September 2020 | Vol 25 Issue 9 SPECIAL FOCUS RETINA CATARACT & REFRACTIVE | CORNEA | GLAUCOMA PAEDIATRIC OPHTHALMOLOGY Relieving the Burden



Publisher Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer
Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett
ESCRS
Tel: 353 1 209 1100
email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983 As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between February and December 2019 was 47,863
18 A humble servant: Dr Peng Sim’s shortlisted essay for the John Henahan writing prize
19 Compensating for hyperopic shift may further improve refractive outcomes
20 EUREQUO finds younger patients, better cataract outcomes over past decade
21 JCRS highlights
22 Relaxing patients can be achieved by consistent team-based approach
www.eurotimes.org CORNEA
31 AI deep learning algorithm can diagnose OSD by assessing OCT images
32 Emerging therapies may improve graft survival and reduce transplant need
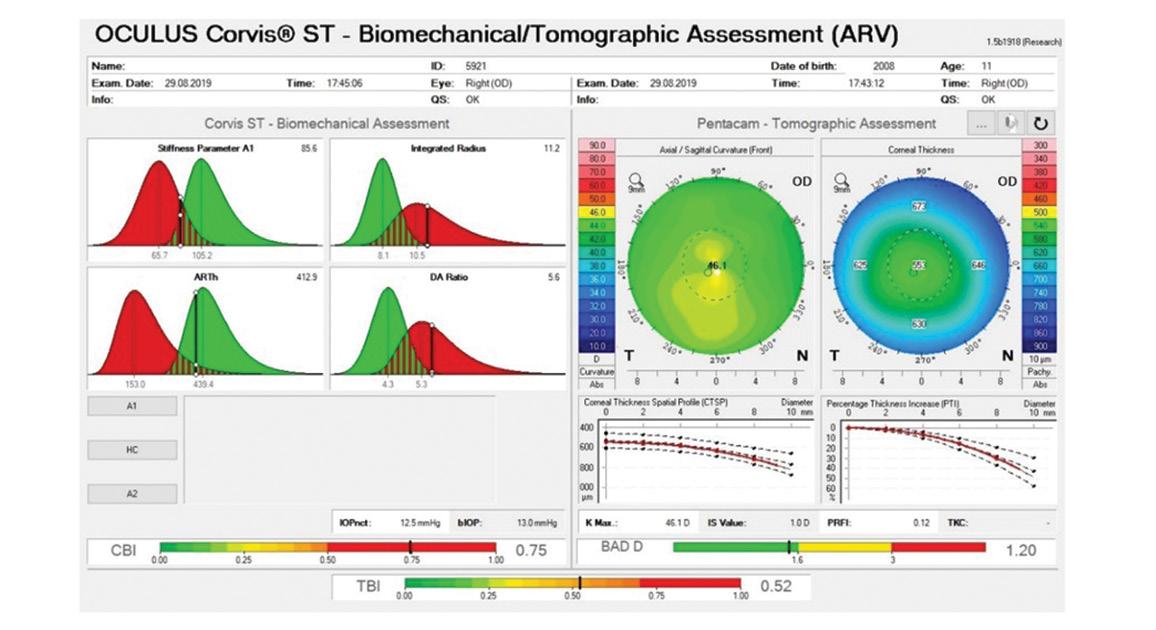
34 Deep learning improves detection of mild ectasia
35 Traces in tears and tissues improve diagnosis, prognosis and management
25 ESCRS President Rudy Nuijts looks ahead to a Virtual Meeting

26 David F. Chang will deliver the Ridley Medal Lecture
27 Congress symposia will highlight new and upcoming breakthroughs in clinical research
28 Looking at the lens at the ESCRS Virtual meeting
29 Main symposium speakers discuss definitions, metrics, and surgical techniques
30 How YOs can get the most from a virtual congress
36 Careful planning and followup are more important than who performs MIGS
39 COVID-19 has sparked an explosion in tele-ophthalmology
P.30 CONTENTS A EUROPEAN OUTLOOK ON THE WORLD OF OPHTHALMOLOGY
GLAUCOMA
PAEDIATRIC
OPHTHALMOLOGY
REGULARS 41 Books 42 Industry News 45 Practice Management 46 Random Thoughts 47 Calendar SPECIAL FOCUS RETINA 04 Treatment burden has become the critical issue in neovascular AMD care 06 EURETINA develops virtual congress experience for 2020 07 Patients consider risk of blindness as a reason to quit smoking 08 Changes in dark adaptation correlate with status of AMD 10 New classification system may help treatment of myopic traction maculopathy 11 Ophthalmologica highlights CATARACT & REFRACTIVE 12 Lenticular astigmatism, effective lens position and toric IOL implantation 14 Intraoperative tools for refractive cataract surgery 16 Do androids dream of the perfect rhexis? Dr Claudette Veldhuizen’s shortlisted essay for the John Henahan writing prize 17 Flap lift for refractive enhancement after LASIK is a feasible surgical alternative
MEETING PREVIEW
VIRTUAL
EUROTIMES | SEPTEMBER 2020
MEDICAL EDITORS
Door Hanger
INTERNATIONAL EDITORIAL BOARD



Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
ESCRS 2020 Keeping Us Connected 2-4 October 2020 www.escrs.org Shhh I'm at the ESCRS Congress Research | Innovation | Vision EUROTIMES | SEPTEMBER 2020
Emanuel Rosen Chief Medical Editor
José Güell
EDITORIAL 2
Thomas Kohnen
ESCRS 2020 Keeping Us Connected 2-4 October 2020 www.escrs.org Shhh I'm at the ESCRS Congress Research | Innovation | Vision DO
Paul Rosen
NOT DISTURB
enclosed with this issue at page 16 Guarantee you will have peace and quiet to attend the ESCRS Virtual Congress 2-4 October 2020 Register now www.escrs.org
Trifocal IOLs
When expectations and outcomes align
Premium trifocal IOL solutions for all your patients
• Advanced 16 diffractive step optic reduces light loss to only 11%:
- Improved contrast sensitivity
- Clinically-proven less photic phenomena

- Improved quality of night vision
• Smallest fully preloaded injector system*
The most complete family of trifocal IOLs in the industry
Speak to your Rayner representative today rayner.com/trifocal
Supplementary:
Support the best visual outcomes with...

An eye drop family designed specifically to support visual outcomes and patient satisfaction before and after surgery. rayner.com/aeon

A free mobile and web-based digital platform that collects powerful Patient Reported Outcomes (PROs) over three years. rayner.com/raypro




and
are proprietary marks of Rayner.
Intraocular Lenses Limited, 10 Dominion Way, Worthing, West Sussex, BN14 8AQ. Registered in England: 615539. EC-2019-122 12/19
*RayOne Trifocal, RayOne Trifocal Toric ©2020 Rayner. Sulcoflex, RayOne,
AEON
RayPRO
Rayner
Relieving the burden
New approaches to AMD focused on reducing burden of treatment. Dermot McGrath reports
With regular intravitreal injections still the norm, treatment burden has become the critical issue in neovascular AMD care. Physicians are now focused on finding effective strategies to extend the dosing interval, avoid under-treatment and maximise visual acuity gains.
“Anti-VEGF agents such as ranibizumab (Lucentis), bevacizumab (Avastin) and aflibercept (Eylea) work very well and are the gold standard, but we need drugs that work longer and have the same efficacy and hopefully even better anatomic results,” said Peter K Kaiser MD, Professor of Ophthalmology at Cleveland Clinic Lerner College of Medicine in Ohio, United States, during
a special session on AMD at the World Ophthalmology Congress 2020 Virtual. Dr Kaiser emphasised the need to reduce the treatment burden for patients and ideally have long-term visual gain.
“A lot of our real-world studies with anti-VEGF agents show that the results are not as good as in the clinical studies where there is more aggressive treatment. The hope for new agents and other approaches currently under development is that we can more closely match the clinical trial results in the real world,” he added.
LONGER-ACTING ANTI-VEGF AGENTS
Any new anti-VEGF treatment hoping to make an impact on the market will need to

