P.6




1,800 MILE BIKE RIDE Upstate to Florida Upstate New York man embarking on a bike trip to Florida to raise money for three nonprofit organizations. P. 8 FREE Michael Slattery rides his bike on the Erie Canal in Fairport. Photo provided. Nursing National Nurses Month Celebration May 1-31 CNYHEALTH.COM MAY 2023 • ISSUE 281
Physician
Declines The highest paid specialty: neurosurgery — salary of about $746,000. Read George Chapman’s column on p. 6 Crouse neurosurgeon Raghu Ramaswamy talks about the stroke that killed Fleetwood Mac singer Christine McVie. P. 4 How Content Are You? Q&A with TRICIA PETERPresident and CEO of ConnextCare discusses further expanding the organization. P. 13 THINGS YOU SHOULD KNOW ABOUT ALLERGIES Take the Quiz Inside 5 P. 10 P. 12
Pay

















Page 2 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023 UPSTATE.EDU/NURSING Celebrating Nurses Week 2023: THANK YOU FOR WHO YOU ARE AND ALL YOU DO. Cardiovascular Group UPSTATE CARDIOLOGY CONTINUES TO GROW Our united exper tise brings you advanced technology and streamlined care As par t of the Upstate Cardiovascular Group, we provide connec tions to research and surgical care. OUR UPSTATE CARDIOLOGY TEAM CONTINUES TO GROW. PHYSICIANS FROM TOP LEFT: Dana C Aiello, MD Larr y S Charlamb, MD Mark J Charlamb MD Christopher A Nardone, MD Michael Fischi, MD Charles Perla MD Theresa Waters, DO Andrew M Weinberg, DO Timothy D Ford, MD Rober t L Carhar t, Jr , MD Debanik Chaudhuri, MD Hani Kozman MD Sakti Pada Mook herjee, MD Amy Tucker MD Daniel Villarreal, MD O U R OF F I C E LO C AT I O N S 5112 WEST TAFT R OAD Liverpool • 315-701-2170 510 T O WNE DRIVE Fayetteville • 315-663-0500 90 PRESIDENTIAL PL A Z A Syracuse • 315-464-9335 208 TOWNSHIP BLVD Camillus • 315-488-2372 102 WEST SENE C A STREET Manlius • 315-464-9335 138 EAST GENESEE STREET Baldwinsville • 315-720-1305

May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 3
Crouse Health nurses make a difference — to our patients, their families, our community and their colleagues. We honor them during Nurses Week — and every day — for their dedication and commitment to providing the best patient experience possible. Thank you for making every moment matter. NATIONAL NURSES WEEK | MAY 6 -12 crouse.org/RN Our Nurses. Our Future.
Thank You.
Hugh Jackman Urges Sunscreen Use After Skin Cancer Scare
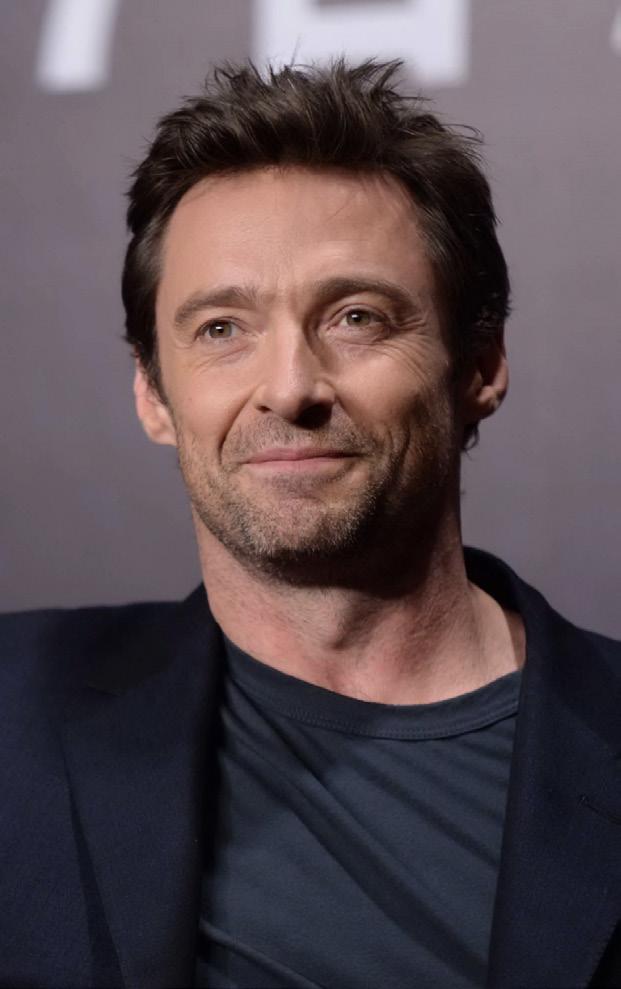
Actor Hugh Jackman is offering a warning about sun damage and skin cancer after having two biopsies.
Jackman was recently wearing a bandage on his nose in a video posted to his Twitter account.
"I just went to my doctor... and she just saw little things — could be or could not be basal cell, in her opinion. She doesn't know," Jackman shared. "Summer is coming for those of us here in the northern hemisphere. Please wear sunscreen. It's just not worth it no matter how much you want to tan. Trust me, trust me, trust me."
Basal cell carcinoma is common and not as potentially harmful as some other types of skin tumors, such as melanomas. It's the type of skin cancer that President Joe Biden had removed after a recent physical.
Jackman, 54, urged people to wear sunscreen. He previously was treated for basal cell carcinoma in 2013, 2014 and 2016.
Jackman reminded viewers that UV exposure in youth can leave a legacy of skin cancer decades later.
"This is all stuff that happened 25 years ago and it is coming out now," he said, pointing to the bandage on his nose. "Put some sunscreen on — you'll still have an incredible time out there."
About eight of every 10 skin cancers are basal cell carcinoma, according to the American Cancer Society.
According to the American Academy of Dermatology (AAD), people can protect themselves by wearing a broad-spectrum sunscreen that protects against UVA and UVB rays, preferably with an SPF of 30 or higher every day. Wear it even on cloudy days, the AAD says.
Avoid tanning beds and sun lamps. If possible, stay out of the sun between 10 a.m. and 2 p.m., when the sun's rays are strongest. Seek shade.
Meet Your Doctor
By Chris Motola
Ramaswamy,
Crouse:
Q: We wanted to lead in on the topic of stroke with Fleetwood Mac singer Christine McVie who recently died of a stroke at 79. How common a cause of death is that for a woman of her age?
A: If you look at stroke statistics that we have, about 87% of stroke patients have the kind of stroke that happened to the singer. These are called ischemic strokes. So we’re talking about over 800,000 people in the U.S. every year are having these kinds of strokes. To put it in perspective, that’s one stroke every 40 seconds and one person dies of a stroke every four minutes. So it’s a fairly common cause of death. It’s the fifth leading cause of death in the U.S.
Q: Have these statistics been fairly consistent over time?
A: Hopefully with the kinds of treatments we’ve started for strokes, the disability and death rates are coming down, but it’s still far too many.
Q: What characterizes an ischemic stroke?
A: There are two main types of stroke. Ischemic is the most common and happens in about 85%- to 90% of stroke cases. The remaining are hemorrhagic strokes, which includes bleeding in the brain or subarachnoid hemorrhages from aneurisms. Ischemic strokes happen due to lack of blood flow to the brain from whatever cause, usually
MBBS
Q: Is stroke mainly a consequence of the same conditions that cause heart attacks? Things like atherosclerosis?
A: Yeah, exactly. If you look at heart disease, atherosclerosis due to basic medical conditions like high blood pressure, high cholesterol, obesity, diabetes, smoking are all major causes. It’s the same for strokes as well. Cardiac disease itself is a very common cause of ischemic strokes. Clots that are formed within the heart can go to the brain and cause an ischemic stroke, so there’s a very big overlap between heart disease and stroke.
Q: Where do the causes diverge?
A: There are other causes for ischemic strokes as well, like some patients who have hypercoagulative diseases. They’re more prone to strokes as well because their blood is basically a lot more prone to clotting. Or in patients who have cancer. They have a tendency toward hypercoagulability. So they can build up a stroke in isolation without necessarily having any cardiac issues.
Q: I noticed in the case of McVie, she also had a cancer diagnosis.
A: Yeah, she did. Although it also appears that she had atrial fibrillation, so it’s very difficult to pinpoint which was the likely cause, but the fact that she had a thrombus in the heart probably makes it likelier.
ference in reducing the number of strokes.
Q: On the interventional side, how quickly do you need to act to minimize or prevent damage from a stroke?

A: When it comes to stroke, time is of the essence. Every second you’re looking about 32,000 brain cells that are dying. So time is of extreme importance. The first thing is recognizing when someone is having a stroke. We have an acronym called FAST. F is for face weakness or droop. A is for arm or leg weakness. S is for slurred speech. And T is for time to call 911 if you noticed any of these symptoms. Once you get to a place like Crouse, which is a comprehensive stroke center, everything moves very, very quickly. We have a separate code for patients having a stroke. It’s like an alarm for different people: emergency physicians, imaging units, etc. They stop doing whatever they’re doing and don’t take any other patients until the stroke patient has been imaged. The same pager goes to neurosurgeons, neuro-interventional radiology techs and nurses; everyone involved in treating stroke. So stroke patients are immediately reviewed by the emergency team, patients are rushed to the CT scan unit where they are scanned to make sure it’s not a bleed in the brain.
Q: What’s the next steps?
A: Once [the stroke] is confirmed, they undergo vascular imaging to see if there’s a large vessel occlusion, which is crucial. And they also have a profusion scan, which basically tells us what damage has already happened, and what kind of damage can happen if action is not undertaken. The area at risk but not yet damaged is called the penumbra. So if there’s a large penumbra and a large vessel occlusion, patients are given clot-busting drugs before intervention. They’re rushed to undergo a mechanical thrombectomy where we either use large-bore catheters to suck out the clot or stent-retrievers, which are metal meshes which can catch the clot and help us pull it out to hopefully open the artery. The faster we do all this, the better the outcomes.
Note: MBBS are MD-equivalent degrees given by medical schools that follow the United Kingdom medical education system. The acronym is derived from Latin and mean “bachelor of medicine, bachelor of surgery.”
Lifelines
Name: Raghu Ramaswamy, MBBS
Position: Neurointerventional physician at Crouse Hospital

Hometown: Bangalore, India
Education: St. John’s Medical College/ Hospital Bangalore University, India
Training: Completed residency in the United Kingdom rotating between Manchester and Preston. Completed his fellowship in skull base neurosurgery at John Radcliffe Hospital in Oxford. Completed an additional fellowship in spinal neurosurgery from Temple University Hospital in Philadelphia, Pennsylvania. He completed his final fellowship in endovascular neurosurgery at SUNY Upstate Medical Center in Syracuse, New York.
Affiliations: Crouse Hospital
Organizations: American Association of Neurological Surgeons
Family: Married, two kids
Hobbies: Wildlife photography
Page 4 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
Neurosurgeon at
‘With the kinds of treatments we’ve started for strokes, the disability and death rates are coming down’
Raghu
Healthcare in a Minute
By George W. Chapman
Medicare Hospital Fund in Jeopardy
The trustees of the Medicare hospital trust fund have projected the fund will be depleted by 2031. Incoming Medicare taxes after that will be insufficient to rebuild a reserve. Thanks to the InflationReduction Act, which fixes monthly insulin costs at $35 and authorizes Medicare to negotiate a few drug prices effective 2026, the fund would have been depleted three years sooner in 2028. So that begs the obvious question: if the projected savings in insulin costs and a dozen or other drugs can push the depletion date out three years, why not let Medicare negotiate all drug prices? Answer: the drug lobby.
Putting Off Care
Artificial Intelligence in Healthcare: Guarded Optimism, Trepidation Among Providers
Artificial intelligence, like ChatGPT (Generative Pretrained Transformer), is being met by providers with the same guarded optimism and trepidation as the now firmly entrenched electronic medical record.
But unlike the electronic medical record, which was slowly and painfully incorporated into healthcare over several years, chatbots will become an integral part of healthcare seemingly overnight.
Google’s chatbot scored 85% on a practice medical licensing exam. Another chatbot scored 90% on a law bar exam.
As with the electronic medical record, if AI is not used properly, there are concerns over privacy, equity, safety and quality. Proponents of chatbots in healthcare see win-win scenarios for providers and
their patients. Chatbots will relieve providers and their support staff of several menial administrative tasks, thereby freeing them to spend more time with their patients and critical clinical issues.
Industry experts believe AI will increase access, improve the patient experience, lower costs and prevent many heretofore frustrated physicians and nurses from leaving healthcare altogether.
Basically, chatbots can: automatically refill prescriptions; provide basic, necessary medical information; check symptoms; assist with coverage and claims; instantly respond to queries; recommend wellness programs; provide medical assistance; and schedule appointments. And all this 24/7.
Physician Compensation Declines

According to a survey of 31,000 full time physicians by Doximity, the average physician compensation declined 2.4% last year. (It went up 3.8% in 2021.) The decline occurred despite a predicted MD shortage, a significant rise in operating costs, and MD burnout. According to the AMA, when adjusted for inflation, Medicare reimbursement declined 22% between 2001 to 2012. (Commercial carriers tend to follow suit.)
According to Doximity, the highest paid specialties are:
• Neurosurgery, $746,000
• Thoracic surgery, $668,000
• Orthopedic surgery, $605,000
• Plastic surgery, $539,000
• Oral and maxillofacial surgery, $538,000
• Vascular surgery, $534,000
• Cardiology, $527,000
• Radiation oncology, $516,000
• Gastroenterology, $486,000
• Radiology $485,000.
Even though 90% of us have health insurance, many are saddled with increasingly higher deductibles and co-pays as employers continue to shift more of the costs to employees. Not surprisingly, most consumers are clueless about their benefits and out-of-pocket costs until they are confronted with a health crisis. Healthcare in our country is confusing, frustrating and terribly expensive. Healthcare debt is still the No. 1 reason for bankruptcy. A recent survey of over 1,000 consumers by a national consulting firm revealed:
• Over 50% of respondents are concerned about their ability to pay for a major healthcare event;
• 65% said they are not able to afford a new $250 a month expense to manage a chronic condition and related medications;
• 64% said they would delay or skip necessary care if they were unsure of their ultimate out of pocket responsibility.
Ironically, putting off care to save money can result in even higher costs to patients as symptoms not treated early worsen over time until there is an acute medical crisis. This non adherence eventually impacts quality, outcomes, productivity and even provider burnout. Hospitals have been slow to display mandatory pricing information on their websites. Once in compliance, this should help consumers calculate what their insurance will pay and then what they will owe out of pocket for selected procedures.
Exchange Rates Up 3.4%
According to an analysis by the Robert Wood Johnson Foundation, health insurance premiums on the federal exchange increased about 3.4% this year. The enhanced subsidies provided by the federal government resulted in record breaking enrollment. The number of insurance companies on the exchange increased to 232. Premiums on the exchange actually dropped 2.2% from 2019 through 2022. The reasons for the 3.4% increase this year are: high inflation beginning last year; uncertainly over enhanced income-based subsidies (the Inflation Reduction Act eventually continued the enhancement through 2025); the end of continuous coverage requirements through the pandemic; uncer-
tainty over the lingering impact of COVID19 and newer strains. Most commercial insurance premiums increased for the very same reasons.
Uber More Than Rides
Uber has been providing non-emergent medical transport (NEMT) since 2018. Uber’s newest venture is delivering prescriptions, over-the-counter drugs and healthy foods. Providers will use the same Uber platform they already use to arrange rides for their patients. Patients who lack their own transportation are more likely to be non compliant by missing medical appointments or by not taking their meds. Uber ride and prescription delivery services are becoming more popular with providers under value-base, contracts which reward providers for positive patient outcomes.

