HOSPITALIST IN CHARGE


Fulton native Nicholas Runeare, MD, is now Oswego Health’s hospitalist medical director — he talks about his new position and his focus on quality, safety and patient satisfaction P. 4




Fulton native Nicholas Runeare, MD, is now Oswego Health’s hospitalist medical director — he talks about his new position and his focus on quality, safety and patient satisfaction P. 4

Adolescent cannabis abuse has increased 245% since 2000 in the U.S., while alcohol abuse has steadily declined over the same period.
That’s according to a national, peer-reviewed study tracking intentional misuse and abuse reported to the National Poison Data System (NPDS) up until 2020.
Findings, published in December in the peer-reviewed journal Clinical Toxicology, find over 338,000 instances of intentional abuse or misuse among American children aged 6-18.

The majority of ingestions occurred in males (58.3%), and more than 80% of all reported exposure
cases occurred in young people aged 13 to 18.
In total, over 32% of instances resulted in “worse than minor clinical outcomes”.
The new report demonstrates a change in patterns over time. For instance, in 2000 the largest number of abuse cases involved exposure to ethanol, yet since then child alcohol abuse has steadily declined over the years.
In contrast, marijuana exposure cases remained relatively stable from 2000 to 2009, then steadily rose from 2011, with an even more dramatic rise in cases from 2017 to 2020.
Experts analyzing the data
attribute the rise in marijuana use to the increased popularity of edible cannabis products, now widely available across the country.
“Ethanol abuse cases exceeded the number of marijuana cases every year from 2000 until 2013,” says physician Adrienne Hughes, assistant professor at Oregon Health & Science University, one of the authors of the study.
However, by 2014 this trend had reversed.
“Since 2014, marijuana exposure cases have exceeded ethanol cases every year, and by a greater amount each year than the prior,” says Hughes.
While rates of all marijuana abuse increased, edible marijuana showed the highest average monthly increase compared with all other forms, suggesting that adolescents have moved away from smoking weed onto alternative modes of consumption. Marijuana extracts, such as those used in cannabis vaping products, were also increasingly popular.

“These edible and vaping products are often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” says Hughes.

However, although they may be perceived as less harmful, studies show this is not the case.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms of marijuana usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” says Hughes.
The dramatic increase in child cannabis use since 2017 coincides with a wave of decriminalization legislation in the US. As of 2022, cannabis is legal for adult recreational use in 19 states and for medical use in 36 states.
While cannabis is only legal for adults and not children, the authors of the study argue that it has rendered the drug more accessible to children and adolescents and contributed to a perception that the drug is safe.
“Our study describes an upward trend in marijuana abuse exposures among youth, especially those involving edible products,” says Hughes.
“These findings highlight an ongoing concern about the impact of rapidly evolving cannabis legalization on this vulnerable population.”




As well as cannabis, the study reveals high levels of over-thecounter medication abuse among teenagers. Between 2001- 2016, the highest number of drug abuse cases related to dextromethorphan, an over-the-counter cold and cough medicine. Oral antihistamines were also among the most commonly misused substances in this study.
Deaths from drug abuse were rare, occurring in 450 young people (0.1% of cases). Deaths were more common in males, and in older teens aged 16-18. They were also most likely to occur after abusing opioids.
And, although there were 57,488 incidents involving children aged just 6 to 12, these cases did not usually include ‘traditional’ drugs but rather vitamins, plants, melatonin, hand sanitizers and other objects.



























Owners whose cats have diabetes now have a new option to care for the condition in their otherwise healthy pets.
The U.S. Food and Drug Administration in December approved the first pill to improve control of diabetes in some cats.
The drug, called Bexacat (bexagliflozin tablets), is not insulin and is not meant for cats who have the type of diabetes that requires treatment with insulin. Rather, it is what is called a sodium-glucose cotransporter 2 (SGLT2) inhibitor.
Bexacat is a once-daily flavored pill given with or without food to cats who weigh at least 6.6 pounds.
The active ingredient in this pill prevents the cat’s kidneys from reabsorbing glucose into the blood. This excess glucose leaves the body through the urine, lowering blood sugar levels.
As part of the approval, the FDA requires that Bexacat labels include a boxed warning about the importance of patient selection. Only certain cats should take the drug, determined through careful screening.
Potential patients must be screened for kidney, liver and pancreatic disease, as well as ketoacidosis, a high level of a type of acids known as ketones in the blood.
Cats who are treated with Bexacat may be at an increased risk of serious adverse reactions, including diabetic ketoacidosis, the FDA said. This can be fatal and should be treated as emergencies.

In a news release about the approval, the FDA explained that like in humans, the cells of a cat’s body need sugar in the form of glucose for energy. Cats with diabetes can’t properly produce or respond to the hormone insulin. Insulin helps cells use glucose for normal function.
The FDA cited two field studies that were six months long and an extended field study in its approval. The studies found the medication was more than 80% effective in improving blood sugar control in cats with diabetes.

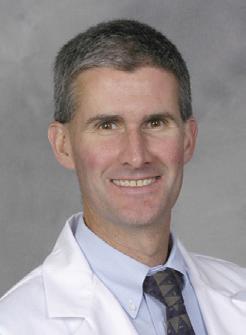
Fulton native is now Oswego Health’s hospitalist medical director — he talks about his new position and his focus on quality, safety and patient satisfaction
Q: You’re an Oswego County native, but how long have you been back home working with Oswego Health?
A: I’ve been a provider for about a year and half. I have kind of a long history with Oswego Health. I’ve been a patient there and there were a number of programs that I engaged with over the years. There was a program in the lab that I was involved with in college, and then in medical school I did the rural health program at Oswego Health. When I finished my residency in Syracuse, I came here to practice. So I’ve been a hospitalist with Oswego Health for about a year and a half. And then I picked up the role of hospitalist medical director last September.
Q: Did you have your sights set on the role or did you more fall into it?
A: A little bit of both. I’ve always gravitated toward leadership positions. I was in leadership positions in medical school and residency, so it always seemed kind of like a natural progression. And then it just fell into place. We needed a new leader, the position was open and with my back-
it’s a year where you’re also looking at quality at the Syracuse VA Medical Center. Whether that’s length of stay, process initiatives, metrics for a wide variety of domains.
Q: For those of us who may be unfamiliar, what is a chief resident?
A: All specialty chief years are a little bit different. So they either, in your last year of residency or an additional year—mine was an additional year, which is typical for hospitalists. Mine was focused on quality and safety, but I was also an attending who interacted with the residents directly. Chief years can be almost entirely administrative, where you’re designing the schedule, but mine was less focused on that and more on maintaining the quality of the hospital and transitions between the VA and SUNY Upstate because our residents were moving between the two hospitals.
Q: What kinds of quality indicators are a priority for a rural network like Oswego Health?
A: I think with all hospitals there are institutional quality goals and patient-centered quality goals.
also important for the patient. They want to be in the hospital for the shortest amount of time possible. By shaving off the amount of time they’re there, we’re reducing the cost to us in resources, which in turn allows us to treat more patients, and make sure the care that we’re giving is the best possible.
Q: Does being based in a college town affect continuity of care given the transient population? For tracking some indicators?
A: Over the care spectrum it might, but we don’t see a lot of college students overall. Most of our patients are longtime members of the community. I think we’re in a somewhat unique position in that we have good relations with our outpatient providers and we’re always working on improving our relationship with them. So I’ve been going out into the community to speak with the outpatient practices to develop connections. I think we recognize that hospitalist medicine can’t really be practiced in a vacuum. We want to connect the dots between being an inpatient and an outpatient and make sure the transitions of care are effective.
Q: I understand you have an interest in orientation and gender identity healthcare. What kinds of resources can Oswego Health offer in that domain?

A: Being sensitive to all demographics is important so that people feel comfortable seeking treatment. All populations have a lot of the same illnesses and comorbid conditions, but social factors do need to be taken into account so that people are comfortable. We offer bread and butter medicine to all populations, but I think connecting gender medicine and sexual health medicine to the resources they need—usually in Syracuse-area hospitals or outpatient providers—is important too. So we can kind of springboard a lot of those patients to the providers who can get them the care that we may not offer.
along with quality, is very important for small, rural hospitals. Resources are ways trying to get more -
Q: What’s the low-hanging fruit, do you think, in terms of indicators that can be improved at Oswego Health going forward?
play. Length of stay has been really focused in the past year.
number of mains.
A: I think patient satisfaction has been big for me and it’s probably one of the easiest to accomplish. We’ve just renovated the inpatient wards. We’re fully staffed with some very experienced, very good hospitalists. I haven’t been in the position long, but I’m hearing this is one of the strongest hospitalist teams that we’ve had. So that allows us to make the patients’ experiences better and making sure the communication they’re receiving is better and that it gets passed on to their primary care providers. At the end of the day it’s about the patients, full stop. And that’s where we can be most effective.
ant for pital, it’s
Name: Nicholas Runeare
Position: Hospitalist medical director at Oswego Health
Hometown: Fulton Education: SUNY Upstate Medical University Affiliations: Oswego Health
Organizations: American College of Physicians
Family: Partner (a nurse at Oswego Health)
Hobbies: Skiing, cooking






















www.connextcare.org













More Americans are dying from gun violence, in both homicides and suicides, than they have in decades, a new report shows.
The U.S. gun death rate hit its highest level in nearly 30 years, with the sheer number of people dying from guns reaching 47,000 in 2021, the highest in 40 years, according to the study.

Increases were higher for women than men, and especially for Black women. Among Black women, firearm-related homicides have tripled
since 2010, while suicides have doubled since 2015.
“Women can get lost in the discussion because so many of the fatalities are men,” study co-author, physician Eric Fleegler, an associate professor of pediatrics and emergency medicine at Harvard Medical School in Boston, told the Associated Press.
Researchers found a 71% increase in the number of women killed by guns, from four per 100,000 in 2010 to seven per 100,000 in 2021. Women comprise about 14% of overall gun
deaths.
In Black women, suicides rose from a rate of 1.5 per 100,000 in 2015 to about three per 100,000 in 2021. Homicides in Black women were 18 per 100,000, while they were four per 100,000 in Hispanic women and just two per 100,000 in white women.
More than 1.1 million people were killed by guns during the study’s 32-year timeframe.
Researchers found a steady increase in gun deaths beginning in 2005, and then a sharp jump from 2019 to 2021, when deaths rose 20%.
Fleegler said that asking why gun deaths would rise during the pandemic was “a straightforward question with probably a complicated answer that no one really knows the answer to.”
Experts said it could be a mix of higher gun sales, stress, mental health issues and disruptions at home and work.
Men also saw an increase in gun deaths, and Black men continued to have the highest gun death rates.
The findings were published Nov. 29 in the journal JAMA Network Open.
Since the outbreak of COVID-19 three years ago, the average length of stay (ALOS) in a hospital has increased 19% according to the American Hospital Association.
It has increased 24% specifically for patients waiting to be transferred to a post-acute facility like a nursing home or psychiatric facility.
The increased ALOS for patients waiting to be transferred is due in large part to staffing shortages at post-acute facilities. These patients have been clinically cleared for discharge. They are literally lingering in hospital beds which in turn delays admissions from hospital emergency rooms.
Consequently, patients are being treated in ER hallways due to lack of available beds.
Hospitals are asking Medicare and commercial insurers for relief. Hospitals are not paid by the day or per diem. They are paid by DRGs (diagnostic related groups). Each DRG payment is based on acuity and procedure and an ALOS. The DRGs were established well before the pandemic. The AHA is suggesting a temporary resurrection of per diem payments, especially for those patients cleared for discharge but are waiting to be transferred to another facility.
While most nonprofit hospitals ran an operating deficit every month through October in 2022, the nation’s three largest for-profit systems reported healthy operating profits through the same period. HCA Healthcare was 11%; Tenet was 8%; and Community Health Systems was 1%.
The United Health Foundation, affiliate of health insurance giant United Healthcare, just issued its annual report on the changes in our overall health from 2020 to 2021. There is very little good news. There was an 11% increase in people describing their mental health as “poor” and a 15% increase in people reporting they were in “frequent mental distress.” There was a 20% increase in drug-related deaths (28/100,000). There was an 18% increase in premature deaths (before age 75). There was a 13% increase in gun related deaths. The number of people with multiple chronic conditions increased 5%. While there was a 7% decrease in the uninsured, part of this gain may be lost if pandemic related insurance flexibilities and incentives expire in 2023. The “good news”? United’s profit was $17.3 billion in 2021.