show similar safety, efficacy and durability to aflibercept which has already been approved by the FDA for four-, eight- and 12-week dosing schedules.
Recently approved by the US FDA, Brolucizumab (Beovu, Novartis) demonstrated superior anatomic outcomes and non-inferior best-corrected visual acuity (BCVA) at eight to 12-week dosing intervals compared with aflibercept dosed every eight weeks in clinical trials. However, concerns about the drug’s safety profile surfaced in the wake of reported cases of retinal vasculitis after brolucizumab injections. A Novartis safety review subsequently found retinal vasculitis, retinal artery occlusion or severe vision loss occurred in 8.75to-10.08 out of 10,000 injections. Several national regulatory agencies, including
EUROTIMES | SEPTEMBER 2020 SPECIAL FOCUS: RETINA 4
the FDA, have subsequently updated their prescribing information (PI) to include these new vision-related side effects.
Abicipar pegol (Allergan/Molecular Partners) is another new drug that successfully extended dosing intervals up to around 12 weeks without loss of efficacy in phase III trials compared to monthly ranibizumab. However, as with brolucizumab, concerns have been raised about the drug’s safety profile, with a high rate of intraocular inflammation (up to 15.3% in the CEDAR and SEQUOIA studies) following abicipar injections compared to almost zero rates with ranibizumab and other anti-VEGF agents. Citing an unfavourable benefit-risk ratio, at the end of June 2020 the FDA declined to approve abicipar pegol for treatment of nAMD.
Conbercept (Kanghong Biotech), an anti-VEGF recombinant fusion protein that was approved in China in 2013, is currently undergoing worldwide, randomised clinical trials (PANDA) to evaluate its efficacy and safety of conbercept delivered every 12 weeks compared to aflibercept every eight weeks in treating nAMD. In earlier trials, a quarterly dosing schedule with conbercept 0.5mg was shown to be effective at maintaining visual acuity gains.
Faricimab (Genentech), a drug that inhibits angiopoietin 2 (Ang2) as well as anti-VEGF A subforms, has shown solid efficacy at 12-to-16 week treatment intervals as opposed to monthly ranibizumab in phase II trials. The drug is currently in phase three twrials with patients randomised to receive either faricimab every 12-to-16 weeks or aflibercept dosed every eight weeks.
KSI-301 (Kodiak Bioscience), a large molecule antibody-biopolymer conjugate with an anti-VEGF A antibody with Lucentis-like binding domains, may also provide an important dosing advantage compared to existing anti-VEGF drugs. Initial results from the phase II DAZZLE study underscored the potential of the drug to extend dosing schedules, with 84% of wet AMD eyes and 76% of DME eyes extended to four months or longer after the last loading doses before receiving their first retreatment.
BIOSIMILARS ON THE HORIZON
A potentially major disruption to the current nAMD treatment landscape may soon arrive in the form of biosimilars, a biologic medical product highly similar to an already approved biological medicine. With the patents on Lucentis expiring in the US in 2020 and in Europe in 2022, a number of ranibizumab biosimilars are already in the pipeline. One such biosimilar, Razumab (Intas Pharmaceuticals Ltd), has been approved for clinical use in India since 2015 for all the indications in which ranibizumab is used. Others such as FYB 201 (Formycon AG) and Xlucane (Xbrane Biopharma) are expected to obtain approval for the US market this year.
Other biosimilars for aflibercept are expected to obtain approval before 2025 in Europe and the US once the patent for aflibercept expires in those regions.
NEW DELIVERY SYSTEMS
Some manufacturers are turning to new delivery systems to potentially ease the treatment burden. Currently undergoing phase III trials, Graybug Vision’s GB-102 injectable microparticle technology delivers sustained release of the tyrosine kinase inhibitor, sunitinib malate. The randomised study will compare 1mg and 2mg doses of GB-102 administered every six months to aflibercept every two months.
Another approach has been embraced by the Port Delivery System (PDS, Genentech). Currently in phase III clinical trials, the PDS is a surgically implanted, refillable intraocular implant that can be filled with a customised formulation of ranibizumab. The implant is placed surgically at the pars plana and can be refilled in the office.
In the phase II LADDER trial, 80% of the patients in the 100mg highest dosage group went greater than or equal to six months without requiring a PDS refill and achieved similar BCVA gains and reductions in central retina thickness to those receiving ranibizumab 0.5mg injections.
The Archway trial met its primary endpoint at 40 weeks, and the PDS with refills every six months provided equivalent visual and anatomical outcomes to monthly ranibizumab injections, while reducing the treatment burden fivefold.
Although the results from the clinical trials were promising, the device may not be suitable for all patients, according to Dante Pieramici MD, one of the study investigators.
“It is a surgical procedure and people
will look at some of the complications such as endophthalmitis which may be higher than with intravitreal injections, so we are going to have to balance those issues for our patients.
“A patient who is doing very well on anti-VEGF and needs an injection every eight-to-12 weeks may not be so enthusiastic about the PDS. On the other hand, a patient who needs the drug every four-to-six weeks and has tried different agents may be a lot more enthusiastic about it,” he said.
GENE THERAPY
Gene therapy could transpire to be the real game-changer in nAMD treatment in the next few years, delivering a durable “once and done” alternative to regular intravitreal injections.
The concept is to use a viral vector to deliver an anti-VEGF gene into a patient’s own DNA. The gene then produces its own therapeutic anti-VEGF protein without the need for ongoing injections.
Initial trials of therapies such as ADVM-022 (Adverum) and RGX-314 (RegenexBio) have shown promise for the treatment of exudative AMD.
In phase I trials, ADVM-022 was found to be safe and well tolerated and showed consistent and sustained anatomic improvements in OCT and stable bestcorrected visual acuity. No rescue injections were required up to one year in cohort 1.
RGX-314 has completed phase I/IIa trials in 42 wet AMD patients with five dosing cohorts. After a single subretinal injection, 50% of patients (3/6) in dosing cohort 3 remain anti-VEGF injection-free over two years, and 67% of patients (4/6) are anti-VEGF injection-free from nine months to two years.
“RGX-314 appears to be well tolerated at all dose levels and in this trial we saw no significant inflammation. The gene therapy has long-term durable treatment effect demonstrated over two years, with improved visual acuity and stable retinal thickness,” said Allen C. Ho MD, of Wills Eye Hospital, Philadelphia, United States, speaking at the World Ophthalmology Congress 2020 Virtual.
Dr Ho said the next trials would examine the safety and efficacy of suprachoroidal delivery of the gene.
“Gene therapy is moving forward and it is very exciting for our patients – the science is very compelling and there is a lot more to come,” he said.
SPECIAL FOCUS: RETINA 5
EUROTIMES | SEPTEMBER 2020
RGX-314 appears to be well tolerated at all dose levels and in this trial we saw no significant inflammation
Allen C. Ho MD
It is a surgical procedure and people will look at some of the complications such as endophthalmitis which may be higher than with intravitreal injections
Dante Pieramici MD
EURETINA 2020 Virtual
EURETINA President Frank G. Holz reports


RAmsterdam this October.
As the annual Congress is a very important event for the Society, we are instead developing a virtual congress experience for 2020 from 2-4 October with a stream of live and pre-recorded adapted programme content including panel discussions, which will also be available on demand after the event.
The virtual meeting will be a new endeavour for the Society and one that will allow us to extend the reach of EURETINA.
environment to exchange new ideas and learnings from our medical community.
I am delighted to announce that we will have some excellent keynote speakers at EURETINA 2020 Virtual. Richard Spaide, USA, will deliver the EURETINA Lecture; Stanislao Rizzo, Italy, will deliver the Gisbert Richard Lecture; and the Kreissig Lecture will be delivered by Marta S. Figueroa, Spain.
Meanwhile, the Board of EURETINA would like to
We are excited at this prospect and truly hope that you will join us for EURETINA 2020 Virtual as we come together in a digital
We have worked very hard to deliver the highest quality scientific content curated by world-renowned experts in the field of retina. We will run four parallel channels across three days, specific details for which will are available on the website over the coming months. To help us best adapt our programme to suit this new virtual environment, we have appointed the expert input of advisors in the field. As a result of this feedback, session durations have been reduced with a greater emphasis being put on discussion time and Q&A in order to best retain audience engagement. The reduced three-day programme means that only the very highest quality scientific content will be included, which has been specifically selected by the programme committee to ensure diversity of topics.
EURETINA Lecture
extend wishes of good health and wellbeing to you and your family and we hope that the information on our website www.euretina.org will prove useful to you in your day to day practice during this extraordinary time.
While I regret that we will not be meeting in person in Amsterdam, I believe that our Virtual Congress will be a major success and I look forward to some excellent discussions through the course of the meeting.
Friday 2 October, 10.15 - 10.45
Stanislao
The restless fight against inherited blindness
Saturday 3 October, 12.30 - 13.00
Richard Spaide

Reconsidering Pachychoroid and What it Means
Saturday 3 October, 13.00 - 13.30
Marta
Plasma Rich in Growth Factors for Macular Holes in High Myopia

EUROTIMES | SEPTEMBER 2020 SPECIAL FOCUS: RETINA 6
We have worked very hard to deliver the highest quality scientific content curated by worldrenowned experts in the field of retina
To help us best adapt our programme to suit this new virtual environment, we have appointed the expert input of advisors in the field
EURETINA Lecture
Kreissig Lecture
S. Figueroa
Gisbert Richard Lecture
Rizzo
Risk of blindness from smoking
Significant risks of retinal disease warrant patient counselling.
Leigh Spielberg reports
Patients seem more likely to consider the risk of blindness as a better reason to quit smoking than the risk of dying, said Caroline Klaver MD, PhD, Rotterdam University Medical Center, the Netherlands, told delegates at the 19th Annual EURETINA Congress in Paris.
“And yet, many smokers are not aware of their habit’s risk of eye disease, so I believe it is our responsibility as ophthalmologists to inform them,” she asserted.



Dr Klaver addressed a session on the epidemiology of retinal disease. Her talk, “Risk of Blindness for Smoking”, seemed to open the eyes of many delegates regarding what role ophthalmologists could play in patient’s ocular health via smoking cessation.
Smoking is known to increase the risk of retinal arterial branch occlusions eightfold. The risks of developing both neovascular age-related macular degeneration (AMD) and geographic atrophy are clearly increased, as are the risks of developing cataract, Graves’ orbitopathy, optic neuropathy, intermediate uveitis, dry eye and floppy eyelid syndrome.
“The synergistic effect of smoking and genetic risk of AMD is particularly strong,” said Dr Klaver, increasing the risk by about 50% compared to non-smokers. Fortunately, quitting smoking can significantly decrease the risk of developing geographic atrophy when compared to patients who continue smoking, although how soon the risk decreases after quitting smoking is not known.
There are approximately 7,000 chemicals in cigarette smoke, so the potential causal pathways for smoking and eye diseases are countless. Free radicals cause damage via mitochondrial impairment, oxidative stress and inflammation. This is responsible for the increased risk of optic neuropathy, AMD and uveitis with cystoid macular oedema. Furthermore, the dioxins present in cigarette smoke promote the release of VEGF. And nicotine itself promotes both the accumulation of lipofuscin and the aggregation of platelets.
And the risks to eye health can even start before birth: maternal smoking during pregnancy increases
the risk of strabismus in offspring by 50%, although the pathogenesis is unknown.

