CHARTING AI’S PROGRESSION IN OP H THALMOLOGY


How much of the AI technology is hype and how much is useful?











How much of the AI technology is hype and how much is useful?








ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Publishers
Publishers Vanessa McCourt
Vanessa McCourt
Operations Director ESCRS
Operations Director ESCRS
Barbara Calderwood
Barbara Calderwood
Mark Wheeler
Mark Wheeler
Executive Editor
Executive Editor
Stuart Hales stuart.hales@eurotimes.org
Stuart Hales stuart.hales@eurotimes.org
Editor-in-Chief
Editor-in-Chief
Sean Henahan
Sean Henahan
Senior Content Editor
Senior Content Editor
Kelsey Ingram
Kelsey Ingram
Design Director
Design Director
Kelsy McCarthy
Kelsy McCarthy
Designer
Designer Jennifer Lacey
Stephanie Donnelly
Circulation Manager
Circulation Manager
Vanessa McCourt
Vanessa McCourt
Contributing Editors
Contributing Editors
Cheryl Guttman Krader
Cheryl Guttman Krader
Howard Larkin
Howard Larkin
Dermot McGrath Roibeárd O’hÉineacháin
Dermot McGrath Roibeárd O’hÉineacháin
Contributors
Contributors
Gearóid Tuohy
Leigh Spielberg Gearóid Tuohy
Soosan Jacob
Clare Quigley
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Colour and Print
W&G Baird Printers
Advertising Sales Roo Khan
MCI UK


Tel: +44 203 530 0100

roo.khan@wearemci.com

Advertising Sales Roo Khan MCI UK Tel: +44 203 530 0100 roo.khan@wearemci.com






Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the executive editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes ISSN 1393-8983
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes ISSN 1393-8983
As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between

The Ridley Medal Lecture given by Béatrice CochenerLamard MD, PhD at the 40th Congress of the ESCRS in Milan was a perfect complement to the Heritage Lecture presented by Lucio Buratto MD at the same conference.
The latter reminded us of how far we have come in the pursuit of improving human vision. He described the evolution of ideas since Harold Ridley first observed that the Perspex found in the canopy of fighter planes did not cause an inflammatory reaction when found in the eyes of injured Spitfire pilots. This began the long saga of trial and error that led to the cataract surgery we know today. Prof Ridley withstood the headwinds of resistance from the surgical establishment, designed the first IOL, and implanted it.
Dr Buratto went on to review how new IOL designs emerged as surgeons sought to overcome problems plaguing previous models while taking advantage of advances in surgical techniques and technologies. Dr Charles Kelman’s famous “aha!” moment in the dentist chair as he realised the potential of ultrasound to break up a cataract safely also illustrates the importance of sheer inspiration in problem-solving.
In each case, the initial resistance to a new idea faded, and other bright individuals jumped in with supportive ideas, from foldable IOLs to capsulorhexis, viscoelastics, and modern biometry. What once seemed impossible became routine.
Prof Cochener-Lamard’s lecture, “How the Digital World is Entering Our Practice,” looked to the future, describing a wave of new digital tools that will transform ophthalmic clinical

practice. She explained how telemedicine, machine learning, and artificial intelligence (AI) are profoundly changing the healthcare landscape for the benefit of physicians and their patients.
Our cover story by Clare Quigley MD continues the theme of digital medicine with an in-depth look at the ever-increasing role of AI in ophthalmic clinical care.
This process of continuing to challenge the status quo is ongoing in ophthalmology. In this issue, you will also find articles on bilateral sequential simultaneous cataract surgery, overcoming the current limits of multifocal lens design, refinements in IOL power calculation, and efforts to create a sustainable model of an ophthalmic surgical clinic.
Follow these links to view the lectures:
Heritage Lecture
www.escrs.org/player-videos/escrs-heritage-lecture-2022
Ridley Medal Lecture
www.escrs.org/player-videos/escrs-ridley-medal-lecture-2022


 Güell
Güell
Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (US), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland), Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
“The only way to discover the limits of the possible is to go beyond them into the impossible.”
—Arthur C Clarke
“This process of continuing to challenge the status quo is ongoing in ophthalmology.”


How much of the AI technology is hype and how much is useful?








Artificial intelligence is in our clinics and here to stay. The quiet incorporation of AI—in biometry formulas and glaucoma progression software (among other applications)—is more humdrum than what may have been first contemplated by ophthalmologists. Smart slit lamps that diagnose ocular pathology and generate treatment algorithms have not come into being. Yet this current era has been described as the Fourth Industrial Revolution (4IR), conceptualised as a rapid advancement in technology due to interconnectivity and smart automation by Klaus Schwab, Chairman of the World Economic Forum.
Whether we subscribe to the 4IR or not, significant change that will affect our patients and our work is underway. While the AI revolution within ophthalmology arguably started in medical retina with IDx-DR—a diabetic retinopathy screening tool and the first US FDA-approved technology within the field—current developments will affect the work of cataract and refractive surgeons. Some of the unmet needs AI can help to address, along with common myths and misconceptions and the means to democratise AI research, were explored in the Digital Medicine session at the 40th Congress of the ESCRS in Milan.
More opportunities for audit and research would arise. Prof Romano is also involved in testing the adapted lens on different ectatic ocular surface lesions. Results of the clinical trial evaluating the camera are anticipated in summer 2023.





New developments facilitating earlier keratoconus detection could prove especially useful in the developing world. Nikki Hafezi MAS, IP, ETHZ, Lead of the SBK Project and founding member of the Light for Sight Foundation, Dietikon, Switzerland, suggested taking a Smart Mobile Affordable Reliable Technology (SMART) approach for developing affordable screening tools for low- and middle-income countries (LMICs).
“Now that we have a treatment that can stop keratoconus progression—corneal cross-linking—our challenge is improving our detection of it,” Mrs Hafezi said.
Mrs Hafezi cited the outcome of a recent study investigating how many ophthalmologists in a high-income country like Switzerland had access to the most basic Placido-type topographer. The study revealed only 60% of ophthalmologists had direct access, and she surmised countries less affluent than Switzerland likely have far worse access to the expensive equipment. This lack of access risks later diagnosis of keratoconus, a potentially blinding corneal ectasia that early screening can detect and allow for cross-linking to preserve the remaining vision.
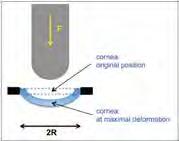
Keratoconus screening can be carried out without a topographer using a smartphone-based keratographer (SBK), which is currently at prototype stage. The SBK project aims to make an affordable, portable, and reliable corneal topographer. The prototype device features a lens and a forehead mount attached to a smartphone with an application that captures the images and generates topographical corneal maps.
Ocular surface disease is a common problem in any general ophthalmology clinic. Documenting clinical signs such as dry eye, keratitis, and corneal neovascularisation has not been found reproducible, with low agreement between graders.


Photography is a useful adjunct for these cases. Apart from daily clinic use, quality corneal photographs are useful in research. Photos of sufficient quality can be labelled and used to train an AI model that could yield further applications, including screening for corneal disease.
“Imaging the front of the eye is always quite challenging. The key point, as you know with research, is to have reproducible data,” said Vito Romano MD, FRCOphth, Associate Professor of Ophthalmology at the University of Brescia, Italy.
Technical difficulties arise in imaging the anterior segment. Some difficulties are easier to overcome, such as consistency of the patient’s direction of gaze or training photographers to improve lighting and focus. Other difficulties are harder to deal with: standard camera lenses commonly focus on only one structure, such as the iris or cornea. This results in bokeh, that aesthetic feature valued in portrait photography for a professional look, rendered by the presence of out-offocus parts in an image. But bokeh is undesirable in medical photography of the ocular surface, where we want to see all the detail without the blur.
In a clinical trial, Prof Romano is testing a specially adapted lens (designed by Occyo) that will allow an anterior segment photo of high quality, where the entire cornea is in focus, along with the bulbar conjunctiva, overcoming the bokeh effect. Prof Romano believes the impact of high-quality imaging could be significant in research and daily practice. Workflow in clinic would improve with imaging carried out before the clinician review, and clinics could achieve more consistent care through availability of historic images when reviewing a patient—who may be seeing different clinicians.
The estimated end-user cost of less than USD$2,000 would be a fraction of the cost of a standard Placido-based topographer. Furthermore, it can be operated by hand or mounted on a slit lamp and gives a readout similar to a conventional topography machine. “SBK is currently a screening tool, not for making decisions about surgery,” Mrs Hafezi said, “but it is already showing great promise.”
Future developments include a machine learning approach


“...this current era has been described as the Fourth Industrial Revolution (4IR), conceptualised as a rapid advancement in technology due to interconnectivity and smart automation.”
where the system learns from physician diagnoses—which Mrs Hafezi said should help SBK provide ever-improving automated diagnostic support to users. The team aims to commercialise the device in mid-2024.
What are common myths in AI? Sunny Virmani, Google Product Manager in San Francisco, United States, explored important misconceptions in AI health applications. One myth he examined is more data is all you need for a better AI-generated model. Not so straightforward.
“You need not just quantity, but quality,” Mr Virmani said. “Another myth: an accurate model is all you need for a useful product. A product must be useable in real-world settings.”
What can be revealed by a photo of an eye? Not a fundus photo, an external photograph? Mr Virmani presented exciting data from an article published in a 2022 issue of Nature Biomedical Engineering i
That study investigated external eye photos for detecting disease. It included a large sample: a training set of more than 140,000 patients with diabetes and a validation sample of more than 40,000 patients with diabetes. A fundus camera captured the external photographs, which trained a deep-learning model that accurately predicted diabetic retinopathy, diabetic macular oedema, and poor glucose control. The prediction performed better than logistic regression models using demographic and medical history data. It is unknown whether other cameras will replicate the results, Mr Virmani said.
If ophthalmologists want to carry out research in AI, do we need to learn how to code? Short answer, no. Pearse Keane MD— Consultant Ophthalmologist, Moorfields Eye Hospital, London, United Kingdom, and Professor of Artificial Medical Intelligence at University College London, United Kingdom—showed alternative, democratic approaches.
“Clinicians will play an important role in the next phase,” Dr Keane said. He believes upcoming developments in AI will be led by those who have the best ideas for clinical applications. And there is a need to make ophthalmology services as throughput and lean as possible.
“Nearly 10% of all clinical appointments in the NHS are for eyes. We have standing room only a lot of the time in our clinics,” Dr Keane said. “AI can play at least some role in mitigating these challenges.”
When asked how he would see AI changing general ophthalmologists’ practice, Dr Keane said one of the biggest areas of improvement is where it can provide specialised
expertise to non-experts.
“I think it will be much more challenging for AI systems to improve the skills of clinicians who are already highly specialised,” he said. “In helping non-experts in this way, I think it could have transformative benefits in medical education. […] Imagine how much more quickly medical students and junior doctors could learn if they had large data sets and a world-leading AI system to help guide them! This might be similar to how chess players increasingly train using computer software.”
Dr Keane has published code-free AI studies, revealing research in the area may be more accessible than most realise.
“I think code-free deep learning is one of the most exciting areas,” he said, recommending the 2021 Nature Machine Intelligence article for those interested in developing their own imaging AI.ii “This describes most of the main CFDL platforms.”
Researchers can access different tools, including an AI short course Dr Keane will run in 2023 focused on this topic.


Ranya Habash MD, Consultant Ophthalmologist, Bascom Palmer Eye Institute and Stanford University, United States, brought the discussion out of this world and into the realm of the metaverse.
“AI and ML in predictive analytics are integral for digital twinning and precision medicine,” Dr Habash said. “This is augmented intelligence, and the metaverse adds another dimension by combining AI, telepresence, and extended reality. There is incredible potential for precision health, decentralised clinical trials, connected care, e-commerce, surgical navigation, and—of course—medical education.
“For example, we’ve created an art gallery,” she continued, “but for eyeballs. Our gallery showcases 3D surgical techniques for eye surgery.”
Dr Habash showed videos of an immersive technology where participants can explore a bright art gallery with framed highquality 3D videos of retina surgeries, screens within screens. She sees applications for surgical education and training, including conferences, grand rounds, and mentoring. All this takes place in the metaverse, an augmented reality that combines aspects of the digital and physical worlds. This harkens back to the AI of our imagination and will educate future generations of medical students and ophthalmology residents.
i Babenko B, et al. “Detection of signs of disease in external photographs of the eyes via deep learning”, Nat. Biomed. Eng, 2022. https://doi.org/10.1038/ s41551-022-00867-5
ii Korot E. et al. “Code-free deep learning for multi-modality medical image classification”, Nat. Mach. Intell, 3, 288–298 (2021). https://doi.org/10.1038/ s42256-021-00305-2
Vito Romano: vito.romano@unibs.it
Nikki Hafezi: nhafezi@lightforsight.org
Pearse Keane: p.keane@ucl.ac.uk
Ranya Habash: ranya@habash.net
Sunny Virmani: sunny.virmani@google.com
“In helping non-experts in this way, I think it could have transformative benefits in medical education.”
POWERFUL.
iStent inject® is the gold standard in Trabecular Micro-Bypass surgery, continuing the legacy of excellence set throughout 20 years of iStent ® devices. It’s backed by the most robust, diverse, and longest-term body of clinical evidence for any MIGS procedure available today, given through clinical rigor and integrity.