HIPAA Privacy Violations
Health Affairs analyzed over 3,700 hospital webpages and found just about all of them incurred at least one third-party data transfer. Specifically, 98.6% had at least one third-party data transfer and 94.3% had at least one third-party cookie. The median number of third-party transfers was a whopping 16. The leading culprits were Alphabet 98.5%; META 55.6%; Adobe 31.4%; and ATT 24.6%. Angry consumers, feeling their privacy has been violated, have filed individual and class action lawsuits against hospitals for sharing their personal information with these website trackers.
Another Attack on the ACA
The Affordable Care Act mandates that insurers offer free prevenservices including screening for breast cancer, cervical cancer, diabetes and vision testing for preschoolers. Inexplicably, judge Reed O’Connor, the same judge who tried to kill the entire hugely popular act in 2018, has ruled that some of the mandated free preventive services are illegal. Really? Who brought this suit? Just about every commercial carrier has vowed to continue with free preventive services because it saves lives and money in the long run.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

Page 6 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023


May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 7 © 2023 St. Joseph’s Health. © 2023 Trinity Health. All rights reserved. At St. Joseph’s Health, we know that nurses are exceptional people. Day in and day out, they provide the safest care for our patients, our community and each other. This week, as with every week, we share our heartfelt appreciation for all that nurses do. A higher level of care is all thanks to you. Work beside the best. jobs.sjhsyr.org Apply to our team today: SJH10290_NR_FY-23_In-Good-Health_9.75x13.75_No-Bleed.indd 1 4/25/23 12:11 PM
Biking for the Best of Reasons
Upstate New York man embarking on a 1,800 mile bike trip to rase money to three nonprofit organizations
By Mike Costanza
Michael Slattery just loves putting miles on his bicycles.
“I average about 5,000 miles a year,” says the deputy town supervisor of the town of Chili.
The married, 57-year-old grandfather plans to put his love for cycling to use for worthy causes on May 8, when he sets out on an over 1,800 mile jaunt down the Eastern Seaboard to raise money for three nonprofits.



The money Slattery brings in will go to the Pirate Toy Fund, the National Center for Missing and Exploited Children and Honor Flight Rochester.
Slattery plans to start his trip in Charlotte and head south, rolling through Penns ylvania, Maryland, Virginia, North and South Carolina and Georgia before ending up in Florida 25 days later. Along the way, he’ll stop at the Alexandria, Virginia headquarters of the National Center for Missing and Exploited Children (NCMEC) as part of his fundraising efforts.
NCMEC, the largest and most influential nonprofit child protection organization in the U.S., helps find missing children, strives to decrease child sexual exploitation and tries to
prevent child victimization.
“We lead the fight to protect children, creating vital resources for them and the people who keep them safe,” says Edward Suk, executive director of NCMEC’s New York branch.
Slattery says the deaths of two young women, 20-year-old Fairport resident Lisa Eisman and 17-yearold Brittanee Drexel of Chili, made NCMEC’s fight particularly important to him. Both young women died violently.
Eisman was Slattery’s cousin. She and her college roommate, who were students at the State University College at Buffalo, were beaten to death in 1985 while hitchhiking to Fort Lauderdale on spring break. Drexel disappeared in 2009 while on a trip to Myrtle Beach. Slattery coached her for a time when she was on the team Chili Soccer.
“My daughters grew up with Brittanee,” he says. “For me, it’s personal.”
NCMEC aided the search for Drexel.
“We had our local and national case management team involved in cultivating leads with law enforcement,” Suk says. “We also handled
targeted poster distribution, and media outreach through our media team.”
Raymond Moody, Drexel’s killer, was convicted of kidnapping, murder and first-degree sexual in late 2022. He was sentenced to life in prison on one charge and 30 years each on the other two charges. Slattery plans to visit the place where Drexel’s remains were found while en route to Florida, and to visit NCMEC’s Washington offices as part of his fundraiser.
Slattery’s upcoming journey south is just one of the rides he’s taken to raise money for NCMEC. Just last year, he participated in The Ride for Missing Children, NCMEC’s annual fundraiser. Mounting his bike, he pedaled through Buffalo, Rochester, Syracuse, Utica and Albany, covering about 100 miles in each city.
Since 1995, the Pirate Toy Fund has headed to hospitals and other locations in the greater Rochester area to distribute new toys to needy children free of charge. As Slattery pedals along to raise money for the nonprofit, he’ll have a friend at his back—literally. Otto Harnischfeger, the Pirate Toy Fund’s executive director, will follow him down the road in an RV, providing aid.
“I can’t believe he’s doing it,” Harnischfeger says of his good friend. “I ride five minutes and I’m sore. I want to get off the bike.”
Harnischfeger has known the Slattery family since he became
friends with Raymond Slattery, Michael’s father, when the two were on the Rochester Police Department.
“It’s a caring family, they really are,” Harnischfeger says.
The money Slattery raises on his long-distance ride should be welcome.
“Our first year we gave out 300 toys,” Harnischfeger says. “Last year, we gave out over 36,000 toys free of charge, all because of the good nature of the Rochester community.”
In addition to raising money for the Pirate Toy Fund, Slattery sits on the nonprofit’s board of directors.
Six times a year, about 60 veterans and their helpers, called “guardians,” head out of Rochester for a weekend in the nation’s capital, courtesy of Honor Flight Rochester.
“Honor Flight Rochester provides airplane trips for veterans to travel together to see their memorials in Washington DC to receive that long-delayed thank-you that they’d not received many years ago,” says Richard Stewart, the nonprofit’s president and CEO.
The trip to the nation’s capital includes hotel accommodations, tours of the World War II, Korean War and Vietnam War memorials and other important sites and a gala dinner in honor of those who once served their country. The veterans travel free, but their guardians, who are usually family members or friends, have to cover part of the cost of the trip.
Slattery says he plans to stop in Washington this May to accompany an Honor Flight Rochester group as it visits memorial sites. After that, he’ll have lunch with them and get back on his bike.
“I plan on leaving Washington in the early afternoon, so I can get in about 30 miles or so,’ Slattery says.
Honor Flight Rochester, an all-volunteer organization, spends about $500,000 a year on its services to veterans, and is supported by donations. Stewart says the nonprofit is able to cover its current costs, but will have to fund new trips to Washington in the future.
“We have a fly-list of 1,000 veterans,” Stewart says. “If we don’t have money, we don’t fly.”
Slattery’s ride south is just his latest effort to help his community.
He has also raised money for other nonprofits, including Camp Good Days & Special Times, which offers residential camping programs and recreational and support activities to children who are affected by cancer or sickle cell anemia and their families. In addition, Slattery sits on the Chili Town Board.
“It’s a passion for me,” Slattery says. “I enjoy giving back.”
The father of two grown daughters and grandfather of four children recently retired from the Monroe County Department of Transportation, where he was the highway maintenance manager.
How to Donate
For more information about Slattery’s upcoming ride or do donate to his fundraiser, go to: michaelscharityride.com.
For more information on the nonprofits for which he plans to raise money, go to: www.missingkids.org/ footer/about/newyork, www. piratetoyfund.org or https://honorflightrochester.org.
Page 8 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
Half of Drivers Say They Often Use Cellphones Behind the Wheels
Texting and driving can be deadly. Holding your phone in your hand to talk and surfing the internet while behind the wheel is dangerous, too.
This is widely known, but a new survey finds that about half of all respondents still use an electronic device most or every time they drive.
“I'd say it's not as much surprising as it is frustrating,” said Adam Snider, a spokesman for the nonprofit Governors Highway Safety Association (GHSA), which wasn't involved in the study but issued a news release after it was released. “Distracted driving is something that is incredibly pervasive.”
In the survey, conducted by the Insurance Institute for Highway Safety (IIHS), more than 2,000 licensed drivers were asked how much they agreed with dozens of statements designed with the health belief model in mind.
That model is described as a behavioral change theory developed to understand why some people don't adopt a certain health behavior. It's usually applied to illness or disease prevention, according to the study.
“I think the results from this study really help shed some light on the reasons why” people are still using their phones in their cars, said
lead author Aimee Cox, a research associate with the IIHS.
Cox said that appears to include “the need or the perceived need to respond to family or friends, the need for information, all these things that modern cellphones have really allowed us to do without thinking about it.”
While distracted drivers are using their phones while driving because they don't want to miss a call from their kids, for example, it's also their family members who they say could motivate them to put the phones down.

“I think that provides a really unique opportunity to where if we can encourage that open and safe communication and dialogue, we can have teen drivers and kids encouraging their parents to practice safe driving behaviors and vice versa. I think it needs to go both ways,” Cox said.
Distracted drivers killed at least 3,000 people in 2020, according to a statement issued by GHSA CEO Jonathan Adkins. That was 8% of all traffic deaths.
Another 400,000 people are injured each year, Snider said, but it may very well be higher, because it can be hard to prove that distracted driving caused a crash.
Biggest Drop in U.S. Pregnancies Seen Since 2010
Pregnancy rates in the United States suffered a steep decline during the last decade, new government data shows.
The overall U.S. pregnancy rate fell by 12% between 2010 and 2019, according to figures released in April by the U.S. National Center for Health Statistics (NCHS).

The pregnancy rate among women aged 15 to 44 was 85.6 per 1,000 in 2019, down from 97.3 per 1,000 in 2010, the report found.
A drop in unintended pregnancies and teen pregnancies contributed to the overall decline in pregnancy rates.
Pregnancies among teens declined by more than half (52%)
during the 2010s, added the researchers, who were led by Lauren Rossen.
Likewise, unintended pregnancies experienced a 15% decline, falling from 42.1 per 1,000 in 2010 to 35.7 per 1,000 in 2019.
The drop in pregnancy rates is reflective of the overall decline in U.S. birth rates that has been going on since the mid-2000s, said Phillip Levine, a professor of economics at Wellesley College in Massachusetts.
“The report is not terribly surprising,” said Levine, who was not involved with the study. “We know that birth rates have been falling pretty dramatically, beginning around 2007.”
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 9
Congratulations to all of our Nurses throughout the ACH healthcare system! NATIONAL NURSES
Thank you for your compassion and for caring everyday for our community. EQUAL OPPORTUNITY EMPLOYER M/F/0/V/SO We honor all of our Employees during Hospital Week of May 7-13, 2023
DAY
By Gwenn Voelckers
Practical tips, advice and hope for those who live alone
How Content Are You? A QUIZ
The Oxford English Dictionary defines contentment as "the state of being happy and satisfied."
This dictionary definition sounds like a nice way to feel, doesn’t it? Oh, if we could just snap our fingers and be content with who we are and what we have.
Wouldn’t life be grand?
I’ve had the privilege of meeting and talking with a lot of women and men who live alone, and our conversations often turn to the subject of contentment: how to find it, how to keep it, and how to find it again once it has been lost.
Those on their own often feel a lack of something in their lives, and many have trouble letting go of a craving for things to be different.
I know. I’ve been there.
For years after my divorce, I had trouble seeing the good in myself and in my life. But with time, intention and practice, I was able to stop yearning for what I didn’t have and start appreciating what existed right in front of me.
It all began with an important first step — taking a hard look at myself.
While I’m no expert in survey design, I created the simple non scientific quiz below to help you
assess where you are on the road to contentment.
Your results may light a new and hopeful way forward.
HOW CONTENT ARE YOU?
Circle the choice that best answers the questions below:
1. If asked, can you readily name your own positive personal qualities? How many come to mind?
A. 5 or more.

