









People wanting to keep wrinkles at bay will soon have a new option now that the U.S. Food and Drug Administration has ap proved the first competitor for Botox in decades.
Daxxify, made by Revance Ther apeutics Inc. in Nashville, Tennessee, is injected into the face along worry lines. It lasts longer than Botox, with about 80% of users seeing no or mild facial lines at four months after injec tion. For half of users, the treatment lasted six months, the company said
in a statement.
“Users do not have to go once every three months,” physician Balaji Prasad, who covers specialty phar maceuticals as an analyst for Barclays Investment Bank, told the New York Times. “In a world where time is of the essence, having a product with a long duration factor is extremely useful.”
The new drug now enters the $3 billion field of facial injection drugs. It is also a neuromuscular blocking agent and a botulinum toxin, like
Abbvie’s Botox.
“It also opens up the door for what we can do with therapeutics,” said Revance CEO Mark Foley, told the Times. “If you think of migraines, cervical dystonia [a neurological condition that affects the muscles in the neck and shoulders], overactive bladder, there’s a huge medical op portunity as well.”
The company has begun testing the drug on these other medical is sues, Foley said. While the company had been trying to create a product that needed no needle, it instead discovered a way to use peptide tech nology to keep the product stable. Typically, animal protein or human serum is used.
Botox is also used for more than just wrinkles. It has been an FDA-ap proved treatment for chronic mi graines since 2010.
Users of Daxxify in the Revance studies included some who expe rienced side effects. About 2% of people developed a drooping eyelid, while about 6% experienced head ache, the company said.
Toxin-based treatment can carry the potential for other side effects, such as general muscle weakness or breathing difficulties, the FDA cau tioned. Daxxify study participants showed none of those symptoms.
Revance had initially hoped for approval of its product in November 2020, but plans were postponed be cause of pandemic travel restrictions, the Times reported. An inspection finally conducted in June 2021 found problems with the quality control process and the company’s working cell bank, which contain the drug’s active ingredient. Those concerns were resolved, the Times reported.

The images depicted contain models and are being used for illustrative purposes only.
The images depicted contain models and are being used for illustrative purposes only.
The images depicted contain models and are being used for illustrative purposes only.
If you have early Alzheimer’s disease (AD) and/or are experiencing problems with memory or trouble thinking clearly, you may qualify to take part in this clinical research study of an investigational medicine.
If you have early Alzheimer’s disease (AD) and/or are experiencing problems with memory or trouble thinking clearly, you may qualify to take part in this clinical research study of an investigational medicine.
If you have early Alzheimer’s disease (AD) and/or are experiencing problems with memory or trouble thinking clearly, you may qualify to take part in this clinical research study of an investigational medicine.
You may be eligible if you:
You may be eligible if you:
are 55–80 years of age
are 55–80 years of age
You may be eligible if you:
are 55–80 years of age

are experiencing a gradual decline in your memory and ability to think clearly over at least the past 6 months or have been diagnosed with early AD (also known as prodromal AD)
are experiencing a gradual decline in your memory and ability to think clearly over at least the past 6 months or have been diagnosed with early AD (also known as prodromal AD)
are experiencing a gradual decline in your memory and ability to think clearly over at least the past 6 months or have been diagnosed with early AD (also known as prodromal AD)
have a reliable close friend, relative, or spouse who can be your study partner. This should be someone who spends at least 10 hours every week with you.
have a reliable close friend, relative, or spouse who can be your study partner. This should be someone who spends at least 10 hours every week with you.
have a reliable close friend, relative, or spouse who can be your study partner. This should be someone who spends at least 10 hours every week with you.
Qualified participants will receive study-related medical care and the investigational medicine or placebo at no cost.
Qualified participants will receive study-related medical care and the investigational medicine or placebo at no cost.
To learn more, Please visit: www.autonomystudy.com or Contact the site at:
Qualified participants will receive study-related medical care and the investigational medicine or placebo at no cost.
Brittonfield Pkwy, B105
Syracuse, NY 13057
To learn more, Please visit: www.autonomystudy.com or Contact the site at:
To learn more,
visit:
760-5905 ext
Janssen Research & Development,
Janssen
 Approved by Sterling IRB; IRB ID:
Approved by Sterling IRB; IRB ID: 8045
Approved by Sterling IRB; IRB ID:
Approved by Sterling IRB; IRB ID: 8045

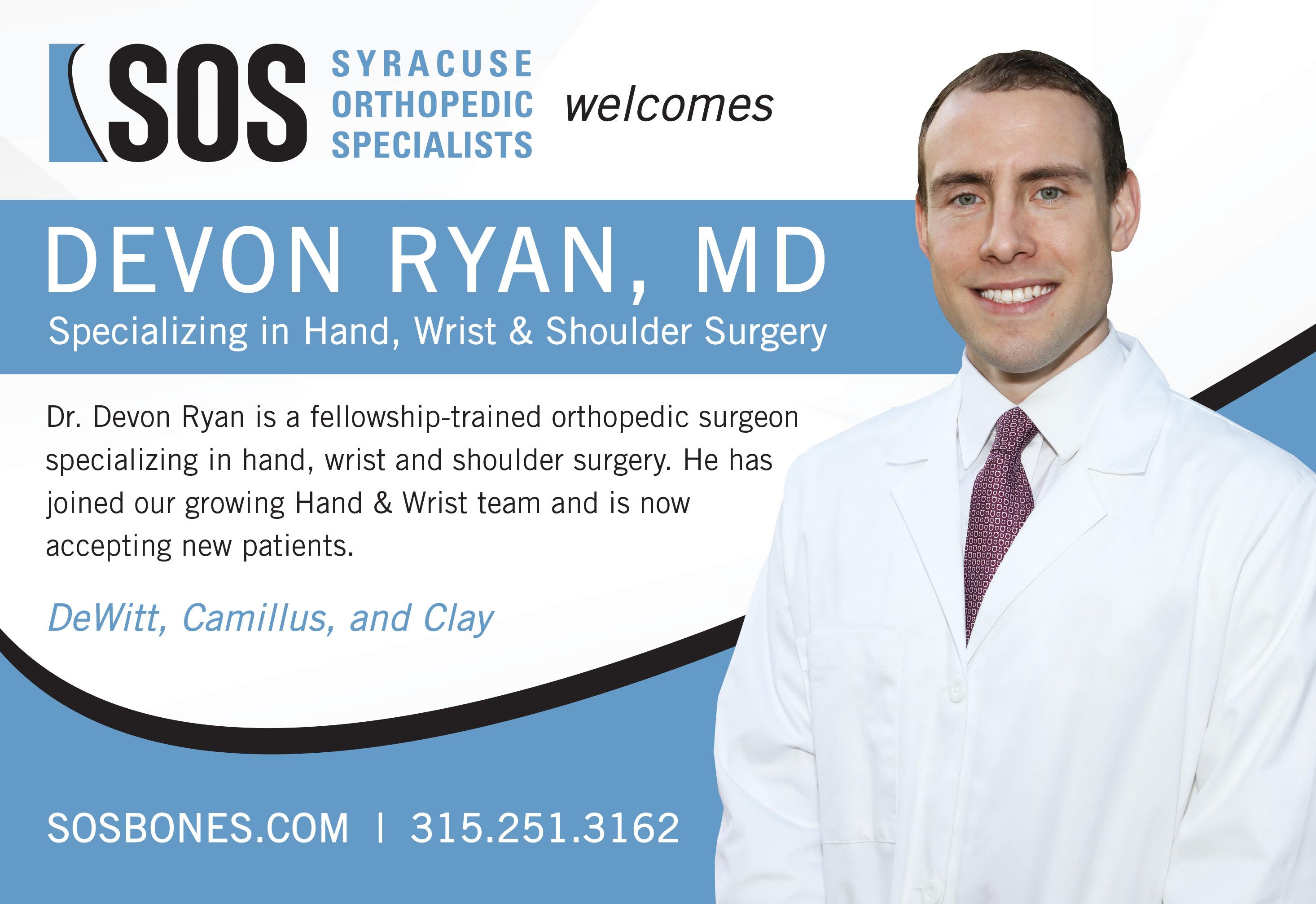
Q: Tell us about the new hand and wrist center you’re joining.

Your dog may like to lick your hand or face, but if you’re using a chemother apy cream that treats certain skin conditions, you should not allow it, the U.S. Food and Drug Administration advises.
The medication fluorouracil is fatal to dogs when ingested. People who keep the cream on a nightstand or counter should put it out of reach of their dogs, who may ingest it if they chew the container, the FDA advised.
with, there are a multitude of other folks who can help with the patient. It’s a great collaborative environ ment. And while I wouldn’t say I’ve never been other places that are col laborative, I certainly wouldn’t say it’s the rule that private practices are collaborative. It’s a nice thing about SOS.

Q: How big is the practice?
A: I’d say it’s around 25 or so across all specialties. So it’s a de cent-sized practice for sure.
Q: Was the collaborative aspect a major selling point for you?
pretty wide range of pathologies. The most common things we see are nerve compression issues like carpal tunnel syndrome and small things like tendinitis and trigger finger. We see a lot of traumas, fractures of the hand, wrist, elbow. We also see trau mas that aren’t fractures, like if you have a laceration on your hand that cut a tendon or nerve. That’s stuff we see pretty commonly. There’s also plenty of uncommon pathology.
Q: How much does nerve repair and preservation figure into orthope dic subspecialties like yours?
The agency has received reports involving dogs that were exposed to the cream; all the dogs have died.
Although the FDA has not yet received any reports of fluorouracil poisoning in cats or other pets, it recommends that this drug be kept away from all pets.
The cream is used to treat some types of skin cancers and a condition called actinic keratosis, which can lead to skin cancer. It may also be used to treat warts in children. Occasionally it is used to treat certain cancers in horses.
A: I’m joining a small handful of — no pun intended — other hand surgeons. One of the nice aspects of it is it’s a core group of a bunch of folks with varying levels of experience, but everyone is early- to mid-career for the most part, with the exception of Dr. [Daniel] Murphy who is very experienced and planning to retire in the next couple years. So it’s essen tially a group that will be relatively intact for quite a long time, which is cool. And I definitely found it to be a very collaborative group, which is one of its appealing features. We already have a hand center, which is an office location where a lot of us see patients. But as it happens they’re also opening at the same location a large area that will accommodate even more providers. And the real benefit of that will be that the occu pational therapists will essentially be in the same location. Right now they’re down the road from us, but after the new section opens up they’ll be right across the hall. And hopeful ly that will give us more collabora tive opportunities. So if there’s ever something unusual going on with a patient or want to discuss a particular rehab program, it’ll be much easier to just send them across the hall. So, yeah, I think we’re looking for ward to it.
A: The nerve compressions are very common, so fixing those could be considered a kind of nerve pres ervation. The main goal would be to improve what are often pain and sensory changes and to improve any further muscle deterioration. Certain ly the traumatic nerve injuries aren’t as common as the more chronic types of issues. But when they happen, they tend to be something we have to address with surgery because the sensations of the hand are so import
A: It was on our short list of destinations. I’m from Boston, my wife’s from Philadelphia, so we were looking at locations in the Northeast. As it happens, Syracuse ended up being a place where a lot of my fam ily transplanted. One of my brothers had taken a job here at Upstate and my parents a couple years ago made the move up to be close to their grandkids, and the cost of living is good as well. So it became a family hub. I got introduced to the practice through my brother. It always struck me as very well-run private practice. It seemed like a fun group to work with, both on the clinical and admin istrative side. And as far as the hand folks go, we take some calls over at Upstate, so we do get the oppor tunity to work with residents and trainees on call and stay a little bit engaged with the academic side of things. So it’s a good combination of those things.
Q: You’re offering a newer tech nique for basal joint arthritis. What is basal joint arthritis and how does the new technique work?
It can be dispersed as an in jection, or as a topical cream or a topical solution that’s applied on the skin. Brand names include Efudex, Carac, Tolak and Fluo roplex.
Pets who ingest fluorouracil may show signs of poisoning within 30 minutes. These signs can include vomiting, shaking, seizures, difficulty breathing and diarrhea.
Affected dogs can die in as little as six to 12 hours.
If you suspect your pet has consumed fluorouracil, imme diately get veterinary care and bring the container of cream with you. Also contact your vet or an emergency vet hospital immediately even if your pet just licks the area where you applied fluorouracil, and definitely call if your pet chews the container and consumes some of the fluo rouracil.
conditions do you usual ly treat?
ied, which is one of the appeals of this specialty. You treat a
cused on the hand and wrist?
A: The upper extrem ities, really, so up to the elbow. To a lesser ex tent the shoulder. There are enough things that crossover across the arm that it’s convenient to patients for us to of fer treatment for issues that may go all the way up to the shoulder. That being said, within the group there are folks we deal with a lot of shoulder issues regularly. So if I ran into something that was outside of the types of things I gen erally deal
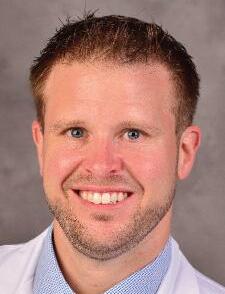
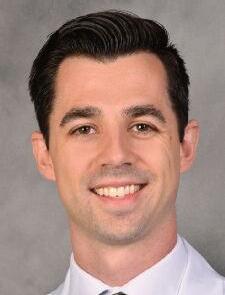
Name: Devon J. Ryan, M.D.
Position: Hand and upper extremity surgeon at Syracuse Orthopedic Specialists (SOS)
Hometown: Bedford, Massachusetts Education: NYU
Affiliations: St. Joseph’s Health; SUNY Upstate University Hospital
Organizations: American Academy of Orthopedic Surgeons; American Society for Surgery of the Hand;
Family: Wife (Rachel); son (Kelly), daughter (Cassie)
Hobbies: Running, pick-up sports, golf, skiing
Page 4 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • October 2022 A: Basal joint arthritis is a com mon type of arthritis that affects the thumb. There are several non-sur gical interventions, but for patients who need surgery there are a few operations that have longstanding good results. One of those is the LRTI, which uses some of your native ligaments to reconstruct the degen erating ligament. One of the ways I was trained to do it uses a very stout, secure device to suspend the meta carpal called a tightrope device. And, basically, it has a little bit of the role of replacing the native ligament. So for the right patient who needs the thumb to get moving again as quick as possible, it can be a great option. Traditionally with LRTIs patients are casted for up to six weeks. Not always, but that would be the histor ical way to do it. It fits with the trend of orthopedics trying to get patients moving again faster, since that’s what most patients want for very good reasons. The design of the implant can get patients moving again two to three weeks after operation.
At St. Joseph’s Health, we know that nurses are exceptional people. Whether your path keeps you close to patients at the bedside or steers you to leadership, education or expansion of your skill set, we provide the collaboration, resources and support to guide and grow your career.
We’re looking for passionate, driven nurses to join our Magnet® designated team. To become part of the team providing Central New York with a higher level of care, apply now.
 A HIGHER LEVEL OF CARE | jobs.sjhsyr.org
A HIGHER LEVEL OF CARE | jobs.sjhsyr.org
$7,050 in 2022, you enter catastrophic coverage but are still responsible for 5% of your prescription drug costs, with no limit.
But in 2024, people with Part D coverage will no longer be responsi ble for any out-of-pocket drug costs once they enter catastrophic cover age. This is significant for seniors who use expensive medications for conditions like cancer or multiple sclerosis.
drugs will be capped at $2,000 per year. This will be a major savings for the more than 1.5 million beneficia ries who currently spend more than $2,000 out-of-pocket each year.
The
climate, tax and health care bill known as the Inflation Reduction Act that was passed by Congress and signed into law by President Biden in August includes significant improvements to the Medicare program that will kick in over the next few years.
These changes will lower pre scription drug prices for millions of seniors by allowing the government to negotiate drug prices for the first time and capping seniors’ out-ofpocket drug costs at $2,000 annually. Some other popular changes will include free vaccinations, lower insu lin costs and expanded subsidies for lower income seniors.
Here is a breakdown of the changes to expect in Medicare and when they will roll out.
2023
Starting this January, all vac cines covered under Medicare Part D, including the shingles vaccine, will be free to beneficiaries. And the skyrocketing cost of insulin will be capped at $35 per month. This will be a significant saving for the more than 3 million Medicare enrollees who currently use insulin to control their diabetes.
Also starting in 2023, drug mak ers will be penalized in the form of rebates that they would be forced to pay to the government if they impose price increases that exceed general inflation.
Cost sharing for catastrophic coverage in Part D will be eliminat ed. Under the current Part D benefit, once your out-of-pocket costs reach
Also starting in 2024 through 2029, Part D premiums will not be allowed to grow faster than 6% per year.
And for lower-income Medicare beneficiaries, eligibility for the Part D Low Income Subsidy (also known as Extra Help) will be expanded to 150% of the federal poverty level, from today’s limit of 135%. This change will mean about 500,000 more seniors will qualify for financial assistance to help pay some or all of their prescription drug premiums and deductibles.
One of the biggest cost reduction measures for Medicare beneficiaries will begin in 2025 when out-of-pock et spending on Part D prescription
When Medicare’s Part D pro gram was enacted in 2003, negotiat ing lower drug prices was forbidden. But because of the Inflation Reduc tion Act, starting in 2026 Medicare will be empowered to begin nego tiating prices with drug companies for 10 of the most expensive drugs covered under Part D. In 2027 and 2028, 15 drugs would be eligible for negotiations and in 2029 and sub sequent years, 20 drugs would be chosen.
And, in addition to all the Medi care improvements, the Inflation Re duction Act also extends the Afford able Care Act (Obamacare) premium subsidies for three years that have helped millions of Americans gain coverage before they’re eligible for Medicare.
Jim Miller is the author of Savvy Senior column, which runs every month in In Good Health newspaper.

