The Future of Laser Vision Correction Surgery

SPECIAL FOCUS CATARACT & REFRACTIVE CORNEA | RETINA | GLAUCOMA | PAEDIATRIC OPHTHALMOLOGY

Belong to something inspiring. Join us. See into the future of eye surgery and patient care. Visit www.escrs.org for information about membership & benefits
Publisher
Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer

Lara Fitzgibbon
Designer

Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers

Advertising Sales
Amy Bartlett
ESCRS

Tel: 353 1 209 1100

email: amy.bartlett@escrs.org

Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983
P.40 EUROTIMES | OCTOBER 2020 CONTENTS A EUROPEAN OUTLOOK ON THE WORLD OF OPHTHALMOLOGY www.eurotimes.org GLAUCOMA 36 Fighting for the middle ground in glaucoma treatment PAEDIATRIC OPHTHALMOLOGY 37 Multiple factors necessary to predict myopia progression 38 Reducing dosage in ROP treatment REGULARS 40 Global Ophthalmology 43 Industry News 44 Outlook on Industry 46 Practice Management 47 Inside Ophthalmology 48 Travel 50 My Life in Ophthalmology 51 Calendar SPECIAL FOCUS CATARACT & REFRACTIVE 04 How surgeons across Europe are dealing with the challenges faced by the COVID-19 pandemic 08 Everything you need to know about laser vision correction surgery 10 Which refractive surgeries are safe to perform during the pandemic? 12 The value of intraoperative imagining remains unclear for toric IOLs 13 Preoperative imaging is a valuable addition for all procedures 14 Understanding the causes of postoperative dysphotopsia 15 Multifocal IOL exchange can remedy failed neuroadaptation 16 A wealth of new IOLs are coming down the line 18 Modern anterior chamber IOLs still have a place 19 Several techniques available for post-op IOL adjustment 20 Rotational stability essential for best results with toric IOLs 21 Which method is best for trifocal IOL power calculation? 22 Large range of options ushers in era of personalised care 23 Reducing subconjunctival haemorrhage after FLACS 24 Communicating with patients to manage expectations 25 JCRS highlights CORNEA
OCT in early keratoconus 28 Monoclonal antibodies and conjunctivitis
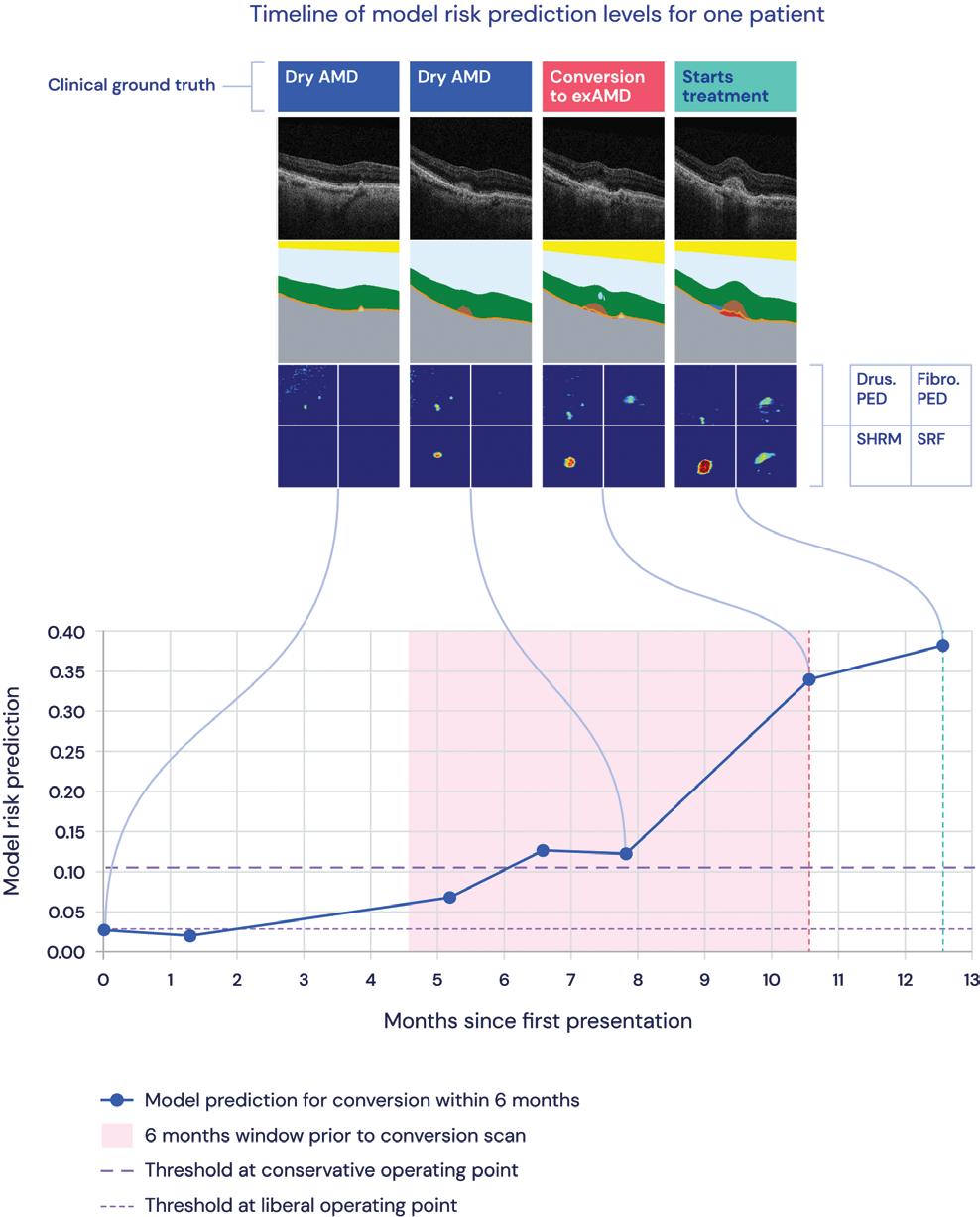
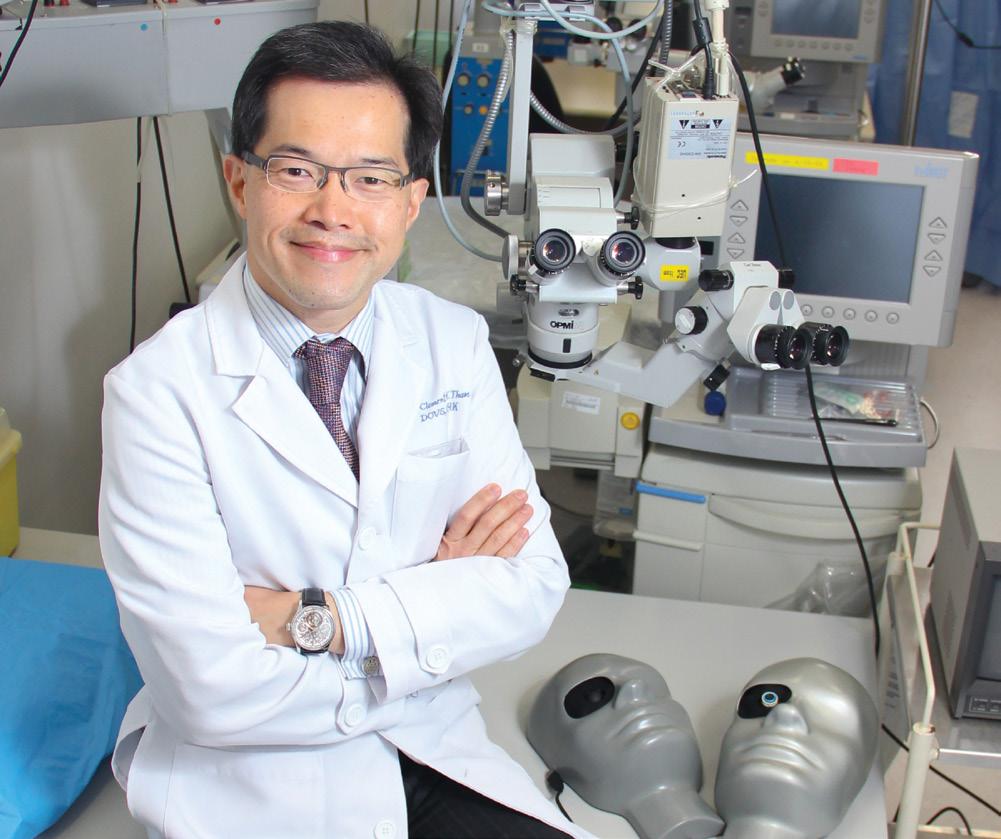
Measuring DMEK outcomes RETINA 30 Using AI to predict AMD in fellow eyes 31 Emerging imaging technique useful in retinal diseases
Artificial vitreous substitute shows promise
Using stem cells for Stargardt’s disease shows promise
Daily exposure to red light could halt declining vision
Anti-VEGF drug shows efficacy with fewer injections Included with this issue... ESCRS/EuCornea Education Forum Supplement and Kowa Supplement An innovative toric IOL with progressive axial correction (PAC) technology 2020 Dysfunction Meibomian GL AND
26
29
32
33
34
35
As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between February and December 2019 was 47,863
MEDICAL EDITORS
Seize the day
Vision correction has never been safer and more effective than now
This issue of EuroTimes has a series of viewpoints that focus on refractive surgery and how vision correction surgery is weathering the COVID-19 storm.
Asia was always ahead of Europe by some months depending on the specific countries you were studying regarding the pandemic, and Europe learned a lot from their experiences of how to contact trace, test widely and wear face masks.
We also heard another aspect that seemed to be counterintuitive: refractive surgery was returning faster than other aspects of ophthalmology. Urgent retinal and glaucoma surgeries were not impacted by COVID-19 in terms of volume, but elective surgeries were greatly affected.
What has the European experience been in this regard? Michael Knorz reopened his practice in Germany to refractive surgery on April 20 and was initially kept very busy with pent-up demand and even though numbers are generally holding up well, he has concerns that the economic impact of the pandemic of employment numbers and consumer sentiment may yet have a negative effect on the excellent recovery.
In Greece, John Kanellopoulos is hopeful that the recovery will persist and has noted that introducing an element of virtual connection between his team and patients and their relatives is enhancing the patient experience and the patient-doctor relationship. He has also introduced new technology to his laser vision correction portfolio and believes that this may have helped LVC rise to 50% of his current procedure volume where previously it made up 33% of the total surgical volume.




Both Drs Knorz and Kanellopoulos have stated that by taking measures to make patients feel safe, they have seen the rewards.
INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
It is interesting and reassuring to see that our own experience in Ireland is remarkably like Germany and Greece. There appears to be a renewed interest in personal health and well-being and an element of “seize the day”. Glasses getting fogged up with mask use, people being reluctant to touch their eyes and all that goes with contact lens wear, are encouraging people to look for more permanent solutions to allow them to see well.
Vision correction by means of corneal laser procedures or IOL procedures has never been safer and more effective than now.
Vision correction specialists and ophthalmologists are in pole position to help our patients come out of the pandemic in better shape than they were going in. That is, as far as their vision is concerned.
EUROTIMES | OCTOBER 2020
A WORD FROM ARTHUR CUMMINGS FRCSEd GUEST EDITORIAL
Vision correction by means of corneal laser procedures or IOL procedures has never been safer and more effective than now
Emanuel Rosen Chief Medical Editor
José Güell
Arthur Cummings
Thomas Kohnen
EDITORIAL 2
Arthur Cummings is a Consultant Eye Surgeon at the Wellington Eye Clinic and Consultant Ophthalmologist at the Beacon Hospital, Dublin, Ireland
Paul Rosen
Faros™ MAKING THE DIFFERENCE WITH LEADING INNOVATION

Precision and efficiency in eye surgery
The Faros surgical platform enables cataract, vitrectomy and glaucoma surgery of the highest level while constantly remaining comfortable and intuitively operable. The reliable flow control makes the surgeon’s work even easier and safer than before. In addition, the Faros impresses with versatility, innovative technologies, exceptional functionality and ease of use.
→ Available as an anterior platform or as a combined anterior/posterior platform
→ Cutting-edge dual-pump system with flow and vacuum control with its unique SPEEP Mode™
→ Proven easyPhaco® technology
→ Continuous Flow Cutter for traction-free vitreous body removal
Make the difference – with the new Faros: www.oertli-instruments.com

EYE SURGERY. SWISS MADE.
Not available for sales in the US NEW
The future of laser vision correction
Cheryl Guttman Krader and Dermot McGrath report on how surgeons across Europe are dealing with the challenges of COVID-19
When the COVID-19 lockdown restrictions were initially eased and Germany began to reopen in the middle of May, the country had one of the lowest death rates from the novel coronavirus in the world.
By the time June was ending, Michael C Knorz MD, Professor of Ophthalmology, FreeVis LASIK Center at the University Eye Clinic, Mannheim, Germany, said that he had essentially taken care of the backlog of cases of laser vision correction (LVC) that had been deferred during
the shutdown. In addition, new inquiries from patients interested in a refractive procedure seemed to have dropped minimally relative to pre-pandemic days.
When asked about his thoughts regarding how COVID-19 would impact the future of LVC, however, Dr Knorz
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 4
offered a dichotomous perspective.
He told EuroTimes: “I am an optimistic person, and I do not believe that COVID19 by itself will have a significant impact on laser refractive surgery. We could live with it, just like we live with the flu.”
Yet, Dr Knorz qualified his comment by noting it represents a rational view. His response based on an emotional reaction is more pessimistic.
“From what I see, the whole world is in a panic mode today and seems to be grossly overreacting to the scientific facts. This extreme overreaction will cause an economic downturn that will affect laser refractive surgery in the same negative way it will affect other aspects of our lives, and it may lead to a global depression,” Dr Knorz said.
“I truly hope that politicians will come to their senses, but we will have to wait and see the course ahead. A reliable prediction of the future of laser refractive surgery is not possible today. In the coming months we will see what happens.”
PRACTICE UPDATE
Dr Knorz reopened his practice to elective surgery April 20. Patients were contacted to reschedule the LVC procedures that were cancelled because of the lockdown, and only a few decided they would not go forward.
“By the end of June, over 90% of the patients whose LVC procedure was deferred had undergone their surgery,” Dr Knorz said.
Interest in LVC remains. Relative to the months preceding the pandemic, Dr Knorz said he has seen a drop of only 5-to-10% in the number of inquiries for consultation visits.
Dr Knorz believes that unemployment, with its accompanying loss of income, will be the primary factor determining uptake of LVC going forward.
“In Germany, we are quite lucky because unemployment is not a big issue yet. Job loss, however, was the main reason given by the approximately 10% of our patients who decided not to go ahead with their planned surgery when we called them back to reschedule it,” he said.
Dr Knorz said that so far, he has not seen any age-related difference in patient willingness to proceed with the elective procedure.
“Both our lens patients in the 50-to-70year age range who are candidates for refractive lens exchange and our LVC
patients are mostly willing to come for surgery,” he observed.
COVID-19 has necessitated new processes to ensure a safe environment, and making patients aware of the strategies being implemented is critical to their willingness to attend office visits and proceed with surgery. At the FreeVis LASIK Center, all patients are given a surgical mask and sanitising gel to disinfect their hands at entry, and no more than six patients are allowed in the 20m-squared waiting room. Disinfection of all contacted surfaces and instruments is being done in view of patients, and all documents are now being handled electronically with Adobe Sign used for informed consent and invoices.
“The feedback we have received from patients is that they feel very safe,” said Dr Knorz.

AGGRESSIVE RESPONSE
Thanks to a swift, aggressive government response to early cases of COVID-19, Greece was one of the first countries to see restrictions eased.
Despite the absence of a mandate, A John Kanellopoulos MD, Director, Laservision Eye Institute, Athens, Greece, chose from March 1 to voluntarily stop performing all elective surgeries at his centre and enforce spacing between patient exams along with wearing of facial masks and gloves for all. By mid-May, just a few weeks after the beginning of staged lifting of COVID-19 restrictions, he was already seeing patients for laser vision correction (LVC) consultation visits and
performing his first operations.

Considering the level of patient interest and the value of laser refractive surgery, Dr Kanellopoulos is hopeful about its future.
“If we do not let our guard down and remain dedicated to delivering safe and ethical care, I believe the volume of LVC will return to the pre-pandemic state,” he told EuroTimes.
Dr Kanellopoulos recalled that during the lockdown period in Greece, he was contacted by several patients who were interested in Laser Vision Correction surgery because they felt the “down time” they had from work and other usual activities offered an opportune time to undergo the surgery.
He also postulated that the stay-athome situation itself, may have fuelled interest in LVC.
“With more unoccupied time, some individuals may have focused more on difficulties they were having with contact lenses and/or self-reflected on making lifestyle changes,” Dr Kanellopoulos explained.
“With safety in mind, we kindly deferred and postponed requests to perform surgery during the lockdown; parallel to this we counselled patients to try to refrain from wearing contact lenses considering that they may become a mode of transmission for the coronavirus.”
Although in general, people in Greece are still somehow limiting some of their elective and leisure activities, including choosing to undergo various elective surgeries, Dr Kanellopoulos said that he is seeing an increased interest in LVC relative to the past.
“Although my surgical volume has not returned to what it was a year ago at this same time, the proportion of my surgical population that is interested in LVC has grown,” he said.
“Previously, laser refractive surgery accounted for approximately one-third of my surgical practice. Now almost half of the patients I see are interested in updating their contact lens prescription and very interested in LVC.
Dr Kanellopoulos suggested the
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 5
I truly hope that politicians will come to their senses, but we will have to wait and see the course ahead. A reliable prediction of the future of laser refractive surgery is not possible today
Michael C Knorz MD
A patient undergoing laser vision correction surgery
Courtesy of Arthur B. Cummings MD, FRCS
“surge” may have been enhanced by his having incorporated ray-tracing customisation and excellent early results since November 2019 using an artificial intelligence platform that combines wavefront, Scheimpflug tomography and interferometry measurements from a single device.
Implementation of measures to minimise risk for virus transmission is critical so that patients are comfortable coming in for a consultation visit and proceeding with surgery. The changes include wearing of surgical face masks at all times-by all staff, breath shields on all slit-lamps, and reconfiguration of the waiting area to maintain social distancing among others.
Prior to their visit, patients are carefully screened for infection or recent exposure to COVID-19. At entry into the building, they are given disposable masks and gloves to wear and must clean their shoes with a disinfectant solution. In addition, adult patients must be unaccompanied unless they require assistance for ambulation or another issue.
“We recognise, however, that in making the decision to undergo surgery and for support postoperatively, many patients rely on an informed family member or friend. Therefore, we have employed extraordinary measures using videoconferencing and live, private online broadcasting of each surgery to fulfil this need,” Dr Kanellopoulos said.


“Our team’s high standards and my personal quest in offering excellence in patient care has been the driving force in rebooting refractive surgery in our practice post COVID-19. I personally have found the great majority of patients to have ‘returned’ to normalcy with a more heartfelt physician-patient relationship, and I am thrilled!”
SCREENING IS IMPORTANT
When Ireland started to ease its lockdown measures, ophthalmologists faced the challenge of getting their practices back up and running to deal with patient demand. The Wellington Eye Clinic in Dublin, one of the country’s best-known cataract and refractive surgery practices, introduced a range of measures to reassure patients and minimise disruption in the wake of the COVID-19 pandemic.
“We have resumed the majority of
appointment types except for contact lens trial appointments. We had virtual consultations and the odd in-person consultation for emergencies during lockdown,” said Arthur B. Cummings FRCSEd, Medical Director
Liz Brennan, Head of Research and Clinical Support at the clinic says they have removed many of the chairs in the waiting area, added screens to separate patients where chairs are closer, asked all patients to wear masks and put phones in zip lock bags and sanitised station set up at the entrance with a motion sensor “welcome doorbell” that notifies the team that someone has arrived at the sanitising station.
“The team wash hands between every patient (as per usual) and the clinical team are wearing gloves for clinical exams. All patients attend the assessment station in the hospital assessment area prior to their appointment in our clinic and all staff have their temperature checked twice daily. This is logged on a tracker that also allows us to monitor staff contacts in the event of a requirement to contact trace,” she said.
They have also added a large splash screen at the front desk and smaller screens and breath shields at devices and slit lamps. Floor stickers also give a visual guide to patients and patients are instructed to conduct conversations in the consultation room once the medical staff is at the sticker (i.e. 2m away)
Screening is also important, said Dr Cummings. All patients visit an assessment station in the concourse where they are asked a series of questions to check potential exposure/ symptoms and they have their temperature checked. They are given a clearance certificate which they present to us on arrival at reception and this is scanned into their EMR file. They also complete and submit
an online COVID-19 form that we send them prior to their appointment where they state the same and digitally sign before submitting.
All diagnostic equipment and rooms are deep cleaned each morning as standard preCOVID and alcohol wipes used between patients. Since reopening, staff at the clinic have increased the frequency of this deep clean throughout the day, ensuring to include phones, keyboards, light switches, door handles and chair armrests as well as the device and equipment tables.
Dr Cummings says that the lessons learned from dealing with the COVID-19 pandemic will have long-term benefits.
“It has been a period of adjustment for us as a team. All of our processes have been challenged with COVID but our team came together via Zoom staff meetings to offer their feedback and ideas of how our new process and patient journey would work. Collectively, we designed a new process that aimed to have maximum safety and convenience for the patient while keeping our team safe too. We have introduced online medical history forms and payment links and we are currently reviewing options to allow patients to book their appointments via an automated SMS system.
“While we are not at the stage yet, I think in time that we will look back on this time as a major challenge for the clinic but one that forced growth that may not have occurred without COVID and which will leave us with a more efficient clinic as a result,” he said.
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 6
We recognise, however, that in making the decision to undergo surgery and for support postoperatively, many patients rely on an informed family member or friend
John Kanellopoulos MD
We have resumed the majority of appointment types except for contact lens trial appointments. We had virtual consultations and the odd inperson consultation for emergencies during lockdown
Arthur B. Cummings FRCSEd
If we do not let our guard down and remain dedicated to delivering safe and ethical care, I believe the volume of LVC will return to the prepandemic state
John Kanellopoulos MD
Research Education Innovation
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Everything you need to know: Laser Vision Correction
LVC can be used for many different refractive errors. Dr Soosan Jacob, MS, FRCS, DNB reports


