20 Years of the National Joint Registry: who benefits?
The development of new robotic MSK surgical services p28
The trainer’s toolkit: A guide to maximising training opportunities
Volume 12 | Issue 01 | March 2024 | The Journal of the British Orthopaedic Association | boa.ac.uk Journal of Trauma and Orthopaedics
p20
p46













Contact us at sales@ledaortho.com to arrange a consultation and open your personal portal to start planning cases.
your most complex cases with a UK-based, straightforward platform, underpinned by LEDA’s commitment to customer service.
UK-based operation Custom Guide Pre-Osteotomy Post-Osteotomy and Correction
point of contact with clear communication
turnaround of 3D printed guides for osteotomies of:
Limb
Limb
clinical applications available
radius
Clavicle HTO SMO ledaortho.com Powered by Insight Surgery Introducing L3D Osteotomy Planning and Custom Implants
Plan
Dedicated
One
Rapid
Upper
Lower
More
Distal
Elbow

3 From the Executive Editor
Deborah Eastwood
5 From the President
Simon Hodkinson
8-9 BOA Latest News
13 News: BOA Annual Congress 2024
14 News: Conference Listing 2024
16 Features:
What really matters?
Hiro Tanaka
20 Features:
20 Years of the National Joint
Registry: who benefits? Part three: Service commissioners, regulators and policy makers, and broader society
Michael Whitehouse, Ashley Blom, Deirdra Taylor and Mark Wilkinson on behalf of the NJR Team
24 Features:
SWLEOC and GIRFT Elective Hub Toolkit –A guide for setting up an efficient elective surgical hub
Richard E Field, Irrum Afzal, Boudine Pearce and Polly Hyde


28 Features:
The development of new robotic MSK surgical services within the NHS
Ricci Plastow, Andreas Fontalis, Nick Ohly and Fares S Haddad on behalf of the Robotic And Digital Assisted suRgery (RADAR) Advisory Group
32 Features:
Robotic surgery in orthopaedics: What does the future hold?
Edward T Davis and Fares S Haddad on behalf of the Robotic And Digital Assisted suRgery (RADAR) Advisory Group
36 Features:

46 Subspecialty:
The British Orthopaedic Association British Casting Certificate (BCC) Development Mark Rees
40 Features:
The National Consultant Information Programme (NCIP)
Sir Norman Williams and Deborah Higgs
44 Subspecialty:
Supporting surgical trainers Deepa Bose
44
The trainer’s toolkit: A practical guide to maximising training opportunities
Emily Baird
50 Subspecialty:
Supporting trainers: The future direction of travel
Pramod Achan
52 Subspecialty:
Training philosophy – the why Donald Campbell
54 In Memoriam:
Nicholas Barton












JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 01
Download the App The Journal of Trauma and Orthopaedics (JTO) is the official publication of the British Orthopaedic Association (BOA). It is the only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is also now available to everyone around the world via the JTO App. Read the latest issue and past issues on the go, with an advanced search function to enable easy access to all content. Available at the Apple App Store and GooglePlay – search for JTO @ BOA Did you know that as well as advertising in our Journal publication, we can offer footer banner advertising on the JTO App! For more information please contact Wendy Parker Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820 Contents Amputation the context T OrthopaedicsT Orthopaedics A Surgical Day Begins Volume 08 Issue 03Volume 08 Issue 02Volume 08 Issue 01 Volume 08 Issue 04 Journal of the British Orthopaedic Association The Journal of Trauma and Orthopaedics (JTO) has a dedicated news section, a features section containing interesting articles on various themes, a subspeciality section and a medico-legal section. Journal of Trauma and Orthopaedics We are committed to sustainable forest management and this publication is printed by Buxton Press who are certified to ISO14001:2015 Standards (Environmental Management System). Buxton prints only with 100% vegetable based inks and uses alcohol free printing solutions, eliminating volatile organic compounds as well as ozone damaging emissions. Open Box Media & Communications are proud to be corporate sponsors of Heart Research UK (Midlands) In this issue...


Medical 1. Berberich CE, Josse J, Laurent F, Ferry T. Dual antibiotic loaded bone cement in patients at high infection risks in arthroplasty: Rationale of use for prophylaxis and scientific evidence. World J Orthop. 2021;12(3):119-128. doi:10.5312/wjo.v12.i3.119 I 2. Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017;99-B(4 Supple B):3-10. doi:10.1302/0301-620X.99B4.BJJ-2016-1212.R1 I 3. Sanz-Ruiz P, Berberich C. Infection Risk-Adjusted Antibiotic Prophylaxis Strategies in Arthroplasty: Short Review of Evidence and Experiences of a Tertiary Center in Spain. Orthop Res Rev. 2020;12:89-96. doi:10.2147/ORR.S256211 I 4. Sprowson AP, Jensen C, Chambers S, et al. The use of high-dose dualimpregnated antibiotic-laden cement with hemiarthroplasty for the treatment of a fracture of the hip: The Fractured Hip Infection trial. Bone Joint J. 2016;98-B(11):1534-1541. doi:10.1302/0301-620X.98B11.34693 I 5. Sanz-Ruiz P, Matas-Diez JA, Villanueva-Martinez M, Santos-Vaquinha Blanco AD, Vaquero J. Is Dual Antibiotic-Loaded Bone Cement More Effective and Cost-Efficient Than a Single Antibiotic-Loaded Bone Cement to Reduce the Risk of Prosthetic Joint Infection in Aseptic Revision Knee Arthroplasty? J Arthroplasty. 2020;35(12):3724-3729. doi:10.1016/j.arth.2020.06.045 12139 EN www.heraeus-medical.com KNOW YOUR PATIENT –AND REDUCE PJI RISK IMPROVED OUTCOMES IN HIGH RISK PATIENTS1 Using dual antibiotic-loaded bone cement as part of set of measures2 in a risk adaptive approach Elective primary hip and knee arthroplasty3 Trauma (FNOF)4 Aseptic revision TKA5 See inside back cover for more information.
Credits
JTO Editorial Team
l Deborah Eastwood (Executive Editor)
l Paul Banaszkiewicz (Editor)
l Simon Britten (Medico-legal Editor)
l Karen Chui (Trainee Editor)
l Deepa Bose (Guest Editor)
BOA Executive
l Simon Hodkinson (President)
l Deborah Eastwood (Immediate Past President)
l Mark Bowditch (Vice President)
l Fergal Monsell (Vice President Elect)
l Hiro Tanaka (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l John Skinner (Appointed Trustee)
BOA Elected Trustees
l Simon Hodkinson (President)
l Deborah Eastwood (Immediate Past President)
l Mark Bowditch (Vice President)
l Fergal Monsell (Vice President Elect)
l Hiro Tanaka (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Cheryl Baldwick
l Deepa Bose
l Caroline Hing
l Andrew Price
l Andrew Manktelow
l Andrea Sott
l Paul Banaszkiewicz
l Stephen Eastaugh-Waring
l Vikas Khanduja
l Dominic Meek
l Benjamin Ollivere
l Amar Rangan
Copyright
BOA Staff
Executive Office
Chief Operating Officer - Justine Clarke
Personal Assistant to the Executive - Celia Jones
Policy and Programmes
Head of Policy and Public Affairs - Gary Robjent
Head of Education and Programmes - Alice Coburn
Programme and Committees Officer - Eliza Heng
Educational Programmes Assistant - Maimuna May
Communications and Operations
Director of Communications and Operations - Annette Heninger
Marketing and Communications Officer - Pujarini Nadaf
Membership and Governance Officer - Natasha Wainwright
Publications and Web Officer - Nick Dunwell
Finance
Director of Finance - Liz Fry
Finance Assistant - Hayley Ly
Events and Specialist Societies
Head of Events - Charlie Silva
Events Coordinator - Venease Morgan
UKSSB Executive Assistant - Henry Dodds

From the Executive Editor
Deborah Eastwood
Perhaps fittingly, as 2024 springs into life, this issue is all about the future and most specifically the art and science of training our younger colleagues in the fields of trauma and orthopaedic surgery. There are rough seas for our colleagues to traverse as they train and many obstacles to overcome as depicted on our front cover by ST6 trainee Rebecca Mazel: it is important that we help them to look forward to the shores of a safe harbour and not to let them concentrate on the difficulties they have faced. As highlighted by Deepa Bose, the SAC Chair for T&O, to support our trainees, we need to understand the needs of the trainers and ensure that they too are well supported and prepared for the delivery of training and the core competencies (p44). The trainers need a tool kit (p46), a philosophy (p52) and an understanding of their direction of travel (p50).
Copyright© 2024 by the BOA. Unless stated otherwise, copyright rests with the BOA. Published on behalf of the British Orthopaedic Association by: Open Box M&C
Advertising
All advertisements are subject to approval by the BOA Executive Board. If you’d like to advertise in future issues of the JTO, please contact the following for more information:
Wendy Parker - Media Manager
Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820
Open Box M&C, Premier House, 13 St Paul’s Square, Birmingham B3 1RB
Disclaimer
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and editor and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
BOA contact details
The British Orthopaedic Association, 38-43 Lincoln’s Inn Fields, London WC2A 3PE
Telephone: 020 7405 6507
How to contact JTO
Email: jto@boa.ac.uk
There is much to learn if the articles featuring robotic surgery on pages 28 and 32 are correct – and they are! Change is with us and we must adapt and make it work for us and our patients. We may need to work differently and the Elective Hub Toolkit outlined on page 24 will help us do this. Along with improving the way we work, the National Consultant Information Programme (NCIP) on page 40 will give us a better understanding of the work we do by perhaps giving more depth and detail regarding our patients, their procedures and their outcomes. The data from NCIP will supplement that available from the NJR helping us all to improve our services and identify areas for development. Unbelievably (to me at least!) the NJR is soon to be 21: the third in our series of articles to celebrate its 20-year milestone is on page 20 and asks the pertinent question of who benefits?
Despite all these advances, it is sometimes important to remind ourselves of our beginnings. It is over 40 years since the British Casting Certificate became a nationally recognised qualification and nine years since the launch of the revised casting standards. The programmes have diversified and grown over time (p36) with a rewarding and ongoing collaboration between Mark Rees, the BOA National Casting Training Advisor and the BOA Casting Committee.
As the world around us continues to be troubled, Hiro Tanaka’s piece on page 16 reminds us that the world can change in the blink of an eye and asks us to ask this question of ourselves: what really matters?
There is good news too – four colleagues of the broader orthopaedic community were recognised in the New Year Honours list, we welcome Dominic Meek as a Trustee and our recent committee appointments represent the diversity of our membership.
On a personal note, I am delighted that the UKHSA/BOA study looking at the radiation exposure that our members receive has started with the results expected in the summer. This will give us the data we need to drive forward appropriate PPE and educational changes. On behalf of the BOA, I would like to thank all the centres that are taking part and Lynn Hutchings and Charlotte Lewis for all their hard work n
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 03



One compact set featuring multiple tools needed to help remove damaged and broken screws:
Screw Removal Pliers
Sharp Hook
T-Handle with A0-End Mini Lexer Gouges
Extraction Screws
Extraction Bolts
Trephines

#4270
Romanelli Deep Gelpi Retractor
Designed by Ron Romanelli, MD
Offers wide, deep exposure in MIS spine approaches
Kolbel Soft Tissue Retractors
Helps in the early phase to retract soft tissue comprising of the gleno-humeral joint
Use facilitates the introduction of deeper retractors which are required for sufficient visibility of the glenoid, acromion and rotator cuff.



Spine/Trauma Deep Tissue Retractor
Designed to help maximize exposure with 90° arms and deep tissue blades

MADE
7

4 Teeth #1863
Hannum Tissue Grasper
Designed by Scott Hannum, MD
Teeth in jaw firmly holds bone and tissue Non-locking design can be easily gripped while allowing greater pressure to be applied. Available in three jaw sizes: short jaw for holding bone, medium jaw for smaller bones, and long jaw for tissue.
Jaw widths at actual size

Rogozinski Locking Needle Driver/Scissors
Designed by Chaim Rogozinski, MD
Scissors

Holding Tips
Designed with a quick lock & release handle, can drive a needle and cut a suture without changing instruments
Standard #3083
MADE

Large #3084
Ortho Self-Retaining Retractors

Calibrated ratchet is used to help accurately measure the size of an opening – useful in procedures to help assess bone graft needs
Features a no-teeth design, available with flat or serrated outside blades Also useful in knee replacement surgery to separate the femur and tibia, where the calibrated design can be used to help balance ligaments Also useful in foot & ankle surgery
Small Grip Handle Version with the grip closer together for easier gripping and to help reduce hand fatigue
Small, Serrated Outside Pads with Small Grip #1842-01-SG


Medium,


EXCLUSIVELY FOR INNOMED IN GERMANY
Deep #T1006-01
Standard #T1006
Small, Flat Medium, Flat Outside Pads #1843
Serrated Outside Pads #1843-01 Small, Serrated Outside Pads #1842-01
EXCLUSIVELY FOR INNOMED IN GERMANY
Teeth #1862
3
8
mm 5 mm
mm
MADE EXCLUSIVELY FOR INNOMED IN GERMANY Long Jaw Shown Short Jaw, 8 mm Wide #1775-01 Medium Jaw, 5 mm Wide #1775-02 Long Jaw, 3 mm Wide #1775-03 Basic Screw Removal System
designed to help remove damaged and broken screws from 1.5 to 7.0 mm Set in Case Complete System with Case #2022-00 Also Available Individually
System
Plate MADE FOR INNOMED IN GERMANY FREE TRIAL ON MOST INSTRUMENTS 1.800.548.2362 103 Estus Drive, Savannah, GA 31404 info@innomed.net 912.236.0000 Phone 912.236.7766 Fax Innomed-Europe Tel. +41 41 740 67 74 info@innomed-europe.com © 2023 Innomed, Inc. ISO 13485:2016 www.innomed.net Innomed-Europe Alte Steinhauserstrasse 19 CH-6330 Cham Switzerland Tel: +41 (0) 41 740 67 74 www innomed-europe com UK Distributor: Hospital Innovations Ltd Concept House Talbot Green Business Park Pontyclun UK CF72 9FG Tel: +44 1443 719 555 www hospitalinnovations co uk
Instruction

From the President
Workforce Challenges
Simon Hodkinson
Ihave just returned from San Francisco having attended the American Academy of Orthopaedic Surgeons (AAOS) as part of the international duties of the President. This is a fantastic opportunity to contribute to the global development of orthopaedics and to share and learn about approaches to the challenging issues of the day. One of the projects the Carousel is looking at is to work with the World Health Organisation (WHO). The WHO has identified that approximately 1.71 billion people have musculoskeletal conditions worldwide, with musculoskeletal conditions being the leading contributor to disability worldwide.
The UK is not alone in having a growing and ageing population, with the consequence that the number of people living with musculoskeletal conditions and associated functional limitations, is increasing rapidly. Nor are we alone in having a surgical workforce that is not keeping pace with the inevitable demands.
We do not have enough qualified surgeons. On a per capita basis, we are at or near the bottom of the league in T&O workforce in the developed world.
The recently launched 2023 UK Surgical Workforce Census Report highlighted the real issues we have with our current workforce and the acute need to retain what we have.
In my last piece I mentioned talking in Australia to UK trainees who have left our shores to go down under and depressingly whilst at the AAOS I met a final year medical student from the UK who, clearly motivated to follow a career in T&O, is seeking to leave our shores for a residency in the USA.
Reasons for leaving are, I am sure, multifactorial but one message was clear and that was the impression that a future career in the NHS is not good.
This was the message from the AIMS study last year and one we all need to work towards correcting.
At the RCS England recently, I raised the issue of single employers for trainees and was told that this was something that was being worked on. I hope this long needed change in how we employ our trainees in England in particular, comes sooner rather than later. Every little helps as someone once said!
The regulation of the Physician Associate role is taking up a lot of bandwidth in the medical profession and in Parliament. My two colleagues in the Presidential line are working with the RCS England to achieve a consensus and currently the plan is for the BOA to develop the scope of practice and competencies required for such practice within the speciality. This is a hugely sensitive issue with many aspects to consider; we need a careful, considered and well-informed discussion as to how best to ensure that Physician Associates complement existing provision for the maximum benefit of patients.
Our work with the MHRA and NHS Supply Chain continues, and we have tacit agreement from industry to keep the profession informed of potential removal of products from the UK. Industry and the MHRA accept that sudden removal of products is not in anyone’s interest, least of all the patients!
I recently met with PHIN to discuss concerns raised by members. Those of you in private practice will be aware of PHIN and the mandate it holds from the CMA.
You will be aware that limited data on your practice will become publicly available in autumn this year. I would urge any of you who have not checked the data PHIN holds on your practice to do so. Whilst we are the best of all specialities in terms of initial engagement only 50% of us have checked our data.
PHIN has reassured me that if any issue as to the accuracy of data held is raised, it will not be published until the issue has been resolved, but not engaging will be taken as tacit approval of its accuracy.
Finally, some of you will be aware of the forthcoming launch of ‘NCIP’, this will become an important part of our practice, so I commend the article to you.
Spring will be upon us soon so we can hopefully look forward to warmer and drier weather and I hope you enjoy this edition of the JTO.
If any member has a burning issue to raise, then please feel free to contact me at president@boa.ac.uk or the BOA direct. n
Ortho Update 2024 Ronnie Davies
After a successful return to a face-to-face format last year, the Update course returned to Manchester on a bright and sunny Saturday. This year, we focused on exams and examination. We had some wonderful clinical examination sessions focusing on foot & ankle, spine and hands. A fantastic group of medical students added to the realism as simulated patients and boy, what a performance they put on! Candidates had several chances to complete CEXs throughout the day for their clinical examinations.
As usual, we ran some case discussions covering important topics for the FRCS, enabling completion of CBDs. The discussions covered paediatric hip pain, the ‘foot attack’, and a return of last year’s favourite session, ‘the good, the bad and the ugly’, in which faculty aired their dirty laundry to discuss principles of fracture fixation.
We had a fantastic session run by senior examiners to demystify the FRCS Orth. The talks covered all parts of the exam, and we even had some guest appearances from recent exam candidates to give their top tips for passing. There was plenty of time for a lively Q&A session so, for once, examiners had to answer some difficult questions, but they all answered admirably!

A highlight of the course was the thought-provoking plenary lecture by David Sellu, who spoke of his experience of a full GMC investigation, imprisonment and eventual acquittal following appeal. He spoke without a hint of bitterness about the protracted process and gave some helpful advice to people facing a GMC investigation. It was certainly the talking point at most tables over lunch.
We are already planning next year’s course, which is provisionally set to cover non-technical skills through a series of simulations, along with an FRCS workshop and some case discussions around critical conditions. Of course, there will be a few surprises to make it another excellent day of orthopaedic education. n

British Orthopaedic Foot and Ankle Society (BOFAS) update
Brown,
Over the last year the British Orthopaedic Foot and Ankle Society has set an agenda of inclusion.
• Inclusion of all our 706 members in the wide-ranging activities of BOFAS is central to us. Our new EDI working group commissioned an external survey, which gave us a deeper appreciation of who we are and the specific concerns of our diverse membership. This led to a new mentorship programme and wider more inclusive faculty selection for meetings.
• Inclusion of the voices of surgeons from the devolved nations was highlighted in our survey. Consequently, we now have bi-annual meetings of their leaders with the BOFAS President.