8 year study with iStent demonstrated sustained protection against visual field loss, as well as preservation of best corrected visual acuity, cup to disc ratio, and retinal nerve fiber layer thickness9
<0.01 decibel mean change in visual field mean deviation from baseline at 24 months in iStent inject-treated eyes in a pivotal trial1
4% of 125 patients in real world study of stand alone and combined iStent inject cases required a secondary procedure during 5 years of follow up4
38 publications demonstrate the power of iStent technologies to protect against visual field loss†
2.6% of 778 patients in a meta-analysis of stand alone iStent inject eyes went on to require secondary incisional surgery during follow up5
Only 1% of 186 eyes in a randomised controlled trial went on to require secondary incisional surgery during 3 years follow up10
Scientific evidence and clinical rigor have been at the heart of Glaukos, with the earliest publication on iStent® dating back to 2002 - years prior to the iStent ® pivotal trial. Today, this same rigor and integrity is applied to our business as we remain focused on generating strong clinical evidence.
Glaucoma Control.” Advances in Therapy (2022): 1-15. 5. Healey, Paul R., et al. “Standalone iStent trabecular micro-bypass glaucoma surgery: A systematic review and meta-analysis.” Journal of Glaucoma 30.7 (2021): 606-620. 9. Salimi, Ali, Harrison Watt, and Paul Harasymowycz. “Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results.” Eye and Vision 8.1 (2021): 1-12. 10. Samuelson TW, on behalf of the iStent inject Pivotal Trial Study Team. Three-Year Effectiveness and Safety of 2nd-Generation Trabecular Micro-Bypass (iStent inject). Paper at the Annual Meeting of the American Academy of Ophthalmology (AAO). Virtual Meeting: November 13-15, 2020. † Data on file.


iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/ PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. © 2022 Glaukos Corporation. Glaukos, iStent inject® and iStent inject® W are registered trademarks of Glaukos Corporation. PM-EU-0163
PREDICTABLE. PROVEN
PROTECTS VISUAL FIELDS1,9
LOW RATE OF SECONDARY SURGERY INTERVENTIONS4,5,101. Samuelson, Thomas
W., et al. “Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results.” Ophthalmology 126.6 (2019): 811-821. 4. Hengerer, Fritz H., Gerd U. Auffarth, and Ina Conrad-Hengerer. “iStent inject Trabecular Micro-Bypass with or Without Cataract Surgery Yields Sustained 5-Year
Surgeons and their patients can look forward to further improvements to intraocular lens (IOL) technology— new designs and materials should deliver enhanced visual outcomes in the near future, according to Ehud Assia MD.



“There are two IOL technologies in particular that I think we will see more of in the future. One is reshaping implanted lenses, and the second is using artificial intelligence to create innovative lens designs,” he said.
Reshaping implanted lenses, Prof Assia said, is a compelling strategy to tackle the recurrent problem of refractive surprise after IOL implantation.
“Today we are somewhere between 75% and 85% of cases within 0.5 D of target refraction and 94% within 1.0 D. But these refractive errors and surprises will always occur. A logical way to improve the accuracy is to implant the IOL first, wait until it stabilises, and only then reshape the IOL in terms of sphericity, toric, and multifocal components,” he said.
One way to achieve this is the approach used by the Light Adjustable Lens (LAL, RxSight) in which UV radiation is delivered to the lens after implantation. This affects the light-sensitive silicon macromeres and changes the optic’s shape and power, Prof Assia explained.
“The optic is changed to the required refraction and then locked in. The manufacturer claims to have 98% of patients within 0.5 D of target refraction,” he said.
Another interesting approach is Refractive Index Shaping (RIS) used by Perfect Lens, which uses a femtosecond laser to modify the refraction of the implanted lens.


“The laser performs an in-vivo modification of the lens refraction by altering the hydrophilicity of the lens’ polymeric material, producing a lens within the IOL. One can use any standard IOL with hydrophilic or hydrophobic material.





The procedure can be repeated and corrected or reversed by using opposite patterns, so you can change the optics several times with the same lens,” he said.
Artificial intelligence—which is already impacting ophthalmology in areas such as big data collection and analysis, diagnostics, and imaging—will also make increasing inroads into IOL design.


“When engineers design a product, they define the ‘what’ and the ‘how’ one step at a time,” Prof Assia said. “For example, to create a bifocal lens, they start with a refractive base, add a diffractive element, and combine them to create a diffractive bifocal lens. With AI, however, the computer can process multiple variables and thousands of options in terms of materials, designs, parameters, optical qualities, and so on—and then come up with a design we never thought of before. With AI, the engineer just needs to define the ‘what’ and leave the ‘how’ aspect to the computer.”
Lens manufacturers have employed a wide variety of approaches to improve current trifocal designs, including refraction optics (Precizon Presbyopic NVA, Ophtec) and sinusoidal optics (Acriva Trinova IOL, VSY Biotechnology), to try to reduce the light dispersion. Another novel approach adopted in the Intensity IOL range (Hanita Lenses) uses a Dynamic Light Utilization (DLU) algorithm to maximise energy and ensure a continuous defocus
Other techniques to improve trifocal lenses include using a mix-and-match approach, using a refractive lens in one eye and a diffractive IOL in the fellow eye, or combining two or more technologies in a single IOL. Modifying the chromatic or spherical aberration, and employing a pinhole effect, can also increase depth of focus and enhance performance, Prof Assia added.
Prof Assia presented at the 40th Congress of the ESCRS in Milan.
Improving technology to reach visual targets. Dermot McGrath reports
“Reshaping implanted lenses... is a compelling strategy to tackle the recurrent problem of refractive surprise after IOL implantation.”

Aretrospective study based on a review of corneal refractive surgery procedures performed in more than 27,000 eyes provides new information about transient light sensitivity syndrome (TLSS) as a complication following laser corneal refractive surgery.
Dan Z Reinstein MD, MA(Cantab) evaluated the incidence of TLSS among cases of myopic LASIK, hyperopic LASIK, and SMILE performed at the London Vision Clinic, London, UK. The research used the VisuMax femtosecond laser (Carl Zeiss Meditec) in all cases and a MEL 80 or 90 excimer laser (Carl Zeiss Meditec) for LASIK.
The study evaluated the potential for incidence to vary based on treatment type, ametropia type, correction magnitude, and patient age. It also looked for “late” cases occurring more than eight weeks post-surgery.
Consistent with the idea TLSS risk depends on the amount of ultraviolet (UV) radiation applied to the cornea, the results showed the incidence of TLSS was higher after LASIK than after SMILE and higher after hyperopic LASIK than myopic LASIK.
Other analyses showed the incidence of TLSS was higher in older patients and increased with the magnitude of correction only in cases of myopic LASIK. The study also documented that while most TLSS cases occurred within eight weeks of surgery, a significant number developed later.
“There are only 11 published papers describing TLSS, of which only four report the incidence after LASIK, and all were with the IntraLase femtosecond laser. TLSS after SMILE has only been described in one case study. In addition, all papers state that TLSS occurs between two and eight weeks after surgery,” Professor Reinstein said. “Our study is the first to look at TLSS using the VisuMax laser, the first analysing incidence of TLSS after SMILE, and the first to show that TLSS can occur after eight weeks and even up to six months after surgery.”
The study identified patients who had undergone LASIK or SMILE between January 2010 and February 2021 by searching the clinic’s electronic medical record. Eyes were labelled as TLSS cases if the patient received a prescription for a topical steroid to manage photophobia between two weeks and six months after surgery.
The analyses showed the incidence of TLSS was 1.2% for SMILE, 5.3% for myopic LASIK, and 9.0% for hyperopic LASIK. Comparisons between groups were statistically significant and remained so when the cases were divided into early- and latepresentation subgroups.
For analysing incidence dependence by ametropia level, researchers classified eyes into subgroups of low, moderate, and high according to attempted spherical equivalent refraction. The results showed a significant increase in the incidence of TLSS with an increasing correction level for myopic LASIK and no correlation in the SMILE and hyperopic LASIK groups. The incidence of TLSS in the low hyperopic subgroup was similar to the high myopic LASIK subgroup.
Discussing the results, Prof Reinstein said TLSS is caused by UV-induced stromal myofibril and keratocyte-induced activation.
The amount of activation is proportional to the magnitude of UV exposure to a certain level but then reaches a plateau.
He explained the incidence of TLSS after SMILE was lower compared to after LASIK and not dose-dependent as the femtosecond laser produces the same intrastromal interfaces regardless of refractive error treated. Therefore, the amount of UV energy delivered to the cornea is the same for all correction levels. In LASIK, UV exposure from the excimer laser ablation increases in higher refractive corrections, so TLSS incidence is dose-dependent. He also hypothesised the presence of a radiant exposure saturation point, above which TLSS incidence does not increase further. The dose-independent nature of TLSS incidence in hyperopic LASIK suggests hyperopic ablations provide sufficient radiant exposure to pass this threshold.
Prof Reinstein presented at the 40th Congress of the ESCRS in Milan.
Dan Z Reinstein MD, MA is the Medical Director of the London Vision Clinic, EuroEyes Group, London, UK. dzr@londonvisionclinic.com
Despite the wide array of sophisticated diagnostic tools now available to clinicians, it is not always possible to predict or determine the source of patient dissatisfaction after implantation of a premium intraocular lens, according to Giacomo Savini MD.
“There are two main issues to consider: preoperative selection of candidates for multifocal IOLs and postoperative assessment of patients complaining of visual disturbances,” he said. “In both cases, we have a lot of instruments available to us but many times we do not have clear answers to assuage our doubts.”
Several parameters need to be considered in the preoperative selection of candidates to achieve successful outcomes, Dr Savini noted. Corneal topography helps exclude cases with irregular patterns—which standard keratometry cannot detect—and may indicate forme fruste keratoconus or decentred ablation after myopic PRK or LASIK.
Although corneal aberrometry is mandatory before implanting a multifocal IOL, no clear evidence-based guidelines are available to determine the cut-off point for excluding certain cases.
The same also holds true for pupil diameter, said Dr Savini.
“We tend to implant multifocal IOLs when the pupillometry shows a photopic diameter of more than 2.5 mm and a scotopic diameter of less than 6.5 mm or 6.0 mm. However, again there are no evidence-based recommendations. We need to better characterise the relationship between actual pupil size during day and night and the IOL performance.”
Before proceeding with any surgery, Dr Savini advised treating ocular surface problems and dry eye disease (DED).
“No patient with severe dry eye should be implanted with these lenses, and we need to manage moderate dry eye using topical therapy and/or punctum plugs. Likewise, we should exclude macular problems, so no epiretinal membranes and no staphylomas for diffractive multifocal IOLs,” he said.
Dr Savini said it was probably also prudent to avoid implanting multifocal IOLs in cases where the IOL calculation is very difficult.
“Eyes that fall outside the ‘normal’ range of measurements require special attention. Long eyes are best avoided, and caution is required with short eyes, which carry a higher risk of refractive surprise,” he said.
Although there are many diagnostic tools to help screen the best candidates for multifocal lenses, no single device captures all the essential information needed to make a full assessment.

“What we really require is a comprehensive, evidence-based artificial intelligence-supported tool able to predict the risk of postoperative visual complaints, the risk of refractive surprises, and the visual performance for distance, intermediate, and near vision,” Dr Savini observed. “The tool should be based on prospective studies correlating the preoperative data from the tear film to the macula to the postoperative visual function.”
Even after rigorous patient selection, uneventful surgery, and ostensibly good visual outcomes, some patients will still complain of hazy or poor quality of vision after surgery, Dr Savini said. While some of these are straightforward to diagnose—such as residual refractive error, dry eye, or macular pathologies—others are less easy to identify the source.
“The reality is that sometimes everything looks perfect with the technology that we have available, and the patient is still unhappy. Neuroadaptation is clearly a factor in many cases, but the complaints do not always resolve in time. It would be nice in the future to be able to objectively quantify these problems and follow up on the visual complaints,” he concluded.
Dr Savini presented at the 40th Congress of the ESCRS in Milan.
Giacomo Savini MD is an ophthalmologist in private practice in Bologna, Italy, and a researcher at the GB Bietti Foundation – IRCCS in Rome, Italy. giacomo.savini@startmail.com
“Although there are many diagnostic tools to help screen the best candidates for multifocal lenses, no single device captures all the essential information needed to make a full assessment.”