Nothing is more aggravating and
frustrating to physicians and their patients alike than having to wait for an insurance company to approve what the physician has ordered to care for their patients. Prior authorization for designated procedures and drug referrals is required by insurers. Purportedly, It is a cost containment tool to deny ineffective or unnecessary drugs and procedures. Approval or denial can often take weeks, which delays care. Typically, 95% are approved anyway, so prior authorization is more of a cost delaying tool. Consequently, CMS has jumped in to speed up and improve the process.
By 2026, Medicare Advantage plans, Medicaid Managed Care plans, and Affordable Care Act commercial plans on the insurance exchanges must implement electronic authorization, eliminating the labor- intensive paperwork seemingly designed to slow things up. There will be incentives for providers to implement this as well. The goal is to improve the patient experience, speed up the delivery of care, decrease patient anxiety and get frustrated providers out of the middle. Insurers must give specific reasons why something was
denied within seven days.
The Institute for Healthcare Management and the AMA recently announced the creation of the “Rise to Health Coalition.” Along with the American Hospital Association and Race Forward, advocates for reducing racial inequities if healthcare, the coalition will recruit providers, payers and drug manufacturers to share solutions on improving outcomes and expunging racial inequities in healthcare. The group will focus on access, workforce, cost, quality, safety and social determinants of healthcare (income, race, nationality, transportation, housing, unemployment, food insecurity and education). Each organization must also develop measurable reductions in inequities within their organization. The coalition has laudatory goals. It remains to be seen how much cooperation can be engendered between not-for-profit organizations and for-profit businesses.
The negative impact of the pandemic on our mental health is undisputed. The Senate Finance Committee is in the early stages of examining the inequities in how insurance plans, both governmental and commercial, treat mental health. The committee is concerned about inaccurate and outdated provider directories, (referred to as “ghost networks”), pay rate disparities between medical/surgical versus mental health providers and disparities between patient cost sharing or out of pocket for mental health services versus all other. The committee has asked the General Accounting Office to investigate payment and consumer out of pocket disparities. Consumers that have selected a plan based upon participating mental health providers are often thwarted by wrong or out of date provider contact information and/or providers not accepting new patients. More mental and behavioral health providers would participate in various insurance plans if reimbursement was fair and reasonable. The committee expects to file a report early 2023.
Hospitals, physicians and ancillary providers have encouraged their patients to set up an account with their patient portal to communicate, bypassing clogged phone lines. The portals are designed for patients to verify, schedule and cancel appointments, update insurance and demographics, seek information about the practice, or what might be required before a visit.
Unfortunately, patients seeking to avoid an office or telehealth visit are abusing the portal by seeking medical advice for free. Consequently, providers like the Cleveland Clinic have begun charging patients for a provider’s time and expertise, usually about $50. Many hospital systems, physician practices and other professionals are contemplating also charging for medical advice sought via their patient portal. I do not know how insurance is viewing this recent phenomenon.
The CDC and the AMA are recommending(and imploring) pregnant mothers to get vaccinated. Since the beginning of the pandemic, pregnancy related deaths are up 80%. Unvaccinated pregnant women and their unborn children are at far greater risk for complications, severe illness or even death. Right now, infants younger than 6 months are being hospitalized for COVID-19 at the same rate as seniors older than 65. Unfortunately, only 45% of pregnant women are vaccinated and only 52% of women who are breast feeding.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

Lasik eye surgery is a common vision-correcting procedure that many Americans view as safe and effective, but the U.S. Food and Drug Administration has now drafted guidance that warns of potential complications.
Although many patients are happy with the results after surgery, the recommended new guidance says complications can include dry eyes, double vision, difficulty with night driving and, in rare cases, chronic eye pain. Even after surgery, some patients will still need eyeglasses.
The draft also notes that certain types of patients may be at higher risk of problems, including people with chronic conditions such as diabetes and those who take certain medications.
Since the recommendations were first released this summer, more than 600 people and professional organizations have weighed in on the issue.
“All we’re asking for is balance,”said Vance Thompson, incoming vice president of the American Society of Cataract and Refractive Surgery, told the Times. “This document mainly emphasizes the dangers and complications of Lasik, with no mention of the advantages, and the tone is negative enough that it will scare patients.”
Thompson noted that more than 90% of patients in the FDA’s studies were satisfied because they were “achieving good vision without spectacles, which is the goal of most patients.”
Surgeons and device manufacturers have sought to have the draft recommendations withdrawn.
But a professional organization representing optometrists recommended adding even more precautions to the draft, to include pregnant women and those with irregular astigmatism.
Lasik is typically a procedure completed in just 15 minutes per eye, where the surgeon reshapes the cornea with cuts and a laser to correct poor vision. Often the procedure is not covered by insurance and can cost patients thousands of dollars out of pocket.
Still, more than 500,000 adults opt for the surgery each year and many ophthalmologists declare it safe, with complications happening very rarely.
To arrive at the draft recommendations, the FDA both collaborated on and analyzed studies on Lasik outcomes published in the past decade.


One of those studies found that three months after Lasik nearly half of patients who had previously not had visual symptoms did after the procedure. This included seeing halos around lights. About one-third of the patients had dry eyes.
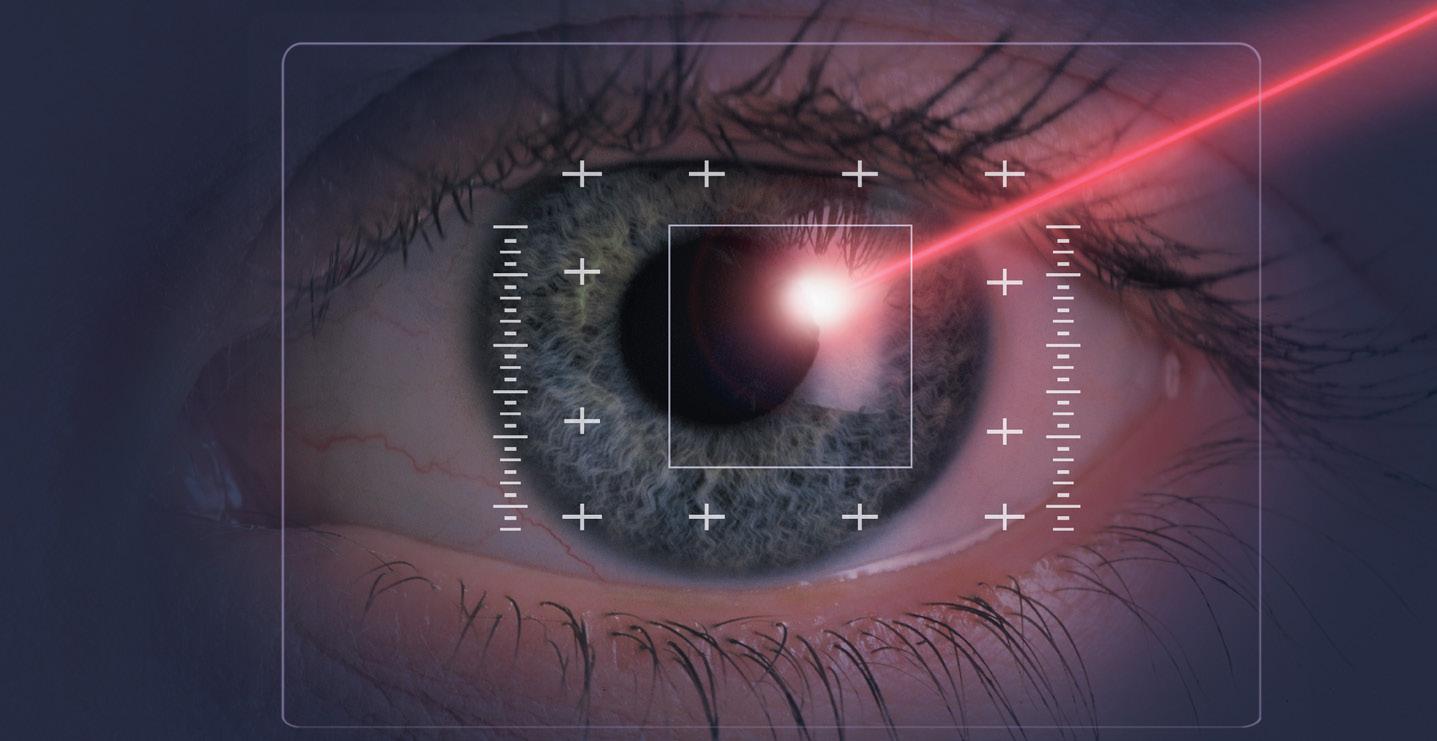
“Patients undergoing Lasik surgery should be adequately counseled about the possibility of developing new visual symptoms after surgery before undergoing this elective procedure,” the study authors wrote.
The FDA has not said when the guidance will be finalized.
A monthly newspaper published by Local News, Inc. 33,500 copies distributed throughout more than 1,000 high-traffic locations, including all Wegmans stores.
In Good Health is published 12 times a year by Local News, Inc.
2022 Local News, Inc. All rights reserved. P.O. Box 276, Oswego, NY 13126 Phone: 315-342-1182
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen
6700 Kirkville Road, Suite 107 East Syracuse, NY 13057 315-760-5905
www.velocityclinical.com
Velocity Clinical Research is committed to making clinical research studies succeed by generating high quality data, while providing exemplary individual care at every step. Our team achieves this goal by making sure quality of care as one of our highest obligations.
Velocity Clinical Research is committed to making clinical research studies succeed by generating high quality data, while providing exemplary individual care at every step. Our team achieves this goal by making sure quality of care as one of our highest obligations.
Our site participates in national and global research studies by partnering with specialists from all different backgrounds. Our team joins together to explore new medical treatments by conducting clinical research studies for investigational edications and diagnostic tools. Our site conducts multiple concurrent studies, all performed in accordance with mandatory guidelines.
Our site participates in national and global research studies by partnering with specialists from all different backgrounds. Our team joins together to explore new medical treatments by conducting clinical research studies for investigational edications and diagnostic tools. Our site conducts multiple concurrent studies, all performed in accordance with mandatory guidelines.
Conveniently located in Central New York, our site offers ease of access from major highways and NYS Thruway. Our site offers free parking along with a commitment to providing individuals safety and data integrity through the duration of each research study
Conveniently located in Central New York, our site offers ease of access from major highways and NYS Thruway. Our site offers free parking along with a commitment to providing individuals safety and data integrity through the duration of each research study
Healthy Memory
Independent with self-care. No memory concerns outside of normal aging.
Independent with self-care. No memory concerns outside of normal aging.
Memory Loss/Mild Cognitive Impairment
Occasional forgetfulness or loss of shortterm memory that interferes with daily life. Possibly experiencing diminished thinking skills, ability to make sound decisions, or forgetting important information.
Occasional forgetfulness or loss of shortterm memory that interferes with daily life. Possibly experiencing diminished thinking skills, ability to make sound decisions, or forgetting important information.
Non-alcoholic steatohepatitis (NASH) is a type of fatty liver disease characterized by inflammation of the liver and fat accumulation in the liver.
Non-alcoholic steatohepatitis (NASH) is a type of fatty liver disease characterized by inflammation of the liver and fat accumulation in the liver.
Utilize trained staff to administer vaccine(s) in accordance with the protocol of the research study.
Utilize trained staff to administer vaccine(s) in accordance with the protocol of the research study.
FDA drafts guidance that warns of potential complications
I’ve discovered that a key to living alone successfully is to determine who you really are and what you want from life.
My own path to contentment took some time, some growing pains — setbacks as well as successes — and some aching losses before I found my “true north.” It hasn’t always been easy, but it’s been well worth the journey.
The reward has been a life on my own filled with more peace, freedom and joy than I could have imagined.
The journey began with a set of soul-searching questions (below) to identify and clarify my beliefs, values, likes and dislikes. I was careful to focus on what matters to me and to steer clear of “shoulds” and other people’s agendas.
The result? I created a list of personal principles and preferences that illuminated a way forward and shaped my future as a self-sufficient, independent woman.
Now, in the happy third chapter of my life, I am comfortable being me and expressing my true self.
In no particular order, below are just a few examples of my insights
(some profound, others practical) that have inspired and guided me:
n Gratitude, forgiveness and loving kindness are life staples to embrace, practice and model on a daily basis.
n Gathering with friends and family around a fire, kitchen counter or dining room table enhances life. It’s warm, relaxing, and relevant — life essentials in my book.

n If I am unhappy with an aspect of my life and choose to stick with the status quo, nothing will get better.
n Hardship, failure and loss can build strength and self-awareness.

Taking time to turn inward can create space for reflection and renewal of the spirit. Remember: After a rain there are rainbows.
n An honest-to-goodness listener (not a pretend listener) melts my heart.
n An honest-to-goodness friend who shares her joys, deepest fears, regrets and dreams melts my heart even more.
n Music makes life better. I enjoy playing and listening to all genres of music, but I always return to the Great American Songbook.
n As an introvert, I find that solitude, nature and meditation recharge my batteries. But that’s me. Others may be energized by morestimulating experiences and venues.
n Letting go of old ways of thinking, a poor self-image or of destructive thoughts, behaviors and habits can free you up to embrace life’s blessings.
n Gardening is a great teacher. Fertile ground exists in each of us, and a little planning, caretaking and patience can produce beautiful results.
n Solo travel is an adventure not to be missed. It’s good for the mind, deepens the soul and fosters confidence.
n Living alone doesn’t mean being alone. We are social beings. We need each other. Relationships are the glue.
Compiling my full list of insights took time and thought. For those coming out of a long relationship or deep loss, determining or rediscovering “who you really are” can be a daunting process.
After years of focusing on the needs and desires of a spouse and family, many discover that, somewhere along the way, they have disappeared around the edges and lost their own sense of self.
Rediscovering yourself and identifying those things that bring joy and meaning in your life can turn living alone into an adventure of the spirit.
Once you establish your individual interests and means of self-expression, you may find that time alone and quieter moments no longer feel empty.
Below is an exercise to help you get back in touch with your true self. These are but a few of some probing questions to contemplate on your road to self-discovery.
1. Search back. What hobbies did you pursue as a child that gave you joy? What did you do particularly well or (perhaps secretly) take pride in?
2. More recently, when do you completely lose yourself in something? What activities make you feel alive and complete, as though
nothing is missing?
3. What do you hold most dear?
4. How do you want to be remembered?
5. What is your biggest regret? If you could have a “do-over,” what would you do differently? Maybe seek help sooner? Or embrace and share a truth about yourself or situation?
6. How would your life change (or get better) if you were a more curious and open person?
7. What brings tears to your eyes?
8. If you were to dedicate your life and resources to a particular cause or charity, what would it be?
9. What does your perfect day look like?
10. How do you want to describe yourself and your life a year from now?
After answering these questions, ask yourself how you can use these insights to influence the direction of your life. What can you do today to reconnect with a past love or pursuit, to delve more deeply into an existing interest or to fulfill a new healthy lifestyle or passion?
When you identify your values and the things you love or need to do, and pursue them, you will feel more integrated and in touch with your true self. You’ll be spending your time immersed in pursuits that bring you personal satisfaction and strength — pursuits that reinforce who you are and who you want to become.
Those of us who live alone have the gift of abundant time to ourselves. Use it wisely. Use the time to get to know yourself all over again.
With each passing day, I am confident you’ll find your internal compass, unique to you, pointing north — your true north.
©
Are you having trouble losing weight and keeping it off? Do you have diabetes, high blood pressure, sleep apnea, heart/cholesterol problems, or other medical conditions associated with extra weight? If so, learn how weight loss surgery can improve your life.
William A. Graber, MD, PC – Weight Loss Surgery is an experienced team dedicated to helping people achieve their weight loss and healthy lifestyle goals. Our board certified bariatric surgeons specialize in laparoscopic and robotic assisted weight loss surgery and have performed thousands of procedures.
Working together with expertise to promote a supportive and safe environment for our patients as they strive to restore health and quality of life.
Offices in Utica and Syracuse
















Seasonal affective disorder is a type of recurrent depression that occurs during the winter months where there is less sunlight throughout the day.
With the season patterns varying, people who suffer from the condition often don’t feel like themselves and can have a sense of lethargic behavior and overall depression.
“Seasonal affective disorder is an essential topic now based on our current hemisphere,” said Samantha Goutermout, a nurse practitioner from Fulton PrimeCare at Oswego Health. “It can be very difficult because this is a condition that people don’t pay enough attention to. It can lead to feeling isolated and various mental health issues.”