After slowly climbing back from the devastation caused by the pandemic, July median hospital operating margins plunged a staggering 64% from June op erating margins, according to industry consultants Kaufman Hall.
Its survey of 900 hospitals revealed an average year-to-date margin of negative 1%.
KH attributes this trend to lower outpatient volumes, more acute and expensive inpatient cases and an end to COVID-19 relief and PPP from the federal government.
Financial services company Fitch Ratings has reduced its hospital out look from “neutral” to “deteriorat ing.” Shaky finances are the driving force behind hospital mergers and
Typically, an ACO is a partner ship between physicians and one or more hospitals to participate in the Medicare Shared Savings Program (MSSP). The goal is to cooperate in exceeding quality benchmarks and reducing per capita cost benchmarks established in advance by Medicare. ACOs submit their bills, physician and hospital, to Medicare per usual. ACOs that reduce per capita costs will share in the savings with Medi care. If ACO costs per capita go up, the ACO must return money to Medicare. The MSSP is designed to encourage and reward the delivery of care by a cooperative of physicians
acquisitions. Not price fixing as skep tics have speculated. To survive and deliver care to their respective com munities, hospitals must be allowed to freely explore opportunities to increase fragile operating margins via shared over head, operating savings, and improved credit without onerous regulato ry oversight. At stake, in many cases, is the survival of smaller rural hospitals. While mergers might save hospitals, there could be a point where there are diminishing returns. For example, the 20-hospital Cleve land Clinic lost just over $1 billion the first half of 2022. While $628 million is attributed to investment losses, the system still lost close to $400 million on operations.
and hospitals working as a team to exceed common goals. An “every man for himself” model won’t work. And it never has. Medicare has learned that the more primary care physicians in the ACO, the better at reducing per capita costs. This makes sense. Effective primary care deliv ery can reduce illness, unnecessary referrals to specialists and overall hospitalization. Last year, 99% of ACOs beat quality benchmarks and 58% beat per capita costs. ACOs beat per capita costs benchmarks by $3.6 billion.
In 2018, the FDA approved the
Apple watch for EKGs. Who would have thought? Now, the NIH has granted $37 million to researchers at Northwestern and Johns Hopkins (and others) to study it. By moni toring atrial fibrillation, the watch can prevent strokes and reduce the amount of expensive blood thinners patients with Afib are receiving. Afib affects 2.5 million to 5 million of us. That is predicted to be 12 million by 2030. The seven-year study will involve 5,400 people with Afib. Some in the study will continue to receive the standard regimen of continuous expensive blood thinners to prevent strokes. Others will have their Afib monitored by the watch and receive targeted blood thinner therapy only when at risk of a stroke.
Congress has discontinued fund ing the government’s COVID-19 vac cine program effective next year. That means it will no longer purchase the vaccine from manufacturers and distribute it for free. It has turned the keys over to Big Pharma. Pfizer and Moderna must be licking their chops. (Is this what it took for Big Pharma to finally agree to negotiate some drug prices?) The government has already dropped free home testing due to lack of funds. Both drug giants claim that with the feds out of the way, they can be “more competitive” in an open market versus a govern ment-controlled contract market. Both also claim they can now focus on “branded education” which is in their area of expertise. It remains to be seen if Medicare and commercial insurers will charge for the vaccine or make it available for free.
The Biden administration and Congress has approved close to $100
million in funding for ACA naviga tors who help people select an insur ance that fits their needs and budget. The increased funding should add 1,500 new navigators. The ACA has been a widely successful program now insuring more than 36 million people. The uninsured rate is at an all-time low below 8%. Open enroll ment begins Nov. 1. To hamstring the ACA, the Trump administration slashed navigator funding to $10 million.

Just about half of all Medicare beneficiaries, or 28 million, are now covered by a commercially operated advantage plan. Sixty-six percent of the beneficiaries are individually covered; 18% are insured via employ er or union; and 16% are enrolled through special programs. Market shares for the largest carriers are Humana 28%; United 18%; and BCBS 14%. Cigna, Centene and Kaiser com bine for 24% market share.
Advantage plans are Part C Medicare. They draw members away from traditional Medicare by offering perks such as dental, vision, OTC drugs, transportation and even meals. Unlike traditional indemnity Medicare, most advantage plans require preauthorization for certain procedures.
George W. Chapman is a healthcare busi ness consultant who works exclusively with physicians, hos pitals and healthcare organizations. He op erates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapman consulting.com.There’s
an easy way to reduce your risk for dementia, heart disease and cancer: Start walk ing.
Getting in those recommended 10,000 steps a day makes a real differ ence, new research affirms, but even fewer will pay big dividends. No matter how many you log, however, step up your pace for the biggest benefit.

For every 2,000 steps you log, up to about 10,000 a day, your risk of early death drops by between 8% and 11%, researchers found.
“So, 10,000 steps maximizes the chances of getting all these benefits, but also for inactive people who can’t engage in so many steps — any steps have benefits — every step counts,” said lead researcher Borja del Pozo Cruz of the Center for Active and Healthy Aging at the University of Southern Denmark in Odense.
And, he added, it’s never too late to get going.
“The range of participants that we had in the study went from 40 to 79,” Cruz said. “That means that any person can actually get the benefits.”
This study, however, doesn’t prove that walking 10,000 steps a day has a health benefit, only that number of steps is associated with a reduction in heart disease, cancer, dementia and early death.
The Upstate Comprehensive Multiple Sclerosis Center is accepting patients with con rmed or suspected MS as well as other neuroimmunological diseases.
The program is unique in Central New York. It is designed to support each patient for the needs associated with MS, including a new infusion center, physical therapy, medication management, specialty pharmacy services, nutrition guidance, urology support, social work services and consideration for clinical trials.
Patients should ask their primary care provider for a referral to the Comprehensive MS Center by calling 315-464-4243


315-464-4243


Fall is such a special time of year. For me, it means all good things: relaxing in front of a cozy fire, making pumpkin soup on Sunday afternoons, donning my well-worn leather jacket for long walks and turning my attention to all those inside projects I neglected over the summer.
The brilliant colors, autumnal aromas and industriousness that arrive with the falling leaves really appeal to me. But this hasn’t always been the case.
After my divorce, the month of October left me feeling melancholy. I missed sharing the beauty of the season with a special someone. And I missed the sunshine as daylight waned.
Nostalgia and wistfulness would creep in, and I just wanted to retreat into myself. For those who live alone, the month of October has unique challenges.
Not one to wallow in a “poor is me” state of mind, I began to develop and employ some strategies to rekin dle my love of the fall season. It can be a great time to mix it up, get busy and expand your horizons.
Below are elements of my annual fall game plan. Take a look and see if one or more of these suggestions might not add a little color to your life palette this fall:
■ Tackle indoor projects. Fall is a great time to accomplish all those
nagging in door projects on your to-do list. I have a long list and I keep it right in front of me — a daily reminder that I have plen ty of home improvements to tackle, both large and small.
Too much idle time is not a friend at any time of year, but it can become downright unfriendly when gray clouds appear and the tempera ture drops. Now is the time to get busy: organize your storage space, do some touch-up painting, update your wardrobe, or clean the garage.
There’s nothing like being pro ductive to beat the autumn blues.
Don’t I know it. I just finished coating my flat-roof porch with a sticky tar sealant. Confession: it was messier than it was fun, but still ... I’m proud of my accomplishment. It lifted my spirits.
■ Get up and get going. Staying ac tive when there’s a chill in the air can be difficult. I can remember many a cold morning when all I wanted to do was hit the snooze button, pull up the covers, and stay in bed.
As nice as sleeping in can be
from time to time, I don’t recom mend it as a steady diet.
In my experience, there’s no better way to start your day than to wake up early. In the early morning’s peace and quiet, there is glorious time to reflect and feel gratitude. I use this important “me time” to meditate and set my intentions for my day.
As the morning brightens, my energy grows, as does my apprecia tion for the precious day ahead me.
■ Start moving and enjoy the great outdoors. Fresh air, sunlight and even a gentle rain can be invigorating first thing in the morning. I find a sunrise walk boosts my energy and kickstarts my day. Do I feel like layering up and taking a walk every morning? No. Do I feel better after I make the effort? Yes, without fail.
I love a long solitary walk to clear my head and be mindful. But I also love a walk with my sister Anne or good friend Kate to enjoy their company and avoid the siren’s song of isolation as the days grow short and get colder.
■ Learn something new. Going back to school and fall go hand-inhand. Who among us isn’t reminded of the nervous excitement associated with returning to school in the fall? It’s a great time to expand your intel lectual horizons.
Each fall I identify a new skill or subject to learn. Last year, I re searched how to divide and relocate perennials (my irises and peonies); this fall, I’m signing up to learn French on Duolingo, the free lan guage-learning app.
Continuing education opportuni ties are abundant in this community and online. Check out colleges and universities, community centers, arts and cultural institutions, your local library, and workshop listings for class and workshop offerings.
■ Invite people in. Over the years,
I’ve discovered a few simple and manageable ways to bring people into my world and into my home. One way is to organize a gathering around a TV show or series — yes, around the TV, as odd as that might sound.
For years, I invited my single friends over to watch “Downton Abbey” with me on Sunday nights. I provided the soup and salad; they provided the good company.
So, what’s your pleasure? Wheth er it’s football, a favorite weekly sitcom, or “Ted Lasso” on Apple TV+ — all of these and other TV shows can become reasons to bring friends and family together. The benefits? You’ll hone your cooking skills (boy, do I now have some great soup reci pes!) and you’ll connect with people you care about.
What better way to enjoy a nice fall evening.
There are so many wonderful and meaningful strategies to enjoy the fall season and to ward off the blues that can sometimes emerge during this changing time of year. But these strategies require effort –conscious, creative effort.
If you are feeling sluggish, lonely, or isolated, try a few of the strategies above. They have stood me in good stead and have reinvigorated my love for the fall season.
If you, too, are ready to turn over a new leaf, October is the perfect time!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com

sleep outcomes, researchers said.
Many
teens look at screens at bedtime, but some apps are more likely to keep them awake than others, leading to sleep problems.
That’s the upshot of a new study in which researchers found YouTube fans experienced consistent and neg ative effects on sleep. Surprisingly, traditional TV was associated with earlier bedtimes.
“We’ve been seeing teenagers who have sleep problems in our clin ic,” said co-author Michael Gradisar, head of sleep science at Sleep Cycle in Adelaide, Australia. “A lot of them have tried refraining from using technology, and clearly that hasn’t worked for them. Many of them mentioned that they would watch YouTube as they try to fall asleep. They find it entertaining without it
being overly stimulating.”
While many studies have been done on devices, little research has looked at the effects of specific apps on sleep, he said.
“We wanted to learn if there were specific apps that people should avoid, so that they could continue using their devices in a healthy way that didn’t affect sleep,” Gradisar said.
For the study, the researchers asked more than 700 12- to 18-yearolds how much time they spent using technology. That included mobile phones, gaming consoles and TV, as well as apps before going bed and in bed before falling sleeping.
While the study looked at the streaming service Netflix as well as YouTube, YouTube was the only app consistently and negatively related to
For every 15 minutes teens spent watching YouTube, they had a 24% greater chance of getting fewer than seven hours of shuteye. Watching YouTube and using gaming consoles both were associated with greater odds of getting insufficient sleep.
Contrary to the classic advice to keep TV out of the bedroom, tradi tional TV was associated with earlier bedtimes.
Gradisar said that might be because teens don’t interact with a TV in the same way they do with a phone. Instead, they just sit back and watch.
A half-hour in bed using phones, laptops, tablets and watching You Tube delayed lights out by seven to 13 minutes.

