





Afull third of American adults take multivitamins, despite prior studies suggesting they do little to boost health.
Now, a study involving almost 400,000 people finds zero benefit from multivitamin use in helping folks live longer.
Among people "without a history of major chronic diseases, we did not find evidence to support improved longevity among healthy adults who regularly take multivitamins," concluded a team led by Erikka Loftfield. She's with the division of cancer epidemiol-

ogy and genetics at the U.S. National Cancer Institute (NCI).
Her team published its findings June 26 in the journal JAMA Network Open.
In the study, Loftfield's group analyzed data from three prospective studies (meaning people were followed over time) with an average 27 years of follow-up.
Over 390,000 healthy adults were enrolled in the studies, and they averaged about 61 years of age upon study entry. Researchers gathered data on the participants' multivitamin use.
Over the nearly three decades of
follow-up, almost 165,000 of the participants died. About 50,000 deaths were attributed to cancer, about 35,000 deaths were caused by heart disease and 9,275 deaths were linked to strokes.
However, Loftfield's group detected no association between multivitamin use and a person's odds of dying within the study period.
In fact, "we found that daily multivitamin use vs nonuse was associated with 4% higher mortality [death] risk," the researchers noted.
People's race, ethnicity, education or dietary quality didn't alter the results.
The NCI team noted that the new findings come on the heels of "several studies that reported no benefit of multivitamin use for reducing risk of cardiovascular disease, cancer or mortality."
In 2020, the U.S. Preventive
Services Task Force, an influential, independent panel of health experts, found "insufficient" evidence to determine whether or not multivitamins could prevent heart disease or cancer.
The message to the public on multivitamins might slowly be getting through: "In the U.S., multivitamin use declined by 6% from 1999 to 2011," Loftfield's group noted.
However, use "remains popular, with nearly 1 in 3 adults reporting recent use," they added.
While the study showed no effect of multivitamins on people's odds for an early death, the team stressed that "we cannot preclude the possibility that daily multivitamin use may be associated with other health outcomes related to aging."

As specialists in women’s healthcare, we pride ourselves on providing the latest services and procedures - personalized to help you thrive. We deliver high quality healthcare from prenatal to senior health to meet your needs at any age.

Physicians:


By Chris Motola
Daniel Lewis, M.D.
Q: You’re a nocturnal hospitalist. What made you want to work that shift?
shooting process I think drew me to both. In the civilian industrial sector, because you really don’t want things to break, you don’t get to do as much troubleshooting. There’s a lot of studying and planning, but generally nothing really happens. So I wanted something a bit more challenging. That’s what led me to medicine.
Q: Did you have the opportunity to learn medical skills in the Navy or did that come after?
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
SPRINGBROOK APARTMENTS
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101
The following services are included in your rent
• Trash Collection • Free Wi-Fi
• Bus for shopping/groceries
• Heat, Electricity & Hot Water
• Snow Removal & Lawn Care
• Planned Activities
• All repairs & maintenance Applications are now being accepted!
A: A couple things, I guess. I’m a bit of night owl. So that works for me. And at night you’re on your own, so there’s more responsibility, but also more freedom and independence. You’re pretty much just there for admissions, so you can focus more on evaluating the patients, working up the patient and then moving on to the next one. Whereas during the daytime you can kind of get sidetracked by secondary calls and stuff like that. So that’s one thing I enjoy about working evenings.
Q: What hours do you work?
A: I work 7 p.m. to 7 a.m. seven days in a row and then I get the following week off. So it’s a seven-seven schedule.
Q: Are there more emergent complaints at night?
A: For the most part people can’t plan emergencies, so they’re scattered throughout the day. Sometimes you do get patients who put conditions off throughout the day and then, later in the evening, decide to present to the hospital to be evaluated. But for the most part it doesn’t really differ too much between day and night.
Q: What kinds of patients do you typically see?
A: Anything that gets admitted. I see a lot of upper respiratory infections, urinary tract infections, COPD exacerbations, heart failure exacerbations. That prob ably makes up the majority of what I see. But I also see everything in between.
Physician brings an eclectic background to the job: Studied electrical and nuclear power theory, served six years in the U.S. Navy as a nuclear electrician’s mate, was deployed during Operation Iraqi Freedom and trained as a fine dining cook under a certified master chef
Q: I assume there are fewer specialists on site at night. How does that affect your work?
A: I do work with an ED attending, so they work on stabilizing the patient, initializing treatment, coming up with an initial diagnosis. And then if there are any needs for surgical involvement, usually they’ll have contacted that service before they reach me. If they haven’t that will usually be my recommendation as well. But if they’re stable enough to be evaluated in the morning by surgery or whichever specialty, that will be my recommendation for the morning team.
Q: You have a pretty eclectic background, with education in cognitive development and military experience with electrical and nuclear engineering. How did this lead to a career as a hospitalist?
A: Not really. I had a family friend before I joined, someone who lived down the street. I can’t remember his specialty, but he was a physician who took a similar path. He did six years in the Navy prior to becoming a physician. I might have had that in the back of my mind. My last year in the Navy was when I really started brainstorming careers. It was up in the air between electrical engineering and medicine and I ultimately chose medicine. At the end of the day I was looking for a challenge and medicine presented more of one to me.
Q: You have some general surgery training. Is that a part of your practice at St. Joe’s?
A: No, I just did what’s called a prelim surgical year, so it’s just signing on for a single year. Sometimes there’s a chance to upgrade it to a full residency in surgery, but I was really only doing it for that one year while I had a gap in training. I don’t currently have plans to pursue it, but what I’ve learned from it helps me pretty much every single day at work, especially down in the ER working with post-op surgical patients, patients who have suturing, wound care.
Q: What brought you to St. Joe’s?
A: Most of my family lives in Saratoga, so that’s not that far away. My girlfriend — longtime partner moved here to work at the zoo. She’s the veterinarian for the zoo. So that’s kind of why I moved here and was looking for residencies in the area and I’d heard multiple great things about St. Joe’s so that made it my number one choice.
Local News Inc., the publisher of In Good Health and 55 PLUS, is hiring a sales person to sell print and digital ads in the Syracuse-Auburn markets. Previous experience in ad sales preferred but will consider any strong sales background. Person will work independently – from home office. Great potential for the right person. Part time with chance to go full time. Weekly salary plus commission.
Resume to editor@cnyhealth.com. Include “Ad Sales Job” on the subject line.

A: It’s hard to say it all came together. But as far as nuclear power goes I grew up right outside of Saratoga. Right outside of it in Malta is a nuclear training plant for the Navy. So growing up there I knew some of the sailors who were training there. And I had no real plans after high school, so that seemed like a reasonable starting point. I always have had a passion for technology, so that’s where I ended up once in the Navy. Electrical work is kind of mechanical as well, so you deal with heavy equipment, large motors, circuit boards, so it kind of split the difference between mechanical and electrical for me. You learn a lot of systems — it’s kind of similar to medicine in that way, especially the large aircraft carriers. It’s all one system. You have the plumbing, the electrical. It’s analogous the body in some ways. So you have to troubleshoot. If something takes out one pump, what does it do down the line? What other systems are affected? So that trouble-
Q: Do you see yourself working the night shift long into your career?
A: It’s taxing on the body. But I’m still early in my career so I’ll do it while I have the energy, probably for the next several years.
Name: Daniel Lewis, M.D.
Position: Nocturnal hospitalist at St. Joseph’s Health Hospital
Hometown: Saratoga
Education: Medical degree from University of Pittsburgh School of Medicine; bachelos’s degree in human development with a concentration in cognitive development from Cornell University’s College of Human Ecology in Ithaca. Trained as a fine dining cook under a certified master chef from the Culinary Institute of America
Affiliations: St. Joseph’s Health Hospital; Mercy Hospital (Pittsburgh)
Organizations: American Board of Family Medicine
Family: Partner (veterinarian)
Hobbies: Working on cars, pets, propagating coral

Loneliness strikes more than a fifth of people worldwide, a new survey warns.
In the Gallup survey published in July, 23 percent of people said they felt lonely "a lot of the previous day." Those experiencing feelings of loneliness often felt physical pain, worry, sadness, stress and anger, as well.
Beyond its emotional toll, loneliness is "a medical problem" that should be taken "very seriously," psychiatrist Sue Varma told CBS News.
"It's the equivalent of having somebody smoke 15 cigarettes per day, and we know that it affects our mind and our body," she said. "It predisposes us to anxiety and depression. It increases our risk by 30 percent for heart disease, for stroke, 50 percent for dementia, and 60 percent for premature mortality."
But there is a way to combat loneliness, she added.
"Look at the quality of your relationships and say, 'Do I feel seen and validated and appreciated?'" Varma said.
"We want to have a mix of micro connections — talking to the barista, talking to your dog walker — but also deep and meaningful connections in your life, where you can feel
vulnerable and open up to share," she explained.
The survey also showed loneliness was worse for young Americans than older ones.
"It's really unfortunate that as much as we want our children to succeed, the emphasis I feel is being put on academic achievement. And for kids, they're looking at financial achievement and a lot of these goals, these milestones that were possible for us years ago, aren't possible for them, mixing in climate change, war," Varma said.
"They're feeling alienated, they're feeling disconnected and the places that they would turn to — friends, parents, coaches — are no longer sources of safe havens. They're sources of stress because of this competition to succeed," she added. "When I speak to high school students, they say, 'I can't remember the last time I did something fun, just for the sake of it, not for my resume.' "
What can ease this angst?
Schedule socialization "as if it was a medical appointment," Varma advised. "Your life depends on it, because the quality of our life depends on the quality of our relationships."



We


health care regimen.
By George W. Chapman

The recent ruling limiting the authority of federal agencies like the EPA, Consumer Protection Agency, Education and the Department of Health and Human Services to promulgate regulations broadly intended to protect consumers will have untold consequences on our healthcare system. The court overturned a 40-year precedent that gave deference to federal agencies over legal challenges to their regulatory au-
As of 2022, we rank 11th in the World Index of Healthcare. We were ranked sixth previously. Our decent, but not great, ranking out of 32 advanced countries was bolstered by our high performance in research and innovation and in our biotech industry. That's the "good" news. Not surprisingly, we are dead last in fiscal sustainability. Our cost of care per capita is nearly twice the average cost of the other 31 countries. Surely, after spending so much, we must rank high on quality. Nope. We rank 19th in quality. Good to know we are getting a good bang for our buck.
A recent poll of 3,300 people older than 50, conducted by the University of Michigan, found that the top three concerns about

thority or decisions based on science. The court has basically deemed itself the expert on everything; the court can now second guess what Congress intended when drafting a law presumably to protect consumers. Basically, this ruling allows every special interest group like hospitals, insurers, equipment and drug manufacturers, to challenge regulations not specified in law. The drug cartel, er industry, is already working hard to reverse the
health were the cost of care overall, the cost of long-term care and the cost of drugs. Also in the top 10 concerns were the cost of insurance, the cost of oral care, financial scams and fraud. Is there an overriding theme here? Considering the recent Supreme Court decision, addressed above, costs could actually get worse if special interest groups like the pharmaceutical manufacturers can challenge cost control regs that are not rooted in law.


law requiring them to finally negotiate drug prices with Medicare. It was to go into effect in 2026. So CMS (Medicare) and the FDA will have to be far more cautious when drafting regulations. Consumers, providers and healthcare systems can expect more uncertainty and confusion and less stability in our already uncertain, confusing and unstable healthcare system.
pacted hospitals and local businesses. Medical students are declining residencies in states with strict abortion laws. Idaho lawmakers remain unphased. Ironically, the Supreme Court interceded, ruling Idaho must allow abortions in medical emergencies per the Emergency Medical Treatment and Labor Act.
Lucky us. Proponents of DTC ads (besides the drug companies) argue it's all about consumer education. Why should drug info only come from your doctor? Gee, I don't know. Opponents of DTC ads argue it has increased costs, addiction and off label use —Ozempic for weight loss, for example. Drug manufacturers spend more than $8 billion annually on TV ads. Three of the top five TV advertisers are drug companies. P&G and Disney the other two.
The retail giant plans to close 25% of its stores over the next three years. Walgreens does $27 billion a year, but has lost $5.6 billion through the nine months ending May 2024. Staff and buildings are expensive. It's far more profitable to sell drugs online. Walgreens actually attributes recent losses on seniors (who can barely afford their scripts) cutting back on dosages (I'm not kidding) and to overly aggressive pharmacy benefit managers who negotiate lower prices for employers. (PBMs are a whole different story when it comes to shady pricing and "savings'' for consumers.) Walgreens will also reduce its stake in the unprofitable clinic chain Village MD. Beating Walgreens to the punch is CVS, which just filed a patent to sell drugs in the metaverse via online stores.
The mask on–mask off saga continues. De pending on where you live, the CDC has relaxed indoor masking standards, schools included, for the 70% of communities with low to medium COVID levels. Over half of counties has low to medium COVID levels. Masks are still recommended for communities with medium to high levels. COVID data is collected and reported daily by 6,000 hospitals. If you test positive or are symptomatic, masking guidance is unchanged. Hospitals may have masking policies in place. Both the AMA and AHA urge indoor masking. Currently, 65% of us are fully vaccinated, but patience with masking is wearing thin. Some states have lifted mandates and schools are feeling the pressure to get rid of masks. The guidance for masks in schools has been in place for three years. The Supreme Court has upheld vaccine requirements for healthcare workers in facilities that participate in Medicare or Medicaid.




