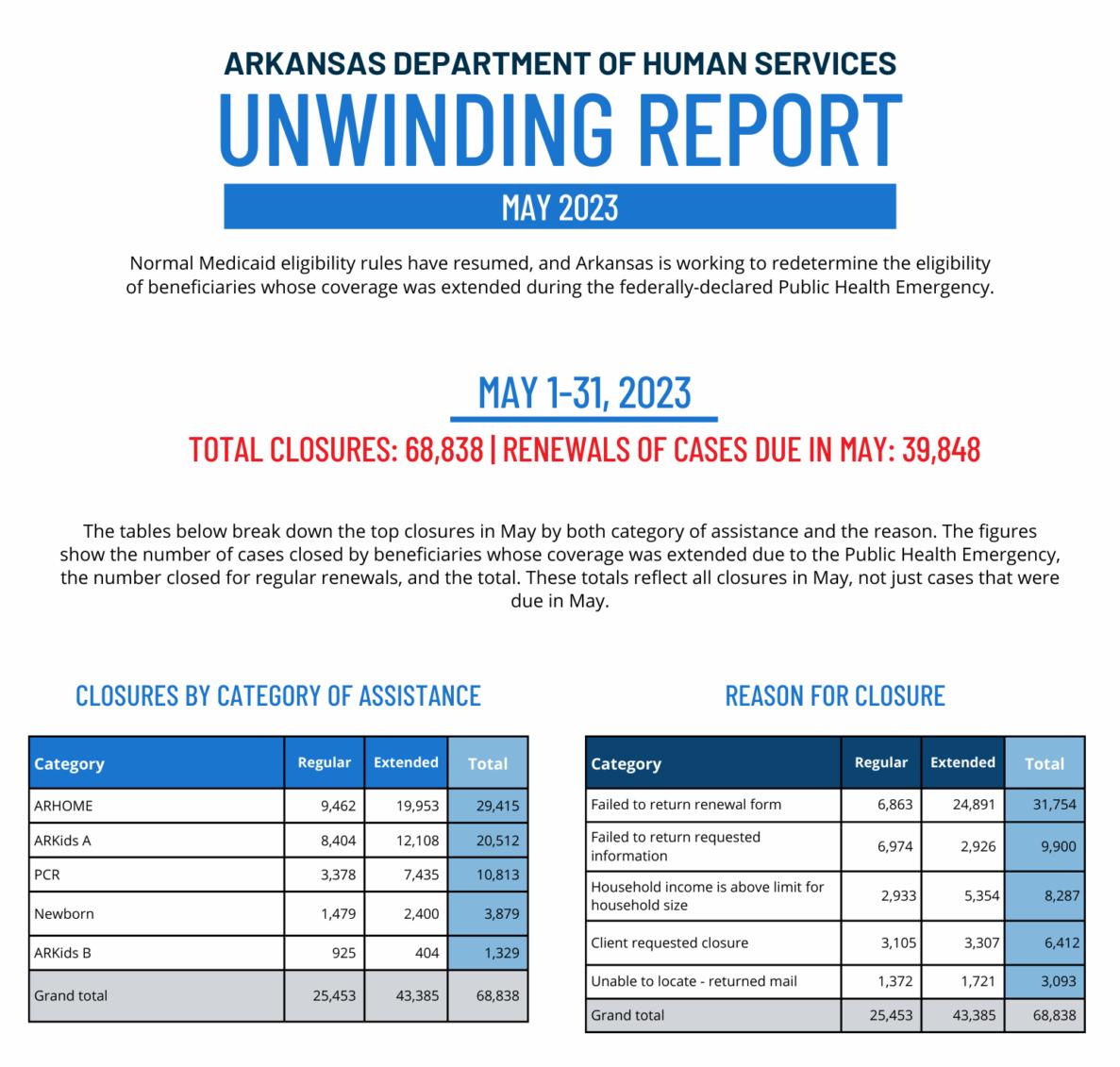
I'd also invite you to join me in raising awareness around what's involved in the current Medicaid Redetermination and what it could mean for the hospitals and patients of Arkansas. As you know, the end of the COVID-19 Public Health Emergency brought with it the end of the continuous enrollment provision,
which prevented states from disenrolling people from Medicaid coverage during the pandemic. We have concerns that, as the unwinding of the Medicaid continuous coverage protection continues, more and more patients who believe they are still covered by Arkansas Medicaid will be surprised to find out they have been dropped from the rolls.
Hospitals certainly know this is coming, and they pledge to help eligible patients get re-enrolled in the Medicaid program. Patients may first discover that they are no longer enrolled when they try to pick up prescriptions that typically have been covered at their local pharmacies. We thank pharmacies throughout the state for helping this first wave of patients reconnect to the marketplace through the Renew Arkansas program. The AHA will continue working with provider groups and insurers to help all eligible Medicaid recipients reconnect if they find they’ve lost access to their coverage.
To be clear, the number of affected patients is already staggering. More than 54,000 children have at present been disenrolled, and we have grave concerns that these numbers – in addition to the numbers of adults who are also being dropped – will only continue to rise.
Our concerns surrounding Medicaid Redetermination and our mission to speak hospitals’ truth in Washington spring from the same source: We are determined to protect Arkansans’ access to quality health care and to support Arkansas’s hospitals as they advance the health and well-being of their communities.
Bo Ryall President and CEO Arkansas Hospital Association

7 ARKANSAS HOSPITALS | SUMMER 2023
PRESIDENT’S MESSAGE




Rest assured with medical professional liability insurance coverage from LAMMICO. 800.452.2120 lammico.com/AH
No matter how many beds you oversee, we make sure you sleep well in your own.
Leading with Heart
This morning I sat, amid a joyful commotion in the “cafetorium” of my son’s public elementary school in the moments just before his fifth-grade promotion ceremony, doing my best to still my mind and be fully present. It requires a concerted effort for me – task-oriented thinker that I am – to leave behind the scramble it took to get everyone out the door wearing the correct attire, with all the necessary and/or required paraphernalia in-tow, with all the heads combed, all the bellies full, and all the teeth brushed. I took a few deep breaths and watched the families around me gather to cross this threshold together.
It’s easy to pooh-pooh an event like this with a, “What’s all the fuss?” or an, “In my day, we didn’t make a big deal of simply completing every single year of school.” In fact, I’m guilty of downplaying it myself for fear of being misunderstood as a rahrah-everyone-gets-a-participationtrophy type of Millennial mom. But mere minutes before I found myself sitting and waiting for the ceremony to begin, I had my attitude adjusted by a whole bunch of little kids.
Before the fifth (almost sixth!) graders left their classrooms to single-file their way to the assembly, the kindergarten-through-fourthgrade students sat, lining the halls of the school, shaking pom poms and cheering, as the fifth ( soon to be sixth!) graders strode through with big smiles and chins held high. It was then I realized – shocked to be blinking back tears – that all the pomp and circumstance wasn’t only about celebrating the fifth (basically sixth!) graders’ achievements – it was also
about inspiring the younger students and reminding the fifth (very nearly sixth!) graders that they are role models playing an important role within a larger community.
As the crowd settled in and the chaos dulled to a gentle rumble, students took turns offering personal reflections on all the fun they had and the learning they did during their time at the school. They sang songs, accepted diplomas, and listened (or mostly listened) as their teachers urged them to go forward with confidence, humility, joy, and a deep awareness that they are moving through the world as junior representatives of their families, their friends, and all the teachers who have poured their hearts into guiding them along the way. This event marks the transition not only from elementary into middle school but also from childhood into adolescence – an era of greater freedom and responsibility. And the resounding message, though it was never said in these words, was that our connections, context,
and community all matter. And they matter deeply.
The focus of this issue’s featured articles is social determinants of health and the persistence of longstanding disparities and inequities in health and health care. The data don’t lie, and the story they tell is not about politics. The disparities that exist result in disproportionate health outcomes across different patient populations. As leaders in our state’s health care system, hospitals play a pivotal role in our communities. Just like the fifth (can’t we just go ahead and say SIXTH already?!) graders I applauded this morning, it behooves us to understand a) how far we’ve come and how far we have yet to go, b) the deep responsibility we have to our communities, and c) that it takes innovation and collaboration from all parties to provide the best possible outcomes.

As Arkansas's hospitals lead us toward a healthier future, they will strive to do so with an awareness of the profound influence that context, connections, and community have on our patients. Together we must continue to develop better and more equitable solutions to address the barriers some Arkansans face to highquality care and improved health outcomes, wherever their paths may lead.
Ashley Warren Editor in Chief

9 ARKANSAS HOSPITALS | SUMMER 2023
EDITOR’S LETTER
2023 Summer Calendar
JULY
July 13
AHAA Board Meeting
AHA Board Room
July 18
340B Quarterly Meeting
Virtual event
July 19
AHA Services Webinar
Qualivis CorHire Webinar
July 20
AHA Quality Forum
Patient and Family Engagement

Virtual event
AUGUST
August 11
AHA Board Meeting
AHA Board Room
August 15-17
20th Annual Mid-South CAH Conference
The Grand Hotel Golf Resort and Spa
Point Clear, Alabama
August 16
AHA Services Webinar
Voyce Webinar
August 17
AHA Quality Forum
Blood Culture Contamination
Virtual event
August 25
Arkansas Society for Directors of Volunteer Services (ASDVS)
Summer Conference
AHA Classroom
SEPTEMBER
September 8
AHA Board Meeting
AHA Board Room
September 14
AHAA Board Meeting
AHA Board Room
September 20
AHA Services Webinar
Vizient’s Managed Care Webinar
September 21
Arkansas Hospital Association
Worker’s Compensation Self-Insured Trust (AHAWCSIT)
Annual Education Conference and Board Meeting
AHA Building
Little Rock
September 21-22
Arkansas Healthcare Human Resources Association (AHHRA)
2023 Fall Conference
Capital Hotel, Little Rock
September 21-22
Arkansas Association for Healthcare Engineering, Inc. (AAHE)
2023 Fall Conference
Washington Regional Medical Center, Fayetteville
September 24
AHA Quality Forum
Sepsis
Virtual event
COMING IN OCTOBER
October 6
Arkansas Association for Medical Staff Services (AAMSS)
2023 Fall Conference
AHA Classroom
10 SUMMER 2023 | ARKANSAS HOSPITALS
HOSPITAL NEWSMAKERS
Michael Stewart, CEO of Saline Health System in Benton, joined Cathy Jacobson, president and CEO of Froedtert Health in Milwaukee, Wisconsin, April 24 in a panel discussion at the 2023 Annual Meeting of the American Hospital Association. Led by AHA Chair-Elect Joanne Conroy, MD, the discussion was titled “Pressure Points: The Financial Future of the Field and Impact on Patients.” Stewart and Jacobson discussed adapting to a post-COVID business model. Stewart noted that the pandemic reaffirmed the importance of community partnerships in the delivery of health care.

Arkansas hospital leaders recently joined AHA staff at the 2023 Annual Meeting of the American Hospital Association. The group met with Senator John Boozman and Representative French Hill, as well as staff members from the offices of Senator Tom Cotton and Representatives Rick Crawford, Steve Womack, and Bruce Westerman.

Results of the compensation portion of the AHA’s 2023 Salary Survey are ready. Results are available to all members who responded to the survey, and contacts at participating facilities have received information on accessing the information. Results include information for the state overall, as well as detailed data cuts for the state and the wider Lower Midwest/South Central region of the U.S. (Missouri, Kansas, Arkansas, Oklahoma). Results of the benefits portion of the survey will be distributed soon.
Izard Regional Hospital, located in Calico Rock, is the new name of the former Izard County Medical Center.
12 SUMMER 2023 | ARKANSAS HOSPITALS
From left, Joanne Conroy, MD, Michael Stewart, and Cathy Jacobson. Their panel discussion took place at the Annual Meeting of the American Hospital Association in Washington, D.C. April 24.
Board members from Conway Regional Health System (left), CEO Matt Troup (behind), AHA Executive Vice President Jodiane Tritt (right) and congressional staff members share a light moment with Representative French Hill and Senator John Boozman. This meeting with Arkansas's congressional delegation occurred concurrently with the 2023 Annual Meeting of the American Hospital Association.
Chris Blair, MBA, BSN, is the new CEO of Northwest Medical Center-Bentonville. Blair, who also serves as Chief Administrative Officer at Siloam Springs Regional Hospital, served as Interim CEO at Northwest Medical Center-Bentonville beginning in March.
Arkansas Children’s recently announced an eight-year, system-wide expansion plan that will increase bed capacity, transform inpatient and outpatient surgical approaches, add an ambulatory surgery center, redesign clinical spaces to promote multidisciplinary care, and create an inviting and accessible campus experience. The $318 million investment includes construction at the Arkansas Children’s campus in Little Rock and the Arkansas Children’s Northwest campus in Springdale. The plan includes recruiting more than 100 new providers and 400 new team members.
Samuel Pieh, DPT, MBA, FACHE, has been named CEO/Administrator for Baptist Memorial Hospital-Crittenden . He most recently served as COO at Baptist Memorial Hospital-Memphis, and he has held leadership roles at Baptist Memorial Hospital-Tipton as well as hospitals in Virginia and Michigan. He earned his Bachelor of Science degree at the University of Memphis, his Master of Business Administration degree from Union University, his Master of Physical Therapy degree from the University of Memphis, and his Doctor of Physical Therapy degree from Temple University.
The University of Arkansas for Medical Sciences recently received a $5.5 million supplemental award from the U.S. Department of Health and Human Services to fund training and outreach programs in rural and underserved areas of the state. The supplemental funding is added to $1.1 million awarded earlier this year, and it brings the total grant award to more than $19.5 million over four years. The funding is designated for projects that will increase the number of primary care physicians practicing in rural and medically underserved communities in Arkansas.
AHA Diamond Awards: Call for Entries
The Arkansas Hospital Association (AHA) is now accepting entries for this year’s Diamond Awards. The open nominations are co-sponsored by the AHA and the Arkansas Society for Healthcare Marketing and Public Relations. This year’s recipients will receive their awards during the November 2, 2023 Awards Luncheon at the Little Rock Marriott.
The 2023 Diamond Awards recognize excellence and encourage improvement in the quality, effectiveness, and impact of health care marketing and public relations in the state of Arkansas. Awards will be presented in several categories, including advertising, annual report, foundation, publications, and writing.
Divisions include hospitals with 0-25 beds (CAHs), 26-99 beds, 100-249 beds, and 250 or more beds. Emphasis will be placed on the budget for each entry within each division.
Nominations and entries, accompanied by appropriate documentation, must arrive at AHA headquarters no later than July 7, 2023, by 4:00 p.m.
A brochure providing details of the awards competition was distributed to hospital CEOs and marketing and public relations directors. The brochure can also be found on the AHA website .
Call for Nominations: AHA Awards
Each year, the Arkansas Hospital Association (AHA) conducts an awards program to recognize individuals whose service represents a significant contribution toward achieving the goals either of the association or one or more of its institutional members.
Nominations for the A. Allen Weintraub and Distinguished Service awards (due this year on or before August 4) are evaluated by the AHA Board of Directors, after which they select the winners. This year, the awards will be presented on Thursday, November 2, during the AHA Annual Meeting Awards Lunch held at the Little Rock Marriott. Learn more by scanning the QR code.
13 ARKANSAS HOSPITALS | SUMMER 2023
Scan this QR Code to get the Award Program Booklet
of
THEY INCLUDE:
• Health Care Access and Quality (physical and mental health needs).
• Social and Community Contexts (food and nutrition, housing adequacy, transportation access, availability of and access to social services).
• Economic Conditions and Barriers (access to employment, economic mobility, income stability).
• Education Access and Quality.
• Environmental and Neighborhood Factors (water quality, air quality, noise pollution, proximity to hazardous waste sites, weather, climate change).

14 SUMMER 2023 | ARKANSAS
HOSPITALS
Social Determinants
Health are the NON-MEDICAL FACTORS that influence health outcomes.
ADDRESSING SOCIAL DETERMINANTS OF HEALTH
Why Are U.S. Health Outcomes Worse Than Those of Other Developed Countries?
By Cliff Fullerton, MD and Jasmin Sumrall, MPH
Study upon study proves it: A person’s overall health is determined not just by their physical and mental status but also by the complex set of environmental and living conditions unique to each individual.
Known as Social Determinants of Health (SDoH), these conditions are defined by the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) as
the non-medical factors that influence health outcomes. They include the locales and environments where people are born, grow up, work, live, and age.
AN EXAMPLE: LONDON
In London, life expectancy can change drastically from one small area of the city to another – even one Underground stop to another.
A famous 2012 study, “Lives on

15 ARKANSAS HOSPITALS | SUMMER 2023
Cheshire, J.
Environment
James Cheshire’s mapping of life expectancy and child poverty in London used the well-known and -utilized Tube map to clearly illustrate how disparities in social condition affect health.
2012. Lives on the Line: Mapping Life Expectancy Along the London Tube Network.
and Planning A. 44
(7). Doi: 10.1068/a45341.
the Line,” by Dr. James Cheshire, University College London, used the London Tube Network (LTN) map to illustrate how life expectancy (at birth) and child poverty can change drastically within just a few blocks or a few miles – or a few Tube stops. Cheshire’s “map” dramatically illustrates the high variability of life expectancy in London from ward to ward and borough to borough.
On the surface, explaining these disparities isn’t hard – life expectancy correlates closely with wealth, and the wealthier boroughs show an unsurprisingly
years within just a few Tube stops. This, in turn, causes a negative gradient in health and life expectancy, even though the health care system does not materially change between the various areas of London. [Marmot notes that the same factors and life expectancy variances occur in other communities, large and small, across the world. He cites Baltimore, Maryland, as another city where life expectancies between neighborhoods can vary as much as 20 years, dependent on SDoH.]
Exercise, healthy eating, and stress management are vital components of our health, but, as the London Tube example indicates, the reality is that there are additional environmental factors, often longstanding, that influence health and well-being.
“We have to put reduction of health inequalities at the center of our public health strategy, and that will require action on the social determinants of health,” Marmot notes.
FORCES AND SYSTEMS
higher life expectancy rate than do boroughs of more modest means.
However, Sir Michael Marmot, a Professor of Epidemiology at University College London, and long an expert in the field of SDoH, believes that differences in life expectancy are affected even more by the complex conditions – the SDoH – of one’s environment. “It’s social conditions that determine health,” he says, “not health that determines social circumstances … and it is not just about the money. Health inequalities and the social determinants of health are not a footnote to the determinants of health. They are the main issue.”
In London, social and environmental conditions vary widely and can deteriorate from borough to borough. Indeed, life expectancies can differ by as much as 20
Also key in any examination of health are the wider set of forces and systems shaping the conditions of daily life in any neighborhood, community, region, or nation.
The CDC suggests that besides an individual’s genetic characteristics and personal behaviors, both the physical environment and the social and economic environments affect overall health.
We see these forces and systems play out as economic policies, agendas for development, neighborhood and regional social norms and social policies, cultural harmony (or disharmony), and even existing political systems. Other factors influencing health include racism, misogyny, climate change, ready access to medical care, and access to education.
Regional studies completed in the U.S. suggest that clinical care accounts for
16 SUMMER 2023 | ARKANSAS HOSPITALS
Health inequalities and the social determinants of health are not a footnote to the determinants of health. They are the main issue.
about 20% of health outcomes, while SDoH account for the additional 80% of health outcomes.
These statistics generally apply to all countries across the world. In both poor and rich nations, health status closely correlates to socioeconomic position. The more economic, environmental, and personal resources an individual can access, the more likely they are to have good health.
HEALTH SYSTEM INVOLVEMENT IN SD o H

When determining an individual’s overall health, SDoH are obvious components of each person’s health status. Intuitively, we understand that insufficient access to financial and educational resources – and lacking basic needs like clean air and water, food, safe shelter, and transportation –makes maintaining personal physical and mental health difficult.
However obvious to “good health” these elements appear, health care systems all over the world have, in the past (notably, pre-pandemic), largely taken a handsoff approach when acknowledging and addressing social contributors to health.
But a new era in health care is dawning. Recognizing, understanding, and addressing SDoH is becoming a priority for many health care systems and networks. For example, a patient who is taking medications to control diabetes and has insufficient funds for purchasing both groceries and medicine faces a dilemma each time they must purchase either. As health care providers, we want to recognize, examine, and address such challenges with our patients and do what we can to help them overcome barriers to improved health.
But the U.S. health care system’s feefor-service payment model complicates physicians’ and health systems’ efforts to meaningfully address SDoH. The fee-forservice payment model pays for office visits, procedures, tests, and other traditional, volume-related services. There is no ready avenue for addressing environmental or economic barriers within this current model.
Not all countries have these same constraints. Countries with less structured
health care models can, oftentimes, be quite nimble in addressing individuals’ health. They can more easily apply limited resources in ways that best benefit individuals.
Take the treatment of asthma: The U.S. health care system pays for an asthmatic child to be evaluated by a physician, and it pays for treating that child’s asthma with medications, but it does not generally pay to assess and improve air quality in the home, though the latter can be less expensive and even more effective than options available through fee-for-service. (There’s more on this below.)
17 ARKANSAS HOSPITALS | SUMMER 2023
Developing maps of barrios around each clinic helps health workers identify homes where health risks exist.
AN EXAMPLE: HONDURAS
Predisan is a not-for-profit health care system operating in Honduras. Its resources include access to physicians, nurses, dentists, pharmacists, physical therapists, and psychologists, and services such as inpatient care, surgical care, radiology, and pharmacy access that all provide fee-for-service care similar to that supplied in the U.S.
However, Predisan can also use donated resources and governmental funding to manage social determinants. One example is a simple tactic that they use to manage childhood asthma in some poor areas.

