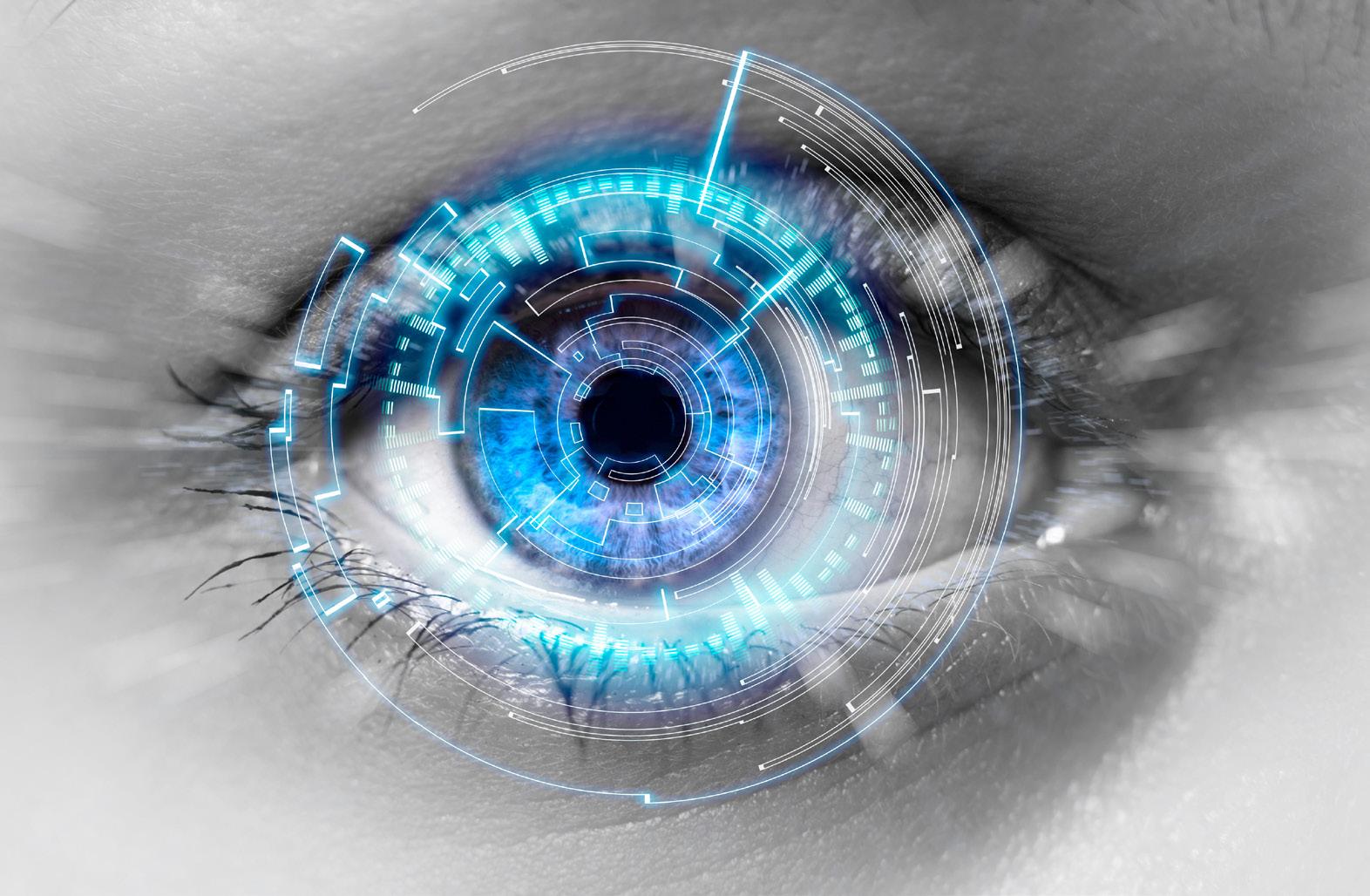
Glimpses into Ophthalmic Genius
How trailblazing innovations are helping shape future advances.









































































































How trailblazing innovations are helping shape future advances.









































































































8th September 2024, Sunday 10:30-10:50
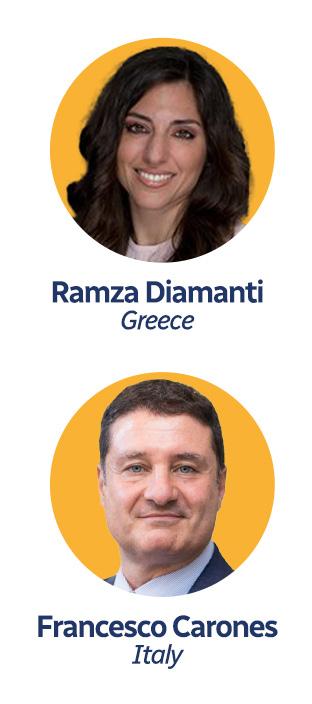
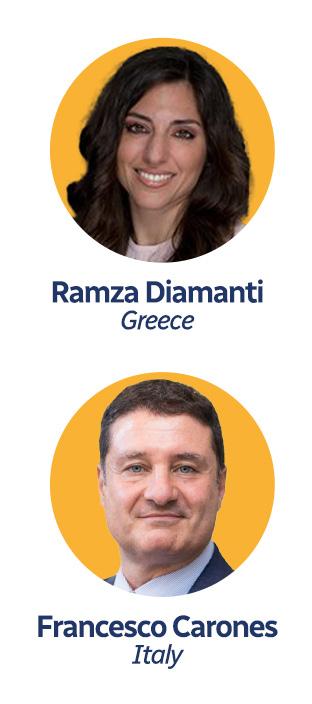
AddOn® Lenses: The Versatile Swiss Knife for Optimizing Patient Outcomes


















8th September 2024, Sunday 16:15-16:35
Visual quality after the implantation of trifocal intraocular lens in patients with various preoperative corneal status

























































































































































