ALSO IN THIS ISSUE
Big Data Can Provide Crucial Evidence
Multipurpose research tool offers more precise measurements to improve clinical practice.
Better outcomes and efficiency could make the digital operating room inevitable.
The Right Formula for Success
Modern approaches to IOL power calculations help surgeons get closer to target refraction.
Ophthalmic

Care in Conflict
Dr Lyubomyr Lytvynchuk outlines the unique challenges of ophthalmic care in Ukraine.
APRIL 2023 | VOLUME 28 | ISSUE 3
https://congress.escrs.org/

BINKHORST MEDAL LECTURE
Jorge L Alió MD, PhD, FEBOphthal will speak on “Corneal Regeneration: The Future of Corneal Surgery.” Dr Alió is a professor and chairman of ophthalmology at the University Miguel Hernández de Elche in Alicante, Spain, and a leader in the emerging topic of corneal regeneration. He conducted the first worldwide clinical trial for the treatment of corneal dystrophies and particularly keratoconus with autologous mesenchymal stem cells, and he has published a series of important scientific papers on this innovative type of corneal surgery.
SMART AND @CTIVE MONDAY
A new addition to the ESCRS Congress, Smart and @ctive Monday will feature “brushups” on retinal surgery, glaucoma surgery, and oculoplastics, a medical writing workshop for young ophthalmologists, an ophthalmic anaesthesia symposium, a surgical video session, and practice management sessions. A “digital track” will offer a “Continents Going Digital” symposium, symposia on automating eye surgery and the digital operating room, and talks and panel discussions about artificial intelligence in ophthalmology.

HERITAGE LECTURE
Marie-José Tassignon, MD, PhD, FEBOS-CR will speak about “The Enigma of the Anterior Interface.” Dr Tassignon is the emeritus head and chief of the department of ophthalmology of the Antwerp University Hospital and University of Antwerp. The first female president of ESCRS (2004–2005), Dr Tassignon developed bagin-the-lens cataract surgery for the paediatric population and holds 10 patents (three earned since 2019). She has been published more than 370 times in peer-reviewed journals and is the author of 27 book chapters and two full textbooks in ophthalmology.
iNOVATION DAY
Building on the success of the inaugural iNovation® Day in 2022, ESCRS is hosting the second iNovation Day on Friday, 8 September. Sessions will focus on the most urgent clinical needs and barriers to success in anterior segment care and how new technologies may address those barriers and clinical needs within the next 5–10 years. Of special interest is a new feature, “The Innovators Den: EyeCare Pioneers,” which will highlight entrepreneurs who have personally developed unique ideas to address some of the biggest unmet needs of Congress attendees.

2 EUROTIMES | APRIL 2023 Better Refractive Outcomes Andreea Dana Fișuș MD 20 Rescuing Eyes from Refractive Disasters A John Kanellopoulos MD GLAUCOMA 28 Glaucoma Treatment Options Expand Philippe Sourdille MD, Daria Lemann-Blumenthal, and Max G Ostermeier 10 Cover Cataract Surgery Goes Digital Better outcomes and efficiency could make the digital operating room inevitable. April 2023 | Vol 28 Issue 3
Publishers
Jemilah Senter
Mariska van der Veen
Mark Wheeler
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Mariska van der Veen
Contributing Editors
Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Soosan Jacob
Leigh Spielberg
Colour and Print
W&G Baird Printers
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 roo.khan@wearemci.com
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes
ISSN 1393-8983
Learn more about EuroTimes or connect with ESCRS at ESCRS.org

3 2023 APRIL | EUROTIMES 36 28 22 18 07
AI is Coming, Ready or Not

AI has the potential to significantly improve the quality of care in ophthalmology and provide better outcomes for patients. However, it is important to note that AI should be used as a tool to augment and support, rather than replace, human expertise and decision-making in ophthalmology.”

The preceding opinion was generated—word for word—by ChatGPT, the open AI online tool capable of producing detailed responses to any prompt based on what it finds online. I’m grateful and somewhat intrigued that a machine reminds us of the human element of what we do.
Telemedicine, robotics, machine learning, and artificial intelligence are profoundly changing countless elements of healthcare. Nowhere is this more true than in ophthalmology, where we are pioneering new ways to use information technology to increase safety and efficiency while improving outcomes.
We should embrace the wave of new digital tools steadily making their way into clinical practice and have the potential to greatly assist in patient care. As Howard Larkin points out in our cover article this month, we are entering the era of the digital OR. We are now seeing every step of cataract surgery begin to integrate data from patient records, preoperative imaging, AI databases, and manufacturers. How much will quality improve, and how much will it cost? This remains to be seen.
Another article in this issue features the work of Dr Flora Lum, who oversees the American Academy of Ophthalmology’s Intelligent Research in Sight (IRIS) Registry.
Her work shows the utility of large data sets for examining practice patterns, reporting quality, improving quality at individual practices, and advancing scientific discovery. Similar projects are underway using data from the European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO).
EDITORIAL BOARD
Oliver Findl
ESCRS President
Thomas Kohnen Chief Medical Editor


INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)
Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)
Cataract surgery has already felt the impact of machine learning through more accurate biometry formulas for IOL power calculation. The recently launched ESCRS IOL Calculator compares many different IOL formula calculators (see https://iolcalculator.escrs.org).
In a related article, Dr Bruce Allan at Moorfields highlights the deficit in large data sets for anterior segment surgery. Recognizing the problem, the ESCRS recently announced a research call for a collection of open-access data sets. The goal is to create richly labelled data sets comprised of imaging and clinical outcomes data for groups of 1,000 to 100,000 patients. We do need to temper our enthusiasm for AI by noting the potential risks and limitations—including concerns about cost, bias, bioethics, data protection, and patient privacy. As the chatbot reminds us, AI should be a tool to augment and support, not replace clinical decision-making.
Medical Editor
Medical Editor
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)

Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
EDITORIAL
4 EUROTIMES | APRIL 2023
Paul Rosen
José Güell
Béatrice Cochener-Lamard MD, PhD is Professor and Head of the Ophthalmology Department at Brest University Hospital, France, and former President of the ESCRS.
“
Apply
for the
John Henahan Writing Prize
What is the potential role of artificial intelligence (AI) in ophthalmology, and what are the negative implications and caveats?
Young ophthalmologists are invited to submit their answer to that question in an 800-word essay for the John Henahan Writing Prize. The author of the winning essay will receive a €500 bursary and a specially commissioned trophy, awarded during the 2023 ESCRS Congress in Vienna, Austria. The winning essay will be published in EuroTimes.