Laser vision correction (LVC) is widely accepted and popular among surgeons and patients alike for changing the refractive status of the eye and allowing ability to function without spectacle or contact lens dependency. Primarily performed for occupational, cosmetic or reasons of pure comfort, LVC may also be used to enhance binocular vision, control squint or help treat anisometropic amblyopia.
With more than 13 million LASIK procedures having been performed in the United States alone as per 2017 data and more than 40 million worldwide, it is a very commonly performed procedure and is used to correct all refractive errors including myopia, hyperopia, astigmatism and presbyopia.
PREOPERATIVE EVALUATION
Soft contact lenses should be discontinued for two weeks and semisoft for four weeks prior to surgery. Pillar stones of preoperative assessment are proper refraction, clinical examination and corneal tomography. Tomography may be done using slit scanning (Orbscan), Scheimpflug (Pentacam, Galilei, Sirius, TMS-5), reflective LED (Cassini) or OCT tomography (MS39).
Anterior and posterior corneal surfaces, keratometric and pachymetric maps are examined for quantitative and qualitative abnormalities. The Belin Ambrosio Enhanced Ectasia Display is useful for detecting early abnormalities that may rule out LVC. Total ocular aberrations are compared with corneal aberrations to detect significant internal eye abnormalities such as early cataract or lens tilt, in which case lens based refractive correction may be preferred.
Epithelial thickness maps unmask effects of epithelial remodelling on corneal tomography and are gaining prominence. Other adjunct investigations include assessment for dry eyes, corneal biomechanics etc. Glare and haloes may occur irrespective of pupil size and pupillometry, though previously considered important is not specifically correlated with night vision problems.
Special consideration should be given to past history of HSV or HZV, significant dry eye, severe allergy or blepharitis, ptosis, squint, uveitis, glaucoma, retinal abnormalities or corneal diseases such as recurrent erosions, dystrophies, scars, neovascularisation, previous surgery etc. Systemic conditions to be looked for include diabetes, connective tissue and immunodeficiency disorders, pregnancy, lactation and use of certain medications.
Personality type, expectations and occupational needs of the patient also play a role. Deep set eyes, nystagmus, unstable fixation, uncooperative and paediatric patients need special precautions and techniques. Unstable refraction, inadequate residual stromal bed (RSB), forme fruste keratoconus and ectatic corneas are contraindications.
TYPES OF LVC
LVC may be done using excimer laser or via all-femtosecond procedures. Excimer laser procedures include photorefractive
keratectomy (PRK), laser epithelial keratomileusis (LASEK), epi-LASIK and LASIK whereas all femtosecond LVC includes Small-Incision Lenticule Extraction (SMILE®) and Femtosecond Lenticule Extraction (FLEx). Most are equally effective in correcting myopia. Patient characteristics and surgeon preference may dictate choice.
LASIK is the most commonly performed LVC worldwide. A flap consisting of epithelium, Bowman’s membrane and stroma of variable thickness is cut with either microkeratome or femtosecond laser followed by excimer laser ablation of stromal bed. The flap is then reflected back and allowed to adhere. Though the flap allows painless, quick recovery and a “wow” effect, it does not contribute to biomechanical strength and can get displaced even years later. RSB is a crucial calculation and too thin RSB can predispose to ectasia. Femtosecond laser flaps allow advantages of predictability, accuracy, repeatability and safety while allowing thinner flaps with better edge profiles, thus decreasing intra- and postoperative complications such as incomplete, torn or buttonholed flaps, free caps, displaced flap, epithelial ingrowth etc.
PRK involves epithelial removal followed by excimer laser ablation of underlying stroma. Epithelium is removed using dilute alcohol, hockey-stick, Amoil’s brush or even the excimer laser itself. In LASEK and epi-LASIK, the epithelium is reflected as a flap, which is replaced after ablation. Epi-LASIK uses an Epikeratome (an oscillating blunt plastic blade) for this purpose. Though debatable, replacing the epithelial flap is proposed to decrease pain, regression and haze that are potential complications of PRK. Surface ablation procedures are preferred when there is inadequate thickness for LASIK, dry eyes, glaucoma, basement membrane disease, recurrent epithelial erosions and occupational hazard of blows to the face. PRK allows larger optical zone and may be useful in larger pupils. It may also be a better option for enhancements and in wavefront-guided ablations to avoid effect of iatrogenic flap aberrations. Surface ablation should be avoided when postoperative pain is an issue, rapid visual recovery is required or if there is predisposition to haze and regression. Intraoperatively, Mitomycin C is used off-label to decrease haze, especially with high corrections and with prior corneal surgery. Postoperatively, steroids are used for much longer. PRK-Xtra combines accelerated cross-linking in eyes with suspicious topographies.
SMILE and FLEx use femtosecond laser to carve an intrastromal lenticule that is extracted either via a small incision (SMILE) or after lifting a flap (FLEx), thus giving smooth and fast visual recovery. While SMILE has advantages of smaller incisions, fewer flap/cap-related complications, better biomechanical strength and better preservation of corneal nerves leading to less dry eye, FLEx loses these advantages. The vertical flap cut that weakens the cornea is avoided as the vertical entry incision in SMILE is just 2mm.
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 8
SMILE may be offered as first-line treatment to patients with normal topography and may also preferentially be used in thin corneas, high powers and those with occupational risk of blows to face. Hyperopic SMILE is not yet commercially available.
SMILE also has advantage of smoother work-flow. Unlike excimer ablation, which is affected by stromal bed hydration and environmental conditions such as temperature and humidity, SMILE and FLEX are not affected by these.

SMILE can have unique complications such as torn retained lenticule, adherent lenticule, epithelial implantation etc as well as complications common to other LVC such as suction loss, opaque bubble layer, rough dissection, decentred ablation, diffuse lamellar keratitis, infectious keratitis, under- or overcorrection, decreased contrast sensitivity, loss of BCVA, night vision symptoms, ectasia etc.
The White Ring Sign and the ‘sequential, segmental, terminal lenticular-side-cut dissection’ techniques described by the author help avoid difficult dissection and are especially important with thin lenticules.
EXCIMER LASER ABLATION
Excimer LVC can be done for myopia, hypermetropia, regular and irregular astigmatism. Centration of ablation on pupillary axis is sufficient in myopes; however, in hyperopes with larger angle kappa, centration is done on visual axis or in between the two. Centration over entrance pupil increases risk of decentration of optical zone from visual axis in large angle kappa.
The Munnerlyn formula (t = S2 D/3) gives tissue ablation depth (t); s= optical zone diameter (mm); D= dioptric correction. At least 300 microns of RSB is advisable. Percentage tissue altered {PTA = (flap thickness + ablation depth)/central corneal thickness} below 40% has been recommended. Excimer laser LVC may employ various ablation profiles such as wavefront-optimised, aspheric, wavefront-guided, topographyguided, tissue-saving and so on.
Conventional ablation profile induces spherical aberration because of decreased peripheral corneal laser ablation due to angle of incident light on peripheral cornea. Wavefrontoptimised ablation compensates for this by applying additional pulses in the periphery. Wavefront-guided ablations attempt to treat both lower and higher order aberrations of the patient’s cornea by applying complex ablation patterns; however, these are limited to dilated pupil size. Topography-guided ablations
treat a wider zone and with much more detailed image of the corneal refractive surface. All commercial excimer lasers have integrated eye-tracking technology.

SPECIAL SITUATIONS
Enhancements are done after minimum three months and only after confirming refractive stability. Presbyopia may be treated with monovision correction or special multifocal ablation patterns. Patients with ocular hypertension and glaucoma need correction factor to be applied to IOP measurements post LVC. The possibility of pressure-induced stromal keratitis, interface fluid syndrome and false low IOPs should be kept in mind and treated. Post-LASIK IOL power calculations need special attention because of altered anterior to posterior corneal curvature ratio.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Sophi Experience #sophifamily
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 9
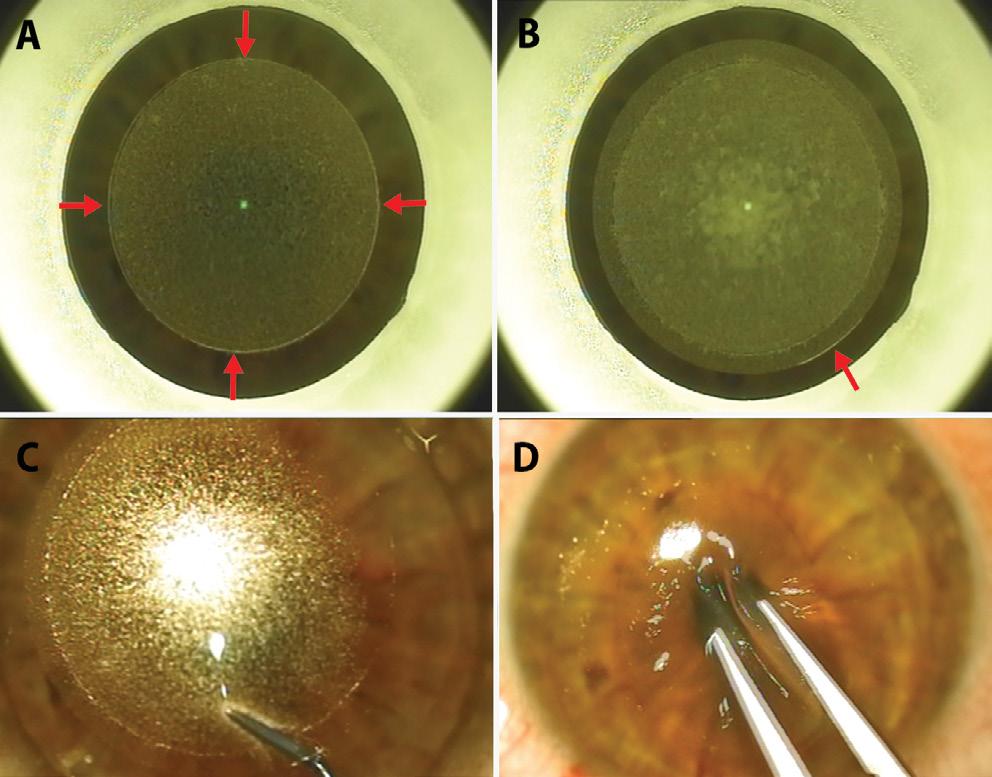
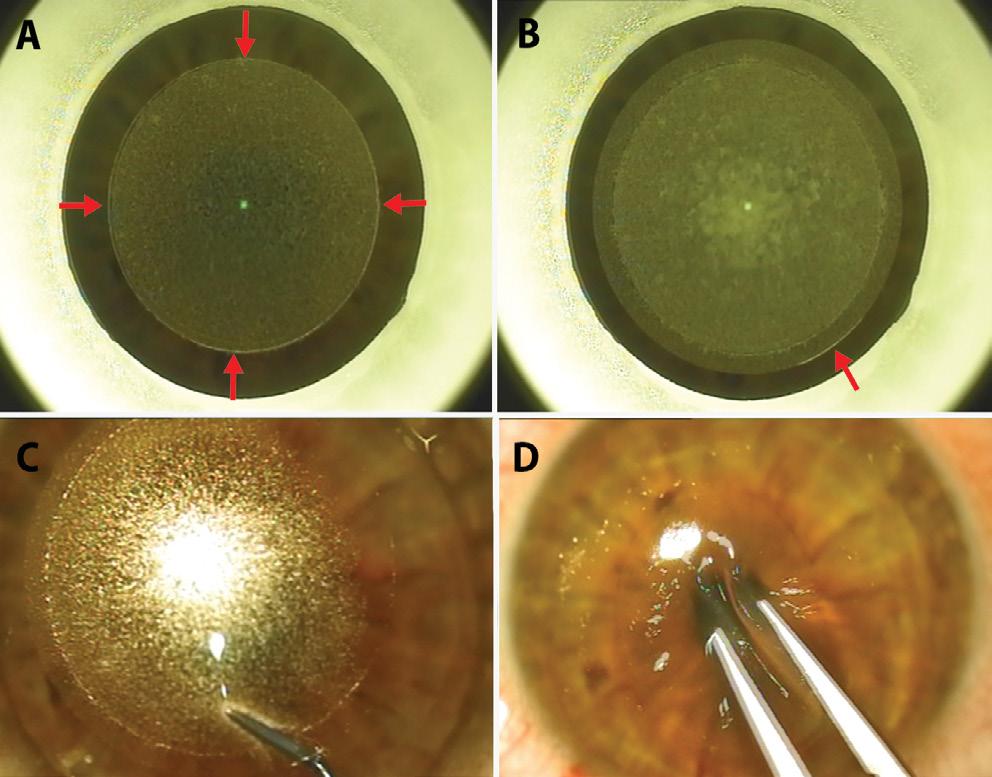
Small-Incision Lenticule Extraction (SMILE): A: Lenticular cut and lenticular side cut (arrows); B: Cap cut and SMILE incision (arrow); C: White ring sign described by the author distinguishes anterior from posterior lamellar dissection; D: Intra-stromal lenticule is extracted.
www.sophi.info
Courtesy of Soosan Jacob MS, FRCS, DNB
«Apart from excellent anterior chamber stability and superior aspiration of cortical material, even with brunescent cataracts, I have much better than expected corneal clarity on the first day post phacoemulsification.»
Junet van der Merwe MD South Africa
A library of symposia, interviews, video discussions, supplements, articles and presentations









Cataract surgeries produce no aerosols
Spotlight on:
Toric IOLs and Presbyopia


Glaucoma
Ocular Surface Disease
Corneal Therapeutics























forum.escrs.org

There are a lot of myths and fear about aerosols pushing doctors to take aggressive precautions
Rohit Shetty MD, PhD, FRCS
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE
10
NEW CONTENT







RayOne EMV is not approved by the US FDA. *Data on file, September 2020. **1.0 D offset between dominant and non-dominant eye. ©2020 Rayner. Rayner and RayOne are proprietary marks of Rayner. Rayner Intraocular Lenses Limited, 10 Dominion Way, Worthing, West Sussex, BN14 8AQ. Registered in England: 615539. EC 2020-73 09/20 MADE IN UK Contact your Rayner representative today. rayner.com/EMV IOLs OVDs RayPRO Rayner Your Skill. Our Vision OSD New patented optic technology is designed to provide: • Up to 2.25 D of extended depth of vision (with 1.0 D offset) • Superior intermediate vision when compared with standard monofocals • Reduced dysphotopsia compared to diffractive multifocal and EDOF IOL designs Delivery via RayOne injector: a fully preloaded two-step system compatible with a sub-2.2 mm incision Dioptres (D) 0.6 0.5 0.4 0.3 0.2 0.1 0 23.5 23 22.5 22 21.5 21 20.5 20 MTF at 50 Ip/mm 24 24.5 0.8 0.7 0.9 1 Far focus, distance vision Aspheric binocular RayOne EMV binocular Aspheric NDE RayOne EMV NDE 2.25 D Through focus MTF at 3mm pupil diameter - L&B model eye** rayner.com/RayPRO Compatible with with rayner.com/RayPRO Three years’ free patient outcomes data on visual outcomes, patient satisfaction, spectacle independence, and more Monovision. Enhanced.* Up to 2.25 D of extended depth of vision
HIGH-TECH cataract surgery
Clinical value of current intraoperative digital technologies for toric IOLs remains unclear. Roibeard Ó hÉineacháin reports
Many new digital imaging technologies designed for intraoperative use in cataract and corneal surgery have become available in recent years, although the increased precision they provide does not always provide the same increase in outcomes, reported Rudy Nuijts MD, PhD, Maastricht University Medical Center (MUMC), Maastricht, The Netherlands.
Two areas where image-guided surgery has made inroads in recent years are digital marking for toric intraocular lens (IOL) rotation and intraoperative aberrometry to increase the accuracy of IOL surgery, said Prof Nuijts at a clinical symposium during 24th ESCRS Winter Meeting in Marrakech.
Dr Nuijts noted that accurate marking of the astigmatic axis is essential to the functionality of a toric IOL. Misalignment by 10 degrees results in 33% reduction in astigmatic correction. The incidence of misalignment greater than 10 degrees in the MUMC cohort is 4%.
Digital marking has the advantages of automatically accounting for cyclorotation and eliminating the need for manual toric eye markings, he said. The first digital marking device to be introduced was the Verion (Alcon). The device is connected to the surgical microscope and provides real-time registration and tracking overlay during surgery. It also receives phaco status information from the phaco machine.
Research suggests that digital marking systems for toric IOLs results in significantly less misalignment of the lens compared to manual marking, although its clinical value remains questionable.
He cited a prospective randomised clinical trial that he and his associates conducted involving 24 patients undergoing toric IOL implantation who were assigned to image-guided or manual marking. That study showed that one hour postoperatively there was significantly less misalignment in the digital marking group compared to manual marking technique (1.2 degrees vs 2.8 degrees, p=.02).


However, there was no statistically significant difference between the two groups
in terms of residual refractive astigmatism, which was less than 0.5D in 82% of the digital group and in 72% of the manual group(p>.05) (Webers, ESCRS 2017, Lisbon) (See also: Webers VSC, Bauer NJC, Visser N, Berendschot TTJM, van den Biggelaar FJHM, Nuijts RMMA. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. JCRS. 2017;43(6):781-788. doi:10.1016/j. jcrs.2017.03.041).
“The improved accuracy does not translate to significantly better uncorrected distance visual acuity,” Prof Nuijts said
Another study indicated that the Callisto digital iris-marking system can also improve the predictability of toric IOL postoperative orientation. However, it indicated that some of the predictability could be lost through IOL rotation during the first postoperative hour.
The study involved 50 patients. Immediately after surgery the deviation from the aimed IOL axis was 0.52 degrees. However, between the immediate postoperative period and one hour postoperatively, the IOLs rotated by a mean of 5.11 degrees with a range of 0.28 degrees to 18.77 degrees (Varsits et al, JCRS 2019;45:1234-1238).
Another imaging approach used in cataract surgery is intraoperative wavefront aberrometry. The technology provides the surgeon with real-time data, enabling the intraoperative refinement of surgical planning. For example, it allows the surgeon to measure aphakic refraction, so that the spherical and cylindrical power of the lens and orientation of the cylinder axis may be adjusted to more accurately match the refraction of the cornea.
At present the only intraoperative wavefront aberrometry system available is
the Optiwave® Refractive Analysis (ORA). The aberrometer is mounted to a surgical microscope cart with touch screen monitor and CPU Secure web-based system. It stores patient clinical data and provides data analysis.
Research suggests that intraoperative aberrometry improves accuracy of spherical power estimation in post-refractive surgery patients compared to older IOL calculation formulas, but performs roughly equally with more modern IOL calculation formulas in astigmatic eyes.
In a retrospective consecutive cases series of 215 patients who had previously undergone LASIK, postoperative refraction was less than 0.5D off target in 67% with the ORA, compared to 46-50% with conventional preoperative methods such as the Haigis formula (Lanchulev et al, Ophthalmol 2014;121:56).
Prof Nuijts reported another study from his centre involving 151 patients, where spherical equivalent refraction was less than 0.5D off target in 89% with the ORA system compared to 74% with SRK-T formula (Webers, JCRS 2017, 43:781-788).
Regarding toric IOLs, in a study involving 50 eyes of 38 patients, the overall prediction error and residual astigmatism did not differ significantly between the ORA aberrometry and the Alcon Barrett Toric calculation, which was 0.49 D with both.
However, among a subgroup of eyes where the ORA suggested different power calculations or astigmatic axis for the toric IOL, the prediction error for the implanted IOL was significantly less with the ORA than with the Barret toric IOL calculator (0.44D vs 0.73D).
“When considering new technology, it is important to keep in mind that results can be quite variable. Different studies have yielded different results with the same devices,” Prof Nuijts cautioned.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 12
The improved accuracy does not translate to significantly better uncorrected distance visual acuity
Rudy Nuijts MD, PhD
Turning to topography
Strong
Dermot McGrath reports
Using preoperative corneal topography or tomography enhances the security and accuracy of biometry and should be considered as a potentially valuable addition to all cataract surgery procedures and not just for implanting toric lenses, according to Steve Arshinoff MD.
“Using topography or tomography allows greater certainty of the corneal contribution to biometry and enables us to achieve the 90% of patients within 0.5D of the targeted refraction, which Warren Hill has claimed is achievable,” Dr Arshinoff said at the World Ophthalmology Congress 2020 Virtual.
Topography defines the anterior curvature of the cornea with technology based on the ground-breaking work by Antonio Placido in the 19th Century, said Dr Arshinoff. Devices based on this concept include hand-held keratoscopes and a range of Placido disc topographers (Atlas, Nidek, OPD, Schwind Peramis, etc). There is the also the scanning slit technique (Orbscan) capable of measuring both the anterior and posterior surfaces of the cornea.
Scheimpflug tomography (Oculus Pentacam, Ziemer Galilei, Schwind Sirius) renders 3D images of the cornea and is better equipped than topographers to detect the posterior cornea, keratoconus and early ectasia, he added.
Accurate biometry requires at least two measurements by different devices of axial length and corneal power (Ks), Dr Arshinoff explained.
The rationale for using topography is that while only about 10% of corneas are found to be irregular, identifying this significant minority is not possible unless you use equipment adapted to the task.
“In 90% of cases the IOLMaster or Lenstar will be accurate enough so that topography can be ignored. However, not all corneas are perfect and using topography or tomography allows us to detect the amount and type of LASIK that a patient has had, an irregular bowtie pattern or other corneal irregularities,” he said.
Dr Arshinoff said that he has been performing preoperative corneal topography in every patient since 1990. This enables him to identify patients with irregular corneas or those who had undergone corneal surgery in the past and to prepare specific treatment plans in order to obtain better outcomes.
However, he believes that tomography is now preferable to topography because it additionally accurately assesses the posterior surface of the cornea.
“If you are still using topography, I advise to estimate 0.5D against-the-rule total corneal power above the value shown by the topographer. My technique is to leave all patients with 0.5D with-the-rule astigmatism postoperatively because that decreases with age and patients are happy because they feel that they get better as time passes,” he said.
• First and Only Single-Use, stand-alone device for ophthalmic cryosurgery