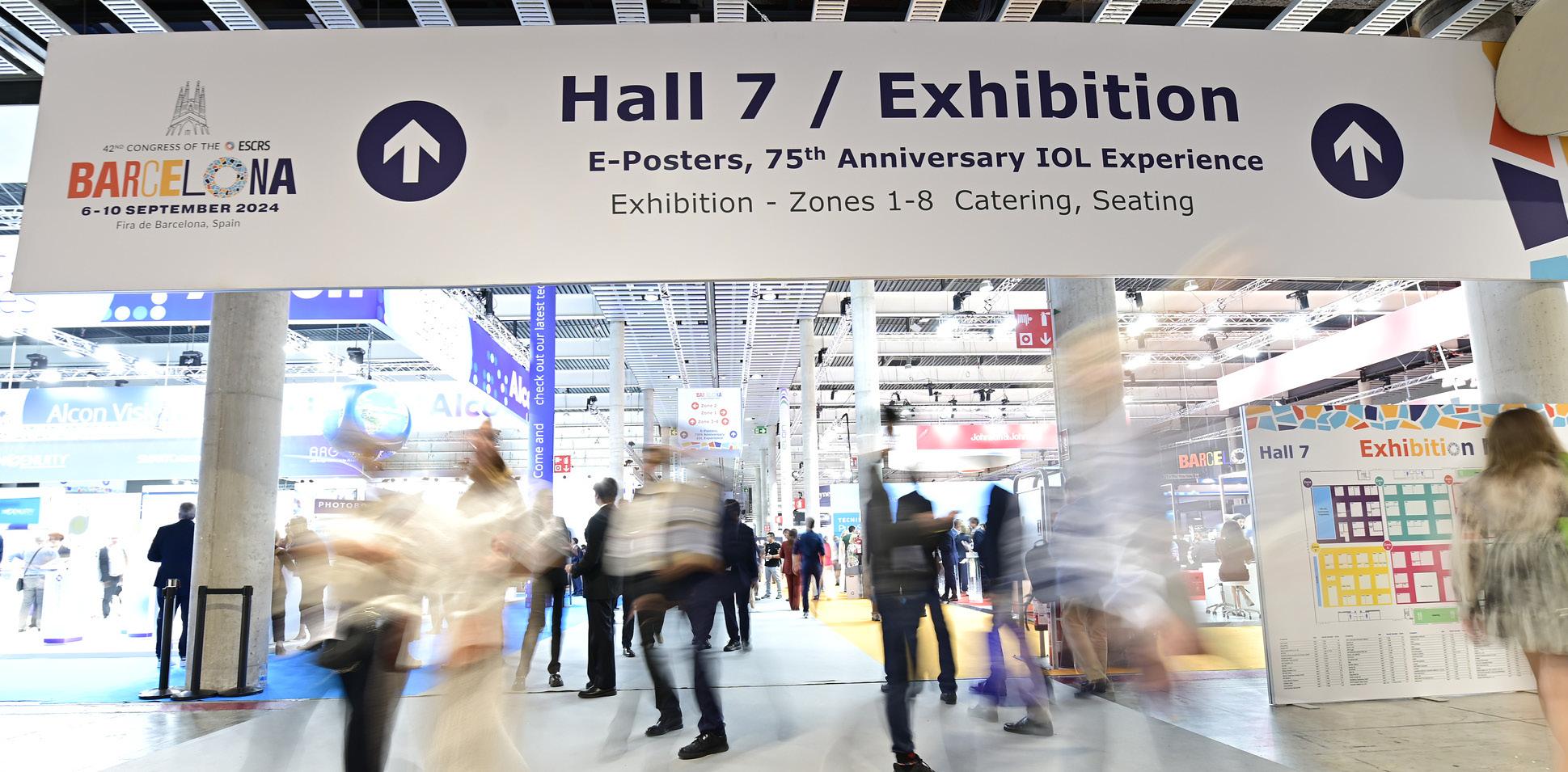
The 2024 Barcelona Congress draws record crowd.
As the 2024 ESCRS Annual Congress opened to a record crowd—nearly 16,000 registrants are on hand, of whom more than 10,000 are doctors—President Filomena Ribeiro portrayed a dynamic Society, changing and moving forward to meet the needs of both surgeons and patients the world over.
“This is very, very good after COVID times. We are growing and have even greater expectations,” she told several thousand attendees in Saturday’s Opening Ceremony.
In addition to awarding the Ridley Medal to Dr Abhay Vasavada and the Heritage Lecture Prize to Dr Richard Packard, Prof Ribeiro thanked the Congress hosts for welcoming ESCRS to Barcelona. “This is our third time in Barcelona, and I would like to thank our Spanish colleagues,” she said, acknowledging Dr Javier Mendicute, president of the Spanish Society of Cataract and Refractive Surgeons.
Prof Ribeiro spotlighted several features of the 2024 Congress programme during her remarks. She began by noting that this year’s Congress includes daily main symposia addressing needs identified by the Programme Committee and ESCRS surveys. The symposia topics range from the latest on keratoconus and IOLs to the future of refractive surgery and telemedicine in oph-thalmology.
Other programme highlights include the third ESCRS iNovation day, in which 10 panels and 18 emerging companies examined how technology innovations are meeting the most urgent clinical needs. More than half the attendees were doctors, Prof Ribeiro noted. She thanked Dr Vance Thompson for his work organising the day. Cornea Day and Glaucoma Day and the first Global Refractive Summit filled out Friday’s agenda.
Prof Ribeiro thanked Drs Oliver Findl, Burkhard Dick, and
Robert Osher for their work on the Near Live Surgery and video symposia focusing on getting it right, making the right call, and learning from getting it wrong. “We are a society of surgeons, so we need to bring a good pro-gramme on surgery,” she said.
Educational offerings at the Congress include 359 didactic and instructional courses, including 80 wet labs and 16 dry labs. The dry labs are new to this meeting and will be expanded at fu-ture conferences, Prof Ribeiro said. Masterclasses will again be on offer, including one on MIGS for 60 participants, while this year’s Leadership, Business, and Innovation (LBI) programme has been revised based on survey results to better meet member needs.
Prof Ribeiro noted that this year’s FEBOS-CR exam was a huge success, with a record 66% pass rate. “This is very good for us,” she said.
The 2024 Congress is noteworthy for its collaborative nature, reflected in Monday’s Global Active programme, featuring symposia with the American Academy of Ophthalmology, ASCRS, APACRS, the Pan-American Association of Ophthalmology, the World Society of Paediatric Ophthalmology and Strabismus, ORBIS, and the Ophthalmology Foundation. “We have challenges together that we can manage better as a broader community,” Prof Ribeiro said.
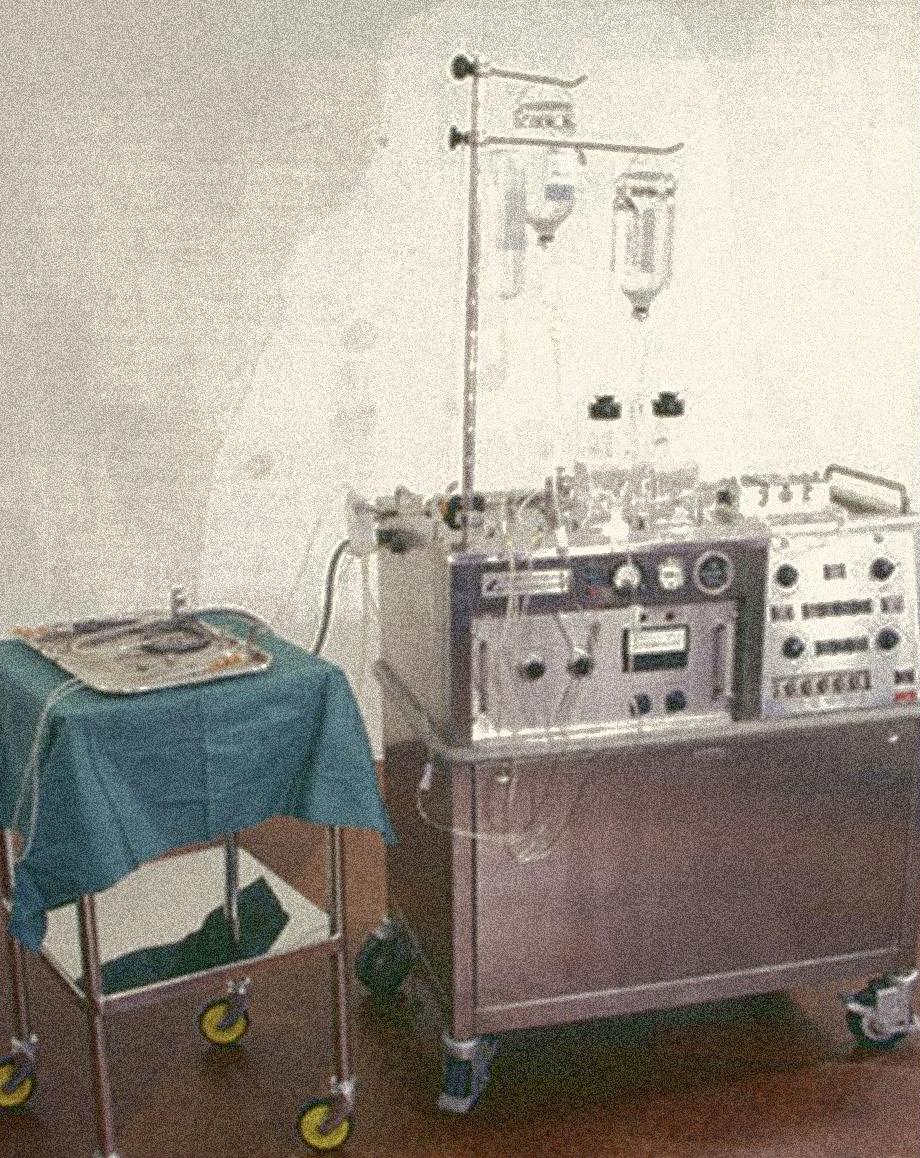
The opening ceremony also highlighted the 75th anniversary of the first IOL implantation, with Dr Richard Packard outlining Sir Harold Ridley’s journey from a shunned maverick to universal recognition for pioneering ophthalmic implants. Prof Ribeiro encouraged attendees to visit the “IOL Experience” exhibit in the exhibition hall, which includes replicas of a 1940s ophthalmic office and operating theatre, giving insight into how far ophthalmology has come and where it can go.

What started as quiet innovation reverberated into a global legacy that continues to save.
“One day, perhaps in 1947, a routine list of operations was performed. At the end, a student who had never before seen a cataract said, ‘It’s a pity you can’t replace the cataract with a clear lens.’ He was told that this was not usual, though many people, including myself, had suggested this project. However, no one had the temerity to take action.” – Sir Harold Ridley, inventor of the intraocular lens
Following this encounter, Mr Ridley, as he then was, went forward with the first intraocular lens (IOL).
He met with John Pike of Rayner and Keeler and, between them, realised the basic ideas of the project. Mr Ridley had been impressed during World War II by the apparent lack of inflammation caused by fragments of aircraft clear canopies when found in the eyes of injured crew. Pike asked his friend John Holt of Imperial Chemical Industries
in the UK to create clinical quality and hopefully biologically inert polymethylmethacrylate (PMMA).
The design he chose for the first IOL mimicked the shape of the human lens. It was inserted into a patient’s eye behind the pupil and hopefully into the capsular bag after an extracapsular cataract extraction. The actual date of the first implantation is not entirely clear. It may have been 29 November 1949, but it was removed and inserted as a secondary operation on 8 February 1950. It produced a gross refractive error of -14 D due to the IOL power calculation conducted in air, not liquid. The error was quickly corrected in subsequent implantations, and the operation promised the first “cure for aphakia,” as Harold Ridley put it.
Mr Ridley wanted to keep his invention a secret until he had sufficient clinical data. However, one of his implanted patients, when going for a follow-up visit, went to
see another ophthalmologist with the surname Ridley by mistake. With his secret out, Mr Ridley decided to go public at the Oxford Ophthalmological Congress in July 1951. He brought two of his patients, one with 6/6 vision unaided, to the meeting so colleagues could examine them. At the meeting was Sir Stewart Duke Elder, the doyen of British ophthalmology at the time, who refused to look at Ridley’s patients or watch the coloured movie of one of the implant procedures. This very negative attitude was mirrored by many senior ophthalmologists across the world.
Lacking haptics for support and weighing many times more than current IOLs, the earliest lenses tended to dislocate, sometimes months or even years after surgery. Despite this, some of the early IOLs continued to give good vision 20 years after implantation. About 15% of Ridley lenses were eventually explanted. Stabilising the implant was a problem that took more than 40 years to adequately solve.
Other frequent complications of early IOL surgery included postoperative infections, haemorrhage, inflammation, corneal oedema, peripheral anterior synechiae, raised
intraocular pressure, capsule and lens opacification, and residual refractive error.
Focusing on the problems rather than trying to find solutions, much of the global academic ophthalmic establishment vehemently opposed ocular implants for several decades.
However, the status quo was not acceptable. “Spectacles for aphakia were horrendous—they magnified and distorted the image, and many patients never really adapted to them. The gross anisometropia made uniocular surgery impossible to rehabilitate,” said Professor David J Spalton, who, as a trainee in the mid-1970s, was among the last to assist Harold Ridley in an implant procedure.
Implants restored normal vision, and “there was a lot to be said for that. It was just a matter of getting the design and techniques right for it,” Prof Spalton said.
To bring together those interested in lens implantology, Mr Ridley and Peter Choyce, a very early IOL pioneer, formed the Intraocular Implant Club (IIC) in 1966. The founder members of what became the International Intraocular Implant Club (IIIC) came from many countries. In the US, it took another decade before Harold Ridley was recognised for his accomplishments at a meeting of the
Mr Ridley wanted to keep his invention a secret until he had sufficient clinical data.
American Academy of Ophthalmology in 1976. For Mr Ridley, the greatest of all his achievements by way of scientific recognition was admission to The Royal Society of London in 1986. Public recognition eventually came after lobbying of a prime minister’s wife when he was knighted in 2000.
Along the way, enterprising surgeons, researchers, and manufacturers made most of the technical innovations. “It was driven by individuals who put a lot of time and thought into the complications and how you would avoid them,” Prof Spalton said.
“It’s truly remarkable to witness the ongoing evolution of these technologies, underscoring our commitment to providing tailored solutions for each patient’s unique visual needs. Continuous progress in the field not only enhances our surgical capabilities but, more importantly, significantly improves the quality of life for those seeking visual correction after cataract surgery,” ESCRS President Professor Filomena Ribeiro said.
David J Spalton FRCS, FRCP, FRCOphth is an ophthalmologist in London, UK, and a former ESCRS president. profspalton@gmail.com
Filomena Ribeiro MD, PhD, FEBO is head of ophthalmology at Hospital da Luz Lisboa, Portugal, and ESCRS president. filomenajribeiro@gmail.com
A novel procedure promises to make allogenic intrastromal ring implantation easier and more effective.
The introduction of corneal allogenic intrastromal ring segment or CAIRS by Dr Soosan Jacob in the mid-late 2010s was a welcome addition in treating non-CXL-eligible patients with keratoconus, an important step forward from the classic PMMA intrastromal rings (with far fewer side effects in severity and frequency), and a new alternative to corneal transplantation.
Despite the innovative approach and the ironclad rationale, introducing soft corneal tissue in the stroma is not an easy task, leading experts to strive for a way to make the procedure less challenging. Dr Shady Awwad was the first to propose stiffening the corneal rings through a process of dehydration, an idea that made the insertion procedure a bit easier but lacked efficacy by comparison.
Inserting a CAIRS has a steep learning curve, since the surgeon is dealing with soft tissue. Even using the technique conceived by Dr Awwad has some procedural difficulties, Dr Cosimo Mazzotta observed. Dehydrating a CAIRS can be helpful in terms of insertion, added Dr Marco Zagari, but surgeons end up with a stiff ring that might not have the same efficacy as the non-processed one.
According to both Mazzotta and Zagari, finding common ground between ease and efficacy was the key to improving this procedure, and the best way to achieve this goal was to use riboflavin and UV light.
To find the lowest common denominator, Dr Zagari noted it was necessary to improve Dr Jacob’s idea through Dr Awwad’s mindset. Keeping that in mind, Dr Mazzotta added the decision was to make allogenic intrastromal rings stronger, but not stiffer, using corneal cross-linking.
Processed with a vector-based customised nomogram, the rings obtain a ‘gummy bear’-like solidity, effectively exceeding the dehydrated rings in terms of ease of use. Dr Mazzotta observed this is unheard of in the field of corneal surgery, a completely distinct perspective that generated something brand new and feasible for surgeons globally.
It is a solution that offers high rates of repeatability and opens previously impossible new prospects, Dr Zagari said. Everything is calculated using topographic data from both donor and recipient and precisely cut with a femtosecond laser—based on a specific nomogram designed by the authors and vectorial analysis provided by MS-39 CSO tomography.
Soon it will be possible to calibrate levels of elasticity and elastic recoil with the potential to have a ring that is perfectly tailored to the patient’s needs, he added.
The PMMA-like consistency of cross-linked CAIRS makes the insertion like the non-allogenic intrastromal rings, underlining how the procedure does not require a second point of access. Moreover, the low or absent immunogenicity of cross-linked and decellularised collagen completely reduces the risk of rejection.
Drs Mazotta and Zagari conducted a preclinical study with the Siena Crosslinking Centre and the Veneto Eye Bank Foundation, with its medical director Diego Ponzin. The study has been presented to the Siena Crosslinking Centre ethical committee, before entering the clinical phase, Dr Mazzotta said. For more information, see C Mazzotta, et al., “Crosslinked All-Femtosecond laser-cut Corneal Allogenic Intracorneal Ring Segments (AFXL CAIRS): Pilot Ex-Vivo and In-Vivo Study in Italy,” Preprints, (2024): 2024081945. As of today, the first all femtolaser-cut X-linked (AFXL) CAIRS has already been implanted in patients with keratoconus in Italy, with very promising results and well-responding patients, Dr Zagari concluded. Dr Mazzotta will present a course covering this topic, “What’s New in Early Diagnosis, Pathophysiology, and Prevention Strategies of Keratoconus,” which takes place Monday, 14:00–15:30, 8.1 P.
Cosimo Mazzotta MD, PhD is founder and scientific director of Siena Crosslinking Centre and adjunct professor at the University of Siena, Italy. cgmazzotta@libero.it
Marco Zagari MD is a surgeon at the Polyclinic European Centre of Aci Castello, Italy. marco.zagari@ hotmail.com
Green and clean
Innovative eco-design saves resources
Less waste and lower disposal costs
Swiss made Medicel quality



































































