Goutermout gives five facts about seasonal affective disorder.
Signs and symptoms of SAD may include feeling listless, sad or down most of the day, nearly every day, losing interest in activities you once enjoyed, having low energy and feeling sluggish and sleeping too much. In addition, people can experience carbohydrate cravings, overeating and weight gain, difficulty
concentrating, feeling hopeless, worthless or guilty and having thoughts of suicide.
“When you have people who are battling through SAD, you can see substance abuse issues, eating disorders and real suicidal thoughts,” she said. “We see people who tend to either have trouble sleeping or sleeping too much. They may have weight loss or weight gain issues and can become agitated and irritable.”
Too often because the condition is not always recognizable to others, there are various stereotypes that have emerged. It can range from people simply calling it the “winter blues” or thinking that people should recover once they see some sunlight during the day.
“There is a reason why people don’t just snap out of it. Research has shown that many factors play into someone having SAD,” said Goutermout. “SAD should be looked at in the same limelight as any other mental health disorder. In general, more women are diagnosed with SAD than men. It occurs more in younger adults than older and those with family history may be at risk.”
A light therapy box mimics outdoor light. It’s thought that this type of light may cause a chemical change in the brain that lifts your mood and eases other symptoms of SAD, such as being tired most of the time and sleeping too much.
“Light therapy can be a fantastic treatment. I would say it is one of the first lines of defense,” said Goutermout. “It really helps those dealing with diminished sunlight in the winter time. This is something that should be done 30 to 40 minutes in the beginning of the morning. The only caveat is that we believe this should be done with the help of a medical professional instead of simply buying something on Amazon. We would recommend light therapy but we would not recommend tanning beds which some people turn to.”
Generally, the light box should provide an exposure to 10,000 lux of light and produce as little UV light as possible.

“People dealing with seasonal affective disorder may want to start treatment before the start of the season and that way they can hopefully create a rhythm for themselves,” she said.
While people are talking about mental health more that doesn’t mean there aren’t still hurdles. No one is immune to mental health problems. People at all levels of social, occupational or economic status can experience a mental illness.
“Mental health is an issue that people need to talk more about and feel comfortable openly discussing in the same way people talk about diabetes or their blood pressure,” said Goutermout. “Mental health disorders such as SAD and depression have been treated
regularly in our offices and around the world during the last couple of years.”
It’s normal to have some days when you feel down. But if the feelings persist and motivation becomes difficult each day, experts say you shouldn’t try to handle the situation by yourself. They suggest seeking out a health care professional, especially if your sleep and eating habits have changed dramatically and you feel thoughts of suicide.
“Many people may be afraid to have a mental health diagnosis because people are worried that others will look at them differently” Goutermout. “But it has become a topic of conversation and we are still learning and improving in the mental health field. If you suspect you may be suffering from SAD, you really need to have a conversation with a physician. If you feel like you have low energy and are overly sluggish along with the other symptoms we mentioned you should consider seeing a professional.”
To distribute copies of In Good Health, CNY’s Healthcare Newspaper, in offices and other high traffic locations in Onondaga and Oswego
/h plus
- $200
When
make health equity a priority,




more at
ExcellusBCBS.com
MD,
A.
MD
Whenever I see a patient with an unusual medical history, I like to learn about their diagnosis and treatment from the patient. Then I review and refresh my knowledge on the subject. A case of someone with a pituitary tumor prompted this article.
The pituitary is a tiny gland inside the skull, just below the brain and above the nasal passages. It sits in a bony depression called the sella turcica — Latin for “Turkish saddle.” Although Google indicates this type of saddle was used on horses, it looks a lot like a camel saddle some friends brought home as a souvenir from their Peace Corps travels in northern Africa. The optic nerve traveling between the eyes and the brain sits just above the pituitary.
The pituitary is sometimes called the master gland because it produces many hormones that control the production of hormones by other endocrine glands. The pituitary has two parts. The anterior section makes the following hormones:
• Growth hormone
Also called somatotropin. This promotes body growth. Too much during childhood, before the bone’s growth plates close leads to gigantism. Too much during adulthood, called acromegaly, causes the hands, feet and face to enlarge.
• Thyroid stimulating hormone
Also called thyrotropin. This causes the thyroid gland to release thyroid hormones. A pituitary tumor producing TSH leads to
hyperthyroidism, whose symptoms include rapid heart rate and makes patients hyperactive and shaky.
• Adrenocorticotropin hormone
Also called corticotropin. This stimulates the adrenal glands to produce too much cortisol, a steroid hormone. This leads to rapid weight gain, high blood pressure and diabetes.
• Luteinizing hormone and folliclestimulating hormone
In women these hormones work on the ovaries, affecting the release of eggs and production of estrogen and progesterone. In men these hormones affect the testicles controlling testosterone production and sperm production.
• Prolactin
Too much can make both women and men produce milk and can affect fertility.
The posterior portion of the pituitary stores and releases hormones made in the adjacent brain region called the hypothalamus:
• Vasopressin
Also called antidiuretic hormone. This affects the ability of the kidney to concentrate urine and retain or excrete fluid. When ADH is too low, patients urinate too much and become dehydrated. This is called diabetes insipidus, a totally distinct condition from diabetes mellitus which raises the blood sugar.
• Oxytocin stimulates uterine contractions in childbirth and lactation after childbirth.
As you can see, the pituitary is a
busy and complex gland!
Most pituitary tumors are not cancerous. And most arise from the anterior, rather than the posterior, pituitary. Despite not being cancerous, pituitary tumors can be troublesome. They can enlarge to invade nearby structures. There is not much space for a pituitary tumor to grow. Symptoms due to enlarging pituitary tumors include vision problems due to optic nerve compression, headaches or damage to the sinuses.
Pituitary tumors are further classified by size. Microadenomas are less than 1 cm. (1/2 inch.) They rarely become large enough to damage adjacent structures but can
nesses?
cause trouble if they secrete any of the hormones described above.
Microadenomas that stay small and don’t secrete hormones are often never found or are found only incidentally when a test like a brain MRI is done for some other reasons.
Macroadenomas
work and imaging such as MRI.
Treatment could include surgery, radiation or medication.
Pituitary tumors are actually very common, occurring in perhaps 10% -20% of people over their lifetime. But pituitary tumors that cause symptoms are far less common. I wasn’t able to find that figure.
From a surge in RSV cases to COVID and the flu, the news headlines can feel overwhelming. Excellus BlueCross BlueShield’s physician Lisa Y. Harris has answers to common questions about RSV and staying healthy this winter.
Q: We are hearing a lot in the news about respiratory syncytial virus — or RSV — and how cases are soaring. What is RSV and who should be worried about it?
A.: RSV is a respiratory virus that usually causes mild cold-like symptoms in otherwise healthy children and adults. While this virus is commonly associated with infants or young children, the Centers for Disease Control [CDC] reports anywhere from 60,000 to 120,000 older adults in the United States are hospitalized with RSV each year. For older adults with chronic heart or lung disease
— or those with weakened immune systems — RSV can be fatal if it turns into bronchiolitis (lung inflammation) or pneumonia (lung infection).
Q: What are the symptoms of RSV and how does someone know if they need to see a doctor?
A.: Early symptoms of RSV include a runny nose, loss of appetite, a cough which may include wheezing, and sometimes a fever. RSV can make conditions like asthma, COPD, and congestive heart failure worse. You’ll want to see a doctor immediately if you begin to have problems breathing. Also, if after a couple of days your symptoms are getting worse instead of better, you should see your doctor.
Q: We are also hearing a lot about the flu, and we know COVID-19 is still around. What is the latest on those ill-
A.: We are in flu season from November until at least February. The flu can be serious especially in older adults, young children, pregnant women, and nursing home residents. The CDC recommends the flu vaccine for everyone 6 months and older. This will help protect you as well as anyone who is particularly vulnerable. And while COVID cases are down, you should stay up to date on vaccines to help prevent a more serious infection if exposed. Talk to your doctor if you have questions about which vaccine is best for you. The good news is getting a flu vaccine or COVID booster is as simple as stopping by your local pharmacy. Visit vaccines.gov to find a vaccination site near you.
Q: What’s your best advice for everyone on staying healthy this winter?
A.: Stay up to date on your vaccinations. Even if you do get sick, being vaccinated can help keep your symptoms mild. Make sure you wash your hands often for 20 seconds with soap and warm water. Frequently use hand sanitizer when out at the grocery store — maybe carry a sanitizer in your purse or car, too. Many people are choosing to continue to wear masks in public or in large gatherings to help protect themselves and others — this is a great idea especially if you
Physician Lisa Y. Harris is vice president of medical affairs at Excellus BlueCross BlueShield. She is a fellow of the American College of Physicians, fellow of the American Academy of Pediatrics and a certified physician executive through the American Association of Physician Leaders. Board certified in internal medicine and pediatrics, Harris has been in clinical practice since 1995.


have a weaker immune system. Finally, avoid close contact with people who are sick and stay home if you are not feeling well.
Submitted by Excellus BlueCross BlueShield.
can cause symptoms by pressing on nearby structures and may produce excess hormones.
Depending on the symptoms caused by a pituitary tumor, evaluation will include blood
Excellus BlueCross BlueShield doctor talks about the prevalence of respiratory syncytial virus and how to stay healthy this winter
Disease Care, Research and Education Program, which has participated in more than 200 clinical studies for Alzheimer’s since 1986, including lecanemab.
“This is one of the largest clinical trials in Alzheimer’s disease and was unique in that it had higher participation of historically underrepresented groups than in previous studies,” Porsteinsson said in a statement. “It also allowed volunteers with more medical comorbidities to enter the study. Usually, participant populations in studies like these are healthy, so this created a more representative sample of the Alzheimer’s population in the real world.”
Among participants not receiving the placebo, 12.5% experienced mild to moderate brain swelling, but it was rarely clinically evident and resolved when medication was halted. The group also experienced micro hemorrhages, which are common among Alzheimer’s patients, but these were monitored carefully.
ic pain. Neuromodulation is the next step, according to physician Hemant Kalia, interventional pain and cancer rehabilitation specialist and managing director of Greater Rochester Region InvisionHealth and medical director of Invision Spine & Pain in Rochester.
“It’s a specialized field of pain medicine where we deliver medications and also electric energy to central nervous system or to nerves to modulate the pain signal, which can help improve their function and quality of life,” Kalia said.
It involves implanting small devices around the nerves to block pain signals from the damage nerves. For example, people with chronic low back or leg pain. Although this modality is not new, the devices will use artificial intelligence so that they can learn and optimize their effect to meet patients’ needs.
By Deborah Jeanne SergeantThe year 2023 should prove a banner year in medicine. Area experts share a few of the big advances they expect soon.
Lecanemab, a new Alzheimer’s medication, is expected to pass FDA approval this year. As reported in the New England Journal of Medicine, lecanemab slows cognitive decline
for certain patients with Alzheimer’s by targeting beta amyloid, the cause of plaques in the brain that are thought to contribute to the disease.
Patients in the early stages of the disease receiving the IV medication experienced slower decline in cognition and function. The study looked at 1,800 patients for 18 months.
Physician Anton Pjetur Porsteinsson leads URMC’s Alzheimer’s
“Alzheimer’s is a very complex, multi-modal disease that varies from person to person,” Porsteinsson said. “This is also a disease where the changes in the brain start maybe 20 to 25 years before you have any clinical symptoms. By the time someone presents with symptoms they are actually very late in the overall disease course.”
He recognizes that lecanemab is only a start towards a cure, but one that may become someday part of a “cocktail” of prescriptions used to treat Alzheimer’s.
Final approval by the FDA may happen by September 2023.
The current opioid epidemic has pushed researchers to find other ways to help patients manage chron-
“Currently, the devices available to us we can’t program them individually to a specific patient’s needs,” Kalia said. “Every patient’s needs are different. With these new platforms, we’ll be able to individualize the pain management.”
The closed loop stimulation in the new platforms will be able to automatically interpret changes in activity and adjust the output without manual control.
Kalia anticipates FDA approval in 2023.

“We are also exploring other non-opioid based medications, which can be delivered directly into the spine as opposed to the oral route of administration,” he added.
This would minimize systemic side effects because physicians would deliver the medication directly to the site of the pain receptors.

Scan the code to learn why you’ll love joining the HOA nursing team!

Among new developments, 2023 should bring better chronic pain management, a new Alzheimer’s drug
– Lisa Clemmons, RN, BSN, OCN
“The ongoing relationships I am able to build with my patients at HOA are very special to me. Our patients and dedicated team members keep me coming back to work each day!”
Smaller hospitals in Upstate New York transfer about 8,000 patients a year to larger hospitals, mainly in Syracuse. A grant from Upstate Foundation will help ambulance companies transfers these patients more efficiently
By Norah MachiaAcross New York State, first responders are traveling greater distances to transfer critically ill patients from community hospitals to those offering higher levels of care.
That includes ambulance services from the many counties surrounding Upstate Medical University in Syracuse, which receives approximately 8,000 patient transfers a year.
But the COVID-19 pandemic, which resulted in staffing shortages throughout the region, has made it increasingly difficult for community hospitals to help support these transports. Hospitals often provide staff to accompany critically ill patients on ambulance transfers or lend specialized medical equipment needed to care for the patient during the transport.
For example, a patient on a ventilator needing an ambulance transfer would typically have to
be accompanied by a respiratory therapist, or a patient being managed with medicine infusions would usually need a registered nurse in the ambulance. Depending on the weather and the distance traveled, these hospital employees may be gone for hours.

