











risk. Having a strong social support network has been linked to better psychological health.
Venting to people in that network is one way to reduce the impact of daily stressors, said Millstein, also an assistant professor in the department of psychiatry at Harvard Medical School. "Calling a friend and letting it out can be helpful. It helps us feel connected to our social support networks, which is a big determinant of life satisfaction and overall well-being."
Speaking to someone who is supportive of your feelings can be helpful, even if that person offers a different perspective, she said.
Shaffer said.
If speaking feelings aloud to someone else feels unsafe, another alternative is to write them down, Shaffer said.
Studies have found numerous health benefits to expressive writing, the practice of writing down feelings on a daily basis. It has been shown to aid in healing from traumatic experiences and to help lower blood pressure, boost the immune system, improve sleep and lessen depression and pain.
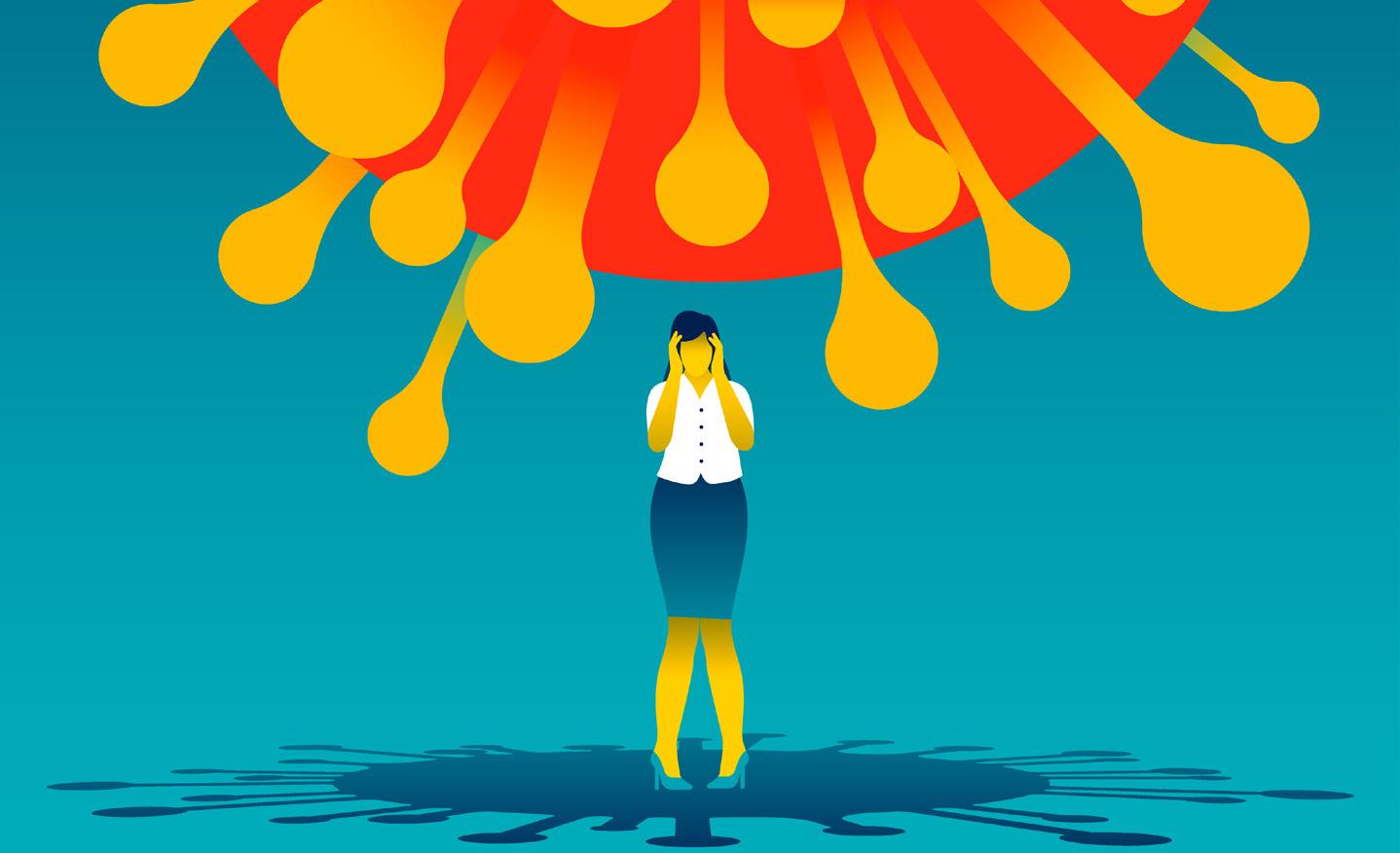
Venting — the release of negative, pent-up emotions — can feel good. But is it actually good for you? Or does it do more harm than good to dwell on negative thoughts and feelings?
Experts say that depends on a number of factors, including who's on the receiving end of a venting session, how often a person does it and what type of feedback they receive.
"By and large, we do need to get our negative emotions out," said Rachel Millstein, a staff psychologist in the behavioral medicine program and the lifestyle medicine clinic at

Massachusetts General Hospital in Boston. "The ways we do it, though, that's where it's healthy or unhealthy, productive or unproductive."
Personal relationships, work, finances and discrimination are just some of the daily stressors that may fuel someone's need to vent. Research shows this kind of stress can raise the risk for cardiovascular disease, whereas releasing or managing stress can improve physical and psychological health, lowering that
But venting to someone who is dismissive of your feelings can be detrimental, said Jonathan Shaffer, an associate professor of clinical health psychology at the University of Colorado in Denver. "It's invalidating to share and get no response from the other person. It might make you feel like you don't have worth or are not loveable."
Venting also can be counter-productive if the listener amplifies negative feelings and "the conversation spirals. Then you can pull each other down," Millstein said.
Another negative consequence could be if the listener gets tired of listening. "If you vent over and over again, this person might not want to be present, and this can fray a social connection," she said.
For major stressors, it might be more helpful to speak to a therapist,
Whether releasing feelings on paper or in person, Shaffer suggests finding ways to focus on the positive, as well as the negative. For example, ending a venting session with a focus on things for which the person is grateful can help restore positive feelings, he said, as can mindfulness practices.
"Make a plan for some type of relaxation, such as deep breathing or meditation afterwards," he suggested.
Exercise also can relieve stress and release negative feelings, Millstein said.
"And don't forget that humor is a really good coping strategy, too," she said. Venting to a friend with a good sense of humor may be twice as helpful, because "sometimes other people can help us see the funny side of things."
It’s about more than just weight loss.
It’s about reducing your risk for serious conditions like heart disease and diabetes — and regaining the stamina, mobility and confidence to take on every day.
Crouse’s bariatric surgery program offers a dedicated team of physicians and providers, as well as psychological and nutritional counseling — all with the expertise to support you every step of the way.
Begin the process from home by viewing our online informational video. Then consult with our bariatric team via telemedicine visits to start your journey. It’s time — and now easier than ever.

Don't let any heart condition go unnoticed or undiagnosed. Whether it's a routine check-up or a complex procedure, you want expert care from specialists who have the experience and training to care for you. The Auburn Heart Institute is home to a dedicated team of exceptional cardiologists who can offer highly advanced, minimally invasive treatments. It's heart care that doesn't only change lives, it saves them.
You don’t have to wait weeks or months for an appointment we have opened our new cardiology offices on the 3rd floor of Auburn Community Hospital. Call today for an appointment: 315-567-0540.
 Meet
Dr. Ronald L. Kirshner & Dr. Praveena Paruchuri
Meet
Dr. Ronald L. Kirshner & Dr. Praveena Paruchuri
bies, had heart defects that were repaired. The surgeries were so good that these babies were able to live full adult lives. But a lot of adult cardiologists don’t know the anatomy and the surgeries. So that’s my specialty. I trained at Texas Children’s Hospital, and I was building a program back in Long Island. As a corollary to that, I do advanced cardiac imaging. But here there’s a strong need for basic, general cardiology. And the basics are still where the biggest bang for the buck is. Not in terms of money, but in the ability to affect positive change in health outcomes.
Q: Given your specialty training and experience at academic centers, are there any changes you’d like to affect at Auburn?
Q: What brought you to Auburn Community Hospital?
A: I’ve always been in New York aside from a brief thing in Houston, and I always wanted to work in a more underserved community. I kind of got spoiled. I was in academic medicine, where you have everything at your disposal, all the way up to transplants. Advanced surgeries are great, but there are a lot of the bang for the buck in prevention and management of things like hyperten-
portunities up in Maine and ended up interviewing at Auburn. And that’s how I ended up here. It sounded like the perfect fit.
Q: What are some of the things you like better about practicing at a community hospital?
A: The first and foremost is I see patients in the office every day. The way my schedule was in the bigger centers, you’re kind of relegated to different services, so you can’t really
A: There’s always the basics, like bringing in more patients and providing immediate and quality service. So aside from that and building my practice, I’d love to focus on prevention, controlling hypertension and hyperlipidemia, weight loss, evaluating patients for disease risks. Women, in particular, don’t really know they’re at risk for heart disease. There’s a lot of awareness about breast cancer, but a lot of women don’t realize that heart disease is still the No. 1 cause of death in women in America. So women tend to be underevaluated and undertreated for heart disease. I just had a woman yesterday who hadn’t realized she’d had a heart attack. I’m not sure what pain she had that she misunderstood. It’s kind of a sign as she’s now dealing with the consequences. So I would really like to focus on that.
Q: As far as prevention goes, what’s something counterintuitive people may not know about heart health? That they may not hear all the

A: I think it’s that the weight loss thing isn’t a gimmick. At the end of the day, losing weight is kind of a science. You eat less than you put out. It’s not so much a mystery, but people get lost in all these diets and fads. You watch what you eat and try to choose the better foods. Weight loss and being a normal BMI does wonders for overall health, for blood pressure, for cholesterol and so much beyond weight. I have my patients keep a food diary so it’s not so much a mystery. It works; you just have to do it. The other thing is water consumption. I didn’t realize how much of a problem this was. I had a really hard time taking care of a lady with heart failure. She was watching these TV shows where they were encouraging people to drink a gallon of water. Water is good for you, but if you have heart disease, you have to really watch it. The blanket advice to drink a lot of water isn’t exactly right for heart patients. There are heart patients where a gallon of water will kill them. So I’d strongly recommend you talk to your doctor about how much water you drink. Same for kidney patients.
Q: I’ve heard horror stories about water toxicity, but that’s tremendous amounts of water in a short period of time. What makes a moderately high amount dangerous for some patients with heart disease?
A: So it’s specifically patients with diastolic heart failure, where your heart doesn’t relax, which is actually quite common. And then there’s systolic heart failure where you have a cardiomyopathy where
the heart muscle is weak. So those patients have to watch their water because too much can send them into heart failure. Some patients need to be restricted to as little as a liter of water per day. I had a younger patient who had bounced in twice in three months with heart failure and couldn’t breathe because there was water in their lungs. They didn’t think they were drinking that much, but we added it all up and it was a gallon of volume. And here I had been constantly putting them on water pills. Now, it’s the opposite problem for most people. Most people don’t drink enough water. But that’s the problem with blanket advice from something like a TV show.
Q: I hear you have quite the side gig. You’re a filmmaker?
A: I make feature films that are on Netflix. I make Indian films. That’s another thing that’s great about Auburn; it offers me the flexibility to do that. That’s another important part of health: work-life balance. One of the films is “Care of Kancharapalem,” which is the number one Telegu film on Netflix and the number one Telegu film of all time on IMDB. The other one is “Uma Maheswara Ugra Roopasya,” which is also on Netflix. The first two films I produced. I just finished my directorial debut on a third project before coming to Auburn.
Q: Now are these American-produced films in the Telegu language or are they Indian films with domestic distribution?
A: They’re Indian-produced. The first had a theatrical distribution and then was sold to Netflix. The second one fell during the pandemic, so I sold it directly to Netflix. The third one is definitely intended for theaters. I’m a big fan of Tom Cruise and appreciate how much he’s doing to bring people back to the theaters. So go see films in theaters, not just on Netflix!
Name: Praveen Paruchuri, M.D.
Position: Cardiologist at Auburn Memorial Hospital