• Inclusion of all ankle arthritis surgeons into regional networks to manage complex ankle deformities has moved forwards this year. This will allow patients across the country access to both replacement and re-alignment surgeons. In November, a consensus group thrashed out our new BOAST guidelines to manage primary, revision and infected ankle replacements as well as the flow of patients through these networks.
• Inclusion of our valued allied health professionals has continued with our successful courses for physiotherapists, while we have initiated discussion with the Faculty of Podiatric Surgery to develop an understanding of each other’s training, scope of practice and regulation.
• Inclusion of overseas surgeons on our courses in Zambia and Togo, while our Principles Course returned to India for the first time since COVID-19.
• Inclusion of a Sports Ankle Arthroscopy course into our acclaimed portfolio of courses which already included the Principles of Foot & Ankle Surgery course and the Advanced Fellows Forum. This hands-on training gives aspiring orthopaedic foot and ankle surgeons essential skills in ankle arthroscopy.
• Inclusion and invitation of all the European Foot and Ankle Surgeons has increased the participation in our two webinar series. Firstly there is the ‘Master Techniques’, where experts discuss their tips and tricks and secondly ‘The BOFAS Journal Club’ where the authors defend and reflect on their published papers.
• Inclusion and co-ordination of units in new multi-centre RCTS began to answer the key questions defined in the JLA initiative by our scientific committee.
• Inclusion of the BOFAS voice on national bodies such as NJR and NICE is vital. We are pleased to have co-badged with GIRFT a consent form for a first metatarsal osteotomy.
• Inclusion of the Irish orthopaedic Foot and Ankle Society as our Guest Nation at our Annual Scientific Meeting in Belfast demonstrates our outward approach, with a further joint meeting planned with the Australians in 2026. n
06 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk News
Rick
BOFAS President
BOFAS Consensus meeting

The complete solution for ophthalmology now new and improved.
Contact us today:
+44 (0)1943 878647 sales@aneticaid.com

Basic Shoulder Arthroscopy Course
Wednesday 15th May 2024
Course convenor: Mr Tan Thangarajah

Thursday 16th May 2024
Course convenor: Mr Ricci Plastow

Suitable for CT1 to ST5 and Scrub Staff
Hosted by
UCH Education Centre, 250 Euston Road
To book a course please e-mail uclh.simulationcentre@nhs.net

Ophthalmic Stretcher
Basic Knee Arthroscopy Course
2024 New Year Honours
The BOA congratulates the following members of the orthopaedic community who were awarded honours at the start of the year.
• Professor Neil Mortensen, Lately President, Royal College of Surgeons of England, was awarded a Knighthood for services to Surgery.
• Professor Simon Kenny, National Clinical Director for Children and Young People, NHS England and Consultant Paediatric Surgeon, Alder Hey Children’s Hospital, was awarded an OBE for services to Paediatric Surgery.
• Professor Panagiotis Giannoudis, Professor of Trauma and Orthopaedics, University of Leeds and Founder of Day One Trauma Support, was awarded an MBE for services to Trauma and Orthopaedic Surgery.
• Professor Antony Johansen, Consultant OrthoGeriatrician, Cardiff and Vale University Health Board, was awarded an MBE for services to Older People.
Committee Appointments
Following a successful round of applications, the BOA would like to congratulate all those who have been appointed onto the BOA Committees:
Orthopaedic Committee
• Jehan Zaib
• Naomi Davis
• Lucky Jeyaseelan
Research Committee
• Andrew McCaskie (Chair)
• Ines Reichert
• Yuri Kulikov
Trauma Committee
• Sue Deakin
• Sarah Johnson-Lynn
Education and Careers Committee
• Ajay Malviya (Vice-Chair)
• Usman Ahmed
• Kapil Sugand
UKITE 2023
We had an excellent turnout of 812 trainees for UKITE in December 2023 from across the UK and Ireland joined by 187 candidates from Malta and South Africa. Candidates received question-level feedback on their responses to better support their learning. Congratulations to West Midlands (Oswestry/Stoke), who were the highest scoring training programme this year with an average score of 57% for the 31 trainees who took part.
UKITE would not be possible without our excellent team of editors and subspecialty leads who write and select the questions. Thank you all for your contributions. If you are interested in getting involved for this year, you can find out more information www.boa.ac.uk/ ukite or email ukite@boa.ac.uk
Robotics in Orthopaedics Research Fellowships
The BOA, the Royal College of Surgeons of England and the Royal College of Surgeons of Edinburgh have produced a series of guidance documents to provide a practical tool kit for hospitals when setting up a new MSK robotic surgical service. A guide for patients has also been produced. They are all available to view at download at www.boa.ac.uk/robotics.


The BOA and Orthopaedic Research UK are delighted to announce the third cycle of BOA ORUK joint Research Fellowships will be open for applications, closing April 2024. Two fellowships of up to £65k will be available for a project in any area of orthopaedics. Funding will be available for salary (maximum £60k) or as a stipend at UKRI levels. BOA Members at any trainee grade and SAS surgeons are invited to apply. To support diversity and inclusion within trauma and orthopaedics, we encourage applications from individuals that wish to undertake their research flexibly or less than full-time (minimum 0.5 FTE). More information at: www.boa.ac.uk/researchfellowships
Clinical Impact Awards (ACCIA) 2024 Process
The 2024 Clinical Impact Awards (successor of the Clinical Excellence Awards) will open for applications from 4th March to 15th April 2024.
The full application timetable and guidance is available on the ACCIA webpages. A link to their Applicant’s quick guide for 2024 outlining what is needed for each level of the awards to assist with applications is available at: www.gov.uk/government/ publications/clinical-impact-awards-2024-applicants-guide
08 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Latest News
2024 Council and Presidential Nominations
Council Trustee and Presidential nominations open on 15th March.
You have the opportunity to bring your skills and expertise to help us grow and develop the BOA and Trauma and Orthopaedics as a whole. A more diverse BOA, and a broader range of voices, better serves our patients and best supports our colleagues and we welcome applications from across our membership.
Please be sure to submit your nominations for Council before the deadline of 15th April and for BOA President by 1st June. More information and how to apply is available after 15th March on the BOA nominations website at www.mi-nomination.com/BOA
As a result of the resolutions passed at the 2023 AGM, all voting members are eligible to stand for election to Trustee posts on the BOA Council.
Death certification reforms in England and Wales
From April 2024 new death certification reforms will come into force in England and Wales. There will be an independent review of all deaths in England and Wales, without exception either independent scrutiny by a medical examiner or by investigation by a coroner.
Other changes from April 2024 include a new medical certificate of cause of death (MCCD) to reflect the introduction of medical examiners, who will scrutinise the proposed cause of death.
Further details can be found on the BOA website at: www.boa.ac.uk/ death-certification-reforms.

Nottingham Clinical Trials Unit: Free Virtual Course on Developing your Research Ideas in Trials in T&O
As part of our partnership with Nottingham Clinical Trials Unit (NCTU), we are delighted to offer opportunities for BOA members and associates to undertake courses about clinical trials and systematic review free of charge.
For further course information visit www.nctu.ac.uk/our-research/otherclinical-research/current-studies/trauma-and-orthopedics.aspx

PHIN Update
PHIN will launch a new portal for consultants during March 2024 – details can be viewed on the BOA website at www.boa.ac.uk/PHIN. The changes are based on feedback PHIN received from consultants and include:
• Consultants will be able to provide information on their fee arrangements with insurers, in addition to information about fees charged to private self-pay patients for consultations and procedures.
• Consultants will be able to nominate a delegate to work with them to submit and manage data to fulfil these activities.
Volume, Length of Stay and Patient Feedback are the only consultant measures published on the public PHIN website – and only data verified by consultants will continue to be published. As currently, consultant data about Adverse Events, Never Events and PROMs will only be available privately in the PHIN portal.
The majority of consultants are providing fee information, with 84% of Orthopaedic consultants submitting their data, however, only around 50% of consultants have validated their data, that is around 1,500 consultants that risk inaccurate data – which is submitted by the hospital – appearing on the website if they do not respond to the numerous prompts made by PHIN. Presumed publication of data is scheduled for Autumn 2024.
Consultants with eight or fewer episodes of data in any publication period will not have data published; patient feedback will only be published when more than 30 responses have been received.
The updated version of Good Medical Practice (www.gmc-uk.org/good-medical-practice) came into effect on 30th January 2024. This includes advice on ‘Being open with patients about your fees and charges’ and within this there is now a section on the requirement to submit fee information to PHIN as set out in the Private Healthcare Market Investigation Order, 2014 as amended.
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 09 Latest News
Zimmer Biomet sponsored travelling fellowship
Lt Col Sushmith Gowda
Iam extremely grateful to the BOA Committee and Zimmer Biomet for the travelling fellowship awarded in 2022. My primary learning objectives for the fellowship were to observe and learn about day-case arthroplasty and the use of roboticassisted hip and knee replacements to help set up a similar practice at Portsmouth.
In December 2023 it was a privilege to shadow and learn from Dr Antonia Chen, Associate Professor at Harvard Medical School and Director of Research for Arthroplasty at Brigham and Women’s Hospital (BWH), Boston, Massachusetts, USA. We also shared cases and arthroplasty related issues in the UK, USA and Hong Kong, for example bone cement for arthroplasty is not widely used in the USA compared to the UK; uncemented femoral implants are used by most arthroplasty surgeons.

At BWH four total joint replacements were handled during the working day; very similar to the NHS practice (pre-COVID era). However, the proficiency between turnover of cases was evident as there was minimal disruption during patient flow. Day-case arthroplasty has been championed at BWH over the last few years and their practice has led the way with evidence and protocols that are followed in the USA and worldwide. The uncemented total hip replacements (THR) were performed through the direct anterior approach (DAA) with the patient in supine position. The surgeons who prefer DAA for THR attribute this muscle sparing technique to faster recovery and quicker discharge. Post-operative radiographs were taken before discharge and follow-up was organised accordingly.

Uncemented total knee replacements were performed with robotic assistance and high-volume, local infiltration anaesthetic was standard practice. Robotic-assisted arthroplasty was standard practice for both hip and knee arthroplasty cases for Dr Chen. As a high-volume arthroplasty, robotic-assisted surgery has been used for more than five years. Data is collected for the registry and patient outcome scores, very similar practice to the UK and our National Joint Registry. This experience was extremely valuable and provided an insight into a different healthcare system with a strong ethos on proficiency, innovation and pioneering new techniques. I am very honoured to represent BOA and the members who gave me this amazing opportunity to travel, meet and learn from other institutions to further my surgical portfolio and develop my practice at Portsmouth. n
New BOA Trustee ( 2024 – 2026)
Dominic Meek
Professor Meek was appointed as a Consultant Orthopaedic Surgeon in 2003 and currently works at the Queen Elizabeth University Hospital, Glasgow. He is a specialist in hip reconstructive arthroplasty surgery in particularly young and complex revision surgery and hip resurfacing. He undertook a fellowship in adult reconstruction of the hip at the Department of lower limb arthroplasty, Vancouver University Hospital. Professor Meek was awarded the British and American Hip Societies Travelling Fellow and the ABC Fellowships, and is the Hip Specialty Editor for the Bone and Joint Journal, UK.
Professor Meek is an Honorary Professor at Glasgow University, immediate Past President (March 2024) of the British Hip Society (BHS), President of the West of Scotland Orthopaedic Research Society (WoSORS) and co-founder (2009) of the Glasgow Orthopaedic Research Society (GLORI) for fundamental science research at Glasgow University. He is a member of the European Hip Society (EHS) and the International Hip Society (IHS). n
10 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
News
British Orthopaedic Trainees Association update
It is with great pleasure that I introduce you to the new BOTA Committee of 2023-2024:
President – Karen Chui
Vice President – Kate Atkinson
Secretary – James Chowdhury
Treasurer – Adrian Andronic
Immediate Past President – Abhinav Singh
Education – Charmilie Chandrakumar
Publicity – Marios Ghobrial
Academic – James Archer
SAC – Kumar Dash
Webmaster – James Allen
Woman in Surgery – Sophie Donoghue
Global Surgery – Alice Campion
Culture & Diversity – Vasudev Zaver
Sustainability & Workforce – Oliver Townsend
Northern Ireland – Jagdeesh Nijjher
Wales – Clara Miller
Scotland – Dominic Waugh
Junior – Sally Rankin
BOMSA – Sophie Heppenstall
The new committee consists of a dynamic and passionate group of trainees from deaneries across the UK, including Northern Ireland, Scotland, Birmingham, London, Yorkshire, Wales, Mersey, East of England, Severn and Wessex. A truly British orthopaedic representation. I am excited to be working with this energetic new committee in the coming year to represent our members and deliver educational events.
This year, our committee promises to continue advocating, at the highest national level, for high-quality orthopaedic training and the protection of training opportunities for trainees. We will champion for increased diversity and inclusion in our specialty, and culture change for a better work-life balance that fits the modern surgeon. Recognising the impact of ongoing industrial action and risk of burnout in trainees, we will campaign for increased measures to look after the well-being of our members.
Furthermore, we will ensure that patient safety and trainees’ needs are prioritised as the NHS Long Term Workforce Plan rolls out, along with the development of the Extended Surgical Team.
Karen Chui, BOTA President
Now more than ever, we need to ensure trainees’ voices are heard and represented. Thank you to our incredible BOTA Regional Representatives network, whom we rely on to help us gather timely and accurate feedback from our members from all regions, to present at national meetings.
The BOTA Committee look forward to delivering to you an exciting calendar of events in 2024 to our membership, including the ASIT pre-conference BOTA course, the BOTA Academic Day, the World Orthopaedic Concern Conference, Sustainability Conference, Culture & Diversity Day, sponsoring BOMSA events and the highlight of the year, the BOTA Academic Congress in Manchester.
In addition, we will be awarding bursaries and prizes throughout the year, including the BOTA Traveling Fellowships, the Junior Essay Prize, the BOTA/ASIT Education Grants, the BOTA/WOC Fellowships, Medical Student Elective Bursaries, and the Dragon’s Den Research Grants. Thank you to the BOA for their unwavering support of BOTA and trainees. We look forward to seeing you at our educational courses and events. n

JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 11
News Why struggle with crutches, when you can be hands-free? kneecrutches.co.uk admin@kneecrutches.co.uk 0800 471 4974 @kneecrutches Pioneering patient mobility Introducing the hands-free alternative for non-weight bearing injuries Scan to learn more ENABLES A RETURN TO DAY-TO-DAY ACTIVITIES INCREASES BLOOD FLOW, DECREASES VENOUS STASIS INCREASES MUSCLE ACTIVITY PREFERRED BY 90% OF PATIENTS HANDS-FREE CRUTCH MR THOMAS GOFF Consultant Trauma & Orthopaedic Surgeon Mid Yorkshire Hospitals NHS Trust “As a Consultant Orthopaedic Foot & Ankle Surgeon, many of my patients have a period of 6 to 12 weeks of restricted weightbearing after major surgery. Using crutches, a frame, or a wheelchair can make it difficult to maintain independence with everyday activitieswashing, cooking, cleaning, climbing stairs. I now recommend the iWALK to these patients, having a hugely positive impact on their recovery.” KC_JTO_February_190x130_AW.indd 4 22/02/2024 17:33
Society for Back Pain Research (SBPR) update
We are excited to invite you to the Society for Back Pain Annual Meeting, which will be held at Robert Gordon University in Aberdeen, 13th-14th June 2024. This meeting is an excellent opportunity to learn about the latest research in back pain and network with other key professionals and researchers in the field.
This year’s meeting is titled ‘Innovation in Research and Management of Spine Pain’
We have an impressive line-up of keynote speakers this year, including
Dr David Hohenschurz-Schmidt from Imperial College and University College of Osteopathy London, who will be discussing innovations in non-pharmacological trials and the roles of explanatory and pragmatic designs. Dr Liba Sheeran from Cardiff University will be presenting on advances in digital and health technologies for management of spine pain. Finally, Professor Tim Holsgrove from the University of Exeter will be discussing complex physiological loading of the spine.
Of course, it wouldn’t be an SBPR meeting without the Friday afternoon

debate, the topic for discussion this year is ‘Technology, is it a help or a hindrance in research and management of LBP?’
In addition to these keynote speakers, there will be the normal excellent variety of presentations and posters covering the latest research on back pain, innovation, and best practices for managing patients with back pain. You will also have the opportunity to network with colleagues in the field and share your own research and seek collaborative opportunities.
Abstract submission is now open, please visit our website at www.sbpr.info/ meetings to download instructions and to submit your abstract. The deadline for submission is Sunday 31st March 2024.
For registration, please visit our online store www.sbpr.info/shop. Please note Early Bird rates end Friday 3rd May 2024.
We welcome members and nonmembers at our meetings and encourage new members.
If you would be interested in becoming a member of our society, please visit: www.sbpr.info/about-us where you can download the membership application form. n
British Orthopaedic Sports Trauma & Arthroscopy Association (BOSTAA) update
Sanjeev Anand and Nick Nicolaou
BOSTAA had a very busy and productive last year.
BOSTAA’s membership base is growing steadily.
BOSTAA hosted its very well attended annual meeting at the home of cricket, Lord’s on Nov 9, 2023. The theme of the meeting was, ‘Instability in sports trauma’. There was a lot of engagement from the audience to the talks presented by many highly accomplished speakers.
We also continued to offer our popular annual educational events, such as the London Research meeting and the Advanced Knee Arthroscopy course. In addition, we introduced two new cadaveric workshops on upper and lower-limb surgical approaches in Sheffield, which were organised by our trainee committee member, Siddharth Shah. These events were very well received and appreciated by the participants.

BOSTAA collaborated with BASK in the ‘James Lind Alliance First Time Soft tissue knee injuries priority setting partnership’ project. Humza Usmani led this project from BOSTAA, which identified the Top 10 priorities for future soft tissue knee injury research using a rigorous and validated process. BOSTAA has also been actively involved in various international events and initiatives to promote the field of sports medicine and arthroscopy, with one of the highlights being its participation in the European Society of Sports Traumatology, Knee Surgery, and Arthroscopy (ESSKA) annual meeting.
BOSTAA is proud to report that it is now recognised by the International Orthopaedic Diversity Alliance as an organisation
committed to improving Diversity, Equity, Inclusion, and Engagement in Orthopaedic Surgery.
Our online presence is also gaining traction on social media platforms, thanks to the creative campaigns run by our trainee committee members, Jimmy Murray and Irrum Afzal. One of our most successful campaigns was the 12-days to Christmas campaign on X/Twitter, where our senior executive team shared a daily surgical tip with our followers.
BOSTAA also had a change of leadership, with Rhidian Thomas taking over the presidency from Professor Deiary Kader, who completed his two-year term with great achievements. n
12 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
News
BOA Annual Congress 2024
17th – 19th September, ICC, Birmingham www.boa.ac.uk/Congress #BOAAC24
This year’s flagship event will take place 17th – 19th September at the ICC, Birmingham with Friday 20th September reserved for BOA courses and workshops. This year's theme is ‘Recruit, Sustain, Retain: The T&O Work Force’.
The programme will include the BOA keynote lectures, plenary speakers and an update from the BOA President, Simon Hodkinson on his Presidential year. We will be working closely once again with the specialist societies to deliver revalidation, hot topic sessions and several thought-provoking lectures.
Please keep an eye on the BOA website over the upcoming months for updates on abstract submissions, the programme and speakers, exhibitors and sponsors, accommodation information and more, www.boa.ac.uk/Congress.



BOA Abstract Submissions
BOA abstract submissions are now open and will close on Sunday 5th May Selected abstracts will be presented between 17th and 19th September. Categories include: ATOCP/Physiotherapy, Basic Science, Developing World Orthopaedics, Education; Foot and Ankle, General Orthopaedics, Hands; Hips, Innovation in Simulation, Knee, Limb Reconstruction, Medical Student, Paediatrics, Quality Improvement, Recruit, Sustain, Retain: The T&O Work Force, Shoulder and Elbow, Spines, Sports Trauma, Trauma, and Tumours.
If any of your colleagues are not currently BOA members and are planning to attend the next BOA Annual Congress in September, please do encourage them to join (www.boa.ac.uk/join) as one of the many benefits of BOA membership is access to the 100% discount on ticket fees during the Early Bird registration period!
Registration
Following changes to our registration process last year, registration will once again open for all bookings (both BOA members and nonmembers) on Monday 8th April. BOA members can take advantage of their membership by registering with a 100% discount on the ticket fee. The member early bird discount period will run for 12 weeks until Sunday 30th June. Full details can be found on the Congress website www.boa.ac.uk/registration
Exhibition and Sponsorship Opportunities
The BOA Annual Congress puts you in a room with over 2,200 healthcare professionals. Join us to build a quality database, increase your sales, meet competitors and keep up to date with the needs of your customers. With over 80 exhibitors every year this is a must-attend event that provides you with a truly unique opportunity to connect with key decisionmakers, showcase new products, solutions and technologies, build relationships and keep up to date with the needs of your customers.
Maximise your exposure at the Annual Congress by taking advantage of our Digital Advertising and Sponsorship opportunities. Our exhibition packages are designed to be comprehensive and competitive. If you are interested in any of the opportunities, please contact the Exhibition Team exhibitions@boa.ac.uk.




JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 13 RECRUIT SUSTAIN RETAIN THE T&O WORK FORCE BOA ANNUAL CONGRESS 2024 17th – 19th SEPTEMBER 2024 ABSTRACTSUBMISSIONSNOWOPEN. CloseonSunday05thMay2024. www.boa.ac.uk/abstracts News
Conference Listing 2024:
BOFAS (The British Orthopaedic Foot and Ankle Society) www.bofas.org.uk
06-08 March 2024, Belfast
BSCOS (British Society for Children’s Orthopaedic Surgery) www.bscos.org.uk
07-08 March 2024, Leeds
BLRS (British Limb Reconstruction Society) www.blrsmeeting.com
14-15 March 2024, Glasgow
BASS (British Association of Spine Surgeons) www.spinesurgeons.ac.uk
20-22 March 2024, Bournemouth
BSSH (British Society for Surgery of the Hand) www.bssh.ac.uk
25-26 April 2024, Leeds
BASK (British Association for Surgery of the Knee) www.baskmeeting.com
16-17 May 2024, London
BAJIS (Bone and Joint Infection Society) www.bajis.org.uk
13-14 June 2024, Gateshead
SBPR (Society of Back Pain Research) www.sbpr.info
13-14 June 2024, Aberdeen







We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital equipment is fully protected in transit.