Many people in rural Honduras cook their food over open fires inside their homes with
no ventilation. This can, of course, lead to patients acquiring and suffering from asthma and emphysema. Predisan will use its resources to build chimneys in these homes. Cleaning up the home’s air is a simple and inexpensive treatment that often cures the asthma of the children living there.
In its Healthy Communities Program, Predisan addresses SDoH directly and encourages healthy lifestyle choices. It offers both counseling and education, such as nutrition and cooking classes, gardening and environmental education, and DIY instruction on how to improve sanitary conditions (like putting in latrines to manage water-borne infections).
Its Healthy Schools Program offers traditional health care within the school itself, providing vitamins, physical exams, and medications to combat parasites. It also offers healthy meals for students and family education courses about nutrition and food preparation. Healthy Schools adds a preventive approach by educating students about the risks of drug use and what to do in cases of home violence. Knowing that education is an important social determinant of health outcomes, Predisan also provides scholarships that allow poor children to finish school.
Some Predisan clinic staffs create home-specific maps of their surrounding neighborhoods. Each citation on the map includes the health specifics being addressed in that home, e.g., tuberculosis, hypertension, malaria, etc. Clinical staff members use this information to organize logistical support for the needs in that home. (For example, a certain patient may need home delivery of medications, transportation to the clinic, or home checks for safety or sanitation. Patients’ health care needs –including those offered in the clinic and those related to SDoH – are addressed on individual bases.)
Funding for Predisan mostly comes from its fee-for-service payments and funding from the Honduran government. The organization also relies on donations, which adds to its flexibility in addressing health issues at the most effective and efficient points of contact. It has created a holistic blend providing both traditional
18 SUMMER 2023 | ARKANSAS HOSPITALS
For those without access to transportation, Predisan provides patient transportation and medication delivery services with vehicles like these.
health care strategies and customized management of local SDoH. The scope of disease management options provided under one health care system allows maximum coordination, resourcefulness, and prioritization.
SD o H IN ARKANSAS
Just as they shape the health of everyone across the world, it is not surprising that SDoH factors shape the health of all Arkansans.
Arkansas ranks among the 10 U.S. states with the highest rates of diabetes, heart disease, kidney disease, and chronic lower respiratory disease.
Recent analysis of U.S. Department of Agriculture data by the Arkansas Center for Health Improvement showed that in more than a quarter of all Arkansas census tracts, at least 50% of the population lives in food deserts, or areas without ready access to grocery stores and healthy foods. In turn, people living in these areas are less likely to attain adequate nutrition which can increase their risk of acquiring diseases such as diabetes, heart disease, and obesity. Living in a food desert is one of the most common determinants of health in our state.
A wide variety of organizations, both governmental and non-governmental, work to address SDoH challenges faced by Arkansans. For instance, the Arkansas Department of Health has multiple avenues for addressing SDoH. The Department identifies points of access to education, and it identifies food deserts and seeks to bring healthy food into these areas. It identifies adverse childhood events, stigma, and lack of access to behavioral health resources so that remedies and resources can be made available where needed. The Department identifies areas with a lack of readily accessible public transportation, and it shines a light on the lack of access to broadband internet as pertinent SDoH for Arkansans.
ADVANCING SOLUTIONS
While health care solutions regarding SDoH are still being researched and developed, there are promising strategies being put in place that identify patients’ needs and
connect them to resources.
For example, Community Health Workers (CHWs) are a strategic tool for addressing SDoH challenges in both the U.S. and abroad.
CHWs are nonclinical health care professionals who have a shared identity with and an intimate knowledge of the community they serve. Some CHWs share the same health conditions and socioeconomic status as their clients. We can think of CHWs as trusted peers that provide a cultural translation of the patient’s care plan.
CHWs use their unique connection with patients to help them navigate complex health care systems and connect patients to resources for overcoming barriers to improved health. In health care, CHWs
for patients
families in immediate need.

are most effective when they’re viewed as complementary members of a care team who can help patients overcome barriers that may undermine the care plan.
In one successful example, Hispanic diabetic patients with Spanish as their first language showed a significant improvement in their diabetes control when Hispanic
19 ARKANSAS HOSPITALS | SUMMER 2023
Baptist Health's Food Rx Program provides non-perishable foods
and
CHWs with Spanish as their first language helped patients understand their care plans. No change in medications, diet, or physician visitation was needed. Patients just needed a better understanding of their medical care plan, and that was provided based on the bonds of trust and common language.
BAPTIST HEALTH’S FOOD RX PROGRAM
At Baptist Health, we recognize the financial constraints that many of our patients face, and, in response, we have developed the Food Rx Program that provides nonperishable food items to patients who have an immediate need.

Arkansas provide food to those in need. The Baptist Health Food Rx Program provides health-needs specific bags of food to patients in our primary care clinics. Diabetes-focused bags offer lower carbohydrate and higher protein food items, while hypertension- and congestive heart failure-focused bags provide lower sodium foods.
While the Food Rx Program provides an immediate, though short-term, solution, Baptist Health recognizes the need for connecting patients to longer-term solutions. Baptist Health partners with findhelp – a search engine for national and local social services providers. Baptist Health and findhelp are working together to build partnerships with community-based organizations that offer social services to which patients can be referred.
Using the example of food insecurity, patients who receive a bag of food through Food Rx can also be referred to the SNAPARK Call Center – an offering of the Arkansas Hunger Relief Alliance. The call center helps people check their eligibility for the Supplemental Nutrition Assistance Program (SNAP) and helps people apply for the program if they’re eligible. SNAP provides a monthly allowance to supplement food budgets of families in need so they can purchase healthy foods and move toward self-sufficiency. The combination of Food Rx and a referral to SNAP-ARK provides both short- and long-term solutions for patients who are experiencing food insecurity.
MOVING FORWARD
Patients are asked two questions using the Hunger Vital Sign TM Screening Tool, and when they indicate that having additional food would be beneficial to them and their household, they are provided with a bag of nonperishable food.
Our partner in food acquisition is the Arkansas Foodbank, which helps more than 400 agencies across Central and South-Central
The United States, when compared with other developed nations, has both a lower life expectancy and higher rates of chronic disease. These statistics are puzzling when we consider that, though the U.S. spends more on health care than these same countries, we have poorer results and outcomes.
One explanation for this disparity may be that U.S. spending on social services lags behind that of other nations. The U.S. has traditionally under-invested in preventive and social care, and, instead, has prioritized sick care, which does not provide the best financial return on investment.
However, in recent years, spurred by the
20 SUMMER 2023 | ARKANSAS HOSPITALS
Baptist Health keeps a well-stocked pantry for its Food Rx Program. Meeting patients' immediate needs for food is a priority.
COVID-19 pandemic, health care providers and payers are beginning to prioritize identification of patients’ social needs and their navigation to social services. A Harvard University analysis by Robert H. Shmerling, M.D. puts it this way: “The social determinants of health likely explain a lot of these disparities. For example, those with the shortest life expectancies in the U.S.

tend to have the most poverty, face the most food insecurity, and have less or no access to health care, all factors that contribute to lower life expectancy.”
As the nation and its health care systems seek to improve health outcomes and life expectancy, we must focus on improving our understanding of and spending on solutions that address SDoH.
Health and Social Care Spending as a Percent of GDP, 2016 or Latest Available Year
 Cliff Fullerton, MD, MS, serves as Senior Vice President for Baptist Health and as its Chief Value-Based Care Officer. Jasmin Sumrall, MPH, serves as Operations Manager for Baptist Health's Population H ealth Services Office.
Cliff Fullerton, MD, MS, serves as Senior Vice President for Baptist Health and as its Chief Value-Based Care Officer. Jasmin Sumrall, MPH, serves as Operations Manager for Baptist Health's Population H ealth Services Office.
21 ARKANSAS HOSPITALS | SUMMER 2023
HEALTHY PEOPLE 2030 and Social Determinants of Health
Healthy People is a project of the U.S. Department of Health and Human Services that provides useful tools and objectives for those seeking to improve the health and well-being of their communities.
The project began in 1990, and at the beginning of each decade it refines and launches 10-year, measurable public health objectives designed to improve the health of every American. The current program, Healthy People 2030, includes new tools to help measure and track progress of program objectives.
The program identifies pressing public health priorities and presents objectives for achieving
being of their populations. Healthy People 2030 includes a multifaceted resource section defining, providing research and statistical information, and connecting those interested in specifically addressing social determinants of health in their everyday work.

A WEALTH OF INFORMATION
Healthy People 2030 includes a resource area, “Social Determinants of Health Literature Summaries,” that provides snapshots of the latest research related to specific social determinants of health: Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhoods and the Built Environment, and Social and Community Contexts.
Is your workgroup looking for ways to improve the economic stability of your region? You might want to access literature summaries in the areas of employment, food insecurity, housing instability, and/or poverty.
Are you working on local improvements to educational access and quality? Specific literature summaries are available in the areas of Early Childhood Development and Education, Enrollment in Higher Education, High School Graduation, and Language and Literacy.
improvement in public health. Healthy People 2030 connects users to dozens of data sources and hundreds of evidence-based resources that can be used to set (and track progress of) national, regional, and local public health improvement targets.
Health care organizations, non-governmental helping organizations, and communities have long made use of the toolkits included in Healthy People to improve the health and well-
If health care access and quality is your main focus, you can explore summaries on the topics of Access to Health Services, Access to Primary Care, and Health Literacy.
Summaries in the area of Neighborhood and Built Environment include Quality of Housing, Crime and Violence, Environmental Conditions, and Access to Foods that Support Healthy Dietary Patterns.
And in the area of Social and Community Context, summaries addressing Civic Participation, Discrimination, Incarceration, and Social Cohesion are now available.
22 SUMMER 2023 | ARKANSAS HOSPITALS
Healthy People 2030, a project of the U.S. Department of Health and Human Services, sets data-driven national objectives to improve health and well-being over the next decade.
HOW DOES HEALTHY PEOPLE 2030 ADDRESS SOCIAL DETERMINANTS OF HEALTH?
One of the project’s five overarching goals specifically relates to social determinants of health: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
More than a dozen workgroups made up of subject matter experts with differing backgrounds and areas of expertise developed the Healthy People 2030 objectives for improving health and reducing health disparities. One of these workgroups is dedicated to the social determinants of health.
Healthy People first introduced social determinants of health objectives in 2010. Addressing social determinants of health means focusing on resources needed to maintain health and quality of life. Healthy People 2030 highlights resources for achieving safe and affordable housing, high-quality education, access to healthy foods, local health and emergency services, and environments free of life-threatening toxins that provide opportunities for safe physical activity.
Lead federal agencies involved in the Healthy People 2030 Social Determinants of Health Workgroup include the Office of Disease Prevention and Health Promotion, the National Institutes of Health, the Centers for Disease Control and Prevention, the Health Resources and Services Administration, and the National Center for Health Statistics. Other agencies and groups engaged with this workgroup include the Robert Woods Johnson Foundation and the World Health Organization, among others.
• Increase the proportion of children living with at least one parent who works full time.
• Reduce the proportion of families that spend more than 30% of income on housing.
• Increase the proportion of high school graduates in college the October after graduating.

• Increase the proportion of federal data sources that include country of birth.

• Increase the proportion of the voting-age citizens who vote.
Representatives of the National Center for Health Statistics involved with this workgroup regularly summarize data on these objectives and track progress toward achieving them.
For more information on Healthy People 2030 and how your organization can utilize its resources as you address social determinants of health in your area, scan the QR code below or visit healthypeople.gov.
USEFUL INFOGRAPHICS
Do you need infographics to support your work on the social determinants of health? You’ll find reproducible infographics on the Healthy People 2030 website that illustrate how social determinants of health can influence health outcomes. Look for infographics in the areas of employment, early childhood development and education, access to health services, healthy foods, and civic participation, among others.
There are eight objectives identified by the Social Determinants of Health Workgroup. These are:
• Reduce the proportion of children with a parent or guardian who has served time in jail.
• Reduce the proportion of people living in poverty.
• Increase employment in working-age people.
23 ARKANSAS HOSPITALS | SUMMER 2023
Scan this QR Code to get information on Healthy People 2030
How can I use Healthy People 2030 in my work? Healthy People addresses public health priorities by setting national objectives and tracking them over the decade. Join us as we work to improve health and well-being nationwide. 1. Identify needs and priority populations Browse objectives to learn about national goals to improve health See how national goals align with your priorities Consider focusing on groups affected by health disparities Use this information to make the case for your program, secure resources, and build partnerships. Healthy People 2030 establishes objectives and targets for the entire United States, but setting local targets contributes to national success. 2. Set your own targets Find data related to your work Use national data to set goals for your program 3. Find inspiration and practical tools Explore critical public health topics relevant to your work » Learn about successful programs, policies, and interventions » Look for evidence-based resources and tools your community, state, or organization can use 4. Monitor national progress — and use our data as a benchmark Check for updates on progress toward achieving national objectives Use our data to inform your policy and program planning » See how your progress compares to national data Visit health.gov/healthypeople/tools-action to get started using Healthy People 2030 — and use #HP2030 to share your successes on social media!
DR. MICHELLE KRAUSE
By Nancy Robertson
Some people cite a defining moment when their career choice is crystallized. Some say they feel pulled toward one field or another. And others just know. They know, with a certainty inside themselves, what their work in this world is to be. Dr. Michelle Krause, Senior Vice Chancellor for UAMS Health and Chief Executive Officer for UAMS Medical Center, says she always knew that she would be a physician. From the time as a youngster when she accompanied her father on rounds at the hospital, she knew. When she saw that care delivery is not always equal, she knew. And when she worked with a mentor who encouraged serving the underserved, she knew.
She. Just. Knew.
Michelle Whittier lost her mother, Joan, a nurse, to ovarian cancer when she was five years old. She and her older sister and two younger brothers learned to depend upon one another and on their dad, Dr. Fred Whittier, as they grew up in the Midwest.
Dr. Whittier told his kids he would pay for their college tuition as long as they stayed in their home state of Ohio. “I wanted to go to school as far away from my hometown of Canton as possible,” she grins, “so I applied to the University of Cincinnati.” There was already a piece of “home” there –Michelle’s sister also attended the University of Cincinnati where she pursued nursing as a career.
“After graduation, I knew that paying for med school was up to me, so, being practical, I chose to stay in Cincinnati to attend the University of Cincinnati College of Medicine,” she says. While in medical school, Michelle encountered a faculty member who would become a beloved mentor. “She was an Internist who taught me that serving patients in underserved areas was one of the most important things we could do as physicians.”
This often meant providing care in clinics and settings that lacked sufficient supplies and resources – but finding ways to provide equal care to every patient, no matter their circumstances or means, became a driving force.
“When it was time to match for medical residency, I applied to the University of North Carolina at Chapel Hill,” she says. “While I was growing up, we sometimes vacationed in North Carolina, and it felt like a friendly and familiar place to me.”
She was accepted for the UNC residency program and began her internship, then residency in internal medicine. Decisions on what direction to follow gripped her. Should she go into private practice? Community medicine? Academic medicine? Research?
“Along the way, I learned that I was drawn to caring for the very sickest of patients and at the same time was drawn to medical research, so an academic setting made sense. I decided to pursue fellowships in nephrology and nephrology research, because this work put me where I wanted to be – in a position to care for patients who are extremely ill while pursuing ways to improve their care.”
24 SUMMER 2023 | ARKANSAS HOSPITALS
LEADER PROFILE
Concurrent with her fellowship training, Michelle attended the university’s Gillings School of Global Public Health, where she earned her Master of Public Health degree in epidemiology.

SEEKING TO SERVE
“As I neared the end of my nephrology training, it was time to find where I would ultimately practice,” she recalls. “It made sense to me that to care for the sickest of patients, I should look at serving in one of the larger cities in the country. I was determined to serve the underserved, so I decided to interview in several of America’s big cities.” Interview after interview occurred. But nowhere did she find people who seemed
excited with their work, nor did she find people who seemed happy to support one another in the medical workplace. “I struggled for months,” she says. “I needed to find a job, but it needed to feel ‘right.’ I reluctantly decided to go with my sister’s urging and settle somewhere near her on the east coast.”
While attending a national meeting for physicians practicing nephrology, she got a call from her old boss at UNC. “I think I have a job for you,” he said, “but I’m not going to tell you where it is.” While still at the conference, a breakfast interview with the “mystery” organization was arranged, and she was introduced to Dr. Sudhir Shah, a division chief at the University of Arkansas for Medical Sciences.
25 ARKANSAS HOSPITALS | SUMMER 2023
“Dr. Shah was so dynamic, and so excited about the possibility of my joining the UAMS team,” she remembers. “He asked me to come to Little Rock to see what UAMS was all about.”
She was frustrated, she says, with not being able to research much about UAMS before coming to Little Rock. “There was no internet, no way to find out much before I made the trip.”
But when she came to the UAMS campus, she felt like it could become “home.”
“People’s doors were open, they were friendly, they seemed to support one another and UAMS’s work, which was so important,” she says. “Though I knew no one in Arkansas, I felt I could come here and not feel alone.”
life taken root, but so had her family and personal life.
Now Dr. Michelle Whittier Krause, she began her work combining research, patient care, and an academic career.
Dr. Krause’s gift of organization led to an offer in Administrative Oversight. This position allowed her to work with others in organizing UAMS’s entire clinical umbrella, bringing needed structure to the massive educational and clinical enterprise that is the teaching hospital.
Michelle’s sister and aunt were very concerned about her impending decision. “They made me feel that I should locate closer to family and to my support system,” she says. “What they said made sense.”
But when she called Dr. Shah in 2002, ready to decline his offer of employment, she surprised herself by instead saying, “Yes, I’ll accept your offer and come to Little Rock.”
AT HOME IN LITTLE ROCK
“At the age of 32, I moved into a 1920s-era home in Hillcrest with a yard of my own,” she smiles. “It was all new to me, and I loved it.”
Across the street lived a single lawyer who came to visit shortly after her move to the neighborhood. “Within several months we were married, and shortly thereafter came three kids in four years.” So not only had her professional
“Roxanne Townsend was our first female CEO, and at the time of her leadership there was a new, national focus on clinical efficiencies and quality of care,” she says. “I was asked to oversee our medical specialties service line, which gave me the opportunity to both concentrate on quality and, at the same time, expand our service to the medically underserved throughout the state. The attention we placed on quality of care got UAMS noticed, and as time went on, we were able to put our attention where it most needed to be – on the patient’s experience when moving from clinic to hospital and back home again. We wanted to build a cohesive experience for our patients, and we believe we’re doing that very well.”
THEN, COVID-19
As COVID hit, all “regular” work at the medical center changed. “Everything we offered, from our medical programming to medical residencies to clinical work in eight locations around the state, became laser-focused on delivery of care to Arkansas patients with COVID,” she says. “Immediately, it became our work to transform care in the communities we served and to make certain every patient had access to the care they needed.”
Dr. Krause was asked to take over UAMS’s COVID response, partly because of her organizational skills, partly because of her dedication to the sickest of the sick, and partly because she could keep a cool head in the midst of the national health crisis.