Survey participants will be entered into a raffle to receive free delegate registration for the 2025 ESCRS Annual Congress in Copenhagen and a summary report before publication.
The 10th annual ESCRS Clinical Trends Survey is launching at the 2024 Congress in Barcelona. This survey builds upon the success of prior surveys, which have included more than 14,000 participants.
The survey asks ESCRS delegates key questions regarding issues they regularly face in their practice. The goal is to obtain opinions from a significant percentage of delegates for ESCRS leadership to review. Using previous surveys as a foundation, the 2024 edition adds questions in evolving clinical and technology areas such as retina.
Data from prior surveys have helped develop content for many of the symposia at this year’s ESCRS Clinical Forum IME programmes. Information from the upcoming survey will continue to drive these efforts and discover new areas of education.
The 2024 ESCRS Clinical Trends Survey includes a wide range of contemporary topics, such as:
• Cataract extraction
• Presbyopia correction
• Astigmatism management
• Ocular surface disease
• Glaucoma
• Cornea- and lens-based refractive surgery
• Retina
• Medical education
Keep your professional journey moving forward after the Congress by becoming an ESCRS member. You’ll join a network of leading ophthalmologists dedicated to advancing the science and business of cataract and refractive surgery.
For more information about ESCRS membership, visit the ESCRS booth in the exhibition hall or visit us online at escrs.org. You can also follow us on major social media outlets including LinkedIn, X, Facebook, and Instagram.

The survey can be completed in person at the ESCRS Congress in Barcelona at the Survey Lounge in Exhibit Hall 6 on 6–8 September. Seating and refreshments will be provided to those who participate. If you are unable to complete this survey during the Congress, we encourage you to take this 15-minute survey by going to https://tfgedu.questionpro.com/ESCRS2024. Please complete the survey as soon as possible, as it will close in October.
By completing the survey and filling in an email address, respondents will be entered into a raffle to win free registration for the 2025 ESCRS Congress in Copenhagen. Additionally, every participant will be emailed a summary of the data shortly after it’s compiled. Finally, and most importantly, by completing the survey, respondents will provide essential data that helps drive future education programming. Respondents can remain anonymous, if desired, and still give ESCRS important feedback.


ESCRS aims to build a sustainable and inclusive society.
The Barcelona Congress will introduce to its new BOSS (Building Our Sustainable, Inclusive Society) programme, which will be one of the key ESCRS initiatives in the coming years. Under the guidance of ESCRS President Filomena Ribeiro and BOSS Working Group Chair Mor Dickman, a comprehensive multi-year programme has been developed with ESCRS consultant Kristine Morrill.
“We started working on the inclusivity programme more than one year ago, so it is exciting to reach this point and share it with the ESCRS membership, as well as the wider ophthalmic community,” Professor Ribeiro said. “The goal of the BOSS programme is to foster an environment where every ESCRS member feels that they have a voice in the Society and feel valued.”
Those interested can visit a related podcast and a new BOSS-focused section of the ESCRS website (https://www. escrs.org/boss/), where they can meet the working group members, watch videos from the team discussing inclusivity and related topics, and visit a library curated by Sotiria Palioura, a member of the working group.
“Building the BOSS programme has truly been a team effort, with everyone getting involved to develop the Barcelona activities and the ongoing programme that will take place throughout the year,” Prof Dickman said. “The themes of leadership and mentorship will be central to our work in the months ahead.”
Two symposia anchor the BOSS programme, with the first opening the annual meeting on Saturday at 8:45 in the Plenary Hall. Entitled “Hidden Bias in Science,” attendees can expect discussions on bias in scientific research, publications, and AI tools.
Jointly organised by the ESCRS Practice Management Committee (Leadership, Business, and Innovation), the second symposium on Monday morning (9:00–11:00) is titled “Leadership and Mentorship in an Inclusive Society.” This symposium will feature industry leaders and the leaders of ASCRS, AUSCRS, BRASCRS, and AAO.
In between, there will be Speed Mentoring Sessions, a workshop on hidden biases by Project Implicit, an instructional course on hidden biases led by Australian surgeon Tanya Trinh, and opportunities to network, including Sunday evening in an event sponsored by Ophthalmic World Leaders (OWL).


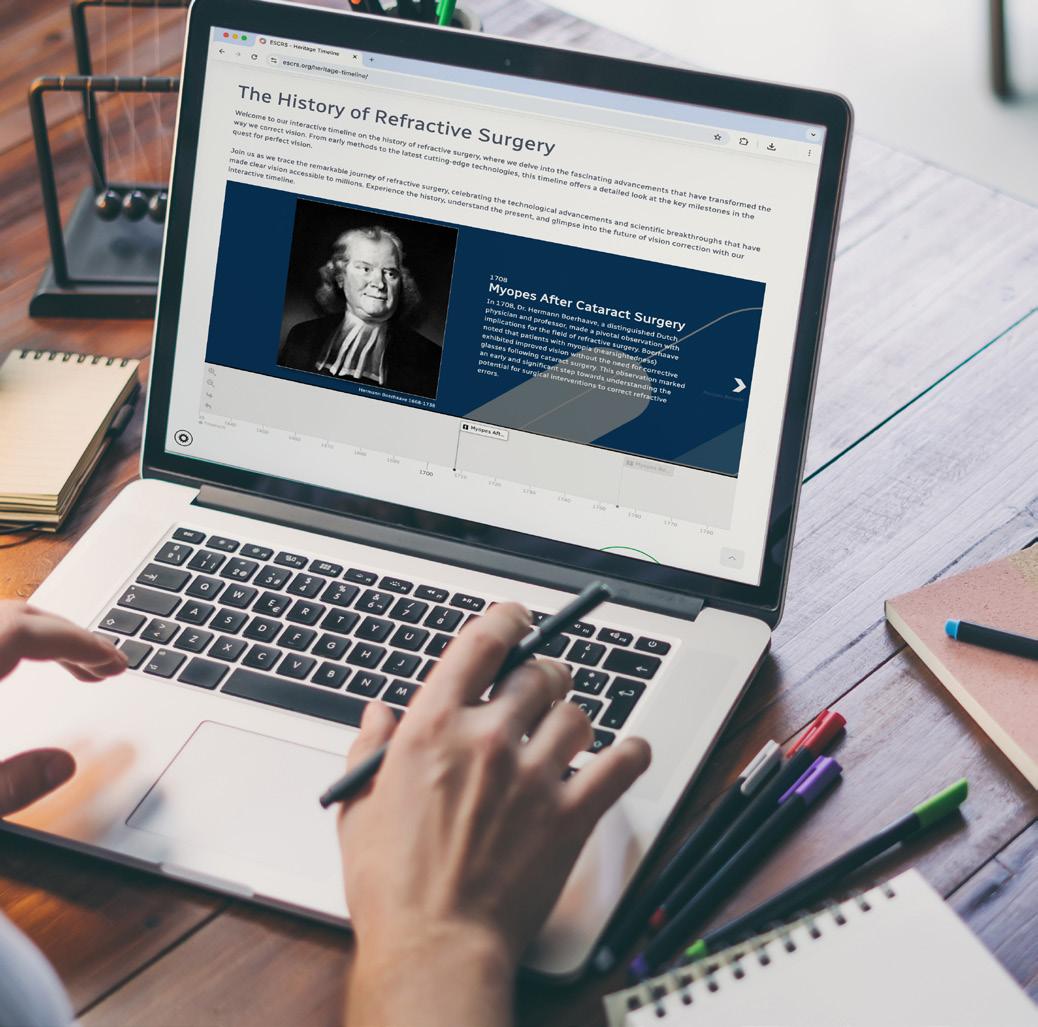
Heritage Lecture to explore the history of the innovative procedure.
This year’s ESCRS Heritage Lecture will recount the story of phacoemulsification from the moment its inventor, Dr Charles Kelman, conceived of it during a eureka moment in a dentist’s chair.
The lecture, “High Wire Act to the Standard of Care: Charlie Kelman and the History of Phacoemulsification,” will be delivered by Dr Richard Packard.
Dr Packard, who first started to perform phacoemulsification in 1979, qualified as a doctor in 1970 from the Middlesex Hospital Medical School after residency at Moorfields Eye Hospital. In December 1978 he went to Charing Cross Hospital as senior registrar, working under Eric Arnott.
Dr Packard retired as senior consultant at Arnott Eye Associates in London in 2022. He had been surgeon at the internationally renowned Prince Charles Eye Unit in Windsor, England.
In 1981, Dr Packard published the first description in the medical literature of the use of a folded soft lens in cataract surgery. Since then, he has continued to teach phaco techniques as well as participate in the development of new intraocular lenses, phaco machines, and other instrumentation.
He was a board member of ESCRS from 1999 to 2007 and has chaired the ESCRS Video Competition Judging Panel since 2000. He is on the Society’s Education Committee and runs the Cataract Surgery Didactic Course.
He has lectured in more than 60 countries and presented many named lectures, including the IIIC Medal Lecture for 2014, the ESCRS Binkhorst Lecture in 2015, the Fyodorov and King Khaled Memorial Lectures in 2018, and the UKISCRS Choyce Medal Lecture in 2021.
In 2018 Dr Packard was the honoured guest of the American Society of Cataract and Refractive Surgery. In 2019, he
published The History and Evolution of Modern Cataract Surgery with Lucio Buratto, with whom he published The History of Refractive Surgery the following year.
The lecture takes place at 10:30 in the Plenary Hall.