“We’re seeing more critically ill patients from community hospitals traveling greater distances in these ambulances because tertiary hospitals are often filled to capacity,” said Douglas Sandbrook, the EMS liaison for Upstate Medical University, and director of EMS Education. “We try to keep people local, but the reality is there are finite number of beds.”
When those beds reserved for critically ill patients at Upstate are filled, ambulances transporting patients must be diverted to the next closest tertiary hospital.
To help address the situation, a new fund was established at the Upstate Foundation to assist ambulance services become more
independent in the transportation of critically ill patients to Syracuse area hospitals and other facilities outside of Central New York.

A total of $35,000 in critical care transport grants was recently awarded to the following ambulance services: $12,500 each to Menter Ambulance in Oswego County and Guilfoyle Ambulance in Watertown, and $10,000 for the Gouverneur Rescue Squad.

The funding will help expand training for paramedics to provide the same level of care for patients inside their ambulances as those patients would receive in a hospital’s intensive care unit, said Sandbrook.

Ambulance services may also use the grant funding toward the purchase of specialized equipment, such as ventilators or IV infusion pumps, eliminating the need to borrow that equipment from community hospitals. Transport ventilators cost as much as $15,000, while IV infusion pumps cost approximately $2,000 each, he said.
“We identified these areas of need when speaking with ambulance services throughout Central and Northern New York,” said Sandbrook. The special fund at the Upstate Foundation was set up specifically to enhance existing or develop new critical care transport services.
Upstate Medical University “wanted to help these agencies build their own resources and give them the additional training to independently manage the patients during the transports,” said Sandbrook.
Menter Ambulance has transported critical care patients from Oswego County to tertiary hospitals in Syracuse for years, but the hospital staffing shortages resulting from the COVID-19 pandemic prompted the organization to further develop its critical care transport service, said Joseph Provost, public information officer at Menter Ambulance.
The private ambulance service has six paramedics on staff who have earned the critical care paramedic or the flight paramedic designations, and plans another critical care training program in the future for a new group of paramedics, he said.
“Oswego County has a strong health care system, but not all patients can be treated at a community hospital,” said Provost.

“The COVID-19 pandemic has shown that is not practical for community hospitals, such as Oswego Hospital, to spare the necessary staff needed to accompany these patients.”
Prior to the COVID-19 pandemic, the majority of patient transfers from Oswego Hospital were to Syracuse, approximately 40 miles away. Since the pandemic, the ambulance service has been transporting patients to destinations farther away, such as Rochester and Albany, he said. These transports have taken staff away from the hospital for several hours at a time.
The Upstate Foundation grant will allow Menter Ambulance to provide the additional training for paramedics, and will also be used toward the purchase of specialized medical equipment. The ambulance service is working toward outfitting a new vehicle with items such as a ventilator, medical infusion pump and ultrasound machine.
This type of equipment would allow the critical care transport team “to be completely self-sufficient in providing transfer services to patients at Oswego Hospital, without the need of additional hospital staff to accompany these patients during transport,” said Provost.
For many years, “the primary transport method of critically ill or injured patients from Oswego Hospital to the regional centers in Syracuse was dependent almost exclusively on air transport,” he added. But that service is not always available, especially during the winter months when poor weather conditions make it difficult for these flights to take off.
For information about supporting this new fund at the Upstate Foundation, visit www. upstatefoundation.org.






Whether you’ve had a bad day, a painful break-up or a normal day dogged by the chills, we all have comfort foods that we turn to when we need some extra TLC.
They could be dishes that are creamy and warm, or recipes that mom used to make, or simply foods that cheer us up!
But which foods are considered comforting can be vastly different based on where you live, what your sex is, and how old you are.
According to the Harris Poll, an American research company that has been tracking the behaviors of American adults since l963, America’s favorite comfort food is…pizza!

Pizza?
Frankly, I thought pizza was America’s all-time favorite food, no matter the need for comfort; but apparently it’s our go-to comfort food, as well.
When we’re not reaching for pizza, Harris noted, we’re getting our culinary hugs from chocolate, ice cream, mac and cheese, chips and hamburgers.
Another research company, which broke down Americans’ favorite comfort foods by state, begged to differ. Basing their study on comfort recipes with the highest Google search volume, the lighting retailer e-conolight revealed that grilled cheese was the most popular comfort food overall and chosen as the top pick in six states: California, Illinois, Maryland, New Jersey, New York and Virginia. Fried chicken was the second most-searched comfort food, winning out in Delaware, Georgia, Louisiana and Texas, followed closely by chicken and waffles, chili and pot roast.
A few unconventional favorites? Iowa’s monkey bread and Tennessee’s chess pie.
Comfort food cravings differ between the sexes. In a study published in the “Physiology & Behavior” journal, researchers from the University of Illinois Food and Brand Lab concluded that “a person’s comfort-food preferences are formed at an early age and are triggered, in addition to hunger, by conditioned associations and gender differences.”
The study illuminated that while men find comfort in foods associated with meals prepared by their mothers (mashed potatoes, pasta, meat and soup) women find comfort from less labor-intensive foods (chocolate, ice cream and candy).
Put another way, what is comfort for men is work for women. Me? I scream for ice cream and so did my mom. My husband? Pasta and stew will only do.
Age also affects our comfort-food leanings. Research shows that younger people preferred more snack-related comfort foods compared to those older than 55. And that folks older
than 70 will take steak and potatoes over pizza any day!
In addition, the time of year affects our cravings, with winter months rousing our need for comfort foods most. Some researchers suspect fewer daylight hours may play a significant role. Since sunlight promotes the release of serotonin, a known mood-booster, and we’re getting less of it during the winter months, we’re more inclined to reach for foods that also prompt the release of serotonin: carbohydrates.
Other studies, however, suggest that nothing more than “feeling cooped up” is what’s sending us straight into the arms of serotonin-boosting comfort foods. Our family can certainly relate to that! When cabin fever strikes our house, we consume more popcorn, pasta, chips and bread than at any other time of year.
Of course, there can be consequences to easing the winter blues with food, especially if those foods involve comfort foods that run higher in calories, fats and carbs. On average, say researchers at Johns Hopkins University, we tend to gain five to seven pounds during winter months due to increased calorie intake. Weight gain aside, many comfort foods are not all that healthy to chow down on a regular basis, from salty chips to high-fat ice cream to refined-flour breads and pizza.
How to cope during the long winter months when the urge to devour the entire casserole is besting your better instincts? Experts weigh in with some helpful tips to keep you on track.
• Let in the light
Early morning light is the most potent energy booster, so open those curtains and take an early morning walk. As mentioned, sunshine increases serotonin levels, which may help calm your food cravings. Also, consider changing your light bulbs to bright, full-spectrum bulbs that mimic bright summer sunlight.
• Keep moving
When it’s chilly outside, the desire to become one with the couch is monumental. But, all agree, staying active during cooler months is key to controlling weight, whether you walk with friends, head to the gym or work out with someone online. A new study, published in the journal Health Psychology, found that physical activity helps to suppress your appetite and boost your mood.
• Fill up first
Oh, those tempting party spreads full of warm, comforting food! Don’t
you just want to eat everything in sight? One way to manage intake is to fill up before you head out. Nutritionists recommend eating high-fiber foods, such as fruits and veggies that take longer to digest, and drinking a big glass of water. Same holds true for other outings and events where temptations abound: grocery shopping, dining out, food festivals, and Sunday football.
• Get plenty of ZZZs
Ever notice how hungry you feel after a poor night’s sleep? Or how strong your cravings are for certain foods like pancakes and donuts? It’s not your imagination. Studies show that even a single night of poor sleep changes your hunger and appetite hormones, leading to increased hunger and an uptick in calories consumed. When people got more sleep, researchers found, they were not only less hungry during the day; they were less likely to reach for sweet and salty foods.
• Give comfort foods a makeover Whether warm and gooey or rich and sweet, many comfort foods are not so comforting when it comes to calories, fats, sodium, and nutrition. But here’s the good news: it’s relatively easy to turn these diet-busters into healthier dishes without sacrificing taste. A few swaps to consider: substitute evaporated skim milk for cream, lower-fat ground turkey for ground beef, baked chicken for fried chicken, whole-wheat pasta (or veggies) for refined-wheat pasta, and low-fat plain yogurt for mayonnaise.

Adapted from skinnytaste.com 6 servings (250 calories each)
1 large head cauliflower, cut into 1-inch florets
1 tablespoon butter
2 teaspoons olive oil
½ cup diced onion
3 tablespoons whole-wheat flour
¼ cup water
2 cups 1% or 2% milk
1½ teaspoons Dijon mustard
1-2 teaspoons hot sauce (optional)
2 cups shredded reduced-fat cheese of choice, divided 1 teaspoon salt
½ teaspoon coarse black pepper ¼ teaspoon garlic powder (or more)
½ cup whole-wheat panko breadcrumbs
Preheat oven to 375ºF. Lightly oil a 9 x 13” baking dish.
Fill a large pot with enough water to cover the bottom about 1 inch; season with salt; bring to a boil. Add the cauliflower, reduce to a simmer, and cover; cook until tender crisp, 6 to 7 minutes. Drain, pat between paper towels to dry, and transfer to the baking dish.
Heat butter and oil in a medium saucepan over medium-low heat. Add onions and cook about 3 minutes. Stir in flour and water, then reduce heat to low and cook, stirring continually, for 1 minute more.
Raise the heat to medium, then gradually whisk in the milk, mustard and hot sauce until combined and smooth. Lower heat and continue cooking, stirring throughout, until it becomes thick, about 5-6 minutes more. Remove from heat and stir in 1½ cups of the shredded cheese (¼ cup at a time), along with the salt, pepper, and garlic powder. Mix well, then pour over the cauliflower and gently stir to combine.
Top with breadcrumbs and remaining ½ cup cheese; bake until bubbly and golden, about 15 to 20 minutes. Switch to broil for 2-3 minutes to brown the top.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

Manufacturers make all kinds of health claims, but can taking a dietary supplement actually lower your heart disease risk?
A comprehensive analysis of prior research suggests that in certain cases the answer is yes. Some types of supplements — such as omega-3 fatty acids, folic acid and coenzyme Q10 (CoQ10) do provide a cardiovascular leg up.
But many supplements were found to offer no heart health benefit of any kind, and others were potentially harmful.
“We evaluated 27 different types of supplements, and found that there are several that offered cardiovascular benefits,” said study author physician Simin Liu, director of the Center for Global Cardiometabolic Health at Brown University in Providence, Rhode Island.
These included omega-3 fatty acids, which reduced the risk of early death due to heart disease.
Other supplements that were shown to benefit the heart included folic acid, L-arginine, L-citrul-

line, Vitamin D, magnesium, zinc, alpha-lipoic acid, melatonin, catechin, curcumin, flavanol, genistein and quercetin.
But some common supplements had no long-term effect on heart disease outcomes or risk for Type 2 diabetes, Liu noted. They included vitamins C, D, E and selenium.
Beta carotene supplements, meanwhile, were associated with an increase in early death from all causes.
The findings are an outgrowth of a research review prompted by what Liu and his colleagues described as lingering confusion in the heart health community as to just how effective supplements can be at preventing heart disease.
The fact that foods rich in micronutrients can protect the heart has not been in question, said Liu, who noted that several large studies have linked a healthy diet to heart health benefits.
For example, micronutrients like antioxidants — which are present in the heart-healthy foods featured in
the “Mediterranean diet” and DASH (“Dietary Approach to Stop Hypertension”) — have long been linked to a reduction in oxidative stress. Because cell tissue damage brought on by such stress poses a threat to heart health, antioxidant-rich diets are thought to be protective, reducing the risk for a number of serious diseases, including diabetes.
What’s been less clear, however, is whether consuming vitamins, minerals, phytochemicals and antioxidants in the form of supplements might offer a similar advantage.
For the new study, Liu’s team poured through 884 prior studies
of supplements, some published as recently as this year. Collectively, the studies involved nearly 900,000 men and women.
In the end, the team concluded that some of the 27 micronutrient supplements under review did demonstrate some benefit.
Those included a number of omega-3 fatty acid supplements – including n-3 and n-6 fatty acids— which were found to help to reduce the risk for heart attacks and coronary heart disease, as well as the overall risk for dying as a result of heart disease.
maintain heart health,” Wulandari said in an ESC news release.
Previous research had shown that women with heart disease received less aggressive treatment compared with men.