26 SUMMER 2023 | ARKANSAS HOSPITALS
Dr. Michelle Krause was on the front lines as UAMS set up mobile testing events at the beginning of the COVID-19 pandemic. Here, she and her colleagues conduct individual testing at Shorter College in North Little Rock June 30, 2020.
“Everything evolved quickly,” she recalls. “We had to learn how most safely to take care of our patients in the hospital, how to safely provide care in clinics throughout the state, how to safely operationalize care for non-COVID patients, and how to provide testing when no testing materials or protocols were available.”
Dr. Krause and the COVID team built a plan of care that involved mobile testing – drive-through clinics where people could be tested in their vehicles. They took testing out into Arkansas’s communities, making it available in remote locations of the state.
Working with colleagues in the pathology department and other areas of the campus, her team developed testing protocols, isolation policies, communication tools, and safety procedures for the main campus, then took them to the field and implemented COVID policies that could be adapted anywhere in the state.
“One of the most important things we did was to break down myths,” she says. “We were transparent about what was known about COVID and what we were learning as time went on. When vaccines became available, we developed ways to take them to the people of Arkansas. Local access was put in place, and we also provided a mobile unit that could take vaccine and vaccinations anywhere in the state.”
As COVID wore on and knowledge about COVID care grew, Dr. Krause and her team continually changed protocols and procedures to meet the needs of Arkansans, Arkansas hospitals and physicians, and fellow staff members at UAMS.
“We were and are passionate about the care we offer to every Arkansan,” she explains. “COVID gave us the chance to evaluate what was and wasn’t working for patients and staff,
and we adjusted at every step. That work was some of the most challenging work I have ever experienced. We all worked every day for YEARS. As parents, we adjusted to having kids attend school virtually from home. We adapted and addressed needs as they came up in every corner of our campus. And at the end of the day, I can honestly say that the work during the pandemic was some of the most fulfilling and rewarding of my career.”
A NEW ROLE
With all of the transitions occurring daily and weekly during the COVID crisis, as it neared its end Dr. Krause was offered a new opportunity that grew out of the leadership she presented during the pandemic.
“I really thought I would always keep doing what I had been doing,” she says, “but then I was offered an opportunity to move into administrative leadership of the operation on a permanent basis.”
In January of 2023, she was named Senior Vice Chancellor for UAMS Health and Chief Executive Officer for UAMS Medical Center.
Her personal guiding goal of improving the lives of Arkansans through better health and health care has always been at the center of her 20-year career at UAMS. “No matter a person’s age, race, socioeconomic status – we intended and intend to close existing gaps so that equal care is offered to every person.”
Her reputation for remaining calm in the center of any storm and her determination to keep the patient’s viewpoint at the center of all UAMS programming helps those around her understand the importance of building trust within work groups, in the patient care setting, and in the communities where UAMS offers service.
27 ARKANSAS HOSPITALS | SUMMER 2023
We must address people’s challenges in order to help them improve and impact their health.
“We must address people’s challenges in order to help them improve and impact their health,” she says. “At the clinic level, at the hospital level, we sort things out patient by patient. We look for ways to connect patients with services. We look for ways to meet people where they are and learn from them about what they need. That gives each of us the opportunity to serve, and it encourages us to develop novel ways of delivering care outside the four walls of the hospital.”
The new Hospital at Home program that encourages home health care for eligible patients, a new collaboration with Hall High School that will prep students to move into health
care careers, the expansion of community clinics to offer innovative services to patients in their hometowns – these are but a few of the projects growing outward from Dr. Krause’s leadership and compassion.
“We can learn from everyone, and everyone can learn from us,” she says.
It’s something she has known, deep down inside since she was a child. Caring for patients is her passion, developing people and programming to make that happen at every level for every person equally is her commitment.
It’s what she set out to do all those years ago when She. Just. Knew.
Leadership Profile Q/A with Dr. Michelle Krause

What is something people don’t know about you?
We bought a home in Ferndale and started a market farm. We are now selling our produce at the Ferndale Farmers Market every Saturday. We also raise chickens for eggs and bees for honey.
What do you like to do in your down time?
I really like being outside, whether that is working in the garden, going to the lake, or taking a walk or going for a run. It helps to clear my mind and gives me inspiration to meet my next challenge.
What’s on your desk right now?
Slides to review for a UAMS town hall meeting on the COVID-19 update and on the impact of the end of the federal Public Health Emergency. I also have slides to review for a presentation at the University of Arkansas Board of Trustees meeting.
Where would you travel if you could go anywhere?
I would like to visit all of our national parks. We traveled to many of them when our children were younger, but I want to get out west and see Yosemite.
What is the most valuable lesson COVID has taught you?
Every single person at UAMS, whether part of the team in clinical areas, research, administration, or education provided input and committed to putting in hard work to face the challenges at the height of the pandemic. No one area was able to work through these challenges alone.

28 SUMMER 2023 | ARKANSAS HOSPITALS
Dr. Michelle Krause
Arkansas Hospitals
MK AH MK AH MK AH MK AH



29 ARKANSAS HOSPITALS | SUMMER 2023 New York Institute of Technology College of Osteopathic Medicine (NYITCOM) at Arkansas State University is committed to training talented physicians who aspire to become servant leaders that positively impact their communities. Contact us to learn more about the two degree programs offered on our Jonesboro campus: Doctor of Osteopathic Medicine (D.O.) Master of Science, Biomedical Sciences Leaders in Medical Education nyit.edu/arkansas | 870.680.8816 | ComjbAdmissions@nyit.edu Training Physicians In Arkansas, For Arkansas



31 ARKANSAS HOSPITALS | SUMMER 2023
VIII VII VI V IV III II I 2023
© MEGAFLOPP STOCK.ADOBE.COM
HOSPITAL STATISTICS
GUIDE
ARKANSAS HOSPITAL ASSOCIATION 2023 HOSPITAL STATISTICS
33 Workforce Challenges by the Numbers
34 Arkansas Hospitals 2023 by the Numbers
35 Arkansas Hospital Association Member Organizations by Type, 2023
36 AHA Members by City, Type, Size, and Services
38 Statewide Hospital Financial and Utilization Indicators, 2016-2021
39 Arkansas Hospitals Receiving Local Tax Support, 2023
40 Key Financial Indicators: Arkansas and Surrounding States, 2021
41 Comparative Financial Indicators: U.S. Community Hospitals
42 Hospital Access by County
43 AHA-Member Organizations by Congressional District
44 AHA Members by Control and System Affiliation
46 Inpatient and Emergency Department Discharges by Payer, 2021
Uninsured Inpatient Admissions and Costs, 2011-2021
47 Hospital Uncompensated Care Costs, 2016-2021
Top 20 DRGs, 2021
48 Arkansas Hospitals Locator Map, 2023
Hospital Statistics uses the latest data available, and this year includes utilization and financial data reflecting the impact of the COVID-19 pandemic. Hospitals experienced massive disruptions in 202021, with reductions in revenue due to deferred and delayed care, expenditures related to pandemic preparedness and response, supply chain issues, staffing shortages, and several major surges of COVID-19. At the same time, federal and state COVID-19 relief funding provided some much-needed assistance, though occasionally with future repayment requirements. Financial and utilization measures included are reported based on hospital fiscal year, and not all 2021 data reflect the same 12-month period for each hospital. This year’s edition of Hospital Statistics reflects a full year’s view of hospital operations during the COVID-19 pandemic, and year-over-year changes in measures should be interpreted with caution.
32 SUMMER 2023 | ARKANSAS
HOSPITALS
2023 WORKFORCE CHALLENGES BY THE NUMBERS
A 2023 study commissioned by AHA found that Arkansas’s current shortfall of 9,000 registered nurses will not be resolved by 2035 if no interventions are made.

RN SUPPLY ADEQUACY BY REGION, 2021 AND 2035
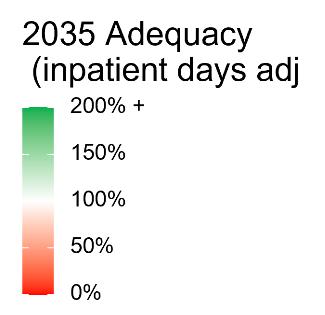

Note: 100% supply adequacy means supply is sufficient to provide the 2021 national average level of care.
RN SUPPLY ADEQUACY BY COUNTY, ADJUSTED FOR HOSPITAL LOCATION, 2021 (LEFT) AND 2035 (RIGHT)

WORKFORCE CHALLENGES BEYOND RN STAFF
To maintain current Arkansas use patterns, the licensed practical nurse (LPN) workforce would need to grow by an additional 55 LPN full-time employees per year above anticipated status quo growth. By 2035, there will be a shortfall of approximately 240 to 580 respiratory therapists to meet the projected demand.
Other specialties showing shortfalls include:

