+ HEALTH MEDICINE
TAKING CHARGE OF OUR HEALTH
JOIN THE MOVEMENT MOVEMENT EMBRACE FOOD AS MEDICINE
LEARN TO ADVOCATE FOR YOURSELF























































































JOIN THE MOVEMENT MOVEMENT EMBRACE FOOD AS MEDICINE
LEARN TO ADVOCATE FOR YOURSELF






















































































by Shawn Jordan, DDS, MS; Cynthia Czaperacker, DMD, MS; Mariel Webber, DDS; & Matthew Fenigstein, DDS, MS

ABOUT
Apex Endodontics is the largest, most technologically advanced endodontic office serving the WNY community. We specialize in saving teeth from extraction by performing root canal therapy and other pain management treatments. The Apex dental team includes twenty team members and doctors that specialize in urgent dental care with a focus on each patient’s individual needs. At Apex, we create a relaxing, positive experience with personalized music, blankets, aromatherapy, and three sedation options. Prospective patients can virtually tour the Apex office and watch a full patient experience video on our website. At Apex, you are treated with the utmost care.
What is a root canal and why might I need one?
Contrary to what you may have heard, a root canal is a painless treatment which aims to clear infection and protect a tooth from further harm. During root canal treatment, affected tissue is removed and the interior of the tooth is cleaned, disinfected, and sealed. The restored tooth can last a lifetime. There are many reasons a tooth may need treatment, including a deep cavity, tooth pain or sensitivity, possibility of cracks, or previous dental trauma. Bacteria can enter the pulp tissue and germs then cause infection. If left untreated, an abscess can form and, if the infection is not removed, pain and swelling can result.
My tooth doesn’t hurt, but I was told by my dentist I need a root canal. What if I don’t do anything?
If left untreated, a tooth infection can impact other areas of the body. A tooth infection may cause bone loss in the jaw, which can harm neighboring teeth. An infection can also spread through the blood and infect vital organs like the brain and heart.
What about taking an antibiotic? Can that get rid of the infection in my tooth?
An oral antibiotic is digested and picked up by your bloodstream. Unfortunately, an infected tooth no longer has a blood supply, so the oral antibiotic can’t get into the tooth to kill the bacteria. Root canal therapy physically and chemically removes and kills the bacteria to resolve the infection and save the tooth.
Why choose Apex Endodontics?
aromatherapy, and many more calming amenities at no additional cost. Apex is packed with the latest technology including Gentlewave, 3D imaging, microscopes, and so much more. Our doctors collaborate on cases, accept payment plans, and offer three types of sedation options. Most importantly, the Apex dental team is the best in the business. Our doctors, dental assistants and administrative team members are trained professionals that thrive on helping patients.
Dr. Shawn Jordan, owner of Apex Endodontics, is an endodontist from Hamburg, NY. He completed his Doctorate of Dental Surgery at UB Dental School. Dr. Jordan also practices at the Buffalo Veteran’s Hospital and has hosted numerous lectures to collaborate with and support local general dentists and dental specialists.
Dr. Cynthia Czaperacker is a board certified endodontist from Western New York. She earned her Doctor of Dental Medicine from the University of Pittsburgh and her Certificate in Endodontics from the University of Illinois in Chicago. She has a special interest in regenerative endodotics, which aims to preserve or regenerate the vitality of teeth.
Dr. Mariel Webber is published in the Journal of Endodontics and teaches as an associate clinical professor at UB Dental School. She is boardeligible and has been practicing endodontics in the WNY community for five years.
Dr. Matthew Fenigstein is a board-eligible endodontist who is passionate about providing the best possible care for his patients. Growing up with dentistry in the family made entering the field himself an easy decision. Spending countless hours in his dad’s office taught him the compassionate side of dentistry, where the patient always comes first.
LOCATION 125 Grand Island Boulevard Tonawanda, NY 14150
Apex is centrally located—just seconds from the I-190. Our new office, built in 2022, is spacious, modern, and peaceful; it was specifically designed to best care for our team and the patients we serve. Patient needs are personalized with choice of music,
Scan to learn more about our doctors.

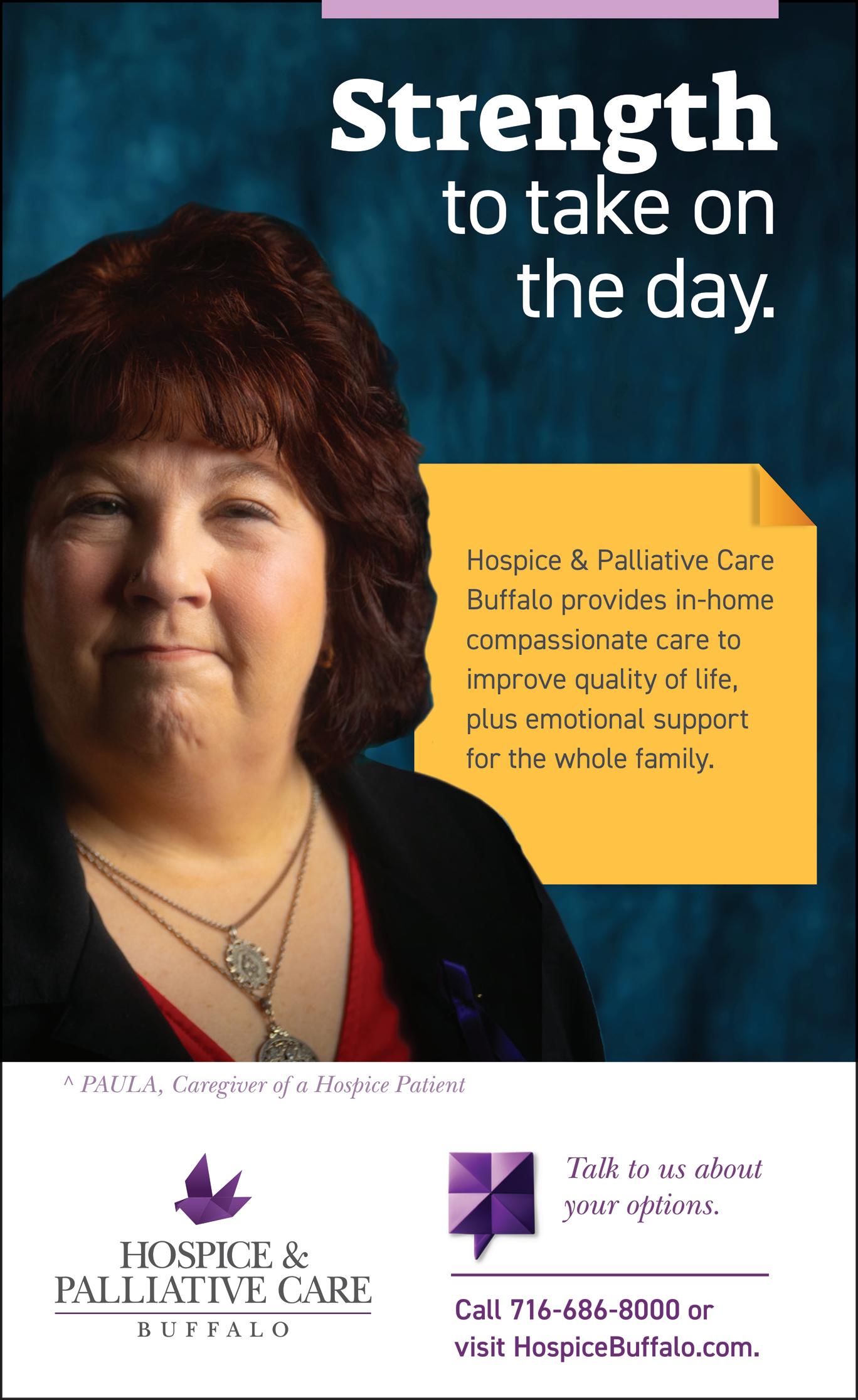
An oncology patient for more than fifteen years, Maryann Salvadore has learned her fair share about research, preparedness, and self-advocacy.