States with strict abortion laws that criminalize abor tion, case in point Idaho, are experi encing an exodus of this specialty. In the last year, Idaho has lost almost a quar ter of its OB-GYNs. The departure of these physicians was felt first and hardest in rural underserved areas. The departure of physicians has im-

Seen enough of them? It wasn't always this bad. Forty years ago, the FDA allowed drug ads on TV if they were the same boring ads as for physicians. But in 1997, the FDA allowed direct-to-consumer (DTC) drug ads. (That's when all hell broke loose with happy people dancing poorly to terrible awful music to sell drugs.) The American Medical Association (AMA) actually lobbied to prevent DTC ads back in the ‘80s. TV drug ads are banned in every country except the US and New Zealand.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.




Say hello to a more convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at eight School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI OFFICE
MONDAY - FRIDAY 7:00AM - 6:00PM
Central Square (315) 675-9200 Fulton (315) 598-4790 Oswego (315) 342-0880 Pulaski (315) 298-6564 Parish (315) 625-388 Phoenix (315) 695-4700 Mexico (315) 963-4133





By Gwenn Voelckers
Asteady rain was falling. It was one of those dreary Rochester days that made me want to pull up the covers and stay in bed.
As I struggled to start my day, I couldn’t help but recall the daunting journey I embarked on after my divorce.
I felt lost and alone in my search for purpose and meaning in my new solo life.
If you are living alone after a divorce or the loss of a spouse or partner, the newfound solitude in a quiet home can feel empty and overwhelming.
But it doesn’t have to.
When I found myself in this situation, I got professional help and was reminded of the transformational power of a positive outlook and acting decisively to create a better life.
Drawing on those insights, I followed a three-step approach for personal growth and happiness. It has worked for me, and I continue to work this plan when life’s challenges seem insurmountable.
Perhaps you, too, will find this approach helpful in trying times.
STEP ONE: Put it all out there
Take a deep breath and list your worst fears, self-doubts, and nega-
tive inner thoughts that keep you up at night. Be honest with yourself — it’s OK to acknowledge the dark thoughts that haunt you.
Here are some examples to get you started:
• I feel guilty for not being able to save my marriage.
• I worry my kids won’t want to be around me anymore.
• I feel worthless and unlovable.
• I worry about my health deteriorating and having no one to care for me.
• I fear never finding love again. Or joy.
• I believe I’m too old to start over.
• I am ashamed of my current situation.
• I feel overwhelmed by loneliness.
• I’m convinced that my life has no purpose.
• I fear dying alone, miserable and penniless.
• I’m terrified of the unknown future.
It’s easy to get stuck in this quagmire of negativity, but know that you’re not alone. Recognizing and articulating your negative thoughts is the first step towards liberation.
STEP TWO: Envision a better future
Next, ask yourself, “How do I want to feel six months from now?” Envision the future you desire, and identify the emotions you want to experience. What kind of person do you want to become?
Here are some sample goals to inspire you:
• More connected with friends and loved ones.
• More confident and courageous.
• Proud of the example I’m setting for my children.
• Filled with hope and optimism.
• Empowered to make decisions and take control of my life.
• Healthier and more energetic.
• Less weighed down by guilt or regret.
• At peace with my past and present.
• More forgiving of myself and others
• Capable of handling challenges and bouncing back from setbacks.
• More comfortable and content in my own company.
A simple shift in attitude can be incredibly empowering. By focusing on what you want to achieve, you begin to move away from self-deprecation and toward self-worth.
Lastly, ask yourself, “What concrete actions can I take today to move closer to my six-month goals?” It might be as simple as:
• Connecting with support groups for people in similar situations.
• Seeking professional counseling or therapy.
• Spending more time with friends or family.
• Engaging in self-care practices like prayer, meditation or journaling.
• Exploring new hobbies or deepening an existing passion.
• Volunteering or participating in community activities.
• Seeking financial or career guidance to alleviate monetary worries.
• Prioritizing physical health and fitness.
• Practicing gratitude and mindfulness.
• Enjoying “me time” on an overnight solo retreat.
Now, remind yourself that progress is not a destination – it’s a journey. Living alone after a significant life change can be overwhelming, but it’s important to remember that it’s never too late to pursue a more fulfilling existence.
By acknowledging your negative thoughts, visualizing a brighter future, and taking action toward your goals, you can feel more content, more confident, and more at peace.
The secret to transformation is already inside you. Embrace it, and watch your life change for the better.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.




Disease is a group of inherited disorders that cause nerve damage, typically in the peripheral nerves in the arms and legs
By Norah Machia
After working in the advertising field and later as a card dealer for the Turning Stone Resort Casino in Verona, Michael Casey decided to return to college and obtained his bachelor’s and master’s degrees in education at the SUNY Oswego.
Although he was certified as a social studies teacher and taught in the Liverpool Central School District, Casey eventually found his calling working as a teaching assistant in the school district’s special education department for nearly 18 years.
But toward the end of his career, Casey’s life took a drastic turn. It started with an occasional fall while walking between classrooms at Liverpool High School. Eventually, Casey could not manage to travel through the hallways without struggling.
“I was actually holding onto the walls to get from classroom to classroom,” he said.
He retired earlier than planned and started seeking answers to his condition through numerous therapists and neurologists.
“It really got to the point where it was very difficult for me to get around,” Casey said. The lack of a diagnosis was also causing him to become depressed. “Nobody could offer any reason for all my problems,” he added.
A fall on the ice in 2017 would give him that answer. The accident
resulted in compressed vertebras in his neck and after having successful surgery, a neurologist diagnosed him with a neuromuscular disease called Charcot-Marie-Tooth.
“It was actually good news,” said Casey. “After so many years, I finally found out what was going on with me.”
Also referred to as CMT, the name stems from the three doctors who first discovered the disorder in 1886 — Jean-Marie Charcot and Pierre Marie from France and Howard Henry Tooth from the United Kingdom. Casey has sought humor to help with his diagnosis, preferring to refer to the CMT acronym as “Can Make Trouble.”
“There are various types of CMT, which causes destruction of the nerves,” he said. “In my case, I have drop feet and balance issues. I use an ankle and foot orthotic and a walking stick. Some people must use walkers to keep moving.”
Charcot-Marie-Tooth disease is a group of inherited disorders that cause nerve damage, typically in the peripheral nerves in the arms and legs, according to the Mayo Clinic. It’s also called hereditary motor and sensory neuropathy and although it’s typically an inherited condition, it may also develop as the result of a new or spontaneous mutation.
The disease results in smaller, weaker muscles, a loss of sensation and muscle contractions and difficul-
ty walking, according to the Mayo Clinic. Foot deformities such as hammertoes and high arches also are common and while symptoms usually begin in the feet and legs, they may eventually move to the hands and arms. The severity of symptoms varies greatly for each individual.
Although the disease usually affects people in a slow progression and there is no cure, it is not a fatal disease.
Keeping a positive attitude can help to maintain a good quality of life, said Casey.
“There are different types and for some people, CMT may also affect their breathing, hearing or speech, but by itself, it’s not life-threatening,” he said. “I have to be careful, because there is always the possibility for me slipping and falling. I do have a slight shake, but it’s not Parkinsons’s disease.”
One of the best ways to deal with CMT it to “keep moving,” said Casey. After his diagnosis, he reached out to the Charcot-Tooth-Marie National Association for more information and support in starting a local chapter. At that time, Casey felt as if he was the only person with the neuromuscular condition.
“The national group has been helping me in so many ways to get the ball rolling,” he said. “We now have a CMTA branch in Central New York. We’re small in number, but we are open to all people who suffer
“There is no negativity allowed in the group, we only talk about the good things, like the efforts being made for new medications, surgeries and eventually a cure,” he said. “We also want people to know they are not alone and that other people have this disease.” 1 3 2
The local group not only offers information about CMT and the research that is being done to find a cure for the neurological disease, but it also offers emotional support to help people with CMT cope, Casey said.
Local CMTA Chapter Sponsors Sept. 14 “Syracuse Walk 4CMT”
The Central New York chapter of the CMTA will hold its sixth annual “Syracuse Walk 4CMT” fundraising event Sept. 14 at Willow Bay in the Onondaga Lake Park, 3832 Long Branch Road, Liverpool. The half-mile walk starts at 9 a.m., but it’s optional.
“Many people may not be able to walk, so it’s not mandatory,” Casey said. “It is mandatory to have fun. We will have breakfast goodies for those attending the event while supplies last.”
There will also be music, entertainment, raffles and a playground for “all the kids and those who never grew up,” said Casey. Each person who collects $100 will receive a “Walk4CMT” T-shirt. The funds raised will go toward finding new treatments and a cure for CMT. The local chapter is also seeking in-kind donations and raffle prizes.
For more information, visit www.cmtausa.org/syracusewalk Or email Casey directly at cmtsyracuse@gmail.com with CMT.”
By Eva Briggs, MD
I’m lucky to live near a park that hosts weekly free concerts during the summer. When the music is going, you can look around and see people dancing, swaying, tapping their toes, nodding their heads or otherwise moving to the music.
There’s a universal irresistible urge to move when people listen to music. Scientists call it groove and it turns out that they’ve done some research on what leads to groove and how it affects the mind.
Music has been around for a long time. The earliest known musical instrument is a Neanderthal flute found in a Slovenian cave. It’s estimated to be 60,000 years old. The urge to move to music is found across cultures, with words for the phenomenon like “balanço” in Brazil, “nori” in Japanese and “lupfig” in Swiss German. Babies as young as 3-6 months old increase their movements in response to music.
All music is not created equal when it comes to its ability to stimulate movement. The degree of complexity of the rhythm turns out to be the key. Scientists have devised a formula to measure the degree of musical syncopation. Syncopation
means that a stressed or accented beat does not fall where the listener expects.
Music that is too predictable rhythmically is less likely to get people moving. On the other hand, music that is too rhythmically complex doesn’t lead to groove, either. It’s the sweet spot in the middle that’s most effective.
Why is that? Scientists theorize that humans have an inborn desire for predictability. Moving along to the music is one way to make things predictable. When the rhythm is too simple there is no need to add predictability. And if it’s too complex it becomes impossible to add predictability. But somewhere in the middle it all comes together.
Interesting things happen inside the brain when people listen to music. Using neuroimaging, researchers found that the more pleasurable a musical passage, the higher the activity in brain centers associated with reward and motivation. And even when people are holding still, music that stimulates groove causes brain areas associated with movement to light up.
There are other factors causing
groove. One is tempo — the speed of the musical beat. The optimum is 107 to 126 beats per minute. It turns out this is the tempo that DJs typically play at musical events. It’s also close to the preferred walking speed of two steps per second.
The vestibular system — how we perceive balance — is also probably involved in groove.
In a study of dance music, researchers turned a very low frequency bass beat on and off. The sound was too low for people to hear but still perceptible by the body’s vestibular system. People danced more when the low bass was turned on. Other studies show that when music is played over speakers that produce more vibrations, people increase their body movement, tapping force and perception of groove.
Since music has been around for so long and in every culture, what is its purpose? One theory is that music synchronizes people to one another. That strengthens social bonds.
So, get out there and listen to some live music before summer is over!