The Building Our Sustainable, Inclusive Society (BOSS) team will introduce the first-ever Speed Mentoring Sessions at ESCRS 2024. Scheduled 6–9 September, these sessions offer a new format for professional development by facilitating brief, focused interactions between emerging talent and more than 40 experienced experts in ophthalmology.
Founded by ESCRS President Filomena Ribeiro, 2024 also marks the inaugural launch of the ESCRS inclusivity initiative. “The purpose of BOSS is to foster an environment within ESCRS where everyone feels they have a place,” said Kristine Morrill, ESCRS consultant and BOSS member. “We’ve created a year-round programme that gives opportunities for members to network and create an environment for career and personal development.”
Each mentorship session will last one hour and allow mentees ten-minute discussion rotations with six mentors, offering the opportunity to benefit from diverse perspectives and expertise with mentors coming from various domains within ophthalmology, including ESCRS leadership, prominent ophthalmologists, and industry innovators. The overwhelming interest in these sessions has already led to a complete booking of all available spots, reflecting the high demand for mentorship opportunities at the Congress.
“We’ve been really surprised and grateful by the response,” explained Morrill. “The mentors are senior leaders in
the industry, key opinion leaders from all around the world, and even the first and second female presidents of ESCRS, Marie-José Tassignon and Béatrice Cochener-Lamard.”
These interactions are designed to provide valuable career advice, share insights into various sub-specialties, and offer guidance on navigating the ophthalmic field. Mentees can expect personalised feedback and answers to specific questions during the one-on-one discussions.
The sessions will cover a range of topics, including the latest trends in ophthalmology, research advancements, and career development strategies. This tailored approach ensures participants gain relevant insights to stay ahead in their profession and can help foster networking connections that could benefit their careers for years to come.
Expected to be a standout feature, the introduction of Speed Mentoring at ESCRS 2024 highlights the importance of mentorship in professional development. Studies have consistently shown mentorship plays a crucial role in career success, and these sessions provide mentees with the opportunity to build their professional networks.
In addition to the speed mentorship, BOSS has organised a series of events designed to foster inclusivity and networking among attendees, including the Boss Networking Mocktail Party. This new initiative underscores the Society’s dedication to supporting the growth and development of the next generation of ophthalmology professionals.







Everyone is susceptible to bias, regardless of conscious beliefs.
LAUREN BLANCHARD REPORTS
On Saturday at the ESCRS Congress, the BOSS “Hidden Bias in Science” symposium examined the impact of unconscious bias in scientific research and healthcare. Chaired by BOSS Working Group Members Dr Mor Dickman and Kristine Morrill, the symposium featured the presentation “What is Implicit Bias?” by Amy Johnson, executive director of Project Implicit.
Johnson began by explaining the core concept of implicit bias, a form of unconscious bias that subtly influences our perceptions and actions. “Implicit bias is a concept that influences our everyday lives, often without us realising it,” she said. “It can shape how we understand and treat others. In healthcare, these biases can impact patient care and colleague relationships.”
Project Implicit is a non-profit organisation committed to advancing scientific knowledge about stereotypes, prejudice, and other biases. Their researchers explore how implicit bias informs attitudes and unconscious beliefs, affecting decision-making and behaviour. They offer educational services with actionable strategies people can implement to build awareness and mitigate implicit bias.
Implicit bias, Johnson noted, “operates automatically” and is “universal,” meaning everyone is susceptible to these biases, regardless of their conscious beliefs. “Implicit biases often do not align with our stated values and beliefs,” she added. “Even if we believe in equality, implicit bias can still affect our actions. These biases often reflect the default assumptions of the society in which we live, which we absorb over time without realising it.
“Biases influence judgments and decisions, and addressing these biases is crucial for ensuring decisions are fair and based on accurate information, rather than assumptions
we make about the people we treat or the people we work with,” she continued. “They can lead us to make decisions that perpetuate systemic inequalities.”
Johnson recommended multiple ways to counter implicit bias, the most important being self-awareness: “By becoming aware, we can start to identify when these biases may be influencing our decisions and take steps to counteract. Understanding that having biases is normal, not a moral failing or indicator of prejudice, allows us to address them with humility and a commitment to improvement.”
Other recommendations for countering bias included objective processes, such as structured decision-making tools like checklists or standardised criteria, to help minimise the influence of subjective impressions and stereotypes, and daily reflections. She additionally recommended mindfulness, as staying present can help disrupt bias.
“Taking a moment to consider a different person’s perspective than our own can interrupt automatic thinking.”
Employers implementing these changes might find conflicts arise between colleagues, however.
“You’re going to have conflicts, and avoiding them isn’t necessarily the right answer,” Johnson said. “Instead, you should be curious after listening to someone else’s perspective. Often, we’re listening to people in order to respond to them, rather than listening to understand what they’re saying. Use empathy to put yourself in their shoes, ask proactive questions, and try to understand where they are coming from.”
Those interested in learning more about their biases can use Project Implicit’s Implicit Association Tests, which provide insights into unconscious attitudes. For these tests and other educational resources on implicit bias, visit projectimplicit.net.
Author: Yoram Gonen, CEO Hanita Lenses
For over 40 years, Hanita Lenses has been at the forefront of manufacturing high-quality IOLs, competing successfully and achieving consistent global growth. In the last 15 years, we have transitioned from a local, conservative company into a dynamic, premium, and innovation-focused organization. This transformation, driven by a talented, cohesive, and energetic team with strong engineering and manufacturing expertise, has allowed us to bring new and exciting solutions to ophthalmologists who seek the most advanced and reliable products - ultimately providing patients with true spectacle independence
The INTENSITY Pentafocal Lens, based on our proprietary Dynamic Light Utilization (DLU) technology, exemplifies the spirit of innovation that has become a cornerstone in how we think and create. Over 30,000 patients worldwide have experienced its outstanding optical performance, enjoying smooth vision at all distances with minimal disturbances. This success has been demonstrated time and again in patient satisfaction surveys and clinical studies. The overall feedback is nothing less than WOW.






"A patient that gets the Intensity lenses enjoys a life that is uncompromised. With the Intensity Pentafocal IOL, the patient forgets about their lenses because vision is a non-issue."


Defocus Curve
Visual Acuity(logMAR)
Monocular (356 eyes) Binocular (241 patients)
Defocus (D)
Figure 1: real-world data reveals that from distance to 40 cm, patients achieve a visual acuity of 0.1 LogMAR or better without any drop in visual performance across the full range of vision - a common limitation in older-generation lenses.
Guided by our belief that "Everyone deserves to see the world's beauty," we are committed to developing technologies and solutions that provide unique added value to patients. We collaborate with our global advisory board, university experts, and research institutions to stay at the forefront of medical advancements in the field.
Monocular VA at different distances

— Prof. Dr. med. Gerd Auffarth


These studies show that the Intensity lens delivers photopic and mesopic vision levels comparable to the phakic population, with patients reporting freedom from glasses and the ability to engage in any activity. A particularly notable study from Japan looked at the number of patients satisfied with night driving – the number of Intensity patients was twice as high as the patients using older presbyopiacorrecting lenses.






The Intensity lens delivers photopic and mesopic vision levels comparable to the phakic population, with patients reporting freedom from glasses and the ability to engage in any activity.





Visual Acuity(logMAR)

Distance (cm)
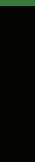
Figure 2: monocular visual acuity, real-world outcomes of 1118 eyes. High visual acuity is maintained along the whole visual range.
To better support our high-end premium clients, we have established five subsidiaries in key markets across Europe and Asia. In 2025, we will launch a second advanced manufacturing site to meet the demands of our fastgrowing Asian markets.
We strive for excellence in every aspect of our business, eager to succeed, and ready to embrace the challenges ahead.