B. 1 to 4.
C. Nothing really comes to mind.
2. How would you describe your home?
A. Very “me” — I’ve made it my own.
B. It’s fine. I keep meaning to redecorate, but I never get around to it.
C. My home looks as tired as I feel.
3. How would you describe your success in letting go of old ways of thinking and of negative thoughts or behaviors that keep you anchored in the past?
A. I live in the present; it’s full steam ahead!
B. I still wallow in self-pity from time to time.
C. I can’t let go of regrets and obsess about the past.
4. Could you imagine planning a trip by yourself and traveling alone to a new or familiar destination?
A. In a heartbeat.
B. Maybe someday.
C. I can’t imagine traveling solo.
5. Does going alone to a café for a cup of coffee or grabbing a bite to eat at a local restaurant feel comfortable — even enjoyable?
A. I do it all the time.
B. Occasionally, but I feel self-conscious.
C. I’m just not ready.
6. Do you exercise, get enough sleep, and stay on top of health screenings?
A. Of course!
B. A little, but I could do more for myself.
C. Sadly, I’ve neglected my health and fitness.
7. How often do you pamper or reward yourself by taking some time just for you or by purchasing that little something special you’ve had your eye on?
A. As often as I can.
B. I tend to put others’ needs before my own.
C. I can’t remember the last time I pampered myself.
8. Can you imagine your life without a special someone on your arm?
A. I would enjoy sharing my life with someone special, but I could also be perfectly content with my "family of friends."
B. Maybe, but not for long; I feel incomplete without a "one and only."
C. Life doesn't feel worth living when I'm not in love.
YOUR SCORECARD
Calculate your total points using this scale:
3 points for each A answer
2 points for each B answer
1 point for each C answer
8 points: Contentment may feel elusive at the moment-beyond your grasp. But it can be found. You may benefit from talking with a professional counselor or spiritual adviser. Help and encouragement might also be found in grief support groups and other gatherings — in person or online — that offer emotional support and practical advice.

9-15 points: You experience feelings of contentment, but you know there’s more to be found. Continue to stretch yourself. Reach out to others. And “try on” healthy pursuits outside your comfort zone. Success and achievement breed contentment. You might also find inspiration and a needed jump-start in workshops, lectures, and retreats devoted to personal growth and development.
16 points: Good for you — what you have is precious. Being content with yourself opens up all kinds of possibilities. It enables you to feel peace and joy, whether you are alone or in a committed relationship. It is an invaluable inner springboard on which you can launch all things imaginable!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com
Page 10 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
Live Alone & Thrive
My Turn
By Eva Briggs, MD

The Pros and Cons of Electronic Health Records


When I started my career, there was no such thing as an electronic medical record. My hospital progress notes and office notes were handwritten. A few documents such as hospital discharge notes were dictated, transcribed by a human and then typed on a typewriter, not a computer!
Now more than 90% of physicians use an electronic health record.
Part of the reason was the 2009 Health Information Technology for Economic and Clinical Health act. This act provided $36 billion in financial incentives to encourage hospitals and clinics to switch from paper charts to EHRs. Then-president Obama said this would “cut waste, eliminate red tape and reduce the need to repeat expensive medical tests.”

Another purported benefit was that EHRs would “save lives by reducing the deadly but preventable errors that pervade our health care system.”
The current state of EHRs is —in my opinion — a mess. There are certainly advantages in terms of legibility. But many bugs have yet to be ironed out.
A big drawback is that there are many different systems and for the most part they can’t speak to each
other. It’s similar to when two people who don’t speak the same language try to converse without an interpreter. A complex conversation can’t happen. That’s why when you go to a hospital facility, it doesn’t matter that your health record is “already in the computer.” Meaning your primary care provider’s computer. If your doctor’s office uses a different system, the hospital facility EHR can’t read it.
Another huge problem is the user interface. The American Medical Association recently teamed up with a healthcare organization called MedStar Health to examine the usability of two of the most widely used EHRs (Epic and Cerner.) Emergency physicians at four Washington D.C. area hospitals were asked to perform stan-
dardized tasks (ordering medications and tests) on a fictitious patient.
Here’s an example of the challenge of ordering acetaminophen (Tylenol) for an adult male patient. That seems like it ought to be quick and straightforward. First the doctor must locate the medication in the EHR. At one hospital the search for Tylenol brought up 80 — yes EIGHTY — options. This included doses for menstrual cramps and for infants, clearly not relevant to this scenario. But when the doctor tried to type in “Tylenol 500 mg.,” the most common strength, the EHR returned zero hits. The doctor had to return to the previous list and scroll down, where the correct dose was the 68th choice in the list. This simple task took a ridiculous amount of time and brain power. This is just one of many frustrations that EHR users face every day.
The researchers found that the time and number of mouse clicks to complete the same task varied widely from site to site. The confusing interface contributed to medical prescribing errors.
For example, when doctors attempted to order a tapering dose of medication, the system complexity meant that at one site the error rate was as high as 50%.
Another problem is the sheer volume of data entry physicians must complete. For example, researchers found that a 31-minute patient encounter consisted of 12 minutes of face-to-face patient interaction, and 19 minutes spent with the EHR. Some physicians use scribes to help enter data, a stop-gap solution that’s really a Band-Aid for the bigger
problem inefficient user interface design.
Is there hope in sight? Perhaps. Some companies are beginning to tap the power of AI to improve EHRs. For example, Epic developed a sepsis-prediction model and one hospital in Louisiana using this system reduced deaths from sepsis by 18%. But this and other “modules” offered by various EHR companies are addon purchases that drive up the cost of EHRs and are often out of reach of many hospitals, health care systems, and private practices.
I don’t want to go back to the paper chart days. But I hope that some day, the sooner the better, we will see EHRs that interface with one another and that are user-friendly.
In the meantime, if your healthcare provider asks you a question that you think is in your electronic record, it’s because they really can’t find it in there. It may be in an incompatible system. It may be buried in a clunky EHR bloated with useless data obscuring with the important stuff.
So it’s in your best interest to keep track of your own medical history and to be patient when we inquire about it.
The right diagnosis means everything.

Your doctor ordered laboratory tests. Tests can diagnose disease, assess the effects of treatment or confirm good health. When you and your doctors know more, you can make better choices sooner and plan the next steps. Decisions that are dependent on timely and reliable laboratory results.
Laboratory Alliance professionals work round the clock, 365 days a year. Laboratory tests make up an estimated 70% of your medical record. We understand the importance of what our testing provides and offer the technology vital to assure accurate and timely laboratory results.
We’re a partner in the care of your health. When you need lab work, we’re in your neighborhood. Learn more at laboratoryalliance.com.
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 11
Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.
Electronic health records were supposed to cut waste, eliminate red tape but the current state of EHRs is a mess
Things You Should Know About Allergies
 By Ernst Lamothe Jr.
By Ernst Lamothe Jr.
While nationwide the temperatures are trending upward and we are experiencing brighter forecasts, we are also seeing an increase in spring and summer allergies.
Around 50 million people suffer from allergies in the U.S., according to The American College of Allergy, Asthma and Immunology, which makes it a very common ailment.
“This is the time of year where allergies are most prevalent. These first few months of the spring can be difficult for allergy sufferers. That is also why it is essential to know what affects you,” said physician Nicholas Groch of Lakeshore ENT at Oswego Health.
Physician Melanie Groch, his wife, also works at Lakeshore ENT. She said because allergies run the gamut it is an ailment that a larger portion of the population has than people believe.
Both physicians discuss five aspects of allergy.
1.Symptoms
Allergic reactions can cause symptoms such as runny nose, sneezing, congestion, itchy or watery eyes and post nasal drip, said Nicholas
Groch. In addition, some people experience scratchy throat and fatigue. Allergies also affect your sleep. Allergies can make it difficult to breathe, leading to sleep apnea, snoring and other sleep disorders, according to Groch.
2.Treatment
Allergies are treated in various ways, ranging from over-thecounter medication such as antihistamines, decongestants and nasal sprays, to severe case solutions such as, allergy shots or immunotherapy. Immunotherapy treatment involves a series of injections of purified allergen extracts, usually given over a period of a few years.
Your physician will help you take steps to identify and avoid your allergy triggers. This is generally the most important step in preventing allergic reactions and reducing symptoms.

Allergy shots are given once a week for six months. It is typically done when allergy season is over so a patient can build tolerance. Then slowly the allergy shots are given once a month.
“There are various over-thecounter methods that can give you some of the relief you need,” said
Enjoy Life in Full Bloom
At Parkrose Estates, we want to help you live life to the fullest. Grab a cup of coffee with friends old and new at our cafe, focus on your health in our fitness center, and relax with a good book in our library. You’ll find what you’re looking for at Parkrose Estates.
Call us today at (315) 494-8050 to schedule your personalized visit and reserve your apartment!
*Some restrictions may apply. Contact community for details.
7251 Janus Park Drive
(315) 494-8050
• Liverpool, NY 13088
• www.ParkroseEstates.com
Melanie Groch. “Allergy shots have been known to be very effective especially when you determine what allergies affect you the most.”
3.Spring vs summer
Common symptoms of allergies include sneezing, runny nose or nasal congestion, itchy or watery eyes, post nasal drip, cough, or feeling tired. Knowing how to recognize and manage these conditions can improve quality of life and overall health.
There are certain trees that grow in different areas in the United States that affect people differently. The same person who lives on the East Coast may not suffer from any allergies. But that person may travel to Florida for vacation and may have constant allergic reactions.
“I have a patient that is only allergic when they cut the grass. They wear a mask and that is the only time they ever have an issue,” said Nicholas Groch. “They make sure to take a shower as soon as they finish mowing, making sure there is no pollen on their clothes.”
4.See a physician
If you think you have seasonal allergies, talk to your doctor. Experts can help you establish your triggers along with possible treatment options. Creating your personal blueprint will help you follow and manage your allergies. An allergist

can provide a skin test, which involves the patient being pricked with small amounts of proteins found in common allergens. If you’re allergic, the patient develops a raised bump or hive at the test location of the skin.
“A doctor will help you establish your triggers along with possible treatment options,” said Nicholas Groch.

5.Misconceptions about allergies
Sometimes the symptoms of allergies can mimic those of other conditions — a cold, for example — so it is important to be evaluated by your primary care doctor and, if needed, see an allergist. Respiratory allergies and colds look and feel a lot alike. Both cause sneezing, a runny or stuffy nose, and tiredness. But unlike allergies, colds are caused by a virus, so you can spread them to other people. Allergic rhinitis can be mistaken for a sinus infection, or coughing that is related to underlying asthma might be mistaken for bronchitis. To make sure of the diagnosis and receive the proper treatment, it is important to be evaluated.
“People sometimes see allergies as just affecting the nasal passages. But allergies can affect the lungs with asthma, the skin with hives and throat and tongue with aplastic shock from food allergens,” said Mealnie Groch.
Page 12 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
5
It’s not like home. It is home.™
Melanie Groch and her husband Nicholas Groch are both board-certified otolaryngologists. They provide care at Lakeshore ENT at Oswego Health.
Move Now & Save up to $3,000!* Editor & Publisher: Wagner Dotto • Associate Editor: Stefan Yablonski • Writers: Deborah J. Sergeant, Jim Miller, Gwenn Voelckers, Anne Palumbo, Chris Motola, Melissa Stefanec, Eva Briggs (MD), Mary Beth Roach, Ernst Lamothe Jr., George Chapman Advertising: Amy Gagliano, Pam Roe, Tom Bachman Layout & Design: Angel Campos-Toro • Office Manager: Allison Lockwood A monthly newspaper published by Local News, Inc. 33,500 copies distributed throughout more than 1,000 high-traffic locations, including all Wegmans stores. In Good Health is published 12 times a year by Local News, Inc. © 2023 Local News, Inc. All rights reserved. P.O. Box 276, Oswego, NY 13126 Phone: 315-342-1182 • Fax: 315-342-7776 • Email: editor@cnyhealth.com ONONDAGA, OSWEGO, CAYUGA & MADISON COUNTIES No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
Q & A with Tricia Peter-Clark
 By Mary Beth Roach
By Mary Beth Roach
Q: ConnextCare seems to have grown exponentially throughout Oswego County. When and how did it grow so extensively?
A: The growth really happened in 2013 when Northern Oswego County Health Services [now ConnextCare], Oswego Health and Oswego County Opportunities colaborated on what was known as preserving primary care safety net initiative. The hospital, at the time, had three primary care practices in Mexico, Parish and Phoenix that they were operating. Oswego County Opportunities had two practices — one in Fulton, one in Oswego — and they were in some financial distress. So, the group had come together to talk about how those five health centers could come under the umbrella of ConnextCare so that we could maintain health service sites for access in our county.
They had been working on this initiative and had received some outside grant dollars to go through the due diligence efforts for consolidating those practices. At the same time, ConnextCare had applied for some new funding to the federal government and was awarded, which actually accelerated the advancement. They had to be operational within 120 days of award for those funds, which meant Jan. 1, 2013, the practice sites needed to be under one umbrella.
In 2013, they went from one health center to six health centers and in January 2013 they brought on the Mexico Middle School school-based health center. That was an additional site that opened, so we have schoolbased health centers in the APW, Sandy Creek, Pulaski and Mexico districts, with a dental site in Fairgrieve Elementary School.
Q: How many offices do you have in this county and what services do the providers offer?

A: We have 15 practice sites and we offer medical services — primary care, dental and mental health services. Dental right now is located in our Fulton site, as well as at our Pulaski site and in several of our school-based health centers.
Q: Is ConnextCare experiencing staffing shortages for nurses and or doctors?
A: We are experiencing a shortage related to licensed practical nurses or LPNS, that has been the biggest challenge for us. We have a lot of nursing homes in Oswego County and that’s where a lot of our licensed practical nurses work, and in the hospital system as well. My medical staff are amazing ambassadors for our organization. They take a lot of students from Upstate, St. Joseph’s, Binghamton — family practice nurse practitioners or pediatric nurse practitioners, as well as some residents — and bring them into our facility, provide the clinical oversight and mentorship for them for their clinical hours while they’re pursuing their degrees. Once we do that, several of them apply and work with ConnextCare.
Q: Do you think this helps attract providers to Oswego County?

A: We are a federally qualified health center working in a rural, underserved community with a significant health professional shortage area designation. A lot of them [staff] live in our communities. They want to give back to the community they grew up in. At the same time, we can offer some opportunities to apply for loan forgiveness through the National Health Service Board program, which provides some assistance to those who are coming out of their graduate programs with significant debt. That’s another attractive option.
Q: When and why did ConnextCare start to integrate the mental health services into your location?