“Despite these risks, only about 40% of eye patients who smoke are aware of smoking-related eye diseases,” she said, citing a study performed by the UK National Health Service. Considering that the worldwide prevalence of smoking is 35% in males and 7% in females, the overall effect of smoking on ocular health is enormous.
The effect of e-cigarettes on eye health is not yet known, although there have been reports of acute globe rupture and corneal burns due to e-cigarette explosion. Moreover, recent reports of acute pulmonary disease and death associated with e-cigarette use provide more incentive to counsel patients on the value of quitting.
SPECIAL FOCUS: RETINA 7 EUROTIMES | SEPTEMBER 2020
www.fciworldwide.com Join our Ophthalmic Community! *Petri, A., Boysen, K., Cehofski, L.J. et al. Intravitreal Injections with Vascular Endothelial Growth Factor Inhibitors: A Practical Approach. Ophthalmol Ther 9, 191–203 (2020).
THAN 1 MILLION INJECTIONS PERFORMED WORLDWIDE!
GOLD STANDARD* FOR
PRECIVIA ® MORE
THE
ALL INTRAVITREAL INJECTIONS
And yet, many smokers are not aware of their habit’s risk of eye disease, so I believe it is our responsibility as ophthalmologists to inform them
Caroline Klaver MD, PhD
New A MD clinical endpoints
Dark adaptation testing a useful clinical parameter in assessing response to AMD treatments. Roibeard Ó hÉineacháin reports
Changes in the speed of dark adaptation (DA) appear to correlate with changes in disease status in patients with early and intermediate age-related macular degeneration (AMD), and could therefore be useful clinical endpoints in trials of treatments for the condition, according to the findings of a longitudinal study presented by Cathy Cukras MD, PhD, at Retina 19, a meeting sponsored by Fighting Blindness, a patient-led charity.
“In our longitudinal analysis we generally observed a decline in DA function over time, which correlated with patient-reported functional deficits, and is accelerated in eyes with greater AMD severity, especially in eyes with reticular pseudodrusen,” said Dr Cukras, Head, Unit on Clinical Investigation of Retinal Disease, National Eye Institute, National Institutes of Health, Bethesda, Maryland, USA.
The ongoing single-centre study involves more than 100 patients with early-to-intermediate AMD. The study’s investigators monitored the responses to DA over four years, using a measure called the rod-intercept time (RIT). Dr Cukras noted that they defined RIT as the time taken after a photobleach for visual sensitivity to recover detection of a 5×10−3 cd/m2 stimulus, a decrease of three log units.

The investigators assigned participants to AMD severity groups based on fundus characteristics drusen, pigmentary changes, and subretinal drusenoid deposits (SDDs). In addition, the mean rate of change was computed and correlations with ocular and patient features measures, such as visual acuity, and structural features obtained through multimodal imaging were evaluated, she noted.
The mean change in DA function over time was calculated using the slope of linear regression fits of longitudinal RIT data. Furthermore, patients provided responses to a Low Luminance Questionnaire (LLQ), which were given at baseline and yearly. Non-parametric statistical testing was performed on all comparisons, she explained.
DA correlates with objective and subjective AMD parameters.
Dr Cukras noted that the analysis revealed that higher rates of RIT prolongation correlated significantly with AMD severity group assignment at baseline (p=0.026) and at year four (p=0.0011). In addition, eyes that developed SDD during followup demonstrated higher rates of RIT prolongation relative to those that did not (p<0.0001). Overall, higher rates of RIT prolongation were significantly correlated with greater four-year decreases in LLQ scores (total mean score, p=0.0032).
Furthermore, an analysis of covariance demonstrated that the variables that correlated with DA measures included age, AMD group and the presence of reticular pseudodrusen. The study also showed that patient-reported functional deficits correlated with both reduced DA and reduced choroidal thickness.
VISUAL ACUITY NOT A SENSITIVE INDICATOR OF DISEASE PROGRESSION
Dr Cukras noted that visual acuity has long been used as the primary endpoint for clinical trials of AMD treatment. However, visual acuity is unchanged
early in disease and late in disease the floor effect makes any changes difficult to measure.
“The lack of a broadly applicable treatment for geographic atrophy may be attributed to an incomplete understanding of the mechanisms resulting in photoreceptor dysfunction and death, and uncertainty about the outcomes measures needed to facilitate the discovery of potential treatments in interventional clinical trials,” Dr Cukras said.

Clinical endpoints reflecting disease progression over earlier stages of disease could potentially increase the feasibility of clinical trials and allow for the identification of eyes with more severe cell dysfunction within early and intermediate categories of AMD. She added that examination of pathologic features in eyes with intermediate AMD demonstrate preferential loss of rod cells in the macula even in eyes with early disease, compared with age-matched controls.
“Dark adaptation is one measure of visual function that has been identified to reveal abnormalities in non-advanced stages of AMD. The RIT prolongation as a measure of changing DA function may be a useful functional outcome measure in AMD clinical studies,” Dr Cukras added.
EUROTIMES | SEPTEMBER 2020
SPECIAL FOCUS: RETINA 8
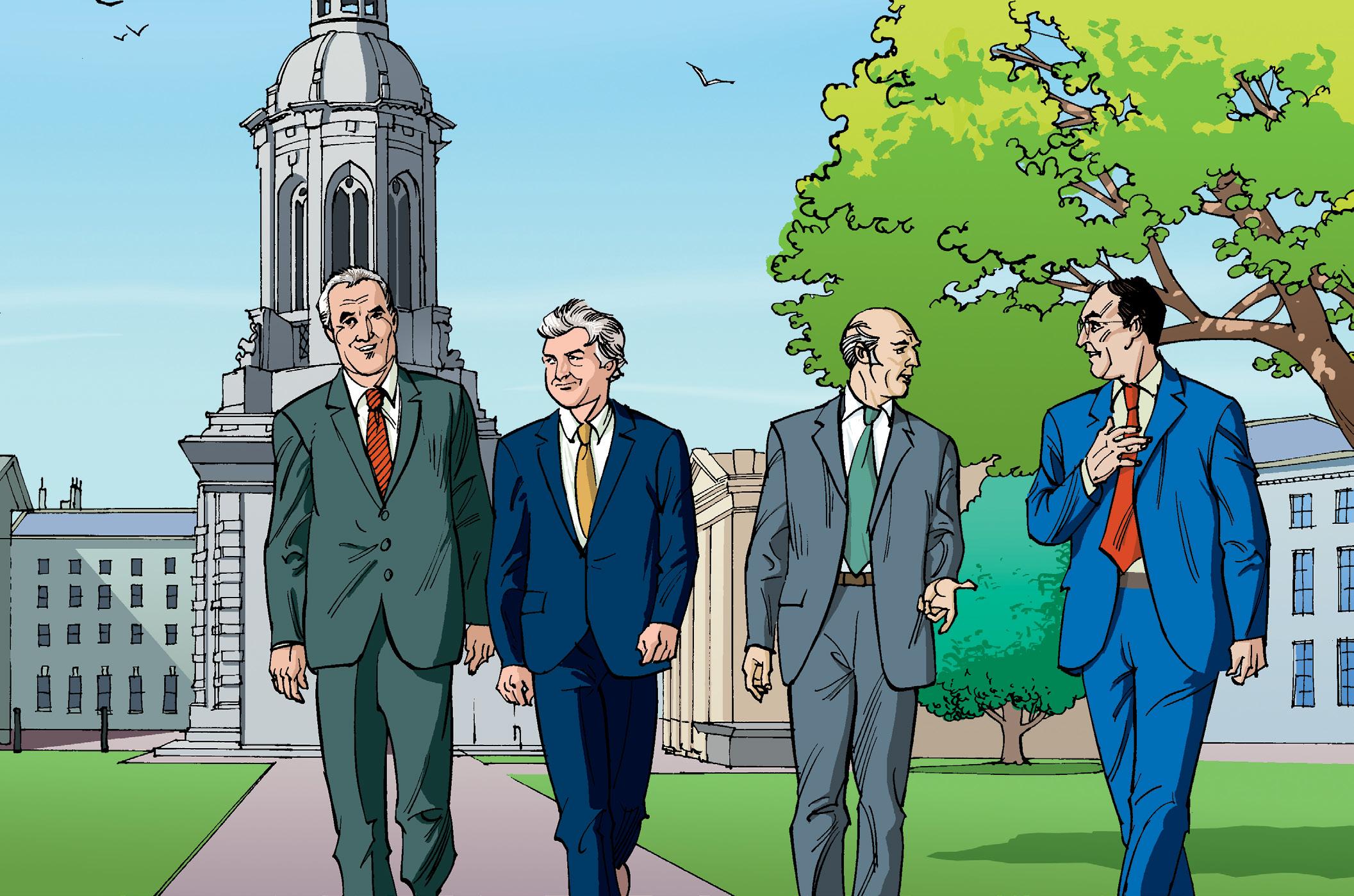
Dr Giuliana Silvestri (left), Clinical Director for Ophthalmic Services, Belfast Health and Social Care Trust and Dr Cathy Cukras, Clinical Researcher, National Eye Institute, USA, pictured at the Fighting Blindness Retina 2019 international conference in Dublin, Ireland
2–4 October 2020 3 days. 4 channels.
Euretina Sessions | Keynote Lectures | Symposia | Courses

We are excited to bring you our first virtual conference. For programme details and to register go to
www.euretina.org