Hometown: Queens
Education: St. George’s School of Medicine; Winthrop University
Affiliations: Auburn Community
Hospital
Organizations: American Heart Association; American College of Cardiology
Hobbies: Filmmaking
Cardiologist from Long Island now practices at Auburn Community Hospital. She talks about weight loss, water consumption — too much can kill some people with certain heart conditions — her relationship with local patients and the movies she has produced for Netflix
The patients here are so appreciative. So many of them thank you for taking the time to talk with them here. In New York City it’s ‘how dare you keep me waiting two minutes!’”
Alarge new study challenges the long-held idea that depression makes people more vulnera ble to cancer, finding no association between the mental health condition and most types of cancer.
The study, of more than 300,000 adults, found that neither depression nor chronic anxiety were linked to increased odds of developing can cer in the coming years. And when researchers looked at specific types of cancer, the findings were largely the same.
The one exception was a slight ly increased risk of cancers that are strongly linked to smoking, includ ing lung cancer. And the analysis suggests that smoking — as well as alcohol and heavy body weight — are the real culprits, rather than depression or anxiety themselves.
Experts said the study, published online Aug. 7 in the journal Cancer, may offer reassurance to people who've blamed a cancer diagnosis on their mental health struggles.
"Our findings show that there is no evidence for this," said study leader Lonneke van Tuijl, a health psychology researcher at University Medical Center Groningen in the Netherlands.
Unfortunately, that kind of self-blame "comes up a lot," said physician William Breitbart, chief of psychiatry at Memorial Sloan Ketter ing Cancer Center in New York City.
"There are many patients who

with me or extend an invitation to join them. I’ve met some of the nicest, most interesting people this way.
hungry. Ha!
By the time this edition of “In Good Health” hits the newsstands, I will have packed my bags, hired a cat sitter and stopped the mail.
I’ll be on my way to France for my annual solo sojourn to Paris to celebrate my birthday and further explore and enjoy one of my favorite places on earth.
In September, the tourist crowds have thinned, the weather is more to my liking (on the cooler side), and the locals have returned from holiday to open their shops, restaurants, homes and hearts to travelers like me.
My love affair with Paris was kindled on my 50th birthday. I wanted that important half-way milestone to be special and memorable. And it was!
I had dreamed of going to Paris for years and I wasn’t going to let my single status derail my dreams.
When I told my friends about my plans, I got mixed reactions. Many exclaimed “Oh, I could never do that! All alone?!”
They were right, of course. They would never experience the fun and fulfillment of traveling solo as long as they held onto that attitude.
Traveling alone, just like living alone, requires the right frame of mind to be successful and enjoyable.
But why travel alone in the first place? Why not grab a friend or two and make it a shared experience? Because the potential for self-discovery
and savoir faire that comes with solo travel is priceless.
I’m not suggesting an exclusive diet of solo travel, but I am encouraging you to consider this mode of travel, from time to time, for this important reason: You’ll gain both confidence and wisdom from your experience.
So, step on board and consider these benefits:
• You call the shots
When you travel alone, you are free to see and do whatever you like. Your decisions and itinerary are your own. And when it's just you, you are reminded of who you are, what you enjoy doing most, and what you like least.
When traveling with friends and family, we tend to stay focused on each other and lose the chance to meet people we might otherwise have met. That could be a missed opportunity, especially if you are single and hoping to meet someone new.
• You can release your adventurous spirit
By yourself (with no one watching), you may be willing to take more risks — dance at outdoor concerts, get a henna tattoo, eat gelato for breakfast, maybe even swim with the dolphins!
I’ve never gone swimming with dolphins, but I have sampled some pretty exotic food, wrestled Old Paint into submission on a horse trail and held on for dear life while rafting down the Colorado River.
• Likewise, you can find some heavenly time to yourself
When you travel with other people, their interests may be at odds with yours. And precious time can be consumed with the inevitable negotiations that come with trying to satisfy everyone’s needs and desires.
Traveling alone allows you to follow your heart and own path.
• You make new friends more easily
I’ve discovered this time and time again. When I’m on my own, other travelers and "locals" are more likely to strike up a conversation
Competitive sports can be a lot of fun for kids and teens, but starting a new season requires some planning.
Nemours TeensHealth, a website specializing in children’s health, offers some suggestions for kids and teens who are taking up a new sport or beginning a new season.

• Start by getting into shape. That will make it easier when you begin your sport.
You can do this by writing down an exercise plan. Ask your coach, gym teacher or trainer for workout ideas. If you can't get to the gym, apps and online workouts offer options for exercising at home.
Write down your goals for the
week and your workout plans. If you schedule specific workout times, it will help you stay motivated and stick to your exercise plan. Make a note of a workout you particularly liked so you can repeat it another week.
• Set realistic goals. While this can include general goals like making the team or getting in shape, smaller, specific goals are easier to achieve and can help you build toward your bigger goal.
Write down those goals and discuss them with a parent or coach. Set new goals once you reach those on your list.
• Gear up. If you're returning to your sport, make sure your
On your own and with fewer distractions, the opportunity for a tranquil, soul-soothing retreat is within your grasp. Whenever I travel, I like to build in time to myself to relax and recharge my batteries. Solo travel makes guilt-free “me” time possible.
Want to sleep in till noon, find splendid solitude in a secret garden, or enjoy your own company and a nightcap at the end of the day? Go for it, because you can.
• You learn a new language faster Je peux en témoigner! (I can vouch for that!). When traveling alone in France, I enjoy practicing the language. It was either that or go
But seriously, without a traveling companion to talk with or to aid in translation, I had to fend for myself. While I am far from fluent in French, I can at least order a croque-monsieur — a hot ham and cheese sandwich on my own. Want to learn a language more quickly? Travel solo.
• You build your confidence and sense of independence
Even a small jaunt can boost your self-confidence. All the decisions are yours, including your budget. You decide how to get where you’re going, where to stay, and how much to spend on transportation, food, accommodations, and things to do.
In no time, you’ll discover your own resourcefulness, ability to solve problems, and capacity to spend some time alone. Those are invaluable, lifelong lessons.
Solo travel is ripe with opportunities for self-reflection, growth, and joy. Start dreaming today. Pack your bags, and with no reservations (pun intended), set out on your journey with a spring in your step and a smile on your face for all the hidden treasures that await you.
Gwenn Voelckers is the founder and facilitator of Alone and Content empowerment workshops for women (now on hiatus) and the author of "Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own " To contact Voelckers or purchase her book, visit www.aloneandcontent.com

equipment still fits. If you're new to a sport, ask your coach what you'll need.
Secondhand or borrowed gear can save you money. Make sure all your gear is clean and safe to use. Ask your coach to look it over if you're unsure, Nemours suggests.
• Think about attending a sports camp. This can be a way to practice skills before a season begins. College players, coaches or other professionals often teach these camps.
Most include drill sessions, then scrimmages toward the end of the day. Drill work helps improve skills, while scrimmaging with other campers lets you practice those skills. This
can give you a sense of what it's like to play on a team.
• See your doctor for a sports physical. It's a busy season for these physicals, so make sure your family sets up an appointment before your season starts. If you wear glasses, consider visiting your eye doctor to check your prescription and get the right protective eyewear.
Be sure to build rest into your schedule, with at least one to two days off a week from competitive sports and training. Take at least two months off each year from any particular sport to prevent repetitive stress injuries, Nemours advises.



























If you take better care of your car than your body, you aren’t alone.
According to the Men’s Health Network, there’s a steady deterioration in the health and well-being of men.
Living long and living well is an uphill battle for most men.
Compared to women, they eat worse, smoke more, drink harder, exercise less and suffer more injuries.
In 1920, women outlived men by only one year. Today, CDC statistics show that the life ex-pectancy gap has widened: women survive men by more than five years. The National Institutes of Health reports that men die at higher rates than women for all of the top 10 causes of death.
It’s no secret that many men hesitate to see a health care professional. And that can lead to a number of problems down the road.
This is the biggest problem for men: the lack of health care earlier in life. Anyone not connected to a health care professional to screen for major health problems is at greater risk of disease and death.
Many of the top causes of death are preventable and treatable if found early. Here are some of the most common men’s health issues that every man should know about and how to reduce your risk:
Although heart disease is the leading killer of both men and women, almost twice as many males die of cardiovascular conditions. According to the American Heart Association, one in three men has some form of heart disease.

“High blood pressure is a leading risk factor for heart disease and stroke,” said physician Cynthia Jones, medical director of Mosaic Health Utica and board member of the AHA. “Because it often has no

symptoms, it’s known as ‘the silent killer.’”
High blood pressure causes harm because it increases the work of your heart and blood vessels, making them work harder and less efficiently. This can damage blood vessels, making them weak, stiff or narrower and that can harm important organs of your body — your heart, kidneys, brain, and eyes, she added.
High blood pressure raises your risk for serious events like a heart attack or a stroke. It’s important to know if you have it as there are steps you can take to prevent serious outcomes.
If you don’t know you have high blood pressure, and you don’t take steps to control it, in addition to a heart attack or a stroke, it can cause heart failure, kidney disease, loss of vision, or sexual dysfunction.
Other things you can do to reduce risk of heart disease or stroke include: stop smoking, get active, eat better, and control your blood sugar, said Jones.
Men are almost twice as likely to develop Type 2 diabetes as women, says the CDC.
“Having diabetes puts a person at high risk for other medical illnesses,” said registered nurse Janet Brown-Friday of the American Diabetes Association. “Diabetes can lead to health complications such as heart disease, kidney disease, nerve damage and problems with feet, oral health, vision and hearing problems, and mental health.”

“With the prevention of diabetes, one may be able to prevent or delay the onset of these conditions,” she added.
Risk factors for diabetes that one can control are weight and level of activity, she said. “According to the ADA, one can make small changes to their lifestyle for big results — like
doing 30 minutes of exercise a few days a week — or make small changes in what you eat or finding ways to manage stress.”
If you have a family history of diabetes, it’s important to see your doctor for regular blood sugar screenings.
According to the American Lung Association, lung cancer is the leading cancer killer. More men are diagnosed with it than women. African American men have a higher risk of dying from the disease. Smoking is the leading cause.
Tobacco is responsible for 90% of lung cancer, which puts the burden of prevention efforts on stopping smoking. Besides smoking, exposure to secondhand smoke or exposure to asbestos or radon are also risk factors.
Prostate cancer is the most common cancer found in men. It’s treatable if found in early stages. This can be a challenge, since prostate cancer may have no symptoms.


Older age is a risk factor for prostate cancer, but younger men should not be complacent. 30% of prostate cancers occur in men younger than 65, says the American Cancer Society. Men with a family history of prostate cancer or who are African American are also at higher risk.
Men older than 45 should seek a regular prostate cancer screening, says ACS.
Free prostate exams during September will be offered by Upstate Urology at MVHS; see mvhealthsystem.org/prostate-screening form for details and to sign up.
Don’t be an average man —get on board with a health care professional and protect your health today.
Men die at higher rates than women for all of the top 10 causes of death.
• Heart: Almost twice as many males die of cardiovascular conditions compared to women
• Lung cancer: More men are diagnosed with it than women
• Diabetes: Men are almost twice as likely to develop Type 2 diabetes as women
No. 1 – Heart Disease
No. 2 – Cancer
No. 3 – Unintentional Injuries
No. 4 – Stroke
No. 5 – Chronic Obstructive Pulmonary Disease (Lung Diseases)
No. 6 – Diabetes
No. 7 – Influenza and Pneumonia
No. 8 - Suicide
No. 9 – Kidney Disease
No. 10 – Alzheimer’s Disease
Source: Illinois Department of Public Health (IDPH)
•
•
•

















As I write this article, COVID-19 numbers at the urgent care are steadily climbing.

I don’t have a crystal ball to see the future, but I suspect that this latest wave may really take off once kids return to school.
In fact, I had COVID two weeks ago — my first bout — and technically it was a mild case.
My oxygen level never dipped low, I didn’t get pneumonia and didn’t get so sick that I needed to be in the hospital. But I can tell you that a high fever, shaking chills, cough, fatigue and muscle aches do not feel mild when you are the patient.
So, this is a good time to review some COVID facts.
First, don’t rely on a loss of taste and smell as required symptoms of COVID. These symptoms are much less common than with earlier variants. COVID is most likely to present as a respiratory illness similar to a cold and can vary from mild sniffles or sore throat to severe with cough, shortness of breath and fever.