• Physician assistants.
• Phlebotomists.
• Clinical laboratory technicians.
• Emergency medical technicians.
33 ARKANSAS HOSPITALS | SUMMER 2023
No. Region Adjusting for Hospital Location 2021 2035 1 Arkansas Valley 74% 87% 2 Metro 74% 82% 3 North Central 76% 98% 4 Northeast 75% 100% 5 Northwest 82% 91% 6 Southeast 76% 90% 7 Southwest 74% 89%
ARKANSAS HOSPITALS 2023 BY THE NUMBERS
113 Hospitals of all types are located in cities, towns and communities throughout Arkansas.
106 Hospitals and other health care organizations are members of the Arkansas Hospital Association.
55 Community hospitals have fewer than 100 acute care beds.
28 Hospitals are designated by the federal government as Critical Access Hospitals, having no more than 25 acute care beds.
41 Counties are served by a single hospital. Eighteen of those counties are served by a single Critical Access Hospital.
$15.2 BILLION
Is contributed by hospitals toward Arkansas’s economy, through the impacts of well-paid, consistent employment, purchases of goods and services, and construction and capital spending.
11% Of Arkansas workers are employed by hospitals or other health care organizations.
25 Arkansas counties and cities believe their hospitals to be important enough that people in those areas have voted to provide local tax support for the hospital.
20 Arkansas counties – over a quarter of all counties in the state – do not have a local community hospital.
60% Of AHA member organizations are charitable, not-for-profit organizations, while 26% are operated by private, for-profit companies, and 13% are public hospitals owned and operated by a city, county, state, or federal government.
65,655 Hospitalizations due to COVID-19 were reported by Arkansas hospitals during the period of August 2020-May 2023.
18,016 Arkansans sought inpatient or outpatient care from the state’s hospitals each day in 2020, on average, for illnesses, injuries, and other conditions that required medical attention.
35,471 Newborns were delivered in Arkansas hospitals in 2021. Over 40% of those births were covered by Medicaid.
34 SUMMER 2023 | ARKANSAS HOSPITALS
ARKANSAS HOSPITAL ASSOCIATION MEMBER ORGANIZATIONS BY TYPE, 2023
General Med-Surg Hospitals (46)
Arkansas Methodist Medical Center
Baptist Health Medical Center-Conway
Baptist Health Medical Center-Hot
Spring County
Baptist Health Medical Center-Little Rock
Baptist Health Medical Center-N. Little Rock
Baptist Health Medical CenterStuttgart
Baptist Health-Fort Smith
Baptist Health-Fort Smith
Baptist Memorial Hospital-Crittenden
Baxter Health
Chambers Memorial Hospital
CHI St. Vincent Hot Springs
CHI St. Vincent Infirmary
CHI St. Vincent North
Conway Regional Health System
Drew Memorial Health System
Forrest City Medical Center
Great River Medical Center
Helena Regional Medical Center
Jefferson Regional
Johnson Regional Medical Center
Levi Hospital
Magnolia Regional Medical Center
Medical Center of South Arkansas
Mena Regional Health System
Mercy Hospital Fort Smith
Mercy Hospital Northwest Arkansas
National Park Medical Center
NEA Baptist Memorial Hospital
North Arkansas Regional Medical Center
Northwest Health Physicians’ Specialty Hospital
Northwest Medical Center Bentonville
Northwest Medical Center Springdale
Ouachita County Medical Center
Saint Mary’s Regional Medical Center
Saline Memorial Hospital
Sevier County Medical Center
Siloam Springs Regional Hospital
St. Bernards Five Rivers
St. Bernards Medical Center
UAMS Medical Center
Unity Health
Unity Health Jacksonville
Unity Health Newport
Washington Regional Medical System
White River Health
Critical Access Hospitals (28)
Ashley County Medical Center
Baptist Health Medical CenterArkadelphia
Baptist Health Medical Center-Heber Springs
Bradley County Medical Center
CHI St. Vincent Morrilton
Chicot Memorial Medical Center
CrossRidge Community Hospital
Dallas County Medical Center
Dardanelle Regional Medical Center
Delta Memorial Hospital
DeWitt Hospital & Nursing Home
Eureka Springs Hospital
Fulton County Hospital
Howard Memorial Hospital
Izard Regional Hospital
Lawrence Memorial Hospital
Little River Medical Center
McGehee Hospital
Mercy Hospital Berryville
Mercy Hospital Booneville
Mercy Hospital Ozark
Mercy Hospital Paris
Mercy Hospital Waldron
Ozark Health Medical Center
Ozarks Community Hospital
Piggott Health System
SMC Regional Medical Center
Stone County Medical Center
Inpatient Psych Hospitals (11)
Arkansas State Hospital
Conway Behavioral Health
Methodist Behavioral Hospital
Perimeter Behavioral Hospital of W. Memphis
Pinnacle Pointe Behavioral Healthcare System
Rivendell Behavioral Health Services
Riverview Behavioral Health
Springwoods Behavioral Health Hospital
The BridgeWay
Valley Behavioral Health System
Vantage Point of NWA
Inpatient Rehab Hospitals (7)
Baptist Health Rehabilitation Institute
CHI St. Vincent Hot Springs Rehabilitation Hospital
CHI St. Vincent Sherwood Rehabilitation Hospital
Conway Regional Rehabilitation Hospital
Encompass Health Rehabilitation Hospital, a partner of Washington Regional
Mercy Rehabilitation Hospital
Fort Smith
Mercy Rehabilitation ServicesNorthwest Arkansas
Veterans Affairs Hospitals (2)
Central Arkansas Veterans Healthcare System
Veterans Health Care System of the Ozarks
Long Term Care Hospitals (4)
Advanced Care Hospital of White County
Arkansas Continued Care Hospital of Jonesboro
Baptist Health Extended Care Hospital
Cornerstone Speciality Hospitals
Little Rock
Special Focus Hospitals (3)
Arkansas Children’s Hospital
Arkansas Children’s Northwest
Willow Creek Women’s Hospital
Out-of-State Border City Hospitals (2)
CHRISTUS St. Michael Health System
Regional One Health
Non-Hospital Facilities (3)
19th Medical Group
Arkansas Hospice
CARTI
35 ARKANSAS HOSPITALS | SUMMER 2023
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
36 SUMMER 2023 | ARKANSAS HOSPITALS CITY HOSPITAL TYPE OF HOSPITAL LICENSED BEDS TRAUMA SYSTEM SELECTED SPECIALTY SERVICE LINES ARKADELPHIA BAPTIST HEALTH MEDICAL CENTER-ARKADELPHIA MEDICAL-SURGICAL 25 LEVEL IV OB/SB/HH ASHDOWN LITTLE RIVER MEDICAL CENTER MEDICAL-SURGICAL 25 SB/ICF/HH BARLING VALLEY BEHAVIORAL HEALTH SYSTEM PSYCHIATRIC 114 PSYCH BATESVILLE WHITE RIVER HEALTH MEDICAL-SURGICAL 224 LEVEL III OB/PSYCH/SNF/REHAB/PALL BENTON RIVENDELL BEHAVIORAL HEALTH SERVICES PSYCHIATRIC 80 PSYCH BENTON SALINE MEMORIAL HOSPITAL MEDICAL-SURGICAL 177 OB/PSYCH/REHAB BENTONVILLE NORTHWEST MEDICAL CENTER BENTONVILLE MEDICAL-SURGICAL 128 LEVEL III HH/PALL BERRYVILLE MERCY HOSPITAL BERRYVILLE MEDICAL-SURGICAL 25 SB/HH/PALL BLYTHEVILLE GREAT RIVER MEDICAL CENTER MEDICAL-SURGICAL 99 LEVEL IV OB BOONEVILLE MERCY HOSPITAL BOONEVILLE MEDICAL-SURGICAL 25 LEVEL IV SB/HH/PALL CALICO ROCK IZARD REGIONAL HOSPITAL MEDICAL-SURGICAL 25 SB/HH CAMDEN OUACHITA COUNTY MEDICAL CENTER MEDICAL-SURGICAL 98 LEVEL IV OB/SB/SNF/REHAB/HH CLARKSVILLE JOHNSON REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 90 LEVEL IV OB/PSYCH/REHAB/HH CLINTON OZARK HEALTH MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB/SNF/HH CONWAY BAPTIST HEALTH MEDICAL CENTER-CONWAY MEDICAL-SURGICAL 120 LEVEL III OB/REHAB CONWAY CONWAY BEHAVIORAL HEALTH PSYCHIATRIC 80 PSYCH CONWAY CONWAY REGIONAL HEALTH SYSTEM MEDICAL-SURGICAL 150 LEVEL III OB/PSYCH/REHAB/HH/PALL CONWAY CONWAY REGIONAL REHABILITATION HOSPITAL REHABILITATION 26 REHAB CROSSETT ASHLEY COUNTY MEDICAL CENTER MEDICAL-SURGICAL 33 LEVEL IV OB/SB/REHAB DANVILLE CHAMBERS MEMORIAL HOSPITAL MEDICAL-SURGICAL 42 LEVEL IV PSYCH/SB/HH DARDANELLE DARDANELLE REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 35 LEVEL IV SB/PSYCH DE QUEEN SEVIER COUNTY MEDICAL CENTER MEDICAL-SURGICAL 14 DEWITT DEWITT HOSPITAL & NURSING HOME MEDICAL-SURGICAL 25 SB/ICF DUMAS DELTA MEMORIAL HOSPITAL MEDICAL-SURGICAL 25 OB/SB/HH EL DORADO MEDICAL CENTER OF SOUTH ARKANSAS MEDICAL-SURGICAL 166 LEVEL III OB/REHAB EUREKA SPRINGS EUREKA SPRINGS HOSPITAL MEDICAL-SURGICAL 15 LEVEL IV SB/HH FAYETTEVILLE ENCOMPASS HEALTH REHABILITATION HOSPITAL, A PARTNER OF WASHINGTON REGIONAL REHABILITATION 80 REHAB FAYETTEVILLE NORTHWEST HEALTH PHYSICIANS’ SPECIALTY HOSPITAL MEDICAL-SURGICAL 20 FAYETTEVILLE SPRINGWOODS BEHAVIORAL HEALTH HOSPITAL PSYCHIATRIC 80 PSYCH FAYETTEVILLE VANTAGE POINT OF NWA PSYCHIATRIC 114 PSYCH FAYETTEVILLE VETERANS HEALTH CARE SYSTEM OF THE OZARKS VETERANS AFFAIRS 73 PSYCH FAYETTEVILLE WASHINGTON REGIONAL MEDICAL SYSTEM MEDICAL-SURGICAL 425 LEVEL II HH/PALL FORDYCE DALLAS COUNTY MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB FORREST CITY FORREST CITY MEDICAL CENTER MEDICAL-SURGICAL 118 LEVEL IV OB/PSYCH/SB/HH FORT SMITH BAPTIST HEALTH-FORT SMITH MEDICAL-SURGICAL 492 LEVEL III PSYCH/HH FORT SMITH MERCY HOSPITAL FORT SMITH MEDICAL-SURGICAL 348 LEVEL III REHAB/HH FORT SMITH MERCY REHABILITATION HOSPITAL FORT SMITH REHABILITATION 50 REHAB GRAVETTE OZARKS COMMUNITY HOSPITAL MEDICAL-SURGICAL 25 SB HARRISON NORTH ARKANSAS REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 174 LEVEL III OB/PSYCH/HH HEBER SPRINGS BAPTIST HEALTH MEDICAL CENTER-HEBER SPRINGS MEDICAL-SURGICAL 25 LEVEL IV SB/HH HELENA HELENA REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 155 SB/HH HOT SPRINGS CHI ST. VINCENT HOT SPRINGS MEDICAL-SURGICAL 282 LEVEL II OB/PSYCH/REHAB/HH HOT SPRINGS CHI ST. VINCENT HOT SPRINGS REHABILITATION HOSPITAL REHABILITATION 48 REHAB HOT SPRINGS LEVI HOSPITAL MEDICAL-SURGICAL 50 PSYCH/REHAB HOT SPRINGS NATIONAL PARK MEDICAL CENTER MEDICAL-SURGICAL 163 OB/PSYCH/REHAB JACKSONVILLE 19TH MEDICAL GROUP INFIRMARY JACKSONVILLE UNITY HEALTH JACKSONVILLE MEDICAL-SURGICAL 29 PSYCH JOHNSON WILLOW CREEK WOMEN’S HOSPITAL MED-SURG (OB/GYN) 64 OB JONESBORO ARKANSAS CONTINUED CARE HOSPITAL OF JONESBORO LONG TERM CARE 99 JONESBORO NEA BAPTIST MEMORIAL HOSPITAL MEDICAL-SURGICAL 228 LEVEL III OB/REHAB/PALL JONESBORO ST. BERNARDS MEDICAL CENTER MEDICAL-SURGICAL 440 LEVEL III OB/PSYCH/HH/PALL LAKE VILLAGE CHICOT MEMORIAL MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB/HH LITTLE ROCK ARKANSAS CHILDREN’S HOSPITAL MED-SURG (PED) 336 LEVEL I REHAB/PALL LITTLE ROCK ARKANSAS STATE HOSPITAL PSYCHIATRIC 222 PSYCH
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
37 ARKANSAS HOSPITALS | SUMMER 2023 CITY HOSPITAL TYPE OF HOSPITAL LICENSED BEDS TRAUMA SYSTEM SELECTED SPECIALTY SERVICE LINES LITTLE ROCK BAPTIST HEALTH EXTENDED CARE HOSPITAL LONG TERM CARE 36 PALL LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-LITTLE ROCK MEDICAL-SURGICAL 871 LEVEL II OB/PSYCH/HH/PALL LITTLE ROCK BAPTIST HEALTH REHABILITATION INSTITUTE REHABILITATION 120 PALL LITTLE ROCK CARTI OP CANCER CENTER LITTLE ROCK CENTRAL ARKANSAS VETERANS HEALTHCARE SYSTEM VETERANS AFFAIRS 505 PSYCH/REHAB/HH/PALL/LTC LITTLE ROCK CHI ST. VINCENT INFIRMARY MEDICAL-SURGICAL 615 LEVEL II PSYCH/HH/PALL LITTLE ROCK CORNERSTONE SPECIALITY HOSPITALS LITTLE ROCK LONG TERM CARE 40 LITTLE ROCK PINNACLE POINTE BEHAVIORAL HEALTHCARE SYSTEM PSYCHIATRIC 127 PSYCH LITTLE ROCK UAMS MEDICAL CENTER MEDICAL-SURGICAL 535 LEVEL I OB/PALL LITTLE ROCK, HOT SPRINGS, RUSSELLVILLE ARKANSAS HOSPICE INPATIENT HOSPICE 24 PALL MAGNOLIA MAGNOLIA REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 49 LEVEL IV OB/HH MALVERN BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY MEDICAL-SURGICAL 72 LEVEL IV PSYCH/SB/HH MAUMELLE METHODIST BEHAVIORAL HOSPITAL PSYCHIATRIC 60 PSYCH MCGEHEE MCGEHEE HOSPITAL MEDICAL-SURGICAL 25 SB MEMPHIS, TN REGIONAL ONE HEALTH MEDICAL-SURGICAL 620 LEVEL I MENA MENA REGIONAL HEALTH SYSTEM MEDICAL-SURGICAL 65 LEVEL IV OB/PSYCH/REHAB MONTICELLO DREW MEMORIAL HEALTH SYSTEM MEDICAL-SURGICAL 49 OB/PSYCH/SB/REHAB/HH MORRILTON CHI ST. VINCENT MORRILTON MEDICAL-SURGICAL 25 LEVEL IV SB/HH MOUNTAIN HOME BAXTER HEALTH MEDICAL-SURGICAL 268 LEVEL III OB/PSYCH/REHAB/HH MOUNTAIN VIEW STONE COUNTY MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB NASHVILLE HOWARD MEMORIAL HOSPITAL MEDICAL-SURGICAL 20 SB/HH NEWPORT UNITY HEALTH NEWPORT MEDICAL-SURGICAL 35 LEVEL IV OB/PSYCH NORTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-N. LITTLE ROCK MEDICAL-SURGICAL 225 LEVEL III OB/REHAB/PALL NORTH LITTLE ROCK THE BRIDGEWAY PSYCHIATRIC 127 PSYCH OSCEOLA SMC REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 25 LEVEL IV SB OZARK MERCY HOSPITAL OZARK MEDICAL-SURGICAL 25 LEVEL IV SB/HH/PALL PARAGOULD ARKANSAS METHODIST MEDICAL CENTER MEDICAL-SURGICAL 129 LEVEL IV OB/SB/REHAB/HH PARIS MERCY HOSPITAL PARIS MEDICAL-SURGICAL 16 LEVEL IV SB/HH/PALL PIGGOTT PIGGOTT HEALTH SYSTEM MEDICAL-SURGICAL 25 LEVEL IV SB/HH PINE BLUFF JEFFERSON REGIONAL MEDICAL-SURGICAL 300 LEVEL III OB/PSYCH/REHAB/HH POCAHONTAS ST. BERNARDS FIVE RIVERS MEDICAL-SURGICAL 50 LEVEL IV PSYCH/SB/HH ROGERS MERCY HOSPITAL NORTHWEST ARKANSAS MEDICAL-SURGICAL 275 LEVEL III REHAB/HH ROGERS MERCY REHABILITATION SERVICES - NORTHWEST ARKANSAS REHABILITATION REHAB RUSSELLVILLE SAINT MARY’S REGIONAL MEDICAL CENTER MEDICAL-SURGICAL 170 LEVEL III OB/PSYCH/REHAB SALEM FULTON COUNTY HOSPITAL MEDICAL-SURGICAL 25 LEVEL IV SB SEARCY ADVANCED CARE HOSPITAL OF WHITE COUNTY LONG TERM CARE 20 PALL SEARCY UNITY HEALTH MEDICAL-SURGICAL 438 LEVEL III OB/PSYCH/REHAB/HH/PALL SHERWOOD CHI ST. VINCENT NORTH MEDICAL-SURGICAL 69 LEVEL IV HH/PALL SHERWOOD CHI ST. VINCENT SHERWOOD REHABILITATION HOSPITAL REHABILITATION 80 REHAB SILOAM SPRINGS SILOAM SPRINGS REGIONAL HOSPITAL MEDICAL-SURGICAL 73 LEVEL IV OB/SB/PALL SPRINGDALE ARKANSAS CHILDREN’S NORTHWEST MED-SURG (PED) 24 LEVEL IV SPRINGDALE NORTHWEST MEDICAL CENTER SPRINGDALE MEDICAL-SURGICAL 222 LEVEL III OB/PSYCH/SB/REHAB/HH STUTTGART BAPTIST HEALTH MEDICAL CENTER-STUTTGART MEDICAL-SURGICAL 49 LEVEL IV OB/SB/PALL TEXARKANA RIVERVIEW BEHAVIORAL HEALTH PSYCHIATRIC 62 PSYCH TEXARKANA, TX CHRISTUS ST. MICHAEL HEALTH SYSTEM MEDICAL-SURGICAL 354 LEVEL III VAN BUREN BAPTIST HEALTH-VAN BUREN MEDICAL-SURGICAL 103 LEVEL IV WALDRON MERCY HOSPITAL WALDRON MEDICAL-SURGICAL 24 LEVEL IV SB/HH/PALL WALNUT RIDGE LAWRENCE MEMORIAL HOSPITAL MEDICAL-SURGICAL 25 SB/PALL WARREN BRADLEY COUNTY MEDICAL CENTER MEDICAL-SURGICAL 33 OB/PSYCH/SB/HH WEST MEMPHIS BAPTIST MEMORIAL HOSPITAL-CRITTENDEN MEDICAL-SURGICAL 11 WEST MEMPHIS PERIMETER BEHAVIORAL HOSPITAL OF W. MEMPHIS PSYCHIATRIC 54 PSYCH WYNNE CROSSRIDGE COMMUNITY HOSPITAL MEDICAL-SURGICAL 25 SB/HH OB=Obstetrics, Psych=Psychatric, SB=Swing Beds, ICF=Intermediate Care Facility, SNF=Skilled Nursing Facility, Rehab=Rehabilitation, HH=Home Health, Hosp=Hospice Sources: Arkansas Department of Health; Self-reported information provided to the Arkansas Hospital Association
STATEWIDE HOSPITAL FINANCIAL AND UTILIZATION INDICATORS, 2016 - 2021
38 SUMMER 2023 | ARKANSAS HOSPITALS
INDICATOR 2016 2017 2018 2019 2020 2021 BEDS AVAILABLE 9,634 9,664 9,517 9,145 9,518 9,590 ADMISSIONS 359,359 363,070 358,222 364,291 342,864 347,411 PATIENT DAYS 1,846,634 1,861,122 1,828,470 1,826,976 1,791,995 1,935,306 AVG. LENGTH OF STAY 5.1 5.1 5.1 5.0 5.2 5.6 NON-EMERGENCY OP VISITS 4,570,177 4,629,383 4,925,120 4,914,195 4,377,227 4,817,914 OUTPATIENT VISITS 6,086,166 6,148,539 6,434,568 6470401 5,729,718 6,228,647 NON-EMERGENCY AS A % OF TOTAL OP VISITS 75.1% 75.3% 76.5% 75.9% 76.4% 77.4% ADJUSTED PATIENT DAYS 3,963,653 4,125,703 4,148,600 4,276,157 4,215,730 4,381,777 OCCUPANCY RATE 52.5% 52.8% 52.6% 54.7% 51.6% 55.3% INPATIENT SURGERIES 94,627 95,013 94,924 92,357 83,032 79,866 OUTPATIENT SURGERIES 200,832 203,105 215,656 226,136 194,138 207,801 TOTAL SURGERIES 295,459 298,118 310,580 318,493 277,170 287,667 OUTPATIENT AS % OF TOTAL SURGERIES 67.97% 68.13% 69.44% 71.00% 70.04% 72.24% TOTAL FULL-TIME EQUIVALENT EMPLOYEES 47,825 49,832 50,358 50,173 49,502 49,027 FULL-TIME EQUIVALENT EMPLOYEES PER ADJUSTED OCCUPIED BED 4.40 4.41 4.43 4.28 4.29 4.08 GROSS REVENUE, INPATIENT $12,460,694,916 $13,396,489,708 $13,777,391,679 $14,814,502,613 $14,965,703,755 $17,185,062,486 GROSS REVENUE, OUTPATIENT $12,952,790,887 $14,212,477,805 $15,450,146,464 $17,025,641,576 $16,733,703,930 $18,570,833,303 GROSS PATIENT REVENUE $25,413,485,803 $27,608,967,513 $29,227,538,143 $31,840,144,189 $31,699,407,685 $35,755,895,789 BAD DEBTS $444,692,383 $469,305,416 $502,016,281 $509,174,368 $503,958,456 $512,576,407 CHARITY $376,732,202 $339,342,080 $358,871,422 $442,315,671 $499,580,152 $574,072,837 MEDICARE, MEDICAID & OTHER PAYER WRITEOFFS $17,636,673,879 $19,440,530,333 $20,647,010,804 $22,702,507,161 $22,706,699,474 $25,738,880,672 TOTAL DEDUCTIONS $18,458,098,464 $20,249,177,829 $21,507,898,507 $23,653,997,200 $23,710,238,082 $26,825,529,916 NET PATIENT REVENUE $6,955,387,339 $7,359,789,684 $7,719,639,636 $8,186,146,989 $7,989,169,603 $8,930,365,873 OTHER OPERATING REVENUE $307,097,211 $381,973,773 $395,516,849 $433,117,737 $760,697,334 $919,369,130 NONOPERATING REVENUE $82,544,865 $118,736,986 $44,821,792 $145,788,360 $164,859,866 $246,467,868 TOTAL NET REVENUE $7,345,029,415 $7,860,500,443 $8,159,978,277 $8,765,053,086 $8,914,726,803 $10,096,202,871 PAYROLL EXPENSE $2,510,431,790 $2,833,267,007 $2,989,469,225 $3,040,326,208 $3,122,035,492 $3,542,564,965 TOTAL EXPENSE $6,803,364,553 $7,372,516,174 $7,797,448,234 $8,049,927,966 $8,206,104,259 $9,161,715,585 PATIENT REVENUE MARGIN 2.19% -0.17% -1.01% 1.66% -2.72% -2.59% TOTAL MARGIN 7.37% 6.21% 4.44% 8.16% 7.95% 9.26% CHARGE PER ADJUSTED INPATIENT DAY $6,411.63 $6,691.94 $7,045.16 $7,445.97 $7,519.32 $8,160.14 PAYMENT PER ADJUSTED INPATIENT DAY $1,754.79 $1,783.89 $1,860.78 $1,914.37 $1,895.09 $2,038.07 EXPENSE PER ADJUSTED INPATIENT DAY $1,716.44 $1,786.97 $1,879.54 $1,882.51 $1,946.54 $2,090.87 PAYROLL PER ADJUSTED INPATIENT DAY $633.36 $686.74 $720.60 $710.99 $740.57 $808.48 PAYROLL AS % OF TOTAL EXPENSE 36.9% 38.4% 38.3% 37.8% 38.0% 38.7% BAD DEBT AND CHARITY AS % OF TOTAL CHARGE 3.2% 2.9% 2.9% 3.0% 3.2% 3.0% TOTAL DEDUCTIONS AS % OF TOTAL CHARGE 72.6% 73.3% 73.6% 74.3% 74.8% 75.0% OUTPT. REVENUE AS % TOTAL PATIENT REVENUE 51.0% 51.5% 52.9% 53.5% 52.8% 51.9% ADMISSIONS PER BED 37.3 37.6 37.6 39.8 36.0 36.2 PATIENT DAYS PER 1,000 POPULATION 618.0 619.5 606.7 605.4 591.2 639.6 ADMISSIONS PER 1,000 POPULATION 120.3 120.9 118.9 120.7 113.1 114.8 POPULATION (000’S) 2,988 3,004 3,014 3,018 3,031 3,026 Source: American Hospital Association, Hospital Statistics
ARKANSAS HOSPITALS RECEIVING LOCAL TAX SUPPORT, 2023
39 ARKANSAS HOSPITALS | SUMMER 2023
HOSPITAL TAX RATE MILLAGE RATE YEAR APPROVED ANNUAL AMOUNT ESTIMATE ASHLEY COUNTY MEDICAL CENTER YES 0.25% 2016 $649,000 BAPTIST HEALTH MEDICAL CENTERHOT SPRING COUNTY YES 0.5% 2009 $1,600,000 BAPTIST HEALTH MEDICAL CENTERSTUTTGART YES 1.00% 2014 $2,300,000 BRADLEY COUNTY MEDICAL CENTER YES 1.00% YES .4 MILL 2009 $1,200,000 CHI ST. VINCENT MORRILTON YES 0.25% YES .25 MILL 2008 $1,000,000 CHICOT MEMORIAL MEDICAL CENTER YES 1.00% YES .5 MILL 2003 $1,100,000 CROSSRIDGE COMMUNITY HOSPITAL YES 1.00% 2000 $2,500,000 DALLAS COUNTY MEDICAL CENTER YES 1.00% 2005 $840,000 DELTA HEALTH SYSTEM YES 1.25% YES .5 MILL 2019 $840,000 DEWITT HOSPITAL & NURSING HOME YES 1.50% 2003 $850,000 DREW MEMORIAL HEALTH SYSTEM YES 0.25% 2015 $670,000 FULTON COUNTY HOSPITAL YES 0.50% 2007 $310,000 GREAT RIVER MEDICAL CENTER YES 0.50% YES 1 MILL 2015/1952 $2,439,800 JOHNSON REGIONAL MEDICAL CENTER YES .3 MILL 1977 $65,000 LAWRENCE MEMORIAL HOSPITAL YES 1.00% 2014 $2,100,000 LITTLE RIVER MEDICAL CENTER YES 0.50% 2000 $834,000 MAGNOLIA REGIONAL MEDICAL CENTER (A) YES 1.125% 2007 $2,600,000 MAGNOLIA REGIONAL MEDICAL CENTER (B) YES 0.250% 2004 $540,000 MCGEHEE HOSPITAL YES 1.00% 1999 $600,000 MERCY HOSPITAL BOONEVILLE YES 1.00% 2003 $360,000 MERCY HOSPITAL OZARK YES 1.00% 2001 $350,000 MERCY HOSPITAL PARIS YES 1.00% NA NA OZARK HEALTH MEDICAL CENTER YES .6 MILL 1951 $150,000 PIGGOTT COMMUNITY HOSPITAL YES 1.00% 2010 $360,000 SMC REGIONAL MEDICAL CENTER YES 0.50% YES 1 MILL 2015/1952 $829,300 ST. BERNARDS FIVE RIVERS YES 1.00% 2007 $800,000 NA=Information not available. Source: Self-reported information provided to the Arkansas Hospital Association
KEY FINANCIAL INDICATORS ARKANSAS AND SURROUNDING STATES, 2021
Hospitals charged this amount for the inpatient and outpatient care they provided in 2021:
But patients and payer groups didn’t pay the full amount of billed charges for various reasons. Government programs like Medicare and Medicaid, workers’ comp programs and others never pay the full hospital bill. Managed care plans and other insurers typically pay discounted amounts only, and individual patietns often can’t afford to pay some or any of the out-of-pocket costs related to their hospital bills. For those reasons, hospitals had to forfeit this much of their billed charges:
As a result, actual payments to hospitals were:
At the same time, hospitals spent this much providing patient care services…
…to patients needing care for this many adjusted patient days while being served.
So the revenue excess (loss) was:
In other words, hospitals made (or lost) this much on each of the equivalent days of care they provided to inpatients and outpatients:
Yielding a “patient service” margin of:
In addition, hospitals also received revenues from normal, day-today operations from services other than health care provided to patients, such as COVID relief dollars, space rental, cafeteria and gift shop sales, and operating gains:
Which raised total operating income to:
As a result, the “operating margin” rose to:
Hospitals also collected other types of revenue from sources including contributions, tax appropriations, and investments. Those amounted to:
That resulted in total funds available to reinvest in new equipment, update facilities, expand programs and repay debt equalling:
Source: American Hospital Association Hospital Statistics
40 SUMMER 2023 | ARKANSAS HOSPITALS
ARKANSAS
LOUISIANA
MISSISSIPPI
MISSOURI
OKLAHOMA
TENNESSEE
TEXAS
UNITED STATES
$35,755,895,789 $67,435,045,649 $37,643,334,521 $95,931,336,978 $55,391,500,253 $97,141,348,020 $439,159,689,906 $4,699,267,017,842
$26,825,529,916 50,807,486,919 29,138,247,404 69,802,922,212 43,481,825,430 75,627,281,740 349,956,574,150 $3,523,744,135,034
8,930,365,873 16,627,558,730 8,505,087,117 26,128,414,766 11,909,674,823 21,514,066,280 89,203,115,756 1,175,522,882,808
9,161,715,585 17,650,751,751 8,694,534,816 26,509,098,117 11,743,640,210 23,110,301,517 85,183,477,210 $1,193,613,054,823
4,381,777 7,119,826 6,660,638 10,016,515 5,317,234 9,429,759 29,239,174 414,003,966
($231,349,712) ($1,023,193,021) ($189,447,699) ($380,683,351) $166,034,613 ($1,596,235,237) $4,019,638,546 ($18,090,172,015)
($52.80) ($143.71) ($28.44) ($38.01) $31.23 ($169.28) $137.47 ($43.70)
-2.59% -6.15% -2.23% -1.46% 1.39% -7.42% 4.51% -1.54%
919,369,130 2,072,775,036 634,745,944 2,267,824,468 933,111,292 2,384,047,591 9,235,474,798 $114,638,278,813
$688,019,418 $1,049,582,015 $445,298,245 $1,887,141,117 $1,099,145,905 $787,812,354 $13,255,113,344 $27,465,885,741
6.99% 5.61% 4.87% 6.65% 8.56% 3.30% 13.47% 2.13%
246,467,868 443,347,943 360,236,827 1,295,197,961 639,869,331 436,143,095 4,985,093,768 $58,168,592,954
$934,487,286 $1,492,929,958 $805,535,072 $3,182,339,078 $1,739,015,236 $1,223,955,449 $18,240,207,112 $85,634,478,695
on investment totalling: 9.26% 7.80% 8.48% 10.72% 12.90% 5.03% 17.64% 6.35%
For a return
COMPARATIVE FINANCIAL INDICATORS U.S. COMMUNITY HOSPITALS
41 ARKANSAS HOSPITALS | SUMMER 2023 AVERAGE CHARGE PER HOSPITAL STAY ($) AVERAGE PAYMENT PER HOSPITAL STAY ($) AVERAGE OPERATING COST PER HOSPITAL STAY ($) MARGIN ON PATIENT CARE SERVICES ($) DISTRICT OF COLUMBIA 115,248 DISTRICT OF COLUMBIA 31,670 DISTRICT OF COLUMBIA 31,779 UTAH 17.65% COLORADO 109,184 CALIFORNIA 24,148 NEW YORK 26,325 IDAHO 16.93% CALIFORNIA 107,732 UTAH 24,057 MAINE 25,058 COLORADO 10.79% NEVADA 100,544 COLORADO 23,491 CALIFORNIA 24,923 VIRGINIA 8.14% TEXAS 88,793 MAINE 23,258 WASHINGTON 23,473 NEW MEXICO 8.07% FLORIDA 87,349 NEW YORK 23,031 MASSACHUSETTS 22,257 ALASKA 6.97% PENNSYLVANIA 84,708 WASHINGTON 22,728 HAWAII 21,815 KENTUCKY 4.74% ARIZONA 84,704 ALASKA 22,471 OREGON 21,311 TEXAS 4.51% UTAH 81,474 DELAWARE 21,376 COLORADO 20,957 FLORIDA 4.23% NEW MEXICO 79,506 IDAHO 20,939 ALASKA 20,905 ARIZONA 4.20% NEW YORK 79,464 NEW MEXICO 20,515 MINNESOTA 20,832 DELAWARE 4.19% WSC REGION 79,185 OREGON 20,104 DELAWARE 20,480 WISCONSIN 3.33% ALASKA 78,732 NEBRASKA 20,065 MARYLAND 19,933 INDIANA 2.61% NEW JERSEY 76,820 MONTANA 19,896 NEBRASKA 19,870 ALABAMA 2.58% IDAHO 75,565 HAWAII 19,821 CONNECTICUT 19,849 WYOMING 2.39% WASHINGTON 74,599 MINNESOTA 19,813 UTAH 19,810 WSC REGION 2.31% U.S. 74,130 MARYLAND 19,071 MONTANA 19,692 OKLAHOMA 1.39% INDIANA 69,972 INDIANA 19,023 NORTH DAKOTA 19,229 MONTANA 1.03% KENTUCKY 67,853 MASSACHUSETTS 18,977 VERMONT 19,162 NEBRASKA 0.97% VIRGINIA 67,787 U.S. 18,544 NEW MEXICO 18,859 GEORGIA 0.95% OKLAHOMA 66,828 CONNECTICUT 18,502 U.S. 18,829 OHIO 0.91% ILLINOIS 65,883 NORTH DAKOTA 18,261 INDIANA 18,526 NORTH CAROLINA 0.37% KANSAS 65,810 OHIO 18,214 OHIO 18,048 DISTRICT OF COLUMBIA -0.34% GEORGIA 64,881 ARIZONA 18,128 PENNSYLVANIA 18,046 PENNSYLVANIA -0.83% TENNESSEE 63,763 VIRGINIA 18,041 NEW HAMPSHIRE 17,991 KANSAS -1.01% OHIO 63,583 TEXAS 18,036 NEVADA 17,595 MISSOURI -1.46% SOUTH CAROLINA 63,219 WISCONSIN 17,972 SOUTH DAKOTA 17,595 U.S. -1.54% MINNESOTA 63,038 PENNSYLVANIA 17,899 ILLINOIS 17,420 NEVADA -2.00% MAINE 62,011 NEW HAMPSHIRE 17,623 IDAHO 17,393 NEW HAMPSHIRE -2.09% CONNECTICUT 61,058 NEVADA 17,251 WISCONSIN 17,372 MISSISSIPPI -2.23% ALABAMA 60,942 SOUTH DAKOTA 17,103 ARIZONA 17,366 SOUTH CAROLINA -2.44% MISSOURI 59,987 ILLINOIS 16,822 TEXAS 17,223 ARKANSAS -2.59% MASSACHUSETTS 59,104 WSC REGION 16,781 MICHIGAN 16,727 SOUTH DAKOTA -2.88% LOUISIANA 58,687 KENTUCKY 16,692 MISSOURI 16,577 CALIFORNIA -3.21% HAWAII 58,433 VERMONT 16,634 VIRGINIA 16,573 WASHINGTON -3.27% NEBRASKA 58,115 MISSOURI 16,338 KANSAS 16,482 NEW JERSEY -3.28% NORTH CAROLINA 57,367 KANSAS 16,318 NEW JERSEY 16,470 ILLINOIS -3.55% NEW HAMPSHIRE 56,895 GEORGIA 16,304 WSC REGION 16,392 MICHIGAN -3.56% DELAWARE 54,162 WYOMING 16,246 WEST VIRGINIA 16,325 WEST VIRGINIA -3.74% MISSISSIPPI 54,043 MICHIGAN 16,151 GEORGIA 16,149 MARYLAND -4.52% WISCONSIN 53,894 NORTH CAROLINA 16,043 RHODE ISLAND 16,068 MINNESOTA -5.14% SOUTH DAKOTA 53,387 NEW JERSEY 15,947 IOWA 15,989 NORTH DAKOTA -5.30% OREGON 52,212 WEST VIRGINIA 15,736 NORTH CAROLINA 15,984 OREGON -6.00% NORTH DAKOTA 50,638 FLORIDA 15,313 KENTUCKY 15,901 LOUISIANA -6.15% MICHIGAN 50,476 IOWA 14,953 WYOMING 15,857 IOWA -6.92% WEST VIRGINIA 50,431 SOUTH CAROLINA 14,662 LOUISIANA 15,361 CONNECTICUT -7.28% ARKANSAS 49,466 LOUISIANA 14,470 TENNESSEE 15,170 TENNESSEE -7.42% IOWA 45,890 RHODE ISLAND 14,396 SOUTH CAROLINA 15,021 MAINE -7.74% MONTANA 44,006 OKLAHOMA 14,369 FLORIDA 14,665 HAWAII -10.06% RHODE ISLAND 43,922 TENNESSEE 14,122 OKLAHOMA 14,168 RHODE ISLAND -11.61% VERMONT 40,076 ALABAMA 12,806 ARKANSAS 12,675 NEW YORK -14.30% WYOMING 39,019 ARKANSAS 12,355 MISSISSIPPI 12,482 VERMONT -15.20% MARYLAND 28,282 MISSISSIPPI 12,210 ALABAMA 12,475 MASSACHUSETTS -17.28% Source: American Hospital Association Hospital Statistics. Calculated using most recent data (hospital fiscal year 2021)
HOSPITAL ACCESS BY COUNTY
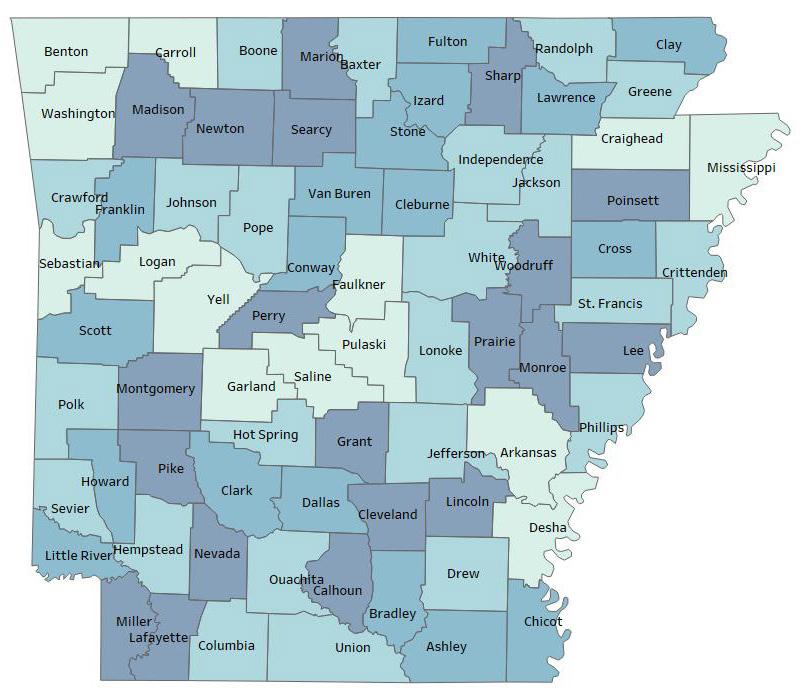