BESS (British Elbow & Shoulder Society)
www.bess.ac.uk
20-21 June 2024, Aberdeen
BOOS (British Orthopaedic Oncology Society) www.boos.org.uk
27-28 June 2024, Cardiff
BIOS (British Indian Orthopaedic Society) www.britishindianorthopaedicsociety.org.uk
5-6 July 2024, Newcastle
BORS (British Orthopaedic Research Society) www.borsoc.org.uk
09-10 September 2024, Sheffield

BOA (British Orthopaedic Association) www.boa.ac.uk
17-20 September, Birmingham
equipment is fully protected in transit. We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to
house implant samples, instruments and any other equipment.
Trifibre Ltd
17 Boston Rpad
Gorse Hill Industrial Estate Leicester LE4 1AW
We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to house implant samples, instruments and any other equipment.
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk
Web: www.trifibre.co.uk
Trifibre Ltd
17 Boston Rpad
Gorse Hill Industrial Estate Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk
Web: www.trifibre.co.uk
14 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
News
BOA Congress 2024, ICC Birmingham
BESS Annual Conference 2024, P&J Live, TECA, Aberdeen
Joint Action - The Orthopaedic Research Appeal of the BOA
The Winter Appeal
Thank you to everyone for donating to the Joint Action Winter Appeal this year. With your generosity, we have raised a fantastic £7,000. If you haven’t already donated and would like to help raise funds for trauma and orthopaedic research, you can donate online at www.justgiving.com/campaign/ jachristmasappeal2023. All funds raised will go to activities like Clinical Trials and Research Fellowships.

Challenge Events - Support our Runners and Riders!
2024 TCS London Marathon
Please support our runners taking part in the TCS London Marathon on Sunday 21st April. Our amazing team raising funds for Joint Action include Emily Baird, Alex Chipperfield, Tom Curtis, Charlie Gozzard, Traceyanne Hughes, John McKinley, Natalia Mojica,


Sanjay Mulay and Benedict Rogers. Please donate and show your support for our runners at: https://2024tcslondon marathon.enthuse.com/british orthopaedicassociation/profile
Ford RideLondon-Essex 100
Please support our riders, Duncan Beedall, Mike Keen and Eugene O’Herlihy who will be cycling 100 miles in the Ford RideLondonEssex 100 on Sunday 26th May to raise funds for Join Action.
You can donate at: https://2024 fordridelondon.enthuse.com/ britishorthopaedicassociation/profile
Find out more about Joint Action, The Orthopaedic Research Appeal of the BOA online and the clinical trials we are currently funding at: www.boa.ac.uk/clinical-trials

JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 15 News
Charlie Gozzard
Natalia Mojica

What really matters?
Hiro Tanaka
This article was originally published 27th December 2023 on Orthopaedics Online (www.boa.ac.uk/O2) and the content was presented by the author at the 2023 BOFAS Annual meeting.
Hiro Tanaka is a Consultant orthopaedic surgeon in South Wales. He is the BOA Honorary Secretary and co-directs the BOA Future Leaders Programme.
A blink of an eye
Did you know that the human blink of an eye lasts a third of a second. You and I are right now blinking 20 times a minute, which means that our eyes are closed for 10% of the time that we are awake. Despite that, it’s imperceptible to us, it’s as if our mind edits out the time as if it never happened. And yet a lot can happen in a third of a second.
When we look up to the night sky, in the vastness of our universe, 300 stars will explode in a spectacular supernova every blink of an eye. On our planet, over 3,000 bottles of coke will be drunk every blink of an eye. In fact, there are so many plastic bottles of coke on this earth right now that if they were laid end to end it would reach the moon
and back… 1,000 times. Within our NHS, 1.5 million patients are treated every 36 hours meaning that on average 17 patients receive treatment every blink of an eye.
So much happens around us that we never see or think about. What do you think we would see if we stopped blinking and really looked at ourselves and the people around us at work?
I’m going to invite to you to take a step back from our clinical minds and ask ourselves the question: ‘What really matters?’ in our work. What are the things that really allow us to find true happiness in the work that we do, sustain it throughout our lifetime and be successful in delivering the highest quality of care to our patients?
Features
16 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
The problem is that we’re all trapped inside our own minds. We create our own life stories where we are the heroes and we pick and choose who and what to include in our story. Like a good movie, we edit and delete the things that happen to us and these are influenced by our beliefs which we often inherit from our parents. For example, we go out into the world thinking that in order to be successful we have to be strong and not show any weakness. Or that we have to please people in order to be loved or that we have to be perfect in everything we do. Or that whatever I do, I’ll never be good enough.
Each one of us is searching for the same thing. Now I can’t help you in the love department and I’m the last person to be telling you how to live a healthier life. But maybe we can explore what it means to be truly happy in our work.
In order to do that we have to let go of two things. Firstly, we need to realise that the stories we tell ourselves about our own lives are just fiction and only exist in our own heads. No one else sees it and they probably don’t care that much anyway because they too are struggling with their own stories. Secondly, true happiness comes from lasting satisfaction. We often confuse pleasure that we get from passing an exam, buying that new car, getting recognition from our peers or being elected to a position of authority as happiness but we all know that it doesn’t last. It becomes an addiction where we end up striving for the next hit of success, something that Arthur C Brooks calls the ‘hedonic treadmill’.
So I’m going to share with you three personal stories from my life where I learnt the meaning of lasting happiness in my life and work. The irony is that it is often through pain that we find true meaning.
The hedonic treadmill
Early on in my career, I was definitely on that hedonic treadmill. Three years into my Consultant appointment, I was Clinical Director with a full private practice and working every other Saturday. At the time, I was earning three times more than I do today but at no point in my life did I feel poorer. For four years, I missed virtually every bath time with my daughters who were aged four and two at that time. One day, after I had been away for a week, I came home late at night and I remember the strangest feeling walking into my own house as if I was sneaking into someone else’s
home. As I walked up the stairs, I felt faint and I managed to get to the bedroom where I collapsed with SVT. As I lay on the floor, I remember my wife crying saying, “Why are you doing this to us? Why are you doing this to us!”. And all I could say was “I’m doing it for us”. To this day, I’ll never forget what she then said. She said, “No… you’re doing it for yourself”. It was her that made me realise just how much I was hurting myself, my family, colleagues and my patients in the pursuit of my goals.
I believed that I should build my career like building blocks. Provide a good living for my family. Be seen to be the best at what I do. Get the respect of my peers and get recognition for the work that I do. And leave a lasting legacy of my career so I’ll be remembered. How wrong I was.
The flaw in this belief is best described by the parable of the three stonemasons. It dates back to the Great Fire of London. As St Paul’s Cathedral was being rebuilt, Sir Christopher Wren visited the site and one morning he spoke with three stonemasons working on the foundations. He asked the first stonemason what he was doing. “I’m making blocks of stones to feed my family”, he said in a rather uninterested voice. He asked the same question to the second stonemason who said, “I’m making a perfect block of stone so that it’ll fit into the wall over there”. The third stonemason seemed happiest in his work and was clearly the
leader of the group and when asked the same question he replied, “I’m building a cathedral”
We could spend our entire careers making blocks of stones, not understanding the greater difference our work was doing or shall we say at the end of our careers that we built a cathedral?
Search for purpose
Dan Beuttner is an Emmy Award winning journalist. In 2005, he published the cover story in the National Geographic entitled ‘The secrets of a long life’. He had spent 20 years travelling and researching places in the world that he called ‘The Blue Zones’. One such place is the village of Ogimi on Okinawa Island in Japan. It’s a normal village made up of families and children except for one odd fact. At the last count, of the 3,000 villagers, 1 in 200 were centenarians and 6 out of 100 are in their 90s. Comparing that to pre-COVID times in the UK, only 2 in 10,000 were above 100 and 9 out of 1,000 are in their 90s. The difference is staggering, some 20-fold difference in longevity! Beuttner’s research sought to explain why. It comes down to three factors: diet, genetics and Ikigai, which is widely practiced by the islanders.
So what exactly is Ikigai? It’s an age-old Japanese ideology that means “a reason for being”. Ikigai lies at the centre of who we are as individuals. During our career, in order to be happy, we must find balance. >>

Features
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 17

When we are on the hedonic treadmill, we focus upon the things we are paid for and the things we are good at. Fortunately, we are lucky in that the world needs our talents but we can easily forget to do the things we love doing and it’s that which gives us purpose
Arthur Brooks calls this the Pivot and it’s particularly important for those of us in the latter half of our careers. During the first half of our career, we have what he calls fluid intelligence which allows us to perform at our work pursuing those worldly rewards. But as we age into our 40s and 50s we start losing that ability and we develop a different form of intelligence, crystalline intelligence in the form of wisdom and experience. This is what allows us to pursue goals greater than ourselves and help others by mentorship, coaching and teaching. Those of us that don’t recognise that can become afflicted by the Striver’s Curse We can end up in an addictive cycle searching for that next hit of success. We put ourselves at risk of taking up jobs we hate just for its title, pursuing dangerous sports to prove that we can still do it, purchasing that sports car we don’t need and performing untested surgical procedures to expand our surgical expertise. These are just to name a few…
Friends or family?
They say that you can’t choose your family but you can choose your friends. When I was looking for my consultant post back in 2005, there wasn’t a job for me in Wales and I applied for a job at the Hillingdon as the only foot and ankle surgeon for the unit. I was the only one shortlisted and I spent a week
getting to know my future colleagues and the staff. I remember that the night before the interview, I was waiting for the bus outside the hospital in the cold and my friend Hari rang me. He had mentored me in my career and had taught me most of what I knew.
During that call he told me that he wanted what was best for me and that the Hillingdon was a great place with an amazing private practice and great opportunities. But he wouldn’t forgive himself if he didn’t tell me what an amazing life and great things we could achieve together and that he had secured a job for me if I agreed to come back. I didn’t know at that time that he’d actually threatened to resign if management didn’t fund my post! After discussing it with my wife, we realised that it’s the people that we work with that make the biggest difference and even when I spoke with my future colleagues on the very day of the interview, they said that if I had a colleague that was willing to do that for me, then that’s the place I should work. My career wouldn’t have been the same without friends like Hari. Surround yourself with colleagues who make you a better human being and surgeon.
I was blind
My final story is about Steve. Steve trained in regional anaesthesia in Cambridge and was appointed at the same time as me in 2005. I remember the discussions we had back then about whether it was even possible to perform day case awake foot and ankle surgery. Bear in mind that foot and ankle surgery at that time was almost all overnight under general anaesthesia. Over the course
of the next nine years, we experimented and developed much of the models of care and pathways which exist today.
We used to do our private list together on a Tuesday after which we would go for dinner or drinks and chat. One of our favourite places was a Sri Lankan restaurant in Cardiff and I still remember the day where he told me that he had been receiving treatment for Seasonal Affective Disorder and that he was leaving the UK to work in New Zealand. I would have been sad to see him leave, he was my friend and we had built so much together but he had three little girls and a wife he needed to think about. So we agreed we would have dinner again a couple of weeks later.
I got a phone call late that Sunday. They found Steve in the anaesthetic department. He’d taken his own life and left his three girls without a father. What a waste of a beautiful life. Maybe I didn’t understand just how serious his depression was or I didn’t ask hard enough. To this day, I don’t understand but I can’t help thinking about how blind I must have been to his pain.
Now, every time I go to the F&A unit, there are echoes of Steve everywhere in what we do. From the block room, to what we say to our patients, to the pathways and the stories we tell each other. And even now, our F&A surgeons go out on Tuesdays for dinner because that’s when Steve and I used to go.
We leave a part of ourselves in the stories of the people that we work with. The achievements and accolades that we gain in life will disappear and be forgotten but the memories of what we do for each other will last. There is so much more that happens in the lives of the people around us that we never see. Especially now, shouldn’t we stop blinking, open our eyes and support the lives of our colleagues that we work with?
When I think about the state of the NHS today, it fills me with sadness but I have hope. Hope that maybe out of this madness comes a new paradigm. A new way of working where we can finally focus on the things that matter the most. A blink of an eye only lasts a third of a second, in that time our world can change and it’s up to us to decide how. n
Features
18 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
20 patients · surgeons · nhs · hospitals · orthopaedic specialist societies · independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals orthopaedic specialist societies · independent sector · healthcare professionals doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals
orthopaedic specialist societies · independent sector · healthcare professionals doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals orthopaedic specialist societies · independent sector · healthcare professionals doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies independent sector · healthcare professionals · doctors · nurses · regulators
Proud to be the global exemplar orthopaedic medical device registry
njrcentre.org.uk

20 Years of the National Joint Registry: who benef its?
Part three: Service commissioners, regulators and policy makers, and broader society

Michael Whitehouse is a Professor of Trauma and Orthopaedics at Bristol Medical School, University of Bristol and Consultant Trauma and Orthopaedic Surgeon at North Bristol NHS Trust. He is a member of the NJR lot 2 contract for Statistical Analysis, Support and Associated Services.

Ashley Blom is Vice-President and Head of the Faculty of Health at the University of Sheffield. Professor Blom is a fellow of the Academy of Medical Sciences, an NIHR Senior Investigator and a member of the statistical analysis team of the NJR.
Michael Whitehouse, Ashley Blom, Deirdra Taylor and Mark Wilkinson on behalf of the
NJR Team
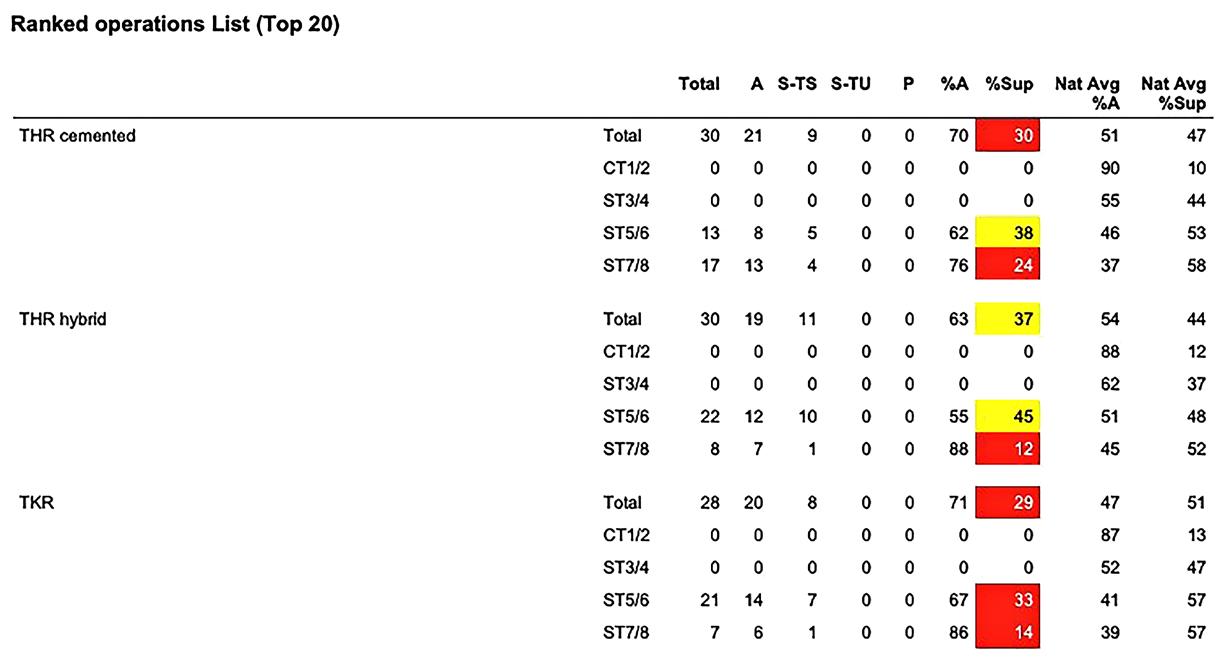
In this final part of the ‘Who benefits?’ series, we outline the benefits of the NJR to service commissioners, regulators and policymakers and to broader society through our research and innovation work. These benefits include quality improvement, cost-effectiveness and value for money, continuous surveillance for implant safety, and our active participation in the broader healthcare community (Figure 1).
Benefits to service commissioners
Service quality
We provide independent evidence of the overall safety, success and health benefits of joint replacement surgery, supporting commissioners to prioritise this service for the benefit of their local populations. The NJR is a mandatory dataset that supports measurement of the Best Practice Tariff (BPT) in England. BPT is a national price paid to providers and is designed to incentivise high quality alongside cost-effective care. The aim is to reduce unexplained variation in clinical quality and to encourage best practice. BPT will only be paid to a hospital if the registry compliance (85%) and consent (‘not recorded’ rate is less than 15%). A new BPT criterion was introduced from 1st April 2019 relating to hip replacement in patients aged over 70 years, whereby providers must use cemented or hybrid prostheses for at least 80% of patients.
Value for money
Implant devices account for a large amount of healthcare spend and thus it is important to ensure that the implants used in the NHS are both clinically effective and cost-effective. In order to support hospitals with the cost-effective
procurement of joint replacement implants, the NJR provides detailed reports to hospital managers as part of our price benchmarking service, to ensure transparency of prices paid by all trusts for similar devices. The NJR also routinely provides data to ‘Getting it Right First Time’ (GIRFT) and The Model Health System to ensure that high-quality metrics are made available to support the assessment of effective and value for money treatment nationwide.
As part of our ongoing research programme, we also support the health economic analysis of NJR data which has reported the relative cost-effectiveness of various implant choices to inform clinical decision-making.
Benefits to regulators and policymakers
Safety and implant surveillance
The NJR provides regulatory authorities with assurance that real-world data is collected, validated, audited and analysed in a robust way to support the effective surveillance of medical device implants, hospitals and surgeons. We provide robust mechanisms for identifying and flagging adverse trends in the outcomes of joint replacement surgery and have developed procedures for alerting the necessary clinical and regulatory bodies to these events. NJR supplier data is made available to the Medicines and Healthcare products Regulatory Agency (MHRA) to support their regulatory work. We routinely notify MHRA of any implant components that raise an alert. The Independent Medicines and Medical Devices Safety Review ‘First Do No Harm’, chaired by Baroness Julia Cumberlege, described the NJR as an “exemplar of national audit” and as “leading in the field”. >>
Features
20 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk

















Significant milestones in the development of the National Joint Registry 2012 2014 2015 2016 2008 2009 2019 2006 2011 2005 2007 2017 2021 2022 2013 2018 2023 2020 An Roinn Sláinte Männystrie O Poustie 2003 Annual Clinical Reports launched, enabling all hospitals to drill down into their performance and identify opportunities to improve. The House of Commons Science and Technology Committee states that the NJR ‘should serve as the gold standard for implant registries’ as part of their regulation of medical implants in the EU and UK report. Work commences with international partners to develop a global database ‘Unique Device Indicator’, which would later inform the development of the component classification system and international prosthesis library. Establishment of NJR patient network, highlighting the importance and value of involving patients in the work of the NJR. 2010 NJR is recognised by the Independent Medicines & Medical Devices Safety Review, chaired by Baroness Julia Cumberlege, which published its report and findings in 2020, as a ‘leader in its field’ and ‘being an exemplar registry with worldleading expertise’. NJR was identified in the government response to the Cumberlege Report as being ‘widely regarded as setting international best practice in analysing outcomes for device procedures.’ NJR reaches its second decade and celebrates its 20th anniversary. Introduction of enhanced NJR data collection with MDSv8, including hip hemiarthroplasty procedures and non-revision re-operations. Updating the dataset to reflect the most recent development in joint replacement practice enables the NJR to stay at the cutting-edge and allows the wider registry data capture to directly benefit a wider range of patients. Work begins to re-establish the NJR patient network and build on the experience undertaken during the period 2012-2017 to create a vibrant forum for the introduction of patient views. Rollout of data quality awards for hospitals with the best rates of completeness to encourage best practice. Our data collection was extended with the launch of MDSv7. NJR Connect - Data services launched, single reporting platform, now providing dynamic customisable reporting of NJR metrics across a range of stakeholders. NJR Scanning Tool introduced to reduce the risk of ‘never events’ eg. wrong side of body implanted. Use of NJR data in surgeon appraisal is recommended by the British Orthopaedic Association (BOA). Implementation of new NJR economic model to reduce, through subscription, the overall cost burden to the NHS. This included sharing operational costs appropriately with implant suppliers through subscription to NJR services. NJR committee structure strengthens with the introduction of the NJR Executive Committee (NJREC) and Medical Advisory Committee (MAC). Development of the NJR Accountability and Transparency Model. Model provided a robust system for monitoring surgeon, unit and implant performance, linking to surgeon appraisal and revalidation. Working with NHSE/I, GIRFT, CQC and BOA this provided a multi-agency approach to performance management, with the NJR leading the way in this area for other audits to replicate. NJR Supplier Feedback, a world first, secure website launched supporting manufacturers in the monitoring of their own implant products. We also saw the first implant withdrawn from the market as a result of NJR outlier notifications. NJR data links with ‘Best Practice Tariff’ hospital payment uplift in England which increased compliance, driving up the completeness of the NJR dataset. Collection of ankle replacement procedures commenced, supported by the British Orthopaedic Foot and Ankle Society (BOFAS) and NJR MDSv4 form was released. NJR Implant Performance Committee reports concerns of early failure rates for metal-on-metal hip replacements to regulatory body MHRA; many related implants are subsequently withdrawn from the market. NJR Fellowship establishes to enable supported research into joint replacement using NJR data. NJR ReportsOnline commences and provides surgeons and hospitals with information about operations, patient characteristics and implant use. NJR Centre website launched and makes relevant information about the registry and joint replacement available. NJR StatsOnline website launched for public viewing and downloading numbers of procedures. NJR established as the Data Collector for joint replacement procedures in England and Wales. NJR Clinician Feedback website launched and provides individual surgeons with the tools they need to carefully examine their activity and outcomes, to refine clinical choices and improve safety and efficacy for patients. Introduction of enhanced NJR data collection with the new MDSv3. 2011 data submission to the registry becomes mandatory in the NHS under the NHS Acute Services Contract. NJR Public and Patient Guide first published, collaboration with patients to translate NJR data into patient-friendly information. NJR Management Feedback platform commences to support hospital executives in monitoring the activity and outcomes of their hospitals. The Patient Decision Support Tool is launched, enabling patients to see what their outcomes are likely to be regarding their risk and benefit for hip and knee surgery and empower shared decision-making discussion with their consultants. NJR extends its scope to the Channel Islands to include Guernsey. First Medical Director and Vice Chair appointed which enables valuable clinical expertise within the registry. The NJR extends its scope to include data collection in Northern Ireland. NJR celebrates its first decade with its 10th anniversary. Consultant surgeon-level information published annually to support patient choices, in partnership with the BOA, specialist surgical societies, HQIP and NHSE. The NJR extends its scope to include the Isle of Man. Data collection is extended with the introduction of MDSv6. One million procedure records now collected. Two million procedure records now collected. Three million procedure records now collected. NJR starts recording hip and knee replacement procedures with our new minimum data set collection form MDSv1 and data entry portal. For the first time, there is a central national collection of joint replacement devices, ensuring that patients can be swiftly identified in the event of a problem. Entering procedure data to the registry is mandatory for independent hospitals. NJR Data quality audit is introduced to identify and capture missed procedures and the NJR is now able to report completeness rates of over 97%. A total of 3,764 000 procedures have now been collected. Adoption of the NJR’s hip and knee component classification by the International Prosthesis Library, enabling unified global classification and reporting. Rollout of targeted elbow volumes data quality audit, partnering with the British Orthopaedic Trainees Association (BOTA) almost doubling registry elbow volumes; enhancing completeness and accuracy of elbow data. 2004 First development of the outlier monitoring process to Identify any problems and support improvement, for implants, hospitals and surgeons. MDSv2 is released to increase the amount of information collected. Wenlock
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 21
Figure 1: NJR Development Milestones

Deirdra Taylor is Associate Director for Communication and Stakeholder Engagement with the NJR. She is a member of the NJR Editorial Committee, supporting the content development and publication of the NJR’s Annual Report.