Because every variant is a little different, don’t assume that a cold
that feels different than a previous bout of COVID can’t be COVID. COVID can also act like a stomach bug with vomiting and diarrhea or the only symptom might be a bad headache.
If you think that you have a cold or the flu, it’s worth testing for COVID. There are antivirus pills that help if you qualify: age 50 or older, overweight or obese, chronic underlying medical conditions such as diabetes, heart disease, and lung disease. These pills reduce the chance that mild or moderate disease becomes severe disease or leads to hospitalization. But the medicine should be started as soon as possible after a positive COVID test, and within five days of illness onset. Even if you don’t want or qualify for these medicines, knowing whether you have COVID can help you take measures to reduce the spread, Rapid COVID tests are not perfect. They may not detect COVID during the first few days. If you have a negative test but continue to feel sick, repeat the rapid COVID test. Or obtain a COVID PCR test which
is sent to the lab. It’s more sensitive although it does take a day or two to receive results.
One of the best ways to prevent severe COVID remains vaccination. Yes, it’s possible that you will get COVID even if you’ve been vaccinated. But the vaccination reduces the chance that you will wind up hospitalized or dead.
Also helpful to prevent spreading or acquiring the disease are face masks. If you only cover your mouth, they are doing very nothing. Make sure the mask covers your nose and mouth. The most protective masks are N95 or KN95 masks. Next best are surgical masks. But you need a fresh mask each day. Cloth masks may look fancy but are not beneficial. You can use a cloth mask over another type of mask if you like the look.
Even if you don’t recall or aren’t aware of being exposed to COVID, you may still have contracted the
disease.
You may have encountered someone who was an asymptomatic spreader, or someone who did feel sick but never told you. Unless you are truly a hermit who has no contact ever with any other human being, you’re at risk.
This information may be basic, but it’s worth reminding everyone so that we can all try to stay healthier this winter.
 Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.
Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.
Goats, donkeys, a camel, horses, alpacas, chinchillas, rabbits, dogs, cats — all these are used to help kids in crisis at the Purpose Farm in Baldwinsville, says founder and volunteer executive director. She explains
 By Mary Beth Roach
By Mary Beth Roach
Q: Tell us about Purpose Farm, what is your mission?
A: We mentor kids ages 6 to 18 who are in crisis, and they work with
animals that have come from similar circumstances of neglect, abuse, or have experienced some sort of trauma. It’s all free of charge.
Q: How long have you been doing this?
A: Since 2008, when God called us to do it, and we saw our first youth in 2012.

Q: You said God called you — how did that happen?
A: We [Sandra; her husband, Howard, and three of their children] took a mission trip in 2008 to Romania, and we used to pass by a horse farm on the way to the orphanage. I thought that’d be a great idea to bring the kids from the orphanage out to the horse farm to get away for a while. But that would never happen in Romania. And then we came back home, I was driving in my car to work, and I heard Erin Maxwell’s story on the radio and I just cried out loud, ‘God, what can I do to save these kids before it gets to the situation with Erin Maxwell?’ And he said, ‘You can do your horse farm idea here in Central New York.’ [Erin Maxwell was a young girl from Palermo, whose stepbrother was imprisoned for her 2008 death; her father and stepmother served jail time for endangering the welfare of a child. According to authorities, the family home had horrible living conditions.]
Q: Did you have any farming or horse experience?
A: Actually, I’ve gone through a lot of the same trauma that the kids that we see have gone through. And I had kids as a teenager. I actually started riding at age 30 after my fourth kid, and I just immersed myself entirely into it.
Q: What are some of the animals on the farm?
A: We have goats, donkeys, a camel, horses, alpacas, chinchillas, rabbits, dogs, cats.
Q: What was your life previous to this?
A: Previously we lived in the suburbs, in East Syracuse. My husband owns a plumbing company, and I cleaned houses for a living. We sold our house, our possessions. We had a camp, renovated it, and sold that. That was what enabled us to purchase the property that is now Purpose Farm. That was a total renovation job as well.
Q: The kids who visit the farm — where do they come from and how is the mentoring experience?
A: The kids come from a variety of different areas — word of mouth throughout the community. We also get references from psychiatrists. Social Services will refer people to us; Hillside, Toomey House, Elmcrest, different group homes.
It’s a youth mentoring program basically. The youth will come on a weekly or biweekly basis because we want to build a relationship with them. We don’t want it to be a oneand-done. They have severe trauma. Most of them don’t have friends or a good family unit. So that’s what this becomes to them. We start in the beginning of the session with a small chore. It helps them to learn not only to give back to the community, but it also shows them how to care for something other than themselves. That’s where empathy starts forming. And it also gives us time to talk with them a little bit. From there, it might be taking the pig down to the river for a walk, or grooming a horse. It depends on where the kids are mentally and what I think that they can handle.
Q: Who does the mentoring?
A: It’s me and my daughter, Raven.
Q: How many kids do you usually have in a week, let’s say?
A: We break it down by sessions, basically about 130 to 160 sessions per year. They’re recurring.
Q: From your experience, what is it about the connection between kids and animals?
A: They are grateful to be here in a safe environment, that somebody is listening to them. They talk consistently the whole time. The animals teach them responsibility, getting them outside of themselves. When you’re working with an animal, you’re totally consumed with that. They also see what the animals have gone through. The kids see that, they relate to it, and then they start talking about their trauma. The feedback that we’ve heard is that they start to be nicer to other people in their classrooms. It softens them and they start to think about other things that are happening around them versus pulling back into their anger and into themselves.
For more information on Purpose Farm, visit www.purposefarm.org.

Larry Lombardo has owned Bridie Manor in Oswego for 36 years … Aug. 27, 1987. He has had MS since he was in fourth grade.
“I was 9 years old.”
But it hasn’t stopped him from helping others.
“I had come-and-go symptoms. From when I was 9 years old until I was 36 years old — every time I went to the doctor, they didn’t know what was wrong,” he said. “I had balance problems, numb feet and numb arm, bad legs, running into telephone poles, falling down — running into moving cars!”
Nobody knew what it was. Then in 1987, he had a major MS attack.
“I went to a neurologist in Syracuse and he diagnosed me,” he said.
“And then, at that point in time,” he said, “there’s nothing available’ — so, you know, luck of the Irish — ‘just do the best you can. Take it easy, no drinking, No this no that. You have to change your lifestyle.’”
‘You’re not going to die from it — but some days, you’re going to wish you did!’ the doctor told him.
“Thankfully, that thing never happened,” Lombardo said. These days, there is a whole bunch of different drugs available.
“I’ve been on infusion for 10 years now. I’ve been on some sort of medication since, let’s see now — I’ve been on medication for 36 years,” he said.

“I’m doing OK. I’m still doing OK when I’m on it,” he continued. “I said to the doctor, is it working? He said, ‘the only way you can tell is if you go off it. If you go off it, I can’t be responsible for what happens,’ the doctor said. So I’m still on it.”
The pandemic hurt a lot of people a lot of businesses, everything, he said.
“During COVID, I had people next to me who had it — but I never got it. Have MS, but people say I’m one of the healthiest guys they know,” he added. “I’m healthy and I feel good. I do a lot of walking here, I stay active.”
Lombardo also helps raise funds for the Multiple Sclerosis Resources of Central New York, Inc. He holds
the annual Bridie Manor Poker Walk, which this year takes place at 9:30 a.m. Sept. 9.
He has been doing the MS event for 10 years. “This will be our 11th year,” he said.
“Celebration of our 25th anniversary, which was 2012, I thought it would be a good idea to have an event. A fundraiser for MS because not only was it our 25th year of being in business but also it was my 25th year of being diagnosed with MS,” he explained. “25 and 25 … I was on their [Multiple Sclerosis Resources of Central New York] mailing list and everything. So I called them up I said what do you think? And they said let’s try.

“We had it the first year and it was a huge, huge success.

They were a little surprised and
I was a little surprised and now it’s just an every year event. We’ve had 120, 130 people take part — a lot of supporters out there.”
The event has raised more than $50,000 over the years.
“I’ve got a sheet of paper that says ‘in recognition’ of the event. I’m not looking for any recognition, I’m a humble guy. It is what it is — you know I’m just looking to help out society, help out the people who need help.
“The MS group helps people. They give walkers, they give people canes. It’s the right thing to do. I have the facility to do it with. I’m just glad to help in some way.”
For more information about the Poker Walk event, call 315-438-4790 or 1-800-975-2404.
The heart remains a remarkable organ at the center of our bodies that provides life and vitality.
The biological marvel is responsible for pumping blood and oxygen through our bodies. Ensuring heart health can be paramount to overall well-being even with healthy individuals.
That was the case recently when Los Angeles Lakers superstar Lebron James’ son, Bronny, suffered a cardiac incident. While details of the situation remain private, it shows the importance of having your heart health checked, recognizing family history and taking care of yourself.
One person dies every 33 seconds from cardiovascular disease, according to the Centers for Disease Control and Prevention.
“The heart is the main organ that provides blood flow to your organs and muscles. It’s essential that you take care of it because you can have a deteriorated quality of life with poor heart health,” said Thomas Grady, a board-certified cardiology specialist in Oswego Health.
Grady discussed five essential things to know about cardiac health.


Often called the engine of the body, a healthy heart ensures the efficient delivery of oxygen and nutrients to all cells, tissues and organs and maintains their proper function. A robust cardiovascular system contributes to increased energy levels, a stronger immune system and an overall enhanced quality of life. On the other hand, neglecting heart health can lead to a host of serious
conditions including heart disease, heart attacks and strokes.
Strong heart health starts with movement. Being physically active can improve your brain health, help manage weight, reduce the risk of disease, strengthen bones and muscles and improve your ability to do everyday activities, according to the Centers for Disease Control and Prevention.
“You need to establish an exercise program in your life,” said Grady. “You should prioritize frequency over intensity. Even a 30-minute walk every day or five days a week can do wonders. Exercises such as swimming, jogging, the elliptical machine or StairMaster can be effective ways for consistent movement that benefits the heart.”
In addition, he suggests eating lean meats, fruits and vegetables. He believes in the adage of what you eat and how you eat will determine your future heart issues.
“It’s important to emphasize the types of foods that we eat that we already know are good for you. We also need to focus on habits because you have people who are grazers who eat throughout the day constantly which doesn’t give your body enough time to digest anything,” said Grady. “Then you have people who tend to eat late at night and that habit can contribute to overweight and bad routines.”
Several heart-healthy myths continue to permeate society. Anything from the idea that women don’t really suffer from heart attacks to
heart ailments only being an older person’s disease are often perceived as fact.
“One of the myths is doing something bad — whether it is in diet or lifestyle — a few times won’t really cause damage. The problem with that philosophy is that people rarely do the wrong thing once,” said Grady.
Another myth he sees is people not connecting peace of mind to heart health.
“I tell people you need to meditate or pray because being at peace is a good thing for your overall being. When you are stressed, it affects many organs in your body, especially your heart. Your exterior life can affect your interior body and we too often don’t recognize the connection,” Grady said.
Prioritizing heart health is a fundamental aspect of maintaining overall well-being. Understanding the symptoms and addressing the factors that contribute to cardiac issues continues to be an essential step toward a healthier heart. When James’ son, Bronny, had a cardiac arrest, it shocked the sports world and the casual observer.
“It is not uncommon for sudden cardiac incidents or death to occur in young athletic men. Sometimes you never know they had a heart problem until the incident occurs. They were able to get to him quickly to resuscitate his heart,” said Grady. “There are
many examples of athletes who died because there was an unknown heart issue.”
4.Bad behavior Recognizing the early signs of potential heart problems is crucial for prompt diagnosis and effective treatment. Common symptoms include chest discomfort, which manifest as a sensation of pressure, squeezing or pain in the chest. In addition, shortness of breath during mild physical activity or while at rest could be indicative of heart problems.
“Smoking destroys the elasticity of your heart. People often talk about the effects that it can have on your lungs, but it can be detrimental to other areas of your body because nicotine can restrict the blood vessels and flow. When any kind of restriction occurs, plaque can form,” said Grady.