Staging myopic traction maculopathy
Classification system proposed for better management of traction maculopathy. Dermot McGrath reports
Aproposed new classification system for myopic traction maculopathy (MTM) may help clinicians to more accurately predict the course of the disease and orient management strategies for better outcomes, according to Barbara Parolini MD.
“MTM is not one disease but a spectrum of clinical pictures. There is no comprehensive classification, and there is no consensus on management. We have tried to remedy this with a classification system that offers not just an easier means to remember all the distinct types of MTM, but more importantly to correlate them to prognosis and treatment,” she told delegates attending the 19th EURETINA Congress in Paris.
Dr Parolini, Director of the Vitreoretinal Service at EYECARE CLINIC in Brescia, Italy, carried out a series of studies in recent years to study the natural history and pathogenesis of MTM and tried to propose the best management for each type of MTM encountered.
The first phase of the study included 281 eyes with MTM that had been operated by Dr Parolini between 2006 and 2018. All of the MTM subtypes were classified based on preoperative OCT analysis. The distinct MTM types identified in the series included four retinal patterns (1. inner-schisis or innerouter schisis, 2. outer schisis, 3. schisis detachment and 4. detachment) and three foveal patterns (a. intact fovea, b. inner lamellar macular hole, c. full thickness macular hole).
The study established a statistically significant correlation between types of MTM and the age of the patients, with the lower
type 1 MTM typically found in younger patients. Following on from this, a phase II longitudinal study was carried out to study the natural evolution of MTM in 126 unoperated eyes with at least three OCTs taken at different time points with at least a one-year interval among them and with up to 11 years’ follow-up.
“Considering the correlation between type of MTM and age and the evolution of MTM types in the same eye, we concluded that MTM should not be divided into types but into stages,” said Dr Parolini. The proposed MISS classification (MTM Italian Staging System) details the patterns of evolution from type 1, 2, 3 and 4 in the retina as well as types a, b, and c in the fovea.
“For each type we show the mean best-corrected visual acuity (BCVA) and also the mean time taken to evolve between one stage and the next,” said Dr Parolini.
To find a good correlation with treatment, Dr Parolini conducted a review of 157 eyes with MTM operated with macular buckle (MB), pars plana vitrectomy (PPV) and combined PPV and MB, with analysis of anatomical and functional response to each treatment per each stage.
“The conclusions were that retinal patterns from schisis to detachment could be better solved with a macular buckle while the foveal pattern with splitting into the fovea should be treated with PPV and manoeuvre with the internal limiting membrane. When schisis and/or detachment are combined with a macular hole, macular buckle can be combined with PPV and ILM management”, she said.

Barbara Parolini: b.parolini@eyecare.it

EUROTIMES | SEPTEMBER 2020 SPECIAL FOCUS: RETINA 10 EuroTimes is your magazine! Contact EuroTimes Executive Editor Colin Kerr at colin@eurotimes.org Do you have ideas for any stories that might be of interest to our readers?
Barbara Parolini MD
vision loss in eyes with untreated premacular membrane (PMM) with macular pucker (MP), a new study suggests. The retrospective observation study involved 342 eyes diagnosed with PMM with MP who were untreated for mean observation period of 448 days. The study’s authors used spectral-domain optical coherence tomography imaging to characterise a range of retinal disease parameters. Additionally, they used en face OCT to identify and calculate the area the thickened retina portion. In the 20% of eyes in which visual acuity worsened by two lines or more, the only consistent predictor of PMM progression was the area of retinal
A library of symposia, interviews, video discussions, supplements, articles and presentations









Spotlight on:
Toric IOLs and Presbyopia

Glaucoma
Ocular Surface Disease
Corneal Therapeutics

















forum.escrs.org


EUROTIMES | SEPTEMBER 2020 SPECIAL FOCUS: RETINA 11
NEW CONTENT
Everything you ever wanted to know: Toric IOL implantation


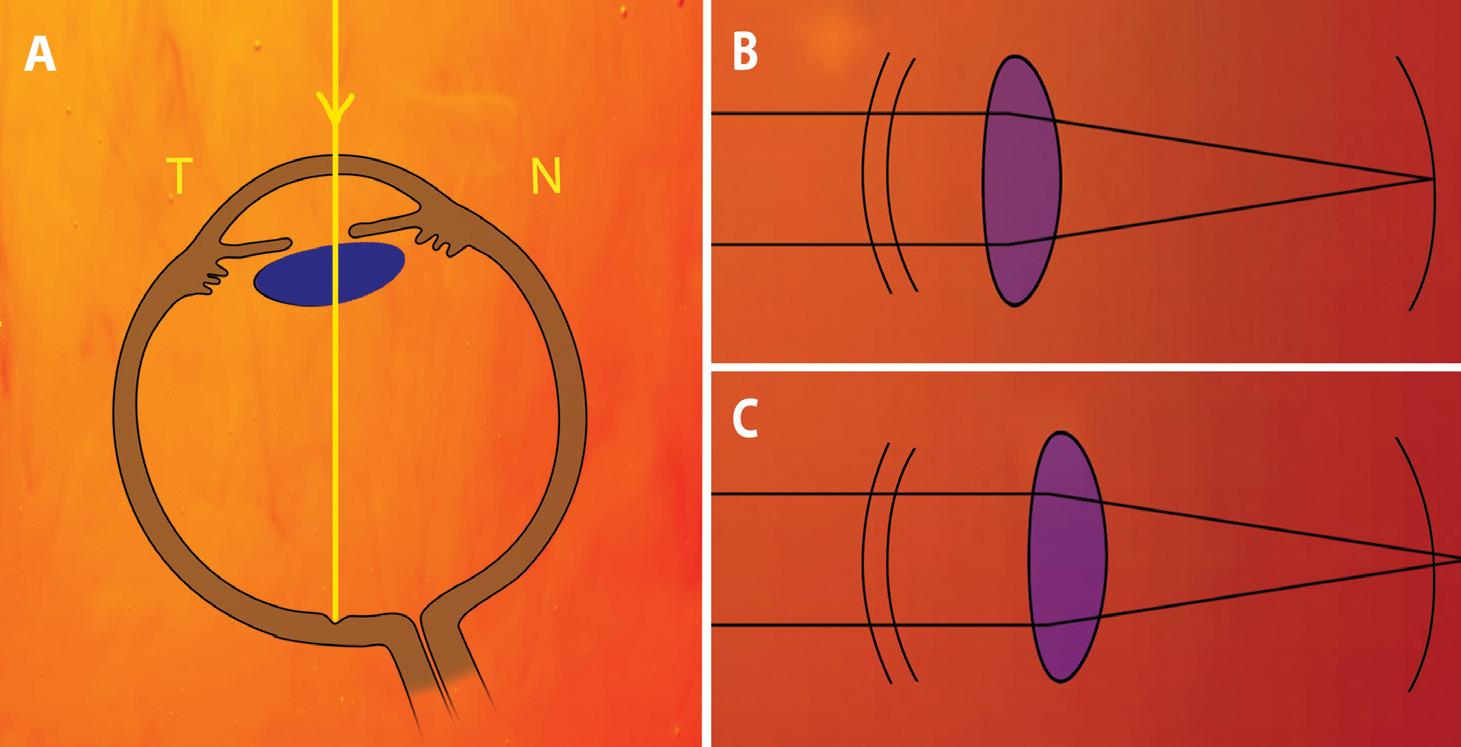
In part one of this series on toric IOL implantation, we read about posterior corneal astigmatism (PCA) and its significance. In this article, we will consider lenticular astigmatism and its relevance in toric IOL implantation.
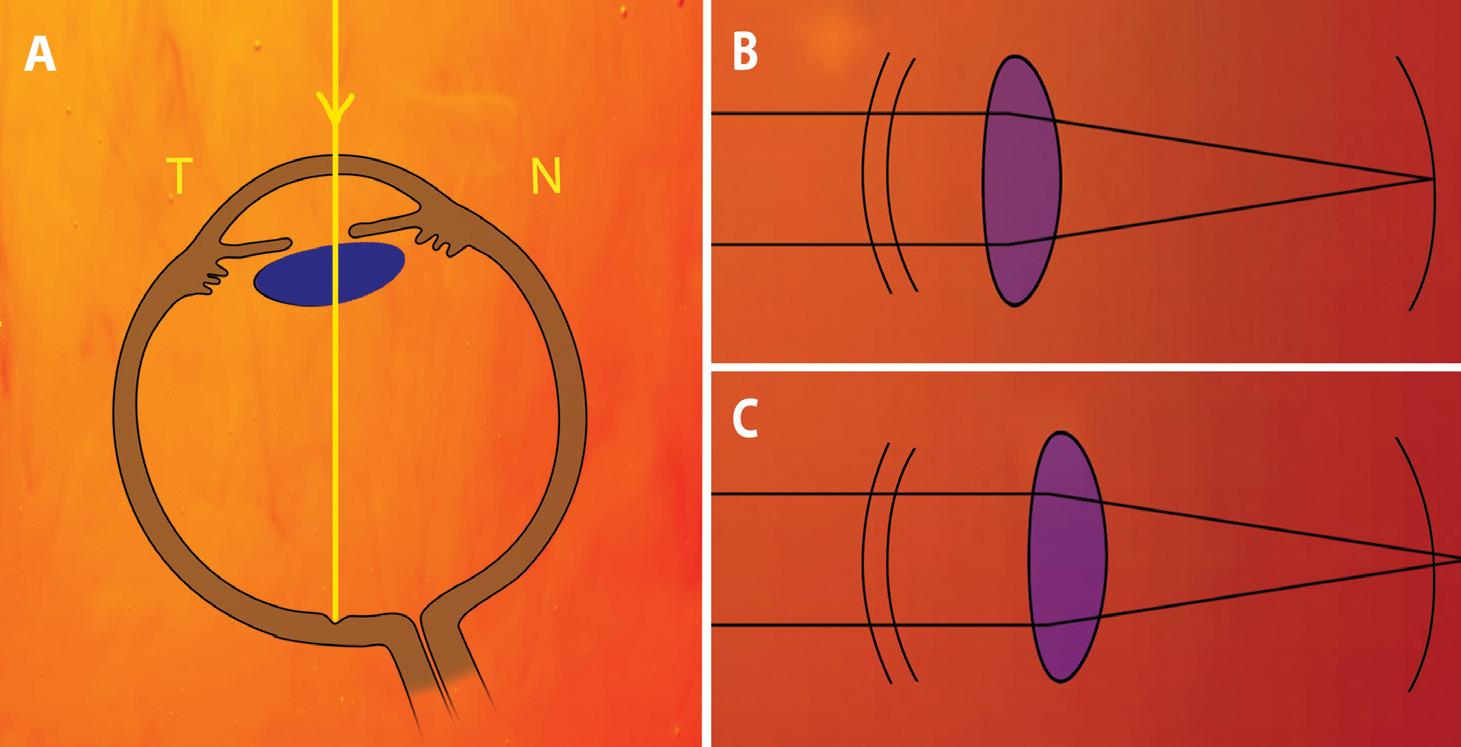
LENTICULAR ASTIGMATISM
In order to place the fovea on the line of sight, our eyes are rotated slightly laterally. This results in the nasal portion of the crystalline lens being positioned more anteriorly than the temporal portion. This lenticular tilt can be assessed using Purkinje reflections, ultrasound biometry, anterior segment OCT, Scheimpflug imaging or swept-source OCT (SS-OCT). SS-OCT biometry has the advantage of whole-eye scanning ability that allows study of lens tilt with relation to the fovea, unlike other techniques, which study lens tilt with relation to iris or pupillary centre.
Using SS-OCT (IOLMaster 700), Hirnschall et al showed that there is an inherent tilt of roughly 5° for the crystalline lens and for in-the-bag IOLs with the nasal aspect rotated anteriorly along the vertical meridian. Using IOLMaster 700, Wang et al also showed a tilt varying preoperatively from 1.1 to 6.7° (average 3.6+/-1.1°) and postoperatively from 0.2 to 9.3° (average 4.8+/-1.6°). They found mirror symmetry in tilt magnitude and direction between the two eyes and a strong correlation between tilt magnitude and angle alpha in
phakic eyes and both angle alpha and angle kappa in pseudophakic eyes.
Tilt magnitude was also found to be negatively correlated with axial length, anterior chamber depth and lens thickness in phakic eyes, and with axial length in pseudophakic eyes. Postoperative IOL tilt magnitude and direction were closely correlated to that of crystalline lens pre-operatively. Preoperative tilt could therefore be used for IOL power calculations, especially in case of toric IOLs to increase accuracy.
EFFECT OF LENS TILT
Lens tilt induces astigmatism, the type and magnitude of which depends on the type and magnitude of tilt as well as the power and type of IOL. The natural horizontal tilt (rotation around the vertical axis) of the lens induces against-the-rule (ATR) astigmatism. Wang et al found that an aspheric IOL of about 28D can cause between 0.14-to-0.56D of ATR astigmatism by tilts between 5 and 10° respectively. These effects are exaggerated in short eyes and eyes with large angle kappa because of greater tilt and higher
IOL power. With secondary IOL fixation, vertical tilt (along the horizontal axis) of large magnitude is also possible.
TORIC IOL AND TILT
Tilt induces astigmatism and reduces the optical quality and performance of a toric IOL. This lenticular astigmatism is likely responsible for overcorrection of eyes with with-the-rule (WTR) corneal astigmatism and under-correction of eyes with ATR corneal astigmatism despite incorporating PCA into calculations. Toric IOLs for WTR astigmatism are aligned vertically and have their higher power aligned horizontally, ie., against-the-rule. A horizontal tilt in this case increases ATR astigmatism and can cause over-correction of WTR. On the other hand, toric IOLs that are aligned horizontally for correcting ATR astigmatism have their higher power aligned vertically, ie with-the-rule.
Horizontal tilt decreases WTR astigmatic effect of the IOL resulting in undercorrection. Putting it simply, a horizontally tilted toric IOL results in over-correction of WTR and under-correction of ATR astigmatism, just as ignoring PCA can result
EUROTIMES | SEPTEMBER 2020
In part two of a series, we look at lenticular astigmatism, effective lens position and their relevance.
Dr Soosan Jacob, MS, FRCS, DNB reports
CATARACT & REFRACTIVE 12
A: The natural horizontal tilt in the crystalline lens induces against-the-rule astigmatism (N-nasal, T-temporal); B,C: The IOL power needs to be higher when ELP is more posterior to allow image focus on retina
Tilt magnitude was also found to be negatively correlated with axial length, anterior chamber depth and lens thickness
in over-correction of WTR and undercorrection of ATR astigmatism. IOL power formulae therefore also need to incorporate IOL tilt predictions to increase accuracy.
The effect of magnitude of toricity depends on alignment of the tilted toric IOL. Weikert et al found that while correcting corneal WTR astigmatism, higher IOL toricities yield greater increases in ATR astigmatism. However, when correcting corneal ATR astigmatism, the reduction in WTR astigmatism correction decreases as IOL toricity increases.
EFFECTIVE LENS POSITION