By Ernst Lamothe Jr
Addiction is a complex and often misunderstood condition that affects millions worldwide.
Contrary to common misconceptions, addiction is not simply a lack of willpower or moral failing, but rather a chronic disease that involves compulsive substance use or behavior despite harmful consequences.
Prevention is an important part of this conversation that is not often discussed, according to Christopher Baszto, executive director of Farnham Family Services in Oswego. “The earlier supports are put in place, the more impactful they can be,” he said.
Counselors often have to negate misconceptions such as addiction is a choice and only weak-willed people become addicted. The reality is that addiction alters the brain’s chemistry and affects judgment, making it a disease that requires treatment. Experts would also like to dispel the viewpoint that addiction involves a failure of the will and that tough love remains the only way to address the issue.
Substance abuse disorders have complex and individualized causes resulting in considerable changes in the brain and is a legitimate medical condition that responds well to treatment and support, according to Baszto.
“Medication, peer support, family involvement, counseling, mutual support groups and life-long
recovery support among others have proven to be effective for those in recovery. The path in recovery is non linear, like many other medical concerns and reoccurrences and remissions are part of the process, not moral or will power failures,” he added.
Addiction manifests in various forms, including substance addiction, which are drugs — prescription and illegal — alcohol and nicotine. In addition, there are behavioral addictions such as gambling, internet use and shopping.
“Common forms encountered by the population include opioid use disorder, alcohol use disorder, cannabis use disorder and stimulant use disorder,” said Baszto. “Compassion, acceptance and support, meeting someone where they are in their recovery journey and helping them connect with support and treatment are often the best approaches.”
If you suspect vulnerability to addiction, opening steps include educating yourself to understand risk factors and warning signs, seeking support such as reaching out to a trusted friend, family member or counselor and considering support groups.
“There is good evidence to support that all of us are vulnerable to addictive dynamics in our lives, dependent primarily on a combina-

tion of bio-psycho-social risk and protective factors. If someone notices an increase in addictive dynamics in their life, a good first step would be reaching out to a therapist to explore further,” said Baszto. “Seeking a walk-in assessment to determine if diagnostic criteria are met would be helpful. There are many mutual support groups that do not involve clinical intervention, but provide a community forum to discuss and explore, where an individual can hear from others in similar situations around specifically identified issues.”
Denial often stems from stigma, fear of judgment or misunderstanding the severity of the problem.
Accepting an addiction can be overwhelming and admitting a need for help can be difficult.
“As in many other aspects of life, most of us have difficulty seeing elements of our own experience that cause us harm, especially when we do not feel equipped to meaningfully address it,” he added. “It has been often shared by individuals in recovery that what has typically been called denial often shares a connection with the judgment or anticipated negative response from others or one’s own lack of resources to meaningfully address an issue. By providing a supportive, accepting environment rich with support, medication and harm-reduction approaches, oftentimes what previously needed to be denied or unspoken in a less
accepting environment, can be freely explored and addressed.”
history and additional insight
Family history plays a significant role in addiction risk, indicating a genetic predisposition. Environmental factors and upbringing also contribute to vulnerability.
“Addictive dynamics and their manifestations have complex causal pathways. That said, there is good evidence to suggest that, as with other conditions, our genetic make-up may leave us with a higher or lower genetic predisposition,” said Baszto. “The interplay between our environment and the activity of genes and their expression is an area receiving significant scientific attention.”
Addiction treatment should be holistic, addressing physical, psychological and social aspects, according to Baszto. Early intervention and support are crucial in managing addiction effectively, he said. Understanding and empathy are vital in combating stigma and supporting individuals on their path to recovery.
Addiction is a multifaceted issue that requires nuanced understanding and compassionate support. Dispelling myths, recognizing trends and acknowledging personal vulnerability are crucial steps in addressing this widespread and impactful condition, according to Baszto.



By Deborah Jeanne Sergeant
Entering a drug rehabilitation program represents an important step toward sobriety. However, the patient still has a lot of work yet to do.
To make this process easier, friends and family can show their support. Instead of simply viewing “going to rehab” as the solution to the problem, it’s more realistic to see it as a step toward wellness. Expressing support verbally when they’re permitted to call (or visit, if it’s a longer-term stay) can also make a huge difference.
Patients in rehabilitation may feel deep shame, self-loathing and regret because of the stigma surrounding substance use.
Some patients may want some solitude and family members should respect that. But they should also remain open to speaking with them if that preference changes.
“It’s important to remember that substance use disorders — SUDs — are treatable chronic medical conditions and like most other chronic medical conditions, there may be periods of stability and times when
extra care is needed,” said physician Ross Sullivan, assistant professor of emergency medicine and medical director of medical toxicology at Upstate Medical University. “SUDs are not moral or ethical failures.”
Family members may also feel responsible for the SUD. Sullivan said that they should keep in mind that they’re not the cause of it and can’t control the other person’s behavior.
“Consider seeking support via live and virtual groups, counseling, advocacy, and education,” Sullivan said.
Self-care should also include proper nutrition, physical activity and stress management.
Christine Haslam, social worker at St. Joseph’s Health Behavioral Health, reminds family members that they’re impacted by addiction as much as the person going through rehabilitation.
“Substance use can be a struggle for the whole family,” Haslam said. “The support system should be people who truly understand and want to offer encouragement. Holding a loved one accountable can be difficult. However, without accountability, your family member will find ways to justify behaviors and actions that are not consistent with their recovery plan.”
She added that learning about the signs and symptoms of drug abuse can help family members identify which substances could be involved and better understand the damage caused by the substance use.
As family members have oppor-
Federal study shows lives lost from overdose crisis are felt across generations, emphasizing need to include children and families in support
An estimated 321,566 children in the United States lost a parent to drug overdose from 2011 to 2021, according to a study published in May in JAMA Psychiatry.
The rate of children who experienced this loss more than doubled during this period, from approximately 27 to 63 children per 100,000.
The highest number of affected children were those with non-Hispanic white parents, but communi-
ties of color and tribal communities were disproportionately affected.
The study was a collaborative effort led by researchers at the National Institutes of Health’s (NIH) National Institute on Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), and the Centers for Disease Control and Prevention (CDC).
Children with non-Hispanic American Indian/Alaska Native parents consistently experienced the
highest rate of loss of a parent from overdose from 2011 to 2021 — with 187 per 100,000 children affected in this group in 2021, more than double the rate among non-Hispanic white children (76.5 per 100,000) and among non-Hispanic Black children (73 per 100,000). While the number of affected children increased from 2011 to 2021 across all racial and ethnic populations, children with young non-Hispanic Black parents (18 to 25 years old) experienced the highest
Support provided by someone who has personally lived with addiction is an effective way to follow-up with ER patients after an opioid overdose, new research shows.
Patients who have had a non-fatal overdose are at great risk of a fatal overdose in the future, and more than one in four high-risk patients in
Rhode Island has a non-fatal opioid overdose within 18 months of leaving the hospital.
A controlled trial involving more than 600 high-risk ER patients found that follow-up support from trained peer recovery specialists was as effective as that provided by a licensed social worker.
“Interviewing and intervention
tunities to interact with the patient “refrain from being judgmental, insulting or condescending,” Haslam said. “Show that your concern is based on the fact you care for that person. If you raise the topic of substance use for discussion, be sure that your loved one is sober, list the behaviors you’ve observed and don’t expect immediate action. Always come from a place of compassion and caring.”
Enabling isn’t just providing the substance itself. Haslam said that it can also include overlooking the person’s actions or providing a ride or funding to obtain substances.
“Ensure you are taking care of yourself: reach out if you need support,” Haslam said. “Remove drugs and alcohol from the home. Be sure that any time spent with him or her is free of any substance use.”
Remaining patient as the person recovers is difficult but vital to recovery. The person may experience setbacks as part of the recovery. It’s not a one-and-done process. Haslam said that the first year of recovery is the hardest part.
“Remember that falling off the path of recovery does not mean that the entire attempt to address a family addiction was a failure,” she said. “Supports can ensure that the family member has the tools and support to guard against relapse. If the family member has been to treatment, ask them what worked for them. They may have a favorite coping skill or distraction.”
techniques informed by lived experience were as effective as those informed by social work theory and practice,” Brown University researchers said.
Certified peer recovery support specialists not only provide referrals for services as patients leave the ER, they also offer follow-up support for up to 90 days. That includes teaching
– roughly 24% – increase in rate of loss every year. Overall, children lost more fathers than mothers (192,459 compared to 129,107 children) during this period.
“It is devastating to see that almost half of the people who died of a drug overdose had a child. No family should lose their loved one to an overdose, and each of these deaths represents a tragic loss that could have been prevented,” said physician Nora Volkow, NIDA director. “These findings emphasize the need to better support parents in accessing prevention, treatment, and recovery services. In addition, any child who loses a parent to overdose must receive the care and support they need to navigate this painful and traumatic experience.”
patients how to prevent an overdose, helping them overcome barriers to treatment and recovery, and encouraging them to stick with it.
Support from social workers typically ends when the patient leaves the ER.
“The results of our trial strongly suggest that trained peers, and the sort of sustained support they deliver, are just as effective at preventing opioid overdoses as the support offered by traditionally trained clinical social workers,” said lead study author Laura Chambers, an assistant professor at Brown University School of Public Health.

Smoking has been found to cause 11 other kinds of cancers — not just in the lungs
By Deborah Jeanne Sergeant
Of course, risk for lung cancer increases with cigarette smoking. According to the Centers for Disease Control and Prevention, smokers are 15-30 times more likely to have lung cancer or die from lung cancer compared with those who don’t smoke.
But smoking affects many more areas of the body and contributes to many other health problems.
“Besides lung cancer, tobacco use has been found to cause 11 other kinds of cancers, including five of the most fatal types,” said Camryn Chaffee, public health educator for Onondaga County Health Department. “Poisons found in tobacco can damage or alter a cell’s DNA, which can cause the cell to grow out of control and cause a cancerous tumor. Thirty percent of all cancer deaths in the United States are attributed to tobacco use.”
She added that smokers are two to 10 times more likely to develop any of these types of cancers: mouth and throat, kidney, bladder, larynx, blood, colon/rectum, esophagus, liver, pancreas, stomach and cervix.
According to the World Health Organization, Type 2 diabetes is a leading cause of blindness, kidney failure, heart attacks, stroke, lower limb amputation, kidney disease and serious damage to the heart, blood vessels, eyes, kidneys and nerves.
“Smoking can change how your body processes and regulates sugar,” Chaffee said. “Because of this, smokers have a 30% – 40% higher chance of developing diabetes than non smokers. Smoking cigarettes makes managing diabetes more difficult. Nicotine can make it harder for the cells in the body to use insulin, which increases blood sugar levels.”
The damage doesn’t stop there. Chaffee said that smoking raises the risk of vascular problems.
“The toxins found in cigarettes cause inflammation and stress to cells,” she said. “This can lead to an increased risk for Alzheimer’s disease, dementia, osteoporosis and ALS.
“Menopause can begin up to nine years earlier in women who smoke due to the tobacco toxins causing a reduction in circulating es-

trogen in the body. The symptoms of menopause can also be more severe.”
In addition to a variety of cancers, and lung and vascular diseases, Kristen Richardson, registered nurse and director of St. Joseph’s affiliated CNY Regional Center for Tobacco Health Systems, noted that smoking “causes reduced overall health, increased rates of missed work school time and increased health care utilization and cost.”
The damage doesn’t stop there. Since tobacco products interfere with normal gum tissue cells, Richardson said that smokers are more susceptible to periodontal disease as smoking “seems to impair blood flow to the gums, which may affect wound healing. Tobacco use, including vaping, is one of the biggest risk factors for gum disease, which over time can lead to tooth loss and is itself a risk factor for heart disease.”
In addition, tobacco use can lead to bad breath, tooth discoloration, decreased taste, increased buildup of plaque and tartar on the teeth and tooth decay, increased loss of bone within the jaw, increased risk of leukoplakia — white patches inside the mouth. It can also cause increased risk of developing gum disease, a leading cause of tooth loss; delayed healing process following tooth extraction, periodontal treatment or oral surgery; lower success rate of dental implant procedures; and increased risk of developing oral cancer.
Moms need to take smoking seriously, as “smoking also increases risks for pregnant women, such as pre-term or early delivery, stillbirth,
low birth weight, sudden infant death syndrome (SIDS), ectopic pregnancy and orofacial clefts in infants,” said Kelly Jordal, senior public information officer with Oswego County.
But smoking harms anyone’s health, with “diminished overall health, increased absenteeism from work and greater health care utilization and cost,” Jordal added. “This makes quitting the most important thing people can do to improve their health — regardless of their age, how much they smoke or how long they have been smoking.”
Smokers or vapers should reach out to their primary care providers or access the New York State Quitline: www.nysmokefree.com with a chat feature. Or call 1-866-nyquits or text Text QUITNOW to 333888.
Kristen Richardson, registered nurse and director of CNY Regional Center for Tobacco Health Systems, offered a few sobering statistics:
• “Tobacco use kills 50% of its users.
• “8 million people, or 15% of all deaths globally, are attributable to tobacco use.
• “Secondhand smoke kills 1.3 million people each year worldwide.
• “Smoking kills more people than alcohol, AIDS, car accidents, illegal drugs, murders and suicides combined, with thousands more dying from spit chew tobacco use.
• “Smoking causes about 90% (or nine out of 10) of all lung cancer deaths. More women die from lung cancer each year than from breast cancer.
• “Smoking causes about 80% (or eight out of 10) of all deaths from chronic obstructive pulmonary disease (COPD).
• “Tobacco use is the leading cause of preventable disease and death in the United States. Smoking kills 28,000 New Yorkers annually.
• “More than 750,000 adult New Yorkers live with smoking related illnesses. Smokers, on average, live 10 years less than non smokers.”