For this study, researchers used data from a U.S. federal health and nutrition survey conducted from 2017 to 2020.
It included more than 8,500 men and women between 40 and 79 years of age with no history of heart disease. More than 2,900 were eligible to receive statin drugs because they had an increased risk for heart disease.
ESC guidelines recommend adults of all ages do at least 150 to 300 minutes of moderate intensity or 75 to 150 minutes of vigorous intensity, aerobic physical activity each week.
Diet recommendations emphasize plant-based foods such as whole grains, fruits, vegetables, legumes and nuts, and limiting salt intake to less than 5 grams per day.
Doctors give men and women different advice to head off heart disease, even though guidelines for both are the same.
Men were 20% more likely to be prescribed statins to lower blood levels of bad cholesterol compared with women, a new study found.
Women, meanwhile, were 27% more likely to be advised to lose weight or reduce their salt intake, and 38% more likely to receive recommendations to exercise.
Women were also 11% more likely to be advised to cut fat and calories.
The study findings were presented in December at a meeting in Singapore organized by the European Society of Cardiology (ESC), the Asian Pacific Society of Cardiology and the Asean Federation of Cardiology.
“Following our analysis, we conducted a review of the literature to find possible explanations for the
results. This demonstrated that a potential root of the discrepancy in advice is the misconception that women have a lower risk of cardiovascular disease than men,” said study author, physician Prima Wulandari of Harvard Medical School and Massachusetts General Hospital in Boston.
“Our findings highlight the need for greater awareness among health professionals to ensure that both women and men receive the most up-to-date information on how to
People who are overweight or obese should lose weight to lower blood pressure, lipids and the risk of diabetes, reducing their risk of heart disease, the guidelines say.
Statins are recommended based on individual characteristics, including age and heart disease risk, according to the ESC.
Findings presented at medical meetings are considered preliminary until published in a peer-reviewed journal.
Research shows some supplements have no effect on heart’s health and can even be harmful
Rescue Mission helps the hungry, homeless. CEO says more people in CNY are depending on its services, he identifies the need for low-income, quality affordable housing as main challenge for the community
By Mary Beth RoachQ: Can you explain the work of the Rescue Mission, including some of its programs and initiatives?
A: We are a 135-year-old local community-based nonprofit organization, based in Syracuse, with some programming in Binghamton and Auburn, as well. Our focus is on helping hungry, housing-unstable individuals, people living on the streets, as well as homeless families, women, children and single men.
Q: How many people do you estimate that you serve in a year?
A: In a year, we serve between 9,000 and 10,000 people.
Q: What is your definition of serve — is it meals? Is it shelters?
A: It could be meals, shelter, housing units that we own and operate, employment services, clothing, coats, shoes, socks — whatever somebody might be in need of.
Q: Over the past year, has this number been on the increase, and if so, why do you think that is?
A: I think the numbers have been on the increase for sure in the last year. The additional supports and resources throughout the pandemic that give people maybe more sustainability — those dollars and checks have gone away. I think people are
struggling to make ends meet and then the rising prices of housing in Upstate and Central New York — it all creates a difficult pattern and position for a lot of people that are already living on the margins of society. Luckily, we’ve been able to continue to meet the needs as it grows.
Q: What are your needs for volunteers over the holidays?
A: Our biggest one-day or twoday undertakings are on Thanksgiving Day and Christmas Day. We serve more than 2,000 meals throughout the community. There’s about 300 to 400 more that get served on our campus, but there’s a lot of homebound individuals or elderly. Meals on Wheels isn’t operating on those two holidays. So, we recruit hundreds of volunteers to come to the mission and we give them an assignment with packaged meals ready to go. Then people go all over Onondaga County, dropping off meals before they sit down for their Thanksgiving or Christmas meal. We still need volunteers to help deliver meals. But then also, as we get through the holidays, it would be great to have volunteers show up in January and February. We always need help preparing meals at our food service center, as well as volunteering in different ways, whether
it’s in our clothing outreach program downtown.
Q: What is the best way for interested people to volunteer?
A: The best way is to go to rescuemissionalliance.org and click the volunteer button. Then there’s a prompt where you have to fill out your information. Once you get in our system, we can get you scheduled. There’s a way where you can click on what days and times work best for you.
Q: What do you see as the major challenges that the Rescue Mission faces?
A: I think the biggest challenge that we see you right now, and it’s, I think, only going to grow, is the need for truly low-income, quality affordable housing. Exciting things are happening in Syracuse, Onondaga County and it sounds like new jobs are being created. The housing that’s going to be created for those new jobs is going to be single-family homes or higher-end homes. I think the need for the right kind of housing for our clients that we serve is not being developed currently and there’s no real incentive to develop that kind of housing.
Q: What do you consider some of the strides that the Rescue Mission has made in the last year?
A: I think we have refocused our organization to truly become a housing developer over the next few years. As we look at the climate for the housing need and what our clients need for sustainability and to really achieve their higher level of independence, we need to be the ones to start to create that kind of housing. We’ve started to lay plans and work out a strategy where over the next 15 years, our goal is to develop 150 units of housing that we create, we maintain, we fully staff and our clients can have a safe space that’s quality, that’s dignified. We also know that some clients are little rougher on facilities and they might not fit into your typical apartment complex. We are going to work to create those kinds of spaces, to make people feel like they’ve got a home and it feels like a safe place for them to get back on track.
Q: As we prepare for 2023, what would you like to accomplish this coming year?
A: This coming year we have started the process to put together layers of funding to start to create some of this housing and start to create the building facilities. It’s going to be a multi-year, multi-funding approach. There’s no quick way to create this housing, especially with everybody else trying to build housing for different uses in our community. We’ve got the vision for what’s needed. Now, we’re going to develop and really home in on our strategy, as well as start to put together some of the funding to make it a reality.
TheDepartment of Veterans Affairs recently announced the appoint- ment of Frank Pearson as the new director of the VA San Diego VA Medical Center. Pearson has served as the Syracuse VA Director since June of 2020.

“It has been my great honor and privilege to be part of the Syracuse VA family and I am grateful to have worked with so many professional and dedicated staff. Syracuse is a unique place and I am very thankful for the many opportunities I have had here” said Pearson.
Under Pearson’s leadership the Syracuse VA has been consistently recognized as one of the highest performing Medical Centers in the VA system in the areas of high quality medical outcomes and patient satisfaction.
Pearson earned both his Doctorate and Master of Physical Therapy degrees from Baylor University and a Master of Physician Assistant Studies degree from A.T. Still University’s Arizona School of Health Sciences.
Michael DelDuca, Syracuse VA associate medical center director, will serve as interim director during the search for Pearson’s successor.

“I think we have refocused our organization to truly become a housing developer over the next few years.”
Syracuse VA director selected as new director of the San Diego VA
Dividing their time among work, childcare and household management leaves little time for many women to take care of their own health, including maintaining a healthy weight.
According to a 2019 Gallup poll, women are more likely than men to take care of parental duties and housekeeping including laundry, cleaning, cooking, grocery shopping and dishwashing.
Women are also more often the primary caregiver of other family members such as one who is disabled or a senior parent, and usually manage the family’s social schedule and health appointments.
Homemakers account for some of that division of labor. In 2019, the Bureau of Labor Statistics reported that 57% of women ages 25-64 were employed, compared with 74.4% of men. But especially for women who work full-time, managing their weight often becomes a low priority.
In addition to having many things vying for their time, women’s experiences such as childbirth and conditions such as polycystic ovary syndrome can also contribute to weight gain. Between 5% and 10% of women have PCOS. Women also receive a barrage of mixed—and often incorrect—messages about weight gain, as they try to live up to the cultural ideal of a svelte figure.
Fortunately, losing weight does not require an hour-long workout at the gym every day.
“You need to be active, even if in small bits,” said Paula Pacini group exercise coordinator at the JCC of Syracuse. “When you go to the grocery store, park far away. Go outside to walk bundled up. Do some videos at home. A lot of places offer Zoom classes like we do. The kids may want to do classes with their mom.”
For those that want to try a gym membership, Pacini said it’s a great time to do so as many have special deals in January to reach people who
set New Year’s resolutions.
“We have $1 and a Dream in January to help people burn some of those holiday calories,” Pacini said. “You can try all the classes for $1 each for the month.”
Many women realize the benefits of moving more for cardiovascular health, such as spinning, jogging, and elliptical machine workouts, but neglect resistance exercise. Resistance training can include performing bodyweight exercises like squats, calf raises, planks and push-ups. Fitness bands, free weights, and kettlebells can also help for home resistance training workouts.


“A lot of times women feel that weight training will get them big
and bulky. However, because of the hormones base we have and lack of testosterone compared to men, genetically we would not be able get big and bulky like men do when they weight train,” said Jill Murphy, personal trainer and co-owner of Mission Fitness in Syracuse.
She added that carrying more muscle helps speed up the metabolism and maintain connective tissues.
Julie Mellen, certified diabetes care and education specialist and registered dietitian at Upstate Medical University encourages people to “take 5- to 10-minute breaks” for exercise throughout the day if that works better for them.
It may seem like a series of short
workouts would not help as much as one long workout of 45 to 60 minutes. However, for some people, breaking up the exercise sessions is not only more convenient, but it can also help them workout at their highest level throughout the workout instead of putting forth less exertion as they begin to feel fatigued.
During times of rest, the body recovers from workouts, including becoming stronger.
“Don’t underestimate the importance of sleep and stress management,” Mellen said. “Commit to a sleep schedule and find activities to help unwind and manage stress that do not involve food or drink.”
Of course, the diet plays a big role in weight loss. Yo-yo dieting has been shown to contribute to weight gain. There’s no need to buy only expensive diet foods or premade entrees. Many of these are full of added salt, sugar and preservatives. Instead, Mellen encourages women to “shop the perimeter of the grocery store. Limit sweet drinks and alcoholic drinks, drink more water or seltzer. Read labels, check serving sizes and be calorie aware.”
She likes the USDA’s My Plate plan, which states that half the plate should hold fruits and non-starchy vegetables, one-quarter should have a lean source of protein and one-quarter should have a carbohydrate source. Three servings of dairy per day, such as yogurt and milk, can ensure adequate calcium and provide more protein.
“Reduce the refined grains— white bread, white flour, white rice, added sugars—and transition to more whole grains,” Mellen said. “Snack on fiber rich fruits and vegetables. Strive for five servings of fruits and vegetables daily. Increase lean protein and incorporate a little protein with each meal and snack.”
A healthful diet includes mostly whole foods such as whole fruit, raw vegetables and whole grains instead of numerous examples processed foods with added sugar, salt and fat. Unhealthful sources of fat are solid at room temperature, such as butter, margarine, shortening and lard.
Plant-based sources of fat in moderation are more healthful, including canola oil and olive oil.
Laurel Sterling, registered dietitian, nutritionist and educator for Carlson Laboratories in Canastota, likes to start the day with a breakfast rich in healthful fat, protein and vegetables, such as an omelet with veggies, a piece of fruit and coffee or tea.


“A protein drink or bar, a small handful of almonds, or a hardboiled egg, or fruit would be some wonderful options,” Sterling said.
Controlling caloric intake relies upon paying attention to the body’s need for nutrients, what Sterling calls “our hunger and satiety cues” with which many people have become out of touch.
“Mindless eating is commonplace now, but can be changed,” she said. “Be in the moment when you are eating, along with enjoying the great company and wonderful atmosphere. Remember to eat slowly, savor each bite and put your fork down occasionally. This way you will eat less.”
Being a parent means experiencing many contradictory things at once. Parenting is both beautiful and scary. Miraculous and redundant. Exhausting and exhilarating. Silly and serious. Pure and gross.
The experience of parenting has almost as many contradictions as there are antonyms in the English language.
However, I can think of at least one thing about parenting that never contradicts itself.
Parenting is incredibly hard. It’s never easy. Granted, loving your children is easy, but parenting them is different.
As a parent, I am literally cultivating another human being. It’s a tremendous and beautiful opportunity, but it has never been easy.
As difficult things often go, I have messed up parenting up so many times. There have been times, in moments of exhaustion or personal weakness, where I have failed my children in very real ways. I want to think that my failures haven’t been catastrophic in nature. I hope I have not salted the Earth where I am tending my children. But, on the hard days, I’m not certain.
So, in light of a new and beautiful year, I’m going to leave the tradition of resolutions at the threshold of 2023. Resolutions are easy to make and easy to break. They don’t teach me much, as they often leave me feeling disappointed in myself.
Instead of making resolutions, I want to start this year off on a note of self reflection and self empathy. So, I’m starting a new tradition. I’m writing a letter to myself to come to grips with the failures of 2022. Perhaps, this exercise will encourage me to offer myself more grace. Perhaps that grace will make a better mother.
As 2022 falls into the rearview mirror, here are some words of encouragement for me.
Dear me,
It’s now 2023. Isn’t that beautiful? I know you’ve been working a lot on yourself as a parent and partner to your husband. I also know that you hold yourself to high standards and beat yourself up when you make mistakes.
There have been so many, haven’t there? Mistakes you wish you could take back. Mistakes you often use to define yourself. There are the things you’ve said to your kids; things you haven’t said to your kids; things you’ve done to or around your kids; and things you should have done but failed to do.
When you see other parents failing, you react with empathy. You say things like, “Almost every parent is doing the best they can for their children, given the circumstances and abilities of that parent.” Why don’t you think that also applies to you?
This year, I challenge you to be and think differently. You don’t define other people by their failures and you should give yourself the same grace.
Next time you want to jump down a self-doubt rabbit hole, try asking yourself this: how many of your failures have caused your beloved children lasting harm? Have you caused the type of harm that makes another person grow away from themselves? Have you hurt your kids in a way that makes them stop believing in the good in themselves or their own value?

Momma, you know you haven’t. You have failed in many small ways. But even then, you were teaching your children things. You’ve shown your children superheroes aren’t always super. You’ve shown them one can recover from mistakes and misdeeds. You’ve shown them one can mess up (or be a total mess) and still be loved.
You’ve shown them beautiful people know how to fail and grow, then fail and grow again.
Learning how to recover from failures is perhaps one the most important things a parent can teach a child. The only way to teach this lesson is to show them this lesson—to live this wisdom.
Perhaps hearing their mother say, “I’m sorry I yelled at you and made you feel ashamed. I let my anger win. That wasn’t right. I will try to do better in the future. I love you forever,” will grow their emotional intelligence in a different way than your good deeds do—not a better way, but an equally important way.

Maybe when you show them we are all hopelessly flawed, they will be more likely to believe they are loved in spite of their flaws. Maybe they will bring their whole selves to you as they continue to grow.
Keep failing and growing.
Love yourself, Melissa
Writing that little note to myself was heavy. Much like parenting, it wasn’t easy. But, it felt good. It felt like a better way to kick off a new year than making a bunch of resolutions. This felt more productive.
I invite my fellow parents to try this approach. It’s OK to abandon resolutions and make way for a more positive and productive tradition. If you could write a letter to something you want to let go, what would you write to? If you were to write a letter to something positive, what would you embrace in 2023?
The truth is, all parents are fighting
hard battles with themselves. Most of us want to be the most amazing people we can for the sake of our children. When you love your kids like crazy, no amount of love or effort can seem good enough.
But, beautiful parent, I assure you of this: you can keep failing and growing and still be more than good enough. If you keep growing and showing humility to yourself and others, your kids will grow into the sorts of humans you always wished they would be.
Here’s to embracing failure and growth in 2023.
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS 100 Rochester St. Fulton, NY 13069 315-598-4700
Females ranked higher than males regarding times they feel stressed, according to a recent Gallup World Poll.
The results aren’t surprising considering the numerous effects of the pandemic that unduly burden women such as changes in their children’s education, supply chain problems, health concerns, all areas in which women typically perform more work than men.
Too much stress is not good for anyone.
In addition to the negative emotional aspects of too much stress, it also contributes to numerous disease processes.
“Women’s lives are so busy, and in addition to career and family, we often find ourselves in multiple nurturing and caregiver situations, which can add additional burdens,” said Renee Hagar-Smith, mindfulness-based wellness coach, speaker, workshop facilitator in Manlius.