It’s more important than ever
by Olivia Guthrie
DESPITE ITS necessity and direct effect on patients, the healthcare industry operates similarly to other industries: transactional, i.e. payment for service. Whereas people can choose to avoid some businesses, as patients, they depend on medical providers and services, which creates a unique dynamic. Nevertheless, assuming we can rely entirely on medical providers for every solution is both impractical and unfair. Medical
professionals are people, too; like everyone else, they have bad days, experience stress, and can become overwhelmed. Recognizing this emphasizes the importance of patients being partners in their own care and advocating for themselves, especially now, when most regions— including ours—are experiencing a persistent shortage of physicians and nurses. Patient advocacy can be challenging but is crucial to obtain the best care. Maryann Salvadore, an oncology patient for the past fifteen years, recognizes the importance of understanding her disease. After a 2009 diagnosis of multiple myeloma, a complicated, incurable blood cancer, “I spent hours familiarizing myself with the ‘language’ of my specific cancer,” says Salvadore, who began online with a nonprofit organization that provides research funding for multiple myeloma. In gathering information, Salvadore advises avoiding websites ending in “.com,” in favor of research institutions. Being armed with the latest information coming out of those places allowed her to play an active role in her team’s
medical decision-making, something many patients may not realize they have the right to do. “I was able to turn down treatment options and choose ones I felt gave me more of a chance,” says Salvadore, who stresses that patient advocacy is a “collaborative exercise”— not accusatory or disrespectful, as she knows many patients feel.
A critical component of patient advocacy is seeking a second— or third—medical opinion; this is especially true after receiving a terminal diagnosis. “I always use the car buying analogy,” Salvadore says. “Most people, when buying a new car, will test drive more than one model or compare the pricing and availability between a few dealerships. Your health is so much more important than a vehicle purchase; why would you value it less?” The analogy makes getting additional opinions seem obvious, but Salvadore says newly diagnosed patients often tell her they’re reluctant to get a second opinion for fear of upsetting their original physicians and having to undergo additional testing.
At what price? Salvadore credits her preparedness and self-advocacy for giving her the confidence to make critical treatment decisions that kept her disease manageable for fifteen years. She’s grateful for her care teams, particularly when she was first diagnosed, noting they always addressed her questions without rushing through appointments. In 2024, Salvadore admits her treatment facility is understaffed. While she trusts her providers, they must prioritize appointments for patients whose disease—unlike Salvadore’s—is not stabilized. She doesn’t hesitate to say our community’s shortage of medical professionals has “absolutely” affected patient care.
Children can’t always communicate their symptoms thoroughly, making it challenging for medical professionals to assess their needs. Jennifer Glogoza, a pediatric nurse and mother, understands this challenge from both perspectives. “Parents
obviously know their children best,” Glogoza emphasizes, highlighting the importance of parents advocating for their children during medical assessments.
Parents’ knowledge of common child illnesses can help avoid inaccurate diagnoses and prolonged treatment plans. According to Glogoza, symptoms of viral and bacterial infections are commonly misinterpreted in pediatric care. “We see a lot of patients brought to urgent care and prescribed antibiotics that most likely were not needed,” she says, adding that parents should be able to differentiate between the two diagnoses to prevent risk of unnecessary antibiotic resistance.
Understanding pediatric health issues requires relying on information from credible sources. “There is a growing number of parents who are misinformed when it comes to a lot of medical issues,” Glogoza says, citing the increasing number of parents seeking medical advice on social media platforms. While access to medical information is great (thank you, internet), an abundance of misinformation can complicate matters. “On the one hand, they are asking questions and trying to educate themselves, but we know these are not all reliable sources of information,” she notes.
Glogoza recalls a time when her advocacy impacted her child’s treatment. Her son was hospitalized for four days after contracting a virus she was not familiar with. Due to limited physician availability, she researched potential treatment options. After she learned that recovering at home was a viable option, Glogoza suggested a different treatment plan, and her son was released later that same day.
Patient advocacy, for yourself or a loved one, is vital to navigating the complexities of the healthcare system, even when there aren’t staff shortages. The collective effort contributes to better-informed medical decisionmaking and improved healthcare experiences. If you wouldn’t allow any other business or professional to make decisions without your input, why make the exception for the person in control of your health?

MEDICAL EXPERTS are crucial for obvious reasons: they are societal icons with life-saving skill sets and years of extensive training. However, patients must consider they are but one of many on a given healthcare provider’s daily schedule. Here’s how you can ensure you receive the most appropriate care:
Before your appointment
• Research your symptoms or condition through reliable sources (.orgs, research foundations, medical university studies).
• Gather a basic understanding of the terminology associated with your symptoms or condition.
• Write down questions and bring them with you.
At your appointment
• Be open and honest about symptoms you are feeling and experiencing. This is not the time to be embarrassed.
• Bring someone to your appointment; a second set of ears is helpful.
• Take notes.
• Ask all the questions you have.
• Write down any unanswered questions. You can call the office the next day, use the patient portal, or find answers through other sources (primary care provider, research, etc.).
• Don’t leave without information and referrals for all treatment avenues available.

by Jillian McGarry
WE ALL WATCHED as the COVID pandemic laid bare the interconnectedness of our global health—and how important collaboration is to shared well-being. Five years after the first reported cases—and shaped forever by those experiences and newfound empathies— today’s medical students work beyond the classroom, learning to practice medicine in ways that address the wellness of the patient in front of them as well as the global healthcare system.
Medical students at University at Buffalo’s Jacobs School of Medicine and Biomedical Sciences train
to work in this evolved landscape in the new Well Beyond Curriculum. The curriculum development team—practicing medical doctors, community leaders, key stakeholders, focus groups, and professors—began drafting coursework in 2019 to prepare the next generation of doctors to not only meet health needs in the field but also to address root causes in the healthcare system.
“The Well Beyond curriculum empowers our students to not just master scientific knowledge but to go beyond it, to learn early on how to take what they’re learning in their classes and to put it to use right away in real-world settings with patients and out in the community,” says Allison Brashear, vice president for health sciences and dean of the Jacobs School.
This coursework employs hands-on educational exposure centered around whole-patient care, honing scientific literacy and lifelong learning skills, creating systemic change in healthcare, and teaching people to maximize health in their unique situations. Outside the classroom, students seek ways to collectivize this knowledge. For some students, this means spending spring break in Belize teaching lifesaving “stop the
bleed” techniques to cacao farmers, elementary school teachers, children, and families.
We may not see commonality in these groups, but they share a critical need. “Most of them knew a family member or neighbor who experienced a traumatic injury that caused excessive blood loss, so they were very engaged with the material,” says second-year medical student Rachel Yerden. In preparing to go to Belize, students discussed the medical needs of the rural Belize population with Belizean healthcare workers and determined this intervention would have the most lifesaving impact, even long after the students had left.
“The Well Beyond curriculum empowers our students to not just master scientific knowledge, but to go beyond it... to put it to use right away in realworld settings with patients and out in the community.”
An integral part of the Well Beyond Curriculum is ensuring care within the City of Good Neighbors. After a faculty member who provides genderaffirming care noticed difficulty finding like-minded practitioners in the region, a group of students saw a need for a website that provides information about local healthcare resources specifically for patients who identify as LGBTQIA2S+ (standing for lesbian, gay, bisexual, trans, queer or questioning, intersex, asexual, and two-spirit).
These students of the digital age connected with the Erie County Department of Health, where Gale R. Burstein, MD, Erie County