Mark Wilkinson is Professor of Orthopaedics at the University of Sheffield and an Honorary Consultant Orthopaedic Surgeon at Sheffield Teaching Hospitals. He is Chair of the Research Committee at the NJR.

A comprehensive analysis is undertaken twice a year of the performance of all implants entered into the registry. This analysis identifies all implants that are performing at a level that is ‘worse than expected’ compared to other implants within their class. This analysis is shared with both implant manufacturers and the MHRA. To date, this process has identified 28 hip implants, 36 hip constructs (combinations of stems and cups) and 19 different knee implants with potentially significantly worse outcomes. The MHRA and manufacturers work together to address this performance and, if necessary, implants are withdrawn from the market (and/ or field safety notices issued). More than 50 implants or constructs identified through this mechanism are no longer implanted in the UK.
NJR data is also provided routinely to the Care Quality Commission to support their key quality indicators present in inspection packs used for all CQC inspections. NJR data is also part of the data that underpins the GIRFT and The Model Health System initiatives to support quality improvement alongside value for money, (https://gettingitrightfirsttime.co.uk/wp-content/ uploads/2020/02/GIRFT-orthopaedics-followup-report-February-2020.pdf)
The risks and benefits associated with join replacement also vary according to patient demographics such as age, gender, and comorbidity profile. NJR data on surgery in the obese versus non-obese patient have directly informed current NICE guidance for the treatment of patients with osteoarthritis, published in October 2022 (www.nice.org.uk/ guidance/ng226). NJR data have also contributed
to recent NICE guidance on joint replacement of the hip, knee and shoulder, published in June 2020 (www.nice.org.uk/guidance/ng157), including outcomes data for knee replacement in which the patella is resurfaced versus when it is not, and on the patterns of use of anatomic versus reverse anatomic shoulder designs.
During 2021-2022, the NJR Data Quality Committee oversaw a large and detailed exercise to identify missing elbow data and source check for mismatched data. The project was conducted in collaboration with the British Orthopaedic Trainees Association, the British Elbow and Shoulder Society, Royal College of Surgeons of England and the British Orthopaedic Association. The NJR already represented the largest elbow series in the world, but as a result of the audit there was a significant increase, almost doubling the numbers of elbows available for analysis in the NJR annual report. These new data are mainly radial head replacements but also include previously ‘missing’ total elbow replacements. These data, together with regular NJR data provided to the British Association of Surgery of the Knee and to the British Hip Society, support national policy work that examines the distribution of services, including the provision for joint procedure revision hub and bespoke services in England.
Benefits to broader society, including research and innovation
Data sharing
The NJR encourages use of the registry dataset for research, to add value to our knowledge about joint replacement practice, clinical performance, cost-effectiveness and patient safety. Researchers use the data to analyse questions about outcomes in relation to particular underlying disease and patient co-morbidity, as well as address clinical and cost-effectiveness outcomes related to the implant prosthesis used. The NJR dataset provides an unparalleled opportunity for research into the clinical epidemiology of joint disease, the epidemiology of its treatment and their associated outcomes. The NJR supports research through our rolling portfolio of internal priority analyses, and by providing access to the dataset to independent research groups through our published access mechanism. This research generates new knowledge to support and improve practice and supports patients and the wider public through public-facing web pages and other outputs to increase broader awareness of research developments. To date, the NJR has released data to 40 external research teams to support 68 projects resulting in 78 scientific papers, independent of NJR. Details of these and other research publications using NJR data can be found at www.njrcentre.org.uk/research/njr-researchpublications-and-outputs
Features
22 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Figure 2: The Independent Medicines and Medical Devices Safety Review report (www.immdsreview.org.uk/Report.html).

Developing the next generation of registry data researchers
Analysis of registry data requires specialist expertise, including methods to clean and order data, to optimise data linkage and advanced statistical methods of analysis. We have led the way in developing and sharing these statistical methodologies and this practice keeps the NJR at the cutting edge in the field of data science. Our flagship NJR Clinical Research Fellowship, delivered in partnership with the Royal College of Surgeons of England, has funded PhD and MD studentships for 12 orthopaedic trainees since its inception in 2012.
Their topics of study cover all of the joints that are recorded in the NJR and include both elective care and trauma. The NJR has also funded two non-clinical PhD studentships and is currently in the appointment process for a third. More recently, we have cofunded a clinical research fellowship with Orthopaedic Research UK, with a second award round currently underway. In 2023, the NJR collaborated with the BOA to provide mentorship support for two sustainable surgery fellows as part of Deborah Eastwood’s presidential initiative in this area.
Broader research citizenship
We make the NJR dataset available to independent researchers through the Data Access Portal, enabling both commercial and non-commercial organisations access to the data for public benefit. The NJR is currently partnering with Health Data Research UK to map the NJR dataset to the Observational Medical Outcomes Partnership Common Data Model, an open community data standard,
Endoprothesenregister Deutschland (German Arthroplasty Register) and the International Society for Arthroplasty Registries (ISAR). ISAR is a worldwide collaboration that supports best practice in joint replacement surgery and its outcomes (www.isarhome.org/ home). The NJR is also a key collaborator with the Organisation for Economic Development on their Patient-Reported Indicator Surveys (www.oecd.org/health/paris).
“Over the 20 years since the inception of the NJR, we have provided patients, surgeons, hospitals, medical device manufacturers, service commissioners, regulators, policymakers, and broader society with a robust and continuously updated and audited highresolution picture of joint replacement care.”
designed to standardise the structure and content of observational data and to enable efficient analyses that can produce reliable evidence. This mapping will facilitate access of the NJR dataset through the European Health Data Evidence Network (EHDEN). In a further international community initiative, the NJR is a leading member of the International Classification System for arthroplasty components, in collaboration with the
Summary
Over the 20 years since the inception of the NJR, we have provided patients, surgeons, hospitals, medical device manufacturers, service commissioners, regulators, policymakers, and broader society with a robust and continuously updated and audited high-resolution picture of joint replacement care (in both the public and private sectors) within the geographical territories we cover. Changes to the way in which medical device outcomes are monitored are currently underway in the UK and the NJR stands ready to continue to play a core role in working for patients to maintain the safety and efficacy of joint replacement services over the next 20 years. n
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 23
Features

Richard Field was appointed as a Consultant Orthopaedic Surgeon at St Helier Hospital, Surrey in 1994 and moved to SWLEOC in 2004. He is the UK’s most experienced surgeon in anterior (DAA) hip replacement.
He was SWLEOC’s Director of Research from 2004-2021. He is a Professor of Orthopaedic Surgery at St George’s University of London. His work at SWLEOC has focused on the development of the centre’s outcome database, leading on the GIRFT and SWLEOC Elective Hub Toolkit for new elective hubs, the development and clinical evaluation of new implants, the development of hip arthroscopy and anterior hip replacement.

Irrum Afzal is Research and Outcomes Manager at SWLEOC. Irrum graduated from Imperial College London securing a distinction in Masters of Public Health and has completed a Postgraduate Diploma in Sustainability Studies. She played a leading role in the development of the GIRFT and SWLEOC Elective Hub Toolkit under the supervision of Professor Field working with NHSE and GIRFT. She is the National Orthopaedic Alliance 2023 Director’s Award Winner. Irrum is the Co-Director of the London Research Course, a professional member of the Health Research Authority Research Ethics Committee and is Equality, Diversity and Inclusivity Lead for BOSTAA.
SWLEOC and GIRFT Elective Hub Toolkit –A guide for setting up an efficient elective surgical hub
Richard E Field, Irrum Afzal, Boudine Pearce and Polly Hyde
In 2000, the United Kingdom government initiated a major investment programme in the National Health Service (NHS)1. This was a timely intervention as waiting lists for elective surgery had grown steadily over the preceding decades. The average wait for NHS hip and knee replacement surgery peaked, in 2001, at over 35 and 41 weeks respectively2 By April 2016, the 2000 initiatives had reduced the average time from referral to treatment (RTT) for elective trauma and orthopaedic care to seven weeks with 88.1% of patients receiving their treatment within 18 weeks3. However, by April 2022, the average wait had doubled and the number of patients receiving treatment within 18 weeks had fallen to 54.1%4
In August 2022, the Secretary of State for Health, announced £1.5 billion of government funding to establish 50 new surgical hubs. This funding is intended to provide 100 new operating theatres, over 1,000 new beds and two million extra elective operations over three years. The plan seeks to provide over 200,000 extra procedures in 2022 to 2023, over 700,000 extra procedures in 2023 to 2024, and one million extra procedures in 2024 to 20254. The beds will be ring-fenced for planned operations, reducing the risk of short-notice cancellations4 and, if successful, the new hubs will help reduce waiting times and provide patients access to life-changing
operations. All surgical hubs should ensure that training opportunities are provided for all staff members. These hubs will be essential platforms for trainees to gain experience, operate and develop the required competencies to ensure there is strong and sustainable trauma and orthopaedic workforce. It is also important to ensure there is a stream of fully trained Certificate of Completion of Training (CCT) surgeons who are able to continue to deliver to the standards required in surgical hubs5
The South West London Elective Orthopaedic Centre (SWLEOC), a partnership of four Trusts, is an NHS Treatment Centre that opened in January 2004. SWLEOC was established as a partnership between Croydon University Hospital NHS Trust, Epsom and St Helier University Hospitals NHS Trust, Kingston Hospital NHS Foundation Trust and St George’s University Hospital NHS Foundation Trust. The centre is located on the Epsom General Hospital campus, as a stand-alone, ring-fenced, unit. SWLEOC opened with four operating theatres and a target of 2,200 hip and knee replacement operations during its first 12 months. Over the last two decades, the centre has opened two additional operating theatres and now completes over 5,000 elective orthopaedic operations each year, with over 3,500 being hip and knee replacements. The increased activity has been achieved with no additional beds.
Features
24 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk

Boudine Pearce undertook her undergraduate studies in South Africa, qualifying as a Physiotherapist in 2003. She specialised in MSK and Orthopaedic conditions including completing a postgraduate Masters Degree in Sports Physiotherapy. She is an Advanced Practice Physiotherapist in Primary and Secondary care and is currently working as a strategic lead at the South West London Elective Orthopaedic Centre. She has worked with NHSE, GIRFT and a core team to develop an online toolkit of effective hub care delivery. She is currently working with NHS England/GIRFT, contributing her expertise as a member of the Hub Accreditation Advisory Group.

Polly Hyde is a Content Development Lead for the Getting it Right First Time (GIRFT) Academy (part of the GIRFT programme within NHS England). Her role supports clinical leaders in the development of best practice content. Prior to GIRFT she has worked as an Associate Lecturer at the University of Lincoln alongside her role as Head of Strategy at United Lincolnshire Hospitals NHS Trust, giving her insight into change implementation in the elective and acute care settings.

In the first year of operation, SWLEOC failed to achieve its caseload and financial targets. The centre incurred a financial loss of £2M. By the end of the second year, resolution of operational bottlenecks enabled the centre to fulfil its caseload targets and the centre achieved consistent financial profits until the COVID-19 pandemic necessitated a temporary reintroduction of block contract funding. Bringing multiple hospital teams to a single site necessitated the development of new strategies to schedule, process and operate on patients. It took the SWLEOC team two years to develop the processes and pathways needed to achieve its targets and similar challenges will face the new generation of surgical hubs that are opening around the country.
The SWLEOC-GIRFT (Getting It Right First Time) elective hub toolkit has been developed by the GIRFT academy and SWLEOC staff to provide a detailed,
comprehensive and easily accessible resource that can be accessed by new surgical hubs and high volume elective surgical providers.
The toolkit is provided on-line at https://girfthubtoolkit.org.uk. The resource is structured as a website that allows visitors to explore the Patient Pathways, Staff and Services, Administration, physical layout (Estate) and access the diverse documents (Appendices) that have been developed to support every aspect of the centre’s operation.
The section on ‘Patient Pathways’ is subdivided into pre-admission, in-patient and post-discharge phases and provides step-bystep guidance on the patient journey from referral to the centre through in-patient care to post-discharge follow-up and support in the community. For each topic, the visitor can download documentation, such as referral proformas, that can be adapted for use in the new hub centres. >>

Features
Figure 1: Homepage of the SWLEOC and GIRFT Elective Hub Toolkit
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 25
Figure 2: Example of the Patient Pathway page on the Toolkit website
Features
The section on ‘Staff and Services’ explains the roles of the 24 teams involved in the centre’s work and provides detailed information on the composition of each team, what they do, the challenges they have faced, how they solved operational bottlenecks, where they work, the resources they use and how they interact with other staff groups.
The section on ‘Administration’ provides information on the financial arrangements that enable the centre to run profitably within NHS tariff funding. The governance programme that has been developed, the partnerships that exist with the host Trusts, suppliers and other organisations, the meetings that take place and the sustainability programme that has been developed. In the section on meetings, the visitor is able to drill down to explore the different meetings undertaken by the clinical and administrative teams and for each meeting, download templates for the specific meeting agendas and minutes.
The section on SWLEOC’s ‘Estate’ provides information on how the centre provides a stand-alone facility on a general hospital campus and allows the visitor to access and download detailed floorplans of the out-patients, pre-theatre area, equipment storage facilities, operating theatres, postanaesthetic care unit (PACU) and wards.

The final ‘Appendices’ section provides access to the range of documents that have been developed by the SWLEOC team over two decades. More than 100 Standard Operating Procedures (SOPs) can be viewed and downloaded. Likewise, consent forms that have been tailored to a spectrum of orthopaedic procedures and all the templates for the letters that are used for communication with patients and other healthcare providers. The Appendices section also provides access to the letters and questionnaires that have been developed to create and support the centre’s unique PROMS database on the outcomes of over 60,000, hip, knee and shoulder replacement operations. The Appendices section details the Service Level Agreements (SLE’s) that have been put in place with host Trusts and other service providers and provides details of the publications and achievements of the centre.
The SWLEOC-GIRFT Elective Hub toolkit plays a pivotal role in promoting sustainability within the expansion of surgical hubs. Having all the documentation in one place on
https://girft-hubtoolkit.org.uk/elective-hubtoolkit not only ensures systematic resource utilisation but also streamlines organisation and accessibility, contributing to a more eco-friendly and efficient workflow. The toolkit enables individuals and teams to access all the information about the SWLEOC surgical hub without the need to visit in person. This not only saves time but also reduces the carbon footprint. The resource enables users to access and download thousands of pages of information.
This extensive resource will assist NHS colleagues to set up and run the new generation of surgical hubs. The toolkit will enable new hub centres to undertake gap analysis to identify where they need to refine their infrastructure, processes and documentation. It is hoped that this will minimise the time it takes hubs to achieve operational targets and Get It Right First Time.
The SWLEOC-GIRFT elective hub toolkit went live on the NHS England GIRFT website in May 2023 and it has more than 7,400 visits from over 3,200 unique visitors. It has also won two awards for Partnership and Integration Initiative and Innovation in Orthopaedics at the 2023 National Orthopaedic Alliance Excellence in Orthopaedics Awards. n
References
1. NHS England. The NHS Plan. Available at: www.bsuh.nhs.uk/library/wp-content/ uploads/sites/8/2020/09/The-NHSplan-2000.pdf
2. Cooper ZN, McGuire A, Jones S, Grand JL. Equity, waiting times, and NHS reforms: retrospective study. BMJ. 2009;339:b3264
3. NHS England. Consultant-led Referral to Treatment Waiting Times Data 201819. Available at: www.england.nhs.uk/ statistics/statistical-work-areas/rtt-waitingtimes/rtt-data-2018-19/#Apr18
4. GOV.UK. Over 50 new surgical hubs set to open across England to help bust the COVID-19 backlogs. Available at: www.gov.uk/government/news/over-50new-surgical-hubs-set-to-open-acrossengland-to-help-bust-the-covid-backlogs
5. NHS England. Establishing an effective and resilient workforce for elective surgical hubs. Available at: www.gettingitrightfirsttime.co.uk/wpcontent/uploads/2022/08/Workforceguidance-for-surgical-hubs-Aug22h.pdf
26 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk

















Ricci Plastow is a Trauma and Orthopaedic Consultant surgeon at UCLH, London. He is the trainee lead for the Robotic and Digital Assisted (RADAR) Working Group within RCSEngland, aiming to introduce and enhance this technology within orthopaedic surgery in the NHS.

Andreas Fontalis is an ST4 Specialist Registrar on the Percivall Pott Rotation in London and a PhD candidate at the Division of Surgery and Interventional Science, University College London. During his academic journey, he has been presented with several awards, including the Freemasons’ Royal Arch Fellowship, supported by the Arthritis Research Trust, the Onassis Foundation Scholarship and has had a previous tenure as an NIHR Academic Clinical Fellow.
The development of new robotic MSK surgical services within the NHS
Ricci Plastow, Andreas Fontalis, Nick Ohly and Fares S Haddad on behalf of the Robotic And Digital Assisted suRgery (RADAR) Advisory Group
The use of robotic-assisted surgery in T&O is growing across the UK with multiple centres putting forward business cases to develop robotic surgical programmes. Emerging evidence suggests this technology improves surgical precision and clinical outcomes.
There is also literature concerning the general implementation of robotics into the healthcare system, highlighting issues that need to be addressed, such as governance of new technology, surgical training, equity of access and public perception1,2. This article summarises the evidence to support the introduction of roboticassisted MSK surgery and provides guidance on how to implement this new technology.
The Royal College of Surgeons of England (RCSEng) has established the Robotic And Digital Assisted suRgery (RADAR) advisory group to consider the benefits and issues around the implementation of robotic-assisted surgery in the UK. The BOA along with RADAR have recently developed a guidance document for centres looking to develop MSK robotic-assisted surgery, which is available on the BOA website at www.boa.ac.uk/robotics
Evidence for MSK robotic surgery
There is a growing body of evidence, showing improved implant positioning, revision rates, length of stay and PROMS, which can support a business case for CT planning and robotic-arm assisted surgery within the NHS.
Improved implant positioning precision and restoration of native joint mechanics
Domb et al. reported 100% accuracy in positioning the acetabular cup within the Lewinnek’s safe zone when robotic-arm assistance was employed, as seen in figure 1. Only 80% were placed within the safe zone in conventional manual total hip arthroplasty (CO THAs) from a sample of 100 patients3. Illgen et al. reviewed outcomes of 300 THAs and highlighted a 71% enhancement in acetabular implant positioning accuracy with robotic-arm assisted total knee arthroplasty (RO THA)4. Moreover, other studies have consistently demonstrated the superiority of robotic-arm assistance in restoring the centre of rotation and native hip joint mechanics, over the conventional technique5-7
Existing literature suggests that RO TKA and UKA outperform conventional jig-based techniques with respect to precision of implant positioning and limb alignment8-11. Studies conducted by Bellemans12, Hampp13, Kayani14 and Moon15 highlight the superior accuracy of RO TKA, not only in achieving the planned component positions, but also in maintaining limb alignment and restoring critical metrics such as the joint line, posterior condylar offset and Insall-Salvati ratio.
Shorter length of stay (LOS) and higher percentage of home discharges
Existing literature indicates a trend toward shorter LOS with RO THA and RO TKA and a
Features
28 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk

Nick Ohly completed postgraduate training in Edinburgh, followed by a fellowship in Adult Reconstruction at the University of British Columbia in Vancouver. He was appointed as a consultant at the Golden Jubilee National Hospital in 2014. His practice is focused exclusively on hip and knee arthroplasty, with subspecialist interests in robotic and computer-assisted surgery, and complex and revision knee arthroplasty.