The issue with YouTube in partic ular may be that it’s so easy to finish
one video and click on a related one, said physician Alon Avidan, director of the UCLA Sleep Disorders Center.
Even homework done on screens late at night can be harmful, added Avidan, who reviewed the findings.
Watching Netflix was also asso ciated with greater sleepiness during the day.
Gradisar said one takeaway for parents is that not all technology use before bed is bad for their teen. Mom and Dad can also apply the findings to their own sleep health, he said.
“We often recommend that people do their own experiments with their tech use before sleep,” Gradisar said. “Find something that’s enjoyable so you don’t develop a bad relationship with your bed or bed room. The tech you’re using should be relaxing, but also be aware if it’s controlling your bedtime.”
Practical tips, advice and hope for those who live alone Practical tips, advice and hope for those who live alone
















Your health is as important as ever. ConnextCare is here to help!
Say Hello to Healthy! ConnextCare offers highly qualified and accessible providers at several locations throughout Oswego County. Keep you and your family healthy, safe, and happy with convenient, compassionate and comprehensive care right in your neighborhood.

• Over 70 dedicated healthcare providers across our network
• Acute care treatment with same-day appointments
• Services include family medicine, pediatrics, dental, psychiatry, chronic condition treatment, behavioral health, and more.


Say hello to the ConnextCare Central Square team. Call today.
3045 East Ave., Ste. G400 Central Square, NY 13036 (315) 675-9200
Fulton, Mexico, Oswego Parish, Phoenix, Pulaski www.connextcare.org
Jessica L. Kimball RN, MSN, FNP-C Maya Werksman RN, MSN, FNP-C Chelsea Claflin RN, MSN, FNP-C Anthony Rotella DOExecutive Director at AccessCNY talks about a new facility the nonprofit plans to build in northern Onondaga County — ‘there is a tremendous need in that part of the county,’ he says
By Mary Beth RoachQ: What is the mission of Ac cessCNY? How many people do you serve and what is your coverage area?
A: AccessCNY offers person-cen tered services that empower individ uals at all ages and abilities to reach their full potential. We serve people of all ages, people with a mental health diagnosis, developmental disability or physical disability. We
support well more than 3,000 people annually. We offer about 30 pro grams to support them. We employ about 1,400 people to operate those programs. We are on the larger scale of human service organizations. Our geographic region is primarily Onondaga County. I would say about 80% of our services are provided in the county, but we do programs in
each of the contiguous counties to Onondaga.
Q: AccessCNY recently received a $1.2 million state grant for a new facility in northern Onondaga Coun ty. Is this grant going to be enough to complete the project or are other funding sources being sought?
A: We’ll definitely need some other funding sources. The $1.2 mil lion covers capital, the land and the building essentially. We know we’ll need other amenities. We’re devel oping a plan right now to do some fund- raising for that those types of things.
Q: Are you starting from the ground up?
A: We’re looking for locations right now. Our preference is to start from the ground up because we will then be able to build a building that best meets the needs of those who will be receiving services.
Q: Do you have any target dates when you want to break ground and complete the project?
A: That’s something we’re devel oping right now. Our target is to be able to open late 2023, but our first step in the process is to speak with children who might receive services from the program when it’s open and their families to make sure we have a really good understanding of what they would like to see and then we will retain an architect to help us develop and design the space.
Q: Is this going to be a children-on ly facility?
A: We have a couple of adultbased respite homes already, but there is a significant need for chil dren’s respite. That was a big need in the community before the pandemic. The pandemic just exacerbated that. We’ll be serving children who have a developmental disability and also a mental health diagnosis or behavior al challenges.
Q: Can you briefly describe what you mean by respite home?
A: There will be two different types or respite, planned respite and emergency respite. Planned respite would be for when parents of a child with developmental disabilities needs to go out of town and they’re looking for a safe place for their chil dren. The emergency respite compo nent is a situation where a child has unstable or unsafe housing or has an immediate need. Maybe a parent or caregiver is suddenly in the hospi tal and there’s an immediate need for that child to receive residential
respite support.
Q: Was there a reason why you chose northern Onondaga County?
A: Because the funding was secured by Assemblyman (Al) Stirpe, we wanted to recognize that by hav ing the location within his district. But also there is a tremendous need in that part of the county. There’s a concentration of people living in that area and therefore a concentration of need also.
Q: Do you have an idea of how many children you might be to accom modate in this facility?
A: Our current thinking is that we will accommodate 10 children. We’re thinking the planned respite would be five or six of those beds and the emergency respite would be four or five.
Q: Do you know some of the ame nities that you want to include or that should be included?
A: We have an idea of a few of them. The 10 or so respite beds, but we want to add social work coun seling, mental health counseling for either the kids that are there or other children in the community who many not be using the respite beds … can go to the location to receive that support as well. We also want to have a recreation area for the kids, probably a playground. Another component is a sensory room, which is especially important for kids with autism. It helps them realize how their bodies react to sensory stimu lation and really helps them develop those skills.
The planned respite could take many different shapes. It doesn’t have to be overnight, but it could be when school’s out for the summer or the holidays. It could be just other times when children need a break and parents need a break.
Q: What will this new facility mean for AccessCNY?
A: It means that we will be able to help address what is a huge need in our community. We’re in the larger scale of human service organizations in our community. We pride our selves on really staying in tune with the needs of people with disabili ties and people with mental health diagnosis to understand how we can address those needs. It was easy for us to decide how we wanted to use this funding if we were to get it, be cause this has been such a huge need, so it helps us by helping the people that we serve.
Are you
and keeping it off? Do you have diabetes, high blood pressure, sleep apnea, heart/cholesterol problems, or other medical conditions associated with extra weight? If so, learn how weight loss surgery can improve your life.
William A. Graber, MD, PC – Weight Loss Surgery is an experienced team dedicated to helping people achieve their weight loss and healthy lifestyle goals. Our board certified bariatric surgeons specialize in laparoscopic and robotic assisted weight loss surgery and have performed thousands of procedures.

Working together with expertise to promote a supportive and safe environment for our patients as they strive to restore health and quality of life.
Offices in Utica and Syracuse




Pediatric urology, treat ment of hernias and hydroce es, robotic surger y, urinar y trac t infec tions, pen le abnormalities
General urology female and reconstruc tive urology




Reconstruc tive urology; incontinence, prosthetics, urinar y fistula, neurogenic bladder urinar y diversion Robot c surger y
Urologic oncology; robotic and laparoscopic surger y of prostate, kidney, bladder and adrenal
















Pediatric urology, treatment of hernias and hydroceles, robot c surger y, urinar y trac t infec tions, penile abnorma ities
 MATTHEW
DMITRIY NIKOLAVSKY, MD
RYAN
TIMOTHY K BYLER, MD
OLEG SHAPIRO,
SCOTT WIENER,
HANAN GOLDBERG, MD, MSc
and adrenal
ANTHONY J TRACEY, MD, MPH, FAAP
TOM SANFORD, MD
Urologic oncology; robotic surger y of prostate, kidney, bladder
NATASHA GINZBURG, IMD MAD NSOULI, MD
GENNADY BRATSLAVSKY, MD
Chairman Urologic oncology; robotic and laparoscopic surger y of prostate kidney bladder and adrenal
STEPHEN BLAKELY, EMD
LIZABETH FERRY, MD
General urology
ROBERT FLEISCHER, MD
General urology
Incontinence, urethral stric ture disease vesicovaginal fistula, reconstruc tive surger y, transgender care
JOSEPH JACOB, MD
Urologic oncology; robotic and laparoscopic surger y of prostate, kidney, bladder and adrenal
MAHMOUD CHEHAB, MD
General urology, male health urologic oncology, enlarged prostate, kidney stones , and robotic surger y
RUBEN PINKHASOV, MD, MPH
NICK LIU, MD
Urologic oncology; robotic and laparoscopic surger y of prostate, kidney, bladder and adrenal
EDWARD IOFFE, MD
General Urology, Endourology and Laporoscopic Surger y
JEFF VILLANUEVA, MD
Pediatric urology, treat ment of hernias and hydroceles, robotic surger y, urinar y trac t infec tions, penile abnorma ities
MATTHEW
DMITRIY NIKOLAVSKY, MD
RYAN
TIMOTHY K BYLER, MD
OLEG SHAPIRO,
SCOTT WIENER,
HANAN GOLDBERG, MD, MSc
and adrenal
ANTHONY J TRACEY, MD, MPH, FAAP
TOM SANFORD, MD
Urologic oncology; robotic surger y of prostate, kidney, bladder
NATASHA GINZBURG, IMD MAD NSOULI, MD
GENNADY BRATSLAVSKY, MD
Chairman Urologic oncology; robotic and laparoscopic surger y of prostate kidney bladder and adrenal
STEPHEN BLAKELY, EMD
LIZABETH FERRY, MD
General urology
ROBERT FLEISCHER, MD
General urology
Incontinence, urethral stric ture disease vesicovaginal fistula, reconstruc tive surger y, transgender care
JOSEPH JACOB, MD
Urologic oncology; robotic and laparoscopic surger y of prostate, kidney, bladder and adrenal
MAHMOUD CHEHAB, MD
General urology, male health urologic oncology, enlarged prostate, kidney stones , and robotic surger y
RUBEN PINKHASOV, MD, MPH
NICK LIU, MD
Urologic oncology; robotic and laparoscopic surger y of prostate, kidney, bladder and adrenal
EDWARD IOFFE, MD
General Urology, Endourology and Laporoscopic Surger y
JEFF VILLANUEVA, MD
Pediatric urology, treat ment of hernias and hydroceles, robotic surger y, urinar y trac t infec tions, penile abnorma ities
treatment with penicillin and several other antibiotics.
How common is rat bite fever? It’s not a reportable disease so data is hard to come by. Probably at least several hundred cases occur in the U.S. every year.
One

of my colleagues recently identified a patient sick with an unusual infectious disease. A disease that I’d learned about in medical school but long since forgotten. It’s one of those that could be easily missed with COVID-19 and other viral infections that cause fever running rampant through the community.
It’s called rat bite fever. The causative bacterium, Streptobacillus moniliformis, is spread by the bite or scratch of rodents. It can enter by a bite, by open skin or through mucus membranes such as the lining of the mouth, nose and eyes.
Another name for this illness is sodoku — not to be confused with the popular game sudoku. The name sodoku is used mostly in Asia where a related bacterium Spirillum mi nus causes the same disease.
Perhaps rodent bite fever would be a better name because rats are not the only culprit. It’s been transmitted by mice, guinea pigs, gerbils and squirrels. It’s not just wild versions of these critters, but also pets. as
well as feeder rats.
People at risk include rodent pet owners, people who handle fresh or frozen feeder rats, workers in pet stores or laboratories, and people who live or spend time in rodent-in fested areas. Those at increased risk of severe disease include children younger than 5, those older than 65, and people with weakened immune systems. The disease does not spread from person to person.
The bacteria can contaminate food or water and cause a similar illness termed Haverhill fever. The name comes from a 1926 outbreak caused by contaminated milk in Haverhill, Massachusetts.
The disease starts as soon as three days after exposure or as long as three weeks later. It’s possible for any bite to be healed and perhaps forgotten by the time symptoms start. The initial symptom is fever. Two to four days later a rash consisting of flat, reddened bumps may appear on the hands and feet. 75% of patients
develop a rash. One or more joints may become red, painful and swol len. 50% of people develop joint symptoms. Rash on the hands and feet can happen with hand-footmouth disease and painful joints occur in Lyme disease. Both of these are much more common than rat bite fever. So, kudos to my colleague who identified the infection after learning that the patient had been bitten by a mouse. Other symptoms include headache, swollen glands, vomiting and muscle aches.
Untreated, the infection can spread to the liver, lung, brain or heart. It can cause internal abscesses. And 10% of people die.
Because bacteria cause rat bite fever, it responds to antibiotic
Prevention boils down to good hygiene: protective gear like gloves and masks for pet store and laborato ry workers and good hand washing with soap and water after handling rodents or cleaning their cages. There is no laboratory test to tell whether your pet is carrying this organism and no indication that treating your pet with antibiotics will decrease the chance they spread this disease to you. If you are bitten, wash imme diately with soap and water. If you develop any symptoms of rat bite fe ver, seek immediate medical care and be sure to tell the treating provider about your rodent bite.
Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.