42 SUMMER 2023 | ARKANSAS HOSPITALS
COUNTY NO ACUTE CARE COMMUNITY HOSPITAL (20) SINGLE CRITICAL ACCESS HOSPITAL (18) SINGLE NON-CAH COMMUNITY HOSPITAL (23) MULTIPLE COMMUNITY HOSPITALS (14) ARKANSAS • ASHLEY • BAXTER • BENTON • BOONE • BRADLEY • CALHOUN • CARROLL • CHICOT • CLARK • CLAY • CLEBURNE • CLEVELAND • COLUMBIA • CONWAY • CRAIGHEAD • CRAWFORD • CRITTENDEN • CROSS • DALLAS • DESHA • DREW • FAULKNER • FRANKLIN • FULTON • GARLAND • COUNTY NO ACUTE CARE COMMUNITY HOSPITAL (20) SINGLE CRITICAL ACCESS HOSPITAL (18) SINGLE NON-CAH COMMUNITY HOSPITAL (23) MULTIPLE COMMUNITY HOSPITALS (14) GRANT • GREENE • HEMPSTEAD • HOT SPRING • HOWARD • INDEPENDENCE • IZARD • JACKSON • JEFFERSON • JOHNSON • LAFAYETTE • LAWRENCE • LEE • LINCOLN • LITTLE RIVER • LOGAN • LONOKE • MADISON • MARION • MILLER • MISSISSIPPI • MONROE • MONTGOMERY • NEVADA • NEWTON • OUACHITA • PERRY • PHILLIPS • PIKE • POINSETT • POLK • POPE • PRAIRIE • PULASKI • RANDOLPH • SALINE • SCOTT • SEARCY • SEBASTIAN • SEVIER • SHARP • ST. FRANCIS • STONE • UNION • VAN BUREN • WASHINGTON • WHITE • WOODRUFF • YELL •
AHA-MEMBER ORGANIZATIONS BY CONGRESSIONAL DISTRICT
1ST CONGRESSIONAL DISTRICT
Arkansas Continued Care Hospital of Jonesboro
Arkansas Methodist Medical Center
Baptist Health Medical Center-Stuttgart
Baptist Memorial Hospital-Crittenden
Baxter Regional Medical Center
Chicot Memorial Medical Center
CrossRidge Community Hospital
Delta Memorial Hospital
DeWitt Hospital & Nursing Home
Forrest City Medical Center
Fulton County Hospital
Great River Medical Center
Helena Regional Medical Center
Izard Regional Hospital
Lawrence Memorial Health Foundation, Inc.
McGehee Hospital
NEA Baptist Memorial Hospital
North Arkansas Regional Medical Center
Piggott Community Hospital
SMC Regional Medical Center
St. Bernards Five Rivers
St. Bernards Medical Center
Stone County Medical Center
Unity Health Newport
White River Health System
WoodRidge of West Memphis, LLC
Total = 26
2ND CONGRESSIONAL DISTRICT
19th Medical Group
Advanced Care Hospital of White County
Arkansas Children’s Hospital
Arkansas Hospice
Arkansas State Hospital
Baptist Health Extended Care Hospital
Baptist Health Medical Center-Conway
Baptist Health Medical Center-Heber Springs
Baptist Health Medical Center-Little Rock
Baptist Health Medical Center-North Little Rock
Baptist Health Rehabilitation Institute
CARTI
Central Arkansas Veterans Healthcare System
CHI St. Vincent Infirmary
CHI St. Vincent Morrilton
CHI St. Vincent North
CHI St. Vincent Sherwood Rehabilitation Hospital, a Partner of Encompass Health
Conway Behavioral Health
Conway Regional Health System
Conway Regional Rehabilitation Hospital
Cornerstone Specialty Hospitals Little Rock
Methodist Behavioral Hospital
Ozark Health Medical Center
Pinnacle Pointe Behavioral Healthcare System
Rivendell Behavioral Health Services
Saline Memorial Hospital
The BridgeWay
UAMS Medical Center
Unity Health
Unity Health Jacksonville
Total = 30
3RD
CONGRESSIONAL DISTRICT
Arkansas Children’s Northwest
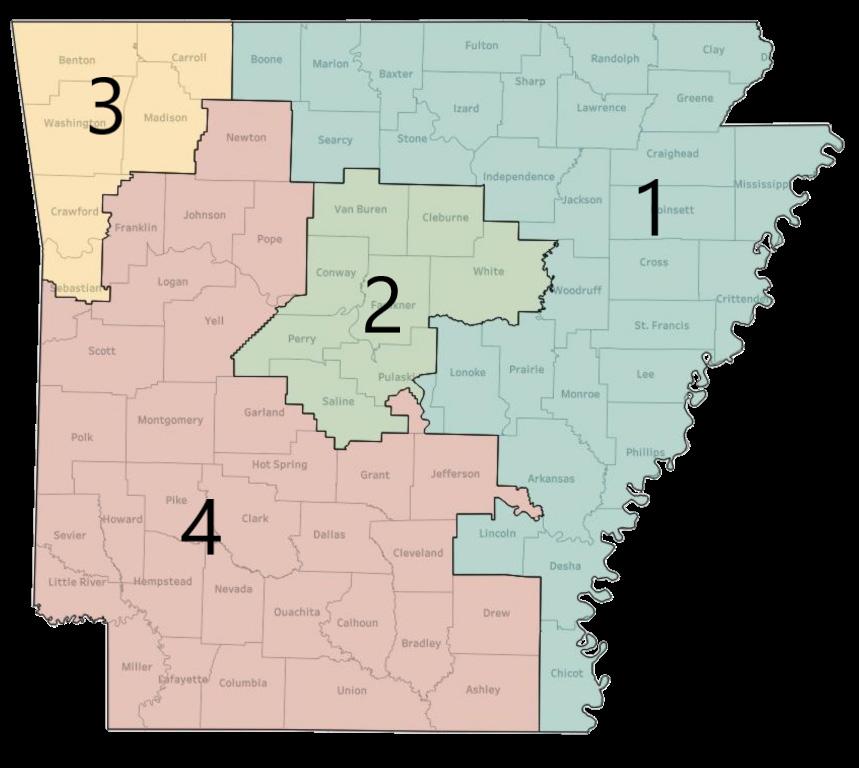
Baptist Health-Fort Smith
Baptist Health-Van Buren
Encompass Health Rehabilitation Hospital, a Partner of Washington Regional Eureka Springs Hospital
Mercy Hospital Berryville
Mercy Hospital Fort Smith
Mercy Hospital Northwest Arkansas
Mercy Rehabilitation Hospital Fort Smith
Mercy Rehabilitation Services - Northwest Arkansas
Northwest Health Physicians’ Specialty Hospital
Northwest Medical Center Bentonville
Northwest Medical Center Springdale
Ozarks Community Hospital
Siloam Springs Regional Hospital
Springwoods Behavioral Health Hospital
Valley Behavioral Health System
Vantage Point of NWA
Veterans Health Care System of the Ozarks
Washington Regional Medical System
Willow Creek Women’s Hospital
Total = 21
4TH CONGRESSIONAL DISTRICT
Ashley County Medical Center
Baptist Health Medical Center-Arkadelphia
Baptist Health Medical Center-Hot Spring County
Bradley County Medical Center
Chambers Memorial Hospital
CHI St. Vincent Hot Springs
CHI St. Vincent Hot Springs Rehab Hospital, a Partner of Encompass Health
Dallas County Medical Center
Dardanelle Regional Medical Center
Drew Memorial Health System
Howard Memorial Hospital
Jefferson Regional
Johnson Regional Medical Center
Levi Hospital
Little River Medical Center, Inc.
Magnolia Regional Medical Center
Medical Center of South Arkansas
Mena Regional Health System
Mercy Hospital Booneville
Mercy Hospital Ozark
Mercy Hospital Paris
Mercy Hospital Waldron
National Park Medical Center
Ouachita County Medical Center
Riverview Behavioral Health
Saint Mary’s Regional Medical Center
Sevier County Medical Center
Total = 27
ADDITIONAL AHA MEMBER HOSPITALS
INCLUDE:
CHRISTUS St. Michael Health System, Texarkana, TX
Regional One Health, Memphis, TN
43 ARKANSAS HOSPITALS | SUMMER 2023
AHA MEMBERS BY CONTROL AND SYSTEM AFFILIATION
44 SUMMER 2023 | ARKANSAS HOSPITALS HOSPITAL DESIGNATION CONTROL NONPROFIT CORPORATE GOV’T SYSTEM INFORMATION MULTI-HOSPITAL SYSTEM? CONTROLLING ORGANIZATION SYSTEM HOME 19TH MEDICAL GROUP √ U.S. DEPARTMENT OF DEFENSE ADVANCED CARE HOSPITAL OF WHITE COUNTY LTCH √ Y UNITY HEALTH SEARCY ARKANSAS CHILDREN’S HOSPITAL CHILDREN’S √ Y ARKANSAS CHILDREN’S LITTLE ROCK ARKANSAS CHILDREN’S NORTHWEST CHILDREN’S √ Y ARKANSAS CHILDREN’S LITTLE ROCK ARKANSAS CONTINUED CARE HOSPITAL OF JONESBORO LTCH √ LOCAL BOARD ARKANSAS HOSPICE INPATIENT HOSPICE √ LOCAL BOARD NORTH LITTLE ROCK ARKANSAS METHODIST MEDICAL CENTER RURAL/RRC √ LOCAL BOARD ARKANSAS STATE HOSPITAL IP PSYCH √ STATE ASHLEY COUNTY MEDICAL CENTER CAH √ LOCAL BOARD BAPTIST HEALTH EXTENDED CARE HOSPITAL LTCH √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-ARKADELPHIA CAH √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-CONWAY URBAN √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-HEBER SPRINGS CAH √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY RURAL/MDH √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-LITTLE ROCK URBAN √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-N. LITTLE ROCK URBAN √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH MEDICAL CENTER-STUTTGART RURAL/MDH √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH REHABILITATION INSTITUTE IRF √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH-FORT SMITH URBAN √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST HEALTH-VAN BUREN URBAN √ Y BAPTIST HEALTH LITTLE ROCK BAPTIST MEMORIAL HOSPITAL-CRITTENDEN URBAN √ Y BAPTIST MEMORIAL HEALTHCARE CORP. MEMPHIS, TN BAXTER HEALTH RURAL/SCH/RRC √ LOCAL BOARD BRADLEY COUNTY MEDICAL CENTER CAH √ LOCAL BOARD CARTI √ LOCAL BOARD LITTLE ROCK CENTRAL ARKANSAS VETERANS HEALTHCARE SYSTEM URBAN/IP PSYCH/LTCH/ IRF/HOSP √ Y U.S. DEPARTMENT OF VETERANS AFFAIRS LITTLE ROCK/NLR CHAMBERS MEMORIAL HOSPITAL RURAL/SCH √ LOCAL BOARD CHI ST. VINCENT HOT SPRINGS URBAN/RRC √ Y COMMONSPIRIT HEALTH CHICAGO, IL CHI ST. VINCENT HOT SPRINGS REHABILITATION HOSPITAL IRF √ Y ENCOMPASS HEALTH BIRMINGHAM, AL CHI ST. VINCENT INFIRMARY URBAN √ Y COMMONSPIRIT HEALTH CHICAGO, IL CHI ST. VINCENT MORRILTON CAH √ Y COMMONSPIRIT HEALTH CHICAGO, IL CHI ST. VINCENT NORTH URBAN √ Y COMMONSPIRIT HEALTH CHICAGO, IL CHI ST. VINCENT SHERWOOD REHABILITATION HOSPITAL IRF √ Y ENCOMPASS HEALTH BIRMINGHAM, AL CHICOT MEMORIAL MEDICAL CENTER CAH √ LOCAL BOARD CHRISTUS ST. MICHAEL HEALTH SYSTEM URBAN (TX) √ Y CHRISTUS HEALTH IRVING, TX CONWAY BEHAVIORAL HEALTH IP PSYCH √ Y ACADIA HEALTHCARE FRANKLIN, TN CONWAY REGIONAL HEALTH SYSTEM URBAN √ Y CONWAY REGIONAL HEALTH SYSTEM CONWAY CONWAY REGIONAL REHABILITATION HOSPITAL IRF √ Y CONWAY REGIONAL HEALTH SYSTEM CONWAY CORNERSTONE SPECIALITY HOSPITALS LITTLE ROCK LTCH √ Y SCIONHEALTH LOUISVILLE, KY CROSSRIDGE COMMUNITY HOSPITAL CAH √ Y ST. BERNARDS HEALTH SYSTEM JONESBORO DALLAS COUNTY MEDICAL CENTER CAH √ COUNTY DARDANELLE REGIONAL MEDICAL CENTER CAH √ Y CONWAY REGIONAL HEALTH SYSTEM CONWAY DELTA MEMORIAL HOSPITAL CAH √ LOCAL BOARD DEWITT HOSPITAL & NURSING HOME CAH √ LOCAL BOARD DREW MEMORIAL HEALTH SYSTEM RURAL/SCH √ COUNTY ENCOMPASS HEALTH REHABILITATION HOSPITAL, A PARTNER OF WASHINGTON REGIONAL IRF √ Y ENCOMPASS HEALTH BIRMINGHAM, AL EUREKA SPRINGS HOSPITAL CAH √ EUREKA SPRINGS HOSPITAL COMMISSION EUREKA SPRINGS FORREST CITY MEDICAL CENTER RURAL/SCH √ Y QUORUM HEALTH FRANKLIN, TN FULTON COUNTY HOSPITAL CAH √ COUNTY GREAT RIVER MEDICAL CENTER RURAL/SCH/RRC √ COUNTY
45 ARKANSAS HOSPITALS | SUMMER 2023 HOSPITAL DESIGNATION CONTROL NONPROFIT CORPORATE GOV’T SYSTEM INFORMATION MULTI-HOSPITAL SYSTEM? CONTROLLING ORGANIZATION SYSTEM HOME HELENA REGIONAL MEDICAL CENTER RURAL/SCH √ Y QUORUM HEALTH FRANKLIN, TN HOWARD MEMORIAL HOSPITAL CAH √ LOCAL BOARD IZARD REGIONAL HOSPITAL CAH √ LOCAL BOARD JEFFERSON REGIONAL URBAN/SCH √ LOCAL BOARD JOHNSON REGIONAL MEDICAL CENTER RURAL/MDH √ LOCAL BOARD LAWRENCE MEMORIAL HOSPITAL CAH √ Y ST. BERNARDS HEALTH SYSTEM JONESBORO LEVI HOSPITAL URBAN √ LOCAL BOARD LITTLE RIVER MEDICAL CENTER CAH √ LOCAL BOARD MAGNOLIA REGIONAL MEDICAL CENTER RURAL/SCH √ LOCAL BOARD MCGEHEE HOSPITAL CAH √ LOCAL BOARD MEDICAL CENTER OF SOUTH ARKANSAS RURAL/SCH √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN MENA REGIONAL HEALTH SYSTEM RURAL/SCH √ CITY MERCY HOSPITAL BERRYVILLE CAH √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL BOONEVILLE CAH √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL FORT SMITH URBAN √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL NORTHWEST ARKANSAS URBAN √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL OZARK CAH √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL PARIS CAH √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY HOSPITAL WALDRON CAH √ Y MERCY HEALTH SYSTEM ST. LOUIS, MO MERCY REHABILITATION HOSPITAL FORT SMITH IRF √ Y LIFEPOINT BRENTWOOD, TN MERCY REHABILITATION SERVICES - NORTHWEST ARKANSAS IRF √ LIFEPOINT BRENTWOOD, TN METHODIST BEHAVIORAL HOSPITAL IP PSYCH √ Y METHODIST FAMILY HEALTH LITTLE ROCK NATIONAL PARK MEDICAL CENTER URBAN/RRC √ Y LIFEPOINT BRENTWOOD, TN NEA BAPTIST MEMORIAL HOSPITAL RRC √ Y BAPTIST MEMORIAL HEALTHCARE CORP. MEMPHIS, TN NORTH ARKANSAS REGIONAL MEDICAL CENTER RURAL/SCH/RRC √ LOCAL BOARD NORTHWEST HEALTH PHYSICIANS’ SPECIALTY HOSPITAL URBAN √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN NORTHWEST MEDICAL CENTER BENTONVILLE URBAN √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN NORTHWEST MEDICAL CENTER SPRINGDALE URBAN √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN OUACHITA COUNTY MEDICAL CENTER RURAL/SCH √ LOCAL BOARD OZARK HEALTH MEDICAL CENTER CAH √ LOCAL BOARD OZARKS COMMUNITY HOSPITAL CAH √ PERIMETER BEHAVIORAL HOSPITAL OF W. MEMPHIS IP PSYCH √ Y WOODRIDGE BEHAVIORAL CARE JACKSON, TN PIGGOTT HEALTH SYSTEM CAH √ CITY PINNACLE POINTE BEHAVIORAL HEALTHCARE SYSTEM IP PSYCH √ Y UNIVERSAL HEALTH SERVICES KING OF PRUSSIA, PA REGIONAL ONE HEALTH URBAN (TN) √ Y REGIONAL ONE HEALTH MEMPHIS, TN RIVENDELL BEHAVIORAL HEALTH SERVICES IP PSYCH √ Y UNIVERSAL HEALTH SERVICES KING OF PRUSSIA, PA RIVERVIEW BEHAVIORAL HEALTH IP PSYCH √ Y ACADIA HEALTHCARE FRANKLIN, TN SAINT MARY’S REGIONAL MEDICAL CENTER RURAL/RRC √ Y LIFEPOINT BRENTWOOD, TN SALINE MEMORIAL HOSPITAL URBAN √ Y LIFEPOINT BRENTWOOD, TN SEVIER COUNTY MEDICAL CENTER RURAL √ COUNTY SILOAM SPRINGS REGIONAL HOSPITAL URBAN √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN SMC REGIONAL MEDICAL CENTER CAH √ COUNTY SPRINGWOODS BEHAVIORAL HEALTH HOSPITAL IP PSYCH √ Y UNIVERSAL HEALTH SERVICES KING OF PRUSSIA, PA ST. BERNARDS FIVE RIVERS RURAL/SCH √ Y ST. BERNARDS HEALTH SYSTEM JONESBORO ST. BERNARDS MEDICAL CENTER URBAN/RRC √ Y ST. BERNARDS HEALTH SYSTEM JONESBORO STONE COUNTY MEDICAL CENTER CAH √ Y WHITE RIVER HEALTH SYSTEM BATESVILLE THE BRIDGEWAY IP PSYCH √ Y UNIVERSAL HEALTH SERVICES KING OF PRUSSIA, PA UAMS MEDICAL CENTER URBAN √ STATE UNITY HEALTH RURAL/SCH/RRC √ Y UNITY HEALTH SEARCY UNITY HEALTH JACKSONVILLE URBAN √ Y UNITY HEALTH SEARCY UNITY HEALTH NEWPORT CAH √ Y UNITY HEALTH SEARCY VALLEY BEHAVIORAL HEALTH SYSTEM IP PSYCH √ Y ACADIA HEALTHCARE FRANKLIN, TN VANTAGE POINT OF NWA IP PSYCH √ Y ACADIA HEALTHCARE FRANKLIN, TN VETERANS HEALTH CARE SYSTEM OF THE OZARKS √ U.S. DEPARTMENT OF VETERANS AFFAIRS WASHINGTON REGIONAL MEDICAL SYSTEM RURAL √ LOCAL BOARD WHITE RIVER HEALTH RURAL/SCH/RRC √ Y WHITE RIVER HEALTH SYSTEM BATESVILLE WILLOW CREEK WOMEN’S HOSPITAL URBAN √ Y COMMUNITY HEALTH SYSTEMS FRANKLIN, TN CAH=Critical Access Hospital; MDH=Medicare Dependent Hospital; RRC=Rural Referral Center; SCH=Sole Community Hospital; IRF=Inpatient Rehabilitation Facility; LTCH = Long-term Care Hospital ; IP Psych=Inpatient Psychiatric. Source: Self-reported information provided to the Arkansas Hospital Association
INPATIENT AND EMERGENCY DEPARTMENT DISCHARGES BY PAYER, 2021
UNINSURED INPATIENT ADMISSIONS AND COSTS, 2011-2021
46 SUMMER 2023 | ARKANSAS HOSPITALS
Arkansas Department of Health, Hospital Discharge Program ED INPATIENT 0% 25% 50% 75% 100% HMO/COMM. INS. MEDICAID MEDICARE OTHER GOV. PROGRAMS OTHER UNKNOWN SELF PAY/NO CHARGE 30% 35% 22% 29% 37% 19% 2% 2% 5% 6% 4% 9% $220 $160 $110 $55 $0 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 30,000 22,500 15,000 7,500 0 Arkansas Department of Health, Hospital Discharge Program SELF-PAY/ NO CHARGE PATIENTS ADMITTED EST. TOTAL UNCOVERED COSTS ($MILLIONS) COST ($MILLIONS) ADMISSIONS
HOSPITAL UNCOMPENSATED CARE COSTS, 2017-2021 TOP 20 DRGS, 2021
47 ARKANSAS HOSPITALS | SUMMER 2023 YEAR GROSS REVENUES (BILLED CHARGES) NET REVENUES (AMOUNT COLLECTED) OTHER OPERATING REVENUE GROSS+ OTHER REVENUE TOTAL OPERATING COSTS CHARGE RATIO 2017 $27,608,967,513 $7,359,789,684 $381,973,773 $27,990,941,286 $7,372,516,174 24.66% 2018 $29,227,538,143 $7,719,639,636 $395,516,849 $29,623,054,992 $7,797,448,234 24.63% 2019 $31,840,144,189 $8,186,146,989 $433,117,737 $32,273,261,926 $8,049,927,966 23.37% 2020 $31,699,407,685 $7,989,169,603 $760,697,334 $32,460,105,019 $8,206,104,259 23.73% 2021 $35,755,895,789 $8,930,365,873 $919,369,130 $36,675,264,919 $9,161,715,585 23.58% CHANGE 29.5% 21.3% 140.7% 31.0% 24.3% YEAR TOTAL UNCOLLECTED AMOUNTS DUE BAD DEBT CHARITY CARE UNCOMPENSATED CARE CHARGES UNCOMPENSATED CARE COSTS UNCOMPENSATED CARE % OF TOTAL COSTS 2017 $20,249,177,829 $469,305,416 $339,342,080 $808,647,496 $199,431,095.82 2.71% 2018 $21,507,898,507 $502,016,281 $358,871,422 $860,887,703 $212,015,528.38 2.72% 2019 $23,653,997,200 $509,174,368 $442,315,671 $951,490,039 $222,318,771.23 2.76% 2020 $23,710,238,082 $503,958,456 $499,580,152 $1,003,538,608 $238,120,014.50 2.90% 2021 $26,825,529,916 $512,576,407 $574,072,837 $1,086,649,244 $256,264,830.53 2.80% CHANGE 32.48% 9.22% 69.17% 34.38% 28.50% Source: American Hospital Association, HospitalStatistics
DIAGNOSIS-RELATED GROUP # DISCHARGES TOTAL CHARGES MEAN CHARGES PER DISCHARGE MEAN STAY PER DISCHARGE MEAN DAILY CHARGE 885 - PSYCHOSES 32,647 $645,239,562 $19,764 9.9 $1,998 795 - NORMAL NEWBORN 18,124 $107,001,168 $5,904 1.5 $3,859 807 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W/O CC/MCC 16,512 $259,829,657 $15,736 1.7 $9,096 177 - RESPIRATORY INFECTIONS & INFLAMMATIONS W MCC 15,521 $712,890,130 $45,931 6.3 $7,256 871 - SEPTICEMIA W/O MV 96+ HOURS W MCC 14,731 $775,058,072 $52,614 6.5 $8,119 794 - NEONATE W OTHER SIGNIFICANT PROBLEMS 9,948 $79,678,555 $8,010 2.0 $4,005 291 - HEART FAILURE & SHOCK W MCC 8,037 $274,478,781 $34,152 7.8 $4,395 788 - CESAREAN SECTION W/O STERILIZATION W/O CC/ MCC 6,171 $142,305,138 $23,060 2.6 $8,973 189 - PULMONARY EDEMA & RESPIRATORY FAILURE 5,282 $175,214,022 $33,172 5.1 $6,569 897 - ALCOHOL/DRUG ABUSE/DEPENDENCE W/O REHABILITATION THERAPY W/O MCC 5,045 $77,717,456 $15,405 5.4 $2,879 392 - ESOPHAGITIS, GASTROENT & MISC DIGEST DISORDERS W/O MCC 4,276 $87,994,537 $20,579 3.1 $6,575 470 - MAJ JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W/O MCC 4,144 $189,271,096 $45,674 2.0 $22,723 057 - DEGENERATIVE NERVOUS SYSTEM DISORDERS W/O MCC 3,850 $146,074,940 $37,942 13.0 $2,921 193 - SIMPLE PNEUMONIA & PLEURISY W MCC 3,820 $143,722,951 $37,624 5.0 $7,585 872 - SEPTICEMIA W/O MV 96+ HOURS W/O MCC 3,651 $92,975,105 $25,466 4.2 $6,122 806 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W CC 3,226 $50,272,932 $15,584 2.0 $7,677 690 - KIDNEY & URINARY TRACT INFECTIONS W/O MCC 3,179 $62,692,248 $19,721 3.6 $5,433 682 - RENAL FAILURE W MCC 2,971 $116,265,016 $39,133 5.6 $6,939 881 - DEPRESSIVE NEUROSES 2,922 $44,791,618 $15,329 6.8 $2,258 683 - RENAL FAILURE W CC 2,921 $67,435,032 $23,086 3.7 $6,240 Top 20 DRGs 166,978 $4,250,908,017 $26,694 4.9 $5,462 Source: Arkansas Department of Health, Hospital Discharge Program
What does it mean to be taken care of?
At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 70 years, providing affordable, reliable health insurance … to keep Arkansans healthy and to help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.