Fares Haddad is Professor of Orthopaedic and Sports Surgery and Divisional Clinical Director of Surgical Specialties at UCLH, and Director of the Institute of Sport, Exercise and Health (ISEH) at University College London. He is Medical Director of Orthopaedics, HCA UK and the Editor in Chief of the Bone and Joint Journal.

higher percentage of home discharges with RO TKA. Caldora et al. in a retrospective analysis of 1,537 uncemented THA patients, revealed a substantial LOS reduction of nearly four days with robotic-arm assistance compared to conventional methods (mean LOS: 4.24 ± 2.04 days vs. 8.04 ± 2.84 days, p<0.01). Notably, there was also a marked decrease in post-operative transfusion rates in the RO THA group at 2.0%, versus 11.2% in the conventional cohort16.
With respect to TKA, Archer et al’s retrospective analysis of 10,296 TKAs revealed a shorter average LOS in the robotic cohort (1.68 ± 0.86 days) compared to the conventional technique (1.86 ± 0.94 days, p<0.00001)17. Other studies have also reported shorter LOS with robotic
assistance18-21, higher percentage of home discharges and lower rate of discharges to rehabilitation facilities17,18,22
Dislocation
Big data suggest a potential correlation between enhanced radiological precision and decreased dislocation rates23-26. A recent study highlighted a low dislocation rate of 0.35% when utilising either computer navigation or robotics in THA24. Another large-scale study encompassing 13,802 primary THAs reported a diminished risk of revision due to dislocation (odds ratio of 0.3, P=0.046)25. Figure 2 highlights the useful function of virtual range of motion in the THA pre-operative plan to assess for bone or implant impingement increasing the risk of dislocation. >>
 Figure 1: Image from a pre-operative robotic THA plan allowing acetabular cup positioning.
Figure 2: Pre-operative RO THA plan showing virtual range of motion with the hip flexed and internally rotated to assess for posterior dislocation.
Figure 1: Image from a pre-operative robotic THA plan allowing acetabular cup positioning.
Figure 2: Pre-operative RO THA plan showing virtual range of motion with the hip flexed and internally rotated to assess for posterior dislocation.
Features
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 29
Features


Survivorship
Batallier et al. studied the survivorship of 80 CO UKAs versus 80 RO UKAs, revealing a lower revision rate for the robotic technique (5% vs 9%). Authors noted that 86% of the CO UKA revisions were due to component misplacement compared to zero in the robotic group27
Further systematic reviews and prospective cohort studies have corroborated the excellent survivorship of RO UKA; reporting a 97% revision-free survivorship at six years28,29
Reduced soft tissue injury
Recent randomised controlled trials have shown that RO TKA is associated with a reduced local and systemic inflammatory response30,31. In a cadaveric study, Khlopas et al. also substantiated the above findings by revealing that RO TKA led to fewer injuries such as PCL damage and tibial subluxation compared to CO TKA32
Improved balancing, functional and patient reported outcomes
This enhanced technology enables personalised alignment philosophies, such as functional and kinematic alignment, which have been associated with improved soft tissue balancing and outcomes33-36,39. Marchand et al. reported improvement in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score with RO TKA over a two-year period38. There are several RO UKA studies using pre and intra-operative planning software, as seen in figure 5, improving implant positioning and patient reported outcomes in similar fashion to the THA and TKA studies above41-43 Figures 3 and 4 highlight the intra-operative robotic TKA workflow where balancing of soft tissues gaps can be achieved before bony cuts are made.
Several studies highlighted in table 1 show improved or equivalent PROMS in RO THA when compared with the conventional technique. One caveat is that the majority of these studies are based on CT image based planning and one robotic-arm system. Other systems will need to be evaluated in a similar fashion.
Practical guide to setting up a MSK robotic-assisted surgery programme
As with the introduction of any new surgical procedure, patient safety is paramount. It is essential that individual hospitals have robust local protocols to enable the safe adoption of robotic-assisted surgery.
We recommend creating an MSK robotics peer review group to develop a robotics business case, with due regard to hospital clinical governance and risk policies. The group should include senior representation from clinical and non-clinical staff as summarised in the RADAR RCSEng / BOA / RCSEd document.
Consideration should also be given to developing a standard operating procedure and necessary training for all users. The robotic vendor should organise cadaveric laboratory training for any surgeons wishing to use their technology. Tips and troubleshooting in the early phase of introducing robotic technology
is best undertaken outside a ‘live’ theatre setting. It is recommended that surgeons with experience in computer navigation and/or robotic surgery are involved initially, as there is evidence that this results in flattening of the learning curve50. Industry support should be readily available and is mandatory for some robotic systems.
Theatre staff will need training on how to set up the robot, the procedural workflow and consumables needed. Training days for all scrub staff should be organised and simulation of the procedure carried out. Clear communication with robotic vendor specialists and team working is needed to allow efficient surgical workflow.
The introduction of any new technology mandates a comprehensive understanding of the risks involved and troubleshooting strategies to prevent potential errors. The learning curve in robotic-assisted arthroplasty is not associated with achieving the desired accuracy10,14,50 but rather acquiring procedural competency and
 Figure 3: Pre-operative planning of robotic TKA.
Figure 4: Intra-operative soft tissue balancing of TKA.
Figure 5: Intra-operative UKA planning and balancing of soft tissues.
Figure 3: Pre-operative planning of robotic TKA.
Figure 4: Intra-operative soft tissue balancing of TKA.
Figure 5: Intra-operative UKA planning and balancing of soft tissues.
30 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
familiarity with the new equipment and technology, streamlining the operation and improving surgical confidence. The literature shows that a low volume of cases are needed to become proficient. It is therefore important for the surgical team to be proficient with the surgical procedure prior to commencing robotic surgery. Furthermore, troubleshooting and recovery workflows should be in place and can be developed collaboratively with the industry representatives. Safety protocols should also be in place for robotic equipment failure and steps to be taken in the event of such failure to protect patient safety. Any adverse event or incident should undergo root cause analysis in accordance with local governance procedures.
The surgical team should plan straightforward cases initially, to take pressure off the list and give the best chance of successful case completion in a timely fashion. It should be possible to introduce robotic cases without losing productivity, i.e. still maintaining a four-joint list, if this is routine with conventional cases. This should form part of the structured development plan for the robotic surgical teams with the recognition that the initial training and implementation phase may entail additional time and costs.
In order to maintain good clinical outcomes, surgeons and hospitals will need to maintain an adequate volume of robotic-assisted cases annually with audit of activity and outcomes. The National Joint Registry dataset does not collect sufficient outcome data for safe governance of new robotic systems and additional prospective data collection is recommended. It may be helpful to set targets for minimum use of the robotic system (at surgeon and department level) to ensure optimal use and progress through the learning curve.
Robotic systems vary in the data that underlies their safety and clinical effectiveness. Recent work has looked at how best to record the effect robotic technology will have on NHS practice. The consensus meeting for the UK RoboCOS study51 led to the agreement of a 10-item core outcome set, which may be a helpful framework for data collection. This includes four main areas (patient level,
Study design, author and year
Clement et al.43 2020
Prospective cohort study - Propensity Score- Matched
Domb et al.44 2020
Retrospective review of prospectively collected data - Propensity Score- Matched
Han et al.45 2019
Systematic review and meta-analysis
Samuel et al.46 2021
Systematic review and meta-analysis
Shaw et al.47 2022
Retrospective cohort study
Karunaratne et al.48 2019 Systematic review and meta-analysis
Ng et al.26 2021 Systematic review and meta-analysis
Fontalis et al.49 2023 Prospective cohort study
Table 1.
Sample size
120 patients (RO THA 40 patients, CO THA 80 patients)
217 patients; 66 patients matched into each cohort
Outcomes Results
PROMs, leg length, implant positioning, patient satisfaction
PROMs, revisions, cup orientation
14 studies included Functional, radiological outcomes, PROMs and complication rates
18 included studies PROMs, dislocation, complications and revisions between RO THA (MAKO and ROBODOC) and CO THA
2247 patients (1724 CO THA vs 523 RO THA)
PROMs, complication rates
14 studies PROMs (fully active and semi-active RO TAH) vs CO THA
17 studies included Learning curve, implant positioning, survivorship, functional outcomes, PROMs (semi-active RO THA vs CO THA)
RO THA, N=50 vs CO THA, N=50
“As with the introduction of any new surgical procedure, patient safety is paramount. It is essential that individual hospitals have robust local protocols to enable the safe adoption of robotic-assisted surgery.”
PROMs at 3 years post-operatively
surgeon level, organisation and population). This core dataset is recommended for all robotic procedures, but is particularly important for new, emerging or unproven technologies. These principles have been established in the IDEAL consensus and the introduction of new technologies such as new robotic systems need to be underwritten by robust clinical data collection52. With the ever-growing number of vendors and robotic devices in contemporary orthopaedic practice, it is vital to ensure high-quality evidence is generated for each system individually.
RO THA: Statistically significant improvement in OHS score of 2.5 95% CI 0.1-4.8 p=0.038
RO THA: 97.5% of patients had components within Lewinnek and Callanan’s safe zone
RO THA: improved PROMs (HHS FJS-12, VR-12 Physical, SR-12) compared to CO THA
Improved implant accuracy within Lewinnek with RO THA vs. CO THA (97% and 73.8% respectively)
WOMAC, HHS and Merle D’Aubigne Hip Score: no statistical difference
RO THA: improved accuracy (within Lewinnek’s safe zone)
CO THA: less dislocations
No significant difference in HHS, FJS, SF scores, Merle D’Aubigne
RO THA: statistically significant improvement in WOMAC
No difference in revision rates
No difference in dislocation rates
Statistical difference only when comparing ROBODOC vs CO THA
No difference in PROMs (PROMIS-GH, PROMIS-MH, PROMIS-PH and HOOS, JR), RO THA: less than one-fourth dislocation rate.
No significant difference in PROMs
Significant improvement in implant accuracy with RO THA and CO THA (77%-100% vs 30% - 82%)
RO THA: Statistically significant improvement in HHS
No statistically significant difference in Oxford hip score, Forgotten Joint Score and University of California at Los Angeles hip score
We recommend recording prospective data from the robot and signing up to available studies.
In summary:
• There is a growing body of evidence detailed in this article showing improved precision and clinical outcomes with robotic arthroplasty surgery.
• The Royal College of Surgeons RADAR group have created a best guide to set up robotic surgery practice, which is available at www.boa.ac.uk/robotics
• It is essential to create a robotic working group to set up, record data outcomes and review the effect of this technology within the NHS. n
References
References can be found online at www.boa.ac.uk/publications/JTO
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 31
Features
Robotic surgery in orthopaedics: What does the future hold?
Edward T Davis
and
Fares S
Haddad on behalf of the Robotic And Digital Assisted suRgery (RADAR) Advisory Group

Edward Davis is a hip and knee arthroplasty consultant at the Royal Orthopaedic Hospital in Birmingham where he is the clinical lead for the arthroplasty department. He is an Honorary Professor at the University of Birmingham and is the orthopaedic curriculum lead at the University of Birmingham and Aston University. He is the Head of the undergraduate academy at the Royal Orthopaedic Hospital.
Interest in robotic assisted surgery in orthopaedics is rapidly increasing with the development of new systems and a generation of evidence on its safety and efficacy. The main applications have been in hip and knee arthroplasty1–3, with increasing interest in its usage in spinal surgery4,5. Robotic systems have been available since the 1990s but were slow to gain acceptance. The true definition of a robot is a “programmed actuated mechanism with a degree of autonomy to perform locomotion, manipulation or positioning”; the definition of autonomy being the “ability to perform intended tasks based on current state and sensing, without human intervention” (ISO standard 8373:2021)6. Therefore, many of the systems in current use do not fulfil the true definition of a robot and are referred to as robotically assisted surgical devices (RAS) by the FDA7. These devices form part of the wider group that are categorised as computer assisted surgical systems that can be used for pre-operative planning, surgical navigation and assisting surgical procedures.
One of the first orthopaedic robots was the ROBODOC system (Curexo Technology, Fremont, CA, USA), which was a fully autonomous device with the surgeon able to plan the bone preparation and the robot executing this without any active input from the surgeon. The CASPAR robot (Ortho- Maquet/URS, Schwerin, Germany) was also available at a similar time performing in a similar autonomous manner to that of the ROBODOC. These early systems were probably slow to
gain widespread adoption, due to the complexities of use and the inability of the robot to distinguish bone from soft tissue. Concerns over the fully autonomous nature of these robots led to the advent of robotic assisted surgery and the development of the ACROBOT (Acrobot Ltd, London, UK) and the RIO Robotic Arm Interactive Orthopedic System (MAKO Surgical Corp., Lauderdale, FL, USA). The number of surgical robots now available for hip and knee arthroplasty has rapidly expanded.
These different systems provide different functionalities in hip and knee arthroplasty. Some provide an active robotic device that positions a cutting guide in the correct orientation, to then allow the surgeon to make the bone cuts using a standard surgical saw, whilst other systems may provide a cutting burr in a small handheld device that has the ability to retract when it is not positioned in an area that requires bone resection. Other devices, such as the MAKO and VELYS (Johnson and Johnson) hold the saw and guide the bone cuts. The different robotic assisted systems use pre-operative CT scans, pre-operative radiographs or use the acquisition of intra-operative anatomical landmarks to provide the three-dimensional plan that guides the bone resections. The levels of automation, active control, cutting tool integration, boundary or soft tissue protection and pre-operative imaging between the different systems, still need to be fully evaluated. The level of evidence for some systems is far greater than for others as summarised in the recent BOA / RCSEng / RCSEd documents, available on the BOA website at www.boa.ac.uk/robotics
Features
32 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk

Fares Haddad is Professor of Orthopaedic and Sports Surgery and Divisional Clinical Director of Surgical Specialties at UCLH, and Director of the Institute of Sport, Exercise and Health (ISEH) at University College London. He is Medical Director of Orthopaedics, HCA UK and the Editor in Chief of the Bone and Joint Journal.
The future of robotic assisted surgery hardware
There has been a recent revolution in the miniaturisation of many technologies, noticeably in mobile telephone capabilities. Within other areas of surgery there is currently a shift to smaller robotic devices, such as the use of natural orifice robotic devices that can undertake procedures within the body using natural orifices as the access point8 Within orthopaedics, the requirements to hold cutting guides or surgical tools with stability, has led to robotic assisted systems being large and cumbersome devices. As technology progresses, we anticipate these systems becoming smaller and more agile. The move away from traditional instruments to the use of burrs, lasers or piezotomes9,10 (such as in figure 1), may allow a reduction in size requirements for these devices with a transition to what can be termed smart instruments11. The miniaturisation of robotic assisted surgery may bring the added benefits of costs savings on the use of standard instrumentation and disposables12. The ability to use these technologies on revision knee replacement has been explored and has the potential to significantly reduce the need for mechanical instruments and guides thereby adding to cost and efficiency savings13
One of the main concerns of the fully autonomous robots was the protection of soft tissues. The addition of haptic or ‘hard stop’ boundaries during the bone preparation that is found within the CT Based Mako system (as seen in figure 2), and the imageless CORI system is an area that is certain to expand and may be one of the fundamental benefits of this type of technology14

Improvements in the ability of the systems to identify soft tissue so that they can be protected, is an important area and in time may allow us to revisit fully autonomous systems. Improvements in the development of intra-articular sensors that can be used particularly during knee replacement to measure soft tissue tensions and optimise ligament balancing, is variable between the different systems and is currently under investigation into how these data can be interpreted and acted on, to provide better outcomes.Again, the ability to miniaturise sensors is of benefit and these types of soft tissue balancers are a key area that will improve the use of robotic assisted surgery to optimise component orientation in a personalised way15,16 .
Most of the current robotically assisted surgery platforms rely on infrared trackers, which are fixed to the bone and require an infrared emitter and a camera to have direct line of sight. This often presents logistical problems of organising the operating staff and equipment but also in the added procedure of fixing the arrays to the bone17. Current developments are utilising the rapid expansion in the field of machine vision, to try to eliminate the requirement for fixed trackers placed in the bone and utilise optical cameras to identify the exposed bone surfaces18 This, combined with the improvements in miniaturisation of cameras, would eliminate the need to have a single fixed camera, opening up the possibility of using multiple cameras so that if one is obstructed then data can still be acquired. Ideally, the camera could be in a position to track the surgeon’s line of sight19 >>

Features
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 33
Figure 1: The robotic burr, example of a smaller 'smart tool'. Figure 2: Screen shot of the robotic system showing the boundary control protecting the soft tissue envelope during tibial resection.