• Few seconds activation to reach cryogenic temperatures1
• Approximately 15 freezing cycles at same patient
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE
rationale to use topography or tomography for all cataract surgeries.
| Straightforward | Compelling
bvimedical.com Unique
BVI, BVI Logo and trademarks are property of BVI © 2020. 1567656-02 References 1 CryoTreq Technical File STED 2.2.4 ”Performance Specifications: In a water bath at a temperature of 37 °C, an ice ball will be formed with a layer thickness of 0.8 mm within 6 seconds”. 1567656-02 BVI CryoTreQ Ad Eurotimes v2.indd 1 9/9/20 2:23 PM 13
In 90% of cases the IOLMaster or Lenstar will be accurate enough so that topography can be ignored
Steve Arshinoff MD
Managing dysphotopsia after cataract surgery
Understanding causes can help avoid or reduce impact. Howard Larkin reports
Understanding the causes of post-cataract and refractive surgery visual disturbances, including positive and negative dysphotopsias and entopic phenomena, can go a long way toward preventing or reducing their impact, according to Jack
T Holladay MD.
The first step in managing such symptoms is to determine if the visual disturbance is entopic or an optical dysphotopsia, said Dr Holladay, of Baylor College of Medicine, Houston, Texas, USA. Entopic phenomena typically are arcuate or central flashes caused by vitreous traction on the retinal periphery or macula and are visible in light and darkness.
“Telling if it’s entopic is simple – the patient sees the flash with his eyes closed,” Dr Holladay said.
Such phenomena are common after cataract surgery because the intraocular lens (IOL) takes up only about 6% of the crystalline lens volume, leaving plenty of room for the vitreous to move after surgery. He recommended referring these cases to a retinal specialist for evaluation and treatment.
NEGATIVE DYSPHOTOPSIAS
Negative dysphotopsias, which generally are arcuate shadows or dark lines along the temporal edge of the lens, sometimes with light on both sides of the line, are fairly easy to see, Dr Holladay said. Using ray tracing, his research shows that the line results from a shadow cast by the edge of the lens when light coming in at steep angles – around 88 degrees – misses the edge of the lens.
These shadows are likely to be wider in eyes with smaller pupils, larger angle kappa, an equi-biconvex or plano-convex IOL, smaller axial distance from iris to IOL and with the anterior capsule overlying the nasal IOL. IOL edge design, material, power, diameter, decentration, tilt and aspheric surfaces also are factors (Holladay JT, Simpson MJ. J Cataract Refract Surg. Feb 2017;43:263-275).
Dr Holladay said negative dysphotopsias appear immediately after surgery in about 16% of cases. Of these, 80% resolve spontaneously.
“That’s because the peripheral capsule, as it opacifies, scatters the light.”
Other treatment or prevention options include removing the nasal overlapping capsule and reverse optic capture. Peripheral shadows also may be eliminated by an IOL with a concave surface around the posterior periphery, which spreads light across the shadow area on the retina (Erie JC et al. J Cataract Refract Surg. July 2019;45:1023-19).
POSITIVE DYSPHOTOPSIAS
Positive dysphotopsias range from snowballs, haloes, starbursts and streaks to night-time arc flashes from headlights, and daytime crescents and partial rings from the sky. Dr Holladay noted that they are more common in IOLs with
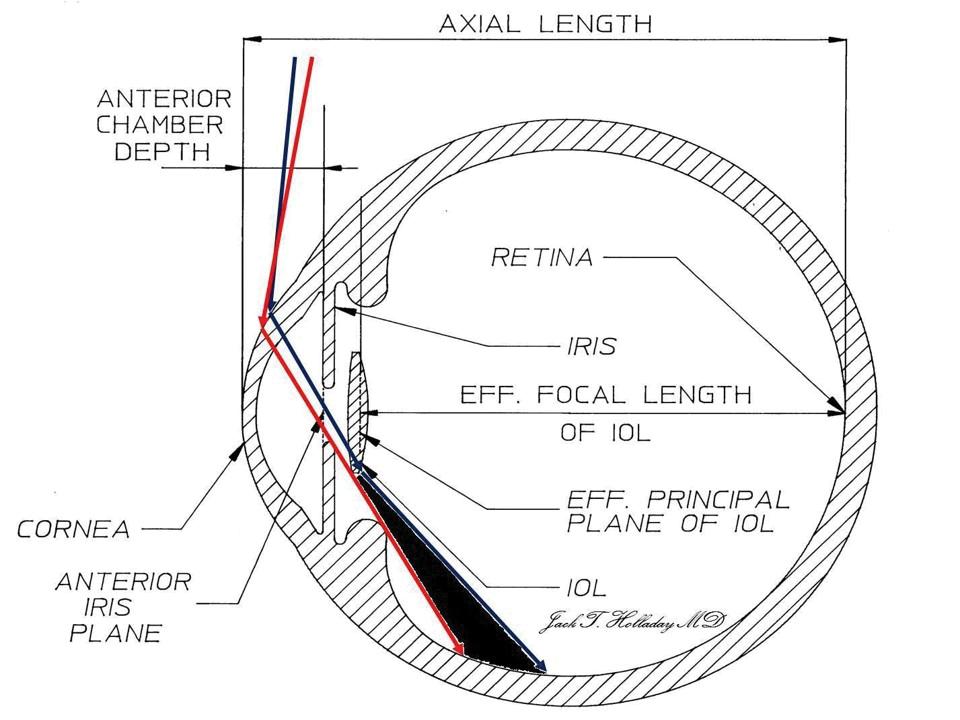
The red ray is the most posterior ray on the retina that misses the IOL. The blue ray is the most anterior ray that passes through the IOL. With high index of refraction IOLs with truncated edges there is a gap (light void) that occurs ~ 16% of the time immediately following cataract surgery and decreases below 2-3% within two years
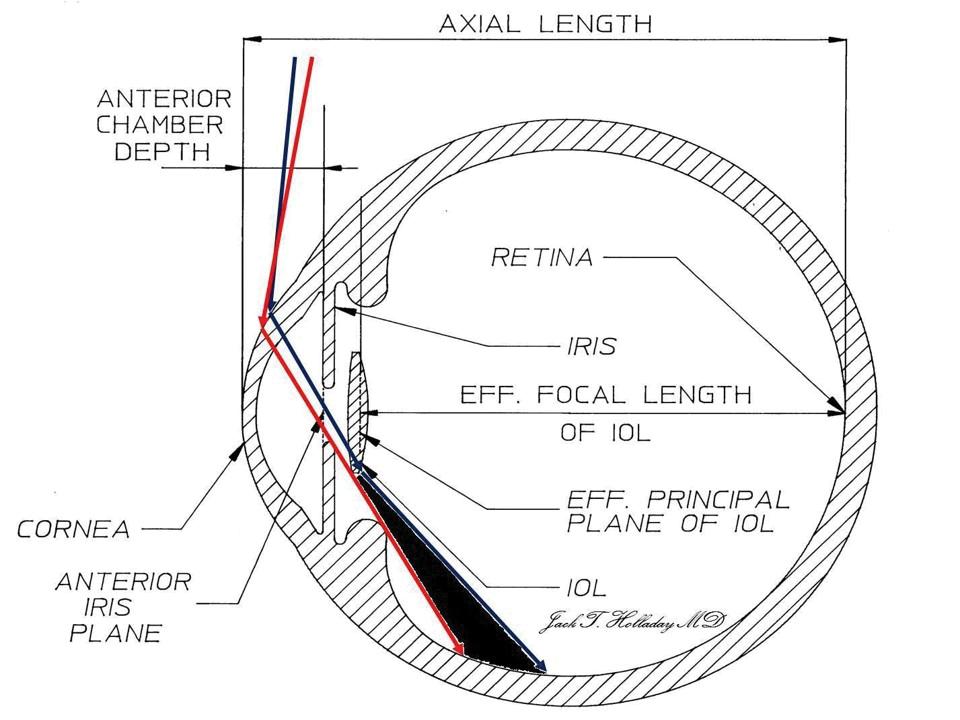
diffractive optics, a high index of refraction and truncated edges. Patient risk factors include a high apparent chord μ or high corneal higher order aberrations.
Chord μ is the distance between the apparent pupil centre and the light reflex, or first Purkinje image, Dr Holladay explained. If it is greater than 0.6mm, performance of diffractive lenses will degrade to the point that they should not be implanted. Most current biometry devices, including the Lenstar (Haag-Streit) and IOLMaster (Zeiss), report chord μ values, he said.
For smaller chord μ distances, centring multifocal diffractive IOLs halfway between the pupil centre and the visual axis minimises dysphotopsias, Dr Holladay said.
“It wants to be in both places, but it can’t, so the best compromise is halfway in between,” he advised.
Topographic measurement of wavefront error due to higher-order aberration is also a good indicator of refractive surgery success, Dr Holladay said.
“If it is over 1.0 micron over a 6.0mm zone, that patient is not going to see well. They’re going to complain of glare and haloes and that’s true whether it is post refractive surgery with a laser or cataract surgery.”
A normal corneal topography value is 0.38±0.14 microns HO RMS. Research shows that patients who were happy with their LASIK outcomes had a mean HO RMS of 0.58±0.21 microns compared with 1.31±0.58 microns for unhappy patients (McCormick GJ et al. Ophthalmology. Oct 2005; 112(10):1699-709).
New research classifying different patient-reported dysphotopsias will help evaluate and improve IOL designs, Dr Holladay concluded.
Jack Holladay: holladay@docholladay.com
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 14
Courtesy of Jack T Holladay MD
Fixing neuroadaptation
Patients with failed neuroadaptation to multifocal IOLs might achieve high satisfaction through exchange with a multifocal IOL with optical characteristics different in the optical profile to the one implanted more suited to their needs, said Prof Jorge Alió MD, PhD, Miguel Hernández University and Vissum Miranza, Alicante Spain.
A series of 43 eyes of 25 patients who failed in their neuroadaptation to previously implanted multifocal IOLs had high levels of satisfaction and significant improvements in uncorrected and best-corrected vision, after exchange of a diffractive multifocal IOL with a refractive multifocal or vice versa, Prof Alió told the 24th ESCRS Winter Meeting in Marrakech, Morocco.
Residual refractive error was excluded as the reason for dissatisfaction in all cases prior to the diagnosis of neuroadaptation failure. Among the explanted IOLs, 42% were refractive multifocals, 21% were diffractive multifocal, 21% were Precizon presbyopic lenses and 16% were EDOF lenses. Of the implanted IOLs, 42% were refractive and 58% were diffractive. The reasons for exchange included photic phenomena in 23%, blurred vision in 61%, insufficient near vision in 8% and monocular diplopia in 8%. The mean time from the initial implantation to multifocal IOL exchange was nine months.

The multifocal IOL exchange procedures were successful in all cases with no significant complications, Prof Alió said.
After a mean follow-up of 2.9 months, the mean uncorrected distance visual acuity (UDVA) improved significantly from 20/35 to 20/26 after the exchange(p=0.001). The corrected distance visual acuity (CDVA) improved from 20/27 to 20/21 (p=0.002) and corrected binocular distance visual acuity improved from 20/23 to 20/19 (p=0.005). There was no significant change in spherical equivalent.
In their responses to a subjective quality of vision questionnaire, the patients’ frequency of visual symptoms subscale values were significantly lower after the IOL exchange (p=0.41). The severity subscale was also lower postoperatively, although the difference did not reach statistical significance (p=0.073).
In addition, the percentage of patients saying they had good and very good satisfaction increased from 33% to 83.3%. Furthermore, 90% of patients reported they would repeat the procedure, compared to 20% before the exchange procedure.


Prof Alió noted that although the surgery can be difficult, previous studies have shown that exchanging a multifocal for a monofocal IOL can produce good results in patients with neuroadaptation failure. However, patients who are highly motivated to be spectacle-free may be disappointed with a monofocal outcome.

“Treatment of neuroadaptation failure following multifocal IOL surgery by multifocal IOL exchange with a different multifocal IOL with a different optical profile improves quality of vision, visual function and significantly increases patient’s satisfaction,” he concluded.
Jorge Alió: jlalio@vissum.com

EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE
Multifocal IOL exchange with different optics can remedy neuroadaptation failure. Roibeard Ó hÉineacháin reports
15
New IOL tech: A lot in the pipeline
Options include EDOF, adjustable modular and accommodating designs. Howard Larkin reports
Arange of new technology intraocular lenses addressing everything from presbyopia to refractive surprise are on the market or on the horizon, Sumit Garg MD, said at the ASCRS Virtual Annual Meeting 2020. He provided a rundown of several.
EDOF MONOFOCAL
Tecnis Eyhance (Johnson & Johnson Vision, Santa Ana, California, USA), now available in Europe and elsewhere outside the USA, is a refractive technology monofocal lens that provides one line of improvement in intermediate vision. This is achieved with a progressive power change and higher order aspheric surface that add power toward the centre of the lens. The lens is virtually indistinguishable from the conventional Tecnis monofocal lens and has a glare profile similar to monofocal lenses, said Dr Garg, of the Gavin Herbert Eye Institute, University of California, Irvine, USA.
EDOF WAVEFRONT
AcrySof IQ Vivity (Alcon, Fort Worth, Texas, USA) extends depth of focus using a proprietary non-diffractive wavefront altering design, creating a continuous range of vision across distance and intermediate range. The lens’s visual disturbance profile is similar to a monofocal lens, with the majority of patients not bothered by haloes, glare or starbursts. Approved by the FDA in February, Vivity is available in Europe and launches in the USA this year.
SMALL APERTURE
IC-8 (AcuFocus, Irvine, California, USA) uses a small aperture to extend depth of focus. The pinhole optics also provide a benefit in aberrated corneas, Dr Garg said. Available outside the USA, IC-8 recently completed enrolment for its FDA clinical trial.
EDOF + MULTIFOCAL
Tecnis Synergy (Johnson & Johnson Vision, Santa Ana, California, USA) combines the diffractive extended depth of focus
(EDOF) technology of the Symfony with multifocality to create a continuous range of vision from distance to 33cm, without the drop-out at intermediate distances seen with many previous multifocal designs, Dr Garg noted. The lens is available in Europe, Australia and New Zealand.
EnVista trifocal (Bausch + Lomb, Rochester, New York, USA), available in Europe since 2017, is in FDA clinical trials for registration in the USA, Dr Garg said.
MODULAR IOLS
Omega Gemini refractive capsule (Omega Ophthalmics, Lexington, Kentucky, USA) consists of a capsule-filling module into which various lenses can be inserted, potentially allowing lenses exchange in cases of residual refractive error or patient intolerance of a multifocal or other lens type. The modular design also allows for placement of drug delivery or sensors in the capsular bag space, Dr Garg said. Harmoni (ClarVista Medical, Alcon, Fort Worth, Texas, USA) is a modular IOL consisting of a base with haptics similar to a conventional IOL, but the optic snaps in and can be exchanged, Dr Garg said.
TRUE ACCOMMODATING IOLS
FluidVision (PowerVision, Alcon) is a true accommodating IOL design consisting of a clear deformable optic filled with fluid attached to peripheral reservoirs that change the shape and refractive power of the lens in response to accommodative effort. The lens is in development, Dr Garg said.
Atia Vision (Shifamed, Campbell, California, USA) is a modular dual optic accommodating lens design in which the accommodating engine and posterior optic are implanted in the capsule with and exchangeable fixed front optic. A hydraulic multiplier changes the shape
of the posterior lens in response to accommodative effort, Dr Garg said.
Opira (ForSight Labs, Menlo Park, California, USA) is a sulcus-based accommodating IOL that fixes haptics in the capsulorhexis, putting them in direct contact with the ciliary body. Contractions pump fluid into the anterior optic, changing its shape and power, Dr Garg said.
Juvene (LensGen, Irvine, California, USA) is a fluid-filled modular accommodating IOL with a base that fits into the capsule, changing the shape and power of the removable optic, allowing continuous vision from distance to near in response to accommodative effort, Dr Garg said. He presented a case from the Grail exploratory study in Mexico.
A 65-year-old female had Juvene IOLs implanted in both eyes through 3.0mm incisions after cataract removal. Six months after surgery she had uncorrected distance visual acuity of 20/25-1 in the right eye and 20/25-2 in the left, with refractions of -0.25D-0.75Dx065 and -0.5D-0.5Dx70 respectively. Binocularly distance corrected, she achieved 20/16+1 at distance, 20/20+2 intermediate and 20/20-1 at near.
Similarly, mean distance-corrected binocular defocus for 15 patients implanted with the lens was 20/16 distance, 20/25+ intermediate at 66cm and 20/32+ near at 40cm.
“What’s exciting about this lens is patients did not complain of dysphotopsias,” Dr Garg said. In addition, PCO formation has not been observed with this lens clinically, and the capsule has remained much clearer than conventional IOLs in contralateral eye rabbit studies.
“There are many innovative designs coming down the pike. The creative optics and designs are certainly exciting. I look forward to the opportunity to use them in my patients,” Dr Garg concluded.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 16
What’s exciting about this lens is patients did not complain of dysphotopsias
Sumit Garg MD



www.icare-world.com DRSplus is a device manufactured by Centervue Spa. iCare is a registered trademark of ICARE FINLAND OY. CENTERVUE S.P.A., ICARE USA INC. and ICARE FINLAND OY are parts of REVENIO GROUP and represent the brand iCare. The world is full of beauty. Our mission is to keep it visible for all. More information: info@icare-world.com iCare DRSplus Automated TrueColor retinal imaging + TrueColor confocal imaging + Ultra-high resolution + Fast image acquisition + No dilation (2.5 mm pupil size) You can meet us at Virtual ESCRS! NEW! Remote Exam functionality allows you to acquire retinal images remotely, extending the distance between you and your patient.
Still a place for the anterior chamber IOL
Careful patient selection and rigorous surgery key to success with modern AC IOLs. Dermot McGrath reports
Although they have a chequered history and a mixed reputation among cataract surgeons, anterior chamber intraocular lenses (AC IOLs) may still be a viable option in carefully selected patients with minimal or no capsular support, according to Richard Packard MD, FRCOphth.
“The advantage for many surgeons in implanting AC IOLs in cases with lack of capsular support is that it is a relatively straightforward technique and can be completed fairly quickly. While there will inevitably be some endothelial cell loss, it is usually manageable and the benefits may outweigh the risks for older patients who might not be able to tolerate a longer operative time,” Dr Packard said at the World Ophthalmology Congress 2020 Virtual.
BAD REPUTATION
In a broad overview of the complications associated with AC IOLs, Dr Packard noted that these lenses understandably received a bad reputation dating back to their initial use by Harold Ridley in the 1950s.
“Harold Ridley found that the posterior chamber IOL was unstable, so he and others moved to the anterior chamber. The most popular design, the Strampelli lens, was widely implanted but the results were not very good. As early as 1956 Hallermann stated that corneal degeneration was a severe complication of angle-fixed IOLs and Nordholm in 1975 reported that Barraquer had to remove 250 of 493 AC IOLs implanted. Bob Drews in 1979 was able to examine half of these explanted IOLs and found them to be rough and poorly
manufactured,” said Dr Packard.
Some of the common complications associated with the early anterior chamber intraocular lenses included reduced corneal endothelial cell count leading to corneal decompensation, glaucoma related to angle obstruction or distortion, dislocation of the implant and chronic uveitis.
“These disasters were due to a lack of understanding of lens design and the effect it would have on the corneal anatomy,” said Dr Packard. The IOL manufacturing standards of the day also played a part, with rough edges of the haptics that were in direct contact with the irido-corneal angle, wreaking havoc on the corneal endothelium.
The rigidity of AC IOLs was also deemed to be a factor in promoting corneal damage, which led to a plethora of flexible loop designs, said Dr Packard.
“None of these IOLs stood the test of time except for one – the Kelman Quadraflex, which was then adapted by Charles Kelman into the Multiflex design. This IOL design incorporated many lessons learnt from Peter Choyce, the most important being the correctly sized footplate and that it should be a planoconvex optic for an AC IOL,” he said.
POTENTIAL COMPLICATIONS
As well as corneal decompensation, surgeons also need to be vigilant concerning several other potential complications associated with AC IOL implantation, said Dr Packard.
“The list includes uveitis-glaucomahyphema syndrome (UGH), where parts of the vasculature of the anterior and posterior chamber would be eroded by the lens
and cause intermittent bleeding and high pressure. Also, if there wasn’t an adequate iridectomy or iridotomy, then iris bombe could form around the lens. Iris tuck could also occur, and sometimes the lens was too small which would cause considerable erosion of endothelial cells,” he said.
The scientific literature on the use of modern-design AC IOLs lends credence to their safety and viability in selected cases, said Dr Packard. For instance, a paper by Kendall Donaldson et al. in 2005 reported that no significant differences were found in outcomes comparing AC IOLs to sutured PC IOLs in complicated cataract extraction with poor capsular support.

In 1996, Bellucci et al. reported that scleral-fixated posterior chamber IOLs were associated with more intraoperative and postoperative complications than angle fixated AC IOLs and surgery took longer. They concluded that anterior chamber IOL implantation should be considered for older patients with relatively good endothelial cell counts.
SUCCESSFUL OUTCOMES
There are a number of factors involved in obtaining successful outcomes with AC IOLs, said Dr Packard.
“We need devices to measure the white to white and incision size and a good understanding of correct lens sizing with an adequate IOL bank of at least three sizes for each IOL power. We need to recalculate for the correct A constant (115.3). We should also have Miochol or a similar product to constrict the pupil and a Sheets lens glide and cohesive viscoelastic to help implantation. A vitrector is also useful to do an anterior vitrectomy if required and perform an iridectomy. Finally, triamcinolone is helpful to expose any vitreous as part of the anterior chamber clean-up prior to implantation,” he said.
Summing up, Dr Packard said that AC IOLs offer an efficient and straightforward implantation method in compromised eyes and particularly in older patients.
“Provided certain basic rules of measurement and insertion are applied you should be able to get good results and avoid any serious complications,” he concluded.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 18
The advantage for many surgeons in implanting AC IOLs in cases with lack of capsular support is that it is a relatively straightforward technique and can be completed fairly quickly
Richard Packard MD, FRCOphth
Post-op IOL adjustment
Several technologies in development and on the market can help reduce residual refractive error. Howard Larkin reports

Several new technologies are available or on the horizon for adjusting intraocular lens (IOL) power after implantation, Burkhard Dick MD told Refractive Surgery Day at AAO 2019 in San Francisco, USA. These include both invasive and noninvasive techniques for correcting residual refractive error, which is especially important for success in post-keratorefractive surgery eyes, and with premium multifocal and extended depth of focus IOLs.
Multi-component lenses require a second surgical procedure to adjust, Dr Dick said. Examples include the PreciSight (InfiniteVision Optics), in which the upper of a two-piece lens system can be changed, and the Harmoni (ClarVista), in which a central optic that is supported by a permanent scaffold can be changed. Monofocal, multifocal, toric and pinhole lenses can be exchanged in these devices, which are available outside the USA.
Dr Dick believes these devices are most appropriate for patients likely to require a secondary IOL intervention, such as those with paediatric cataracts, progressive corneal pathology including keratoconus, or tamponades from vitreoretinal surgery.