Started by a former ‘lunch lady,’ the organization honors the memory of Erin Maxwell
By Stefan Yablonski
Going from a lunch lady to the executive director of a nonprofit was certainly a big jump, Sheila Dion admits. “But I knew we had to do something,” she recalled recently.
She’s the founder and executive director of Erin’s Angels of CNY. They started in 2017.
According to its website, Erin’s Angels addresses childhood food insecurity in the memory of Erin Maxwell of Palermo “who suffered unimaginable abuse and was starved regularly.”
“We began with the goal of turning the tragic death of Erin Maxwell into a powerful way to create lasting change,” Dion said. “We first approached the Phoenix Central School District because Erin was a student at Maroun Elementary School.”
“We aren’t just addressing an immediate need. We’re also fostering a sense of empowerment and resilience within the student community,” she continued. “By providing resources and support, we are contributing to a foundation that enables students to overcome challenges and thrive in their academic journey.”
Dion said she was the “lunch lady” when she had the idea to start a nonprofit. “I was working in the schools, in the food service department; was a lunch lady for about five years, then a TA (also in the lunch room) for two more years. When I worked in the Phoenix Central School District, I saw the need — so many children were going hungry. I witnessed firsthand the significant number of students facing food insecurity.”
When the bell rang, kids got up, got their backpacks and everything
and headed out to class.
“But a few of the same kids every time would come back and ask for another piece of fruit on their way out and put it in their backpack,” Dion said. “I went to the school social worker and asked her what was going on. She said, ‘we are the only school in Oswego County without a weekend backpack program.’”
That’s when Dion knew she had to act.
“I was inspired by their [students’] resilience, motivated to make a difference,” she said. “That’s why I started it — every student deserves the opportunity to focus on their education without the burden of hunger.”
She said she just started talking to people. It took several years to find an organization that would be their physical sponsor so they could start.
“I asked a lot, I just wasn’t getting anywhere,” she recalled. “Finally, I found this group called the Southern Oswego County Council of Churches. They agreed; so we were under their umbrella for about a year until we raised enough money to get an attorney and get our own 5 01 C3, which we got in 2019.
“We fundraise and get donations of food and apply for grants. We have a volunteer grant writer (an attorney). She helps write grants. We have a fundraising committee which plans some events all year round. Businesses and other community groups do food drives as well.”
In 2018, they received a $5,000 grant from Shineman Foundation.
“We’ve been very active with them. We got another $6,000 grant last year for a life cycles assessment,


So, for all these reasons it is meaningful when weekend meal programs stop working in silos and join hands to create a larger impact.”
On a weekly basis in Phoenix and the West Genesee school districts it comes out to about 250 students a weekend; “so it’s over 40,000 meals a year just in the school year,” she said. “And then our summer meals program right now we’re serving about 36 kids in the Phoenix district.”
When people come together and share their talent, resources and their time good things can happen, she said, adding — “we’re proof of that!”
Last year, they partnered with the Upstate Foundation to create an endowment. Now, through the end of December, Upstate is doubling donations up to $5,000.
which paid a consultant to help us with our growth and sustainability plan.”
Erin’s Angels is a volunteer run, year-round business.
“Some programs focus solely on the school year,” Dion said. “We’re proud to be a year-round advocate for ending hunger in our community. When a teacher’s class goes to a different classroom, the teacher will take bags of food and put them in the kids’ backpacks — it’s discreet, there’s no stigma or anything like that.
“In the summer, we utilize DoorDash. Every Friday, they come to the office, pick up food and deliver it directly to the kids’ homes. Our commitment doesn’t stop when the school year ends. Hunger doesn’t take a break and neither do we!”
A lot of communities have programs at schools or churches, “which is wonderful,” she said. “But for people who are really desperate and in poverty, a lot of times they don’t have transportation. To have a free summer meals program at a certain site is kind of a moot point. That’s why we use DoorDash and deliver food directly to the kids’ homes in Phoenix.”
“We partnered with West Genny in 2023. This collaboration is built on the foundation of shared goals and mutual support, enabling us to maximize our impact,” she said.
West Genny’s program ran under a church as a fiscal sponsor.
“They didn’t have a donor management’s system, website or any infrastructure really. So, when they aligned with us, they got all of that and more,” she added. “For instance, we share our insurance with them.
“The collaboration with Upstate aims to ensure the perpetuity of our mission. It’s opened doors to sustainable funding, expanded outreach and our ability to continue making a meaningful difference in the lives of those we serve,” she said.
Dion has a marketing business outside of Erin’s Angels (and works at a business in Phoenix).
“My background is pretty much marketing, social media and website,” she said. “I do work outside of this, but honestly about 10 to 20 hours on my outside business and about 40 to 50 hours a week on Erin’s Angels. To run a nonprofit is a lot of work. But I can’t stop what I’m doing — it’s making such a positive impact! You have moments of ‘oh this is so worth it!’
“We started in Phoenix and we will always be there but our focus is Central New York and beyond. So we are not just limited; we want to help all communities in Oswego County as much as possible.”
Erin’s Angels of CNY 219 County Route 57 Phoenix, NY 13135 315-934-0181
Website: https://erinsangels.com https://erinsangels.com/legacy-giving
Info on upcoming fundraisers: Locktoberfest (https://erinsangels.com) Friendsgiving (https://erinsangels.com)
By Anne Palumbo
My love affair with farro began at first bite. Nutty and satisfyingly chewy, farro soon became my favorite whole grain, finding its way into soups, salads, and sides.
My fondness only deepened as I got to know its many health benefits and ready availability, downright remarkable for a 20,000-year-old ancient grain!
Why the grain-crush? Let me count the ways.
Farro, like many whole grains, is a good source of fiber, an essential nutrient that many American diets lack. While fiber is important for every age, it’s especially important for older adults whose systems may be sluggish because of inactivity, less muscle mass and slower metabolisms.
of daily calories. Niacin, a B vitamin, keeps our bodies humming by converting food to energy, raising “good” cholesterol, and boosting brain function.
Whole grain farro brims with antioxidants — beneficial molecules that neutralize harmful free radicals that have been linked to multiple illnesses.
Why do free radicals, which are constantly being formed in your body and serve important functions, ever need to be neutralized?

Of course, fiber does a whole lot more than relieve constipation: it also helps with weight maintenance by promoting a full feeling; it stabilizes blood sugars; and it can even help lower blood cholesterol levels.
Multiple studies confirm that a high-fiber diet is associated with a lower risk of heart disease and Type 2 diabetes and a higher probability of a happier gut.
This versatile grain is also a great source of protein and niacin, each providing about 20% of our daily needs. Eating more protein can positively affect your health (and waistline!) by keeping muscles and bones strong and by curbing the urge to snack.
One study in overweight men showed that cravings and late-night snacking were reduced by over 50% when protein was increased to 25%
In a word: Too many roaming around can damage your DNA, increasing your risk of diabetes, heart disease and cancer. And today’s lifestyle—from sunbathing to cigarette smoke to alcohol intake to air pollution—unfortunately has been linked to excessive free radical formation.
Although farro comes whole (with its hull intact), most farro sold in the U.S. is hulled to some degree, rendering it “pearled” or “semi-pearled.” Hulled versions do not need to soak overnight and take only 30 minutes to cook. Cooked farro keeps in the fridge for five days, but can be frozen to last longer. To freeze, spread the grains in a single layer on a baking sheet and transfer to the freezer for at least two hours.

Rich and hearty, farro is naturally low in fat, sodium, and cholesterol, clocks in at around 80 calories per average serving, and is a delicious, nutritious alternative to refined grains.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
For the salad:
2 cups cooked farro
2 cups greens of choice, spinach, kale, mixed greens, etc.
2 large peaches, pitted and sliced
1½ cups blueberries
1½ cups grape tomatoes, halved
2 small ears sweet corn, kernels removed (about 1½ cups)
½ to 1 cup crumbled feta cheese
3 tablespoons chopped basil
1. In a large bowl combine the farro, greens, peach slices, blueberries, tomatoes, corn, feta, and basil.
2. In a small bowl, combine the olive oil, lemon juice, vinegar, garlic, shallot, salt, and pepper.
For the dressing:
1/3 cup olive oil
Juice of 1 lemon
1 tablespoon champagne vinegar or white balsamic vinegar
2 cloves garlic, minced
1 small shallot, minced (optional)
Salt and black pepper, to taste
Whisk until well combined.
3. Drizzle some or all of the dressing over the salad and gently toss until salad is well coated. Serve immediately.

Come
The term has been criticized as patronizing and vague and is falling out of favors
By Deborah Jeanne Sergeant
The euphemism “special needs” has come under fire in recent years as derogatory when referring to people with disabilities, in part because of the term’s misuse as a slur.
“Special needs” also seems to indicate that someone with a disability and their family expect extraordinary treatment.
“I haven’t personally used ‘special needs’ in a very long time,” said Christine Ashby, Ph.D., professor in the School of Education and director for the Center on Disability and Inclusion with Syracuse University. “It’s not a term we typically use in our programs at the university, partly because wanting a life where students have access to education and inclusion in the community aren’t ‘special needs.’ They’re needs. Calling them ‘special’ tends to imply there are needs that are special.”
On the other hand, attempts at normalizing disability may lead
to euphemisms like “exceptional” which may downplay disability instead of seeing disability as a source of pride and personal identification.
“We use identity first, ‘autistic person,’ ‘disabled person,’” Ashby said. “It’s not something to shy away from. Like all language, it’s personal. Some prefer person first. That’s more common in intellectual disability. But others are proud to be part of the disability community and they can’t separate it from themselves. It’s part of their identity. It’s not that people shouldn’t use person first language but respect the person.”
But such gangly phrases like “individuals with developmental disabilities” easily become clumsy with repeated use, whether in print or spoken. Asking individuals for their preferred term when in a oneon-one conversation is both frank and thoughtful. When writing or speaking to a large group, it’s impossible to use the favored term of each
By Deborah Jeanne Sergeant
Visiting the doctor’s office — even for a well-child visit — can feel stressful for some children.
They may worry about receiving a shot or having an unfamiliar grownup perform an examination.
For autistic children, these worries are magnified as the stimuli that’s mundane for typical children seems intolerable: bright lights in the waiting area and exam room, loud cartoons on the TV, pungent cleaning solution odors, scratchy exam gowns and exam tools that touch their bodies in unfamiliar ways, like the otoscope in the ears. Overstimulation can cause behavioral issues as children try to express their discomfort.
Planning can make doctor’s visits easier for children, including the doctor.
“I’ve found the most important thing is to have the same provider,” said pediatrician Sarah Marsh at St. Joseph’s Health. “Here, I have 70 kids on the spectrum and we know them and that they’re coming. The provider may write a note to the nurses. Parents shouldn’t lie, ‘We’re going to the bank’ and surprise! They’re going to the doctor. I never tell a child it won’t hurt if it will.”
She added that any new nurse should be warned about the child’s