Developments in augmented reality systems will also play a part in future developments, helping the surgeon visualise the anatomy and implant positioning during the planning stages20,21. Augmented reality headsets are now more ergonomic and will provide surgeons with data and information within the surgical field. However, there will need to be a careful balance between providing important and meaningful data at the appropriate time vs simply distracting and overloading the surgeon with information22 . There have been very significant advances in the field of virtual reality 23 , which simulates the operation to either enable surgeons to learn the procedure or for preperformance practise24, which is known to be beneficial when completing technical tasks. Robotically assisted surgical systems often disrupt the standard dynamics within an operating theatre with potential detrimental as well as beneficial effects on team working and the non-technical aspects of surgical procedures25. Virtual reality has the potential to help simulate these environments and to train staff and teams on the integration of technologies into the operating theatre environment.
Software and artificial intelligence/ machine learning
One of the most rapidly advancing fields is in the software for robotic assisted systems. This provides huge opportunities but also complexities in analysing the outcomes of different systems, especially when multiple versions have evolved since the system was first evaluated. The ability for precise tracking and the wealth of data that these systems collect is leading to a better understanding of optimising component orientation in knee replacement and will certainly expand to other areas of orthopaedics. The ability to track the surgical tools has been shown in other disciplines such as urology to even predict post-operative outcomes and discriminate on surgeon performance26 Many current systems still require significant human input from technicians in the segmentation and planning stages of robot assisted surgery, which is time consuming and costly. Many of these human contacts could be eliminated using analytics based on artificial intelligence (AI). Many systems still require complex surgical decision-making in interpreting data
provided by the robotic systems, leading to possible cognitive overload with the potential for component malpositioning or errors. AI systems and data analytics provide the benefit of being able to analyse previous data sets and provide optimised component orientation plans or provide prompts (nudges) to guide surgeons to the most appropriate position. Advanced analytics such as AI and machine learning can easily absorb and analyse these very large data sets; combining these with the electronic patient record produces a personalised plan based on validated data sets. AI and machine learning can already predict complications and outcomes following joint replacement27-29 and its integration into robotic systems will potentially enhance pathways and outcomes.
However, AI and machine learning bring concerns with data governance and data protection. Concerns on sharing anonymised large data sets, which may allow patient identification due to the granularity of the data will require changes in data protection law and possibly more punitive charges if individuals or organisations actively reidentify patients from anonymised datasets30
Features
34 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Figure 3: Personalising component orientation using the hip modeler showing impingement in activities of daily living.
The future of robotic assisted surgery workforce and education
One of the most controversial areas within the development of robotic assisted surgery in orthopaedics has been the implication on training and education31. Concern regarding the ability of trainees to gain access to robotic systems for training and more importantly for performing the surgery (rather than assisting) presents many challenges. Equality of access to these systems for both patients and trainees needs to be resolved32. During the adoption phases, trainees are often displaced while the consultant surgeon becomes proficient at using these systems and therefore not only access to robotic systems but access to robotic systems in centres with experienced users is required. As widespread adoption occurs, these issues will become less pertinent but in the transition phase, solutions will be needed. During the transition phase it will be important that training surgeons gain access to robotic systems but also that their training is balanced with an understanding how to use conventional instrumentation. As robotic systems become the standard of care then the necessity to use standard instrumentations will be less, but there will still be the requirement to understand how standard instrumentations work in the event of a technical failure.
be present throughout the surgery may reduce. This may allow the surgeon to be responsible for running multiple operating theatres with more reliance on allied health professions and technicians for certain elements of the procedure. This will enable the surgeons to be more focused on dealing with complex anatomy or scenarios where there may be ambiguity in the optimisation of component orientation or dealing with complications. This area brings with it huge controversy and will be difficult to navigate. Parallels with the acceptance of
technology and this will certainly dictate the pace of change depending on patient confidence in this technology. The accountability and liability if complications occur will also be a challenging area particularly as the technology takes on more decision-making functionality and as the systems progress to become more autonomous.
Research and evidence generation
“The development and adoption of robotic assisted surgery is intrinsically linked with big data and the requirements of sharing data across different providers and regions as well as between industry and the healthcare sector.”
fully autonomous cars and the presence of human pilots being required despite aircraft being more than capable of automated flight have shown that this area is highly controversial and often takes much longer to adopt even when technology is available to undertake the tasks.
The ability to demonstrate the safety and efficacy of these systems will be fundamental to the pace of adoption. Health economic research will also be critical with the increasing challenges that healthcare systems are put under in trying to reduce costs and improve care. Conducting research into rapidly evolving technologies has always been challenging particularly where software iterations are continually changing. Clinical studies and real world evidence will be important in the development and adoption of this technology with large randomised controlled trials already being conducted. One of the main challenges will be the classification of different systems and different software algorithms that may provide very different benefits and risks to patients.
Conclusion
Assisted technologies such as navigation and robotics have the potential to accelerate education in surgical specialties and improve the understanding of surgical techniques such as ligament balancing in knee replacements and component optimisation in both hip and knee replacement33, as figure 3 shows with a wealth of information to plan surgery. Future work will improve the training methodologies that are used to educate surgeons in robotic technologies. Different educational methodologies may be required. Within the field of robotically assisted prostatectomy, data taken from the robotic systems can help delineate the skill set of different surgeons34, who can then focus training needs on specific aspects of surgical performance.
Implications for surgical workforce planning may also be heavily influenced by the development and implementation of these technologies. Currently, all of the systems require significant surgeon involvement and surgical skill and therefore the surgeon must be present during the procedure. As the systems advance and move towards more intuitive designs encompassing decisionmaking, component position optimisation, soft tissue protection and automation, then the requirement for the surgeon to
The future of robotic assisted surgery legal and ethical implications
The development and adoption of robotic assisted surgery is intrinsically linked with big data and the requirements of sharing data across different providers and regions as well as between industry and the healthcare sector. The legal and ethical implications of this type of data sharing must be addressed and be transparent to patients35. Many of these issues are already being addressed in other sectors, such as within the automotive industry who are leading on the issues of privacy, as automated cars continually recording their surroundings. As discussed earlier, there may be a requirement to move forward with more punitive charges for individuals or companies who misuse big data in an effort to allow more open data sharing and a more rapid development of these systems. Concerns over the validity of AI algorithms on minority groups will need to be addressed and transparency on the training data sets used in the development of these algorithms will need to be robust.
Patients perception of robotic assisted surgery will also need to be more fully explored as we move to more automated
Robotic assisted surgery in orthopaedics is a rapidly evolving area and brings with it the hope of improving patients’ outcomes with particular focus on consistency and quality of surgical outcome. As systems evolve and develop it is vital that we maintain safety whilst also being cognisant of the health economic challenges that we face. Technology is rapidly evolving in all areas of our lives and will certainly be part of surgical practise in the future. It is vital that the adoption is undertaken supported by evidence-based medicine and addresses the potential changes in the way that we provide education and training in this area to both surgeons in training and established consultants. These systems potentially allow a more personalised approach to surgery and these factors need to be considered when looking at evidence generated on their efficacy. The current RACER trials and other level 1 studies will help inform and possibly dictate the pace of change with respect to hip and knee arthroplasty and are eagerly awaited14,36-38. n
References
References can be found online at www.boa.ac.uk/publications/JTO
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 35
Features
The British Orthopaedic Association British Casting Certificate (BCC) Development
Mark Rees

Mark Rees is the BOA National Casting Training Advisor and has been in post since 2020. Mark is a qualified Operating Department Practitioner (ODP), holds the British Casting Certificate (BCC) and has previously run the BOA validated BCC course within the military. Mark works closely with the British Orthopaedic Association Casting Committee (BOACC), overseeing the national course content to maintain the high levels of musculoskeletal casting and splinting education in the UK, validating the regional BCC courses, and overseeing the OSCE Examination process.
The British Casting Certificate (formerly known as the BOA/RCN (SOTN) AOT Casting Techniques Certificate) has been the only nationally recognised qualification in casting since 1982 for both orthopaedic practitioners and nurses whose role includes casting and splinting. Alongside the British Casting Certificate the BOA also runs courses for T&O Surgical trainees and tailored courses for A&E Casting.
In 2015 the BOA Casting Committee published a new version of the BOA Casting Standards which are available on the BOA website (www.boa.ac.uk/casting-standards). The standards align to evidence-based practice and how this then integrates into the delivery of best-in-class patient treatments and care pathways. They can be used as an audit tool
to review casting room practices and ensure that ALL practice meets the standards and best practice guidelines. This can also be used to help build CPD programmes for casting room personnel. The standards outline the importance of correct staffing levels, correct qualification levels, the activities carried out in the orthopaedic practitioner role, and the importance of the role in multi-disciplinary teams ensuring the delivery of optimum patient treatments and care.
The seven standards cover; qualifications of staff in a quality casting service, health and safety, communication & documentation, cast application, cast adaptation and removal, patient education, and information & personal professional development. As well as a section on audit there are also additional appendices covering; general principles of casting,

Features
36 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Stanmore BCC Casting Course.
Features
BOA BCC SYLLABUS FOR EXAMINATION
RELEVANT ELEMENTARY ANATOMY AND PHYSIOLOGY
LOCOMOTOR SYSTEM
• Basic knowledge of the skeleton: nomenclature & major joint movements.
• Details of bones and surface anatomy of the upper and lower limbs.
• The vertebral column, bony structures, normal curves, and intervertebral discs.
• Joints: basic details of the upper and lower limb joints.
• Muscular system: main groups of muscles moving the limbs.
• Nervous system: spinal cord in brief, positions of nerves relevant to casting work.
• Circulatory system: main blood vessels of the limbs.
TRAUMA
• Fractures: types, healing, and complications.
• Description, treatment, and any specific complications of trauma to:
o Wrist and hand
o Forearm
o Elbow
o Humerus
o Clavicle and shoulder
o Foot and ankle
o Tibia and fibula
o Knee
o Femur
• Awareness of complications and handling of patients with these injuries:
• Trauma to the Pelvis and Spine
ORTHOPAEDICS
• Brief description of each condition and treatment, especially those where casting is involved:
o Bone infections: osteomyelitis/tuberculosis
o Congenital talipes equino varus
o Developmental dysplasia of the hip
o Foot conditions, e.g. hallux valgus
o Knee conditions
o Osteoarthritis and Rheumatoid disease
o Osteochondritis e.g. Perthes disease
o Osteoporosis
BANDAGING: Techniques of bandaging and the use of slings, collar n cuff
WALKING AIDS: Basic principles and instructions
CASTING ROOM ISSUES
• Health & safety
MEDICO LEGAL:
• Record keeping / documentation
• Informed consent
• Ethical matters
cast adaptation and removal, cast request form, patient information leaflet, crutches information leaflet, exercise information leaflets, coping with a cast at home, skill mix / staffing of a casting room, and the syllabus for the British Casting Certificate.
The certificate and training courses are recognised internationally, and this is reflected by the continuing application to courses by students from abroad. As well as the original fiveweek block, courses run from the Royal National Orthopaedic Hospital in Stanmore, there are BOA validated regional day release courses in Newport and Bradford.
To become a fully qualified orthopaedic practitioner now takes a minimum of 20 months and in most cases two years. Before attending one of the BOA validated courses, the students must
CASTING TECHNIQUES
• Assessment of patient including relevant history
• Basic casting technique
• Use of apparatus in the casting room
• Care of patients in casts:
o Trimming, drying, and windowing
o Checking of patients in casts
o Verbal and written advice given to patients
o Communications skills
o Complications of cast fixation, prevention, detection, and treatment
• Walking attachments for leg casts
• Removal of casts and subsequent care
SPECIFIC CASTS
Appropriate use of materials including plaster of Paris and alternative casting materials.
• Understanding of how to use and create:
o Soft products and combi cast techniques.
o Producing the correct layers of resin-based materials and using products making use of their properties
• Positions, extent of cast and basic technique of:
Casts:
• Below Elbow
• Bennett’s type
• Above elbow
• Below knee
• Above knee
Plaster of Paris Lightweight resin-based materials
Slabs:
• Volar slab
• Below elbow
• Above elbow
• Below knee
• 'U' Slab
• Below elbow
• Below elbow (FRC or Soft combi cast)
• Thumb Spica
• Scaphoid
• Arm cylinder
• Above elbow
• Slipper
• Below knee
• Leg cylinder
• Above knee
• Sarmiento type
• Should have had demonstrated or applied these casts on the course and understand the principles.
• Should be able to discuss care and troubleshoot any problems
o Corset/jacket
o Frog type
o Shoulder spica
o Hip Spica
o Functional Bracing: Humerus, Femur & Tibia
• Understand the principles of orthopaedic bracing and be aware of the following applications:
o Futura wrist brace
o Humeral brace
o Range of movement knee braces
o Tri-panel knee splint
o Walking boots
o Casts for Club Foot
o Negative Casting
o Resting Splints for Limbs
work in casting for at least one full year. During this time, they complete a portfolio-learning log, which includes a record of casting related experience, including removal and application across a variety of materials, for a wide range of orthopaedic and traumatic conditions. They must also have experience of the application of ‘off the shelf’ devices. The students are also required to show reflection of learning resulting
from their clinical experiences by giving three examples. This portfolio-learning log is completed ahead of the OSCE component.
Next is attendance at one of the validated courses held over five weeks full time study at Stanmore three times a year or one of the six-month validated day release courses held annually at Bradford or Newport.

The courses are followed by an Objective Structured Clinical Examination (OSCE), where knowledge and skills are all tested. This examination now has stations for preparation and reading of notes, assessment of the patient and their injury, informed consent, application and removal of casts in various materials, communication and a documentation station, where the candidate writes in the notes. There is a separate station for the viva with the orthopaedic consultant where knowledge of anatomy >>
Table 1.
Newport BCC Casting Course.
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 37
and physiology, orthopaedic conditions, trauma and trauma complications is examined.
Application and Removal
Application and Removal of 'Off Shelf' Appliances
Diabetic Foot Ulcer Off-loading Casts Wound Care Management
In addition to the OSCE, a 3,000 word assignment is completed. This essay is usually based around a case study and the student is given guidance on suitable topics and how to progress. Students complete the assignment either during the six-month day release courses with some time following or, in the case of the students attending Stanmore, they are written in the months after they have completed the course. Not until all these sections have been completed successfully does the candidate receive the BCC. The programme is in depth and covers an array of areas as outlined in the exam syllabus in table 1.
External Fixator & Pin Site Management
Focused Rigidity Casting (FRC) Techniques
Plaster Room Management
Ponseti Casting for CTEV
Functional Stabilisation (FS) Casting Techniques
Running Virtual Fracture Clinics
Specialist Casting (Hip Spica’s, Jackets etc) Theatre Casting
Paediatric Casting
Service Development
Research
Table 2.
Currently orthopaedic practitioners do not have a registered body such as the Health and Care Professions Council (HCPC). Today the BOA holds a voluntary register, which all active orthopaedic practitioners are encouraged to join, however this is not mandatory. Thus, we need continued support from all trusts and employers to ensure that being active on the register is a prerequisite of employment into an orthopaedic practitioner role.
The orthopaedic practitioner in conjunction with the voluntary register is required to maintain their Continual Professional Development (CPD) by ensuring that they record more than 150 hours of practical casting over a three-year period (since their last renewal), and record details of their required professional development of five days or 35 hours of relevant study within
Neurological Casting and Splinting
Education & Training in Casting Techniques
Audit



three years. All these requirements align to the code of conduct for orthopaedic practitioners.
The role of the orthopaedic practitioner is wide and varied, both working autonomously and as part of multidisciplinary teams interacting with consultants, doctors, nurses, physios, occupational therapists, orthotists, podiatrists, social services, A&E departments, wards, operating theatres and beyond. Depending on the individual, the trust and job profile the roles and responsibilities can include areas such as those in table 2.
So, what does the future hold for the profession? Currently the BOA Casting Committee are exploring new university options to allow collaboration and engagement to build on the current British Casting Course syllabus and qualification with an aim of moving the academic qualification to diploma/degree level. This in turn will allow the profession to gain greater recognition for both the qualification and the role itself, which in turn will hopefully help position future discussions into both professional recognition and accountability and allow alignment to national job profiles.
If anyone has any comments regarding this article then please direct them to Mark Rees, BOA National Casting Training Advisor (NCTA), e-mail: markpaulrees@gmail.com or phone 07884 114191. n

Features
38 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Bradford BCC Casting Course.
ċ PJI: current aetiology
ċ Antibiotic prophylaxis: systemic, local, or both?
ċ Multi-Drug resistance in bone and joint infections
ċ Open questions in 2-stage exchange
ċ Advances in microbiology to diagnose and treat PJI
ċ FRI: new joined definition
ċ New approaches to fight orthopaedic infections
ċ Large clinical trials in bone and joint infections …and much more!
Submit your abstract now!
Important dates
Abstract submission deadline: 8 April 2024
Early registration deadline: 1 July 2024
#EBJIS2024 www.ebjis2024.org


the
26
·
·
of the European Bone
EBJIS 2024
Save
date!
- 28 September 2024
Barcelona
Spain Topics 42nd Annual Meeting
& Joint Infection Society
The National Consultant Information Programme (NCIP)
Sir Norman Williams and Deborah Higgs

Professor Sir Norman Williams was Professor of Surgery at Barts and The London, Queen Mary’s School of Medicine and Dentistry, Honorary Consultant Surgeon at Barts and The London (1986-2016), Director of the National Centre for Bowel Research and Surgical Innovation (2012-2016) and Past President of The Royal College of Surgeons of England (2011-14).
He was Senior Clinical Advisor to the Secretary of State for Health (2015-18), Chaired the Rapid Review of Gross Negligence Manslaughter in Healthcare (2018) and was a NonExecutive Director of St George’s NHS Foundation Trust (2016-19).
He is Chair of the National Consultant Information Programme (NCIP), Chair of the Independent Reconfiguration Panel (IRP), President of Bowel Research UK and a Non-Executive Director of the Private Healthcare Information Network (PHIN).
The National Consultant Information Programme (NCIP) is a quality improvement tool in which individual outcome data for all consultants are presented via a confidential portal restricted to the profession and not for publication. It has been developed for the profession by the profession and embodies lessons learnt from exemplar registries like the National Joint Registry (NJR) (www.njrcentre.org. uk) and has been developed under the aegis and funding of the Getting It Right First Time (GIRFT) programme (www.gettingitrightfirsttime.co.uk).
NCIP has been developed with the full support of the RCS and all the Specialty Surgical Associations including the BOA. Our NCIP Clinical Leads for each specialty together with several of their interested colleagues have spent many hours with dedicated analysts developing the content, checking its validity, and making it meaningful from a clinical standpoint. The relationship between NCIP and GIRFT has been key in NCIP’s development and data within each are complementary with GIRFT displaying outcome data at unit level and NCIP concentrating on outcomes at the individual clinician level.
As we have developed the content of the portal hand in hand with the profession, colleagues should feel confident that this is not something foisted on them by the powers that be but is an example of the profession taking on the responsibility for quality improvement with a secondary aim of improving clinical governance. The involvement of leaders in each specialty endorsing and contributing to the portal is something the profession should feel immensely proud about.
The portal has some unique features that are not available even in registries such as the NJR. Thus, it allows the consultant to drill down to view individual patient details. It tracks
readmissions of patients to any NHS trust in the country and not just the consultant’s own hospital. It also records the death of a patient that may occur once he/she has left hospital.
The NCIP portal has many potential uses. One important use is to streamline the appraisal and revalidation process. The GMC within its guidelines for appraisal (www.gmc-uk/revalidation) states that clinicians should be mindful of the following as evidence of involvement in quality improvement:
“Review of your performance against local, regional or national benchmarking data where this is robust, attributable and validated.”
NCIP by providing your individual performance benchmarked in this way supplies the evidence you need and what is more can be downloaded with ease from the portal in a simple, digestible form for discussion at your meeting with your appraiser, (Figure 1).
Your clinical impact award application can also benefit by including your NCIP data. Thus, consultants are asked in their application “to provide compelling evidence that includes measurable information such as outcomes data with dates, sources and relevant benchmarks and show the outcome and results of the changes they made”4 (www.awards.national-clinical-impact.uk).
The NCIP portal fulfils this requirement. There are also wider benefits for surgical practice. Innovation is the lifeblood of surgery. However, it can take years for reliable evidence to accrue to demonstrate the benefit or otherwise of a new procedure. The NCIP database by encompassing all NHS activity has the propensity to identify such innovative procedures and determine their efficacy or otherwise. Thus, ensuring that if appropriate they can be disseminated quickly throughout the system as well as provide evidence for the purchase of appropriate equipment and technology.
Features
40 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Excerpts of this article were originally published in: Williams N. NCIP: the National Consultant Information Programme. Bull R Coll Surg Engl 2024;106:34–8.
Features

Deborah Higgs is a Shoulder and Elbow Consultant at the Royal National Orthopaedic Hospital, Stanmore. She is also one of the National Consultant Information Programme (NCIP) Clinical Leads for Orthopaedics.
In getting NCIP from the development stage to business as usual however requires more work. The system relies primarily on HES data (although ONS data is used for mortality and certain demographic characteristics) which although much improved still has flaws. One particular problem in some trusts relates to attribution i.e., the accurate recording of the individual who performed the procedure. However, we have found that if this problem exists within a trust, it can be very much improved by those clinicians who are using NCIP engaging with management and coders to redress the issue.
GIRFT/NCIP have also been instrumental in creating a mandated theatre data collection whereby trusts will have to complete and return details of all individuals including trainees and anaesthetists involved in a procedure. This will assist trainees in maintaining their logbooks but also and perhaps more importantly track the outcomes of the patients they have operated upon over the longer term. Similarly, it will be possible to provide SAS doctors with their outcomes and the performance of locums will also be available which has not been possible hitherto. This facility fulfils important clinical governance responsibilities.
We are also considering the approach to risk adjustment as we realise that it is important that surgeons who take on highrisk patients are not inhibited from doing so. We do already have a section within the portal which profiles the demographics and risk factors of an individual surgeon’s practice that helps mitigate this criticism, (Figure 2). Nevertheless, this process must be improved. >>

JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 41
Figure 1: Screenshots showing example PDF summary of primary total hip replacement for uploading into appraisal documentation. The blue dot represents the individual consultant’s outcome compared with the national (blue line) and local median (dotted line).