Laser-induced refractive index change (LIRIC) technologies, in which a femtosecond laser is used to change the refractive power or inscribe Fresnel lenses in corneal tissue or an in vivo IOL, are getting close to market, Dr Dick said.
Clerio Vision has successfully used LIRIC to write a -2.0D Fresnel lens in contact lenses as well as a live cat eye and has successfully induced refractive index changes in a living human cornea. A first-in-human study by Scott McRae MD inscribed a presbyopia-correcting pattern in corneas that significantly improved near vision, Dr Dick noted. Perfect Lens has successfully adjusted the power of IOLs implanted in living
rabbits and has added or cancelled multifocality in a model eye. Merck has developed LicriEye, a polymer designed to accept reversible refractive index changes, though no commercially viable product has yet been presented. Medicem has developed a hydrogel IOL material that is specifically designed to accept high LIRIC power changes, Dr Dick said.
Furthest along is the Light Adjustable Lens (LAL), which has gained FDA approval in the USA, with a 2.0 version on the market in Europe. The new lens and device reduce retinal UV irradiance by ten-fold and supports new optical patterns, including an expanded range of astigmatism correction and extended depth of focus, said Dr Dick, who helped develop the LAL.
With nearly 30% of patients missing refractive targets by 0.75D or more, IOL adjustment technologies will improve patient outcomes, Dr Dick said.
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE
19 Perfectionist. Analyst. Visionary. Organizer. Visit us at the virtual ESCRS 2 – 4 October All your benefits at a glance at: www.oculus.de/online-show Experts on diagnostics, refractive and cataract surgery and IOLs on all OCULUS products for a limited period only Schedule an exclusive chat with one of our product experts by Dr Auffarth, Dr Kohnen and Dr Savini Online Seminars Anniversary Discount NEW Supplement Live Chat What Pentacam® type are you? Find the answers online. There’s lots of inspiration waiting for you at our interactive OCULUS Online Show.
Preventing toric IOL rotation
Rotational stability remains key to optimal results with toric IOLs.
Dermot McGrath reports
Improvements in toric intraocular lens (IOL) material and design, as well as refinements in surgical technique, have greatly enhanced postoperative rotational stability of these lenses in recent years, according to Boris Malyugin MD.
“Toric IOLs deliver excellent visual acuity and high patient satisfaction by a reduction or elimination of the astigmatic error. However, residual error may happen and can impact on the clinical results we obtain, so the stability of the lens in the capsular bag is absolutely vital with these IOLs,” Dr Malyugin said at the World Ophthalmology Congress 2020 Virtual.
Underscoring the importance of stability in toric lenses, Dr Malyugin, Professor of Ophthalmology at the S. Fyodorov Eye Microsurgery Complex Federal State Institution, Moscow, Russia, noted that a postoperative rotation of 30-degrees equates to 100% loss of cylinder power.
“In other words, the entire effect of the toric lens is lost. Even just a 1-degree rotation translates to 3% loss of cylinder power and a 90% rotation actually doubles the astigmatism – this is why it is so important for the IOL to remain stable in the capsular bag,” he said.
Precise axis alignment is a critical step in obtaining optimal refractive outcomes with toric IOLs, and there are a wide range of low- and high-tech approaches available to achieve this, said Dr Malyugin. As well as traditional methods to mark the eye manually using handheld instruments, many manufacturers now offer specialised devices for intraoperative corneal marking, digital alignment and centration of the IOL.
“Although manual marking remains very popular, it is prone to error. There is a growing body of evidence in the scientific literature showing that digital marking or image guided systems are superior to manual marking methods, and we need to keep that in mind,” he said.
Another interesting high-tech approach, described by H Burkhard Dick and Tim Schultz, is to use spectral domain
OCT combined with a femtosecond laser to create two perpendicular intrastromal marks on the anterior capsule for precise axis marking.
Dr Malyugin noted that certain ocular co-morbidities can also have a direct impact on postoperative toric IOL stability.
“High myopia, for instance, is usually associated with a large diameter of the capsular bag. Likewise, ocular trauma, pseudoexfoliation and uveitis are all conditions that may lead to the weakening of the lens zonular apparatus and create instability of the lens,” he said.
In terms of lens material, Dr Malyugin noted that several studies have shown greater propensity to rotation with lenses made of silicone compared to acrylic IOLs. Furthermore, a study by Draschl et al (JCRS, 43(2):234-238) comparing two identical non-toric IOL designs found that hydrophobic material offered greater rotational stability than the lens made of hydrophilic material.
The development of strong adhesions between the IOL and lens capsule in the early postoperative period seems to be a key factor in the superior performance of hydrophobic acrylic IOLs, added Dr Malyugin.
Early postoperative rotation is also influenced by axial length. A study by Shah et al ( JCRS, 38(1):54-59) of the AcrySof (Alcon) toric IOL in 168 patients found a strong correlation between axial length and IOL rotation, with longer axial length associated with greater rotation of the lens.
SURGICAL TECHNIQUE
Rigorous surgical technique can play a role in safeguarding toric IOL stability, said Dr Malyugin.
“It is very important at the end of the implantation step to ensure that all the ophthalmic viscosurgical device (OVD) is aspirated from the capsular bag. Otherwise it can remain underneath the IOL optic and allow the lens to rotate,” he said.
Certain situations may also call for the use of a capsular tension ring (CTR) to avoid rotation of the lens.
“The CTR has been shown to be effective with a silicone plate-haptic toric IOL and may also help to stabilise loophaptic hydrophobic acrylic IOLs. There are some publications showing double use of standard CTRs in the capsular bag to obtain rotational stability in patient with long axial length,” he said.
Suturing the CTR to the toric lens has also proved effective for long axial length eyes in a method described by Claudio Orlich (https://www.eurotimes.org/howto-deal-with-iols-in-large-eyes/).
Dr Malyugin noted that the vast majority of the postoperative rotation is believed to take place within the first hour after surgery.
“This was shown in an interesting study by Inoue et al ( Ophthalmology 2017 Sep;124(9):1424-1425). With that in mind, it is better that patients avoid physical activity or movement in the first hour after surgery in order to allow the lens to settle in the capsular bag,” added Dr Malyugin.
Summing up, Dr Malyugin said that careful biometry, precise axis alignment and rigorous surgical technique could help to ameliorate many of the problems related to postoperative toric IOL rotation and deliver consistently good outcomes for astigmatic patients.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 20
Toric IOLs deliver excellent visual acuity and high patient satisfaction by a reduction or elimination of the astigmatic error
Boris Malyugin MD
Trifocal IOL power calculation
Pentacam corneal map best for trifocal IOL power calculation. Roibeard Ó hÉineacháin reports
Intraocular lens (IOL) power calculations for trifocal IOLs performed with standard formulas appear to be more predictable when using keratometric data from total corneal power maps obtained using the Pentacam®(Oculus) than when using keratometric data from the IOLMaster, according to a study presented by Sergey Shukhaev MD, S. Fyodorov Eye Microsurgery Federal State Institution, St Petersburg, Russia.

The study involved 45 eyes of 30 patients with axial lengths ranging from 23mm to 24mm who underwent femtosecond laser-assisted cataract surgery (FLACS) with a main corneal incision of 2.3mm and implantation of a trifocal diffractive AcrySof IQ PanOptix IOL (Alcon), Dr Shukhaev told the ESCRS Winter Meeting in Marrakech.
At one-to-three months postoperative, IOL power was calculated on the IOLMaster 500 (ver. 5.4 Carl Zeiss Meditec AG) using four formulas (Haigis, HofferQ, Holladay 1, SRK / T) and four different types of keratometric data, namely the IOLMaster, the total corneal power in the 4mm zone from the Pentacam Cataract Pre-Op map (map 1), keratometry in the actual zone from the Pentacam EKR Holladay report (map 2) and keratometry (axial/sagittal map) in the actual zone from the Pentacam Power Distribution (map 3). Their analysis showed that the deviation of the calculated refraction from the postoperative values of refractometry and subjective correction was significantly lower when using the Hoffer Q and Holladay 1 formula with the Pentacam total power map (map 1) keratometric data than it was when using IOLMaster keratometric data, Dr Shukaev said. That is, the mean absolute error (MAE) when using the IOLMaster keratometric data was 0.60D with the Hoffer Q formula and 0.87 D with the Holladay 1 formula, compared to respective values of 0.37D and 0.64D when using the Pentacam map 1 data (p<0.05).

There were no significant differences between the MAE obtained with the IOLMaster compared with the keratometric data Pentacam EKR Holladay map 2 and the Pentacam power distribution map 3, which had respective values of 0.51D and 0.59D, when using the Hoffer Q formula, and 0.78 and 0.57D, when using the Holladay 1 formula.
“When calculating using the keratometric data from the Pentacam Holladay EKR Detail Report and Power Distribution cards, there were no significant differences compared to the IOLMaster data. However, there was a lower average calculation error when using data from the presented Pentacam cards compared to the IOLMaster data,” Dr Shukaev noted.
Sergey Shukhaev: shukhaevsv@gmail.com



EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE
Pod F GF 2017 Pod L GF 2019 To be continued Micro F 2010 Pod F 2013 Pod FT 2014 BVI, BVI Logo and trademarks are property of BVI © 2020. 1565388-03 bvimedical.com 1565388-03 FineVision 10 Year Thank You Ad EuroTimes FINAL.indd 1 9/8/20 5:49 PM 21
...for providing the Gold Standard to your patients
The study involved 45 eyes of 30 patients with axial lengths ranging from 23mm to 24mm
Sergey Shukhaev MD
Multifocal IOLs
Better patient selection leads to better results in an era of personalised visual care. Dermot McGrath reports
The performance and safety of the latest generation of multifocal IOLs gives surgeons the opportunity to offer presbyopic patients a truly customised solution for their visual needs with high levels of patient satisfaction, according to Daniel Kritzinger MD, president of the Southern African Society of Cataract and Refractive Surgery.
“There are so many modalities available today with bifocal, trifocal and extended depth of focus (EDOF) lenses in addition to traditional monovision with monofocal IOLs. The goal I feel should always be individualised decision-making, whichever approach one prefers to take. We are in a position where we can address our patients’ needs and deliver high levels of spectacle independence,” he said at the World Ophthalmology Congress 2020 Virtual.
Dr Kritzinger, in private practice at Visiomed Eye Laser Centre, Johannesburg, South Africa, said it was important not to get drawn into a sterile monofocal versus multifocal IOL debate.

“There is no one-size-fits-all solution for presbyopia correction in cataract patients, but I strongly feel that if total spectacle freedom is high on the agenda for the patient and surgeon, then they will definitely have the best chance of achieving this result using a multifocal intraocular lens. I see no other way of achieving that,” he said.
With only about 6% of cataract procedures involving a presbyopiacorrecting IOL, the preference for most surgeons today is still a monovision approach using a monofocal IOL, noted Dr Kritzinger. Issues of haloes and glare and reduced contrast sensitivity associated with multifocal IOL
implantation have definitely hampered their uptake but are far less of an issue with modern lenses, he said.
As evidence, he cited the fact that IOL exchange rates for unhappy multifocal patients have dropped dramatically over the past decade.
“In addition, a lot of the reasons for unsatisfactory results are actually treatable and if you address residual refractive errors postoperatively as well as posterior capsule opacification (PCO), up to 80% of these unhappy cases could be resolved,” he said.
Dr Kritzinger stressed the importance of managing patient expectations and selecting a lens based on factors such as lifestyle, occupation and needs.
“Published results and studies have confirmed that spectacle independence is far more possible and likely when implanting a multifocal IOL than just relying on monofocal monovision. A 2017 meta-analysis showed a mean spectacle independence rate of over 80% with multifocal lenses,” he said.
He added that evolving lens technology along with artificial intelligence applications and the ability to assess preoperatively the patient’s objective behavioural data will allow more personalised and precise lens selection in the future.
The importance of rigorous preoperative assessment in implanting multifocal IOLs was also emphasised by Professor Marie-José Tassignon, who used a case study of an unhappy multifocal IOL patient to illustrate some of the key issues that may arise in such cases.
The 52-year-old female patient with an uneventful medical history was hyperopic in both eyes, with a visual acuity of 10/10 in her right eye and 4/10 in the fellow eye with amblyopia. Although she was satisfied with her multifocal implant in the immediate
postoperative period, she started experiencing visual difficulties in her left eye one month to six weeks after her surgery.
The corneal topography showed a regular corneal surface of normal curvature with a small amount of regular astigmatism (0.53D in the right eye and 0.70D in the left eye).
“What was interesting was her axial length: 20.64 mm for the right eye and 20.38 mm for the left eye, which is an outlier. She had a normal retinal correspondence in the right eye, but she had cyclorotation of the macula in the left eye,” said Prof Tassignon, Professor and Head of Ophthalmology Department, University Hospital, Antwerp, Belgium.
Orthoptic examination, which is mandatory in such eyes said Prof Tassignon, showed that she had no strabismus or diplopia, a small hyperphoria and esophoria, poor fusion and poor stereopsis. Examination of the problem eye revealed a decentred lens, an irregular anterior capsulorhexis and fibrotic tissue.
“This proliferative tissue was caused by a reaction of the capsular bag to the presence of the foreign body intraocular lens. I used a bimanual technique to pull off the fibrotic tissue and clean out the capsular bag while supporting the zonules as much as possible. The next step was to restore the anterior capsulorhexis and reposition the IOL. After clean up, I decided to leave the lens as it was now well centred and the Purkinje reflex was okay,” she said.
Several lessons could be drawn from the case, concluded Prof Tassignon.
“Orthoptic examination is mandatory in all cases of refractive outliers whether the patient is hyperopic or a high myope. Fundus examination should also be done carefully including retinal correspondence. Patients with amblyopia and poor fusion are bad indications for multifocal implantation unless they present a certain degree of suppression. Patients with high ametropia are also bad candidates in general for these lenses, but if there is good quality of vision immediately after implantation then later complaints might be related to IOL foreign body reaction,” she said.
If this is the case, peeling of the proliferative tissue might improve patient’s quality of vision and does not require IOL exchange.
Daniel Kritzinger: drkritzinger@visiomed.co.za
Marie-José Tassignon:
Marie-jose.tassignon@uza.be
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 22
Daniel Kritzinger MD
There is no one-size-fits-all solution for presbyopia correction in cataract patients... but they will have the best chance of achieving this result using a multifocal IOL
Daniel Kritzinger MD
FLACS complications
Preoperative brimonidine reduces post-op conjunctival haemorrhage. Cheryl Guttman Krader reports
Asingle drop of brimonidine 0.15% instilled into the eye preoperatively significantly decreased the severity of subconjunctival haemorrhage after femtosecond laser-assisted cataract surgery (FLACS), reported Eric S Tam, MD, at the 2020 ASCRS Virtual Meeting.
“Subconjunctival haemorrhage is a common side-effect following FLACS. Brimonidine is a selective alpha-1 adrenergic agonist that lowers IOP and has a vasoconstrictive effect, and its preoperative use to reduce conjunctival haemorrhage has been studied for various ophthalmic procedures,” said Dr Tam, University of Toronto, Toronto, Canada.
“To our knowledge, this is the first study to evaluate the vasoconstrictive effect of brimonidine or any other agent for FLACS.”
The efficacy of brimonidine to reduce subconjunctival haemorrhage after femtosecond laser suction ring application was investigated in a prospective, masked study. Patients were randomised to receive the usual preoperative eye drops with or without one drop of brimonidine 0.15%. Dr Tam performed all surgeries using the samefemtosecond laser and phacoemulsification platform.
Subconjunctival haemorrhage was evaluated using images obtained
prior to preoperative drop instillation and 15 minutes after surgery using the Oculus Keratograph M5. A Bulbar Redness Score (BRS) and Analyzed Area (AA) were recorded. Patients were excluded if they were on anticoagulation therapy, had prior conjunctival surgery, experienced an intraoperative complication, or if the Analyzed Area was less than 25 mm2 or differed by more than 10% between preop and postop values.
The final analysis included 25 brimonidine-treated eyes and 37 control eyes. Mean BRS and mean AA values did not differ significantly between the two study groups preoperatively or postoperatively. There was also no statistically significant difference between groups in the mean change in AA from pre-op to post-op.
However, compared with the preoperative value, the mean BRS decreased postoperatively in the brimonidine group and increased postoperatively in the control group. The difference between groups for the mean change values was statistically significant (p=0.03).
Dr Tam acknowledged that it had a low sample size. There was also a trend towards a higher preoperative BRS in the study group (p=0.07). He also suggested that use of phenylephrine 10% for pupil dilation preoperatively may have partially masked the effects of brimonidine.
Eric S Tam: es.tam@utoronto.ca
• Reduced Registration Fees for ESCRS Congresses

• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand
Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
EUROTIMES | OCTOBER 2020 SPECIAL FOCUS: CATARACT & REFRACTIVE 23
FREE 5 year membership for trainees Join today. www.escrs.org
ESCRS Membership
Monovision or multifocals?
Patient suitability and tolerance should determine presbyopia correction method. Howard Larkin reports
Rigorously assessing patients’ suitability for specific presbyopia options, and managing expectations, are critical for successfully offering monovision or multifocal intraocular lenses, said Mitchell A Jackson MD at the ASCRS Virtual Annual Meeting 2020.
Communicating effectively with patients starts with using language they can better understand, Dr Jackson said. “Terms like ‘monovision’ or ‘micro-monovision’ seem like you are going to be a cyclops. We prefer terms like ‘blended vision’ and ‘natural vision’ for multifocality. These relate better to the patient’s experience and help set expectations on the limits of their vision.”
BLENDED VISION
In assessing patients for “blended vision”, Dr Jackson first considers occupation. Favourable jobs that require frequent viewing distance changes include teaching, performing arts, public speaking, sales and flight attendant. Unfavourable occupations requiring prolonged distance or near vision or good stereoacuity include commercial driver, surgeon, seamstress and pilot.
Personality is considered, with perseverance a more important trait than motivation, Dr Jackson said (DuToit R et al. Optom Vis Sci. 1998;27:119-125). Introverted men do not adapt well (Erickson DB, Erickson P. Percept Mot Skills. 2000).
Prior wearers of contact lenses adapt most easily, Dr Jackson noted. “Actually, if blended vision is not given these patients will be extremely unhappy because it is what they are used to.”
He typically does a contact lens trial for six weeks or more before surgery. The longer they have done it the more likely they are to tolerate it. Still, patients should be prepared for an adaptation period for night vision. It is worth considering prescribing spectacles for night driving and low-light tasks.
Eye dominance is also important, with
about 75-to-80% preferring the dominant eye for distance – though up to 25% may strongly prefer the dominant eye for near, so it’s important to figure that out, Dr Jackson said. Monovision is most successful in patients with alternating dominance, which allows for better blur suppression.
To determine dominance Dr Jackson typically uses a motor eye technique, sometimes as simple as asking a patient to close one eye and look at his finger across the room.
“They don’t know what you are testing for and usually the unclosed eye is dominant,” he said.
The amount of myopia induced in the near eye depends to an extent on occupation and frequent activities, with -1.00 dioptre affecting stereoacuity very little but giving poor near vision, out to -2.00 dioptres delivering J2 to J1 near, but stereoacuity about half of normal at about 158 arc seconds (Hayashi K et al. J Refract Surg. 2010 Sept 1:1-7.)
Dr Jackson usually targets about -1.5 dioptres for the near eye and plano for the distance eye, which must be perfect. He recommended correcting astigmatism with a monofocal toric lens, and using lenses such as Crystalens, Trulign or Envista to extend the depth of the blended vision zone. Options for correcting distance vision after surgery, such as contact lenses or laser vision correction, should be in place.
NATURAL VISION
While “natural vision” attempts to replicate some of the range of natural youthful vision, it actually imposes a static multifocal solution in place of a dynamic accommodating system, Dr Jackson said.
“There are good, but not perfect, options available – EDOF, trifocals and low-add bifocals. But perfect, not good, candidates are needed,” he added.
Because stable tear film is essential for good multifocal lens performance, a “perfect” candidate starts with pristine ocular surface in terms of osmolarity, MMP-9 presence, low ocular surface disease index and functional meibomian glands.
No macular pathology should be present, Dr Jackson said.
Because multifocal IOLs depend on precise refraction, corneal topography, tomography and epithelial mapping should show the possibility of correcting any residual refractive error with PRK, LASIK or SMILE®, Dr Jackson
added. Corneal astigmatism should be corrected, preferably with a toric IOL if it exceeds 0.77D. Multifocal lenses should not be implanted in patients with an angle alpha or kappa of greater than 0.7 mm, or with corneas with a higher-order aberration RMS greater than 0.38 microns. For optimal predictive precision, Dr Jackson recommended using fourthgeneration IOL formulae, such as the Barrett, Barrett True K, Hill-RBF or Holladay 2.
Selecting a proper refractive target is also critical for success, and this can vary by patient and lens, Dr Jackson said. For example, in a study he conducted with fellows, Dr Jackson determined that optimal vision was achieved in patients receiving bilateral extended depth of focus lenses with the dominant eye targeting emmetropia and the non-dominant eye between -0.21 and -0.63D (Jackson M et al. Clin Ophthalmol 2020;14:455-62). For the trifocal PanOptix lens, he targets plano dominant and one click below plano for the non-dominant eye.
And always, realistic patient expectations should be reinforced in terms of near, intermediate and distance vision, glare and low light performance, and adaptation time, Dr Jackson concluded.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 24
Terms like ‘monovision’ or ‘micro-monovision’ seem like you are going to be a cyclops
Mitchell A Jackson MD
THOMAS KOHNEN European Editor of JCRS


JCRS HIGHLIGHTS
VOL: 46 ISSUE: 8 MONTH: AUGUST 2020
FLACS META-ANALYSIS







Previous studies comparing femtosecond laser-assisted cataract surgery (FLACS) with conventional cataract surgery (CSS) have provided contradictory results. A new comprehensive meta-analysis was conducted to try and provide answers about the relative merits of the two approaches. Researchers included 73 studies (25 randomised controlled, 48 observational), with a total of 12,769 eyes treated with FLACS and 12,274 eyes treated with CCS. The studies involved five different laser platforms. Both procedures were similarly safe and effective with few complications. No significant differences among groups were found in visual acuity at one week and after six months. However, in most of the studies, FLACS provided slightly better visual acuity in the medium-term. FLACS required lower ultrasound energy, which was associated with less injury to corneal tissues. Moreover, FLACS appears beneficial in the short-term for patients with low endothelial cell density and dense cataract. However, questions of cost efficacy remain. CM Kolb et al. “Comparison of femtosecond laser–assisted cataract surgery and conventional cataract surgery: a metaanalysis and systematic review”, Vol 46, #8, p 1075-1085.
REDUCING FLACS INFLAMMATION


A single dose of topical NSAID 30 minutes before FLACS surgery appears sufficient to minimise inflammation in the aqueous humour, a new study suggests. Researchers investigated interleukin (IL)-1β, IL-6 and total prostaglandin (PG) levels in the anterior chamber in 40 patients undergoing immediate sequential cataract surgery. One eye underwent low pulse energy FLACS, with the second eye undergoing conventional phaco surgery. No difference was noted in levels of IL-1β and IL-6 between the groups. There was a small but statistically significant increase of PG levels in the femto group. No statistically significant correlations were noted between levels of 1β, IL-6, or total PG and suction time or lens density. L Schwarzenbacher et al., “Intraindividual comparison of cytokine and prostaglandin levels with and without low-energy, highfrequency femtosecond laser cataract pre-treatment after singledose topical NSAID application”, Vol 46, #8, p 1086-1091.