‘How common is rat bite fever? It’s not a reportable disease so data is hard to come by. Probably at least several hundred cases occur in the U.S. every year.’
One of two centers in the state, the Syracuse operation serves 54 counties
By Norah MachiaWhen the Upstate New York Poison Center opened 65 years ago in Syracuse, the primary focus was to help children suffering from lead poisoning.
At the time, it was known as the Central New York Poison Cen ter and it served 14 surrounding counties. The center operated as a “physician-to-physician” service to help doctors caring for children with high levels of lead detected in their bloodstreams, said T. Michele Caliva, Upstate New York Poison Center administrative director.
In those days, children could be exposed to lead-based paints and other dangerous substances that have since been taken off the market. Doc tors in the community could contact a physician at the poison center if they needed help in managing treat ments, said Caliva.
“At the beginning, there was a lot of pediatric focus,” she said. But as the center expanded, it also started to serve an increasing number of adults and senior citizens with a wider range of emergency poisoning and prevention calls.
In 2011, the center increased its coverage to 54 counties statewide. At the time, there had been five poison centers serving the entire state, but they were consolidated into two operations. The state’s other poison center is based in New York City and covers the five boroughs, Westchester County and Long Island.
Funding for the poison center is provided through the New York State Health Department and Upstate Medical University (the center is located on the campus).
There is no charge to call the poison center hotline at 1-800-2221222. All information provided by the caller remains confidential.
The Upstate New York Poison Center handles more than 50,000 calls each year and is open 24 hours a day, 365 days a year. It also serves as a site for medical student rotations.
“We take calls about anything that should not be in your body, on your skin, or in your eyes,” said Caliva.
Many of those calls are made by worried parents whose children have gotten into medications, personal care products or household clean ers. In some cases, the children have swallowed foreign objects such as coins or batteries.
The packaging of these types of products often attracts the attention of children, who can mistake them for food or candy, Caliva explained.
Callers don’t usually need to provide identifying information, although they may be asked to give a name and call back number if staff offer to check on a child being mon itored at home. If the caller requests help for an ambulance transport, the staff can make those arrangements. The caller’s zip code is requested only for record-keeping purposes.
“We don’t share the caller’s information,” said Caliva. “We don’t want any parent or caregiver to be afraid to call us about an uninten tional poisoning.”
The same advice goes for adults and senior citizens, who may feel embarrassed because they have, for example, taken the wrong dose of their medication.
A total of 16 registered nurses and pharmacists with specialized training in toxicology answer calls for the poison center. They determine if a person should be monitored at home, seen at a physician’s office or taken to an emergency department at a nearby hospital.

The poison center also has toxicologists and pharmacists with advanced training on call who may be consulted for a complicated poi soning emergency.
“There are layers of clinical expertise behind every call,” Caliva said.
Approximately 90% of calls for children aged 5 and younger, howev er, can be managed at home without a visit to a physician or hospital.
“The primary goal of every poison center is to reduce any serious illnesses or deaths that could result from an accidental poisoning,” said Caliva.
But there is also a focus on preventing unnecessary visits to the hospital, which could place a strain on the health care delivery system, particularly the emergency department staff and the ambulance services, she added. It’s also better for the parent and child not to risk unnecessary exposure to illness by going to a hospital if they don’t need emergency care.
Staff have recently seen an alarm ing increase in the number of calls for children who have ingested edible marijuana gummies and in those cases, hospitalization is required, said Caliva.
A bag of marijuana gummies left on a counter top is an open invitation for a young child to try them, she warned.
Accidental poisonings of these gummies, other medications and per sonal care products may be avoided if they are kept out of reach of young children. The poison center recom mends lock boxes for all medications, particularly for senior citizens who have grandchildren visiting them in their homes. Children are natural explorers and have a strong curiosity to learn more about new things, so it’s best to keep anything harmful out of their sight, Caliva said.
Phone calls from adults often involve unintentional overdoses of prescription or non-prescription drugs. Sometimes a person has mistaken a medication for a personal care product, and it could just be a matter of not wearing reading glasses at the time.
The highly trained poison center staff also consults on calls from hospitals, nursing homes and private practices, along with 911 operators, school officials and industry repre sentatives, said Caliva.
They may consult with a physi cian in an emergency department if a patient has intentionally taken an overdose of drugs, but it’s not clear what drugs were actually taken, she said. The center also receives calls about dangerous street drugs, such as fentanyl, and handles calls about exposures to hazardous chemicals or materials.
The Upstate New York Poison Control Center has management staff employed throughout the state as well, along with public educators who speak to community groups, schools and organizations about a variety of poison prevention topics.
For more information on the cen ter, visit: www.upstatepoison.org
T. Michele Caliva is Upstate New York Poison Center administrative director. “The primary goal of every poison center is to reduce any serious illnesses or deaths that could result from an accidental poisoning,” she says.




In most households, women are the managers of their families’ health care needs.* Combined with the challenges associated with juggling child care and workplace demands – it can be a struggle to ensure women, quite literally, take care of themselves.
FCMG can help. Available across CNY’s widest network of general practitioners and specialists – with short wait times, convenient hours and family-friendly offices – we make it easy to access a wide range of women’s care options, including:

• Reproductive health care and gynecology, including ultrasound exams
• Heart health, cholesterol management, and treatment of high blood pressure
• Type 1 and Type 2 Diabetes
• Chronic care and pain management
• Nutrition
• Dermatology
• Bone density, including diagnosis and care of Osteoporosis
• Among others
To learn how FCMG can address women’s health care needs – for women of all ages – contact us today. New patients and families are welcome!
Vegetarians may be at higher risk for hip fractures. A Uni versity of Leeds research paper compared the rate of hip fracture among 26,318 women who occasion ally eat meat; pescatarians, people who eat fish but not meat; and vege tarians.
Even after adjusting for factors like smoking and age, vegetarians evidenced a 33% greater risk of hip fracture in the median 22.3-years the women were followed for the study.
“There is a lower bone densi ty and greater risk of hip fracture among vegetarians and vegans,” said Susan E. Brown, certified nutrition ist, director of The Center for Better Bones and The Better Bone Foun dation in East Syracuse and author of The Acid–Alkaline Food Guide (Square One Publisher, 2006). “There are many benefits from vegetarian diet, but many studies indicate there is concern about bone health. Several studies indicate a higher hip fracture risk. But vegetarians can have fine bone strength if they supplement.”

She recommends supplementing
(800-2,000 IUs), vitamin C (500-3,000 mg.), vitamin A (5,000 IU or less), vitamin B-6 (25-50 mg.), folic acid/ folate (400-1,000 mcg.), vitamin B-12 (150-1,000 mcg.), vitamin K1 (2501,000 mcg.) and vitamin K2 (180-200 mcg.).
Healthful fats should comprise 20%-30% of total calories and it is also important to eat 1.0-1.5 grams of protein per kilogram of body weight.
She cautions vegetarians and vegans against highly processed foods and encourages the consump tion of whole, natural foods in addi tion to supplementation.
“Eating a vegetarian diet can have many health benefits but becomes tricky when considering optimal calcium intake,” said Erin Palma, a registered dietitian with Kelly’s Choice in Skaneateles. “While eliminating animal sources of calci um, one must eat a varied diet that includes calcium fortified foods such as soy, oat and rice drinks. Other sources include tofu, sesame and Tahini, dried fruit like prunes and apricots and figs.”
milk supply is not fortified. Most Americans who drink milk consume vitamin D-fortified milk. Few foods contain sufficient levels of vitamin D. The body generates vitamin D through sun exposure, which is limited in northern climates. Because vegans do not drink milk, they need to take vitamin D supplements. One eight-ounce serving of fortified milk contains around 150 IUs towards the National Institute of Health’s RDA of 600 to 800 IUs of vitamin D.
Calcium and vitamin D are only a part of maintaining strong bones. Protein is also important.
“Focusing on eating complete proteins will help ensure bone health,” Palma said. “Complete proteins are foods that contain all the necessary proteins for cell forma tion. Items like tofu tempeh, quinoa, hemp, chia and edamame are com plete proteins.”
She added that it is difficult to find a complete protein in vegetarian sources. Combining certain foods will meet that need. She recommend ed rice and beans; whole grain bread and nut butters; spinach and sun flower seeds; lentils and a source of whole grains; and peas and rice.

Juliann M. Mellen, dietitian with Upstate University Hospital, rec ommends that vegetarians “avoid nutrient deficiency by including high quality protein—dairy and eggs, if not vegan—and eating a good

good sources of minerals such as magnesium which aid in calcium absorption.
Becoming too slim may be one reason why some vegetarians are at higher risk for hip fracture, as that can mean weaker bones and less cushion for bones during a fall.
“Achieve and maintain a healthy weight,” Mellen said. “A lower BMI in vegetarians may be a contributing factor. In addition, exercise that in cludes resistance exercises—strength training and weightlifting—to pro tect bone.”
 Susan Brown
Susan Brown
To get the most out of ap ples, leave the skin on, as it con tains half the fiber and most of the polyphenols. Eat them raw, if possible, since cooking can deplete some nutrients. Wash all apples (including organic) before preparing or eating. Apples stored in the refrigerator can last six to eight weeks. Kept at room temperature, apples last about a week.
my kids were young, I used to call all fruit “na ture’s candy.” The nickname won them over, especially when it came to apples. As a family, we de voured apples by the bushelful!
Although the kids are long gone, apples continue to be my go-to fruit and here’s why: they’re delicious; they’re always available; they last forever in the fridge; and they’re loaded — absolutely, positively load ed — with powerful health benefits.
Let’s begin with apple’s most bountiful nutrient: fiber.
Apples are a good source of both soluble and insoluble fiber, with one medium apple providing about 20% of our daily needs. Soluble fiber protects against heart disease by lowering bad cholesterol, while insoluble fiber keeps us regular and feeling full. Both fibers, along with an apple’s high-water content, help with weight control, which further benefits the heart by lowering the risk of high blood pressure.
Apples are packed with polyphenols, an import ant group of antioxidants that might help prevent cancer. Antiox idants protect our bodies from disease and accelerated aging by

neutralizing free radicals — harmful by-products of daily living— that can wreak havoc with healthy tissues.
Many studies suggest that eating an apple a day (or more) is associated with a reduced risk of certain can cers, including colorectal, oral, lung, prostate and breast cancers. Al though the results so far look prom ising, researchers point out that more studies are needed.
Eating apples may also reduce your risk of Type 2 diabetes, a chron ic condition that results in too much sugar circulating in the blood stream. Even though apples taste sweet, they have a low glycemic index, which means your blood sugar levels don’t spike when you eat them. Research ers at Tufts University found that people who ate one or more apples a day had up to a 23% lower risk of Type 2 diabetes than non-apple eat ers. Experts say the fruit’s fiber helps stabilize blood sugar, along with its high concen tration of antioxi dants.
Just under 100 calories, nutrient-rich apples are also a decent source of im mune-boost ing vitamin C and have no fat, cholesterol or sodium.
Dieters who believe that eating a big breakfast followed by a small dinner is the surest way to lose weight will likely be very dis appointed by the findings of a new, small study.

What did the researchers dis cover? Eating the largest meal early in the day is unlikely to make any difference.
“The notion of timing of eating to influence health has been around for a long time,” said study author Alexandra Johnstone, a registered nutritionist and professor in the school of medicine, medical sciences and nutrition with the Rowett Insti tute at the University of Aberdeen in Scotland.
Johnstone acknowledged that the advice to “breakfast like a king and dine like a pauper” has plenty of adherents.
And prior research has in fact “suggested that eating earlier in the day enhanced weight loss, affecting energy metabolism, compared to
eating later in the day,” she noted.
Still, “chrono-nutrition” — the relationship between food intake and time of day — “is a relatively young science,” Johnstone cautioned.
To try to separate myth from fact, she and her colleagues decided to conduct a diet test involving 16 men and 14 women. For a month, each participant was randomly assigned to follow a morning-heavy diet or an evening-heavy diet, the study authors explained.
All meals were based on a 30% protein, 35% carbs and 35% fat break down, while total daily calorie intake was fixed.
But those on the morning-heavy diet consumed 45% of their daily calories at breakfast, followed by 35% and 20% at lunch and dinner, respec tively.
In contrast, those on the eve ning-heavy diet followed a 20%, 35% and 45% daily calorie split.
At the end of the month, all participants took a one-week break,
Adapted from twopeasandtheirpod.com
Serves 4-6
Maple-mustard dressing:
¼ cup olive oil
1 tablespoon fresh lemon juice
2 tablespoons apple cider vinegar
½-1 tablespoon pure maple syrup
2 teaspoons Dijon mustard
1 clove garlic, minced
Kosher salt and black pepper, to taste
Apple quinoa salad:

2/3 cup quinoa, rinsed
1¼ cups water
4 cups mixed greens
2 cups chopped apples
½ cup dried cranberries
½ cup crumbled goat, feta or Gor gonzola cheese
½ cup chopped walnuts Kosher salt and black pepper, to taste
which was then followed by a switch: for the following month all the morning-heavy eaters became eve ning-heavy eaters, and vice versa.
The result: “We found weight loss was similar with both diets,” Johnstone said.
All participants did lose a nota ble amount of weight, with an aver age loss of about 7 pounds during each of the one-month periods. It’s just that neither dietary pattern prompted more weight loss.
However, Johnstone and her colleagues did identify one big differ ence between the two styles of eating: diminished hunger among those on the morning-heavy diet.
While “there was no impact on energy expenditure,” she noted, “there was a positive influence of big breakfast to control appetite through out the day, with less hunger.”
And that could give a morn ing-heavy diet a leg up in the long run, she said.
“Hunger is one of the main reasons that people fail to comply to a weight-loss or calorie-restricted diet,” said Johnstone. “So if we have diet strategies that can help control hunger, then it would be beneficial in the real world.”
Johnstone and her team also
First, make the quinoa. Combine the quinoa and water in a medium pot. Bring to a boil, cover, reduce the heat and simmer for 15 minutes. Remove from the heat and let it sit, covered for 10 more minutes. Fluff with a fork.
While quinoa is cooking, make the maple-mustard dressing. In a small bowl, whisk together all the dressing ingredients. Set aside.
In a large bowl, add the mixed greens, cooked quinoa, apples, dried cranberries, crumbled cheese, and walnuts. Toss until the salad is combined. Then, drizzle with dressing (add the amount that suits you) and toss again.
Season to taste with more salt and pepper, if needed.
Anne Palumbo is a lifestyle colum nist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