5.Good choices early on Grady said because it is very difficult to turn back the clock on a weakened heart, people should look to make good choices early on so they become routine.
“While it is never too late to establish healthy habits, I encourage parents to focus on their child’s health early on in elementary school. That is where you plant the seed of nutrition, emotion, personality, determination and habits,” said Grady.
A Q&A with personal trainer coordinator Will Masiclat

Q: Many people have heard about Pilates but may not know what it is. Can you tell us exactly what Pilates is?
A: Pilates is a mind-body exercise discipline that focuses on breathing and control of movement. Developed by Joesph Pilates, the exercises are designed to strengthen muscles, improve flexibility and mobility and improve overall health. With regular practice, participants can expect to feel stronger, move more gracefully, and stand or walk for longer periods of time. Exercises are low impact and suitable for all ages, with modifications implemented as needed.
Q: What type of Pilates does JCC offer?
A: The JCC already offers regular mat Pilates classes on the recurring Group Fitness schedule. With mat Pilates, exercises are done using only body weight for resistance. With the reformer, resistance is added to exercises via straps and springs that allow for deeper connection to the movements. Props are used when appropriate in both mat and reformer.
Q: How do you take advantage of Pilates at JCC?
A: All fitness members have access to mat Pilates class with their membership! Pilates reformer training is offered either privately or as a duet with another participant. Reformer sessions are booked by appointment only. Contact the JCC today for more information on membership or booking a reformer session!
You may love high-intensity interval training for its quick calorie blast. However, HIIT also provides benefits to your heart.
“HIIT is one of the best ways to increase and sustain cardiovascular health through exercise in the sense that the idea is to bring your heart rate up quickly to a high degree and then let it recover,” said Jill Murphy, personal trainer and co-owner of Mission Fitness in Syracuse. “So your heart rate is fluctuating between the heart rate maximum and a much slower more recovered heart rate, also known as a resting heart rate. Allowing you to push yourself to such a degree is actually one of the best ways to bring yourself to cardiovascular health through exercise alone.”
Of course, someone who’s sedentary should not engage in HIIT, as it’s pretty intense.
HIIT involves working as hard as possible for 15 seconds at a physical movement, such as jumping jacks, riding a stationary bike or running on a treadmill and then taking a break for 10 seconds before engaging in a different activity. The times vary, depending upon the HIIT program. Some involve working hard for 30 seconds and rest for 30. The whole session could be as short as 15 to 20 minutes.
Murphy follows physician Joseph Mercola, an alternative medicine proponent, who posted on his website an interview with Olympic coach Phil Campbell who explained that the best way to produce cardiovascular health through exercise is by using a specific modality of HIIT.
 Will Masiclat Personal Training Coordinator
Will Masiclat Personal Training Coordinator


wmasiclat@jccsyr.org

(315)445-2360 ext 144
5655 Thompson Rd, Syracuse NY 13214
“He trains his athletes to do what’s called a ‘sprint 8’ protocol, where you go as fast as you can on the elliptical or treadmill or stationary bike for 30 seconds getting your heart rate up as high as you can, then recovering for one and a half minutes, and repeating that for eight times.”
By Deborah Jeanne SergeantMurphy added that HIIT can help lower body fat, increase energy and improve speed and performance.
HIIT is definitely a hit for timecrunched people who cannot cram in hour-long workouts into their schedules.

“I think people have realized that they can knock out in 30 minutes more calories and get in better shape than just going for a walk with a coworker for 30 minutes,” said Randy Sabourin, owner of Metro Fitness in Fayetteville and Syracuse. “It is very effective of conditioning the cardiovascular system. You need just three to four days a week.
“The other thing that people should know with HIIT is you get a big after burn. When you move you burn calories, but the higher the intensity, the resting metabolic rate will stay higher after you’re done.”
HITT’s exertion on the heart helps it become stronger and supports its good health. Sabourin explained that since the heart is a muscle, working it harder can help increase its strength.
In addition, “HIIT training will make you breathe heavily, so it forces the heart to push circulation,” he said. “You can make up a HIIT routine with calisthenics and body weight.”
At his clubs, a HIIT workout could include air bikes, weighted sleds, rowing machines, tire flips, sand bags, medicine balls, and kettle bell swings.
“Typically, people perform a movement for 30-45 seconds as high as they can tolerate with a 15-20 transition to the next station,” Sabourin said. “You do a circuit for 30-45 minutes like that and it produces a pretty good result.”
As with any exercise regimen, it’s vital to ensure capability of performing it before engaging in it. HIIT can be scaled down to the participant’s level of fitness.
ADVERTISE IN THIS SPECIAL EDITION
Stages: Understanding the stages of breast cancer: 0, 1, 2, 3 and 4 | Screening: Breast cancer screening: Is it worth if you’re over 70? | Diagnosis: Older women’s is often overdiagnosed, raising risk of unnecessary treatment: study | Fertility — When are women most likely to conceive? Understanding “fertile windows.” | Contraceptive: The FDA just approved the first overthe-counter oral contraceptive | Early Menopause: What are the signs and what can women do to mitigate its effects?

Fatal heart disease in the United States dropped about 4% a year between 1990 and 2019, but Americans need to quit smoking, drinking and overeating or those gains could be wiped out, according to new research.
The declining rates of fatal heart disease have stalled, according to the research from Rutgers University-New Brunswick in New Jersey.
“The overall numbers are good. We saw a substantial decline in deaths from all types of coronary heart disease for both females and males,” said study lead author Cande Ananth, chief of the division of epidemiology and biostatistics in the department of obstetrics, gynecology and reproductive sciences at Rutgers Robert Wood Johnson Medical School.
“However, because we examined how these three modifiable risk factors affected mortality rates, we can see that there is room for considerable improvement,” he said in a Rutgers news release.
Among people aged 25 to 84, deaths from heart disease fell from more than 397,000 deaths in 1990 to about 237,000 in 2019, even while Americans' median age increased from 33 to 38, the researchers found.

Among men, the death rate dropped 3.7% a year, while women saw a 4% annual decline during those years.
Those declines, however, slowed significantly between 2011 and 2019. People born after 1980 were even at slightly increased risk of dying from coronary heart disease at any age than people from the previous generation, the researchers said.

Future advances in treatment could continue reducing fatal heart disease, but lifestyle modifications are also important: Eliminating smoking, drinking and obesity would have prevented half of the deaths observed during the study period, the authors said.
A bright spot is that tobacco usage is trending downward, with the percentage of smokers falling from 26% to 14% during those years.
Yet, obesity rates rose sharply from 12% in 1990 to 43% in 2019. Alcohol use also rose slightly during the study period.
Besides reduced tobacco use, researchers credited cholesterol-lowering statins and better diagnostic tests with the reduction in heart deaths. The study findings were published recently in the American Heart Journal.
 By Anne Palumbo
By Anne Palumbo
Quinoa (pronounced KEENwah) is a whole grain whose popularity has skyrocketed in recent years. Beyond being delicious, versatile and easy to prepare, quinoa is so nutritious that NASA feeds it to crews on long space missions.
Considered a bona fide superfood by many, quinoa serves up a powerful mix of desirable nutrients, many of which have been linked to the prevention of disease.
Let’s take a look at four good reasons to embrace this healthy whole grain.
1. Higher in protein than most whole grains.
Quinoa not only packs a whopping 8-9 grams of protein per cooked cup, it delivers protein that’s “complete,” which is uncommon among grains. Complete proteins contain all nine essential amino acids (protein’s building blocks) that your body can’t make on its own. Feeling sluggish, weak, under the weather? You may not be getting enough protein.
2. Loaded with heart-healthy fiber.
Quinoa delivers 5 to 6 grams of fiber per cooked cup, putting a sizable dent into the recommended 25 to 30 total grams we should be eating daily. Fiber keeps us regular, lowers cholesterol levels, helps prevent spikes in blood sugar after eating and may help us live longer. Studies suggest that increasing your fiber intake—especially from whole grains—is associated with a reduced risk of dying from heart disease and some cancers.
3. Packed with important vitamins, minerals, and antioxidants.
Regularly eating quinoa can help meet your needs for a wide variety of vitamins, minerals and phytochemicals (antioxidants that reduce inflammation and promote
longevity). Quinoa’s top five include folate, manganese, magnesium, phosphorous and zinc, all of which come together to help build bones, keep our immune system humming, promote healthy cell growth (crucial during early pregnancy), manage blood pressure and so much more.
4. Great for people with gluten intolerance.
Unlike most whole grains (though quinoa is technically a seed, like buckwheat), quinoa is gluten-free. What sets it apart from some gluten-free substitutes in grocery stores—many of which are made from refined starches and may have added sugar, fat, and salt—is its bounty of nutrients coupled with its paucity of fat, sugar, sodium, and cholesterol. Go, quinoa! Go, happy gut!

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

Some quinoa needs to be rinsed to remove the bitter-tasting compound that naturally coats it. Although most packaged quinoa bought in the U.S. comes “prerinsed,” I always rinse mine under cold water for a few minutes, using a fine sieve. Also, quinoa is pretty high in oxalates, which may cause concerns if you have kidney issues. Cooked quinoa, stored in an airtight container, can last up to a week in the fridge.

Serves 5-6
1 cup quinoa, rinsed, drained
2 cups water
½ cup pitted Kalamata olives, quartered
½ small red onion, thinly sliced (optional)
1 cup cherry tomatoes, halved
1 medium cucumber, peeled, seeded, diced
1 cup crumbled feta, divided ½ cup basil, slivered juice of 1 lemon
1/3 cup olive oil
2 teaspoons Dijon mustard
1 clove garlic, minced ½ teaspoon kosher salt ¼ teaspoon coarse black pepper
1. Place the quinoa in a saucepan with the water; heat to a boil. Reduce to a simmer, cover and cook until all the water is absorbed (about 15 minutes). Set aside.
2. Place the olives, onion, cherry tomatoes, cucumber, ¾ cup feta and basil in a large bowl. Add quinoa; stir gently to combine.
3. Whisk together the lemon juice, olive oil, mustard, minced garlic, salt and pepper. Pour over the quinoa mixture; toss to combine. Let stand at room temperature for an hour before serving. Refrigerate for longer keeping. Stir gently before serving.
Sprinkle each serving with remaining feta crumbles.
September 14, 2023 from 9am - 1pm

CNY Regional Market E Shed 2100 Park Street, Syracuse, NY
Enjoy



















Millions of Americans are addicted to drugs or alcohol, and millions more struggle with an addicted family member or friend, a new poll finds.
Two-thirds of those surveyed said either they or a family member have been addicted to alcohol or drugs, been homeless because of an addiction, or overdosed or died from drug use.
Moreover, 19% say they themselves have been addicted to drugs or alcohol, had a drug overdose or were homeless because of an addiction.
“It’s pretty surprising to think about when we talk about addiction and issues with drugs and alcohol, we typically talk about them as isolated incidents,” said Ashley Kirzinger, director of survey methodology at KFF (formerly known as Kaiser Family Foundation).
“I think what we’re seeing in this is that it’s not isolated,” she said. “It’s impacting almost a majority of American families and when we ask about the impact that it’s had on them, a large share say that addiction issues have had an impact on their mental health and their family’s financial situation. It’s pretty surprising to think about how pervasive of a problem it is in the U.S.”
Addiction is affecting everyone, regardless of where they live, regardless of their household income, she noted.
“There isn’t a typical person with addiction problems. It seems like it’s affecting families regardless of their race and ethnicity, regardless of their income and regardless of where they live,” Kirzinger said.
Addiction has been seen in 42%
of people in rural areas and 33% of white adults, she added. Yet, many people aren’t getting help. Only 46% of those with addiction in their families say that person got treatment. Among white adults, 51% got treatment, compared with only 35% of Black and Hispanic adults.
Families affected by addiction say it has damaged family relationships (76%) and mental health (70%), while it stresses family finances (57%).


Many families are also worried that their addicted loved one will overdose or unintentionally use the dangerous and potent drug fentanyl.
On the positive side, Kirzinger
said more people polled said their doctor (57%) talked to them about the pitfalls of prescription opioids, including the danger of addiction. Doctors (60%) were also more likely to offer alternative medications to manage pain, she said.
Kirzinger also noted that both Democrats and Republicans support addiction treatment centers in their community (90%) or making the drug Narcan (naloxone), which can reverse an opioid overdose, available for free at bars, health clinics and fire stations.
The poll of over 1,300 U.S. adults was conducted from July 11 to 19 either online or by telephone.
“These findings are not surprising,” said Robyn Oster, senior research associate of health law and policy at the Partnership to End Addiction. “With over 110,000 overdose deaths predicted in 2022 and more than 46 million people reporting having substance use disorder in 2021, it is inevitable that so many people would have family members impacted and be concerned about the mental health and addiction crises. Pervasive stigma and underinvestment have predictably led to a lack of access to needed services.”
Oster said that prescription painkillers are a driver of the opioid epidemic.
“A 2013 study found that four in five people who use heroin misused a prescription opioid first, and that was a big contributor to how this overdose crisis started,” she said. “As those prescriptions became more difficult to get, due to prescribing enforcement, cost or other factors, people switched to heroin and other illicit drugs, and now increasingly fentanyl.”
Yet, nearly half of people who misused a prescription pain reliever got it from a friend or relative, either by being given them, buying them or taking them without asking, Oster noted.
“Some people start using substances to self-medicate or in a social setting,” she said. “With the increasingly deadly drug supply, substance use can be dangerous even before someone is addicted.”
Oster said that given the size of the crisis there are not enough resources to support people affected by addiction.
“We know, both from this poll and from other national data sources, that far too few people with addiction receive any care, and even fewer receive quality care, including medications for addiction treatment,” she explained.

