

CAREGIVING
Madelen Barkins provides care for both of her in-laws, who were diagnosed with Alzheimer’s five years ago.
PLUS: 7 Myths About Alzheimer’s



Madelen Barkins provides care for both of her in-laws, who were diagnosed with Alzheimer’s five years ago.
PLUS: 7 Myths About Alzheimer’s
John and Judy Messenger remember the day in 2012 when they heard a knock on the door of their home. When they opened it, two policemen told them that James, their 30-year-old son, had taken his own life. Almost 12 years later, they still wonder why he left them that way.
September is Suicide Prevention month. See stories starting on page 9.




Thursday Oct 3rd 2024, 9am -1pm
CNY Regional Market E -Shed, 2100 Park st syracuse
We will be showcasing the attractions, classes , volunteers opportunities, part time jobs, experiences, travel, and living options for retirees in cny.

Cancer rates are rising among Gen Xers and millennials, a new study reports.
Successively younger generations are more frequently being diagnosed with half of the 34 known cancer types, researchers found.
For example, people born in 1990 have two to three times higher rates of pancreatic, kidney and small intestinal cancer than people born in 1955, results show.
Generation X is the demographic cohort following the baby boomers and preceding millennials.
“These findings add to growing evidence of increased cancer risk in post-baby boomer generations, expanding on previous findings of early-onset colorectal cancer and a few obesity-associated cancers to encompass a broader range of cancer types,” said lead researcher Hyuna Sung, a senior principal scientist of surveillance and health equity science at the American Cancer Society.
For the study, researchers analyzed cancer data from 23.6 million patients diagnosed between 2000 and 2019. The analysis also included data on 7.3 million patients who died of cancer.
Researchers broke the data down into five-year birth intervals from 1920 to 1990, and analyzed how cancer risk changed between birth cohorts.
Incidence rates increased with each successive birth cohort since
1920 for 17 of 34 cancers, researchers found.
Other cancers that have increased in younger generations include liver, breast, uterine, colorectal, gastric, gallbladder, ovarian, testicular and anal cancers, as well as Kaposi sarcoma, results show.
“The increase in cancer rates among this younger group of people indicate generational shifts in cancer risk and often serve as an early indicator of future cancer burden in the country,” said senior researcher and physician Ahmedin Jemal, senior vice president of surveillance and health equity science at the American Cancer Society.
Cancer death rates increased in successively younger generations for liver, uterine, gallbladder, testicular and colorectal cancer, results show.
Unfortunately, Sung said there's no clear explanation for why these rates are rising among younger generations.
“The data highlights the critical need to identify and address underlying risk factors in Gen X and millennial populations to inform prevention strategies,” Jemal said.
The results, published July 31 in the Lancet public health journal, also highlight the need for comprehensive health care among middle-aged and younger Americans, said Lisa Lacasse, president of the American Cancer Society Cancer Action Network (ACS CAN).


Don’t wait to get the care you need. When you visit the St. Joseph’s Health Cardiovascular Institute, you can expect the best. They’re rated high-performing in more heart procedures than all other area hospitals.* You’ll be back home and feeling better in no time. *U.S. News & World Report

For decades, millions of Americans popped a low-dose aspirin each day to lower their heart risks.
Then, accumulated data prompted the nation's two leading cardiology groups — the American College of Cardiology and the American Heart Association — to overturn advisories in 2019 and recommend against daily aspirin, citing a risk for bleeding that exceeded any benefit for most people.
Trouble is, many Americans aren't heeding that message and continue to take the daily pill, a new survey finds.
The survey, from a sample representing over 150 million U.S. adults, found that almost a third of heart-healthy people aged 60 or older said they took a daily low-dose (81milligrams) aspirin each day in 2021.
That's about 18.5 million older Americans, said a team led by Mohak Gupta, a physician in internal medicine who conducted the study while at the Cleveland Clinic. He's now practicing at Houston Methodist.
Add in folks under 60 and the number rises to more than 25.6 million Americans taking daily aspirin, the researchers estimated.
Given aspirin's now dubious risk-benefit ratio for folks at average heart risk, "our findings highlight the urgent need for physicians to inquire about aspirin use, including self-use, and engage in risk–benefit discussions to reduce inappropriate use for primary prevention in older adults," the researchers said.
They published their findings June 24 in the Annals of Internal Medicine.
As Gupta's team explained, data from trials published in 2018 cast doubt on prior recommendations for daily aspirin. That data instead showed a "limited benefit for primary prevention" when it came to heart issues.
"Therefore, the 2019 guidelines from the American College of Cardiology and American Heart Association discourage primary prevention aspirin use in adults older than 70 years," the team said.
Current advice from the American Heart Association (AHA) states that "because of the risk of bleeding, aspirin therapy is not recommended if you have never had a heart attack or stroke, except for certain select people."

By Chris Motola
‘We’re diagnosing people in their 30s and 40s with colon cancer,’ he says as he discusses ways to prevent the disease
Q: Tell us a bit about your work with colorectal cancer prevention in younger patients.
A: With screening guidelines going from 50 to 45 we’re diagnosing people in their 30s and 40s with colon cancer. It’s just becoming more prevalent, so we’re trying to be more proactive with those guidelines. The US Preventive Services Task Force made that recommendation in 2021. It takes a little time for the insurance companies to get onboard with new recommendations, but I think we’re pretty much there now, where they’re willing to cover screenings for at 45 for people who don’t have a family history of colon cancer. People born in the 1980s or beyond are at twice the risk of developing colon cancer under 50 compared to someone born in the 1950s. So that and just seeing these kinds of numbers in practice. It used to be the fourth leading cause of cancer death in men under 50, now it’s the leading cause of cancer deaths for that age group, and second for women under 50. The thing about colon cancer is that it’s preventable, so we want to intervene where appropriate. We’re seeing a lot of patients around age 45 who know someone who got a diagnosis or had polyps, so they tend to be motivated to get screened themselves.
Q: Does screening mean colonos copy or is it a broader umbrella?
A: We have multiple screen ing options. You’ve probably seen commercials for the non invasive testing options like Cologuard.
Q: I got a Cologuard test last year. How effective are they relative to invasive screenings?
A: It’s a stool test, so it’s a bit easier to do. The thing is, you can’t have any family history of colon cancer. You can’t have any symptoms. The idea is that as the stool is rolling around in the co lon, it would bump into any pol yps and cancers and pick up the
DNA that the test is looking for. There is a high false-positive rate of around 13%. The main benefit to a colonoscopy is when we do the procedure we’re looking for pre cancerous polyps that we can remove. Ideally, we’d remove them when they’re less that a centimeter. They can get larger and larger until they eventually become colon cancer. So we can just clean out anything we find. The large the polyp becomes, the higher the risks. So a colonoscopy is both diagnostic and deal with the polyps immediately if they’re there. With a positive Cologuard — and it may be a false positive — there’s a risk of stress from getting a positive result and having to wait with that knowledge until you get a colonoscopy.
Q: Why are colon cancer rates increasing this much?
A: There are a lot of theories. Sedentary lifestyle. Obesity. Smoking. Alcohol. Low fiber, high-fat diets. Processed meats and foods.
Q: If you do find polyps, what kinds of recommendations do you have for the patient afterwards?
A: First, we’ll send the polyps off to a lab, because there are different kinds of polyps that can occur. Some may be completely benign. Dependwhether there’s family history, we can clear you for up 10 years. If we find just a few adenomas, which are pre-cancerous, we’re looking at a five-year follow-up. If we find five or more, then years. If we take a very large polyp off, then we’d need to keep a closer eye on it for six months to a
What’s causing higher number of colon cancer? Potential culprits include sedentary lifestyle, obesity, smoking, alcohol consumption, low fiber, high-fat diets, processed meats and foods.
half of Americans who qualify for one are hesitant to proceed with a colonoscopy. It’s uncomfortable; they don’t like the idea of an invasive test. The worst part of it is probably the bowel prep. You have to be on a liquid diet the day before. The bowel cleanse itself has a lot of options now, though, where you don’t have to drink as much of the medicine, just more fluid. We even have pills as an option. So it’s a matter of finding which option works best for the patient. We also use sedation to make the patient more comfortable, so we do require a driver for the day of the colonoscopy. But thanks to the sedation most patients don’t feel or remember the procedure. They’re shocked we’re done by the time they wake up. Most people do pretty well.
Q: What got you interested in gastroenterology?

Q: Considering how effective early interventions are, what are the main barriers to preventing colorectal cancer?
A: Unfortunately, the data shows that less than
A: I like the combination of the surgical and procedural element mixed with the medical. You get to take direct action, preventing colon cancer with interventions, address bleeding issues. At the same time, we also treat a lot of chronic conditions where we can develop long-term relationships with patients with conditions like inflammatory bowel disease or liver disease. So you can watch patients you’ve diagnosed when they were young reach life milestones while helping to improve their quality of life and manage their condition.
Name: Thomas Lee, M.D.
Position: Gastroenterologist at Associated Gastroenterologists of Central New York, P.C.
Hometown: Buffalo
Undergraduate: Yale University; medical school: New York University School of Medicine; internship: New York University School of Medicine; residency: New York University School of Medicine; fellowship: Cooper University Hospital, Camden, New Jersey; board certification: internal medicine and gastroenterology
Affiliations: St. Joseph’s Health Hospital
Organizations: American College of Gastroenterology; American Society for Gastrointestinal Endoscopy
Family: Wife, two children
Hobbies: Scuba diving, skiing, cooking, tennis, international travel

In findings that suggest more young Americans struggling with mental health issues are getting the help they need, a new poll shows that nearly a third of American adolescents and teens received some sort of mental health treatment in 2023.
That translates to over 8 million young people between the ages of 12 and 17 getting counseling, medication or another treatment, the survey from the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) found.
"We're pleased to see that more people received mental health treatment in 2023 than the previous year," SAMHSA Administrator Miriam Delphin-Rittmon said in an agency news release announcing the survey.
Among adolescents, the biggest increase from 2022 was in the number of those getting mental health medications: Nearly 14% of those age 12 to 17 received such a prescription in 2023, up from 12.8% the year before.
SAMHSA officials said the increase shows that mental health treatment is finally being destigmatized.
Rates of adolescents getting mental health treatment has increased virtually every year since 2009, though the agency noted that changes in how the survey was done were
introduced in 2021.
In 2022, the survey estimated that 7.7 million youths aged 12 to 17 had received mental health treatment of some kind. The increase in 2023 amounts to more than 500,000 more young people getting treatment, SAMHSA noted.
Meanwhile, the rate of adolescents reporting a major depressive episode has remained roughly flat since 2021, at just over 18% of those aged 12 to 17, the survey found.
Psychiatrists classify a major depressive episode as a period of feeling depressed for at least two weeks.
While trends in substance abuse did not see major shifts in the 2023 survey, alcohol use did see a statistically significant drop.
In 2023, 47.5% of adults and adolescents — about 134.7 million Americans — reported drinking alcohol in the past month, down from 48.7% in 2022.
But rates of problem drinking were largely unchanged in 2023, with 21.7% reporting binge drinking and 5.8% reporting "heavy alcohol use." And around 10.2% of adolescents and adults reported drinking to the point where they met the criteria of alcohol use disorder.