stressed that there is unlikely to be a one-size-fits-all approach to how dietary planning affects metabolism. Yet broadly speaking, “our work sug gests that the distribution of calories throughout the day does not influ ence energy metabolism or weight loss,” she said.
The findings were published online Sept. 9 in the journal Cell Metabolism.
Many people experiencing heart surgery likely assume that the nurse operates the “heart-lung machine” responsible for keeping them alive while the surgeon stops their heart to repair it.
But that is incorrect. Perfusionists do this work.
These operating room specialists monitor equipment that pumps and oxygenates their blood and also help when ventilating sick patients is not enough, such as those very sick with COVID-19.
SUNY Upstate is the only school in the region and one of about 20 nationwide that offers a degree in clinical perfusion.
The school requires a few bache
lor’s level prerequisites in the scienc es. Student perfusionists complete 75 cases. To become certified, graduates must pass the board exam of the American Board of Cardiovascular Perfusion. To remain certified, the perfusionist must take 40 cases a year, minimum and over three years, complete 40 hours of continuing education credits.
In general, candidates should have strong math and science apti tude.
“You have to handle stress well,” said Bruce Searles, chairman of cardiovascular perfusion at SUNY Upstate. “You will work in a stressful environment. When someone’s head is on fire, you can stay calm and not
feel the need to get into arguments. You need a thick skin as you may get yelled at when it’s not your fault. Works well independently. There’s no one in the room who knows the technology that we use. The surgeon says, ‘This is what I need to have happen’ and they could not do that. There’s no one else there to do that.”
The remuneration is pretty good. According to Salaryexpert.com, an entry-level perfusionist in the Central New York area earns an average sala ry of $92,987.
“It’s a great job for people who work well under stress and also people who like to work behind the scenes,” Searles said. “The patient never knows you. You never get Christmas cards from them. It’s not like high touch like respiratory care or physical therapy. We’re very be hind-the-scenes. I love how the heart and lungs work and I get to do that — I replace them. I get to practice at a very advanced level intensive care. People say, ‘you monitor a machine’ but that’s like saying, ‘You monitor your car’ when you drive it.”
The demand for perfusionists remains keen, even as the pandem ic has wound down. In addition to practicing, perfusionists can work in equipment sales, training and academia.
Searles said that Upstate current ly has 12 students enrolled in the per fusionist program currently and the school received 284 applications. The lack of opportunities to receive the education has created a bottleneck for minting new perfusionists.
“There are only 4,500 of us na tionwide and we need more as we’re in a serious shortage,” said Carla Maul, perfusionist and director of perfusion.com, a site boasting 12,000 members worldwide. The Fort My ers, Florida-based company provides temporary and permanent perfusion staffing.
quality of life for children with au tism and their families.
Upstate joins 24 other hospitals in the network, including Children’s Hospital of Philadelphia (CHOP), University of Rochester Medical Cen ter – Golisano Children’s Hospital, and Cincinnati Children’s Hospital Medical Center in the network.
She likes how the career has pro gressed in technology in the past 20 years, noting that people who want to become a perfusionist should be comfortable with technology.

“I enjoy seeing really sick pa tients recover and have a healthy, wonderful life,” she said. “We are the ones that patients never ever know are there. People don’t know what we do. Kids in college don’t think of this as a profession because they’ve never heard of it.”
That represents one of the reasons that perfusion needs more workers. The small number of educa tional opportunities available is an other reason. Maul compared getting into a perfusion program as difficult as getting into Harvard because of the limited number of spots open. As a result, patients sometimes must delay vital surgery.
Sometimes, perfusionists are on stand-by for patients who may need their help during surgery.
In addition to the operating room, perfusionists also work bed side with extra corporeal membrane oxygenation (ECMO), supporting the lungs or the heart and lungs.
“Some COVID patients couldn’t oxygenate even on full ventilator settings,” Maul said. “ECMOs are in ICU.”
Perfusionists may also work on the go, as patients receiving ECMO sometimes need transportation to a larger medical center for more spe cialized care.
“I have never once regretted choosing this as my profession,” Maul said. “My profession chose me. I would encourage all the young people thinking about what profes sion they’d go into to think about this. If they’re interested with patient care and surgery and interested in technology, this would be a perfect profession to consider.
can become research or clinical initia tives.
Upstate Golisano Children’s Hospital will confer with oth er top centers on best practices and care for children with autism.
Upstate Golisano Children’s
Hospital has been invited to become a member of the Autism Care Net work, the first and only network of its kind focused on better autism care, aimed to improve health and
Henry Roane, Ph.D., division chief of the Center for Development, Behavior and Genetics at Upstate and the executive director of the Goli sano Center for Special Needs, said inclusion in the network will benefit clinicians, patients and their families in several ways.
“The goal of the care network is to bring centers together to discuss what’s working at their clinics,” Roane said. “It is also a venue for providers and parent advocates to say, ‘these are the problems we’re seeing’ and to provide a network to problem solve and troubleshoot with the ultimate goal of improving clinical care and quality of life for children with autism.”
Launched in April 2021, the network is supported by Autism Speaks, AIR-P, the J. Donald Lee and Laurelle Lee Family Foundation and PCORnet.
Roane said the network is also a way for centers to give feedback to Autism Speaks about issues families deal with, and in turn, these issues
“It really has a direct impact on the families, it has a direct impact on the clinicians, but it also has a little more of a global impact on setting directives and some objectives for Autism Speaks,” said Roane, who is among a team of four experts that re cently received a grant from Autism Speaks to work toward improving care for autistic people experiencing severe behavioral challenges.
Members of the care network meet via monthly webinars led by a different center each time, where things like best practices and changes in the field will be discussed. Inclu sion in the network includes a small amount of grant money to support the salary of a site coordinator.
“Being connected with these other programs enables us, almost forces us, to be more engaged and to have greater awareness to practice guidelines, changes to best practices, changes to care models that we are not currently doing,” Roane said. “We will be able to take our collective knowledge from all of those sites in the network and apply it to care pro visions in Syracuse, which will make our program better.”
Roane said Upstate has seen a 17% increase in the number of ap pointments for patients with autism in the past year.
Surgery assistant perfusionist operates a modern heart lung machine with an artificial cardiac valve in an operating room in cardiology clinic. Getty ImagesThe FDA announced in June its approval of baricitinib (brand name Oluminant, among oth ers) to treat alopecia areata.
Many people experience hair thinning and loss related to aging or medication. Alopecia areata is differ ent. The autoimmune disease causes sudden, round patches of hair loss all over the head.
The patches may grow in size and come and go in different areas over weeks and months. Alopecia to talis means that all of the hair on the patient’s head falls out and alopecia universalis refers to complete bodily hair loss.
About 6.8 million Americans have alopecia areata.
For Tracy Higginbotham, the benefits of baricitinib offer hope of regrowing her full head of hair. At present, taking prescription Olumi nant for 45 days has started her hair growing again. Higginbotham leads Women TIES, a women’s business promotion organization in Syra cuse and is the author of Under the Rose-Colored Hat, an autobiography of her alopecia areata journey.
For many years, she had experi enced the patchy hair loss of alopecia areata, treating it with medication such as steroids and cortisone. In 2006, she lost 80% of her hair, which she believes was prompted by the stress of her father’s unexpected death. Her hair grew back, but in 2018, the death of her stepmother plunged her back into alopecia uni versalis—complete hair loss from her entire body.
“It was very difficult,” Hig ginbotham said. “I was also going through menopause. It could be something with the hormones.”
During the pandemic, she caught COVID-19 and lost all the hair that she had grown, one and a half inches long.
Thanks to taking Oluminant, “I have hair growing, my eyebrows are
growing back. I have eyelashes in ev ery place where I should have them growing,” she said. “My eye doctor noticed that at my last appointment.”
She said that she’s remaining “cautiously optimistic” that her hair is back to stay.
Diagnosed in 1997, Thea Chassin of Scarborough, founded awareness and support group Bald Girls Do Lunch, Inc. She decided that barici tinib is not right for her, but she can also understand why many women with alopecia areata feel eager to try the medication.

“The stigma of female hair loss is very big in our culture,” Chassin said. “Women feel less feminine and have concerns about their looks and acceptance should they choose to go without supplemental hair. There’s a lot of worry about feeling normal and feeling they fit in. Our society prizes hair, not just in the US. Hair is a defining part of a woman in most cultures. A lack of hair is a very big deal. It affects self confidence and self-esteem.”
Although Chassin appears pub licly without a head covering, she knows that many women do not feel that is the right choice for them.
Beyond appearance, a lack of hair otherwise affects health. Without eyebrows and eyelashes, dust and sweat get into the eyes easier and mucus flows readily out of the nose without hairs to stop it. Chassin said that some people with alopecia areata have painfully brittle fingernails.
She views wearing wigs, scarves, hats, turbans or nothing at all on one’s head as daily choices that women with alopecia areata can make, depending on their situation or preference.
Chassin’s hair fell out slowly in patches and in overall thinning for three decades. Eventually, it had fallen out to the point where it “was hair, but not a hairdo,” she said.
She likened her appearance then
Tracy Higginbotham leads Women TIES, a women’s business promotion organization in Syracuse and is the author of “Under the Rose-Colored Hat,” an autobiography of her alopecia areata journey. She is taking the prescription drug Oluminant for 45 days and has started her hair growing again. She said that she’s remaining “cautiously optimistic” that her hair is back to stay.
to Bozo the clown.
“When I shaved it off, I felt like a huge weight had been lifted off me,” she said. “It was truly a step forward to self-acceptance.”
She also felt a powerful sense of control over a situation which had previously spun out of control for years.
For women interested in medi cation, Chassin views baricitinib as
“a game-changer.

There are many people who have been waiting for a medication that they can try. Previously, the options were limited. It’s an oppor tunity for people to try something if they’re not contraindicated. It doesn’t work 100% in everybody, but for those who want to try it, it’s FDA-approved.”


Using marijuana after the first weeks of pregnancy is linked to mental health issues in children that linger well into early adolescence, a new study shows.
Exposure to cannabis after about five to six weeks of fetal development was associated with attention, social and behavioral problems, according to the findings. These problems con tinued as the children reached ages 11 and 12, raising the risk of mental health and substance use disorders in the teen years.
Researchers from Washington University in St. Louis cautioned against using the drug during preg

nancy.
The team used data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study, which gathers information on brain devel opment and health in 12,000 children and teens in the United States.
As part of the ABCD study, investigators regularly measure par ticipants’ brain structure and activity using MRI scan. They also collect psychological, environmental and cognitive information.
The study only found an associ ation and not a cause-and-effect link between pot during pregnancy and children’s mental health outcomes.
Last month’s column was really heavy. It was also polariz ing, bold and self-revealing. It dealt with abortion and I highly recommend you read it (even if you don’t agree with what I wrote). The column is online at www.cnyhealth. com. In the search menu, just type my name.
This month, I’m letting the pendulum swing.
I’m writing about something almost every parent can agree on — how hard it is to make friends after you have children.
I am fortunate to have numerous close friends whom I can’t imagine my life without. However, I am geograph ically separated from many of them. At this point in my life, even a 30-minute drive can feel overwhelming and out of reach. A plane ride can feel impossi ble.
Despite the distances, my old friends are a great emotional support network. But I, like many parents I know, lack a local support network. So many of us don’t have close rela tionships with people who live close to us. Said another way, we lack a tangible, extended community.
Under normal circumstances,
finding that community is tough. The pandemic has made it that much harder. Overscheduled lives have made it harder still. Making new friends is like a strange sort of dating that no one ever prepared you for. Most of us are pretty bad at it and could use some help.
Nevertheless, THC, which is the main psychoactive sub stance in cannabis, can cross the placenta and potentially affect brain development, according to past research on cannabis use in pregnancy.
About 3% of pregnant women used cannabis in 2002, but that grew to 7% in 2017. Those numbers were 4.7% in 2018 and 5.4% in 2019, accord ing to the National Survey on Drug Use and Health.
The study was supported by the U.S. National Institute on Drug Abuse (NIDA) and was published Sept. 12 in JAMA Pediatrics.
If you’re a parent who wants to make new friends who live in your zip code, look no further than this column. It’s chock full of terrible advice. It contains pickup lines you should never use to spark a friend ship between you and another par ent. Hopefully, these lines give you a laugh and inspire you to put yourself out there.
If you’re a parent who is looking to trying to make friends while your kids are playing together, try these terrible pickup lines:
• Your child seems to be equally good at [insert sport] as my child. Perhaps we should nurture a healthy relationship by letting them compete in the sport of princes. Are you inter ested in going bowling with us?
• Your kid has a cat shirt on. My family has four cats! We possibly love them too much. Would you and your child like to come over and hang out with the cats next week end? We’ll be there too!
• Our kids seem to enjoy wres tling on the ground together. Would you like to let them do that in my backyard while we enjoy snacks and small talk?
• My kid heard from a friend who heard from another friend that your kid has a crush on my kid. Do you want to take them out for ice cream while we slyly listen to their conversations?
• My kid talks about your kid a lot. Maybe we should see if they are ready to take their friend ship to the next level of friendship. Maybe we should let them hang out in person.
• I see your kid is a playground daredevil, just like mine. Do you want to take them to some place full of pad ding and trampolines so they can show off to each other in a less dangerous environment?
If you’re a parent who is looking to hang out with other parents solo, try these terrible pickup lines:
• While watching this riveting lacrosse practice, I’ve noticed you smile a lot at people you don’t seem to know while pushing your hair behind your ear. I do that too. Should we get coffee sometime?
• I couldn’t help but notice the sweet hybrid you rolled up to this baseball practice in. Would you like to pull invasive species from the cree kwalk with me next Saturday?
• Our kids have been playing all of these sports that demand a crazy amount of equipment. I bet your garage and basement look like mine. Would you like to go halfsies on a dumpster with me? I bet you have a lot of crap to get rid of too. It would be fun to help each other sort and load!
• Our kids share a music stand in orchestra. Are you an artist too? If you like singer-songwriter songs, I have Spotify premium. Maybe you can come over sometime and listen to sad songs and drink tea.
• I noticed you don’t yell at your kid or the referees during sporting events. I also noticed you talk to your kid like they’re a human after the game is over. I like your respectful style. Want to go for a walk on the canal path with me sometime?
• Isn’t this a great book fair? It’s way better than the last one. My kid spent $8 on an eraser that was shaped like a hamburger but smelled like cotton candy last year. Anyway, my kid totally loves that title your kid just picked up. Maybe we have stuff in common too. Guess we will have to hang out to find out!
All mom jokes aside, making new friends as a grownup is really hard. It involves putting yourself out there in a way you likely haven’t in a long time.
Next time a parent comes up to you with an awkward opening line, cut them some slack. Or, even better, be the parent that strikes up a con versation with that parent that looks a little lonely.
We all want the same things for ourselves and our kids—things like love, acceptance, kindness and a sense of community. If we are willing to put those things out there, we might be really happy about what comes back to us.
‘Next time a parent comes up to you with an awkward opening line, cut them some slack. Or, even better, be the parent that strikes up a conversation with that parent who looks a little lonely.’
Breastfeeding
is one of the most healthy things a mother can do for her newborn baby.
It helps create a deeper connec tion between mother and child, and provides children the vital nutrients they need for survival and growth.
It’s also something that doesn’t always come natural to everyone and can provide stress for a new mother if her intention was to breastfeed.
Nearly two out of three infants are not exclusively breastfed for the initial recommended six months, according to the World Health Orga nization.
“Breastfeeding is beneficial in so many ways for both the mother and child. The child receives essential nu trients from the mother’s milk,” said Amy Ilardi, a certified lactation con sultant at Oswego Health. “It’s also an incredible bonding time between mother and child.”
Ilardi works with delivering mothers to increase their chances of having a long and successful breast feeding experience. She talks about five aspects of breastfeeding.
When it comes to breastfeed ing, myths run rampant. Common ones include the notion that breast feeding hurts and a laundry list of certain foods to avoid while breast feeding.
“There are a lot of old grand mother’s tales about what to eat and behaviors around breastfeeding,” said Ilardi. “But there are so many interesting facts that people should know about breastfeeding including that the type of milk changes as the child is growing to give them differ ent nutrients they need. It is really incredible what the human body can do.”
There are many benefits of breastfeeding, for both the lactating parent and infant. Breastfeeding can help protect babies against some short- and long-term illnesses and diseases. Maternal health benefits of breastfeeding include reduced risk of breast and ovarian cancer, type 2 diabetes, and cardiovascular disease. Recovery from childbirth can be quicker and with less risk of heavy postpartum bleeding, said Ilardi.
Breastfeeding moms release hormones and have benefits for a woman’s uterus. It can offer lifelong benefits so that is why many profes sionals advocate for breastfeeding if you can.
While breastfeeding has been encouraged in recent history, guidelines have changed to respect to how long it should occur.
“The benefits of breastfeeding are well documented even to the point where the World Health Organiza tion and the American Academy of Pediatrics recommended exclusively breastfeeding for the first six months. Then they went further and recom mended that with a complement of solid food, mothers can continue breastfeeding until 2 years old and beyond,” Ilardi said.
Amy Ilardi is a certified lactation consultant at Oswego Health, specializing in breastfeeding, among other things. “It’s also an incredible bonding time between mother and child,” she says about breastfeeding.