TORIC IOLS IN CHILDREN
Toric IOL implantation can produce excellent results in paediatric eyes undergoing non-traumatic cataract surgery, a long-term study concludes. The study included 76 eyes of 51 children, with a mean age of 7.41 ± 2.82 years and mean preoperative keratometric astigmatism of 1.56 ± 2.13D. The mean corrected distance visual acuity improved significantly from 0.59 logMAR preoperatively to 0.23 at 36 months. Mean postoperative uncorrected distance visual acuity was 0.32. Mean refractive astigmatism at final follow-up was -0.55 ± 0.40 D, with 74% patients having a UDVA of at least 20/40. Five per cent of eyes needed treatment for visual axis obscuration. None developed glaucoma. No eye required repositioning of the toric IOL until final follow-up. V Vasavada et al., “Visual outcomes after toric intraocular lens implantation in paediatric eyes undergoing cataract surgery”, Vol 46, #8, p 1102-1107.
EUROTIMES | OCTOBER 2020
SPECIAL FOCUS: CATARACT & REFRACTIVE 25 JCRS is the official journal of ESCRS and ASCRS
Update on OCT
The capability of modern optical coherence tomography instruments to accurately distinguish the corneal epithelial layers from the underlying Bowman’s layer and stroma makes them an essential tool in the early diagnosis of keratoconus and also the treatment of the condition, said Mouchine Al Bakkali MD, Clinique de La vision de Rabat, Rabat, Morocco.
“In the past we were told that keratoconus starts in the posterior surface because we didn’t have OCT, but now we know we can detect it earlier on the anterior surface,” Dr Bakkali told the 24th ESCRS Winter Meeting in Marrakech, Morocco.
He noted that before the development of OCT, assessments of the cornea were less reliable, because the tomography technologies relied on the image extrapolation, using mathematical reconstruction that can miss some abnormalities. In addition, the older devices do not allow segmental assessment of the corneal layers and therefore cannot disassociate the epithelium from the stroma. Furthermore, tear film stability and resolution issues can undermine the reliability of the data the instruments provide.
EPITHELIAL MAPPING
OCT has greater sensitivity and specificity because it overcomes the deficiency in segmental analysis with spectral OCT providing a high resolution from 4-to-5 microns for spectral domain and 8-to-9 microns swept source, he said. It therefore can be a reliable tool for the diagnosis and followup of all corneal abnormalities. It also has a range of potential applications in the treatment of corneal disease. For example, surgeons can use OCT intraoperatively for placement of intracorneal rings segments (ICRS), before trans-epi PRK and also before and after corneal graft surgery.
In healthy corneas the corneal layers are aligned in a parallel fashion, but in eyes with keratoconus that alignment is disturbed. The corneal epithelium has a characteristic pattern of growth, wherein the epithelium grows more thickly at the base of the cone and more thinly at its apex in a classic donut image. In this way, the epithelium masks the cone and makes the change in the anterior surface less abrupt.
He added that since adopting epithelial mapping when assessing corneal refractive surgery candidates, he will always rule out LASIK in eyes with epithelial abnormalities despite normal topology and will instead opt for a surface ablation procedure.
“Epithelial mapping in keratoconus could be an accurate device for early diagnosis, and more attention should be paid to the three types of data, namely a thinning variation with a standard deviation greater than six microns, a thinning point localisation outside the 2.0mm optical zone, and the index superior more than 5.0mm,” Dr Bakkali said.
PREOPERATIVE AND INTRAOPERATIVE OCT
Dr Bakkali noted that epithelial mapping is mandatory before epi-off CXL, as it can determine whether the stromal thickness beneath the epithelium is superior to 500 microns and can therefore safely undergo the procedure. Corneal OCT also has a role in the follow up of CXL by providing accurate pachymetry showing the demarcation line as an index of efficient crosslinking.
“Therefore, we can conclude that corneal OCT is essential before any classification we might make for keratoconus, and we should take into account the corneal OCT data of the epithelium, the Bowman’s membrane and the stroma. The Belin ABCD classification of keratoconus should be the ABCD E classification, taking into account the epithelium behaviour,” Dr Bakkali said.
OCT IN THE OPERATING ROOM
OCT can also be very useful in the operating room. It can be used for diagnostic purposes in patients who are not able to be examined in consultation, for example paediatric patients. Intraoperatively it makes transparent structures visible increasing surgical precision and allowing the surgeon to adapt their surgery in real time as unexpected situations arise. In addition, OCT may enable surgeons to perform new types of surgery, including new minimally invasive techniques that were not possible without OCT.
OCT can also play a useful role in the implantation of ICRS by insuring the three principle criteria for their safety and efficacy, namely correct pupil centration with regard to angle kappa, insertion at 80% of stromal depth and a healthy endothelium covering the ring to prevent extrusion.
Similarly, in eyes undergoing transepithelial PRK, OCT allows accurate measurement of epithelial thickness. Even in healthy eyes the epithelium thickness can range 48-to-57 microns. Relying on the supposed epithelial thickness provided by the literature increases the risk of over- or under-correction.
He added that in corneal graft surgery, swept-source OCT devices combined with a surgical microscope enhances the corneal surgeon’s ability to perform some of the more technically difficult but less invasive keratoplasty techniques such as deep anterior lamellar keratoplasty (DALK) l and Descemet’s membrane endothelial keratoplasty (DMEK).
“My take-home message is that we should keep in mind the cornea’s structure and function and by combining corneal tomography, topography, OCT and biomechanics, the question is are we able to identify all the risky corneas or not quite yet,” Dr Bakkali concluded.
Epithelial mapping with OCT a valuable tool in diagnosing early keratoconus. Roibeard Ó hÉineacháin reports
CORNEA 26 EUROTIMES | OCTOBER 2020
Epithelial mapping in keratoconus could be an accurate device for early diagnosis
Mouchine Al Bakkali MD
We should take into account the corneal OCT data of the epithelium, the Bowman’s membrane and the stroma
Mouchine Al Bakkali MD
47,863 * * Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk Reach at a Glance The number of countries in which EuroTimes is distributed 169
European Union Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
Ocular effects of eczema drug
Dupilimab-induced conjunctivitis can require long-term steroid therapy.
Roibeard Ó hÉineacháin reports
Around a third of patients receiving the monoclonal antibody dupilumab (Dupixent®, Regeneron) for eczema may develop conjunctivitis, and most of those will require the use of topical steroids long-term, said Magdalena Popiela MD at the 24th ESCRS Winter Meeting in Marrakech, Morocco.
Dr Popiela, Gibraltar Health Authority, Gibraltar, presented a review of the course of therapy and results in a series of nine patients who developed dupilumabassociated conjunctivitis between January 2017 and August 2019. She noted that the patients represented 32% of those receiving the biologic agent at the Southampton University Hospital, Southampton, UK, where she was based at the time of the study. The study was a collaboration between the ophthalmic team, led by Professor Hossain, and the dermatology department under the care of Prof Arden-Jones.
The patients developed conjunctivitis within six weeks of starting treatment with dupilumab. Forty-four per cent had previous allergic eye disease, which was quiescent when treatment started. Their mean age was 39.5 years and there was no statistically demographic difference between those at the Southampton centre who did develop conjunctivitis and those who did not.
the ECCTR Registry
Join Track
your Surgical Results
www.ecctr.org
ECCTR is a project funded by the ESCRS with initial support from the EU
As a first-line treatment, all received topical steroids and lubricant eye drops, which resulted in significant improvement in their condition. However, one patient required additional topical ciclosporin. She noted that at a mean follow-up of 16 months, seven of the nine patients remained on low-dose weak topical steroids due to relapse of symptoms upon discontinuation of the drops. Of the remaining two patients, one remained on lubricants and another is using lubricants and olopatadine (Opatanol). One patient had severe conjunctivitis causing the loss of eyelashes and necessitating the discontinuation of dupilumab. No patients lost any vision.
Dr Popiela noted that dupilumab is the first biologic agent to be approved by the FDA for use in atopic eczema. It also has been used in asthma and nasal polyposis but interestingly, dupilumab-associated conjunctivitis mainly affects patients with atopic eczema. The drug targets the interleukin (IL)-4 receptor alpha and thereby inhibits IL-4/ IL-13 signalling. In initial trials with the drug, up to 28% of patients developed conjunctivitis, which was generally mild and only occasionally necessitated discontinuation of therapy. Predisposing factors to the adverse event include prior allergic eye disease and more severe atopic eczema.
The aetiology for dupilumab-associated conjunctivitis is not fully understood. The drug may sensitise susceptible patients to develop chronic ocular inflammation after the acute episode of conjunctivitis. There appear to be two principal types of dupilumab-associated conjunctivitis, namely, the papillary type and the follicular type, both requiring topical steroids in Southampton series. Conjunctivitis can result in conjunctival cicatrisation and also may be associated with periocular skin changes. Acute presentation responds to topical steroids, ciclosporin can be used as second-line therapy, Dr Popiela explained.
EUROTIMES | OCTOBER 2020 CORNEA 28
Postitive outcomes in DMEK study
Afive-year follow-up study of 500 patients who underwent Descemet membrane endothelial keratoplasty (DMEK) resulted in high graft survival rates, excellent visual outcomes and acceptable corneal endothelial cell loss comparable to other keratoplasty techniques.
Jorge Peraza-Nieves MD, Netherlands Institute for Innovative Ocular Surgery (NIIOS), Rotterdam, The Netherlands, presented the study at the 24th ESCRS Winter Meeting in Marrakech, Morocco. The study involved a consecutive series of 500 eyes of 393 patients who underwent DMEK for Fuchs’ endothelial corneal dystrophy (FECD), bullous keratopathy, failed corneal transplants and other endothelial indications. The series excluded the first ever 25 DMEK cases to take into account the learning curve of the DMEK technique itself.
The patients in the study had a mean age of 68 years, 56% were female and 44% were male and 75% of patients were pseudophakic. The main indication for DMEK was FECD (89%). All underwent evaluation of best-corrected visual acuity (BCVA), central endothelial cell density (ECD) and central corneal thickness before, and up to five years after DMEK, Dr Peraza-Nieves said.
GOOD GRAFT SURVIVAL AND BCVA
At a follow-up of five years, cumulative survival probability was 90%, with higher rates for eyes operated on for FECD (93%) than for other indications (72%). In addition, the mean logMAR BCVA improved from 0.49 preoperatively to 0.06 at one year postoperatively and remained stable at 0.05 at two and five years postoperatively. In addition, at five years postoperatively, BCVA was 20/25 or better in 82% of eyes, 20/20 or better in 54% eyes and 20/18 or better in 15% of eyes.
Regarding endothelial cell density, there was initially a steep decline followed by a stable annual decrease similar to that seen after DSAEK. The mean ECD decreased by 37% at six months, by 40% at one year and by 55% at five years postoperatively, Dr Peraza-Nieves said.
The main postoperative complication was partial graft detachment, which occurred in 15.8% in the early postoperative period, 9% were detachments of one-third or less of the graft surface and 6.8% were larger detachments. The principal longer-term complications are secondary graft failure in 2.8%, 0.6% occurring within the first year and 2.2% after the first year and allograft rejection in 2.8%, 0.8% occurring within the first year and 2.0% after the first year. In total, re-transplantation was required for 8.8% of the eyes within the study period. An overview of all results of the study by Birbal et al. can be found here: http://bit.ly/ET-DMEK-outcomes
Jorge Peraza-Nieves: peraza@clinic.cat
Continue your education all year with our range of online resources Visit education.escrs.org Ready when you are. • ESCRS Research Portals (Find details of ESCRSSponsored research) • Astigmatism Double Angle Plot Tool (JCRS) • JCRS Online Case Reports • Landmark Articles • ESCRS Eurotimes Podcasts • ESCRS Player Videos
ESCRS On Demand
ESCRS iLearn
EBO-ESCRS Exam and more...
•
•
•
DMEK shows good graft survival and visual outcomes at five years.
Roibeard Ó hÉineacháin reports
EUROTIMES | OCTOBER 2020 CORNEA 29
The patients in the study had a mean age of 68 years, 56% were female and 44% were male...
Jorge Peraza-Nieves MD
Using AI to predict AMD progression
AI system detects imminent conversion to exudative AMD in fellow eyes. Roibeard Ó hÉineacháin reports
Anew artificial intelligence system can predict with a high degree of accuracy the likelihood of conversion of the fellow eye in patients with unilateral exudative age-related macular degeneration (exAMD), a new study published in the journal Nature Medicine suggests.
The AI system consists of two complementary components: first predicting conversion to exAMD based on an interpretable tissue segmentation of the OCT and, second, making a prediction based on the raw OCT itself. The former adapts a two-stage architecture trained on a subset of manually segmented scans. This first segments 13 relevant tissue types and subsequently applies a classification network adapted to predict the risk of conversion to exAMD within the next six months.
The system also interprets the raw OCT Data using a twostage network with a model trained for the same task to take into account imaging features that occur in the conversion to exAWMD that are not yet captured by the segmentation model, such as reticular pseudodrusen and reflectivity of tissues.
The study’s authors trained and tested the system using a retrospective, consecutive cohort of 2,795 patients across seven different sites who were first diagnosed with exAMD between June 2012 and June 2017, achieving a per-volumetricscan sensitivity of 80% at 55% specificity, and 34% sensitivity at 90% specificity within a clinically actionable six-month time window. This level of performance corresponds to true positives in 78% and 41% of individual eyes, and false positives in 56% and 17% of individual eyes.
To compare the accuracy of the testing to human performance, three retinal specialists and three optometrists trained in medical retina were asked to predict the likelihood of fellow eye conversion to exAMD using individual and sequential scans from a randomised subset of patients. They found that system performed better than five experts (all three retinal specialists, two optometrists) and matched one (an optometrist) for the single scan task.
Furthermore, even when the experts additionally had access to each patient’s previous OCT scans, fundus images and additional clinical information, the AI system still outperformed two retinal specialists and all three optometrists an about the same as retinal specialist.
“This AI system overcomes substantial interobserver variability in expert predictions, performing better than five out of six experts, and demonstrates the potential of using AI to predict disease progression,” the authors concluded.
Speaking to EuroTimes, Pearse Keane MD said: “In this paper, we use artificial intelligence (AI) to create an early warning system for ‘wet’ AMD in the ‘good’ eye of patients. In a subset of these patients, our system can predict the imminent development of wet AMD with high specificity (i.e., within a six-month time period). As a next step, we are planning how this can be used in AI-enabled clinical trials of preventative therapies.
“By treating eyes at high risk early, such trials may lead to better outcomes for patients, or even prevent development of wet AMD in the first place,” he added.
The full article, “Predicting conversion to wet age-related macular degeneration using deep learning”, J Yim et al., Nat Med (2020), is available at https://www.nature.com/articles/ s41591-020-0867-7.
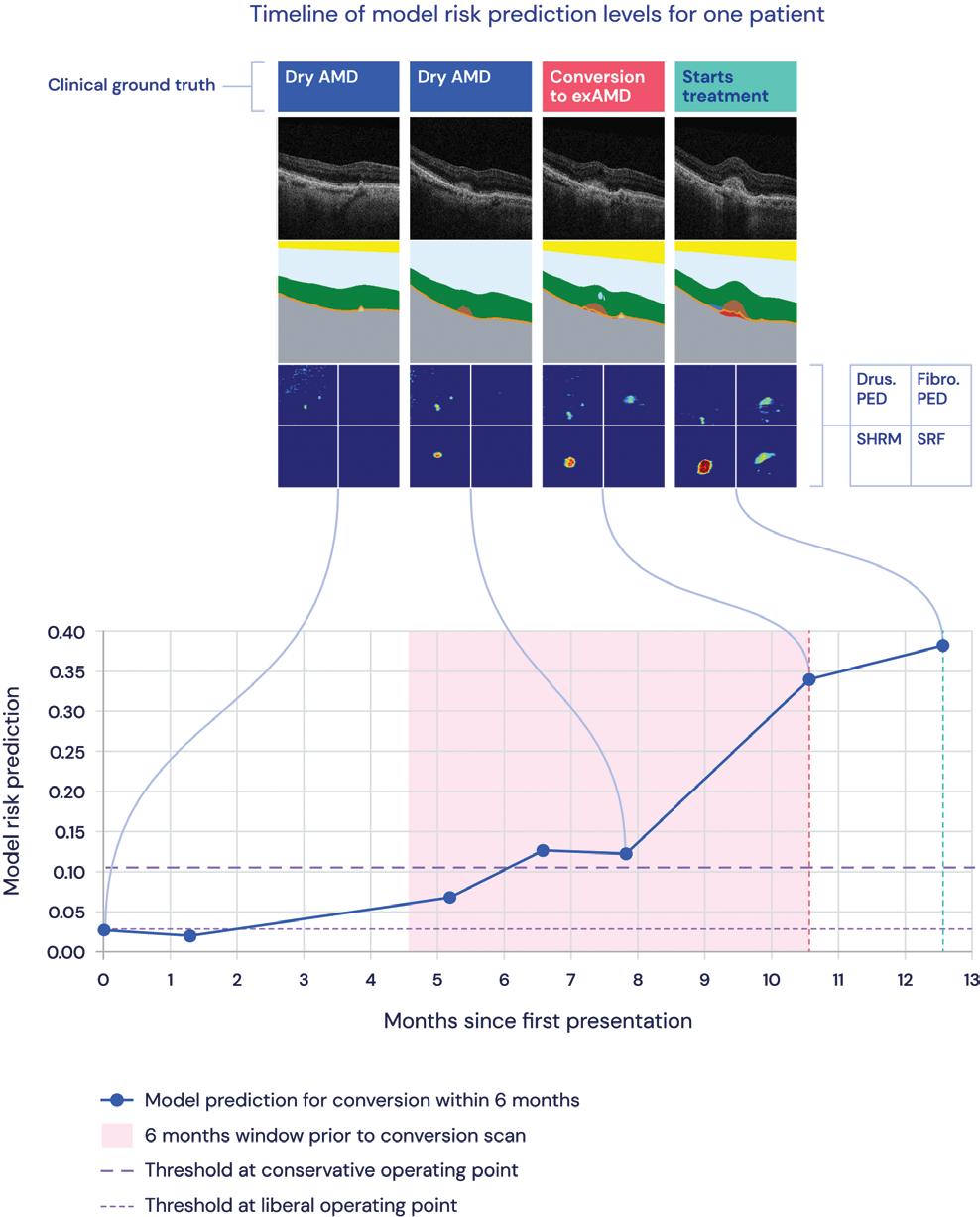
EUROTIMES | OCTOBER 2020 RETINA 30
By treating eyes at high risk early, such trials may lead to better outcomes for patients, or even prevent development of wet AMD in the first place
Pearse
Keane MD
Example scans from a patient over 13 months of regular monitoring, showing raw OCT scans, the anatomical segmentations output by the AI system and a top-down view of the segmentations
Courtesy
of DeepMind
Imaging technique shows potential

An emerging imaging modality to measure autofluorescence of the human fundus in vivo has the potential to improve the diagnosis, treatment and follow-up of retinal diseases such as age-related macular degeneration and macular telangiectasia type 2 (MacTel), according to Lydia Sauer MD.
Fluorescence lifetime imaging ophthalmoscopy, or FLIO, is a non-invasive imaging technique capable of capturing highly reproducible measurements in the retina and revealing valuable information on a range of retinal diseases, Dr Sauer said.
“FLIO provides unique high-contrast images on information on retinal fluorophores and their environment. We get very high-contrast images in about two minutes per eye that help us to identify diseasespecific patterns and information on the metabolic signature in the eye. Our studies on MacTel have also demonstrated its potential utility in establishing earlier diagnosis for patients that would not have been identified using standard imaging techniques,” she said.
Dr Sauer explained that FLIO works via a prototype device based on a Spectralis HRA system (Heidelberg Engineering), which uses a picosecond-pulsed diode laser at 473nm wavelength and 80MHz repetition rate to excite the retinal fluorophores. Fluorescence decay times are then measured in both a short (498-560nm) and long (560-720nm) spectral channel by time-correlated single photon counting.
A laser is used to excite the retinal fluorophore, which then releases photons to revert back to the ground state. This time can be calculated and assessed, as fluorescence lifetimes are specific for individual fluorophores and depend on the metabolic environment.
Applying the technology to a rare inherited disease such as MacTel yielded some interesting results, said Dr Sauer.
“The onset of MacTel is usually between 40 and 60 years but by investigating these patients in more detail with FLIO we found individuals as young as 21 years of age who were affected. So, it is not just a disease of older patients and we also think it is a lot more common than initially believed,” she said.
Looking at the family members of MacTel patients also provided some useful insights into the disease, said Dr Sauer.
One case in point was the aforementioned 21-year-old patient whose two sisters, aged 26 and 28, and father were also examined using FLIO.
“The father also has MacTel and when he came to the clinic we saw that he had no arms of his sisters also had the mutation and the other sister did not. Both of the sisters had completely normal fundus exams but early changes were clearly visible in the FLIO scans of the affected sister, so we could actually plan a treatment strategy for her.
“It is exciting to see that we can use this technology to potential diagnose and intervene earlier in the disease course,” she said.
Keep learning. Whenever, wherever. Learn more at https://elearning.escrs.org Trainers: use the task list to assign courses for trainees and monitor their progress. Learn online in your own time, with self-paced and assessed ESCRS iLearn courses on: ∙ Cataract Surgery ∙ Cornea ∙ Refractive Surgery
Visual Optics EUROTIMES | OCTOBER 2020 RETINA 31
∙
FLIO sheds light on the development of retinal diseases.
Dermot McGrath reports
Innovative vitreous substitute study
Artificial vitreous substitute shows promise in early trials. Dermot McGrath reports
Amanufactured hydrogel-based artificial vitreous has shown highly favourable biophysical characteristics in ex vivo models, strongly suggesting its further application as a potential vitreous substitute in vivo, according to a study.
“It is still early days and we need larger controlled clinical trials to fully test this hydrogel, but we are very excited by the possibilities of having a viable, safe and effective alternative to current tamponade methods, which have a lot of limitations,” said Kai Januschowski MD, FEBO.