LAURA GASPARI REPORTS
As 2024 marks an important year for ESCRS in raising awareness of diversity, equity, and inclusivity (DEI) issues in ophthalmology, many challenges need to be acknowledged and faced, according to ESCRS President Filomena Ribeiro MD, PhD, FEBO and ESCRS consultant Kris Morrill.
Professor Ribeiro stated clearly that social responsibility, equity, and inclusivity would be the priorities ESCRS will embrace during her tenure as president.
“Diversity and inclusion are about making sure everyone feels welcomed and respected for who they are,” she said. “It is about understanding and appreciating that people are different in many ways.”
Most know uniqueness is strength, not weakness: in ophthalmology, it can bring different perspectives and experiences, enhancing innovation to achieve better results. Many challenges currently serve as obstacles to more inclusive, equal, and diverse ophthalmology, such as the under-representation of minorities (especially in leadership positions), unequal career, mentorship, and surgical training opportunities. Additional discrimination factors
include gender identity, sexual orientation, age, religion, and political views.
The more visible example is the representation of women in ophthalmology, especially as surgeons. A recent survey published by the Journal of Cataract & Refractive Surgery on surgical training in Europe revealed female specialists reported a mean 18% fewer entire cataract surgical procedures than their male counterparts. Women also felt less confident about their surgical skills, and female residents in ophthalmology reported continued gender bias.
“In 2024, we should not see barriers if people want to become surgeons in ophthalmology. There should be pathways to do that,” Kris Morrill stated. “It is very difficult to become a sur-geon in certain countries—especially for women, because of family issues, motherhood, et cetera. This should not be happening, and we need to stop it.”
One of the greatest barriers to overcome is unconscious bias, or judging someone based on stereotypes and cultural backgrounds without even realising it. “The first step is to understand nobody is immune to unconscious bias and all decision-making processes we make are influenced by it,”
Prof Ribeiro said. In this regard, ESCRS collaborated with Project Implicit, a think tank led by scientists from Harvard University and the University of Virginia, in refining an online tool to measure unconscious biases.
“The immediate reaction I saw from most people was saying they had no biases; they were very open-minded and made no judgements,” explained Ms Morrill. “Then, you start to dig in a little deeper and realise every single decision we make is based on some preconceptions in our minds. So, you start to scratch the surface and start to think twice about decisions and how you react to people. It is a very interesting process.”
ESCRS is tackling this issue by introducing new activities addressing it, such as the workshop last Winter Meeting in Frankfurt. “Leaders need to face this challenge to start a process of change that should be transversal to all members,” Prof Ribeiro affirmed. The next step, she said, is involving membership and industries. Frankfurt’s escape room experience took a step towards that, providing an opportunity for people to work together.
The ESCRS annual meeting in Barcelona will have a DEI symposium, workshops, and instructional courses. Most
importantly, ESCRS is preparing a survey for its members to assess the real obstacles to DEI issues they face, using their input to develop a more effective DEI strategy. The survey is based on the one proposed by the British Hip Society and published in the British Medical Journal.
“As their demographics reflect ours, we asked their permission to use their survey with adaptations to ophthalmologists and to benchmark against another surgical society,” Ms Morrill explained. The hope is this survey will establish a baseline as there is no existing data on the topic, according to both Prof Ribeiro and Ms Morrill. A good starting point is reflecting on the issue and working towards a common goal, even if the change will not be fast and smooth.
“I think people should plan to attend activities in Barcelona to learn and understand where we stand today as a Society, as well as where we want to go,” Ms Morrill concluded.
Even if surgeons think they know the way forward, Prof Ribeiro encourages attending the sessions willing to learn.
“It is important to be open-minded and willing to learn from others who are different from us,” she concluded. “By taking these steps, we can help break some barriers and create a more inclusive environment for everyone.”




LAURA GASPARI REPORTS
Mitomycin Intravascular Chemoembolization (MICE) continues to demonstrate efficacy in the surgical treatment of corneal neovascularization (NV) and lipid keratopathy, according to Dr Michael Mimouni.
“In order to have optimal optical clarity and optical vision, you need to not have any blood vessels in the cornea,” he stated.
Corneal NV results in the formation of lipids onto the cornea, astigmatism, scarring, haze, and eventually loss of vision. Herpes keratitis and blepharokeratoconjunctivitis (BKC) are among its causes. However, even if the ophthalmologist treats the underlying causes, the blood vessels are still there, making surgery the primary outcome.
“Some of the surgical options include fine-needle diathermy, but the problem is you put a needle in the cornea, which can lead to perforations,” Dr Mimouni said.
He further noted a retrospective study on 17 eyes reported that 82% required retreatment due to corneal NV recurrences, and there were microperforations in deeper vessels.
There are also treatments with subconjunctival (or intrastromal) injections of anti-VEGF (such as bevacizumab)— but these only seem to work on patients with a recent onset of corneal NV, and some studies had to stop due to the inefficacy of the treatment.
So, what is there to do?
MICE is a term coined by Dean P Ouano, and it is a very recent and promising technique for well-formed corneal NV. Performed under an ophthalmic microscope, the surgical procedure involves putting a 1.0 cc syringe filled with mitomycin C at 0.4 mg/mL concentration attached to a 33-gauge TSK needle angled 15 degrees away from the ocular surface within the corneal stroma.
Dr Mimouni suggested a look at the reflux of heme at the needle edge to know if one is in the correct position. “Make sure that when you perform it, you are actually injecting it into the blood vessel itself and not into the surrounding stroma if you want to achieve the best possible results for your patients.”

Then, injection starts and the vessel blanches. “The mitomycin disperses into the entire network of the blood vessels and destroys its inner lining. After a few days, the blood vessels start to dissolve, and after a few weeks, they are no longer there, and you eventually see them completely regress,” he commented. “The more you wait, the more the lipid that was on the cornea starts absorbing, achieving great results.
“When it comes to MICE, less is more: you only need 0.01 to 0.05 mL. From my personal experience, we had good results with corneal NV secondary to herpes and BKC, but I am sceptical about corneal NV and filled graft,” he said. “And finally, of course, avoid performing a MICE on corneal NV related to limbal stem cell deficiency, that is a completely different ideology.”
Michael Mimouni MD is a Cataract, Corneal, External Diseases, and Refractive Specialist at the Department of Ophthalmology, Rambam Health Care Campus, Haifa, Israel.





LAURA GASPARI REPORTS
New drugs for neurotrophic keratitis (NK) are currently undergoing clinical trials, which may result in superior efficacy and/or decreased adverse effects, according to Dr Pedram Hamrah.
NK is a significant loss of quality of life for patients, Dr Hamrah said, further defining it as a neurotrophic disease correlated with loss of neurotrophins. The fundamental role is played by neurotrophins in the cornea, which help the corneal nerve regeneration.
The first drug ever approved by both EMA (2017) and FDA (2018) for NK is the Recombinant Human Nerve growth factor (rhNGF) 0.002% (cenegermin-bkbj), with a 70% efficacy demonstrated by studies, compared to roughly 30% effect in the placebo control group.
“However, despite epithelial closures, there was no improvement in corneal sensitivity or visual acuity measurements at the time of the studies, with disease recurrence in the follow-up,” Dr Hamrah noted, adding there were also some adverse effects, the most common being eye pain and ocular discomfort. “Several studies have shown an increase in the sensitivity of the corneal nerves in stage 1 patients but not stage 2 cases.”
Therefore, new drugs in the pipeline are needed to treat NK patients. One is platelet-rich plasma, which includes platelet-derived growth factor, epithelial-derived growth factor, fibroblast growth factor, and TGF—in addition to NGF and insulin-like growth factor. Studies have shown considerable ulceration healing, particularly in combination with preservative free tears in stage 1 cases; more clinical trials are coming, with an estimated completion date of next year. RGN-259 (Thymosin β4) is a peptide with 43 amino acids that promotes corneal wound re-epithelization, diminishing inflammation and inhibiting apoptosis.
“Previous studies have shown healing in nine patients with NK and ulcers, and there is currently an ongoing
randomised phase III trial, which resulted in healing at four weeks,” Dr Hamrah said.
Anothr drug he cited was KPI-012-C-001, a human mesenchymal stem cell secretome. “Mesenchymal cells are self-renewal, multicoding stem cells,” he explained. “They can be isolated in humans, and they can secrete neurotrophins, IGF, hepatic growth factors, and TGF.”
These drugs show good results in clinical trials: Connexin43 antisense oligonucleotides, for example, which is a gap junction protein that facilitates communications of the epithelial cells, results in the improvement of the adhesion of the epithelial to the stroma.
“The previous studies showed an improved closure of the epithelium. It is currently in clinical trial in two trials,” he said.
Topical insulin was considered and used for a while, as it mimics IGF-1 and plays a role in cellular growth, corneal repair, and healing regulating cell growth, proliferation, and metabolism, as demonstrated in several ongoing studies on animals and humans.
Lastly, MT8 (or REC 0559)—a low molecular weight, synthetic peptide-mimetic of NGF—binds the TrkA receptor, mimicking the anti-apoptotic and corneal trophic activity of NGF and CSB-001 (a human recombinant hepatic growth factor), both showing promising results. New neuro-regenerative therapies with multiple concurrent neurotrophins also showed very good outcomes.
“There are new cell-based therapies coming, like Plasmacytoid dendritic cells, which have been shown to be necessary for the neuronal homeostasis and demonstrated to be able to secrete all neurotrophic factors and increase neural regeneration,” he concluded.
Pedram Hamrah MD specialises in Cornea, External Disease, and Cataract Services in Boston, US.
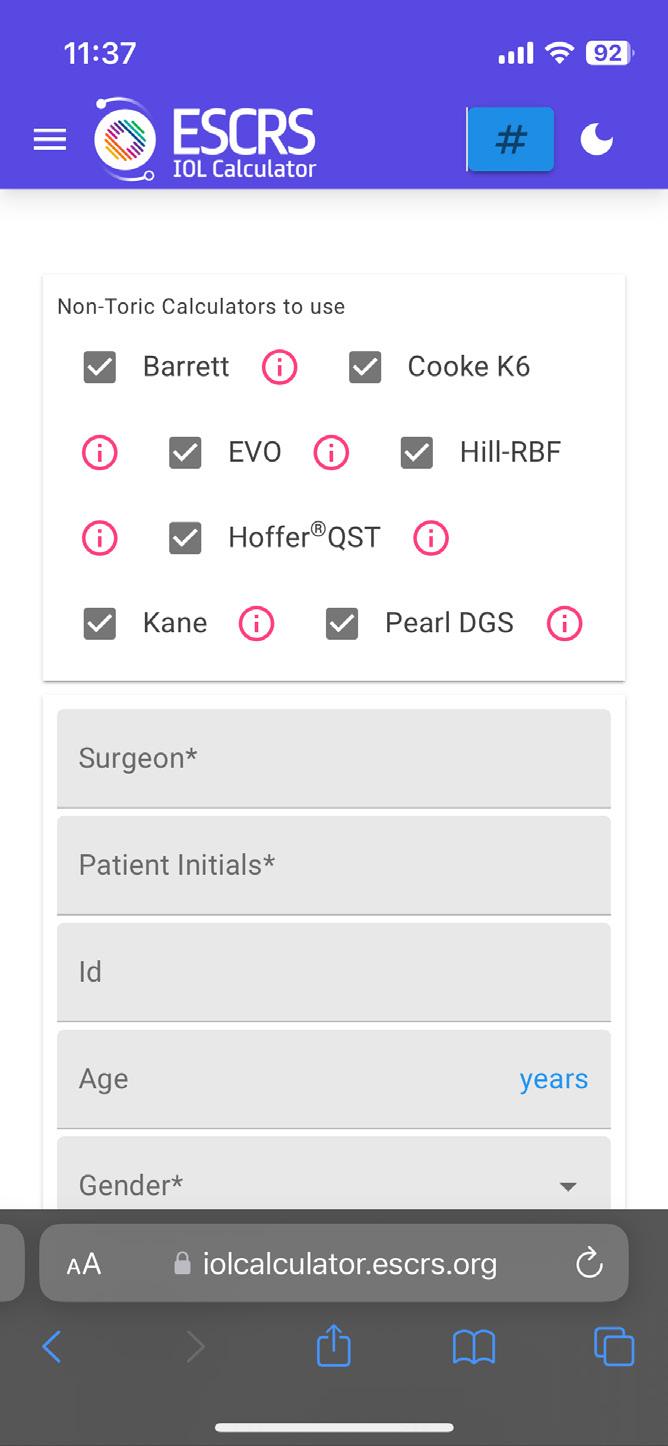
The ESCRS online IOL calculator is becoming more powerful and useful with the addition of calculations for toric IOLs and ongoing efforts to include calculations for keratoconus and cases after refractive surgery.
Launched in 2022, the calculator has quickly proved its value, receiving more than 450 uses per day. The calculator employs web scraping to aggregate results from several current calculators, including Barrett, Cooke, Evo, Hoffer, and Kane, thereby allowing ophthalmologists to obtain multiple results with only one data entry session.
“The IOL calculator stands as a testament to innovation and collaboration within the ophthalmology community, bringing together experts with the shared goal of enhancing patient outcomes,” says ESCRS President Filomena Ribeiro.
Developed by Dante Luis Buonsanti and Miguel Raimundo, the calculator is gradually broadening its reach and attracting interest from other formula creators wanting to collaborate with ESCRS. In addition to the keratoconus and post-refractive calculations under development, possible longer-term enhancements include:
• Incorporating artificial intelligence more deeply into the calculator so surgeons can better understand the variables between different eye/lens structures;
• Refining and customising the user interface so each user can log in and check their historic calculations; and
• Collating more specific data points around patients who have already gone through laser eye surgery and those who have had cataracts. iolcalculator.escrs.org