Getting rid of stress would not be possible—or desirable, as even positive circumstances produce a certain amount of stress, such as going on vacation, receiving a promotion or adding a new baby to the family. But whether positive or negative sourced stress, mitigating its effects is important.

“Because we often put ourselves last on the list of priorities, adding consistent self-care practices is essential to cultivating more balance and joy into our lives,” Hagar-Smith said.
She encourages women to add small bits of self-care, which is easier to do—and stick with—than to add larger practices like a day at a spa.
Morning and evening routines can offer a good time to include self-care and Hagar-Smith said that it can be grounding.
“Some ways to add self-care into your morning or evening routine is to take a short mindful walk, spend five minutes free-write journaling, or incorporate some time focusing on your breath,” she said. “A few minutes of breathing with a simple four-count inhale and four-count exhale can have an immediate calming effect on your mind and body. If you are feeling extra stressed, try lengthening the exhale to a count of seven. Longer exhales allow you to release more tension and relax your nervous system.”
The body-mind connection is also behind why exercise can help lower stress.
Paula Pacini group exercise coordinator of the JCC of Syracuse, encourages women to de-stress through yoga and tai chi.
“We have both of these classes, and they are very calming,” she said.
One of the reasons exercise works so well is that it releases endorphins, hormones that induce a positive mood. Exercise can include meeting up with a friend for mall walking and catching up, joining a group class brimming with camaraderie or enjoying the outdoors while snowshoeing at a park. Companionship, fresh air and sunshine: all of these aspects of the activity help manage stress.
“One of the ways I always tell my clients on how to de-stress is by completing exercise,” said Jill Murphy, personal trainer and co-owner
of Mission Fitness in Syracuse. “It’s a win-win.”
Eating a healthful, balanced diet comprised of whole foods and laying off the alcohol and processed foods can help reduce stress on the body and support good health. Sometimes stress can manifest in an unhealthful diet, such as emotional eating.
Exercise is part of self-care, as are physical treats such as those listed by April L. Cacciatori, licensed massage therapist, wellness coach and owner of Zensations Therapeutic Massage in Rome.
“Get a massage,” she said. “Try a long, warm bath. Light a candle and listen to music.”
Stress can include chaos in the environment such as a perpetually messy closet or room or even the entire house. Cacciatori said that getting rid of unnecessary things and organizing can create a lower-stress home.

In a similar sense, reducing “clutter” activities—things they do not have to do but that take up time— can help women reduce stress.
“What can I take off my plate?” Cacciatori said. “Can I delegate? This is where I found life coaching so helpful. Let go of the ‘proving syndrome’ where asking for help is a sign of weakness.”
Oftentimes, stress results from taking on too many responsibilities. Instead of insisting on doing it all, delegating can help change a to-do list to an “all done” list. Asking for help can also relate to asking for mental health help, whether the listening ear of a wise, caring friend or a professional, who can help navigate through the reasons behind why some circumstances seem inordinately stressful.
Cacciatori said that in acute moments of stress, taking a few moments to breathe deeply can help manage stress.
“Allow yourself the ability to let go, even if it’s short-term,” Cacciatori added. “Fear creates stress of what’s coming and not coming. We think we’re in control and we’re not. The only thing we can control is how we react and respond.”
If you want to look up to three years younger, facial yoga may be the answer.
Purported to tone the facial muscles and provide facial rejuvenation, facial yoga involves following a regimen of facial movements and poses to provide results.
Gary Sikorski, founder of the Happy Face Yoga method (happyface.com) in Cleveland, Ohio, has been training adherents in the practice since 2006.

“The Effects of Facial Exercise on the Appearance of Aging,” a small study by Northwestern University Medicine published in JAMA Dermatology in 2018, demonstrated that a 30-minute daily then alternate-day facial exercise program for 20 weeks helped middle-aged women improve their fullness of their upper and lower cheeks.
“I’m the first person to medically prove my techniques work,” Sikorski said. “I teach muscle resistance facial exercise. There are 57 muscles in the face, neck and scalp. As you strengthen those muscles, that’s what helps
bring a more youthful appearance as it lifts the cheeks and strengthens the jawline. Also, it can improve blood circulation to improve the complexion. As those muscles are lifted and toned instead of sagging, it tightens the skin which helps soften those fine lines. It’s all these things that add to aging.”
He eschews gadgets advertised online as he believes these are ineffective because they don’t strengthen the muscles, although they can stimulate blood circulation.
“That helps with brightness, but it won’t tone the face, so they don’t offer lasting results,” Sikorski added. “Some just do stretching, which won’t add a youthful look to the face.”
His program uses the fingers,
hands and, for resistance, the teeth.
One of the criticisms of face yoga is that repeatedly making the same facial expressions will cause wrinkles. However, Sikorski said that in 16 years, no one has complained about wrinkles forming from following his program.
He said that how quickly adherents see results depends upon the condition of their face initially and their age. Factors such as smoking, drinking alcohol, lack of sun protection and poor diet can affect the skin also. Those following the program should perform the exercises daily for six-10 weeks.
“The more exercises you do, the faster and better the results,” Sikorski said. “Once you achieve the maximum success, then maybe one or two times for 20 minutes per week.”
He likened the effects to people who work out at a gym. Stopping the workouts will mean lower muscle tone.
“As we age, facial muscles weaken and begin to sag,” Sikorski said. “Weakened muscles will cause many aging problems in the face. These problems can be corrected, or for younger people, prevented, by practicing facial exercise.”

These include eyes that appear narrow, sagging cheeks, downturned corners to the mouth, jawline jowls and pouches.
Calling it face “yoga” is not entirely inaccurate, since yoga involves breathing exercises and a meditative, spiritual element.
Ramsey Farah, dermatologist with Farah Dermatology & Cosmetics in Syracuse, said that the small amount of research available on face yoga suggests it may be helpful. However, most of the studies are not long-term nor of a large enough size to appear conclusive. Still, he can see some merit to the notion of strengthening facial muscles.
“One of the ways you could look at it is working out your facial muscles,” Farah said. “What happens when you do resistance is your muscles grow. Look at body builders. In a similar principle, that’s what is supposed to happen. The muscles
work against the resistance provided by your fingers.”
But he also said that it’s a lot of work to spend building facial muscle every day. The results are also likely varied by the initial damage, age, consistency of the workouts and diet. Most skin damage comes from sun damage, smoking, pollution, consuming too much sugar and alcohol and skimping on water. People can control most of those factors to improve their skin’s appearance.
“Sunscreen and sun avoidance are number one for protecting your skin,” Farah said. “A good product regimen can affect the appearance of aging. Just like you brush your teeth every day, a sunscreen and product regimen is a must.”
Skin care topical product, mild procedures like hydro-facials and facials and skin rollers affect the appearance of the outer layers of the skin. No non-invasive procedures affect the deeper components of the skin.
• The Cheek Lifter: Open your mouth to form an “O” and fold your upper lip over your teeth. Smile to lift cheek muscles up, then put your fingers on the top part of the cheek before releasing the cheek muscles to lower them. Lift the cheeks back up and repeat by lowering and lifting 10 times.
• Happy Cheeks Sculpting: Smile without showing your teeth. Purse your lips together and then smile — forcing the cheek muscles up. Place your fingers on the corners of the mouth and slide them up to the top of the cheeks, holding for 20 seconds.
• The Eyebrow Lifter: Press three fingertips under each eyebrow to force your eyes open. Smile while trying to push your eyebrows down against your fingers. Close your eyes and roll your eyeballs up to the top of your head, holding for 20 seconds.
Makeup techniques can go a long way toward fine-tuning your features to make you look younger. So give these a try.
•
To make your eyes look bigger, line the inside of your lower lid with a white or flesh-colored eyeliner. Then brighten up your eye area by dabbing pale pink, flesh, or oyster color shadow to the inside corners of your eyes. Also, add a couple of more dabs just under your lower lashes moving from the inner corner of your eye to the center.
For your lashes, flare them. First, brush through your lashes as usual with mascara. Then sweep through them again and pull your outer lashes outward and inner lashes inward. Repeat these steps with your lower lashes.
• Youthful lips
Full lips make you look younger. So invest in a quality, long-lasting lip liner, and line your top and bottom lip. For fuller lips, line just to the outside of your lip line.
• A flawless complexion Foundation can do wonders to give you flawless, youthful-looking skin. But your skin type and age may dictate what type works best. On younger skin, sheer coverage is best. On mature skin, foundation can make your lines
more noticeable. So look opt for a sheer, very lightweight foundation or skip it altogether.
• Avoid the dry look
Unless you have very oily skin, skip the face powder because it can make your skin look dry and any lines more noticeable. If you must use powder to control too much shine, apply it only in your oily areas. Also, look for a translucent pure silica formulation and avoid mica or talc.
• Add some color
Use soft pink or bright coral blush to add color and brighten your face. Avoid bronze tones, which only serve to age your skin. Also, use cream rather than powder blush since powder makes your skin look dryer. Apply blush along the top of your cheekbones, forehead, and center of your chin.
Regardless of how gracefully we want to handle aging, we often find ourselves making heroic efforts to stave it off, starting in early adulthood.
The proof is that women of all ages (even in their 20s) are spending small fortunes on Botox injections, fillers and plastic surgery. Also, many who don’t go to such drastic measures still spend hundreds of dollars a year on anti-aging lotions and potions.
Fortunately, you don’t have to undergo risky and costly injections and surgery or resort to ineffective concoctions to enjoy a more youthful appearance.
Your clothing can either add years or subtract them from your appearance. Consider the following tricks to make clothing work in your favor.
• Out with the black
If you’re over 35, banish black above your waist. As you age, black draws attention to your fine lines. For tops and jackets, wear colors that compliment you. Everyone looks great in particular colors. So play those up. This also goes for black-framed eyeglasses. Opt instead for metallics, bright colors, or lighter colored frames.
• Keep it stylish, but don’t overdo it.
As you age, dressing trendy from head to toe is hard to pull off without drawing attention to your age. Instead, mix a pair of classic pants and shirt, with a trendy sweater. Or add style to a pair of jeans and a classic top with a pair of fashionable boots (so long as they aren’t bulky). Another option is to choose pieces that are mostly classic but have a stylish flair.
• Shapers aren’t what they used to be That’s excellent news. At one time, many women wouldn’t be caught dead wearing the hideous shapewear that existed. But lingerie companies have finally gotten the message. You can find shapewear
now that’s both sexy and more comfortable to wear. Shapewear can shave years off your appearance by creating a sleek look.
Physical and emotional wellness goes a long way toward both looking and feeling younger. A positive outlook on life is beneficial to your physical health. In contrast, anger, stress, and depression increase your risk of disease. Negative emotions also reflect in your posture and face. So, make wellness a priority.
Exercise is an essential part of physical and mental wellness and should be a part of your daily routine. A regimen of aerobic exercise for your heart and lungs and weight lifting for muscle tone and bone health will help you maintain your youth longer. As an added benefit, exercise also releases endorphins, which elevates your mood.
So remember good health and a positive attitude have the most significant impact on maintaining a youthful appearance. With these, you’ll glow and emanate radiance.
If you possess diverse interests in medicine and science, working as a nuclear medical technologist might be for you. It also takes a close attention to detail, as these technologists work with radiation.
Each patient only receives the equivalent of radiation received in a CT scan. Nuclear medical technologists “prepare, administer, and measure radioactive isotopes in therapeutic, diagnostic and tracer studies using a variety of radioisotope equipment,” stated the Bureau of Labor Statistics.