commissioner of health and clinical professor of pediatrics in the Jacobs School, spoke to the need. “People seeking gender-affirming healthcare should know that our region has a solid foundation of clinical and medical resources,” says Burstein. “Now, these resources have been compiled and can all be easily found on the Erie County Department of Health’s website (erie. gov/health). While these interventions may seem minor and distant from the operating room, they are critical to ensuring everyone in the community can readily access the healthcare they need.”
Three other medical students addressed a growing need by developing a new course in partnership with community voices, Buffalo SNUG (Should Never Use Guns), Buffalo Rising Against Violence (BRAVE), church leaders, and neighborhood residents. After a year marked by a significant increase in shootings, Jacobs School students Katherine Foote, Pia Corujo Avila, and Sydney Johnson looked at their curriculum and knew that beyond learning to treat these wounds, a larger gap existed— education about gun violence as a public health issue and how to use interventions with trauma patients to address larger systemic issues.

The new elective—Trauma Surgery and Trauma-Informed Care—centers on providing surgical care that understands the context of gun and community violence. By allowing opportunities for students to spend extended time with patients and their families during recoveries, students learn firsthand how trauma surgeons can provide empathetic care with a deeper understanding of patient experience. As part of the course, medical students work with social workers, psychologists, and case managers—all parts of the healthcare system and patient care team—far outside the medical classroom.
Medical school doesn’t involve as many lecture halls these days. Students evaluate their surroundings and step outside the academic environment to meet needs they see in their community, locally, and globally. Once they’ve earned their white coats, this generation will be prepared to meet the needs of tomorrow even as they provide the care needed today.















































Nonprofits champion equity
by Christine Pearl

IN AUGUST, the Centers for Disease Control and Prevention’s (CDC) Foundation, an independent nonprofit created by Congress to mobilize philanthropic and private-sector resources to support the CDC’s critical health protection work, awarded the Buffalo Center for Health Equity (BCHE), Best Self, and Erie County Department of Health Equity a $3.6 million grant. These groups will work together to assess mental health challenges for children in high risk communities by evaluating what services are being provided and how they can better help these children. The CDC Foundation’s focus has been on collaboration among different sectors, so this grant will fund these three entities effectively working together.
BCHE is a relatively new nonprofit committed to eliminating our region’s health inequities by addressing persistent racial, economic, and other social conditions in our community. Founded in 2019, the Center strives to eliminate health inequities holistically by combining policy analysis, research, advocacy, community engagement, and program development among its partner organizations in government, academia, and faith-based and community membership. The Center focuses on the social determinants of health: conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health and quality-of-life outcomes. Examples include safe housing, transportation, and neighborhoods; racism, discrimination, and violence; education, job opportunities, and income; nutritious food access and physical activity opportunities; and quality of air and water. These factors all impact human health, and addressing one or two while ignoring others will not create long-lasting, systemic changes.
Chronic disease is one of the major issues BCHE is tackling. Founder and CEO Pastor George Nicholas points to diabetes and hypertension as two diseases more common in their focused neighborhoods on the East Side. “Data shows us that if you’re African American and live in one of these communities, you’re more than 300 percent more likely to have one of these diseases than if you were white and live outside of that community. Those are alarming statistics.” Nicholas points out that all social determinants of health drive poor outcomes with these diseases.
Addressing racism and having meaningful conversations about race is part and parcel of the work BCHE does. “We are unapologetic about engaging in conversations about race, because structural and systemic racism, and historical racism, have been historical factors in the poor health outcomes for African Americans, not only in Western New York, but across the country,” IN WESTERN NEW YORK 2024
PHOTO BY STEPHEN GABRIS
explains Nicholas. “And we saw evidence of that, certainly when COVID hit, and the fact that if you had diabetes, hypertension, heart disease, or asthma, you would be more vulnerable to the virus, and those were the communities that had high numbers.”
BCHE has a core belief that five aspects of a family’s life have to change to improve health outcomes: every child needs to be at grade level in reading and math; housing must be quality and affordable; everyone should be operating at maximum level of employment; and healthy food and trusted primary care doctors must be accessible. These five factors are related, and all five need to happen to see large scale changes in health outcomes.
BCHE board member Dr. Joseph Fritz points out the great need for trusted, community-based medical professionals in these neighborhoods. When underserved communities have untreated health conditions, they often lead to more intensive and expensive treatments in hospitals, which are created to treat acute issues, not the

underlying social determinants of health. Hospitals aren’t built to be value based and trusted management resources for chronic health issues. That’s why community engagement is a key component to BCHE’s plan.
Consultant Dr. Ana Stearns, MD adds that community engagement within BCHE and its partners is crucial to the organization’s success. Anyone
with any educational background and work history is welcome to volunteer.
“Reach out to us,” she says. “We have a lot of different initiatives and programs and we can link up people with their skills. There is always space for everyone to come. We want people to be inspired. Change happens when it’s everyone’s problem. We want to be proactive about that.”

What do the people working behind the scenes at BCHE want Western New Yorkers to know about their mission?
“These are good people who have the odds stacked against them,” says Fritz.
“Unfortunately, aid is often seen as ‘handouts that promote laziness.’ The real culprit is failure to address root causes. With a highly collaborative strategy that uses data to guide programs and connect resources to family needs, our goal is sustainable change that gradually reduces the need for special assistance. We are collectively better when the least of our brethren have an equitable opportunity to thrive in our economy.”

DR. JOSEPH FRITZ and Pastor George Nicholas combined their talents and passion for helping others to form a powerhouse team at Buffalo Center for Health Equity. Fritz, who retired as the CEO of DENT Neurologic Institute in December, is now on the board for the BCHE. Under Fritz’s leadership, DENT became one of the top eight neurology practices in the United States. Nicholas recently retired as senior pastor of Lincoln Memorial United Methodist Church on Masten Avenue. He’s the founder and CEO of BCHE and has been working to address health inequities based on race, geography, and economics across Buffalo and Western New York for years. Their partnership— one of faith, education, and profound passion for service—is dedicated to helping underserved populations in Buffalo.