A wide variety of artificial vitreous substitutes have been investigated over the years to repair retinal tear and detachment and for other vitreoretinal conditions, with mixed results, noted Prof Januschowski, Eye Clinic Sulzbach, Germany.
The most commonly used vitreous substitutes designed to
produce an effective tamponade for detached retinas include expansile gases, perfluorocarbon liquids (PFCLs) and silicone oil. These can be used only as temporary substitutes, however, and they come with significant drawbacks, said Prof Januschowski.
“Whether we are putting gas or silicone oil into the eye there are limitations to hydrophobic tamponades that we need to be aware of. Only one tamponade vector is possible with these agents, so a complete tamponade is physically impossible, while retracting the gas bubble has unfavourable fluid dynamics,” he said.
INITIAL TESTS
Furthermore, PFCLs tend to be routinely used only intraoperatively for complicated retinal detachments because of their toxicity over longer periods of time.
To overcome these obstacles, a team around Prof Januschowski came up with a biocompatible, cross-linked, hyaluronic acid (HA)-based hydrogel.
The generated hydrogel was successfully tested as a vitreous substitute in two distinct ex vivo eye animal models in order to investigate short-term biocompatibility and IOP development.
MICRO SERRATIONS ON THE BROAD PLATFORMS
–360° HANDLE ACTUATION

–INNOVATIVE « 3D » ANTI-SHREDDING TIPS WITH EXTRA GRASPING POWER
–LONGER SHAFTS FOR MYOPIC EYES

LONGER SHAFTS FOR MYOPIC EYES
JOIN OUR OPHTHALMIC COMMUNITY!
The initial tests in the first human patients have also proved promising, said Prof Januschowski, although the experimental nature of the hydrogel means that its application has been limited to extreme rescue situations.
“The first patient that we tested this on had a severely damaged eye after multiple operations and was close to being enucleated. We performed a penetrating keratoplasty and the hydrogel stayed beautifully inside the eye. That was almost two years ago and I saw the patient recently and he was very happy,” he said.
The artificial vitreous has been successfully deployed now in nine patients: five with multiple retinal detachments, two ocular trauma cases, one case of ischaemia and another of chronic uveitis following severe hypotony.

“We are talking about very difficult situations – this is really a last option that we can offer these patients before enucleation. We managed to control the IOP and relieve the pain that these patients were experiencing. The next steps will be to try to test this in eyes where there is still some prospect of obtaining good visual acuity. However, we need to very selective because we have to be very careful about potential adverse events,” he concluded.
Kai Januschowski: Kai.januschowski@med.uni-tuebingen.de
EUROTIMES | OCTOBER 2020
RETINA 32 TRY OUT OUR LATEST SUPER GRIP FORCEPS FOR FIBROUS MEMBRANES PEELING!
fciworldwide.com
NEW FCI - Presse EUROTIMES 84x130 - Super Grip Forceps.indd 1 08/09/2020 11:48
Kai Januschowski MD, FEBO
Stem cells for Stargardt’s
Injecting stem cell-derived retinal pigment epithelium (hESC-RPE) in Stargardt’s disease has been shown to be both safe and feasible in initial phase I/II trials of the technique, according to Rodrigo Brant MD, PhD.
“The surgical procedure for subretinal implantation of hESC-RPE proved feasible and safe, without cell migration, signs of rejection or inflammation or development of ocular or systemic tumours. All patients improved their visual acuity over baseline and the gains have been maintained for up to four years in some patients. We have now treated 12 patients with this approach and the results are very promising,” he said at the World Ophthalmology Congress 2020 Virtual.
Autosomal recessive Stargardt’s macular dystrophy is the most common form of inherited macular degeneration, affecting roughly in 1-in-10,000 people. There is currently no cure for the condition, in which patients develop irreversible vision loss due to atrophy of the macular RPE and loss of photoreceptors.
Dr Brant’s initial study at the Federal University of Sao Paulo, Brazil, included six patients with Stargardt’s disease who received a hESC-RPE solution (2 million cells/0.1ml) implanted into the subretinal space. All patients received oral prednisolone and cyclosporine for the first three months postoperatively.
Surgery to inject the cells was uneventful, said Dr Brant.
“We performed a routine pars plana vitrectomy followed by the creation of a subretinal bleb with balanced salt solution. After creating the bleb, we then inject the suspended cell solution through another incision in the subretinal space. After that, we perform air-fluid exchange and the surgery is complete,” he said.
In terms of results, the best-corrected visual acuity (BCVA), visual fields and electrophysiological tests showed improvement in all six patients. No adverse effects or complications related to the surgery occurred during the oneyear follow up, said Dr Brant.
Discussing the mechanism of action of the treatment, Dr Brant said that the gains seem to be coming from the zones adjacent to the area of central atrophy where some photoreceptor function is still present.
“We never saw any improvement in any of the patients in the central area of atrophy where the RPE is entirely gone. However, in areas where the photoreceptors are suffering, the injection of cells perhaps improves that environment sufficiently for them to return to their previous function and they start to give some light perception.
“There is therefore maybe a rationale to employ this type of treatment earlier in the disease course to avoid progressing to advanced degeneration,” he concluded.
Rodrigo Brant: rodrigo.brant@ ophthal.com.br
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
Convenient Web-Based Registry
Cataract, Refractive and Patient Reported Outcomes in One Platform
Join Track the EUREQUO Platform your Surgical Results EUREQUO is free of charge for all ESCRS members www.eurequo.org
Early trials show promise and improved visual acuity.
Dermot McGrath reports
EUROTIMES | OCTOBER 2020 RETINA 33
After creating the bleb, we then inject the suspended cell solution through another incision in the subretinal space
Rodrigo Brant MD, PhD
Red light revolution
Brief daily exposure to deep red light could improve declining vision in older adults. Priscilla Lynch reports
Could simply staring at a deep red light regularly help slow or reverse age-related visual decline?
Yes, according to a firstin-human study recently published in the Journals of Gerontology, which showed that daily three-minute exposure to a specific light wavelength for two weeks significantly improved retinal function in those aged over 40 years of age.
Speaking to EuroTimes, lead study author Prof Glen Jeffery PhD, University College London Institute of Ophthalmology, explained that the retina consumes more energy than any other part of the body; mitochondrial density is greatest in photoreceptors, particularly cones that have high energy demands and mediate colour vision.
Thus the retina ages faster than other organs and at around 40 years-old retinal ageing accelerates, leading to a significant decline in photoreceptor function and consequently vision deterioration.
Mitochondria have specific lightabsorbance characteristics influencing their performance. Longer wavelengths spanning 650->1,000 nanometres (nm) have been found to improve mitochondrial complex activity, membrane potential and energy production in the form of ATP.
So exposing eyes to a red-light source of a long wavelength, which is absorbed by mitochondria in the retina, could therefore rejuvenate photoreceptor function and improve declining vision, explained Prof Jeffery.
This hypothesis was tested successfully by his team in a number of animal model studies (in aged flies, bumblebees and mice), which recorded significant improvements in retinal photoreceptor function when the animal eyes were regularly exposed to 670nm (long wavelength) deep red light over relatively short time periods.
For this human study, 24 people (12 male, 12 female), aged between 28 and 72 years, who had no ocular disease, were recruited. All participants’ eyes were tested for the sensitivity of their rods and cones at the start of the study. Rod sensitivity was measured in dark-adapted eyes (with pupils dilated) by asking participants to detect dim light signals in the dark, and cone function was tested by subjects identifying coloured letters that had very low contrast and appeared increasingly blurred.
All participants were given a small LED torch to take home to look into its deep red 670nm light-beam for three minutes a day for two weeks. They were then re-tested for their rod and cone sensitivity.
The 670nm light had no impact in younger individuals, but in those around 40 years and over, significant improvements were obtained.
In the tritan axis, baseline cone colour contrast sensitivity increased significantly in those about 40 years or older compared to younger subjects by maximum of around 20%.
Improvements were more significant in the blue part of the colour spectrum that is more vulnerable in ageing.
Rod sensitivity also improved significantly in those aged around 40 and over, though less than colour contrast.
“We’ve basically shown that deep red-light wavelengths can recharge the energy system that has declined in the retina cells, rather like re-charging a battery,” Prof Jeffery told EuroTimes
He now plans further larger scale, longer studies, as well as working on bringing a financially accessible, evidenced-based version of this simple light technology to market.
“We had some people’s retinal function improve by 20%, others by about 5% and we’d love to know why. While the improvement was not immediately obvious, two people in this study, who were unaware of what we were testing for, mentioned that colours seemed clearer so that was interesting.
“We also know now since we completed this study that we can get this to work with perhaps a couple of exposures a week, and the effect will last for about three to four days so there are plenty more avenues of research to explore.”
RETINAL DISEASE USES?
Would the technology have any potential in the treatment of retinal diseases like agerelated macular degeneration (AMD)? “We tried it in AMD and it didn’t work. But we looked at why that was, and now have a clear idea of the reasons. Firstly, it was because we only ran it for a year and AMD is a really slow disease; whereas the control group did really well,” Prof Jeffery noted. Moreover, the tested AMD patients had advanced disease, a number of whom had begun to develop geographic atrophy. “So we need to start earlier with such patients, and in those with more advanced disease we need to assess them over a longer period of time because our prediction is that if we measure the spread of geographic atrophy it will be slower [in those using the light technology], but that will require significant funding.”
For now, Prof Jeffery is excited about the broad potential of this safe, cheap light technology to potentially slow and partially reverse age-related visual loss in the global population.
“The key issue for me is that everybody gets old. Not everybody gets an eye disease.”
Glen Jeffery: g.jeffery@ucl.ac.uk
EUROTIMES | OCTOBER 2020 RETINA 34
We’ve basically shown that deep red-light wavelengths can recharge the energy system that has declined in the retina cells, rather like re-charging a battery
Prof Glen Jeffery PhD
We had some people’s retinal function improve by 20%, others by about 5% and we’d love to know why
Prof Glen Jeffery PhD
New anti-VEGF effective for AMD
The new vascular endothelial growth factor (VEGF) inhibitor abicipar (Allergan plc, / Molecular AG) appears to be as effective when administered on a quarterly basis as ranibizumab is when administered on a monthly basis in eyes with neovascular age-related macular degeneration (AMD), according the pooled results of CEDAR and SEQUOIA randomised, double-masked, active-controlled, phase III clinical trials recently published in the journal Ophthalmology
The two multi-centre studies had identical protocols and involved a total of 1,888 patients with treatment-naïve active choroidal neovascularisation secondary to AMD. They were randomised on a 1:1:1 basis to receive treatment with three different anti-VEGF regimens: abicipar 2.0mg every eight weeks after three initial doses at baseline and weeks four and eight (Q8); abicipar 2.0mg every 12 weeks after three initial doses at baseline and weeks four and 12; or ranibizumab 0.5mg every four weeks.
Overall, 1,620 (85.8%) patients completed the first 52 weeks of the study. The mean best-corrected visual acuity (BCVA) improved in all treatment groups, with the improvement after the initial doses maintained through week 52. At week 52, there was a mean gain in BCVA from baseline of 7.5 letters in patients receiving abicipar every eight weeks, 6.4 letters in those receiving it once every 12 weeks and 8.4 letters in the ranibizumab group.
In addition, the mean central retinal thickness deceased by 144µm and 145µm in the eight- and 12-week abicipar groups, respectively, and by 144µm in the ranibizumab group. Optical coherence tomography showed that abicipar-treated eyes had a more rapid and more complete resolution of intraretinal and subretinal fluid than ranibizumab during the initial dose phase of the study.
However, the incidence of inflammatory intraocular adverse events was 15.4% and 15.3%, among patients receiving abicipar once every eight weeks and once every 12 weeks, respectively, compared to only 0.3% of patients receiving ranibizumab. Most inflammatory intraocular adverse events were mild or moderate in severity and responded to topical corticosteroids, but 32% of patients with the complication required oral and/or injectable corticosteroids.
The study’s authors note that inflammation in the abicipar group may have been the result of impurities remaining from the bio-engineered E. coli cells used to generate the abicipar molecules. Molecular Partners AG has since adopted additional purification measures which may eliminate the problem.
Abicipar pegol is the first designed ankyrin repeat protein (DARPin) to enter therapeutic use. It is genetically engineered antibody-mimetic protein that binds all isoforms of VEGF-A with high affinity and specificity.
https://doi.org/10.1016/j.ophtha.2020.03.035

everywhere. See everything Catch up on what you’ve missed
ESCRS
up on
the
at
Be
www.escrsondemand.org With
On Demand, members can view the presentations from any conference. Catch
all
sessions
a time and place that suits you.
New VEGF-inhibitor shows long duration efficacy with fewer injections. Roibeard Ó hÉineacháin reports
EUROTIMES | OCTOBER 2020 RETINA 35
The two multicentre studies had identical protocols and involved a total of 1,888 patients...
Treatment options
Space for cyclodestructive procedures in the middle ground of glaucoma management. Dermot McGrath reports
Although traditionally considered as a last-resort treatment option for refractory glaucoma in poorly sighted eyes, cyclodestructive procedures (CPC) are enjoying a renewed lease of life thanks to novel technologies such as endoscopic cyclophotocoagulation and micropulse transscleral cyclophotocoagulation, according to Prof Clement C Tham.
“I think there is definitely a role for these treatment options as part of what I call the ‘middle ground’ for glaucoma management in terms of invasiveness and IOP lowering capability,” Prof Tham said at the World Ophthalmology Congress 2020 Virtual.
In the treatment spectrum described by Prof Tham, IOPlowering drugs have the lowest risk, are least invasive and have low-to-moderate IOP-lowering properties, while at the other end of the scale trabeculectomy and glaucoma drainage device implantation carries a relatively higher risk, is more invasive but has a substantial IOP lowering capability.
Prof Tham, Chairman of Ophthalmology and Visual Sciences at The Chinese University of Hong Kong (CUHK), said that CPC belonged somewhere alongside classic minimally-invasive glaucoma surgery (MIGS) in the middle ground of this spectrum.
He said that moderately advanced glaucoma patients could potentially benefit from modern CPC techniques.
“For early to moderate glaucoma, it may be patients who cannot accept topical drugs or have poor drug compliance, those not adequately controlled by maximally-tolerable glaucoma drugs or laser trabeculoplasty, or patients who do not need substantial IOP reduction for sight preservation. For more advanced glaucoma, it may include patients with only one eye or high surgical risks who prefer intervention with lower surgical risk or patients who prefer a more rapid recovery and rehabilitation,” he said.
Today’s cyclodestructive procedures are usually performed by laser, explained Prof Tham.
“This technique of cyclophotocoagulation can be either transscleral (TSCPC) performed by diode or micropulse laser, or (ECP) endoscopic laser. The traditional method was cyclocryotherapy which was reserved for refractory glaucoma with poor visual potential because of significant complications associated with its use,” he said.
Prof Tham showed a video of micropulse cyclophotocoagulation which is regularly performed at his hospital.
“It works well. The laser probe glides over the area over the ciliary body in a continuous fashion to reduce aqueous production by coagulating the ciliary epithelium,” he said.
In terms of results, Dr Tham said that the scientific literature showed about an average 30% reduction in IOP using this technique.
“It is important to remember that even though the pressure reduction is not dramatic the procedure is safe and noninvasive, and it can be repeated in future if necessary,” he said.
Another option is endoscopic cyclophotocoagulation (ECP), which may be a good option in the presence of cataract, said Prof Tham.
“This technique requires access to the anterior chamber so usually a small corneal wound is required. However, when combined with phacoemulsification no additional incisions are required and it is a safe and effective way to address moderately controlled glaucoma and cataract in one procedure,” he said.
To assess the clinical benefit of ECP performed in conjunction with phacoemulsification, Prof Tham and co-workers recently carried out a randomised controlled trial. Of 48 eyes with primary
open-angle glaucoma, 21 underwent phacoemulsification alone and 27 received combined phacoemulsification and ECP.
“With phaco alone, the IOP reduction was 19.8% compared to 28.5% for combined phaco and ECP. The mean reduction in glaucoma drug use after surgery was 0.9 drugs (29%) for the phaco eyes and 1.6 drugs (48.5%) for the combined group, so there is a clear benefit in adding ECP to the mix when treating cataract at the same time,” he said.
As its name implies, the advantages of minimally invasive glaucoma surgery (MIGS) include the fact that it is less disruptive to the ocular anatomy than traditional glaucoma surgery, has a better safety profile and offers a faster procedure and faster recovery. Some MIGS devices may also be combined with phacoemulsification without the need for additional wounds, noted Prof Tham.
“There are some downsides to MIGS, however. It is still more invasive compared to transscleral forms of CPC and offers less IOP-lowering capability than traditional glaucoma surgeries. The cost of some of the devices may also be a prohibitive factor for some surgeons and patients,” he added.
Prof Tham predicted that sustained-release glaucoma drug implants such as iDose Travoprost (Glaukos) and Bimatoprost SR (Allergan) will soon join the middle ground of glaucoma treatments and help to address problems of adherence and correct administration.
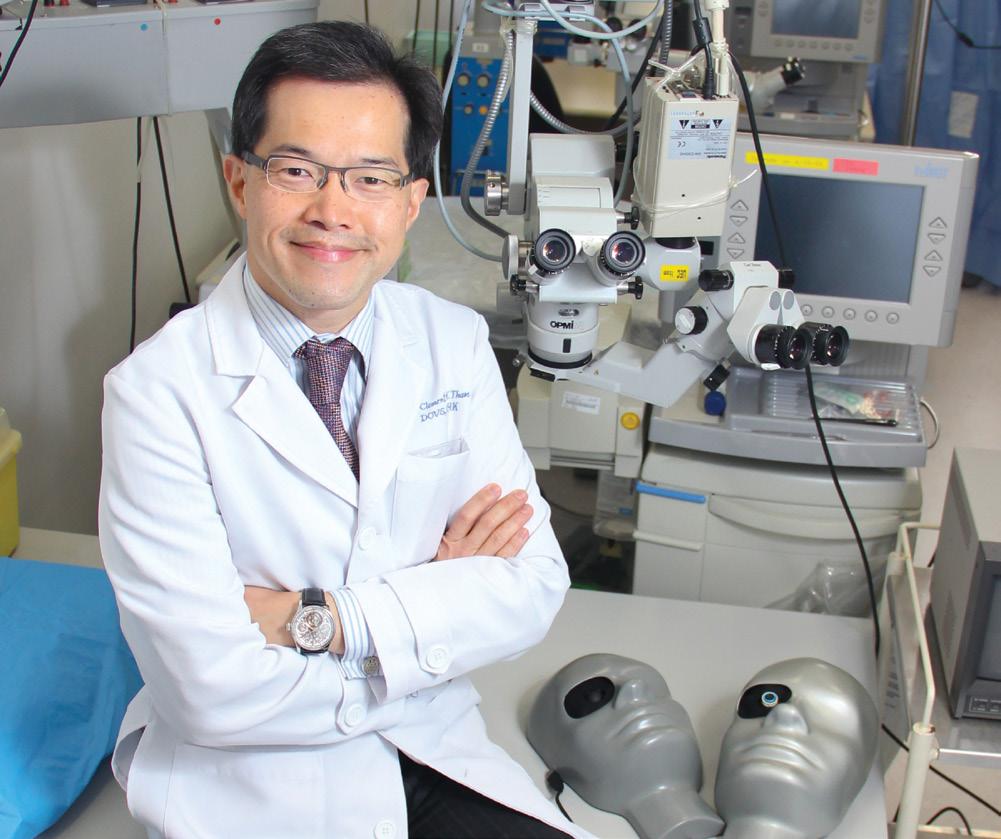
Summing up, Dr Tham said that selecting the right treatment option will depend on a range of factors that need to be carefully weighed in each individual case.
“We need to ask how much IOP and/or drug reduction is needed. How much surgical risk can the patient accept, or the eye tolerate? The age of the patient is important, too, since more elderly patients may need less aggressive IOP lowering. Do they have visual significant cataract as this can change the strategy? What about the angle anatomy because some MIGS cannot be implanted in eyes with angle closure? And finally, the cost factor needs to be taken into account as well,” he concluded.
Clement C Tham: clemtham@cuhk.edu.hk
EUROTIMES | OCTOBER 2020 GLAUCOMA 36
Prof. Clement C Tham
Predicting myopia progression
Arecent survey of paediatric ophthalmologists worldwide found that the rate of myopia progression was the most common indication for initiating treatment to reduce future progression.
According to new findings from the Singapore Cohort Study of the Risk Factors for Myopia (SCORM), however, annual myopia progression as a standalone factor cannot fully predict subsequent year or long-term myopia progression. The SCORM investigators emphasised the need for patient compliance with annual visits and recommended that a personalised management strategy for reducing myopia progression should be based on multiple patientspecific factors.
The research was presented by Noel A Brennan, PhD, Global Lead of Myopia Control, Johnson & Johnson Vision Care, Inc, at ARVO 2020. SCORM is a joint collaboration between the Singapore Eye Research Institute and Johnson & Johnson Vision Care.
“A number of studies have examined potential risk factors for faster progression of myopia, but to our knowledge no predictive paradigm exists. Yet, it appears from the survey of paediatric ophthalmologists that there is a perception among clinicians that a faster progression rate is the preferred method in choosing who to treat. We recommend that the decision should take into account myopia progression in the previous year along with initial refractive error, age of myopia onset, and parental myopia,” said Dr Brennan.
The analyses investigating predictors of myopia progression included data from 674 children (mean baseline age 8 years) who had ≥0.5D of myopia at baseline and completed at least two annual follow-up visits. The results showed that myopia progression in Year 1 correlated with progression in Year 2. However, the correlation coefficient (r) was only 0.47, and Year 1 myopia progression only accounted for about 20% of the variance in progression during the next year, Dr Brennan said.
“According to a multivariable model, using Year 1 annual myopia progression would fail to detect one in four fast progressors in Year 2 and misclassify one in three children as fast progressors.”
The study also showed that Year 1 myopia progression correlated significantly with Year 3 myopia progression, but the correlation was even weaker (r=0.30). There was no significant correlation between Year 1 myopia progression and Year 4 myopia progression.
Noel A Brennan: NBrenna2@its.jnj.com
JOHN
THANK YOU To everyone who entered this year’s essay competition for young ophthalmologists. Details of the John Henahan Prize 2021 competition will be available soon on www.escrs.org
HENAHAN PRIZE 2020
New data highlight fast progressors best identified using multiple factors. Cheryl Guttman Krader reports
EUROTIMES | OCTOBER 2020 37 PAEDIATRIC OPHTHALMOLOGY
...there is a perception among clinicians that a faster progression rate is the preferred method in choosing who to treat
Noel A Brennan, PhD
Low-dose Avastin for ROP
Smaller dosages of bevacizumab as effective in ROP treatment.
Roibeard Ó hÉineacháin reports
Retinopathy of prematurity (ROP) can be treated effectively with a fraction of the dose of bevacizumab used in the currently recommended regimen, greatly reducing systemic exposure and the dangers it may pose to infants’ development, according to the findings of a new study published in JAMA Ophthalmology
“In the current study, we found that 0.004mg of bevacizumab – a dose that’s merely 0.6% of the dose used in the 2011 study of Avastin for ROP – may be the lower limit to be effective for most infants with ROP,” said the study’s protocol chair, David K. Wallace MD, MPH, Jaeb Centre, chair of ophthalmology at the Indiana University School of Medicine.
The masked, multi-centre, dose de-escalation study involved 59 preterm infants with type 1 ROP that underwent a single intravitreal injection of bevacizumab (Avastin®, Roche) at low dosages ranging from 0.008mg to 0.002mg between April 2017 and May 2019. The patients had a mean birth weight was 664 grams, and a mean gestational age of 24.8 weeks.
The patients were treated in consecutive groups that received progressively lower dosages of bevacizumab than the previous group. Upon each dosage group’s completion of four weeks’ follow-up, an independent data safety and monitoring committee reviewed the outcomes to determine the bevacizumab dosage to use in the next treatment group.
Short-term success –defined as improvement in ROP within four days after the injection and no recurrence requiring treatment within four weeks – was achieved in 13 of 13 eyes (100%) receiving 0.016mg bevacizumab, nine of nine eyes (100%) receiving 0.008mg, nine (90%) of 10 eyes receiving 0.004mg but only 17 (74%) of 23 eyes receiving 0.002mg.
Previous research has shown that bevacizumab enters systemic circulation following intravitreal injection and decreases the plasma levels of vascular endothelial growth factors (VEGFs) the study’s authors said. That raises concerns about possible adverse effects, since VEGFs are essential for normal development of the brain, lungs, bones, kidneys, and retina.
The authors also note that the strength of the study’s finding was limited by the small number of patients it included and its short follow-up time. However, the researchers will continue in their follow-up of the infants in the study and report recurrences and two-year results. The study was conducted by the Paediatric Eye Disease Investigator Group (PEDIG) and supported by the National Eye Institute (NEI), part of the National Institutes of Health.