We appreciate there are a variety of audits and registries such as the NJR that are well established and already provide useful insights into individual and team performance. We therefore intend to work with these to ensure linkage with the NCIP portal.
NCIP also has a role in tracking the fate of those patients who undergo procedures which require implants, especially those that are not already recorded in a registry. Readers will be aware of the problem with mesh implants which was highlighted in the report from Baroness Cumberlege1. That report made it clear that there was a need to ensure that there was a reliable system that identified what implant was implanted into which patient and what happened over the lifetime of that patient. NCIP in collaboration with the newly established Surgical Device and Implant Collection (also overseen by GIRFT) can fulfil this role.
We appreciate there is concern about the identification of outliers. However, it is understood by all concerned that an individual may be identified as such for a variety of reasons that has nothing to do with their
performance. We do not believe that NCIP should act as a regulator. If an outlier is identified by the NCIP data, we will notify the individual concerned and their specialty clinical lead in the first place so the accuracy of the data can be investigated. The onus will be on the trust to take the matter further if that is what is required, and we would only require that the trust informs us of the outcome.
NCIP as part of GIRFT is now a programme that has been prioritised within NHSE, and the team is being enhanced. We have 15 specialties on the portal, including orthopaedics, and are live in most trusts in England thanks to the hard work of our NCIP clinical leads working alongside our implementation team. There are at present over forty orthopaedic dashboards in the portal. Over the next 6–18 months we will be providing all consultants with access to the portal in a stepwise manner specialty by specialty. The national roll out for orthopaedics will take place in March 2024. We intend to work in a collegiate manner, continually learning and iterating improvements and will try to act on the feedback we receive.
We recognise that some surgeons may be reluctant to engage believing that in their trust the data is not precise enough. However, we would counter that it will only improve if consultants engage with the process and provide the feedback to those in their trust that can make the necessary changes. Our mantra here is “use it to improve it.” We wish to encourage use of the portal by every NHS consultant surgeon. Whereas we do not wish to be prescriptive, various Responsible Officers (ROs) and Medical Directors after viewing the NCIP portal have seen its benefit and have been keen for them and their appraisers to gain access. It has been emphasised that this would be particularly useful for those appraisers who are not from the same specialty as the appraisee.
We are currently in discussion as to how we can incorporate outcome data relating to private patients treated in the private sector thus establishing a single repository for an individual consultant’s whole practice. This will go a long way to fulfil Recommendation 1 of the Paterson Report3
Hopefully, we have demonstrated that NCIP has many benefits for individual surgeons, their teams, the profession in general and of course our patients. We recognise that it will take time to produce the ideal product however with your help we believe that NCIP can become a byword for quality improvement and show the world how British surgeons are prepared to aspire to be the absolute best they can be. n
Guidance on using the portal and more programme information can be found on our webpage: www.gettingitrightfirsttime.co.uk/ associated_projects/ncip
To request access to the NCIP Portal please email: England.NCIP@nhs.net
Non-clinical NHS Staff can view provider level NCIP data by logging onto the Model Health System at: https://model.nhs.uk
References
1. First Do No Harm – The report of the Independent Medicines and Medical Devices Safety Review. Available at: www.immdsreview.org.uk/downloads/ IMMDSReview_Web.pdf
2. Lilford R, Mohammed MA, Spiegelhalter D, Thomson R. Use and misuse of process and outcome data in managing performance of acute medical care: avoiding institutional stigma. Lancet. 2004;363(9415):1147-54.
3. Report of the Independent Inquiry into the Issues raised by Paterson. Available at: www.gov.uk/government/publications/ paterson-inquiry-report
Features
42 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Figure 2: Screenshots showing examples of the demographic and co-morbidity data in the portal.
38th Edinburgh International Trauma Symposium & NEW Edinburgh FRCS(Tr&Orth) Revision Course
EDINBURGH INTERNATIONAL TRAUMA SYMPOSIUM -14-16 AUGUST 2024
Three-day meeting for orthopaedicsurgeons and AHPs
Renowned international and UK faculty
Focus on revalidation and update through short interactive lectures and CBDs
Break out sessions include cadaveric surgical approaches and fixation techniques

Edinburgh FRCS(Tr&Orth) Revision COURSE -13-16 AUGUST 2024
Four-day intensive revision course
Comprehensive coverage of the syllabus
Viva practice sessions and mock exam
For more information on booking please visit: www.trauma.co.uk or email: symposium@trauma.co.uk
 VENUE: SHERATON HOTEL AND EDINBURGH MEDICAL SCHOOL
VENUE: SHERATON HOTEL AND EDINBURGH MEDICAL SCHOOL

Deepa Bose is a Consultant in orthopaedic trauma and limb reconstruction at the Queen Elizabeth Hospital Birmingham. Her practice is exclusively in adults, and includes general trauma, major trauma and posttraumatic limb reconstruction. She is Chair of the Specialist Advisory Committee for T&O, and the lead for CESR approval process.
She is the Past Chair of World Orthopaedic Concern UK, which focuses on teaching orthopaedics in low resource countries. Deepa has been on the Emergency Response Team of UK-Med, a first response team for international disaster relief, since 2012 and regularly participates in humanitarian projects in Guyana, Gaza and Ukraine.
Supporting surgical trainers
Deepa Bose
It is my great honour to have been asked to be guest editor for this edition of JTO, under the banner of a topic very close to my heart - supporting surgical trainers. The training landscape has undergone some seismic changes in the recent past. Many events have conspired to reduce the time and opportunities available to train within the NHS. There has been a gradual decline in the time trainees spend with their trainers over the last decade or more. Restricted working hours were introduced for the best of reasons, but have resulted in a very different way of working for doctors. Shift working reduces continuity of training and means fewer working hours spent during a normal working week. This loss of alignment between trainers’ and trainees’ working patterns in turn leads to reduced operative and clinical experience, and less developed procedural and decision-making skills.
The COVID-19 pandemic then threw the proverbial spanner into the works by grossly exacerbating the loss of training opportunities. Even in the recovery phase, a variety of factors contribute: lack of staff and theatre space, increased case complexity, loss of working efficiency and institutional pressures on productivity.
In this environment, we must learn to train smart; we can no longer rely on opportunistic training or an apprenticeship model. Emily Baird’s excellent article on the trainer’s toolkit will, I hope, provide some guidance on how we can address this.
Support for surgical trainers has always been sporadic and sparse, whether from the hospitals or from the wider NHS. Yet, as Pramod Achan says, they are “the most vital worker and servant”, for without training what provision is there for the future of the profession? We would do well to take note of his thoughts on how trainers can be supported and promoted at all levels. It is certain that without this the training ship will continue to sink.

Finally, we can all take inspiration from Donald Campbell’s philosophical piece on what it means to be a trainer, that complex interplay of roles that is required to nurture and grow the next generation of surgeons. We need to step up and give freely of ourselves as trainers to do so. As Donald says, “It is the preservation of fire, not the worship of ashes that is important.”
I urge you all to preserve that fire, and to respond to the rallying cry ’No training today, no surgeons tomorrow’. Remember, we all need good colleagues to operate on us in our twilight years, so let’s make sure they are good enough by training them well! n
Subspecialty
44 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk


For full details about warnings and precautions read the IFU. For more information and the IFU please visit www.arthrosamid.com or contact us at enquiries@arthrosamid.com
@Contu r aLt d Contu r a-O rth opae d ics-Lt d Contu r a O rth opae d ics Lt dar th r osami d
ww w. arthro sami d .co m
References: 1. Henriksen, M., et al. (2023) 3 Year Results From a Prospective Study of Polyacrylamide Hydrogel for Knee Osteoarthritis. Poster 483 presented at OARSI 2023; 2. Bliddal, H., et al. (2021). Polyacrylamide Hydrogel Injection for Knee Osteoarthritis: A 6 Months Prospective Study. J Orthop Res Ther. 6(2). 1188. ISSN 2575-8241. OUS/ARTHRO/MAR2023/053

A new class of injectable therapy to treat knee osteoarthritis maintaining pain relief for 3 years1
Safe and sustained pain relief with a single injection2 INTRODUCIN G Statistically significant reduction in pain maintained at 3 years1 NEW 3 year data available

Emily Baird is a Consultant Paediatric Orthopaedic Surgeon at the Royal Hospital for Children and Young People in Edinburgh, with an interest in paediatric trauma, and congenital conditions of the hip and foot. She trained primarily in the West of Scotland with Fellowships in Edinburgh and Toronto.
Emily is passionate about increasing diversity and inclusion in the workforce and broadening access to orthopaedics through mentorship and medical education. She is heavily involved in providing medical student education as an Undergraduate Lead, and Post Graduate Education as Training Programme Director for Orthopaedic Trainees in South East Scotland and examining for FRCS Tr & Orth.
She is the Chair of the Education Committee of the British Society for Children’s Orthopaedic Surgery, a Fellow of the Faculty of Surgical Trainers, Faculty Member for Non-Technical Skills for Surgeons and Tutor for the MSc in Patient Safety and Human Factors.
She lives in Edinburgh with her husband and two young boys, and likes to dance and run!
The trainer’s toolkit: A practical guide to maximising training opportunities
Emily Baird
In light of the overwhelming pressures we currently face in the NHS, in terms of increasing patient complexity and expectation, set against increasing waiting times and an increasingly resourceconstrained environment, it may be all too easy to side-line training. However, with the rallying call of ‘No training today, no surgeons tomorrow’1 our trainees, and the generations of patients we will treat in the future deserve better. Already we are seeing trainees approach Completion of Certificate of Training (CCT) with far less experience, as evidenced by lower logbook numbers, and there is a risk of a whole generation of young surgeons being underexposed and under-trained. So, how do you go about maximising training and stocking up your ‘Trainer’s Toolkit’ with all you need to support training in the most efficient way possible? How do you ensure your training tools are regularly sharpened? How do you gauge whether you are training to today’s standards?
The loss of the firm structure and the reduction in working hours has meant that the days of spending time as a stable team has gone. To make up for this, training must not be thought of as separate from service, but integral to it. This re-framing will allow training opportunities to be realised in the everyday and the appreciation that running a good service leads to good training, which in turn positively feeds back into the service (Figure 1).

However, the trainee may be unfamiliar to you; rotating rapidly through their attachments, pulled into teams at short notice to cover gaps and often managing multiple clinical areas simultaneously with a bleep that does not seem to stop. Trainers may feel less invested in individual trainees if they have not nurtured them from their earlier days and not been involved in their recruitment, or feel they have no say in the overall direction of travel of orthopaedic training. And with training being under-recognised in terms of time and remuneration in consultant job plans, it is no mean feat to prioritise it on a day-to-day basis, and something personally I struggle with, despite my passion for training. Let us consider an average day at work as an illustration.
The day flows from one clinical activity to another with little time to catch your breath, let alone formal teaching. Grasping the scalpel from our trainers’ toolkit, here we must dissect out each activity, create space and look for opportunities, (Figure 2).
Trainer tools
Check in. It sounds obvious, but asking how your trainee is before diving headlong into the trauma meeting can take a minute or two, but allows you to appreciate what state the trainee is in. Did their car break down on the way to work? Do they have an unwell child at home? Did they get next to no sleep because they were paged ten times overnight? Are they fasting?
All of these factors will affect performance, and potentially dictate how much supervision and encouragement they need that day, and how much training is possible. Grab the depth gauge from your toolkit to sense how they are doing that day (Figure 3).
Subspecialty
46 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Figure 1: The ‘ying and yang’ of training and service.

Create psychological safety. Meetings such as the trauma meeting and morbidity and mortality meetings are traditionally hierarchical and transactional and this can be an intimidating environment. Trainers may look upon trainees as less able and less experienced than they were at a similar stage, and even as ‘snowflakes’ but this is from a place of privilege at the top of the hierarchy and often through the lens of survivorship bias. Trainers may also become accustomed to heated debates over decision-making, but this may be perceived as hostility and lacking a supportive environment. We would all benefit from a more psychologically safe environment to discuss cases robustly, but with civility3, and seek out the learning points from differing opinions. Grasp your favourite pair of dissecting scissors from your toolkit to create safe space to operate and avoid causing harm.
Allow trainees to lead. The end point of training is no longer a time-based phenomenon, but with the new curriculum2 and in accordance with standards set out by the GMC’s Excellence by Design and Shape of Training reviews, it has become outcomes-based, with the goal of achieving the competencies of a day-one consultant. As such, trainees no longer ‘serve time’ as an apprentice, but require an individualised approach. Generic Professional Capabilities
(GPCs) need to be demonstrated in a range of Capabilities in Practice (CiP) as evidenced with Work-based Assessments (WBAs) and in the Multi-consultant Report (MCR). Leadership is an essential GPC, often poorly taught and up until recently, usually not assessed. Allowing the trainee to lead the trauma meeting, ward rounds and pre-operative briefing goes against the age-old, hierarchical grain, but serves to trust and allows the trainee to make decisions in a supported environment, developing their leadership style and enhancing performance. So figuratively, take your tools, hand them over and switch to the other side of the table and observe, so that you can fill out the leadership section of the MCR with robust evidence.
Allow trainees to operate. Literally hand over your tools! Every trainer has their own ‘set-point’ of how much of a case they are prepared to ‘give away’ to the trainee. This is based on many intrinsic factors such as a trainer’s own experience and comfort level with the procedure, their engagement with training as a process and their perception of risk. Many extrinsic factors are at play, such as the complexity of the case, time pressures and their assessment of the trainee’s competence. The latter in particular is
subject to internal bias, and we should all seek to turn our unconscious biases to conscious biases so we can take steps to address them.
Often conversations and decisions about who is holding the scalpel are made whilst scrubbing, but in an ideal world, this should be discussed in advance to allow the trainee to prepare. When that is not possible, for example an urgent trauma case, a useful tool in the box is the Surgical education checklist4 (Figure 4). >>

Subspecialty
Figure 2: Dissecting out the opportunities of a typical day at work. Key: Capabilities in Practice (CiP) 2 Green: Manages the emergency take; Yellow: Manages ward rounds and the ongoing care of in-patients; Red: Manages an operating list; Blue: Manages an outpatient clinic; Purple: Manages MDT working.
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 47
Figure 3: “On 1-9 of the rubber duck scale, how are you doing today?”

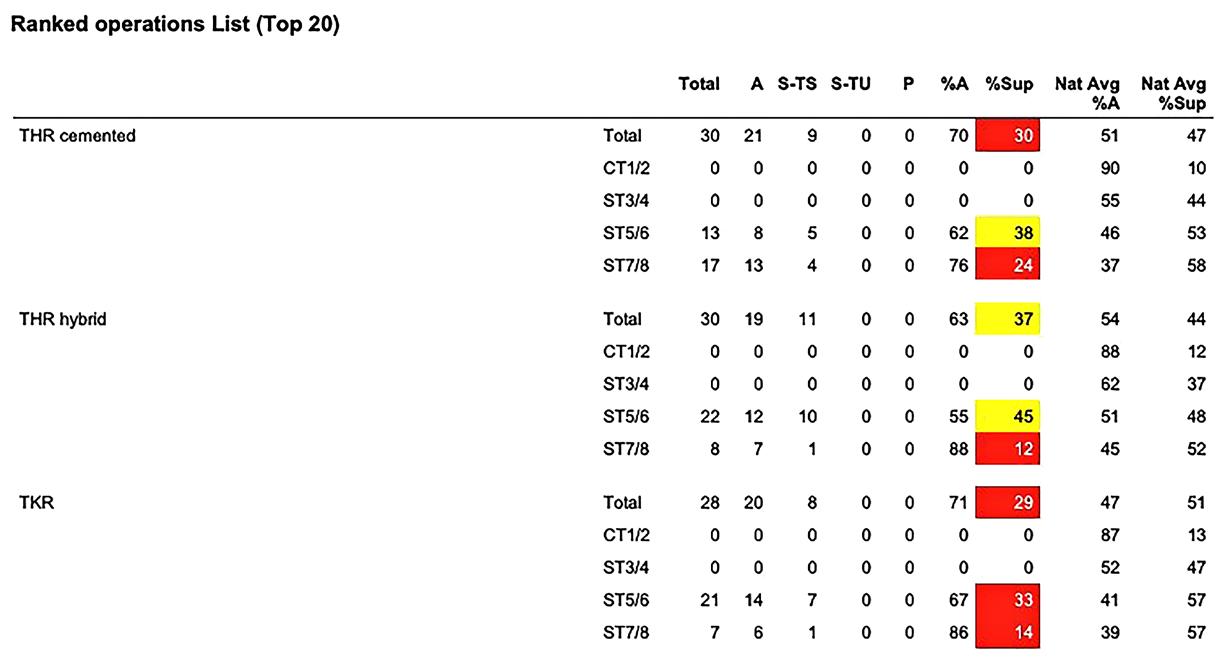

Where possible cases should be identified to the wider team as ‘training cases’ and lists planned accordingly to minimise the occurrence of “I’m sorry we’ve run out of time, I’m going to have to crack on with this one…”
Hopefully we heed the clarion, postCOVID-19 call of the Joint Committee of Surgical Training (JCST), the Association of Surgeons in Training (ASiT), the British Orthopaedic Trainees’ Association (BOTA) and the Confederation of Postgraduate Schools

of Surgery (CoPSS) to champion ‘Training anytime, any place, every case – no excuses’5 despite the challenges in doing so. You can download your own record of which cases you supervised trainees versus those you perform yourself from the e-Logbook6 (Figure 5), and Training Programme Directors (TPDs) can use this to help in planning rotations to maximise training opportunities.
Non-technical skills (NoTS) are fundamental tools in your surgical toolkit, and there is growing recognition of their importance at improving surgical outcomes7. Trainees are now formally taught NoTS, and these competencies feature heavily in the T&O curriculum2 and should be assessed just as technical skills are. Although the cognitive skills of situational awareness and decision-making, and the social skills of communication, teamwork and leadership develop with time and experience, few trainers were specifically taught them, and as such it is important to reflect on your ability to teach and assess NoTS. The NOTSS behaviour assessment tool and training system was developed by surgeons using human factors methodologies, and using the taxonomy below, trainers can observe, rate and provide feedback (Figure 6). Make sure your non-technical tools are as sharp as your technical ones and consider a masterclass to hone your skills8
Give feedback regularly. Normalise everyday conversations about what went well and what didn’t, such that the skill of giving honest and appropriately critical feedback is developed with time, and trust between trainer and trainee built up. A good trainer cares about their trainee and is invested in them, but is not afraid to challenge and act with radical candour9 (Figure 7).
Feedback can take many forms, from informal to formal, verbal to written. Ask the trainee what they prefer – often they will be more educationally savvy than you are!
Feedback ideally should be documented contemporaneously on ISCP, as a Workbased Assessment (WBA), post-MCR feedback session or a Journal Note10. A practical guide to improving feedback and reflection to improve learning11 and the BOA’s virtual Training Orthopaedic Trainers (V-TOTs) course12 cover this in greater depth and are highly recommended.
Many trainers do this automatically, and for some it needs to be more effortful. Look around your colleagues, reflect and mirror their positive behaviours, and seek their feedback. Many trainers are unaware of the functionality of ISCP and its important place in the Trainer’s toolkit.
Subspecialty
Figure 6: The non-technical skills for surgeons (NOTSS) taxonomy.
Figure 5: An example of a Trainer’s Analysis Report from the e-Logbook.
Figure 4: The surgical education checklist.
48 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Figure 7: Radical candour.

Here you can find space to create your own Trainer profile to set expectations for trainees and what they can expect from their time with you (Figure 8), collect data on the number (Figure 9) and timeliness of WBA completion (Table 1), and collate feedback from trainees and trainers – all excellent evidence for appraisal and obtaining Recognition of Trainer (RoT) status13

Escalation. As medics, and particularly surgeons, we feel we need to have the solutions to problems and be the one to personally act to resolve issues. Sometimes we don’t have the correct tool in the toolkit at all. Trainees lead complex lives, full of challenges, many of them unseen, and trainers need to know where their limits are in terms of being able to adequately
support trainees who divulge issues, and when to escalate. If a trainee comes to you actively listen. Your greatest tools are your ears. Often acting as sympathetic ear or a sounding board is all that is required, but most trainees will need additional support at some time of training, so reach out to your TPD who will be able to signpost to local resources or refer them on to services such as occupational health, or professional support, wellbeing and development services14-16
Role modelling. It is not just what tools you have in the toolkit that matters, but how you use them, and how your trainees go on to develop their own skills and behaviours. Trainers can adopt many roles: educator, coach, manager, advocate, academic, mentor, but running through all of these is role modelling: demonstrating skill, providing feedback and emulating professional behaviour. A great trainer will shape the lives of their trainee, not just in the six months they are working alongside them, but potentially their entire career. We can all remember influential trainers and their impact. Strive, even with the challenges we face on a daily basis, to be that trainer.
I would be fascinated to hear what is in your trainer toolkit, and how we can work together to champion training. Please get in touch and let me know: Emily.baird@nhslothian.scot.nhs.uk or @emilyjanebaird. n
References
References can be found online at www.boa.ac.uk/publications/JTO
WBA type Average days from WBA to submission Average days from submission to validation System-wide average days from submission to validation CEX 28 8 16 CBD 12 5 18 DOPS 18 4 19 PBA 18 6 21 Audit 6 3 14 Teaching 3 5 17
Figure 8: The ISCP Trainer’s Area.
Table 1: ISCP evidence of timeliness of WBA completion.
Subspecialty JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 49
Figure 9: ISCP evidence of WBA completion.
Supporting trainers: The future direction of travel
Pramod Achan

Pramod Achan is TPD for the Percival Pott Training Programme, member of the SAC for T&O, Consultant Lead for Leadership Development at Barts Health NHS Trust.
Surgery has always been a subject taught at the coalface with apprenticeships evolving into the modern curriculum delivered by trainers to competitively selected trainees. In orthopaedic surgery we have often led the way with the creation of training programmes, courses, exams and competency based evaluation all aimed at the singular communal goal of delivering a final product that is a surgeon who is competent, empathic, knowledgeable, skilled and dedicated to the care of their patients.
In that journey the most vital worker and servant is the surgical trainer, without whom it is impossible to train the next generation of surgeons. In an evolving world of simulation, augmented reality and artificial intelligence that is a statement that has to be challenged and I often do, yet I stick by it and so when asked to write about how ‘we’ could support the orthopaedic
surgical trainer, I have tried to be sensitive to the fact that for far too long they have been unsupported, both in terms of personal development and recognition of their work.
Support is defined in many ways, one of which is ‘to give assistance to’ and another ‘to bear all or part of the weight of’ and in my working life for the surgical trainer it has largely consisted of assistance in the delivery of training based around a curriculum with a focus on their roles and responsibilities in that delivery and the paper trail of accountability that goes with it. In this short article I want to suggest that supporting a trainer can be much more, eventually reaching a stage where it can help in the aim of developing a trainer from good to great. In order to do this, we must consider who has the influence to ‘support’ them and what incentivises the trainer to develop and what could incentivise others to invest in that development.