In addition, they “prepare stock solutions of radioactive materials and calculate doses to be administered by radiologists; subject patients to radiation; and execute blood volume, red cell survival, and fat absorption studies following standard laboratory techniques.”
Beyond earning a degree in nuclear medicine and completing nine months of clinical work, candidates must also pass a board exam, which then gives them a nationally recognized credential. Solid math and science aptitude can help. In addition, “you need to have that natural feeling of wanting to help someone,” said Logan Aument, nuclear medicine technologist at Oswego Health. “If you do not typically find yourself caring about the wellbeing of strangers, you will most likely not enjoy working in any healthcare field.”
She finds that patience helps, as she must also wait with some patients for hours waiting until test results come back. An easygoing per-
sonality improves the experience.
“Most patients are very nervous when they come in,” Aument said. “If you naturally have a calming demeanor this will benefit both you and the patient. You will be able to reassure them in a calm manner and that will enable them to relax and trust the process easier.”
Aument also thinks that the job also requires the ability to multitask, manage one’s time well and communicate well with the patients and with the rest of the healthcare team.
Despite few people outside the hospital knowing what Aument does, she finds it rewarding work because “you know that you are doing something to help those who are ill.”
The Bureau of Labor Statistics further stated the annual mean wage in the Rochester area is $80,220 (information for the Central New York area wasn’t available). That’s pretty good for a career that requires only a bachelor’s degree. Many schools encourage cross training for other modalities such as CT scanning or MRI. This can help candidates for nuclear medicine technician positions remain nimble in the imagery field and more employable as they would possess more skills to offer.
Only a limited number of schools offer degrees aligning with this career path, one of which is University at Buffalo.
Robert Miletich, chairman of the department of nuclear medicine in the Jacobs School of Medicine and Biomedical Sciences at UB, called the educational requirements “in-
With low or no-carbohydrate diets rising in popularity in recent times, the humble potato is now regularly overlooked in favor of other vegetables.
In fact, research literature has previously indicated potatoes may have a detrimental effect on health, such as possibly increasing the likelihood of developing Type 2 diabetes.
However, new Edith Cowan University (ECU) research has shown while spuds may not have all the same benefits as some other vegetables — such as lowering risk of Type 2 diabetes — health issues associated with potatoes may

actually be due to how people are preparing them and what they’re eating them with.
More than 54,000 people reported their dietary intake for the long-term Danish Diet, Cancer and Health study.
A recent analysis of this study led by physician Nicola Bondonno from ECU’s Nutrition and Health Innovation Research Institute, found people who consumed the most vegetables were 21% less likely to develop Type 2 diabetes than those who consumed the least amount of vegetables.
PhD candidate Pratik Pokharel carried out work on the analysis and
tense” and “very rigorous.” Plus, the required GPA is a B average.
“I did this because I’m a brain scientist,” Miletich said. “What we do in all nuclear medicine is study the physiology of different organ systems. These radiologic drugs mimic molecules already in the body. It’s mostly physiology. I wanted to be able to study the functioning brain non-invasively and there’s no better way than nuclear tags. It’s a very exciting field. The fact that we can do these things in humans and not have to do anything invasively is how we cure diseases. We study the disease itself, not models.”
Miletich is board certified in both neurology and nuclear medicine.
Nuclear medical technologists can eventually take on administrative roles in hospital leadership, segue into research, or enter academia.
The demand for the career is high as every hospital needs nuclear medicine technologists. Susan Tiby, assistant director nuclear medicine at Upstate at Community Campus, has noticed a decline in the number of young people entering nuclear medical technologist programs.
“As soon as you say it’s a lot of
said while potatoes didn’t have the same impact on Type 2 diabetes, they also didn’t have any negative effect.
“In previous studies, potatoes have been positively linked to incidence of diabetes, regardless of how they’re prepared — but we found that’s not true,” Pokharel said.
“In Denmark, people consume potatoes prepared in many different ways; in our study, we could distinguish between the different preparation methods.
“When we separated boiled potatoes from mashed potatoes, fries or crisps, boiled potatoes were no longer associated with a higher risk of diabetes: they had a null effect.
Pokharel said underlying dietary patterns were the key.
“In our study, people who ate the most potatoes also consumed more butter, red meat and soft drink — foods known to increase your risk of Type 2 diabetes,” he said.
“When you account for that, boiled potatoes are no longer associated with diabetes. It’s only fries and mashed potatoes, the latter likely because it is usually made with butter, cream and the like.”
math and science, they don’t want to do it,” Tiby said. “There are numerous people retiring in the next three - five years and there’s already a shortage. There will be a lot bigger shortage then.”
She finds that the combination of skills that involve direct patient contact, pharmacy, radiation safety and computer software make this a well-rounded career.
“You’re helping a variety of patients, from inpatients to oncology to cardiac patients,” Tiby said. “It’s rewarding to know you’re helping people.”
Mr Pokharel said findings from the study indicate vegetables could play a key role in reducing Type 2 diabetes, as people who ate a lot of leafy greens and cruciferous vegies such as spinach, lettuce, broccoli and cauliflower had a significantly lower risk of developing the condition.
He said the relationship between vegetables and diabetes should be incorporated into public dietary guidelines — as should the benefits of eating potatoes.
“The finding that vegetables lower diabetes risk is crucial for public health recommendations, and we shouldn’t ignore it,” he said.
They may not have all of the benefits as other vegies, but potatoes are still a healthy option
Ahigh number of preteens and teens in the United States have viewed pornography and many have also sent or received nude or seminude photos — sexting — over their smartphones, a new study reveals.
“The prevalence rates we found in this study suggest that school counselors must be prepared to talk about sexting and pornography use with students, and to change the narrative about these behaviors,” said Amanda Giordano, lead author of the study and an associate professor in the University of Georgia Early College of Education in Athens.

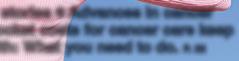
“It’s important that students know that sending a sext is not a new requirement for romantic relationships and that pornography does not reflect expectations for sexual activity,” Giordano added in a university news release.

For the study, the researchers questioned 350 students, aged 12 to 17 years. The investigators found that 15% had sent a sext to someone.
About 25% had ever received a sext. About 25% had ever been asked to send a sext. About 12% said they had felt pressure by someone to send a sext in the past year.

This pressure was concerning because of the unintended consequences of sexting, such as having the picture forwarded to others, put online or used as a form of blackmail to get the person to meet other demands, the researchers said.



“If your boyfriend, girlfriend or peer is asking for a sext, let’s talk through some of the possible risks,” Giordano said. “These are conversations that we need to have with adolescents, and they can happen at home or in schools. Adults need to keep up with technology and current trends so that we’re not just giving youth access to smartphones and hoping they make wise decisions. We need to prepare them for potential risks.”
About 50% of adolescents said they had been exposed to pornography. On average, kids were exposed
to pornography for the first time at age 11.5 — typically the age of American 6th graders and younger than previous studies have suggested.

Increased smartphone access among teens and the ease of finding free internet pornography likely drove that age drop, Giordano said.
More than one in three of the participants said they had viewed pornography at least once in the previous year. And 8% of the students said they watched pornography about every day.
Pornography use was significantly more common among males, the study found.
“Pornography use has been linked to a range of negative outcomes among children and adolescents. And pornography is a terrible sex education teacher for kids. However, for children who haven’t had conversations about healthy sexuality, they might not have anything to compare it to,” Giordano said.

“What we see from the research is that adolescents are developing their sexual scripts and beliefs about sex from what they’re seeing in pornography, which can have varying degrees of violence, aggression and degradation of women,” she added.


It’s important for schools to have

a sexting policy already in place, Giordano said. Then when a student comes to a staff member with a picture they have received or are being asked to send, the school will have a plan for what to do.
“Schools need to have conversations with legal counsel about what the sexting policy should look like in their state given the child pornography laws, so they already know how they will respond,” Giordano advised.


Providing accurate information to students about pornography and the risks of sexting is key as well, she said. For example, explaining that pornography uses actors and often isn’t an accurate depiction of healthy, consensual, safe sexual practices is important.
“We’re teaching students to be good citizens, and that should include promoting responsible, healthy tech use, known as digital citizenship,” Giordano said. “Technology isn’t going anywhere, so we need to set students up for success by teaching them how to be good global, local and digital citizens.”
The report was published online recently in Professional School Counseling.







For people recovering from an injury or joint surgery, aquatic therapy may be helpful in getting better sooner.
Like land-based (“dry”) physical therapy, aquatic therapy doesn’t require a physician’s prescription and most insurers cover treatment for a total of 30 days. At that point, a prescription would be required.
“To understand aquatics, you have to understand the hydrodynamics of water,” said Carol Sames, associate professor in department of physical therapy education at Upstate Medical University. “There’s buoyancy and resistance. As the water gets deeper, you have resistance. You also get buoyancy. At waisthigh water, you weigh 50% of your bodyweight. It’s less force on joints. At chest-high, you’re unweighted by 80%.”
Unlike land-based exercise, the pool challenges their posture, balance and core strength. But the water reduces risk of falls.
“Maybe a patient is someone who’s been sedentary and lacks muscle strength to bear weight a long time,” Sames said. “Or someone with a neuro-muscular condition. They’ve started using a cane, crutch or wheelchair for longer distances. They get in the pool and can walk. For individuals with chronic pain from osteoarthritis or rheumatoid arthritis, you have less force on joints. That can be very helpful.”
The water also helps patients who have cerebral palsy, multiple sclerosis or impairment from a stroke if land physical therapy is too challenging.
The 86- to 96-degree F temperature of most therapy pool also helps keep patients comfortable.
“You want to be in warm water for physical therapy,” said Elizabeth Cullen, physical therapist and owner of CNY Physical Therapy & Aquatic

Center in Camillus. “You don’t want it too hot, or you’ll have difficulty with cardiovascular movement. If it’s too cold, you’ll start to shiver a little. The joints won’t move as well.”
Most physical therapists use devices in the pool like noodles and flotation boards to help with movement or to encourage patients to stretch further and challenge themselves.

Most therapy pools are relatively shallow, as they’re not meant for diving or swimming laps. Cullen can accommodate people of varying heights with depths of four to five and a half feet. The pool’s smaller size, handrails and nearby walls help keep comfortable clients nervous about being in the water. The pool also features a chair lift for those who cannot manage the stairs.
Kuss Physical and Aquatic Therapy in Central Square offers “prehab” in anticipation of joint replacement surgery to help patients build strength without as much pain.
“It’s a great way to prepare for people waiting for surgery,” said John Kuss, physical therapist and owner of the practice. “They can maximize their strength and mobility. The better off you are going in, the better the outcome of the surgery. In the water, you’re exercising and burning calories. That will benefit people who need to lose weight before surgery. You’re constantly moving in the water without the same stress to the joints.”
“The same goes for people who want to start exercising but feel that traditional exercise is too hard because of chronic joint pain and fear injury,” he added.
Kuss also said that patients with edema—swelling in their legs—often find that the pool’s hydrostatic pressure helps reduce their swelling, even if their purpose of being in the pool is to treat a different area of the body.
Growing numbers of older Americans are dying from drug overdoses and alcohol abuse.
That’s the tragic takeaway from two new reports by the U.S. Centers for Disease Control and Prevention.
More than 5,000 people aged 65 and older in the United States died of a drug overdose in 2020, and this number has tripled since 2000, according to one of the reports.

The other report revealed that more than 11,600 U.S. seniors died from alcohol-induced causes in 2020. Alcohol-induced death rates in this age group have been on the rise since 2011 and jumped more than 18% from 2019 to 2020.
The new research wasn’t designed to look at why more older Americans are dying from drug overdoses or alcohol abuse, but the
findings mirror what has been seen in younger age groups.
Abuse of fentanyl and other synthetic opioids has had a big impact on the older population as well as younger folks, said study author Ellen Kramarow. She is a demographer at the CDC’s National Center for Health Statistics, which published the data Nov. 30 in an NCHS Data Brief. Death rates from these drugs increased by 53% from 2019 to 2020 among people aged 65 and older, Kramarow said.
The increase in deaths from drug overdoses and alcohol use has been rising faster in men, she added.
The study also highlighted a racial gap in deaths from drug overdoses among older adults. Drug overdose death rates among 65-year-olds are highest among Black people with one exception: white women aged
Once their round of physical therapy is complete, patients can purchase a gym membership at Kuss to continue improving their health and movement with therapists nearby to assist as needed.
In addition to their training in
physical therapy, physical therapists who provide aquatic therapy take continuing education credits to learn how to apply physical therapy principles in the water.
Few conditions contraindicate aquatic physical therapy, such as an open wound or incision. Patients should ask their primary care providers about any concerns.
75 and older have the highest death rates from drug overdose.
The risk of dying from alcohol-induced causes among people aged 65 and older was highest among American Indian and Alaskan Native people, the investigators found.
Experts who reviewed the new study were distressed but not surprised by the statistics.
The findings sadly reflect what Anne Fernandez is seeing in her practice. She is an associate professor in Michigan Medicine’s department of psychiatry, in Ann Arbor.
“I am struck by the increase in fatality from alcohol and drug use among both older adults and among younger adults, as well,” Fernandez said. “The two things that stand out to me are deaths from alcohol-associated liver disease and deaths from a drug overdose.”
What’s behind this?
Many factors play a role in this uptick, she said. “The baby boomer generation is now reaching older adulthood, and baby boomers histor-
ically have higher rates of substance use than the generation before,” Fernandez explained.
It’s also been a perfect storm for drug and alcohol abuse. “Alcohol and drug use also tend to increase when there are economic challenges, when drugs and alcohol are accessible and affordable, and when major stressful events take place, like the COVID-19 pandemic,” she said.
In addition, the drugs people take now are also more lethal than they were even a decade ago. “Early on, the opioid overdose crisis was driven by prescription opioid use but now it is driven by highly lethal synthetic opioids like fentanyl in the drug supply,” Fernandez noted.
• New life for Congressman John Katko. • When should you claim Social Security benefits? • Knitting: music for the soul. Meet the local pros. • Blacklights: old school band plays on • Former ‘New Times’ publisher Art Zimmer — remember him? — still has many irons in the fire • Bill Knowlton: bluegrass in his blood • New life for Congressman John Katko • Fulton author writes about snowstoms

If you are eligible at age 65, your initial enrollment period (IEP):

• Begins three months before your 65th birthday.
• Includes the month of your 65th birthday.
• Ends three months after your 65th birthday.
If you are automatically enrolled in Medicare Part B or if you sign up during the first three months of your IEP, your coverage will start the month you’re first eligible. If you sign up the month you turn 65, your coverage will start the first day of the following month. This won’t change with the new rule.
Starting Jan. 1, 2023, your Medicare Part B coverage starts the first


day of the month after you sign up if you sign up during the last three months of your IEP.

Before this change, if you signed up during the last three months of your IEP, your Medicare Part B coverage started two to three months after you enrolled.

If you don’t sign up for Medicare Part B during your IEP, you have another chance each year during the general enrollment period (GEP). The GEP lasts from Jan. 1 through March 31. Starting Jan. 1, 2023, your coverage starts the first day of the month after you sign up.
You can learn more about these updates on our Medicare webpage at www.ssa.gov/medicare and our Medicare publication at www.ssa. gov/pubs/EN-05-10043.pdf.


Please pass this information along to someone who may need it.
Q.: What are some of the documents Social Security will accept as proof of identity for a child?
A.: While you can use a birth certificate to prove age or citizenship, you cannot use it as proof of identity. Social Security needs evidence of the child’s existence after birth. An acceptable document must show your child’s name, identifying information, and, preferably, a recent photograph. Your child must be present unless the picture ID also shows your child’s biographical information (i.e., age, date of birth, and parents’ names). We generally can accept a non-photo identity document if it has enough information to identify the child (such as the child’s name and age, date of birth, and parents’ names). We prefer to see the child’s U.S. passport. If that document is not available, we may accept the child’s:

• Adoption decree.
• Doctor, clinic, or hospital record.