Effective lens position (ELP) is the distance behind the corneal vertex that an equivalent IOL with no thickness would be positioned. It can influence IOL power calculation and is therefore important to predict preoperatively. As ELP increases, IOL power has to increase to maintain focus of the image on the retina. Similarly, because of the distance between the cornea and the IOL, the cylinder value implanted at the IOL plane is more than the cylinder value to be corrected at the corneal plane. The higher the ELP, the higher this difference and therefore the same IOL, if placed more posteriorly, has less effect at the corneal plane than when placed anteriorly.
The toricity ratio (ratio between the IOL cylinder and corneal cylinder) determines
the final power of the toric IOL to be implanted. Older toric IOL calculators used a standard toricity ratio for all eyes to convert IOL cylinder to corneal cylinder. This led to under-correction in myopic eyes and eyes with larger ELP and over-correction in hyperopic eyes and eyes with shorter ELP. Steeper corneas and eyes with longer axial length require the use of a higher toricity ratio, whereas flatter corneas and shorter eyes need a lower toricity ratio to be used for calculating IOL power. This difference is mainly because of the effective lens position in these eyes, with a more posterior ELP resulting in a higher toricity ratio. Finally, the spherical power of the IOL implanted also has an effect on the ELP with higher power IOLs having a more anterior ELP and low powered IOLs having a more posterior ELP.
Achieving a final IOL position close to the targeted ELP is important to maintain postoperative refractive accuracy. Factors influencing ELP include wound healing, IOL
power, thickness, shape, and the refractive index of the material. The usefulness of femtosecond laser-created rhexis has been debated for achieving the targeted ELP.
Third-generation formulae like SRK/T, HofferQ and Holladay 1 use axial length and corneal power to calculate ELP and IOL power. Though acceptable in the average eye, it leads to errors in short and long eyes. The Barrett toric calculator based on Barrett Universal II predicts PCA and ELP based on a theoretical eye, though recent updates allow input of measured values as well. It uses anterior chamber depth (ACD), axial length, toricity ratio and SIA centroid for its calculations. The Baylor nomogram uses a regression approach based on population averages.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
EUROTIMES | SEPTEMBER 2020 CATARACT & REFRACTIVE 13 VISIT OUR WEBSITE FOR INDIAN DOCTORS
www.eurotimesindia.org INDIA
Steeper corneas and eyes with longer axial length require the use of a higher toricity ratio
Hitting the mark in cataract surgery
Intraoperative tools provide useful guidance in a range of refractive situations. Cheryl Guttman Krader reports
Intraoperative tools for refractive guidance during cataract surgery can enable decision-making, especially in complex cases and for premium cataract surgery cases that demand premium results, said Kendall E Donaldson MD, MS, in a live presentation during the 2020 ASCRS Virtual Annual Meeting.
Dr Donaldson, Professor of Clinical Ophthalmology, Bascom Palmer Eye Institute, University of Miami, Miami, FL, USA, provided an overview of the available intraoperative refractive guidance systems and provided information from the published literature and case examples demonstrating their utility.
Defining intraoperative refractive guidance tools as any type of technology that is designed to assist cataract surgeons to improve refractive outcomes, she described four systems – ORA System with VerifEye+ Technology (Alcon), VERION Image Guided System (Alcon), CALLISTO Eye (Zeiss) and IntelliAxis (Lensar).
The ORA System is comprised of two components: 1) a real-time intraoperative refractometer that uses wavefront aberrometry to assess the refractive power of the eye in the phakic, pseudophakic, or aphakic states; and 2) software that analyses surgeons’ results and helps with outcomes optimisation and reporting (AnalyzOR).
“The intraoperative aberrometer is used for guiding toric IOL alignment and for IOL power selection in complex cases, such as in post-refractive, long or short eyes. It can also be useful in any case where there is discrepancy in the preoperative measurements and for confirming IOL power in patients having premium refractive cataract surgery who in particular have extremely high outcomes expectations,” Dr Donaldson said.
Published data show that use of the intraoperative aberrometer reduces
enhancement rates after cataract surgery and improves refractive results in patients with a history of myopic refractive corneal surgery as well as in unusual eyes, eg, those with axial myopia.
“A study we performed found that the accuracy of toric IOL power selection was improved by the use of the ORA system in patients with significant astigmatism and a history of refractive surgery,” Dr Donaldson said.
Results of a surgeon poll also indicate that the vast majority hold favourable opinions of intraoperative aberrometry. The survey included 50 surgeons who are aware of the technology and implant at least 50 toric IOLs annually. Among those surveyed, 90% said they would want intraoperative aberrometry used in their own surgery if they had a history of a corneal refractive procedure and 80% would want it used if they were being implanted with a toric IOL.
Callisto Eye is part of a technology suite with functions that include markerless guidance for toric IOL alignment. Published evidence show that its use increases the safety and consistency for toric IOL marking. Studies also show it is very accurate and very efficient, Dr Donaldson reported.
The VERION Image Guided System uses the VERION reference unit to capture a high-resolution digital image of the eye that is used intraoperatively to guide precise positioning of femtosecond laser-created incisions and toric IOL alignment.
As a feature of the LENSAR femtosecond laser, IntelliAxis is a method for making permanent capsular marks on the steep axis that can be used for guiding toric IOL alignment intraoperatively and checking alignment postoperatively.
Dr Donaldson presented two cases that illustrated the use and benefits of intraoperative refractive guidance technology.
One case involved a 68-year-old man with a history of multiple corneal refractive procedures. He presented with 4D of astigmatism OD and 1D OS. Keratometry measurements obtained with multiple instruments showed poor agreement. Using the different measurements to calculate IOL power led to results that varied by 3.0D OD and 1.5D OS. The patient was implanted bilaterally with a monofocal IOL using the power determined with intraoperative aberrometry that fell within the suggested range. He achieved 20/20 UCDVA bilaterally, and his UCNVA was J1 OD and J2 OS.
“In cases where I am unsure, I try to err on the side of the higher-power IOL that potentially would leave the patient with a little myopia. In this case, however, I followed the guidance from the intraoperative aberrometer, and the patient did extremely well,” she said.
The second case was a 62-year-old man with early cataracts and 1.5D of againstthe-rule astigmatism OU. He presented requesting a LASIK evaluation because of blurry vision but was recommended to undergo clear lens extraction because he wanted presbyopia correction.
In this case as well, the keratometry measurements did not agree. The calculated IOL powers varied across a 1.0D range. With power selection guided again by the intraoperative aberrometer, Dr Donaldson implanted a diffractive multifocal toric IOL in both eyes. The patient achieved 20/20 UCDVA at distance and J1+ UCNVA in both eyes.
Dr Donaldson ended her discussion with the following caveat about the benefit of the intraoperative guidance tools.
“Technology has really allowed us to be our best as cataract surgeons and to improve our refractive accuracy. Outcomes, however, depend on getting accurate preoperative measurements,” Dr Donaldson said.Providing a future perspective, she added: “The field is rapidly evolving with increased availability of adjustable IOLs and refractive indexing. We have a very exciting time ahead.”
Kendall E Donaldson: KDonaldson@med.miami.edu
EUROTIMES |SEPTEMBER 2020 CATARACT & REFRACTIVE
14
The intraoperative aberrometer is used for guiding toric IOL alignment and for IOL power selection in complex cases
Kendall E Donaldson MD, MS