Lenticular intrastromal keratoplasty now ready to advance to a multicentre trial.
Cheryl Guttman Krader reportsPromising results in a feasibility study investigating LIKE (Lenticular Intrastromal Keratoplasty) as a hyperopia treatment support plans to initiate a prospective multicentre study to further evaluate this additive, allograft-based procedure, reported Theo Seiler MD, PhD.
Presenting data from follow-up ranging from one to four years for a series of 15 eyes treated with LIKE for +3.5 to +8.0 D of hyperopia, Dr Seiler reported the achieved refraction was within 0.5 D of attempted in 87% of eyes and ±1.0 D in all eyes.
“These results are much better than with any LASIK treatment for hyperopia,” Dr Seiler said.
Dr Seiler and colleagues began investigating additive hyperopia correction by implantation of a pre-cut donor lenticule about 20 years ago. The idea to perform an additive procedure was based on recognition of the healing response after LASIK resulted in astigmatism and regression.
“Removing a doughnut-shaped tissue ring from the cornea leads to filling of the deficit by epithelium and stromal tissue,” he explained. “Therefore, we instead proposed to implant a prepared lenticule of donor tissue under a LASIK flap.”
Initially, the lenticule was prepared with an excimer laser, but that technique had poor reproducibility. A femtosecond laser obtained better precision for lenticule creation. The LIKE lenticule is cut to a diameter of 7 to 8 mm, keeping Bowman’s membrane intact. The lenticule is implanted under a LASIK flap that is 10 mm in diameter and about 110 μm thick. Based on image guidance (Verion™, Alcon), the lenticule is centred halfway between the Purkinje reflex and pupil centre.
After one month, retreatment with flap lifting and wavefrontor topography-guided ablation of the implanted lenticule is performed for refractive fine-tuning and regularisation of the optical condition. Dr Seiler demonstrated a need for the
retreatment by presenting a graph showing high spread in the refractive outcomes one month before the fine-tuning procedure. He illustrated its benefit with a case of a patient whose uncorrected visual acuity was 0.3 just prior to the retreatment and 0.9 at two months after the procedure.
“Because of the relifting of the flap, we felt having Bowman’s membrane in the lenticule is an integral part of the procedure because it lets you see and then stretch any irregularity in the lenticule,” Dr Seiler said.
He added that as another benefit compared to LASIK, LIKE is a reversible procedure.
“In LIKE, only the lenticule is ablated, and it can be taken out if the patient is unhappy with the result,” Dr Seiler said.
He acknowledged the potential for BCVA loss after LIKE because the procedure results in loss of the magnification effect of the positive lens in the front of the eye. In the pilot study, BCVA loss of two lines occurred in one eye (6.5%), and two eyes (13%) had a one-line loss.
Dr Seiler presented the study at the ESCRS Symposium during the AAO 2022 Refractive Surgery Subspecialty Day meeting in Chicago, US.
Theo Seiler MD, PhD is the founder of IROC eye clinic in Zurich, Switzerland. theo.seiler@iroc.ch
ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
“Because of the relifting of the flap, we felt having Bowman’s membrane in the lenticule is an integral part of the procedure.”
Results from a 12-month multicentre study investigating SMILE for spherocylindrical hyperopia suggest it is a safe, effective, and predictable procedure that appears to be associated with marginally better refractive results and less regression compared to hyperopic Femto-LASIK.
“We have been working on SMILE for hyperopia since 2010, and now, in my opinion, it is one of the biggest breakthroughs in laser refractive surgery since SMILE was introduced,” said Dr Walter Sekundo MD, PhD.
“We need a faster laser for the procedure. As performed with the VisuMax femtosecond laser in this study, the treatment takes 32 seconds. Once approved, however, the treatment will be done with the new VisuMax 800 laser, and then it will only take about 12 seconds.”
The multicentre study was conducted to obtain CE approval for the procedure. It involved eight centres in Europe, China, and India and included 374 eyes of 199 patients. The procedure used a 6.3 mm optical zone, 2.0 mm transition zone, and lenticule thickness of 25 µm centrally and 10 µm at the edge. Mean attempted hyperopic sphere was +2.76 D (maximum +6.00 D), mean attempted refractive cylinder was +0.88 D (maximum +4.75 D), and mean attempted spherical equivalent refraction (SEQ) was +3.20 (maximum +6.50 D).
Safety results showed the safety index was low on postoperative day one but steadily increased to about 1.0 at month 12. No eyes lost more than two lines of BCVA, 1.2% of eyes lost two lines, 11%
lost one line, and 10% gained one line. Loss of contrast sensitivity was seen only at 12 and 18 cycles per degree.
Visual acuity outcomes analysed for the subgroup of 219 eyes treated with a plano target showed 68% achieved 20/20 UCVA at 12 months, and 88% saw 20/25 uncorrected.
“Remember that these hyperopes are often older patients who already have some degree of presbyopia. Two-thirds of my patients were treated with mini-monovision,” Dr Sekundo said.

Refractive results showed good predictability. At 12 months, SEQ was within 0.5 D of attempted in 81% of eyes and ±1.0 D in 93%.
“I think it is important to note the undercorrection was predominantly in eyes treated for greater than +3.0 D SEQ, and the only adjustment to the nomogram was from an earlier study of hyperopic femtosecond lenticule extraction. There is room for improvement in the accuracy of the procedure, but I think it can be achieved with further nomogram adjustments,” Dr Sekundo said, adding astigmatism correction was also very satisfactory.
He described the refractive stability as excellent, although he noted a change in SEQ of 0.07 D between 9 and 12 months.
“It is necessary to overcorrect initially when treating for hyperopia because epithelial healing leads to some regression. Most studies follow patients for only 9 months. In our study, there was very little change in refraction beyond 9 months, but we need to look further to see if it is related to late epithelial healing or presbyopia progression,” Dr Sekundo said.
He acknowledged visual recovery after SMILE was slower than Femto-LASIK for hyperopia and hyperopic astigmatism. However, he said it is a trade-off worth taking, considering SMILE seemed to have an advantage of less regression and less postoperative neurotrophic keratopathy/dry eye symptoms.

Dr Sekundo also reported the procedure was associated with a higher incidence of visible haze compared to myopic SMILE.
“The haze was transient, but it is an issue that is being looked at more closely,” he said.
Dr Sekundo presented at the 40th Congress of the ESCRS in Milan.
Walter Sekundo MD, PhD, Professor and Chairman, Department of Ophthalmology, Phillips University of Marburg, Germany. sekundo@med.uni-marburg.dePositive results in study indicate current technique overcomes past challenges.
Cheryl Guttman Krader reports
“We have been working on SMILE for hyperopia since 2010...it is one of the biggest breakthroughs in laser refractive surgery.”
Dutch analysis finds ISBCS holds advantages in a post-COVID era.
DermotIn an era of increased demand for cataract surgery in ageing populations, one potential solution to reduce the burden on health systems may be to operate on both eyes on the same day without any compromise in safety or efficacy, according to Lindsay Spekreijse MD.

“An increasing number of surgeons are considering switching to immediate sequential bilateral cataract surgery (ISBCS). The current evidence shows no differences in effectiveness and complications compared to delayed sequential bilateral cataract surgery (DSBCS) when adhering to general principles and if suitable patients are selected carefully,” Dr Spekreijse said.
Although ISBCS is a safe and cost-effective alternative to DSBCS, some hurdles need to be overcome to encourage greater uptake among surgeons and patients.
“Even though ISBCS is currently not a routine procedure in the Netherlands, it is being considered by almost 50% of surgeons. In order to improve implementation, potential barriers—such as fear of bilateral endophthalmitis, potential medicolegal issues, and a lack of availability of separate products for both eyes—should be addressed. Education and advocacy could also increase the acceptability of ISBCS among patients,” she said.
The COVID-19 pandemic led to an increase in ISBCS in many European countries as health systems sought to maximise resources and reduce the risk of infection among patients.
“In the UK, for instance, it was recommended as part of the official post-COVID guidelines,” she explained. “One potential advantage of ISBCS, particularly highlighted during the pandemic, was the reduction in the number of postoperative visits needed by the patient. Furthermore, the reduction in visits to the hospital also contributes to a lower carbon footprint in ISBCS compared to DSBCS.”
Other probable advantages include faster visual recovery, no anisometropia, lower costs, less use of home care, and reduced carbon footprint. Potential downsides include fear of bilateral complications such as endophthalmitis, fear of refractive surprise, and possible reduction in reimbursement.
Looking at the available evidence for some of the perceived disadvantages, Dr Spekreijse and colleagues conducted a Cochrane Review in April 2022 with information from randomised controlled trials (RCTs) and non-randomised comparative studies. The authors found limited evidence on endophthalmitis rates, with a very low risk of endophthalmitis in both ISBCS and DSBCS and no evidence of an increased risk with ISBCS. The review found no major difference in refractive outcomes between the groups based on the evidence in one RCT and several other non-randomised studies. It also found lower costs with ISCBS compared to DSCBS.
A further analysis of some database studies that became available after the Cochrane Review also showed no increased risk for unilateral endophthalmitis in cases of ISBCS. Some cases of bilateral endophthalmitis were reported in both DSBCS and ISBCS groups, said Dr Spekreijse.
“Most of the cases of bilateral endophthalmitis published as case reports in the literature did not adhere to the general principles of the International Society of Bilateral Cataract Surgeons. This emphasises the need [for following] these principles by [observing] a strict separation of procedure, instruments, and
intraocular medication for right and left eye and ensuring standard administration of intracameral antibiotics.”
A recent multicentre RCT of 865 patients in 10 Dutch hospitals (the BICAT-NL study) also found ISBCS was non-inferior to DSBCS in refractive outcomes, visual acuity, complications, and patient-reported outcomes. Dr Spekreijse said ISBCS costs were also lower than DSBCS.
Dr Spekreijse presented at the 40th Congress of the ESCRS in Milan.
Lindsay Spekreijse MD is a PhD candidate and resident in Ophthalmology at the University Eye Clinic Maastricht, Maastricht University, the Netherlands.
lindsay.spekreijse@mumc.nl
McGrath reports
“Although ISBCS is a safe and cost-effective alternative to DSBCS, some hurdles need to be overcome to encourage greater uptake among surgeons and patients.”
Novel biosynthetic collagen microlens demonstrates efficacy and biocompatibility in 12-month clinical trial. Cheryl Guttman Krader reports
Abiosynthetic corneal inlay (CorVision, LinkoCare) offers a safe and reversible approach for presbyopia correction that overcomes the biocompatibility problems of previous inlays and the drawbacks of other surgical methods, said Pavel Stodůlka MD, PhD.

Dr Stodůlka presented results from 12 months of follow-up in a clinical trial, adding the inlay was expected to receive the CE mark no later than 2024.
The device is a microlens made of a medical grade, type I collagen originally developed for an artificial cornea with a 10-year history of clinical use in human eyes. The microlens has a central thickness of 20 to 30 μm, a diameter of 1.8 to 3.0 mm, and is implanted in a pocket in the non-dominant eye, centred over the Purkinje reflex. The surgeon creates the pocket using a femtosecond laser at a depth of 140 to 220 μm and up to a 6.0 mm diameter.

“The material is porous, so it biointegrates with the corneal collagen. Therefore, we do not see any longterm problems with the cornea or the interface,” Dr Stodůlka said. “Of course, a femtosecond laser is needed to create the pocket with precision, but the surgery for implantation is very straightforward, and the inlay is easier to manipulate than others on the market.”
central thickness 20 –30 microns
diameter 1.8 to 3.0 mm

manufactured by LinkoCare (Sweden)

110 patients operated
Results 106 eyes at 12 months (2 explanted, 2 lost follow up)
Median age 51 years (range 40 – 65 years)
54 male and 56 female
The clinical study enrolled 110 patients aged 40 to 65 years with “healthy emmetropic presbyopic eyes”. To be eligible for participation, patients had to have a near addition of +1.25 D to +3.50 D, spherical equivalent (SE) -0.75 D to +1.50 D and cylinder less than or equal to 1.5 D in the non-dominant eye, and CDVA greater than or equal to 0.7 logMAR in both eyes. Patients with a central corneal thickness less than 470 μm, curvature greater than or equal to 50 D, or pathology that could affect the outcome were excluded.
Of the 110 patients, 106 were evaluated at 12 months. Two patients were lost to follow-up, and the inlay was explanted in two other patients unable to adapt to the induced monovision.
Presenting a slide depicting a mathematical summation of Scheimpflug imaging maps from the 106 eyes, Dr Stodůlka explained the implanted device creates a central steepening of the cornea and increases its refractive power by inducing spherical aberration.
“Although the central corneal curvature changed by an average of 3.0 D in the centre, the change in curvature decreases away from the centre because of the spherical aberration. Mean manifest refraction SE changed only from +0.25 D to about -1.25 D,” he said.
Near vision testing using ETDRS charts showed all patients could read J1 uncorrected at 40 cm with the implanted eye. The results were even better in testing at optimal reading distance, which averaged 36 cm for the group. At 12 months, mean logMAR uncorrected near visual acuity (UNVA) was 0.16 at 40 cm and 0.13 at optimal reading distance.
“Monocular uncorrected distance vision for the implanted eye decreased as expected, but corrected distance visual acuity was almost unchanged at just below 0.0 logMAR,” said Dr Stodůlka.
“In binocular testing, which is what matters in real life, uncorrected distance visual acuity was unchanged, and UNVA improved by an average of three lines—from logMAR 0.46 preoperatively to logMAR 0.14 at 12 months.”
Patient satisfaction at 12 months was very high, with 94% of patients saying the surgery met their expectations and 96.5% agreeing they would recommend the surgery to family and friends.
“Even though we induce monovision with this inlay, these patient survey results show it is an acceptable way to surgically treat presbyopia,” Dr Stodůlka said.
OCT images obtained during follow-up showed the inlay maintained its transparency.
“The device could hardly be detected, even on the best OCT,” he added.
Adverse events during the study included transient increase in IOP in nine eyes—deemed a steroid response to the tobramycin-dexamethasone drops used postoperatively. Additionally, four patients experienced disturbing photic phenomenon, there were two cases of dry eye, and mild corneal pocket haze was visible at the slit-lamp in two eyes but was not bothersome to the patients.
The experience with inlay explantation showed it as straightforward and demonstrated its reversibility.
“Despite studies showing fibroblasts and nerves go through the inlay, vessels do not, and the removal was easy, which was required in two patients who did not adapt for monovision. In addition, while removing other corneal implants leads to haze, haze did not develop in these eyes, and the cornea more or less returned to its original shape.”