A: About six years ago, ConnextCare was able to apply for some dollars through the Health Resources and Services Administration for behavioral health integration and primary care and were successful, which allowed for us to employ our licensed clinical social workers at our main health centers — a child psychiatrist one day a week in office, and we contract with an independent provider for adult psychiatry services. We also have one psychiatric
physician assistant and three other psychiatric nurse practitioners and another one joining us in June. We’ve really grown that program. The need is just so prevalent, and the patients really need to continue to have access to care. Telehealth has been a great opportunity for us to expand. A lot of our mental health patients are really taking advantage of that. It’s a great avenue for us to ensure we continue to meet the needs, but it also offers our primary care team an outlet when they have a case that’s beyond their primary care training that they have a colleague right in house that they can do a warm hand-off to, to better help better assist the patient with the care they need.

Q: Do you have plans to expand beyond Oswego County?
A: At this time, we do not have plans to expand outside of Oswego County, but we do have plans to expand within Oswego County. In addition to our primary care, mental health and dental services. We also do some substance abuse disorder services to try and address some of the concerns we have in our community as well. As far as expansion goes, we are in the process of working with the Oswego City School District on expanding a school-based health center site in one of their schools. We are getting ready to submit a federal grant next week to the Health Resources and Services Administration to financially support the expansion of that site.
ConnextCare just finished the development of what we’re calling our external respiratory care center. It’s a new building located behind our Pulaski office, which has two negative pressure rooms, so that patients can drive under the canopy and they can either have their COVID-19 testing in their vehicle or they can come into an exam room. We’re just waiting on the final approval from the NYS Department of Health to be able to open that. We have construction plans in place to renovate some space in the Pulaski office to open up an acute care wing to bring back more of our acute care walk-in services that we used to have in Pulaski and that construction is slated to start on June 5. By the end of summer, we hope to have those services up and running for the community as well. We are working right now on design plans to move our Oswego office. We are hopeful that by the middle of next year we’ll be in our new practice site in Oswego and that will include the expansion of dental.
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 13 HUD Subsidized 1 Bedroom, Unfurnished Apartments Weekly Transportation to Walmart In-House Laundry Facility SNACK Lunch Program For More Information Visit stoneleigh@christopher-community.org Applicants must meet the income guideline, be at least 62 years old, or have a long-term mobility impairment. or call (315) 697-2847
President and CEO of ConnextCare discusses further expanding the organization. It provides primary, dental and mental care and plans to increase its presence in Oswego schools
Member of Operation Northern Comfort Help Victims of Hurricane Ian
By Mary Beth Roach
When most Central New Yorkers travel to Florida, it’s for a vacation. But not so for some volunteers connected with Operation Northern Comfort.
A group of 10 from this organization traveled to Fort Myers in mid-March to work on three homes and the group’s host church that had been damaged by Hurricane Ian, which ripped through that area last fall.

An advance team from ONC had gone to the area in January to meet with representatives from Faith
Church, a United Methodist congregation, the host church that was serving as project coordinators.
“Their whole lives are out on the curb,” Laurel Flanagan said of the families whose homes and lives have been destroyed. Flanagan is the CEO of Operation Northern Comfort.
While the work may be hard and sweaty, she said, she believes that the volunteers may get more out of the experience than those they’re helping.
A volunteer coming from as far away as New York gives those they
assist a “glimmer of hope,” she said. “Giving them that hope is so rewarding as a human being. You’ve accomplished something — that feeling of accomplishment; that feeling of helping someone. It’s the most hopeful thing you can do for other human beings.”
This is the 64th trip that ONC has made since it began in 2005 when organization founder Norm Andrzejewski took a group of friends to New Orleans, a town he fell in love with while attending Tulane University, to help the residents there after Hurricane Katrina.
Since then, the organization has grown substantially and volunteers have traveled to such locations as Louisiana, Mississippi, Florida and North Carolina to help people reconstruct after natural disasters have ripped through their communities.
Starting out as Operation Southern Comfort, the group rebranded itself in 2012 when they began focusing a lot of their energies and working on projects in the Central New York area.

The mission trips are personal investments of time, money, and a lot of sweat for these volunteers. They pay for their own transportation to and from the locales they work in, and some need to take personal or vacation time from their jobs to go. ONC funds some equipment; materials; the rental of a van, when needed; food; and a stipend to the host organization for providing accommodations.
These trips are just one of three facets that Flanagan sees as the work of the ONC. Their other initiatives are closer to home.
Volunteers construct and install equipment to help those in Central New York with physical challenges. The organization also provides equipment and funding for other local grassroots non profits. Starting during the pandemic, teams from ONC built desks for students in need. To date, more than 1,300 have been built. Shelving units have been constructed for food banks and a local animal shelter.
Operation Northern Comfort Sponsors Syracuse Crawfish Festival

The majority of funding for projects that Operation Northern Comfort undertakes comes from the Syracuse Crawfish Festival. This year the festival will take place from 11 a.m. to 7 p.m., May 6, at Clinton Square. There will be entertainment on two stages, food trucks, beverages, and of course, Cajun food booths, with crawfish, shrimp, salt potatoes, beignets, pulled pork, and mac and cheese. That flavor of the event harkens back to ONC’s roots in New Orleans, where it all began.

CNY Senior Housing & Care Expo
Join
May 31, 2023
from 9am 1pm
CNY Regional Market E Shed 2100 Park Street, Syracuse, NY
Coordinated by:
Presented by:
Enjoy the music and food while you plan your next adventure in living, discover how to stay in your home as long as possible, or find programs and services you didn’t even know you wanted.

Easy free parking, door prizes, and giveaways...

Page 14 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
From left, Steve and Mary Schug, Tom Ogden, Mike Flanagan and Laurel Flanagan, foreground, take a break.
Last year’s Crawfish Festival. The event is the main funding generator for the Operation Northern Comfort, a local nonprofit.
Us!
M E E T I N G Y O U W H E R E Y O U A R E



























– CNY’s Healthcare Newspaper • Page 15 M E E T T H E U P STAT E U RO LO GY T E A M FO R A N A P P O I N T M E N T, C A L L 315.464.1500 Female and reconstruc tive uro ogy, urinar y ncontinence n women pelvic oor treatment and neurourology MATTHEW D MASON, MD, FAAP DMITRIY NIKOLAVSKY, MD RYAN SIDEBOTTOM, DO General urology, male health, urologic oncology enlarged prostate, kidney stones At Upstate Urology of Auburn TIMOTHY K. BYLER, MD MRI fusion male hea th prostate cancer and kidney stones ZAHI N MAKHULI, MD General urology, andrology JC TRUSSELL, MD Male infer tility erec tile dysfunc tion andro ogy, general urology, prosthetics, and Peyronies OLEG SHAPIRO, MD Urologic oncology and endourology robotic and aparoscopic surger y of prostate, kidney, b adder and adrena ; kidney stones SCOTT WIENER, MD K dney Stones, M nimally Invasive Kidney Surger y, Enlarged Prostate HANAN GOLDBERG, MD, MSc Urologic oncology; robotic and laparoscopic surger y of prostate, k dney, bladder, and adrenal ANTHONY J TRACEY, MD, MPH , FAAP Pediatric urology, treatment of hernias and hydroceles, robotic surger y urinar y trac t infec tions peni e abnormalities NATASHA GINZBURG, MD IMAD NSOULI, MD GENNADY BRATSLAVSKY, MD Chairman Uro ogic oncology; robotic and laparoscop c surger y of prostate, k dney, bladder and adrenal STEPHEN BLAKELY, MD ELIZABETH FERRY, MD General uro ogy ROBERT FLEISCHER, MD General urology SEETHARAM BHAT, MD, MBBS Urologic oncology; robotic and laparoscopic surger y of prostate, kidney bladder, and adrenal Reconstruc tive urology; incontinence, prosthetics, ur nar y stula, neurogenic bladder urinar y diversion Robotic surger y General uro ogy female and reconstruc t ve uro ogy Pediatric uro ogy treatment of hernias and hydroceles robotic surger y urinar y trac t nfec tions, penile abnormalities Incontinence urethral stric ture disease vesicovaginal stula, reconstruc tive surger y, transgender care JOSEPH JACOB, MD, MCR Urologic oncology; robotic and laparoscopic surger y of prostate, k dney, bladder and adrenal MAHMOUD CHEHAB, MD Genera urology, male health, urologic onco ogy, enlarged prostate, kidney stones , and robotic surger y GARRETT SMITH, MD General urology, male health, urologic oncology, enlarged prostate, kidney stones At Upstate Urology of Auburn. NICK LIU, MD Uro ogic oncology; robotic and laparoscop c surger y of prostate, kidney, bladder and adrenal EDWARD IOFFE, MD General Urology Endourology and Laporoscopic Surger y JEFF VILLANUEVA, MD Pediatr c urology treatment of hernias and hydroceles robotic surger y, ur nar y trac t infec tions, peni e abnorma ities
Parenting
By Melissa Stefanec MelissaStefanec@yahoo.com
Adolescent Girls Are So…
What would you say if you were asked to finish that headline?
Would you say difficult? Or maybe 13 going on 20? Dramatic? Not fun? So much harder than boys? Trouble? A nightmare? Filled with attitude? Defiant? Grouchy? Mean? Instead of finishing the thought, would you roll your eyes?
My guess is a lot of folks would fill in the blank with something less than kind.
Almost everywhere I go, I hear folks freely criticizing adolescent women. Mothers, fathers, relatives and other adults all have commentary to offer, and it isn’t usually kind or constructive. I can’t imagine this commentary, which is often said within earshot, does anything good for these young ladies’ developing psyches.

As the mother of an almost 12-year-old daughter, I am going to make an unpopular assertion: The world isn’t terribly kind to adolescent girls, and we adults are the ones who need an attitude adjustment.
Sure, adolescents have complicated emotions and intense reactions stemming from those emotions. But, the nearly constant criticism and negative tropes are hurting our girls, and they deserve better.
If us adults had to put up with so many negative stereotypes, tropes, reactions and treatment, we would likely be hurt, angry and disengaged. And, we would feel all of those feelings with our fully formed brains,
a decent amount of self-esteem and some tried-and-true coping mechanisms.
Maybe, adults should pause and ask ourselves: Why do we expect our girls to overcome such negativity when they are dealing with so many complex things? Why don’t we start praising young women for all the ways they are amazing? Maybe, if we did, we would have the courage to help us girls grow into adulthood instead of making them endure our negative projections.
So, because young women deserve plentiful support from their communities, here are some reasons I think adolescent girls are awesome.
They are funny
By the time they hit double digits, most kids are catching on to adult wit and humor. Girls have a special kind of wit. Sure, most of them find fart jokes funny, but they also make keen observations about the world around them, often with hilarious results. The more I engage with young women, the more wonderfully amusing I find them to be.
They keep us on our toes
Some of their remarks may be a little unfiltered or surprising. But I’m thankful the compliant little girls I once knew are growing into discerning, free-thinking, righteous little rebels. I would rather have a young woman keep me on my toes than
blindly follow every order I give her. The world needs strong and assertive women.
They are finding themselves
When we’re young, so much of what we do is directed by our parents or guardians. When girls start thinking about who they are, what they want, what they like doing and what they don’t want, it’s actually beautiful. Finding oneself is a lifelong experience. Watching young women set off on that journey is a privilege I embrace.
They nurture their friendships
Sure, it can be frustrating when your daughter wants to spend all of her time with her friends, but she’s invested in her tribe. Isn’t it cool when people find common ground and take pleasure in each other’s company? I admire the way young women nurture their friendships and watch out for one another, even if they get in occasional disagreements.
They are athletes
As someone who was once a young, female athlete, I’m going to let you in on a little something: adolescent girls are tough. The grit young female athletes possess is nothing short of impressive. They also understand the importance of teamwork—something us adults could take a cue on. Most adolescent girls I know are stronger, faster and far more coordinated than most adults I know.
They are scholars
Remember middle school, high school and junior high? Remember going to school all day and then studying for much of the evening? Remember how much you were expected to memorize and learn? You did all of this while you were navigating the social and societal hardships of late childhood. It hasn’t
gotten any easier for today’s girls. The fact they can excel academically while dealing with a lot of nonsense is pretty impressive.
They are talented
Young girls do things like play in bands and orchestras. They are in literary clubs. They build robots and small businesses. They are engineers and coders. They make beautiful artwork. They write songs and poetry. They sing, and dance and create, often beyond the abilities of many adults. When they invest in their talents and passions, that’s amazing.
They are willing to try new things
We fuddy-duddy adults are often stuck in our ways by the time we hit 30. Young girls are open to trying new things. Whether it’s new food, new music, new sports, new books, traveling, new friends, new clubs or new experiences, young women are ready to explore this world and be amazed by it (even if they roll their eyes to hide that wonder). The fact they consistently step outside their comfort zones is something us old people should admire.
So the next time you find yourself wanting to say something negative about adolescent women, pause and think about why you want to say that. Ask yourself if you’re helping or hurting young women. Then, challenge yourself to say something nice. Be a narrative influencer. That’s the sort of influencer our daughters actually need.
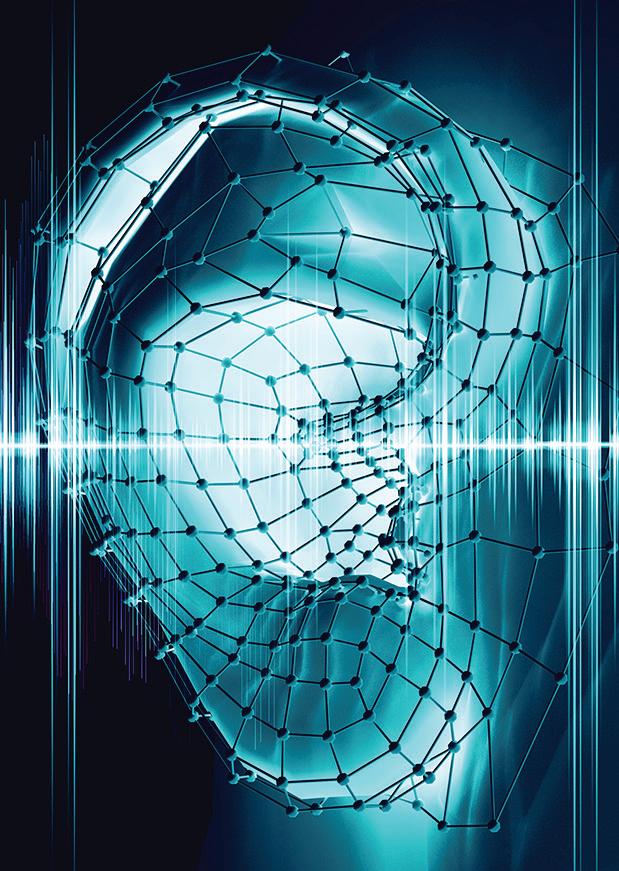
Services / Products Available:
n Baseline and monitoring testing for chemotherapy and other hearing – harmful medications
n Hearing measurements for personal (medical, communication) or occupational (OSHA, DOT, law enforcement) purposes.

n Hearing protection counseling and devices for loud recreational (music listening, hunting, motor sports, landscaping) and occupational (professional musicians, fire and police personnel) activities.
n Hearing aid selection, fittings and repairs

n Tinnitus evaluations and treatment.
n If you have any questions or concerns regarding your hearing or how to protect it. 315-410-1295
Page 16 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
dB Audiology Associates, PC 5992 East Molloy Road Syracuse, NY 13211 www.dbaudiologycny.com Hearing Measurement services and advice provided by a NY State Licensed audiologist who has been providing professional hearing care to Central NY for over 40 years.
Almost everywhere I go, I hear folks freely criticizing adolescent women
By Appointment Give Doug Brown a Call!
SmartBites
By Anne Palumbo
The skinny on healthy eating
Why Swiss Cheese Makes Healthiest-Cheese Lists
My cheese-loving friend has sworn off cheese for a while, saying it’s “too caloric, too fatty, too tempting.”
She’s not the first to go on a cheese moratorium, and I get it: cheese can be all those things. But not always. There are healthy cheeses to be had and recommended ways to eat them.
Swiss cheese, in fact, is one of the healthier cheeses, a designation bolstered by its appearance on nearly every healthiest-cheese list out there.
Why does Swiss cheese make the coveted cut?