The competition is open to ESCRS members (including the free membership available to trainees) age 40 or younger on 1 January 2023. Please submit your cover letter and essay no later than 1 June to seanh@eurotimes.org.
For more information, visit https://www.escrs.org/eurotimes/john-henahan-writing-prize/
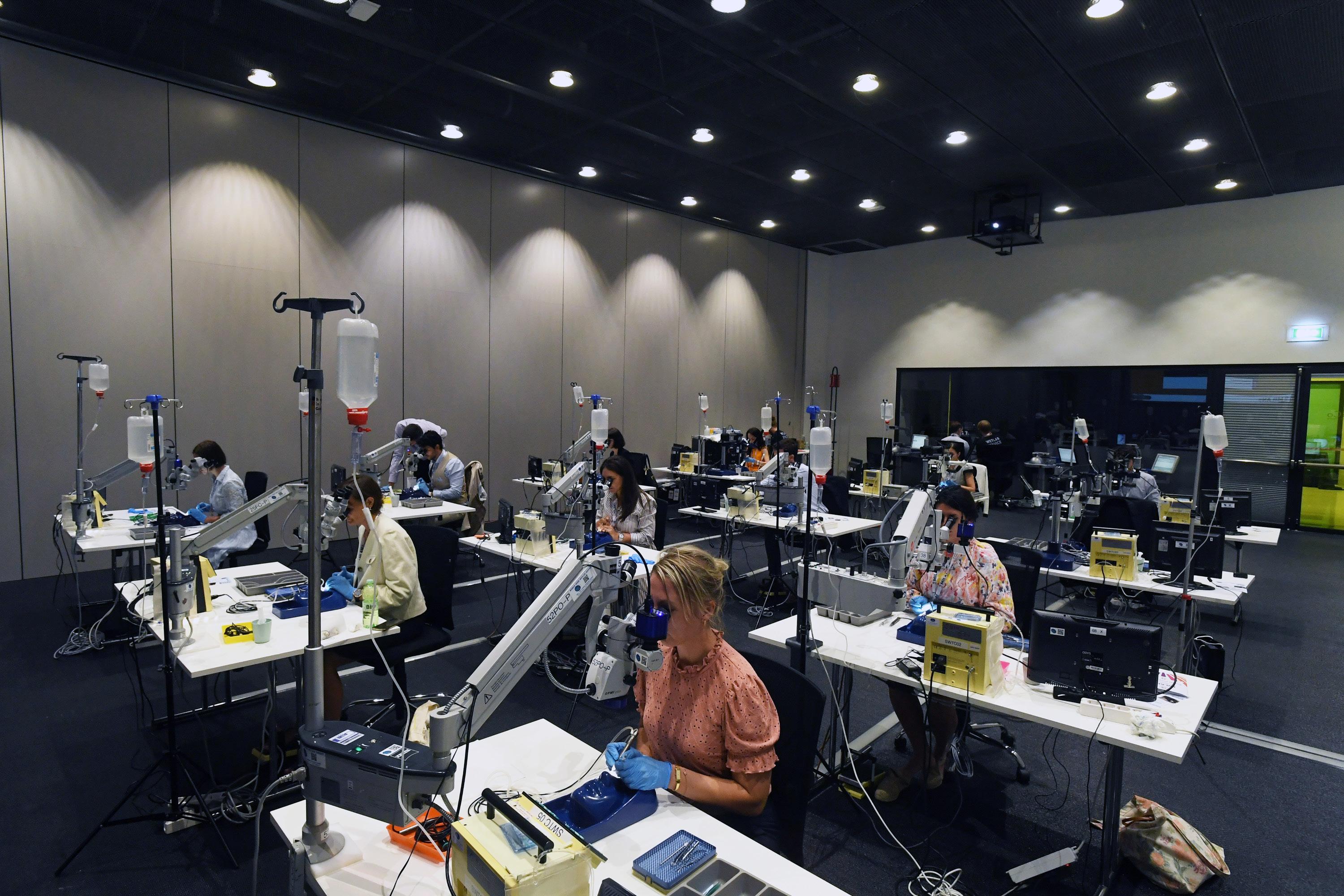
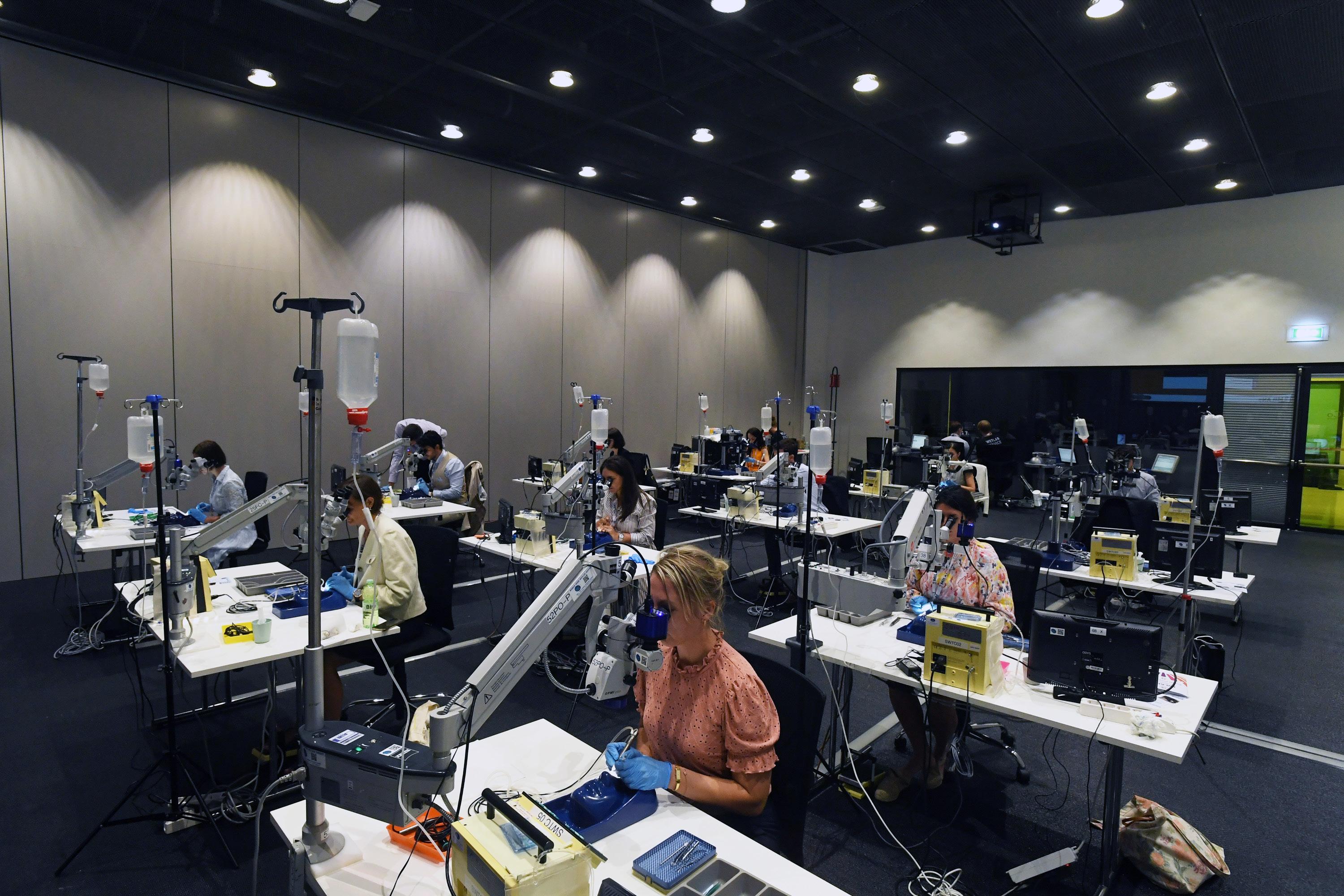
MASTERCLASSES AIM TO REPLACE ANXIETY WITH PROFICIENCY
Small pupils. White cataracts. Eyes with corneal scars and poor visibility. Pseudoexfoliation syndrome.
The challenges that can complicate cataract surgery are many, while opportunities to acquire the skills and knowledge to overcome them are few. Beginning this month, the ESCRS hopes to change that dynamic by providing an intensive “masterclass” to train qualified ophthalmologists to tackle complex cataract cases. Three other masterclasses will focus on microinvasive glaucoma surgery (MIGS) for cataract surgeons, toric IOLs, and presbyopia-correcting IOLs.
“I think quite a few surgeons out there would like to get into one of these technologies but simply have a little anxiety about some of the issues that may arise,” says Dr Oliver Findl, president of the ESCRS. “If you have a really comprehensive curriculum that extends over several months and then ends up in a face-to-face, wet lab/dry lab sort of situation, you can really be much more effective on the topic.”
The four masterclasses resulted from a two-day retreat on education the ESCRS Executive Committee held in October. Other projects inspired by the retreat, including simulators that travel through Europe to provide opportunities for simulated training and a digital education platform, are under development and will roll out in the coming months.
Masterclass Structure
Each masterclass will admit no more than 50 participants and divide students into groups of 10, each with a mentor. Experienced surgeons who are knowledgeable about the class topic will serve as mentors.
The groups will hold monthly Zoom meetings to discuss the class topic and share insights about published articles they are reading. ESCRS also plans to create a WhatsApp group so students and mentors can exchange questions that may arise in between their meetings.
The masterclasses will begin in May and have four modules, one month for each—May, June, July, and August—covering the four topics.
The masterclasses will conclude at the ESCRS Annual Congress in Vienna in September with a face-toface element immediately beforehand. The one-and-ahalf days of intensive exploration will consist of small groups solving different cases and scenarios as well as participating in dry labs and wet labs.
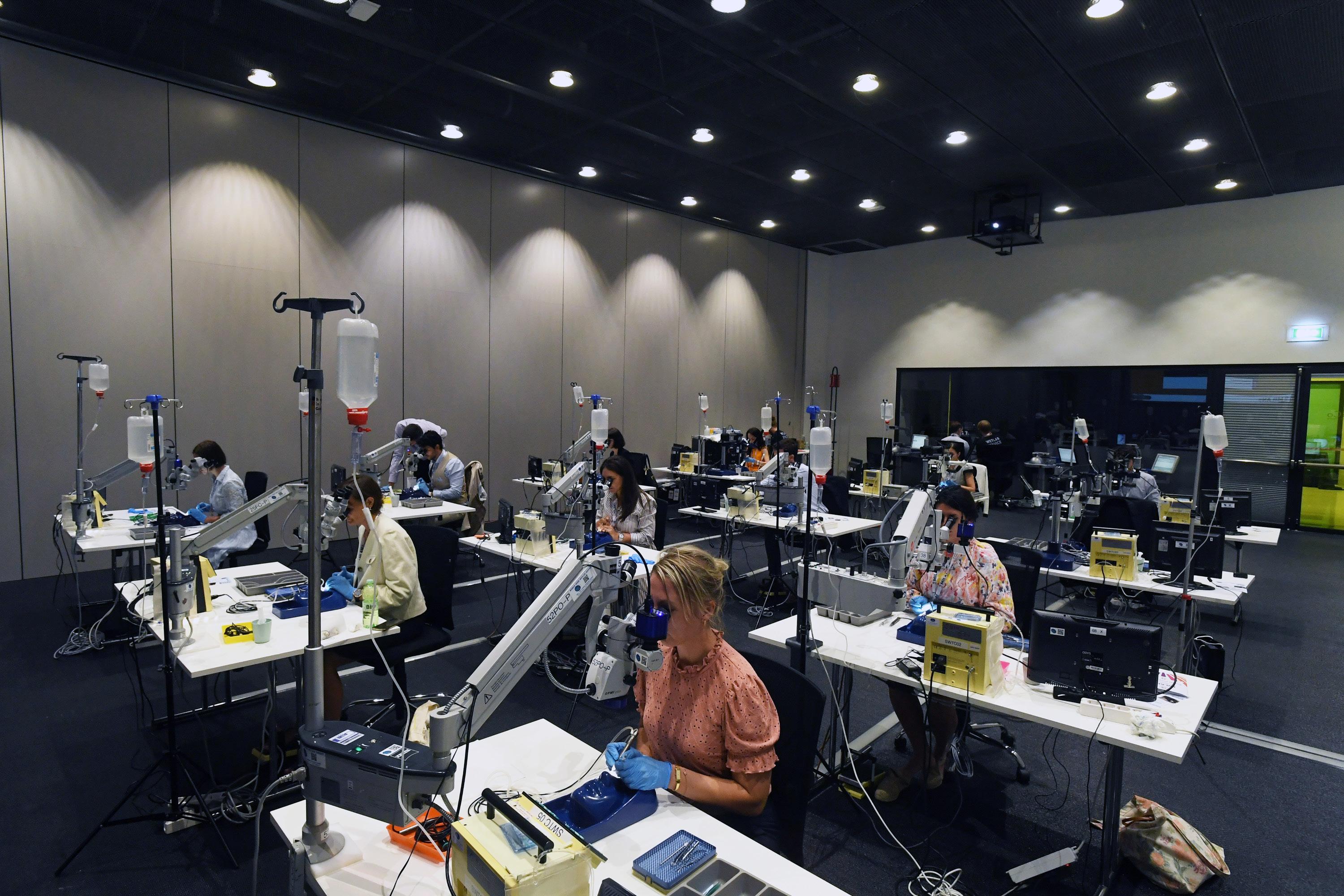
“It’s essentially self-learning at your own pace, with Zoom meetings and WhatsApp groups in be tween to enable students and mentors to have ex changes,” Dr Findl says. “Then, at the Congress, there will be intense, face-to-face small group discussions and hands-on work on cases and dry labs, wet labs, and simulator training.”
Masterclass Teachers
The masterclass tackling complex cataract cases is intended for surgeons who have performed 300–500 cataract surgeries but have shied away from cases with out-of-the-ordinary complications. It will be coordi nated by Richard Packard, a UK ophthalmologist with extensive experience teaching cataract surgeries.
Dr Findl says the masterclass covering microinvasive glaucoma surgery is intended for “the cataract sur geon who gets a patient who also has glaucoma—not the worst of all glaucomas, but one that needs maybe one, two, or three drops.” The class will be led by Ziad Khoueir, a specialist in glaucoma and cataract surgery.
Adi Abulafia, a renowned cataract surgeon in Israel, will teach the third masterclass on toric IOLs, while Ramin Khoramnia from Heidelberg University Hospital in Ger many will lead the fourth on presbyopia-correcting IOLs.
Ophthalmologists who want to enrol in the classes should expect to put their newfound knowledge and skills to work immediately.
“These are really for somebody who wants to take this step now and really wants to change their practice in the next few months,” Dr Findl says. “We don’t want people to take a course just to have another certificate on their wall, but really to be able to engage with the topic immediately afterwards. The idea is that when they go back to their practice or their hospital after the Congress, they can start using their new skills straight away.”
Prior to starting the masterclasses, students will complete a knowledge self-assessment on the chosen topic. A similar survey will be administered after the course ends, then again six months later.
“We want to find out whether they have actually changed their practice patterns—for example, whether the junior surgeon who has really not done any toric IOLs or very few is now doing 10 per month,” Dr Findl says. “We want to get feedback from the participants and see how they ranked the classes, and that will obviously be critical for us to develop the programme further.”
6 EUROTIMES | APRIL 2023
INSIDE ESCRS
2023 ESCRS Masterclasses
The ESCRS will be offering four masterclasses in 2023 on the following topics (class leaders in parentheses):
• Microinvasive Glaucoma Surgery (Ziad Khoueir)
• Toric IOLs (Adi Abulafia)
• Presbyopia-Correcting IOLs (Ramin Khoramnia)
• Complex Cataract Cases (Richard Packard)
7 2023 APRIL | EUROTIMES
It’s essentially self-learning at your own pace, with Zoom meetings and WhatsApp groups in between to enable students and mentors to have exchanges.





ESCRS This Week: 36,574 eTimes: 36,590 Weekly Emails ESCRS Website 6,129 Monthly users 17,372 Page views ESCRS Media Channels (as of January 2023) EUROTIMES | APRIL 2023 8 ESCRS AT A GLANCE
Ophthalmic Care in Conflict
Eye surgeons in Ukraine face almost insurmountable challenges.
ROIBEARD O’HEINEACHAIN REPORTS
Amidst the chaos of war, eye surgeons in Ukraine are fighting a heroic battle against blindness with depleted facilities and loss of personnel, said Dr Lyubomyr Lytvynchuk.
“As cataract surgeons, trauma surgeons, vitreoretinal surgeons, and plastic surgeons, we have to forget about quick and minimally invasive surgeries—there are multiple difficult cases [every] day.”
The many challenges for the eye departments in Ukraine include facility destruction, clinic occupation, material and equipment destruction, and the loss of medical staff and ancillary personnel such as engineers and accountants. There are also additional costs to maintain clinic security.

At the time of his presentation, 927 medical institutions had been damaged or destroyed. Some 127 medical facilities—including eye departments—were completely destroyed. The most affected medical infrastructure has been in Kyiv, Chernihiv, Donetsk, Mykolaiv, Kharkiv, and Kherson.
“In the past 10 years, many experienced surgeons in trauma moved to private departments, so at the beginning of the war, the civil medical healthcare was paralysed, and many doctors went abroad,” he explained. “Many went to western Ukraine, and normal medical service was not possible.”
The National Military Hospital in Kyiv is currently playing a major part in coordinating medical and ophthalmic healthcare in the region. A report of their experience dealing with the RUSSO-Ukrainian conflict from 2014 to 2019 provides a picture of the kind of injuries they are dealing with, Dr Lytvynchuk said.
The overall incidence of ocular trauma has been 7% to 8%. Around half of ophthalmic injuries were the result of mines and other explosives, a further 40% were due to shrapnel wounds, around 9% were due to bullet wounds, and the remaining injuries were the result of blunt trauma. Approximately two-thirds of ocular injuries were in combination with other injuries: skull and brain (31.9 %); ear, nose, and throat (15.6 %); maxillofacial (15.6%); and limb (23.7%).
Surgeons saw perforating eye injuries in 71.9% of cases and perforating eye injuries with intraocular foreign bodies
in 43.8%. The injuries were bilateral in 21.8%—resulting in unilateral blindness in 28.1% and bilateral blindness in 9.4%— and often required multistage reconstructive surgery.
“Very often, there is bilateral trauma requiring surgery on both eyes. The surgery lasts longer. Vitreoretinal surgery can last two to seven hours and includes reconstructive surgeries,” Dr Lytvynchuk reported. “We [returned] to 20-gauge vitrectomy because [of the difficulty removing] some of the foreign bodies with 23- and 25-gauge instruments.”
In many cases, he said, surgeons must combine different techniques for both the anterior and posterior segments, including temporary keratoprostheses to improve visualisation because of opacified optic media. The complex posterior segment surgery involves bimanual techniques, and very often, the eye remains in a state of post-traumatic aphakia and aniridia.
“The surgeon has to have the skills of a posterior segment surgeon and an oculoplastic surgeon,” Dr Lytvynchuk explained. “Despite our best efforts, some cases will fail. There is a high risk of intraocular hypotony with development of phthisis bulbi and secondary optic nerve atrophy.”
After the initial stages of surgery, patients are often transported to centres in countries such as Germany, Poland, the United Kingdom, Canada, and the United States. In addition, since the early days of the conflict, European ophthalmic organisations—including the ESCRS and the German Ophthalmological Society (DOG)—have provided medical supplies and equipment to Ukraine.
“In spite of the damage done to our country, we will fight on to defend it,” he concluded. “As a Ukrainian ophthalmologist living in the western part of Europe, I am obliged to fight on and assist our colleagues in Ukraine. And I would like to thank the ESCRS for the great help they have organised for us.”
UKRAINE
Dr Lytvynchuk spoke at the 40th Congress of the ESCRS in Milan.
Lyubomyr Lytvynchuk MD, PhD is based at Justus-Liebig-University, Giessen, Germany. Lyubomyr.Lytvynchuk@augen.med.uni-giessen.de
Better outcomes and efficiency could make the digital operating room inevitable.