reader or listener. That’s why in those cases, Ashby tends to use person-first language.
“But I never use ‘special needs’ because it’s vague and unhelpful,” Ashby said. “We should be recognizing that they’re not ‘special’ needs. We all have needs. If some people have ‘special needs’ what do others have?”
“Special needs” could mean anything from a person who struggles to read to someone completely dependent on others for activities of daily living. She added that support is dynamic because anyone who lives long enough will likely need more support, yet older adults who need help aren’t referred to as “special
needs” people.
Claiming that everyone has some kind of special needs is disingenuous to families who have fought school boards and intensely struggled to help their children access school resources, for example.
The fact that terms like “special education” change over time doesn’t strike Cathy Leogrande, Ph.D., as kowtowing to political correctness.
“It’s because we know more now,” Leogrande said. “It’s not politically correct to use a better term when we’ve gotten smarter.”
Leogrande is a professor in the education department at Purcell School of Professional Studies at Le Moyne College. She sees the shift away from “special needs” as reflecting the movement away from the medical model towards the social model.
“There’s a ‘typical’ and a ‘not typical’ category that means different, not less than or bad,” she said. “When you reflect that in your language, we know everyone could probably benefit from some kind of adaptation or need. We have to slap this label on kids if they want services. That’s the way the law is.”
Most employers use “disabled” because of the Americans with Disabilities Act (ADA) law. In her writing, Leogrande tends to use disclaimers whenever possible to avoid offending readers.
needs. Marsh said that most children with autism don’t like having their ears touched, for example. But holding a favorite toy or other significant object or playing on a tablet helps.
Marsh also recommends consolidating doctor’s visits if possible. But that depends upon the child’s tolerance level.
No one likes shots. That’s why Marsh uses “immunizations” or “vaccines” instead of “shots” in children’s presence.
“If parents can be completely attentive during the visit, it helps,” she added. “Put away your phone and be as present as you can.”
Planning at home also makes visits go better. Of course, an emergency visit can’t have the same level of planning as a well-child visit. However, for the latter, prepare with a few strategies. YouTube videos can help children prepare for visits, as well as children’s books about doctor’s visits.
“Research says role playing at home helps,” said Cathy Leogrande, PhD, professor in the education department at Purcell School of Professional Studies at Le Moyne College.
She advises parents to buy their children a toy doctor’s kit to play with at home. Perhaps mom and dad could be patients or a doll or stuffed
toy. Leogrande said that this type of play can help normalize doctor’s visits as just another activity.
“Some doctors are good at helping kids through the visit,” she added. “They may say, ‘Would you like to put the stethoscope on your chest? Would you like to touch it?’ Some may put a cover on it.”
Planning the day of the visit can make things go more smoothly as well.
“Arrange the day such that you don’t have to stop a fun or reinforcing activity to transition to the doctor’s office,” said Courtney R. Mauzy IV, Ph.D., and research instructor at Upstate Pediatrics at Golisano Center for Special Needs.
But planning something fun to happen directly after the doctor’s visit can give kids something happy to look forward to. Making the trip more enjoyable could include free access to favorite toys or snacks — a better association than the discomfort from needles and throat swabs at the doctor’s office.
“I encourage parents to not provide a lot of unnecessary demands or instructions during these visits,” Mauzy said. “They are already being asked to do something outside of their normal routine and schedule and are surrounded by a lot of unfamiliar people and things, so we can try and not add to that by adding additional demands.”
This could include advocating only for medically necessary procedures. Why go through measuring height when the child presents with an upset stomach?
Don’t forget the stimuli soothing items such as sunglasses, head-
phones, favorite stuffed toy or fidget toy to help curb the potential for feeling overwhelmed.
Mauzy said that offering the child the choice of a positive reinforcer during the most difficult parts of the visit such as a blood draw may help, such as a sticker immediately.
“A parent can always ask about conducting certain tests if they know it might be difficult for their child,” he said.
He added that consistently praising behaviors they want to see during the visit and avoiding drawing attention to challenging behavior is particularly helpful during stressful times.
“I encourage caregivers to use very clear and objective instructions to communicate exactly what is expected of the individual,” Mauzy said. “We often refer to this as ‘first/ then’ statements. ‘First, you stand on the scale, then you can have your tablet back.’ This both makes the expectations as clear as possible and signals what will happen once the individual complies.”
He offered another strategy to gain compliance: a preferred reinforcer with a “high probability demand” before asking the child to do something hard. If it’s tough to measure weight, start with something easy, like “Give me a high five.”
“If they comply with the easy demand, you can provide the reinforcer and the child starts to experience the rule of ‘OK, I comply, I get something I want,’” Mauzy said. “You build some momentum with compliance with easy demands and sometimes that can make jumping to a more challenging demand easier.”
All of sudden, it seems there is a huge number of ‘special needs’ kids. How did that happen and what’s driving the increase in the number of such kids. Experts weigh in
By Deborah Jeanne Sergeant
If it seems like more children you know have an individualized education plan, you’re not imagining things.
Data gathered by the Pew Research Center from the National Center for Education Statistics states that the number of students in special education soared from 3.6 million in the 1976-77 school year, to almost 7.3 million in 2021-22. That’s 15% of the nation’s students.
“There’s more awareness of disability and the educators and providers are more attuned to possibilities,” said Christy Ashby, professor of inclusive special education and disability studies and the director of the Center on Disability and Inclusion at Syracuse University.
Universal screening is recommended at pediatrician’s offices. Changes in the diagnosis criteria make it easier for identifying children presenting with subtler symptoms of things like autism spectrum disorder who might still benefit from support.
In previous generations, children who might be noticed as “quirky” or “odd” may receive closer scrutiny — a second look that could help more children receive support they need.
As for identifying any kind of learning disability or other reason for an IEP, schools may be looking harder at students who lag.
“The pressure in schools has gone up,” Ashby said. “More kids were ending up in segregated education because of concerns that they wouldn’t keep up. There seems to be a rise of kids with mental health and sensory concerns. I’m not sure what that’s about, whether environmental.”
Heather Burroughs, director of advocacy and education at AutismUp in Rochester, referred to “From Snake Pits to Cash Cows: Politics and Public Institutions in New York” (Castellania, 2005) which said that in 1935, there were 135 cases of autism across the US compared with “hundreds of thousands now,” Burroughs said.
A mother of four children on the autism spectrum, Burroughs doesn’t pin the entire reason for more autism diagnoses on shifts in screening and diagnosis. She said that part of the reason could be that people with autistic traits are having children, meaning that more people would have autism.
“There’s a hereditary component; you can see it in several members of some families,” Burroughs said, noting that several people in her family are on the autism spectrum. One of her grandmothers exhibited traits then thought of as quirky, but not autism.
Burroughs also thinks that an

environmental aspect may play a role in why people have autism. Anecdotally, some families have reported that eliminating certain food types or food additives helps mitigate their autistic child’s behavioral issues.
The “trigger” food varies even in the same family. Gluten, casein, refined sugar and certain food additives and preservatives are often named as culprits. However, improved behavior and life quality does not indicate a causal effect between foods and autism. But some people have discovered that eliminating some foods reduces unwanted behaviors in their children on the spectrum. No large-scale studies have identified a cause for autism.
Cathy Leogrande, PhD, professor in the education department at Purcell School of Professional Studies at Le Moyne College, has worked in education for 50 years. She said that in general, more children are being identified in school as require more support and intervention than ever in part because without a label, kids who are behind may not be able to receive appropriate help.
“Some of it is just unfortunate that we’ve lost things like reading teachers and support staff that was supported by the government,”
Leogrande said. “There’s always money given for special ed and that’s sometimes the only way to get support for kids.”
Among some of those students are children who will not experience lifelong or large-impact impairment. They may lack the support at home to come to school as prepared as other children. When fourth, seventh and ninth grades come; those with moderate or less coping skills significantly struggle.
Leogrande said that’s when she receives the most referrals because the curriculum becomes tougher and with more homework.
“As the curriculum gets more difficult, kids who developed their own strategies get outmoded,” she said.
She also said that there are more children with problems, in part single-parent homes or homes where both parents work two jobs. This can leave gaps in skills that keep kids from excelling at school.
By contrast, she added that some children who could probably benefit from extra services don’t receive them in a formal way through an IEP because their teachers accommodate them in the classroom.
Hospice of Central New York and of the Finger Lakes will show donors the movie “Angels in the Outfield” at their fourth annual Film on the Field fundraiser at NBT Bank Stadium in Syracuse.
The event is set for 5:15 – 9:30 p.m., Wednesday, Aug. 14.
The evening begins with concessions and entertainment, including face-painting, balloon twisting, a photo booth and a visit from Syracuse University’s Otto. It ends with a fireworks show.
Advance sale tickets for the event are required, and can be purchased at filmonthefield.givesmart. com.
All proceeds from the event support the hospice mission to serve as the community’s expert resource at the end-of-life, by providing comprehensive comfort care to patients and families through unique interdisciplinary services, bereavement counseling, education and collaboration.
People attending this rain or shine event are able to watch the film on the field or in the stadium seats. The stadium concession stands will be open for purchasing refreshments, and parking for the event is free.
“Hematology-Oncology Associates of CNY (HOA) is proud to be the presenting sponsor for this event to support the tremendous love and caring hospice provides to our community,” said HOA’s CEO Maryann Roefaro. “The services Hospice provides to improve the quality of life and dignity for patients and their families is invaluable.” Film
Required donations are $25 for adults and $10 for children 6-12; children 5 and under are free. There also are limited VIP packages that can be purchased and a silent auction that can be accessed with the same link.
By Deborah Jeanne Sergeant
Nothing reverses autism. However, a few holistic strategies can help their children cope in a world that can be hard for them to understand and deal with.
Tips from Courtney R. Mauzy IV, Ph.D., research instructor at Upstate Pediatrics, Golisano Center for Special Needs
• “Provide choices when possible. For a lot of individuals, providing choices can instill a sense of independence, assent and control over their environment that can really help a lot of individuals. This can apply in a lot of different contexts. From choosing what reward or activity you want to work for, to choosing between which homework subject you are going to do first or choosing between which vegetable you have to eat, simply providing choices can often be an easy-to-use and highly effective strategy.
• “Schedule and give clear expectations. This kind of goes back to my first point about trying to plan the most preferred or fun activities to happen after the really fun activities. For example, I often sit down with caregivers who struggle with
challenging behavior in the evenings after their children get home from school. The first thing we do is go through their typical schedule in the afternoon and usually parents will report that kids get home from school, they get a snack and some free time to relax and then they have dinner and then they have to do their homework. Going from free time and dinner to doing homework is one of those high-preferred transitions to a low-preferred activity and is not surprising that a lot of individuals struggle to get started with their homework without challenging behavior. But simply re-arranging the typical schedule to have homework come before free time can be really helpful.
• “There’s a difference between ‘bribing’ and ‘providing reinforcement.’ Reinforcement strategies have a very robust research history showing their effectiveness in the treatment of challenging behavior. But I have often heard ‘I don’t want to bribe my child with rewards all the time’ or ‘I shouldn’t need to bribe my child to behave at the doctor’s office.’ There is a clear difference between what is a bribe and what is setting up a reinforcement strategy and the
By Deborah Jeanne Sergeant
Child life specialists do more than break out the crayons and coloring books with sick kids. The work can be incredibly demanding.
“Sometimes it’s really hard when we go into a room and we have to have difficult conversations and a child isn’t doing well and then we go to the next room and play Candy Land,” said Regina Lozito, manager of Upstate’s child life program. “We can’t always make it better. We can do our best to help them through it.”
At Upstate, the team of 17 child life workers include 15 certified child life specialists. Lozito has a bachelor’s in child psychology and master’s in child life, along with 600 hours of internship. After those achievements, she was able to sit for the certification exam.
“People think you get to play with kids all day, but there’s a lot of psychology that goes into it,” Lozito said. “We make sure kids and
research has shown bribing is likely to make behavior worse in the future while reinforcement is an extremely effective strategy. A bribe is when you ask your child to do something, they respond by being noncompliant or start engaging in challenging behavior and then you offer them a reward for complying. In a bribe, the opportunity to earn a reinforcer or reward only happens once the individual starts engaging in challenging behavior, thus teaching the child in the future ‘Hey, if I want to earn this, I should just start being noncompliant.’ However, when you set up a reinforcement strategy, the rule or contingency is made clear from the start and is stated prior to any noncompliance or challenging behavior. ‘Today we are going to the doctor’s office. If you go the whole visit with safe hands, we will stop at Chick-Fil-A on the way home.’ This way it is clear that only the ‘positive’ behaviors are what produces the reinforcer. That may have been a little bit of a soap box but it applies both to doctor’s visits and in general.”
Tips from Cathy Leogrande, Ph.D., professor in the education department at Purcell School of Professional Studies at Le Moyne College
• “Don’t look on the internet. I do think that one thing that it does well is connect parents who were maybe the only one in their sphere of life. Now they can read what other people are doing. They may read something that doesn’t fit their child, but they’ll try it. One thing that came out of the internet is parent advocacy and information. Other parents are helpful. They’re in the same situation and are one of your best resources. Or a teacher may recommend things
to do at home.
• “A low-processed food diet is not going to hurt and might help. But it’s problematic when parents read it and think ‘My kid is going to be cured.’ Your child will never be different, but they’ll gain strategies to be more independent.”
Tips from Lisa M. Latten, whose son, Ian, is on the autism spectrum, clinical administrator for the division of developmental and behavioral pediatrics at University of Rochester Medical Center.
• “Keep a regular bedtime. At 19 we still do shower and bed at 8. It works better for him and for us as a family. The routine is so critical. Visual schedules work well for him. We have a magnetic calendar weekly on the fridge. He has yoga, piano lessons and any doctor or dental appointments so he can see his week in advance or anything special at school so there are no surprises. You need to tell him before you put it on the calendar. He likes to know beforehand what we’re doing.
• “If there’s a family event, he likes to know who will be there. He likes to see photos of the hotel if we’re going on vacation. He has particular toys and objects he likes to take with him. My husband and I joke that he has an old cookie monster plastic toy we found when he was 3 and a Leapfrog drum toy. He sets them up in a line at the hotel or Airbnb. The TV has to be on The Weather Channel. I have to make sure the place has cable TV.
• “It takes lots of planning. Preplan everything. We don’t have the luxury of doing anything at the drop of a hat.”
families understand why they’re in the hospital, what’s expected of them, what will happen. What does anesthesia mean? Will they spend the night? We do a lot of normalizing the environment. What happens on the outside we have inside the hospital.”
That could include trick-or-treating, providing access to education so kids don’t fall behind, and maintaining a family resource center and playrooms. Child life services include helping children adjust to lifelong changes that result from an illness or accident and bereavement support to the family as well.
Child life specialists may work in a variety of medical settings, both out patient and in patient. They often perform a psychological evaluation on the fly to assess how much information children can process and understand.
“A lot feel like they’re being punished,” Lozito said. “We’ve taken away their control and things they

love to do. Our job is to make sure they understand why they’re there and we’re not trying to be mean. It’s not fun here always.”
The goals of child life work include improving emotional outcomes as well as ones more easily measured, such as lower blood pressure, less pain medication, better compliance during procedures and recovery and faster healing. The results can be long-lasting.
“Kids who experience a positive situation in the hospital are much more likely to be medically complaint adults,” Lozito said. “They understand the medical system better. You know what’s happening and
Regina Lozito is the manager of Upstate’s child life program. “We make sure kids and families understand why they’re in the hospital, what’s expected of them, what will happen,” she says.
what’s expected of you and everyone’s job. Your job is to sit still; the nurse’s job is to insert the IV.” Showing children a procedure on themselves or on a doll can help them prepare.
Lozito encourages anyone interested in working as a child life specialist to look at www.childlife. org to become accustomed with what the profession entails. She sees the potential for a lot of growth in the field in that at her organization alone, the staff grew from three in her department in 2000 to 17 currently.
“We’re growing fast and we need more people to fill the positions,” Lozito said. “I have clinics contacting me.”
The Bureau of Labor Statistics states that the average mean wage is $60,380 for a child life specialist.