PARTNERS WITH AHA SERVICES, Brings Value-Based Care to More Arkansans
From the moment ChartSpan’s leaders began researching AHA Services, Inc. (AHASI), they knew they wanted to partner with the organization.
“After spending time with the AHASI team and a select few of [AHA’s] members, it was abundantly clear that our organizations are aligned,” says Shane Grivich, Chief Strategy Officer for ChartSpan.
A value-based care organization, ChartSpan is committed to creating positive health outcomes for Medicare patients and increased revenue for health care practices, systems, and hospitals. The company’s leaders say they are impressed with AHASI’s commit-

ment to experimenting with new, cost-effective health care strategies that can benefit member hospitals and their patients.
Through the partnership, ChartSpan will offer its services – Chronic Care Management (CCM), Annual Wellness Visits (AWV), Remote Physiological Monitoring (RPM) Enrollment, and Quality Improvement – to the Arkansas Hospital Association's member hospitals across the state.
Here’s a brief overview of ChartSpan solutions from which AHA’s member hospitals can choose to improve outcomes for their Medicare patients.
CHRONIC CARE MANAGEMENT
More than two-thirds – 68% – of Medicare patients have two or more chronic conditions. The Centers for Medicare and Medicaid Services (CMS) created Chronic Care Management to improve care for these patients while reducing their health care costs.
ChartSpan offers full-service Chronic Care Management (CCM), with trained clinical staff who provide CCM services every month. These services include:
Care Coordination: ChartSpan’s clinical staff works closely with patients to create treatment plans, refill medications, schedule appointments, locate community resources, and identify gaps in care.
24/7 Nurse Line: Nurses are available around the clock to answer patient questions and triage patients to urgent care or emergency services, if needed.
Comprehensive Documentation and Compliance: The ChartSpan team documents all patient interactions to ensure each person receives 20 minutes of care a month. All interactions and updates are shared back with the provider.
On average, CCM patients save $240 a year in health care costs and experience 20% fewer hospitalizations. Providers also benefit, with every 300 patients enrolled in CCM generating more than $100,000 in practice revenue.

50 SUMMER 2023 | ARKANSAS HOSPITALS
M
*Based on average Arkansas reimbursement rate
AHA SERVICES PRESENTS
QUALITY IMPROVEMENT
Continuous Quality Improvement helps health care organizations deliver optimal, cost-effective care to patients. Quality Improvement is especially important for health care systems that embrace value-based care, that are members of ACOs, or that participate in the Merit-based Incentive Payment System (MIPS).
ChartSpan offers complimentary Quality Improvement services for Chronic Care Management clients. Quality Improvement often means lowering the cost of care per patient while ensuring each
patient has positive health outcomes – the exact challenge CCM addresses.
The ChartSpan clinical team identifies patient gaps in care based on monthly CCM interactions and the data contained in the EMR. The staff can then talk to patients about vaccinations, cancer screenings, and other preventive care measures to improve their health and reduce their health care costs. Providers and health care practices can report these improved outcomes to their ACO or to Medicare.
ANNUAL WELLNESS VISITS
Preventive care plays a pivotal role in maintaining patients’ overall health, which is why CMS values Annual Wellness Visits . But patients often skip preventive care.
• Only 24% of Medicare patients receive AWVs.
• Preventive care visits have close to 50% no-show rates
ChartSpan’s AWV software, RapidAWV™, empowers providers to conduct AWVs during alreadyscheduled appointments. This strategy prevents patients from missing their AWVs and gives providers the chance to create preventive care plans, close gaps in care, and increase their revenue.
RapidAWV™ helps with three critical components of Annual Wellness Visits:
Determining Eligibility: RapidAWV™ checks the HIPAA Eligibility Transaction System (HETS) to see which Medicare patients are eligible for an AWV on the day of their visit. Eligible patients are clearly marked
so the clinical staff can hand the patient a Health Risk Assessment (HRA).
Performing the Health Risk Assessment: Patients complete their Health Risk Assessment on a tablet that utilizes a simple, accessible interface. The interface is designed to have one question per page, written in an easily readable font.
Analyzing the HRA Report: ChartSpan’s AWV software automatically generates a report for each patient based on the HRA. The report indicates the areas of greatest concern, from fall prevention to smoking cessation, cognitive impairment, and management of chronic conditions. The provider can then address those concerns and help the patient create a personalized health care plan.
AWVs increase the frequency of vaccinations and preventive screenings and can reduce health care costs by an average of 5.7%, making them a valuable tool in any practice’s preventive care arsenal.
REMOTE PHYSIOLOGICAL MONITORING ENROLLMENT
Remote Physiological Monitoring (RPM), sometimes called Remote Patient Monitoring, allows providers to monitor patients’ vital signs and health data between in-person visits. But many health practices don’t implement RPM because the enrollment process can be complex and time-consuming.
ChartSpan’s RPM Enrollment Service can help. The
ChartSpan team starts by examining patient data to determine which patients are eligible for RPM. They reach out to those patients through voicemail, email, and direct mail to talk about RPM and its benefits.
If the patient chooses to enroll, the ChartSpan team records their consent and archives it so the provider can access it throughout the RPM program.
VALUE-BASED CARE FOR AHASI MEMBERS
ChartSpan’s services, including Chronic Care Management (CCM), Annual Wellness Visits (AWV), Remote Physiological Monitoring (RPM) Enrollment, and Quality Improvement, strive to create positive health outcomes for Medicare patients and increase revenue for health care practices, systems, and hospitals.
If you’re an AHA member and would like to learn about how ChartSpan can help you navigate health care’s evolving landscape, please visit chartspan.com.
51 ARKANSAS HOSPITALS | SUMMER 2023
THE IMPACT OF THE RURAL SETTING
On Social Determinants of Health
The last time I wrote about the social determinants of health for ArkansasHospitals was in the spring of 2021. Re-reading my column, I realize that though the COVID pandemic vividly illuminated the health inequities and social disparities existing in America, very little has improved along this front in the last two years.
IMPACT ON COMMUNITY HEALTH
Definitions of “social determinants of health” vary by source, but there is general agreement on its components and their impact on community health:
• Health Services Factors include access to physical and mental health care, quality of care, and reliably safe care.
• Social and Economic Factors include nutrition and food access, housing adequacy and
homelessness, access to employment, economic mobility, access to education, transportation access, and availability of community and social services.
• And finally, Environmental Factors, which include water and air quality, noise pollution, proximity to hazardous waste sites, weather, and the effects of climate change on a person’s environment.
SOCIAL DETERMINANTS OF HEALTH IN THE RURAL HEALTH ARENA
Many of the social contributors to health are exacerbated in the rural setting, and with 13.9% of the U.S. population (and approximately 41% of Arkansans) living in rural areas, I’d like to address these from a rural perspective.