Being active is more than “exercise”
by Amanda Jowsey
BEING PHYSICALLY ACTIVE doesn’t just mean “working out,” i.e. weightlifting or intense cardio. Moving your body—even when it’s not about counting reps or measuring heart rate—is its own measure of success when it comes to well-being. Consider those three fitness rings on the ubiquitous Apple watch: only one is for exercise minutes, while the other two measure movement calories and the number of times you stand up in a day. Exercise is important for some
goals, but those other two play a big part in boosting and maintaining overall health.
Focused exercise is often achievement-based: weight loss, muscle building, cardio fitness, even winning a game. Movement, however, refers to a wide range of activities that involve physical motion, from daily tasks like cleaning or shopping to hobbies like gardening or bowling. Movement, like exercise, can have a profound impact on physical and mental health.
“The benefits of physical activity apply to healthy people of all ages, people at risk of developing chronic diseases, and in people with existing chronic conditions,” says Ann Kuhn, Ph.D., assistant professor of exercise and nutrition sciences at the University at Buffalo School of Public Health and Health Professions. “Health benefits include lower risk of all-cause mortality, cardiovascular disease, hypertension, type 2 diabetes, and certain types of cancers. Other benefits include improved cognition, reduced risk of developing dementia, reduced adverse mental health outcomes, i.e., anxiety/ depression, weight loss, and prevention of weight gain. However, health benefits are not the only reason to be active, as physical activity provides a way for people to have fun, be with other people, and enjoy nature.”

Conversely, says Kuhn, more time spent in sedentary behavior increases the risk of those same conditions.
“Any physical activity is better than no physical activity,” she says.
For optimal adult health, the Centers for Disease Control and Prevention recommends 150 minutes of moderate intensity physical activity each week and two days of strengthening activity.
Moderate intensity is what most people think of as “exercise.” But those minutes don’t have to take place in a gym or gym setting and, more importantly, continuing the movement beyond those minutes—i.e. not spending the rest of the day at a desk or on a couch—is just as important. We should be aiming to move our bodies consistently throughout the day.
We’ve probably all heard the hack about parking our car farther away when we go to a store or taking the
“We’re trying to reframe walking and running from being this performancebased activity to more of a practice .”
stairs instead of the elevator, but are we doing it? Or setting a timer at work to get up and walk at least once an hour? Walking while on the phone? Using the upstairs bathroom when downstairs? Dance breaks while waiting for the microwave? Or starting each day with a five-minute stretch or walking in place? To paraphrase Isaac Newton, a body in motion tends to stay in motion, and beginning the day with movement makes it easier to move our bodies all day long. Forming habits is the easiest way to make more movement a mindset instead of an “ugh, do I have to?”
The idea of daily “exercise” is intimidating to many people. Chris Muldoon, long-time runner and

A STRONG SUPPORT SYSTEM can provide the encouragement and motivation you need to incorporate more movement into your daily life. If you use the measures on a watch or FitBit, use the ability to set challenges with friends to meet those daily goals.
Since using a check-in with friends, “I move 100 percent more than I was a few months ago—almost always hitting my walk goal,” says Sarah Walczak. “We discuss why we didn’t hit our goal that day or week, what’s going on with work or in our personal lives. We encourage each other with mostly kind words, and we get together to walk, so it’s more fun.”
Walczak notes that check-ins can be daily, weekly, etc. One virtual group, VideoFitness Morning Madness has been checking in for over twenty-five years! The group first met on the VideoFitness online platform and later migrated to Facebook.
“Goals are individual, but it is easy to be motivated to try new things from other people in the group,” says Lisa C. “At various periods in my life, having accountability groups helped keep me moving when I sometimes didn’t feel like it.
“We’ve all had times when we need some motivation,” adds Jennifer Ann. “We are a ‘kind words’ kind of group and always remind one another that something is better than nothing—five minutes of stretching, a short walk, etc. It is one factor in keeping me motivated and I hope by checking in, I also motivate others.” — A.J.


Dr. Alisha Lall
running coach, co-founded Strideful with this in mind. Strideful is a company that focuses on walking and running for mental health. Developed with licensed therapists, Strideful’s running and walking plans encourage sustainable movement to enhance mood and manage stress. That word, “sustainable,” is key.
“When you say exercise, there’s some weight to that and you get into these preconceived notions of what counts as exercise and what doesn’t, and it usually errs on the side of going harder or longer than you necessarily have to. There’s something to redefining it and breaking down that barrier,” he says. “We’re trying to reframe walking and running from being this performancebased activity to more of a practice the same way that someone would get into a meditation practice or yoga practice.”
Understanding how clients rate the importance of mental health versus physical activity was a large part of Strideful’s research. As part of the “movement plans,” individuals receive coaching tips and psychology-based tools, as well as a movement journal, to support them on their wellness journeys.
“It’s about helping people change their perspective and have a better relationship with physical activity,” says Muldoon. A long-term approach to wellness fosters self-acceptance and consistency.
Brian Harper, a coach at Buffalo’s Pace Run Studio, also values “a combination of mental and physical health” when it comes to staying active, he says. Reframing thinking from dreading exercise to enjoying activities is a game changer. “Try to find something that appeals to you,” he advises. “Whether it’s roller blading, biking, hiking, swimming... Mix it up. There’s a lot of stuff out there.”
Harper commonly sees clients hold themselves to unachievable standards or an all-or-nothing mentality. He stresses longevity and consistency on wellness journeys. “There’s not a start and stop,” he points out. “You’re not training for a competition. You want to be active for as long as you can.”
The little things count as much as the big things. If you didn’t go to the gym but did yard work, “that still counts,” Harper says. “It’s about being mentally healthy as much as physically.”

Dr. Natalie Penn is a Western New York native who received her medical degree from the Jacobs School of Medicine and Biomedical Sciences in Buffalo, NY. She subsequently completed both her Internal Medicine Residency and Gastroenterology and Hepatology Fellowship at the University of Rochester Medical Center in Rochester, N.Y. Dr. Penn will be seeing patients in the Williamsville and Orchard Park offices.

A native of Western New York, Dr. Corey Higley received his medical degree from New York Institute of Technology College of Osteopathic Medicine. After Medical school, he completed his internship and residency in internal medicine at Georgetown University Hospital in Washington, D.C. He completed his Fellowship in Gastroenterology and Hepatology at Rush University Medical Center in Chicago Illinois. He also has a Master of Public Health from the State University of New York at Albany. Dr. Higley will be seeing patients in the Williamsville office. Celebrating
Providing

Prioritize your health and well-being with OWM Integrative Wellness. We combine cutting-edge medical treatments with holistic practices to support and enhance your body’s natural healing abilities. Whether you're looking for pain relief, stress management, or a personalized wellness plan, our expert team is dedicated to guiding you every step of the way on your path to better health.
OUR SERVICES:
Regenerative Medicine: Cutting-edge treatments to repair and rejuvenate your body.
Functional Medicine: Personalized care plans tailored to your unique needs.
SonoCiné Whole Breast Ultrasound provides advanced breast cancer screening for dense breast tissue, detecting small tumors that mammograms may miss, and is FDA-approved as a secondary screening tool.
On-site Partnership with Prenuvo: Full Body MRI Imaging Trailer for Early Detection of Over 500 Cancers and Diseases. We also provide a comprehensive range of physical medicine, healing treatments, IV immunotherapies, and much more.