By George W. Chapman

The Centers for Medicare & Medicaid Services developed the five-star system so consumers could make informed decisions.
Based on a survey of 46 quality measures, CMS assigns ranking from one to five stars. Undoubtedly, COVID-19 has had a significant impact on ratings. According to the ranking, 766 hospitals received four stars; 825 received three; 595 received two stars and 277 got just one star. You can check any hospital ranking at the
In order to maintain their tax-exempt status, nonprofit hospitals must provide charitable (free) care. Several states have established oversight of their nonprofit hospitals in order to determine whether or not the amount of charitable care provided is adequate enough to remain tax exempt. Charitable care can include free or discounted care, health education, free screenings and clinics. The obvious dilemma is just how much charitable care is enough to satisfy oversight committees? Ten states require their NFP hospitals to establish broad community benefit plans. Another 25 states require hospitals to publicize their financial assistance policies. Industry analysts believe it is far too difficult to establish fair metrics. Most likely, no steadfast rules are forthcoming and the whole issue may be kicked down the road. 90% of all NFP hospitals are already cash strapped and a 2.9% increase

Hospital Care Compare website. It should be noted CMS will penalize a hospital for deficiencies, but will not reward a hospital for good or improved performance. Hospitals are still reeling from the devastating impact of the pandemic, including staffing shortages, continuing inflation and fragile finances. Despite having fought the COVID-19 war, CMS chooses to kick hospitals when they are down. Lowering hospital ratings makes little sense in lieu of what they
from payers certainly won't make up for historical operating losses and increasing expenses associated with charitable or free services. About half of our 5,000 hospitals are NFP. There is roughly $220 billion in medical debt among consumers.

Since the Supreme Court overturned Roe v Wade a couple years ago, according to JAMA, the Journal of the American Medical Association, self-managed abortions are increasing. (All abortions are increasing.) Per the JAMA report, women cite privacy, the cost of travel to another state, fear of reprisal, the criminalization of abortion, the cost of child care and lost wages as reasons for self-managed abortions. Eleven percent used the abortion pill mifepristone. This has doubled since the overturning of Roe v. Wade. Others
and a half. Both of these metrics are constantly pressured by the massive increase in volume. The White House has recently granted more than $45 million to organizations fighting our

more than $27 billion. Despite this success, ripping off insurers and harming patients must still be worth risking your reputation and license to practice medicine. Physician Adrian Talbot operated Medex Clinical Consultants in Louisiana. He knowingly took cash from drug seekers. Prescriptions were pre signed and he rarely saw the patient. He falsified records to cover his tracks. He illegally distributed 1.8 million pills including opioids and morphine. He has been convicted of conspiracy and unlawful distribution of controlled substances. He is facing 20-40 years in prison.
have been through. Penalizing them is pouring salt on their wounds. CMS continues to be stingy when it comes to hospital payments. Effective Oct. 1, battle weary hospitals will get just a 2.9% increase from Medicare and Medicaid. Private insurers typically follow suit. Skilled nursing facilities, also subject to the five-star rating system and also still reeling from the COVID-19 war, will fare slightly better with a 4.2 % increase Oct. 1.
have resorted to drugs, alcohol, heavy lifting and hot baths to induce an abortion. States like Louisiana have moved mifepristone to the dangerous and controlled substance category meaning any illegal use could result in 10 years imprisonment. Legal use would now be only via prescription from a physician. Two hundred and fifty physicians in Louisiana signed a letter in opposition to changing the status of the abortion pill to a dangerous and controlled substance as mifepristone has been proven to be safe and not addicting.

Most of us are unaware of this potential life saver. Since being established in July 2022, monthly calls, texts, chats now average more than half a million. That is up 90% in just two years. The 988 hotline provides crisis counseling, resources and referrals. There is an 89% answering rate and wait times are down to less than a minute
Less than half of us challenge them. But half of us who do challenge denials prevail per a Commonwealth Fund survey. One third of us who disputed a medical bill had their balance reduced or eliminated. Medicare and Medicaid patients were more prone to disputing denied claims or questionable bills than those commercially insured. Most people are not aware of their right to dispute denied claims or questionable balances due. The Commonwealth Fund suggests more consumer protections and education and increased public awareness. Fifteen percent of all claims submitted to commercial insurers are initially denied. Three percent of all denied claims were actually pre approved via prior authorization. About half of all denied claims are ultimately paid. But that wouldn't happen unless disputed.


George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.
By Eva Briggs, MD
My daughter suggested this article after noting that several of her co-workers mentioned their recent cleanses and detox experiences.
This is not about legitimate detoxification to help people stop using alcohol or drugs. And it’s not about chelation therapy to treat lead poisoning. It’s about the multi-billion-dollar business of selling people juices and other herbal concoctions that claim to remove toxins from the body.
Yes, in the course of daily life we are all exposed to environmental toxins from air pollution, cigarette smoke, household cleaning products and ultra-processed foods.
Fortunately, our bodies are designed with various organs to deal with these assaults. Most toxins are excreted naturally in sweat, breath, urine and feces. The liver breaks down many toxins from food, alcohol and medications. The kidneys filter out these broken-down toxins which are then urinated out.
You can help your body’s natural mechanisms with a healthy lifestyle starting with a balanced diet. This includes drinking plenty of water, eating protein-rich foods, vegetables, fruits, beans and nuts. Limit alcohol and ultra-processed food.
Juice and herbal cleanses don’t
add anything to your body’s innate abilities.
The term “toxins” is very vague. A few years ago, dietitian and journalist Cara Rosenbloom contacted a dozen companies and practitioners. She asked what toxins their products claimed to remove. Pesticides, bisphenol A, phthalates? As she points out, it isn’t possible to design a study to determine whether any actual toxins are being removed effectively without knowing the target. Not a single one provided any evidence or studies to support their claims.
This entire vague concept becomes fertile ground for deceptive marketing. People naturally want a quick fix.
Many Americans eat a lot of ultra-processed foods that are low in fiber. This leads to gastrointestinal discomfort and perhaps constipation. So, drinking a lot of juice while avoiding solids has a laxative effect, leading people to believe that toxins were removed. Sometimes weight loss is touted as a benefit. There is no more weight loss than would occur with any other very low-calorie diet. And much of the weight loss from a cleanse derives from fleeting temporary water loss.
You may wonder whether cleanses have any harmful effects, other than to the patient’s wallet.

With food products or juices the risk of harm is low. Supplements are poorly regulated, so there is potential harm because it’s impossible to know what ingredients and how much is in there. Short term — less than seven days — cleanses are generally safe. Longer term cleanses could cause nutrient deficiencies, fatigue, electrolyte imbalance, low blood sugar and mood disturbances.
There is also the potential for mental harm. Cleanses can play into the restriction-binge cycle that leads to eating disorders.
On a final note are detoxifying foot pads and foot soaks. They don’t work. If you leave the foot pads on overnight they will change color. That does not signify any sort of toxins leaving the body. It’s simply a chemical reaction between the
substances in the pad itself and your normal foot sweat. The same for foot soaks with special ionizing devices. The change in water color comes from the device itself, not from toxins leaving your body.
The bottom line — spend your money on something you need or enjoy. Don’t waste it on fancy cleanses or devices which do nothing.

By Gwenn Voelckers
It’s early September, and I can already see the leaves on my sunset maple transitioning from vibrant green to a deep reddish hue.
I love the change of seasons.
And as I sit here staring out the window, I can’t help but reflect on my own journey of change after my divorce.
Just like fall's colorful display of resilience, I've come to realize that life is a series of seasons — and embracing change is the key to personal growth.
It’s just one of many life (and leaf!) lessons nature has taught me.
For those living alone after a significant life event like divorce or the loss of a loved one, it's crucial to acknowledge that change is a natural part of life.
While it can be daunting to embrace yet more change in the midst of an already challenging transition, it's through this process that we discover our strengths and uncover new aspects of ourselves.
As I embarked on this journey of self-discovery, I came to appreciate the benefits of embracing change:
• Personal Growth: Change encourages us to learn, adapt and acquire new skills. We become more
versatile and competent individuals. I felt so proud when I purchased a new car all on my own.
• Resilience: Facing and overcoming life's challenges helps us develop our capacity to recover from setbacks and pull through tough times. Spending a Friday night alone can feel victorious!

• Flexibility: Developing the ability to adapt to change fosters flexibility, a valuable trait that enhances our capacity to navigate life’s twists and turns with grace and ease. This is especially helpful while traveling solo through life, as well through airports.
• Overcoming Fear: Learning to embrace change can help us overcome the fear of the unknown and build confidence in our ability to face and conquer challenges. With

practice, I was finally able to walk into an event alone without shaking like a leaf.
• Self-Discovery: By stepping out of our comfort zones and navigating change, we uncover hidden strengths, values and passions that may have otherwise gone undiscovered. Who knew I would become a drummer at my age?! What’s your yet-to-be-revealed talent?
Over the years, I've developed strategies that have helped me embrace change and foster positive transformations in my life. Check ‘em out:
• Develop a growth mindset, which views challenges and setbacks as learning opportunities rather than insurmountable obstacles. Living alone gives us all plenty of problems to solve. Embrace them!

• Be patient and kind to yourself as you navigate change, recognizing that setbacks and struggles are a natural part of the process.
• Strengthen your resilience by engaging in self-care activities, such as exercise, meditation, and spending time with people you love. I can vouch for pickleball!

• Build a support network of friends, family or advisers who can offer encouragement, advice and accountability as you pursue positive changes. Finding a trusted financial adviser was one of the best decisions I ever made.
• Remain open-minded and flexible in your approach to change,
recognizing that there may be multiple paths to achieving your goals.
• Regularly reflect on your progress and celebrate milestones, no matter how small, to maintain motivation and momentum. Think ice cream, a massage or — my favorite — Saint-André triple crème cheese on a warm baguette. Yum!
• Approach change with curiosity and a desire to learn, recognizing that each experience teaches you valuable lessons about yourself and the world around you.
As you navigate the ever-changing landscape of your own life, remember that each of us possesses a remarkable potential for personal growth and transformation. This capacity is already inside you. It just needs to be tapped.
I found inspiration in nature. It showed me that change is essential for survival and growth.
Just as the leaves change in response to their shifting environment, you, too, can learn to adapt and grow from your circumstances. And enjoy the changing seasons of this new life chapter.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
As kids and teens return to school, parents might not have protecting their child's lung health on the top of their to-do lists. But experts say it should be.
“A new school year often means a new environment for students and staff, including new asthma triggers, exposure to new viruses, peer pressure to smoke or vape and other stressors that can impact the health of students,” said Harold Wimmer, president and CEO of the American Lung Association (ALA). “Students and staff spend a significant amount of time in school, so it is critical to their well-being and education that they are in the healthiest environment and are making the healthiest
choices possible.”
To that end, the ALA has created a youth initiative to help schools and caregivers address chronic lung issues like asthma, air quality and tobacco-free policies. The initiative offers information, guides and sample policies that can be implemented in schools to protect students and staff.
The group is also working to educate parents, students and school officials in four key areas of lung health:
• Asthma: There are 6.1 million kids under the age of 18 living with asthma, a leading cause of missed school days. The ALA has in-depth resources for parents, young adults