The recent guidelines published by the AAP are supported by several previous studies confirming that the nutritional content of breast milk remains relatively consistent into the second year of life. Although zinc and potassium levels appear to be reduced during the second year of life, total protein content, as well as lactoferrin, lysozyme and immu noglobulin A (IgA) levels appear to increase.
Current evidence suggests that breast milk is not likely to spread the virus to babies. If you have COVID-19, wash your hands before breastfeeding, and always wear a mask within six feet of your infant. Get a lot of rest and take good care of yourself. Follow CDC recommenda tions regarding isolation from others.
“We recommend that moth ers can still breastfeed if they have COVID-19 if they follow the CDC guidelines,” she added. “It would be some of the same advice we would give if the mother had various other viruses. You just have to be continu ously diligent on handwashing and wearing a face mask.”
Ilardi received training and competency verification in breast feeding and human lactation sup port, including assessing the latching and feeding process, providing corrective interventions, counseling mothers, understanding and apply ing knowledge of milk production including in special circumstances and other commonly encountered situations. There are currently more than 23,000 certified lactation coun selors in the US.
“In the hospital there are lac tation experts so I would advise families to take advantage of that,” she said. “You can’t be afraid to ask questions. If you struggle then you need to get help because the resourc es are available to you in ways that were not the case decades ago. We would definitely recommend that before simply deciding not to breast feed.”
The miracle of new life can also provide a life-saving gift for others.
The umbilical cord that connects a mother and baby until birth is rich in blood cells that help provide treatments for 80 different conditions, including cancers. Yet the umbilical cord is usually discarded upon delivery.
Expecting? Think about saving a life. Think about donating your cord blood.
Learn more: UpstateCordBloodBank.com The region’s only public cord blood center.
 OUR PARTNERS IN THIS LIFE GIVING, LIFE SAVING INITIATIVE
OUR PARTNERS IN THIS LIFE GIVING, LIFE SAVING INITIATIVE

InNew York state, 83% of indi viduals who are recommended to have a mammogram are follow ing the state’s screening guidelines, a percentage that’s been stable for two decades according to a review of state data by Excellus BlueCross BlueShield.
That means a persistent number of individuals (17%) are non-compli ant and putting their lives at risk.
According to data self-reported to the state, of those who have not had a mammogram within the past two years, 92.2% had health insur ance and 83.4% had a regular health care provider.
“Maybe we should change October from breast cancer aware ness month to mammogram month since, while awareness is important, detecting breast cancer early with a mammogram can save someone’s life,” says physician Lorna Fitzpat rick, Excellus BCBS vice president of medical affairs and senior medical director.

A mammogram can detect breast cancer at its earliest stages when treatment is most successful.
According to the Centers for Disease Control and Prevention, for every 100,000 women in the United States, there will be 124 reported cases of breast cancer and 20 deaths from the disease. In New York state, breast cancer is the most diagnosed form of cancer, with approximately 16,500 new cases and 2,500 deaths each year.
New York state guidelines rec ommend a mammogram every two years for individuals aged 50 to 74 who should be screened. Those who are 40 to 49 years of age, those with a family history or other risk factors for breast cancer, and those who have any symptoms or changes in their breasts should talk to their health care provider about the most appro priate screening schedule.
New York’s “Get Screened, No Excuses” legislation, signed in 2017, eliminated out-of-pocket costs and

Oswego 85.6%

Cortland 84.1%
Onondaga 80.3%
Cayuga 77.3%
Tompkins 77.2%
Central New York 80.9%
Source:wwws.health.ny.gov
many access issues associated with breast health care and services, including mammograms (the law does not apply to self-funded health insurance plans).
“With so much attention given to breast cancer awareness, and so many barriers removed to getting a mammogram, there should be 100% compliance with screening guide lines,” says Fitzpatrick. “Sadly, that’s not the case.”
Mammography rates across the five counties of Central New York average 80.9% or about two points lower than the state average (83%) for individuals aged 50 to 74.
Says Fitzpatrick, “It’s great that so much energy is directed toward
breast cancer awareness, but aware ness needs to translate to action.
Mammograms detect breast cancer early, when treatment has a high er rate of success and lives can be saved.”
Physician Lorna Fitzpatrick, Excellus BCBS vice president of medical affairs and senior medical director.Cancersurvivors all have a different story, as everyone’s journey in life and cancer is unique.
Nonetheless, most say that their experience has given them a new perspective on life after undergoing the devastation of their diagnosis, the struggle to select their next step, their treatment and their recovery.
The support of family, friends and their medical team helped in ways they never expected.
Fulton resident Liz Schremp received her breast cancer diagnosis in 1991 at age 45.
“I said, ‘This isn’t fair to my kids,’” Schremp recalled.
She lost her father to lung cancer and her mother to ovarian cancer while she was a youngster. Initially, Schremp shielded her two children from the truth of her cancer’s seri ousness and delayed her mastectomy by a month until after they were dropped off at college.
“At the time, I was trying to pro tect them and downplay it,” she said. “I didn’t think about their mental state.”
Chemotherapy and radiation fol lowed her surgery, as she had cancer in four of her 20 lymph nodes.
She underwent chemotherapy twice a month for six months and radiation five days a week for eight weeks. Schremp also took prescrip tion drug tamoxifen for five years.
After 13 years had passed, her oncologist said she no longer needed check-ups related to cancer. During treatment, she continued to work as an accounting clerk at the library in Fulton, as living in a state of near-normalcy benefited her mental health. In addition to the support her husband, Michael, and family offered, “I have a very deep faith,” she said. “I asked God to save me so I could be there on the kids’ gradua tion day and weddings, and rock my grandchildren. He gave me all this. I felt the Holy Spirit talking to me that I would get through all of this.”
A year after her recovery, she began Sharing and Caring Breast Cancer Support Group in Fulton, although she is no longer involved with the group. Many of the treat ments and medical protocols have changed over the years, so she feels her input is not the most up to date. But she will talk with anyone diag nosed who reaches out to her.
“Stay strong,” she said. “Stay positive and go to a support group. Support groups are healing and very beneficial. Don’t go through it alone. The thing about support groups is we know what you’re going through opposed to family and friends.”
Tricia Donahue, certified teach er currently working as a teacher’s assistant in the Tully School District, received her diagnosis of breast can cer in 2018. The Jamesville resident
was only 38 and had daughters aged 2 and 4.
“Two days prior when I had my biopsy, the surgeon said, ‘I looked at your scans from the sonogram; it looks smooth. You have nothing to worry about,’” she said. Upon hearing the grim news, “I think I was in shock. All along, I didn’t think cancer. There’s no history of cancer in my family.”
She received the diagnosis over the phone on a Friday, which meant she had to endure the weekend with little idea of what lay ahead. Her best friend spent the weekend to offer emotional support.
On Monday, an MRI revealed that the cancer had not spread to her lymph nodes, which was good news. Her surgeon recommended lumpec tomy with radiation. Donahue did not feel comfortable with that option and chose double mastectomy.
“I felt I had a better chance to not have recurrence,” she said.
She received expanders so she could have reconstruction months later. To her relief, Donahue’s provid ers advised that her biopsy revealed chemotherapy and radiation would not offer additional benefit.

Although granted a clean bill of health, Donahue found the mental health effects tough to deal with. She self-diagnosed with post-traumatic stress disorder, as she lived in fear daily. She felt that once the cancer was removed, “life would be good. That’s not true. I thought that would be reality. I was still living in fear: I had cancer. How could I get past this? I remember lying in bed unable to get my mind to turn off.”
The support of her husband Michael and friends helped her get through the ordeal. She advises anyone newly diagnosed to “do your research. Really look into your best treatment options. Get second and third opinions. Make sure you develop a relationship with all your healthcare providers that will go through this process with you.”
She also said that it’s important to let others know what is going on. She felt tentative about posting her diagnosis on social media. However, the outpouring of support that result ed proved invaluable.
“People really did come through,” Donahue said.
She began seeking holistic health modalities at Peaceful Remedies in Oswego, including reiki. Especially for moms of young children, self-care is often a missing part of the cancer patient experience.
“Doctors don’t talk about stress, nutrition and lifestyle,” she said.
Supplements, yoga and medita tion have helped Donahue.
Tricia Caroccio, an Oswego resident and reading coach at Kings ford Park Elementary School, also found support at Peaceful Remedies. She received her diagnosis of breast cancer in 2020.
“I just felt shock,” she said. “We were in the middle of the pandemic. This was one more thing.”
After her biopsy and MRI on the other breast, she learned that lumpec tomy was not an option. She decided to go with a double mastectomy, which proved the right choice as she had suspicious cells in the breast that received the MRI. After her surgery at St. Joseph’s Health, she did not need radiation or chemotherapy.
Two months later, she also un derwent reconstruction at Upstate University Hospital.
“I really had to shift to a posi tive mindset to keep me going every day,” Caroccio said. “My three teen agers watched me go through this. I wanted to set an example, that you can do this with grace. You cannot let it just be the end. I wouldn’t let this end me. I wanted to do this with mindfulness and nutrition and the people I surrounded myself with. I was also seeing an integrative doctor to look at everything. I wanted the best team approach. I surrounded myself with an incredible team to stay so positive about it.”
She learned more about nutrition and mindfulness at Peaceful Reme dies. During a low moment, repeat ing a positive affirmation three times helped her remain upbeat.
She tells anyone newly diag nosed to “get your team together: your family, friends and doctor. If you’re local, I always suggest reaching out to Peaceful Remedies. Nutrition is huge. Find what tools will be good for you, whether mas sage, reiki, acupuncture. Those are all things I used.”
She feels she was “beyond blessed” with the care she received from her husband, Shawn, and her children.
“Don’t let the diagnosis be the end but the start of the journey and decide how you’re going to get through that,” she said. “It’s not your sentence. It was almost in many ways a gift. It woke me up to being present and grateful for even the smallest moments. I always felt like a really grateful person, but this has made me tremendously grateful.”
Fulton resident Liz Schremp received her breast cancer diagnosis in 1991 at age 45. After 13 years had passed, her oncologist said she no longer needed checkups related to cancer. “I have a very deep faith,” she says. “I asked God to save me so I could be there on the kids’ graduation day and weddings, and rock my grandchildren.”Oncologist Daniel Thomas, Up state Cancer Center, assistant professor of surgery, SUNY Upstate Medical University, has a special interest in the treatment of patients with melanoma, sarcoma and diseases of the endocrine system including thyroid cancer, parathyroid disease and adrenal tumors.

His primary research interest is improving the care of elderly and frail patients who undergo cancer surgeries.
We asked him about the outlook in cancer treatment, whether there is hope for those affected by this disease.

Q: Are rates of death from cancer decreasing?
A: We’ve seen a decrease in the risk of Americans who die from cancer in the last three decades. Over that time, there’s been about a one third decreased risk of dying from cancer, once it’s diag-nosed. Further more, a recent report from the Na tional Cancer Institute showed that, even in the last five years, the overall cancer death rate for Americans has fallen even more sharply.
It’s important to put these numbers into context when you consider how many people in U.S. are diagnosed with cancer every year. In 2020, it was estimated that almost two million people would be diagnosed with cancer, and 600,000 would die.
A decrease of one-third the risk of dying means that our current preventive strategies and cancer treatments are making a significant impact.

Q: What is the reason for the de crease in death?
A: There are many reasons why the risk of dying from cancer has decreased. One of the biggest con tributors has been public health and cancer prevention programs that focus on preventing cancer and early detection of cancers.

