With November as Lung Cancer Awareness Month, Hematology/Oncology
Associates of CNY (HOA) and CRA Medical Imaging (CRA) are offering free lung cancer screenings from 8 a.m. to 2 p.m., Saturday, Nov. 12, in three locations:
• HOA, 5008 Brittonfield Park way, East Syracuse
• HOA, 4900 Broad Road, Syra cuse (Onondaga Hill)
• Diagnostic Imaging Center, 37 W. Garden St., Auburn
Appointments are required by calling 315-472-7504, extension 1300. Walk-ins are not allowed.
Each patient will require a COVID-19 precautionary screening and must comply with safety proto cols, including wearing a mask.
According to CRA’s CEO Mary ann Drumm, “Joining with HOA to offer this free screening during Lung Cancer Awareness Month is one small way we can increase knowledge of lung-cancer treatment options and smoking cessation pro grams, to ultimately save lives.”
This free lung cancer screening is available for people at high risk for lung cancer, meaning they must meet all the following criteria:
• Are between the ages of 50 and 80
• Are currently a heavy smoker or one who has quit within the last 15 years
• Have not previously received a free lung cancer screening through this program
Anyone unsure if they meet the guidelines can take the simple, nostrings-attached quiz at hoacny.com/ lungscreening.
This annual clinic is absolutely free as a community service from HOA and CRA. However, anyone who meets the above criteria can contact HOA or CRA at any time to arrange a lung cancer screening at a time convenient for them. In most cases insurance will pay for the procedure. The procedure also can be paid out-of-pocket for approximately $175.
The only recommended screen ing test for lung cancer is low-dose computed tomography (also called a low-dose CT scan, or LDCT). During an LDCT scan, the patient lies on a table and the CT scanner uses a small amount of radiation to make detailed 3D images of their lungs. The scan only takes less than 5 minutes and is not painful. While this scan will ex pose you to a low dose of radiation,
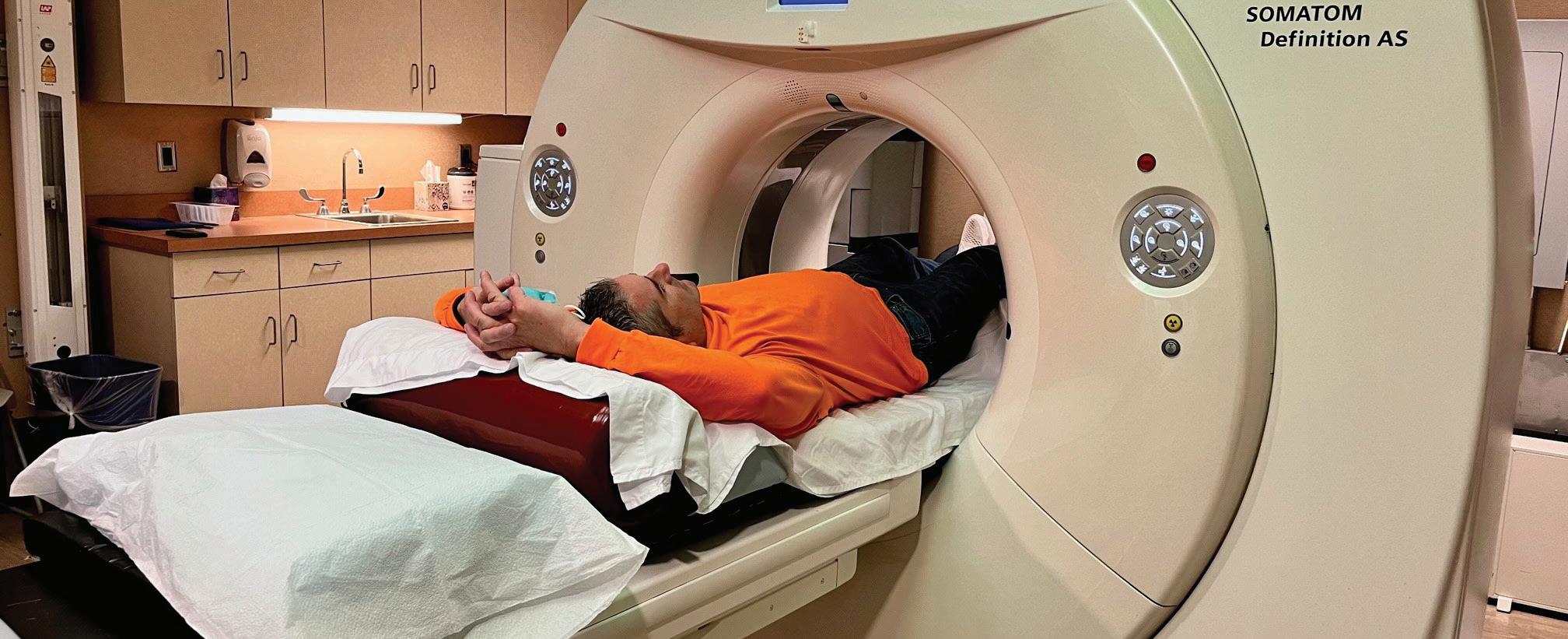
LDCT uses 75% less radiation than a traditional CT scan and shows more detail than a standard chest X-ray.
“Lung cancer screening is a regular preventive health check, like a mammogram or a colonoscopy, and most people who get screened do not have cancer” explains Ajeet Gajra, a medical oncologist from HOA “The low-dose CT checks your lungs while you are healthy and looks for any changes from year to year. With that information we can intervene with any necessary medical care as soon as possible.”
All screening patients will be en couraged to share results with their primary care physician. With permis sion, the HOACNY and CRA Imag ing staff can directly send a patient’s
results to any physician they choose.
“A lung cancer screening may find nothing or it may find some thing abnormal or suspicious. An ab normality does not always mean it’s a cancer, but that it may need closer follow up or may need additional testing,” explains Gajra.
“The value of annual lung screenings is the opportunity to find lung cancer at an early stage where we have the greatest likelihood of curing it.”
Based on results, patients are welcome, but not required, to seek follow-up care with a HOA physician and thoracic nurse navigator (TNN). The TNN supports the care of any lung disease patient from prediagno sis through all phases of treatment. She works with patients and their families to help overcome healthcare system barriers and facilitate access to quality medical and psychosocial care. The TNN can also facilitate referrals for smoking cessation pro grams at HOA.
See how Excellus BlueCross BlueShield is bringing Medicare plans with lower costs and better benefits to people throughout our community. That way, everybody benefits.

• Preventive dental +$1,000
•
to
all plans
in all regions with
and nationwide
•
A nonprofit independent licensee of the Blue Cross Blue Shield Association. Excellus BlueCross BlueShield is a PPO and/or an HMO plan with a Medicare contract. Enrollment in Excellus BlueCross BlueShield depends on contract renewal. Our Health Plan complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-877-883-9577 (TTY: 711).注 意:如果您使用繁體中文,您可以免費獲得語言援 助服務。請致電 1-877-883-9577 (TTY: 711)















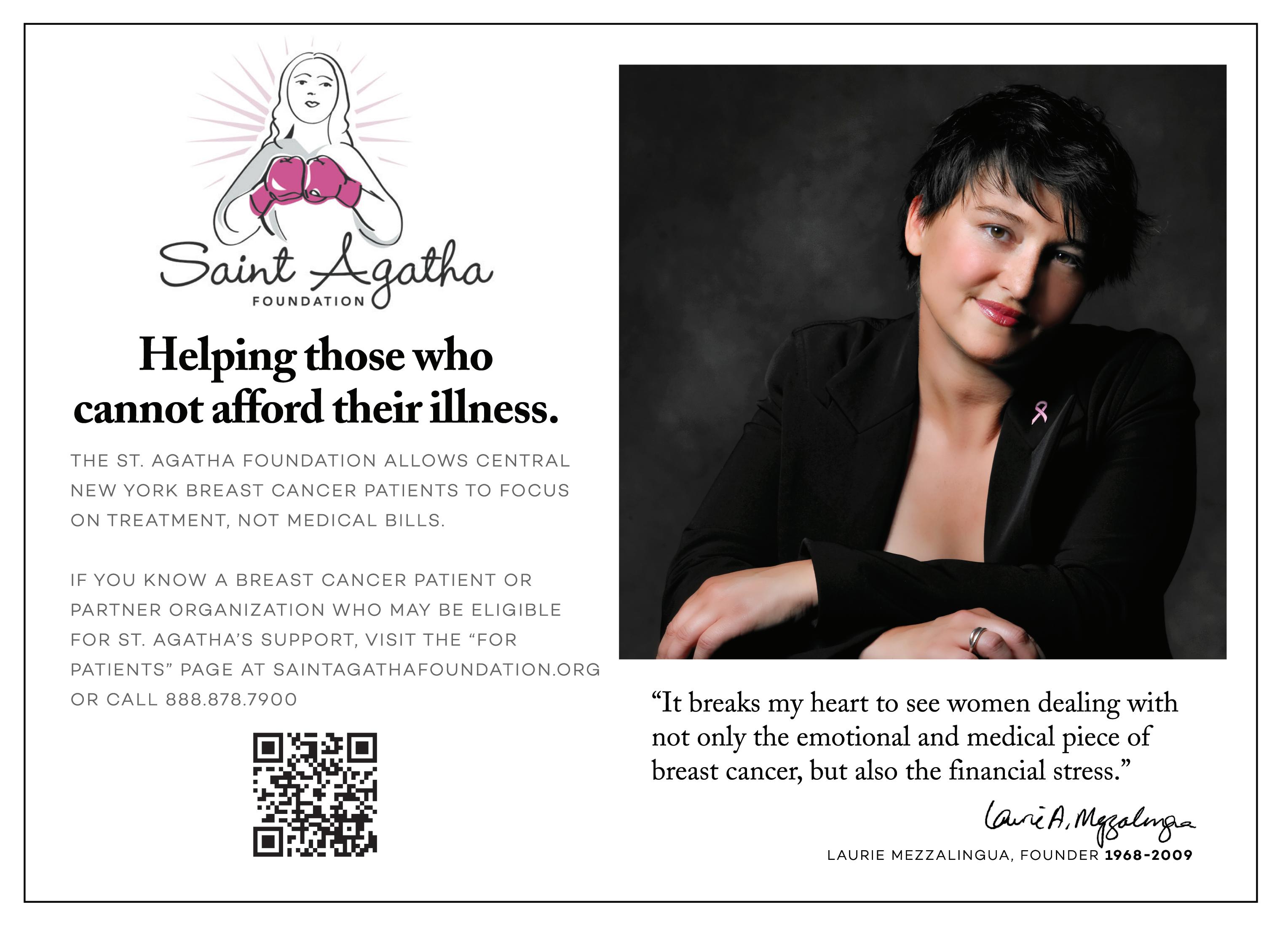
Former TV newswoman and TODAY show anchor Katie Couric has breast cancer.

Couric shared that information late September on Instagram, while also releasing an essay about the experience on her media website.
“Every two minutes, a woman is diagnosed with breast cancer in the United States,” Couric wrote on Instagram. “On June 21st, I became one of them.”
Couric, 65, received her cancer diagnosis in June, had a lumpectomy on July 14 at NewYork-Presbyterian/Weill Cornell Medical Center and then began radiation treatments on Sept. 7, TODAY.com reported.
The anchor’s name is often associated with cancer awareness because her first husband, Jay Monahan, died from colon cancer at 42, when their children were young. Couric has long been a spokeswoman for getting colonoscopies to catch cancer early.
Couric wrote about sharing her cancer news with her daughters, Ellie, now 31, and Carrie, 26.
“Finally, four days after I was diagnosed, I FaceTimed each of them,” she wrote. “I tried to be as reassuring as Dr. Newman. Their faces froze in disbelief. Then shock. Then they began to cry. ‘Don’t worry,’ I told Carrie then Ellie, ‘I’m going to be fine,’ trying to convince myself as well as them.”
“They’d already lost one parent. The idea of losing another was unfathomable,” she wrote.




Although Couric’s family has no history of breast cancer, the family has endured many cancer diagnoses and deaths. In addition to Monahan, Couric’s sister died at age 54 from pancreatic cancer. Her mother-inlaw died from ovarian cancer. Her parents also have a cancer history.
“Please get your annual mammogram,” she wrote. “I was six months late this time. I shudder to think what might have happened if I had put it off longer. But just as importantly, please find out if you need additional screening.”
Q: You’ve recently completed your fellowship at SUNY Upstate Medical Center, correct?
A: Yes, I completed it in the first quarter of this year. I did my internal medicine training at Upstate and then went on to do my fellowship there as well.
Q: What was that experience like?
A: It was a great experience. It’s the only academic center in Central New York. I had good training with great mentors throughout both my residency and fellowship.
Q: And you’re originally from the area?

A: I grew up just north of Syracuse in Cicero.
Q: Was the plan always to stay local or were you looking elsewhere in the country?
A: No, I was always planning to stay local, close to home.
Q: I don’t see the combination of D.O. and oncology that often. It’s mostly in primary care?








A: I think a lot of people are still somewhat confused about what a D.O. is. There are a few of us at Hematology Oncology Associates who are D.O.s [doctor of osteopathic medicine], so it’s not too uncommon. But there aren’t as many of us as M.D.s. Osteopathic schools are pretty much the same as M.D. schools, but the focus is a little more holistic, which may entice someone more toward a primary care path. But I think oncology can be quite a holistic specialty as well. My training
swing me away from oncology and, if anything, I think it helped the foundation of me choosing that specialty.
Q: What would you consider to be a holistic approach to oncology?
A: Basically the holistic approach is mind, body and spirit. I think that’s particularly important for someone who is facing a cancer diagnosis. It’s not just about being diagnosed with a disease and treating it. It’s all-encompassing. There’s a lot of emotional support that’s needed. All of the support services that go along with it. Nutrition is vital. Family support is important as well. So a very well-rounded approach to their care is vital.
Q: You’ve also worked as an internist.
A: I worked as a nocturnist. I always loved internal medicine, but it was always a stepping stone to oncology for me. It was a chance I had to work as internist, and something I thoroughly enjoyed.
Q: What will you be doing at your new position with HOA?

A: I just joined with HOA last month. I’ve known a lot of these providers for many years. It’s a pretty small town, so we interacted with each other a lot during fellowship. I’ve developed relationships with them over the years. I’m a general hematology oncologist so I’ll be seeing patients with a variety of blood disorders as well as cancers. I don’t have a particular sub-specialty. That may change over time, but I’m happy to see any patients in need of my specialty. I truly enjoy seeing all of the potential disease processes and keeping all that knowledge fresh.



Q: Under what conditions might a patient be referred to you?

A: You can think of hematology and oncology as two separate things. There are a lot of benign blood disorders that someone might be referred for. Say if they develop anemia or some other issue with their blood count that their primary care physician has identified. And, of course, there’s the malignant disorders you’d generally associate with cancer. So if the primary care physician ordered a screening test, for example, or they’re sent our way when a patient becomes symptomatic.
Q: How has oncology changed over the course of your training? Has anything
Jill Yeager, a medical oncologist and hematologist, has recently joined Hematology-Oncology Associates of CNY (HOA) in Syracuse. A native of Central New York, she is board-certified in internal medicine, and a graduate of Lake Erie College of Osteopathic Medicine in Erie, Pennsylvania. She completed an internal medicine residency, serving as chief resident, and specialty training (fellowship) in hematology and oncology at SUNY Upstate Medical Center. While completing her training, Yeager also worked as a hospitalist at Crouse Hospital and the VA Medical Center in Syracuse.
surprised you or changed your philosophy?
A: The time I was in training was both exciting and challenging, because it was hard to keep up. So here you are as someone who is training to learn about oncology but it changes day to day almost. So it’s a lot to keep up with, but it’s all good things and advances in the field. Definitely the advances that we’ve made in immunotherapy or molecular targeted treatment have made leaps and bounds over the last decade or so.
Q: Aside from receiving timely treatment, what are the most important factors in cancer survivability?

A: It’s a difficult question to answer because it’s very specific to the disease. We talk about cancer as though it’s a single disease, but it’s really a lot of different similar diseases. But they can be very different in how they behave. Catching them early is the most important thing. That’s why we talk about the importance of screening exams. That’s really the best way to avoid having a cancer that becomes difficult to treat.
Q: What attracted you to HOA in particular?
A: It’s been for a long time. It’s got a really solid foundation with a hardworking staff that are there day in and out taking care of patients. Even though patients are generally coming in for sad reasons, there’s so much camaraderie amongst the staff. I think that’s evident in anyone you speak to at HOA. We’re there to give the best care we can to patients. That’s something I saw before I joined and something I continue to see now that I have.
Q: Have you started seeing patients yet?



A: Yes, I have.

Name: Jill Yeager, D.O.













Position: Hematologist and medical oncologist at Hematology-Oncology Associates of CNY (HOA)









































Hometown: Cicero, New York
Education: Lake Erie College of Osteopathic Medicine






Affiliations: : Crouse Hospital; St. Joseph’s


Organizations: American Society of Clinical Oncology; American Society of Hematology, American College of Physicians

Family: Husband, two sons
Hobbies: Hiking, traveling, cooking, reading
New oncologist and hematologist at Hematology-Oncology Associates, who grew up in Cicero, discusses her training and the importance of a holistic oncology approach to treating cancer

 By George W. Chapman
By George W. Chapman

Last year, we spent $603 billion on drugs. That’s about $1,800 per person in the US. Half of the $603 billion was spent on specialty drugs alone. Soaring prices, not increased utilization, drove up the overall drug spending. Specialty drug prices have increased a staggering 43% over the last five years. To reign in drug costs, the Inflation Reduction Act caps all Medicare Part D drug price increases at the inflation rate and out-ofpocket spending for Medicare members is limited to $2,000 annually. This went

The 88 Catholic hospital system lost $1.4 billion in the fiscal year just ended June 30.

St. Joseph’s in Syracuse and St. Peter’s in Albany are local members. Two other national Catholic hospital systems, CommonSpirit and Ascension (Lourdes in Binghamton), lost almost $2 billion each. Deficits were attributable to declining revenues and significant contract labor (mostly nursing) costs. In fairness to hospitals, their fees are either predetermined by Medicare and Medicaid or predetermined with commercial insurers. So, unlike drug manufacturers, they cannot arbitrarily raise prices to increase revenues.
Large national hospital systems have not fared much better than smaller local or regional hospital systems. Industry observers have speculated that the smaller systems (comprised of “across the street mergers”) may be more efficient because their proximity allows them to share clinical staff, consolidate overhead, and merge departments.
Industry experts Kaufman and Hall don’t see things improving for hospitals through next year. If hospitals continue to lose money, they will
into effect Oct. 1, 2022. In addition, Medicare will finally be allowed to negotiate a handful of drug prices — but not until 2026. Seemingly in anticipation of prices being controlled by Medicare, drug manufacturers increased the prices of some 1,200 products an average 31.6% from July 2021 to July 2022. In the meantime, physicians are lobbying Congress not to cut their payments by almost 5% next year. With inflation at 8%, the 5% cut is tantamount to a 13% decrease in reimbursement.

be forced to make painful staff cuts, mostly in non-clinical areas, to keep their doors open.




You are eligible for Medicare the month you turn 65. Open enrollment, which began this Oct. 15, allows people to change their plan for 2023.
Medicare anticipates the trend to enroll in Advantage plans will continue with 32 million seniors, or more than half of all eligible seniors, enrolling. Advantage plans are operated by commercial carries like United, Humana, Aetna, Blues, Cigna and Anthem. As the popularity of Advantage plans grows, so do the markets served by the carriers. These plans offer more services than traditional Medicare, often for no additional cost, such as dental, vision, hearing, transportation and even meals.
Incredibly, Advantage Plan premiums are expected to decrease 8% in 2023. Open enrollment for the Affordable Care Act and most employer plans began Nov. 1. The Kaiser Family Foundation estimates ACA premiums will increase 10% and commercial-employer premiums about 7%.


Prior to the pandemic, 11% of adults suffered from depression and anxiety. Since the pandemic, it is up to 40% of adults.

As the stigmatization associated with mental health declines, more and more people are seeking treatment. But therapists are struggling to keep pace and meet the demand.

Adding to the problem, since 2011, the number of practicing psychiatrists (MDs) has declined 6%. Most don’t accept Medicare and many don’t accept any insurance. Psychiatric nurse practitioners are increasingly critical in providing mental health services. Their numbers have increased 162% since 2011. Since then, NPs have provided 30% of all mental health visits. Start-up companies are assisting these NPs with establishing and running their private practices by lowering overhead and billing costs and contracting with both Medicare and commercial insurers.
Consumer surveys reveal 70% of respondents worry about their mental health coverage. Many plans still restrict coverage or have expensive copays.
















A survey of 8,000 adults by the Commonwealth Fund revealed insurance does not provide enough financial protection against rising healthcare costs.

43% of those surveyed were inadequately covered and 9% had no coverage. 29% of those with employer sponsored insurance and 43% of those with individual insurance were underinsured because of high outof-pocket expenses like deductibles and copays. Underinsured is defined as spending more than 10% of your income on out-of-pocket costs. 50% of those surveyed said they could not pay an unexpected medical bill of $1,000 within 30 days. Pollsters West
Health Gallup asked 5,000 adults to grade US healthcare for affordability, equity, accessibility, and quality. 44% of respondents graded US healthcare “F” and 33% graded it “D.” Only 22% of those taking the poll rated US healthcare either “A” or “B.”



Virtual care was growing VERY slowly in the several years prior to the pandemic.
The technology was there, but the acceptance by both providers and consumers was not.
The pandemic caused virtual care, by necessity, to rapidly proliferate. It is now widely accepted by insurers, providers and consumers and it is integral to healthcare access and delivery.
The Massachusetts Blues have teamed up with the Carbon and Firefly healthcare systems to offer their members virtual primary and mental health care by early 2023. The Blues are touting better outcomes, easier access, lower costs, less anxiety and improved outcomes. There will be no copays. You will be able to access your provider via laptop, desktop or phone. In addition to no commuting, waiting times will be minimal. There will be wellness coaching and support and specialists will be engaged, as necessary. The Blues will also provide free medical devices, such as blood pressure monitoring, to its members. United Healthcare, Aetna and Cigna are all considering similar products.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.


at concerning

The Upstate Comprehensive
is


U.S.
officials reported in October.
About 2.5 million middle school and high school students reported that they had vaped in the past 30 days in 2022, according to new data from the U.S. Centers for Disease Control and Prevention and the U.S. Food and Drug Administration.


That was 14.1% of high school students and 3.3% of those in middle school.
“This study shows that our nation’s youth continue to be enticed and hooked by an expanding variety of e-cigarette brands delivering flavored nicotine,” said Deirdre Lawrence Kittner, director of the CDC’s Office on Smoking and Health.
“Our work is far from over,” Kittner said in a CDC news release. “It’s critical that we work together to prevent youth from starting to use any tobacco product — including e-cigarettes — and help all youth who do use them to quit.”
The findings are from the National Youth Tobacco Survey, conducted among U.S. students in 6th through 12th grades between Jan. 18 and May 31. They were published Oct. 6 in the CDC publication Morbidity and Mortality Weekly Report.


Among the youth who vape,
about 85% used flavored e-cigarettes. The brands they used were Puff Bar, with 14.5% calling it their usual brand, Vuse at 12.5%, Hyde at 5.5% and SMOK at 4%. More than half used disposable e-cigarettes. Most used flavors were fruit at 69.1%, candy or desserts at 38.3%, mint at 29.4% and menthol at 26.6%.
About 27.6% of youth who vape did so daily. About 42.3% vaped on 20 or more of the past 30 days.
E-cigarettes contain nicotine, which is addictive and can harm the developing adolescent brain, the CDC said. It may also increase risk for future addiction to other drugs. E-cigarettes have been the most popular tobacco product for U.S. youths since 2014.
“Adolescent e-cigarette use in the United States remains at concerning levels, and poses a serious public health risk to our nation’s youth,” said Brian King, director of the FDA’s Center for Tobacco Products.


“Together with the CDC, protecting our nation’s youth from the dangers of tobacco products — including e-cigarettes — remains among the FDA’s highest priorities, and we are committed to combatting this issue with the breadth of our regulatory authorities,” he said in the release.
as well as other neuroimmunological
patients with con rmed or suspected
The program is unique in Central New York. It is designed to support each patient for the needs associated with MS, including a new infusion center, physical therapy,




management, specialty pharmacy services, nutrition guidance, urology support, social work services and consideration for clinical trials.
Patients should ask
for a





If you are facing Thanksgiving alone for the first time, you may be anticipating a lonely and depressing fourth Thursday of November.
But it doesn’t have to be so.
Whether you’re divorced, widowed or just can’t make it home for Thanksgiving, this family-centered holiday can be an opportunity for personal growth and expression. Plus some fun, too!
Below are some tips and creative ways to manage and embrace what can be a challenging day in the life of those alone this time of year.
• Be thankful — And why not start with yourself? Consider making a list of all the things you are thankful for this year: Your health? Your children? Good friends who have stood by you through thick and thin? A career or volunteer job you love? A beloved pet? Or perhaps even this opportunity now to experiment and learn new things about yourself?
• Take the long view — While you may be alone this year, it doesn’t mean you’ll be dining solo on leftover turkey the rest of your life. This one day doesn’t dictate your destiny.
Who knows what the future holds? Over the next year, you may meet someone special or achieve a measure of inner peace and confidence that enables you to enjoy a holiday on your own or with a “family of friends.”
• Do good — Helping others this time of year can take your mind off
being alone and give you something worthwhile to do. Shelters and food kitchens often welcome volunteers, but, truth is, many of these agencies fill up fast with regular volunteers. You may need to plan and be creative.
As an alternative, many local YMCAs host Turkey Trots and need volunteers to register and cheer on runners of all ages. Instead of serving stuffing at the shelter, you could be serving up smiles at the finish line.
• Throw your own little holiday dinner for fellow “strays” or “untethered” friends — Have some fun! It doesn’t need to be elaborate or even planned far in advance. Sometimes last-minute dinner invitations can turn into the best, most memorable get-togethers.
Chances are you know others who may be alone this Thanksgiving. Extend a warm invitation and invite your guests to bring along a beverage or holiday side-dish to pass. This gives everyone a chance to make a meaningful (and delicious!) contribution.

• Beware of “euphoric recall” — When you are feeling lonely, it can
be easy to glorify the past. Did last year’s Thanksgiving live up to the Norman Rockwell ideal? Or did all the bickering, bad blood, and woozy, overstuffed relatives make you want to run for the hills? Maybe, just maybe, being with your own good company is a blessing.
• Rent a movie and indulge in a tasty guilty pleasure — Oh, why not? Rent a favorite “feel good” film and make a night of it. You might check out “Tootsie” or “On Golden Pond,” two of my favorite oldies, which never fail to warm my heart.

Or find a new movie you haven’t seen and enjoy the novelty of seeing something for the first time. Top it off with a favorite treat. I love everything pumpkin this time of year: pumpkin soup, pie, ice cream and fry cakes!
• Pick up the phone — I’ve modified one of Abe Lincoln’s famous quotes for my own purposes: "Folks are usually about as lonely as they make up their minds to be." The difference between isolation and engagement can be as simple as sending a text or dialing a seven-digit phone number.
My experience happily tells me that most folks welcome a call on Thanksgiving. Why not pick up the phone to connect with out-of-town friends and family members? Catch up and make their day, as well as yours, a little richer.
Or connect locally with a neighbor or friend with an invitation to go for a walk around the block or see a matinee while the turkey is in the oven. Many folks welcome the diversion and chance to get out of the kitchen before or after the big feast.
• Decorate your home inside and out. — Do it for you. It may help put you in the spirit of the holiday. This past weekend, I recreated my annual stacked-pumpkin display for my front porch. It gives me a warm feeling every time I pull up to the house.
Add harvest accents to your

home and feel the essence of Thanksgiving in your heart.
• Nurture yourself — On your own, Thanksgiving can be a great day to do whatever you enjoy doing. Carve out well-deserved time to read, do some early online shopping for the holidays, give yourself a manicure or whatever tickles your fancy.
On Thanksgiving Day, I plan to nurture myself with a solo walk in the woods, where I find peace and feel connected to all living things: trees, birds, critters and insects — even creatures I can’t see within the ponds, underground and in the sky.
I never feel alone when I’m in nature and use the time alone to count my blessings and be grateful.
So pamper yourself for at least 30 minutes and take a mini-vacation from your worries, doubts and fears. Then seize the day with a renewed outlook on life.
• Write “thank you” notes — Now here’s an idea that’s so obvious it often gets overlooked on Thanksgiving. “Build bridges the rest of the year, and cross them during the holidays,” said Craig Ellison, PhD, author of “Saying Goodbye to Loneliness and Finding Intimacy.” If you can’t be with friends or family this holiday, pick up a pen and thank them for their support and friendship.
Who wouldn’t love to receive a hand-written card after Thanksgiving that begins, “I’m sitting here on Thanksgiving morning thinking of you. On this day of thanks, I can’t help but be thankful for our (fill in the blank).”
In preparation for this kind gesture, purchase cards and stamps in advance.
There you have it: Survival tips for a single-serving Turkey Day. The good news? It will be Friday before you know it and you can look back and be proud of yourself for rising to the occasion and treating yourself to big helping of joy and gratitude this Thanksgiving.
Playing sports can benefit children in many ways, but all sports are not equal when it comes to their bones.
New research suggests children will have healthier bones if they participate in multidirectional sports such as soccer or basketball, rather than unidirectional activities such as running.

Mixing it up a bit with a variety of sports instead of focusing on just one is also less likely to lead to overuse injuries, the researchers noted.
“Our data shows that playing multidirectional sports when younger versus specializing in one sport, such as running, decreased a per-
son’s bone injury risk by developing a bigger, stronger skeleton,” said study author Stuart Warden. He is associate dean of research and professor of health and human sciences at Indiana University-Purdue University Indianapolis.

“There is a common misperception that kids need to specialize in a single sport to succeed at higher levels,” Warden said. “However, recent data indicate that athletes who specialize at a young age are at a greater risk of an overuse injury and are less likely to progress to higher levels of competition.”
While researchers have traditionally looked at bone mass to
determine skeleton health, previous studies by Warden’s team have found that bone mass and size are equally important.
For this study, they used high-resolution imaging to examine bones in the shins and feet of women who compete in college cross-country running. These athletes often suffer bone stress injuries, such as stress fractures.
The investigators found that the women who participated in both running and multidirectional sports when younger had 10% to 20% greater bone strength compared to their counterparts who only ran.
In addition, those who had played sports like soccer or basketball when younger had better bone structure and strength than those who solely ran, swam or cycled, the scans revealed.
“We want to ensure people have better, stronger bones as they grow, become adolescents and go through life,” Warden said in a university news release. “Specializing in one sport at too young of an age means they are more likely to get injured and not make it at the collegiate and professional levels.”
Athletes should be given time to allow for proper growth and development, not specializing until at least their freshman year of high school, Warden advised.
Those who already play multiple sports should take time off for rest and recovery during the year, he added. This can improve both bone strength and performance.
The findings were recently published in the journal Medicine and Science in Sports and Exercise.







































































RecentlyI saw a patient with a previously undiagnosed condition called Charcot foot. This is a foot deformity occurring in patients with diabetes or others with decreased sensation in their feet.
The path to Charcot foot begins when diabetes damages small blood vessels.
This impedes circulation to the nerves, causing nerve damage called neuropathy. Patients with neuropathy lose the ability to detect cuts or other damage to the foot. Poor circulation also impairs the body’s ability to heal cuts, injuries, and infection. The foot is not only at higher risk for injury and infection, but heals these problems slowly.
This is an important reason for patients with diabetes to work with their doctors to control their blood sugar as best as possible. They should inspect their feet every single day to discover cuts, blisters or other problems right away. Clean feet, clean socks and well-fitting protective footwear are essential.
Charcot foot — also called Charcot arthropathy — develops only when neuropathy is present. The foot becomes injured, and the patient does not feel or sense the injury. The injury can be from obvious trauma, such as a fall, a twist, dropping something on the foot, or hitting the foot against an object. Often the injury is a series of small, undetected, cumulative microtraumas.
In a normal foot, abnormal forces or weight distribution is detected right away, and leads to automatic correction by adjusting the stance.
People without neuropathy do

this all day, every day, automatically without conscious awareness. But diabetic patients lack this ability to auto-adjust. These small traumas accumulate and lead to fractures and other injuries.
Without the ability to sense pain, the diabetic patient continues to walk on their injured foot. The injuries worsen leading gradually to foot deformity.
Less than half of patients with a Charcot foot even recall any injury. The risk of developing Charcot foot increases with obesity and with increasing age.
The deformity in Charcot foot makes fitting into normal shoes difficult or even impossible. The foot and ankle may become unstable, preventing normal walking. Most dangerous of all, the deformed bones in Charcot foot may push against the skin leading to a high risk of ulcers. Skin ulcers are at high risk of infection. Poor circulation makes healing of the ulcer and any associated infection difficult. Patients with infected Charcot foot ulcers have an incredibly high 50% risk of an amputation.
The first sign of a developing Charcot foot is swelling, usually painless. This often manifests as trouble fitting into one’s shoes. Another sign is redness and warmth, the body’s inflammatory response to injuries in the foot. Although this resembles infection, the risk of infection is low when the skin is intact. The redness and warmth of Charcot foot usually improve with elevation. Redness and warmth are less likely to resolve with elevation in infection.
To diagnose Charcot foot, your
doctor will review your history and examine your foot. Tests that may help with the diagnosis include X-ray, CT, MRI or bone scan. These tests help distinguish Charcot foot from infection and aid in planning the best treatment.

The goal of treatment is to create a foot that can rest flat on the floor, is without ulcers, and if possible, can use a commercially available diabetic shoe.

Nonsurgical treatments for early-stage Charcot foot include casts or boots to allow the bones to heal in a stable position and to prevent further deformity. Casts can reduce swelling and protect the bones. While wearing a cast, the patient will likely need to avoid weight bearing and use crutches, a knee scooter or wheelchair.
Patients unable to wear regular over-the-counter shoes on a deformed foot may need custom shoes, braces or orthotics.

When these treatments are insufficient, surgery may be an option. Some types of surgery include debridement (cleaning) foot ulcers, lengthening the calf muscle or Achilles tendon to relieve pressure points on the foot and removing bony
prominences that push on the skin creating the risk of ulcers. Sometimes more complex surgeries are required to correct the deformity. Due to the complexity of the surgery combined with diabetes, these surgeries carry a higher risk of complications, infection and amputation than routine foot and ankle surgery. For this reason, it is imperative to strive for the best possible blood sugar control and to avoid weight bearing until OK’d by the surgeon.
If you have diabetes, your best bet to protect your feet is controlling your diabetes, checking your feet daily and wearing strong supportive footwear. If you do notice a foot problem, don’t delay in seeking medical care.
Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.

 By Norah Machia
By Norah Machia
During the past year, the Upstate Golisano Children’s Hospital has seen a 17% increase in the number of autism patient appointments, a reflection of a nationwide trend.
In 2021, the Centers for Disease Control estimated that one in 44 children will be diagnosed with an autism spectrum disorder by the age of 8. That represents the highest rate since the federal agency began tracking cases in 2000.
The increasing number of cases is the result of “more awareness of autism spectrum disorder on two fronts,” said Henry Roane, Ph.D., division chief of the Center for Development, Behavior and Genetics at Upstate.
As a society, the discussions surrounding autism spectrum disorder have become more public, helping to reduce the stigma of seeking care and treatment, he said. In fact, “we’ve even had calls from adults who believe they may have gone undiagnosed as a child,” said Roane, who also serves as executive director of the Golisano Center for Special Needs.
Autism, or autism spectrum disorder, refers to a broad range of conditions characterized by challenges with social skills, repetitive behaviors, speech and nonverbal communication, according to the Autism Speaks organization.
“We know that there is not one autism but many subtypes, and each person with autism can have unique strengths and challenges,” the nonprofit agency states. Autism Speaks is both an autism advocacy group and the largest autism research organization in the United States.
“People have become more aware of autism spectrum disorder” as a result of an increasing number of movies and television shows focusing on children with autism and their families, Roane said.
While the increasing number
of autistic children’s portrayals is helping to create a better understanding of the condition, “sometimes those children with the most difficult behaviors are still not as readily accepted,” Roane said. Children with aggressive behavior, for example, are not typically the ones portrayed in the media, he noted.
“That type of awareness is really important for the population, and definitely helps with inclusion and acceptance,” he said. “But there are many children who have severe impairments, including cognitive and language, who also have autism. The media portrayals of these children are lacking.”
Parents of children with more challenging autism disorders, such as those who harm themselves or are not toilet trained “may feel left out of the discussion. That’s not their child on the television,” Roane said.
To help cope, parents of these children have often chosen to form their own support groups to help raise awareness of the “more severely impaired individuals with autism,” he said.
On a local level, the establishment of the Golisano Center for Special Needs in 2021 has also been a major factor contributing to the increase in autism patient appointments, Roane said.
The center provides comprehensive, coordinated and scientifically based medical and behavioral care for children and adolescents with many types of intellectual and developmental disabilities, according to Upstate Medical University. “The center acts as the umbrella, creating a framework to increase collaboration resulting in better patient care,” according to Upstate. “It helps to centralize programs and services available to this population.”
As a result of establishing the Center for Special Needs, which was supported through a major fund-raising campaign by the Upstate Foun-
dation, awareness has increased about the many different treatments and services available to autistic children and their families throughout Central New York, Roane said. It has also resulted in additional referrals from pediatricians in surrounding counties, particularly rural areas.
“The research is clear – the earlier you can start treatment for core symptoms, the better the outcome,” said Roane. “Two years of age is where you want to be for early intervention.”
Advances in medical research have allowed health care professionals to identify children with autism spectrum disorder at an even earlier age. “Now researchers are noticing low muscle control in infancy, how they move their eyes and other characteristics” that could indicate an autism case, he said. There is also experimental saliva testing being conducted as a way to help with diagnosis at an early age, he said.
Roane, a professor of pediatrics, is one of four experts who received grant funding from Autism Speaks to help improve the care provided to those with autism who experience severe behavioral challenges.

The grant funding is designed to collect and compile information nationwide about the current practices in identifying and handling challenging behavior from a wide variety of sources, including pediatric offices and specialized clinics.


The experts plan to analyze the information, including the outcome data, to determine the best care and treatment for these types of problem behaviors. A follow-up clinical trial will later be conducted to determine the success of these care and treatment approaches.
It was also recently announced that Upstate Golisano Children’s Hospital would join the Autism Care Network, a premier network focusing on improving the quality of health care children with autism and
their families.
Upstate will be joining 24 other hospitals nationwide in the network, which is supported by Autism Speaks, Roane said.
The partnership will be a valuable resource in helping to continually improve clinical care and quality of life for children with autism because it will allow health care professionals from throughout the country to share information about “what’s working in their clinics,” he said. “It will help to make our program even better,” Roane said.
• Upstate Golisano Center for Special Needs: 315-464-3555
• CNY chapter of the Autism Society of America: 315-447-4466
• Autism Speaks (Autism Response Team) 1-888-288-4762
Upstate Golisano Children’s Hospital has seen a 17% increase in number of appointments
Head of Clear Path for Veterans in Chittenango talks about programs in place that help veterans transition from military to civil life
By Mary Beth RoachQ: When and why was Clear Path for Veteran created?
A: Clear Path was created in 2011 by our cofounders Melissa Spicer, Melinda Sorrentino and Steve Kinney. The reason was to provide a
community-centric resource center for veterans and their families, who are transitioning from military ser vice to civilian life, as well as those veterans who already reside in our community, to establish a place for
them to connect with other veterans. The primary focus at the time of the founding was to create a service dog training program for veterans experiencing post-traumatic stress, military sexual trauma or a traumatic brain injury.
Q: The center has evolved a lot over the past 10 or 11 years.
A: Yes, it has. The main facility at our Chittenango location is on 78 acres. Shortly after the formation of the service dog training program, the family support program was established. This was to ensure that veterans, military members, and their families were able to connect with other veterans, but also to receive individualized support to address any barriers or immediate needs the veteran and family member was experiencing and those who are tran sitioning from this area to a different area.
Q: Explain the range that you serve — age, military branches of service, geography?
A: Clear Path provides our holis tic programs and services to veterans and their families throughout 33 counties in New York state — the counties in the North Country extend all the way to the Canadian border through Central New York, into the Southern Tier region in the Bingham ton area, and then most recently in the Hudson Valley area. We serve all veterans of all eras, all branches, regardless of discharge status or disability.
Q: How many people do you esti mate that you serve?
A: Last year we served just shy of 8,000 veterans through our events, our programs, our Wednes day canteen lunches. [This number represents veterans and family mem bers who make repeat visits to the facility.] Unique veterans and family members in 2021, we served just shy of 2,000 veterans.
Q: What facilities and amenities do you offer to veterans and their fam ilies at your center?
A: At our main campus, we house our canine training program. We also house our peer and family support program. The peers go into the community and meet the veter ans where they’re at if the veteran can’t get to our campus in Chittenan go. Our warriors working program is housed in Chittenango and our different locations throughout the state. That’s a career-services focused program, providing career placement services to veterans and transitioning military members.
We also have a holistic wellness program at our main facility and that focuses on the six dimensions of wellness and delivering alternative methods of wellness — everything from polarity to acupuncture or mas sage therapy, yoga, meditation, reiki.
Q: Do you have satellite locations?

A: We have folks that work in the Broome County region, at the Broome County office building. The peer in Hudson Valley has an of fice at the Castle Point VA medical facility. The Rochester and Western New York peer, as well as the North Country peer, work remotely.
Q: Did I see something in the media about a capital campaign in the works?
A: Yes. The growing demand for our canine service dog training pro gram, as well as the general holistic programs and services we’re offering at our main facility, are currently out growing our infrastructure. We are planning on embarking on a capital campaign to bring a stand-alone ca nine training facility to the property, as well as overnight efficiency cabins for those going through the intensive canine training service dog program, as well as those who attend our fam ily and caregiver retreats throughout the year at our campus.
Q: Why do you think a center like Clear Path is so important?
A: Being a veteran myself [Unit ed States Marine Corps, 2005 to 2010] I’m biased to the mission of what we’re doing on a day-by-day basis, but I also have the opportunity to see the impact that we are able to have, not only transitioning veterans, but veterans throughout the Central New York and Greater New York region — providing a center where people can feel welcome, become well and then re-enter into their community whole, meeting veterans where they’re at, and providing a welcoming place for veterans to come interact with other veterans. We feel that when veter ans return to their communities and thrive, the community thrives. Ev erything we’re doing is also helping prevent veterans from taking their own lives. That’s a big, big piece of the struggle in the veteran communi ty. Everything we do on a day-to-day basis is a multi-pronged approach to ensure that there is overall veteran well-being.
For more information: Clear Path for Veterans is located at 1223 Salt Springs Road, Chittenango. Phone: 315-6873300. Website: www.clearpath4vets.com.




American Thanksgiving is one of my favorite holidays. It gives me a chance to combine two of life’s most wonderful things—gratitude and gravy. One of the times I am most thankful is when I have the privilege of dousing an entire plate of food in gravy. It’s the little things that make life worth living.
Gratitude. The word of the season is a trendy concept these days. One can hardly shop without seeing the commercialization of gratitude. It has taken up residence on notebooks, candles and wooden plaques. The G-word is everywhere and often sporting a calligraphy suit. The corporate fat cats want us to believe that we can cut corners on the path to gratitude. All we have to do is plaster our homes with some gratitude street preachers.
No notebook can teach us how to be grateful. Instead, we need to convince ourselves to be grateful for the beautiful privilege of owning a notebook in which to write in. We need to be thankful for all of the small things in life that are true blessings.
We all know that’s easier said than done.
One of the aspects of parenting I’ve found most difficult is raising my kids to be grateful. I know the best way to do that is to demonstrate gratitude in my daily life. My family lives a truly blessed life, but having the mental maturity to accept that is difficult; radiating that gratitude is even harder.
What are my kids thankful for?
Recently, I asked my kids what they are thankful for. I wanted to hear their thoughts about gratitude. I expected them to quickly list things like family and friends and then diverge into hoverboards and tablets. To be frank, I kind of expected them to say the proper thing and then move onto the superficial stuff that they indulge in.
However, that didn’t happen. When I asked my kids what they were grateful for, they quickly listed family and our pets. They didn’t stop there. Their lists never diverged to stuff. As I listened to them, I came to a beautiful realization: my kids understood being grateful much better than I had anticipated. In a way, they understood it better than I did.
My kids listed things like food,
cotton candy ice cream, books, friends, our outdoor fire pit and our neighbors. They also listed things like flowers, shade underneath a tree, white puffy clouds, swimming, exercise and glasses of ice-cold water.

I was pleasantly surprised by how well my kids understood what to be thankful for. So, I moved on to my husband. When I asked him what he was thankful for, his list had many of the same things. He said he is grateful for fall colors and pumpkins and the salmon run. He was thankful for healthcare and good jobs. He is thankful to have kids who light up the room and are open to trying new things. He is thankful to live near so many beautiful state parks. He is thankful for his band and for friends with whom he can be himself. He is thankful for me and everything I do to keep our lives running smoothly.
As I listened to all of the beautiful things that made my family feel gratitude, I had a moment of intense realization—the very best things in our lives are the things that are at our fingertips every single day.
All too often, we look forward to the next big thing. We look forward to the weekends, the vacations, the parties and the events. Meanwhile, there are many days when the things that make our lives worth living don’t even make it on our radar.
As a parent, how many times have you raced to a practice or school drop-off and ignored the artistry of fall leaves? How many times have you spent an evening in an urgent care cursing your bad luck instead

of being thankful for your access to quality healthcare? How many times have you ignored your pet’s request for affection so that you could squeeze in one more chore before work? When’s the last time you paused and let yourself enjoy the intense pleasure of a glass of ice-cold water?
Sure, vacations, parties and fun events make us happy. But they don’t always make us grateful. After a big event is over, the fleeting happiness doesn’t get us very far and instead of being grateful for what passed, we start chasing the next big thing.

What if I could take a lesson from my kids and chase the next tiny happiness? What if I could find gratitude hidden in the complexity of a fall mum? What if I could pause long enough to appreciate the softness of my cat’s cheek? What if I could get insanely happy about my son mispronouncing arithmetic for the 15th, adorable time? What if I belly laughed at my daughter trying to assemble a list of lame Dad jokes? What if I gave myself permission to get giddy about all of the red hairs in my black-haired husband’s beard? What if I felt special when a family member called to share something completely silly and boring with me?
If I could do all these things, I would be more grateful for my beautiful, blessed life. And, just maybe, I would radiate the kind of gratitude that actually teaches my kids something. As we approach Thanksgiving, it can’t hurt to pause and give thanks. I’ll start with savoring some gravy.
During the pandemic, Peloton exploded in popularity as homebound people explored ways to get fit and stay active.
The exercise equipment manufacturer makes not only exercise bikes but also programs to keep users moving and motivated.


The combination of equipment and programming proved so successful during the pandemic that the company struggled to keep up with demand.
But does Peloton live up to the hype?
For around $2,500, the bike comes with a rotating screen so that users can participate in cycling on the stationary bike and in non-biking classes. Peloton also makes a treadmill (around $3,500) and a rowing machine (around $3,100). In addition to the equipment, users can sign up for a separate membership for $44 a month to access all the Peloton programming, accessible to the entire household.

“I’d never say no to people who want to do something active,” said Randy Sabourin, owner of Metro Fitness in Syracuse. “It’s a great supplement to going to a real, live class or gym where you meet real people. The instructor will coach, instruct and challenge you but won’t be in front of you. If you stop, you won’t feel as accountable as if you have people pedaling in front of you. There’s strength in numbers. You’ll always try your best when your effort contributes to the team. You feel

that energy in a class. You get more out of it with people around you.”
He fears that without the in-person group or in-person trainer accountability, “it will become a coat hanger.”
Tuning into a live session can offer real-time feedback and a measure of accountability. Or users can select pre-recorded sessions. Its programming includes classes in yoga, stretching, walk, running and resistance.
Another layer of anonymity may provide a protective buffer, but it also forces users to rely solely upon themselves to feel motivated to participate and to participate fully once involved. There’s no one to check in on them if they do not show up or to monitor form and progress as they participate.
Peloton offers a rental option and month-by-month program option.
“It’s worth it if you use it on a regular basis,” said Jill Murphy, certified personal trainer and co-owner of Mission Fitness in East Syracuse. “The return you get on any exercise equipment or investment will be contingent on whether you use it or not.”

“The good thing about it is the membership adds more opportunity
Peloton bike: The company makes not only exercise bikes but also programs to keep users moving and motivated.
for you than just having the bike or treadmill by itself,” she said. “Most exercise equipment comes with only a few programs. The Peloton has limitless programs for you to choose from.”
Unlike an in-person class, it can be difficult for people with limitations to use recorded or virtual classes.
“My client who has Peloton and has some back issues,” Murphy said. “When she uses it, it exacerbates those issues.”
An in-person trainer would be more able to modify movements and offer moment-by-moment guidance on them to help someone with an injury avoid further aggravating it.



can be both unpredictable and inconvenient.
Whether you are dealing with seasonal issues or year around nuisances, there are various factors that affect your sinuses. Climate change will potentially lead to both higher pollen concentrations and longer pollen seasons, causing more people to suffer more health effects from pollen and other allergens, according to the Centers for Disease Control and Prevention.

Pollen is like tiny seeds dispersed from flowering plants, trees, grass and weeds. The amount and type of pollen in the air depends on the season and geographic region. Though pollen counts are typically higher during the warmer seasons, some plants pollinate year-round.
“Allergies are more than a $6 billion industry so it is an essential topic that affects many people,” said Nicholas Groch, a board-certified ear,


nose and throat physician at Oswego Health in Oswego.













When it comes to allergies, because people have various reactions, there are common misconceptions that experts attempt to dispel. For example, doctors deal with patients coming into their office with self-diagnosis.
“They will come and say all they need is antibiotics and they will be fine,” said Groch. “The problem is that not every situation requires antibiotics. There can be dire, life-threatening consequences for people who take antibiotics for conditions that do not match their symptoms.”
Another misconception surrounds allergy tests. Even though a given patient may be tested for more than 60 different environmental and food allergens, testing negative
doesn’t mean the situation is resolved.
“All your tests could come back that you are not allergic to these substances but there could still be various allergens within those elements that you are allergic to. It doesn’t mean that you should stop trying to find answers,” said Groch.
Allergies occur when your immune system reacts to a foreign substance or a food that doesn’t cause a reaction in most people. While symptoms can vary, there are some common ones including itching of the nose, eyes or roof of the mouth, along with watery, red or swollen eyes and overall congestion.
Hay fever, also known as allergic rhinitis, occurs when allergens like pollen enter your body and your immune system mistakenly identifies them as a threat. If you have allergic rhinitis, your body then responds to the allergen by releasing chemicals that can cause symptoms in the nose. Symptoms of allergic rhinitis can occur during certain seasons or yearround, depending on the allergen and affect as many as 60 million people per year in the United States.
Symptoms from allergic rhinitis include sneezing, runny nose, and congestion.
When determining what else can be done to eliminate allergy symptoms, Groch has some baseline advice.
“One of the excellent options is to use saline nasal spray. It is relatively inexpensive and doesn’t require a prescription,” he said.
Various allergy diagnosis and treatments can lead to many different diagnoses. Environmental allergies are diagnosed by proper history-taking, examination and allergy testing. Treatments may include medications such as non-sedating antihistamines, steroid nasal sprays and allergy shots.
Food allergies are diagnosed with proper history-taking, examination and allergy testing. Treatments include avoidance, and certain types of food allergies may necessitate carrying an epinephrine auto injector pen and having an allergy action plan. For patients with particular types of food allergies, there are also newer treatments, including oral immunotherapy. In addition, patients can misdiagnosis themselves.
“One way to determine between a sinus infection or simply allergies is




Nicholas Groch, a board-certified ear, nose and throat physician Oswego Health in Oswego.







that in a sinus infection there is thick, yellow nasal drainage versus clear runny nose when we are dealing with allergies,” said Groch.

Allergy experts believe the field and symptoms are growing exponentially so they advocate for allergy sufferers to consult a professional. Simply pointing to your family history or self-diagnosis can lead to unnecessary trial and error.
“Allergy medication can be taken at any time of the year where you have symptoms or you can wait until those symptoms develop when you become stuffy, runny or sneezy,” he added.
A runny or stuffy nose, cough, tiredness, even shortness of breath and a lack of smell and taste can occur in both allergies and COVID-19. But a cough from COVID-19 is typically dry, whereas in allergies, a cough is wet and usually more sneeze-like.
“This is one of the reasons why we tell our patients to consult with their primary care or specialist physician. Some of the symptoms of COVID-19 and allergy can, on the surface, be the same but they are very different,” he added.
Everyearly November, my family has the most absurd conversation. We talk about Thanksgiving sides as if they were open for discussion. Who are we trying to kid? Like most Americans, we would never switch up our cherished favorites—our beloved stuffing, mashed potatoes and green bean casserole. Thanksgiving is about peace and togetherness, after all, not acrimony and war!
Green bean casserole is our favorite and that’s because, of all the sides, the nutritional chops of green beans somehow justify all those tempting seconds and thirds.
Green beans pack a decent fiber punch, delivering about a fifth of our daily needs in one cooked cup. Fiber promotes regularity, ferries bad cholesterol out of our bodies and helps to stabilize blood sugars. What’s more, multiple studies suggest that increasing fiber reduces our risk of dying from heart disease, cancer, stroke and diabetes.
On the vitamin front, this tasty legume provides admirable amounts of vitamins K, C, A and folate. While vitamin K helps blood clot properly and maintain strong, healthy bones, vitamins C and A promote healthy immune systems, which is especially
important during flu and cold season. Folate, a critical B vitamin that prevents birth defects in newborns, also contributes to heart health by lowering an amino acid that can lead to hardening of the arteries.
Green beans are a good source of minerals, especially manganese. This essential mineral supports bone health, promotes wound healing, and has antioxidant abilities, much like vitamins C and A, that protect our bodies from disease and accelerated aging by neutralizing toxic free radicals.
A versatile bean that can be eaten raw or cooked, green beans are naturally low in fat, sodium, cholesterol, and calories: only 44 per cooked cup.
What’s more, fiber-rich beans take longer to digest, which helps us feel full longer, snack less, and maybe, just maybe, reach for only two helpings this Thanksgiving instead of three!
Adapted from slenderkitchen.com
2 pounds fresh green beans
2 tablespoons butter, divided
1 cup shallots or onions, thinly sliced
½ cup whole-wheat panko breadcrumbs

¼ cup sliced almonds
1 pound mushrooms, sliced 3 garlic cloves, minced
2 tablespoons white whole-wheat flour
2 cups reduced-fat milk
2 vegetable bouillon cubes (or chicken)
1 teaspoon dried thyme ½ cup grated Parmesan cheese (optional)
Salt and pepper to taste
Preheat oven to 400 F.
Bring a large pot of water to a boil. Add the green beans and cook 3-4 minutes until bright green and tender crisp. Immediately add to an ice bath to stop the cooking. Strain and dry.
Melt 1 tablespoon of butter in a pan over medium heat. Add the shallots or onions and cook 5-7 minutes until tender. Transfer to a small bowl. Add the breadcrumbs to the

Folks who drink two or three cups of coffee daily appear to live longer than people who don’t care for the beverage, new research shows.
Coffee lovers also seemed to have healthier hearts, which might contribute to the longevity boost, said the team of Australian investigators.
The findings were published Sept. 27 in the European Journal of Preventive Cardiology.

“Ground, instant and decaffeinated coffee were associated with equivalent reductions in the incidence of cardiovascular disease and death from cardiovascular disease or any cause,” study author physician Peter Kistler, of the Baker Heart and Diabetes Research Institute in Melbourne, said in a journal news release.
While other studies have suggested that the coffee habit might be a healthy one, Kistler’s team said there’s not been much investigation into the health effects of various forms of coffee.
To try to find out, they analyzed data from the ongoing UK Biobank database, looking at data on people aged 40 to 69. In this study, the average age was 58 and the Australian researchers focused on levels of daily coffee intake and life span, as well as heart disease, heart failure and stroke.
Overall, data on almost 450,000 Britons was included in the research. Regarding daily coffee intake, participants were divided into six groups: No coffee; less than a cup a day; one cup per day; two to three cups per day; four to five cups per day; and over five cups per day.


Purchase fresh when possible. Look for firm beans that are bright green and free of black spots. Fresh green beans should be refrigerated in a plastic bag and eaten within a week or less, since they lose their fresh flavor quickly. Since cooking green beans may cause a reduction in some nutrients, such as vitamin C, cook them for the least amount of time necessary, whether boiling, steaming, sautéing or roasting. Steaming beans is better than boiling, since it uses less water and prevents the beans from overcooking.
pan, toast for 1-2 minutes until light brown, and transfer to the cooked onions. Stir in the sliced almonds. Set aside.
Wipe out the pan with a paper towel. Add the remaining tablespoon of butter. Once melted, add the mushrooms and cook 6-8 minutes until tender. Add the garlic and cook 1 minute more. Add the flour, along with a splash of water, and stir well. Cook for 1 minute. Add the milk and bouillon cubes. Bring to a simmer and cook for 6-8 minutes, stirring often, until thick and creamy. Turn off the heat and stir in the thyme and Parmesan cheese (if using). Season with salt and pepper to taste.
Lightly oil a 9 by 13 inch baking pan. Add the green beans and mushroom gravy, Stir to combine. Top with the onion mixture.
Bake for 20-25 minutes until browned and bubbly.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

Medications for Hope, a new program that provides free prescription medications to the poor, enrolls fewer people than expected
By Mary Beth Roachprescription program
launched by Upstate Medi cal University a few months ago for qualifying patients has not reached its target enrollment num bers yet, but there is no minimum number of enrollees that will cause the program to stop, officials said.
They had hoped to sign up 10 to 15 people a month for the Medica tions for Hope program, according to Eric Balotin, director of Retail/Spe cialty Pharmacy Services at Upstate, but since its was unveiled in Septem ber, the program had a total of about 10 patients signed up by the end of September.
While he’s surprised that the numbers aren’t higher, he and his
team are ramping up efforts to reach target audiences.
It provides free prescriptions for most drugs to those patients without insurance and whose income is at or below 300 percent of the federal poverty guidelines. Even delivery of the meds is free, regardless of wheth er they’re shipped or sent through a courier service.
“We know there is a significant need in the community. We know we have a very high poverty rate among children and a very high poverty rate in general compared to the national,” according to Balotin.
The introduction of Medications for Hope comes at a time when the poverty rate in Syracuse is at 32.6%,
 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant
The ear-splitting, chainsaw-like sounds coming from the other side of your bed does not nec essarily mean that your beloved has sleep apnea.
“Snoring is an indication of narrowing of the airway,” said Sherif El Bayadi, medical director of St. Joseph’s Health Sleep Services.
“This usually happens most remarkably in the back of the throat and may be worsened with sleeping in the supine position In a supine position, the tongue and soft tissue get closer together due to gravity.”
About half the population snores sometimes, but that does not mean the person necessarily has sleep apnea.
With sleep apnea, “there is no air movement because of a collapsed airway,” Bayadi said.
For 10 to 20 seconds, the patient does not get enough air and may gasp and choke.
This sporadically awakens the person to breathe all night and results in feelings of exhaustion the following day.
During deep sleep, apnea is worse, as the muscles relax even more. With snoring, it is usually just the non-snorer whose sleep is disrupted.
Sleep apnea fragments sleep, making the person feel less rested. Quality of life is typically why pa tients seek treatment for sleep apnea. But sleep apnea can contribute to an increased risk for many health
conditions.
Soda Kuczkowski, sleep health educator and owner of Start with Sleep in Buffalo, listed weight gain, memory loss, and tied to a greater risk of high blood pressure, heart attack, stroke, congestive heart fail ure, atrial fibrillation, diabetes, and certain cancers among the increased risks associated with untreated sleep apnea.
Risk factors for developing sleep apnea include being overweight or obese, large neck size, age, male or menopausal, having high blood pressure, a family history, diabetes or being a member of a minority and veteran status.
“Veterans are four times more likely than other Americans to suffer from sleep apnea,” Kuczkowski said.
The disruption in breathing deprives the brain and the rest of the body of sufficient oxygen. The condition has four types: obstructive, central, complex and positional.
Obstructive “involves a de crease or complete stop in airflow despite an ongoing effort to breathe,” Kuczkowski said. “It occurs when the muscles relax during sleep, causing soft tissue in the back of the throat to collapse and block the upper airway.”
Central sleep apnea involves the brain not sending signals to the mus cles that control breathing. Kuczkow ski said that this breathing disorder involves problems in the brain or heart, not a blockage.
compared to 15.1% across New York state, according to welfareinfo.org and the U.S. Census has reported that Syracuse has the highest level of child poverty in the country at 48.4%.
“We know there is a significant need in the community. We know we have a very high poverty rate among children and a very high poverty rate in general compared to the national,” Balotin said.
The initiative has been several years in the making and it was rolled out earlier this summer throughout Onondaga County. In early Septem ber, Upstate broadened the pro gram’s scope to include communities as far north as Watertown, south into the Ithaca and Binghamton areas, east to Oneida and west to Auburn.
Anyone who meets the criteria, even if they are not Upstate pa tients, can receive their prescriptions through this program.
While there are certain medica tions that are not available through the program, referred to as specialty meds, Balotin explained that there is a whole class of therapy meds that can be provided. Insulin, which has increased in cost in the United States by more than 1,000%, is also available through Medications for Hope. However, the needles used for injection, can be cost-prohibitive and are not covered.
Balotin said they will work with patients to make everything as af
fordable as possible.
While New York City has five similar programs, Medications for Hope is unique to the Upstate New York area.
The project is due to the gener osity of the generic manufacturers, he said. Most of the meds are being provided free of charge from manu facturers to a centralized location and then Upstate gets its supply shipped from this site. The manufacturers have, at certain times, an abundance of extra medications, so instead of discarding them because they’re go ing to expire, they offer them through the program, Balotin explained.
While the hospital assumes the cost of shipping and the labor to pre pare the prescriptions, Balotin point ed out that the costs are still less than hospitalization for someone without the financial means or insurance, adding that 30% to 40% of prescrip tions are never filled, which often results in added hospital admissions and readmissions.
“We’re really trying to get on top of this, trying to help our community and that what it’s all about,” he said.
Those interested in learning more about the program can call the Up state Pharmacy at 315-492-5311, ask their doctor or visit www.upstate. edu/outpatient-pharmacy/index. php
Complex sleep apnea is a mix ture of obstructive and central apnea. Positional sleep apnea is as its name denotes: sleep apnea involving body position during sleep.
Easy, home remedy interventions for snoring include a nose dilator, eu calyptus essential oils, side sleeping, using a humidifier, proper hydration, limiting alcohol and maintaining proper weight.
Sleep apnea requires profession al treatment. Typically, insurance
coverage permits patients to self-re fer to a sleep specialist. Most people can have a sleep study performed at home. However, some do need to stay overnight at a sleep center.
Many patients also assume that treatment involves a cumbersome CPAP, or continuous positive airway pressure device. But newer therapies like dental devices and Inspire, an implantable device, can make treat ment easier.
About 80 autoimmune disorders exist, depending upon how these conditions are classified.
Although affecting different areas and systems of the body, this group of disorders possesses a few similarities.
Some share a few core symptoms, such as fatigue, body aches, fever, swelling, difficulty in focusing, weight fluctuation and skin changes.
Most autoimmune conditions present with other specific issues. Some inexplicably go into remission and flare up later, but in most cases are lifelong upon onset.
Medical care and good self-care can usually make living with an autoimmune condition much more comfortable. No cures exist for autoimmune conditions.
“The effects of having an autoimmune disease extend beyond the physical symptoms, as depression and anxiety frequently co-exist with autoimmune disease,” said Molly Murray, president and CEO of the Autoimmune Association in Clinton Township, Michigan. “Autoimmune patients can feel stressed from
navigating healthcare coverage and treatments, having to go to frequent medical appointments, and trying to balance their condition with other life responsibilities. They can feel isolated and misunderstood and can grieve the lifestyle they had before their diagnosis. Autoimmune patients should know they are not alone. Mental health providers can provide coping tools, and we encourage everyone to share their stories and connect with other patients.”
Some autoimmune conditions are invisible and can be minimized by outsiders.
Crohn’s disease and colitis cause diarrhea, urgency, abdominal pain and cramping, bloody stool, fatigue and weight loss and “it is not just ‘tummy pain’ or diarrhea,” said Becky Johnson Rescola, vice president of education and community engagement at the Crohn’s & Colitis Foundation in New York City. “Many people don’t understand the fatigue, chronic pain, and day-to-day accommodations that are part of coping with these diseases.”
The organization operates a chapter in Rochester that serves all of
Western and Central New York.
Alopecia areata is another example of an autoimmune condition. Tracy Higginbotham was diagnosed in 1993. She is founder of Women TIES in Syracuse and author of Under the Rose-Colored Hat, an autobiography about her journey with alopecia in Syracuse. She has experienced a variety of autoimmune disorders since 1977 when she was diagnosed with hypothyroidism.
When alopecia areata hit in 1987, her hair would fall out in small patches and regrow.
Eventually, she experienced more widespread hair loss. The cortisone shots and prednisone she had been taking to ward off hair loss no longer worked. By 2006, she had alopecia universalis—complete bodily hair loss.
As the leader of an organization promoting women in business, Higginbotham wears pink as her signature color. That occasionally leads to confusion as people connect her lack of hair with chemotherapy and assume she has cancer until she explains she is not sick or in pain.
“I also got my ears pierced to look more feminine as sometimes I’ve been confused for a man,” she said.
Higginbotham sometimes wears wigs and other times a sporty hat when bicycling or engaging in other
• Rheumatoid arthritis, in which the immune system destroys the joints, followed by the organs.
• Psoriasis/psoriatic arthritis causes skin cells to build up and form inflamed scales on the skin. About one-third of people with psoriasis also have psoriatic arthritis.
• Multiple sclerosis attacks the myelin sheath which surrounds the central nervous system’s nerve cells, slowing impulses from the brain to the body, resulting in difficulty in movement.
• Systemic lupus erythematosus causes joint pain, severe body fatigue and skin rashes.
• Inflammatory bowel diseases include Crohn’s disease, inflaming any portion of the GI tract and ulcerative colitis, which affects the colon and rectum.
• Addison’s disease affects the how much hormones the adrenal glands produce, which regulates how the body uses and stores carbohydrates and regulates sodium in the bloodstream.
• Although in different ways, Graves’ disease and Hashimoto’s thyroiditis affect the thyroid, a gland important for controlling the metabolism.
• Sjögren’s syndrome attacks the glands that produce saliva and tears, meaning the patient experiences dry eyes and a dry mouth.
• Celiac disease causes the immune system to attack and inflame the small intestine whenever the patient eats foods containing gluten, a naturally occurring protein in wheat and rye. Gluten is not harmful to people without celiac disease or sensitivity. Gluten sensitivity is not an autoimmune disease.
physical activity.
She encourages anyone with an autoimmune disorder to seek information through a reputable, national organization and seek support from others with the same condition because other people likely will not understand.
“The National Alopecia Areata Foundation has up-to-date research,” Higginbotham said. “You can listen to doctors talk about things with webinars. With autoimmune diseases, have a good endocrinologist who can help you. You need a specialist. Don’t be afraid to go outside the area. I went to the Mayo Clinic to see if there’s anything else. The answer was that there wasn’t anything else I could do. That was a good enough answer. The Cleveland Clinic is another place. I went to Boston to the Women’s and Children’s hospital. It helps to get opinions outside the area. Don’t stop locally.”

Fornearly 20 years, Upstate University Hospital has helped grieving families find a special way to preserve some precious mem ories of their lost loved ones.
The hospital’s caring medi cal staff works with terminally ill patients and their families to create memory boxes, a lasting and impact ful initiative that provides comfort to families long after they leave the hospital. In some cases, the boxes may be created in honor of those who pass away unexpectedly.
“The memory boxes are intro duced to patients and their families as a comfort care measure, and to help preserve the memory and leg acy of that person,” said physician Suman Swarnkar, associate professor of medicine and director of palliative care. The memory boxes offer a way for the family to honor their loved one and have something special to remember them by, she noted.
Each memory box comes with moldable clay to create a handprint of the patient. Other items that can be collected for the box include finger prints, locks of hair and even EKG strips.
These are typically combined
with remembrance items from the family, such as personal letters or cards, photographs and special jewelry or other sentimental keep sakes. The patient or family members decide what will be placed in the memory boxes.
“Patients may use these nice ly decorated boxes to create their own stories,” Swarnkar “They may include items related to loved ones, and those that have significant mean ing in their lives and their family’s lives.”
The family may also be pro vided with books (particularly for young children who have lost a close relative) and other support materials to help with the grieving process.
“These boxes are made to last, and families hold onto them for a long time,” she added.
Memory boxes are created only after the medical staff determines it would be a good option for patients and their families. The medical staff is sensitive about which families may or may not want to participate, said Swarnkar.
“Everyone is different” when it comes to handing the loss of life, she noted. “Some may just want a hand
It definitely pays to know what charges to expect when pre-plan ning a funeral. Most people don’t have a clue and can often be upsold thousands of dollars’ worth of extra services they may not want or need.
Here’s a breakdown of what you can expect.
The first thing you need to be aware of is that funeral costs will vary considerably depending on your geographic location, the funeral home you choose and the funeral choices you make. With that said, here’s a breakdown of what an average funeral costs, nationwide, according to the most recent data from the National Funeral Directors Association.
• Professional services fee: This is a basic non-declinable fee that covers the funeral provider’s time, expertise and overhead: $2,300.
• Transfer of the remains: This is for picking up the body and taking it to the funeral home: $350
• Embalming and body preparation: Embalming is usually mandatory for open-casket viewing, otherwise it’s not required unless the body is going to be transported across state lines. Embalming costs $775. Other body
preparations, which includes hair dressing and cosmetics runs $275.
• Funeral viewing and ceremony: If the viewing and funeral ceremo ny is at the funeral home, you’ll be charged for use of the chapel and any necessary staff. Costs: $450 for view ing, and $515 for funeral ceremony.
• Metal casket: This is a big money maker for funeral homes, with mark ups of up to 300 percent over the wholesale price: $2,500.
• Funeral transportation: Use of hearse and driver; $325 to transport the body to the cemetery. Use of a service car or van: $150.
• Memorial printed package: This includes printed programs and me morial guest book: $183.
In addition to these costs, there are also a number of cemetery costs like the plot or mausoleum fee, the vault or grave liner that most ceme teries require, and the opening and closing of the grave, all of which can run between $2,000 and $3,000; and the gravestone, which typically runs between $1,000 and $3,000.
You’ll also need to budget for related expenses like flowers for the funeral ($200 to $400), the newspaper obituary fee ($100 to $800 or more), the clergy honorarium ($200 to $300) and extra copies of the death certif icate ($5 to $35 per copy depending
print or may take home a neck pillow that had belonged to the patient.”
The memory boxes are covered through the annual fund for Upstate University Hospital called “Friend in Deed.” It’s one of many programs and services offered to patients and their families for which there are no other funding sources.
Donations made to the Friend in Deed fund are also used for pro grams such as nutritional support for cardiac patients, home monitor ing and telemedicine resources for diabetes and hypertension patients, a behavioral health education library, and spiritual care support for pa tients, along with many others.
The annual fund is administered through the Upstate Foundation, a nonprofit organization that is the primary resource for receiving and distributing philanthropic gifts to Upstate Medical University. Donated funds help to support patient health care, health care provider education, scientific research and community health initiatives.
Sometimes more than one mem ory box will be created, particularly if a family would like each child to have one, said Lori-jeanne West, nurse practitioner in the Upstate Uni versity Hospital Intensive Care Unit.

In one case, a mother in her 30s had died after sudden cardiac arrest, and a memory box was created for each of her three young children, all who were less than six years of age, said Ms. West, who is also an assistant professor at the College of Nursing.
“Many people are interested
Nurse practitioner Lori-jeanne West holds a memory box that’s offered to families of terminally ill patients.
in having something to hold” that contains memories of their lost loved one, she said. Families often put the memory boxes in a special place in their homes where they can sit quiet ly and look through them.
It often helps a family member to relax or meditate while thinking of the person who passed away. Some families have also saved the boxes for their young children to look through when they get older, Ms. West said.
“Sometimes it’s such an over whelming experience that a family can’t looks at the box right away, but they look at it after some time has passed,” she said. “It’s been so mean ingful for so many families and has helped them through their grieving process.”
For more information on how to support the Friend in Deed cam paign, go to www.upstatefoundation. org/give
on the state).
All told, the average cost of a total U.S. funeral today with view ing and cemetery burial is around $12,000.
If this is more than you’re willing or able to pay, there are ways to save. For starters, you should know that prices can vary significantly by funeral provider, so it’s wise to shop around. If you need some help, there are websites you can turn to like Parting.com that lets you easily compare prices online based on what you want.
When evaluating funeral provid ers, be sure you get an itemized price
list of services and products so you can accurately compare and choose what you want.
The most significant way to save is to request a “direct burial” or “di rect cremation.” With these options the loved one would be buried or cremated shortly after death, which skips the embalming and viewing.

If you want a memorial service, you can have it at the graveside or at your place of worship without the body. These services usually run between $1,000 and $3,000, not counting cem etery charges.
Jim Miller is the author of Savvy Senior, a column that runs every issue in In Good Health.
have already researched prior to the conversation. Whether you visit them in person or do online research, keeping a few facilities in mind can ease any nervous feelings about the process.
the conversation as early as possible, and focus on what matters,” said Angela Catic. She’s a geriatrician and associate professor in the Roy M. and Phyllis Gough Huffington Center on Aging at Baylor College of Medicine in Houston.
“Think about if an assisted living environment could not just support, but enrich things that really bring joy to that individual’s life,” Catic said in a college news release.
As people age, it gets harder to take care of a house and yard. Adult children often start talking about assisted living when they see their parents are struggling, Catic said. After the death of a partner, a person may feel alone and lose their social connections. This is where transitioning into assisted living could benefit an older person, as such facilities often provide various social activities for their residents.
When starting a conversation with a loved one, consider covering these topics:
• Mention a few facilities you
• Present a few options close to your loved one’s home or facilities near the home of a family member. This could remind them that they won’t be completely alone and will still have access to their family.
• Stay mindful of their feelings, as they could feel anxious or sad about having such a conversation. These emotions may prompt them to resist the move altogether.
• Mention any of their friends that you have heard from or ask them if they know anyone who has already moved into an assisted living facility, to normalize the idea.


• Make sure they feel involved in the process so they feel like they have control over what happens.
• Encourage them to come with you to tour a few facilities so they can visualize what their stay would be like there.

“Find a place they feel good about, too, and bring some of their belongings,” Catic said. “It’s typically a major downsizing of space, but it is important to bring things that
have meaning to them and make it feel like home as much as possible. This may include items like a favorite chair, items they need to engage in a favorite hobby or family photographs.”
If your loved one says no to the idea of moving to an assisted living facility, don’t keep pushing the idea unless you’re truly worried about their safety. Hospitalization due to an accident or other health issues can also be a good reason to bring up the idea of assisted living again.

If they decline initially, you can always return to the conversation later, as their initial hesitation could be due to other factors that change, Catic said. When bringing the topic up again, ask them if they had time to reconsider the idea. Welcome their thoughts on the subject and offer ways you can make the process more comfortable for them.
Catic advises prioritizing finding

your loved one a place that fits their needs and learning as much about it as you can so you know exactly what you are signing them up for. Even if a place looks nice in the lobby or on the tour, finding out more about what they have to offer can be an important part of finding the best fit for your loved one.
Additionally, learn about the staff and how often people move in and out. On another note, some facilities might have connections to different social groups such as veterans or other interesting people with whom your loved one could socialize.
“Go beyond the beautiful, fresh flower bouquet in the lobby because this is going to be someone’s home, not a hotel they’re staying in for a couple of nights,” Catic said. “You’re looking for a feeling of home and fitting in with other residents and a staff that feel like family.”
reduce their risk for further vision loss, including avoiding exposure to smoking and eating a balanced diet.
Supplements can also help, in cluding brands such as Preservision and Ocuvite.
papayas.
N-acetyl cysteine is a supplement form of cysteine, which is in many high-protein foods, like meat, poul try, yogurt, eggs, cheese, sunflower seeds and legumes.
degeneration is one of the nation’s leading causes of blindness and low vision, affecting 1.8 million Americans, according to the Centers for Disease Control and Prevention.
Age-related macular degenera tion (AMD or “dry” macular de generation) is more commonplace, 70%-90% of cases, than wet macular degeneration (WMD).
“They are the same condition, but there are varying degrees,” said Angeliki ArvanitoGiannis, ophthal mologist with VA Hudson Valley Healthcare System in Montrose and in Rochester. “Macular degeneration is either ‘wet’ or ‘dry,’ but they pres ent differently as far as the signs.”
Either type of macular degenera tion affects the central vision, which is important for reading, filling out paperwork and driving. Patients may see fine in their peripheral vision, but not in the center. For example, they may see a person’s clothing and hair, but not the face.
WMD occurs when blood vessels grow abnormally under the macular and leak blood and fluid. This vision loss is rapid, and typically presents with straight lines appearing wavy. AMD is a slower process as the macula thins, which eventually blurs vision. Patients have a 10% chance of progressing into WMD.
As WMD progresses, “when the eye is under stress, it will form new, weak blood vessels,” Arvani toGiannis said. “They don’t respond the way they should. They can leak blood or fluids.”
Patients need a clinical diagnosis after a dilated eye exam so provid ers can form a treatment plan, as ArvanitoGiannis said that other eye conditions can present with similar symptoms.
“There is no cure for it, but with early diagnosis, you can be a little more on top of these preventative measures and if you have the dry form, the sooner you are seen and managed, the better visual outcome you have. If you notice any sudden changes in your vision, don’t delay.”
Mark Breazzano, ophthalmolo

gist with Retina-Vitreous Surgeons of CNY in Liverpool, encourages people with symptoms to seek a dilated eye exam from a retinal specialist.
“This allows us to take a look in the back of the eye,” he said.
His practice also has offices in New Hartford, Binghamton, Ithaca and Watertown.

“Sometimes, the difference be tween wet and dry age-related macu lar degeneration can be quite subtle,” Breazzano added. “We also typically rely on optical coherence tomogra phy. This tool can assess smaller than what we can see on a normal dilated eye exam, that are distinct between wet or dry age-related macular de generation.”
Doctors can treat WMD to reduce its effects with anti-VEGF injections to decrease the bleeding and fluid in the back of the eye. Breazzano said that the treatment is “quite effective. A number of patients will improve; some maintain what vision they have and some will do worse. But the con sensus is that even among those who do worse, it’s generally better than not treating at all.”
Taking AREDS2 supplements has also shown to help for people with DMD and help reduce the risk of complications including conversion to WMD.
Lori Youngman, optometrist with Harbor Eye Associates in Oswego, said that patients will need to return to their provider for injections to prevent further damage.
“I would say that 70% of my pa tients who go that route do better for a while,” she said. “Unfortunately, it’s an age-related disease and with anything age-related it can slowly get worse.”
Ignoring symptoms or delaying treatment are the worst things to do. Even a week’s delay can negatively affect vision. With effective treat ment, WMD can be managed for years — even decades — thanks to current protocols with a much lower risk of losing vision.
Youngman also advises patients in lifestyle modifications for those with macular degeneration that can
Early diagnosis can help patients make lifestyle changes that can slow macular degeneration progress. In addition to smoking, the greatest risk factors for macular degeneration include age, family history, gender (women are more prone), high blood pressure, high cholesterol and poor diet.
Laurel Sterling, registered dieti tian, nutritionist and educator with Carlson Laboratories in Canastota, recommends improving the diet by including more healthful foods to prevent further degradation for eye health and in general to promote eye health and reduce the risk of eye issues.
She recommends improving intake of “carotenoids like lutein and zeaxanthin, beta-carotene, vitamin C, bilberry, N-acetyl cysteine and minerals like zinc and copper work as antioxidants that can assist overall eye health.”
Leafy green vegetables like spin ach and dark-leaf lettuce, cruciferous vegetables like kale and broccoli, and eggs and peas are good sources of lutein and zeaxanthin. Beta-carotene is found in green leafy vegetables; or ange vegetables like squash, carrots and sweet potatoes; and fruits like melons, sour cherries, mangoes and

Your fondness for midnight snacks has caused you to pack on the pounds over the years, and now researchers have a better un derstanding of why.
While late-night eating has long been linked with an increased risk for obesity, researchers weren’t sure exactly how it caused weight gain until now.
“When meals are delayed by four hours and everything else stays the same, you burn fewer cal ories, have an increased drive for food, and experience changes in fat tissue that would promote weight gain,” said study author Frank Scheer. He’s the director of the medical chronobiology program at Brigham and Women’s Hospital in Boston and a professor at Harvard Medical School.
The solution? Eat earlier in the day, he said.
“The new data suggest, to gether with the literature, eating earlier in the waking day results in changes in physiology that would promote weight loss and limit weight gain,” Scheer said.
For the study, 16 people who were overweight or obese stuck to a strict early and late meal sched ule for one day each in a lab. In the weeks before each experiment, folks maintained fixed sleep sched ules. They also ate identical diets and stuck to the same meal times at home.
Stellar sources of vitamin C in clude oranges, strawberries, raspber ries, cantaloupe, red peppers, cauli flower, broccoli and Brussels sprouts. Nuts and seeds are rich in numerous minerals.
The participants reported on their hunger and appetite, provid ed blood samples throughout the day, and had their body tempera ture and calorie use measured. Researchers also collected samples of fat tissue.
Due to the study’s design, researchers were able to tightly control for exercise, sleep and light exposure, which could affect how many calories participants burned.
More research is needed to see if these findings hold in real life, Scheer said.
“In the real world, when peo ple change meal times, they may also change other behaviors such as timing or quality or time of sleep or how much they exercise, which could affect weight,” he said.
The study was published Oct. 4 in the journal Cell Metabolism.
Aging brings its own rewards— wisdom, experience and sense of accomplishment—along with a few challenges. With planning
a few
Losing muscle is not merely a vanity issue. Along with poor balance, it can contribute to falls and subsequent frailty. It begins grad ually in middle adulthood but can occur more rapidly if an older adult has been laid up because of sickness or injury. That is why beginning a physical fitness regimen earlier in life is so important.

But exercise and activity at any point in life is better than never starting.
“If you don’t practice balance, you start to lose the skill,” said Ran dy Sabourin, owner of Metro Fitness in Syracuse. “As we get older, we take less risk and do things that are more conservative to protect against falling. In reality, you want to be challenging yourself in a safe way, like exercising on one foot, using a BOSU ball and doing things to safely challenge stability and balance.”
Muscle tone and cardiovascular is also important for getting up after a fall and continuing to perform activities of daily living. Sabourin encourages adults to continue to stay strong through exercising with functional movement such as squats, performing resistance exercises and cardiovascular training.
“Find something to enjoy, like stationary cycling or indoor rowing,” he said. “Your 50s and 60s is the time to put in the effort. I plug personal training, especially if you don’t have the confidence to start this one your own. Sometimes, it’s just a buddy to keep you accountable.”
Poor eating in older adults can stem from food inaccessibility, lack of ability or motivation to cook, depres sion, or medication that suppresses appetite and/or the senses of smell and taste. Nutritional deficiencies can contribute to a host of health prob lems, including mental health.

“A high-quality multi-vita min-mineral can help ensure that we are getting the RDA requirements of several important vitamins and min erals,” said Laurel Sterling, registered dietitian, nutritionist and educator with Carlson Laboratories in Canas tota. “Multis ideally should have a substantial amount of calcium, mag nesium, omega-3s, and vitamin D3 and K2 as MK-7 for men and wom en’s bone and heart health.”
She added that omega-3 fatty acids support the health of the brain, nerves vision, joints, cardiovascular health and more.
Many older adults experience digestive issues that can lead to malabsorption of nutrients. Sterling said that probiotics with a variety of strains of lactobacillus and bifido bacterium can support improved gut function and a health immune system.
“Digestive enzymes are more and more important as we age be cause our digestive enzymes tend to decrease as we age and this can po tentially lead to more GI upsets, bow el issues, and impaired digestion,” Sterling said. “Digestive enzymes can be taken on a regular basis with meals or on an as needed basis.”
She also said that vitamin D3 supports immune and cardiovascular health and overall physical and men tal health. Recent research has also underscored the importance of vita min K and minerals such as calcium and magnesium for numerous health concerns. Blood tests can determine any deficiencies and primary care providers can recommend supple mentation or dietary changes that can promote good health.
The pandemic ramped up social isolation for older adults. It has also highlighted the importance of con nectedness and good relationships for mental health.

“Older adults need to look at all dimensions of health,” said Mary Pagan, professor in the Department of Health Promotion and Wellness Management School of Education at SUNY Oswego. “The social dynamic is the biggest one. They’ve lost con nections and they need to reconnect. Social isolation is paramount to like smoking for health risk.”
Recent events also increased anx iety and stress among older adults in the community. In addition to the mental and emotional stressors of the pandemic, Pagan said that many worry about finances, among other issues.
The same barriers exist for men tal healthcare as physical healthcare, along with stigma for seeking help. Normalizing screening at primary care visits has helped reduce stigma, especially among older adults.

SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
N. Jefferson St. Pulaski, NY 13142 315-298-6101
“People need to make sure do all of their cancer screenings,” Black said. “The earlier you catch it, the more likely you are to be cured. There’s also screening for osteopo rosis and any other screenings their doctor recommends.”
Numerous community resourc es can help ensure good nutrition. Check into congregant meal sites, grab-and-go meal boxes, Meals on Wheels and other resources listed on the Oswego County Office for the Aging site, https://www.oswe gocounty.com/departments/hu man_services/office_for_the_aging or Onondaga County Office for the Aging site, http://www.ongov.net/ aging/nutrition.html.
The NY Connects program at 315-435-1400 can also offer tips on area supports.
Christopher Black, medical direc tor at Loretto in Syracuse, often sees cardiovascular disease, which can manifest in patients as major events such as heart attack and stroke, and chronic heart failure and kidney failure.

“This major burden of disability in older folks starts with prevention,” Black said. “It starts with physical activity and avoiding obesity, keep ing active, not smoking and keeping track of your cholesterol. Family history also contributes.”
He knows this all too well. While in his 30s, his father experienced car diac bypass. Black began tracking his cholesterol and keeping closer tabs on his health.
Many people feel confused when choosing a Medicare plan.
The numerous options and in dustry jargon can make plan selec tion challenging.
Fortunately, area Medicare experts can help guide those new to Medicare or those changing plans during the current open enrollment period, which ends Dec. 7.
“This is the time to do it,” said Daniel Goetzmann, insurance agent and broker with Goetzmann & Asso ciates in Syracuse. “This is the year where they should be talking with Medicare specialists and getting as much information as possible.”

Beyond the basic Medicare, the additional plans vary depending upon company and type of plan. Goetzmann recommends that clients shop around to find the plan that best fits with their health and prescription drug needs “because of the number of benefits being added this year. I’ve never seen it added to this much,” he said. “There are plans that give you a reduction of your part B premium so it’s a refund. Some are a $42 a month refund for Part B. Those plans have a $0 premium. They’d gone up $22 a month last year which is a shock to older people on fixed incomes.”
He has also seen improvements in dental, hearing and vision bene fits, along with fitness membership discounts. The competition among healthcare benefits providers has
grown so much that many have participated in open house events to educate Medicare policyholders — something that Goetzmann has not seen before.
Typically, HMOs will not cov er routine issues addressed out of network; PPOs offer some coverage outside the network. Goetzmann encourages policyholders to consider how often they travel, as some net works offer benefits outside the area for nonemergency care and some do not.
“Medicare.gov has a provider listing you can follow for doctors, listing and facilities,” he said. “Ev ery major insurance provider makes finding a provider accessible on their websites. It can be tough to call someone. You should attend a seminar and arrange a one-on-one meeting with an adviser. The cost of the Medicare plans is the same if you go direct or if you go to an adviser.”
How much people use their healthcare benefits also affects their decision. Frequent users with chronic conditions or who want to see a pro vider with every ailment will want a plan that supports that level of care.
“You’re not married to the choice forever,” said Maura O’Toole, Medi care adviser at FitzGibbons Agency, based in Oswego.
She said that sometimes, compa nies change which prescription drugs they cover or at what level they cover them. Or sometimes, policyholders’
Obtaining a driver’s license as a teenager represents a step towards autonomy and inde pendence. The inverse is also true: giving up driving as an older adult can mean more reliance on others.
In addition, it can affect health, as adults often need more medical care from their primary care provid ers and specialists as they age. Delay ing medical and dental appointments can worsen health problems. Lack of transportation can prove a barrier for timely appointments.
“It is a key indicator of inde pendence to come and go when you want to or need to,” said Sharon Brangman, chairwoman of geriatric medicine, director of the Geriatric Medicine Fellowship Program and director of the Upstate Center of

Excellence for Alzheimer’s Disease at SUNY Upstate Medical Universi ty. “We all will reach a point where driving is not a feasible activity.
Public transportation isn’t often well established in Upstate New York as compared with bigger cities. It’s not as accessible.”
She wants more options that are both affordable and accessible to old er adults. Of course, public transpor tation can help provide rides. How ever, the costs of these services can add up for people visiting a different specialist each week or completing rounds of pre-op, post-op and reha bilitative visits. Plus, there’re also trips to the grocery store, hairdresser, house of worship and social gath erings. Unfortunately, some older adults pare their trips down to the
health changes in ways that may make different coverage more appro priate.
“If things change and you’re put on a different prescription, you can look to change your plan,” O’Toole said.
Typically, that is during the open enrollment period. However, an ad viser may be able to find a reason for special election period where the pol icyholder could change companies.
“If you find someone you can trust, you can discuss this,” O’Toole said.
She also encourages current clients to reach out to her during the open enrollment period to review their plans, as the companies some times offer improved plans that could provide clients with better coverage.
medical necessities to save money.
There are some local transporta tion options for the general public, such as Centro. Its Call-a-Bus service includes special considerations for disability, such as wheelchair acces sible vehicles and assistance to the door and with packages (if request ed), but age and lack of a vehicle are not qualifying factors. Those who are ambulatory should take Centro and not Call-a-Bus.
Typically, public transportation options do not cross county lines, which can make it difficult for people living in one county who must see a specialist in another. Centro offers services among CNY counties.
“We need options for people who might need a little assistance getting in and out of a car or a building,” Brangman said. “I had a patient whose granddaughter would order her an Uber. But she had to be able to get in and out of the car. If you use a walker or need assistance you need different transportation than a ride share.”
Many senior transportation pro grams rely upon volunteers, typically newer retirees who still drive. The pandemic has decimated the num ber of volunteers, which has caused many of the programs to reduce their trips to medical appointments only. Most transportation programs for older adults require two weeks’ advance notice, as the slots fill quick
Some people are stuck on a certain company. Although brand loyalty may seem like a money-sav er, often, it is not. Some companies’ prescription plans may not cover a policyholder’s medication at the same level as another’s for example.
“Find an adviser you trust in stead of paying attention to the ads you hear on the news,” O’Toole said.
“Some people get called about plans and are unsure of what they’re sign ing for and when they get it, they’re not happy. You can find someone who does this for a living and can guide them. That’s important. The longer I’m in this business, the more horror stories I hear. There’s no charge for the services of the consul tants like myself. We get paid by the carrier if the plan is sold.”
ly. This can prove problematic for a patient whose medical appointment must be rescheduled because of an issue in the office.
Sometimes, it’s not just about the ride, but getting the errands done.
“I have patients who say they already have to plan what they want to buy because they can’t carry it all,” Brangman said. “One lives in an apartment who has a bus one time a week to the grocery store but has a cane and purse and doesn’t have the best balance. She’s OK in the store because she can lean on her cart; but can’t carry it all once she arrives home. We need solutions to help the most vulnerable among us stay connected and have their needs met. There are people who live by them selves and don’t have family. We need to meet their needs, too.”
Brangman said that starting in the pandemic, many people have turned to Instacart for grocery deliv ery for their older parents, as the app provides a convenient way to elimi nate trips to the store.
It may help to request that shop pers package items in separate bags so that seniors are not burdened with a huge box or bag full of cans. Also note to place the parcels on a bench on the porch, for example, if lifting from the floor is too challenging.
more than six mil lion people in the US live with Alzheimer’s disease and 410,000 of those live in New York. By 2050, those figures are anticipated to double, according to the Alzheimer’s Association.
Eisai and Biogen’s lecanemab, in phase 3 of its clinical trial, has been shown to slow the rate of cognitive decline caused by Alzheimer’s by 27%. The anti-amyloid monoclonal antibody drug is meant for people with mild cognitive impairment.
Cathy James is the chapter exec utive of the Alzheimer’s Association, Central New York Chapter.

“These are very, very encourag ing results in clinical trials in treating the underlying cause of Alzhei mer’s,” said James. “Currently, the medications available right now help with the symptoms of the disease. It’s very important that we’re finding and approving medications that help with the underlying cause.”
Time is not on the side of people with Alzheimer’s and their families. With Lecanemab slowing the dis ease’s progression, they will have more time.
“For people in the earliest stages, this can change the course of the dis ease in a clinically meaningful way,” said James. “Lecanemab may give
people more time at or near their full abilities to participate in daily living skills, remaining independent and making future care decisions. There are a lot of legal and financial deci sions the family and person diag nosed need to make.”
More detailed results yet forth coming will give a better indicator as to how much time patients will have near their baseline cognition while using lecanemab. It is also not yet clear as to the side effects.
Contraindications are not yet available. They are especially im portant for older adults who may be taking other medications for unrelat ed health conditions.
“The main issue is that we have not had any medications that actual ly change the course of the disease,” said Sharon Brangman, chairwoman of geriatric medicine, director of the Geriatric Medicine Fellowship Program and director of the Upstate Center of Excellence for Alzheimer’s Disease at SUNY Upstate Medical University. “The current medications treat the symptoms but don’t delay the progression of the disease.”
Although not cures, medica tions such as lecanemab are part of a group of drugs under much research currently. Current medication for Alzheimer’s disease only treats
symptoms. Lecanemab works by combating the excessive accumula tion of amyloid proteins in the brain, which is believed to be the cause of Alzheimer’s.
Brangman said that while lec anemab breaks down and removes the amyloid, it may cause swelling of the brain and bleeding. However, “for most people, this doesn’t seem to be very serious,” she said. “We’re awaiting information on its safety and efficacy.”
Providers would need to look at each patient’s comorbidities and medications to assess risk.
Brangman noted that although Alzheimer’s affects each race, Blacks have double the risk and Hispanics are at 1.5 times the risk Hispanics compared with whites. Twenty-five percent of the participants in the lecanemab research were Black and Hispanic.

from previous page
For older adults who want to select their own groceries such as produce, scheduling regular de livery of all of their bulk or heavy items through a standard website can reduce the amount of items se niors need to pick up. Most of these sites offer free shipping at a certain minimum total. By paring down the shopping list, they need to carry only a bag or two each week. Most public transportation options do not provide assistance with carrying packages.
Using an online pharmacy or a brick-and-mortar pharmacy that delivers can eliminate another trip. Many health insurers cover prescrip tions filled through online pharma cies. Some traditional pharmacies that deliver will also add a few small items to the order if requested.
The Gogograndparent.com site allows older adults an easier means of obtaining groceries, takeout deliv ery and rides without relying on their adult children. Ideal for people who do not use smartphones, gogogrand parent employs phone operators to act as a concierge to connect older adults with services such as Grub hub, Lyft, Uber and Instacart. After signing up, all users need to do is call and ask for what they want from a live operator. Updates on the request
are texted to the user’s emergency contact such as “Delores has been picked up by Lyft” and “Delores has arrived at her destination.”
Many senior center programs provide discounted transportation for older adults to go to the senior center for socializing. That often includes a hot meal.
It may also help to contact a house of worship. Some of these provide a ministry of free or low-cost transportation to appointments and other places. Neighbors and friends may be willing to help as well.
The senior transportation options in the area include:
www.oswegocounty.com/ departments/human_services/ office_for_the_aging/transporta tion.php
www.ongov.net/nycon nects/documents/NewYorkCon nectsResourceGuide.pdf
For more help, call New York Connects at 315-349-8697 (Os wego County) or (315) 435-1400 (Onondaga County).
“Most pharmaceutical companies have not made efforts to reach all members of our community and all age groups,” Brangman said.
She added that in April, the FDA began requiring pharmaceutical researchers to submit a recruiting
program that demonstrated recruit ment across racial groups to better ensure solid representation.
After FDA approval, health insurance coverage for the new drug depends upon whether Medicare and Medicaid Services provide coverage. Most health insurance companies follow their lead. The only other anti-amyloid treatment, Aduhelm, would have cost $30,000 per month out-of-pocket. In a similar class as lecanemab, Aduhelm was also an infusion drug, but was not approved by the FDA.
“Alzheimer’s is a very complex disease,” Brangman said. “Some people may enter it through different pathways. If you enter through the amyloid pathway, this may help. We have to address all the different piec es here. I wouldn’t be surprised that we’ll have to look at each person’s profile and come up with a cocktail of drugs beneficial for them.”
Support and information from the Alzheimer’s Association are available for free anytime, day or night for individuals with Alzhei mer’s disease and their caregivers at 800-272-3900.
Does retiring from work mean retirement from working out? It may seem that way for people whose fitness activities linked to their employment. Once they are no longer in a workaday routine, it’s easy to let fitness slide.
For example, perhaps they took a morning run before leaving for work. Or maybe they walked with a group of coworkers on their lunch break. Perhaps the employer offered a fitness center, discount on a gym membership or their health insurance benefits included a gym membership reimbursement.
When fitness endeavors closely align with employment, it takes plan ning to stay fit as a retiree.
“Start exercise first thing in the morning,” said Jill Murphy, certi fied personal trainer and co-owner of Mission Fitness in East Syracuse. “As the day goes on, most of us lose motivation for exercise. Doing it first thing in the morning will eliminate that challenge.”
Many people view exercise as only gym-related because they have limited time to cram in a hard, fast workout. Retirement eliminates those time restrictions and “workouts” can mean engaging in enjoyable physical activities.
Murphy encourages retirees to find activities they like doing so they will perform the movement longer and will engage in it more frequently.
“Do you prefer going to the gym
and working out in an environment with others?” she asked. “Do you prefer more of a class environment? Do you like to walk, swim, or ride a bike? It’s important to like what you are doing, in order to sustain the activity.”
“A body in motion stays in mo tion. Keep yourself active so you can remain active and independent,” she added.
Workplace-oriented workouts of tentimes involve others. But retiring pares down the social circle. Estab lishing a new social circle around activity can help people meet those fitness goals. Joining a fitness group or class can also help keep retirees connected and accountable. Many fitness organizations offer lower rates for people 65-plus and provide regi mens that can accommodate people with limitations from past injuries.
There is no reason a bum knee or painful shoulder should eliminate activity. Community based walking clubs, hiking groups or other ac tivity-based groups can help keep retirees moving.

Mary Pagan, professor in the Department of Health Promotion and Wellness Management School of Education at SUNY Oswego, leads a “Fit for the Next Fifty” group during the summer at Onondaga Lake Park. She said that the camaraderie helps members want to return. Howev er, their main motivation is to stay healthy enough to enjoy their retire
ment and stay independent in their own home.
“They also want to do it for men tal health now,” Pagan said. “That went down significantly during COVID-19.”
She also encourages older adults to try a yoga class or join a gym or the YMCA.
“Make sure you do something every day that involves movement,” she said. “Understand that we are going to wake up with aches and pains. You can give into them or continue to move. If you don’t move, it will actually make it worse.”
Pagan encourages older adults to use more resistance training such as body weight exercises, especially as they lose muscle as they age. Build ing more muscle reduces the risk of chronic health conditions and falls and improves the chances of being able to carry out activities of daily living well into old age.
Like Pagan, Randy Sabourin, owner of Metro Fitness in Syracuse, encourages retirees to join a club or take fitness-oriented lessons to stay accountable and consistent. Going it alone often results in engaging in activity that is not intense enough and offers minimal results. Going too intense can lead to quitting or, worse, injuries.
“A lot of people are playing pickleball,” Sabourin said. “There are skeet clubs, cross-country skiing clubs and so many things.”
He views retirement as a chance to get active with one’s family.
“It’s a great opportunity to strengthen the relationship with your spouse,” he said. “If you’re both retired, you should do things togeth er. Sign up for Cure de Cure and train together all winter. Join with in your family and your friends. Try to
Mary Pagan leads a senior’s class in broomstick ballet. A professor in the department of health promotion and wellness management School of Education at SUNY Oswego, Pagan leads a “Fit for the Next Fifty” group during the summer at Onondaga Lake Park.

get them to commit. If you’ve been physically active, it’s time to put that to practical use. You may not have been able to take time off from work to climb peaks in the Adirondacks. Get active with your grandkids.”
shortage has forced Oswego County Hospice to discontinue operation. The county program ceased as of Nov. 1.
However, the Friends of Oswego County Hospice, a nonprofit that maintains the county hospice pro gram, is scrambling to support hos pice patients — with new partners.
“We are not closing, in spite of what may happen to the county program,” Elena Twiss, executive director, FOCH, said. “At the end of [October] it will be technically closed. But we will still have bereavement cases open. So they will be taking care of their patients or families, I want to say, until December.”
FOCH is separate from county government.
“We are still up and running. We have gone through some changes just because it was always our mission to
support the Oswego County hos pice program. With them closing, of course, the need for hospice doesn’t go away. So Hospice of CNY in the Finger Lakes will be coming in to serve our patients. Also helping is Hospice of Jefferson County, which will take patients on a case by case basis,” she said.
“I think there will be another hospice agency coming in later as well for the east side of our county.”
It’s going to take a team effort to make sure everyone is still covered and receive the care that they need, Twiss added.
The Friends of Oswego Coun ty Hospice is dedicated to helping enhance the time that Oswego County patients and their families have together by providing financial assistance and non-medical support, she emphasized.
“We, as a separate, independent, nonprofit organization, will contin ue to operate and assist patients in Oswego County through whatever organizations are providing ser vices,” she said.
“What we’re going to do is con tinue on with what we have been do ing — but just do it alongside these other agencies,” she explained. “We have been meeting with them and co ordinating on kind of where we can fit in with what they are doing.”
What FOCH has always done is provide, the non-medical aspect of things. So if a patient or a family needs some extra support, maybe it’s a specific personal care item or whatever, they have helped.
Twiss wasn’t sure of the exact number of patients left in Oswego County at the end of October. “But I think whoever is left will switch over to one of the other hospice agencies,” she added.
“We’re there to, I guess you could say, provide extra comforting type items. Our mission may be modified, but our goal is still the same: to support and assist hospice patients in our county,” she said.
“It’s a very new thing. We are still ironing out all of the details on how we will be able to fit in.”
For additional information on FOCH, visit www.friendsofhospice. org, or call 315-343-5223.





Can

There’s
If your husband uses a smartphone
tablet, two of my favorite app-based hearing tests are the hearWHO app created by the World Health Organization, and the Mimi

apps are free
use and are available through the



As winter approaches, along with the icy conditions, it is crucial to practice fall prevention.
Falls can happen at any age, but for seniors, there is an increased risk — and falls can be especially dangerous.
Luckily, there are lots of ways we can try to avoid falls. In my 16 years of experience as a physical therapist at PACE CNY, I have worked with my team to help many participants practice fall prevention.
In the wintertime, it is important to be aware of upcoming storms and plan ahead. We encourage participants to avoid going out when it is icy or snowing. However, if you do go out, here are a few tips to avoid potential falls:
• Take your time Rushing increases the potential for falls.
• Wear proper footwear. Buy shoes or boots with rough-textured, anti-slip soles to provide a good grip in rough conditions.
• Create a safety plan. Have a plan for snow and ice removal. Tell a loved one, neighbor or friend when you are leaving and where you are going. If possible, have someone walk with you to ensure you don’t fall.
Although winter is a high-risk time for falls, older adults are at an increased risk of falling year-round. That’s why we practice fall prevention every season. Here are some key strategies:
• Assess Your Home for Risk Factors. At PACE CNY, we conduct home
assessments for participants to make recommendations and look for potential fall hazards. Some key things we look for include unnecessary clutter or trip hazards, such as throw rugs. These should be removed to provide ample walking space with room for any assistive devices. It is also important to have proper lighting throughout the home.
• Stay Moving. Staying active promotes strength, mobility and balance. At PACE, we offer fun programs to stay active, including tai chi, Wii bowling, walking groups and more.
• Physical and occupational therapy This can help evaluate your situation and develop a personalized treatment plan for strength, improved mobility and balance.
If you want to create a comprehensive plan for fall prevention, consider learning more about PACE CNY, where we take a team approach to fall prevention.
Trisha Wameling holds a doctorate in physical therapy and works as a physical therapist at PACE CNY. For more information,visit pacecny.org.


you are eligible at age 65, your initial enrollment period (IEP):
• Begins three months before your 65th birthday.
• Includes the month of your 65th birthday.
• Ends three months after your 65th birthday.
If you are automatically enrolled in Medicare Part B or if you sign up during the first three months of your IEP, your coverage will start the month you’re first eligible. If you sign up the month you turn 65, your coverage will start the first day of the following month. This won’t change with the new rule.
Starting Jan. 1, 2023, your Medicare Part B coverage starts the first
Q.: When a person who has worked and paid Social Security taxes dies, are benefits payable on that person’s record?
A.: Social Security survivors benefits can be paid to:






• A widow or widower—unreduced benefits at full retirement age, or reduced benefits as early as age 60.
• A disabled widow or widower—as early as age 50.
• A widow or widower at any age if he or she takes care of the deceased’s child who is under age 16 or disabled, and receiving Social Security benefits.
• Unmarried children under 18 or up to age 19 if they are attending high school full time. Under certain circumstances, benefits can be paid to stepchildren, grandchildren, or adopted children.
• Children at any age who were disabled before age 22 and remain disabled.
• Dependent parents age 62 or older.
Even if you are divorced, you still may qualify for survivors benefits. For more information, go to www.ssa.gov.
Q.: I plan to retire soon. When are Social Security benefits paid?
A.: Social Security benefits are paid each month. Generally, new retirees receive their benefits on either the second, third or fourth Wednesday of each month, depending on the day in the month the retiree was born. If you receive benefits as a spouse, your benefit payment date will be determined by your spouse’s birth date.
day of the month after you sign up if you sign up during the last three months of your IEP.
Before this change, if you signed up during the last three months of your IEP, your Medicare Part B coverage started two to three months after you enrolled.
If you don’t sign up for Medicare Part B during your IEP, you have another chance each year during the general enrollment period (GEP). The GEP lasts from Jan. 1 through March 31. Starting Jan. 1, 2023, your coverage starts the first day of the month after you sign up.
You can learn more about these updates on our Medicare webpage at www.ssa.gov/medicare and our Medicare publication at www.ssa. gov/pubs/EN-05-10043.pdf.
Please pass this information along to someone who may need it.
Here’s a chart showing how your monthly payment date is determined:
Day of

For a calendar showing actual payment dates, see the Schedule of Social Security Benefit Payments at www.ssa.gov/pubs.
Q.: Will my Social Security disability benefit increase if my condition gets worse or I develop additional health problems?
A.: No. We do not base your Social Security benefit amount on the severity of your disability. The amount you are paid is based on your average lifetime earnings before your disability began. If you go back to work after getting disability benefits, you may be able to get a higher benefit based on those earnings. In addition, we have incentives that allow you to work temporarily without losing your disability benefits. For more information about disability benefits, read our publications “Disability Benefits and Working While Disabled — How We Can Help.” Both are available online at www.ssa. gov/pubs.

Nascentia Health recently announced that registered nurse An
than 10 registered nurses and 120 home health aides.
MacDonald
drea MacDonald, the organization’s clinical operations manager, was named the winner of the 2022 Joan Anne McHugh Award for Leadership in LTSS (long-term services and supports) Nursing.
The award is given by LeadingAge, a national organization comprising more than 5,000 aging services nonprofits. The award is given annually to one nurse leader in the United States who “creates a supportive and engaged workplace environment by displaying excellent leadership skills while managing nursing and frontline staff.”
The award was given in person in October at LeadingAge’s Annual Meeting and EXPO in Denver. Along with the award, MacDonald received $1,000 toward leadership training of her choice.
MacDonald has more than 40 years of experience in the nursing field and has been with Nascentia Health for the past seven years. She oversees the organization’s licensed home care services agency (LHCSA), which provides certified home health aides to care for patients across Central New York.
In that role, she manages more

Chiropractor Kori Birchenough has joined the Family Chiropractic Office in Fulton.

“We are pleased to welcome Dr. Birchenough to our practice,” chiropractor Brett Tallents, owner of the practice, said. “She’s a native Fultonian and she brings a wealth of experience with her, having also practiced in Boston and Syracuse.”
Birchenough earned a bachelor’s degree in biology from Binghamton University and earned her Doctor of Chiropractic degree from New York Chiropractic College in Seneca Falls. She is continuing her education and working toward becoming a certified chiropractic sports practitioner. She practiced for three years in Boston and several years in Syracuse. She, her husband and three daughters live in Fulton.
The practice was founded in 1987 and is accepting new patients.
According to a company press release, MacDonald is a hands-on leader who is always focused on including her team in the decision-making process. Her team says that she is a compassionate leader whose unique blend of strength and empathy is the perfect fit for her role
MacDonald received her bachelor’s degree in nursing from Hartwick College in Oneonta. She resides in Auburn.
St. Joseph’s Health has an Green
nounced the return of physician G. Randall Green to its cardiac surgery team. Green was with St. Joseph’s Health for 12 years, from 2005-2017.
“I’m rejoining St. Joseph’s because the cardiac surgery and cardiology teams are committed to the highest quality of care, and we’ve accomplished some incredible outcomes together in the past,” Green said. “The last five years helped me recognize just how incredibly rewarding it was to be part of St. Joseph’s and among the great people there.”
“We are pleased to welcome Dr. Green back to our award-winning cardiac surgery program for which he was a major contributor over the years,” said physician Philip Falcone, chief clinical officer. “The clinical
excellence of our program was built and sustained by a group of excellent heart surgeons, including Dr. Green, making it one of the best in the country.”
Green performed hundreds of surgeries a year while at St. Joseph’s Health and was one of six heart surgeons in the state and the only one in Central New York with a risk-adjusted patient death rate for open heart and valve surgery much lower than the state average.
“Our cardiovascular institute, from cardiology to vascular services, delivers superior outcomes and consistently exceeds national quality benchmarks,” said Falcone. “Dr. Green’s return to our team of esteemed surgeons will only strengthen the high level of safe care our heart patients have come to expect from us.”
“I’m excited to get home to St. Joe’s to rejoin my colleagues and the tradition of cardiac excellence for which we are known — and the camaraderie of working with such a high performing team,” said Dr. Green.
Green earned his medical degree at Northwestern University, an MBA from Cornell University, a law degree from Syracuse University and a bachelor’s degree from Le Moyne College.

Excellus BlueCross BlueShield has been recognized by Forbes as one of the best employers in New York state.
In New York state, Excellus BCBS was ranked 19th overall.
Excellus BCBS also finished as the:
• Highest ranked company head-
quartered in the Rochester region
• Highest ranked insurance company in the state.
“We’re proud to be recognized as
a great place to work,” said President and CEO Jim Reed.
“As a large Upstate New York employer, we’re committed to engaging and supporting our employees through our strong mission, inclusive culture, flexible work environment and comprehensive employee benefits.
Reed
“Last year, we also raised the minimum wage for all employees from $15 to $18 an hour given this commitment to our employees,” he added.
Forbes, and its market research partner Statista, surveyed 70,000 individuals nationwide who worked for companies with at least 500 employees. Forbes divided its list into 51 rankings — one for each of the 50 states and the District of Columbia.
Surveys were conducted anonymously and considered various aspects of the employee experience, including working conditions, salary, potential for growth, and diversity.
Access the full list of rankings at Forbes.com.
Excellus BCBS employs more than 4,000 individuals across 39 counties of Upstate New York.

St. Joseph’s Health recently
welcomed physician SaraAnn Fox to St. Joseph’s Physicians Primary Care.
Fox
“I am both honored and thrilled to be practicing in my hometown of Camillus, a place I love calling home,” said Fox.
“I will be providing full spectrum family medicine care, meaning delivering babies to end-of-life care with everything in between.”
Fox is a board-certified family physician. She completed her residency at St. Joseph’s Health and will continue to provide care to St. Joseph’s Health patients as a primary care physician and a faculty physician for the St. Joseph’s Family Medicine Residency Program.
Fox earned her Doctor of Medicine from SUNY Upstate Medical University and her Bachelor of Science in bio-medical sciences from University at Buffalo. She also has a minor in pharmacology and toxicology from University at Buffalo.
The American Heart Association and American Medical Association bestowed Gold Plus-level recognition as part of the Target: BP initiative onto St. Joseph’s Health, for its commitment to improving blood pressure (BP) control rates. The Gold Plus award recognizes practices that demonstrate a commitment to measurement accuracy and in which high blood pressure is controlled in 70% or more of the affected adult patients.

High blood pressure, or hypertension, is a leading risk factor for heart attacks, strokes and preventable death in the U.S. There are 121.5 million U.S. adults living with hypertension. The is nearly half of all adults in the country.
“Addressing blood pressure management is key for better cardiovascular health — and critical today, when heart disease and stroke continue to be leading causes of death for adults in the U.S.,” said Russell Silverman, cardiologist at St. Joseph’s Health. “High blood pressure is a leading risk factor of heart disease and stroke that can often be prevented if diagnosed early and managed effectively.”
Target: BP is a national collaboration between the American Heart Association and American Medical Association aimed at reducing the number of adults in the U.S. who suffer from heart attacks and strokes each year by urging physician practices, health systems and patients to prioritize BP control. The initiative aims to help health care organizations improve blood pressure control rates using evidence-based protocols and recognizes St. Joseph’s commitment to improving hypertension control.
“By committing to helping more people in Central New York control their blood pressure and reduce their risks for future heart disease and stroke, St. Joseph’s Health is taking a key step to helping more people live longer, healthier lives,” said physician Howard Haft, volunteer expert for the AHA and executive director of the Maryland Primary Care Program, in Baltimore. “St. Joseph’s participation in the Target: BP initiative shows its dedication to turning clinical guidelines into lifelines for patients and their families.”
Board-certified family nurse practitioner Robert Beaumont recently joined the center for cardiology at Oswego Health. Beaumont is now part of the 103 physicians and advanced practice providers employed by Oswego Health and the 270 providers on the medical staff representing multiple specialty services across the community.
Beaumont earned his master’s degree in nursing in 2015 from SUNY

Upstate Medical University and his Bachelor of Science with a major in nursing in 2011 from Keuka College.
Beaumont has over 20 years of
experience he will bring to the local community, including all aspects of emergency care. He served as a family nurse practitioner for Auburn Community Medical Services in an urgent care setting, CNY Spine and Pain Medicine in Liverpool and NY Spine and Wellness Center in North Syracuse.

Beaumont








The Centers for Medicare and Medicaid Services (CMS) announced its 2023 quality ratings. Excellus BlueCross BlueShield again achieved some of the highest ratings in the state and the nation for quality performance in clinical care and outstanding service to its Medicare members.

CMS awarded Excellus BCBS’s Medicare Advantage HMO plans a 5-star rating. This is the second year in a row Excellus BCBS has received the highest rating possible from Medicare. For the seventh consecutive year Excellus BCBS’s Medicare Part D prescription drug plan received a 5-star rating.
Additionally, the health plan’s Medicare PPO plans earned 4 stars.
For more than a decade Excellus BCBS Medicare plans have consistently received above average quality ratings (4 stars or higher).
“Our ratings are a testament to our health plan’s commitment to the health and experience of our Medicare members,” said Sharon Palmiter, vice president for population health strategic programs at Excellus BCBS.


Star ratings measure a variety of health benchmarks, including how a Medicare member’s chronic conditions such as diabetes and high blood pressure are being managed; whether Medicare members are receiving their preventive screenings and vaccines; and whether the plan is teaching members about correctly taking their medications as prescribed. Member satisfaction and experience with the health plan and its providers are also important measures in the overall quality ratings.
“No health plan can reach this level of quality care without a real commitment to partnering with local health care providers,” said physician Stephen Cohen, senior vice president and corporate medical director for Excellus BCBS. “Working together, especially through the ongoing challenges brought on by the pandemic, our providers delivered quality care to our Medicare members. These ratings reflect our passion and commitment to help people in our communities live healthier and more secure lives through access to high-quality, affordable health care.”