Free
Membership to WSPOS is available for FREE on www.wspos.org World Society of Paediatric Ophthalmology and Strabismus Contact Info: WSPOS, Temple House, Temple Road, Blackrock, Co. Dublin, Ireland Tel: +353 1 288 3630 Fax: + 353 1 209 1112 Email: wspos@wspos.org Join our society and become part of one of the largest networks of paediatric ophthalmologists in the world. You’ll gain access to our wide library of videos, including our “Masters in Surgery” archive and also get the chance to collaborate on our global case report quiz. At WSPOS, we believe that “Expertise Resides ALL Over the World”
Membership
EUROTIMES | OCTOBER 2020 PAEDIATRIC OPHTHALMOLOGY 38
...we found that 0.004 mg of bevacizumab – a dose that’s merely 0.6% of the dose used in the 2011 study of Avastin for ROP
David K. Wallace MD, MPH





Practice Management & Development Rebuilding Your Practice in a Challenging Environment Paul Rosen UK Faculty Moderator
Include: Back To Work – Lessons Learned, Reimagining a High Performing Practice, Enhancing the Patient Experience, Marketing Your Practice in a Challenging Environment
Topics
Arthur Cummings IRELAND
WEBINARS For further information visit www.escrs.org
Kris Morrill FRANCE Rod Solar UK Guy Sallet BELGIUM
CATARACTS in refugees
Czech surgical mission helps displaced Syrians improve sight and lives. Howard Larkin reports
Once or twice a year, Prof Nada Jiraskova MD and the team of the University Hospital in Hradec Kralove, and Charles University, Czech Republic, travel to Amman, Jordan, to perform cataract surgery for Syrian refugees. In seven trips, the team has done more than 1,200 cataract surgeries, Dr Jiraskova told an ORBIS International symposium.
Operating in a hospital surgical suite equipped with Centurion (Alcon) phaco machines identical to those they use at home, the surgeries have been accomplished with no serious complications despite the very hard, mature cataracts they typically see. Most are successfully removed with phaco, though a few require conversion to extracapsular extraction with a loop, Dr Jiraskova said. In most cases posterior segment lenses are implanted, though in cases of very loose zonules or damaged capsules, sulcus or anterior chamber lenses are used.
The improvement in vision significantly
helps, Dr Jiraskova said. “It really changes the lives of those patients a lot.”
The cataract mission is run by the Czech Republic government through its MEDEVAC humanitarian programme. Focusing on providing medical care to vulnerable groups in regions stricken by humanitarian crises, it provides speciality care at no charge in a variety of disciplines, including cardiac, orthopaedic and plastic surgery in addition to ophthalmology, Dr Jiraskova added.
LOCAL COLLABORATION
Outreach and follow up can be significant issues for cataract surgery missions. In this case, Dr Jiraskova cooperates extensively
with local Jordanian ophthalmologists. They screen and prep all but the most complicated cases, which are prepared by the visiting surgeons. Routine follow-up is also provided by local practitioners.
In some cases, the team sees patients after surgery. Occasionally a lens cannot be implanted in a patient after removing the cataract. In these cases, an anterior chamber lens is implanted on the next trip. YAG capsulotomies are also needed for some patients, Dr Jiraskova said.
“It’s not just surgery. Sometimes the patients are there for five years. They are in a refugee camp and no one knows when they will go home.”

EUROTIMES | OCTOBER 2020
GLOBAL OPHTHALMOLOGY 40
Nada Jiraskova MD and team working in Jordan
Most are successfully removed with phaco, though a few require conversion to extracapsular extraction with a loop
Nada Jiraskova MD
Images courtesy of Adam H ř íbal, MEDEVAC Czech
Dr Jiraskova noted that her country has sometimes been criticised for not accepting enough refugees. She believes the MEDEVAC missions are just as important. “To help the patients without taking them from their families is the most valuable help we can give.”
ABOUT MEDEVAC
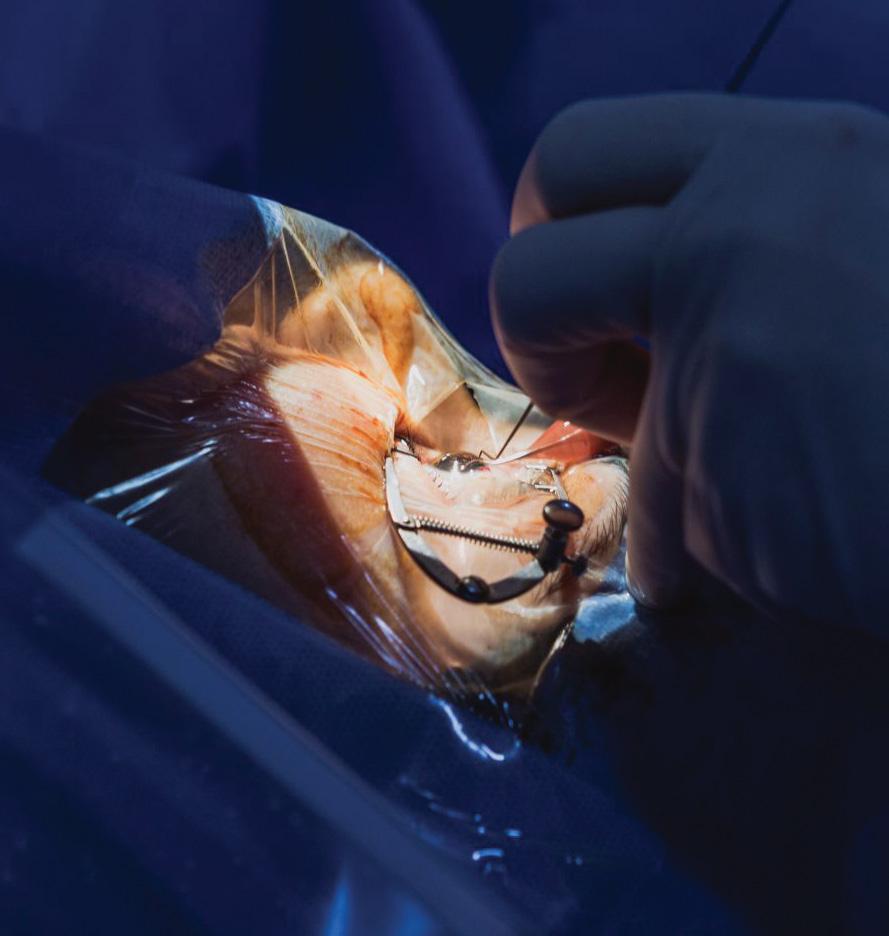
MEDEVAC is a permanent government programme of the Czech Republic, which focuses on providing medical care and assistance for vulnerable groups in countries affected by migration or burdened by a large number of refugees. Its four key efforts are evacuating patients for medical treatment to the Czech Republic; deploying of Czech medical teams abroad; expert trainings for foreign medical staff; and supporting medical projects aimed at rebuilding health infrastructure.
The inception of the MEDEVAC Programme (from English: “MEDical EVACuation”) dates back to the conflict

in Bosnia and Herzegovina. The initial inspiration came from an incident where a child was evacuated from Sarajevo by the UK air force and brought to London for treatment. She did not survive, yet her story became a symbol for healthcare providers across Europe.
The MEDEVAC programme treated children and adults from Bosnia who had been injured in the conflict. It resumed its activities during the wars in Kosovo and Iraq, focusing on treating children with severe injuries.
From its inception until 2013, the focus

of the programme was on medical airlifts. From 2013 onwards, MEDEVAC began medical missions to countries including Jordan, Kenya, Cambodia and Senegal. These missions have included paediatric heart surgery, plastic and reconstructive surgery, orthopaedics, traumatology and ophthalmology.
Since 2015, the programme has been training local medics, and since 2016 it has supported projects aimed at rebuilding health infrastructure.
Nada Jiraskova: nada.jiraskova@fnhk.cz
VISIT OUR WEBSITE FOR INDIAN DOCTORS
INDIA EUROTIMES | OCTOBER 2020 GLOBAL OPHTHALMOLOGY 41
www.eurotimesindia.org
It’s not just surgery. Sometimes the patients are there for five years. They are in a refugee camp and no one knows when they will go home
Nada Jiraskova MD



For more information, visit: annualmeeting.ascrs.org Submissions open August 17, 2020 – ﹐ 2021 ASCRS Annual Meeting August 13–17 San Francisco, CA Featuring ASCRS Subspecialty Day August 13 J IN US!
CE Approval
SCHWIND eye-tech-solutions has received CE approval for the SCHWIND ATOS femtosecond laser. According to Schwind this enables refractive surgeons to offer their patients SmartSight, the latest generation of lenticular extraction developed by SCHWIND, as a treatment option.
The refractive correction is performed entirely with SCHWIND ATOS. Featuring intelligent eye tracking with pupil recognition and cyclotorsion compensation, the laser system provides precise centring of the patient’s eye along the visual axis. This ensures maximum safety and predictable treatment outcomes.

SmartSight is suitable for the treatment of myopia and astigmatism up to five dioptres. In addition, SCHWIND ATOS offers high-precision flaps for FemtoLASIK. “With the CE approval for our femtosecond laser, we have reached another milestone,” said managing director Rolf Schwind. www.eye-tech-solutions.com
IOL’S EXTENDED DIOPTRE RANGE
AcuFocus, Inc. has announced that the IC-8 small aperture intraocular lens (IOL) power range now extends from +10.0D to +30.0D (0.50D steps).
“Having the IC-8 IOL in my practice has provided an exceptional option for my patients who are looking for spectacle independence,” says Professor Sathish Srinivasan, cataract and refractive surgery specialist at University Hospital Ayr, Scotland, and Medical Director of Ayrshire Eye Clinic.
Clinical studies demonstrate the IC-8 IOL produces unparalleled visual outcomes that deliver nearly 3.00D of continuous and uninterrupted range of vision compensation for up to 1.50D of corneal astigmatism and excellent image quality,” he said. www.acufocus.com

REDUCED GAS EMISSIONS
Rayner has announced that changes to their manufacturing and packaging procedures will reduce CO2 greenhouse gas emissions by more than 800 tonnes over the next five years.
The reduced emissions are the result of three dedicated projects: Revising manufacture of the RayOne Hydrophobic IOL so that 26,200 litres of Isopropyl alcohol (IPA) will now be internally recycled annually. IPA will be diverted to hand-gel manufacturers to help combat COVID-19
Completely removing single-use plastic from its IOL manufacturing process. Updating packaging across the entire RayOne IOL portfolio.
www.rayner.com
Visit player.escrs.org for latest episodes Take the opportunity to listen to expert opinion, and share your own INDUSTRY NEWS
INDUSTRY NEWS
43 EUROTIMES | OCTOBER 2020
Santen Vision 2030
MicroShunt pending FDA approval exemplifies new focus on unmet patient need. Howard Larkin reports

Perhaps one of the most conspicuous unmet needs in ophthalmology is the gap in primary open-angle glaucoma (POAG) surgical options between minimally invasive glaucoma surgery (MIGS) for mild-tomoderate cases, and filtration surgery – with all its risks – for advanced and severe cases. There’s virtually no procedure in the middle for patients needing low-teens intraocular pressures (IOP) long-term to slow possibly decades of visual field loss.
Santen is directly targeting this gap with its PreserFlo MicroShunt, said Omar Sadruddin MD, Global Senior Medical Director of Santen Inc. First CE marked in 2012 and commercially available in Europe since late 2018, the device is now under review for approval by the US FDA. The goal is to offer a device with greater efficacy than current MIGS with a safety profile that will encourage implantation earlier than trabeculectomy.
“MicroShunt fits well with our new longterm vision through 2030 for the company,” Dr Sadruddin said. “As an organisation, our contribution to society starts by being ‘in service of patients’, and in targeting a significant unmet need MicroShunt provides great value for the patient.”
Implanted through a conjunctival/ Tenon’s flap, MicroShunt is an 8.5mm tube that shunts aqueous from the anterior chamber through a 70-micron lumen into a filtration bleb. Fins on the tube help keep the shunt in place and prevent excess drainage around the device.
Early multi-centre studies show mean IOP reduction of 30-to-55%, with success rates, defined as IOP >6mmHg and <21mmHg or ≥20% IOP reduction from baseline with/without medication and no reoperation, varying from 81-to-86% at two years. (García-Feijoó J et al. Poster
presented at WGC 2019.)
Indeed, one early study achieved overall success (IOP ≤14 mmHg and >20% reduction in IOP from baseline with or without meds and no reoperation) in approximately 80% of the patients at three years. Five-year results demonstrated similar IOPs, a mean of 11.4mmHg, to those reported in the three-year follow-up paper, suggesting the MicroShunt may provide long-term mid-teens IOP control. (Batlle JF et al. J Glaucoma. 2016;25:e58–65. Batlle JF et al. APAO, Bangkok, Thailand, 2019.) Six- and seven-year data are being prepared for future presentation, Dr Sadruddin said.
ANATOMY OF AN INNOVATION
Every aspect of MicroShunt reflects a spirit of innovation, right down to the material of which it is constructed. Poly(styrene-block-isobutylene-blockstyrene) (SIBS) is a novel polymer with unique elastic attributes designed specifically for long-term implantation in the body – Santen expects its inert chemical properties should allow it to last the lifetime of the patient. It was first implanted in humans as a coating on a drug-eluting cardiac stent in 1999, and has established a strong track record for long-term biocompatibility in cardiac applications (Pinchuk L et al. Biomaterials. 2008;29:448–60).
However, its long-term suitability in the eye as a glaucoma shunt has not yet been established by large-scale trials, which are ongoing, Dr Sadruddin said. “We are taking a very careful approach to generate this data and not make any claims in the meantime. The US [phase III pivotal] trial will provide good longterm data and will be mandated by the FDA. We will probably be asked to follow all patients up for five years.”
Another important feature of SIBS
is it provokes minimal inflammation and encapsulation when compared with commonly used implant materials such as silicone rubber and polypropylene. The material is also thermoformable. This allows it to assume the shape of the globe without a tendency to return to its original shape. By contrast, thermoset materials such as silicone rubber tubes slowly straighten over time, requiring they be covered with a patch graft to prevent erosion. SIBS has no tendency to straighten, which should eliminate the need for a patch graft.
The MicroShunt went through three major design iterations over the course of its 20 years in development. The current device’s 70-micron lumen diameter is sufficiently large to allow passage of sloughed endothelial cells, which are approximately 40-to-50 microns in diameter, yet small enough to prevent clinically significant postoperative hypotony.
The device’s 1.1mm wingspan fin is located halfway down the tube, fixes the device in a 1mm wide scleral pocket, thereby preventing migration into the eye. The fin also prevents leakage around the tube and helps orient the device bevel-up in the anterior chamber (AC), preventing the lumen from being blocked by debris or iris tissue.
When correctly placed, the distal end of the MicroShunt is located 6.0mm posterior to the limbus. This placement directs aqueous humour more posteriorly than trabeculectomy, which may eliminate the thinner-walled anterior blebs that can occur with trabeculectomy. Research is ongoing into how the MicroShunt’s unique posterior bleb, which tends to vascularise while remaining functional and usually remains flat out to three years or more, responds over the long term, Dr Sadruddin said. “As one of our investigators stated, this is not your grandfather’s bleb”, alluding to unique characteristics of a MicroShunt bleb, which is very different than trabeculectomy blebs and understanding this better should provide surgeons with a visual cue on functionality. Studies of how the device might affect corneal endothelial cells in the long term are also under way.
IMPLANTATION
The MicroShunt’s length was designed to allow it to be positioned through a
EUROTIMES | OCTOBER 2020
OUTLOOK ON INDUSTRY 44
As an organisation, our contribution to society starts by being ‘in service of patients’, and in targeting a significant unmet need MicroShunt provides great value for the patient
Omar Sadruddin MD
3mm-long scleral needle tunnel with the outflow end above the scleral surface behind the excursion of the upper eyelid, which minimises potential erosion. Positioning the device to the temporal or nasal side also minimises the risk of damaging the superior rectus muscle while preserving the other side for possible future filtration procedures, if needed.
Implantation is less invasive compared with trabeculectomy, Dr Sadruddin pointed out. An approximately 5-6mm-wide fornix-based conjunctival/ Tenon’s flap is created, followed by formation of a deep sub-Tenon’s pocket of 6.0-to-8.0mm. Wet field cautery is applied to prevent bleeding. Several corneal LASIK shields soaked in mitomycin C are placed within the flap for two-to-three minutes, after which they are removed and the ocular tissue rinsed with balanced saline solution (BSS).
After marking the sclera 3mm from the limbus, a 1mm-deep scleral pocket is made using a triangular knife. A 25-gauge needle is introduced into the pocket and a scleral needle track is created into the AC. The MicroShunt is inserted through the pocket and track, bevel-up, into the AC. When correctly placed, the MicroShunt should bisect
the angle without touching the endothelium or the iris. The fin is tucked in the scleral pocket. After flow is established, Tenon’s and conjunctiva are pulled up, avoiding tucking the distal end of the tube into Tenon’s capsule, and sutured watertight.
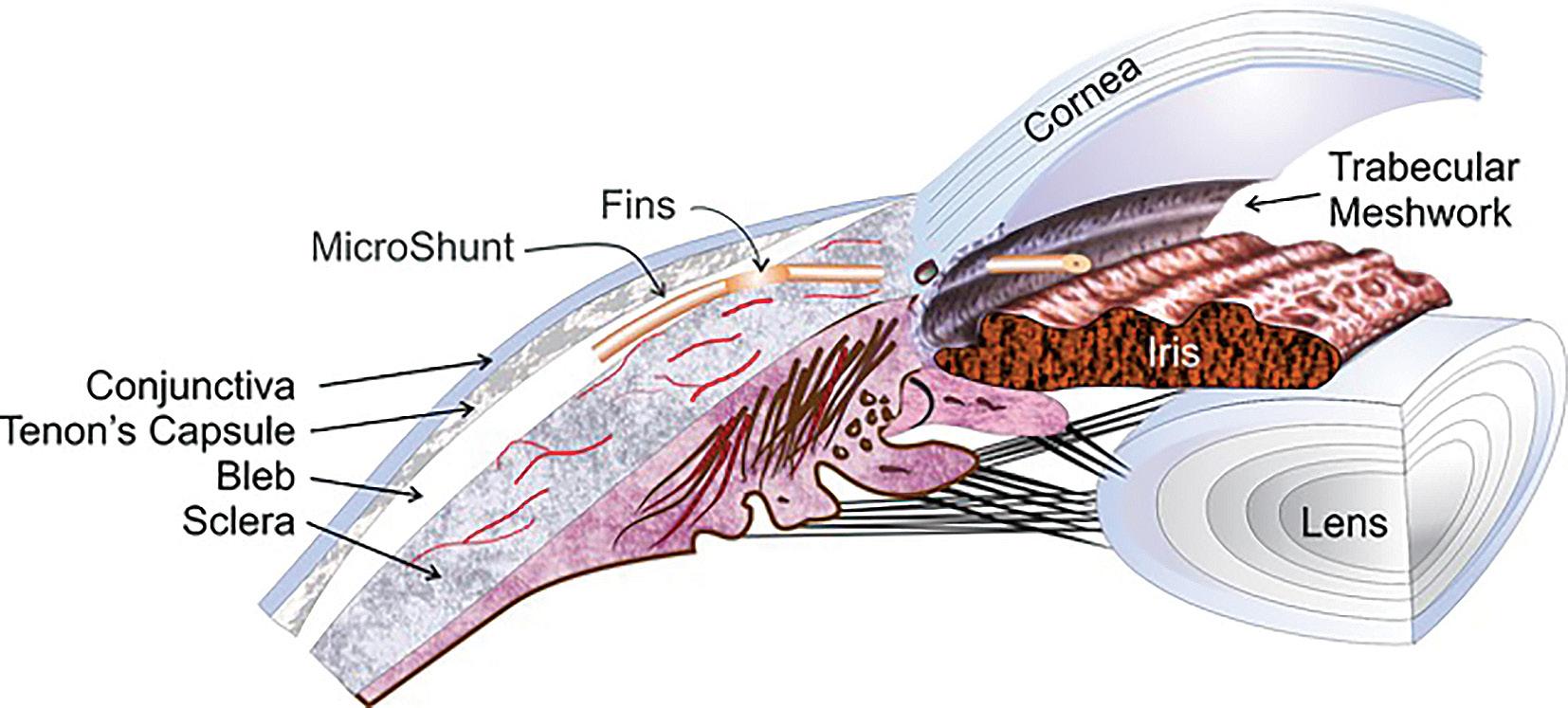
MicroShunt is designed for POAG patients whose IOP is not well controlled on maximum tolerated meds, Dr Sadruddin said. But if the ease of earlier intervention and long-term efficacy pan out, the definition of maximum meds may change from three or more to two – particularly given there is ample research suggesting that adding more meds don’t necessarily lower pressures significant for a long duration.
While implantable with or without cataract surgery, Dr Sadruddin sees glaucoma specialists as the primary target clinicians due to the need to manage the bleb. He sees MicroShunt as another tool in the armamentarium for customising treatment. “If you want an IOP <15mmHg for your patient, and the only remaining options are trab or tubes, MicroShunt may be a reasonable alternative.”
Santen offers a structured course for implanting the device that includes didactic material, virtual simulator and wet labs, as well as supervised procedures. Dr Sadruddin credits having a standardised technique to the users of the product and their willingness to share nuances and pearls of the procedure with new users. “By having created a community of MicroShunt users, we continuously focus on ways to optimise the technique and bring that education to current and future users of the MicroShunt.”
He acknowledged, however, that more long-term studies need to be done to validate the device performance and clinical results. These may include remote sensor studies to monitor IOP 24 hours a day.
“We have made strategic investments in companies looking at sensors. It’s a way to provide more feedback to surgeons to create better management plans, which allows to preserve as much of the patient’s vision as possible,” Dr Sadruddin said. It’s another way Santen is innovating in service of patients.
EUROTIMES | OCTOBER 2020 OUTLOOK ON INDUSTRY
45
The MicroShunt’s length was designed to allow it to be positioned through a 3mm-long scleral needle tunnel with the outflow end above the scleral surface
Courtesy of Santen
We have made strategic investments in companies looking at IOP sensors. It’s a way to provide more feedback to surgeons to create better management plans
EuroTimes is your magazine! Contact EuroTimes Executive Editor Colin Kerr at colin@eurotimes.org Do you have ideas for any stories that might be of interest to our readers?
Omar Sadruddin MD
Integrating telehealth












As ophthalmic practices reopen in the COVID-19 era, telehealth will play a major role. Presenters at the ASCRS Virtual Annual Meeting 2020 discussed how virtual technology can be integrated into revised patient flow to reduce infection risk.