HOWARD LARKIN REPORTS
COVER STORY 10 EUROTIMES | APRIL 2023
ore than half of the 1,500 delegates interviewed in the latest ESCRS Clinical Survey believe a more integrated digital operating room has the potential to improve efficiency and workflow. What remains to be seen is just how—and by how much—automating the OR and the entire surgical process might improve quality and efficiency.

Currently available digital integration platforms touch every step of the surgical process, from patient registration and diagnosis to surgical planning to follow-up. Data is automatically captured and forwarded to populate devices at the next step, increasing efficiency and reducing the chance of transcription errors—such as automated patient registration data updates to ensure record continuity.
Biometry and other data flow directly from measuring devices to decision support portals, automatically populating intraocular lens (IOL) power calculation formulas. Images and other data, such as corneal astigmatism and asphericity, are available at a keystroke for treatment and surgical planning, such as fine-tuning IOLs to meet specific patient anatomic and refractive needs.
The operating room, too, has seen more automation. Often checked manually, lenses are also automatically scanned for accurate documentation and to ensure an exact match to the surgical plans. Information—such as the axis of orientation for toric lenses—can be directly loaded into microscopes that project it onto the surgical image in real time.

11 2023 APRIL | EUROTIMES
Follow-up exam data supports quality improvement after surgery, such as customising personal A-constants to improve the refractive accuracy of future lens implants.
AI’s three domains
Artificial intelligence (AI) has rapidly incorporated into ophthalmology in three major domains—big data, imaging, and roboticization, said Professor Béatrice Cochener-Lamard in her Ridley Medal Lecture at the 40th Congress of the ESCRS. She has researched AI solutions in ophthalmology with partners for 20 years at LaTIM (Laboratory of Analysis and Treatment of Medical Imaging), Inserm unit 1101 (the French National Institute of Health and Medical Research), and OPHTAI. They developed patented algorithms on photos (retinophotography, OCT), videos (cataract, simulator, tear film), or multimodal approaches for automated recognition or grading of eye diseases.
“The targets are detection, follow-up, prognosis, and gain in medical efficiency,” she noted.
With several diagnostic and screening devices already approved by regulators around the world, AI has radically changed ophthalmic imaging, setting up to improve workflows as well.
One example is the PEARL-DGS Calculator, which applies both AI and linear algorithms to predict postoperative spherical equivalents for IOLs, Prof Cochener-Lamard said. Another is WeOptimeye, which uses AI at every step of the cataract workflow—including managing surgical scheduling and tailoring IOL power calculations and lens choices to specific patient needs.
What of the cost?
Cost is another challenge to implementing the digital OR. Two-thirds of ESCRS delegates surveyed see cost as a barrier, with one-quarter reporting no access to such technology. But it won’t stop the digital OR from becoming a reality, said Dr Eric D Donnenfeld.
“I think it is inevitable we will all be using digital ORs in the future, just like we are now doing digital medical records,” Dr Donnenfeld said. “First of all, it’ll be mandated by the government, and secondly, the economies of scale will make it better, and data entry will be seamless.

“When this happens, [the digital OR] will be our greatest ally for improved outcomes and fewer mistakes, so it will pay for itself. Cost is an issue today, but in the long run, this is actually going to pay for itself many times over.”
The ESCRS will have a major symposium on digitizing the operating room at the 41st Congress in Vienna in 2023.
Béatrice Cochener-Lamard MD, PhD is Professor and Head of the Ophthalmology Department in Brest University Hospital, France, member of LaTIM (Inserm 1101 – Laboratory of research in analysis and treatment of medical imaging), and dean of faculty of medicine and medical sciences at the UBO University. beatrice.cochener-lamard@chu-brest.fr
Euan S Thomson PhD is president of ophthalmic devices, head of the digital business unit, and CEO of Carl Zeiss Meditec Inc.
Sunny Virmani MS is group product manager in ophthalmology and dermatology at Google. svirmani@google.com
Eric D Donnenfeld MD is clinical professor of ophthalmology at New York University in New York City, US; trustee of Dartmouth Medical School in Hanover, New Hampshire, US; and in private practice in New York State. ericdonnenfeld@gmail.com
At Carl Zeiss Meditech, AI supports a training module that monitors and helps analyse every step of cataract surgery by comparing it with a reference video, said Dr Euan S Thomson, president of ophthalmic devices, head of the digital business unit, and the company’s CEO. Future plans for the Zeiss information platform include a database able to support AI research.
Google’s Sunny Virmani MS noted improving data quality is also critical, adding Google and other organisations are building expertise in collecting and standardising all kinds of imaging data from both the anterior and posterior segments.
However, Dr Thompson shared that one barrier to using AI applications in clinical practice is regulators will only approve them for use with data collected on the device that provided the training data set used to develop the programme—which makes it difficult to develop applications capable of using data from any source.
Prof Cochener-Lamard also identified bioethics, data protection, and distrust by clinicians who see AI as a threat to their profession. She suggested addressing this scepticism by encouraging them to think of AI as a way to help answer questions while remembering they must formulate those questions and supply answers.
12 EUROTIMES | APRIL 2023 COVER STORY
I think it is inevitable we will all be using digital ORs in the future.
Big Data Can Provide Crucial Evidence
IRIS Registry proves to be a multipurpose research tool for improving clinical practice.
The risk of developing endophthalmitis after anti-VEGF injections for age-related macular degeneration does not appear significantly greater with bevacizumab than with ranibizumab or aflibercept. We know this thanks to big data.
Academy Journey with Big Data: IRIS Registry Current Stats (July 1, 2022)
Very large clinical data sets collected from thousands of ophthalmology practices make possible not only studies of rare diseases and events but trends over time, said Dr Flora Lum, who oversees the American Academy of Ophthalmology’s Intelligent Research in Sight (IRIS®) Registry. It is useful for examin ing practice patterns, reporting and improving quality at individual practices, and advancing scientific discovery.
a rare disease for US Food and Drug Administration (FDA) treatment regulations.
The IRIS Registry helped determine whether cataract surgery is associated with a decrease in central retinal vein occlusion, Dr Lum said. “We weren’t able to find a decrease but were able to look at this with minimal cost and time.”
A study of anti-VEGF use by type of insurance, whether public or private, found significant differences, leading to additional questions—including reasons for the differences and whether they lead to differences in clinical outcomes and costs of care that may be answered, in part, by registry data, Dr Lum said.
Launched in 2014, IRIS Registry now includes electronic health record data from close to 500 million visits by more than 75 million patients in the United States, making it the largest depository of ophthalmology practice data in the world.
“We collect [data on] every patient on every disease condition, and we have a majority of ophthalmologists in the IRIS Registry,” Dr Lum said. “And we can look longitudinally because we have unique patient ID numbers and about one decade’s worth of information.”
Change over time
Because it receives electronic data directly from electronic health records used by more than 12,000 ophthalmologists, IRIS Registry can track practice trends in real time. For example, at the start of the COVID-19 pandemic in March 2020, the IRIS Registry showed a precipitous drop in patient visits by all ophthalmologists, though non-retina specialists showed a much larger drop than retina specialists.
Since it tracks such a large population, the IRIS Registry is suitable for studying rare diseases. It estimated 40,000 cases of myopic choroidal neovascularization, documenting it as
Adverse events also can be tracked. One IRIS Registry study helped characterize the incidence of uveitis associated with patients taking various checkpoint inhibitors used in cancer treatment, Dr Lum said, adding such studies can have a direct impact on clinical practice.
Another adverse event, an outbreak of infections associated with repackaged bevacizumab, led to a call to ban the practice. “In a couple of days, we were able to amass the data in the IRIS Registry, and we showed there was no difference in endophthalmitis rates across the three agents,” she said. As a result, there was no ban.
“Because we can measure more precisely, we can manage better. We can select more effective interventions based on real-world big data now,” Dr Lum concluded.
13 2023 APRIL | EUROTIMES
Dr Lum spoke at the inaugural iNovation symposium at the 40th Congress of the ESCRS in Milan.
HOWARD LARKIN REPORTS
Flora Lum MD is vice president, quality and data science at the American Academy of Ophthalmology. flum@aao.org
1 Contracted for EHR Integration o 15,799 physicians from 3,002 practices Number of patient visits o 454.00 million, representing 75.40 million pts 0 50 100 150 200 250 300 350 400 450 500 20152016201720182019202020212022 IRIS
Registry Growth in Millions of Visits and Unique Patients
CATARACT & REFRACTIVE
We can select more effective interventions based on realworld big data now.
Measuring Outcomes Using Digital Innovations
New projects will enhance ophthalmology data sets.
New digital tools have enormous potential to change the ways data collected in routine clinical care can be stored, analysed, and exploited to enhance research and improve patient outcomes, according to Dr Bruce Allan.
“By collecting data in a structured and protocol-driven manner and storing it electronically as part of routine clinical practice, the data begins to resemble that collected in clinical trials,” he said. “This presents an opportunity to use existing data for analysis—rather than spending time and money collecting new data for every research question.”
Highlighting the potential benefits of using data collected in routine clinical care, Dr Allan noted that under Article 9 of the General Data Protection Regulation (GDPR), anonymized healthcare data can be shared and used for analysis without the need for special measures for consent or Institutional Review Board (IRB) approval.
“This removes two of the biggest hurdles to accessing data—not just to track our outcomes but to perform analyses designed to improve them,” he said.

Ophthalmology, a field rich in image data, is particularly amenable to deep learning analysis. Labelling image data with diagnostic information can help train deep learning algorithms to perform classification and prediction tasks accurately. Dr Allan noted even untrained individuals, including medical students and high school students, can use code-free solutions to develop useful deep learning algorithms.
“The bottom line is you don’t need to be an expert in AI to engage with these tools and exploit the data you may have already collected in routine clinical care,” he said.
Anterior segment data lagging
Whether a novice or expert, users need access to well-ordered data sets, which Dr Allan observed is currently limited—particularly for the anterior segment.
“Nearly all of the available open-access data sets are for retina, so this is a ‘data deficit’ that needs to be addressed,” he said.
In recognition of the problem, he said the ESCRS recently announced a research call to collect open-access data sets. The goal is to create richly labelled data sets of imaging and clinical outcomes data for groups of 1,000 to 100,000 patients.
Machine learning has already made an impact in cataract surgery through the creation of more accurate biometry formulas for IOL power calculation, Dr Allan noted. The ESCRS recently launched a new tool that uses web scraping technology to allow users to see results from different IOL formula calculators in one place (see https://iolcalculator.escrs.org).
To further improve the accuracy of machine learning biometry algorithms, Dr Allan stressed the importance of collecting
good quality data, including biometry, IOL details, and refraction measurement information.
“In machine learning, the size of the data sets needed diminishes if you have good-quality information available,” he said, adding data export in a common format remains problematic for contemporary biometry devices.
“We still have some work to do to get the data from the scanners into the cloud, where it can be properly exploited,” he said.
Streamline data collection
To collect data reliably, Dr Allan said, the process needs to be automated as far as possible. In the operating theatre, he
14 EUROTIMES | APRIL 2023 CATARACT & REFRACTIVE
DERMOT MCGRATH REPORTS
The bottom line is you don’t need to be an expert in AI to engage with these tools.
suggested using barcodes on lens packs to streamline data collection and reduce the need for manual transcription. Machine learning algorithms can also, potentially, be trained to recognize steps in surgical procedures and assist with writing operating notes.