Discover the power of CASIA2 through real-world cases provided by eye care professionals like you. In this brochure, we proudly present a collection of diverse patient experiences that showcase the versatility and clinical utility of CASIA2 Cornea / Anterior Segment OCT.
Dive into the insights, outcomes, and lessons learned from these cases. See firsthand how CASIA2 is transforming ophthalmic care.


TIMOTHY NORRIS REPORTS
With 1.8 billion people with presbyopia in the world, the idea of an intraocular lens able to effectively simulate accommodation could be a perfect goal. Professor Thomas Kohnen posits there is interest for companies and researchers to find a feasible solution.
According to a recent article he published with prominent members of ESCRS in the Journal of Cataract & Refractive Surgery, there are five types of premium IOLs: monofocal aspheric, monofocal plus, multifocal, EDOF, and accommodative.
Focusing on the accommodative lens, Prof Kohnen added optic shift, dual optic design, and fluid-filled intraocular lenses help to define the subgroups.
For optic shift, the optic moves forwards or backwards depending on the contraction of the ciliary muscles, like the TetraflexHD and the Crystalens, which represent the early generation of accommodative lenses. The problem with the early generation, Prof Kohnen said, was they did not prove totally capable of satisfying different aspects of everyday life, such as reading and intermediate visual acuity.
The second group, the dual optic design, considers two optics that work by changing the anterior optic position in relation to the posterior optic, which he observed presented a better set of outcomes than previous generations. However, they had more dysphotopsia as they were mimicking the natural lens.
He noted the last category, fluid-filled intraocular lenses, will be a focus for the future. “And if we can achieve it, we will probably find the principle that works perfectly,” he said. “The idea of performing a real and natural accommodation is the goal.”
These fluid-driven intraocular lenses are made using proprietary hydrophobic acrylic material with lens and haptics filled with a proprietary, index-matched silicon fluid in a quantity measuring a little bit less than a drop. The capsular bag squeezes a thin amount of fluid from the haptic to the lens, which inflates the lens optic. On the other hand, he said, near vision deflates the optics.
According to Kohnen, there should be a push on the market to further develop accommodative intraocular lenses.
“Accommodation is really promising, but unfortunately, not all devices are reaching the market,” he said. “We have a hope for the future that fluid-filled intraocular lenses may have success. So, I’m really looking forward to the research we can do, because accumulated lenses will potentially be the future. The only question is if it will come in 5, 10, or 20 years. So far, we have a lot to offer to our patients.”
Thomas Kohnen MD, PhD, FEBO is Professor and Chair, Department of Ophthalmology Goethe University, Frankfurt, Germany. kohnen@em.uni-frankfurt.de
There were many obstacles to what has become modern cataract surgery, the surgery of any type with the highest safety and patient satisfaction. Pioneers took chances and faced both scientific and institutional challenges. Part of the ESCRS Heritage Project involves revisiting the early days with some of the people who made it happen.
Sean Henahan (EuroTimes) and Dr Richard Packard (Packard Medical Practice) sat down with Professors Thomas Neuhann (EuroEyes Clinic Group) and Hans-Reinhard Koch (University of Bonn) to discuss IOL visionaries past and present. Profs Neuhann and Koch recount the evolution of IOL surgery from perilous to commonplace, describing early phaco surgery uncertainties, industry struggles, and the genius of visionaries like Dr Charles Kelman and Dr Richard P Kratz. Get ready for a whole lot of insight— sprinkled with a pinch of laughter!

Visit OASIS at ESCRS Booth #6.F10

QTY/BoxDescription
8,000 cps

Scan here to view the International Catalog
by
Preservative-free and designed to keep the cornea hydrated. It adheres to the cornea and forms a thin, optically neutral clear film.
Intended Use: VISCO SHIELD HPMC Viscoelastic
Topical is a sterile, viscoelastic irrigating device to be used on the exterior cornea to prevent drying of the epithelial layer during ophthalmic surgical procedures. HPMC
• 1.5ml filled syringe with cannula
• Stores at room temperature
To see if this product is available in your country, please contact international@oasismedical.com
1950s:
1950s:
Posterior to anterior designs
Posterior to anterior designs
1950s: Posterior to anterior designs
1980s: Flexible haptics to foldable lenses
1980s: Flexible haptics to foldable lenses
1980s: Flexible haptics to foldable lenses
1960s–1970s:
1960s–1970s:
Iris fixation to posterior stabilisation
Iris fixation to posterior stabilisation
1960s–1970s: Iris fixation to posterior stabilisation
In 1675, Sir Isaac Newton wrote, “If I have seen further, it is by standing on the shoulders of giants.” The same might be said of today’s intraocular lenses (IOLs), which benefit from three-quarters of a century of innovation by giants to help patients see farther and nearer—literally.
Though the first attempts at IOL implantation date to the late 18th century, Sir Harold Ridley achieved the first successful implants around 1950. His very first attempt in November 1949 produced about -14.0 D myopia. The power error was quickly corrected in subsequent implants, with one patient measuring 6/6 unaided when the results were first presented in July 1951.
But even that was just the beginning. It took some 40 years of innovation before the challenge of reliably stabilising lenses in the posterior chamber was finally met. This made possible the array of presbyopia-correcting and even accommodating lenses on or near the market today. Here are some of the significant milestones along the way.
1950s: Posterior to anterior designs
Sir Harold’s first IOLs closely followed the dimensions of the natural crystalline lens. Composed of polymethyl methacrylate (PMMA), these rigid lenses were placed in the posterior chamber after an extracapsular cataract extraction through a large incision closed with sutures.
Manufactured by Rayner, several ocular implant pioneers used these implants during the early 1950s. Though many patients did well with these lenses for decades, the relatively heavy and unsupported lenses tended to dislocate, sometimes months or years after implantation. Other frequent complications included hyphaema, glaucoma, iris atrophy, and inflammation. As a result, about 15% were eventually explanted.
1990s:
1990s:
Hydrophobic acrylic and toric lenses
Hydrophobic acrylic and toric lenses
1990s: Hydrophobic acrylic and
IOL pioneers such as Drs Joaquin Barraquer, Benedetto Strampelli, and Peter Choyce designed many anterior chamber lenses in the 1950s to overcome these challenges. But many of these angle-supported lenses wreaked havoc on the corneal endothelium, leading Dr Barraquer to explant more than half of his. While they enjoyed a renaissance in the 1970s and early 1980s, AC IOLs are no longer used.
1960s–1970s: Iris fixation to posterior stabilisation Realising the importance of keeping the lens implant away from sensitive tissues, the late 1950s saw Dr Cornelius Binkhorst design his four-loop lens for use with intracapsular extractions. The lens was fixated to the iris with two loops in front and two loops behind, and the optic in the anterior chamber. This led to many iris-fixated lens designs throughout the 1960s and 1970s, including Dr Jan Worst’s medallion lens, which remained popular through the 1980s.
In the 1960s, Dr Binkhorst believed the capsular bag left behind after extracapsular extractions could further stabilise the lens. He designed the two-loop lens, which placed two haptics in the bag with the optic in front of the iris. Dr Binkhorst performed many experiments to determine what shape of capsulotomy contributed most to lens stability, and his design led a shift back to posterior lens designs that included Dr John Pearce’s 1975 tripod PC IOL and Dr Steve Shearing’s 1977 J-loop PC IOL. Based on an anterior lens design by Dr Barraquer, the Shearing lens was among the first of a new generation that did not extend into the anterior chamber.
1980s: Flexible haptics to foldable lenses
Improvements in IOL manufacturing technology in the 1980s led to the single-piece PMMA lens with long,
Sunday, September 8th | 9:30 to 10:45
Room 8.0 B | Fira Barcelona Gran Via, Spain flexible haptics for better stability in the eye. But the rigid lenses still required a large incision. With the advent of phacoemulsification by Dr Charles Kelman, a much smaller incision could be used to remove the cataract. His AC lens with three-point, L-shaped haptics and a 4.5 mm optic could be inserted through a 4.5 mm incision. Yet realising the promise of small incision phaco would require foldable lenses.
A materials revolution made foldable lenses possible. Among the first was a poly-HEMA hydrogel lenses implanted in rabbits by Mr Richard Packard and colleagues in 1979. The first foldable silicone lens was implanted in a human in 1978 by Dr Ki-yi Zhou, followed by Dr Tom Mazzocco patenting the silicone lens in 1982. The lenses took off throughout the 1980s but have since fallen out of favour due to their tendency to discolour and develop calcium opacities.
Foldable hydrophilic and hydrophobic acrylic lenses ascended during the 1990s, with Mr Packard implanting the first foldable hydrophobic lens in a human in 1990. Three-piece and one-piece posterior chamber lenses became the norm throughout the decade. The stability of these designs also enabled development of toric lenses that could resist rotation, though this also required improving on early designs.
With the problem of IOL stability mostly solved, new lens designs have proliferated since 2000. These include lenses with blue light filters and multifocal and extended depth of focus lenses for presbyopia. And now we stand on the brink of true accommodating lenses. The innovation never stops!


Join leading experts today for an insightful and in-depth look at refractive intraocular lenses (IOLs).