Let’s begin with why Swiss cheese is the cheese for you if you’re watching your salt intake. With only 52 mg of sodium per slice, Swiss cheese has significantly less sodium than most other types of cheese. Considering that the American Heart Association recommends no more than 2,300 mg of sodium a day, you’ll barely make a dent with a few slices of Swiss. Make the same sandwich with American cheese, however, and you’re looking at 900 mg.

Swiss cheese also has more vitamin B12 than any of its peers—a whopping 36% of your daily requirement. An essential vitamin, B12 helps the body produce energy, maintain nerve health and lower blood pressure. Unfortunately, many people— from older adults to vegetarians—are deficient in this important vitamin.

Incorporating a slice or two of Swiss cheese into your weekly diet can help keep your B12 levels up.
Much like milk, Swiss cheese serves up healthy doses of protein, calcium and phosphorous, three nutrients that contribute to the development and maintenance of strong bones. But unlike many milk products, Swiss cheese is super low in lactose, making it a great cheese option for people with lactose intolerance.
On the downside, Swiss cheese has 5 grams of saturated fat per slice, which is about a quarter of the recommended daily amount. Although some research indicates there may be no link between saturated fat and heart disease, experts still advise limiting your intake.
On the plus side, Swiss cheese’s full flavor, along with its slow-to-digest proteins and fats, may help thwart the urge to overindulge.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.



SWISS, SPINACH & MUSHROOM CRUSTLESS QUICHE

Serves 6-8

1½ tablespoons olive oil

3 cups sliced mushrooms
10-oz box frozen chopped spin-
ach
½ cup chopped onion
1 clove garlic, minced
5 large eggs
½ cup milk
1-2 teaspoons Dijon mustard
1 teaspoon thyme
½ teaspoon salt
¼ teaspoon coarse black pepper
1½ cups shredded Swiss cheese

Helpful Tips
The majority of Swiss cheese made in America, often called baby Swiss, is only aged for about a month, while traditional Swiss cheese is aged from two months to many years. Because of the shorter aging, baby Swiss has smaller holes, tastes slightly sweet and nutty, and is great for melting. Traditional Swiss, on the other hand, is more expensive, has larger holes, and tastes sharp and tangy.
Preheat oven to 350F. Thaw and squeeze moisture from spinach. Lightly coat 9-inch pie pan with cooking oil; set aside. Heat oil in large nonstick skillet over medium heat. Add mushrooms and cook for 4 minutes, stirring frequently. Add onion and garlic and cook for 4 minutes more, stirring often, until tender. Turn down heat if mixture starts to burn. Remove from heat, transfer to medium bowl and let cool. Gently mix in spinach.
In large bowl, whisk eggs, milk, mustard, thyme, salt, and pepper. Fold in the mushroom mixture and cheese. Transfer to prepared pie pan and bake until set, about 50 minutes. Let stand for 10 minutes. Slice and enjoy!
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 17
Your Medicare Specialist and Independent Agent Ser ving New York State’s Medicare eligible population since 2008! Why Call a 1-800 number when you can get personalized ser vice with face-to-face consultation & Enrollment. Theresa Cangemi, CSA, CLTC Medicare Made Simple, LLC 3 years October 2021 Your Medicare Specialist and Independent Agent Ser ving New York State’s Medicare eligible population since 2008! Why Call a 1-800 number when you can get personalized ser vice with face-to-face consultation & Enrollment. Medicare Advantage • Medicare Supplement • Prescription Drug Plans Long Term Care (CLTC) • Life Insurance • Final Expense (Burial) • Dental Plans Travel Insurance Coverage www MyMedicareMadeSimple com “Commissions Paid by the Carriers, Not Fee Based” DO YOU HAVE PROPER MEDICARE COVERAGE? FIND OUT Theresa Cangemi, CSA, CLTC 315-727-4933 • tcangemi@MyMedicareMadeSimple.com www.MyMedicareMadeSimple.com “Celebrating 14 years in October 2022!”
Nursing Shortage: Attracting Nurses to the Bedside
 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant
The pandemic exacerbated the longstanding shortage of bedside nurses. Tougher conditions, supply scarcity, employee illnesses and many sicker patients prompted many hospital nurses to quit the profession or move into a non hospital role in nursing. And about 100,000 left nursing in 2021 alone.
“It’s still a struggle,” said Scott Jessie, master’s trained nurse and chief nursing officer at Upstate University Hospital. “We have some acute care beds closed. We are still relying on a large number of travel staff.”
Hospital nursing has seen a good amount of turnover because of the rise of travel nursing, which Jessie said “exploded” during the pandemic. Replacing retiring and quitting nurses isn’t easy. Jessie said that nationwide, schools decline about 90,000 would-be nursing students annually because of lack of faculty.
Some quit for the variety of travel nursing assignments, so Upstate highlights that it offers the most specialties in nursing in the CNY region. Upstate also has “significantly improved” its pay over the past 18 months, Jessie added, admitting that it “wasn’t as competitive” before.
“We have excellent benefits and retirement packages,” Jessie said. “We pay up front for tuition for education: bachelor’s, master’s and doctorate degrees.”
On the hospital floor, efforts to improve the employee experience for nurses includes using robots to aid in mundane tasks and smaller electronic medical record devices so nurses no longer have to roll around
a computer on wheels room to room.
“We’re a magnet organization,” Jessie said. “Magnet hospitals have a nurse-friendly culture top down and bottom up. Our staff at the bedside comes up with an awful lot of ideas we in senior leadership wouldn’t.”
Rounding with bedside staff also helps keep leadership in touch with nurses. Upstate’s nurse residency program helps new nurses get on board with mentoring and camaraderie opportunities.
Extending recruitment to Syracuse City Schools from the middle school level upwards raises awareness of nursing as a career option. A greater presence on social media has also helped, with clips of employees sharing why they work at Upstate, or the benefits offered.
Reaching mid-career job changers is another way Upstate seeks to combat the nursing shortage. These potential nursing candidates may already have a bachelor’s degree and qualify for an accelerated program. But they also need more flexibility in the program with evening, weekend and hybrid classes. Jessie said that many who have been in service-oriented careers such as firefighters or the military have shown more interest in nursing in recent years.
Workplace violence has begun to deter people considering nursing as their career—and it’s not coworker to coworker but directed toward nurses by patients and family members.
To reduce this issue, Upstate maintains a police department onsite, screens for weapons at all entry points and operates an employee assistance program to counsel staff
on personal and mental health issues.
At VA Medical Center in Syracuse, travelers have also helped fill in the gaps, although Megan Queary, nurse recruiter for VA Medical Center in Syracuse, said that the need is lessening now that the pandemic has subsided. The VA has partially opened one of its med-surg units that was closed during the pandemic.
To reach more potential employees, the VA has been participating in job fairs and tours of their facility.
“We’re reaching out to the community for graduated students,” she said. “We’re and really ‘selling’ what the VA has to offer, like the benefit package and the mission the VA has to take care of America’s heroes. It’s a big selling point. Many people share that value and want to give back.”
The VA has also increased its pay rates and offers tuition reimbursement for nurses.
“Our RNs get five weeks of vacation and two weeks of sick leave that they start accruing once they get here,” Queary said. “The government matches 5% of our retirement. You’re vested after five years. You can take your healthcare and retirement with you.”
Suzanne Talarico, registered nurse and manager of talent acquisition at St. Joseph’s Health, described the capacity at the hospital as “a continuous ebb and flow over the past three years. The leadership is monitoring what’s going on in the community. There has been shifting of units, some that have closed temporarily and reopened. We’re experimenting with a discharge lounge to navigate patients differently.”
This can free up beds for new patients. In addition, the hospital is looking at different staffing models to use licensed staff at their highest scope of practice. Talarico said that virtual nursing may roll out by the end of 2023 to help address healthcare needs that are manageable remotely.
“We’re trying to be creative and flexible and try a variety of tactics,” Talarico said.
“Headhunters” are part of how St. Joseph’s is seeking nursing candidates. The organization seeks to learn about applicants’ goals so they can provide what they want, such as benefits, flexible scheduling, tuition reimbursement and workplace culture. St. Joseph’s is started to look at loan repayment as a benefit.
Drawing from the college also helps attract more nurses for St. Joseph’s, compared with hospitals that do not operate a college. Talarico said that opening up hiring to refugees who want to learn nursing and medical professionals from other countries may prove another means of attracting more talent to St. Joseph’s.
“We’re becoming much more flexible and open to what a potential candidate or hire would want or need and bringing that to our leadership team to vet,” Talarico said.

The organization is looking at adjusting its pay scale to better reflect that of other organizations. Travel nursing has been part of its strategy to address the nursing shortage. However, as the pay rates for travel nurses have come down, fewer people seem interested in this type of employment.
Employee wellness and safety is another benefit that St. Joseph uses to differentiate itself from other hospitals, as well as keeping lines of communication open between leadership and frontline staff.
“The people we call ‘boomerangs’ — we pay attention to why they come back,” Talarico said. “It speaks to our culture and missions. We had so many people who left for many reasons, like family-life balance or for travel nursing. Reaching out to them can help. They missed the culture and the way people worked together and the type of care that we provide. They’re always very happy to come back.”
Page 18 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023 Nursing National Nurses Month Celebration May 1-31
Scott Jessie is the chief nursing officer at Upstate University Hospital.
Like us on Facebook!














































May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 19 Your health is as important as ever. ConnextCare is here to help! Say Hello to Healthy! ConnextCare offers highly qualified and accessible providers at several locations throughout Oswego County. Keep you and your family healthy, safe, and happy with convenient, compassionate and comprehensive care right in your neighborhood. • Over 70 dedicated healthcare providers across our network • Acute care treatment with same-day appointments • Services include family medicine, pediatrics, dental, psychiatry, chronic condition treatment, behavioral health, and more. Say hello to the ConnextCare Pulaski team. Call today. Pulaski 61 Delano Street, Pulaski NY 13142 (315) 298-6564 Other Locations Fulton, Mexico, Oswego Parish, Phoenix, Central Square www.connextcare.org
Meet our Pulaski Area Providers
Mary Barbara, PA Physician Assistant Pulaski
Nicole Brubaker, FNP Family Nurse Practitioner Sandy Creek School
Annette Digby, FNP Family Nurse Practitioner Pulaski
Grace Nasri, MD Family Practice Physician Pulaski
Lisa Beagle, PNP Pediatric Nurse Practitioner Lura Sharp School
Mikayla Fox, PA Physician Assistant Pulaski
Carolyn Dudden, NP Nurse practitioner Fulton
Lauren Hehir, AGNP Adult-Gerontology Nurse Practitioner Pulaski
Richard Salvagno, DDS Dentist Pulaski
Jill Brushaber, FNP Family Nurse Practitioner Pulaski
Patrick Carguello, DO Family Practice Physician Pulaski
Celeste Carnes, FNP Family Nurse Practitioner Pulaski, Mexico
Dean Gardner, FNP Family Nurse Practitioner Pulaski
Brittany Gehrke, RDH Dental Hygienist Pulaski, Sandy Creek School
Anna Gofman, DDS Dental Pulaski, Fulton
Jody Hipple, FNP Family Nurse Practitioner Pulaski High School
Megan Hollister, FNP Family Nurse Practitioner Pulaski
Annalise Isgar, RDH Dental Pulaski
Blaze Kravec, FNP Family Nurse Practitioner Pulaski
Kwi Lee, DDS Dentist Pulaski
Melissa Noel, DDS Dentist Pulaski, Fulton
Jessica Overton, RDH Dental Hygienist Pulaski, Fairgrieve School
Megan Pecha, MD Pediatrician Pulaski
Mary Shaben, FNP Family Nurse Practitioner Pulaski
Marissa Taber, RDH Dental Hygienist Pulaski
Glenn Thibault, MD Family Practice Physician Pulaski
Dorese Vecchio, RDH Dental Hygienist Pulaski, APW Schools
Jenna Walker, RDH Dental Hygienist Pulaski
Edward G Wolfe Jr., RPA-C Physician Assistant Pulaski
Mary Ellen Xavier Flanagan, FNP Family Nurse Practitioner Pulaski
Ryan Kasarda: Like Mother, Like Son
By Deborah Jeanne Sergeant
Like many nurses, Ryan Kasarda of Cicero became interested in the profession as a young person because of knowing a nurse firsthand.
In this case, it was his mother, Karen Kasarda. Both mother and son work for St. Joseph’s Health.