and schools on managing asthma, including a free online course for school personnel who administer asthma medications and seek to understand and implement quick-relief stock asthma medication laws, policies or programs.
• Tobacco Use: A new school year can also mean peer pressure increases to vape or smoke. According to the 2023 National Youth Tobacco Survey, more than 2 million middle and high school students reported that they had used e-cigarettes in the last 30 days. The ALA has resources to prevent tobacco use and help youth quit, specifically designed for schools, parents and teens.
• Indoor Air Quality: Some breathing hazards are not as obvious, like indoor air pollution and greenhouse gas emissions. Poor air quality in schools can affect student, teacher and staff's attention, thinking and ability to learn. The ALA offers a free downloadable guide on how school administrators can improve their indoor air quality.
• Infectious Respiratory Diseases and Vaccinations: A new school year means new friends, new teachers and sometimes, new viruses, so students need to practice good health hygiene habits and get recommended vaccinations, including influenza and COVID-19 shots.
By Kyra Mancine
Suicide is a topic that makes many uncomfortable. Yet it needs to be addressed.
According to the National Alliance on Mental Illness, 20% of high school students reported serious thoughts about suicide. As we start a new school year, your child’s safety, health and well-being are more topof-mind than ever. Suicide prevention month is the perfect opportunity to learn how to recognize and address mental health concerns.
After emerging from years of COVID-19 restrictions, we are just beginning to see how isolation has impacted children, teens and young adults.
While suicide affects individuals of all ages, young people are the most vulnerable.
Did you know that suicide and self-harm incidents have increased by 87% over the past five years? Besides everyday pressures, today’s students face challenges previous generations
didn’t have to worry about, including cyberbullying.
Be aware of the warning signs and risk factors
A family history of suicide, trauma, anxiety disorders, lack of social support or the loss of a relationship can make someone contemplate suicide. Talking about wanting to die, looking online for a way to die, withdrawing, and giving away possessions can be red flags that require intervention.
Don’t be afraid to start a dialogue with someone who is struggling. It’s important to establish rapport and trust. Be genuine and empathetic with your choice of words and tone of voice. Talking about suicidal thoughts still has a stigma to it. Let
By Deborah Jeanne Sergeant
The loss of a loved one is compounded when suicide was the cause of that loss.
In addition to the grief that accompanies any death, the surviving family may feel numerous other emotions that are difficult to experience.
“A peer-led grief support group offers families who have lost someone to suicide a unique space where they can connect with others who truly understand their pain,” said Kelly Ocampo, executive director of Hope for the Bereaved in Syracuse. “Sharing experiences with those who have faced similar loss fosters a sense of community, reduces feelings of isolation and provides valuable emotional support.
“Additionally, participants often find hope and resilience through hearing how others are navigating their own grief journeys.”
Understanding suicide can also help the surviving family members.
“Connecting with others in a structured and supportive environment can help individuals better understand the struggle of depression and suicidal ideation, understand they are not to blame and receive support from others,” said Monique
your child know it’s OK to have uncomfortable feelings. Reassure them that you are not there to judge, but to help and support.
Are you familiar with how your school handles mental health issues? Many districts use web monitoring software and other technologies to flag, review, and de-escalate harmful language and content before it’s too late.
There is no shame in reaching out for help. Struggling students can benefit from teletherapy, mental health coaching sessions and, if necessary, assistance from trained crisis counselors with expertise in support-
ing children and teens. Recently, there has been a national push to reduce or eliminate cost barriers to these services, which should help to increase participation. By sharing information, we can increase awareness and help support young people in need. From there, compassionate, proactive approaches and tools, including the appropriate interventions, can make a real difference. Staying up-to-date on the latest services and resources can mean the difference between life and death.
If you or someone you know is struggling, there is help
• 988 Suicide & Crisis Lifeline 24/7 free, confidential support https://988lifeline.org/
• National Alliance on Mental Health www.nami.org
Winnett, Ph.D., and clinical psychologist at St. Joseph’s Health.
Losing a loved one can feel surreal and more so if the cause of death is suicide. The conversations in a support group can help survivors’ emotions feel more normal, as they can range from sadness to regret to anger to guilt.
Other loss groups typically can’t provide the same level of understanding as suicide bereavement groups as the stigma attached to suicide makes it difficult for survivors to feel as welcomed in other groups.
“Families often want to keep it a secret when a member dies by suicide,” said physician Robert Gregory, director of the Psychiatry High Risk Program and professor at Norton College of Medicine at Upstate Medical University. “In addition to the social embarrassment, there is usually also a deep sense of guilt and anger that can interfere with the normal and healthy bereavement process.
Family members may be asking themselves, ‘Why didn’t I recognize the signs, so obvious in retrospect?’ ‘Did that argument I had with them last week cause the suicide?’ ‘Why didn’t I reach out more?’”
He added that it’s also normal

to feel anger toward the person who died because of the trauma and pain they caused. Or sometimes anger toward the healthcare providers who could not help prevent the person’s death.
“Groups, counselors and other supports may be very helpful for the family member to process their emotions in healthier ways, to facilitate the bereavement process and to normalize some of their reactions to reduce their sense of stigmatization,”
Gregory said. “Suicide happens despite the best efforts of family members, friends, health care providers and the individual themselves.”
Joining a support group can facilitate healing through sharing what helps ease the pain and realize that it’s OK to experience their full range of emotions. The groups can also help people know how to deal with outsiders’ often inappropriate and painful questions and comments.
Overall, joining a support group can help the surviving family by feeling that others understand the type of pain they’re experiencing. That support can help them feel not so alone.
The following organizations host group meetings and offer resources for people who have suffered loss through suicide:
Hope for the Bereaved https://hopeforbereaved.com/services/support-groups
American Foundation for Suicide Prevention https://afsp.org/chapter/greatercentral-new-york
Alliance of Hope https://allianceofhope.org
National Alliance on Mental Illness https://namisyracuse.org

By Deborah Jeanne Sergeant
Why my loved one? Why my friend? What could have kept him from taking his own life?
Preventing death by suicide is not straightforward. But as with any health crisis that causes death, most people want to know afterwards what increased the risk for that individual. Warning signs are common and can point to many other scenarios, yet suicide is rare.
“A helpful way to think about suicide risk is that thoughts of suicide emerge when people are feeling
stuck alone with overwhelming pain,” said physician Robert Gregory.
“Feeling stuck” indicates helplessness and hopelessness — even for people who have loved ones near them.
Gregory is the director of the Psychiatry High Risk Program at Upstate Medical University. He also teaches at Norton College of Medicine at Upstate.
It may seem hard to believe that people with loved ones all around them—caring friends and family--feel alone. But it’s not about the
presence of other people. It’s how connected individuals feel.
“They may feel alienated from those people and create a false self that appears to be happy and cheerful; but inside they are actually in deep pain,” Gregory said. “For the elderly, the pain may be physical. For young people, the pain is usually an inability to acknowledge and process painful emotions, such as shame, sadness or anger.
“We know that suicidal individuals have deficits in the emotion processing system of their brains, causing them to be easily overwhelmed by emotions and become anxious, irritable or depressed.”
Meaningful connections matter when looking for suicide risk. Watch someone who’s becoming more isolated and adopting unhealthy coping mechanisms like substance use or self-harm. Gregory said these are all red flags.
“There may also be decreased functioning at school or work and a preoccupation with negativity and thoughts of worthlessness or death, which may come out in conversations or artwork,” he said.
It may seem like asking if someone is considering suicide may “put the idea in their heads,” but Gregory said that’s not so. In fact, it shows family members that you care about them enough to ask tough questions.
“An example of how that might be asked includes, ‘I noticed that you have not been yourself lately and wondered if you are struggling with thoughts of ending your life?’” he said. “If the answer is affirmative, ask follow-up questions such as, ‘Tell me more about that’; ‘Have any plans run through your head?’ and ‘How close have you come to carry-
ing out those plans?’ The follow-up questions can give you a sense of severity and imminence. But you also have to watch out for the individual minimizing the risk. Therefore, any thoughts of suicide should be taken seriously.”
It’s not a matter of seeing one or two signs of elevated risk, but multiple factors or extreme examples of one or two risk factors.
Monique Winnett, Ph.D., and clinical psychologist at St. Joseph’s Health, said that the factors that increase suicide risk include “chronic and/or life changing physical health conditions; depression, anxiety, substance abuse, other behavioral health conditions; feelings of hopelessness and helplessness; isolation/lack of community or meaningful relationships; absence of spirituality or faith; and recent psychosocial stressors or losses, such as job, relationships, death of others.”
Like Gregory, she advises worried family members to voice their concerns, as well as keep the person company and offer support. One means of doing that is helping to connect them with professional resources that can help. Of course, in an emergency, call 911 or “go to the local emergency room if they cannot keep themselves safe,” Winnett said. “Contact their primary care provider or their behavioral health provider if they have one.”
Contact Upstate’s Psychiatry High Risk Program (www.upstate. edu/phrp) at (315) 464-3117. Contact crisis support by dialing 988 or in Onondaga County, The Contact Hotline at (315) 251-0600 or Crisis Connect at (315) 251-0800. All these options are confidential and available 24/7.

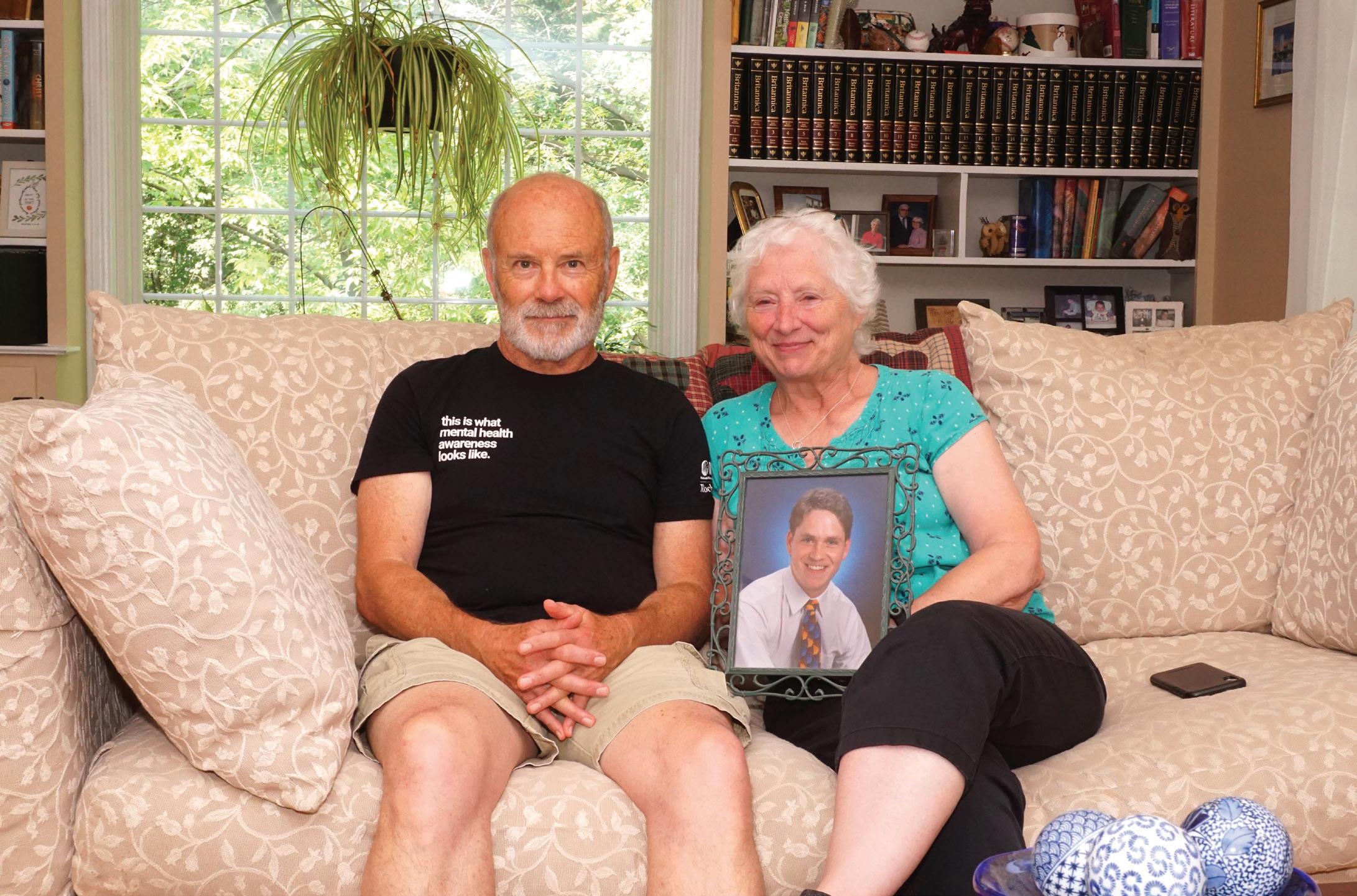
John and Judy Messenger present a photo of their son James that was tak en when he graduated from Sharon High School. The Messengers lived in Sharon, a suburb of Boston, Massachusetts, until they moved to Pittsford in 1999.