I have broken influences into domains where there are possibilities to elicit and garner support.
Personal
This is a domain that focusses on the personal development of the trainer. Others are going to cover the domain of developing skills in competent training and evaluation, but we must not overlook the support and oversight of the wellbeing of trainers. This includes having a support infrastructure to ensure trainers are cared for and protected, that their family and friends understand the time, dedication and stresses that modern day training can place upon a surgeon irrespective of the attitude, ability and competence of the trainee.
Subspecialty
50 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
Influences on a surgical trainer in 2024.
Some investment in their professional development with qualifications they can put in their CV and also some formal support through the difficult situations they may encounter are all areas that should be improved.
Training community
This community is often quite detached from the trainer at the coalface. Interactions during formal visits and HEE assessments are not great opportunities for maximising support. Any TPD would benefit from having time to visit and build relationships at a personal level with trainers that are bound to develop into supportive roles. The trainees have made great strides in introducing recognition of training excellence by virtue of the TOTY (Trainer of The Year) awards. These are cherished by the trainers who receive them and in the right spirit coveted by those that haven’t, yet rewarding just one TOTY per year in a large region means the majority of trainers go largely unrecognised. Is there a role for awards in each subspecialty? It is also easy to see how the metrics that make a trainer attractive to trainees may not always sit hand in hand with the metrics that a TPD or HEE find helpful and supportive when dealing with trainees who are in difficulty or need curated training support. Should the training programme directors be giving a parallel award for that trainer group?

External organisations
What roles are the various external organisations playing in supporting trainers in orthopaedic surgery? We can look at Industry, implant companies, indemnifiers, private health providers, innovation hubs, consultancy firms all of whom potentially have the opportunity to work with and support trainers to maximise their own potential and worth.
Newer players
The SAC also play a huge role in overseeing and supporting trainers and trainees but can often feel detached from the trainers in the region that they are liaison members in. Inviting them to events where such relationships can be forged would provide an increase in the depth of support and understanding of any given training programme.
The orthopaedic community
This has layers of leadership where the British Orthopaedic Association (BOA) sits at the top with its President and Council overseeing the strategic position of the services that the community provide. This is not just limited to clinical services but also to education, training, research, communal standing and wider global influence. The BOA can support trainers with recognition of excellence in the same way that BOTA have opted to, by providing opportunities for trainers to exchange ideas and best practice and reflect on dealing with
difficult situations and challenges (not only with trainees in difficulty) with the aim of maximising the help they can offer. They can also help with support to counter the challenges arising from the local pressure that trusts and departments project in the constant battle between service provision, efficiency and comparative throughput against the rhetoric of training. There is also an opportunity for the specialist societies to award their own recognition in support of training opportunities and trainers at specialist registrar as well as fellowship level. The specialist societies are becoming more influential in specifying the services and their delivery and it is easy to overlook the prioritisation of training and trainers. We are seeing evidence of this as GIRFT is identifying both volumes and efficiency of units and surgeons to determine where revision knee surgery should take place in partnership with BASK. The implications for training and trainers is potentially huge and it is unclear who is championing the trainers position in these endeavours.
The academic community
Universities have always played a large part in the research arm of training and yet the educational needs of trainers is not something they have embraced outside of medical school needs delivered by honorary contracts. American universities have shown how faculty members can be recognised by offering them educational opportunities, discounted courses and further qualifications and perks. This form of support for surgical trainers enhances their own portfolios, which in turn enhances their passion for teaching and training.
Organisations like the NJR and GIRFT also have a role to play in the support of trainers recognising the need for trainers to prioritise training ahead of efficiency gains. Training may result in some unexpected outcomes which impact a given surgeon’s figures and funnel plots. The journals and the NJR need to recognise the work many trainers do in delivering the high volume case numbers that makes this big data credible and the publications that this data generates having the impact that they do.
Trainers also need some support from the vulnerability of their positions to new unregulated vehicles such as social media and potential influencers who have the power hitherto unknown, of making rash judgements or statements that can mobilise a mob mentality retaliation.
To summarise, the traditions of surgical training are bound intimately with the dedication and commitment of the many surgical trainers up and down the country. It seems incredible that the workforce that underpins this most vital component of developing the surgeons of the future work largely out of a sense of good will, while constantly being analysed, assessed and often pressured in the other facets of their working lives. Recognition could be described in three ways:
• Monetary recognition – a purely financial reward for their efforts
• Social recognition – recognition from society for the efforts that a person or group of people expend and
• Moral recognition – a sense of doing the right thing because it is the right thing to do.
As our society inevitably changes, it may be time to re-evaluate how we offer recognition in these three areas to our amazing surgical trainers, without whom, training the orthopaedic surgeons of the future would be impossible. Thank you to you all. n
Subspecialty
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 51
Training philosophy – the why
Donald Campbell

Donald Campbell is a Consultant T&O surgeon in Ninewells Hospital and Medical School, Dundee. He was TPD for six years in the East of Scotland Deanery until 2019 and is now the UK and Ireland TPD forum Chair. He is also the SAC liaison member for the Military and Northern Ireland.
The George Bernard Shaw quote1 sometimes thrown at those who teach and train is “Those who can, do; those who can’t, teach”. To me, it conjures up the image of a doyen of surgery, whose technical mastery of the craft is so profound that even the most outrageous behaviour is excused. The implication is that to excel in your field you must have a singleminded focus on yourself and your own work and not waste your time teaching.
The flip side of this coin is the disappointing trainer who, while dedicated to teaching, has no clinical credibility. But when inspirational training co-exists with clinical excellence, the combination can be transformative. Some of the greatest minds in history, from Socrates to Hawking, so believed in the primacy of teaching, they made it a core part of their working lives.
To be a good trainer takes hard work, patience and humility. I consider myself fortunate to have had many great trainers in my career and witnessed teachers who could captivate an audience by amusing, entertaining and educating with somehow effortless ease. I now know that none of this talent came without discipline, preparation and practice. We are a composite of parts of trainers we have had, and with reflection, I hope the good bits.
As a trainer in a craft speciality, we have a unique relationship with our trainees. We hand a scalpel to them over our patient’s bodies and say, “Now… it’s your turn”. This is not easy for trainers, as they ultimately own the responsibility for the outcome and complications. However, they must try to remember the very first time they were handed a scalpel or did their first hip replacement. This burden is eased if the trainee is honest, hardworking and humble. It is much more
pleasant to work with a trainee who enthuses “I get to go to clinic” instead of moaning, “I have to go to clinic”. Life is about our choices and how we react to situations, many of which are beyond our control.
We no longer have the hegemonic power of surgeons in the last century. We depend on working in complex team structures and have the ultimate responsibility of creating an educational environment that brings the team on the training journey with us. A healthy team structure is not only better for patient safety and outcomes but also for our own protection and well-being.
Football manager Sir Alex Ferguson would stop his players in the training ground and make them look to the sky if a flock of geese flew overhead. “That is teamwork” he would say. It is one of the most remarkable examples of teamwork in the animal kingdom, which humans would do well to emulate. They fly in strict formation and call out to each other offering encouragement and take turns at leading the flock to fly incredible journeys together, through all kinds of adversity. We have to teach our teams in today’s pressured working environment that it is fundamental the trainee gets to lead the flock too.
“Humility is not easy for the surgeon to acquire, but a good start is reflecting critically and openly on one’s complications through audit. The ancient wisdom is true: know thyself, be humble.”
It’s important to keep reminding ourselves that we are momentarily passing through our careers as but a small cog in a giant machine. We are not immortal and may not be here to lead the team next year. Memento mori (death memory) should never be far from our thoughts, particularly when we receive adulation. These words were whispered in the ears of the conquering Roman generals as they returned to victory parades from war2 “Look behind you. Remember that you are a man. Remember that you are mortal.”
Subspecialty
52 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
We have the great privilege of performing life-changing operations with the societal rewards of praise and gratitude. But hubris is never far away from our success and a fall from grace can be as swift as lighting. Ego and hubris can affect the trainee too, often creeping in after their first successful solo operation. We must be constantly watchful as Ego is the greatest enemy of us all. This was understood by the ancient Greek philosophers whose wisdom is carved on the pillars of Delphi “Surety brings ruin”, “Nothing to excess” and “Know thyself”.
Ego is not just a barrier to training, but to our own development. Stoic philosopher Epictetus said, “Throw out your conceited opinions, for it is impossible for a person to learn what he thinks he already knows”3. It is incumbent on the trainer to set the ground rule that there are no stupid questions, in fact these are often the best questions that everyone was too afraid to ask. Socrates knew that coming to terms with our own ignorance was fundamental, he said, “The only thing I know, is that I know nothing”.

It is one of the great joys of training to have a fresh pair of eyes look at what you teach and question it. It forces you to re-examine what you thought you knew and stay fresh to the constant changing of what is understood. It is true that to teach a subject is to ‘learn it twice’ and as your understanding deepens, so too does your enthusiasm.
During his incarceration in prison, Oscar Wilde wrote on humility, “It is the last thing left in me, and the best… one cannot acquire it, except by surrendering everything that one has”4
Humility is not easy for the surgeon to acquire, but a good start is reflecting critically and openly on one’s complications through audit.The ancient wisdom is true: know thyself, be humble.
Some surgeons prefer to work without a trainee. They see every single one of their patients and perform all of the operations, often as part of a well-oiled familiar team. I guess for some, this can reduce stress by maintaining constancy and control and it may be a good model in your first year as a new consultant, for getting your feet under the table. But to continue this way for the next 30 years without the challenge, stimulus and company of a trainee, for me, would be dull. Every trainee I have had has taught me something.
Emerson said, “Every man I meet is my master in some point, and in that I learn of him”5. There is also a shared responsibility that helps with the ‘loneliness of command’ when making decisions over people’s lives. I look at the trainer-trainee partnership as a journey together. There will be high points and low points, but both always learning. Through these shared experiences comes camaraderie and friendship that can be lifelong. It is one of the greatest rewards to see your past trainees succeed and become better than you. It is the preservation of fire, not the worship of ashes that is important.
The role of the trainer as mentor and advisor is rewarding. As the philosopher (and boxer) Mike Tyson said, “Everyone has a plan… until they get punched in the face”. During surgical training, it is not uncommon for some significant personal or work trauma to knock a trainee off their trajectory. Never underestimate the help that can be given from just talking through the problem. It is often the case the trainee has not shared the problem with their peers. Listening is a skill. The philosopher Zeno said, “The reason we have two ears and only one mouth is so we might listen more, and talk less”6. Unless you and the wider team hear that help is needed, the problem is hard to solve. It’s important that the hierarchal barriers are broken so delicate topics can be approached and discussed privately. Kindness and calmness are contagious. Foster an environment people want to share, learn and work in.
Adapting your training style to the differing needs and personalities of your trainees is an interesting challenge. A foundation built
on principles is vital so we can adapt to the multiple needs and presentations of trainees (and our patients too). Stoic philosopher Epictetus, when asked by a pupil “what to do?” said, “What advice could I possibly give? No, a far better request is ‘train my mind to adapt to any circumstances’”7. The stoics believed in following the harmony of nature as a model in life, just like Alex Ferguson and his geese. Our role is not just teaching surgery but skills such as working with challenging people and coping with stress. Epictetus, when dealing with difficult people or situations advised, “Every event has two handles – one by which it can be carried and one by which it can’t. If your brother does you wrong, don’t grab it by his wronging, because this is the handle incapable of lifting it. Instead use the other – that he is your brother, that you were raised together, and then you will have hold of the handle that carries”8
In the end, our ultimate goal is not to just teach and train, but to inspire the next generation of surgeons as role models. This requires enthusiastic engagement with potential surgeons, particularly medical students, to show what a fascinating and rewarding career we have. It’s like planting trees in a garden we will never see grow.
I think this quote from Aristotle better sums up training: “Those who know, do. Those who understand, teach.” n
References
References can be found online at www.boa.ac.uk/publications/JTO
Subspecialty
JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk | 53
Stoic philosopher Epictetus.
Nicholas Barton
28th May 1935 – 11th October 2023
Obituary by Tim Davis, Neil Barton and Joseph Dias

Nicholas Barton, retired consultant orthopaedic and hand surgeon at the Queens Medical Centre and Harlow Wood Hospital, Nottingham passed away on 11th October 2023. He was a gifted, questioning surgeon and teacher who served as Chair of the Education Committee of the British Orthopaedic Association and Speciality Advisory Committee (SAC) for Trauma and Orthopaedics (19941995). He was Honorary Secretary (1983-1985) and President (1989) of the British Society for Surgery of the Hand (BSSH) and Editor of the Journal of Hand Surgery, British Volume (19871991). In 2007, he was made a Pioneer in Hand Surgery by the International Society for Surgery of the Hand (IFSSH).
Nicholas studied medicine at Cambridge and the Middlesex Hospital, qualifying in 1959. His orthopaedic training was completed at the Robert Jones and Agnes Hunt Orthopaedic Hospital in Oswestry, and the Rancho Los Amigos Hospital in Los Angeles.
Nicholas developed his main medical interest, hand surgery, after his appointment as consultant in Nottingham in 1971. Throughout his career, he researched the treatment of scaphoid fractures, and delivered his Hunterian Lecture to the BOA annual meeting in Birmingham in 2001.
One of Nicholas’ great assets was his curiosity. The first sentence of his article “Twenty Questions about Scaphoid Fractures” (1992) demonstrates his enquiring mind: “When I was appointed a consultant in 1971, I had no doubt about fractures of the scaphoid: I had been taught all I needed to know during my training –or so I thought”. This article became, and remains, essential reading for any young surgeon planning to research injuries to this bone.
Nicholas was an active teacher of medical students and trainee orthopaedic surgeons. He was an excellent mentor of junior colleagues, and guided their management of patients by asking questions, rather than telling them what to do. He was the single-handed editor of the Journal of Hand Surgery for five years.
Nicholas’ curiosity was not confined to surgery conundrums. When a student, he worked on a barge on the River Thames in London, and became interested in its tributaries. This led him to write the book ‘The Lost Rivers of London’.
When a young doctor in London he met Margaret when she was looking for a speaker for a Christian Union meeting. She described him later as “a walking encyclopaedia, with boundless curiosity, who reads constantly”. They were married in 1960. Nicholas leaves Margaret, their five children, 13 grandchildren and three great-grandchildren. He will have left his mark on those who worked with, or trained under him. n

In Memoriam 54 | JTO | Volume 12 | Issue 01 | March 2024 | boa.ac.uk
25TH EFORT
Congress 2024
www.efort.org/hamburg2024

Late registration deadline 24 April 2024



25TH EFORT Congress
Hamburg, Germany: 22-24 May 2024
Congress Highlights | Main Theme: Collaborating For Success
Interdisciplinary Research
Clinical Outcomes Measurement And Monitoring
Healthcare Innovation And Technology Adoption
Now And The Future Of Joint Arthroplasty
Advancements In Surgical Techniques
For Orthopaedic Trauma Management
Key dates
Advanced Programme online: 01 April 2024
#EFORT 2024
Musculoskeletal Infections
Best Practices For Involving Industry User Groups
Ensuring The Safe Adoption And Regulation
Of Robotics And AI In Healthcare
Patient Engagement & Shared Decision-Making
Regulatory Science Late registration deadline: 24 April 2024



RECRUIT SUSTAIN RETAIN
THE T&O WORK FORCE
BOA ANNUAL CONGRESS 2024
SAVETHEDATE! CONGRESS


SEPTEMBER20TH
SEPTEMBER17TH-19TH COURSES& WORKSHOPS




Preventing PJI in arthroplasty patients
Know your patient – and reduce PJI risk!
A tremendous challenge in arthroplasty
Periprosthetic joint infection (PJI) is a frequent, severe, and costly complication following total joint arthroplasty, accounting for up to 2% in primary surgery and 4% after revision.1 Potential complications can range from superficial skin infections to more serious problems such as loss of limb or amputation which can be caused by deep PJI. Implant infections can result in substantial morbidity, mortality, and health care costs and have a negative impact on patients’ quality of life and psychological well-being. Treatment of PJI usually requires surgical intervention and prolonged intravenous or oral antimicrobial therapy.2
Despite many advances in research and clinical practice over the last decades, prevention and management of PJI remain challenging not only for the orthopaedic team, but also for the patient.
Take your patients’ risk into consideration
Not all patients undergoing total joint arthroplasty are equally at risk of developing post-operative infections. Identifying and addressing associated risk factors prior to surgery is essential in reducing PJI after surgery. Risk factors can be both patientrelated or treatment-related.
Some patient-related PJI risk factors are: older age, diabetes, cardiovascular disease, obesity, previous infection, smoking and revision surgery.3-5 According to a clinical risk
score established by Sanz-Ruiz & Berberich, a high risk of PJI is defined by the presence of two or more of the above-mentioned risk factors in knee arthroplasty patients and three or more in hip arthroplasty patients.3 Based on results obtained with this score approximately 60% of patients aged 65 years or older are at higher risk for infection.3
An integrated and effective preventive approach to reduce the risk of infection in patients with risk factors is essential. In this respect, individually tailored measures for infection prevention may include optimisation of surgical procedures, such as skin preparation and wound irrigation, improved peri-operative blood management, pre-operative optimisation of patient risk factors and comorbidities, normothermia and adequate oxygenation as well as systemic peri-operative antibiotic prophylaxis. Last but not least, the addition of high-dose antibiotics to bone cement can be implemented as part of a risk-adapted approach.3,5-8
Dual antibiotic-loaded bone cement: effective in various clinical prevention settings
In particular, using dual instead of single antibiotic-loaded bone cement such as COPAL® G+C can provide a viable option within the set of preventive measures.3,7 Clinical trials have demonstrated effectiveness of high-dose gentamicin- and clindamycin-loaded COPAL® G+C bone cement in common clinical settings such as in primary and revision hip and knee arthroplasty as well as in trauma.
In elective primary hip and knee arthroplasty
dual antibiotic-loaded bone cement has been shown to reduce PJI frequency from 3.7% to 2.5%;3 in fractured neck of femur, PJI frequency was reduced from 3.5% to 1.1%;9 and in aseptic revision knee arthroplasty a reduction from 4.1% to no PJI was shown.10
Furthermore, dual antibiotic-loaded bone cement appears not only to be more effective but also more cost-efficient than a single antibiotic-loaded bone cement in aseptic knee arthroplasty.10
Lower PJI burden – now!
Due to demographic aging, arthroplasties such as hip replacement surgery are projected to be performed in a growing number of patients. The number of PJI-related implant failures and the need for revision surgeries associated with PJI are, consequently, expected to further increase. Accordingly, it is essential to lower the high burden of PJI faced by clinicians, institutions, and patients.11,12
Clinical evidence shows that arthroplasty patients can benefit from an integrated and risk-stratified preventive approach.3 In particular, elderly high-risk patients obtain advantages from prevention measures that may include the use of high-dose dual antibioticloaded bone cement for implant fixation.8 n
References available upon request.
SPONSORED CONTENT www.heraeus-medical.com
consultant
two patient complaints led to my exclusion from work
When I was told I was being excluded from work following complaints of rough treatment from two of my urology patients, it was like being punched.
Medical Protection immediately assigned me a medicolegal consultant, who was able to downgrade the exclusion to a restriction while the situation was under investigation.
He negotiated a meaningful action plan and consistently moved things forward. Eventually, after two long years, the complaints were found to be based on a misunderstanding and I was fully back in my role. It was a hard lesson on the need to explain everything to patients, especially uncomfortable procedures.
There is no way I could have got through it without Medical Protection. They know their stuff inside-out and are exceptionally skilled at dealing with difficult working relationships. They really are, as they say, always there for you.

Get protection you can depend on from just
I’m a
and...
medicalprotection.org/case3
£549*
The Medical Protection Society Limited (“MPS”) is a company limited by guarantee registered in England with company number 00036142 at Level 19, The Shard, 32 London Bridge Street, London, SE1 9SG. MPS is not an insurance company. All the benefits of membership of MPS are discretionary as set out in the Memorandum and Articles of Association. MPS® and Medical Protection® are registered trademarks. For information on MPS’s use of your personal data and your rights, please see our Privacy Notice on our website. *Cost shown is the annual membership price for a UK Medical Consultant working exclusively in the NHS. Subject to protection requirements and underwriting approval. This case is based on a real scenario, with some facts altered to preserve confidentiality. 2310245327:02/24











































































































































 Figure 1: Image from a pre-operative robotic THA plan allowing acetabular cup positioning.
Figure 2: Pre-operative RO THA plan showing virtual range of motion with the hip flexed and internally rotated to assess for posterior dislocation.
Figure 1: Image from a pre-operative robotic THA plan allowing acetabular cup positioning.
Figure 2: Pre-operative RO THA plan showing virtual range of motion with the hip flexed and internally rotated to assess for posterior dislocation.


 Figure 3: Pre-operative planning of robotic TKA.
Figure 4: Intra-operative soft tissue balancing of TKA.
Figure 5: Intra-operative UKA planning and balancing of soft tissues.
Figure 3: Pre-operative planning of robotic TKA.
Figure 4: Intra-operative soft tissue balancing of TKA.
Figure 5: Intra-operative UKA planning and balancing of soft tissues.


















 VENUE: SHERATON HOTEL AND EDINBURGH MEDICAL SCHOOL
VENUE: SHERATON HOTEL AND EDINBURGH MEDICAL SCHOOL