Eight healthy habits could add years to your life.
A new study of more than 700,000 U.S. veterans breaks down the habits that when adopted by middle age, can help someone live substantially longer than folks who don't have these habits.
These are the big eight:
• Be physically active.
• Don't smoke.
• Don't get addicted to opioids.
• Don't binge-drink on a regular basis.
• Eat a healthy diet.
• Manage stress.
• Practice good sleep habits.
• Maintain positive social relationships.
The study found that men with all those habits at age 40 could live an average of 24 years longer than men who have none of them. Women could gain an additional 21 years compared to their peers who have none of these habits.
The findings were presented in July at a meeting of the American Society for Nutrition, in Boston.
“We were really surprised by just how much could be gained with the adoption of one, two, three or all eight lifestyle factors,” said
study presenter Xuan-Mai Nguyen, a health science specialist at the U.S. Department of Veterans Affairs and student at Carle Illinois College of Medicine in Urbana, Illinois.
“Our research findings suggest that adopting a healthy lifestyle is important for both public health and personal wellness. The earlier the better, but even if you only make a small change in your 40s, 50s or 60s, it still is beneficial,” Nguyen said in a meeting news release.

Researchers used data from medical records and questionnaires collected between 2011 and 2019 from more than 719,000 participants in the VA's Million Veteran Program. This included adults aged 40 to 99 and included more than 33,000 deaths during follow-up.
Low physical activity, opioid use and smoking had the biggest impact on life span among the study participants. These were associated with a 30% to 45% higher risk of death during the study period.
Stress, binge-drinking, poor diet and poor sleep habits were each linked to about a 20% increase in the risk of death. A lack of positive social relationships was associated with a 5% increased risk of death.




Researchers said their findings highlight the role of lifestyle factors in chronic diseases such as Type 2 diabetes and heart disease that lead to premature disability and death. These results also help quantify the degree to which healthy lifestyle choices can help people reduce their disease risk and live longer.
“Lifestyle medicine is aimed at treating the underlying causes of chronic diseases rather than their symptoms,” Nguyen said. “It provides a potential avenue for altering the course of ever-increasing health care costs resulting from prescription medicine and surgical procedures.”
While adopting the healthy lifestyle factors had a smaller impact for those who were older, that impact still was significant.
“It is never too late to adopt a healthy lifestyle,” Nguyen said. Although the study can't prove cause and effect, the findings align with a growing body of research supporting the role of lifestyle factors in preventing chronic diseases and promoting healthy aging.

Findings presented at medical meetings are considered preliminary until published in a peer-reviewed journal.

Although fall prevention is important, keeping bones strong in case of a fall represents another vital strategy for avoiding bone breaks.
Strong bones rely on a few key areas. Strong bones require a proper diet, which may need supplementation.
“Our bones are in a constant balance of break down and build up,” said Sharon Brangman, chairwoman of geriatric medicine, director of the geriatric medicine fellowship program and director of the Upstate Center of Excellence for Alzheimer’s Disease at SUNY Upstate Medical University.
She recommends taking a supplement of calcium citrate, about 1,000 to 1,200 mg. daily.
“Calcium carbonate isn’t absorbed as well and can cause constipation,” she said. “Divide the calcium over different parts of the day; your body doesn’t absorb it at once.”
Dietary sources of calcium include milk, cheese and yogurt. For those with lactose intolerance — which includes many middle-aged and older adults, lactose-free milk and aged cheese is often well-tolerated.
“Lactose-free milk doesn’t taste any different from regular milk,” Brangman said.
Some fortified foods such as calcium-fortified orange juice may include milk solids so read the label. Non-dairy sources of calcium include sardines with bones, leafy green vegetables, certain nuts, dried fruits and figs.
“Avoid sodas,” Brangman added. “The phosphoric acid can interfere with calcium absorption.”
Don’t displace nutritious foods with nutrient-void choices. A care provider can recommend the right amount of calcium and other nutrients, as the exact amount needed depends upon age, gender and other factors.
Kristine Cervantes, doctor of physical therapy and professor of practice in the department of occupational therapy at the Purcell School of Professional Studies at Le Moyne College, said that overall health, including healthy bones, “involves a good balance of diet, exercise, sleep and lifestyle.”
In addition to calcium, Cervantes recommends vitamin D.
“For calcium to be absorbed, we need vitamin D, which our bodies can produce through our skin and exposure to sunlight,” she said.
She listed as vitamin D sources: oily fish such as salmon, sardines and mackerel; egg yolks and liver.
“Like calcium, many foods are fortified with vitamin D such as milk, orange juice and cereal,” Cervantes added. “Other nutrients required for good bone health include phosphorus (found in dairy products and meat), magnesium (bananas, nuts and avocados), vitamins A (eggs, green leafy vegetables, carrots), K (leafy greens, avocado) and C (citrus fruits).”
She emphasizes stimulating bones to become stronger through weightbearing or impact activity such as walking, running, tennis, pickleball, dancing, or anything that requires weight to be placed on the bones.
“Swimming, while an excellent exercise for endurance and flexibility, would not be an example since the bones do not take on the weight of
the body,” Cervantes said. “Another form of exercise to stimulate and stress the bones is through muscle training exercise. These can include body weight exercises such as squats, pull ups or push-ups as well as weight machines, resistance bands or free weights.”
Building muscle stresses bones so that bones build back stronger.
People with osteoporosis are losing bone at a faster rate than they’re replacing it with new bone, so Cervantes recommends low-impact exercise such as walking or using resistance bands.
“This process of ‘bone remodeling’ is a major reason why therapists promote early mobility after injury or during hospitalization,” Cervantes said. “Prolonged bedrest or inactivity weakens bones. Injury or illness or not, don’t be a couch potato if you want strong bones.
“It is also interesting to know that we can influence bone strength at a young age by engaging in activities that involve weightbearing and strengthening. Doing so can build up a reserve of bone density to prepare for the aging process when the remodeling process may change, and breakdown and buildup of bone is not equalized.”
Excellus BlueCross BlueShield is once again inviting nonprofit organizations to apply for 2023 Health Equity Innovation Award (HEIA) funding. The awards help fund health and wellness programs that address racial and ethnic health disparities in Upstate New York. The online application period closes at 11:59 p.m., Sept. 14.
“Excellus BlueCross BlueShield Health Equity Innovation Award funding aims to support initiatives, programs, and research that specifically target and address the root causes of health inequities, with a focus on addressing structural racism. We believe that by investing
Deadline
in projects that tackle the underlying social, economic, and systematic factors that contribute to health disparities, we can work towards creating a more just and equitable healthcare system,” says physician Lisa Harris, senior vice president and chief medical officer, Excellus BlueCross BlueShield.
All 501(c)(3) organizations in Ex-
cellus BlueCross BlueShield’s service area are invited to apply for Health Equity Innovation Award funding up to $30,000.
Application proposals for innovative initiatives or projects that have proven data outcomes and can be expanded will be considered. Proposals must include clear, defined goals for reducing health disparities and the burden of health inequities and social disadvantages. Organizations will be required to specify how funding will measurably assist in improving racial and ethnic health equity outcomes.
Health Equity Innovation Award categories include, but are not limited to:
In addition to eating right and engaging in weight-bearing exercise, Cervantes said that some choices negatively affect bone health:
“
1. Alcohol: Blocks calcium absorption and disrupts the bone remodeling process. Not only does it weaken bones but can slow the healing process after a fracture. Chronic alcohol use can disrupt hormones needed for bone health.
2. Salt: reduces calcium content by increasing its excretion through the kidneys.
3. Soda: phosphoric acid draws calcium from the bones; caffeinated sodas are a double whammy.
4. Coffee, Tea with Caffeine: disrupts the absorption of calcium.”
Emotional stress also affects bone health. Poor coping mechanisms such as substance use and poor eating habits can harm health and cause bone loss. Internalizing stress increases the body’s fight-or-flight mechanism, which raises cortisol levels and inflammation.
When stressed, it’s important to get enough rest, exercise and healthful food along with using healthful means of coping, such as engaging in an enjoyable hobby and talking with a trusted friend.
Reducing health disparities in racial, ethnic, LGBTQIA+ communities, people with disabilities, people living in rural or urban communities, or other groups of people that may be at a higher health risk for:
• Medical issues and conditions (chronic or acute)
• Behavioral health or mental health conditions
• Negative outcomes from the above, including death or suicide
According to the Centers for Disease Control and Prevention, 28% of Americans 65plus will fall this year.
The National Institutes of health reports “Falls in older adults are a common occurrence and may lead to serious injuries (like head injury and fractures). Recurrent falls are also frequent and are responsible for significant morbidity and mortality in older adults.”
The consequences of falling are great for people who cannot rise and lie on the floor injured for hours or even days. What often happens after a fall and serious injury is that older adults remain less active because they’re recovering from the fall. Or they choose to reduce their activity level because they fear another fall injury.
Reducing activity level also leads to greater dependence upon others for activities of daily living. Ideally, preventing falls is better than trying to introduce fall reduction measures after a fall has occurred.
Environmental factors can make a big difference in preventing falls.
“The big one we see are patients who live in older homes with the washer and dryer in the basement and steep steps, which are especially hazardous if carrying a laundry basket,” said physician Sharon Brangman, chairwoman of geriatric medicine, director of the geriatric medicine fellowship program and director of the Upstate Center of Excellence for Alzheimer’s Disease at SUNY Upstate Medical University.
She wants patients to have their washer and dryer moved up to the first floor, if possible. It’s also important to keep stairs in good repair and eliminate carpets or runners on stairs.
“You also want them well-lit at night and have handrails,” Brang-
man said.
She added that household spills and clutter can also contribute to falls.
“Keep the floor dry and pick up things that are a trip hazard,” she said. “If your feet stick, that’s a trip hazard. Be careful about sneakers with thick treads and cushion. It can change your perception of where your foot is. Some people don’t lift their foot as high while walking as they get older. Sometimes thinner soled shoes are better for walking. Avoid heels. Make sure that the soles are rubber, so they have some traction.”
Shoes with medium to high heels, open backs and ill fit can often contribute to falls.
When Mike Ritter, director of Rehabilitation for PACE CNY of Loretto, assesses a living space for falls, he looks for throw rugs and poor condition carpeting.
“Does it fold up on the edges?” he said. “Some carpets are old and worn and have flipped up on the edge over time. That may mean removing area rugs or using tape on the edges to hold them down.”
Bath rugs should be non-skid and hung up once no longer in use. Grab bars in the bathroom and maybe along a long hallway can also help, but one doesn’t need to “put grab bars anywhere,” but rather use “strategic placement of grab bars,” Ritter said.
Typically, near steps, the tub or shower and near the toilet are the key places. A floor-to-ceiling transfer pole can help getting in and out of bed. A transfer bench can also help people bathe more easily.
“They can sit first and then swing their legs in,” Ritter said. “Once you’re in, you can stand up to clean properly, using the grab bar in
the tub. It can be useful and helpful for that.”
Handrails at home entrances and grab bars — not the suction cup kind — near the tub and toilet can also reduce falls. These should be installed by a pro and sturdy enough to support an adult’s weight. Towel bars are not enough.
Most people require more lighting to see well as they grow older. To help mitigate this effect, Ritter recommends contrasting duct tape on steps and sufficient lighting over staircases. Motion sensing lights can illuminate the pathway to the light switch. For homes with insufficient outlets, battery-operated and solar lights can help.
The raised threshold between rooms or uneven flooring on a patio or porch can cause falls, as can stairs, since people don’t perceive the difference in height. Contrasting tape on steps to make these transitions easier to see.
Along with changes in vision, many people experience changes in balance as they age. For this reason, medication that was fine before may now dramatically increase risk for falling.
Kristine Cervantes, doctor of physical therapy and professor of practice in the department of occupational therapy at Purcell School of Professional Studies at Le Moyne College, wants older adults to ask their healthcare provider about their medication, including “psychotropic medications — antidepressants, antianxiety, mood stabilizers,” she said.