By Melissa Stefanec MelissaStefanec@yahoo.com
certain concept has made the rounds in many parenting circles. I don’t know how I feel about this concept. At best, it seems defeatist. At worst, it’s a self-fulfilling prophecy that destroys what should be some of the best moments of our adult lives.
The concept is this: it’s not really a vacation if your non-grown children are with you. Children make vacations so demanding that it’s impossible to truly enjoy yourself.
I just can’t buy into this. Don’t get me wrong; when I vacation with friends or my husband and the kids aren’t around, I do tend to have a less-demanding vacation. However, I see vacation with kids as a different version of fun, but not a lesser version.
I don’t want to distract from the fact that kids make vacationing stressful. But there is another side to vacationing with kids. There is the laughter and unbridled joy. There is the break from routine. There is the opportunity to get to know each other better. Vacationing with kids is fodder for some of the best memories of our lives.
But how do you make that so?
Can you vacation well without taking a vacation from parenting? I don’t have all of the answers. But I do have some parenting hacks that avoid or redirect stressful moments. Here are some of those hacks.
• Include your kids in the planning.
If your kids can talk, they can be included in the planning. Many family fights stem from a perceived lack of control. Bring your family into the planning process. Give everyone small choices. For example, let one child pick which ice cream stand to stop at. Let each child and parent pick an activity. Give everyone a little say and people tend to be satisfied.
• Train them to pack.
Even if your kids can’t read yet, they can pack. I’ve been giving my kids packing lists from an early age. At one point, those lists were numbers and pictures. Bringing the kids into the planning process may seem like more work at first, but it will pay out in the long run.
• Clearly communicate what needs to be done and when.
Getting out of the house and packed up to leave have to be two of the most stressful events in any family vacation. Clearly communi-

cate what needs to be done and by what time. Make lists. Hold yourself and your family accountable. Plan to finish packing early. If there is any time to be serious about deadlines and expectations, this is that time.
• No matter how old your kids are, pack baby wipes.
There will be messy faces and hands. There will be car spills and smears. There will be dirt. Someone will get bug repellent on their fingers. Someone will get sunscreen in their eyes. Someone will get sweaty or have to blow their nose. Whatever the minor trauma, baby wipes will rescue you.
• Pack a small first-aid kit.
This kit can just be some essentials in a zip-top bag. I swear by the following lineup: pain relievers, antibiotic cream, bandages, a few alcohol wipes, motion-sickness medicine, oral antihistamine, a tick spoon, a travel ice pack, anti-itch cream or spray, antacids and eye drops. It may seem like a lot, but this combination of items will have you prepped for almost any family first-aid need.
• Break the rules while staying firm.
Vacations are about indulgence. But, we all know overindulgence leads to bad behavior and displeasure. Let everyone break the rules, but do it in a planned and structured way. For example, let the kids stay up past their bedtime, but still set a bedtime (and stick to it). Eat ice cream for dinner one night. Let the kids play the rigged claw machine but set a clear budget for the claw machine. Do things you wouldn’t usually do, but set firm boundaries.
• Set expectations with others. If you’re vacationing with other people, clue them into your planning and schedules. Clearly communicate expectations about meals, screen time, nap schedules, activities, fears,











phobias and off-limits topics. The clearer you are with everyone, the less likely folks will be to get frustrated with each other.
• Limit screen time. What kind of monster would limit screen time during vacation? The kind of monster who doesn’t want little monsters destroying the positive vacationing vibes. Too much time on phones or tablets makes kids short-tempered and prone to melting down. Be firm about how much time kids can engage with electronics and what they are allowed to watch on them. You won’t regret doing this. Trust me.
• Be the hype master.
Before the trip and before events, keep things positive. Talk about how fun or interesting activities will be. Don’t frame less-desirable aspects of the trip as something negative. Try to see the good in every aspect and broadcast that positivity to others. If you set up the car ride to be miserable and long, the car ride will be miserable and long.
• Bring emergency toys.
When we travel, I always pack emergency toys. Those toys aren’t just for the kids. I bring stuff like sidewalk chalk, drawing notebooks, foam footballs, beach buckets, a deck of cards, mini board games or a frisbee. You never know when you will find yourself stuck somewhere for too long. Having a few toys will keep children and adults in a better headspace.
• Hack a smile.
Here’s hoping these hacks help you vacation a little calmer and happier. And, if all else fails, just fake it until you make it. Many stressful moments can be solved with a sense of humor, a little resilience and a big smile.







Elemental Management Group, which operates senior facilities in Rochester, Oswego and in the Mohawk Valley, has recently developed a 75-hour, three-week hybrid course nurse aide training program. It is designed to help expedite CNA training.
It enables students to complete the program in less than three weeks — instead of 164 hours across four to six weeks. The hybrid CNA program can accommodate up to 20 students, providing sufficient instructors are available for clinical time.
Recently, In Good Health spoke with Judy Harding-Staelens, registered nurse, licensed nursing home administrator and regional director of operations for Elemental and Peg Reith, registered nurse, regional nurse educator and CNA educator for Elemental.
Q: Is this a new program in the state?
A: (Peg) This is new for New York state, yes.
Q: So, this course is user-friendly?
By Stefan Yablonski
with the residents. Sometimes they are just there as companions.
A: (Peg) This course is very user-friendly for anybody who is dealing with life right now. They download the app, they use a laptop, they can use a tablet, whatever. Everything that they need to learn is right online. The CNA videos are online for them as well. They only have to come into the building to do their on-hand skills and the clinical portion of it. So it is very user-friendly for anybody who is short on time that wants to advance their career.
Q: How many graduates have you had so far?
A: (Judy) We are at least 320 graduates. We have this up and running in five facilities right now … and two more starting in August. Each facility is a little bit different, but programs are offered every month, currently. It’s about every three weeks on average. Students unable to finish in the prescribed three weeks can jump into the next session without having to redo material previously covered.
Q: What are the duties and responsibilities of a CNA?
A: (Peg) A CNA does the bathing, shaving, feeding, caring — working
(Judy) We want to get CNAs into the workforce quicker. We offer a hybrid program and the goal is to get as many CNAs as possible certified in the quickest amount of time. We found that students were having a hard time being able to sit in a 100plus hour course for weeks to get certified to get a job. This offers them the opportunity to do all the work on the phone, computer at home. They can work nights; they can take care of their kids, their parents, they can take care of a neighbor.

(Judy) The role of a CNA is a vast one. For long-term care, they are the primary direct caregivers. They have a lot to do with long-term care facilities on how well we care for our residents, how many we can take care of. They have a very big role there with all the residents.
Q: Who are the instructors?
A: (Peg) I am one of the instructors. I work in multiple buildings. Each building has an educator. They do have to be approved by the NYS Department of Health and have a train-the-trainer certificate as well.
Q: Where do students go to work after successfully completing the course?
A: (Peg) When they finish the course, they are offered employment. They get interviewed — some buildings interview them prior to taking the course. Students who finish the course can apply to work in that building. Usually, they stay and work at the facility that they went through the course with. If they choose to go elsewhere, they absolutely can if they choose to; depending on if they signed a contract or not.
Q: Is there a cost to the student?
A: (Judy) This is free for the students. They can come to the facility and the facility pays for the training.
And a lot of these facilities offer a sign-on bonus at the end of the class. It’s definitely a win-win.
Q: Do you train others?
A: (Judy) We do the training for other facilities. If a facility doesn’t have a CNA training program — or even if they do — they can connect with us and we’ll come in and train their trainer in our program and then it is theirs to use. Elemental has two packages. One provides training for educators who want to teach the hybrid CNA classes at their own facility. The other package completely handles the hybrid CNA classes as a third-party entity.
Q: How long have you been doing this?
A: (Judy) We are a year and five months into this. We haven’t changed it; we are getting better at it — adding more instructors and more buildings. The more students taking this, the better for New York state nursing homes.
Q: This is a growing profession?
A: (Judy) Yes, people are starting to come back to this profession after the end of the pandemic.
(Peg) We are very proud of what we have been able to do for the communities; putting CNAs back out there when they are really needed. They are coming back in droves now.

Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN UP




Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP
















MANAGEMENT GROUP

Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today ELEMENTAL MANAGEMENT GROUP
CONTACT:

Peg Reith BSN, RN
CONTACT:
Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
CONTACT:
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com





















Do
Do



SBy Warren Beck Social Security District Manager in Syracuse.
ocial Security helps you secure today and tomorrow with financial benefits, information and tools that support you through life’s journey. If you don’t have enough Social Security credits to get benefits on your own record, you may be able to receive benefits as a spouse. Your spouse must be receiving benefits for you to get benefits on their record. If your spouse does not receive retirement or disability, you’ll have to wait to apply on your spouse’s record.
In addition, to be eligible for spouse’s benefits, you must be one of the following:
• 62 years of age or older.
• Any age if you have a child who is younger than 16 in your care or has a disability and is entitled to benefits on your spouse’s record.
If you wait until you reach full retirement age to receive benefits, you’ll receive your full spouse’s benefit amount, which is up to one-half the amount your spouse receives. You’ll also get your full spouse’s benefit if you are under full retirement age, but care for a child and one of the following applies:
• The child is younger than age 16.
Q: My same-sex partner and I recently married. Will we be eligible for Social Security benefits?
A: You or your spouse could be eligible for benefits, or a higher benefit amount, based on your marital relationship. Many factors affect your eligibility for benefits, including how long you worked and your age. You can apply online at www.ssa.gov/ apply, by phone by calling 1-800772-1213 (TTY 1-800-325-0778), or contacting your local Social Security office. We encourage you to apply for benefits right away, even if you are not sure if you are eligible. Applying now will protect you against the loss of any potential benefits. Learn more about Social Security for same-sex couples by visiting www.ssa.gov/ people/lgbtq/couples.htm.
Q: I’m 17 and eager to start my first summer job, but my mother misplaced my Social Security card. How can I get another?
A: If you know your Social Security number, you may not need to get a replacement card to obtain employment. However, if a prospective employer requests it, you can get a replacement Social Security card by following the steps below. There is no charge for a Social Security card, but you are limited to three per calendar year and 10 replacement cards during
• The child has a disability and is entitled to benefits on your spouse’s record.
If you receive retirement on your own record, we will pay that amount first. If your benefits as a spouse are higher than your own benefit, you will get a combination of benefits that equals the higher spouse’s benefit.
Consider this example: Sandy is eligible for a monthly retirement benefit of $1,000 and a spouse’s benefit of $1,250. If she waits for Social Security until her full retirement age, she will receive her own $1,000 retirement benefit. We will add $250 from her spouse’s benefit, for a total of $1,250 a month. Sandy only gets an additional spouse’s benefit because her own benefit is less than half her spouse’s full retirement age benefit. Want to apply for either your retirement or your spouse’s benefits or both? Are you at least 61 years and 9 months old? If you answer yes to both, visit www.ssa.gov/benefits/ retirement to get started today. Are you divorced from a marriage that lasted at least 10 years? You may be able to get benefits on your former spouse’s record. For more information, please visit our website at www.ssa.gov/planners/ retire/divspouse.html.
your lifetime. Your parent can:
• Use our online “Social Security Number Card” application at www. ssa.gov//number-card/replace-card and answer a few questions to find out the best way to apply. Your parent can start the application online and complete the process in a local Social Security office or card center, usually in less time.
• Fill out and print an “Application for a Social Security Card” if they are not able to complete it online.
• Take or mail your application and original or certified documents proving your identity to your local Social Security office or card center. For more information, read our pamphlet, Your Social Security Number and Card at www.ssa.gov/pubs/ EN-05-10002.pdf.
Q: I’m reaching my full retirement age and thinking about retiring early next year. When is the best time of year to apply for Social Security benefits?
A: You can apply as early as four months before you want your monthly benefits to begin. To apply, just go to www.ssa.gov/apply. Applying online for retirement benefits from the convenience of your home or office is secure and can take as little as 15 minutes. It’s so easy!
By Jim Miller
Dear Savvy Senior,
I need to hire a good in-home caregiver to help my elderly father who lives alone. What’s the best way to do this?
Searching Sarah
Dear Sarah,
Finding a good in-home caregiver for an elderly parent is not always easy. How can you find one that’s reliable and trustworthy, as well as someone your parent likes and is comfortable with? Here are some tips that can help.
Know His Needs
Before you start the task of looking for an in-home caregiver, your first step is to determine the level of care your dad needs.
For example, if he only needs