by Christine Pearl
LIKE THE REST OF the country, Western New York is experiencing a shortage of nurses and doctors. According to the American Association of Colleges of Nursing, the Registered Nursing workforce capacity is expected to expand by six percent over the next decade, from 3.1 million in 2022 to 3.3 million in 2032. With workforce exits and US need factored in, this translates to a projected 193,100 RN openings each year through 2032. Similarly, the Association of American Medical Colleges projects the US will be short as many as 124,000 physicians by 2034, more than a third of them primary care providers. An estimated thirty percent of Americans don’t have a primary care physician, due in part to the shortages.
While we might be feeling these effects for a

while, local colleges and hospitals have plans to address these shortages.
The Erie County Medical Center (ECMC) has noticed the greatest need for nurses in their mental and behavioral health departments.
“There’s more need here than I’ve ever seen before,” says Charlene J. Ludlow, MS, RN, CIC, and ECMC senior vice president of nursing. “ECMC has 136 inpatient beds for behavioral health, and we are always full. We’ve seen a lot more people starting to understand the feelings they’re having and some of the changes that are going on, and they are reaching out for mental health services. We also have outpatient facilities as well.” Ludlow points to the trauma of living through the COVID pandemic, and increased stresses at home and work for this increase.
To combat the corresponding rise in stress levels among staff, ECMC has implemented several incentives to improve work life for employees. There is a serenity room where staff can take a few minutes to relax and recharge in recliners and massage chairs. An ECMC gym is available for staff to focus on their own health. Scholarships for staff to attain higher levels of education has been a popular incentive. To train and recruit new nurses, ECMC has relationships with all local nursing schools in WNY. Student nurses learn onsite during rotations, which removes an unknown and attracts local students, a factor that allows the schools and ECMC to collaboratively cultivate the next generation of nursing talent.
For physicians, the most pressing shortage nationally and locally is among primary care doctors. University at Buffalo’s Jacobs School of Medicine and Biomedical Sciences recognizes its power to implement changes in the local landscape, as seventy to eighty percent of WNY physicians have connections to the school.
“In true Buffalo fashion, we need more quarterbacks to manage our patients,” says Dr. Allison Brashear, vice president for health sciences and dean of the Jacobs School. “We are really leaning into that metaphor because healthcare is changing, and the primary care doctor is the one calling the plays and making sure that the patient gets to the right specialist when they need to.”
The Jacobs School’s multi-prong approach focuses on lowering or eliminating student debt while fostering a passion for primary care. A generalist scholars program encouraging interested students go into primary care and diversify the physician workforce, and the WNY Medical Scholarship Fund offers incentive. The Jacobs School has seen an increase in students applying for admission since the COVID pandemic began, and its goal is to keep students here for residency post-graduation and, ultimately, to treat patients and, eventually, raise families.
Brashear mentions a shift in US medicine that focuses on primary care and keeping people outside of the hospital and home with friends and family. The most important thing is to have a partner in your healthcare journey, and Brashear believes a robust network of primary care doctors keeps people healthy and prevents sickness.
These plans can all succeed, but help is needed. You can invest in the health of yourself and fellow Western New Yorkers by donating to the WNY Medical Scholarship Fund on the Jacobs School’s website; money raised supports the education of local students who have demonstrated excellent academics, financial need, and a commitment to staying in WNY after medical school and residency.
Additionally, encourage students in your life to consider medical career paths. ECMC offers summer programs and campus tours that allow high school students to see the many jobs required to run a hospital. With time and dedication, this workforce can grow.

by Amy Lynn Hardy
HAVE YOU EVER felt like you were getting a cookie-cutter remedy for your illness or pain? Or perhaps that your doctor was under such pressure to get to the next patient that they didn’t have adequate time to get to the root of your problems?
Doctors are busy people. General practitioners (GPs) average around 2,000 (or more!) patients and see up to fifty a day; they are simply not able to spend extended time with each one. Many doctors practice conventional medicine, which adheres to a disease-centered approach in treatment protocols, often ending with a bottle of prescription medication or a referral.
Conventional medicine is by no means bad— it is an essential system that saves lives—yet it sometimes has blind spots in the holistic nature of the human body and interactions with food
and environment. This is where functional medicine shines.
According to local functional medicine practice Invision Health’s website, “functional medicine integrates traditional medical practices with integrative medicine, creating a focus on prevention and treatment through nutrition, diet, and exercise; use of the latest laboratory testing and other diagnostic techniques; and prescribed combinations of drugs and/or FDA approved medical foods, nutritional pharmaceuticals, botanical medicines, supplements, therapeutic diets, detoxification programs, or stressmanagement techniques.”
Functional medicine practitioners are typically able to spend more time with their patients, recording their complete medical history and evaluating interactions among genetic, environmental, and lifestyle factors that can influence long-term health and complex chronic disease. It is more patient-centered, looking “upstream” to understand the origins of the specific ailment.
Our bodily systems are all interconnected, and functional medicine aims to analyze these interactions and see the synergistic effect on the body. Take the gut, for example. Something as simple as taking birth control pills can deplete key nutrients that impact the thyroid; the

thyroid in turn impacts motility of digestion and elimination pathways. The good news is that simple changes often have positive effects, and sometimes a single root cause contributes to multiple ailments.
Sarah Marlette, a functional medicine licensed nutritionist and founder of Nourish Thrive Glow, defines functional medicine as “a holistic, whole systems, biology-based approach that addresses the root cause of a medical issue as opposed to giving a blanket diagnosis.” She got into functional medicine because she wanted answers about her own medical issues. “My passion grew from pain,” she says. “I was given one thing to fix a problem, but it created another problem. So, I thought, ‘there’s got to be a more sustainable, holistic approach.’” Through her studies of functional medicine and nutrition, she was able to find solutions for her own body and also help others find theirs.
Women often come to Marlette with hormone imbalance, desperately seeking answers to hair loss, weight gain, or irregular cycles. “When working with someone dealing with hormonal issues, it’s not just the hormones,” Marlette says. “It’s generally going to be blood sugar, digestion, potentially detoxification pathways, or lack of sleep.” In an appointment, a patient will typically have their bloodwork analyzed and then have a lengthy conversation about their medical history, lifestyle, digestion, etc. “[Seeing a functional medicine practitioner] is a little bit like storytelling,” Marlette says. Therapeutic interventions are often multifaceted and entail long-term lifestyle changes. They are “not just nutrition, but lifestyle interventions, sleep interventions, and sometimes supplementation interventions as well,” Marlette says. “I want to get all the pieces and I want to get the ‘why’—to get to the root cause.” This requires commitment, consistency, and followthrough, i.e. it’s not the quick fix many people seek.
Marlette looks at it this way: “What can we do with what we have, and how can we add in more as opposed to restrict? Most of us are so depleted of nutrients because either we’re not eating enough or we’re not eating the right things. We’re inside too much. Our circadian rhythms are disrupted. Our digestion is off because it boils down to you are not what you eat, you are what you absorb.”
Some other pro tips from a functional medicine standpoint are these:
Get daily sunlight and movement for ten to thirty minutes to support your circadian rhythms. Eat meals around similar times each day to improve blood sugar; have breakfast within one to two hours of waking and dinner three to four hours before bed. These two simple practices will start to regulate hormones and digestion.
Other functional practices and practitioners around Western New York include Buffalo Functional Medicine, OWM Integrative Wellness, Pana Health, Benna Lun BSc ND, Michelle Adams Functional Wellness, and Sanford H. Levy, MD.
A Google search will also yield many results for naturopathic or integrative doctors practicing functional medicine. Though not all visits are covered by health insurance, working with a functional medicine practitioner offers crucial insight about your health and may change your life.