Do androids dream of the perfect rhexis?
In her shortlisted essay for the 2020 John Henahan Prize, Dr Claudette Veldhuizen looks to the past to imagine the future of robots in cataract surgery
Will cataract surgeons be rendered obsolete by the cold, detached, digital arms of robots? Those who attended the ‘Artificial Intelligence in Ophthalmology’ symposium during the 2019 ESCRS congress in Paris may agree. In some ways, the writing is on the wall: artificial intelligence and robotics seem to be taking over not only in terms of cataract surgery, but ophthalmology, and medicine in general. After all, ophthalmology is an image technology-based specialty. Other image-based fields like radiology and pathology have seen an even faster machine takeover. But are robots creeping their way into the cataract surgeon’s operating room? And perhaps even more importantly: should cataract surgeons, and future cataract surgeons, fear being made redundant, or maybe even worse, irrelevant?
Here’s a synopsis of the promises on offer: the developers of microsurgical smart tools are working to steady the surgeon’s hand to a tenth of the human tremor, enabling even the most experienced surgeons to benefit from this technology. Co-manipulation and tele-manipulation allow for human-directed robotic movements into hard-to-reach places with a superhuman range of motion and a far greater accuracy than humanly possible. Also, unlike people, robots don’t get tired or bored – meaning that repetitive tasks become a breeze. In all likelihood, so long as these fields continue to improve, then the stage is indeed set for the future of cataract surgery to move into the realm of robotics. And one can imagine that as with many technological innovations, with time, the technology will become safer and cheaper – and perhaps inevitably, as ubiquitous as the laptop, or in our case, the slit lamp.
But is automation per se something to be
feared? I would say, not necessarily. Allow me to explain by use of what I believe is the best predictor of the future: the past. Every aspect of civilisation has undergone some form of automation, which includes every human endeavour, from cosmology to agriculture. This pursuit forward has made neither the farmer, nor the cosmologist irrelevant. One could even go so far as to say that in the case of farming, domestication of plants and animals approximately 11,000 years ago directly led to a sharp population growth, which, in turn, only made the farmer even more relevant. New technology means new problems, as well as opportunities for reinvention.
More recently, dairy cattle farmers have begun to rely on automated milking by way of robotic arm laser sensors. This move has effectively freed farmers of the traditional rigid grind that manual milking entails, allowing more time for other activities, like supervision. But the farmer isn’t the only winner in this scenario, as more frequent milking also happens to mean happier cows.1 Ophthalmology of course has its own rigid grind – one need only to consider the hundreds of thousands of OCT scans pumped out each year by ophthalmology clinics worldwide. But can we say the same for cataract surgery? Some would certainly say yes, and if not for the whole procedure, at least in part. Femtosecond laser technology already allows for semiautomation, including capsulorhexis and fragmentation. Now pair this with robotic arm laser sensors for automated docking and voilà, we have the idea behind the French-developed KERANOVA. This technology allows for nearly fully automated ‘photoemulsification’ with 80% of the procedure performed sans human interference.2,3 And cataract surgery isn’t alone: the first successful robotic intraocular vitreoretinal surgery has already
taken place using the Dutch-developed PRECEYES surgical system.4 In both these examples, the technologies augment and support the abilities of the surgeon. The makers of the PRECEYES even hint that a possible consequence may inadvertently be the extension of the career of the surgeon…
However, before we talk any more about the future of cataract surgery, let’s look at the past of cataract surgery: Maharshi Sushruta first described couching as a visual rehabilitation technique in approximately 800BC. If we imagine him being able to time travel over 28 centuries to view how we perform modern phacoemulsification surgery today, he may of course be hesitant, but I imagine that he would attempt to understand and ultimately, embrace our technology – especially given the increased patient safety and precision. We may even slightly smugly envision that he would at least be a little impressed. Cognizant of how far we have come, let’s reconsider the potential grandness of the future of cataract surgery. Perfectionism is a common trait amongst cataract surgeons. Hopefully this drive to create not only visual rehabilitation, but visual performance for our patients, should keep us in good stead, come what may.
To conclude, fear, which often manifests as hesitance or reluctance, is hardwired through years of evolution, and is not always without merit. However, perhaps we should aim to translocate and transform it, using it to energise a deep reflection on the profound aspects of cataract surgery that cannot be replaced by robots: the human touch. Robotics and artificial intelligence may promise to open doors and free up our time to further improve our understanding and expertise. However, lest we forget that a gentle touch of the arm of a scared patient lying in the preoperative holding area awaiting surgery, asking with genuine interest if a patient is still doing alright during the procedure, these cannot be replaced.
Dr Claudette Veldhuizen MD is a PhD candidate at the University Eye Clinic Maastricht; her research focuses primarily on cystoid macular oedema after cataract surgery.
EUROTIMES | SEPTEMBER 2020
CATARACT & REFRACTIVE 16
Also, unlike people, robots don’t get tired or bored – meaning that repetitive tasks become a breeze
Late LASIK flap study
No need to flap over late LASIK enhancements. Dermot McGrath reports
Lifting a LASIK flap for refractive enhancement five or 10 years after the initial procedure can be safely and successfully achieved, according to Jorge Alió del Barrio MD, PhD, FEBOS-CR.
“Our study showed that flap lift for refractive enhancement up to 10 years or more after LASIK is a feasible surgical alternative, which provides good efficacy and safety with fast visual recovery. The rate of surgical intervention for significant postoperative epithelial ingrowth (EI) was low as far as early EI is properly managed with YAG laser as previously described by our group,” Dr Alió del Barrio told delegates attending the 37th Congress of the ESCRS in Paris.
Late residual refractive errors, years after the initial LASIK procedure, are a common problem faced by refractive surgeons, noted Dr Alió del Barrio, a surgeon at the Cornea, Cataract and Refractive Surgery Unit, Vissum Corporación, Alicante, Spain.
“Studies have shown that there is about a 10-year re-treatment rate of 20.8% for myopia up to -10D, and after hyperopic LASIK, a progressive increase in hyperopia from the original LASIK has also been reported up to 16 years postoperatively,” he said.
The two main options to treat refractive errors in these patients are either PRK over the flap, or a flap re-lift followed by refractive enhancement.The advantages of a late LASIK flap lift include fast visual recovery, no postoperative pain and no risk of haze, said Dr Alió del Barrio. The disadvantages of this approach are similar to the original LASIK procedure that are primarily flap related – folds, interface debris and the most important one is the risk of EI at the flap interface.

“It has been shown that the risk of epithelial ingrowth increases over time from the primary LASIK procedure, which helps to explain why the currently available literature discourages refractive surgeons from lifting LASIK flaps older than three years,” he said.
Dr Alió del Barrio’s study included 70 eyes of 48 patients. The primary LASIK procedure was myopic in 45 eyes, hyperopic in 22 eyes and presbyopic in three eyes. The flap was dissected using a
mechanical microkeratome in 62 eyes (89%) and a femtosecond laser in the remaining eight eyes (11%).
The mean time from primary LASIK to the flap lift was 12.3 years. In 57 eyes, the primary LASIK flap was created at least 10 years before the enhancement. The mean pre-lift spherical equivalent was −1.29D in the myopia group and +0.65D in the hyperopia group.
Three months after the surgery, 88% of myopic eyes and 74% of hyperopic eyes had an uncorrected distance visual acuity of 20/20 or better and all patients achieved at least 20/25. No eye lost two lines or more of corrected distance visual acuity.
Mild EI developed in 31% of eyes (not requiring any intervention) and clinically significant EI in 11% of eyes, with only 4% of eyes requiring a re-lift for severe EI. As far as progressive or moderate EI is early diagnosed and treated with YAG laser, the risk for severe EI requiring a new flap lift for interface cleaning is marginal.