52 SUMMER 2023 | ARKANSAS HOSPITALS
COACH'S PLAYBOOK
Health Services Factors: The Federal Office of Rural Health Policy says that, ideally, rural residents should be able to conveniently and confidently access services such as primary care, dental care, behavioral health, emergency care, and public health services. But we know that access to care, especially in medical specialties, is often limited in rural communities. This requires patients to travel varying distances, perhaps without adequate means of transportation or the ability to take time off from work, for medical services beyond routine health care.
While telehealth – which allows patients and physicians to connect over the internet, sometimes reducing the need for travel – grew exponentially during the COVID crisis, patients living in rural areas may not have access to reliable, affordable high speed internet, thus reducing their ability to connect with remote mental health and medical providers. (Arkansas ranks 49th out of 50 states for availability of high speed internet.)
In addition, the overwhelming shortage of health care workers persists as a challenge in every Arkansas community, particularly the rural areas of the state where hospitals are also at risk of closing. Rural hospitals cannot compete for physicians and clinical staff at wage scales equal to those available in cities. Becker’s Hospital CFO Report (November 2022) reports that, nationally, more than 630 rural hospitals are at risk of closure, including their assessment that 22 rural Arkansas hospitals are among these. What isn’t represented by these already stark numbers is the relative scarcity of rural hospitals already in existence in rural America.
Social and Economic Factors: Again, the Federal Office of Rural Health Policy reports that “Rural residents are more likely [than their urban counterparts] to experience some of the contributing social factors that impact health, such as poverty. The impact of these challenges can be compounded by the barriers already present in rural areas, such as limited public transportation options and fewer choices to acquire healthy food.”
Food insecurity can be a real challenge in rural areas, and the realities of unemployment and low-wage jobs can cause a reliance on safety-net programs. Rural residents are often more limited in individual resources and may have less access to reliable transportation than those in other parts of the country; these factors all correlate with poorer health.
Eighteen counties in Arkansas are ranked as areas of persistent poverty in a report released May 9 of this year by the U.S. Treasury Department. And Arkansas, along with the rest of the country, is facing declining populations in rural counties, which exacerbates many of the other contributing factors to poor community health.
Environmental Factors: Physical environment is one of the most recognized social determinants of health. Environmental basics such as air and water quality, noise pollution, and absence of chemical pollution are often taken for granted, but they affect the health of every person, whether living in rural or urban areas.
The U.S. Environmental Protection Agency in March 2023 announced that nearly $19 million from the new federal infrastructure law is being
53 ARKANSAS HOSPITALS | SUMMER 2023
With limited available resources, rural hospitals must prioritize their efforts.
made available to Arkansas to address emerging contaminants such as per- and polyfluoroalkyl substances (PFAs) in drinking water – a problem in rural as well as urban areas of the state.
Some of the issues particular to rural Arkansas environmental quality include well water contamination, chemical pollution from farming operations, herbicide usage and its impact on water quality, and the effects of drought and flooding in rural counties.
HOPE FOR RURAL HOSPITALS
The Baldrige Excellence Framework has long placed a focus on societal contributions, but about a decade ago it expanded the health care version of the Criteria to include a responsibility for improving community health. As shown in the sidebar, it is now reflected as one of the Baldrige Core Values and Concepts, meaning that it is a
theme that cuts across various categories and serves as a foundation for the Framework.
This Core Value emphasizes the need for leadership in these efforts: Without your leadership, it will be nearly impossible to have a positive impact on your community’s health. What must you do?
The first step is to publicly commit yourself and your organization to addressing those social determinants of health that are most prevalent/ require the most attention in your community. While rural counties share many common characteristics, they often have unique needs that require leaders’ focused attention.
With limited available resources, rural hospitals must prioritize their efforts. What are the primary causes of a decline in life expectancy and increase in infant mortality in your county? The data sources, while often lagging by a year or two, are
BALDRIGE CORE VALUE AND CONCEPTS: SOCIETAL CONTRIBUTIONS AND COMMUNITY HEALTH
Considering societal well-being and benefit means leading and supporting –within the limits of your resources – the environmental, social, and economic systems in your organization’s sphere of influence. Public health services and the support of the general health of the community are important societal responsibilities of health care organizations. Such leadership and support might include efforts to determine and address social determinants for health and to provide both charity care and investment in your local community and/or beyond, such as by establishing free clinics or affordable health care programs, increasing public health awareness programs, contributing to community organizations, or fostering neighborhood services for the elderly.
It also might involve being a role model for addressing socially important issues, such as diversity, equity, and inclusion; practicing resource conservation; reducing your carbon footprint; performing community service and charity; improving health care industry practices; and sharing non-proprietary information. Increasingly, such societal contributions are a customer or stakeholder requirement.
Leadership in this area may entail influencing other organizations, private and public, to partner for these purposes. Managing societal contributions requires your organization to use appropriate measures and your leaders to assume responsibility for those measures.
54 SUMMER 2023 | ARKANSAS HOSPITALS
Baldrige Performance Excellence Program. 2023. 2023-2024 Baldrige Excellence Framework® (Health Care): Proven Leadership and Management Practices for High Performance. Gaithersburg, MD: U.S. Department of Commerce, National Institute of Standards and Technology. https://www.nist.gov/baldrige.
plentiful. What other local organizations should you recruit as collaborators in your effort? Is there an already established model for forming such a collaboration?
The “Communities of Excellence 2026” program is a Baldrige-based program that applies Baldrige principles not just to a single organization but to a collaborative of community-based organizations striving to elevate the performance of the community, as a whole.
“Communities of Excellence 2026” (COE 2026) is a 501(c)(3) nonprofit organization that hosts a national learning collaborative of communities across the country, trains communities in the Baldrigebased CommunitiesofExcellenceFrameworkand provides opportunities for communities to work together; to share successes, challenges, ideas, and best practices; and to learn from each other throughout their performance excellence journey.
READER RESOURCES
By definition, the program’s efforts include addressing social determinants of health.
The mission of COE 2026 is to ensure that every person living in America has the opportunity to live their best life in communities that are thriving. In many of these communities, a health care organization serves as a “backbone” organization, recruiting partners, convening meetings, and sharing best practices from other communities of excellence.
To learn more about “Communities of Excellence 2026,” you may contact me or visit the COE 2026 website ( www.coe2026.org ). Specific questions may be addressed to Stephanie Norling, Executive Director, at snorling@ communitiesofexcellence2026.org

These three resources may be particularly useful as you work on social determinants of health in your own organizations.
The Arkansas Department of Health’s Office of Health Equity, Arkansas Minority Health Commission’s Red County Life Expectancy Profile, 2018 (published May, 2020)
The Arkansas Department of Health’s Primary Care Needs Assessment of Arkansas, 2020

Rural Profile of Arkansas, University of Arkansas Division of Agriculture, 2021
The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 24 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.
55 ARKANSAS HOSPITALS | SUMMER 2023
COMMON CAUSE: Adverse Childhood Experiences and Social Determinants of Health
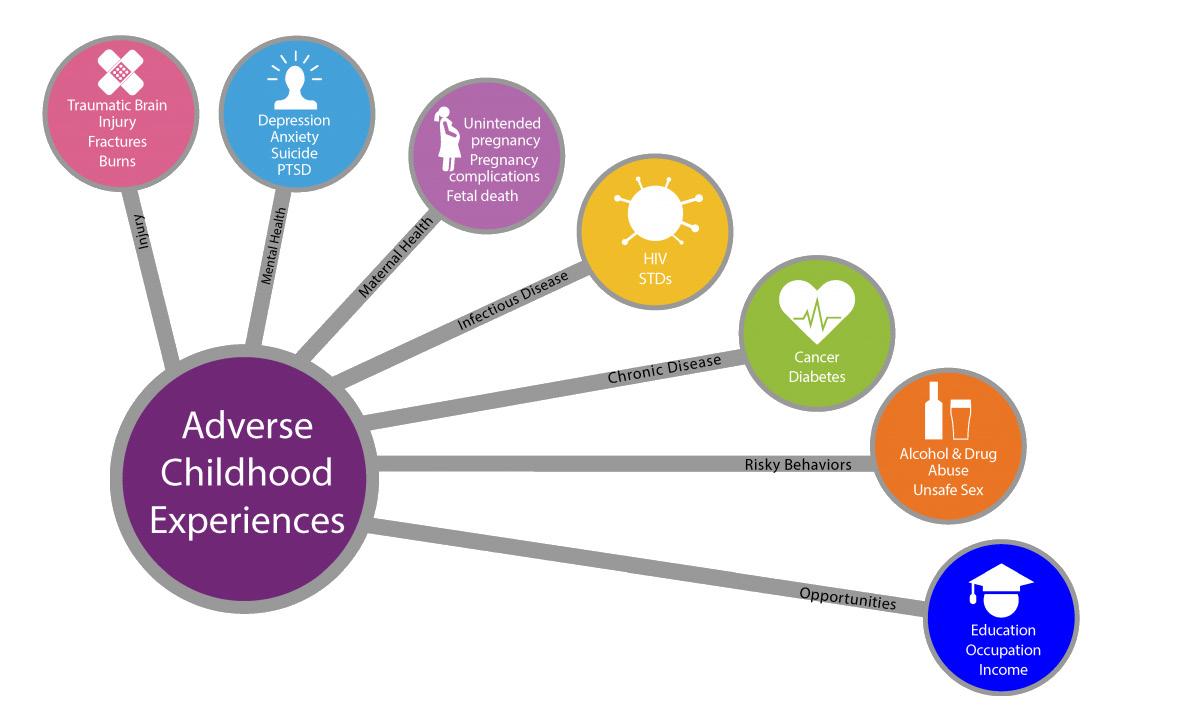 By Chad T. Rodgers, MD
By Chad T. Rodgers, MD
Screening for Social Determinants of Health (SDoH) in medical practices and hospitals has become increasingly common. We use well-established tools to identify our patients’ needs; this helps us begin to address underlying basic needs with the goal of moving toward improved health.
We commonly screen for anxiety and depression, food insecurity and housing issues, substance abuse, family and community support, and connection.
Too often, we don’t realize that we are also screening for the causes and
results of what is commonly known as Adverse Childhood Experiences (ACEs). And while providers are asking the right questions, do we know what to do with all the answers?
ACE s , DEFINED
Adverse Childhood Experiences (ACEs) are a collection of, sadly, common experiences that occur early in infancy and in early childhood – both of which are crucial developmental periods of the brain and the body. Undergoing these experiences without the safety net of protection from a nurturing
caregiver can cause toxic stress. This type of stress results in a survival response triggering the release of stress hormones that prepare the body and mind to fight or flee from real or perceived danger.
A child’s not being able to remove themselves from this stress results, often repeatedly, in a prolonged and detrimental response.
The original ACEs study, screening tools, and related information can be
EARLY ADVERSITY HAS LASTING IMPACTS
56 SUMMER 2023 | ARKANSAS HOSPITALS
found on the CDC website (https:// www.cdc.gov/violenceprevention/ aces).
Using the ACEs screening, providers can elicit 10 possible experiences that have been identified and studied and are now well known to have detrimental effects on long-term health. They include physical, emotional, and sexual abuse, emotional and physical neglect, and household dysfunction, including a caregiver with a mental illness or substance abuse problem, seeing a caregiver treated violently, and parental separation from divorce or incarceration.



These 10 are not inclusive of all traumas. But we know that the more ACEs you experience, the poorer your mental and physical health, with an overall reduction in quality of life and early death.
An individual with an ACEs score of seven or more is more likely to have a mental illness, use illicit substances and abuse alcohol, have chronic health conditions such as asthma, diabetes, or cancer, and have a significant risk for suicide.


POSITIVES CAN OFFSET NEGATIVES
These traumas are, unfortunately, common. And if you have experienced one, you are more likely to have experienced others. But the important thing to know is that all hope is not lost. Your ACEs score does not commit you to a life of suffering.
Trauma and stress are part of the human experience. However, protective factors such as having consistent and nurturing caregivers who provide support and who both model and help build resilience can

57 ARKANSAS HOSPITALS | SUMMER 2023
Mitchell, Williams, Selig, Gates & Woodyard, P.L.L.C
THE
OF
Jeffrey H. Thomas, Managing Director
POWER
EXPERIENCE IN EMPLOYMENT LAW
WORKPLACE RESOLUTION
LITTLE ROCK | ROGERS | JONESBORO | AUSTIN
(501) 688 - 8800 | MitchellWilliamsLaw.com 425 West Capitol Avenue, Suite 1800 Little Rock, Arkansas 72201
AUDRA HAMILTON
offset these traumatic experiences. The more positive experiences you have, the better chance they have of outweighing the bad.
And, as a medical professional, simply knowing and acknowledging that your patient has experienced trauma enhances and improves the patient’s experience and outcomes, as well.
E.J.’S STORY
When we screen for SDoH, we can also assess for ACEs. Take E.J., a 45-year-old accountant treated for high blood pressure, high cholesterol, and depression/anxiety. He lives alone after a divorce and admits to drinking heavily. You know from his social and family history and the screening that his uncle adopted him after his father was incarcerated for involvement with
drugs (parental separation due to incarceration). His mother completed suicide after a long struggle with depression (mother with mental illness). Growing up in poverty, he moved from house to house and sometimes wasn’t sure where and when he would have his next meal (physical neglect). He wore tattered clothes to school, where he was made fun of by others and never felt like he belonged.
His uncle tried to do his best, but he often called him “stupid,” and E.J. always felt like he was a burden to his uncle (emotional neglect and abuse). E.J., fortunately, had a grandmother, who, despite poor health, often picked him up from school and kept him on the weekends. She provided a safe and loving environment and reminded him of his mother. A schoolteacher observed that E.J. was very smart and encouraged

him to attend college (positive experiences build resilience factors). He was awarded scholarships and found work during college to complete his degree. E.J. has an ACEs score of five or more. But he had two positive factors in his life – his grandmother and an encouraging teacher.
Simply knowing that E.J. has a high ACEs score, we can identify factors contributing to his mental and physical health. Instead of wondering, “What is wrong with E.J.?” we can ask ourselves, “What happened to E.J.?” in order to build a therapeutic and empathetic relationship with him.
IDENTIFYING ACEs: THE IMPACTS
Research tells us that knowing and acknowledging his trauma can improve E.J.’s health outcomes. Looking at
58 SUMMER 2023 | ARKANSAS HOSPITALS
While providers are asking the right questions, do we know what to do with all the answers?
underlying causes, we can address their impact on his social issues. We can address his substance abuse while also addressing his anxiety and depression. Increasing social support for him with his family and community through appropriate referrals will improve his ability to make decisions and make changes that will improve his blood pressure, control his cholesterol, and improve his quality of life.
Improving our own and our staff members’ knowledge of ACEs improves health care. AFMC provides training on ACEs awareness and strategies to better care for our patients and will host the ACEs and Resilience Summit – “The Power of Belonging” – on Thursday, August 3, 2023, at Pulaski Technical College in North Little Rock. We hope you can join us!
ACEs AND RESILIENCE SUMMIT: THE POWER OF BELONGING

Thursday, August 3, 2023 Pulaski Technical College, North Little Rock Cost: $50
for more information
Arkansas Senior Health Insurance Information Program

SHIIP supports Arkansans turning 65, and those already on Medicare and questions about their Medicare options. Our local area certified Medicare counselors are available to offer them the information they will need to make best choices for their healthcare coverage. Topics cover from Part B Deductible, Medicare Supplements (Medigap), Medicare Advantage Plans, and Part D Drug Plans.
AR SHIIP supports Arkansans turning 65, and those already on Medicare and have questions about their Medicare options. Our local area certified Medicare counselors are available to offer them the information they will need to make the best choices for their healthcare coverage. Topics cover from Part B Deductible, Medicare Supplements (Medigap), Medicare Advantage Plans, and Part D Drug Plans.
Call AR SHIIP toll free 1-800-224-6330
AR SHIIP supports Arkansans turning 65, and those already on Medicare and have questions about their Medicare options. Our local area certified Medicare counselors are available to offer them the information they will need to make the best choices for their healthcare coverage. Topics cover from Part B Deductible, Medicare Supplements (Medigap), Medicare Advantage Plans, and Part D Drug Plans.
Call AR SHIIP toll free 1-800-224-6330 let us find a partner in your area today.




let us find a partner in your area today.
publication is supported by the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS) as part of a financial assistance award SAPG0077 with 100 percent funding by ACL/HHS. The contents are those of the author and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.
publication is supported by the Administration for Community Living (ACL), U.S. Department of Health and Services (HHS) as part of a financial assistance award SAPG0077 with 100 percent funding by ACL/HHS. The are those of the author and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.
This publication is supported by the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS) as part of a financial assistance award 90SAPG0077 with 100 percent funding by ACL/ HHS. The contents are those of the author and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.
59 ARKANSAS HOSPITALS | SUMMER 2023
scan
QR code
Please
the
For more information on the
and Resilience
please visit https://www.afmc.org/acesummit
Chad T. Rodgers, MD, FAAP, serves as Chief Medical Officer at AFMC.
ACEs
Summit,
AR SHIIP
free
us find a partner in your area today. ARKANSANS SENIOR HEALTH INSURANCE INFORMATION PROGRAM
Call
toll
1-800-224-6330 Let
Information
Arkansas Senior Health Insurance
Program
MEDICAID UNWINDING:
The May 11 end of the COVID-19 Public Health Emergency (PHE) brings with it a redetermination of Medicaid beneficiary eligibility. This redetermination is also known as the “unwinding” of PHE extensions, and it creates new obstacles for not only beneficiaries but also for state officials.


During the PHE, Congress enacted the Families First Coronavirus Response Act, which effectively gave special funding to states that agreed to keep Medicaid beneficiaries enrolled continuously through the end of the PHE – meaning that no enrollees would be removed from Medicaid rolls due to income or eligibility while COVID created its many health- and economic-related complications. Beneficiaries could be disenrolled if they moved out of state, died, became incarcerated, or requested their coverage to end; otherwise, their coverage remained intact.
In 2021, the General Assembly enacted legislation that requires the Department of Health and Human Services to conduct and complete the redetermination of eligibility in a short, six-month time frame. This requirement

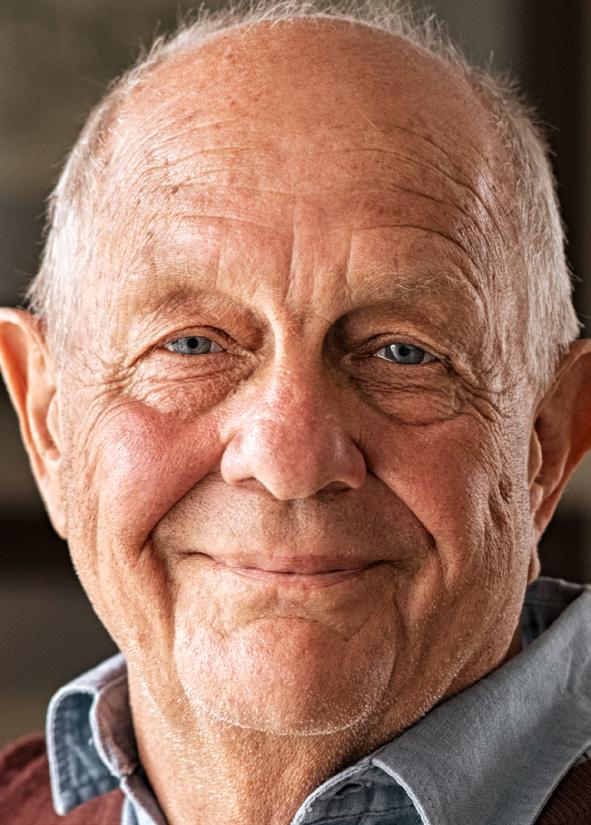
applies exclusively to “extended” cases that have not been re-evaluated within the past 12 months. Arkansas is the only state in the Union that requires this short time frame. A few other states have 9–12-month requirements, and most states adopted a 12-24-month grace period for the redetermination to be completed.
States that have allowed more time for determinations of eligibility
have the freedom to be more discerning, and they have time to attempt to locate and directly contact beneficiaries for dialogue re: eligibility, rather than relying on what is called “procedural termination” –where beneficiaries are dropped from the Medicaid rolls simply because they did not respond to mailed or emailed eligibility inquiries from state offices.
60 SUMMER 2023 | ARKANSAS HOSPITALS
The Arkansas Department of Health and Human Services has only six months to complete the unwinding process.
Patients, Including Kids, Losing Coverage

ARKANSAS’S RAPID UNWIND
Arkansas began the unwinding process in the earliest month designated by the federal government as possible to do so: February of 2023. Notices that people receiving “extended Medicaid” needed to renew their enrollment in Arkansas Medicaid were mailed immediately, starting that same month.
As of April 1, 2023, the Department of Human Services (which oversees Arkansas Medicaid) could and did begin terminating coverage for those no longer eligible or who did not verify eligibility with the department.
In its February 1, 2023, Arkansas Comprehensive Unwinding Plan, DHS reports that it is unwinding the cases of 422,112 individuals with “extended” coverage, seeking information from these beneficiaries so that their eligibility for Arkansas Medicaid benefits can be redetermined.
These Arkansans may no longer be eligible to receive Medicaid benefits for several reasons:

• They have an income that now exceeds eligibility levels.