“I was always interested in what
she did, although I never understood everything,” the son said. “Now I fully understand it and I’m glad I went down my path. It’s my way to help people and do it for a living.”
Karen Kasarda has worked as a nurse at St. Joseph’s since she began her career in 1991.
A 2019 graduate of Nazareth
College’s nursing program, Ryan Kasarda had worked at Wegmans for five years as a stocker. His Wegmans wages and scholarship helped him pursue his nursing education.

He likes the nursing schedule of 12 to 16 hours per day, three-day weeks, he said.
But more than that, he likes that nursing enables him to help people in a concrete, one-on-one way at what may be the most difficult and frightening time of their life.
Like many people, the shift from school to work surprised him.
“There’s the difference on everything they emphasized,” he noted. “Work focuses on the practical. They teach you a concept in school and then you focus on different things in real life, but schooling gives you the understanding of why you do it at work. You have a foundation to go off of and can ask more critical questions of doctors and make suggestions on patient care.”
He began his nursing career in the cardiovascular ICU at St. Joseph’s Health after completing his residency and six months of rotations at Strong Memorial Hospital in Rochester.
Kasarda enjoys the fast-paced environment of the ICU and completed the education for advanced certification in critical care in February 2022.
“It gives a better understanding in treating your specific patient population and different things to look for advanced treatment,” Kasarda said. “It gives better insight on things to suggest that can fix problems before they happen. This leads to much better patient outcomes.”
Kasarda values his experience in the field, as he believes it further enhances what he has learned in school.
“You can think of patients you had and understand why you learned what you learned,” he added. “It’s more in-depth knowledge of your specialty.”
He also believes that his handson experience will help him advance his career as he plans to go back to school to become a nurse anesthetist — at which school he is unsure. Currently, he is waiting for a school to accept him, as the acceptance rates for nurse anesthetist programs are about 10% to 15% because the programs are so competitive.
“There are a lot of people who want to do this and few schools offering nurse anesthetist programs,” Kasarda said. “I love working with anesthesia on my floor.”
Although his mom warned him about how challenging nursing school would be — “it’s no joke when you go into nursing school, with eight hours of studying per day for four years,” — he feels proud of Ryan’s accomplishments.
“He listened, enjoyed it and learned a lot,” Karen Kasarda said. “He’s done very well — better than his mother. He excelled beyond my expectation. He picked the right field. I’m just so proud of him. He has a good grasp of clinical care and is a hard worker. I always knew he’d do well.”
In his downtime, Kasarda enjoys biking, kayaking and fishing, as a self-described “very outdoorsy person.”
Nursing National Nurses Month Celebration May 1-31
NEW
We’re here to help ensure your golden years are your best years! Committed to exceptional, family-focused care – and provided by over 60 physicians, 40 nurse practitioners and physician assistants, and 28 locations across our region – FCMG is uniquely situated to care for seniors. Our comprehensive range of services includes: •General family care & internal medicine •Endocrinology, including diabetes testing, care and education • Physical medicine and rehabilitation •Among many others FCMG is also a proud partner in Salt City Senior Care Advantage – which provides a new approach to care delivery by focusing on preventative care and care coordination resources when you need them. Will you be turning 65? Consider choosing a Medicare Advantage plan and be part of the Salt City Senior Care Advantage. Talk to your provider or call a broker to compare Medicare Advantage options. Let our family care for yours! 315-472-1488 • fcmg.org
NURSE
Nursing National Nurses Month Celebration May 1-31
post-anesthesia unit.
The Cicero resident had always felt fascinated by nursing, even though there were no medical people in her family.
EXPERIENCED NURSE
Karen Kasarda: Over 30 Years Nursing at St. Joseph’s
By Deborah Jeanne Sergeant
In the year that Karen Kasarda started working as a nurse at St. Joseph’s Health, “Home Improvement” was on TV, Motorola introduced the first GSM cell phone and
“Home Alone” and “Silence of the Lambs” played in theaters.
Since 1991, she has nursed at St. Joseph’s, first in the intensive care unit for 16 years and now the
She babysat a child whose mother worked as a nurse at St. Joseph’s operating room, who encouraged her as a teen to consider nursing for her career. Kasarda earned her bachelor’s degree in nursing at Niagara University in 1991.


A lot has changed in nursing in the past 32 years. As one example, Kasarda recalls using paper charting when she began nursing.
“Things are a lot more documented now and acuity is a lot higher,” Kasarda said. “They’re able to take care of patients outside of the hospital a little longer, so when they come in, they really need to be here. We can manage more out of the hospital to continue to keep people going outside the hospital.”
She misses the in-services at lunches when unit directors would share educational information and up-and-coming medical advances.
“Now it’s on your own time,” she said about continuing education. “You don’t have time anymore to get away from the bedside and have a meeting. You’re lucky to get lunch; we used to have lunch as a group. You got more friendly with the staff you’ve worked with. It was like a family. We had Christmas parties at our house. So many nurses are coming and going after just a year. You don’t get that unity you used to
WE CARE
We Care is our pledge. It’s a mantra that every one of our teammates carries throughout their day. Simply said, it’s what they do, and defines who they are. Our team cares about the little things. About making connections. About collaboration. About our community.

As Oswego Health continues to build upon our 142-year tradition as an independent healthcare system, we want to take a moment to say thank you.
Thank you to our healthcare team! We Care about what matters most…YOU!



have.”
Travel nursing used to be seldom seen in the hospital setting, with only an occasional traveler for the summer. Kasarda said that since the pandemic, travelers are used much more frequently in hospitals—and they’re not just doing it for the opportunity to see the country.
“Some are from the same town,” she said. “They’re not loyal to an institution. They have to start reaching out with something that will inspire people to stay at an institution.”
Kasarda’s example of faithfulness both to her career path and to an institution helped inspire her son, Ryan, to pursue nursing as well. He began working at St. Joseph’s as a nurse in 2019.
Although some nurses seek further education to expand into leadership roles or academia, nurses in other settings such as doctor’s offices or schools leave nursing altogether. Kasarda said that she enjoys caring for patients at the bedside at St. Joseph’s.


“Many aren’t at the bedside after this many years,” she said. “I can feel I can make something good in someone else’s day. I feel accomplished and I have good skills I’ve worked toward and perfected. So, I still do it. A lot of nurses want to expand their roles, but I’ve always been happy with a bachelor’s degree and bedside nursing. We need more of them.”
In her spare time, she enjoys cooking, baking and gardening.
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 21
How to Become a Nurse
By Deborah Jeanne Sergeant
People who want to work as a nurse have many pathways to receive their credentials. Unlike many careers, nursing does not have to cost a lot to enter.
Many people begin nursing in entry-level work, such as a certified nurse assistant (CNA) through a free tuition program with an employer such as a home health company or nursing home.
CNA programs typically run four to 12 weeks. Many organizations offer tuition in part or in full to become a licensed practical nurse (LPN), a credential that requires a yearlong program and next, a registered nurse (RN), an associate degree program that requires passing a state exam before receiving licensure.
Since 2017, RNs are required to complete a bachelor’s degree (BSN) within 10 years, which is a four-year program (including the two years to complete the RN program). Again, most larger healthcare organizations assist with tuition so their employees can comply with this requirement.
The next level is the advanced practice registered nurse, or master of science in nursing (MSN).
This could include a nurse practitioner (NP), clinical nurse
leader (CNL), clinical nurse specialist (CNS), certified registered nurse anesthetist (CRNA) or certified nurse midwife (CNM).
Beyond these levels are the non clinical specialties such as doctor of nursing practice (DNP), which enables people to serve as a nurse administrator, nursing informaticist, nurse educator or nurse researcher.
With each level comes a higher level of responsibility, scope of practice and salary.
Physician David Page, past president of the Onondaga County Medical Society and provider at FamilyCare Medical Group in Camillus, said that his practice provides some tuition support to LPNs who go back to school to become RNs.
“I’m not sure the nursing shortage will ever go away,” he said. “I’ve been a doctor for 40 years, though COVID exacerbated the shortage.”
He believes that younger nurses want more flexibility in their schedule for juggling childcare and for better work-life balance. Page added that this desire has drawn more nurses away from the entry level degrees and towards the BSN and NP degrees, along with higher requirements in the field.
Burnout Levels High Among U.S. Health Care Workers
Cafeteria workers. Receptionists. Pharmacists. Janitors. Administrators. Physical therapists.
Much has been made of burnout among doctors and nurses, but a new survey has found high rates of work fatigue in nearly every type of job associated with health care.
Physicians, nurses, clinical staff and non clinical support workers in health care all are experiencing substantial levels of burnout, according to a report published recently in the Journal of General Internal Medicine.


For example, the percentage reporting burnout was very similar between nurses (56%), clinical staff (54%), doctors (47%) and non clinical staff (46%).
“Every member of the health care team is really critical to patient outcomes and patient experiences of
care,” said lead researcher, physician Lisa Rotenstein, an assistant professor of medicine at Harvard Medical School. “It’s just really important for us to remember that as we are trying to optimize both patient outcomes and experiences for our workforce.”
For this study, Rotenstein and her colleagues surveyed workers at 206 large health care organizations between April and December 2020, at the height of the pandemic.
The participants included more than 15,000 physicians and 11,000 nurses.
But researchers also surveyed more than 5,000 clinical staff such as pharmacists, nurse assistants, therapists and social workers, as well as more than 11,000 non clinical staff including housekeeping, administrators, lab technicians and food service
“The RNs have to have a BS now,” he said. “It’s been a long time coming. It was a hot topic for a long time.”
Seeking more education can only help nurses in furthering their careers in the future, especially in management education or leadership roles, opportunities which have expanded in nursing. This has prompted another change in nursing that Page has observed: more men in the field.
At the master’s level, nurses can specialize in areas of interest so they can command higher wages and practice more independently. But the DNP is not as important for handson nursing but for roles in leadership and academia.
“We are looking for ways to provide tuition support for those who aren’t working for us yet,” said Scott Jessie, master’s trained nurse and chief nursing officer at Upstate University Hospital.
“We do as much as we can to accept as many students as we can.”
He described Upstate’s program as a “completion degree program” which accepts students from multiple entry points, including people who have worked in nursing or another
field and returned to school and those who have stayed in school with the goal of a higher-level degree in nursing.
“We hire nursing students who maybe want to be a PA and have to have clinical hours before they can be accepted,” Jessie said. “They work directly with our staff to see what the work is. They gain a tremendous amount of experience. They can get some money during school, and they get exposure to us. We often hire directly from the program.”
Regardless of the school, it’s “safer” for students to seek their education at one school to ensure all their credits transfer. This factor becomes especially important as the requirements for nurses’ education evolve.
Beyond the required “BSN in 10” requirement, Cathy Brownell PhD, RN, and chairwoman and professor of nursing at LeMoyne College, foresees more people seeking higher-level degrees for more opportunities.
“Money is a motivator, but different positions or ways of practicing motivate people,” Brownell said. “We see a lot of people that once they have BSNs are interested in more education to become NPs. The motivation is multi-faceted, but a different scope of practice is a big one. You’re an individual care provider and can be a significant difference in income and you can go into your own practice and have more autonomy.”
She also envisions nursing curriculum to have a greater emphasis on diversity, inclusion and equity, as well as care across the lifetime and how social determinants of health affect health outcomes. Nursing will include more patient education on how to stay healthy rather than only trying to help people become well.
“Nurses are the foundation of our healthcare system,” Brownell said. “When we’re so terribly understaffed and we have just a faintly healthy staff, we have a difficult time delivering the quality of care we need to deliver. I worry about my new grads burning out. There’s nothing worse than feeling like you can’t do a good job because there’s just so much on you. These hospitals and healthcare systems need to look to keep the nurses they have.”
workers.
In addition to high levels of burnout, the researchers also found that many workers intended to leave their jobs within two years-nurses (41%), clinical and non clinical staff (32%) and doctors (24%).
Substantial numbers also reported work overload, including 47% of nurses and clinical staff, 44% of non clinical staff and 37% of doctors.
Even though the survey was conducted during the height of the
pandemic, Rotenstein suspects that things haven’t improved for health care workers in the subsequent years.
“Some of the stresses have persisted as we have moved into a new phase of the pandemic,” Rotenstein said. “There are staffing shortages. There are patients who have delayed care because of the COVID pandemic, and so now we’re seeing an increase in demand for health care. Oftentimes, health care workers are being asked to do more with less.”
Page 22 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023 Nursing National Nurses Month Celebration May 1-31