help with daily living tasks like shopping, cooking, doing laundry, bathing or dressing, a “homemaker” or “personal care aide” will do. But if he needs health care services, there are “home health aides” that may do all the things a homemaker does, plus they also have training in administering medications, changing wound dressings and other medically related duties. Home health aides often work under a nurse’s supervision.
Once you settle on a level of care, you then need to decide how many hours of assistance he’ll need. For
example, does your dad need someone to come in just a few mornings a week to cook, clean, run errands or perhaps help him with a bath? Or does he need more continuous care that requires daily visits?
After you determine his needs, there are two ways in which you can go about hiring someone. Either through an agency, or you can hire someone directly on your own.
Hiring a personal care or home health aide through an agency is the safest and easiest option, but it’s more expensive. Costs typically run anywhere between $20 and $30 an hour depending on where you live and the qualification of the aide.
How it works is you pay the agency, and they handle everything including an assessment of your mom’s needs, assigning appropriately trained and pre-screened staff to care for her and finding a fill-in on days her aide cannot come.
Some of the drawbacks, however, are that you may not have much input into the selection of the caregiver, and the caregivers may change or alternate, which can cause a disruption.
To find a home care agency in your dad’s area use search engines like Google or Bing and type in “home health care” or “non-medical home care” followed by the city and state your dad lives in. You can also use Medicare’s search tool at Medicare.gov/care-compare — click on “home health services.” Most home health agencies offer some form of non-medical home care services too.
You also need to know that original Medicare does not cover
We may not think of loneliness as posing serious health risks, but if feelings of loneliness are not addressed, they can significantly impact our health. There are ways to help prevent loneliness and the resulting health impacts. If you’re feeling lonely, consider the following:
• Seek support: Reach out to friends, family or a therapist. Support groups can also foster a sense of community and understanding.
• Volunteer: Helping others can boost self-esteem and foster meaningful relationships.
• Take up a hobby: Engage in activities that bring you joy. Join a club or group with shared interests to meet new people and build relationships.
• Practice self-care: Maintain a healthy diet, get enough sleep, exercise regularly, and practice mindfulness and self-compassion.
• Try something new: Step outside your comfort zone. It can be intimidating but can also lead to new connections and relationships.
Listen to our episode, “The Loneliness Epidemic” on the Community Check-in to learn more about this issue and who is most at risk.

in-home caregiving services unless your dad is receiving doctor-ordered skilled nursing or therapy services at home too. But if your dad is in a certain Medicare Advantage plan, or is low-income and qualifies for Medicaid, he may be eligible for some coverage.
Hiring an independent caregiver on your own is the other option, and it’s less expensive. Costs typically range between $15 and $25 per hour. Hiring directly also gives you more control over who you hire so you can choose someone who you feel is right for your dad.
But be aware that if you do hire someone on your own, you become the employer so there’s no agency support to fall back on if a problem occurs or if the aide doesn’t show up. You’re also responsible for paying payroll taxes and any worker-related injuries that may happen. If you choose this option, make sure you check the aide’s references thoroughly and do a criminal background check at companies like eNannySource.com.
To find someone use an elder-care matching service like Care. com or CareLinx.com, which both provide basic background checks.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

Upstate University Hospital
urologists Gennady Bratslavsky and Joseph Jacob have been recognized as two of America’s Best Prostate Cancer Surgeons for 2024 by Newsweek.
The inaugural list of best prostate cancer oncologists and surgeons includes 150 physicians nationwide.
“I am honored not only to be named as one of the top US surgeons, but to lead the only academic urology department recognized between New York City and Ohio,” said Bratslavsky, who serves as chairman of Upstate Urology and the Phillip Capozzi, MD, endowed professor of urology. “Even more impressive is the fact that Upstate Medical University and Upstate Cancer Center has not one but two surgeons [Joseph Jacob] recognized for such honor. Even more, in the entire country, there were only a handful of academic departments with two surgeons recognized as best in their field.”
“It is gratifying to be recognized nationally based on the independent and unsolicited study that focused on surgical outcomes,” said Jacob, chief of urological oncology at Upstate. “This further underlines our efforts in improving patient outcomes and our ability to perform this major surgery that allows patients to go home the same day of surgery. It was also
St. Joe’s ranked No. 1 by U.S. News & World Report ranks

St. Joseph’s Health Hospital retained its No. 1 ranking in Syracuse and was named a best regional hospital by U.S. News & World Report on its list of 20242025 best hospitals. It is also tied for 24th in New York state.
This is the 10th consecutive year St. Joseph’s Health Hospital has received the best regional hospital designation.
In addition, St. Joseph’s Health was ranked as a high performing hospital for nine procedures and conditions. This is the highest distinction a hospital can earn for U.S. News’ best hospitals and conditions ratings. The procedures and conditions are: aortic valve surgery, heart bypass surgery, heart failure, heart attack, chronic obstructive pulmonary disease (COPD), pneumonia, hip replacement, knee replacement and kidney failure
The annual procedures and conditions ratings are designed to assist patients and their health care providers in making informed decisions about where to receive care for challenging health conditions or elective procedures.
“I am incredibly proud of the leaders, physicians, nurses, support
rewarding to see that Upstate was the only cancer center other than Memorial Sloan Kettering Cancer Center in New York City recognized in all of the New York state.”
Bratslavsky and Jacob are fellowship-trained in urologic oncology, which requires two additional years of training after completing at least five years of residency training. Bratslavsky and Jacob also serve on the board of the Society of Urologic Oncology Clinical Trial Consortium.
Upstate’s urology clinical practice performs cutting-edge cancer surgeries, conducts groundbreaking clinical trials as well as teaches the new generation of surgeons.
According to Newsweek, the ranking reflects physician performance information based on Medicare data, an online survey of thousands of medical experts, a quality-of-care rating from each specialist’s peers and consideration of their certifications from the American Board of Urology, Radiology and Internal Medicine.
The uniqueness of this ranking is in the methodology that Newsweek had undertaken. It reviewed the data from hundreds of thousands of patients, and specifically focused on objective or measurable outcomes, such as deaths after surgery, any complications, readmissions (need to come
staff, and colleagues at St. Joseph’s Health for earning high accolades from U.S. News & World Report again this year,” said Meredith Price, senior vice president of acute oper ations at St. Joseph’s Health. “Being recognized as the No. 1 regional hospital underscores our unwaver ing commitment to providing safe, compassionate, and comprehensive care for all our patients. We are proud of this annual milestone, and it motivates us to keep delivering the best possible care to every family we serve.”
U.S. News evaluated nearly 5,000 hospitals across 15 specialties and 20 procedures and conditions. Hospitals awarded a “Best” designation excelled at factors such as clinical outcomes, level of nursing care, and patient experience.
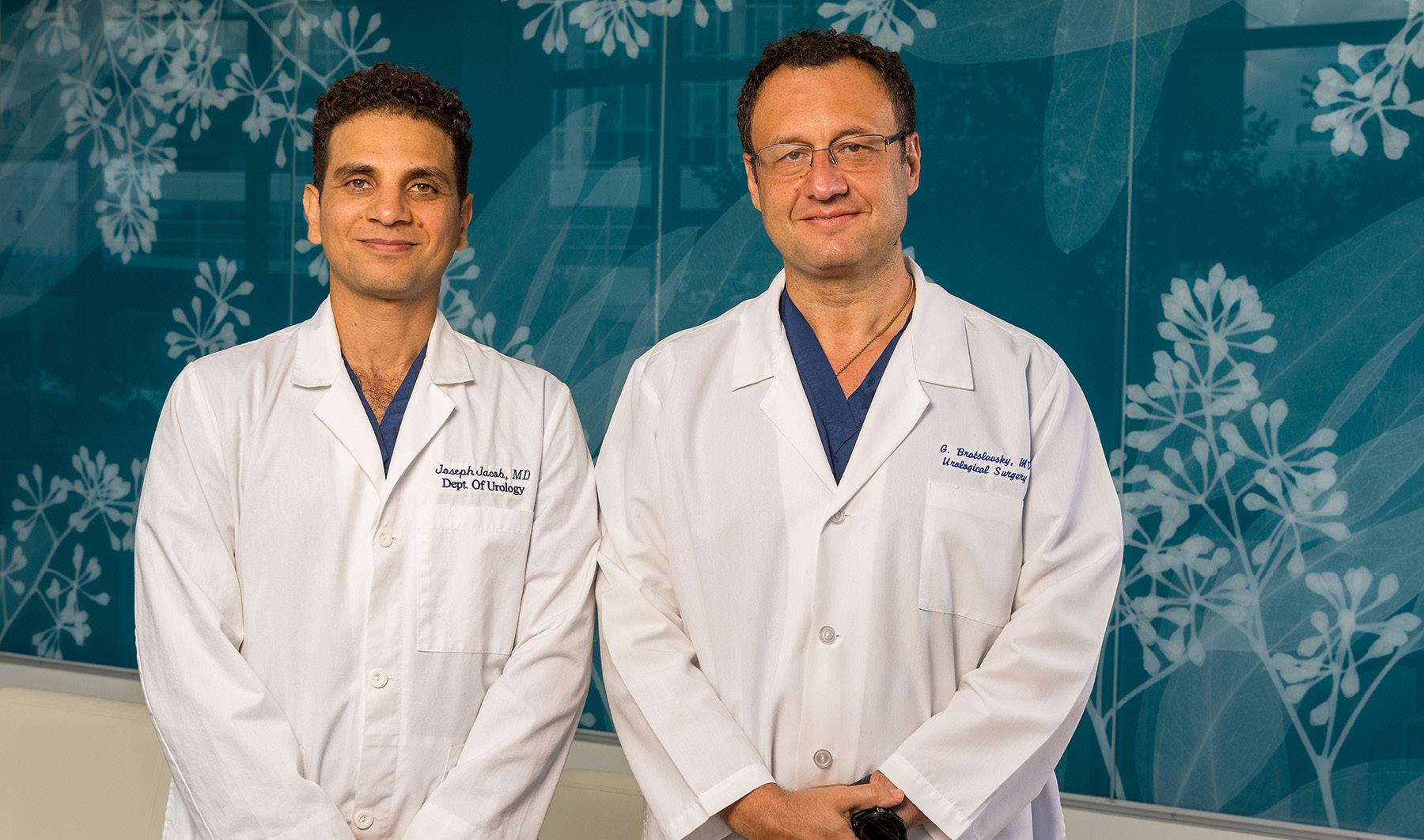
back for more procedures or further treatment), or length of the time that patients spent in the hospital.
In cases of Bratslavsky and Jacob, all these parameters were among the best in the country, in the group of elite surgeons with the best outcomes.
Previously, there has have been very little objective data on surgeons’ performance as much of the surgeons’ reputation is based on the “word of mouth.”
In releasing its list of best prostate cancer surgeons, Newsweek said: “For men dealing with prostate cancer, the doctors recognized here represent the best individuals to
sory Board.
They are:
• Physician Louis Bonavita Jr. — he attended SUNY Upstate School