ship, but we deal with certain things differently,” he said.
By Mike Costanza
John turned to friends, relatives and members of his church to talk about his loss, including Tim Smith, a friend from First Presbyterian who is a Stephen Minister. Stephen Ministers are specially trained, volunteer lay counselors who provide one-toone, Christ-centered care to people who are experiencing life difficulties.
John and Judy Messenger remember the day in 2012 when they heard a knock on the door of their Pittsford home.
When they opened it, two policemen told them that James, their 30-year-old son, had taken his own life.
Almost 12 years later, they still wonder why he left them that way.
“We have no idea what was going on in his mind or why he did it,” Judy said.
James, the second of the Messenger’s three sons, was easygoing, kind and sensitive to the feelings of others.
“I used to say he was exactly like me, only younger, taller, better-looking and more talented,” John said.
James had a talent for music, played the trumpet, guitar and keyboards and sang in his family’s church and at school events — he played Daddy Warbucks in his middle school’s production of “Annie.” As a young man, he played his guitar and sang in local coffee houses and toured Europe with Mastersingers USA, the top-notch men’s chorus of which John is a member. He also enrolled at Syracuse University, intent upon acquiring a degree in communications, but dropped out after two years. He lived in Syracuse for a while, then spent several years living with his parents. During that time, he became a deacon in the First Presbyterian Church of Pittsford, the house of worship his family attended. By the time of his death, James had long grappled with mental health issues. He heard voices and sometimes carried on conversations under his breath with people who didn’t exist. In his early 20s, he was diagnosed with schizoaffective disorder and bipolar disorder and ended up being hospitalized three times for brief periods.
Those suffering from schizoaffective disorder can experience a mix of symptoms, including visual and auditory hallucinations, delusions, depression and mania. Bipolar disorder manifests itself in extreme mood swings. The person diagnosed might feel euphoric one moment and
depressed the next. Both conditions require treatment with medications and counseling. Those who do not obtain treatment are at a greater risk of suicide than the general population.
James obtained treatment for his disorders, but sometimes did not take his medications as required. In addition, he sometimes drank heavily and smoked marijuana, reducing the drugs’ effectiveness. As his disorders and use of alcohol and marijuana took their toll, James lost interest in the things he’d once enjoyed.
“He was failing,” Judy said. “He wasn’t taking care of himself.”
As James struggled, the Messengers had to deal with their own issues. Both were laid off from their jobs in 2012 — John was an in-house attorney and Judy was a regulatory analyst and manager for a local telecom firm. By October of that year, Judy had retired and John was hunting for a new position and doing freelance legal work. The couple was also preparing to sell their Pittsford home and move into a new, smaller residence in Brighton.
Oct. 8, 2012, was a bright, sunny fall day, according to John. He took James to a local Bruegger’s Bagels shop for a sandwich, then home for a visit. James spent hours in his parents’ backyard alone, then joined them for dinner. After that, John drove him to Pinnacle Place, the Rochester high-rise in which he was living.
James hugged his mother just before he left, a gesture that struck Judy, since he had grown distant from her down through the years. At 5 o’clock the next morning, she and John learned from the police that James had jumped from the roof of Pinnacle Place. He was just shy of his 31st birthday.
The news of James’ death hit the Messengers hard.
“We had just spent the previous afternoon and evening with him at our house and everything seemed fine,” Judy said. “If anything, he was a little bit more friendly than he had sometimes been.”
Each of the Messengers reacted to the loss in their own way.
“I think in each of our separate ways, we were a little bit on autopilot and in shock and therefore doing practical things, because it was so hard to process fully,” John said.
Judy offered coffee and breakfast to the officers, which they declined.
“I was trying to process the whole thing, because it didn’t make sense to me,” she said.
John wanted to learn more about the way James died. After the two police officers left, he dressed and drove to Pinnacle Place. The night security guard was still on duty.
“He took me out and showed me a bush that had been crushed by his [James’] fall,” John said.
The couple then started the long, painful journey through their grief.
“Even in the course of a conversation, you experience several different ways of experiencing the grief,” Judy said.
Anger was part of that experience.
“There’s some anger with yourself that you missed it,” she said. “How could you not see the signs?”
Some of that anger was reserved for James.
“I was angry with him for doing it,” she said.
Though family members, friends and members of First Presbyterian offered their support, Judy began working through her feelings on her own.
“A lot of it is being left alone to process through myself,” she said.
Though she turned to some of the women in her church, it wasn’t for sympathy.
“They were just there,” she said. “I knew that if I needed them, they were available to me.”
John was also there for her.
“He was my rock, my support,” she said. “I knew that if I had a question, a concern, I could always go with him.”
John was much more comfortable talking to others about the loss of James.
“Judy and I have a great relation-
“I tend to want to talk things out. [Judy] often processes things first to herself,” John said. “It was helpful to have some third person to talk to.”
The couple also found they could draw comfort from helping others who had lost someone to suicide or had relatives or friends who were at risk of taking their own lives.
“Both of us, I think, get a lot of our value and purpose in life from helping other people,” Judy said. “I think we are empathetic for someone who has gone through this.”
First Presbyterian’s associate pastor began referring members of her congregation to them for assistance.
“Folks who had someone who was considering suicide or had mental illness of some degree would come and talk to us,” Judy said.
The couple has continued to make themselves available since moving to Rochester’s Asbury First United Methodist Church a few years ago. In addition, Judy volunteers as an office manager for NAMI Rochester, the local chapter of the National Alliance on Mental Illness and makes herself available to talk to those in need.
“When we get a call from NAMI that someone has lost a child, that call comes to me,” Judy said.
Though it’s been 12 years since James left them, he is never far from his parents’ thoughts. They have wind chimes hanging from their car’s rear-view mirror that they bought to remind them of James.
“Whenever they play, I think it’s James talking to me,” Judy said. “It’s just lovely.”
The Messengers moved into a new home in Brighton in 2013. John landed a job that year as an attorney for a local firm and remained in that position until he retired in 2021. As he looks back on the years since James took his own life, he marvels at the way he and Judy have come through them.
“This is the sort of thing that has a lot of collateral damage and we’ve been very aware and lucky that we’re both very strong and resilient people and we have a fabulous relationship,” he said. “If anything, it made us stronger together.”
The national initiative that is raising awareness about the 988 suicide and crisis lifeline celebrates two years
The National Suicide Prevention Lifeline in 2022 transitioned to 988 (Suicide and Crisis Lifeline), an easy-to-remember number that promotes access to free, 24/7 crisis support available via phone, chat or text. Its celebrating two years this year.
In Central New York, Contact Community Services is one of the over 200 centers nationally that has trained crisis counselors who answer 988 and has played a role in the 10 million calls, chats and texts that have been answered to date.
Contac, 988 centers across the nation and SAMHSA (Substance Abuse and Mental Health Services Administration) continue to raise awareness surrounding 988 through a national campaign that promotes mental health support by sharing the message of “No Judgement. Just Help.”
Contact asked its counselors what this message means to them. Here’s what they said:
• “There are no barriers to accessing our services, you can share as much or as little as you feel comfortable;”
• “There’s always a hand reached out to help-no matter what your experience is;”
• “988 is always here for you, 24/7 support at your fingertips.”
To spread the message of “No Judgement. Just Help.” and the availability of 988, share #988Day on social media and in conversations with others within your community, urges the organization.

Executive director discusses the 75th anniversary of Prevention Network and talks about its mission to prevent addictions and address substance abuse
By Mary Beth Roach
Q: What is the mission of the Prevention Network?
A: The mission is to provide support, services and opportunities to our community through implementing and supporting strategies that promote healthy choices that prevent addictions and address related concerns.
Q: What are the specific programs you offer?
A: We have services under three primary buckets. Our largest is our primary prevention services, which is what people would most likely consider typical prevention services we offer individuals, and prevention education on substance-related topics.
We also offer parenting courses to individuals who either are mandated or who just need a little extra support in the parenting arena, maybe because they have a substance-use disorder or possibly because their substance use is related to some challenges that they’re facing in that area.
We also educate the community. We do a lot of what we call health promotion events, where we table and provide resources and information on current drug trends, what’s being seen in the community, signs and symptoms of potential substance use and provide that information for people who might be concerned that they don’t understand a substance or that their loved one might be experiencing a challenge with it.
A newer area of primary prevention is environmental prevention,
provide the technical assistance and training to help those groups address their goals and move through possible funding.
Q: How has the legalization of cannabis impacted your work?
A: Anytime a substance gets more attention, it brings a lot more questions to us as an organization. It’s been a challenge for a lot of parents as to how to have conversations with their young family members about a substance that used to be illegal and now it isn’t. They need to address it the same way they address alcohol. It’s still for adult use only, not for teens. But I think the main thing is that a lot more people are reaching out to get more information. We provide a lot of education around cannabis and the different forms being offered for adult use, the potency and what that means.
Q: As your agency marks its 75th anniversary, what changes have you and your team seen?
A: Because we’ve had our 75th anniversary, we actually dug through a lot of old historical documents for the organization. The organization’s official name is the Onondaga Council on Alcoholism and Addictions. So, the agency started out primarily focusing on alcohol and alcoholism and that was a focus for a long time. From what I can gather from the historical documents, somewhere in the late ‘80s, they added the business name of Prevention Network. In the last decade a huge focus has been on opioids and availability of that in the community. In Syracuse, we still have a high concentration of individuals who are using what’s called synthetic marijuana or “spike.”
where we work more within the community, bringing people together to address the environment in which people live and how they’re exposed to substance use. Organizations will band together to create policies or messages around how to have safer use of substances or how to protect substances, so they don’t get diverted to children or others.
Another bucket of service is family support. Navigators are charged specifically with working with families who have a loved one who is experiencing a substance-use disorder. Often in the treatment cycle, the families are neglected. There’s not an understanding on their part necessarily of why their loved one continues to use even though they know it’s bad for them, of the connection to mental health or how they get services for themselves. There are services that our family navigators can offer.
And then we are the home to the Central Region Prevention Resource Center, which is a separate initiative that the New York State Office of Addiction Services and Supports funds to provide a team of community development specialists working in a 13-county central region to form and support coalitions who might be working on substance use and related topics.
A lot of communities, since the opioid epidemic, have formed county drug task forces or a school or community group might come together to address youth substance use. Our prevention resource center can
Our knowledge needs to broaden and expand to understand the new substances that are available and make sure that we’re providing the up-to-date information. A lot of these things aren’t new; it’s just new to how it’s being used.
Q: What do you see moving forward for your organization?
A: I like to think that through the different programs that we’ve offered over the years, one of our strong areas is providing education and training. We’d like to get back to providing some community-based education for professionals and the community.
Stigma has such a huge impact. There’s so much stigma that it’s some kind of a moral failing or that you should just be able to stop what you’re doing. So many people still don’t reach out and get the help they need because they’re concerned about the stigma associated with it. We try to do education around that. How is this any different than the other health concern that somebody has? Individuals that are suffering should be treated the same way as those who are experiencing other health-related concerns.
Q: Is there anything you’d like to add?
A: I did some research when we were getting ready to celebrate the 75th anniversary. As a not-for-profit, that’s pretty monumental. A lot of not-for-profits fold by year 6. The fact that this organization has been around for 75 years is a testament to the need and the type of people who we have working at the organization. They’re all very compassionate, dedicated people who want to help.
MANAGEMENT GROUP
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN UP
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEM OUP




Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP
















MANAGEMENT GROUP

Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
CONTACT:

Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
CONTACT:
Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
Phone: 315-529-3267
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com




