For example, smoking rates have plummeted in the last several decades which clearly decreased the number of Americans dying from lung cancer. Also, our ability to detect early cancers has improved with screening programs, such as mammography for breast cancer or colonoscopy for colon cancer.
When patients are screened, can cers can be detected earlier, at an ear lier stage, and therefore have a better chance of being treated successfully before the cancer can spread to the rest of the body. Early detection and early treatment translate into pro longed survival.
The second and most exciting reason for the improvement in cancer survival is our ever-improving treat ment options. We all hope that the patient’s cancer will be at the early stage when discovered, but even patients who have advanced stage
cancer, new treatment discoveries are allowing patients to live longer after their diagnosis. Lung cancer and melanoma are two great examples of how cancer discoveries have led to prolonging survival for patients, compared to even just 10 years ago. The discovery of cancer treatment such as targeted drug therapies and immunotherapies have drastically changed the landscape, especially for patients with advanced or metastatic disease.
Q: What are the most promising new therapies for cancer patients?
A: The discovery and advance ment of immunotherapy has been groundbreaking and quite literally life-changing for cancer patients. Immunotherapy is a type of cancer treatment which can be used to treat many different types of cancer and can be used alone or often in combi nation with chemotherapy and other cancer treatments.
Immunotherapy has really come to the forefront in the last decade. These cancer treatments help the patient’s own immune system fight cancer by boosting the im mune system’s response to the presence of cancer cells. And since your immune system goes throughout your whole body, this type
of treatment can attack cancer cells anywhere in the body. This has been proven to be a game-changer in the treatment of patients with advanced or metastatic cancers.
I’m an expert in the treatment of melanoma, a type of skin cancer which can have a poor prognosis in patients who have advanced or metastatic disease. However, immu notherapy advances in the last five to 10 years have allowed patients with advanced and metastatic melanoma to live longer. It’s very exciting that the five-year survival rate for mela noma patients has doubled over the last 10 years.
There is much hope for the future of cancer treatments. Patients should maintain hope when facing these difficult diagnoses. Here at Upstate Cancer Center and at cancer centers across the world, we continue to study new and innovative cancer treatments like immunotherapies and continue to make headway in our struggle to fight cancer.
As an example of hope, a re cently a study in the New England Journal of Medicine reported the results of 14 patients with advanced rectal cancer who were treated with a new immuno therapy medication. With only six months of treatment with this new immunotherapy drug, all 14 patients had a complete response to treatment and so far, have been spared the need for ad ditional chemotherapy, radiation, or surgery. This is groundbreaking, and although it is just one study and only 14 patients, it demonstrates the possibilities as we continue to discover new therapies to treat patients with cancer.
Oncologist Daniel ThomasAnyone who has received a clean bill of health after cancer treatments wants to maintain their good health. Although nothing can guarantee cancer won’t come back, people in remission can cer tainly increase their chances of good health by taking a few steps.
“Survivorship is a key part of cancer care,” said Arnold Baskies, chairman of the Global Health Ad visory Council and past chairman of the board of directors, American Cancer Society, Inc. “The Commis sion on Cancer has recommended that all hospitals and providers pro vide a survivorship plan to patients. The American Cancer Society also recommends it. It includes informa tion on the treatment rendered and what should be done in terms of follow-up and surveillance.”
Since 14 million people in the US have survived cancer—and Baskies estimates it will likely swell to 20 million in the next five to 10 years— developing survivorship plans will only increase in importance.
“The specific recommendations are relative to the type of cancer and treatment rendered,” Baskies said. “A specific survivorship care plan should be personalized.”
For example, a colon cancer survivor may have scheduled colo noscopy and blood tests or for lung surgery, CT scans and other tests. General recommendations typically include healthful diet, exercise, stress management and smoking cessation.
Baskies noted that any time sur vivors change providers outside their health system, “they need to take with them the information of what treatment they had and what needs to be done going forward.”

Following all the provider’s protocols and follow-up treatments is vital for continued good health. Some cancer patients receive radiation as part of their treatment. This may result in burns from the treatment. Caring for these injuries properly is important for timely healing once the radiation regimen is complete.

Hyperbaric therapy promotes healing of radiation therapy wounds.

“Fifty percent of patients with cancer receive radiation therapy,” said Olivia VanSanford, program director at The Center for Wound Healing at Oswego Health. “It’s a wonderful therapy for treating cancer, but unfortunately, it can have a long-lasting effect many patients
aren’t aware of.”
From a few months to up to 20 years after receiving radiation, patients can present with symptoms including pain, wounds that struggle to heal, and blood in their urine.
Katie O’Reilly, certified hyperbar ic tech and licensed practical nurse at the center, administers treatments for radiation wounds using the hyper baric oxygen chamber.
“The patient will lie inside it and receive 100% oxygen at a greater atmospheric pressure,” O’Reilly ex plained. “It shrinks the oxygen mole cules you’re breathing in so it floods your body with the oxygen you need to heal your tissue. Normally, that wouldn’t be possible, as only 21% of the air you’re breathing is oxygen.”
Patients do not need a doctor’s referral for hyperbaric oxygen thera py. Sessions last two hours. Patients typically receive 80 to 120 two-hour treatments, Monday through Friday, depending upon their injury.

Diet contributes to supporting good health for cancer survivors.
“Post treatment, extra protein is usually needed to heal tissues and help fight infection, and rebuild muscle mass,” said Erin Palma, registered dietitian with Kelly’s Choice in Skaneateles. “Rather than red meat, the bulk of protein should come from fish, poultry, eggs, low-fat dairy products, nuts and nut butters, dried beans, peas and lentils, and soy foods.”

She added that some treatments like radiation “may indicate limit ing citrus and spicy foods, whereas chemotherapy you limit raw and undercooked items. Seeking out the services of a dietitian can help determine the best plan of support for you.”
In general, she advises cancer survivors to limit red meat consump tion, as it can increase the risk for colon cancer and possibly other kinds of cancer in the future.
“The American Institute for Cancer Research recommends eating no more than 18 ounces of cooked red meat a week, but less is better,” Palma said.
and
one bedroom apartments close
and
as well as emergency
well as
Seniors (over 62) or
SS
Seniors (over 62) or receiving SS
Katie O’Reilly, certified hyperbaric tech and licensed practical nurse at the center, administers treatments for radiation wounds. Arnold BaskiesCancer patients already have a lot to deal with emotionally and physically. But research shows that insured patients under 65 are also paying more for their treatments out-of-pocket than ever before.
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101
The study highlights the “grow ing financial burden for non-elderly patients with cancer with private health insurance coverage,” said senior study author Robin Yabroff, scientific vice president of health services research at the American Cancer Society (ACS).

“Policy initiatives to mitigate financial hardship should consider cost containment as well as insur ance reform, as most Americans will not be able to afford such an unex pected expense,” she said in an ACS news release.
Researchers from the ACS and the University of Texas MD Ander son Cancer Center found that as costs of cancer treatments rise, this led to greater out-of-pocket costs for the four most common types of can cer in patients younger than 65 who were privately insured.
Those out-of-pocket costs went up more than 15% between 2009 and 2016, to more than $6,000 for those being treated for breast, colon and lung cancers, and to $4,500 for those receiving treatment for prostate cancer.
To study the issue, researchers analyzed 105,255 breast, 23,571 co lon, 11,321 lung, and 59,197 prostate cancer patients using claims from the Health Care Cost Institute.
The data included cancer-relat ed surgery, intravenous systemic therapy and radiation. The research team calculated associated total and out-of-pocket costs.
The study found that the total mean costs per patient increased from $109,544 to $140,732 for breast cancer patients, an increase of 29%.
Costs increased from $151,751 to $168,730 for lung cancer treatments, or 11% jump. Those costs grew from $53,300 to $55,497 for prostate cancer, about 4%. The increase for colon can cer, went from $136,652 to $137,663, which was not considered statistical ly significant.
“This trend of rising OOP [out of pocket] costs among patients with private insurance is concerning because high-deductible plans are becoming more common in the pri vate insurance market,” said study author Ya Chen Tina Shih, a profes sor of health services research at MD Anderson.

“The recently passed Inflation Reduction Act is a step toward addressing this challenge, focusing on reductions in pricing for high-cost Medicare drugs and limiting out-ofpocket costs for seniors,” Shih said in the release.
Researchers found that the use of intravenous systemic therapy and radiation statistically significantly in creased, except for lung cancer. Can cer surgery costs increased for breast and colon cancer, while decreasing for prostate cancer.
The findings were published Sept. 13 in the Journal of the Nation al Cancer Institute.
• Silver tsunami: by 2030, all boomers will be over 65
• Why retirees are returning to work
• Budgeting for and during retirement; how to create budget that works.
• Ready to volunteer? Retirement is the perfect time to give back and volunteer. CNY offers abundance of options.
• Save on cable TV—cut the cord
• Fall foliage is still happening in. Local experts suggest places to go

•
Zoom 101: What you need to know
Hello.
Can you recommend any services that check in on elder ly seniors who live alone? I live about 200 miles from my 82-yearold mother and worry about her falling or getting ill and not being able to call for help.







 — Worrywart Daughter
— Worrywart Daughter
There are actually several differ ent types of check-in services, along with some simple technology devices that can help keep your mom safe at home while providing you some peace of mind. Here are some top options to look into.
• Check-in app: If your mom uses a smartphone, a great solution to help ensure her safety is Snug (SnugSafe.com), a free app that would check in on her every day to confirm she’s OK. This app is used by thousands of elderly seniors who live alone and want to make sure that if something happens to them, their loved ones will be notified quickly so they can receive help in minutes, rather than days.
Here’s how it works. After down loading the app, your mom will choose what time(s) throughout the day she’d like for Snug to check in. Snug will send a push notification at those times asking your mom to check in by tapping the big green check button on her smartphone screen. If she doesn’t check in within 10 minutes or respond after multiple pings, Snug will notify her emergen cy contacts and share her last known location so that she can receive fast help.
For extra peace of mind, your mom can purchase Snug’s premi um plan ($10 per month) where in addition to notifying her emergency contacts, Snug will request an in-per son wellness check by a police officer who will visit her house to confirm she’s OK and provide assistance as needed. The app works with iPhone and Android smartphones.
• Check-in calls: If your mom doesn’t use a smartphone, another option to help ensure her safety is a daily check-in call service program. These are telephone reassurance programs usually run by police or sheriff’s departments in hundreds of counties across the country and are usually provided free of charge.



Here’s how they work. A comput er automated phone system would call your mom at a designated time

each day to check in. If she answers, the system will assume everything is OK. But if she didn’t pick up or if the call goes to voice mail after repeated tries, you (or whoever her designee is) would get a notification call. If you are not reachable, calls are then made to backup people who’ve also agreed to check on your mom if necessary.
The fallback is if no one can be reached, the police or other emergen cy services personnel will be dis patched to her home.
To find out if this service is avail able in your mom’s community, call her local police department’s none mergency number. You should also check with the local county office of the aging in your mom’s area — call 800-677-1116 for contact information.


If, however, her community doesn’t have a call check-in pro gram, there are businesses like CARE (Call-Reassurance.com) and IAmFine (Iamfine.com) that offer similar ser vices for under $15 per month.





• Technology devices: You may also want to invest in some simple technology aids to keep your mom safe. One of the most commonly used devices for this is a medical alert sys tem that cost about $1 per day. These systems come with a wearable “help button” that would allow her to call for help 24/7.

Another option that’s becoming increasingly popular is smart speak ers, like Amazon Alexa or Google Home. These devices work with third-party applications — AskMy Buddy.net and MySOSFamily.com — that would let your mom to call multiple emergency contacts with a simple verbal command.
And be sure to check out Ama zon’s Alexa Together (Amazon.com/ AlexaTogether), a new $20 month ly subscription service that helps families support and keep tabs on their older loved ones who live alone through an Alexa-enabled device.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

 By Julie Sheedy
By Julie Sheedy
Across the healthcare industry, organizations have found that company culture is essential to keep employees happy, which leads to greater employee retention and ul timately, improved quality of service. While opportunities for skill devel opment and career advancement used to be considered a perk, these benefits are rapidly becoming less of a bonus and more of an expectation.
In fact, LinkedIn’s 2022 Global Talent Trends survey showed more than half (59%) of respondents selected professional development opportunities as a top area to im prove company culture. That’s a pretty clear message regarding how organizations — especially health care organizations that critically need more staff — can attract and keep employees.
Beyond retention of employees, investment in professional devel opment opportunities can lead to increased engagement, better work performance and higher overall job satisfaction among employees. Happier, more engaged employees have been proven to deliver better service — including, but certainly not limited to, the healthcare industry.
In response to this expectation for more career opportunities, orga nizations should take stock of the programs that they offer to employ ees, and thoughtfully consider the positive long-term impacts these investments could have on patients, customers, community residents, and of course, employees.
As Loretto’s chief marketing and engagement officer, I am constantly working alongside the other senior leadership team members to research and develop enhancements to our employee training and support pro grams. A recent survey once again showed that Loretto employees want even more training and advancement opportunities, so Loretto launched a new series of training programs called EDGE, which stands for “Edu cate, Develop, Grow, Excel.” We have begun implementing several new programs this summer and plan to launch more.
With offerings like leadership training for today’s changing health care environment and nationally recognized certification programs in specific areas like dementia, advanced rehabilitation and food ser vices, it’s easy to see how an organi zation’s investment in its employees can improve patients’ experiences and the quality of healthcare in our community.
Want to learn more about new opportunities at Loretto? Visit loret tocny.org/careers
By Warren Beck, Social Security District Manager in SyracuseThis year, Oct. 12 is National Savings Day. This day serves as an important reminder to plan for your financial future.
Social Security is a vital part of any financial plan. We have online tools to help you understand your potential Social Security benefits and how they fit into your financial future.
You should periodically review your Social Security statement using your personal my Social Security account at www.ssa.gov/myaccount. Your statement is an easy-to-read summary of the estimated benefits you and your family could receive,
including potential retirement, dis ability and survivors benefits.