Another commonly overlooked aspect of fall prevention is assistive devices. Ironically, a cane or walker can contribute to falls if it’s not the right device, adjusted correctly or maintained.
“An occupational or physical
therapist can properly prescribe and size as well as teach proper use of any assistive device,” Cervantes said.
Patients in New York do not need a prescription or referral from a doctor to see a physical therapist for 10 visits or 30 days. A physical therapist can help with assistive devices, provide fall risk assessment and help patients reduce fall risk through exercise.
Cervantes recommends that people stay active to prevent falls, as this helps maintain muscle mass, bone strength, agility and balance.
“Choose an activity or exercise or a few that you enjoy and incorporate into a daily routine and stick with it,” she said. “Continue to challenge yourself with new or different activities. Incorporate balance and strength exercises. Try yoga or tai chi, which has been shown to very effective at reducing falls.”
Many older adults reduce their activity level because they fear falling. Instead, Cervantes recommends creating a plan in case of a fall, including practicing how to get up off the floor and having a friend or neighbor check in regularly. Using devices can also summon help more quickly.

“Emergency response systems are very common,” Cervantes said. “They are activated by pushing a button on a wearable device such as a necklace or wristband and are directly connected to 911 services. However, there is a fee. Carrying a cell phone is another option, but with smart devices ever so common, setting up a voice activated call system like Alexa is an excellent and reliable option to either call family, friends or emergency services.
“Smartwatches can even be set up to make emergency calls at the push of a button and others can even detect sudden fall-like movements and automatically call for help. These smartwatches also have fitness tracking capability with free apps that can help people choose and stay motivated with activities and exercise,” Cervantes said.
She also said some free apps can help with fall assessment, like HCPA StopFalls, Senior Safety Quick Fall Screen.

Although pets bring many mental and physical health benefits, some older adults find caring for their cat or dog more challenging than it used to be. Fortunately, area resources can make it easier for them to enjoy their pets and keep up with their animals’ care.
“Pets are really, really important,” said Sharon Brangman, chairwoman of geriatric medicine, director of the geriatric medicine fellowship program and director of the Upstate Center of Excellence for Alzheimer’s
By Deborah Jeanne SergeantDisease at SUNY Upstate Medical University. “As with everything, there are pros and cons.”
Brangman had a patient whose leashed dog bolted after a squirrel. This caused the patient to fall and dislocate her shoulder.
“If you have a big dog, you need some obedience training,” Brangman said. “You need to have a good relationship with a groomer and someone who can walk your dog, especially in winter, when it’s icy.”
To minimize the risk of tripping,
Brangman recommends a light-up collar or bell for the pet’s collar so it’s easier to navigate around it.
For some patients, a fixed budget can make caring for the pet challenging. Brangman recalled a patient who continued to lose weight even while receiving Meals on Wheels because as it turned out, she was feeding food meant for her to her dog.
“Some Meals on Wheels now provide pet food,” Brangman said.
One source of pet assistance could include non-medical domestic help. Some of these services will scoop litter boxes, transport pets to vet and groomer appointments and feed animals, but typically do these as an add-on service for people already needing services such as errand transportation, light housekeeping, organizing and decluttering, and companionship. Otherwise, it likely would not be cost-effective.
Automation to streamline pet care, such as automated feeders, waterers and cat box can reduce the frequency of these pet care chores.
Buying the right products can help also, such as light weight litter or small pack ages of litter if carrying
25-pound containers is too difficult. Clumping litter can reduce the frequency of lifting a full litterbox to dump it, as it’s easier to scoop out soiled clumps and conserve the remaining clean litter. Many online companies like Chewy.Com will regularly deliver products right to the doorstep, reducing the need to heft bags of food and litter.
Whether a professional service or a responsible neighbor kid who wants to make some money, hiring a dog walker can reduce pet care work while still providing exercise and stimulation to a dog. Dog waste removal services can make yard clean-up easier.
A vet who performs house calls and a mobile groomer can help people who struggle to transport their pet. Laura Hearn, owner of Sherlock Bones Mobile Grooming in Syracuse, travels to groom clients’ 25 pounds or smaller dogs.

“Many senior living facilities allow seniors to bring their pets, which is awesome — for all parties involved, including the pets. But finding transportation to the vet or groomer can be a little tricky,” Hearn said.
Some dogs are too big to easily transport, for example. And for older adults who no longer drive, it can be challenging to find public transportation that accepts pets.
“I can do all the services right in their home,” Hearn said. “I don’t offer any veterinary or dog walking services, but I can certainly point them in the right direction. Many of my senior clients even opt to get their own hair done at the beauty salon on the same day as their dog’s so they can both feel pretty.”
To transport pets to the vet or groomer, services such as Huckleberry & Co. in Syracuse provide “pet taxi” assistance. Owner Olivia Harris said that the service includes going in with the pet and obtaining all the information that the vet or groomer wants to pass along to the owner.
“One of the biggest services we do is dog walking for people working at home, people not at home and seniors,” Harris said. “We’ve had plenty of clients over the years for people who want us to come give their dogs stimulation. Their dog is still getting the right amount of exercise and stimulation. If they don’t get that long-term, it will create serious behavioral issues. It’s a huge carryover effect as a dog being rambunctious to eventually resource guarding and it doesn’t have a good relation-
In addition, Harris offers training and in-home care, such as pet sitting, scooping litter, administering oral medications or insulin, feeding and watering.

Alzheimer’s is an incurable degenerative disease of the brain. However, people diagnosed with Alzheimer’s can benefit from exercise.
A growing body of research indicates that in addition to offering some protective advantages, regular exercise can also slow the disease’s progression for those who have been diagnosed.
A 2022 study indicates that exercise helps promote the level of a brain-protective protein that can
delay onset of Alzheimer’s and other dementias and slow the progression of the disease in those diagnosed.
The study’s author, Kaitlin Casaletto, is an assistant professor of neurology in the Memory and Aging Center at the University of California San Francisco, said that other studies show physical activity lowers the chances of dementia by 30% to 80% but researchers still don’t know exactly why except that it may have to do with synaptic functioning.
“There has been research that
shows exercise is the number one thing we can do for supporting brain health, for preventing disease and those diagnosed seem to do better when they exercise,” said Sharon Brangman, chairwoman of geriatric medicine, director of the geriatric medicine fellowship program and director of the Upstate Center of Excellence for Alzheimer’s Disease at SUNY Upstate Medical University. “We don’t know all the details yet and it doesn’t keep the disease from progressing, but it can help you function at the highest cognitive level you can.”
She said that regular exercise helps increase circulation. Because nerve growth factors exist in the bloodstream and exercise helps take this to the brain to make new nerve connections.
“There are a lot of benefits of taking a walk,” she said. “I encourage patients to get up every hour and walk a few loops around their house.
Pick the parking spot a distance from the store. If you can handle stairs, use them instead of the elevator. Think of little ways of adding motion and walking into your daily routine.”
She recommends mall walking to patients once the weather turns icy or if they don’t have a safe neighborhood in which to walk.
“Exercise is probably the number one thing you could do to maintain your overall health,” Brangman added.
Body condition can decline with people who have been diagnosed with Alzheimer’s. To battle this effect, Mary Koenig, administrator of The Heritage Memory Life Community at Loretto and board member of The Alzheimer’s Association of CNY, encourages people to exercise, including strength training.
“Strengthening muscles is good for balance and mobility problems,” Koenig said. “It can help promote a normal day or night routine that can help when people get days and nights mixed up. It’s difficult for them and their caregivers. It can help with sleep and mood. It can in some cases decrease the need for behavior modifying medications.”
She also referenced studies indicating that exercise can slow the rate of decline and improve comorbidities like obesity, diabetes and heart disease.
“When diagnosed with dementia, you’re at an increased risk for falls,” Koenig said. “Anything to help with bone density is good, like weight bearing exercise. Strength building and yoga for flexibility helps decrease falls too.”
Of course, what a person does depends upon their physical condition and interests. Following a typical workout may not be feasible for someone with advanced dementia. But at any stage, finding enjoyable activities that increase movement, build strength and maintain balance are helpful in maintaining independence longer. Activities that include a body-mind connection, like ballroom dancing or tai chi may prove particularly beneficial.

Benefits of becoming a CAREPro

• Competitive Pay starting at $16.20 per hour

• CAREPro Referral Program
• Paid Time Off for illness/appointments
• Paid training and continued learning 24 hour Administrative support

any produce is a better choice than items like chips or candy. Snack on baby carrots, celery stalks or broccoli spears with hummus dip.
Whole grains are complex carbohydrates. Whole grain bread (not just “wheat bread” that’s dyed with caramel food coloring to look darker), popcorn, oatmeal, and whole grain crackers such as Triscuit are a few examples. But watch out for added salt, flavoring agents and sugar. Making your own foods, such as air popped popcorn instead of bagged popcorn can help you control what’s in your food.
Brangman also mentioned the Mediterranean diet as supporting heart and brain health.
Unfortunately, there’s no silver bullet for brain health. Avoiding Alzheimer’s and other forms of dementia isn’t as simple as, “Eat this and you’re guaranteed to never have dementia.”
But diet does play a role in supporting brain health.
“Alzheimer’s probably starts somewhere in our 30s and 40s,” said Sharon Brangman, chairwoman of geriatric medicine, director of the geriatric medicine fellowship program and director of the Upstate Center of Excellence for Alzheimer’s Disease at SUNY Upstate Medical University. “What you eat has a direct impact as to how you age when you’re older.”
She advised staying away from alcohol — it’s toxic for brain cells — and saturated fat, like butter, fried foods and whole fat cheese.
“Be careful about the amt of sweets you eat,” Brangman added.
“We see an association between diabetes and dementia. Minimize foods like white potatoes, white bread, white sugar, white pasta. Your body changes those to sugar. There’s increasing research looking at insulin resistance in the brain and how that might play a role in memory loss as you get older. Diets high in sugar are one way to get insulin resistance.”
Eating right can be tricky at times. Supplements can help ensure sufficient nutrient intake for overall good health. However, taking excessive amounts of supplements is not necessary.
“A recent study suggested a daily multiple vitamin may help but there is not much proof that supplements for ‘brain health’ are helpful,” Brangman said. “Maybe take one multivitamin a day. Especially for older people, it should not have iron in it. The only ones who should take a multi with iron are younger women

People who carry a gene that's associated with Alzheimer's disease may lose their sense of smell long before memory and thinking problems occur, a new study suggests.
This early sign of potential dementia is not seen in people who don't carry this gene, called APOE e4, researchers report July 26 in the journal Neurology.
"Testing a person's ability to detect odors may be a useful way to predict future problems with cognition," said researcher Matthew GoodSmith, a physician resident at the University of Chicago.
"While more research is needed to confirm these findings and determine what level of smell loss would predict future risk, these results could be promising, especially in
studies aiming to identify people at risk for dementia early in the disease," GoodSmith added in a journal news release.
For the study, the researchers surveyed more than 865 people about their ability to detect an odor and identify what they were smelling. Tests were given over five years. Those with memory or thinking problems were tested twice, five years apart. The investigators also took DNA samples.
People who carried the gene variant for Alzheimer's were 37% less likely to have good odor detection than people without the gene, the researchers found. Those with the gene experienced reduced smell detection from age 65 to 69. At that age, gene carriers could detect an average of about three of the test smells,
who are still menstruating.”
Ideally, most of the nutrients should come from dietary sources rather than supplementation. Brangman recommends a heart-healthy diet as it’s also good for brain health.

The American Heart Association’s heart healthy eating plan offers benefits for supporting brain and heart health. The organization’s website said that diet promotes, “a wide variety of fruits and vegetables; whole grains and products made up mostly of whole grains; healthy sources of protein (mostly plants such as legumes and nuts; fish and seafood; low-fat or nonfat dairy; and, if you eat meat and poultry, ensuring it is lean and unprocessed); liquid non-tropical vegetable oils; minimally processed foods; minimized intake of added sugars; foods prepared with little or no salt; limited or preferably no alcohol intake.”
A “whole food” is one with little or no refining or processing. It should also contain no artificial additives or preservatives.
Ideally, the fruit should be a whole piece, such as a peach but not a canned peach. But a peach canned in natural juices is a better choice than in heavy syrup. And
“That’s what the Alzheimer’s Association is pushing,” said Mary Koenig, administrator of The Heritage Memory Life Community at Loretto and board member of The Alzheimer’s Association of CNY. “It doesn’t include fatty foods, but more high-fiber, fruits and vegetables, lean on meat and more fish-based.”
According to the Mayo Clinic, the Mediterranean diet includes vegetables, fruits, whole grains, beans, nuts and seeds, olive oil and seasoning with herbs and spices. The Mayo Clinic further stated, “The main steps to follow the diet include: each day, eat vegetables, fruits, whole grains and plant-based fats; each week, have fish, poultry, beans, legumes and eggs; enjoy moderate portions of dairy products, limit how much red meat you eat; limit how many foods with added sugar you eat.”
“Obviously, there needs to be more research and no one is saying that if you eat all these things you won’t get Alzheimer’s or dementia,” Koenig said. “It’s complicated or else we’d have more treatments and a cure.”
Eating right should also be teamed with staying mentally and physically active, getting sufficient sleep and finding healthful ways to mitigate the effects of stress.
compared with about four smells for the people who lacked the gene, the researchers found.
People with the gene variant did not show a difference in the ability to identify what they were smelling until ages 75 to 79. Once the ability to identify odors declined, it declined faster than in those who did not carry the gene.
At the start of the study, think-
ing and memory skills were similar among the two groups. Not surprisingly, the researchers said, thinking skills declined more rapidly among those carrying the gene variant than among those without the gene.
"Identifying the mechanisms underlying these relationships will help us understand the role of smell in neurodegeneration," GoodSmith said.