Going to the gym is good for your overall health, but if you and the gym aren't practicing good hygiene you could still catch a nasty illness, an expert says.
“Good hygiene prevents sicknesses like a cold, influenza and even salmonella, but cleanliness can also indicate that a gym is well-maintained overall, including the quality of equipment,” said Melanie McNeal, a physical and occupational therapy manager at Baylor College of Medicine in Houston. “If hygiene rules are not followed you could get sick, get others sick or even have your membership cancelled.”
When going to a new gym for the first time, there are a few key indicators to determine if hygiene is prioritized in the space:
• A lack of sanitary wipes for members or staff to wipe down equipment after use often means equipment is harboring unseen bacteria
• No signs posted asking members to clean equipment after using or no cleaning schedule posted suggests cleanliness is not a priority for the gym
• Other gym members using equipment and not cleaning it afterwards on a consistent basis can show there is not a culture of cleanliness
• Caked on layers of dust on equipment can indicate that equipment has not been cleaned in
• Lots of broken-down machines for extended periods of time can be due to a lack of interest from gym management in ensuring the space is well-kept
To do your part in practicing good gym hygiene, there are several things you can do.
• Wear clean clothes each time you exercise; used clothes accumulate sweat and other bacteria that can cause foul smells or that can spread among gym members
• When approaching equipment, check to see if it is clean
• If you encounter a bench or other piece of equipment with wet residue from a chemical cleaning solution, allow it to dry on its own. This residue indicates that the time it takes to kill all the bacteria is not complete
• After completing your exercise, take a wipe or solution sprayed on a napkin and wipe where your skin made contact with the equipment or where sweat dripped. Avoid directly spraying chemical solutions onto equipment, as excess moisture can cause damage
• If you choose to shower after a workout, McNeal always

recommends wearing flip flops or other footwear that prevent contact between your feet and the floor, as these environments tend to be breeding grounds for mold, fungi and bacteria that can infect your feet
“Expect a clean gym and report concerns to management if
you have any,” McNeal said in a Baylor news release. “You should feel free to ask management about the cleaning schedule and always clean up after yourself. Leave equipment as you would want to find it when you walk up to it."


By Anne Palumbo
Years
Choose bright yellow squash that feels heavy for its size and has no soft spots. Store cooked spaghetti squash in an airtight container in the fridge for up to 5-7 days. Before storing, allow the squash to cool completely.

in numerous ways. With proper hydration, your heart can pump blood more efficiently, which reduces strain on your heart. Consuming enough water further reduces heart stress by helping to reduce sodium levels in your blood.

ago, spaghetti squash and I got off to a rocky start.
It refused to yield to my knife; I got frustrated; it retaliated by turning mushy; I huffed, “Never again!”
Stubborn me.
I now adore spaghetti squash and regret not giving it another chance sooner. But now that I know the ropes, I always look forward to its late-summer arrival, above and beyond how easy it is to cook.
Called “spaghetti squash” because it produces angel-hair strands of squash that mimic the appearance of noodles, this squash is a nutrient-dense food, meaning it’s low in calories but a decent source of a wide variety of nutrients.
I’m a fiend about fiber, and spaghetti squash helps meet my 25-grams-a-day fiber goal.
Besides keeping the digestive system in good working order, fiber is a major player in so many of our body’s systems that, according to a study in the Journals of Gerontology, getting enough can actually help us live longer and stay healthier. Fiber works its anti-aging magic by cutting cholesterol, reducing inflammation, protecting against diabetes and controlling weight.
Water—one of spaghetti squash’s most abundant nutrients—also contributes to good health and longevity
A recent National Institutes of Health study found that people with higher levels of serum sodium, which can be caused by not getting enough fluids, have a higher risk of dying earlier and may experience biological aging that’s greater than their biological age.
On the vitamin front, spaghetti squash is a good source of several B vitamins, the vitamin group that many experts, like Harvard’s nutritional psychiatrist Uma Naidoo, prioritize most to keep everything in top working order, especially the brain. B vitamins can help slow the aging process by reducing the risk of heart disease, creating new blood cells, and protecting our DNA from free-radical damage.
What’s more, B vitamins can lower levels of homocysteine, an amino acid that, when high, has been linked to dementia, Alzheimer’s disease, and cognitive decline.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Excellus BlueCross BlueShield members with stage 4 or 5 chronic kidney disease (CKD) may be eligible for a new program, REACH Kidney Care, which helps improve care and quality of life while delaying the need for more costly interventions such as dialysis. The National Institutes of Health estimates that 1 in 7 adults has a form of CKD. That’s about 37 million
Americans. People are diagnosed with CKD when their kidneys are damaged and unable to perform their normal function of filtering blood.
About 808,000 Americans are currently living with end-stage kidney disease often requiring dialysis. On average, the cost of dialysis is $15,000 per patient per month.
“When you think about chronic kidney disease, it affects so many
1 spaghetti squash
1 - 2 tablespoons olive oil
1 small onion, thinly sliced
1 teaspoon dried rosemary or thyme
Salt and coarse black pepper
3 cups chopped kale or spinach leaves
1. Preheat the oven to 400°F and line a large baking sheet with parchment paper for easy cleanup.
2. Slice the spaghetti squash in half lengthwise (see tip below), scoop out seeds and discard. Brush the insides of each half with some olive oil, lightly sprinkle with salt and pepper, then place halves cut-side down on the prepared baking sheet.
3. Bake for 30 to 40 minutes, until the cut sides are golden and the interiors are fork tender, but still a little firm. (Strands turn mushy if cooked too long.)
4. Remove squash from the oven and flip to cut-side up. When cool to touch, use a fork to scrape and fluff the insides into delicate strands. Set aside.
5. In a large skillet, heat 1 tablespoon olive oil over medium heat, then add the thinly sliced onion, rosemary, a few pinches of salt and coarse black pepper.
1/4 cup fresh lemon juice
1/2 can beans of choice, rinsed and drained (I used cannellini)
1 cup cherry tomatoes, halved
1 garlic clove, minced
1/3 cup grated Parmesan cheese
1/4 cup toasted pumpkin seeds (or preferred nuts)
6. Once the onion starts to soften, add the kale, lemon juice, beans, cherry tomatoes and garlic and cook for a few minutes until the kale starts to wilt. (Add some water if mixture appears too dry.)
7. Once the kale is partially wilted, add the squash strands (all or most), ¼ cup Parmesan cheese, and more salt and pepper, to taste. Toss to incorporate, using a large fork to facilitate mixing. Remove from heat and top with the toasted pumpkin seeds and remaining grated cheese.
Tip: To soften skin for slicing, first pierce the squash all over with a fork. Next, score the squash down the middle on each side, lengthwise. Make several slits along the score line with a paring knife. Microwave for 4-5 minutes, rotating squash at 2-minute mark. Before cutting, slice ends off squash and stand upright for lengthwise halving.
people,” said physician Kathleen Robischon, vice president of medical affairs and clinical services at Excellus BlueCross BlueShield. “At Excellus BCBS, we provide care management for members with chronic kidney disease stages 1 through 3,” adds Robischon. “When a member moves into stage 4, we offer the support of REACH Kidney Care.”REACH Kidney Care is a kidney health management program designed to help members with stage 4-5 chronic kidney disease navigate services and follow their physician’s treatment plan. Members work one-on-one with a multi-disciplinary care team
that provides personalized support to help members make the most of their care and manage their CKD. The REACH program is offered virtually, over the phone and in-person at no cost to members that have this benefit included in their plan.
“We are pleased that our eligible patients have the opportunity for additional support and resources,” explains physician Philip T. Ondocin, affiliated with Nephrology Associates of Syracuse, PC. “We encourage all patients to maximize their insurance benefits to support their kidney function and slow down the progression of their disease.”
By Deborah Jeanne Sergeant
Roger Hare of Marcellus thought he was in pretty good shape when he was 44.
He had played sports in college and had remained active. His cholesterol was low and his diet was pretty good.
But he had a few strikes against him — he was a heavy smoker, his stress was through the roof and his genetics were against him.
Just before turning 45, he experienced his first heart attack.
Afterwards, he quit smoking and began exercising more and made a few changes in his business to lower his stress level.
“I was forced well before my time to face my mortality,” Hare said. “I tried to make some conscious decisions about how I wanted to live my life, finding a balance between normal attributes of life and improving my heart health.”
Ten years later, however, he had a second heart attack, a severe one, which caused him to reevaluate his health regimen, including his diet.
Hare began eating organically and decided to eat red meat for occasionally.
He realized that self-employment was much better for his health since it lowered his stress.
Hare began practicing yoga
and keeping more physically active. When he was very young a friend’s father had a heart attack and Hare recalls that he never went outside again.
“It’s always been a balance between my awareness of my health and genetics and history and trying to balance that with living a meaningful life,” he said. “The most difficult thing for me is avoiding denial because it’s very easy for me to sit around and say, ‘It’s not a good time.’ Be aware of what your body is telling you and seek help, which I did not do until the second time.”
Heeding wise counsel is also vital to good health after a heart attack (or, in his case, a second heart attack). Hare sees physician Russell Silverman at St. Joseph’s Health four times a year.
“I’ve become a much better person at listening to my doctor,” Hare said. “I’ve maintained an active relationship with him. He monitors the meds I’m on. It’s important to have an open, honest relationship with your cardiologist.”
Hare also credits his support network, including family and the other people he met at his monthly cardio rehabilitation meetings, which he attended after his second heart attack. The group discussed what they were

Hare of
had
later, he had a second one. “I’ve become a much better person at listening to my doctor,” Hare says. “I’ve maintained an active relationship with him. He monitors the meds I’m on. It’s important to have an open, honest relationship with your cardiologist.”
going through beyond the medical aspects of their heart attacks.
“It was good to share those feelings,” Hare said. “It seems like if you haven’t experienced this, it is difficult to understand the emotional perspective. It was important to look for that support and not wait for it to come to you.
“It’s a very difficult situation to go through when you’re forced to face your mortality and try to deal with it and reach a balance in your life and personal relationship.”
Now 78, he “feels great” for the first time in 20 years and plans to stick around for years to come.
By Deborah Jeanne Sergeant
Your probably know that stress is bad for heart health. But both acute stress — the shock of catastrophe — and chronic stress, like the daily grind of a terrible job and domestic strife — are both bad for your heart.
Generalized anxiety disorder and stress in general are increasing among the population and this is increasing the number of cases of heart attack. That kind of stress can gradually creeps into people’s lives keeping them in a perpetual fight-orflight mode.
“Stress is a leading factor for heart disease right along with unhealthy diet, physical inactivity, smoking, excessive alcohol use and obesity,” said Lynne Shapiro, American Heart Association board president in Syracuse and chief nursing officer at Crouse Health. “Stress can increase inflammation in the body and this is linked to factors that can harm your heart such as high blood pressure. Stress can also affect your ability to sleep well, make poor food choices and less motivation to exercise.”
Chronic exposure to stress hor-
mones also raises inflammation in the body.”
Physician Andrew Mathias, affiliated with University of Rochester Medical Center, said that inflammation plays a role in heart disease in causing plaque build-up in the heart arteries. During a heart attack, plaque ruptures and blood doesn’t flow to the heart.
Stressed patients are also more likely to engage in behaviors deleterious to good health, such as smoking, poor diet and low activity level. All of these contribute to heart problems.
“Recognize that stress can have harmful consequences,” Shapiro said.
“Talk with your health care provider; they can share helpful recommendations, resources and tools to help people better manage your stress.”
One way to manage stress is practicing mindfulness.
Allison Graff, owner of A. Graff Mindful Health Coach in Camillus, is a mindfulness coach.
She describes mindfulness as “being present wherever your feet are; your mind is there too. It’s a state of being, a practice, whatever you find that helps you be in the here-


and-now.”
She said that meditation is one example of mindfulness, and that mindfulness is also part of yoga. But people don’t have to take classes to be mindful. It’s more about remaining completely in that moment without thinking of the past or future and becoming absorbed into the sensory input of that moment.
“Anxiety is typically produced when we ‘future tell’ and think about it,” Shapiro said. “Depression is commonly the replaying of things that have past.”
Reducing stress can mean walking away from difficult people and situations. Is a relationship, friendship or job that’s constantly embroiled in stress really worth it?
If eliminating the source of chronic stress isn’t possible, miti-
gating its effects can help reduce the negative impact of the stress. Take time to engage in a pleasurable activity each day. Journaling, keeping a gratitude list, prayer, mindfulness and meditation can all help lower chronic stress levels. Going on more frequent vacations such as quarterly long weekends instead of one week altogether may help manage stress better.
Stay better organized to reduce daily stressors. Streamlining things with fewer daily choices, tasks and options can simplify life and lower stress. Letting go of unrealistic expectations, such as controlling other people’s responses and choices, can also reduce stress. Learn to delegate, lower standards and accept one’s limitations.

















SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126
315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069
315-598-4700
SPRINGBROOK APARTMENTS
4920 N. Jefferson St.



After equipment is returned, it’s cleaned and sanitized before going back onto the floor, Jennings said. Most of the items loaned out have been donated, but the nonprofit does periodically purchase replacement mattresses.
walkers, canes, crutches, commodes and other
The nonprofit loaned out its first piece of equipment in 1928, Kisselstein said. It was a wooden wheelchair that now resides as a permanent fixture in the front right corner of the building.
Now, nearly 100 years later, the program continues serving the community.
and out,” said Bonnie Kisselstein,
She said between 30 and 40 people come to the loan closet weekly, a mix of those returning, borrowing and making donations. The closet is open from 10 a.m. to 2 p.m., Monday through Friday or by appointment.
The operation is run by volunteers and there are a limited number of items available, Kisselstein said.
“Call ahead if you think you’re going to need something and be sure
For example, during graduation season and the span of the New York State Fair, wheelchairs are especially in demand, she said. There is no age
Knee walkers have been sought after lately, said Ellen Jennings, the
“This is our most popular piece right now,” Jennings said, as she grabbed one and set it aside for someone who called minutes prior.
On that recent weekday morning, Jennings helped Luke pick out an adjustable black cane with padded handles to help him get around before his surgery. She only had two questions for him after they found the perfect fit: was he a resident of the school district and did he need anything else?
“You don’t repair knees, do you?” Luke asked with a chuckle. She took down the inventory number on the side of the cane, Luke’s phone number and wished him well.
“I’ll bring it back after I get my knee repaired,” he said. “Thank you.”
At a Glance
• What: Medical supply loan closet run by the Female Charitable Society of Baldwinsville.
• Where: 10 River St., Baldwinsville. The closet is open from 10 a.m. to 2 p.m., Monday through Friday. Appointments are also available.
• Who: There is no age requirement. Anyone who resides in the Baldwinsville Central School District is eligible to borrow the free medical equipment from the nonprofit.
• Contact: 315-638-6277.

By Melissa Stefanec MelissaStefanec@yahoo.com
s a parent, I see a lot of things normalized that I wish weren’t.
Things like violence, hypersexualization, gender norms, disrespect, bullying and sexism are so prevalent in our society, that it’s sometimes hard to find them remarkable.
But instead of writing a column about things I want to denormalize, I’m going to keep things positive and write about things that I wish were normal.
Normalize is a word with many meanings. It’s a mathematical operation. It’s a verb meaning to return things to their previous typical state. The type of normalize I’m talking about is a little different. I want to make things that aren’t currently normal into widely accepted and lauded practices.
The following is a list of actions I wish were a standard part of our societal fabric. These are things I wish were almost universally agreed upon by all parents, no matter their creed or lot in life. These are things I think would make for healthier children, healthier parents and a healthier community.
• Normalize saying, “I’m sorry” to children
When we don’t apologize to children, we teach them dangerous lessons. We’re teaching them adults can’t be wrong and to blindly obey adults. We’re also teaching them that one day, when they are old enough, they will outgrow apologizing. We’re teaching them they aren’t worthy of amends and don’t deserve to have their feelings validated.
• Normalize never using physical force to punish or correct
When we hit, push, grab, shove, kick or punch our children, we are teaching them that adults are allowed to solve problems with their hands. We are teaching them it’s OK to lose control when you’re an adult. We are teaching them they deserve to be physically injured when they do something wrong. We are teaching them that belittling, embarrassment and pain will make things right.
• Normalize never talking about physical attributes
We need to stop talking about people’s weight, age, race, hair styles, visible abilities, ears, height and anything else that you can decipher about a person in a matter of seconds. What people are born with or how they choose to style themselves is really none of our business. Unless someone is literally threatening someone with their bodies or attire, we need to leave them alone. We need to teach our kids to look past the things they can learn in one second.
• Normalize being wrong
We need to raise our kids in a world where it’s OK to be wrong and to fail. Each of us will be wrong and fail every day of our lives. If we don’t teach children to process failure and being wrong, they will grow into adults who don’t apologize. They will turn into people who are afraid to take chances.
• Normalize healthy sexual relationships
We should start normalizing sexual relationships where all parties are making safe and loving decisions. There is so much out there that portrays sex in unhealthy and unrealistic


ways. We need to talk to our kids about sex and sexual health. We need to talk to them about what healthy sexual relationships look like.
• Normalize talking about mental health
We need to talk about mental health the same way we talk about physical health. No one is embarrassed to talk about their ailing knee or asthma. What if we could be as free with talking about mental health issues?
• Normalize believing your children
Children may have wild imaginations and have juvenile ways of communicating, but they are experts on their own experiences. When children tell something about their feelings, bodies or perspectives, we should believe them. All too often, us adults dismiss their pain or experiences. When they tell us something about themselves, we should do our best to believe them.
• Normalize complex and conflicting emotions
Many kids and adults want to see the world in black and white. It seems easier that way, but we need to normalize complexities being part of life. It’s OK to be nervous and excited about something. It’s alright to be angry at someone and respect and love them. We need to embrace cognitive dissonance for ourselves and instill it
in our kiddos.
• Normalize embracing negative emotions
We need to normalize emotions like frustration, fear, anger, despair, sadness and disappointment. These emotions are a natural part of life. All too often, we tell kids to just get over it. When we do that, we teach them to choke back and disregard their emotions. What we should be doing is coaching them on processing and working through difficult emotions.
• Normalize harmless things that others enjoy
People are wonderfully and beautifully weird. We should normalize celebrating harmless things that give other people joy. We often dismiss or put down other people’s interests. What if we collectively agreed to celebrate other’s joy, even if it stems from different places than our own?
• Normalize being bored
Boredom plants the seeds of wonder and creativity. We should normalize and embrace our kids being bored sometimes. They don’t need to be entertained all of the time. We don’t need to schedule every minute of their days. Kids need free time to invent, meander and grow. We need to teach them that boredom is nothing to fear.


By Mary Beth Roach
Stephanie Brown, 39, was diagnosed with breast cancer earlier this year. One month later, she was receiving chemotherapy and even though she said that her cancer was completely responsive to the chemo, she opted for a double mastectomy, fearful that there might be a recurrence.
Throughout her journey, Brown credits the team from the Breast Care Partners with being strong advocates for her, helping set up appointments and even calling her late on a Friday afternoon to give her pathology results so she didn’t have to worry over a weekend.
Brown is one of more than 200 patients that the Breast Care Partners has helped this year alone — steering them through their breast cancer treatments during a time that can be marked by fear, stress and physical issues for the patients.
As of early June, the organization had seen 270 patients, according to Karen Callahan, executive director.
Breast Care Partners is a collabo ration begun by the Hematology and Oncology Associates in Syracuse in 2004, along with St. Joseph’s Health Hospital and Crouse Hospital, to provide more organized care for patients that involves medical profes
sionals across a variety of specialties, said Callahan. Making it unique, she said, is that the program has not only the HOA medical and radiation oncologists collaborating but also includes the partnership of two local hospitals.
The team of professionals includes a medical oncologist at HOA that specializes in breast cancer; an HOA radiation oncologist; pathologists from both hospitals; HOA nurse practitioners and physicians’ assistants.
As Callahan explained, nurse navigators and an executive assistant guide the patients through their treatment, making sure that all appropriate appointments are scheduled; determining if patients have any barriers to receiving treatment;

GUIDE AD: 9.75” W X 6.69” H
We’re in your corner in the fight against breast cancer.
“Being able to take away a breast cancer patient’s financial stress is huge.”
As someone who deals directly with breast cancer patients – and as a cancer survivor herself – AnnMarie Gianno, from CancerConnects, has seen first-hand the positive impact Saint Agatha Foundation’s support has on CNY breast cancer patients. By helping with unmet financial needs – like transportation costs, co-pays, specialized garments, and much more – the CancerConnects/ Saint Agatha Foundation partnership helps alleviate financial strains for those already fighting a breast cancer diagnosis. If your medical or non-medical organization would like to provide financial support to CNY breast cancer patients, too – visit s saintagathafoundation org/ for-providers to learn more and watch an interview with AnnMarie. New provider partners are always welcome!