Our plan for retirement tool in your personal my Social Security account allows you to check various benefit estimate scenarios. You can compare the effect different future earnings and retirement benefit start dates have on your future benefit amount.
Please let friends and family know they can take steps to improve their financial knowledge by signing in to their secure my Social Secu rity account. If they don’t have an account, they can easily create one at www.ssa.gov/myaccount.
Q.: My child, who gets Social Security, will be attending his last year of high school in the fall. He turns 19 in a few months. Do I need to fill out a form for his benefits to continue?
A.: Yes. You should receive a form, SSA-1372-BK, in the mail about three months before your son’s birth day. Your son needs to complete the form and take it to his school’s office for certification. Then, you need to return page two and the certified page three back to Social Security for processing. If you can’t find the form we mailed to you, you can find it online at: www.ssa.gov/forms/ssa1372.pdf.
Q.: I worked for the last 10 years and I now have my 40 credits. Does this mean that I get the maximum Social Security retirement benefit?
A.: Probably not. The 40 credits are the minimum number you need to qualify for retirement benefits. However, we do not base your bene fit amount on those credits; it’s based on your earnings over a lifetime of work. To learn more about how you earn Social Security credits and how they work, read or listen to our publication How You Earn Credits, available at www.ssa.gov/pubs.
Q.: Are Social Security numbers reas signed after a person dies?
A.: No. We do not reassign Social Security numbers. In all, we have assigned more than 500 million Social Security numbers. Each year we as sign about 5.5 million new numbers. There are over one billion combina tions of the nine-digit Social Security number. As a result, the current system has enough new numbers to last for several more generations. For more information about Social
Security, visit our website at www. ssa.gov.
Q.: Is it illegal to laminate your Social Security card?
A.: No, it is not illegal, but we discourage it. It’s best not to laminate your card. Laminated cards make it difficult — sometimes even impos sible — to detect important security features and an employer may refuse to accept them. The Social Security Act requires the Commissioner of Social Security to issue cards that cannot be counterfeited. We incorpo rate many features that protect the card’s integrity. They include highly specialized paper and printing tech niques, some of which are invisible to the naked eye. Keep your Social Se curity card in a safe place with your other important papers. Do not carry it with you. Learn more at www.ssa. gov.
Q.: Someone stole my Social Security number, and it’s being used repeatedly. Does Social Security issue new Social Security numbers to victims of repeat ed identity theft?
A.: Identity theft is one of the fastest growing crimes in America, so you aren’t alone. If you’ve done all you can to identify and fix the problem, including contacting the Federal Trade Commission (FTC), but someone is still using your number, Social Security may assign you a new number. If you decide to apply for a new number, you’ll need to prove your identity, age, and U.S. citizen ship or immigration status. You’ll also need to provide evidence you’re having ongoing problems because of the misuse of your current Social Security number. You can read more about identity theft at www.ssa.gov/ pubs.
Julie Sheedy is Loretto’s chief marketing and engagement officer.Our united exper tise brings you advanced technology and streamlined care. As par t of the Upstate Hear t Institute, we provide connec tions to research and surgical care.














Now more than ever, your emotional wellbeing is key to overall health. Having meaningful connections with others is important for both physical and mental health.


Spend time with family and friends. Connections and support are important for your emotional health.
You don’t have to pump iron or run a marathon. Short walks around the block throughout the day have big benefits.
Check out our podcast episode, “An Honest Conversation About Mental Health” in the Community Check-in. Find it wherever you listen to podcasts.
Find a new hobby or old one. Or sign up to volunteer somewhere. You’ll give your brain and mood a boost.

The Community Memorial
(CMH) health care system recently an nounced that physician Grego ry Ripich has joined the organization’s surgery team as a general surgeon. This addi tion provides the community with a greater scope of care and allows CMH to care for a greater volume of patients. Ripich will perform elective procedures and surgeries, specializing in various surgeries such as colon and rectal, breast, thyroid, skin and wound.
service fellow working with victims of domestic violence and assisting in legal matters for persons with mental illness. She has worked on numer ous committees, campaigns and boards. She currently serves on the CNY NOW board of directors and supervises election day polling sites for the Onondaga County Board of Elections.
Christopher Community, Inc.
Gregory Ripich
has announced the appointment of Joe Harris as director of facilities and construction.

“The Community Memorial team is excited to bring Dr. Ripich on board. He brings a broad range of skills and experience to our patients,” said physician Michael Walsh, chief medical officer. “With his focus on a specialty covering various medical issues, we’re confident that patients will be pleased with the care offered here in Hamilton.”
Ripich studied neurobiology at Cornell University, where he also played lacrosse and continued his education at the University at Buf falo before graduating from SUNY Health Science Center at Syracuse. His postgraduate training was at St. Joseph Mercy Hospital in Michigan. His extensive career has defined his surgical interest and experience in advanced minimally invasive sur gery and endoscopic procedures. He most recently served as the medical director for Surgical Associates of CMA in Ithaca.
Crouse
Health has become the only hospital in Central New York to acquire the innovative da Vinci SP (single port) system, which provides surgeons with ro botic-assisted technology designed for access to tissue in the body with greater precision and enhanced mo bility, according to a hospital news release.
The da Vinci SP’s innovative design enables single port placement and optimal internal and external range of motion (e.g., 360-degrees of anatomical access and rotation) through the single SP arm. Surgeons control the fully articulating instru ments and the camera on the SP system.
The SP platform allows surgeons to get inside the body in a very delicate way to perform minimally invasive surgeries that solve prob lems ranging from reconstructive to cancer surgery.
Currently, the new robotic system is being used for prostatecto my procedures, says Crouse Health urologist Po Lam, who has more than 17 years of experience using the da Vinci robotic technology.

“The ability to enter the body through a single, small incision helps surgeons perform procedures in a less invasive way, helping to reduce trauma and discomfort to the pa
tient,” said Lam.
“This advancement in robotic surgery allows for a unique option to prostate removal in patients with pre vious abdominal surgery. Not only do patients not need to worry about previous scar tissue, the SP approach eliminates the risks of bowel injury.”
Other patient benefits making for an all-around improved patient experience include faster recovery, reduced risk of infection and shorter hospitalization, according to Lam.
Since its inception in 2008, Crouse Health’s robotic surgery program has grown to become the region’s largest multispecialty robotic surgery program, performing more than 1,900 procedures in 2021, ac cording to the hospital.
With seven surgical robots and 25 surgical specialists supporting the program, specialty areas include general surgery; bariatric; colorectal; GYN oncology; gynecology; thoracic and urology.
“We are proud of the program we have built in collaboration with many of the region’s top surgeons and look forward to utilizing this innovative technology to continue to improve patient outcomes,” said Crouse Chief Medical Officer and Chief Operating Officer Seth Kronen berg, a physician.
Sandra Carter has been appoint
ed executive director of NAMI Syracuse. She previously served on the organization’s board of direc tors.
NAMI Syra cuse, an affiliate of New York State NAMI and National NAMI (National Alli ance on Mental Illness) is a nonprofit, self-help, support and advocacy organization dedicated to improving the lives of all persons affected by mental illness through outreach, edu cation and community collaboration.
Sandra Carter

She earned her Master of Social Work degree at Syracuse University and has a professional background in public policy, mental health advoca cy and capacity building for small nonprofits.
She is experienced in grant writing and reporting, fundraising and event planning, and campaign management. She has served two years as an AmeriCorps National
Joe Harris
“Our organi zation is pleased to welcome Joe as director of facilities and construction,” said Christopher Community President and CEO Justin Rudgick. “His 20-plus years of experience in facilities, property management, and commercial–resident construction will be a tremendous asset to Chris topher Community and our portfolio of properties and new projects.”
Harris has extensive knowledge and experience with day-to-day orga nizational leadership and manage ment, as well as strategic direction and oversight on several capital projects throughout his career.
A resident of Brewerton, Harris is a graduate of Alfred State College, with an associate’s degree in applied science – mechanical engineering.
Sarah Morse has been promoted to director of intensive care unit and respiratory therapy at Oswego Hospital. Sstarted at Oswego Health

as an RN in the ICU in 2010. She spent nine years caring for critically ill patients through out the commu nity. In 2019 she started a new track as a clinical trainer, before transitioning to clinical admin, clinical trainer and staff educator in 2020.
Sarah Morse
Morse has been instrumental in training clinical staff at Oswego Hos pital and has served as mentor to so many. Most recently she was pivotal in onboarding 17 graduate nurses.
Page 30 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • October 2022 Health News “Throughout the pandemic, Sarah has proven to be not only a remarkable RN and educator but a leader who has continuously stepped up and often one who took on addi tional shifts in the ICU to help her colleagues, said Director of Nursing Melissa Purtell. “We’re so proud of her accomplishments and look for ward to continuing to see her grow here at Oswego Health.”
Crouse Health urologist Po Lam, has more than 17 years of experience using the da Vinci robotic technology. “The ability to enter the body through a single, small incision helps surgeons perform procedures in a less invasive way, helping to reduce trauma and discomfort to the patient,” he says.ConnextCare has appointed three new family nurse practi tioners at the Mexico, Phoenix and Pulaski offices and a social work er at the APW School Based Health Centers.
• Carolyn Dudden, a certified family nurse practitioner, graduated from SUNY Upstate Medical Univer sity earlier this year with a master’s degree in nursing. Dudden had pre viously worked in various hospitals in the Syracuse and Rochester areas before joining the team at Connex tCare. She will work in the Mexico office.

• Alison Flood, a certified family nurse practitioner, attended SUNY Upstate Medical University where she received her master’s degree in nursing. Prior to joining Connext Care, Flood worked at Upstate Uni versity Hospital as well as working as a cross country traveling nurse. She will see patients in Phoenix.
• Amanda Quinn, a certified family nurse practitioner, graduated from SUNY Upstate Medical Uni versity with a master’s degree in nursing. Previously, Quinn worked at both Upstate and St. Joseph’s hospi tals in Syracuse. She will be based in Pulaski.
• Erica Monaco, who holds a LMSW (licensed master social work) degree will work in the school based health centers at the APW elementary and high school. Monaco attended Keuka College and then the University of Kentucky, where she received her Master in Social Work degree. Before joining ConnextCare she worked as a clinician at Elmcrest Family Transitions. Monaco will offer behavioral health services to students in the APW district that are enrolled in the school-based health center pro gram. Services offered will include individual counseling, group coun seling, substance abuse counseling, family counseling and more.
“ConnextCare has committed to training family nurse practitioner students across our network, which has led to the successful recruitment of this local and talented provider staff,” said Tricia Peter-Clark, presi
dent and CEO of ConnextCare. “The addition of these four new providers allows for increased stability and access across ConnextCare’s network as we continuously work to meet the needs within our community.”
seph’s School of Nursing in Syracuse (now known as St. Joseph’s College of Nursing) and worked as a charge nurse on a cardiac telemetry unit and then an endoscopy unit at the hospital.
Natoli resides in Baldwinsville with her family.
Loretto promoted long-time
its commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guide lines, ultimately leading to more lives saved and reduced disability.
Tammy Natoli
employee and registered nurse, Tammy Natoli, to director of marketing and intake at PACE CNY. In her new leadership role, Natoli will play an integral part in promoting PACE CNY programs and services by developing, maintaining and implementing existing and new marketing plans that align with Loretto’s business initiatives. Natoli will report to the executive director at PACE CNY.
An employee of PACE CNY since 2001, Natoli has spent the past 21 years working at the organization as a registered nurse intake coordinator, a role that also supports the sales and marketing department. Before joining Loretto, Natoli worked as a registered nurse at POMCO and at St. Joseph’s Hospital Health Center (now known as St. Joseph’s Health Hospital).
In her new role, Natoli will collaborate closely with the vice president of marketing to develop and execute new marketing efforts that meet all government regulatory guidelines while supporting Loretto’s overall business goals and initiatives. In addition, Natoli will maintain reg ular contact with established markets and identify new opportunities. She will also supervise, educate, devel op and direct all intake specialists and admissions representatives to maximize potential in reaching their personal and enrollment goals of PACE CNY. As a director, Natoli will also help support the career devel opment and growth of other PACE CNY employees.
Natoli is a graduate of St. Jo
Laboratory Alliance of CNY is moving its corporate offices on Aug. 4-5 to be closer to the company’s main laboratory located in the Elec tronics Business Park in the town of Salina.
The corporate offices building is located at 115 Continuum Drive, Liverpool, directly across from the operations center main laboratory in the office and industrial business park that is home to Lockheed Mar tin Corp.
The space will house the compa ny’s management, human resources, finance, information systems, cus tomer service, marketing and sup port staff.
“In 2006 our corporate offices were relocated a couple miles away to dedicate much-needed floorspace to our operations center laboratory,” Jeff Coyne, director of sales sup port and services, said. “Returning our corporate offices to Electronics Business Park aligns with our plans to expand to meet increased regional and national requests for our labo ratory services. The close proximity to our main lab, the additional floor space and the contemporary reno vation made this the perfect site for Laboratory Alliance as we approach our 25th anniversary.”
All phone numbers will remain the same.
In addition to the corporate offic es and operations center, Laboratory Alliance has 11 patient service centers in Onondaga, Madison and Oswego counties and two rapid response lab oratories that provide on-site testing at St. Joseph’s Health and Crouse Hospital.
St. Joseph’s Health has received the American Heart Association’s Stroke Silver Plus with Target: Type 2 Diabetes Get With The Guidelines –Stroke quality achievement award for
Stroke is the No. 5 cause of death and a leading cause of disability in the United States. A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts. When that happens, part of the brain cannot get the blood and oxygen it needs, so brain cells die. Early stroke detection and treatment are key to improving survival, minimizing disability and accelerating recovery times.
“We are proud to be a primary stroke center and this latest recogni tion proves that St. Joseph’s Health is committed to improving patient care by adhering to the latest treat ment guidelines,” said Fahed Saada, neurologist at St. Joseph’s Health. “Get With The Guidelines makes it easier for our team to put proven knowledge and guidelines to work on a daily basis, which studies show can help patients recover better. The end goal is to ensure more people in Central New York can experience longer, healthier lives.”
Get With The Guidelines puts the expertise of the American Heart As sociation and American Stroke Asso ciation to work for hospitals nation wide, helping ensure patient care is aligned with the latest research- and evidence-based guidelines. Get With The Guidelines – Stroke is an in-hos pital program for improving stroke care by promoting consistent adher ence to these guidelines, which can minimize the long-term effects of a stroke and even prevent death.
Each year, program participants qualify for the award by demon strating how their organization has committed to providing quality care for stroke patients. In addition to following treatment guidelines, Get With The Guidelines participants also educate patients to help them manage their health and recovery at home.

St. Joseph’s Health also received the American Heart Association’s Target: Type 2 Diabetes Honor Roll) award. Target: Type 2 Diabetes aims to ensure patients with Type 2 diabe tes, who might be at higher risk for complications, receive the most upto-date, evidence-based care when hospitalized due to stroke.
October 2022 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 31 Health News With nearly 80 providers across 15 sites, ConnextCare strives to con tinue to be the largest primary care provider in Oswego County.