Crouse Health has reached a rare milestone in the field of minimally invasive surgery –15,000 robotic-assisted procedures performed since the launch of the program in 2008.

The paper is free to you but very expensive to produce and distribute. Keep the publication going. Consider supporting it. If you are a reader, please become a paid subscriber. If you’re a nonprofit, a medical practice or organization, consider advertising. You will get a great


Since that time the robotics program at Crouse has expanded to include eight robotic systems, with seven da Vinci XI systems and the latest addition of a da Vinci Single Port (SP) system, the only one in Central New York.
The program’s 27 surgeons provide the procedures and technology that support a variety of medical conditions in a wide range of specialty areas, including general, bariatric, colorectal, thoracic surgery, GYN oncology, gynecology and urology.

“Our surgeons have been pioneers in robotic-assisted surgery for 15 years. This achievement highlights Crouse’s regional leadership in minimally invasive robotic surgery and reflects our dedication to improving
the lives of patients through leading-edge technology,” says Crouse President and CEO Seth Kronenberg, MD, speaking at a recent celebration for the robotics team.
The da Vinci surgical system integrates robotics and extremely sophisticated computer technology with the skills of the surgeon. The system allows surgeons to see and move in three dimensions, giving them the ability to perform delicate operations with greater precision but requiring only tiny surgical openings. By avoiding the large incisions of open surgery, this computer-assisted micro-surgery helps avoid many post-surgical complications while shortening patient recovery time.
“We’re proud of the program we have built in collaboration with many of the region’s top surgeons and look forward to utilizing this innovative technology to continue to improve patient outcomes,” says Kronenberg.
4920

What can you tell me about green funeral options? At age 80, I would like to preplan my funeral and make it as natural as possible.
Old EnvironmentalistGreat question! Green funeral options are becoming increasingly popular in the United States as more and more Americans are looking for environmentally friendly alternatives to traditional funerals. Here’s what you should know about “green burial” and “green cremation” options, along with some tips to help you locate services in your area.

If you wish to be buried, a green–natural burial will minimize the environmental impact by forgoing the embalming chemicals (which is not required by law), traditional casket and concrete vault. Instead, you’ll be buried in either a biodegradable container or shroud with no vault, and you won’t be embalmed. This allows the body to decompose naturally and become part of the earth.
If you want to temporarily preserve the body for viewing or a memorial service, instead of embalming, you can request dry ice or Techni ice, a refrigeration unit, or a nontoxic embalming agent.


You’ll also be happy to know that green burials are much cheaper than traditional funerals, which average around $8,000 in 2023. By scrapping the coffin, vault and embalming, which are expensive, you’ll save yourself several thousand dollars on your funeral costs.
To find green burial services in your area, a good first step is to see if there’s a certified green funeral home in your area and contact them. The Green Burial Council offers an online directory of providers and other resources at GreenBurialCouncil.org.
If there isn’t one nearby, your next step is to contact several traditional funeral homes to see if they offer green funeral service options — many do.

You’ll also need to find a green cemetery. There are nearly 100 green cemeteries throughout the U.S., along with more than 300 traditional (hybrid) cemeteries that offer green burials too. To find them, the New Hampshire Funeral Resources, Education and Advocacy website has a list at NHfuneral.org. Or, if you own rural property you may be able to have a home burial there, if your state and county allow it.
If, however, there are no green cemeteries nearby you can still make
your burial more environmentally friendly by not being embalmed. And, if the cemetery allows, using a biodegradable casket or shroud and skipping the vault. If a vault is required, ask to have holes drilled in the bottom, or use a concrete grave box with an open bottom so the body can return to the earth.
If you would rather be cremated, you have some green choices here too. While cremation has always been touted as being more eco-friendly than a typical burial, a traditional cremation, which uses high heat to incinerate the body, does emit greenhouse gases into the air.
A green cremation, however, uses water and potassium hydroxide to reduce a deceased body to its basic element of bone ash within a few hours. This green technique, which is known as alkaline hydrolysis, is a little more expensive than traditional cremation but, unfortunately, it’s not legal in every state. Contact some local funeral providers to find out if this is available in your area, or Google “alkaline hydrolysis cremation” followed by your city and state.
Another green consideration is deciding what to do with the remains. Instead of scattering, which can be harmful to the environment, there are a wide variety of biodegradable urns that dissolve into the earth or water over time, and memorial urns that will grow a plant or tree in combination with your ashes.
Park
Independent Living at the Oaks
the Oaks
18 Arbor Lane, Syracuse
18 Arbor Lane, Syracuse
Independent Living at the Oaks
18 Arbor Lane, Syracuse
Live independently and give loved ones peace of mind knowing help is always available. Spacious 1 & 2 bedroom apartments, fine dining, 24-hour security, free Wi-Fi, social/cultural activities and much more!
18 Arbor Lane, Syracuse
Live independently and give loved ones peace of mind knowing help is always available. Spacious 1 & 2 bedroom apartments, fine dining, 24-hour security, free Wi-Fi, social/cultural activities and much more!
Live independently and give loved ones peace of mind knowing help is always available. Spacious 1 & 2 bedroom apartments, fine dining, 24-hour security, free Wi-Fi, social/cultural activities and much more!
Live independently and give loved ones peace of mind knowing help is always available. Spacious 1 & 2 bedroom apartments, fine dining, 24-hour security, free Wi-Fi, social/cultural activities and much more!
Assisted Living at the Inn Hodes Way, 4101 East Genesee Street, Syracuse
Inn Hodes Way, 4101 East Genesee Street, Syracuse
Assisted Living at the Inn Hodes Way, 4101 East Genesee Street, Syracuse


more!
Ask about our Summer Move-In-Special!
about our Move-In-Special!
Hodes Way, 4101 East Genesee Street, Syracuse
Over time we all need help. The Inn provides superior accommodations and a dedicated team. Furnished apartments, all meals in beautiful dining areas, housekeeping, social programming, personal care, nursing staff and much more!
We continue to make it easier for you to access our programs and benefits. Our website offers a convenient way to apply for benefits online. Here are five ways you can apply for benefits using ssa.gov.
Over time we all need help. The Inn provides superior accommodations and a dedicated team. Furnished apartments, all meals in beautiful dining areas, housekeeping, social programming, personal care, nursing staff and much more!
Over time we all need help. The Inn provides superior accommodations and a dedicated team. Furnished apartments, all meals in beautiful dining areas, housekeeping, social programming, personal care, nursing staff and much more!
Over time we all need help. The Inn provides superior accommodations and a dedicated team. Furnished apartments, all meals in beautiful dining areas, housekeeping, social programming, personal care, nursing staff and much more!
1. Retirement or Spouse's Benefits — You must be at least 61 years and 9 months and want your benefits to start in no more than four months. Apply at www.ssa.gov/retirement.
income and resources below specific financial limits. SSI payments are also made to people aged 65 and older without disabilities who meet the financial qualifications. If you meet certain requirements, you may begin the process online by letting us know you would like to apply for SSI at www.ssa.gov/ssi. If you do not have access to the internet, you can call your local Social Security office to make an appointment to apply.
Let us help you plan your move. Call Lisa
Let us help you plan your move. Call Lisa at 315-449-3309
Over time we all need help. The Inn provides superior accommodations and a dedicated team. Furnished apartments, all meals in beautiful dining areas, housekeeping, social programming, personal care, nursing staff and much more!
When you and your doctors know more, you can make better choices sooner and plan the next steps. Decisions that are dependent on timely and reliable laboratory results.
Laboratory Alliance professionals work round the clock, 365 days a year. We understand the importance of what our testing provides and offer the technology vital to assure accurate and timely laboratory results.

We’re a partner in the care of your health.
When you need lab work, we’re in your neighborhood. Learn more at laboratoryalliance.com.

2. Disability Benefits — You can use our online application, available at www.ssa.gov/benefits/disability to apply for disability benefits if you:
• Are age 18 or older.
• Are not currently receiving benefits on your own Social Security record.
• Are unable to work because of a medical condition that is expected to last at least 12 months or result in death.
• Have not been denied disability benefits in the last 60 days. If your application was recently denied, our online appeal application is a starting point to request a review of the determination we made. Please visit www.ssa.gov/apply/appeal-decision-we-made.
3. Supplemental Security Income (SSI) — SSI provides monthly payments to adults and children with a disability or blindness who have
Q: I lost my Medicare card. How can I get replacement?
A: The easiest and newest way to get a replacement Medicare card is by using your My Social Security account. Go to www.ssa.gov/myaccount for more information on how to create an account. You also can get a replacement Medicare card by calling us toll-free at 1-800-772-1213 (TTY 1-800-325-0778). Keep your card in a safe place. You don’t want anyone getting hold of your Social Security number. They could steal your identity.
Q: I pay my monthly premium directly to my Medicare prescription drug plan provider. Why can’t I also pay my income-related monthly adjustment amount directly to my Medicare prescription drug plan provider?
A: By law, we must deduct your income-related monthly adjustment amount from your Social Security payments. If the amount you owe is more than the amount of your payment, or you don't get monthly payments, you will get a separate bill from another federal agency, such as
4. Medicare — Medicare is a federal health insurance program for:
• People aged 65 or older.
• Some people younger than 65 who have disabilities.
• People with end-stage renal disease or amyotrophic lateral sclerosis (ALS).
• If you are not already receiving Social Security benefits, you should apply for Medicare 3 months before turning age 65 at www.ssa.gov/ medicare.
5. Extra Help with Medicare Prescription Drug Costs — The Extra Help program helps with the cost of your prescription drugs, like deductibles and copays. People who need assistance with the cost of medications can apply for Extra Help at www.ssa.gov/medicare/part-dextra-help.
Please share this information with those who need it.
the Centers for Medicare & Medicaid Services or the Railroad Retirement Board. Read Medicare Premiums: Rules for Higher-Income Beneficiaries for an idea of what you can expect to pay at www.ssa.gov/pubs.
Q: I'm retiring early, at age 62, and I receive investment income from a rental property I own. Does investment income count as earnings?
A: No. We count only the wages you earn from a job or your net profit if you're self-employed. Non-work income such as annuities, investment income, interest, capital gains, and other government benefits are not counted and will not affect your Social Security benefits. Most pensions will not affect your benefits. However, your benefit may be affected by government pensions earned through work on which you did not pay Social Security tax. You can retire online at www.ssa.gov. For more information, call us toll-free at 1-800772-1213 (TTY 1-800-325-0778).
Loretto has promoted Julie Smith
to marketing and communications director.
funds are earmarked to help support St. Camillus’s initiative to upgrade
projects in Onondaga and Madison counties that focus on the areas of arts and culture, civic affairs, education, health, human services, and the environment. In addition, the funds will be supplemented by an additional $30,000 allocated from donations raised from internal initiatives by St. Camillus to help support this effort.
best employers for women in 2023, according to Forbes.
Upstate Medical University was ranked number 33 on the list.
This list is produced by Forbes and Statista Inc., the world-leading statistics portal and industry ranking provider.
 Mike Schafer
Mike Schafer
and replace resident room furniture which will significantly improve the homelike environment, overall functionality and positively impact the resident experience through an enhanced quality of life.
Drakos Pediatric Urgent Care,
Julie SmithFormerly marketing and communications manager, Smith started at Loretto in September 2020. She holds a Bachelor of Science degree in business management with a concentration in marketing and a minor in communication and journalism from St. John Fisher College. Smith resides in Liverpool.
“Julie has led several strategic marketing campaigns for our recruitment efforts, effectively grown our social channels and managed all successful employee events. She is an incredible asset to her team and I am excited to see her continue to grow in this leadership opportunity!” said Julie Sheedy, chief marketing and engagement officer at Loretto.
Smith is a recent graduate of Loretto’s Leadership Academy. Her new role involves strategically developing and implementing marketing programs, driving recruitment and retention efforts, enhancing social media presence, managing employee events and sponsorships, promoting employee engagement and communication, and supporting Loretto’s reputation, mission and strategic growth.
St. Camillus recently received a $60,000 grant from the Central New York Community Foundation. The
“We are thrilled with the support from Cen tral New York Community Founda tion,” said Michael Schafer, president of St. Camillus. “It is through its dedication to our community and overwhelming generosity that we are able to improve the overall experi ence and create a homelike setting for our residents and patients.”
Studies have shown that interior design elements, including furni ture, have a positive impact on the health and wellbeing of those living in long-term care facilities. It creates a comfortable and inviting space to promote a person-centered focus that enhances the resident, patient, and visitor’s overall experience.
“With the grant from the Central New York Community Foundation, we are able to improve both quality of care as well as quality of life,” said Schafer.
St. Camillus’ continuum of care program includes skilled nursing (long-term care), beds for sub-acute patient rehabilitation, a NYS-certified brain injury rehabilitation unit and a certified home health agency. The funds will provide chairs, tables, nightstands, dressers, and other furnishings to upgrade three facility units, benefiting approximately 125 residents.
The grant was provided through the Central New York Community Foundation’s Community grant program, which funds innovative
ConnextCare recently held a ribbon cutting ceremony for the External Respiratory Center (ERC), a brand new acute care space constructed at the Pulaski office, the largest health center within the ConnextCare network.