“For 35 years, U.S. News has been a leading resource for patients navigating their health care decisions,” said Ben Harder, chief of health analysis and managing editor at U.S. News. “The ‘high performing’ designation acknowledges hospitals that consistently deliver high-quality care for specific medical procedures and conditions. This recognition highlights their expertise and commitment to patient well-being.”
Excellus BlueCross BlueShield has named two prominent leaders to its Central New York Regional Advi-
of Medicine in Syracuse, gradu ated cum laude in 1988, received the Bruce Farrell Memorial Award for Medical Excellence, and was elected into the Alpha Omega Alpha honor society. He completed his residency in family medicine at St. Vincent Health Center in Erie, Pennsylvania, in 1991. He was elected chief resident and received the Society of Family Medicine Teaching Award.
partner with in pursuit of a healthy future.”
According to the American Cancer Society, prostate cancer is the most common cancer in men in the United States. One in eight men will be diagnosed with prostate cancer at some point in their life. Other than skin cancer, it is the most common form of cancer in men and the second leading cause of cancer death in men.
The complete list of America’s Best Prostate Cancer Surgeons can be found on Newsweek’s website, www.newsweek.com/rankings/ americas-best-prostate-cancer-surgeons-2024.
ing year. Bonavita has been in private practice for the last 32 years.
• Elin R. Dowd — she joined the

Greater Tompkins County Municipal Health Insurance Consortium’s management team as executive director and its first full-time staff member in 2019. Dowd has been instrumental in growing the organization and remains committed to ensuring the consortium continues to deliver high-quality, trustworthy, cost-effective solutions to its members.
He completed his undergraduate studies magna cum laude from St. Bonaventure University in 1984.
Bonavita is a founding partner of CNY Family Care in East Syracuse and actively teaches medical students and residents in family medicine. He is an associate clinical professor in the department of family medicine at SUNY Upstate, an attending physician at St. Joseph’s Hospital. He is a member and fellow of the American Academy of Family Physicians.
His many accolades also include being elected NYS Family Physician of the Year in 2002 and being recognized as one of the nation’s “Top Docs” for family practice by the Consumer Research Council the follow-
Before relocating to Upstate New York in 2017, she was executive director of the Learning Centers at Fairplex in Pomona, California, and served on the Los Angeles County Fair Association’s board and management team. Dowd was a strategic adviser for the China-based Zhejiang Senhe Seed Co., Ltd., and vice president of human resources and learning for Monrovia Growers, one of the nation’s largest wholesale growers of ornamental plants and shrubs, prior to being named its president.
Dowd received her Bachelor of Arts in psychology from Drew University and her Master of Behavioral Science in human resource design from Claremont Graduate University. Dowd has served on several boards including Mann Packing Compa-
ny and California Botanic Garden. Dowd and her husband, Marcus, live in Watkins Glen and are the sole proprietors of the Idlwilde Inn.
“As a local health plan, our mission is to help people in our communities live healthier and more secure lives through access to high-quality, affordable health care. Dr. Bonavita and Elin will make immediate posi tive impacts to our board as we work to fulfill our mission,” said Mark Muthumbi, Excellus BCBS regional president for the Central New York region.
board of

utive at Advance, has 30 years of leadership experience as an operator, investor and adviser to technology companies, where she has focused on mobile, data and video communications, space technology, information technology and emerging technologies centered on improving the customer experience. In her current role as a senior leader at Advance, Bergman is focused on corporate development, investments and strategic partnerships. Previously president of Bright House Networks, Bergman was one of the company’s founders who led it to become the sixth-largest cable operator in the U.S., with 8,500 employees, 2.5 million customers, and over $4 billion in annual revenue. She also served as CEO of 1010data, an innovative data analytics platform which specialized in serving large retailers.
honors and supports innovators in information and communications technology. Bergman is also a trustee of her alma mater, the University of Rochester, Adaptive Spirit, Bridging Voice, the Cable Center, One Revolution and Syracuse University.

• Laurence Bousquet is a found
ing member of Bousquet Holstein, PLLC and currently serves as a member of the Crouse Health Foundation board trustees. Bousquet also serves as special counsel and as general counsel to businesses across many industries. Bousquet is committed to his community, a core value of his firm’s company culture. Throughout his career, Bousquet has served on the boards of many local charitable organizations, including president of the Hiscock Legal Aid Society, chairman of the Volunteer Lawyers Project of Central New York, chair man of the Crouse Health Founda tion, and chairman of the Everson Museum of Art and Rosemond Gifford Foundation.
Bousquet is especially proud of the work of the Onondaga Citi zens League where, in 2005, he was chairman and principal writer of the study on strategic governmental consolidation, guiding a year-long community wide process that exam ined all aspects of municipal consol idation and its applicability to local governmental structures. Bousquet currently serves as the Dunbar Association’s treasurer. He is also a director, treasurer, and co-founder of Central Current, a new home for nonprofit, nonpartisan and indepen dent journalism. Bousquet is an hon ors graduate of Kenyon College and Syracuse University College of Law, where he was previously an adjunct faculty member.
ric mental health team.
Bryant attended State University of New York at Delhi, where he obtained his Master of Science in Nursing degree. He attended State University of New York Polytechnic Institute for his post-master’s advanced certification in psychiatric mental health.
“We are excited to add another psychiatric professional to our integrated team,” said Tricia Peter Clark, president and CEO of ConnextCare. “There is increased demand in our community for additional mental health resources so we are delighted to have Tones onboard to further expand the collaboration with our primary care providers, who work collectively as one team, to meet the needs of our patients!”
Bryant will work in the Fulton office at 510 S. Fourth St. as well in the Central Square office at 3045 East Ave.
practiced clinically in at locations in Syracuse, Batavia and Medina. He completed his residency in podiatry at Staten Island University Hospital where he was chief resident of podiatric medicine and surgery. He earned his podiatric degree at the Temple University School of Podiatric Medicine, and his Bachelor of Health Science degree with honors at the University of Western Ontario in London, Ontario, Canada.

Svetlana (Lana) Dyer has joined
Bergman is an experienced board member who previously served as director of Comcast Corporation in addition to her current roles as a director of publicly-held Visteon Corporation, privately-held HawkEye 360 and Black & Veatch, and the Marconi Society, a nonprofit that
ConnextCare announced nurse practitioner Anthony (Tones) Bryant as the newest member of its psychiat-
Oswego Health recently announced the recent appointment of physician Wajeeh Sana as chief medical officer for the nonprofit healthcare system.
With over 17 years of experience as an emergency physician, Sana has been a member of the medical staff at Oswego Hospital since 2013. In 2023 he was appointed president of the medical staff. He’s held various leadership positions throughout his career in CNY including service medical director for McFee Ambulance and clinical assistantp at SUNY Upstate Medical Center. In 2015 he became medical director and chairman of the Oswego Hospital emergency department, Fulton and Central Square urgent care centers.
Sana earned his medical degree from one of the most prestigious medical schools in Pakistan, Allama Iqbal Medical College, and completed his residency at St. Vincent’s Mercy Medical Center in Toledo, Ohio.
In this new role as CMO, Sana will provide leadership, direction and planning for a wide variety of medical and related activities for the entire nonprofit healthcare system. As CMO he will serve as the liaison and resource to management on matters about medical staff activities to further the mission of the organization.
He will serve in a leadership capacity promoting and implementing changes that benefit patients and act as a liaison between the 100+ physi-
(SOS) announced the hiring of podiatrist Zerah Z. Ali. He is a board-certified podiatrist who has joined the SOS foot and ankle team. He is trained in all types of podiatric medicine and surgery, treating patients from pediatric to geriatric, with both surgical and non-surgical strategies. He is also trained in wound care with proficiency in hyperbaric oxygen therapy (HBOT), an advanced treatment of non-healing and traumatic injuries.
“I am thrilled to start working for Syracuse’s premier orthopedic team and look forward to being a part of their practice family,” says Ali. “I am very dedicated to my patients and my profession. I look forward to treating patients and providing the highest quality care to restore their foot health.

Prior to joining SOS, Ali was the head of the podiatry department with Wyoming County Community Health System. Before that he
Lana Dyer Loretto as manager of employee experience and retention, part of the human resources team that helps create a positive employee experience.
In this position, she leads employee engagement activities, develops retention initiatives and manages Loretto’s employee coaches who help employees connect with the resources they need to be successful on and off the job.
Dyer will also co-chair a newly formed cultural advisory committee, oversee recognition programs, support diversity, equity, and inclusion initiatives, and manage other responsibilities as part of the learning, development and employee experience department.
Before joining Loretto, Dyer worked as an economic development specialist for Onondaga County in the Office of Economic Development. Prior to that, she worked for over 10 years in healthcare as a guest relations manager at Crouse Hospital.
Dyer is a graduate of Henninger High School in Syracuse. She earned a bachelor’s degree in business administration (BA) from Keuka College and a master’s degree in business administration (MBA) from Monroe College.
“Lana brings a wealth of experience in the healthcare industry and customer satisfaction,” said Diana Wolgemuth, director of learning, development and employee experience.

cians and advanced practice providers employed by the health system and the 270 providers on the Medical Staff representing multiple specialty services across the community.
“We are fortunate to have Dr. Sana leading the clinical team here
at Oswego Health,” said Michael C. Backus, Oswego Health’s president and chief executive officer. “His commitment to our mission of quality, safety, service, and improvement of patient clinical outcomes is exemplary.”































From paddleboarding to sailing, the Finger Lakes region is perfect for staying fit — no matter your age!
By Jennifer Aline Graham

There’s no better place to stay active, healthy and mentally fit than in the stunning Finger Lakes region. Whether spending time dockside or wading in the water, the region is the ideal place to not only escape with family for a long weekend, but also to venture to when focusing on your own health and well-being.
When you’ve already experienced so many wonderful things and made so many memories during your lifetime, it’s only fair to continue making memories in a relaxing, beautiful environment.
And what’s more relaxing and beautiful than staying fit on a Finger Lake?

Whether at Skaneateles, Owasko or Otisco Lake, in a nearby pool or at the local gym, swimming is just as energizing as the next water sport or lakeside activity.
Swimming doesn’t have to be some basic activity — as the younger generations may say — just because it’s been a popular hobby and sport for many years.
It is an absolutely terrific activity to squeeze into your daily routine — especially if it’s happening at a lake!
Swimming can bring so many physical and mental benefits to the body and mind. Some of these benefits are:
• Less strain on your joints due to the reduction of gravity
• Provides mental and emotional clarity.
• Less pressure on certain parts of your body such as your hips,
knees and spine.
• Necessary self-care time to focus on clearing your mind and setting your body at ease.
Whether wading in the lake or working on your go-to stroke, spending time in the water is an activity to add to your spring, summer and fall. fitness regimen.


Though kayaking has been a popular lakeside hobby for many years, it doesn’t mean it isn’t just as thrilling as the next new activity. The thrill of exploring nature while gliding atop the water is a feeling like no other. The Finger Lakes region is filled with kayaking clubs, meet-ups and events where individuals of all ages can connect and kayak. There are many reasons this activity has remained so popular over the years:
• Enjoyable physical activity for all ages.
• Helps relax the brain and body.
• Improves coordination and balance.
• Supports cardiovascular health and wellness.
Connect with groups on social media, check out the local community center or reach out to locals in the town you’re staying in to see if and when kayaking clubs are getting together near you.
Take a sailing course
Sailing is no joke. This activity takes a lot of perseverance, focus and energy and is absolutely worth all of those dynamics and more. The
feeling of satisfaction your mind and body receives when you gain that balance on the water and let the sails take to the wind is a freedom like no other.
Some reasons sailing on the Finger Lakes is an activity to partake in are:
• Improves cognitive stimulation and focus.
• Deeper connection with nature.
• Reduces stress and anxiety being active on the water.
• Helps you learn and conquer new skills.
Sailing isn’t just an activity for you do alone. Your grandchildren will love learning from you and tagging along on your sailing adventure across the Finger Lakes.

Stand-up paddleboarding isn’t just for the zoomers and millennials. It’s also a great physical — and social — activity for the older generation to take a chance at and conquer. Though it may seem like paddleboarding popped back into the mainstream over the last decade, it is actually something that has been around for more than 3,000 years — originating in Peru. It has become a more normalized activity on the Finger Lakes and the reasons are evident:
• Improves balance and coordination.
• Provides growth of confidence and self-esteem.
• Lowers the risk of Alzheimer’s and memory loss.
• Supports cardiovascular health. Why not try something new this summer and fall? Go snag a paddleboard, snag a friend and try out a paddleboard class.

Whether you call it water aerobics, aquatic fitness or Silver Sneakers, one thing is for sure — it’s making a comeback. Or, to be honest, it may have never really disappeared in the first place.
Water aerobics is a way to stay fit and have fun while spending time in the water. There are many classes available to seniors on the Finger Lakes and all you have to do is find them, sign up and prepare to have a great time. There are reasons why water aerobics has continued to stay at the top of the list of favorite fitness activities to take part in when visiting a lake:
• Great cardiovascular exercise.
• Lessens pressure on joints.
• Improves range-of-motion.
• Boosts mental health.
When you want to stay active while having fun out in nature, try a water aerobics class in one of the Finger Lakes. You’ll find yourself feeling more energized and confident afterward.