“Clinically relevant epithelial ingrowth is not an exceptional complication after late flap re-lift. However, an adequate noninvasive management with YAG laser minimises the risk of requiring surgical re-intervention, being an acceptable risk for both the surgeon and the patient,” he said.
Jorge_alio@hotmail.com
EUROTIMES | SEPTEMBER 2020 CATARACT & REFRACTIVE 17
Studies have shown that there is about a 10-year re-treatment rate of 20.8% for myopia up to -10D, and after hyperopic LASIK...
Jorge Alió del Barrio MD, PhD, FEBOS-CR
Moderate and progressive grade II epithelial ingrowth that requires treatment with YAG laser to solve the problem and avoid further progression. No need for surgical intervention if YAG laser is used for such cases
...An adequate non-invasive management with YAG laser minimises the risk of requiring surgical re-intervention
Jorge Alió del Barrio MD, PhD, FEBOS-CR
Courtesy of Jorge Alió del Barrio MD, PhD
A humble servant
That’s excellent…”, whispered my consultant. My heart sank as I stared at a large posterior capsule hole. Hands trembling, I hastily injected visco with the old adage “visco is cheaper than vitreous” playing on my mind. The case proceeded uneventfully as I held my breath and watched an experienced pair of hands go to work, steady and unperturbed by the aftermath I have created.
Yet another complication added to the logbook. I was disheartened. But I realised I needed more practice. Focused and determined, I spent every free moment I had for the rest of the week on the department’s Eyesi simulator. Consumed by the drive to improve, I practiced each step over and over with deliberation and purpose on this unwavering and forgiving machine.
Slowly but surely, I became more adept and competency gradually came within grasp. But as hard as I worked and as much as I would like to claim sole credit for this achievement, I did not get here by myself. Unbeknownst to me, robotassisted learning, albeit a rudimentary version, helped pave the ascent up the steep learning curve of cataract surgery. Through virtual simulation, I was able to refine my techniques in an unparalleled manner. However, like many others, I realised how I have taken this important privilege for granted in the pursuit of surgical excellence.
In an accelerating world, it is easy to lose sight of how technology has become intertwined with almost every aspect of contemporary life. Cataract surgery is no exception. We heavily rely on modern day phacoemulsification machines with advanced technology that most of us are benignly oblivious to.
Over the 50 years of its existence,
phacoemulsification has undergone countless incremental upgrades culminating in an intelligent, automated system that now self-adapts to changing conditions within the eye. As much as this is a display of human ingenuity, it is important to recognise the reciprocal relationship between us and our machines. Like a rider on a horse, both elements engage in a continuous cycle of flexibility and reconfigurability, learning from and supporting each other.
The dawn of automation, robotics and artificial intelligence is upon us. Although the adoption of surgical robotic systems into ophthalmology has trailed behind other surgical specialties, this landscape is rapidly changing. The concept of robot-assisted cataract surgery has been gaining unprecedented momentum since it was first explored using the da Vinci Xi surgical system in 2017. As more and more manufacturers join the expanding robotic bandwagon, we can look forward to a rapid development and proliferation of novel robotic systems that will continue to expand the realm of possibility in cataract surgery.
WORKING IN SYNERGY
Despite its promising potential, there are challenges ahead for robotic cataract surgery: How do we ensure that we bestow the best of qualities of a master cataract surgeon on our robots? And how do we nurture our robots to understand our instincts? In our ongoing endeavour to increase automation of surgical robots, we must not overlook the importance of symbiosis – not either surgeons or robots, but surgeons and robots working in synergy for the ultimate benefit of our patients.
With a new normal racing in after COVID-19, there will be a new impetus for robots to power change in the
pandemic’s wake. This adversity has revealed the vulnerabilities of our healthcare systems but at the same time inspired us to innovate and accelerate the pace of robotic revolution in surgery.
PERSONAL AI ASSISTANT
It is the year 2050. I wake up and get ready for my cataract list in the comfort on my living room. While I brush my teeth, my personal AI assistant consents the first patient and sets up my personal settings on the latest “photo”emulsification robot. I don my virtual headset and haptic gloves as the coffee brews in the background. I get down to business in no time. With just a few taps, I seamlessly optimise the photoemulsification parameters on my index finger which now houses the entire surgical machinery…
Given the limitless possibilities of robotics, it is perhaps not too farfetched to envisage such a future where robotic telesurgery coupled with an armamentarium of novel cataract removal techniques becomes our next reality. As we leap forward, we would do well to take a look back and remember the struggles of the likes of Sir Harold Ridley and Charles Kelman who believed and persevered with what seemed impossible in their times. Regardless of what the future holds, one thing is certain: the robotic approach will continue to grow and it will be up to us embrace it for all it has to teach us.
EUROTIMES | SEPTEMBER 2020
In his shortlisted essay for the 2020 John Henahan Prize, Dr Peng Sim explains how he sees humans and technology working together like a rider on a horse
CATARACT & REFRACTIVE 18
Dr Peng Sim is a second-year ophthalmology trainee at the Royal Free Hospital in London, UK
I hastily injected visco with the old adage “visco is cheaper than vitreous” playing on my mind
The dawn of automation, robotics and artificial intelligence is upon us
Dr Peng Sim
DMEK plus cataract surgery

In theory, combining Descemet membrane endothelial keratoplasty (DMEK) with cataract surgery should produce similar refractive results to cataract surgery alone because the graft does not change keratometry. In practice, however, a hyperopic shift frequently accompanies combined DMEK-cataract procedures.
Compensating for this shift when calculating intraocular lens power calculations may further improve refractive precision and outcomes, which are already substantially better than with the traditional penetrating keratoplasty triple procedure, Guillaume Boutillier MD of Rouen University Hospital, France, told the 37th Congress of the ESCRS in Paris.
In a retrospective, descriptive study of 133 Fuchs’ dystrophy patients undergoing combined DMEK-cataract procedures at four French centres, Dr Boutillier found the mean difference between target and post-surgical refractions was +1.21 dioptres at two months, and +1.12 dioptres at six months. Because many procedures targeted slight myopia, this left patients with a mean uncorrected refractive outcome of +0.72±1.0D. Still, corrected outcomes improved substantially from a mean 0.49±0.3 log MAR, or about 20/63, preoperatively to 0.14±0.14, or about 20/30, at two months and 0.05±0.1, or just shy of 20/20, at six months.
These results are similar to other studies of DMEK-cataract combined procedures, which report mean refractive errors after surgery ranging from +0.43D to +0.9D, Dr Boutillier said (Laaser K et al. Am J Ophthalmol. 2012;154:47-55. Schoenberg ED et al. J Refract Surg. 2015;41:1182-9. Girbardt et al. Ophthalmal Z Dtsch Ophthalmol Ges. 2016;113:213-6).
But he believes it is possible to do better.
“We need to use compensation means to avoid this refractive error.”
COMPENSATING STRATEGIES
Dr Boutillier suggested several strategies to compensate for this hyperopic shift that could further improve refractive precision. The simplest may be to adjust the target refraction to the myopic side by an amount similar to the anticipated hyperopic shift.
Adjusting keratometry may be another approach. One study found that subtracting 1.19D on both axes produced an average final error of -0.23D in combined Descemet stripping automated endothelial keratoplasty (DSAEK)-cataract procedures (de Sanctis U et al. Am J Ophthalmol. 2013 Aug;156(2):254-259).
Similarly, optimising the manufacturer’s A constant for DSAEK-cataract combined procedures significantly improved IOL power predictive accuracy, from a mean absolute error of 1.09±0.63D to 0.61±0.4D (Bonfadini G et al. Ophthalmology 2013 Feb;120(2):234-9). A similar adjustment might be made for DMEK combined procedures, Dr Boutillier said.
DMEK-cataract is a safe and effective technique for treatment of Fuchs’ dystrophy associated with cataract, Dr Boutillier concluded. But frequent hyperopic shifts occur that must be compensated for to achieve the goal of emmetropia. This hypermetropic shift is almost constant but with variable values. It would be interesting to understand which parameters are responsible for this shift and therefore which patients are most at risk of postoperative refractive error, Dr Boutillier added.
EUROTIMES | SEPTEMBER 2020 CATARACT & REFRACTIVE
Compensating for hyperopic shift may further improve refractive outcomes. Howard Larkin reports
19
Join Track
the EUREQUO Platform your Surgical Results
Practice patterns across Europe
EUREQUO finds younger patients, better cataract outcomes over past decade. Howard Larkin
reports
Over the decade ending in 2017, European cataract patients on average grew younger, had better preoperative visual acuity, and better visual and refractive outcomes with fewer complications, according to a study based on data from the European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO). Use of topical anaesthesia and hydrophobic acrylic intraocular lenses also increased, Sonia Manning MD told a session of the 37th Congress of the ESCRS in Paris in September 2019.
Convenient Web-Based Registry Cataract, Refractive and Patient Reported Outcomes in One Platform
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
Based on records from 2,714,108 cataract cases performed in 17 European countries from 2008 through 2017, the study found that mean age at surgery decreased continuously year-over-year from 74.5 years to 73.0. Mean preoperative visual acuity also improved from 0.46 log MAR to 0.37 log MAR, or from about 20/60 to about 20/45. The percentage of patients without ocular co-morbidities also increased from 70.0% to 73.0%, which is consistent with a decline in the percentage of anticipated difficult surgeries from 12.6% to 10.6%.
ANAESTHESIA
Based on records from 1,522,576 surgeries, use of topical anaesthesia skyrocketed from 28.1% in 2008 and then levelled off at just over 70% in 2015 to 2017. At the same time retrobulbar anaesthesia dropped from 24.7% to under 10% in 2013 to 2017. Subtenon, intracameral and peribulbar anaesthesia also dropped continuously while general anaesthesia use remained steady at about 2.5% of cases.
Phacoemulsification remained by far the most popular cataract extraction choice, holding steady at about 99% of cases in Europe for the entire period. Acrylic hydrophobic lenses gained, moving from about 79% in 2008 to about 90% in 2015 to 2017. Hydrophilic acrylic dropped from about 14% to about 10% while silicone lenses fell from 5.8% to zero in 2015. The use of multifocal and toric IOLs was low in this database, Dr Manning reported.
COMPLICATIONS
EUREQUO is free of charge for all ESCRS members
www.eurequo.org
Based on records from 1,129,944 cases, capsule complications dropped from 1.44% to 0.66%. Iris damage and dropped nuclei were low and dropped by about half. Postoperative complications varied considerably year to year but ended the study period where they started at 1.88%. Central corneal oedema was most common and increased, followed by uveitis, uncontrolled intraocular pressure and endophthalmitis.
The percentage of patients within 0.5 dioptre of target refraction rose steadily from 66.9% to 73.4%, while those within 1.0 dioptre increased from 89.6% to 93.6%. Patients reaching post-op corrected-distance visual acuity of at least 0.0 log MAR, or 20/20, jumped from 58.3% to 75%.
Dr Manning ended up by thanking all surgeons contributing to the EUREQUO database.
Sonia Manning: sonia.sofia1@gmail.com
EUROTIMES | SEPTEMBER 2020 CATARACT & REFRACTIVE
20
THOMAS KOHNEN European Editor of JCRS