May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 23 FCMG wishes to acknowledge and thank our exemplary nursing team – across all of our locations, disciplines, and specialties. Your compassion and empathy for our patients; your selfless dedication to, and excellence in, providing care; and your passion for your craft, collaborative spirit, and generosity and grace in the face of adversity – especially over the last couple of years – make FCMG one of the most impactful, reliable, and dynamic healthcare providers in our region. More than that, you make us the family we are. Celebrating our family of ever-competent, caring, and compassionate nurses! Let our family care for yours! 315-472-1488 • fcmg.org
Nursing Shortage Affects Independent Practices Differently
By Deborah Jeanne Sergeant
The shortage of nurses to work in hospitals pre-existed the pandemic. However, the health crisis made the problem worse. The nursing shortage has affected independent practices similarly, but for different reasons.
“It’s been horrible since COVID-19 hit,” said physician David Page, with FamilyCare Medical Group in Camillus. “My office is not known for a lot of turnover, but we’ve lost two to three nurses and trying to replace them was extraordinarily difficult. We use LPNs and a limited number of RNs. It impacted operations and the workload of everyone else.”
His staff includes about 10 LPNs and RNs.
One of the issues is the rise in wages among nurses at larger organizations, including hospitals.
Page, who is past president of the Onondaga County Medical Society, said his office offers a competitive retirement plan and raised salaries

two or three times to attract nurses. However, small organizations can only sustain so many raises and still remain within the budget.
What small offices like Page’s can do is provide better work-life balance than many large organizations can.
“Our office has historically had low turnover,” Page said. “We’re family-oriented. If you have a sick child, we can make arrangements to have internal coverage or if you have to take off early, we accommodate that. Some of our nurses have fairly fixed times they need to get out to take care of their children.
“It’s a friendly environment and we try to make people feel appreciated. I have a great nursing coordinator who takes good care of our nurses. Private practices should be a fun place for people to be. It’s less time demanding and a different type of working environment.”
That doesn’t mean that every independent practice hires nurses with ease.
Lisa Olson-Gugerty, who holds a master’s in public health and is an associate teaching professor at Syracuse University David B. Falk College of Sport and Human Dynamics, said that although many nurses prefer the better work-life balance at private practices compared with hospitals, private practices tend to pay less on average. “So it can be difficult to fill positions due to the lower pay rate. I think the nursing shortage is hitting all places of employment. The shortage is not necessarily due to lack of RNs available, but due to the storm of COVID-19, travel nurse positions, retirements and other opportunities for nurses.”
Some nurses have segued into case management, school nurse positions or, with additional education, academia, rather than office or bedside nursing.
Yvette Conyers, doctor of nursing practice, registered nurse and past president of the Rochester Black Nurses Association, said that many nurses have been pursuing additional education, such as a bachelor’s degree, making it challenging for some organizations to hire nurses at the entry level LPN education.
“It’s about using the nurses to their full education; they don’t want to hire BSNs and have them only on the phone triaging calls,” Conyers said. “That’s not what they’re prepared to do. They’re prepared to manage, look at a complicated picture, note the sociological determinants of health.”
Many large healthcare organizations reimburse or pay upfront for employees’ education, but with a stipulation that they work for them for six months to three years, depending upon the organization and the level of education. Although this brings many more nurses into the workforce, it also keeps them away from choosing small, independent practices and instead working in the larger healthcare systems, such as those operating larger hospitals and the freestanding offices owned by the same healthcare systems. The strategy is often successful in keeping nurses in the same organizations for
and trying to replace them was extraordinarily difficult.”
years after they have fulfilled their obligation.
Conyers said that independent practices struggling to find nurses can improve their staffing by partnering with educational institutions. All students in nursing programs are required to complete a number of supervised clinical hours before sitting for their LPN and RN board examinations.
“This would help address the shortage of providers and open up the eyes of the students who are usually working in hospitals to the vast areas in out patient settings,” Conyers said.
Many students choose hospitals because of the availability of slots for clinical hours, the skillset and the fast-paced environment. But Conyers said that 80% of healthcare occurs outside of the hospital, making that a more needful place to focus on healthcare.
“Working in primary care and in the community is important and these are great areas to work,” she said.
She wants to see more nursing programs promote primary care and public health in nursing education.

Page 24 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023 Nursing National Nurses Month Celebration May 1-31
NURSES
800-858-8109 100% OSHA Compliant • Patient Gowns • Lab Coat Service • Scrubs • Sheets/Pillow Cases • Bath/Hand Towels • Massage Linens • Professional Mat Service • Fluid Resistant Garments Serving Central New York HealthWearRental.com
Enjoy reading In Good Health newspaper? The paper is free to you but very expensive to produce and distribute. Keep the publication going. Consider supporting it. If you are a reader, please become a paid subscriber (see coupon in this issue). If you’re a nonprofit, a medical practice or organization, consider advertising. You will get a great deal of exposure since the paper is everywhere for the entire month. We will even design your ad at no charge. For more information, send an email to editor@CNYhealth.com — Type “Support” on the subject line. WORTH SUPPORTING It’s
Physician David Page practices at FamilyCare Medical Group in Camillus: “We’ve lost two to three nurses
YOUR SUPPORT



May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 25 Join the Study for Alzheimer’s Disease www.HOPEStudyForAD.com/GAP
Golden Years
Why Prompt Hearing Evaluations Matter
By Deborah Jeanne Sergeant
Every baby born in a hospital receives a newborn hearing exam. Unfortunately, the next time that the person’s hearing is considered is typically once a significant degree of hearing is lost.
Parents of young children may find themselves repeating directions to a seeming oblivious child. Or the child may hold musical toys close to hear them or turn up the volume on devices.
“They may need the TV volume turned louder than what others like to listen,” said. Nicole Anzolone, an audiologist with Syracuse Hearing Solutions. “It can affect their ability to learn and use language.”

Anzolone said that school-aged children may seem to not listen in school, affecting their performance. They may keep the TV or other
devices loud or seem confused when given directions that are age-appropriate in complexity.
For adults, it’s typically other adults who signal a hearing problem is present, as the one with hearing loss will ask others to repeat what they say—or miss it altogether.

“People with hearing loss a lot of times don’t know they have hearing loss, but I bet their family and work know,” said Clayton Andrews, a board certified audiologist with more than 35 years’ experience, who operates Upstate Hearing Solutions in Oswego.
Some less obvious signs he included are not hearing the crickets at night or the birds during the day. Dizziness or ringing in the ears (tinnitus) can also indicate a hearing problem.

Losing hearing can cause different and significant problems across the lifespan.
“Hearing is very important for developing speech and communication,” Andrews said. “With a hearing loss, it’s very difficult to have appropriate language skills.”
For school-aged children who have lifelong hearing loss, early intervention can help them stay abreast with their schoolwork. Neglecting hearing issues can cause them to fall behind.
Andrews said that working adults with untreated hearing loss tend to make less income than those who hear well. One factor is that not hearing correctly for long periods of time can make workers appear inept, ambivalent or uncommitted. For people working in environments such as construction or agriculture, not hearing well can compromise their safety because they don’t realize what they’re missing.
Waiting can also make acclimating to hearing aids more challenging as the brain has to relearn how to process sounds again. Untreated hearing loss can also increase risk for
falls.
“If you have hearing loss, don’t leave it untreated; it can lead to auditory depravation: depriving your brain of sound, which can lead to processing sound later,” said Kristopher Rookey, hearing instrument specialist at Port City Hearing in Oswego. “Your understanding will decrease. When the brain forgets how to do something, it’s harder to do in the long run.”
He added that not hearing can cause isolation, as people become disengaged, though physicallypresent. This contributes to depression.
“If you have hearing loss, it’s absolutely important to take care of it sooner than later,” Rookey said.
For older adults, letting hearing loss go too long can increase the risk of cognitive impairment because the part of the brain stimulated by hearing sounds receives less input. The Centers for Disease Control and Prevention has stated that 40% of dementia and early cognitive decline is modifiable. Part of that involves treating hearing loss.
“If addressed early enough, there’s a 19%-20% reduced risk of cognitive decline and dementia,” Anzolone said.
She added that even waiting one to three years before treating mild hearing loss can change the brain. Unfortunately, it can take many people a long time to discover and treat hearing loss—the average time is seven years, even though their insurance often covers the entire cost of hearing aids.

Page 26 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
Nicole Anzolone, audiologist with Syracuse Hearing Solutions.
Fayetteville | Lyndon Office Park 7000 E Genesee Street Bldg E, Fayetteville, NY 13066 315.565.3250 | Hours: M-F 9 am to 5 pm Camillus | Aspire Medical Center 5639 W Genesee Street | Camillus, NY 13031 315.468.2985 | Hours: M-F 9 am to 5 pm You can now visit us in Camillus or Fayetteville! HEARING BALANCE COGNITION TINNITUS Now open! SyracuseHearing.com We Go the Extra Mile for Our Patients! Our 5 star reviews say it all!
By Jim Miller

How to Choose an Assisted Living Facility
Dear Savvy Senior,
What’s the best way to go about choosing an assisted living facility for my 86-year-old father? Since mom died last year, his health has declined to the point that he can’t live at home anymore but isn’t ready for a nursing home either.
Searching Susan
Dear Susan,
If your dad needs help with things like bathing, dressing, preparing meals, managing his medications or just getting around, an assisted living facility is definitely a good option to consider.
Assisted living facilities are residential communities that offer different levels of health or personal care services for seniors who want or need help with daily living.
There are nearly 29,000 assisted living communities (also called board and care, supportive-care or residential-care facilities) in the U.S. today, some of which are part of a retirement community or nursing home. Most facilities have anywhere between 10 and 100 suites, varying in size from a single room to a full apartment. And some even offer special memory care units for residents with dementia.
To help you choose a good assisted living facility for your dad, here are some steps to follow.



• Make a list: There are several sources you can turn to for referrals to top assisted living communities in your area including your dad’s doctor or nearby hospital discharge planner; friends or neighbors who’ve had a loved one in assisted living; or you can do an online search at Caring.com.
• Do some research: To research the communities on your list, put a call into your long-term care ombudsman. This is a government official who investigates long-term care facility complaints and advocates for residents and their families. This person can help you find the latest health inspection reports on specific assisted living facilities and can tell you which ones have had complaints or other problems in the past. To find your local ombudsman visit LTCombudsman.org.
• Call the facilities: Once you’ve identified a few good assisted living facilities, call them to see if they have any vacancies, what they charge and if they provide the types of services your father needs.



• Tour your top choices: During your visit, notice the cleanliness and smell of the facility. Is it homey and inviting? Does the staff seem respon-
sive and kind to its residents? Also be sure to taste the food, and talk to the residents and their family members, if available. It’s also a good idea to visit several times at different times of the day and different days of the week to get a broader perspective.
On your facility visit, get a copy of the admissions contract and the residence rules that outline the fees (and any extra charges), services and residents’ rights, and explanations for when a resident might be asked to leave because their condition has worsened, and they require more care than the facility can provide.
Also, find out their staff turnover rate, COVID-19 infection-control procedures and if and when medical professionals are on site. To help you rate your visit, Caring.com offers a checklist of questions that you can download and print at Caring.com/ static/checklist-AL-tour.pdf.



• How to pay: Monthly costs for assisted living ranges anywhere from $2,500 to $6,000 or more, depending on where you live, the facility you choose, and the services provided. Since Medicare does not cover assisted living, most residents pay outof-pocket from their own personal funds, and some have long-term care insurance policies.
If your dad has limited financial resources and can’t afford this, most states now have Medicaid waiver programs that help pay for assisted living. Or, if he’s a veteran, he may be able to get funds through the VA’s Aid and Attendance benefit. To find out about these programs, ask the assisted living facility director, or contact his local Medicaid office (see Medicaid.gov) or the regional VA benefit office (800–827–1000).
May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 27
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.
daily living.
Assisted living facilities are residential communities that offer different levels of health or personal care services for seniors who want or need help with
Call me to set up in-person or over the phone consultation and let me help you, at no cost!! www.ballardassoc.com • ballardassoc@gmail.com AARON BALLARD President & Owner, Ballard & Associates, LLC. Happy with your Prescription Coverage? Happy with your copays? Do you have extra $$$ set aside for burial expenses? Do you know if you qualify for help paying for your prescriptions? Aaron Ballard is a licensed Insurance broker representing all the top Medicare carriers in CNY & beyond! 315-374-1783 Insurance Made Simple Turning 65 or just confused about Medicare? We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options. Over-the-counter hearing aids now available! near the pharmacy Discreet, more affordable, & highly effective for those with mild to moderate hearing loss. Try risk-free with 60-day guarantee. New! ENGAGE® RECHARGEABLE & BATTERY ENLITE® BATTERY ENLITE® PLUS RECHARGEABLE ENRICH® PRO BTE BATTERY ENRICH® BATTERY
Ask From the Social Security District Office
The Social Security Office Q&A
By Warren Beck Social Security District Manager in Syracuse.
Stay Informed With Social Security’s Top Five Social Media
We strive to provide the public with accurate and helpful information. In addition to the resources available on our website at www.ssa.gov, we also regularly post useful information on our blog and on social media. We invite you to read our posts and share items of interest with your family and friends.
1. You can subscribe to our blog. We post articles about programs, policies, current topics and new online services. Read more and subscribe at blog.ssa.gov.
2. You can follow us on Facebook at www.facebook.com/socialsecurity. You can also share Facebook posts with family and friends.
3. We have many informative videos on YouTube. Our videos cover online services, applying for