IN JUNE, I had my first personal experience with functional medicine after I was bitten by a tick and diagnosed with Lyme Disease. (I never even noticed the bite, so be vigilant after you go outside!) After becoming extremely ill for about a week, I was prescribed six weeks of the antibiotic doxycycline from my general practitioner. Soon after, I met with the naturopathic doctor Kim Howes of OWM Integrative Wellness, one of Western New York’s top Lyme disease specialists.
The appointment went deep into my medical history, lifestyle, cycle, and eating habits. She prescribed botanical supplements known as herbal biotics to follow the course of doxycycline to eradicate the remaining Lyme bacteria; oregano oil; and Cat’s Claw support normal microbial levels. I was also advised to take a probiotic, as my gut health was in distress from long-haul antibiotics. During our follow-up appointment five weeks later, she ordered eight blood panels to check organ function, vitamin deficiencies, hormone levels, and thyroid health post-Lyme. I feel like I’m in really good, thorough hands, which is imperative because Lyme disease bacteria can hide in tissue and attack later in life when the immune system is compromised. I learned so much about the disease with her. We also talked about my overall health.
For years, I’ve suffered from irritable bowel syndrome, difficulty losing weight, a sensation of food getting stuck in my esophagus, and bloating after meals. Dr. Howes explained that these are attributed to inflammation in my gut; “something in there is fermenting,” she said. But I never could figure out what it was. There are optional stool panels that can be done, but they are expensive, so I opted out for the time being. After years of eating dairy, gluten, and processed foods, it seems my body has begun to scream, “stop!” with these symptoms. I’m now eating less dairy and notice a major difference in my digestion. I will transition to a paleo diet in the next few weeks. It’s a sacrifice to give up some favorite foods, yes, but feeling much better is worth it. I am also trying Sarah Marlette’s morning walks and buying a sun lamp for the Buffalo winter. — A.L.H.
Examining health advice you’ve heard your whole life
by Nancy J. Parisi
AS IN ALL sectors of our wild and wonderful human society, health has its share of oft-repeated chestnuts of dubious veracity. Often these statements are borne of speculation and outdated understandings that add up to immense inaccuracies. If you’ve heard any of the popular myths below, read on to put them in proper context.
Exercise turns fat into muscle. “Ugh! That is a giant misconception. We’ll start here: fat cannot turn into muscle,” says Shannon Connors, owner of Shannon Connors
Fitness and 2023 Spree Best Of winner for Best Outdoor Fitness Classes. “Fat and muscle are two distinct types of tissue. Fat is stored energy in your adipose tissue while muscle is made up of protein fibers. When someone loses fat because of diet and exercise, they [may also be building] muscle. It happens at the same time, but fat is not turning into muscle; [you may just be changing the proportions of the two tissues]. Likewise, if you stop exercising, muscle does not turn into fat; [the proportions have just begun to reverse]. The key is this: get moving!”
Wait at least an hour after eating before swimming.
“This statement is based upon one published in a Boy Scout handbook from the early twentieth century,” says Dr. Eric Waffner, an internal medicine specialist affiliated with Buffalo Medial Group. “There is no science to back it up.”
Multivitamins keep you healthy.
“A good, quality multivitamin can be beneficial if you have nutrient deficiencies,” says Connors. “Let’s say you have a diet high in processed foods and don’t eat a lot of fruits and vegetables. You
will probably have vitamin C and K deficiencies and, in that case, taking a multivitamin will have some health benefits. But individuals who eat a balanced diet daily will have minimal benefit. Use food over supplements. The best option is to strive for a healthy, well-balanced diet full of lean proteins and healthy fats that include eggs, olive oil, nuts, et cetera.”
Expert advice points to avoidance of supplements, which aren’t FDA regulated the same way drugs are and echoes Connors in advising vitamins come from food and not pills, as many studies have linked supplements to adverse health risks.
“Oh no, that’s so not true,” laughs Kathleen Granchelli, owner of Pace Run Studio and founder of Buffalo Run Club. “If we have been training outside, changing to running in a different temperature, climate, or scenery should not affect how you would get a virus.”
In fact, being in the cold without a coat seems to stimulate the immune system rather than destroy it. This myth seems to be left over from a time when science was lacking and people searched
for “logical” explanations.
However, it’s not quite that simple. Cold temperatures can increase your chances of getting a cold but because of viruses, not weather. A 2015 study conducted on mice and published in the Proceedings of the National Academy of Sciences did conclude that having a cold nose can make you more likely to catch a virus if exposed. Cold viruses try to enter the body via the nose, but usually get trapped in mucus, which is passed back into the body, where the virus is neutralized by stomach acids. But when we inhale cold air, the nasal passage cools down, which slows the movement of mucus. This means live rhinoviruses—which thrive in cold weather— have more opportunity to break through the mucus barrier and into the body.
In short, cold temperatures do not suppress the immune system as a whole, but can suppress the localized immune system inside the nose. Which means if your kid is outside without a jacket— alone—their chances of catching a cold don’t increase.
While we’re on the subject, you also won’t get sick if you go outside with wet hair and you don’t lose most heat through your head—just about



