Should monofocal plus be the new standard?
TIMOTHY NORRIS REPORTS
Whether monofocal plus should be the new standard "is a good question," said ASCRS President Vance Thompson at the beginning of his presentation at Saturday’s main symposium. An enhanced monofocal, with something extra special in it—a little spherical aberration to extend depth of focus—is a lens designed to maintain distance vision while improving intermediate vision compared to a conventional monofocal implant, he added. How to categorise this kind of lens, however, is still debated.
The American National Standards Institute (ANSI) has not really considered these lenses as a new category, but Dr Thomson underlined the necessity of finding a correct place for the monofocal plus, starting with considering ANSI’s definition of EDOF. Extended depth of focus lenses in general are designed to help patients with intermediate vision, defined by ETDRS 66 centimetres, he said. Moreover, ANSI stated that an EDOF lens needs to demonstrate at least .5 D of depth of focus for a monoclonal control at 66 centimetres.
Monofocal plus lenses do not match the criteria of this definition, so they do not qualify as EDOF, Thompson said, despite the fact they extend depth of focus. It is not so simple to find a perfect definition, he added. It could make patients very unhappy if they expect something that is similar to an EDOF while not being an EDOF. According to Thompson, now is the right time to make a clarification, to decide and
especially to properly communicate to the patient about the loss of accommodation that follows an implant.
It is known that in patients with early cataract or presbyopia, with a fair amount with pseudoaccomodation there are wonderful aberrations in their natural lens, Thompson said. That works like an EDOF, with a natural spherical aberration. It is not surprising that companies use spherical aberrations to create monofocal plus, but it is worth remembering that these are not the same thing, and the patient will end up with something different and be unhappy about it, he stated. According to Thompson, this can be mitigated with some precise precautions, keeping in mind that correcting spherical will improve contrast and reduce depth of focus. Also, it is important to remember that it is related to pupil size, requiring perfect centration, especially in younger patients.
During the discussion, Thompson underlined the necessity of patient happiness, pointing out the need to carefully inform patients of the implantation they will be receiving. Cataract surgery is like pizza, he said. It is difficult not to enjoy pizza, or a cataract if there were only classic monofocals. However, with recent advancements, the risk of disappointing patients is growing, especially if they have to pay extra money for these solutions. For this reason, it is very important to double down on information and provide the correct consultations, he concluded.

Tulaya Tungsiripat, hailing from Thailand, humorously mentioned she’s here for some “shopping.” However, her real purpose at ESCRS is to explore and acquire the latest devices and innovative products that can benefit her patients back home. In addition to discovering new technologies, she’s eager to participate in the wet labs, where she can gain hands-on experience with the latest techniques and tools in the field.
Mohammed Mohammed, visiting from Egypt, is eagerly anticipating the lectures at ESCRS. He’s also looking forward to relaxing in the member lounge, where he can network with peers. However, what excites him the most is the opportunity to attend the cataract eye surgery sessions, where he can deepen his expertise and stay updated on the latest advancements in the field.



Meet the Precizon Family: best-in-class IOLs for any cataract challenge. Monofocal, enhanced intermediate vision and full range of vision lenses with patented CTF technology. Regular and Toric. With a natural fit and ingenious optics that deliver extraordinary results. For successful surgery and perfect natural vision.
ophtec.com/precizon-family












BY BURAK MERGEN MD
“As the morning light fills the clinic, I’m met with a rush of patients awaiting care. Throughout the day, I juggle consultations, surgeries, and paperwork, each task demanding my full attention. The growing administrative load weighs heavily on me, leaving little room for breaks, and lunch becomes a distant luxury amidst the constant flow of patients.
In this whirlwind, a sense of disillusionment begins to creep in. While once finding immense satisfaction in restoring sight to patients, now fatigue looms large, overshadowing my efforts. Interactions feel routine, lacking the empathy and connection that once fuelled my passion for ophthalmology.
As the day progresses, I yearn for deeper connections, yet fleeting conversations offer little solace amidst the challenges of our profession. The camaraderie that once lifted our spirits has faded, replaced by a pervasive sense of isolation as we each navigate our own struggles.
By day’s end, exhaustion sets in, overshadowed by the looming threat of burnout. Despite my unwavering dedication to patient care, doubts linger, questioning whether there’s anything more I can give.” This sobering fictional reality underscores the urgent need to address burnout within ophthalmology.
In the realm of ophthalmology, where precision and empathy come together to safeguard one of humanity’s most treasured senses, burnout casts a pervasive shadow over the profession. With the escalating demands of training and practice, an increasing number of young ophthalmologists find themselves trapped in its grip, considering early departure from a field they once wholeheartedly embraced. Addressing this pervasive issue requires a multifaceted approach that integrates institutional support, self-care practices, and a cultural shift within the profession itself.
Erich Fromm’s profound insights into the essence of human existence offer guidance towards a more sustainable approach to ophthalmology.1 He posits true values stem not from material possessions but from intrinsic qualities that define our ‘being.’ This challenges the prevailing culture of
materialism, urging us to redefine success and fulfilment in terms of inner richness rather than external acquisitions.
Critical to mitigating burnout is addressing systemic stressors entrenched within training and practice environments. Institutions must proactively implement measures to alleviate burdens placed upon trainees and practitioners. Overwork, administrative pressures, and lack of support contribute to the erosion of well-being among ophthalmologists, necessitating systemic reforms.
Prioritizing self-care practises is paramount to weathering the storms of burnout. Encouraging a healthy work-life balance through flexible scheduling and time management strategies allows individuals to recharge and reconnect with their passions beyond the operating theatre. Cultivating inner richness through mindfulness, meaningful relationships, and personal growth serves as a buffer against burnout’s insidious effects.
Crucially, effecting lasting change demands a cultural shift within the ophthalmic community. Destigmatizing vulnerability and fostering open dialogue regarding mental health are paramount. By embracing vulnerability as a strength, ophthalmologists can cultivate a culture of authenticity and mutual support, bolstering resilience against burnout’s tide.
Furthermore, recent studies have shed light on specific risk factors contributing to burnout among ophthalmologists. For instance, research by Chang (et al.) examined LGBTQ identity as a potential risk factor for burnout within an international ophthalmologist cohort.2 Their findings revealed that LGBTQ ophthalmologists reported higher levels of personal and work-related burnout compared to their non-LGBTQ counterparts. Additionally, discrimination or harassment based on LGBTQ status in the workplace was identified as a contributing factor to increased burnout among this demographic.
Moreover, Sedhom (et al.) conducted a survey among ophthalmologists in the United States, uncovering significant associations between burnout and demographic factors such
as gender, employment setting, and practice type. Specifically, female ophthalmologists exhibited nearly twice the odds of experiencing burnout compared to their male counterparts, while physicians employed in academic and hospital settings reported higher rates of burnout than those in large private groups.3 These studies underscore the importance of addressing diverse demographic factors and workplace dynamics in mitigating burnout among ophthalmologists.
Through collaborative implementation of the recommendations below, stakeholders in the ophthalmology community can create a supportive environment fostering resilience, preventing burnout, and enhancing well-being:
1. Institutional Support: Implement policies promoting work-life balance, allocate resources to cope with stress, and offer tailored support programmes.
2. Self-Care Practises: Prioritize physical, emotional, and mental well-being through regular exercise, healthy habits, and engaging activities outside work.
3. Workload Restructuring: Assess workloads critically, identifying tasks incongruent with strengths or patient care contribution.
4. Promotion of Autonomy: Empower ophthalmologists to make decisions aligned with values, fostering collaboration and professional growth.
5. Peer Support and Mentorship: Establish networks enabling sharing experiences, seeking guidance, and fostering camaraderie among colleagues.
In conclusion, nurturing resilience and alleviating burnout in ophthalmology requires collective action from institutions, individuals, and the profession. By integrating Fromm’s insights and fostering a culture of openness and support, we can transcend burnout’s limitations, paving the way for a future defined by passion, purpose, and fulfilment.
Dr Mergen’s essay came second in the 2024 John Henahan Writing Prize answering the prompt ‘Burnout is a chronic issue in ophthalmology, leading a growing number to abandon the field early in their careers. What should be done to reduce unnecessary stress in training and practice, allowing for a successful long-term career?’.
Burak Mergen MD, FEBO, FICO is a second year resident in Gengenbach, Germany. burakmergen@gmail.com
References
1. Fromm, Erich. Haben oder sein. München: Deutsche Verlags Anstalt, 1976.
2. Chang TC, A R, Candelario C, Berrocal AM, Briceño CA, Chen J, Shoham-Hazon N, Berco E, Valle DS, Vanner EA. “LGBTQ+ Identity and Ophthalmologist Burnout,” Am J Ophthalmol, 2023 Feb; 246: 66–85. doi: 10.1016/j.ajo.2022.10.002. Epub 2022 Oct 14. PMID: 36252675.
3. Sedhom JA, Patnaik JL, McCourt EA, Liao S, Subramanian PS, Davidson RS, Palestine AG, Kahook MY, Seibold LK. “Physician burnout in ophthalmology: U.S. survey,” J Cataract Refract Surg, 2022 Jun 1; 48(6): 723–729. doi: 10.1097/j.jcrs.0000000000000837. PMID: 34596630.
Sunday, September 8th | 9:30 to 10:45
Room 8.0 B | Fira Barcelona Gran Via, Spain


Join leading experts today for an insightful and in-depth look at refractive intraocular lenses (IOLs).