Solutions are also coming onstream to improve the quality of refraction data.
“Autorefraction is quick but not so accurate, whereas subjective refraction is the gold standard but is really slow to do and hard to integrate into high-volume practice,” he said. “However, there are new ways of [performing] refraction that [do not] rely on standard blur testing that are potentially faster, more accurate.”
Dr Allan also highlighted the importance of incorpo rating patient-reported outcome measures (PROMs) into the data collection process. For example, his primary facility, Moorfields Eye Hospital, developed a screenbased questionnaire with 11 questions to assess criteria such as emotional well-being, visual quality, comfort, and spectacle dependence.
By leveraging the wealth of data collected in routine clinical care and utilizing new analysis techniques, Dr Allan concluded, it is possible to gain insights and make improvements to benefit patients and the healthcare system as a whole.
Non Contact Tono/Pachymeter New Design Innovations that Incorporate Operator and Patient Comfort with Gentle Measurements

• Fully-automatic measurement
• Gentle voice guidance (available in 9 languages)
• Reliable tono/pachymeter
• Flexible and space-saving design
• A variety of options to meet your needs
Dr Allan presented at the 40th Congress of the ESCRS in Milan.
Bruce Allan MD, FRCS is a consultant ophthalmic surgeon at Moorfields Eye Hospital, London, UK. bruce.allan@ucl.ac.uk
www.nidek.com ET 93 x 266mm
The Right Formula for Success

Choosing a modern IOL formula in tandem with accurate preoperative biometry can increase IOL power calculation accuracy and reduce the risk of refractive surprise after surgery, according to Professor Filomena Ribeiro.
“It is possible to get 90% of our patients to within less than 0.50 D of target refraction,” she said. “For that, we need very good validation of our measurements and ensure they fit well in the range of the population. We also need to select a modern IOL formula and regularly analyse our results to improve them.”
Discussing the development of modern IOL formulas, Prof Ribeiro said the choice has evolved from outdated regression formulas to more sophisticated methods incorporating additional biometric variables, such as anterior chamber depth,
lens thickness, and white-to-white measurements, among others. These formulas increasingly embrace different optical approaches and techniques—such as exact ray-tracing and artificial intelligence—in trying to improve prediction accuracy.
“The probability of success with a more modern IOL formula such as Kane, Olsen, Barrett, or EVO is more than 80% of cases will end up within 0.50 D of target and 98% within 1.0 D,” she explained. “However, this could be even better as several publications show different results for the same formulas.”
By comparison, she noted that data from 100 cataract surgery clinics in the EUREQUO database in 2014 and 2015 showed 73% of patients within 0.5 D of target refraction and 93% within 1.0 D.
16 EUROTIMES | APRIL 2023
DERMOT MCGRATH REPORTS
Modern approaches help get closer to target refraction.
CATARACT & REFRACTIVE
90%
“If we look at the ESCRS survey of preferred lens formulas over different years, we see that up until around 2019, most surgeons were using SRK/T,” she said. “Whereas in 2021, other, more modern formulas were chosen more.”
Rather than trying to compare the advantages and drawbacks of each formula, Prof Ribeiro recommended surgeons take advantage of the ESCRS IOL calculator ( https://iolcalculator.escrs.org ), which provides results for up to seven different modern formulas—including the Barrett Universal II, Cooke K6, EVO, Hill-RBF, Hoffer QST, Kane, and Pearl GDS.
“You only need to input the data once, and with this approach, it is easy to assess the range of residual refractive
error predicted, which can be small in some cases but much larger in extreme eyes,” she said.
The key improvements in modern formulas derive from factors such as better effective lens position (ELP) estimation, correction of the keratometer (K) index error, optimization of optical biometry measurements of axial length, and empirical adjustments using linear regression and machine learning.

Although most modern formulas perform well for normal eyes, Prof Ribeiro said accuracy might be affected when performing biometry in long and short eyes and those with flat and steep corneas. For instance, a comparative study by Melles [et al.] found the Haigis formula was most affected by variations in lens thickness, while the Hoffer Q was impacted by varying anterior chamber depth. Another study showed that SRK/T was particularly sensitive to eyes with very flat or steep corneas.
Surgeons can potentially improve IOL power predictions by using second eye adjustment.
“It has been shown that second eye adjustment can provide better results if there is good symmetry between both eyes and regression factors we need to incorporate are related to the ELP estimation,” Prof Ribeiro said. “Some modern formulas like the Pearl-DGS allow us to perform this calculation directly in the online calculator.”
Industry also has a role in improving outcomes, she said, by disclosing basic information about the IOL design that is important for accurate IOL power calculation.
A recent JCRS article noted the need for more specific information concerning IOL design—including the refractive index, the central optic thickness, the anterior and posterior curvature radii, the toricity location, the spherical aberration, and haptic angulation.i
“With that data, we can really personalise the IOL power calculation with exact ray tracing and improve our outcomes even more,” she concluded.
Prof
17 2023 APRIL | EUROTIMES
Ribeiro gave this presentation as part of a recent ESCRS eConnect Webinar, available through the QR code above.
Filomena Ribeiro MD, PhD, FEBO is Head of the Department of Ophthalmology at the Hospital da Luz, Lisbon, Portugal. filomenajribeiro@gmail.com
iOlsen et al. JCRS. 2023 Feb 6. doi: 10.1097.
It is possible to get 90% of our patients to within less than 0.50 D of target refraction.
We can really personalise the
IOL
power calculation with exact ray tracing and improve our outcomes even more.
Biometry Advances Driving Better Refractive Outcomes
Improvements in the accuracy and repeatability of measurements obtained with the latest biometry devices combined with increasingly sophisticated IOL formulas have led to greatly improved refractive outcomes for cataract patients, according to Dr Andreea Dana Fișuș.
In an overview of the range of biometry devices currently available, Dr Fișuș highlighted the importance of not only removing the cataract correctly but achieving accurate postoperative refractive error.
“Precise measurement of ocular biometry is critical for determining the power of IOLs being implanted,” she emphasised. “And as a rule, the higher the generation of the IOL calculation formula, the higher the accuracy and the more ocular biometric parameters are required.”
When comparing biometry devices, she said, it is important to define what is meant by accuracy.
“When we speak of ‘accuracy,’ we are really describing the combination of two distinct concepts—trueness and precision,” Dr Fișuș explained. “The trueness of a measurement refers to the closeness between the mean of many measurements and an accepted value or standard. And precision refers to the closeness between repeated measurements—i.e.,
the repeatability and reproducibility. For a system to be as accurate as possible, it requires both precision and trueness.”
Although ultrasound biometry served as the standard in clinical practice for many years, optical biometry approaches that are faster, non-contact, and more reliable have superseded it. Methods include partial coherence interferometry (PCI), optical low-coherence reflectometry (OLCR), and sweptsource optical coherence tomography (ss-OCT). Another promising new technology is hyperparallel OCT, which can capture more than 300,000 A-scans per second for rapid, high-resolution artefact-free volume measurements of posterior and anterior segments.
Many studies have shown measurements obtained with ssOCT devices correspond well with those of PCI or OLCR devices.
“Although some of the differences in axial length, anterior chamber depth, and lens thickness parameters were statistically significant, clinically, they were insignificant,” Dr Fișuș said.
A review by Kane [et al.] in 2020 showed that all optical biometry devices surveyed delivered highly reproducible measurements, and most comparative studies showed little difference in the average measures for the biometric variables between devices.

18 EUROTIMES | APRIL 2023 CATARACT & REFRACTIVE
DERMOT MCGRATH REPORTS
“The good outcomes reported in many of these studies led to the conclusion that swept-source OCT will be the new gold standard in optical biometry technology,” she said.
Other studies have shown good agreement between the IOLMaster 700 and other ss-OCT devices, such as ANTERION (Heidelberg Engineering Ltd) and ARGOS (Alcon).
With such good repeatability in biometric measurements between different ss-OCT devices, Dr Fișuș noted clinicians may choose a device based on other criteria.
“They may look at the speed of the device, the ease with which it is used, and other features—such as if the device also measures the posterior cornea, or if it offers a view of the fovea, or whether it is compatible with an intraoperative microscope,” she said.
And while intraoperative aberrometry using a device such as the ORA (Alcon) has shown usefulness in post-refractive cases, she said these have not shown an advantage compared to routine preoperative biometry in normal eyes.
The ARGOS device also offers a promising new method to obtain axial length measurements using individual refractive indices to measure each eye segment. Dr Fișuș explained this is unlike other biometers that typically convert the optical path length to a geometric axial length measurement using a mean group refractive index.
“Studies have shown that in normal eyes, axial length measurement using this Sum-of-Segments (SOS) approach is similar or identical to conventional biometry using a mean refractive index. However, there is a difference when used in longer and shorter eyes. The segmented axial length is longer in short eyes and shorter in long eyes using this method,” she said.

Swept-source OCT may also be useful in predicting postoperative IOL tilt, said Dr Fișuș, as it offers a volumetric eye measurement.
“We can use these preoperative images to predict the tilt of the IOL postoperatively. This could be interesting for toric IOL calculations, although we do need more studies to confirm this,” she said.
Dr Fișuș added a final word of caution about using ss-OCT for biometry measurements in patients with vitreoretinal disorders undergoing cataract surgery:
“We all know that when patients with epiretinal membrane have combined surgery, the IOL power calculation is often incorrect—usually due to errors in axial length measurements. A recent study [comparing] axial length measurements obtained by ss-OCT and PCI found no statistically significant difference between them, which means there is still a risk of a myopic shift after combined surgery.”
Dr Fișuș gave this presentation as part of a recent ESCRS eConnect Webinar.
19 2023 APRIL | EUROTIMES
Andreea Dana Fișuș MD works at the Vienna Institute for Research in Ocular Surgery, Hanusch Hospital, Vienna, Austria. fisusandreea@yahoo.com
Precise measurement of ocular biometry is critical for determining the power of IOLs being implanted.
Rescuing Eyes from Refractive Disasters
Innovative solutions necessary to salvage vision in eyes with severe complications from corneal refractive surgery.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
When corneal refractive surgery goes wrong, the results can be devastating, but often remedies exist that can optimise outcomes. To illustrate the possible complications and the means to resolve them, Dr A John Kanellopoulos described a few cases referred to him over the years, and his treatment strategies.
The first case involved a 62-year-old physician who had undergone femtosecond laser-assisted cataract surgery but experienced irregular astigmatism in his right eye as a result of eccentrically placed astigmatic keratotomies. One of the incisions crossed the visual axis, causing a significant corneal irregularity. Dr Kanellopoulos treated the patient with a topographically guided LASIK procedure. Afterwards, the patient’s eye had an uncorrected visual acuity of 20/15, and with bifocal spectacles, near visual acuity of 20/20.
The second case was much more complex. It concerned a woman who underwent an unsuccessful small lenticule extraction (SMILE) procedure. Due to three incomplete passes with the femtosecond laser, the surgeon converted to refractive lenticule extraction (RELEX) with manual removal of the lenticule. The patient started with a refractive error of around -6.0 D but postoperatively had a sphere of -10.0 D and a cylinder of -2.5 D at 160 degrees in her right eye and a sphere of -8.25 D and a cylinder of -4.5 D at 160 degrees in her left eye with best corrected visual acuities of 20/100 and 20/200, respectively.
Athens Protocol
After carefully reviewing the topographic imaging, OCT pachymetry, and corneal epithelial mapping, Dr Kanellopoulos offered the patient the option of undergoing the Athens Protocol treatment. The four-step procedure occurs in a specific order: First, a topographically guided, minimal tissue removal, photorefractive keratectomy (PRK), followed by a phototherapeutic keratectomy (PTK), the application mitomycin-C 0.2% for 30 seconds, and lastly corneal cross-linking (CXL) for 15 seconds with a fluence of 6 mW/cm2. The patient also underwent a minor PRK enhancement six months later, finally achieving an uncorrected visual acuity of 20/40 and a corrected visual acuity of 20/30.
“Although not an ectasia case, in view of a normalising the corneal surface and stabilising the very thin cornea, we used the Athens Protocol with a PRK enhancement resulting in a drastic improvement in visual acuity,” Dr Kanellopoulos observed. “This is just a reminder that the Athens Protocol is a very frugal, in-tissue removal, therapeutic approach to treat irregular corneas.”
Another patient whose vision he helped improve with the protocol was a 26-year-old helicopter pilot from New York City grounded after developing post-LASIK ectasia. In this case,

the treatment not only restored corneal surface regularity but improved his vision from 20/60 to 20/15. The patient has since enlisted in the US Air Force and serves as a fighter pilot.
The last example was a patient who developed a corneal melt after undergoing hyperopic LASIK and implantation of a Teardrop (ReVision Optics) corneal inlay in the non-dominant eye. The patient was an “avid” eye rubber and returned to Dr Kanellopoulos with a melt in the inlay area with significant inflammation and corneal irregularity. Corrected visual acuity was 20/80. After removing the inlay, he chose the non-surgical option of long-term treatment with steroid and cyclosporine eyedrops to manage the severe central scar and corneal divide.
Three months of treatment later, the patient’s eye improved to UDVA 20/100 and corrected visual acuity of 20/40 with a refraction of +6.0 D and -0.5 D at 76 degrees. Five years postoperatively, the scar had subsided significantly, and uncorrected and corrected visual acuity had improved to 20/30 and 20/25, respectively, and refraction had improved to +1.75 D and -0.75 D at 125 degrees. With these outcomes, the patient discontinued treatment, and at nine years, the patient’s cornea had a near normal curvature and corrected and uncorrected visual acuity improved to 20/20.
“In this case, the cornea’s stromal and epithelial natural remodelling was able to diminish the irregularity with the help of topical medication without surgical intervention, apart from removing the inlay,” he noted.
20 EUROTIMES | APRIL 2023 CATARACT & REFRACTIVE
Dr Kanellopoulos presented his findings at the 40th Congress of the ESCRS in Milan.
A John Kanellopoulos MD is the Director, Laservision Eye Institute, Athens, Greece, and Clinical Professor, Department of Ophthalmology, NYU School of Medicine, New York, US. ajk@laservision.gr
21 2023 APRIL | EUROTIMES NOW OPEN! Applications for the Peter Barry Fellowship 2023 are The Fellowship of €60,000 will allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year. The application deadline is 2 May 2023. For more information: escrs.org/education/grants-awards/peter-barry-fellowship
Bioengineered Lenticules
SMILE-derived lenticules may provide a new form of drug delivery.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Bioengineered stromal lenticules obtained from small incision lenticule extraction (SMILE) procedures may provide a viable means of sustained drug delivery to the cornea.
A recent study suggests stromal lenticules can be efficiently decellularized and poly lactic-co-glycolic acid (PLGA) microparticles embedded with recombinant human nerve growth factor (rhNGF) incorporated into the lenticules. The study also showed the embedded lenticules released the rhNGF from the microparticles for up to one month while preserving rhNGF activity, according to Dr Mario Nubile.
“RhNGF microparticles embedded in decellularized lenticules are an efficient method to achieve a greater concentration of drug substances for an extended period in diseased corneas, paving the way for combined surgical and medical therapy,” Dr Nubile said. “Hypothetically, bioengineered lenticules could be used for every kind of eye drug substance—not only for corneal therapy but also for other ocular diseases.”
The process
The researchers obtained the lenticules from patients undergoing SMILE for -4.0 D to -6.0 D of myopia. The lenticules had a diameter between 6.0 mm and 6.3 mm and a maximum thickness ranging from 100 to 150 microns. Decellularization treatment first involved rinsing the lenticules in a phosphate buffer solution (PBS) before incubating them in a 0.1% sodium dodecyl sulphate (SDS) solution for 24 hours under 300 rpm agitation followed by three washes in PBS.
Bioengineering the lenticules required the researchers to dehydrate the tissue samples 60 degrees centigrade for two hours at room temperature, incubate them in rhNGF PLGA microparticle suspension for five hours under 200 rpm agitation, and then wash them in 0.4 ml of 0.5% sodium chloride solution.
Dr Nubile noted immunofluorescence and immunohistochemistry analysis showed the absence of cells in the lenticules as well as the presence of rhNGF microparticles within the decellularized tissue. Experiments testing the kinetic rhNGF release from the engineered lenticule showed an 80% neurotrophin release during the first 24 hours, with a massive release in the first two hours and a slow release sustained for up to 30 days.
Further investigations showed the released rhNGF preserved its activity in binding to its receptor on pheochromocytoma (PC-12) cells at 70% and 81% compared to its reference standard (0.750 ng/ml and 0.1875 ng/ml).

Dr Nubile and his associates are now conducting animal experiments with bioengineered lenticules, first testing the efficacy of rhNGF release in normal rabbit eyes, then in the eyes of a rabbit model of neurotrophic keratopathy.
Addressing an unmet need
The topical use of rhNGF has shown promising therapeutic results in managing neurotrophic keratopathy and other ocular surface diseases. This approach promotes endothelial healing and improves corneal sensitivity and overall nerve fibre regeneration. However, there is still room for improvement, particularly in bioavailability, since generally only around 5% of topically applied medication reaches its target inside the eye, Dr Nubile emphasised.
Alternative delivery approaches have also shown promising results for replacing and regenerating diseased ocular tissue. They include drug encapsulation into natural or biosynthetic micro- and nanoparticles, tissue engineering approaches based on hydrogel/collagen contact lenses, and synthetic scaffolds engineered with drugs incorporated in microparticles. But these, too, have critical disadvantages, including possible irritation from the material used, reduced transparency causing blurred vision hypoxia, and variable drug bioavailability, he cautioned.
“The development of a natural, biocompatible, non-immunogenic delivery system that ideally combines the advantages of tissue engineering and pharmaceutical approaches may allow us to obtain effective concentrations of drug molecules in the eye for a sufficient period.”
CORNEA 22 EUROTIMES | APRIL 2023
Generally only around 5% of topically applied medication reaches its target inside the eye.

Noting more than six million SMILE procedures have been performed as of 2022, SMILE-derived lenticules are biocompatible, transparent, avascular, and mechanically strong. Their discard represents an enormous waste of a valuable resource of tissue that can be reused for therapeutic applications. Apart from neurotrophic keratopathy, bioengineered lenticules could also help improve outcomes in stromal lenticule addition keratoplasty (SLAK) procedures in eyes with progressive keratoconus.

“A crucial point is proper tissue preservation. Cryopreservation represents a valid method for long-term storage that maintains lenticule vitality,” he said. “Creating a lenticule bank to collect, catalogue, process, cryopreserve, and distribute could be advantageous, safe, and feasible.”
Mario Nubile MD is based at Ophthalmology Clinic, Department of Medicine and Aging Science, “G. d’Annunzio” of Chieti-Pescara, Chieti, Italy. mario.nubile@unich.it, nubilemario@gmail.com

23 2023 APRIL | EUROTIMES
Multifunction Unit Booth 33 Meet us at the ESCRS Winter Meeting 2023 : Get to know its excellent features
6 in one: Ref, Kerato, Tono, Pachy, Topo, Dry Eye + Measurement cone interchange in just 4 seconds + Pupil and cornea ø measurement
Auto-alignment and auto-measurement
Quick refraction mode + Corrected IOP tomey.de
MR-6000
+
+
+
Dr Nubile spoke at the 40th Congress of the ESCRS in Milan.
5%
Corneal Stromal Regeneration
Stem cell therapy reduces scarring and haze.
ROIBEÁRD O’HÉINEACHÁIN REPORTS

Intrastromal injection of adipose-derived stem cells has potential as a minimally invasive treatment for stromal corneal dystrophies and scarring, reports Professor Jorge Alió.
To demonstrate, he outlined a study he conducted in which five patients with advanced keratoconus underwent injection of adipose-derived autologous mesenchymal stem cells (ADASCs) into a stromal pocket created with a femtosecond laser. The ADASCs differentiated into adult keratocytes and appeared to promote anterior corneal stromal remodelling, producing new collagen and restoring corneal transparency in the eyes with corneal scarring and haze.
His team obtained the ADASCs by elective liposuction from the abdomen or hips. In a five-minute procedure, they created a 9.5 mm diameter stromal pocket in the mid-stroma before injecting one million cells in 1.0 ml of saline solution through a 3.0 mm incision under local anaesthesia. There were no surgical or postoperative complications.
By one month after surgery, all patients had an improvement of one to two lines in uncorrected and best-corrected visual acuity, which remained stable over three years of follow-up. However, the improvement was more likely the result of an intrastromal pocket, as it is well known their creation induces a regularisation of keratoconic corneas, thereby reducing aberrations and improving vision, he noted.
Corneal remodelling
Over three years of follow-up, there was no significant change in refraction or keratometry. However, by one year, there was a mild 14.5-micron improvement in central corneal thickness that has since remained stable.i

In a confocal biomicroscopy study, Prof Alió’s team could show the implanted cells survived—the small change in corneal thickness truly occurred as a result of the ADASC implantation. The cells still maintained their round appearance in the early postoperative months rather than the fusiform appearance of mature stem cells. And later, the team could easily distinguish the new collagen surrounding the cells from the surrounding native collagen.ii
What really showed the potential benefits of the cellular therapy of the corneal stroma was the observation that in those eyes with corneal scars and haze, the scars disappeared, and corneal transparency increased over the follow-up period.
Prof Alió noted they could objectively demonstrate their patients’ increase in corneal clarity by corneal densitometry, which showed a decrease in the anterior cornea’s optical density. While the mid-stroma initially had an increase in density, as expected from the surgery, it then had progressive improvement until finally the density was equal or better than preoperative values.iii
The decrease in cornea density and corneal scarring appears to stem from the ADASC cells that matured into
keratocytes, he said. Confocal biomicroscopy showed the progression: one month after surgery, the stem cells were round and different from the rest of the keratocytes; six months later, they started a fusiform appearance; by one year, they were indistinguishable from the regular keratocytes. Another finding was a gradual increase in the cellularity in the anterior mid and posterior stroma compared to preoperative levels.
“Basically, the stem cells promote the remodelling but also stimulate the keratocytes to multiply to increase the stroma’s cellularity and promote the cornea stroma turnover,” he said.
The team hopes to confirm these findings in a larger sample size. A further question is whether the autologous stem cells, having the same genetic defect that caused the keratoconus, will become dysfunctional in the same way later. However, that may not be an issue since allogeneic adipose stem cells may also be as safe and effective. Prof Alió said preclinical trials involving rabbit eyes showed human ADASCs produced the same results as they later did in the clinical trial and did so without inducing inflammation.
“It might be sufficient to have a stem cell bank with cells obtained from healthy donors and then take and transplant allogeneic stem cells since the human stem cells did not produce an immune response in an animal model,” he added.
iM El Zarif et al., Cornea, 2020; 40(6): 741–754.



iiM El Zarif et al. Investigative Ophthalmology & Visual Science, 2020; 61(4): 22.
iiiM El Zarif et al., Cornea, 2020; 40(6): 741–754.


CORNEA 24 EUROTIMES | APRIL 2023
Prof Alió spoke at the 40th Congress of the ESCRS in Milan.
Jorge Alió MD, PhD, FEBOphth is professor and the chairman of ophthalmology at Miguel Hernández University of Elche and scientific director at Vissum in Alicante, Spain. jlalio@vissum.com.
Evolving Treatments for Corneal Transplantation
DMEK continues to win adherents.
Descemet membrane endothelial keratoplasty (DMEK) represents a clear advance over penetrating keratoplasty and is currently the best choice for surgical treatment of endothelial failure, according to Dr José L Güell.
“Endothelial keratoplasty techniques, and DMEK in particular, have significantly replaced full-thickness penetrating keratoplasty (PK) techniques worldwide for [managing] irreversible endothelial failure,” he said, “with well-known advantages: visual rehabilitation time, refraction and optical quality, globe strength, and immunological behaviour.”

Reflecting on the evolution in corneal transplant techniques over the past few decades, Dr Güell explained the steady shift away from PK towards selective lamellar transplantation using techniques such as deep anterior lamellar keratoplasty (DALK), Descemet stripping automated endothelial keratoplasty (DSAEK), and DMEK.
“If we look at surgical data from any part of the world, endothelial keratoplasty has almost completely substituted full-thickness keratoplasty in most of the cases where it is possible,” he said.



While several endothelial keratoplasty techniques exist, Dr Güell said DMEK is usually his preferred choice for specific indications.
“Based on the currently available evidence in the literature, DMEK looks significantly better for patients than DSAEK,” he said. “These studies do have some limitations, but overall, we can say vision with DMEK is as good as normal eyes in most cases and one or two lines better than DSAEK, and patients experience more rapid visual recovery. There is also better optical quality with fewer posterior corneal higher-order aberrations and visual distortions.”
The procedure’s limitations include its technical difficulty for less experienced surgeons and the high rate of rebubbling interventions required to reposition the donor tissue.
However, these shortcomings have not seriously hampered its uptake as the preferred technique for endothelial keratoplasty.
“Due to the robustness of the technique and the associated growing experience, number of DMEK surgeons, and surgeries performed worldwide, there has been a progressive expansion of its indications to include more complex eyes and clinical situations,” Dr Güell said.
Once limited to non-complicated Fuchs’ dystrophy cases, DMEK is now performed in eyes with glaucoma devices, corneal decompensation due to phakic IOLs, aniridia, post-vitrectomy, and aphakic eyes.
“DMEK is also a feasible, safe, and highly effective rescue technique in eyes with failed penetrating or anterior and posterior lamellar grafts,” he added.


Although he currently prefers DMEK to DSAEK, Dr Güell said newer refinements of the latter procedure—such as Ultrathin-DSAEK (UT-DSAEK) and Pre-Descemet’s endothelial keratoplasty (PDEK)—may overcome some of the drawbacks of DSAEK.
“They are interesting approaches, but we still have a lower standardization profile for donor lenticule preparation with these techniques,” he said. “However, if could persuade eye and tissue banks to go deeper on the lenticules, we might be able to design proper randomised multicentre comparative studies with our more standard DMEK technique. As it stands, we need more data before considering replacing DMEK with either approach.”
25 2023 APRIL | EUROTIMES
Dr Güell presented at the 40th Congress of the ESCRS in Milan.
José L Güell MD, PhD is Director of the Cornea and Refractive Surgery Unit and IMO Barcelona Grupo Miranza and Associate Professor of Ophthalmology at the Autonomous University of Barcelona, Spain. guell@imo.es
DERMOT MCGRATH REPORTS
Endothelial keratoplasty has almost completely substituted full-thickness keratoplasty in most of the cases where it is possible.
The Intracorneal Implant Pipeline
Novel technologies and techniques target multiple indications.
CHERYL GUTTMAN KRADER REPORTS
Intracorneal ring segments have withstood the test of time as a keratoconus treatment—with allogenic intrastromal ring segments and Bowman layer inlay transplantation both showing positive results as follow-up lengthens. But in the spirit of advancement, several novel intracorneal implantation approaches are being developed for keratoconus management. The implant pipeline also includes innovations for presbyopia correction and keratoplasty.
One such device is the GROSSO implant (RECORNEA)— entering a two-centre phase 1 clinical trial and designed to reshape the cornea. This dome-shaped nitinol device with patented shape memory is placed into an intrastromal pocket and intended to be reversible.
“The device would work somewhat like the meshwork used for abdominal hernias, and results from numerical modelling simulations show it is capable of inducing corneal reshaping,” said Dr Nuno Moura-Coelho.
Other investigational approaches using implants for keratoconus include Dr Bader Khayat’s work to develop a 360-degree allogenic intrastromal ring. For allogenic inlays, researchers provided evidence in a small series of patients that intrastromal implantation of a Descemet membrane graft resulted in keratoconus stabilisation for up to 24 months.i
“Suggesting that stromal wound healing is more important for the benefit of long-term stabilisation with intrastromal implantation for keratoconus than the origin of the graft, Oganesyan and colleagues were interested in using Descemet membrane as an easier [means] to harvest an alternative to Bowman layer,” Dr Moura-Coelho explained.
Bioengineered inlays are also in development to treat keratoconus. In a study of eyes with advanced keratoconus, intrastromal implantation of LinkCor (LinkoCare), a cell-free bioengineered implant, was reported to be associated with an average 13.0 D decrease in maximum keratometry along with improvement in logMAR BCVA from 1.36 at baseline to 0.12 at two years.ii
Presbyopia correction
In the presbyopia correction pipeline, the Phase Diffractive Corneal Inlay is an experimental hydrogel corneal inlay disc with a trifocal design. Measuring 4.2 mm in diameter, it features a 1.4 mm central hole and five rings of microholes drilled into the surrounding material. The central opening is designed to improve intermediate vision by a pinhole effect, while the microholes help with far and near focus, Dr Moura-Coelho explained.
“In bench testing, the inlay showed peaks for near, intermediate, and distance vision in the defocus curve,” he said. “And it had slightly better modulation transfer function performance when compared to a commercially available refractive corneal inlay.”
The same company developing the bioengineered inlay for keratoconus has also introduced the CorVision Bioengineered Corneal MicroLens (LinkoCare), a cell-free bioengineered device for treating presbyopia. This small inlay is implanted into a laser-created anterior stromal pocket of the non-dominant eye and received European Regulatory Authority approval after undergoing successful European testing. Dr Moura-Coelho noted it is still under evaluation in clinical trials, and results are not yet publicly available.
Applications in the queue
Additional developments for LinkCor cell-free bioengineered corneal implants include full-thickness transplantation and partial-thickness intracorneal implantation. A 2020 paper reported femtosecond laser-assisted anterior lamellar keratoplasty with the bioengineered corneal implant effective in improving visual quality in eyes with anterior stromal opacities. iii
Other bioengineered devices in development for intracorneal implantation include 3D-printed lenticules for corneal grafting and vision correction procedures (Precise Bio partnering with Carl Zeiss Meditec).
CORNEA
EUROTIMES | APRIL 2023 26
Already commercially available, the ENDO-K PRO (AJL Ophthalmic) is a single-piece double circular PMMA ring with a peripheral ring and central optically clear disc positioned in different planes. It is implanted between the host corneal endothelium and donor corneal graft in anterior lamellar keratoplasty. By mechanically separating the two tissues, it may reduce the risk of allograft rejection, but no clinical data are available to date.
Allogenic inlays include intrastromal ring segments (CAIRS) that, when combined with cornea cross-linking, have been shown to improve uncorrected and corrected distance VA, RSE, keratometry, and cylinder. In addition, extensive work with Bowman layer inlays show encouraging results with follow-up of five to seven years. However, the technique has had limited effect in advanced KC and is technically challenging, limiting widespread adoption.
Intrastromal lenticules for correcting hyperopia and presbyopia have had some favourable long-term results, but there remains a need to refine nomograms for increased predictability—to customise both the lenticule and implantation depth and overcome the surgical complexity of the technique.
The new OS 4 marks the beginning of the next generation of retina, glaucoma and cataract surgery. The all-in-one platform has received numerous exciting features that provide even more comfort, precision and safety.
Laser integration: More safety, fully automated user protection filter
Light: 45% more power*, maximum visibility

Pedal: Multifunctional with over 100 setting options
Phaco: Speedier readiness, greater controllability
User comfort: Even more userfriendly and communicative
Make the difference –with the new OS 4: www.oertli-instruments.com

iOganesyan O, et al. Eye Contact Lens. 2021; 47(4): 223–225.
iiRafat M, et al. Nat Biotechnol. 2022 Aug 11. Online ahead of print.
iiiKhodaparast M, et al. Cornea. 2020; 39(9): 1184–1189.
27 2023 APRIL | EUROTIMES
Dr Moura-Coelho presented at the 40th Congress of the ESCRS in Milan.
Nuno Moura-Coelho MD is a clinical researcher at the Portuguese Retina Institute, Lisbon, Portugal. Nunomouracoelho.oft@gmail.com
EYE SURGERY. SWISS MADE.
Not available for sales in the US *Oertli data on file
NEW FEATURE
OS 4TM THE NEXT GENERATION
The device would work somewhat like the meshwork used for abdominal hernias.
Glaucoma Treatment Options Expand
Agrowing number of patients present both cataract and glaucoma symptoms. New glaucoma devices, including a minimally invasive implant, an advanced laser treatment, and a remote disease monitoring tool could give surgeons more options for addressing glaucoma with or without cataract surgery.

Scleral implant
One issue with existing minimally invasive glaucoma surgery devices (MIGS) is they restore aqueous outflow, which lowers intraocular pressure (IOP), by penetrating the anterior chamber or creating subconjunctival filtration. However, this can put the corneal endothelium at risk. Dr Philippe Sourdille described a new MIGS device that may lower IOP using a different approach.
Rather than create a new channel out of the anterior chamber, the Cilioscleral Interposition Device (CID), under development at start-up firm Ciliatech, instead opens up the space between the ciliary body and the sclera just outside the anterior chamber. This removes what Dr Sourdille, Ciliatech’s medical director, identified as the main obstacle to uveoscleral outflow.
CID is a curved, one-piece hydrophilic acrylic implant 6.0 mm long, 4.0 mm wide, and 200 microns thick. It is inserted through two scleral incisions 2.0 mm posterior to the limbus, and then pushed anteriorly into contact with the iris root. Grooves in its surface facilitate aqueous outflow that oth-
erwise would be blocked by contact between the ciliary body and sclera. Because it does not enter the anterior chamber, “no endothelial threat would be present,” Dr Sourdille noted.
Early results of two clinical studies involving patients with grade 3 or 4 primary open-angle glaucoma (POAG) found a 33% IOP reduction at one year in 20 patients with one implant and 35% in 22 patients at six months with two overlapping implants, Dr Sourdille reported. Topical glaucoma medication use was eliminated in 86% and 89% of patients in the two groups, respectively.
As for safety, CID remained stable, did not change gonioscopic results or visual acuity of visual fields, and did not require additional surgeries. Another clinical study is underway examining narrow- and closed-angle glaucoma patients, with a fourth study planned for CE mark certification, expected in 2024, Dr Sourdille said. “We have the proof of concept. It is possible to lower the IOP without entering the anterior chamber.”
Automated SLT
Due to its efficacy in lowering IOP, selective laser trabeculoplasty (SLT) has gained favour as a first-line glaucoma treatment in recent years, with even the UK’s National Institute for Health and Care Excellence (NICE) now recommending it over eyedrops in suitable patients. But the conventional SLT procedure itself is painstaking and time-consuming, limiting its adoption.
28 EUROTIMES | APRIL 2023 GLAUCOMA
HOWARD LARKIN REPORTS Innovative new devices could reduce risks and enhance outcomes.
A simpler way to use SLT—known as direct SLT or DSLT— may solve the problem, said Daria Lemann-Blumenthal, CEO of Belkin Vision, which is developing and marketing the technology. Rather than requiring 100 or so laser shots aimed individually with a gonioscope, as does conventional SLT, DSLT allows the entire treatment of 120 laser shots to be automatically delivered to the trabecular meshwork through the limbus.
In a subgroup analysis of a clinical trial involving OAG patients on zero or one glaucoma medication at baseline comparing SLT and DSLT outcomes, 48 patients receiving SLT saw a mean IOP reduction of 5.55 mmHg six months after treatment, compared with a mean reduction of 5.49 mmHg in 47 patients receiving DSLT (p = 0.020). More than 70% of both groups were drop-free at 12 months.
“The efficiency of DSLT allows you the freedom to offer your patients laser first, before drops, when it’s most effective, and it leaves all future glaucoma treatment options open,” Lemann-Blumenthal said. The device is CE marked and in controlled release in Europe. She expects DSLT will eventually become the first-line treatment of choice for patients with OAG.
Remote IOP monitoring
Moving IOP monitoring out of the office and into the real world could provide information vital to improving glaucoma treatment. The Implandata Eyemate platform does that, said CEO Max G Ostermeier.
“In between office visits, there is no understanding at all of how effective a therapy is for the patient,” Ostermeier said. The Eyemate platform consists of an implantable device that continuously monitors IOP and communicates with a handheld device, sending alerts to physicians when the disease gets out of control. The system also empowers patients to track their condition, encouraging therapy compliance.
The platform is CE marked and slated for a soft launch with early adopting eye centres in Europe. Eyemate also has been designated a breakthrough device by the US Food and Drug Administration. Integrating real-time IOP monitoring with imaging and other studies could eventually help better understand and treat glaucoma, Ostermeier said.
These presentations occurred at the inaugural iNovation programme at the 40th ESCRS Congress in Milan.
Philippe
Daria Lemann-Blumenthal is CEO of Belkin Vision in Yavne, Israel. daria@ belkin-vision.com
Max G Ostermeier is CEO of Implandata Ophthalmic Products in Hannover, Germany. mostermeier@implandata.com
The Gamechanger for ophthalmic surgeons



Pentacam
Essential to refractive practice for 20 years
Thanks to the streamlined measurement workflow and application-oriented overview screens you further improve your time efficiency. Plus, with tons of studies and a huge user community to support data validity, you are always on the safe side. Optimized workflows, satisfied patients and best possible clinical results are all achieved quickly and reliably and without long training periods. No risk, just fun – the Pentacam® AXL Wave
www.pentacam.com/axl-wave
Meet us at ESCRS Winter Meeting
Booth: 31
Visit our Symposium at CIRP Friday, 10th March, 12:00 h Room: VEGA ROOM
29 2023 APRIL | EUROTIMES
®
AXL Wave
IT ʼ
S TIME TO CHANGE
Sourdille MD is an ophthalmologist, researcher, inventor, and medical director and cofounder of Ciliatech in Chavanod, France. philippe.sourdille86@gmail.com
2023 ESCRS
Clinical Research Awards
Real-world studies with improved patient outcomes.

The ESCRS Clinical Research Awards (the “Awards”) is an initiative sponsored by the ESCRS to support and encourage independent clinical research in the field of cataract and refractive surgery.
The competition is open to all clinicians and researchers with at least three years of ESCRS membership holding a full-time clinical/ research post at an EU-based clinical or academic centre.
https://www.escrs.org/education/grants-awards/clinical-research-awards/
From AI to Eye to Gene
AI algorithm predicts inherited retinal disease genotype from multimodal imaging.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Anew artificial intelligence (AI) algorithm called Eye2Gene can predict the type of inherited retinal disease (IRD) a patient has from retinal scans with a high degree of accuracy, said Dr Nikolas Pontikos.
“We have an AI system that has been tested on several populations, and always the top-five accuracy has been better than 75%,” he said. “The performance is similar to a consensus of experts in our preliminary benchmarking.”
Eye2Gene consists of five distinct convolutional neural networks for each of three scanning modalities, namely, fundus autofluorescence (FAF), infrared (IR), and spectral-domain optical coherence tomography (SD-OCT). The algorithm was trained on a Moorfields Eye Hospital data set consisting of 44,817 images from 1,907 IRD patients with a known genetic diagnosis using five-fold cross-validation to identify up to 36 genetic disorders.
In a data set of 264 Moorfields IRD patients not included in the training set, the correct IRD was Eye2Gene’s first choice in 66.7% of patients and among its top five choices in 85.6%. The correct IRD was Eye2Gene’s first choice in 66.7 % of an external cohort of 1,277 patients from University Hospital Bonn (UHB) and included among its top five in 88.2%. Additional cohorts in Liverpool and Oxford, United Kingdom, and São Paolo, Brazil, showed the correct IRD was Eye2Gene’s first choice in 57.1% to 86.7% of cases and within its top five in 80% to 93.3%.
As a benchmark for the algorithm against human performance, eight ophthalmologists with varying levels of experience in IRDs evaluated a subset 50 FAF scans from the withheld Moorfields and external UHB sets, providing their top five guesses of genetic disorder out of 36 possible choices. On the benchmarking data set, Eye2Gene achieved a top-five accuracy of 72%, compared to 78% for the combined ophthalmologists’ group, meaning at least one of the eight ophthalmologists included the correct gene in their top five guesses 78% of the time. However, none of the ophthalmologists obtained a maximum individual top-five accuracy higher than 36%.
With most genes, there was little difference between the scanning modalities in Eye2Gene’s diagnostic accuracy, but for some genes, such as CRB1, the algorithm worked best with OCT images. Combining the scan data with age at onset and mode of inheritance data improved its accuracy.
Noting there are more than 270 single-gene inherited retinal disorders, Dr Pontikos said identifying the causative gene is crucial for gene targeted treatments, recruitment to clinical trials, prognosis, and family planning. However, access to diagnosis and care does not reach the majority of IRD patients in many parts of the world. He cited a recent epidemiological study that showed among the estimated 30,000 IRD patients in the United Kingdom and Ireland, less than one-third had a genetic diagnosis, with the average time to diagnosis as five years from onset.i Eye2Gene could increase IRD patients’ access to care by improving detection of suspect cases and reducing the number of false positives referred for genetic testing, he said.
But there is still more work to do before the algorithm reaches this point, Dr Pontikos added. The team aims to increase the data set’s size and diversity as well as improve AI interpretation to fully grasp the basis on which the AI makes its decisions.
“We will include age of onset in the algorithm and look at ways to detect rarer and novel inherited retinal diseases,” he said, adding they have two more years of development for Eye2Gene. “And, when we are done, it will allow wide availability of inherited retinal disease expertise.”

31 2023 APRIL | EUROTIMES
Dr Pontikos presented at the Retina 2022 Congress in Dublin.
Nikolas Pontikos PhD is based at the Institute of Ophthalmology, University College London and Moorfields Eye Hospital NHS Foundation Trust, London, London, United Kingdom. n.pontikos@ucl.ac.uk
i Galvin et al., Clinical Ophthalmology, 2020; 14: 707–719.
RETINA
Evidence-based medicine supports quality science
The ESCRS Systematic Review Award (“SRA”) is an initiative sponsored by the ESCRS to produce a high-quality body of research aimed to prepare, collate, analyse, synthesise, and report medical research.
For more information, visit https://www.escrs.org/education/grants-awards/systematic-review-awards/

32 EUROTIMES | APRIL 2023 Systematic
2023–2024
Review Award
CRISPR Therapy Shows Promise
The new gene editing technique could offer a safe treatment plan for patients with severe retinal degeneration.
DR GEARÓID TUOHY REPORTS
Preliminary clinical results using CRISPR gene editing technology to treat patients with a form of Leber congenital amaurosis suggest the treatment is safe and clinical trials should expand, according to Professor Mark Pennesi.

Prof Pennesi worked with a US-based gene-editing company, Editas Medicine, to evaluate the treatment in patients with LCA10, a severe retinal degeneration with no current treatment plan. His clinic is one of five US centres that have recruited patients for the experimental treatment. The research group recently presented preliminary data from their phase 1/2 trial with an ascending dose study of the EDIT-101 CRISPR gene editing treatment for CEP290-related retinal degeneration.i
He noted cohort 1 (low dose) and cohort 2 (mid-dose) patients had no serious adverse effects and no dose-limiting toxicities. The most frequently reported adverse event was eye pain related to the surgical procedure. Key outcomes for BCVA (visual acuity), FST (full-field light stimulus threshold), and visual navigation included early efficacy signals in the mid-dose cohort, suggesting “positive biological activity and potential early clinical benefits,” Prof Pennesi reported.
Up to 34 participants will be enrolled in up to 5 cohorts to evaluate up to 3 dose levels of EDIT-101, designed to eliminate the mutation on the CEP290 gene that results in retinal degeneration. Patients receive a non-randomised single administration of EDIT-101 through subretinal injection in one eye and are monitored every three months for a year, then less frequently for an additional two years. (Those interested in the study protocol can view it at clinicaltrials.gov using identifier NCT03872479.)
Despite these results, a subsequent press release from Editas Medicine dated 17 November 2022, stated: “[t]he results from the BRILLIANCE trial provide a proof of concept and important learnings for our inherited retinal disease programmes.
We’ve demonstrated that we can safely deliver a CRISPR-based gene editing therapeutic to the retina and have clinically meaningful outcomes. While we will not progress EDIT-101 on our own and have made the decision to pause enrolment, we have the patient community top of mind and are looking for a collaboration partner to advance this programme.”ii
CRISPR (clustered regularly interspaced short palindromic repeats) is a recent gene editing technology that emerged from research into prokaryotic immune defence systems, then adapted and applied to multiple uses from agriculture to human gene therapy.
In brief, Cas9 (or “CRISPR-associated protein 9”) is an enzyme that uses gene sequences as a guide to recognise and cleave specific strands of DNA complementary to a CRISPR sequence, not unusual to a copy and paste process in a writing document. The development of this gene editing technique was recognized by the Nobel Prize in Chemistry in 2020, awarded to Emmanuelle Charpentier and Jennifer Doudna.
Prof Pennesi presented at the 22nd EURETINA Congress in Hamburg.
Mark Pennesi MD, PhD is based at the Oregon Health & Science University (OHSU), Portland, Oregon, US. He is a Professor of Ophthalmology and Chief, Paul H Casey Ophthalmic Genetics Division. pennesim@ohsu.edu
i, iii Maeder ML et al., “Development of a gene-editing approach to restore vision loss in Leber congenital amaurosis type 10”. Nat Med. 2019 Feb; 25(2): 229–233.
ii“Editas Medicine Announces Clinical Data Demonstrating Proof of Concept of EDIT-101 from Phase 1/2 BRILLIANCE Trial.” www. editasmedicine.com, November 17, 2022. Editas Medicine. https:// ir.editasmedicine.com/news-releases/news-release-details/editas-medicine-announces-clinical-data-demonstrating-proof.

33 2023 APRIL | EUROTIMES
RETINA
Stargardt Variations
Inherited retinal diseases caused by ABCA4 mutations cover a broad range of phenotypes, from severe childhood-onset to classic Stargardt disease to mild- and late-onset disorders sometimes masquerading as AMD. Until now, determining patient prognoses and selecting the appropriate patients when treatments become available remained difficult. But by combining modern genetic screening techniques with advanced clinical imaging and the increased knowledge of the natural history of diseases and associated ABCA4 variants, it is possible to create a genetics-based clinical model for predicting disease outcomes.
“The proposed precision ophthalmology approach will uncover genetic factors of disease expression beyond the ABCA4 gene to tailor specific patient care and treatment,” said Professor Rando Allikmets. “We can determine the disease modifiers and genetic interplay for the entire spectrum of the ABCA4 disease.”
As a recessively inherited condition with variable onset and severity, Stargardt disease’s most characteristic features include deteriorating central vision due to progressive macular atrophy and flecks across the fundus. Mutations in the ABCA4 gene, which codes for the photoreceptor-specific ABC transporter of vitamin A, cause the disease. The dysfunction of the mutant proteins results in the accumulation of toxic waste (lipofuscin) in retinal pigment epithelium, ultimately leading to cell death.
More than 2,200 pathogenic variants in the ABCA4 gene are known. Around 37% of pathogenic mutations cause severe or very severe disorders, 55% have a mild to moderate effect,
and a further 10%, called hypomorphs, only manifest mild effects later in life. Among the genetic defects, 75% are coding variants, 15% are splice site variants, and 10% are deep intronic variants, he explained.
Mapping ABCA4 variations
Winston Lee, a PhD candidate in Prof Allikmets’ laboratory, led a study showing it possible to devise a system that leverages both genetic and clinical insight to predict long-term outcomes in patients with ABCA4 disease.i The study included 112 unrelated Stargardt disease patients 50 years of age or older to accommodate subtypes with later onset. The team defined four distinct prognostic groups according to the spatial severity of disease features across the fundus, as assessed by retinal imaging and full-field electroretinogram testing.
The researchers found milder prognoses had recurring genotypes, including a newly defined class of rare hypomorphic alleles that shares features with a more common class—such as slowly progressing disease and persistent sparing of the fovea. Mild alleles tended to promote a moderate effect even when paired with a severe allele on the opposite chromosome. In addition, the analysis identified a large group of missense variants associated with the more severe prognoses.
Using this data, Mr Lee and his co-authors constructed a genotype-phenotype correlation matrix to quantifiably predict clinical outcomes based on the detected ABCA4 variants. Prof Allikmets noted similar analyses of larger cohorts of patients would refine the prognostic accuracy further.
34 EUROTIMES | APRIL 2023
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Integrated clinical and genetic analysis provides Stargardt prognosis.
RETINA
More than 2,200 pathogenic variants in the ABCA4 gene are known:
37% 55% 10%
Around 37% of pathogenic mutations cause severe or very severe disorders, 55% have a mild to moderate effect, 10%, called hypomorphs, only manifest mild effects later in life.
“This is a kind of map for physicians and genetic counsellors who see Stargardt patients, so they can [share] what [to] expect through their lifetime,” he said. “This is the beginning of precision ophthalmology—now we can figure this disease out in a very specific manner.”
Professor Allikmets presented his paper at the Retina 2022 Congress in Dublin, Ireland.
Rando Allikmets PhD is the Acquavella Professor of Ophthalmology and Pathology and Cell Biology at Columbia University, New York, US. rla22@cumc.columbia.edu.
iLee et al., JCI Insight, 2022; 7(2): e156154.
CTF/TCT optic designed to:







REDUCE GLARE & HALOS1
TOLERATE THE KAPPA ANGLE2
TOLERATE DECENTRATION
TOLERATE MISALIGNMENT 4

PRESBYOPIA & ASTIGMATISM CORRECTION REINVENTED












35 2023 APRIL | EUROTIMES
1) Broader Toric meridian designed to be more tolerant of misalignment. White paper: Evaluation of a new toric IOL optic by means of intraoperative wavefront aberrometry (ORA system): the effect of IOL misalignment on cylinder reduction. By Erik L. Mertens, MD Medipolis Eye Center, Antwerp, Belgium 2) The misalignment tolerance and the use of segments instead of concentric rings reduces photic phenomena, helping patients to adapt more naturally to their new vision. 3) The central zone of 1.4 mm in diameter is larger than most available mIOLs and allows a wider tolerance so that the visual axis passes through the wider central segment avoiding visual disturbances. 4) In cases of tilt or misalignment, the patient can still benefit from good near and far vision, as the segmented zones allow a balanced far/near light distribution in a steady optical platform. OPHTEC | Cataract Surgery
3
LEVERAGING TECHNOLOGY CAN OPTIMISE AN ALREADY WELL-PERFORMING PRACTICE
BY HOWARD LARKIN
With nine surgeons and thousands of satisfied cataract, refractive, glaucoma, medical retina, and general ophthalmology patients, Dr Guy Sallet’s Eye Institute Aalst, located between Brussels and Ghent in Belgium, was already the high-quality, active, prosperous clinic many ophthalmologists dream of.

So, when marketing guru Rod Solar took on the task of increasing its leads, appointments, and conversions whilst spending no more than €1,000 monthly, it was indeed a challenge—especially given Belgium’s restrictions on advertising, patient testimonials, cost comparisons, and actively prospecting website visitors. Nevertheless, strategically deploying technology and training could further improve clinic efficiency and profitability.
Solar and Dr Sallet broke down their efforts to guide the patient value journey from prospect to satisfied patient advocate into three stages: traffic and leads, appointments and patients, and reviewers and referrals.
Building traffic and leads
Building a practice starts with recruiting patients—and assessing how the practice attracts them is an important first step. At Dr Sallet’s practice, 90% of refractive patients came for the first time for that specific service, with many from outside the immediate area. Most patients have referrals from friends or family, but the practice also attracts patients through its website. It includes detailed information on procedures, the team, and introductory videos, as well as the address, practice hours, and payment methods.
Referrals also come through patient reviews published on Google and Facebook. Staff are trained to answer questions and help guide patients on the phone, where most appointments
are made. And while Dr Sallet said he had enough patients due to a shortage of providers, he felt he could strengthen his active enrolment with professional help.
Solar suggested adding a chat option to the practice’s Google page and homepage. “This helps you capture people who are just wandering by your website but not doing anything.” It is particularly effective for attracting younger patients, many of whom are reluctant to make or receive phone calls, he noted.
Linking the chat feature to a practice customer relations management (CRM) system allows staff to respond immediately from their computers. Such a system can also combine with self-tests and other decision-support and appointment booking features. Automatically generated SMS text and email follow-ups reinforce the message.
It works best when the response time is less than five minutes, preferably within one, Solar added. Automating the text response process allows for fast responses even outside staff hours.
Appointments and patients
Once the patient arrives, the goal of every practice is to get the diagnosis, treatment, and outcome right, Dr Sallet said. But preparation and teamwork to ensure every team member knows why patients are there and what exams, diagnostics, and other services they need helps differentiate the practice, improve patient flow, and create a feeling of professionalism and personalised service patients appreciate.
Cross-training staff on both clinical and administrative tasks is vital to success and helps keep staff engaged,
36 EUROTIMES | APRIL 2023 LEADERSHIP AND BUSINESS INNOVATION
Dr Sallet added. Regular physician-led staff meetings in which employees are encouraged to discuss any issues also help build teamwork and improve practice processes.
In a basic rundown of the cycle, testing and running diagnostics on patients finish in about 15 minutes. Patients then receive education on treatment options and informed consent via PowerPoint and video presentations. So, when the doctor arrives, patients already have an understanding of their treatment options before the clinical examination and final treatment decision. Lastly, staff assists in making surgery and follow-up appointments, providing personalised leaflets, and arranging payment. Dr Sallet noted 75% of complaints stem from non-physician factors, emphasising the need for great service.
Solar suggested automating these processes and recording each interaction in the patient CRM could further strengthen them. The system should include templates for talking, texting, and emailing patients. Automated appointment reminders and missed appointment follow-ups also help increase efficiency.
Reviews and reviewers
With 90% of refractive patients new to the practice, retaining them for other services, such as oculoplastics, glaucoma, retinal issue, dry eye, or general ophthalmology, helps build it, Dr Sallet noted. He provides videos of surgery and small gifts—such as chocolates and birthday and holiday greetings—to keep in touch. Dr Sallet also encourages patients to promote the practice through referrals with personalised leaflets and reviews on Google, Facebook, and other social media.
Solar recommended automating card generation while hand addressing and signing to add a personal touch. He also suggested using the existing patient database to offer additional services.

37 2023 APRIL | EUROTIMES
Dr Sallet and Mr Solar spoke during the practice management and development programme at the 40th ESCRS Congress in Milan.
Guy Sallet MD is medical director at Eye Institute Aalst, Belgium. dr.sallet@ ooginstituut.be
Rod Solar is co-founder of LiveseySolar Healthcare Marketing, London, UK. info@liveseysolar.com
JOIN the leading community and trusted source for SCIENCE, EDUCATION & PROFESSIONAL DEVELOPMENT in the fields of cataract and refractive surgery. learn more about membership at escrs.org
Cross-training staff on both clinical and administrative tasks is vital to success and helps keep staff engaged.
Two new products from Nidek
Nidek announced the launch of the Cube ɑ Ophthalmic Surgical System, which incorporates new ultrasound technology that delivers more powerful and effective phacoemulsification. The Cube ɑ incorporates Gyro torsional technology in a compact body. Torsional ultrasound oscillation ensures efficient delivery of ultrasound energy, especially for moderate cataracts. Design enhancements increase surgical safety by protecting intraocular tissues, the company reports.
The relatively straight Gyro tip design makes the device easy to handle while minimising fluid turbulence during lens emulsification. The newly designed Neo sleeve series provides better fluid dynamics and excellent anterior chamber stability. Improved fluid dynamics in the eye from the tip and sleeve, the company said, contribute to surgical efficiency and safety.
Nidek also announced the launch of the AL-Scan M Optical Biometer with the MV-1 Myopia Viewer software. The device measures axial length, useful for predicting and monitoring myopia progression. As most facilities already have an auto refractometer, clinicians can immediately begin myopia management with the AL-Scan M and MV-1 software.

The AL-Scan M incorporates 3D auto tracking and auto shot functions for easy operation and quick measurement, similar to an auto refractometer. Measurements over time can be monitored and compared with the growth curve. The MV-1 software presents the history of treatment and patient behaviour—important for clinical decision-making—and the intuitive displays are helpful for patient and parental education.
The AL-Scan M is CE mark approved.
www.nidek-intl.com
Bausch + Lomb acquires AcuFocus
An affiliate of Bausch + Lomb has acquired AcuFocus—best known for the IC-8® Apthera™ intraocular lens (IOL). The US FDA approved the small aperture IOL last summer. It is the first and only small aperture non-toric extended depth of focus (EDOF) IOL for certain cataract patients who have as much as 1.5 dioptres of corneal astigmatism and wish to address presbyopia at the same time. Also known as the IC-8 IOL, the lens is available in select markets across Europe, as well as in Australia, New Zealand, and Singapore.

38 EUROTIMES | APRIL 2023 INDUSTRY NEWS
ESCRS TRENDS SURVEY
Details of the ESCRS Clinical Trends Survey—conducted online or in person during the ESCRS congresses from 2016 to 2021—featured heavily in this table findings were a rise in trifocal and extended depth of focus (EDOF) intraocular lens use, a reduction in glaucoma surgeons among respondents, and a transatlantic divide over the amount of rotational error acceptable with toric IOLs.
“Surveys such as these are important tools to evaluate how real-world practice patterns align with recommended evi dence-based standard of care and highlight areas where patient care can be enhanced through the adoption of new technolo gies and/or surgical approaches,” said lead author of the study, Professor Thomas Kohnen MD, PhD, FEBO, in his editorial.
The study showed that the proportion of cataract patients implant ed with presbyopia-correcting IOLs rose from 6.5% in 2016 to 9.5% in 2021. The use of trifocal/multifocal IOLs also increased significantly. These are now the most commonly implanted IOLs for presbyopia correction, followed by EDOF and enhanced monofocal IOLs.
In addition, the proportion of cataract patients implanted with toric IOLs more than doubled in the same period. Regarding the methods used for managing astigmatism in patients receiving monofocal IOLs, most surgeons said they used an on-axis inci sion for 0.75 D of cylinder, on-axis incision and toric IOLs for 1.25 D of cylinder, and toric IOLs for 1.75 D or 2.50 D of cylinder.
The study also showed ASCRS members are more strin gent than ESCRS respondents regarding rotational error in toric IOLs: only 9.4 % of ASCRS respondents were comfort able with 10 degrees of rotational error, compared to 16.0% of ESCRS respondents. Similarly, 65.0% and 53.8%, respec tively, agreed that five degrees or more of rotational error would significantly affect visual quality and visual acuity.
Lastly, the number of respondents who perform glaucoma surgery significantly decreased, with an increasing number of delegates reporting having only a medical glaucoma practice. On average, 5.4% of patients with cataract and glaucoma underwent combined minimally invasive glaucoma surgery and cataract procedures in 2021.
“This current ESCRS survey reports on trends in our field over time and demonstrates nicely how our subspecialty continues to change,” Prof Kohnen said. “Research in cataract and refractive surgery keeps moving us forward to evolve our practices for the benefit of our patients.”

T Kohnen et al., “ESCRS Clinical Trends Survey 2016–2021: 6-year assessment of practice patterns among society delegates”, 49(2): 133–141.

ESCRS Academies
Committee representatives of ESCRS organise and present sessions at meetings organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies promoting and sharing benefits across both memberships.
escrs.org/education/academies/
39 2023 APRIL | EUROTIMES JCRS HIGHLIGHTS
2023 ESCRS Pioneer Award
True innovation comes from good research.
The ESCRS Pioneer Award is an initiative sponsored by the ESCRS to support and encourage independent clinical research in the field of cataract and refractive surgery.
The competition is open to young ophthalmologists up to the age of 40 with at least three years of ESCRS membership holding a full-time clinical/research post at an EU-based clinical or academic centre.
https://www.escrs.org/education/grants-awards/pioneer-research-awards/

Upcoming Events
April 23–27
ARVO
New Orleans, US

April 23
May 5–8
ASCRS
San Diego, US

May 22–25
Royal College of Ophthalmologists

Birmingham, UK
May 26–28
EuCornea Congress
Barcelona, Spain
June 15–17
European Society of Ophthalmology (SOE)

Prague, Czech Republic
June 28–July 1
World Glaucoma Congress
Rome, Italy

Sep 8–12
41st Congress of the ESCRS
Vienna, Austria
May 5
May 22
June 15
41 2023 APRIL | EUROTIMES
PRIORITISING SAFE AND EFFECTIVE OUTCOMES COMPARABLE TO CATARACT SURGERY ALONE1
LOWESTREPORTED ECL=ENDOTHELIAL CELL LOSS; PAS=PERIPHERAL ANTERIOR SYNECHIAE.
NO REPORTS
RATES OF SIGNIFICANT ECL (>30%) & PAS IN ANY MIGS PIVOTAL TRIAL1
OF HYPOTONY, SIGNIFICANT HYPHEMA, OR CHOROIDAL HEMORRHAGE OR EFFUSION1
0.01 DECIBEL MEAN CHANGE IN VISUAL FIELD MEAN DEVIATION FROM BASELINE AT 24 MONTHS IN THE PIVOTAL TRIAL1
99 % OF EYES WERE WITHIN 1 DIOPTER OF TARGET** 2

72 % REDUCTION IN THE PERCENTAGE OF PATIENTS WITH SEVERE OSD SYMPTOMS 3

changes
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only.
• This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. Glaukos®, iStent®, and iStent inject® W are registered trademarks of Glaukos Corporation. All rights reserved. ©2023 PM-EU-0208
 **Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease
in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.
**Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease
in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.




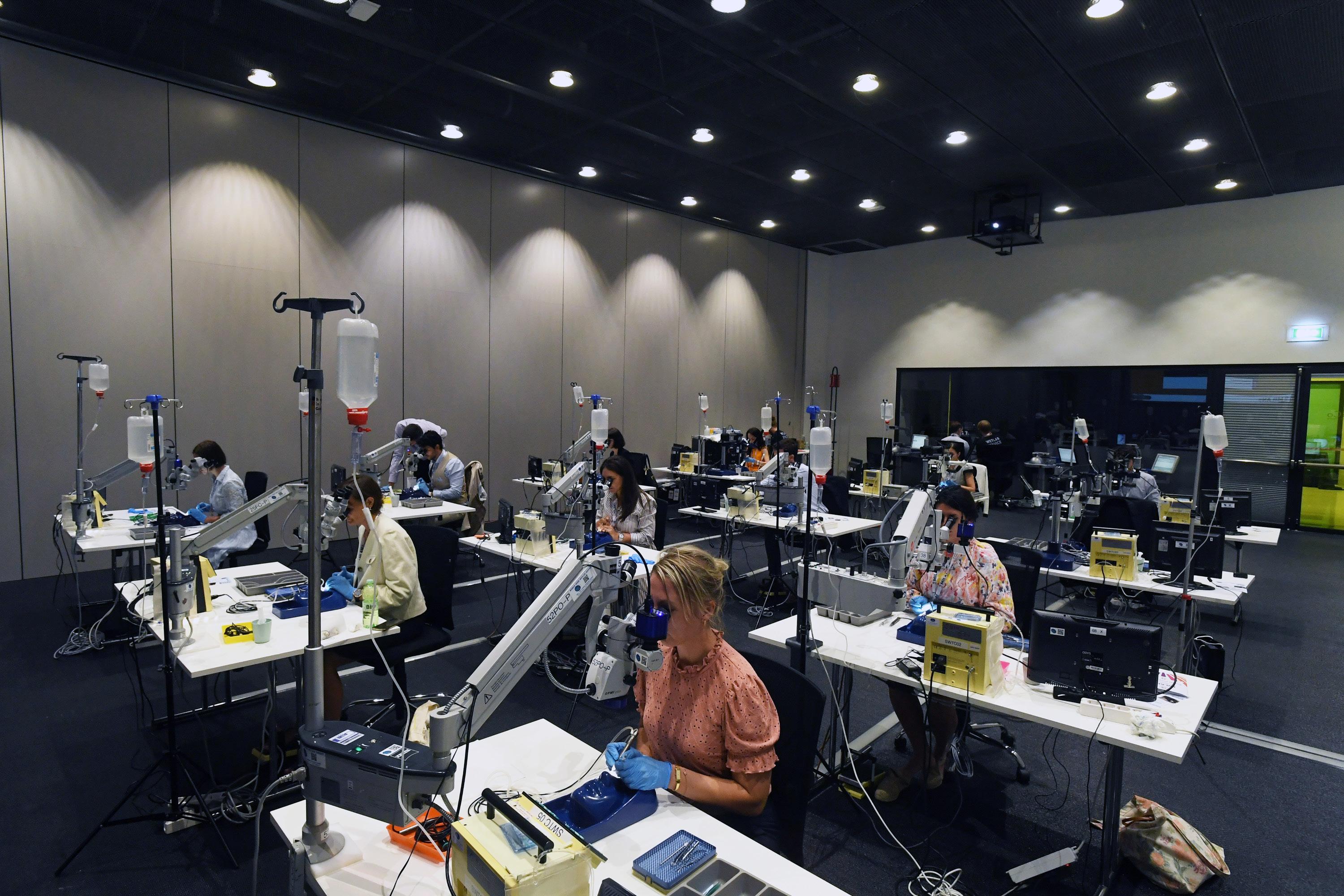





























































 **Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease
in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.
**Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease
in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.