ten percent of total body heat, i.e. the proportionate amount to the skin on your head. It’s just that if the rest of the body is covered, most of the heat escaping will be through an uncovered head.
Organic food is better for you. Compared with conventionally farmed produce, organic produce has the same vitamins, minerals, antioxidants, proteins, lipids, and other nutrients, as well as the same number of calories. Both are beneficial to your health and the most important thing is to include fruits and vegetables in your daily diet.
In 2012, a review of data from 237 studies conducted at the Center for Health Policy at Stanford University concluded there were no convincing differences between organic and conventional foods in nutrient content or health benefit. The organic ban on synthetic chemicals also fails to improve food safety in the US, since pesticide use is now significantly regulated in conventional farming. If your primary reason for buying organic foods is to further reduce pesticide risk or to support environmentally and animal friendly farming practices, the additional cost may be worth it to you. More, when it comes to organic meat, poultry, eggs, and dairy, the animals must have not been given any antibiotics or growth hormones.
“When food is grown with fewer synthetic chemicals, that is fewer chemicals going into the ground and our bodies,” says Jen White, marketing and communications manager for Lexington Co-op Markets. “If you determine that this is the healthiest option for you, then it would be true that organic food is better for you. There are a lot of hoops to jump through to receive the USDA certified organic label. The Co-op does have an abundance of organic products, including produce at multiple price options.”
10,000 steps a day is best for health. Not quite. This one seems to have come from a pedometer produced in Japan after the 1964 Olympic Games in Tokyo; its name translated roughly to “10,000 steps meter,” and somehow created a global walking aim that persisted for decades.
In recent years, scientists have deduced we don’t need quite so much;
benefits—including premature death from heart disease—began with as few as 4,000 steps and plateau at about 7,500. More won’t hurt you, but likely won’t confer additional benefit.
“Walking is one of the best things that you can do for your body,” says Connors. “It’s the least impactful exercise on our joints and accessible, doesn’t cost money, and provides lubrication to the joints. The older you get, you’ll reduce your need for a knee or hip replacement and walking helps to improve your cardiovascular health by improving circulation. Walking reduces stress and cortisol, decreases body fat, and is easily incorporated into everyday life.”
But also consider…
Walking is enough to keep you fit as you age.
Beginning around age thirty, our muscle mass begins to decline, which contributes to the fat we start to see creeping on (muscle burns more calories than fat). To combat this, we need strength training in addition to
cardiovascular exercise like walking. As we lose strength, activities can become more difficult because we don’t have the muscle to power them; as we age, that can mean increasing loss of independence. So whatever cardiovascular exercise you choose, complement it with two to three strength training sessions a week. Your body will thank you!
Chocolate causes acne.
Experts suspect it may have been parents who perpetuated this myth lumping other junk food like potato chips and pizza into the group of acnecausing culprits. “The short answer is not really,” says Woodhouse Spa esthetician Dara Thomas. “When it comes to breakouts, the majority are caused by hormone imbalances or not taking proper care of your skin.”
Thomas does add, however, that some ingredients in milk chocolate, such as dairy and sugar, can cause inflammation or breakouts when eaten in excess. A better alternative is dark chocolate which has many health benefits
including antioxidants that help protect the skin from sun damage and can slow the appearance of aging skin.
Acidic drinks and foods are bad for your teeth.
“Lemons are the one food that’s potentially causing damage to tooth enamel, but a slice of lemon in tea or water is fine,” says Julia Kagan DDS, owner of Integrative Dental Arts of WNY. “In excess and in extreme cases, lemons can erode enamel. Coffee and tea are all right, and don’t cause damage to our enamel, but they do cause staining. Sugar is the worst substance for teeth; it feeds all the bad bacteria of gum disease and tooth decay. Enamel is the strongest substance in the body; take care of what you have—brush and floss every day and see your dentist twice a year.”
Sugar makes kids hyper.
Sorry, parents, let them have the cookie. Placebo studies have proven that the sugar-monster theory is all in parents’ heads.

When and how to use the quickest stop
by Judith A. Rucki
THERE IS NEVER a convenient time to fall ill. Weekends, holidays, and the middle of the night can be the worst. Even if you start feeling unwell during your physician’s regular office hours, getting last-minute appointments isn’t always easy.
If your primary care physician (PCP) is not available, do you tough it out, head for the emergency room (ER), or go to an urgent care facility? Originally intended to take pressure off emergency rooms, urgent care facilities can treat a host of conditions, but are not intended to be emergency rooms nor replace primary care physicians (PCPs). So when to go?
“Certain conditions are potentially life threatening. If anybody has chest pain or severe abdominal pain, I’d recommend they go to the ER [or call 911],” says Dr. Michael Mineo, emergency physician and chief medical officer of Kaleida Health. “Otherwise, if it’s not a big emergency, urgent care is okay for many conditions.”
Know your PCP’s preference before illness
strikes. They may want you to call first if you’re experiencing common illness or minor injury. You may be able to get advice over the phone.
“If you have pain in just a fingertip or toe, then there are other options,” Mineo says. “I would call your [PCP], and they can best judge whether to have you go to the emergency department or go to urgent care.”
Urgent care facilities, also referred to as walkin clinics, provide fast and immediate services to patients with conditions, illnesses, and injuries that don’t warrant a visit to the ER, where wait time could be longer if your condition is not lifethreatening.
“At the emergency department, we treat everybody who comes to our door, but we have to triage patients and determine who is more likely to have a life-threatening condition. So unfortunately, some people may have to wait longer, and people who come in after them may be seen first,” Mineo says.
An urgent care facility visit may also cost less than a visit to the ER. Urgent care fees can, however, depend on several factors, including health insurance and care provided. If you have insurance, you may need to pay only a copay. Check with your health insurer before you need urgent care and learn which facilities are covered by your plan.
If you don’t have insurance, check with the urgent care center to learn what their policy is regarding payment.
The Urgent Care Association (UCA) is one of the nation’s premier independent organizations for urgent care. With locations in Amherst,
Buffalo, Depew, and Orchard Park, WNY Immediate Care has met the UCA’s rigorous accreditation standards, where members are recognized for the highest quality and safety requirements. Virtual care is available at each of these four locations twentyfour hours a day, seven days a week. Visit wnyimmediatecare.com for locations, office hours, to reserve a time, or to start a virtual care visit. WNY Immediate Care accepts most major insurance plans.
For uninsured patients and those with high deductible insurance plans, a prepayment deposit is required.
WellNow Urgent Care is considered one of the best urgent care providers in the United States. Find locations locally in Amherst, Batavia, Buffalo, Cheektowaga, Depew, Dunkirk, East Amherst, Grand Island, Hamburg, Lewiston, Lockport, Niagara Falls, Orchard Park, Springville, West Seneca, Wheatfield, and Williamsville. Visit wellnow. com for office hours and virtual care, which is available twenty-four hours a day, seven days a week. WellNow works with all insurance plans and has a flat rate fee for self-pay visits.
Focus Urgent Care has locations in Amherst and Williamsville. Locally owned and operated, it claims short wait times and fast results and accepts most major insurance plans. Patients are encouraged to bring insurance questions to a team member. See focusurgentcare.com for more information.
Pediatric & Adolescent Urgent Care of WNY has two convenient locations in Williamsville and Orchard Park. There is always a pediatrician on site, and they are open from 10:00 a.m. to 10:00 p.m. every day, including holidays. No appointment is necessary, and they are in network with most major and local insurance companies. Check pedsurgentcare.com for more information, including out-of-network and self-pay policies.
Excelsior Express—with locations in Amherst, East Amherst, Orchard Park, and Niagara Falls—allows patients at least two years of age direct access to expert orthopedic care—think broken bones! Walkins are accommodated, but scheduling is encouraged. Excelsior accepts most major insurance plans, and a co-pay may be due at time of treatment. Patients are asked to contact their insurance providers to verify that Excelsior accepts their coverage. See excelsiorortho.com for more information and to make an appointment.

URGENT CARE facilities can treat a wide range of illnesses, infections, diseases, and injuries but are intended primarily for conditions that need immediate care but are not life-threatening emergencies. Chronic conditions— unless they result in an acute episode—are best managed by a PCP.
Examples of good urgent care use include:
• Abdominal pain
• Open wounds that might need stitches
• Cold and flu symptoms
• Conjunctivitis (pink eye)
• COVID
• Dehydration
• Diarrhea
• Ear infections
• Eye problems (minor)
• Fever without a rash
Injuries:
• Abrasions
• Abscesses and cysts
• Animal and insect bites
• Broken bones
• Burns
• Cuts and lacerations
• Foreign body removal
• Food Poisoning
• Respiratory syncytial virus (RSV)
• Sexually transmitted infections (STIs)
• Shingles
• Sinus infections
• Sore/strep throat
• Upper respiratory infections
• Urinary tract infections (UTI)
• Yeast infections
• Vomiting
• Frostbite
• Hypothermia
• Minor head injuries
• Nosebleeds
• Poison ivy, oak and sumac
• Sprains and strains
For diagnostics in a hurry, call ahead to see if the facility has what you need. Some available tests might be:
• X-rays
• Complete metabolic panel
• Chem 13
• COVID testing
• EKG
• Electrolyte testing
• Glucose
• STD testing
• Monkeypox testing
• Mono screen
• Pregnancy tests
• Rapid Flu
• Rapid Strep
• STD testing