• They have not responded to a request for information as part of the renewal process.
• They had a level-of-care or medical change that made them no longer eligible.
• They have aged out of eligibility.

DHS CONCERN: TRYING TO CONTACT BENEFICIARIES
The DHS plan indicates that outdated contact information for beneficiaries is likely to be a problem. “One concern nationwide is that eligible beneficiaries – especially more vulnerable populations like those who are aged, disabled, or who have developmental/intellectual disabilities – will lose coverage during the unwinding because states were not given updated contact information and cannot reach them,” the report says. That is a real concern for Arkansas, and the state is taking steps to mitigate this, including:
• Calling all beneficiaries who have had their coverage extended to verify their contact
information. At least three, and often more, attempts have been or will be made to reach each of these beneficiaries.
• Opening an Address Update Hotline that beneficiaries can easily call to verify and update their contact information. DHS is promoting this through earned, organic, and paid media and social media.
• Requesting that partners across the state share messaging about the importance of updating their addresses and contact information with DHS.
• Receiving approval for an (e)14 waiver from the federal government to allow the State to accept verified beneficiary addresses from managed care organizations, including the Provider-led Arkansas Shared Savings Entities (PASSE), without the need to do additional verification.
The plan indicates that the State also requested approval to accept United States Postal Service/National Change of Address data and verified
61 ARKANSAS HOSPITALS | SUMMER 2023


62 SUMMER 2023 | ARKANSAS HOSPITALS
Our hospitals have always worked for the ability of every Arkansan to be able to attain health care coverage.
addresses from Qualified Health Plans (QHPs) that provide coverage for Arkansas Health and Opportunity for Me (ARHOME) beneficiaries without the need for additional verification.


PATIENTS’ AND PROVIDERS’ CONCERN: PROCEDURAL TERMINATIONS
Coupling the dilemma of retrieving updated contact information with the legislature’s requirement that “extended” coverage recipient cases be unwound within six months is creating chaos for patients and providers of care. In April, the first month of Medicaid unwinding in Arkansas, 72,802 Medicaid beneficiaries were dropped from the Arkansas Medicaid rolls, including 29,067 children. Income ineligibility caused 5,414 of these terminations. Requests by beneficiaries to discontinue their enrollment numbered 5,791.
Most of the terminations reported from April data – 82% – are due to procedural issues such as failure to return renewal forms, failure to supply other enrollment information, or inability to locate the beneficiary at last known address or contact number. These terminations are called “procedural terminations.”



Procedural terminations of Medicaid coverage – terminations of Medicaid coverage without interaction-based determination of the beneficiary’s income eligibility –cause “churn.” Churn is the process where Medicaid beneficiaries are dropped from the rolls, entering a period of non-coverage while they learn they are no longer covered and seek coverage once again, only to be subsequently re-enrolled.
When individuals who remain income-eligible for Medicaid are dropped from the rolls for procedural reasons, they find themselves without medical coverage and become vulnerable to unnecessarily poor health outcomes. In many cases, these beneficiaries are blindsided as to their status and find out when they go to
63 ARKANSAS HOSPITALS | SUMMER 2023
Your organizational wellbeing is our priority. There’s nothing more important to the wellbeing of your business than the wellbeing of your people. That’s why for more than 90 years we’ve been here for businesses, communities and people around the globe. Customizing insurance programs and benefits, and HR solutions tailored to their needs. Consulting with companies through every challenge to drive better outcomes. Helping you build the confidence to handle whatever comes next. AJG.com
© 2023
CONNECT WITH US Gallagher 6325 Ranch Drive Little Rock, AR 72223 501.485.3075 43936 GBS 2023 MWR AHA_AD_FINAL.indd 1 1/31/2023 1:33:50 AM
| The Gallagher Way. Since 1927.
Arthur J. Gallagher & Co. | GBS43936
pick up medications at the pharmacy or access care from their provider.
The May Unwinding Report from Arkansas DHS, released just before this magazine’s press date, indicates that 68,838 people were dropped from the Medicaid rolls in the month of May 2023. Of these, 65% were procedural terminations, caused by beneficiaries failing to return renewal forms, failing
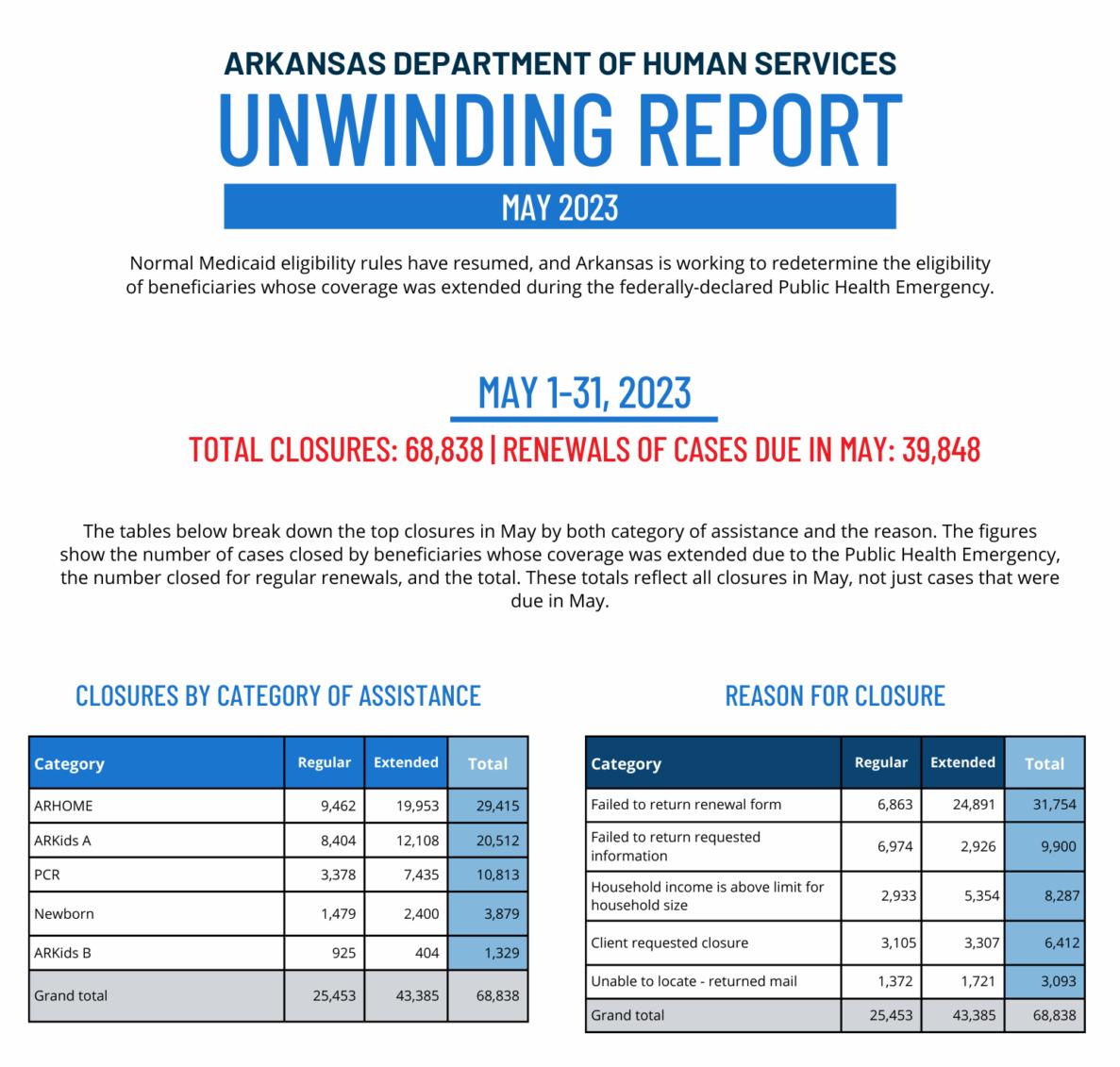
to return requested information, or DHS staff being unable to locate them (returned mail).
Once again, the number of children impacted is extremely worrisome. Added to the 29,607 children who lost their Medicaid coverage in April, an additional 25,720 Arkansas children lost coverage in May. That means more than 54,000 Arkansas kids have lost coverage.

“STAGGERING NUMBERS” NATIONWIDE
A June 1 article from Kaiser Health News says that more than 600,000 Americans lost Medicaid coverage in the first month of the unwinding process. The vast majority of these, says author Hannah Recht, “were removed from state rolls for not completing paperwork.”
64 SUMMER 2023 | ARKANSAS HOSPITALS
You are not the darkness you endured You are the light that refused to surrender John Mark Green
More than 54,000 Arkansas children have already lost their Medicaid coverage.
KFF is sounding the alarm that tens of thousands of children are losing coverage. As stated above, more than 54,000 Arkansas children lost coverage in just the first two months of unwinding.
WORKING TOGETHER
Patients (and their advocates), hospitals and care providers (and their advocates), marketplace insurers, and DHS are all working together in the unwinding process,


MethodistFamily.org 501-803-3388 Info@MethodistFamily.org
Improve quality, outcomes and financial performance

DataGen® offers analytical insights focusing on payment policy impacts, value-based programs, market dynamics and patient safety.
Our product portfolio includes:
• analytics to support Accountable Care Organizations and Alternative Payment Model programs;


• custom analytics to evaluate market dynamics and financial and quality outcomes; and
• applications to support culture of safety surveys and community health needs assessments.

65 ARKANSAS HOSPITALS | SUMMER 2023
1.844.DATAGEN Learn more at DATAGEN.INFO.
info@datagen.info |
seeking to keep all eligible Medicaid beneficiaries enrolled in the program and helping those no longer eligible to access coverage through the Arkansas Health Insurance Marketplace and other sources.




Arkansas Hospital Association Executive Vice President Jodiane Tritt says she is especially grateful

to Amy Webb and the DHS team for their transparency in this endeavor and their willingness to work with the AHA to keep all eligible beneficiaries enrolled without interruption.
“Our hospitals have always worked for the ability of every Arkansan to be able to attain health care coverage,” she says. “It is a given that with today’s
financial constraints, hospitals cannot absorb any additional uncompensated care. We applaud DHS for their efforts to keep all eligible Medicaid beneficiaries covered, and for steering them to the Arkansas Health Insurance Marketplace or employer-based plans if they need to find coverage elsewhere.”

66 SUMMER 2023 | ARKANSAS HOSPITALS
Pulaski Tech, NLR Campus Center Grand Hall A&B
The Power of Belonging Positive Childhood ACEs23
Thursday August 3rd, 2023
Thursday August 3rd, 2023
8 AM - 4 PM
8 AM - 4 PM
Pulaski Tech, NLR
Pulaski Tech, NLR Campus Center Grand Hall A&B
7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT
The Power of Belonging Positive Childhood ACEs23
7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT

67 ARKANSAS HOSPITALS | SUMMER 2023 The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging –Positive Childhood Experiences ACEs23 7TH ANNUAL ACES & RESILIENCE SUMMIT © 2023, AFMC, INC. ALL RIGHTS RESERVED. REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM
Campus Center Grand Hall A&B The Power of Belonging Positive Childhood ACEs23 7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging Positive Childhood ACEs23 7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging Positive Childhood ACEs23 7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging Positive Childhood ACEs23 7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B The Power of Belonging Positive Childhood ACEs23 7TH ANNUAL ACES & RESILIENCE REGISTER AT AFMC.ORG/ ACESUMMIT Thursday August 3rd, 2023 8 AM - 4 PM Pulaski Tech, NLR Campus Center Grand Hall A&B s

















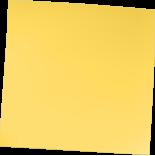








 Cliff Fullerton, MD, MS, serves as Senior Vice President for Baptist Health and as its Chief Value-Based Care Officer. Jasmin Sumrall, MPH, serves as Operations Manager for Baptist Health's Population H ealth Services Office.
Cliff Fullerton, MD, MS, serves as Senior Vice President for Baptist Health and as its Chief Value-Based Care Officer. Jasmin Sumrall, MPH, serves as Operations Manager for Baptist Health's Population H ealth Services Office.














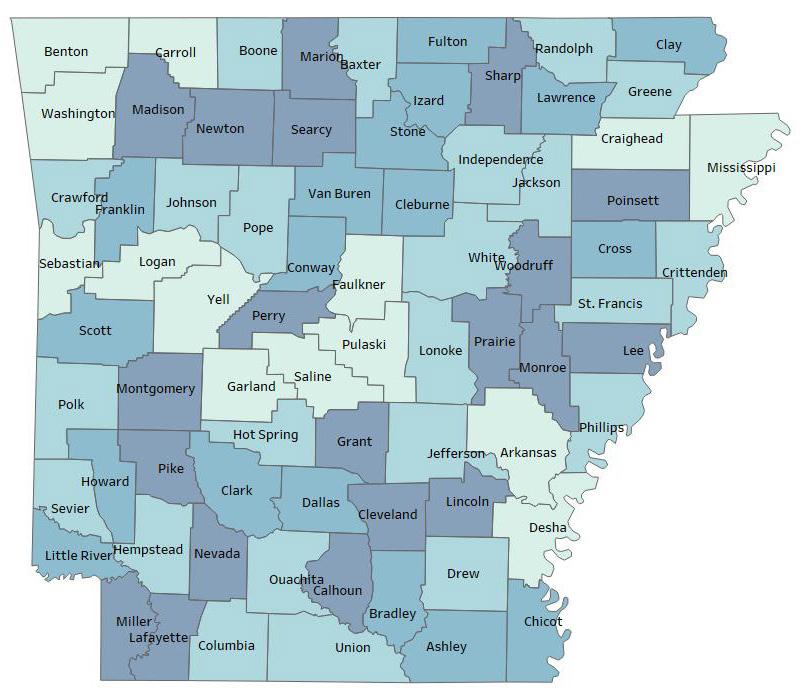

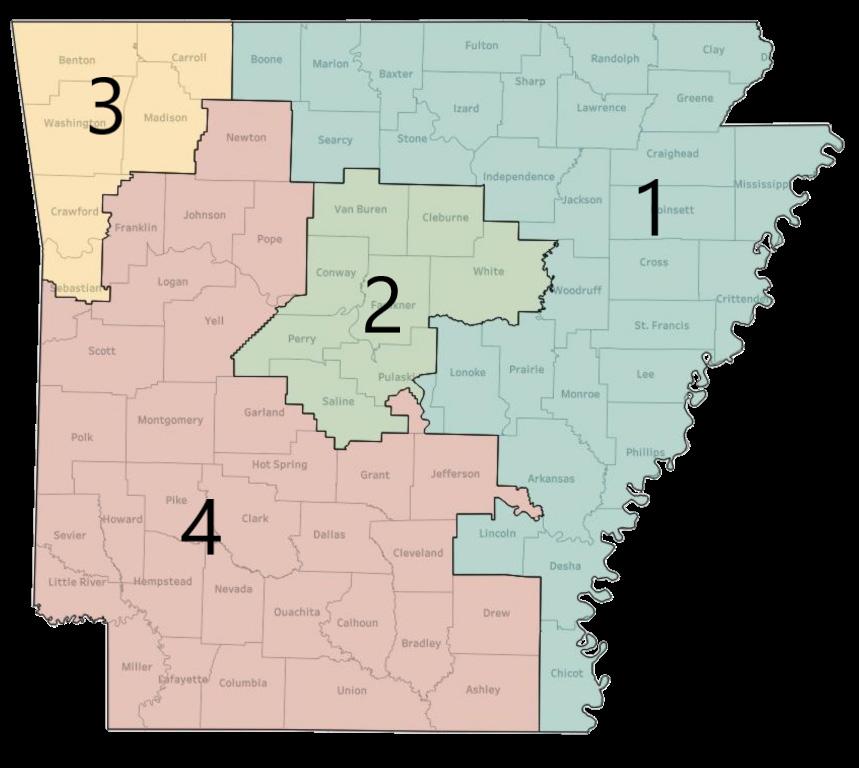





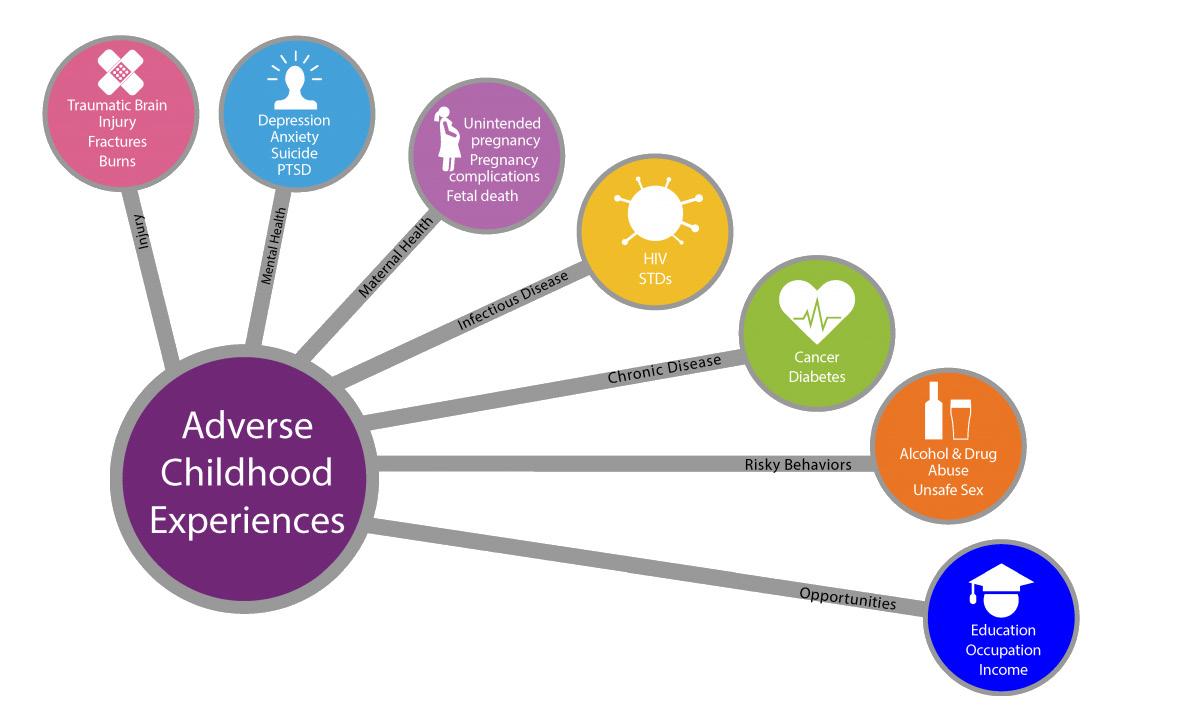 By Chad T. Rodgers, MD
By Chad T. Rodgers, MD