• Religious record (e.g., baptismal record).
• Daycare center or school record.
• School identification card.
All documents must be either originals or copies certified by the issuing agency. We cannot accept photocopies or notarized copies of documents. To find out more, visit www.ssa.gov/ssnumber/ssnumber. There, you can also find out what
documents you need, fill out and print an application, and then bring or mail the needed information to Social Security. You may also want to read the publication, Social Security Numbers For Children, available at www.ssa.gov/pubs.
Q.: I served in the military, and I’ll receive a military pension when I retire. Will that affect my Social Security benefits?
A.: You can get both Social Security retirement benefits and military retirement at the same time. Generally, we don’t reduce your Social Security benefits because of your military benefits. When you’re ready to apply for Social Security retirement benefits, go to www.ssa.gov/applyonline. This is the fastest and easiest way to apply. For your convenience, you can always save your progress during your application and complete it later. We thank you for your military service!
Q.: I’ve decided I want to retire. Now what do I do?
A.: The fastest and easiest way to apply for retirement benefits is to go to www.ssa.gov/retireonline. Use our online application to apply for Social Security retirement or spouses benefits. To do so, you must:
• Be at least 61 years and 9 months old.
• Want to start your benefits in the next four months.
• Live in the United States or one of its commonwealths or territories.

What tips do you recommend to Medicare beneficiaries dealing with hefty medical bills? My husband recently had open heart surgery and is recovering slowly, but the medical bills are coming in fast and furious and they’re putting us in medical debt.
— Struggling in Springfield

I’m sorry to hear about your billing struggles, but medical debt has unfortunately become a chronic problem in this country. According to U.S. Census data 19% of Americans households carry medical debt, including 10% of households headed by someone 65 or older. Even seniors on Medicare can easily get snagged in a web of complicated billing and coverage problems.
To help you slash your medical bills, here are some tips recommended by health care experts that you should try.
• Double check your bills: Almost half of all medical bills contain at least one error, including duplicate charges or charges for services you never received. If you’re facing a high bill and are on the hook for some portion of it, request itemized invoices from the hospital and other providers that detail everything you were charged for and go through them line by line. If you find something you don’t understand or find fishy contact the provider for an explanation or a correction.
• Wait for your EOB: Doctors’ offices and hospitals may mail initial bills to you before they even submit them to your health insurer. So, hold off on any payment until you receive an explanation of benefits (EOB) from your provider — Medicare, supplemental Medicare, Medicare Advantage or private insurer. This will show what you owe after your insurance has paid its portion.
If your EOB shows that your insurer is refusing to pay for services that you think should be covered, call them to see whether it’s a correctable mistake, such as a coding error for a certain test or treatment. If it’s truly a denial of coverage, you may need to file an appeal. For details on how to file a Medicare appeal, see Medicare. gov/claims-appeals/how-do-i-filean-appeal.

• Ask for a discount: Call the hospital’s accounting office or the billing staff at your doctor’s practice and ask if they can reduce your bill. You’d be surprised how often this works. Or if you have the funds to pay the entire
bill, ask the hospital or provider for a “prompt pay” discount which may save you 15% or more.













If it’s best for you to pay your bills over time, ask the billing office to set up a no-interest payment plan for you. It’s in the provider’s interest to work with you to obtain payment.
You can also call the hospital where your husband had his surgery and ask a billing specialist if the facility offers financial assistance. According to the American Hospital Association, about half of U.S. hospitals are nonprofit. This means they are required to offer free or discounted services in some instances. This is usually reserved for low to moderate income patients who have limited or no health insurance, but requirements vary from hospital to hospital.
• Get help: If you’ve gotten nowhere on your own, contact the Patient Advocate Foundation (patientadvocate.org, 800-532-5274) who can help you understand and negotiate your medical bills, free of charge. Or consider hiring a medical billing professional to negotiate for you but be aware that these services can cost upward of $100 an hour. You can find potential candidates through the Alliance of Professional Health Advocates (advoconnection.com). Be sure to choose someone who is credentialed by the Patient Advocate Certification Board.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.


Loretto is opening a new memory special care unit [MSCU] Jan. 2. With the support of some grant funding, the nonprofit has invested $750,000 in renovating an entire floor of its main campus to support the unique needs of those in the most advanced stages of the disease. The new 12th floor unit will offer 30 individual rooms for longterm memory care residents.
In a statement, Loretto said the demand for dedicated memory care services in Central New York has continued to increase, far beyond what the community can currently support.
Rita Romano has recently become Laboratory Alliance of Central New York’s new CEO.

She serves as a liaison between the board of managers, medical directors and management of the independent clinical and anatomic pathology reference laboratory.
Romano has a long history with
Laboratory Alliance. She first joined the company in 2011 as manager of its rapid response laboratory at Upstate University Hospital at Community General. In 2013 she was appointed director of the operations center, Laboratory Alliance’s main laboratory. In this role she was responsible for the oversight and management of clinical and anatomic pathology laboratory services in accordance with the accreditation authorities, physicians’ orders, policies, procedures, established standards and administrative policies.
With a focus on meeting each resident’s individual needs based on the complexity of their disease, Loretto’s 12th floor will incorporate a new wholistic approach. Using an emerging Montessori care philosophy, the environment will be filled with cues and memory supports that enable individuals to care for themselves, others and their community. Staff in this unit will undergo a detailed training program to prepare the team to deliver this Montessori-based approach to specialized care.
“Our memory care programs are based on the most up-to-date, evidenced-based research. As the
She returns to Laboratory Alliance after leading Quadrant Laboratories, LLC since March 2021, where she oversaw the establishment of 43 community-based testing sites for COVID-19 across New York state.
She has been dedicated to Central New York healthcare since beginning her career as a medical technologist at Community General Hospital in 1988. She held laboratory and management positions with St. Joseph’s Hospital Health Center, LabCorp, Northern Syracuse OB/ GYN Associates and North Medical Laboratory Services.
Romano earned her Master of Arts in strategic leadership and her Bachelor of Science in medical laboratory technology from St. Bonaventure University. She is certified by the American Society of Clinical Pathologists as a medical technologist. She is a graduate of the Ahern & Murphy Associates leadership course and Joel Ettinger Associates’ leadership development program.
She is serves as the president and board member and is an active member of the Clinical Laboratory Management Association Central New York chapter and an associate member of American Society of Clinical Pathologists.
Laboratory Alliance, established in 1998, provides all inpatient and outpatient clinical and anatomic pathology testing for Crouse Hospital and St. Joseph’s Health and for
region’s leader in memory care, we focus on improving the well-being of individuals with Alzheimer’s and other dementing illnesses through therapeutic means and supporting them in meeting the challenges of their late-life stages,” said Loretto President and CEO Kim Townsend. “We believe that those living in our memory care unit desire a quality life and we are here to support them within their individual capacity and culture, by anticipating needs and providing comfort, autonomy, and security.”
Loretto estimates that more than a third of residents across its system
have a diagnosis of dementia and that number is expected to increase. Currently, 410,000 people aged 65 and older are living with Alzheimer’s in New York today, and that number is expected to grow by close to 15% by 2025. Additionally, Loretto recently completed a comprehensive needs assessment of CNY’s aging population and created an action plan to address unmet needs, which led to the expansion of Loretto’s dedicated memory care space to meet this increased demand for dementia services.
regional hospitals, long-term care facilities and healthcare practices in a 16-county region in Central New York. The company performs more than 10 million tests per year through its 11 patient centers and three laboratory locations.

Hematology-Oncology Associates of CNY (HOA) successfully attained accreditation from the American Society for Radiation Oncology (ASTRO) APEx – Accreditation Program for Excellence.
APEx provides external validation that a radiation oncology facility is delivering high-quality patient care. HOA’s accreditation is effective through November 2026.

“HOA is pleased to receive APEx accreditation from ASTRO, the largest radiation oncology society in the world,” said Maryann Roefaro, HOA’s CEO. “Our radiation oncology team is invested in evaluating our processes to meet ASTRO’s high standards for safety and quality. Achieving APEx accreditation shows our local community that we are dedicated to delivering consistently safe patient-centered cancer care.”
APEx, the fastest-growing
radiation oncology practice accreditation program in the United States, is a voluntary, objective and rigorous multi-step process during which a radiation oncology practice is evaluated using consensus-based standards. The practice must demonstrate its safety and quality processes and show that it adheres to patient-centered care by promoting effective communication, coordinated treatments and strong patient engagement.
“ASTRO commends HOA for achieving APEx accreditation,” said physician Geraldine M. Jacobson, chairman of the ASTRO board of directors. “By undergoing this comprehensive review, the facility demonstrated their strong commitment to delivering safe, high-quality radiation oncology services to their patients.”
APEx is the only radiation oncology accreditation program that includes a self-assessment, which allows practices to internally assess compliance with quality improvement standards. The practice then proceeds to a facility review by an external surveyor team that includes a radiation oncologist and a medical physicist.
HOA is a private community cancer center established in 1982 with a mission provide the highest level of quality care in a healing environment for the mind, body and spirit of patients dealing with cancer
and blood disorders.
A member of the Community Oncology Alliance, HOA has offices in Auburn, Camillus, East Syracuse and Onondaga Hill.
Lisa White has been appointed as chief administrative officer and executive vice president at Excellus BlueCross BlueShield. White, in her new role, has also joined the company’s executive leadership team.
White started her career at the health plan 31 years ago as a customer care representative. She’s since held a variety of positions throughout the company. White, for example, helped start the company’s first compliance department, focusing on government regulations, mandates and more.
She now oversees about a dozen
departments whose primary responsibilities support the enterprise, including legal, audit, facilities, governance, strategy, corporate development, corporate communications, business resilience, risk management and ethics, privacy and compliance.
“Lisa brings years of experience and expertise overseeing complex administrative support functions, and we’re proud to have her join our executive leadership team,” said Jim Reed, President and CEO, Excellus BCBS.
“We’ve been lucky over the years to have Lisa at the helm, especially during COVID-19,” Reed added.
“Lisa played a pivotal role in our organization’s response to the pandemic, helping us focus on supporting our members through challenging times.”
A graduate of Syracuse University, White earned her master’s degree from the New England College of Business and Finance. She serves on the board of trustees for the MakeA-Wish Foundation of Central New York.
White and her husband reside in Syracuse. They have three children.
without the personalized care of our devoted staff. We are excited to continue to hold ourselves to the highest standard of excellence while delivering exceptional care,” said Kate Rolf, president and CEO of Nascentia Health.
Development Association (NEHDA) for four years. She has also served at Open Hand Theater, Hospice of Central New York and consulted with several other nonprofit agencies.
Nascentia Health recently announced that the organization was nationally ranked No. 31 among healthcare providers and insurers in Modern Healthcare’s 2022 Best Places to Work award program.

This annual award program identifies and recognizes outstanding employers in the health care industry nationwide. Modern Healthcare partners with the Best Companies Group on the assessment process, which includes an extensive employee survey. The complete list of this year’s winner rankings is available at ModernHealthcare.com/bestplacestowork.
”I am so proud of what our staff has been able to accomplish this past year. What an honor it is to be among the top healthcare providers and insurers in the nation. We have been able to provide care where our patients want it most, in their homes. None of this would be possible
“The healthcare workforce has undergone a true test in the past year and a half, oftentimes pitting employees against employers. So how best to keep harmony in a workplace that is inherently stressful? This year’s winners have an easy tip to incorporate show respect. In high-performing and successful teams, regard for employees’ well-being, acknowledgment of their contributions, and deference to their experience and dedication all helped maintain professionalism and productivity,” said Aurora Aguilar, editor of Modern Healthcare. “We congratulate all of the Best Places to Work in Healthcare for emphasizing that compassion and respect are essential to an engaged and productive workforce.”
Andrea Wandersee is joining
ACR Health as the chief operating officer. She has more than 25 years of experience in nonprofit and higher education leadership, with a background in organizational development.
She is passionate about promoting healthy communities, especially for those who are underserved by mainstream systems.
Prior to joining ACR Health, Wandersee served as the executive director of The Northeast Hawley
Wandersee currently serves on the board of directors of the Syracuse Cooperative Federal Credit Union and Exceptional Family Resources. She has an MPA from the Maxwell School of Citizenship and Public Affairs at Syracuse University and a BA in History from Hartwick College.
Wandersee has lived in Eastwood since 2007.
Oswego Health recently promoted long-time employee Jen Baker to oversee talent acquisition.


Experienced human resource specialist, Baker started at Oswego Health in 1999 and for the past 23 years has held various titles positions not only at the hospital but at The Manor, including CNA, CNA manger, director of activities, nurse recruitment and retention specialist, benefits manager and, most recently, HR generalist.
In this new role, Baker will be responsible for providing a superior candidate experience throughout the full lifecycle recruiting process. In addition, she will provide proactive support to hiring managers and creatively source and attract qualified candidates for all roles using strategic recruiting methods.
“There is probably not a more deserving and suitable person for this role, than Jen Baker. We are very excited to have her step into this new role as we all know how critical talent acquisition is right now,“ said Vice President of Human Resources Marq Brown.
With more than 1,200 employees, Oswego Health is the third largest employer in Oswego County.
The quality and care at The Manor at Seneca Hill remain one of the best in Central New York. The Manor has earned a 5-star quality rating and a five-star rating overall from the Centers for Medi-
care and Medicaid (CMS).
CMS created the five-star quality rating system to help consumers, families and caregivers compare skilled nursing facilities easily. This rating considers differences in the
levels of residents’ care needs in each skilled care facility and is based upon numerous care metrics that include staffing, inspections, and quality.
The Manor is the only nursing home in Oswego County to receive a fivestar rating in 2022.
The Manor features 120 licensed beds and offers residents a homelike environment with spacious, private,
or semi-private furnished rooms.
“I am incredibly proud of our staff at The Manor for earning this prestigious achievement again this year,” said Leigh Hilgenberg, executive director and administrator at The Manor. “This rating truly demonstrates the dedication staff has for our residents and their commitment to providing exceptional care.”