Choose
your diet for your health
by Amy Lynn Hardy
“LET THY FOOD be thy medicine and medicine be thy food,” Hippocrates once said, and as much as we might want to honor this sentiment, nachos and hotdogs are still pretty popular. Compared to other countries, the Standard American Diet is far less healthful. In addition to the American penchant for large portions, prepackaged foods, refined grains, red meat, processed meat, high-sugar drinks and snacks, and low intakes of fruits, vegetables, whole grains, and lean proteins, our food also contains much more high fructose corn syrup,
refined sugar, seed oils, antibiotics, growth hormones, and pesticides in our food than, for example, the European Union, which abides by different regulations governing additives.
According to the Sustainable Restaurant Foundation (SRF): “While 783 million people worldwide are affected by hunger, over 2.6 billion people are considered overweight or obese.” To be more specific, the obesity rate in the US is over forty percent, diabetes at almost six percent, and cardiovascular disease at a whopping forty-eight percent.
Not surprisingly, those numbers add up to high costs when it comes to medical care and overburdening the system. A 2019 National Heart, Lung, and Blood Institute-funded study put a price tag on American’s bad eating habits: $50 billion a year in healthcare costs, attributable to cardiometabolic diseases such as heart disease, stroke and type 2 diabetes. The research sought to zero in on the national healthcare costs of unhealthy diet habits, which are known to account for up to forty-five percent of all cardiometabolic deaths.
So, how are Americans told to eat? Even as we’re barraged by Mountain Dew and Doritos ads, the United States Department of Agriculture implements a “My Plate” (the new food pyramid) structure for dietary recommendations. This

incorporates (in descending order of recommended consumption) grains, vegetables, proteins, fruits, and dairy. However, in a country where a container of chopped watermelon costs $11.49 and a package of Sour Patch Kids is $2.69, choices often priortize financial health over physical health. The SRF further reports: “Over forty percent of the world’s population is unable to afford healthy food, and one in five deaths is linked to poor diet.”
Furthermore, humans are genetically predisposed to crave sugars and fats, which companies capitalize on by creating and marketing processed foods that push our buttons (think Snickers: sweet, salty, calorie dense, the “you’re a diva when you’re hungry” thing). And then there’s the American need for convenience: takeout, fast food, DoorDash, frozen meals, drive through—the norm for many busy people. Our country makes it easy to eat poorly.
Sigh. Is there any good news here?
“What we eat literally becomes who we are. What we put into our bodies and how we digest it is the foundation for our state of health—or disease.”
Indeed! There is a thoroughly researched diet that claims to be healthy for humans and the planet. In 2023, the 365-page Nordic Nutrition Recommendations (NNR) came out as the most health-conscious and sustainable way of eating. It was created by hundreds of scientists and experts who write: “Overall, we recommend a predominantly plant-based diet rich in vegetables, fruits, berries, pulses (beans), potatoes and whole grains, ample amounts of fish and nuts, moderate intake of lowfat dairy products, limited intake of red meat and poultry, and minimal intake of processed meat, alcohol, and processed foods containing high amounts of added fats, salt and sugar.” Their research examines which macronutrients (protein, carbohydrate, fat), vitamins, and minerals humans need to obtain optimal health at various ages and bases the diet on those findings.
The NNR might come across as strict, but it doesn’t necessarily mean cutting out chicken wings or ice cream forever. It means reducing the frequency of their consumption and eating more plant-based whole foods. Aim to swap out two

BIG BIG TABLE on Hudson Street is a payas-you-can community café that offers fresh meals—fully vegan on Wednesdays—to help combat food scarcity and provide healthy meals to the community. Farm-to-table dining reduces the distance your food travels as well as limits pesticide use. Try also the Grange, Angeline, or Becker Farms.
Fresh Catch Poke Co. is not only nourishing and flavorful but provides a map of where each menu item is sourced.
CoreLife Eatery, with locations in the Northtowns and Southtowns, also serves up nutritious bowls, including warming bone broth for the fall and winter months.
Peace of the Pie in North Collins has generously priced and delicious, fresh options daily, which includes soups, salads, wraps, and paninis. While their desserts are not low in calories, they are made fresh without any additives.
If fast food is the only option, you can choose wisely at Popeye’s by ordering grilled chicken instead of fried chicken. Most fast-food chains also offer vegan/plant-based items that taste just as good! Have you tried the Impossible Super Mighty burrito?! Or Burger King’s Mushroom Veggie Burger? Or Taco Bell’s vegan crunch wrap?
Speaking of vegan, visit Sunshine Vegan Eats, Evul and Guud, Strong Hearts Café, or Buffalo Plant Burger for sustainable nutritious food that won’t make you miss the meat and cheese.

servings of processed foods each week, says Dr. W. Taylor Kimberly, a professor of neurology at Harvard Medical School and the senior author of a recent study linking ultra-processed foods to dementia and stroke. Kimberly shares a good rule of thumb: prepare meals at home as much as possible and when choosing foods outside the home, consider what could be. “If you look at it and think, that could be made in my kitchen, that’s a good indicator,” he said.
Changing diet to improve health has a synergistic effect on the entire body. You can heal your gut, increase your energy, balance your hormones, clear up your skin, and simply feel better. According to nutritionist Dr. Samantha Attard, “Refined vegetable oils, sugar, deep fried foods, and processed meats cause inflammation in the body and create a host of problems for our health. Same with corn syrup. On a more subtle level, alcohol, caffeine, and [possibly] nightshade vegetables.”
The truth is that most of us love all those “naughty” foods. Yet, finding ways to make them with healthier ingredients and fewer calories could be as simple as finding an account on Instagram (recommendations: @broccoli_mum, @chef_bai, @betterfoodguru). You’ll be pleasantly surprised at the colors and flavors—and where you can sneak in chickpeas and cauliflower without anyone knowing. You’ll still eat delicious food but will be nourishing your body instead of filling it with refined carbohydrates and unpronounceable Franken-ingredients. “The fewer ingredients your food has, the better,” Attard adds. “The shorter those labels are, the better.”
Think of it this way: don’t be perfect, just be better. And more aware.
“What we eat literally becomes who we are,” says Attard. “What we put into our bodies and how we digest it is the foundation for our state of health—or disease.”
THE BUFFALO NIAGARA Medical Campus (BNMC) holds a Food as Medicine Symposium October 18-19 at University at Buffalo’s downtown campus. Presentations, expert panel discussions, an urban farm tour, and more will educate attendees on the importance of “treating” ourselves with food. Attendees will learn to cook amazing meals that combat disease and nourish the body with evidence-based nutrition science.
BNMC also partners with Independent Health to organize Healthy Restaurant Week in the spring, for which select menu items are analyzed by a registered dietitian to meet the standard for calories, fat, saturated fat, and sodium. Restaurants that have participated in the past include Mister Pizza Elmwood, Undergrounds Coffee House and Roastery, and Giacobbi’s Cucina Citta.