The Aug. 9 ceremony coincided with National Health Center Week, a nationwide week of celebration to increase awareness of America’s 1,400 Community Health Centers, such as ConnextCare.
In June of 2021 the ConnextCare team began the early stages of planning for this project and exactly one-year later the team broke ground on the construction for what ConnextCare President and CEO Tricia Peter-Clark describes as the company’s “most innovative project to date.”
The ERC is the most progressive model of care of its kind in the region. It includes three new exam rooms, two of which are negative-pressure rooms utilized to
complete acute care exams and pulmonary function testing for patients with COPD, as well as spirometry testing to assess asthmatic patients. The ERC also includes a lab to allow for point of care testing for things such as flu, COVID-19 and strep throat. A covered canopy outside the building even allows for patients with limited mobility to remain in their car while being treated. Prior to the soft opening of the ERC in May 2023, services such as these were only available to patients if they had the ability to travel outside of Oswego County.
In addition to the new clinical building, ConnextCare also added four electric car charging stations, a gazebo powered and equipped with Wi-Fi, an 1,100 square-foot walking trail for staff and community use, .7 acres of new parking spaces and reconstruction of the existing staff parking lot.
The updates to the Pulaski
Employers have been identified in an independent survey of 60,000 workers at companies with at least 1,000 employees within the United States. The sample included about 40,000 women.
Survey participants were asked to offer their perceptions on various issues, including atmosphere and development, working conditions, salary and wage, workplace and diversity, parental leave, family support, representation and career, and pay equity.
Danielle Tongue
the only standalone pediatric urgent care in Central New York, has hired Danielle Tongue as senior practice manager. In her new role, Tongue supervises and manages a team of healthcare providers, oversees clinic operations, maintains the quality of patient care and streamlines and manages the clinic’s electronic health record system and other healthcare technology solutions.


Tongue comes to Drakos with 18 years of experience in project management and healthcare operations, including as the director of operations at CIRCARE, an outpatient behavioral health clinic. Her expertise in project management enables her to effectively oversee and manage a diverse portfolio of projects, ensuring the integration of best practices and compliance with security standards.
Drakos Pediatric Urgent Care, a member of the Drakos Dynamics family of healthcare services, is the only standalone pediatric urgent care in Central New York.
Upstate Medical University has been named among America’s
Participants were given the chance to evaluate other employers in their respective industries that stand out either positively or negatively concerning diversity. Only the recommendations of women were considered. Diversity among top executives and boards was also considered.
“This important recognition reflects Upstate’s ongoing work to build on a centuries-old tradition and culture of inclusiveness and equity for all,” said Upstate Medical University President Mantosh Dewan, MD. “We are pleased with this recognition from Forbes and believe it is reflective in the work we do in teaching, research, clinical care and community outreach. All of our employees should take pride in this well-deserved accolade.”
Dewan said the highlight is welltimed in that it is comes during the 175th anniversary of coed medical education at Upstate, the first co-ed medical college in the nation. Elizabeth Blackwell became the first woman to earn a medical degree in the United States when she graduated in 1849 from Geneva Medical College, the precursor to Upstate Medical University.
Upstate has also appeared on the following Forbes lists: best large employer in America (2023) and America’s best employers by state (2022)
ConnextCare staff and board of directors — along with state, county and village representatives — participate in the External Respiratory Center’s ribbon cutting Aug. 9. In attendance was NYS Senator Mark Walczyk. “Thank you for having this vision and investing in Pulaski because there is nothing more important than access to good healthcare, especially in rural areas”, he said.
office were made possible with the assistance of GYMO Architectural and Engineering Firm and National Grid. Funding was made possible by the Health Resources and Services
Excellus BlueCross BlueShield recently awarded grant funding to two Central New York organizations dedicated to assisting local communities in the fight against overdose deaths and to healing family relationships wounded by the scourge of substance use disorder.
Excellus BCBS has awarded ACR Health with a $6,499 Health & Wellness Award to support the organization’s overdose awareness and prevention programming, and also awarded a $5,000 Health & Wellness Award to the Consortium for Children’s Services for its nurturing parenting families in substance abuse treatment and recovery program.
“Our mission as a local, non
profit health plan is to help people in our communi ties live healthier and more secure lives through access to high-quality, affordable health care,” says Mark Muthumbi, regional president, Excellus BlueCross BlueShield. “We see the devastating ripple effects of the opioid epidemic and substance use across the nation and in our Central New York communities. We’re eager to partner in this way with ACR Health and the Children’s
Consortium in an effort to save lives and families.”
According to the U.S. Department of Health & Human Services, more than 100,000 people in the U.S. died from a drug overdose in 2021. And right here in Central New York, the story is no different. Since January of this year, already more than 700 overdoses have been reported in Onondaga County alone, according to data released by the Onondaga County Health Department.
This Health & Wellness Award funding supports ACR Health’s yearround community overdose awareness education and training. Serving Onondaga, Cayuga, Herkimer, Jefferson, Lewis, Madison, Oneida, Oswego, and St. Lawrence counties, ACR Health utilizes peer educators to perform targeted outreach and
re-establishing and strengthening their connections with their children.
As parents and children work through the eight-to-10-week program (offered in five separate sessions throughout the year), their relationship should improve as certain essential factors, specifically mutuality, authenticity, and empathy, become more vital and pervasive in the relationship. In-person and virtual options are offered to families in Onondaga, Cayuga, Cortland, Madison, Oneida and Oswego counties.
Syracuse Orthopedic Specialists
(SOS) announced orthopedic surgeon Jessica R. Albanese will join the practice’s neck and back Team.
Albanese received her bachelor’s degree from Arizona State University, graduating summa cum laude. She has held several leadership positions during her academic career and presented at many conferences. Albanese is a member of the American Academy of Orthopaedic Surgeons, American Medical Association, American Medical Women’s Association, Association of Women Surgeons, North American Spine Society, and the Ruth Jackson Orthopaedic Society.
“SOS is thrilled to welcome Dr. Albanese to our practice,” said Mike Humphrey, CEO, Syracuse Orthopedic Specialists. “She has received outstanding training in spine care at prestigious institutions and her skill and expertise will be of great benefit to patients needing neck and back care in Central New York.”
supports The Consortium for Children’s Services’ nurturing parenting families in substance abuse treatment and recovery programming, which encompasses its circle of security and active parenting programs and focuses on the effects of substance abuse on families, parenting, and parent-child relationships. Combining experiential and didactic exercises, this programming enhances parents’ self-awareness and assists them in
Physician Jonathan P. Miller, professor of neurological surgery at Case Western Reserve University (CWRU), whose expertise includes movement disorders, epilepsy, chronic pain, peripheral nerve disorders and neural engineering, has been named chairman of the department of neurosurgery at Upstate Medical University.
The appointment is effective Sept. 1.
In addition to his faculty appointment at CWRU, Miller serves in a number of key positions at University Hospitals Cleveland Medical Center, including director of the Functional and Restorative Neurosurgery Center and inaugural George R. and Constance P. Lincoln endowed chair. He also has served as vice chairman of educational affairs, associate residency program director, and fellowship director for two accredited neurosurgery fellowships (stereotactic-functional and peripheral nerve) within the department of neurological surgery.
“Dr Miller’s experience in academic medicine as a clinician, leader and researcher will serve Upstate and its department of neurosurgery well as it continues to grow and expand its service area beyond Central New York,” said Lawrence Chin, MD, dean of the Norton College of Medicine. “I expect his expertise will be shared broadly throughout campus
and I look forward to his insight on many issues.”
Miller will oversee the clinical services of a multispecialty group featuring more than a dozen clinicians offering advanced care and technologies. He will be directing basic, translational and clinical research aimed at finding new treatments and improved strategies for disorders of the brain and spine. The department is known for its longstanding residency program that has graduated nearly a hundred neurosurgeons since 1966. The department plays a central role in the Upstate Neurological Institute and following Upstate facilities: the region’s only adult and pediatric Level-1 trauma center, a dedicated Cancer Center, the Upstate Golisano Children’s Hospital, the region’s neonatal care units, the region’s first Comprehensive Stroke Center and the region’s Telestroke Network, supporting stroke care at 12 hospitals across Upstate and Central New York.
Miller has published more than 100 peer-reviewed papers and been honored with numerous awards in recognition of his research and teaching. He has led multiple translational research projects, including studies of brain-computer interfaces, gene therapy for Alzheimer’s disease, stem cell implantation for ischemic stroke, and deep brain stimulation for tinnitus, hypertension, memory
A fellowship-trained spine surgeon she will join a team of experts who use a team approach to diagnose and care for spinal conditions and injuries.
Prior to joining SOS, Albanese completed a fellowship in adult spine surgery at Duke University School of Medicine. She completed her residency at the Kirk Kerkorian School of Medicine at University of Nevada, Las Vegas, and received her medical degree from the University of Nevada, Reno School of Medicine.
Albanese brings a unique perspective to SOS. Initially she thought of focusing on geriatric care for her medical career. As she began anatomy labs and working with her hands, she realized she enjoyed the focus on biomechanics and fell in love with surgery. “The spine offers interesting, complex problems and we’re able to provide solutions for many patients, not only pain management,” she said. Her early work in geriatrics enables her to connect with the many older adults she sees with aging-related spinal issues.
Albanese is also one of a growing number of female orthopedic surgeons.
In 2022, Medscape’s Physician Compensation Report indicated that the percentage of female orthopedic surgeons was at its highest at 9%.
viewed live by more than 10 million people.
A prolific teacher, he organized and ran the third-year clinical neuroscience course at Case Western Reserve University School of Medicine as part of the clinical curriculum. He was given the Kaiser Permanente Teaching Award by the medical school class of 2017 and is a threetime recipient of the Golden Apple Teaching Award for the neurosurgery residency at University HospitalsCase Western Reserve University.
loss, and epilepsy. He holds several patents related to neuromodulation and recently served as clinical principal investigator and sponsor for the ReHAB (Reconnecting the Hand and Arm to the Brain) clinical trial, a $3 million DOD- and NIH-funded project involving the first ever use of an implanted system to allow brain-controlled reanimation of paralyzed limbs in individuals with quadriplegia.
He is a much sought-after speaker at home and abroad, addressing a myriad of issues including steretotatic and functional neurosurgery, neurostimulation, brain health and concussions in youth, among others. In 2015, he performed the first ever live televised brain surgery, which was broadcast internationally on National Geographic Channel and

He is a fellow of the American College of Surgeons and has served on the board of directors of the American Society of Stereotactic and Functional Neurosurgeons, executive council of the AANS-CNS Joint Section on Pain, and secretary of the Ohio State Neurosurgical Society. He is a member of CAST, the national accreditation committee for neurosurgery fellowships, and section editor for the journal Neurosurgery. He is chair of the NIH Brain Injury and Neurovascular Pathologies study section and a member of the orthopedic research programmatic panel for the U.S. Army Congressionally Directed Medical Research Program.
Miller earned a bachelor’s degree from Yale University and his medical degree from CWRU School of Medicine. He completed his residency in neurosurgical surgery at University Hospitals Cleveland Medical Center–CWRU and fellowship in functional and stereotactic neurosurgery at Oregon Health & Science University. He is a member of medical honor society Alpha Omega Alpha.