Not every aspect of ophthalmic practice can be virtualised, especially advanced diagnostics, slit-lamp examinations and, of course, surgical procedures. So, the first task is determining what steps can and cannot be done remotely – and explain to patients what will be done at home and in the office and why, said Vance Thompson MD, of Sioux Falls, South Dakota, USA.
For a refractive cataract practice, talking with patients, educating them in real time or with videos, reviewing information from referring physicians, registration and insurance, and counselling them on their vision needs and premium lens choices can all be accomplished remotely, Dr Thompson said. “That is a lot of time in the office that can be done at home.”
Before COVID, most of these steps took place in the office, Dr Thompson said. Now, videos must be watched, and technician interviews and counselling done remotely.
Inside the clinic, half of waiting room chairs have been removed to ensure safe social distancing. The parking lot and patients’ cars are now the first stage of the waiting room. The office texts patients when they are ready for the waiting room.
On surgery day, testing is double checked in the clinic only as necessary and patients are counselled in person and signed consent forms collected before surgery, Dr Thompson said. He suggests mapping
out the patient’s journey before and after arriving at the office to ensure a positive experience. Satisfied patients are more likely to choose a premium lens that better meets all their visual needs, he added.
TRIAL AND ERROR




Ranya Habash MD, medical director for technology innovation at Bascom Palmer Eye Institute, Miami, USA, outlined steps for integrating telemedicine based on her institute’s experience to date.
“New telehealth visit types have been key to adapting to a changing healthcare environment,” she said.






First, providers should go through the patient schedule and proactively determine which patients and which types of visits can be done remotely. These include urgent care telehealth visits, preprocedure counselling, routine follow up and consultations with other physicians, Dr Habash said. A quick look at a televised image can help an ophthalmologist determine if redness can be treated at home with artificial tears or is a condition requiring immediate attention that may not be apparent to a general practitioner. Be sure to include technicians and scribes in telemedicine practice and create templates for each kind of visit to ensure no important points are overlooked, Dr Habash said. At Bascom Palmer, registration personnel call patients to schedule them, and a technician calls 24-to-48 hours in advance to confirm the appointment and ensure the patient has the video platform needed. A coordinator schedules technicians and scribes 24 hours in advance of the visit, and initiate calls and workups before patients speak to a physician.
MARKETING SAFETY
Safety is particularly important consideration, said Elizabeth Yeu MD, of Eastern Virginia Medical School and ASCRS Secretary. In a recent survey of 5,500 patients, depending on location, about one-quarter to two-thirds expressed nervousness about receiving elective health services. She recommended contacting patients and communicating with them prior to their appointments about what your clinic is doing differently to protect them, what they should expect, and any differences with future appointments.
“Traffic jams” at patient check-in and checkout and within the testing and diagnostics area challenge physical distancing. The check-in and out areas in her clinic have thus been separated, and there are also free-standing check-in kiosks within a check-in tent directly outside of the office. Patients are advised to show up no sooner than 10 minutes prior to their scheduled appointment, and family and caregivers now wait outside.
Initially, Dr Yeu’s clinic tried to split three-hour appointments for new cataract and glaucoma patients into two shorter appointments. But patients overwhelmingly preferred one longer appointment. To accommodate, clinic schedules now start earlier and end later with fewer appointments scheduled per hour. Remote telehealth visits for post-op day-one appointments for routine cataract surgery have proven very popular. The perioperative kit has been adjusted to include Diamox immediately after surgery and brimonidine for one week after surgery to prevent IOP spikes.
Dr Yeu believes even more services, including panretinal photography and possibly even slit lamp exams may one day be possible remotely.
Many practice tasks can be virtualised; patient communication is crucial. Howard Larkin reports
EUROTIMES | OCTOBER 2020 PRACTICE MANAGEMENT 46
Staring down the microscope, I recalled the last time I’d done this; my last time operating in theatre had featured kicks in the abdomen without warning, 10 long months ago. That had been when I was pregnant, and now I was back in the operating chair again – free of any physical jabs, but suffering from some bothersome mental ones – this long out of practice, was I up to this? Quieting my mind’s chatter was essential. I found myself using a mental trick from my old handbook on skiing; you replace your train of thoughts with a simple mantra, which reinforces what you want to bring out in your form on the slopes. That allows you to better concentrate on your movement and stay in the present, or in my case, to better focus on my operating without worries getting in the way. Smooth and clean. These words can be repeated on loop, to be played over unwanted thoughts, making them less audible. Smooth and clean. My hands were able to take over then, when I calmed down –they remembered.
Back to work
case. Then when your operating day is coming up – practice with the microscope, remind yourself of the settings. Day of surgery – examine and consent the patients yourself, so you know what to expect. Don’t be afraid, you’ll remember how to operate, but do try to do straightforward cases on your first few theatre sessions. It sounds too simple, but it worked for me.
Another change – we work with masks on all day. The masks cause problems – to prevent fogging of the slit lamp or operating microscope, a lot of us resort to taping the masks down on our faces – not pleasant.
Quieting my mind’s chatter was essential. I found myself using a mental trick from my old handbook on skiing; you replace your train of thoughts with a simple mantra, which reinforces what you want to bring out in your form on the slopes

The cataract was on the dense side – denser than I’d estimated – the grooves needed deepening, and deepening again, as my cracking attempts had to be repeated. Patience – smooth and clean – go again. Finally, under the encouraging gaze of my Consultant – who was sitting in the corner of the theatre, watching the progress on screen – I cracked it. The rest went by quickly; suddenly I was sealing the wounds. It had been fine, my first case back was over. It turned out that what I had been reassured by mentors was true – getting back operating is not that bad.
My predictions about getting back to work after maternity leave have turned out different to what I imagined – I was not alone in being out of practice. The other trainees, and even the Consultants, had not been operating. The COVID pandemic had drastically reduced elective procedures for close to three months in my hospital, the Royal Victoria Eye and Ear Hospital in Dublin. So everyone could sympathise and understand what it’s like to get back into performing surgery, and to have to face down fears that you might have gotten rusty. Before that first Monday back I had gotten some excellent advice from ophthalmic surgeons who had taken maternity leave and been through it. Before your first theatre list – visualise the steps of surgery, write them down even. Close your eyes and see yourself proceeding through a straightforward
Sometimes when I’m examining a patient I’ll wonder why my view is poor; then I’ll see that the patient’s mask is up, and my 90D is beaded with condensation from their breath. So now I usually ask if they can pull the mask down just below their nose. The masks may cause more serious problems; on an evening on call I saw an elderly patient who had an intravitreal avastin for their macular degeneration, performed in another hospital, who presented to us a week later with a dense vitritis and tender globe –endophthalmitis. Theatre staff were quickly mobilised for a tap and inject. I had heard of increased infections in some units, and read reports of more oral flora-related endophthalmitis cases during COVID. Thinking about oral flora, and how dangerous a bite injury is, with a high likelihood of polymicrobial infection, it makes sense to me to be cautious about masks, which can direct a patient’s breath up to their eyes, when carrying out an invasive procedure like an injection. So when we do injection lists now, while the nurse and I kept our masks on, I have the patients lower theirs for the injection.
An added dimension to getting back to work, which I had not accounted for, is the sleep deprivation. Having an infant at home, one who still wakes to feed at night (a few times) does not make for restful sleep. I used to depend on my eight hours, or so I thought, but I am surprising myself with how functional it is possible to be on quite broken sleep. Someday perhaps, our baby might sleep through the night... Not yet. Getting babies to sleep can be trickier than cataract surgery.
Clare Quigley is a resident at the Royal Victoria Eye and Ear Hospital, Dublin, Ireland
47
Maternity leave and lockdown have similar effects on out-of-practice surgeons. Clare Quigley reports
INSIDE OPHTHALMOLOGY EUROTIMES | OCTOBER 2020
Illustration by Eoin Coveney
Let the world come to you
For many of us it’s been a long time since we last routinely packed a bag and hopped on a plane for a short break or a business conference. Who could have imagined a few months ago that a virus would put a stop to that familiar lifestyle? COVID-19 might have cancelled our travel plans but it hasn’t taken away our desire to explore and to travel. Nor has it diminished the determination of tourist boards to keep our interest in their city alive. It’s fair to say that by diving into their updated websites we might see and understand more of iconic cities like Paris, Barcelona and Amsterdam, among others, than we ever could ‘in person’.
I’ll admit that the queues at Amsterdam’s Rijksmuseum have always discouraged me from exploring one of the world’s most renowned museums. So it was enjoyable to make a private visit online (https://www. rijksmuseum.nl/en/from-home). I thoroughly recommend the tour of the most famous masterpieces on show, from Rembrandt’s Night Watch to Vermeer’s Milkmaid. If you are already familiar with the museum, dip into #rjksmuseumfromhome to connect with a series of YouTube videos in which curators talk about the works in their care. Exit through the gift shop.

Even if you’ve visited the Van Gogh Museum previously, you’re sure to find something new on their website. For me, it was the trove of Van Gogh’s translated letters. Never has the artist seemed as contemporary as he does here, thanking his brother for some much-needed money, gently critiquing another artist’s work, describing his own plans for future paintings to his mother and sister. Browse the correspondence online at https://www. vangoghmuseum.nl/
Barcelona reaches out to the virtual tourist, too; Gaudi’s unfinished church, the Sagrada Familia, is endlessly fascinating. Construction started in 1882 and is due to be completed by
2026. A virtual tour offers more detail than anyone could access ‘in person’. The online visit offers remarkable 360º views inside and out as well as the work-in-progress areas closed to ordinary tourists. https:// sagradafamilia.org/visita-virtual
The Picasso Museum is another Barcelona museum that showcases its treasures online. http://www.bcn.cat/ museupicasso/en/collection/highlights html. For a change of pace, check out the Camp Nou website for an up-close look at the famous stadium. Visit the pitch, the stands, the VIP boxes, the official store, the locker rooms and the FCB Museum. https://www.youvisit.com/ tour/campnou. Otherwise, you can treat yourself to a leisurely virtual tour of the whole city. https://www.youvisit.com/tour/ barcelona?pl=undefined
As the Parisian tourist website puts it: “Can’t get to Paris? Well then Paris will come to you!” And it does. https:// en.parisinfo.com/what-to-do-in-paris/info/ guides/virtual-visit-paris. You might start
with an online exploration of the Louvre museum – there are five itineraries to follow. Would you prefer a moment of quiet contemplation? Let yourself be immersed in the beauty of Sainte-Chapelle. Explore Palais Garnier, the Paris opera house, from the underground lake to the view from the roof; there are four virtual tours to guide you. Then stretch your imagination, if not your legs, with an online tour of Montmartre or a visit to the Eiffel Tower.
London and other major cities also put their best touristic feet forward online. Find them on Google’s fascinating arts and culture portal. https://artsandculture. google.com/search/partner?em=m0k3p&ca tegoryid=place
But what if you’d rather get away from it all.? You can’t get much further away than outer space. The NASA website includes internal views when the crew is on duty and Earth views at other times. https://www. nasa.gov/multimedia/nasatv/iss_ustream. html. Or you might be interested in the Palmer Station — the only US research facility on the Antarctic Peninsula. It’s online at all times. Sit back and observe either the penguins or the researchers braving sub zero temperatures: https://www. usap.gov/videoclipsandmaps/palwebcam. cfm. Warm yourself up with a cup of cocoa and a safari in South Africa courtesy of Africam: https://www.africam.com/wildlife
The whole world awaits. Virtually.
With international travel restricted due to COVID-19, Maryalicia Post explores the wonders of virtual travel
EUROTIMES | OCTOBER 2020 48 TRAVEL
I thoroughly recommend the tour of the most famous masterpieces on show, from Rembrandt’s Night Watch to Vermeer’s Milkmaid
47,863 * * Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk Reach at a Glance 10 issues per year
Intrigued by technology
In the first of a new series Guy Sallet, Medical Director, Eye Institute Aalst, Belgium, talks about his life in ophthalmology

Why ophthalmology? I was destined to be an ophthalmologist as my father was an ophthalmologist.
What I liked about ophthalmology was the physics of the visual optics, how precious the sense of vision is and how great the gratitude was from people getting their vision back after surgery. The other thing I liked was that you have full control over the process, from making the diagnosis, proposing the treatment, doing surgery and seeing the final results. You work very independently, so this was quite attractive to me.
The prospect of doing private practice was also attractive as this meant you were not entirely dependent on working in a clinic.
During my training in ophthalmology
I was also intrigued by the evolution of the technology in ophthalmology.
MAJOR INFLUENCES
One of the major influences in my career was my father. He told me: “Guy, you should go about technology in a totally different way to the way I did it.” When I started in the 1990s in Belgium, the only downside to our education was that we did not have a lot of exposure to ocular surgery. That is why at the beginning I concentrated on medical retina and became a retina specialist.
I did a lot of research on melanoma, macular degeneration and various retinal diseases because we did not have any access to surgery. This triggered my interest in clinical studies and the scientific part of ophthalmology.
LEARNING LASIK
I also had contacts in South Africa and in the last year of my residency I went for one year to the University of Pretoria. I made friendships for life there. I also got the opportunity to carry out anterior segment surgery and to expand my surgical skills.
In 1994 there had been no LASIK procedure carried out in Belgium. A group of distinguished Belgian doctors started an excimer laser group. I wanted to be part of this group, which was not easy as I was not well known enough. Eventually I was able to become part of this group and through my contacts in South Africa I learned the LASIK procedure because at that time LASIK was quite popular in South Africa and as a young ophthalmologist, this boosted my refractive practice.
EXPANDING KNOWLEDGE
As you progress in your career, you take on added responsibilities. Having newer and younger doctors involved and having regular staff meetings helps this process. Over the years, I have come into contacts with different leaders in the field and in their different sub-specialties. This has triggered my interest in new things and has helped me to expand my knowledge. I started off in a solo practice, which grew gradually, and I am now working with eight ophthalmologists and with a staff of 12 people. The younger ophthalmologists have given me an insight into new developments in medicine, which as I student I did not have access to. I’m thinking about genetics, molecular biology and other treatment resources.
LEADERSHIP SKILLS
You need to have the character to be comfortable with leadership. As a resident I was a board member of the Belgian Society of Residents in Ophthalmology and in this way, I became involved in organising congresses. My involvement as a board member of the Excimer Laser Group also helped me to become a Practice Manager. We do not have a large practice. At the beginning I was doing everything, including administration, recruitment and financial management. As the practice grew, I tried to develop a framework where everybody has their own tasks and this was the next evolution in developing my management skills.
ADVICE FOR YOUNG OPHTHALMOLOGISTS
I would advise young ophthalmologists to get a comprehensive knowledge of ophthalmology, to know the different aspects of the eyes and then to get involved in sub-specialties. The other advice is that you should be triggered by new treatment modalities and new technologies. This will ensure that your job will never become boring and ophthalmology will be a great thing to do for the rest of your life. The training opportunities available now with virtual training modules for surgery and platforms like the ESCRS training platform are also very useful.
This article is based on an interview in the EuroTimes Eye Contact video series, which can be accessed on the ESCRS Player at https://player.escrs.org
EUROTIMES | OCTOBER 2020 MY LIFE IN OPHTHALMOLOGY 50
I did a lot of research on melanoma, macular degeneration and various retinal diseases because we did not have any access to surgery
You need to have the character to be comfortable with leadership
Guy Sallet, MD
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
↙ LAST CALL
OCTOBER 2020
38th Congress of the ESCRS
Virtual Meeting
2 – 4 October
www.escrs.org
20th Euretina Congress
Virtual Meeting
2 – 4 October
www.euretina.org
NOVEMBER
BEAVRS 2020
Virtual Meeting
6 November
https://beavrs.org/
AAO 2020
Virtual Meeting
13 – 15 November
https://www.aao.org
/annual-meeting
100th SOI
National Congress
25 – 28 November
Rome, Italy
https://www.congressisoi.com
XXI International Congress of the Brazilian Society of Ophthalmology
26–28 November
Rio de Janeiro, Brazil
https://sistemacenacon.com.br/site/ sbo2020/mensagem
DECEMBER
14th EGS Congress
14 – 16 December
Brussels, Belgium
www.egs2020.org/
2021
JANUARY
6th Annual Congress on Controversies in Ophthalmology: Asia-Australia (COPHy AA)
29 – 30 January
Bangkok, Thailand
http://cophyaa.comtecmed.com/
FEBRUARY
25th ESCRS Winter Meeting
19 – 21 February
Krakow, Poland
www.escrs.org
10th EURETINA Winter Meeting
26 – 27 February
Vilnius, Lithuania www.euretina.org
MARCH
6th San Raffaele OCT & Retina Forum
5 – 6 March
Milan, Italy
https://www.octforum2021.eu/
12th Annual Congress on Controversies in Ophthalmology: Europe (COPHy EU)
18 – 20 March
Lisbon, Portugal
http://cophy.comtecmed.com/
CALENDAR 51
EUROTIMES | OCTOBER 2020
The 38th Congress of the ESCRS will be streamed live from Amsterdam
JUNE
AECOS 2021 European Symposium
3 – 6 June
Florence, Italy
https://aecosurgery.org/ 2021-european-symposium/
46th Meeting of the European Paediatric Ophthalmological Society (EPOS)
17 –19 June
Copenhagen, Denmark

https://epos2021.dk/
JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA
https://aecosurgery.org/ 2020-summer-symposium/
JULY
33rd APACRS–SNEC
30th Anniversary Joint Meeting
29 – 31 July
Suntec City, Singapore
https://apacrs-snec2020.org/
AUGUST
ASCRS Annual Meeting 2021
13 – 17 August
San Francisco, USA
https://ascrs.org/news/ascrs-news/ 2021-ascrs-annual-meeting-update
SEPTEMBER
5th International Glaucoma Symposium
3 – 4 September Mainz, Germany
https://glaucoma-mainz.de/
49th ECLSO Conference
3 – 4 September Paris, France
https://www.eclso.eu/
CALENDAR 52 Watch the latest video content from ESCRS and EuroTimes, FREE on the ESCRS Player Advanced Instructional Courses Eye Contact Interviews Video of the Month Video Journal of Cataract, Refractive & Glaucoma Surgery Young Ophthalmologists Videos: “My Early Surgeries” Online Museum player.escrs.org
EUROTIMES | OCTOBER 2020
The 46th Meeting of the European Paediatric Ophthalmological Society (EPOS) will take place in Copenhagen, Denmark
The 49th ECLSO Conference will take place in Paris, France

www.ziemergroup.com/escrs
REFRACTIVE LENTICULE NEW: CATARACT THERAPEUTIC VIRTUAL ESCRS 2020 Join our Satellite Symposium and get to know the newest developments at our virtual booth.
THE MOST VERSATILE DEVICE

For indications, contraindications and warnings please refer to the relevant product’s instruction for use. © 2020 Alcon Inc. 09/20 EMEA-VIV-1900035 1.AcrySof® IQ Vivity® Extended Vision IOL Directions for Use. 2. Alcon Data on File. TDOC-0055576. 29-Mar-2019. 3. Alcon Data on File. Optical Evaluations of Alcon Vivity®, Symfony*, and Zeiss* AT LARA* IOLs. *Trademarks are the property of their respective owners. Adva ncing CATARACT SURGERY LEAVE HALOS & GLARE BEHIND1-3 With the visual disturbance profile of a monofocal IOL, the AcrySof ® IQ Vivity® lens is the clear choice for delivering an extended range of vision with minimal halos and glare.1-3 See the difference it can make for your patients. Move Presbyopia Correction Forward Join us at the 2020 Virtual ESCRS Congress to learn more! Presbyopia correction with monofocal simplicity: AcrySof® IQ Vivity® Date: Friday 2 October 2020 | Time: 2.00 PM – 2.45 PM CET Moderator: Kjell Gunnar Gundersen (Norway) #VivaVivity SAVE THE DATE!