• Fully-automatic measurement

• Gentle voice guidance (available in 9 languages)
• Reliable tono/pachymeter
• Flexible and space-saving design
• A variety of options to meet your needs
“Patient satisfaction at 12 months was very high, with 94% of patients saying the surgery met their expectations.”
SMILE leaves the cornea more intact, but LASIK may be preferred for many patients. Howard Larkin reports
Corneal damage is a significant risk of laser refractive surgery, leading to complications such as dry eye, corneal haze, and even ectasia. Vance Thompson MD and H Burkhard Dick MD, PhD debated the merits of laser in situ keratomileusis (LASIK) versus small incision lenticule extraction (SMILE) for minimising corneal damage in the Journal of Cataract and Refractive Surgery Symposium at the 40th Congress of the ESCRS in Milan.
Arguing for LASIK, Dr Thompson noted while he does LASIK and SMILE as well as photorefractive keratectomy (PRK), SMILE is likely the procedure of the future. Nonetheless, LASIK, particularly wavefront-guided and topography-guided procedures, is safe for most patients and still offers optical advantages that make it preferable for many.
“I do PRK, LASIK, and SMILE, and I am a fan of all three.”
Regarding minimising corneal damage, LASIK reduces risk of a decentred ablation because it is easier and more reliable to achieve precise centration with patient fixation than suction femtosecond laser docking required for SMILE. Though, Dr Thompson noted the difference may wane as SMILE docking and tracking technology improves.
When doing SMILE, “I tell patients if we can’t centre the laser, we are going to cut a flap and do LASIK,” Dr Thompson said. “As my experience with SMILE has increased, this has become a very rare event. My comfort with centring SMILE has increased with my experience.”
Biomechanics: Laboratory Study


Important Aspect: Cut Dimensions & Affected Area

SMILE: lenticule cut (6.5 mm diameter) & the small pocket incision (2.5 - 3 mm arc diameter)

LASIK: substantially larger (80% larger side-cut area, 30% larger cap incision)


The procedure also reduces the surgeon’s learning curve and related intraoperative risk. When retreatment is necessary, LASIK allows for it using the same technology, while SMILE retreatment usually requires switching to LASIK or PRK. However, SMILE is superior for reducing dry eye risk, preserving corneal surface sensitivity, and preventing flap dislocation due to postoperative eye trauma. SMILE also preserves the biomechanical integrity of the cornea, though ectasia is still a risk, Dr Thompson allowed.
Beyond corneal damage, LASIK is superior for treating hyperopia, low myopia, and cylinder, as well as visually significant higher-order aberrations and topographic irregularities such as when topographic cylinder and manifest cylinder diverge, he
noted. Some studies show that wavefront-guided LASIK may also yield slightly better visual acuity and contrast sensitivity.
“LASIK wins on fixation—when there is a need for topoguided or wavefront-guided surgery, when there is low cylinder. … SMILE wins when the correction [it can provide] is ‘high enough’, where there is dry eye concern, where topoor wavefront-guided are not needed, or where trauma is a risk. If correction is optimal and centred well, SMILE is my preferred lamellar approach, with these exceptions,” Dr Thompson concluded.


Advocating for SMILE, Dr Dick noted that “lenticule extraction” (LE) is a better generic term to avoid confusion with similar procedures competing with SMILE, which is a trademark of Carl Zeiss Meditec, including CLEAR (Ziemer), SmartSight (Schwind), and SILK (Johnson & Johnson).i
Beyond the obvious patient appeal of a smaller incision “keyhole” surgery, several studies have shown lenticule extraction surgery preserves corneal strength better than LASIK, Dr Dick noted. Corneal hysteresis, or the ability to rebound after impact, is also greater after lenticule extraction than LASIK—out to three years.
Dry eye inflammatory factors—including MMP-9 and cytokines—also lessen after lenticule extraction than after LASIK, while CGRP, a tear film factor that helps maintain the corneal epithelium, reduces after LASIK, Dr Dick observed. This reduction relates to a further jump in ocular surface disease index (OSDI) scores and reduced tear film break-up time after LASIK compared with lenticule extraction. Nerve damage also increases in LASIK than lenticule extraction, with sensation better immediately after surgery, even after six months in some studies.
At the same time, Dr Dick said visual outcomes for myopic patients have been excellent with lenticule extraction. The few studies comparing LE with wavefront-guided LASIK that have found better 20/20 results with LASIK, he noted, have compared outcomes for early or suboptimal iterations of LE. More recently, larger studies using optimised laser energy and spot placement as well as improved surgical instruments and techniques have improved the percentage of LE patients corrected to 20/20 or better.
Lenticule extraction complication rates are also low, Dr Dick said. In one large study, suction loss occurred in 0.46% of patients, though all completed surgery. Small lenticule remnants were left behind in 0.11% of cases, but these were also managed intraoperatively. Induction of irregular astigmatism occurred in a few cases, indicating a need to convert to LASIK.
“There is evidence that lenticule extraction causes less dry eye disease and other ocular surface problems, leaves more corneal nerves intact, is better for corneal biomechanics, and provides comparable, excellent results. For me, it is the best option for patients,” Dr Dick concluded.

In 2021, Dr Thompson reported doing about 15% PRK, 20% SMILE, and 65% Femto-LASIK procedures, while Dr Dick reported 15% PRK, 15% LE, and 70% Femto-LASIK. When asked which they would choose for themselves as a younger person, both felt it was a tough decision but chose FemtoLASIK, assuming no ongoing corneal difficulties.
But that could change. “SMILE is a procedure in evolution; it is an elegant procedure, and a modern-day refractive surgeon needs to have the ability to do SMILE-type procedures,” Dr Thompson said.
i-ii Reinstein D, Archer T, et al. Journal of Refractive Surgery, 2022.





Vance Thompson MD is founder of Vance Thompson Vision and professor of ophthalmology at the University of South Dakota Sanford School of Medicine, both in Sioux Falls, South Dakota, US. vance.thompson@vancethompsonvision.com


H Burkhard Dick MD, PhD is full clinical professor of ophthalmology and Chairman at Ruhr University Eye Hospital, Bochum, Germany. DICKBurkhard@aol.com


Anovel artificial endothelial implant may provide a safe, efficient, and cost-effective treatment modality for chronic corneal oedema and dispense the need for donor tissue in severely compromised corneas, according to Gerd Auffarth MD, PhD, FEBO.
“The results to date with this implant are very encouraging. The surgery is much easier than conventional Descemet membrane endothelial keratoplasty (DMEK), and the implant is very forgiving in terms of intraoperative handling,” he said. “We have not experienced implant-related material degradation so far. No immunosuppression is required, and the implant is effective at reducing corneal swelling and relieving the pain from bullous keratopathy.”
The EndoArt® implant (EyeYon Medical) is embedded through a clear corneal incision and positioned on the posterior stroma using an air-gas mixture.
“The implant looks like a contact lens—it is dome-shaped, 6.0 mm in diameter, and made of optically clear and flexible hydrophilic material that is bio-compatible and bio-stable. It works by preventing the transfer of aqueous humour into the cornea, thereby decreasing chronic corneal swelling,” Prof Auffarth said. Importantly, the implant allows vital nutrients to reach the cornea on the periphery while blocking the harmful build-up of fluid in the centre.
“Both patients had very compromised corneas with severe pain deriving from bullous keratopathy after multiple surgeries, corneal decompensation, and failed DMEK. On postoperative day one, we could see clear corneas and a marked decrease in corneal thickness,” he said, adding the follow-up on both patients is now over 30 months and 36 months, respectively, and the corneas remain clear with no recurrence of oedema.
Binkhorst Lecture focuses on compromises and challenges in optics.
Dermot McGrath reports from the 39th Congress of the ESCRS in Amsterdam
Every intraocular lens designed to correct presbyopia, irrespective of its design properties and material, involves a trade-off in visual performance once implanted in the eye, said Gerd Auffarth MD, FEBO, during the annual Binkhorst Medal Lecture.
Prof Auffarth presented some case studies of some of the first patients implanted with the device in Heidelberg, Germany, in June 2019.
In a wide-ranging lecture focused on the inherent compromises in multifocal and presbyopic-correcting IOLs, Professor Auffarth stressed the importance of neuroadaptation and brain function in the performance of any implanted lens, adding it was important to appreciate how intraocular lenses perform under real-life conditions once inside the eye.
“If an intraocular lens company tells you that its new lens is perfect and that everything is great, we should be immediately on our guard as the reality is a lot more complex than that—there really is no such thing as a free lunch in IOL optics,” he said.
Turning to the question of optical performance, Prof Auffarth noted presbyopia correction remains one of the greatest challenges in ophthalmology.
He said any attempt to correct presbyopia, a natural but complex process of physiological insufficiency of accommodation associated with eye ageing, needs to take due account of three interrelated concepts: visual quality, depth of field, and dysphotopsia.
Looking at the analysis of the global data of EndoArt devices, Prof Auffarth said a total of 100 patients received implants to date with up to 36 months follow-up. For 22 patients, the implantation was performed as part of the first-in-human study, while for another 25 patients as part of the phase II study with a new surgical protocol.
The cornea, the crystalline lens, and the implanted IOL can all contribute to chromatic aberration. The type of IOL material used also plays a role in the extent of the chromatic aberration, Prof Auffarth explained.
Under the new protocol, 80% of 20 patients implanted needed just one rebubbling procedure or less, while 44% required zero rebubbling.
“IOL material affects chromatic aberration and has a direct impact on it. For instance, hydrophilic IOLs have a lower LCA than hydrophobic lenses. While a refractive optic produces a given chromatic aberration, with a diffractive optic, the chromatic aberration can be manipulated and reversed to reduce the dispersion.”
“If we want to increase the depth of field, we will reduce visual quality and increase dysphotopsia. We have to play with the aberrations of the eye and other factors to maximise visual quality and balance out a certain amount of depth of focus in order to achieve our goal,” he said.
Dysphotopsias include a wide range of visual symptoms such as halos, glare, and starbursts, but not all of them are necessarily caused by the implanted IOL, he noted.
“The optics of an intraocular lens are really the reason for the halos. However, glare and starbursts can also be introduced by refractive error, defocus issues, ocular surface diseases, or other opacification in the optical pathway,” he said.
Chromatic aberration is another important influencing factor in IOL performance. It occurs when light rays pass through an optical media at different points according to their wavelength. Longitudinal chromatic aberration (LCA) causes shorter wavelengths to focus in front of longer wavelengths resulting in a difference of focus.
While this sounds beneficial in principle, the reality is LCA correction actually has a negative impact on the depth of focus in pseudophakic eyes, Prof Auffarth concluded.
“Once again we are back to the reality of there being no free lunch in optics,” he said.
Prof Auffarth said the variety of lenses on the market, using different optical principles, and the terminology used to describe them—enhanced monofocal, extended depth of focus (EDOF), extended range of vision (ERV), and trifocal lenses—was understandably confusing for many ophthalmologists.
“We have learned a lot since the first cases were performed more than two years ago. The descemetorhexis needs meticulous endothelial removal with no tags or overlapping. We know now the optimal design of the implant is the 6.5 mm model in eyes with white-to-white corneal diameter greater than 10.8 mm. Rebubbling is best performed with 10% PFP air-gas mixture. We also use a single 10/0 nylon suture and keep the patient supine for four hours postoperatively,” Prof Auffarth said, concluding the implant held a lot of promise considering the chronic shortage of donor tissue worldwide.
“These categories are overlapping and interacting, and it is really difficult sometimes to match the patient profile with the lens category being proposed,” he said. He noted that as a general rule, the further one moves away from monofocal designs towards EDOF-ERV and then trifocal lenses, the greater the propensity for dysphotopsias to occur.
One compelling solution to try to maximise the specific advantages of different lenses is by adopting a mix-and-match approach Prof Auffarth calls “binocular trifocal”.
“With a device like this, there is no waiting list or eye bank needed for human tissue. It is safe, easy to implant, and can be removed or exchanged if necessary. The costs are lower than for conventional transplants, and it is a less traumatic surgery, which is obviously appealing to the patient,” he said. “It will be interesting to see what other expanded indications might enable this implant to be used in an ambulatory day care setting.”
“We can for instance put a bifocal lens in one eye for distance and near vision, and an EDOF lens in the other eye for distance and intermediate vision. Or we can try blended vision with an EDOF lens in both eyes but use different power additions to target different distance ranges,” Prof Auffarth said.
Prof Auffarth gave this presentation at the 40th Congress of the ESCRS in Milan.
Combining different lens types in an individualised manner can achieve better binocular visual outcomes with enhanced depth of focus and reduced incidence of dysphotopsias, he concluded.
Gerd Auffarth MD, PhD, FEBO is Chairman of the Department of Ophthalmology at the Heidelberg University Eye Hospital and Head of the David J Apple Center for Vision Research, Heidelberg, Germany.
Professor Auffarth is Head of the International Vision Correction Centre (IVCRC) and Director of the David J Apple International Laboratory for Ocular Pathology in Heidelberg, Germany. Gerd.Auffarth@med.uni-heidelberg.de
Gerd.Auffarth@med.uni-heidelberg.de

“Under the new protocol, 80% of 20 patients implanted needed just one rebubbling procedure or less, while 44% required zero rebubbling.”
9
CATARACT & REFRACTIVE
“Once again we are back to the reality of there being no free lunch in optics.”

Polyhexamethylene biguanide (PHMB) 0.08% monotherapy is equivalent to dual therapy with PHMB 0.02% + propamidine 0.1% for achieving medical cure suggest results from the phase 3 study Orphan Drug for Acanthamoeba Keratitis (ODAK).
In addition, a comparison of the results with findings from a retrospective study of Acanthamoeba keratitis (AK) therapy demonstrates that use of a detailed empirical protocol for treatment delivery improves outcomes compared to individual physician standard of care. The aim of the ODAK programme was to develop a licensed PHMB treatment for AK, said John K G Dart MD, principal investigator of the study.
“Acanthamoeba keratitis is the worst form of keratitis and often a life-changing disease. Treatment is delayed for many patients with AK due to unavailability of medication. If we had a licensed therapy, we could be [more confident] that it would be safe and more readily available,” said Dr Dart.
“Monotherapy is always preferable to dual therapy, and we hope to obtain licensing for PHMB 0.08% as monotherapy for AK on similar grounds of non-inferiority that supported the ciprofloxacin license for bacterial keratitis. The application is with the European Medicines Agency (EMA), an application will be going to the US Food and Drug Administration soon, and we hope to get an answer from the EMA next summer.”
Sponsored by the SIFI pharmaceutical company, the doubleblind phase 3 study was conducted at six European centres and randomised 135 subjects to PHMB 0.08% or PHMB 0.02% + propamidine 0.1%. Inclusion criteria required diagnostic confirmation of AK with in vivo confocal microscopy. To make the study as pragmatic as possible, the team set other eligibility criteria so the participants would be representative of a clinic population.
“Patients could be on steroids and have bacterial keratitis. We only excluded patients with active herpetic or fungal keratitis,” Dr Dart said.
The treatment protocol defined regimens for intensive and continuation therapy and included guidelines for antiinflammatory drug use, managing infection relapse, managing exacerbated inflammation, and treatment discontinuation.
The full analysis subset for the phase 3 study involved 127 patients. Medical cure at 12 months—the primary outcome—was achieved by identical proportions of patients in the monotherapy and dual therapy arms (about 87% in a covariate-adjusted analysis). In both groups, 80% of eyes achieved medical cure within 200 days.
There were also no differences between study groups in analyses of BCVA outcomes, corneal scarring rates, adverse events, blood chemistry values, cataract, and anti-inflammatory drug use after baseline. Median BCVA was 20/20, and BCVA was less than 20/20 in only 25% of eyes.
“These are exceptional visual outcomes that I think are replicable in clinical practice if treatment is delivered the way we described in the study,” Dr Dart said.
Comparing the medical cure and BCVA results achieved in the phase 3 study with those reported in the retrospective study in which treatment delivery was according to individual physician standard of carei, Dr Dart reported the empirical evidence-based protocol was associated with “huge improvements”. In the phase 3 study, the rate of medical cure at 12 months was 1.5-fold higher than in the retrospective study, the proportion of eyes achieving BCVA better than 20/25 was two-fold higher, and the proportion of eyes with BCVA worse than 20/60 was almost 50% lower.
Dr Dart delivered the Jones-Smolin Lecture at the AAO 2022 annual meeting in Chicago, US.
Papa et al. British Journal of Ophthalmology, 2020; 104(4): 575–581.
John K G Dart MD is principal investigator ODAK phase 3 programme and consultant ophthalmologist, Moorfields Eye Hospital, London, UK. j.dart@ucl.ac.uk
“80% of eyes achieved medical cure within 200 days.”

National and international corneal transplant registries such as the European Cornea and Cell Transplantation Registry (ECCTR) are extremely valuable in determining the real-world success rates of different keratoplasty techniques and enabling benchmarking to drive quality improvement and reduce healthcare costs, among other benefits, according to Mor M Dickman MD, PhD.
“There is a lot we can learn from major registries like the ECCTR. For instance, it gives us real-world data to show selective lamellar keratoplasty outcomes such as Descemet stripping automated endothelial keratoplasty (DSAEK) and Descemet membrane endothelial keratoplasty (DMEK) vary a lot,” Prof Dickman said. “In best-case scenarios, they have advantages over penetrating keratoplasty (PK), but in the real world, the results may not be as good as we originally thought.”
Possible reasons for the shortfall include the learning curve with lamellar keratoplasty, variable surgical techniques, and patient selection, among other factors.
Established in 2016, the ECCTR has collected data on more than 13,000 transplants from 15 European countries—including information on the recipient, donor and eye bank processing, transplant procedure, and two-year follow-up with graft survival and failure and patient-reported outcome measures (PROMs).

Registry data such as that contained in the ECCTR constitutes a mine of valuable information beneficial to practitioners and patients.
“Measuring is the basis for improvement—if we don’t know where we are in terms of our results, and we have no basis for comparison with others, how shall we ever improve? Registries are important because they improve health outcomes and reduce healthcare costs,” he said.
The ECCTR has already yielded important data on the safety, quality, and efficacy of corneal transplantation in Europe, with two peer-reviewed papers published in 2021 on practice patterns and outcome data for corneal transplantation, respectively.
Key findings included a mean recipient age for a corneal graft of 70 years, with Fuchs’ endothelial dystrophy the primary reason for corneal transplantation, followed by graft failure, pseudophakic bullous keratopathy, and keratoconus, Prof Dickman noted.
“We can see that patient age changes according to diagnosis, with keratoconus patients considerably younger than Fuchs’ patients. Patients with pseudophakic corneal oedema tend to be the oldest patients in the registry,” he said.
DSAEK (46%) was the most performed technique, followed by PK (30%) and DMEK (9%). Vision improvement was the main reason for corneal transplantation.
Surgical technique and reason for transplantation differed between indications. “It is interesting to see some of the nuances, with the desire to reduce pain as well as improve vision more evident in PK patients compared to other lamellar techniques,” he said.
In terms of graft survival and visual outcomes, Prof Dickman said the data constitutes a sharp reality check for lamellar keratoplasty.
“The real-world survival of lamellar grafts was shown to be poorer than penetrating keratoplasty grafts,” he said. “Other studies have shown surgeons who perform less than 100 lamellar grafts a year have poorer graft survival, so the learning curve is probably a factor.”
Beyond graft survival rates, endothelial keratoplasty provides better vision than PK, resulting in a decreased threshold for intervention, Prof Dickman added.
He outlined the potential of registry-based randomised trials to inform best clinical practices in corneal transplantation. One such trial is currently underway comparing two steroid regimens— dexamethasone and fluorometholone—for IOP elevation and endothelial cell loss. The trial will also evaluate cost-effectiveness, with indefinite follow-up ensured via the registry data and in line with evidence-based medicine guidelines.
Further information and details on how to contribute to the ECCTR and other registries supported by the ESCRS are available at https://registries.escrs.org/
Mor M Dickman MD, PhD is a professor of ophthalmology at the University Eye Clinic, Maastricht UMC, the Netherlands. m.dickman@ maastrichtuniversity.nl

“There is a lot we can learn from major registries like the ECCTR. For instance, it gives us real-world data to show selective lamellar keratoplasty outcomes.”

Using pre-cut and preloaded donor graft tissue for endothelial keratoplasty (EK) can significantly reduce operating time, minimise intraoperative tissue manipulation, and facilitate access to EK procedures for less experienced surgeons, according to Stefano Ferrari PhD.

“We have seen a major evolution in recent years with the shift from full-graft penetrating keratoplasty (PK) procedures towards selective lamellar and endothelial procedures. This has led to an increased demand for eye bank prepared and preloaded tissues for Descemet stripping automated endothelial keratoplasty (DSAEK) and Descemet membrane endothelial keratoplasty (DMEK),” he said.
Speaking to EuroTimes, Dr Ferrari said there are several advantages to using preloaded tissue from eye banks.
“The first advantage is the reduction in surgery time, as the surgeon no longer has to prepare the tissue in the operating room,” he explained. “In many hospitals in Italy, there is a specific time slot allocated for the use of the surgery room. Sometimes the ophthalmology department has its own surgery room, but often they need to use shared platforms and all the ophthalmology procedures have to be performed in an allocated amount of time. So, it stands to reason that if you reduce the time of every single procedure, then you can perform more procedures in the same amount of time.”
The next clear benefit of using preloaded tissue is it significantly reduces the learning curve for surgeons who perform only occasional corneal transplants and for whom the more technically challenging DMEK procedure can be daunting.
“The learning curve of DMEK procedure is quite steep, and the more cases you do, the better you become. But it remains technically difficult, and preparing the tissue is stressful for many surgeons,” Dr Ferrari remarked. “By contrast, our technicians in the eye bank prepare up to 10 tissues for DMEK or DSAEK a day, so they have perfected their skills over time. This is another advantage—because the technicians are so used to performing the tasks, the quality of the tissue is much better.”
Having preloaded tissue also removes the risk of stripping Descemet’s membrane in the operating room and compromising the surgery if not performed correctly.
“It is a delicate procedure and a lot can potentially go wrong when stripping the endothelium. This can mean a postponed surgery and a wasted cornea. And even if you have a backup cornea, there is obviously an extra cost involved in having to use that as well. Having the tissue ready to be transplanted makes life a lot easier and reduces a lot of the stress for the surgeon,” he said. With demand increasing for preloaded tissue, Dr Ferrari believes better delivery devices and storage techniques will continue to drive improved efficiency and outcomes in the future.
“There are a lot of different delivery systems currently available for graft delivery in DMEK, for instance, but none of them are optimal in all aspects of the procedure. We need better and smoother delivery methods, more transparency for easier handling, and greater visibility during the graft transfer.
There are many issues that can be improved to make the devices even better,” he said.
Dr Ferrari believes the eye bank of the near future will also evolve to take account of advances in bioengineering and cellular technologies.
“I can see eye bank services expanding to the point where we have laboratories incorporated that work with cells as well as tissues. So, eye banks will offer cellular therapies under good manufacturing practices (GMP) where cells can be amplified and manipulated for transplantation—or artificial corneas for patients with advanced keratoconus. There are so many possibilities, and it’s exciting to see how it will evolve in the coming years,” he concluded.
Dr Ferrari presented at the 40th Congress of the ESCRS in Milan.
Stefano Ferrari PhD currently serves as Head of Research and Development at the Veneto Eye Bank Foundation in Venice, Italy (www. fbov.org). stefano.ferrari@fbov.it
“There are a lot of different delivery systems currently available for graft delivery...but none of them are optimal in all aspects of the procedure.”




Implantation of an artificial endothelial layer (EndoArt®, EyeYon Medical) is a promising treatment for select eyes with chronic corneal oedema from corneal endothelial dysfunction, according to Arie Marcovich MD, PhD.
“EndoArt is endothelial keratoplasty simplified. With it, there is no risk of damaging the graft, disease transmission or infection, rejection, melting, or inflammation. Furthermore, EndoArt can be readily available because it has a long shelf-life under ordinary storage conditions,” said Dr Marcovich.
“Of course, it cannot compete with optimal high-quality Descemet membrane endothelial keratoplasty (DMEK). However, EndoArt is a new technology in evolution that might become even better through optimisation of the implant, surgical technique, and management.”
Results from the phase 1 study enrolling 22 eyes with poor visual potential showed recovery of corneal transparency and normal thickness that has been maintained during follow-up—reaching three years without any device-related complications.
Currently, EndoArt has been implanted in 101 eyes, including 48 enrolled in a multicentre phase 2 trial and 31 compassionate use cases.
Presenting results from a series of 77 eyes, Dr Marcovich reported mean central corneal thickness (CCT) decreased from 748 µm to 572 µm at 4 months (n = 51) and 586 µm in 14 eyes evaluated at 12 months. In the phase 2 study, average eye pain score decreased by 1 month and continued to improve. Among eyes with good visual potential, BCVA improved. In a series of five eyes with the implant procedure—with or without cataract surgery/IOL implantation as an alternative to first-time DMEK— CCT improved from 743 µm to 482 µm at 3 months, and mean BCVA improved from count fingers to 6/12.
Aside from rebubbling, complications included two cases of infectious keratitis judged unrelated to the implant resolved with antibiotic treatment, a single case of stromal herpes keratitis treated with an antiviral agent, and cases of persistent peripheral bullae/vascularisation managed with a bandage contact lens. Like DMEK, the procedure induced a hyperopic shift in several patients due to the implant’s effect on the posterior curvature.
Synthetic endothelial replacement proves safe and effective.
Cheryl Guttman Krader reportsEndoArt with the “F” mark for proper orientation. Preoperative pseudophakic bullous keratopathy. Clearing the corneal oedema 12 months post-EndoArt implantation. Outline of the implant is visible. Slit photo of the “F” mark indicating proper orientation of the EndoArt (Images courtesy of Ruth Lapid-Gortzak MD, PhD).
“EndoArt is a new technology in evolution that might become even better through optimisation of the implant, surgical technique, and management.”
Dr Marcovich said the artificial endothelium offers a strategy for treating blind and suffering patients in countries with a shortage of donor corneas. However, it also has a role in Western countries for eyes suffering multiple graft rejections or at high risk for rejection. In Israel, where the device is approved, EndoArt has been used in a limited number of eyes without those indications as an alternative to first-time DMEK. The EndoArt also has the CE mark, Breakthrough Therapy designation from the US FDA, and Fast-Track Priority Approval status with the Chinese NMPA.

The implant is a biocompatible, biostable hydrophilic acrylic plate attached to the posterior stroma, replacing the diseased endothelium and preventing corneal hydration by acting as an impermeable barrier to aqueous inflow. It is 50 µm thick and has a 6.5 mm diameter allowing nutrients to reach the peripheral cornea. Dr Marcovich said the minimally invasive implantation surgery is straightforward.


Modifications to the procedure with placement of a fixation suture and injection of a C3F8 80% gas bubble were introduced to address early problems with attachment—and the implant was marked with an “F” to verify proper orientation.
“The first 11 patients underwent an average of 3.26 rebubblings, and 8 of the first 20 implants were removed due to poor adhesion at the request of the patients who did not want another rebubbling. Using the new surgical protocol, a single rebubbling was needed in only half of eyes,” he said.

Detecting and treating dry eye disease (DED) preoperatively is imperative for optimising outcomes of patients undergoing cataract and refractive surgery—but as more treatment modalities emerge, clinicians may find the number of options overwhelming.
Karl Stonecipher MD has devised a simple algorithm for managing meibomian gland dysfunction (MGD), the most common cause of DED. He based the recommendations on a retrospective review of his experience treating a large cohort of patients.
“Dry eye disease, particularly MGD, is common in patients presenting for cataract and refractive surgery. Left untreated, it can limit the accuracy of the measurements used for surgical planning; affect postoperative visual quality, patient comfort, and satisfaction; and even increase risks for infectious complications,” said Dr Stonecipher.
“While there are many effective in-office modalities for treating MGD, having all the devices can be cost-prohibitive for a practice, and it is unnecessary. Our simple algorithm is useful for finding treatment that is both efficacious and cost-effective for physicians and patients.”
The first step in choosing management, he said, is to diagnose MGD and determine whether it represents anterior, posterior,
or mixed eyelid margin disease. There is also no need to use expensive tools for performing the diagnostic evaluation.
In his practice, Dr Stonecipher examines patients at the slitlamp to measure tear break-up time and grade MGD severity and conjunctival lissamine green staining. He uses the Ocular Surface Disease Index (OSDI) for symptom assessment.
“Looking for change in the OSDI at follow-up is very helpful for determining if the condition is improving or if the current treatment plan is not working,” Dr Stonecipher said.
To examine the efficacy of various methods for treating MGD, Dr Stonecipher and colleagues conducted an evidence-based review of the literature and the outcomes for a series of 1,721 eyes of 861 of his patients. Most of the patients had been referred for surgery by other clinicians and previously diagnosed with DED but had failed treatment with various topical and systemic pharmacotherapy options.
Dr Stonecipher suggested low-level light therapy (LLLT) can be used to treat anterior, posterior, or mixed disease and offers a good entry point for equipment acquisition based on affordability. A multicentre retrospective study of 230 patients demonstrated
Personal and published experience provide evidence for management algorithm.
Cheryl Guttman Krader reports
its safety and benefit when used in conjunction with intense pulsed light (IPL) therapy. Another study showed the efficacy of LLLT with a standard pharmaceutical regimen for treating recalcitrant chalazia.
“Intense pulsed light is generally used when rosacea is present, but it is somewhat expensive. However, IPL also has cosmetic benefits and so is something that might be considered by clinicians who are interested in offering aesthetic treatments in addition to serving as a dry eye clinic,” Dr Stonecipher said.
For MGD, the LLLT device can be set for blue or red light therapy. Blue light is helpful for anterior lid margin disease and especially for rosacea. Red light causes endothermic heating that melts meibum, enabling expression.
“Meibomian gland obstruction is part of the problem, and addressing it with expression should be part of the treatment,” he said.
The retrospective review found devices providing blinkassisted thermal energy, thermal pulsation, and radiofrequency energy effective as well. However, they carry higher costs for the practice and patients.
Recently, Dr Stonecipher began collaborating with the Canadian group CSI Dry Eye (csidryeye.com) to develop machine-learning, cloud-based software to improve DED diagnosis and patient care. He encouraged others to participate in the project.
“The more data available, the better the recommendations,” he said.
Dr Stonecipher presented at the 40th Congress of the ESCRS in Milan.
Karl Stonecipher MD is a Clinical Professor of Ophthalmology at the University of North Carolina, US, and a Clinical Adjunct Professor of Ophthalmology at Tulane University, Louisiana, US. He is also the Medical Director of Laser Defined Vision Greensboro, North Carolina, US. stonenc@gmail.com
Universal slit lamps with pioneering features


• Five-step magnification changer

• Bright, homogeneous slit illumination
• Decoupling function is standard feature
• „Digital ready”, no need of footswitch
• One of the smallest and lightest full-HD image documentation systems worldwide
• Records entire slit lamp examinations as video sequences
• Includes a beam splitter
“Our simple algorithm is useful for finding treatment that is both efficacious and cost-effective for physicians and patients.”
Why care and counselling should consider systemic diseases and medications.
Cheryl Guttman Krader reportsPatients with glaucoma should be asked about existing systemic diseases and medications because certain medical conditions and drugs can be associated with increased IOP and risk for glaucoma development and progression, advised Gerhard Garhöfer MD.
“It makes sense to look at our patients as a whole. We should not only concentrate on the eye,” Dr Garhöfer said.
Learning about a patient’s blood pressure (BP) and existing treatment for systemic hypertension is important, especially considering almost one-third of the world’s adult population suffers from systemic hypertension.i
“I am pretty sure that all of you who see glaucoma patients regularly have been asked whether having systemic hypertension affects glaucoma,” Dr Garhöfer observed.
The answer to the question is both yes and no. From a statistical point of view, there is an association between BP and IOP. However, from a clinical point of view, the association is “very, very” weak, and is probably not clinically relevant for most patients, Dr Garhöfer said.
Findings from a meta-analysis showed an increased risk of primary open-angle glaucoma (POAG) among patients with hypertension and a positive association between BP and IOP. The average increase in IOP with a 10 mmHg increase in systolic BP or a 5 mmHg increase in diastolic BP was minimal.
“A 40 mmHg increase in systolic BP would translate to just a 1 mmHg increase in IOP,” Dr Garhöfer explained.
Discussing the potential association between ocular perfusion pressure (OPP) and glaucoma risk, Dr Garhöfer noted available evidence also establishes an association between low diastolic OPP, which can occur in subjects treated for systemic hypertension, and increased glaucoma risk. Yet, doubts have been raised regarding whether OPP is the right measure for assessing glaucoma risk considering it cannot be measured directly and instead is a calculated value based on mean arterial pressure and IOP.
“So, OPP is not independent of IOP, which raises the question of the relative contributions of IOP and systemic BP to OPP. A lot of people believe we should look at these two factors differently,” Dr Garhöfer noted.
“As a take-home message, however, it is clear that patients with a very high IOP and a low BP are at considerable increased risk of glaucoma.”
Ophthalmologists should also be aware that patients treated aggressively for systemic hypertension to manage cardiovascular risk may suffer from nocturnal dips in BP that have been shown to increase risk of glaucoma progression. According to the findings of a meta-analysis focusing on this issue, a nocturnal decrease of more than 10% in systolic or diastolic BP confers a significant risk for progressive visual field loss.ii
“We should be particularly careful and obtain 24-hour BP measurements in these patients,” Dr Garhöfer suggested.
Multiple epidemiological studies show a significant association between type 2 diabetes and higher risk of OAG but have yet to establish a biological explanation for the connection. A slight increase in IOP also found in patients with diabetes does not fully account for the increased risk. A current theory proposes accumulation of advanced glycation end products may lead to retinal ganglion cell apoptosis, Dr Garhöfer said.
A variety of systemic inflammatory and autoimmune conditions can also involve ocular structures and lead to increased IOP. The list includes sarcoidosis, Behçet’s disease, HLA-B27-related uveitis, juvenile idiopathic arthritis-associated uveitis, and VogtKoyanagi-Harada syndrome.
In addition, there is a striking association between increased body mass index (BMI) and risk for increased IOP.
“It is not easy to treat increased BMI, but it is still a good thing to talk to patients about,” Dr Garhöfer said.
Considering glaucoma prevalence increases with age, clinicians should recognise there is also an age-related increase in systemic medication use and certain medications increase IOP.
“Two-thirds of adults aged 48 to 64 years and 90% aged 65 years and older take five or more medications,” Dr Garhöfer said.
Uncovering use of an oral beta-blocker is relevant when deciding on topical IOP-lowering therapy because a topical beta-blocker may be less effective in patients on a systemic betablocker. Concomitant use of the two medications also increases the risk for adverse beta-blocker effects.
Corticosteroids, however, are the classic drug culprit for raising IOP. An increase in IOP occurs in 30% of patients using a corticosteroid, and approximately 5% of individuals are “high responders”, meaning their IOP will increase significantly by greater than 15 mmHg and to more than 31 mmHg. Increased IOP can occur regardless of the administration route and is a concern considering the frequency of corticosteroid use.
“An estimated 7% to 10% of adults in Europe are on a corticosteroid, which is quite a high number.”
Dr Garhöfer presented at the Glaucoma Day session of the 40th ESCRS Congress in Milan.
i Mills KT, Stefanescu A, He J. “The global epidemiology of hypertension”. Nat Rev Nephrol. 2020 Apr; 16(4): 223–237. doi: 10.1038/s41581-019-02442. Epub 2020 Feb 5. PMID: 32024986; PMCID: PMC7998524.
ii Bowe A, Grünig M, Schubert J, Demir M, Hoffmann V, Kütting F, Pelc A, Steffen HM. “Circadian Variation in Arterial Blood Pressure and Glaucomatous Optic Neuropathy--A Systematic Review and MetaAnalysis”. Am J Hypertens. 2015 Sep; 28(9): 1077–82. doi: 10.1093/ajh/ hpv016. Epub 2015 Mar 11. PMID: 25767134.
Gerhard Garhöfer MD, Section Head, Department of Ophthalmo-Pharmacology, Medical University of Vienna, Austria. gerhard.garhoefer@meduniwien.ac.at
“It makes sense to look at our patients as a whole. We should not only concentrate on the eye.”
With 20 years of follow-up since publication of its initial results, the Ocular Hypertension Treatment Study’s (OHTS) findings provide a strong basis for treating pre-perimetric glaucoma in ocular hypertension patients with the glaucoma risk factors the study identified, said S Fabián Lerner MD.
Dr Lerner noted the original OHTS study was a randomised controlled clinical trial involving 1,636 OHT patients without glaucoma designed to determine whether early treatment with intraocular pressure IOP-lowering medication could reduce the patients’ incidence of POAG. Another aim of the study was to determine whether baseline demographic and clinical factors can predict the level of risk an OHT patient has for developing POAG.
The study also provided further validation of the OHTS-based glaucoma risk calculator showing the highest risk of glaucoma was among those in the highest risk quartile (59.8%), followed by those in the medium risk profile (47%) and the lowest risk profile (31.7%).

“Consider early treatment for OHT in patients with high and maybe moderate risk. Individualised assessment of risk is useful—therefore, take into consideration a patient’s family history, social situation, life expectancy, health status, preferences, and possible side effects of treatment,” Dr Lerner concluded. “Future risk models may include optical coherence tomography information, genetics, and other factors.”
Dr Lerner presented this report at the Virtual World Ophthalmology Congress.
i Kass MA et al. Archives of Ophthalmology, 2002; 120: 701–703.
ii FA Medeiros et al. Arch Ophthalmol, 2005; 123(10): 1351–1360.
iii Gordon M, Kass M. American Journal of Ophthalmology, 2018 May; 189: xxiv–xxvii.
iv Kass MA et al. JAMA Ophthalmology, 2021; 139: 558–566.
The study showed that at 60 months, the cumulative probability of developing POAG was 4.4% in the medication group and 9.5% in the observation group. Risk factors such as older age, higher IOP, thinner central corneal thickness (CCT), larger vertical cupdisc ratio measurements, and higher visual field pattern standard deviation (PSD) values also were significantly associated with an increased risk for glaucoma development.i
A subsequent study showed a glaucoma risk calculator based on the OHTS’s findings performed well in assessing the five-year glaucoma development in separate OHT patient populations.ii
“The impact of the risk calculator was that in simulated case scenarios, glaucoma specialists changed their recommendations in OHT cases when they included a risk calculator, and specialists were more consistent with OHTS published results,” Dr Lerner said.
The OHTS phase 2 was designed to determine whether delaying treatment with IOP-lowering medications was detrimental to the observation group patients, he said. Participants randomised to observation for 7.5 years received IOP-lowering medications for a mean 5.5 years. Participants in the treatment group continued with treatment. The study showed the medications’ protective effect had a relatively rapid onset, and protection was better for the high-risk group.iii
“Initiating ocular hypotensive medications in OHTS subjects originally randomised to observation significantly reduced the velocity of visual field progression. The greater the amount of absolute IOP reduction, the more important the improvement of visual field change,” Dr Lerner said.
OHTS phase 3, conducted from 2016 to 2019, provided further information on the natural history of OHT and the impact of treatment. It showed that after 20 years follow-up or over a lifetime (within 2 years of death), the cumulative incidence of POAG was 49.3% in the observation group and 41.9% in the medication group. In addition, African Americans had a higher risk at 55.2%, compared with 42.7% among other races.iv
S Fabián Lerner MD is Professor and Head of Ophthalmology, University Favaloro School of Medical Sciences and director, Fundación para el Estudio del Glaucoma, Buenos Aires, Argentina. glaucomas@yahoo.com.ar

Long-term OHTS results confirm risk calculator validity. Roibeárd O’hÉineacháin reports
“The study showed the medications’ protective effect had a relatively rapid onset, and protection was better for the high-risk group.”
European glaucoma experts are gradually reaching a consensus regarding minimally invasive glaucoma surgery (MIGS) in their practice, reports Luis Abegão Pinto MD, PhD.
Dr Pinto noted that when MIGS first came into clinical use, the enthusiasm surrounding the new techniques led to a pressure to “publish or perish,” inevitably leading to some unintentional exaggeration of efficacy and underestimation of potential drawbacks. Now, after 10 to 15 years of experience with the techniques, the dust is beginning to settle, allowing for a more objective appraisal of their clinical value.
“We are trying to move away from the eminence-based approach to a more consensus and evidence-based approach, as we did for the currently existing guidelines on glaucoma by the European Glaucoma Society (EGS),” he said.

In 2021, the EGS initiated a project to provide clinical guidance on practical issues and recommendations regarding MIGS. It asked 50 European glaucoma specialists for their top clinical questions regarding the preoperative, intraoperative, and postoperative issues with the new techniques. Thirty surgeons from 18 countries responded with 240 questions. The participating surgeons then had three meetings to review and analyse the available data to reach a consensus.
Regarding trabecular surgeries with devices such as the iStent® (Glaukos) and the Hydrus® (Alcon), there was a strong consensus they can reduce the number of drops a patient requires, but it is best to restrict the devices to those without progressing disease




and those who do not need very low IOP levels. The project participants also agreed the devices are best used in combination with cataract surgery, since very few occasions allow a standalone procedure. They also agreed the safety profile is very strong, cautioning the long-term outcomes are unknown.


As for bleb-forming devices, such as the Xen® Gel Stent (Allergan) and the PreserFlo MicroShunt (Santen), the group’s consensus was only surgeons with bleb-related experience should implant the devices. Their use entails administering intraoperative and postoperative metabolites, and the devices often require postoperative interventions such as needling and bleb revision, Dr Pinto noted.
The group also agreed that open-bleb revisions have a higher success rate than needling and recommended not repeating a failed needling. A more conventional surgery, such as trabeculectomy may be indicated if bleb revision is unsuccessful. In patients with cataract and glaucoma, it is best to perform phacoemulsification first (if the severity of the glaucoma permits) before placing the bleb-forming device—whether carrying out the procedures simultaneously or sequentially.
Dr Pinto said the EGS project yielded many more techniques. For example, techniques involving angle surgery must have the angle open, and the surgeon must have experience with intraoperative gonioscopy. The project further advised surgeons to audit their results and consider the cost-effectiveness of the
“We want to learn from cumulative experience in order to have an unbiased view of these new tools and where they fit in our practice and whether they do best fit our patients.”




Dr Pinto presented this report at the Virtual World Ophthalmology Congress.
Luis Abegão Pinto MD, PhD is Head of the Glaucoma Unit and Assistant Professor of Ophthalmology, Lisbon University, Portugal. abegao.pinto@chln.min-saude.pt
European Glaucoma Society finds place for MIGS in the ophthalmic surgeon’s daily practice. Roibeárd O’hÉineacháin reports
“We want to learn from cumulative experience in order to have an unbiased view of these new tools and where they fit in our practice and whether they do best fit our patients.”
We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With over 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.

Ophthalmologists who perform intravitreal injections can reduce the environmental impact of the procedures by taking advantage of reusable instruments and multi-use medication vials and eliminating post-injection topical antibiotics, according to the results of a Royal Australian and New Zealand College of Ophthalmologists (RANZCO) fellowship survey presented by Sukhpal S Sandhu FRANZCO.
With the increasing demand for intravitreal injections, he said ophthalmologists try to standardise and streamline the pathway for patients—but there remains considerable variation in the procedure and the equipment used.
To consider the range of intravitreal injection practices and look at options for reducing waste, RANZCO’s sustainability committee sent a survey to its organisation’s members regarding the equipment and materials they used when performing intravitreal injections.
Nearly all 405 respondents (96%) said they perform the procedures in an office or treatment room, whereas 3.7% said they do so only in operating theatre. In addition, nearly all (99%) said they use masks, while a minority (up to 11%) said they use additional personal protective equipment, such as gowns and shoe and head coverings.
For local anaesthetics, 289 (78.7%) respondents said they use sterile minims—and, of those, 116 (40.1%) use a new minim for each patient. In addition, 236 (64.3%) respondents reported using an injected sub-conjunctival local anaesthetic, of whom 87 (36.9%) use a single vial per patient. Regarding topical anaesthetics before subconjunctival ones, 185 (78.4%) reported minim use.

The survey also showed a marked difference in the use of reusable instruments between those who used a customised intravitreal pack—which include disposable instruments—and those who used a basic dressing pack. In the former group, 85.9% used disposable speculums, and 84.6% disposable callipers. That compared to only 14.1% and 15.4%, respectively, in the basic dressing group.
“Of course, we must put this in perspective. Many wasteful practices are enforced by local infection control guidelines and protocols regarding which types of packs (particularly overequipped customised packs for intravitreal injection procedures) and minim use per patient,” Dr Sandhu added.
He noted up to 28.5% of respondents reported using both povidone and chlorhexidine prior to injection and 24.8% using topical antibiotics after injection. Other findings included 56.4% stating they did not use drapes. Some respondents volunteered suggestions for reducing waste, such as limiting the items in packs that go unused and end up in the landfill: e.g., gauze, cotton balls, and plastic forceps.
“This survey highlighted gaps in evidence-based medicine best practices. Combined antiseptics are not evidence-based for this procedure, and there is good evidence that there is no requirement for post-procedure antibiotics,” Dr Sandhu said. “Office-based intravitreal injections are safe. We should make efforts to reduce the waste of customised intravitreal injection packs and single-use disposable equipment.”
Dr Sandhu presented the survey’s findings at the Virtual World Ophthalmology Congress.
Sukhpal S Sandhu FRANZCO is a member of the RANZCO sustainability committee and is based at The Royal Victorian Eye and Ear Hospital, Centre for Eye Research Australia, Melbourne. sukhpal.sandhu@unimelb.edu.au
Study finds plenty of room for waste reduction in intravitreal injections. Roibeárd O’hÉineacháin reports
“We should make efforts to reduce the waste of customised intravitreal injection packs and single-use disposable equipment.”



Working in high-volume clinics with close and prolonged proximity to patients puts ophthalmologists at risk of contracting COVID-19. The risk significantly reduces, however, if both patients and physicians wear surgical masks. Moreover, the COVID-related mortality rate for US physicians has fallen since the start of the pandemic, is currently lower among physicians than in the non-physician population, and is lower among ophthalmologists compared to some other medical specialists, according to Azin Abazari MD.
Speaking during a symposium devoted to the topic, Dr Abazari helped distil the latest information on SARS-CoV-2’s impact on ocular health and the practice of ophthalmology. She noted incidents such as Chinese ophthalmologist Dr Li Wenliang’s death in February 2020—just a few months after warning of an outbreak—raised early concern that ophthalmologists might be more susceptible to contracting the viral infection.
“Over the past two and a half years, however, our understanding of the SARS-CoV-2 virus, its transmission, and its implication for ophthalmology have evolved,” Dr Abazari said.
Reviewing current knowledge, she said COVID-19 transmission is thought to mostly occur through exposure to droplet particles emitted from the respiratory tract of infected persons. The droplets, however, travel only about one to two metres and do not remain suspended in the environment for very long. Thus, transmission via droplets requires being in the same room, at the same time, with the infected person.
Aerosols, which are smaller particles than droplets, can remain suspended in the environment and travel farther than droplets. They can also transmit infection even if the infected individual is not in the same place as the susceptible person or in a relatively enclosed space with poor ventilation.
“According to the World Health Organisation, aerosol transmission of COVID-19 is not proven,” Dr Abazari said, adding that contact with contaminated surfaces is considered a minor mode of COVID transmission.
PCR can detect viral RNA in tear or conjunctival samples of a small minority of COVID-positive patients. Dr Abazari stressed the importance of knowing there is no proven risk of transmission because of contact with tears or conjunctiva of a COVID-positive individual. RNA particles can be detected in tear or conjunctiva of patients simply because of exposure to aerosolised particles or viremia in the setting of systemic infection.



Understanding COVID transmission occurs mainly through droplets provides a basis for recommending strategies to prevent disease contraction, including the recommendation of ophthal mologists and patients both wearing surgical masks.

“Some studies show that surgical masks worn by both parties are as protective as the physician alone wearing an N-95 mask,”








Other recommendations include administering screening questionnaires to patients prior to their visit and using breath shields on the slit lamp, although these need frequent sanitising. Careful hand hygiene and disinfecting/sanitising other equipment will reduce contact transmission but are less important since contact with contaminated surfaces is a minor means of transmission.
This presentation was made at AAO 2022 in Chicago, US.
Azin Abazari MD is an Associate Professor of Ophthalmology, SUNY Stony Brook, Stony Brook, New York, US. azin.abazari@
“Over the past two and a half years...our understanding of the SARS-CoV-2 virus, its transmission, and its implication for ophthalmology have evolved.”
While technically challenging, implanting intraocular lenses (IOLs) using an optic capture through the posterior capsulotomy may help avoid the anterior vitrectomy usually performed using an in-the-bag technique in very young children, recommends Shail A Vasavada DO, DNB, FICO.
“Although there is no literature to suggest that vitrectomy affects x-thing or y-thing, I think if we can avoid disturbing any of the natural structures, particularly in these young-development eyes, I’m sure it should help us in some way or the other in the long run,” Dr Vasavada said.
Dr Vasavada based his comments on a prospective randomised clinical trial he and colleagues conducted. It compared five-year outcomes of a conventional in-the-bag IOL implantation— including anterior and posterior capsulorhexes and a limbal anterior vitrectomy—with an optic capture through the posterior capsule without vitrectomy in children four years old or younger.
Thirty eyes were randomised to the in-the-bag group, of which 27 were followed for five years or more, while 31 were assigned to the optic capture group, of which 28 were followed for at least five years. Postoperative outcome measures were significant visual axis opacification (VAO), defined as VAO encroaching on the central visual axis, requiring a secondary vitrectomy or membranectomy; glaucoma development; and significant inflammation markers including large or small cell deposits on IOLs or posterior synechiae—all assessed during the five-year follow-up.
Overall, there were no significant differences in visual outcomes or complications between the two groups within the five-year follow-up period. Visual acuity improved in both groups—0.49 ± 0.19 logMAR for in-the-bag IOLs and 0.66 ± 1.22 logMAR for optic capture—though there was no statistically significant difference between them, Dr Vasavada reported.
Two eyes in the in-the-bag group required a secondary procedure for significant VAO: one at 14 months and one at 16 months after initial surgery. One eye in the optic capture group required a secondary procedure for VAO at 21 months postoperatively. In the in-the-bag group, one child requiring a secondary procedure was under one year old, while the optic capture child was under one year old.
Two eyes in the in-the-bag group and none in the optic capture group developed glaucoma. Both children affected were under one year old at the time of surgery, and symptoms were controlled with topical medications.

A limitation of the study was the skill required to create a posterior capsulotomy and optic capture without disturbing the vitreous face. If the face is disturbed, the surgeon must perform a vitrectomy, Dr Vasavada noted. A small capsulorhexis may also make it difficult to execute the optic capture.
“Serious long-term complications were the same when you do a vitrectomy or don’t do a vitrectomy. … The optic capture of the IOL whenever possible can avoid vitrectomy and yet reduce visual axis obscuration with similar incidence of glaucoma and inflammation postoperatively,” he concluded.
Dr Vasavada presented at the 40th Congress of the ESCRS in Milan.
Shail A Vasavada DO, DNB, FICO is a surgeon and researcher at Raghudeep Eye Hospital and Iladevi Cataract and IOL Research Centre, Amedabad, Jaipur, India. contact@raghudeepeyehospital.com or icirc@abhayvasavada.com
Howard Larkin reports
The leading community and trusted source for SCIENCE, EDUCATION & PROFESSIONAL DEVELOPMENT in the fields of cataract and refractive surgery.
Over the past decade, healthcare greenhouse gas emissions surged 30%, David F Chang MD said in the Practice Management & Development Programme at the 40th Congress of the ESCRS in Milan. Healthcare currently accounts for about 10% of emissions in the US and about 25% in the UK public sector.i
With about 70% of healthcare emissions produced by operating rooms and labour and delivery suites, and cataract surgery one of the highest volume surgeries worldwide, ophthalmic practice contributes significantly. And global annual cataract surgery volume is projected to jump to 50 million in 2050 from 29 million in 2019, and its climate impact along with it, Dr Chang explained.
“We are going to have to do so much more surgery to reduce the burden of cataract blindness.”
So, what can be done now to cut cataract surgery’s climate impact? Noting cataract surgery produces about 20 times as much waste in Europe and the US as in India, with no difference in postoperative endophthalmitis, there’s plenty of room for improvement, Dr Chang said. Greatly reduced costs are another benefit.
To give surgeons the tools they need to reduce climate impact while maintaining safety, ESCRS partnered with ASCRS and the American Academy of Ophthalmology (AAO) to create eyesustain.org, which Dr Chang chairs. ESCRS is also developing a cataract surgery sustainability index for disposables to help surgeons identify opportunities to safely reduce resource use and practice costs, and provide benchmarks for evaluating supply tenders, said ESCRS President Oliver Findl MD, also an EyeSustain.org board member.
Drs Findl, Chang, and other presenters highlighted several actions surgeons and programme directors can take now to reduce the environmental impact—and related health risks—of ophthalmic surgery.
In a 2020 survey, 98% of ophthalmologists were willing to use multidose bottles of topical drugs on multiple patients, but less than half actually did.ii Multidose drug bottles were more likely used in ambulatory surgery centres than hospital-based units, though even in ambulatory clinics, just 12% continued using them until their expiration date—instead throwing them out at the end of the day, week, or month.iii
The waste adds about $150 per case and about 23,000 to 105,000 metric tonnes of unnecessary CO2 equivalent emissions annually in the US alone.iv To reduce this waste, ASCRS, AAO, and the American Glaucoma Society jointly endorsed using multidose containers on multiple patients, using them until their expiration date, and allowing patients to take home partially used containers for postoperative use, Dr Chang noted.v
Standardising surgical device and supply use consistently with lower utilisation programmes within European countries would significantly cut waste, said Dr Findl, who practices in Vienna.
“If we were to reduce all the [supply] packs in Austria to the lower third, we would reduce emissions by 20% to 27%, depending on whether materials were recycled.” Tools for identifying superfluous instruments are available on EyeSustain.org, he added.
Surgical drapes are a major waste source, with some programmes using full-body drapes and others just ocular drapes, Dr Findl said. “There is a lot of variation within the same country where we all use the same techniques and technology.”
The Dutch Task Force on Sustainable Ophthalmology also recommends against body drapes and eye shields in most uncomplicated cataract cases, said Sjoerd Elferink MD and Redmer van Leeuwen MD.
Properly executed, short-cycle sterilisation can save significant energy compared with wrapped full-cycle sterilisation and drying and is effective for sequential-same-day cataract surgery, Dr Chang noted.vi The Dutch Task Force on Sustainable Ophthalmology recommends employing internal sterilisation departments and reusable sterilisation containers.
Reusable diamond keratomes are an option, Dr Chang said. “Our diamond paracentesis blades cost $425 and can last more than a year.”
Using alcohol hand sanitizer to scrub between surgeries can save an estimated 61,631 L of water annually per operating room and $280,000 to $348,000 in scrub time, Dr Chang added.vii
Calculating the practice’s carbon footprint and educating staff can make a huge difference, Dr Chang noted.
“If they understand this, they will think of ways to reduce waste.”
Presenting studies that support operational changes is also critical for convincing administrators to change policies. He advised searching EyeSustain.org for its many supporting documents online, adding mygreendoctor.org as another great source for educational materials and supporting sustainable practices.
i Morris DS et al. Eye (Lond), 2013 Apr; 27(4): 495–501.
ii Chang DF, Thiel CL. J Cataract Refract Surg, 2020; 46: 933–940.
iii Thiel CL et al. J Cataract Refract Surg, 2022; 48: 1092–1094.
iv Tauber J et al. JAMA Ophthalmology, 2019; 137: 1156–1163.
v “Reducing Topical Drug Waste in Ophthalmic Surgery – 2022”, American Academy of Ophthalmology, April 6, 2022. https://www.aao.org/clinicalstatement/reducing-topical-drug-waste-in-ophthalmic-surgery.
vi Chang DF et al. Ophthalmology, 2018; 125: 1320–1324.
vii Javitt MJ et al. JAMA Ophthalmology, 2020 Apr 1; 138(4): 382–386.
Oliver Findl: oliver@findl.at
David Chang: dceye@earthlink.net
Sjoerd Elferink MD and Redmer van Leeuwen MD: sustainable. ophthalmology@gmail.com
First, could you remind us of the purpose of the IOL calculator project? Why did you think this was necessary?
The purpose was to bring together all the excellent online formulas into one convenient location. There are at least 20 separate formulas for IOL power calculation online. They are updated regularly, either with AI or new data, new IOL constants, etc. On the other hand, we have expensive biometry machines used to calculate the IOL power, but those biometers are not connected to the internet for various reasons.
New online formulas come all the time, while the biometers use older formulas that are not updated as much. Before our tool was developed, you would do the biometry and then visit four or five sites, entering the exact same data each time. Or you might decide to use one or two formulae to save time, and do the surgery after you choose the IOL power, when maybe you might have gotten a better result with another formula. We wanted to help surgeons by providing an easy way to load the patient data just one time for multiple calculator sites.
At first, I thought I would do a personal web page called alliolformulas.com. I wrote to all the formula authors, including Kenneth Hoffer and Graham Barrett, to explain my intention and ask permission to include their formulas. Kenneth Hoffer connected me with the ESCRS, and the board liked the idea. They wanted to make a calculator, but they didn’t know what to do. It was the right time and the right place. The ESCRS team included Oliver Findl, Nino Hirnschall, Filomena Ribeiro, and Miguel Raimondo. We met regularly and started to polish the idea, adding features, finally resulting in the finished product that is now online.

There may have been some concern at first when I started emailing people. Perhaps they had questions about the purpose, maybe some concern about errors or liability. But once the ESCRS came on board, we had no problems. All the authors were happy with the idea and glad to participate.
The site uses a technique called webscraping. This sounds something like Google Travel, where I can enter my flight requirements and find out all the options from the various airlines.
It is exactly like that. Our site uses no internal calculations. When you enter the data, it goes to the various sites and returns to our site with the results. Entering data once saves time and reduces the chances of typing errors. If the different sites update, we update ours. Most of the formulas are not published, so the only way of getting the results is to use these online calculators. Also, our site makes doctors aware of the existence of all these formulas they may not even know about.
The site has been online for a little while now. Are you getting user feedback, thinking about making any changes?
The ophthalmology community really seems to accept and like it. The traffic has been huge. Next, we will launch a toric IOL version, then add a calculator for post-refractive eyes that uses the newest formulas.
What are your thoughts on the evolution of IOL power calculators over time?
The tools we have now are great. That is why cataract surgery is now refractive surgery. We are getting close to perfection. I think we may have reached the limit for standard eyes, with 85% or more getting within +/-0.5 D of the target. Biology plays a role, so I expect we will always have some outlier cases. We are getting better with more complex cases, such as high astigmatism and eyes that have undergone previous refractive surgery, but we still have a lot of work to do.
The ESCRS IOL Calculator is free to all ophthalmologists at https://iolcalculator.escrs.org
dantebuonsanti@gmail.com
“We are getting close to perfection.”

Heru announced the launch of a new screening tool for dark adaptation in AMD patients. The wearable device provides a non-invasive, dark adaptation exam in as little as 4.5 minutes for a rapid exam, or 20 minutes for an extended exam. The dark adaptation function supplements an existing contrast sensitivity exam that uses the same headset. The company hopes the device will lead to earlier detection of AMD, as well as longer term monitoring of existing disease.
www.seeheru.com
The Susvimo (ranibizumab injection) ocular implant has been recalled by Genentech/ Roche to evaluate a manufacturing issue. The device received US FDA approval last year for wet AMD treatment. The recall has led to a pause in implantations and clinical trials involving the device.


“We noticed in our laboratory testing— reliability testing—that in certain cases, the septum, which is the seal on the port delivery device that prevents the medicine from leaking out once it has been injected in, could fail after repeated dosing. … Because it didn’t meet our performance standards and we want to make sure we have high reliability, we decided to voluntarily stop distribution of the Port Delivery System,” said Bill Anderson, CEO, Roche Pharmaceuticals in a call with investors. Approved in October 2021, the refillable Susvimo allowed patients to receive as few as two treatments per year. The company emphasised the recall does not involve the ranibizumab vial or refill needle, and treatment with refills can continue.
www.gene.com

Heidelberg-based Novaliq announced the US FDA New Drug Application (NDA) approval of CyclASol® (cyclosporine ophthalmic solution) for treating the signs and symptoms of dry eye disease.
“If approved, CyclASol would be a highly potent but comfortable anti-inflammatory therapy for patients with dry eye disease. It shows impressive and rapid therapeutic effects objectively measured on the ocular surface in the majority of patients, with clinical benefits on the signs and symptoms of the disease,” said Christian Roesky PhD, CEO, Novaliq.
CyclASol employs Novaliq’s EyeSol® proprietary water-free technology, using ultrapure semifluorinated alkanes (SFAs) physically, chemically, and physiologically inert with excellent biocompatibility and a very good safety profile.
www.novaliq.com

Studies assessing and comparing outcomes for enhanced monofocal, EDOF, and multifocal IOLs require an unambiguous standardisation of the measurements for refraction visual acuity and contrast sensitivity, according to updated recommendations. The authors note better harmonization of study design will give meta-analyses greater statistical power.
Among the recommendations, clinicians should 1) adjust manifest refraction to infinity rather than six metres, for example, by adding 0.25 D to the obtained refraction with a four-metre chart distance; 2) avoid using non-standardised charts or scales at intermediate and near distances and instead use ETDRS test and logMAR values; 3) clearly state and define the distances and luminance levels at which they measure visual acuities; 4) include the distances at which they measure contrast sensitivity; 5) predictability reports should contain the IOL calculation formula, the IOL constant, and the biometer used; and, 6) standardise patient satisfaction questionnaires to encompass questions regarding spectacle-dependence and visual symptoms.

J Fernández et al., “Standard for collecting and reporting outcomes of IOL-based refractive surgery: update for enhanced monofocal, EDOF, and multifocal IOLs”, 48(11): 1235–1241.

Cataract patients without comorbidities almost always have better uncorrected distance visual acuity (UDVA) than their preoperative distance-corrected visual acuity (CDVA) by their first postoperative week following immediate sequential bilateral cataract surgery (ISBCS), according to a new chart review study. In the series of 116 patients who underwent ISBCS in 2019, postoperative UDVA was stable or improved compared with preoperative CDVA in 48% on the day of the procedure, 79% postoperative day one, and 90% postoperative week one. Furthermore, 92% of eyes had a UDVA of 20/40 or better on postoperative week one. Five of the remaining 18 eyes had limited visual potential due to comorbidities.
K Kwedar et al., “Visual recovery after immediate sequential bilateral cataract surgery at a veterans’ hospital”, 48(11): 1260–1263.


The new Tecnis Synergy multifocal (ZFR00V) IOL can provide cataract patients with an extensive range of vision, particularly through near distances, and better mesopic performance than the AcrySof PanOptix Trifocal IOL (model TFNT00), according to a new study. Among 95 patients with Tecnis IOLs and 52 patients with AcrySof IOLs, most achieved 20/25 or better binocular CDVA (100% vs. 96.2%) and distance-corrected near visual acuity (DCNVA) measured 40 cm (88.4% vs. 75.0%) and 33 cm (78.9% vs. 51.9%) at three months follow-up. Mean binocular DCNVA at 40 cm was better by 0.5 Snellen lines in the Tecnis group than the AcrySof group. The mean binocular photopic and mesopic DCNVA at 33 cm was better by 0.8 Snellen lines in eyes with the Tecnis lens than the AcrySof lens and better by 0.5 lines in photopic high-contrast and low-contrast CDVA. Patientreported ocular symptoms and safety were generally similar in the two IOL groups.

HB Dick et al., “Comparison of 3-month visual outcomes of a new multifocal intraocular lens vs a trifocal intraocular lens”, 48(11): 1270–1276.


MARCH
ESCRS Winter Meeting
10–12 March
Vilamoura, Portugal

APRIL
ARVO
23–27 April
New Orleans, US
MAY
ASCRS
5–8 May
San Diego, US
Royal College of Ophthalmologists
22–25 May
Birmingham, UK
JUNE
European Society of Ophthalmology
15–17 June
Prague, Czech Republic
World Glaucoma Congress
28 June–1 July
Rome, Italy
SEPTEMBER
41st Congress of the ESCRS
8–12 September
Vienna, Austria

ESCRS Educational Forum is supported by multiple industry partners to provide independent didactic education on selected therapeutic areas. The platform combines presentations from ESCRS Winter and Annual Congresses, selected EuroTimes articles, videos, and webinars to provide an in depth overview on current clinical outlooks.
escrs.org/education/forum/

The 2022 ESCRS Digital Research Awards are an initiative sponsored by the Society to support and encourage research leading to digital transformation in the fields of cataract, refractive, and corneal surgery.
The competition is open to ALL clinicians and researchers with the selected project(s) eligible to receive funding of up to €500,000 over a maximum of three years.
NOVEMBER 14, 2022
Deadline for receipt of preliminary applications
NOVEMBER 28, 2022
Invitation to shortlisted applicants to submit full proposals
JANUARY 30, 2023
Receipt of full proposals from shortlisted candidates
FEBRUARY 27, 2023
Notification of successful candidates
For more information: escrs.org/education/grants-awards/digital-research-awards/