The ESCRS Inclusivity Programme has released the findings of a members survey conducted between April and July aimed at helping identify barriers to inclusion and diversity within the Society.
Under the guidance of ESCRS President Filomena Ribeiro and BOSS (Building Our Sustainable, inclusive Society) Working Group Chair Mor Dickman, the ESCRS Inclusivity Programme intends to gather essential data on the Society’s membership. “As a scientific society, it is beneficial to base our findings on data,” explained Dickman. “We looked at this survey as a baseline measurement. It gives us facts to discuss, not just perceptions. Hopefully, we can revisit it in the future to see how things change.”
The team identified a relevant survey from the British Hip Society, which aligned with the objectives of the Inclusivity Programme. After securing permissions to adapt the survey, it was distributed to ESCRS members in April.
“It was very difficult to find a survey from a surgical society,” Dickman noted. “It’s good to have a tool that’s been developed and already validated and published. Surveys like this are common in the United States, but in Europe, we just don’t have the data yet.”
The survey participants predominantly hailed from Europe (68.1%), with smaller representations from Asia (11.8%), North America (10.5%), and other continents. The average age was 52 years, with the majority (54.1%) between 45 and 64. The gender distribution revealed a male majority (66.8% male to 32.8% female). Additional key insights include religious affiliations (57.6% Christian), sexual orientation (87.3% heterosexual), and current position held (52.8% identified as a fully qualified ophthalmic surgeon in private practice).
One of the pivotal survey questions explored whether members had faced barriers related to equality or diversity in their progression within ophthalmology. A notable majority (71%) indicated they had not encountered such barriers; among those who had, 49% said they had experienced gender discrimination, 39% cited limited access to training, and 33% mentioned age as a factor.
It is also noteworthy that among those who reported encountering challenges, the majority came from underrepre-
sented groups: 44% of women reported challenges compared to 22% of men, and 49% of those between 25 and 45 reported issues compared to only 5.9% of those 65 to 84. Additionally, African respondents, those with other sexual orientations, and Hindu respondents were more likely to report facing barriers.
“We see a group that thinks there are no issues and a group that thinks there are issues,” explained Dickman. “Generally, the groups that think there are issues are those experiencing them. We are in a field where people are highly educated, and it is very disturbing to see that in 2024 there is still an issue with inclusivity in this industry. It is a problem if one in every three people is experiencing such difficulties.”
The survey revealed many respondents are satisfied with the progress ESCRS has made towards fostering an environment where members are encouraged to contribute, innovate, and lead regardless of gender, ethnicity, sexual orientation, or physical disability. “People really feel at home within ESCRS; they see it as a network where they can connect with their friends and feel included in discussions,” Dickman said. “But while people recognise that our members are quite happy within ESCRS in general, it doesn’t mean they are getting the opportunities they deserve outside of the Society.”
Within the survey, respondents were invited to provide feedback on how ESCRS could foster a more inclusive environment. Their suggestions included increasing diversity and inclusion in leadership positions and panels, promoting geographic and cultural representation, expanding networking and mentorship opportunities, increasing social and interactive events, making the events more affordable and accessible, improving communication channels, incorporating interactive sessions, and openly acknowledging the need for these improvements.
“This is a long process, and we are just at the start of it,” Dickman stated. “We are really setting the building blocks. We are making sure this year that we recognise this is an important issue we need to work on.
“One of our responsibilities is to prepare our future leaders and help them get training in this area so they can create a more inclusive environment,” Dickman said. “It’s very enriching, but we also don’t want it to be perceived as imposing. We really want to engage people to make them understand how these things work and what they can do to negate it.”
HOWARD LARKIN REPORTS
When patients asked how long their intraocular lenses (IOLs) would last, Dr Abhay Vasavada would confidently answer, “Oh, it will remain there as long as you live!”
But more recently, the emergence of late spontaneous IOL decentration many years after uneventful ‘in the bag’ cataract surgery has caused him to modify that advice, he said in the 2024 Ridley Medal Lecture. He now stresses that patients continue to have their eyes checked periodically for life.
Dr Vasavada outlined two causes of late IOL decentration. One is primary zonular disease that causes the entire capsular bag with the lens inside to decentre or dislocate.
Zonular disease risk factors are well known, including pseudoexfoliation, capsule fibrosis, vitreo-retinal surgery, and high myopia. So, he focused his lecture on the lesser-known second cause—posterior rupture of the capsular bag, which results in the lens decentring or dislocating completely into the vitreous while the bag remains attached to the zonules. It happens because the posterior capsule grows thin and fragile over time in an effect called ‘dead bag syndrome.’
Exploring ‘dead bag syndrome’
Dr Vasavada reported a prospective study of 90 patients with late decentration conducted at the Iladevi Cataract and IOL Research Centre and Raghudeep Eye Hospital in India. Of these, 52 (or 58%) had dead bag syndrome. More than 90% were male, and half had an axial length of more than 24 mm, making male gender and myopia risk factors. Three-quarters
occurred between 11 and 20 years after surgery, and about one-third of cases are bilateral.
Surgery is the only treatment option, Dr Vasavada said. The decentred IOL can be re-fixated, but IOL exchange is more common. Options to fixate the new IOL include iris claw lenses and transscleral or intrascleral fixated IOLs. “Our preference has been Yamane technique of intrascleral fixation.”
He cautioned, however, that the technique has a learning curve, requiring precise scleral marking to correctly anchor the lens, though complications are acceptable and not serious.
Dr Vasavada also presented evidence that the bag is not really dead bag syndrome. Citing histological studies conducted by Dr Liliana Werner, he found scanty or no lens epithelial (LE)cells in the bag. However, he also found abnormal LE cell activity producing Soemmering rings in 70% of the patients. “This was a big surprise.”
In addition, genetic tests identified variants with moderate correlation to LE cell survival and posterior capsule fragility, suggesting possible genetic causes for this relatively rare late complication. Vitreoretinal surgery and vitreous changes may contribute to the posterior capsule weakening as well. And single-piece lenses may be more prone to dislocate, though this is very uncertain.
Further research is needed to better understand the causes and development of dead bag syndrome, which may enable prediction and prevention of late IOL dislocations, Dr Vasavada concluded. In the meantime, he advises patients to “keep coming every five years or so for life.”
Abhay Vasavada MS, FRCS is based in India.

Memorable moments from the ESCRS 2024 Congress, capturing key connections and collaborations.








This main symposium moderated by two former ESCRS presidents takes a deep dive into the growing importance of telemedicine in ophthalmology and the associated technological developments. The programme includes Mor Dickman discussing the changing definitions of telemedicine; Matthew Burton looking at a global perspective; Danson V Muttuvelu discussing applications and limits for the posterior segment; Sunil Mamtora discussing applications and limits for the anterior segment; Mostafa El Habib Daho talking about added value with AI; and Afsun Sahin looking at the environmental and financial aspects.
Monday, 11:00–13:00, Plenary Hall
Moderators: Oliver Findl and Béatrice Cochener-Lamard
The editors of the Journal of Cataract and Refractive Surgery will share their selection of the most interesting articles in two back-to-back sessions. The first session will present a series of case reports, including a case of positive dysphotopsia after implantation of an EDOF intraocular lens, and explantation of a light-adjustable intraocular lens. The second session looks at three novel techniques.
• Editors’ Pick: JCRO Case Report 14:00– 15:00
• Editors’ Pick: JCRO Technique 15:00–16:00 Both sessions meet in room 8.0 B.
Join moderators Vance Thompson, Béatrice Cochner -Lamard, and Ronald Yeoh for a discussion of the many paths to becoming a great refractive surgeon at the CSCRS Symposium. They will be joined by Filomena Ribeiro, Sri Ganesh, and Robert Ang in addressing the limits of various refractive surgery options.
CSCRS Symposium: My refractive surgery path Monday, 08:15–10:15, Plenary Hall
Moderators Vincent Qin (Belgium) and Eszter Szalai (Hungary) will host a session looking at many facets of training programmes around the world. Speakers include Víctor Lázaro-Rodríguez (Spain), Valentin Hooijer (Germany), Yassir Imani (Morocco), Pooja Khamar (India), and Alfonso Sentatore (Italy).
Arena Training and Symposium: Cataract Surgery Training Across the World Monday, 15:30–16:45 8.1 N/ ARENA
Hope to see you on Sunday night as the ophthalmologist rock band OftalmoRock take the stage! Attendees can choose contributions of €5, €10, or €15. All funds raised from this concert go directly towards ESCRS-supported projects in low- to middle-income countries, principally in Sub-Saharan Africa.
Venue: Sala Apolo
20:30 Doors Open | 21:30 Concert Starts | 23:00 Concert Ends
Day two of the 2024 ESCRS
Annual Congress offers something for eye surgeons of all backgrounds and interests, from sessions on quality management systems and shared decision making to a course on combatting unconscious gender bias and a debate about femtoLASIK surgery.
Got some openings in your schedule? Check out these featured presentations.

EU Clinical Trial Spotlight Symposium
08:30 – 10:00
Main Symposium: The Future of Corneal Refractive Surgery
11:00 – 13:00
Room 8.0 H
Team Collaboration/Culture/Values of an Organization
08:30 – 10:15
Patient Decision Making: The Move to Shared Decision Making 10:30 – 12:15
Marketing: Staying Competitive and Innovative without Breaking the Bank 14:15 – 15:45
Quality Management Systems: Why They’re One of the Best Investments You Can Make 16:00 – 17:00
Room 8.1 N
Surgical Pearls: Anterior Segment
08:30 – 09:10
Surgical Pearls: Cornea 09:10 – 09:50
TABLAO ARENA
Room 8.1 N
Sustainability: Implementation of e-IFU for IOLs in Europe 12:00 – 12:45
Corneal Refractive Debate: Femto-LASIK is the Standard Procedure! 14:30 – 15:30
Forum: How Should I Start Refractive Surgery? 15:35 – 16:05
Room 8.0 I
Combatting Unconscious Gender Bias in Ophthalmology, Industry, and Medicine: An Evidence-Based and Practical Course 11:00 – 12:30
Sessions will cover hot topics in cataract and refractive surgery.
Delegates will find a stimulating variety of clinical discussions by leading ophthalmic surgeons in the Independent Medical Education (IME) Symposia during the Congress. These sessions aim to provide balanced, non-branded, category-based education with expert faculty presenting meaningful, independent content for sincere peer-to-peer education. A common thread running through the various sessions is the use of information gained from the ESCRS Clinical Surveys.
Sunday, September 8th | 09:30 - 10:45 CEST
Room 8.0 B | Fira Barcelona Gran Via, Spain





RIOL IME Forum:
Location: 8.0 B, Fira Barcelona Gran Via
Date:
Sunday, 8 September, 2024
Time: 9:30–10:45 CET
Grant Supporters: Alcon (Platinum), Johnson & Johnson Vision (Bronze), Zeiss (Bronze)
Phaco IME Forum:
Location: 8.0 J, Fira Barcelona Gran Via
Date:
Monday, 9 September, 2024
Time: 9:00–10:15 CET
Grant Supporters: Alcon (Platinum), Zeiss (Bronze), Bausch + Lomb (Bronze)
Toric IME Forum:
Location: 8.0 J, Fira Barcelona Gran Via
Date:
Monday, 9 September, 2024
Time: 13:00–14:00 CET
Grant Supporters: Alcon (Platinum), Zeiss (Bronze)

iStent ® technologies have been proven to stabilize visual fields loss and glaucoma disease progression with a favourable risk-benefit ratio1

+3 YEARS FOLLOW-UP
15 STUDIES ON ISTENT TECHNOLOGIES
1,115 EYES

26.6 % MEAN IOP REDUCTION WAS SUFFICIENT TO ACHIEVE THIS FUNCTIONAL EFFECT
-0.024
DBS/YEAR MEAN RATE OF PROGRESSION SIMILAR TO THAT REPORTED IN NONGLAUCOMATOUS EYES
1. Gillmann K, Hombeak DM. BMJ Open Ophth 2024;9:e001575.doi:10.1136/bmjophth-2023-001575. iStent inject ® W IMPORTANT SAFETY INFORMATION INDICATION FOR USE: The iStent inject ® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject ® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject ® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations.
• In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS:
• For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject ® W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject ® W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with the iStent inject ® W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. ©2024 Glaukos Corporation. Glaukos, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation PM-EU-0317