saintagathafoundation.org

AnnMarie Gianno Patient Program Coordinator, CancerConnects




Madelen Barkins provides care for both of her in-laws, who were diagnosed with Alzheimer’s five years ago
By Deborah Jeanne Sergeant
Family and community supports have enabled Madelen Barkins to care for her father-in-law and mother-in-law who were diagnosed with Alzheimer’s five years ago.
She started seeking help at Upstate University Hospital’s department of geriatrics where Kathy Royal, a community liaison, helped her learn about available resources.
Sharon Brangman, director of the Upstate Center of Excellence for Alzheimer’s Disease, also helped answer Barkins’ questions.
As to who would care for her inlaws, Barkins held no doubts.
“Once it does happen to a family member in the African American community, we tend to take care of them at home,” she said.
She attended geriatric workshops to learn more about caregiving and became involved with Alter, an organization based in Atlanta that reaches African Americans about caregiving for people with Alzheimer’s. The program works through churches, which spurred Barkins to have her pastor, Steven Williams of Four Square Gospel Church of God in Christ in Syracuse, to work toward becoming a dementia-friend-
ly church. One of those efforts is the God’s Abundant Love Abides program that helps people caring for someone with a brain disease to feel welcomed with their loved one.
“I have found so many people; it’s such a hard caregiving,” Barkins said.
She has learned that relying solely on herself leads to burnout. Within a year of caregiving, she realized that others’ help can make her caregiving role more sustainable.
Now, she delegates some of the responsibilities to other family members in the area, as one manages the couple’s finances, another helps ferry them to doctor’s appointments, another picks up groceries and supplies and another gets them ready for church. Barkins is also no longer the only caregiver.
“We’re fighting for as long as we can to care for our parents,” Barkins said. “They will be at home.”
Barkins encourages other caregivers to take their loved ones to places and events they enjoy. For her in-laws, that’s church, among other things. Since they were involved with the church for more than 50 years, it’s a second home to them.
love and love is bigger than Alzheimer’s. If we see people who are burned out, we help.
“There’s a lot of poverty. If you’re on the south side of Syracuse and there’s a single mom with two kids and a grandma with Alzheimer’s, there’s stress. You may not be able to care for the mom, so you feel guilty. They want to keep grandma home as long as possible. You want her home, around family.”
Mary M. Koenig, administrator of Loretto Heritage Memory Life Community, said that because caring for someone with Alzheimer’s or dementia is an isolating experience, establishing a care team and delegating — just as the Barkins family has done — will help with reducing stress.
“If friends reach out and say ‘What can I do to help?’ maybe they could stay with mom for an hour so you can go to the grocery store or go play pickleball,” Koenig said. “Take people up on what they’re offering to do to help.”
“What I learned the most is you have to meet people where they’re at,” Barkins said. “Learning this, my in-laws aren’t the same as they were personality-wise but they’re still there. If they’re having a good day, we’re there for them. If they’re having a bad day, we’re there for them.”
She continues to tap into spiritual resources, relying on her faith to see her through.
“God is bigger than Alzheimer’s,” Barkins said. “Within the church community, we see God is
In addition, caring for yourself is essential. Koenig said that people caring for someone with Alzheimer’s are at greater risk for anxiety, depression and overall poor quality of life. Instead of forgoing hobbies and relationships, they should “carve out time each day to do something they like, like reading a book, meditating, going to the gym,” Koenig said. “Don’t lose yourself in caregiving. Oftentimes, caregivers succumb to physical illnesses while caring for someone with dementia. It’s all-encompassing and exhausting.”
Getting enough rest, eating well, exercising and taking time off are all part of self-care.
If you’ve met one person who cares for a family member with Alzheimer’s or another form of dementia, you’ve met only one person who’s a caregiver.
Most caregivers are retirement age. Some care for people with early onset dementia and are younger themselves, such as a 30-year-old caring for a 55-yearold parent with dementia.
Early onset dementia occurs in people younger than 65, accounting for about 5% to 6% of those with dementia.
A younger adult childcaring for someone with dementia may still work and have young children at home, bringing a whole different set of challenges to the caregiver role.
Learning about Alzheimer’s can help make caregiving easier.
That’s a strategy recommended by physician Sharon Brangman, faculty at SUNY Upstate Medical University, distinguished service professor, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease.
“Be educated to understand
this complex disease and all its nuances,” Brangman said. “Realize there’s a mix of emotions that come into play when you care for someone, like guilt, sorrow and anger and happiness. Some say they feel privileged to provide this care but it’s exhausting. Find all the resources in your community that can support you and enlist home health aides and family members to give you regular breaks. It’s the toughest type of care to give.”
It is vital for providers to connect caregivers to community resources and to help in developing strategies to manage the challenges in this role. Many social organizations such as community groups and churches provide both formal and informal assistance such as senior day programming, congregant meals, transportation and senior sitting and respite care, which can support family caregivers, depending upon their needs.
These resources can also save money compared with the costs of paid assistance.
By Deborah Jeanne Sergeant
Many people don’t know much about Alzheimer’s disease, a form of dementia. Here are the myths and facts of the disease.
Physician Sharon Brangman, faculty at SUNY Upstate Medical University, distinguished service professor, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease:
Myth: Forgetfulness means you have Alzheimer’s.
Fact: “There are characteristics of normal aging that are not like Alzheimer’s. With aging, we have slow retrieval. It’s like a big hard drive where you have lots of things on it. Those are examples of slow retrieval where you can’t pull up the information right away. It’s part of the normal aging process. You can retrace your steps and find them. Someone with dementia can’t retrace their steps and their keys will be in a not very normal place, like in the freezer. Most of us are on overload where there’s too much information coming into our brains. You’re putting down your keys but thinking of 10 different things. Our brains were meant to do one thing at a time. We put our brains on overload by trying to multitask. It’s not good for our brains.”
Myth: My parent had Alzheimer’s, so I’m going to get it.
Fact: “If there’s a certain genetic trait that runs in families, that’s a possibility but it’s rare. It usually happens in families who have early onset where they get it in their 50s or earlier. This disease is very complex and we don’t know all the factors that can trigger Alzheimer’s. It seems as if there are other components that can turn this on, like lifestyle. There is increasing research about air pollution and how it affects cognition. Those who regularly consume highly processed foods and those who smoke have higher risk. In addition, those who have very low amount of exercise in their lifestyle or those who don’t get enough sleep are at higher risk. Especially in the deep phases of sleep, our brains clean up bad chemical reactions in our brain. People who drink alcohol on the regular increase their risk. There are things in our lifestyle and environment that may play a bigger role as to whether we’ll get Alzheimer’s than our genes.”
From Mary M. Koenig, administrator of Loretto Heritage Memory Life Community:
Myth: Once you get diagnosed, it’s ‘over’ for you.
Hematology-Oncology Associates of CNY (HOA) has successfully treated a patient with bispecific antibody therapy for small-cell lung cancer as an outpatient. Reports show that while this therapy has been successfully administered in the outpatient setting in other parts of the United States, this is the first time it has been provided for someone outside of the hospital in New York State.
Bispecific antibody therapy is a powerful treatment option for patients with liquid and solid tumors that uses the body’s own immune system to fight the disease by binding to two different cells – the disease cells and T-cells (a type of white blood cell that protects the body from infection and fights cancer). Studies show that depending on the bispecific agent, up to 60% of patients receiving therapy have a positive response whereby disease progression is slowed or stopped, thus improving their quality of life and extending their life expectancy.
Prior to HOA’s program, the risk of complications from bispecific therapy’s initial dosing period required
Fact: “There’s a lot of people who live very full lives with a dementia diagnosis. All of these treatments they’re working on will focus on early detection. That’s where the treatments are most effective. A lot of people are afraid to even get into clinical trials to see if it’s likely they’re get dementia. But a diagnosis doesn’t mean your life is over. There are lifestyle changes you can make.”
Myth: If you have Alzheimer’s, you didn’t take good care of yourself.
Fact: “There are a lot of studies out that talk about things you can do to improve your brain health like eating right. If it’s good for the heart, it’s good for the brain. Making social connections. There’s no doubt that can have an effect. But by saying if you make certain choices you can avoid dementia, is unfair. It’s a dangerous myth.
Myth: Once you have a diagnosis of Alzheimer’s, you have to live in a nursing home.
Fact: “I’m constantly amazed at the number of people who come here and they have gotten to this point and haven’t tried any of the other resources available. They don’t have a support group, use adult daycare or have brought anyone into their home. Thirty years ago, there weren’t many options available. You stayed at home unsafely or you went to a nursing home and many people didn’t need that level. Assisted living and memory care aren’t the answer for everyone. People like to be cared for at home and with support that is an option available.”
From Desta Anthony, nurse practitioner certified in adult health and palliative and hospice care, specializing in dementia care at Loretto Heritage and The Nottingham, and in the community in private practice:
Myth: You should not tell a person their diagnosis if they have Alzheimer’s disease.
Facts: “This myth can prevent patients and families from getting the information they need to understand the disease or help those affected. Just as a patient has the right to be told that they have cancer, patients should be told that they have Alzheimer’s disease so they can take part in making decisions for themselves early in the disease, plan appropriately for the future, and have the opportunity to take part in research or build a care team that will support their quality of life. Sometimes fear of the unknown — not having a diagnosis — is worse than the known.”
Myth: Later in Alzheimer’s disease, there is no point in visiting loved ones because they will not recognize you.
Facts: “The relationship you have with your family member will change and sometimes in later stages, but not always, patients may forget a name or mix up relatives. The individual’s need for love and affection does not go away, and you need to balance that with your need to be recognized. Patients find joy and comfort with the time you take to share a moment and engage with them where they are.”
a patient be admitted to the hospital for administration of the medication and monitoring of reactions which many times do not occur. The hospital stay for bispecific therapy can range from a day or two on multiple occasions up to as long as 14 days.
“Our program includes a very sophisticated outpatient monitoring plan that allows our patients the freedom to stay at home, avoiding potential infection risks, costs associated with a hospital stay, and time away from family,” explains medical oncologist Steven Duffy, M.D., physician champion for the Bispecific Therapy Program and HOA’s director of research. “Improving our patients’ quality of life during treatment for cancer and hematologic conditions is the impetus for this new program. We want to embrace these exciting new therapies so that people can get the best treatments close to home.”
Patients in the program are required to have an at-home caregiv-
er and live within a one-hour drive to HOA’s East Syracuse office and Crouse Hospital. Additionally, each patient and their caregiver receives extensive education before agreeing to participate in the program. That education includes understanding how to use an electronic blood pressure monitor, pulse oximeter and thermometer, which are all sent home with the patient.
During a patient’s initial dosing period - the time period during which the patient is at the greatest risk for adverse events — HOA’s bispecific therapy team closely monitors the patient with help from the at-home caregiver who checks the patient’s blood pressure, pulse and temperature every four hours while awake. HOA clinical staff call the patient’s caregiver every eight hours during the initial dosing phase to receive report of the vitals and discern if there are any abnormal reactions to the medication.
Reactions are classified into three grades.
• Grade 1 reactions can be managed at home with an oral steroid and Tylenol and continued monitoring.
• Grade 2 reactions — no matter the time of day — require the patient to be driven to the HOA office where they will be met by a physician, an advanced care provider and other clinical staff who will administer a rescue medication and fluids.
• If a patient has a grade 3 reaction or worse — which happens
in less than 3% of all cases — they must be driven to the Crouse Hospital’s emergency department and will be admitted to the intensive care Unit. Crouse staff have received special training for this occurrence and are ready to respond as necessary. Additionally, each patient carries a special card identifying they are being treated with bispecific therapy and must be treated at Crouse.
“It’s important to note that HOA has been treating patients with bispecific therapy in a maintenance mode for several years,” says Duffy. “It’s just the initial, or ramp-up, dosing process that is new for us, but easily accommodated by our highly trained staff who are extensively familiar with monitoring reactions from chemotherapy and immunotherapy.”
“Providing bispecific therapy at HOA is what community oncology is all about — making cutting-edge treatments available to all, not only to those with access to large centers. Treating our patients at HOA allows them to go home at the end of the day to the comfort of their own home,” explains HOA’s CEO Maryann Roefaro. “Prior to this new program patients were asked to travel outside of Central New York and spend time away from their loved ones in a hospital setting.”
HOA also intends to add clinical trials using bispecific antibodies in the outpatient setting to their already established clinical trial program.
By Jim Miller

Dear Savvy Senior,
I recently received an email that I needed to update my online Social Security account. Is this legit or is it a scam?
Suspicious Susan
Dear Susan,
The Social Security Administration did indeed send out a legitimate email in July to notify recipients that they are making changes to the way you access Social Security’s online services, including your personal “my Social Security” account.
The changes will simplify your sign-in experience and align with federal authentication standards, while at the same time provide you safe and secure access to your account and other online services.
If you created an online My Social Security account before Sept. 18, 2021, you’ll need to shift to a Login. gov account to be able to continue to access your account.
Online My Social Security accounts enable both beneficiaries and people who are not yet receiving benefits to access services, including requesting Social Security card replacements, estimating future benefits, checking on the status of benefit applications and managing current benefits.
The online services aim to save time for both current and future beneficiaries, as well as the Social Security Administration, as the agency grapples with long wait times for its national 800 phone number. The average speed to answer those calls was about 36 minutes in the second quarter, according to the SSA. The agency is working to bring that average wait time down to 12 minutes by the end of September 2025.
If you already have a My Social Security account, go to ssa.gov/ myaccount and sign in with your Social Security username. You’ll then


be guided through the process of creating a new account with Login. gov. Once you successfully link your personal My Social Security account with your new Login.gov account, you’ll get a confirmation screen and have immediate access to online services. In the future, you’ll sign into your account with Login.gov and not your Social Security username.
If you already have either a Login.gov or ID.me account, you do not have to take any action.
To be sure you’re taking the appropriate steps to update your account, it is important to verify any websites or links leading you to the Social Security website. Legitimate Social Security Administration website link is www.ssa.gov and the agency link to my Social Security account is www.ssa.gov/myaccount.
It’s very important to be mindful of potential scam artists who may send you fraudulent websites pretending to direct you to Social Security.
These sites will closely mimic the format of the agency’s links to try to lure you into entering your personal information.
If you see a suspicious email or link, it is best not to respond or click on it. Instead, you can report it to the website of the SSA’s Office of the Inspector General or call the fraud hotline at 800-269-0271.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

Walk-ins welcome
Baldwinsville, Camillus, Cazenovia, Cicero, East Syracuse, Fayetteville, Liverpool, Pulaski, Syracuse and now open in Watertown
Open Monday through Friday and four centers open Saturdays Prompt, courteous and no appointment needed. Hours and directions at laboratoryalliance.com


By Warren Beck Social Security District Manager in Syracuse.


Social Security works with the Office of the Inspector General (OIG) to protect you from scams that use Social Security as bait. Section 1140 of the Social Security Act allows OIG to impose severe penalties against anyone who engages in misleading Social Security-related advertising or imposter communica-

OIG may impose a penalty
• Mails misleading solicitations that appear to be from or authorized
• Operates an imposter website or social media account designed to look like it belongs to or is autho-
• Sends emails or text messages or makes telephone calls claiming to be from Social Security.
• Sells Social Security’s free forms, applications, and publications without our written approval.
• Charges a fee for a service that Social Security provides free of charge without providing a clearly visible notice that Social Security provides the service for free.
If you receive a misleading or suspicious Social Security-related advertisement, phone call or email, you should let us know right away. Try to capture as many details as you can.



Here’s what you can do:
• For suspicious websites or social media accounts, please take a screenshot of the page. Note the website address or social media link — and how you came across it.
• For emails and text messages, capture the entire message and any links or attachments.
• For mail, retain the complete communication, including the outside envelope and all inserts.
• For telephone solicitations, note the caller identification phone number and any company name or call back number provided by the caller or recorded message. You can help us stop misleading advertising and communications. We encourage you to report possible scams to the OIG at oig.ssa.gov/ report. You can also call our fraud hotline at 1-800-269-0271 or send an email to OIG.1140@ssa.gov.
To learn more, check out our publication, "What You Need to Know About Misleading Advertising", at www.ssa.gov/pubs/EN05-10005.pdf. You can also review Section 1140 at www.ssa.gov/OP_ Home/ssact/title11/1140.htm.
Please share this information with friends and family and help us spread the word on social media.
Q.: Who can get Extra Help with Medicare prescription drug coverage?
A.: Medicare Part D prescription drug coverage is available to anyone with Medicare. Joining a Medicare prescription drug plan is voluntary, and you pay an additional monthly premium for the coverage. People with higher incomes might pay higher premiums.
If you have limited resources and income, you may be eligible for Extra Help to pay for the costs — monthly premiums, annual deductibles, and prescription co-payments — related to a Medicare prescription drug plan. To be eligible for Extra Help, you must reside in one of the 50 states or the District of Columbia. If your resources and income meet the requirements, you can save nearly $5,900 in prescription costs each year. For 2024, your resources must be limited to $17,220 (or $34,360 if you are married and living with your spouse). Resources include such things as bank accounts, stocks, and bonds. We do not count your house and car as
resources. Your annual income must be limited to $22,590 (or $30,660 if you are married and living with your spouse).
In some cases, you might be able to get assistance even with a higher income. Learn more at www.ssa. gov/medicare/part-d-extra-help.
Q.: I noticed that my date of birth in Social Security’s records is wrong. How do I get that corrected?
A.: To change the date of birth shown on our records, take the following steps:
• Complete an Application for A Social Security Card (Form SS-5).
• Show us documents proving:
– U.S. citizenship (if you have not previously established your citizenship with us).
– Age.
– Identity.
• Take (or mail) your completed application and documents to your local Social Security office.

Medical oncologist and hematol
ogist Cherie Tan has recently joined Hematology-Oncology Associates of CNY (HOA). She will work in the new Camillus Cancer Center, which is scheduled to Sept. 16. Until then she is caring for patients in the practice’s Brittonfield location.
A native of Toronto, Tan is board-certified in internal medicine and a graduate of University of Toledo College of Medicine. She completed an internal medicine residency at Robert Wood Johnson Medical School, in New Brunswick, New Jersey, and specialty training (fellowship) in hematology and oncology at University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center, where she served as chief fellow. While completing her training, Tan also worked in mixed tumor and bone marrow transplant services at the University of Maryland Medical Center.
“We’re honored that Dr. Tan chose to join HOA,” says Maryann Roefaro, HOA’s chief executive officer. “In the short time she has been with us, she has already demonstrated her complete commitment to providing patients with the best possible care for the body, mind and spirit.”
St. Joseph’s Health Hospital has received the American Heart Association’s Get With The Guidelines –

Stroke Gold Plus quality achievement award for its commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines, ultimately leading to more lives saved and reduced disability.
Stroke is the fifth cause of death and a leading cause of disability in the United States. A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts. When that happens, part of the brain cannot get the blood and oxygen it needs, so brain cells die. Early stroke detection and treatment are key to improving survival, minimizing disability and accelerating recovery times.
“St. Joseph’s Health Hospital is committed to improving patient care by adhering to the latest treatment guidelines,” said Meredith A. Price, senior vice president, acute operations at St. Joseph’s Health. “Get With The Guidelines makes it easier for our teams to put proven knowledge and guidelines to work on a daily basis, which studies show can help patients recover better. The end goal is to ensure more people in Syracuse can experience longer, healthier lives.”
“Our team is dedicated to enhancing and maintaining the highest quality of care while rigorously following the latest treatment guidelines,” said physician Fahed Saada, stroke program director and section chief of neurology at St. Joseph’s Health. “We are committed to providing evidence-based care to every patient, every time. The Get With The Guidelines program has been crucial in helping us achieve this goal.”
Additionally, St. Joseph’s Health Hospital announced that it had received re certification from DNV as a primary stroke center. The DNV Primary Stroke Center Certification
Matthew Chadderdon, who has held key leadership roles in public affairs with Auburn Community Hospital, Welch Allyn Inc., and UTC/Carrier Corp., has been named chief of staff, associate vice president for Upstate Medical University. As chief of staff, Chadderdon will play a lead role in strategizing and promoting priorities and initiatives of the office of the president and of the university. He will serve as a liaison between the office of the president and campus and external groups and play a critical role in planning and decision-making on university-based priorities.
is based on standards set forth by the Brain Attack Coalition and the American Stroke Association and affirms that the medical center addresses the full spectrum of stroke care — diag nosis, treatment, rehabilitation and education – and establishes clear metrics to evaluate outcomes.
The medical staff at Oswego Hospital recently appointed new leadership for 2024-2025.
• Physician Michael Alcasid has

Additionally, Chadderdon will oversee and manage the operational functions of the office of the president and will support government relations, community relations, marketing, and public and media relations.
“I am delighted to have Matt join the senior leadership team here at Upstate,” said Upstate President Mantosh Dewan, MD. “His experience in health care and his background in communications and in coordinating complex initiatives make him well suited to join the talented team we have at Upstate.”
Chadderdon brings to Upstate decades of leadership and accom-
rights of its members in all stages of the hospital’s credentialing process.

Hospital. In 1998 he started as a staff physician while also working as a primary care physician for Oswego County Opportunities. In 2008 he transitioned to being a hospitalist, a position he’s held ever since. Alcasid has held various leadership positions including chairman of the ICU committee from 2008-2017; QICA/QAPI chairman from 2016-2018; chief of medicine service from 2012-2016; hospitalist director from 2008-2018; and vice president of the medical staff 20162018 as well as president from 2018-2020. As the newly elected president of the medical staff, he will also serve as chairman of the medical executive committee and as a member of the Oswego Health board of directors. In this role, he is responsible for communicating and representing the opinions and concerns of the medical staff and its members on organizational and specific matters affecting hospital operations to the board. He will also oversee compliance on the part of the medical staff with the procedural safeguards and

plishment in a variety of areas, including communications, government relations, strategy development, brand management and com-
David Bass selected as vice president. Since 2020, he has provided cardiovascular care with the Center of Cardiology at Oswego Health Medical Practice. Board-certified in cardiovascular disease and internal medicine, he earned his medical degree from New York College of Osteopathic Medicine. In addition, Bass completed his fellowship in cardiovascular medicine at the Nassau University Medical Center. He has extensive cardiovascular experience throughout New York state, including being a noninvasive cardiologist at Canton Potsdam Hospital. He is a fellow of the American College of Cardiology, has diplomate status with the American Society of Nuclear Cardiology and has diplomate status with the National Board of Echocardiography. As vice president of the medical staff, Bass will chair the Oswego Health quality assurance and process improvement committee and will serve as a member of the medical executive committee.
Crouse Health Foundation’s Polo for Preemies raises $80,000
Crouse Health Foundation’s seventh annual Crouse Health Polo for Preemies, held July 28 at the Skaneateles Polo Club, was attended by over 850 guests and raised more than $80,000 to benefit the Baker Regional NICU. The “Little Fighters” in the NICU receive exceptional care from a dedicated, expert staff of neonatologists, nurses and pediatric specialists at the highest level NICU
munity relations with institutions, such as Welch Allyn, (2006-2014) where he served as vice president of marketing communications, global brand management and shareholder relations, and UTC/Carrier Corp., (1994-2001) as vice president for corporate communications and community relations, and most recently at Auburn Community Hospital, serving since 2018 as vice president for marketing communications and government relations.
At Auburn Community Hospital, Chadderdon was instrumental in securing more than $40 million in state and federal funding and developing and executing a new brand strategy for hospital and its primary care practices.
Chadderdon earned a Master of Public Administration degree from Syracuse University’s Maxwell School and a bachelor’s degree from the State University College of New York at Buffalo.

in a 14-county region.
In addition to the thrilling polo match, family activities and silent auction the afternoon was made even more special by the attendance of Coach Adrian Autry and members of the Syracuse men’s basketball team.
For more information or to inquire about the 2025 Polo for Preemies, contact Bree Amborn, breannaamborn@crouse.org or by phone at 315-470-7006 in the Crouse Health Foundation office.
The Saint Agatha Foundation has awarded the Oswego Health Foundation with a grant of $75,860 to support the purchase of the most advanced software packages that will reduce appointment and interpretation wait times for patients needing breast imaging.
Providing financial assistance to individuals in CNY who are afflicted with breast cancer, the Saint Agatha Foundation is dedicated to providing support, comfort and care to breast cancer patients through financial assistance programs. The Saint Agatha Foundation provides support, allowing patients to focus on their treatment, not their bills.
“The Saint Agatha Foundation is pleased to provide funding for software mammography upgrades, ensuring access to state-of-the-art technology for patients in Oswego County. For the past 15 years, Saint Agatha Foundation has been a provider of funds to Oswego Health, providing cancer patients with financial assistance for not only medical but personal bills to ease the burden of a breast cancer diagnosis. We are pleased to carry on the legacy that my daughter, Laurie Mezzalingua established when she founded the Saint Agatha Foundation,” said Kathleen Mezzalingua, Saint Agatha’s board chairwoman.
The Loretto Foundation will present its 2024 community awards at the foundation’s 16th Annual Hope Celebration called “Blues & Brews Festival” which will be held 6 – 9 p.m. Oct. 10 at Middle Ages Brewing Company Beer Hall, 120 Wilkinson St. in Syracuse.
Two community leaders will be recognized.
• Felisha Legette-Jack, the Syracuse University women’s basketball coach is receiving a 2024 Community Impact Award, which recognizes individuals or groups who champion the Loretto mission and have contributed to the overall well-being and vitality of the community.
• Ryan McMahon, Onondaga County executive is receiving the 2024 Loretto Distinguished Service Award, which is presented to an individual who has demonstrated exceptional commitment, leadership and impact in improving care for older adults within Loretto.










Say hello to a more convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at eight School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI OFFICE
MONDAY - FRIDAY 7:00AM - 6:00PM
Central Square (315) 675-9200 Fulton (315) 598-4790 Oswego (315) 342-0880 Pulaski (315) 298-6564 Parish (315) 625-388 Phoenix (315) 695-4700 Mexico (315) 963-4133