Pages
retirement and disability benefits, Social Security-related scams, and much more. We also offer some of our videos in Spanish. You can view and easily share our videos at www. youtube.com/SocialSecurity.
4. You can join our many Twitter followers at www.twitter.com/ socialsecurity. We use Twitter to announce new my Social Security features and other service or program changes.
5. We’re also on Instagram. We share stories and resources that can help you and your loved ones. Check out our Instagram page at www. instagram.com/SocialSecurity.
Connect with us on social media to learn helpful information. Follow along and share our pages with a friend, neighbor, or loved one today. Check out all our social media channels at www.ssa.gov/socialmedia.
Caring for all parts of you. EVERYBODY
Q.: I’m reaching my full retirement age and thinking about retiring early next year. When is the best time of year to apply for Social Security benefits?
A.: You can apply as early as four months before when you want your monthly benefits to begin. To apply, just go to www.ssa.gov/applytoretire. Applying online for retirement benefits from the convenience of your home or office is secure and can take as little as 15 minutes. It’s so easy!
Q.: Will my retirement benefits increase if I wait and retire after my full retirement age?
A.: Yes. You can increase your Social Security retirement benefit in two ways:
• You can increase your retirement benefit by a certain percentage if you delay receiving retirement benefits. We will add these increases automatically from the time you reach full retirement age until you start receiving benefits or reach age 70.
• If you work, each additional year you work adds another year of earnings to your Social Security record. Higher lifetime earnings may result in higher benefits when you do retire.
For more information, visit www. ssa.gov/pubs to read, print, or listen to our publication, "When to Start Receiving Retirement Benefits." You also can use our retirement estimator at www.ssa.gov/estimator to determine your estimated future benefits.
BENEFITS
Q.: What is the earliest age that I can receive Social Security disability benefits?
A.: There is no minimum age as long as you meet the Social Security definition of disabled and you have sufficient work to qualify for benefits. To qualify for disability benefits, you must have worked under Social Security long enough to earn the required number of work credits and some of the work must be recent. You can earn up to a maximum of four work credits each year. The number of work credits you need for disability benefits depends on the age you become disabled. For example, if you are under age 24, you may qualify with as little as six credits of coverage. But people disabled at age 31 or older generally need between 20 and 40 credits to qualify, and some of the work must have been recent. For example, you may need to have worked five out of the past 10 years. Learn more at www.ssa.gov/disability.
Q.: What is the purpose of Supplemental Security Income, or SSI?
A.: The purpose of SSI is to help aged, blind, and disabled people who have little income and few resources to support themselves. It provides financial assistance to meet basic needs for food, clothing, and shelter. You can receive SSI even if you have not worked and paid into Social Security. SSI is a federal income supplement program funded by general tax revenues (not Social Security taxes). Find out more at www.ssa.gov/ssi.
Wellness is about actively nurturing your physical, mental, emotional, and spiritual health and making choices that promote balance in all parts of your life. Here are some tips for keeping all of you healthy.
1. Physical Wellness: Exercise regularly, eat more fruits and vegetables, reduce processed and sugary foods and get more sleep.
2. Emotional Wellness: Maintain a positive attitude, take time for self-care (meditation, reading, or quiet relaxation), and practice gratitude.
3. Social Wellness: Keep in touch with friends and family. Connect with others by joining a club, starting a new hobby or volunteering.
4. Intellectual Wellness: Take an online or in-person class, read a book on a new topic, challenge your mind with puzzles or games.
Learn more about taking care of yourself at ExcellusBCBS.com/PreventiveCare
5. Spiritual Wellness: Connect with your inner self. Practice mindfulness by focusing on the present moment. Reflect on your personal values and beliefs.
6. Environmental Wellness: Boost wellbeing by spending time in nature. Care for our planet by reducing waste, composting or recycling.
7. Occupational Wellness: Seek professional development, strive for work-life balance, connect with coworkers.
Page 28 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023
Loretto nurses do so much to care for our residents and their own families. That’s why we’re committed to caring for them and supporting their growth by offering competitive pay and benefits, flexible hours and, most of all, a chance to move up.

Find your future at Loretto. Explore opportunities at lorettocny.org/future.
To hear more of Frank’s story and learn if CyberKnife is right for you, visit hoacny.com


Frank chose non-surgical CyberKnife® at HOA –offering 5 treatments instead of 35!



“The original diagnosis was to treat my prostate cancer with seven weeks of radiation, five days a week. I was kind of upset that I was never given the option of CyberKnife,” said Frank. “The precise radiation achieved by CyberKnife, far fewer treatments, and the personalized care I received from Dr. Chin and his team made my decision an easy one. Better, the treatment was a real success!”

May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 29
Frank Guido couldn’t be happier he had a choice for treating his prostate cancer!
Find your at Loretto
Happy Nurses Week!
David Landsberg Appointed as Crouse’s Chief Medical Officer

Physician David Landsberg has been appointed chief medical officer (CMO) at Crouse Health.
In this senior leadership role, Landsberg will provide clinical leadership for Crouse Health and will work with the medical staff to drive the hospital’s mission to provide the best in patient care. Landsberg will also oversee the quality improvement department and medical affairs.


A long-time member of the Crouse Health, Landsberg most recently has served as chief of medicine, a position he has held since 2012. From 2018 to 2020 he served as immediate past-president of the medical staff, and was president of the medical staff from 2016-2018. He currently serves as an intensivist and ICU director at Crouse as well as site director for Upstate’s internal medicine residency program.

Landsberg received his medical degree from Saba University School of Medicine and completed residencies at Mount Sinai School of Medicine and critical care fellowships from Memorial Sloan Kettering Hospital and New York Presbyterian Hospital – Cornell Medical College.
Landsberg currently serves as professor of medicine and emergency medicine for Upstate Medical University. He also is director of adult critical care and ECMO programs at
Crouse and is medical director of Finger Lakes Donor Recovery Network. Additionally, he serves as deputy coordinator for Onondaga County Emergency Management.
“I am proud to appoint Dr. Landsberg to this important leadership position. He is well-respected, a proven leader among his peers and colleagues and is recognized for his strong ethics and professional standards,” says Crouse President and Chief Executive Officer Seth Kronenberg, MD.
Page 30 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • May 2023 HAPPY
Thank you for your care, compassion, strength, and skill. JOIN OUR TEAM bassett.org/careers LOCAL HEALTH PROFESSIONALS DELIVERING INNOVATIVE HOME CARE FOR 45 YEARS • Skilled Nursing • Physical Therapy • Occupational Therapy • Speech Therapy • Medical Social Work • Home Health Aides • Nutrition Services • Care Management JOIN OUR CARING TEAM TODAY! HCRhealth.com/careers Health News
NURSES MONTH!
NAME ADDRESS CITY/TOWN STATE ZIP 1 YEAR (12 ISSUES) $21.00 $35.00 2 YEARS (24 ISSUES) Clip and Mail with payment to: In Good Health P.O. Box 276, Oswego, NY 13126 SUBSCRIBE TODAY and get In Good Health: CNY’s Healthcare Newspaper right to your home or office!
David Landsberg


May 2023 • IN GOOD HEALTH – CNY’s Healthcare Newspaper • Page 31 The Alzheimer’s Association® offers round-the-clock support a Alzheimer’s disease and other dementias. Free 24/7 Helpline: 800.272.3900 Alzheimer’s and Dementia Caregiver Center: alz.org/care Caring for someone with Alzheimer’s isn’t easy. Reaching us is. 18365436


Acupuncture Center USA 7th Generation Rui Wang, LLC Northeast Medical Center, Suite 209 4000 Medical Center Dr., Fayetteville, NY 13066 Tel1: 585-358-6186; Tel2: 315-378-5556; Tel3: 607-372-2082 Ancient Wisdom Integrated with Modern Medicine LIFE CHANGING MEDICINE, MOVING MEDICINE FORWARD ONE OF THE BEST ACUPUNCTURE CENTERS IN THE WORLD Acupuncture is a general practice alternative medicine, it can help a wide range of health problems at different extents. Ask for professional, confidential, personalized evaluation / consultation appointment before starting any treatment Balance Immune System Build Stronger Immunity www.AcupunctureCenterUSA.com 7th Generation Medical Acupuncture Rui Wang, MD of China, L.Ac. Featuring RUI Anti-Inflammatory Acupuncture, Medical Oncology Acupuncture, and Neuromedicine Acupuncture Experienced in both Western Medicine & Traditional Chinese Medicine Experienced in both Academic & Private Practice Experienced in both Basic Science & Clinical Science Experienced in Cancer Research at Major Medical Centers in USA THE WORLD’S GREATEST TREASURE OF MEDICINE 靈樞抗癌 7th Generation Medical Oncology Acupuncture for Cancer Care, Cancer Survivor Care, and Cancer Prevention Part of Comprehensive Cancer Care Build Anti-cancer Immunity, Improve Cancer Immune Surveillance Ability; Relieves Cancer Complications and Cancer Treatment Induced Side Effects; Drug-Free Care without Drug Interactions with Conventional Cancer Treatment; Personalized Cancer Supportive Care, Integrative Cancer Care. *Do Not Stop Your Conventional Western Medicine Cancer Care during the Acupuncture Care, since Medical Oncology Acupuncture Is Only Part of Comprehensive Cancer Care.




















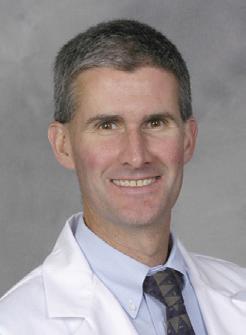


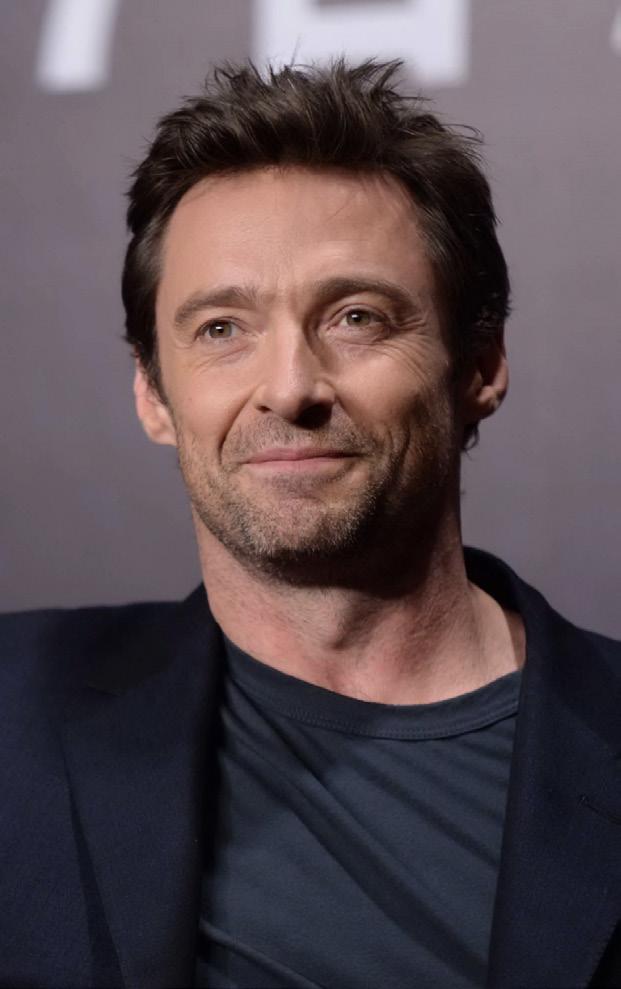















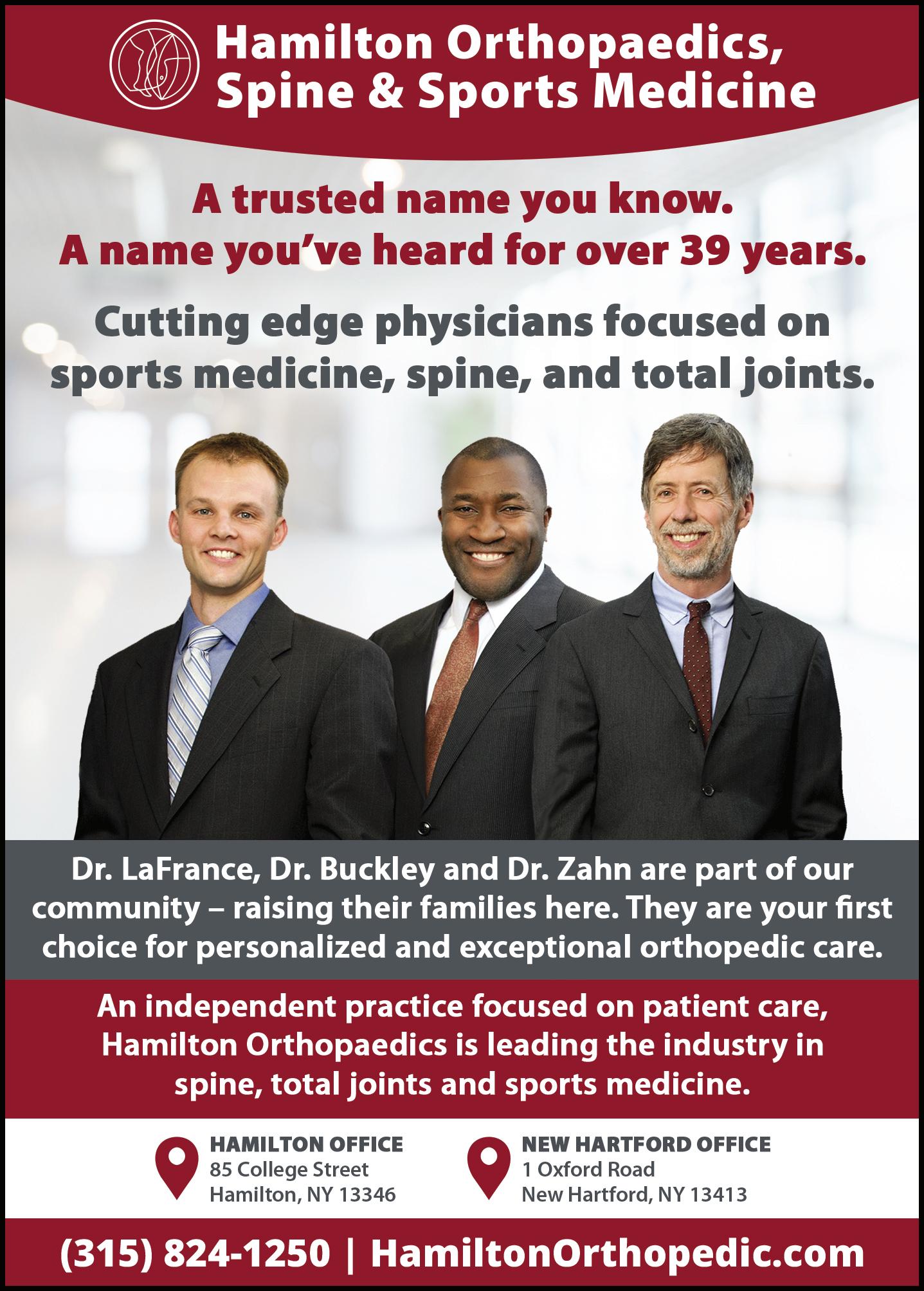






 By Ernst Lamothe Jr.
By Ernst Lamothe Jr.



 By Mary Beth Roach
By Mary Beth Roach





































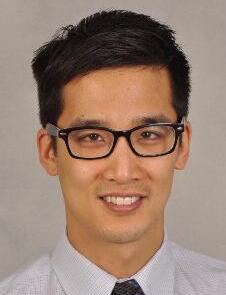













 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant