Progenitor cells offer great hope for heart failure patients
The 5D Heart Patch Project, led by Prof Kenneth Chien, has identified human ventricular progenitor (HVP) cells that can create self-assembling heart grafts in vivo. The research has the potential to offer hope to millions of people suffering from heart failure.



The 5D Heart Patch Project forms a vital step in a scientific journey that could be on the cusp of something extraordinary, with the goal of generating a fully functioning heart graft patch in vivo, in humans. Enabled with the backing of an ERC grant and with the support and involvement of Swedish pharma, AstraZeneca, and the biotech SmartCella, the ground-breaking project has profound implications to potentially provide a viable treatment for the millions of people who suffer from heart weaknesses, heart failure and damaged hearts after heart attacks.
The World Health Organisation (WHO) has stated that cardiovascular diseases are the leading cause of death in the world, responsible for the death of an estimated 17.9 million people every year, which equates to around 32% of all deaths worldwide.
“Heart failure is a progressive, chronic disease. There are drugs that work, primarily symptomatically, but nothing that stops the fundamental process of heart failure,” said Kenneth Chien, Professor of Cardiovascular Research at Karolinska Institute, and cofounder of Moderna.
“It’s the number one cause of morbidity and mortality as a single entity and is growing exponentially. The drivers are diabetes and hypertension and it’s a disease of the elderly although it can affect anyone of any age, including neonates if they have a genetic abnormality. This is one of the
The search for heart cells

The project is the latest step after twenty years of diligent searching for a specific type of progenitor cell for the heart.
What we have done is identify a cell, a kind of ‘master ventricular progenitor’ that makes only one type of cardiac muscle, but also can make its own matrix, trigger the formation of blood vessels following transplantation, migrate to the site of heart injury, prevent fibrosis, and then go on to expand to form huge grafts of functioning cardiac muscle.
single largest unmet clinical needs in all of medicine. For end-stage heart failure, there is no cure other than heart transplantation and there is a limitation in the number of available donors. Finding ways to rebuild heart muscle in heart failure is one of the holy grails in regenerative medicine, specifically regenerative cardiology and in medicine in general.”
“We want contracting muscle cells and it has to be a specific type because there are many different types of heart muscle cells and each of the heart muscle cells has a different electrical signature. All the heart cells need to beat in synchrony, to beat ‘to a single drummer’ if you will – that’s your pacemaker. What if you have a rogue cell and it doesn’t listen to your pacemaker? You’re going to have electrical confusion and you are going to have an arrhythmia that could be life-threatening,” explained Professor Chien.
Arguably, the first milestones in this scientific quest were based on studies between 2005-2009 in a mouse, where a marker of master heart progenitors, which could make any type of heart cell, was identified. Subsequently, a progenitor cell was identified in the mouse heart that would make only ventricular muscle, the main type of muscle responsible for propelling blood into the circulation. After a search spanning over a decade, the Chien lab at Karolinska Institutet managed to identify a similar cell from human embryonic stem cells, that would only make the right type of contracting muscle cell and nothing else. The search for human ventricular progenitors or HVPs was over, but the work toward developing human cell therapies for regenerating healthy heart muscle was just beginning.

“What we have done is identify a cell, a kind of ‘master ventricular progenitor’ that makes only one type of cardiac muscle, but also can make its own matrix, trigger the formation of blood vessels following transplantation, migrate to the site of heart injury, prevent fibrosis, and then go on to expand to form huge grafts of functioning cardiac muscle. When you put this cell anywhere; in a dish, in a mouse heart, in a pig heart – and this has all been done – you make a chunk of human ventricular muscle, and it does it all on its own, sort of a ‘self-assembly’ process that is a natural program of the cell. When we saw this, initially in a mouse, I thought, this is a cell, after twenty years of searching, that is worthy of trying to put into the clinic.”
A treatment to replace surgery?
Such a heart patch can repair a damaged heart in just six weeks and the cells do the majority of repair intuitively. The process is less invasive than open heart surgery and requires an injection of the cells into the heart. The HVPs appear to be incredibly adaptive and focused in carrying out their ‘pre-programmed’ task.
The research team were encouraged by the cell’s ability to generate contracting ventricular heart tissue in so many circumstances and with just one cell it was possible to make billions more. In one experiment they found when the cells were introduced to a mouse kidney they made a beating, moving, heart muscle patch
on the kidney despite the difference in the organ. It was the same result, putting human heart progenitors from embryonic stem cells in slices of a dead monkey’s heart in a petri dish. The human progenitors took over to build a human patch on top of the dead monkey’s heart tissue and the tissue started beating.
The HVPs apparently navigate many of the challenges that present themselves with cell therapy for hearts. A major problem with implanting heart cells is when they already have a beat. This is because the heart has to maintain a consistent rhythm and a clash of rhythms in beating cells put together, can be dangerous or fatal.
5D HEART PATCH
A Functional, Mature In vivo Human Ventricular Muscle Patch for Cardiomyopathy
Project Objectives
The discovery and development of human ventricular progenitors that form large, functional heartgraft-patches in injured pig hearts could lead to clinical studies within a few years, offering new hope to patients waiting for a heart transplant.
Project Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under ERC AdG grant agreement No 743225.

Swedish Research Council Distinguished Professor Grant Dnr 541-2013-8351, Astra Zeneca research collaboration agreement Dnr 4-2539/2021.

Contact Details
Kenneth R. Chien MD PhD

Distinguished Professor of Swedish Research Council
Department of Cell and Molecular Biology
Karolinska Institutet

T: +46 70-676 6365
E: kenneth.chien@ki.se
W: ki.se
W: https://ki.se/en/cmb/kenneth-r-chiens-group : linkedin.com/in/kenneth-chien
“The beauty of these progenitors is that they are not beating when we put them in and what we found before was that most arrhythmias occur when you put the cells in, so if the cells are already beating, they are beating to their own ‘drummer’, but when we put our cells in there, they are not beating and they have a chance to get ‘trained’.”
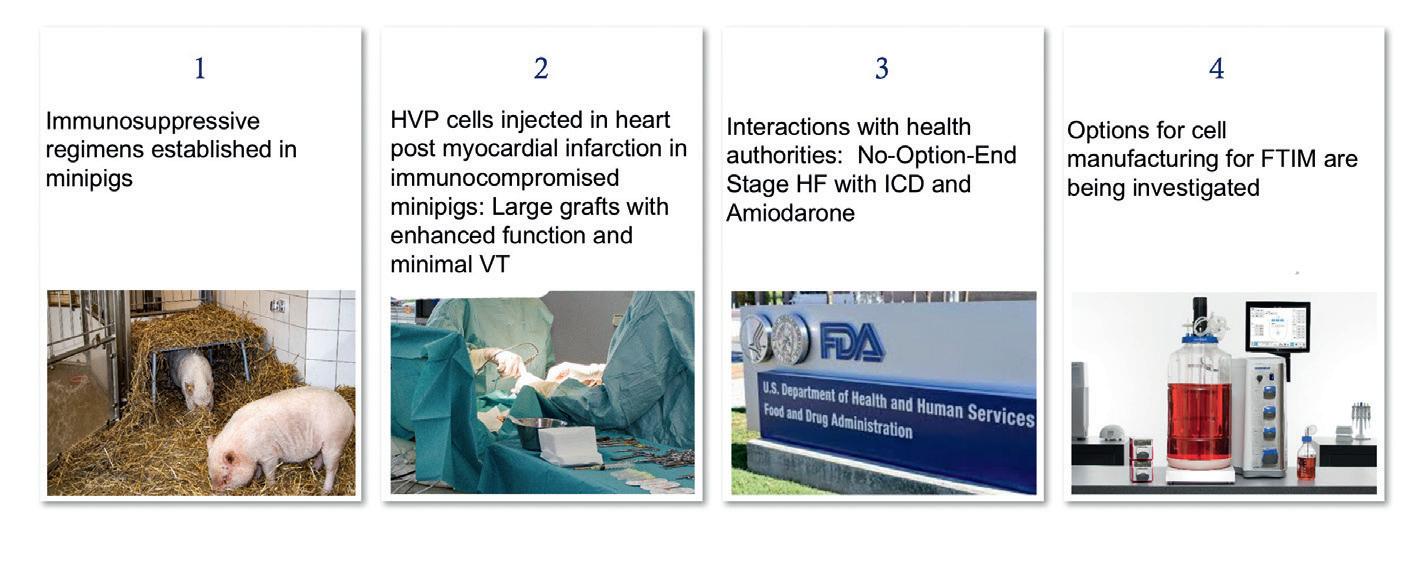
A team led by Karl-Ludwig Laugwitz, Professor of Cardiology at Technical University of Munich, (TUM) and Regina Fritsche Danielson, SVP and Head of Early CVRM, Biopharmaceuticals R&D, AZ, demonstrated that HVPs could form functional grafts in pig hearts following heart attack. In addition, the team demonstrated in a laboratory how the HVP cells migrated to actively seek out damaged regions of the heart to repair. When a heart attack occurs, as many as a billion heart muscle cells, known as cardiomyocytes, can die from the reduced blood supply, causing scar tissue which further deteriorates heart function. Normally, this could present an irreversible decline in heart function and health.

Chien said: “They migrate to the area of injury because they move, as they are progenitors, whereas cardiac muscle cells just want to beat. It was also discovered that they break up scar tissue, which was very surprising.”
The path to a new therapy
To keep his laboratory available for purely academic research, Professor Chien created a ‘bridge’ company, called SmartCella, to work with the industry partner, AstraZeneca on the path to the development of a new heart regeneration therapy, with Chien as a senior advisor.

“I started the company that makes these cells, for toxicology studies, for the pig studies, because you don’t want your lab turned into a company – I am against that. What you want to do is enable your lab to lead to the evolution of a company. And you can work interactively with the company if it is allowed, which at KI it is. And you let people who know how to make drugs do that and you help them. It’s early days still.
Dr Kenneth Chien is a Distinguished Professor of the Swedish Research Council in the Department of Cell and Molecular Biology at the Karolinska Institutet and the Co-Founder of Moderna, and is a global leader in cardiovascular biology, medicine, and biotechnology.
For hearts that are damaged by heart attacks and strokes, this could be game-changing, in terms of making a recovery. This kind of selfrepair treatment has not been possible before.
“Conveniently, they don’t keep dividing forever,” Chien continues. “They divide, and they stop growing at the right time because that is how a heart is built, so they’re programmed for true self-assembly. We are still trying to understand everything they can do.”
“We have discovered that these cells exist and the amazing properties they have. We show that it improves function after a heart attack in a pig, which is an important step. Now what we have to do is to identify an appropriate dose, decrease the risk for arrhythmias and devise an initial clinical study. At this stage, I don’t want to over-promise and I don’t want to say this is guaranteed to work. What I think is, this is worthy of further testing.”
The project has moved over into industry and a lot of work remains to be done. Despite the tests and trials that are ahead, there is a tangible sense of anticipation from those involved that a novel therapy could emerge, which has the potential to address one of the biggest health challenges of our time.