JCRS HIGHLIGHTS


VOL: 45 ISSUE: 6 MONTH: JUNE 2020



MILD MYOPIC TARGET BOOSTS INTERMEDIATE VISION
Bilateral monofocal IOLs implanted with mild myopic targeting produce good intermediate vision while avoiding the problems associated with multifocal IOLs or monovision surgery, a new study suggests. The prospective study implanted one group of 30 patients with bilateral monofocal IOLs targeting plano to -0.25D and a second group targeted for -0.50D. Post-op defocus curve analysis showed a significant difference between Group 1 (emmetropia) and Group 2 (mild myopia) binocular vision, with Group 1 seeing significantly better than Group 2 at +1.00, +0.50 and 0, but significantly worse in all other points of the defocus. Patients in Group 2 at 0D of defocus curve (infinite) had a visual acuity close to 0 logarithm of the minimum angle of resolution (logMAR). The main outcome of Group 2 defocus curves was that, at defocus point 0D, even if the mean refraction was -0.67 0.15 × 160, mean uncorrected logMAR visual acuity was 0.0 ± 0.06. Broader optimisation of the target with patient-based formulas might be able to further improve outcomes, the researchers note.
P Vinciguerra et al., “Comparison of visual performance and satisfaction with a bilateral emmetropic vs a bilateral mild myopic target using a spherical monofocal intraocular lens”, Volume 46, #6, 839-843.











ORA INTRAOPERATIVE ABERROMETRY
While intraoperative aberrometry has produced promising results in astigmatism correction in post-corneal refractive patients, its role in less complicated cases is still being debated. A large retrospective study compared the outcomes of an intraoperative aberrometer (ORA) to the Barrett Universal II (Barrett II) and Hill-RBF 2.0 (Hill-RBF) intraocular lens (IOL) power calculation formulas in eyes without history of previous corneal refractive surgery. All three methods performed well regarding spherical equivalent predictive ability. However, supplementing preoperative formulas with intraoperative aberrometry did not improve refractive outcomes. R Nikolas et al. “Intraoperative aberrometry vs modern preoperative formulas in predicting intraocular lens power”, Volume 46, #6, 857-861.
CUSTOMISED IRIS PROSTHESIS
Photophobia and glare are common problems in patients with congenital aniridia. A custom-made, flexible iris prosthesis appears to reduce these photic symptoms in congenital aniridia, a study of 50 patients (96 eyes) concludes. The custom-made prosthetic iris device greatly reduced the photic symptoms, with subjective reduction in photophobia and glare reported in 95.7% and 95.2% of cases, respectively. Implantation of the custom-made prosthetic iris device did not increase the risk for aniridia fibrosis syndrome. Intraoperative complications occurred in 14 eyes (14.6%), including 12 anterior capsule breaks and two posterior capsule breaks. The custom, flexible iris device was well tolerated in congenital aniridic eyes. GB Figueiredo et al., “Long-term follow-up of a custom-made prosthetic iris device in patients with congenital aniridia” Volume 46, #6, 879-887.
EUROTIMES | SEPTEMBER 2020
CATARACT & REFRACTIVE JCRS is the official journal of ESCRS and ASCRS 21
Relaxing the patient
Relaxing a patient who is undergoing surgery reduces their stress and that of the surgeon and can be best achieved with a coherent and consistent team-based approach, said Andrew Presland FRSA, PhD, at the 37th Congress of the ESCRS.
“My hypothesis is that a relaxed, comfortable patient, tended by caring professional colleagues and surrounded by an experienced familiar team, results in a relaxed surgeon,” said Dr Presland, of Moorfields Eye Hospital, London, UK.
Relaxing the patient ideally begins before the day of surgery, he noted. Patients should receive succinct information, free of jargon, on what to expect in their surgical experience. Consideration must also be taken of language barriers. The surgical team needs to have a common understanding of the objectives and limitations.
“Expectation management is the single most important concept. Getting this wrong – at any stage – sows the seeds of dissatisfaction,” Dr Presland said.
Expectation management is relevant to general anaesthesia but more relevant to local anaesthesia. The local anaesthetic should be sufficient on its own for the patient’s comfort, as sedation and deep breathing is a poor substitute. Patients must also understand what is and what is not normal light touch and pressure.
During surgery it is best to avoid medical terms, he said. For example, instead of saying “I’m going to put a speculum in your eye”, perhaps say “I’m going to place a clip to keep your eyelid where I need it”, Dr Presland suggested.
Reassurance measures such as hand-holding can help relax the patient, as can ambient music. Patients with experience with selfhypnosis, progressive muscle relaxation and mindfulness techniques can also use those approaches to achieve further relaxation.
He added that the person administering sedation needs to consider such factors as the length of the procedure and the invasiveness of the procedure. In addition, one practitioner should be dedicated to monitoring the patient both during and after surgery. Dr Presland stressed that an over-sedated patient is much more difficult to deal with in a surgical situation and requires postoperative recovery facilities.
“Expectation management is absolutely key. You have to tailor your approach to the patient and the circumstances that you find yourself working in. Fostering a team approach that is coherent and consistent is going to achieve success,” Dr Presland summarised.
Andrew Presland: a.presland@nhs.net


What about my future?
OCULUS Myopia Master ®


For early myopia detectio n and management
Myopia in children and young people is increasing worldwide. Early detection and treatment can slow or stop the progression of myopia. The new Myopia Master® combines all important parameters for myopia management in a myopia analysis software.

A relaxed patient means a more relaxed surgery. Roibeard Ó hÉineacháin reports
EUROTIMES | SEPTEMBER 2020 CATARACT & REFRACTIVE 22
www.myopia-master.com Follow us! Eurotimes Myopia Master International Max 178x130 e 07.20 v3.indd 1 27.07.2020 16:23:58






2-4 October 2020 38th Congress of the ESCRS Online. Interactive. Live from Amsterdam. Programme Preview

Belong to something unique. Join us. Don’t go unnoticed. Visit www.escrs.org for information about membership & benefits
VIRTUAL CONGRESS will broadcast live from Amsterdam
2020 has been a year like no other with the international medical community facing an unprecedented crisis following the outbreak of the COVID-19 pandemic.
Some ESCRS members have been on the front line of the battle against COVID, joining their colleagues in emergency departments to treat seriously ill patients suffering from the virus.
Professor Rudy MMA Nuijts, President of ESCRS said “From the very start of the pandemic it was clear that ESCRS had a commitment to give the ophthalmology community every support in dealing with the New Normal.”
CUTTING-EDGE RESEARCH
Professor Nuijts pointed out that the ESCRS, even in difficult times, must continue to promote cutting-edge science and research that has made the Society a major force for change not only in Europe but in the rest of the world.
For ophthalmologists worldwide, the annual Congress of the ESCRS Congress is a hugely valuable educational resource. “In early May it became obvious to the leadership that ESCRS would have to host its annual Congress on a virtual platform from 2-4 October, 2020.” Professor Nuijts said.
Although the programme has been shortened from five to three days, Prof Nuijts believes that this year’s Congress will be remembered, not only because it is taking place against the backdrop of the COVID pandemic but also because the virtual meeting will open up exciting new networking opportunities for delegates. The virtual Congress will be accessible to many ophthalmologists worldwide who for different reasons have never travelled to an ESCRS Congress.

SPEAKERS BROADCASTING LIVE FROM AMSTERDAM
“All of the main session speakers will gather in Amsterdam and will broadcast live from there. A high level of discussion and debate is assured, and we expect our virtual attendees to contribute through dynamic question and answer facilities, polling and more. The personal connections that are so valuable to
our attendees will remain,” he said.
“I am very much looking forward to this year’s Ridley Medal Lecture from David Chang and Heritage Lecture from Theo Seiler,” said Prof Nuijts. “Registered delegates will also have exclusive access to all the presentations until the end of 2020 on the virtual meeting platform.
“Our industry partners are also lending their full support. They will be hosting a virtual exhibit hall as well as a full programme of Industry sponsored satellite symposia from an opening at 10.00 am on Friday 4 October,” said Prof Nuijts.
In conclusion, Prof Nuijts said that while he very much looks forward to meeting colleagues again face to face in 2021, he is confident that with the assistance of modern technology the 2020 Virtual Congress will be a dynamic and interactive educational experience for the ESCRS community.”
EUROTIMES | SEPTEMBER 2020 25 VIRTUAL MEETING PREVIEW
The personal connections that are so valuable to our attendees will remain
Professor Rudy MMA Nuijts
The greatest team
David F. Chang, MD, Clinical Professor, University of California, San Francisco, will deliver the Ridley Medal Lecture at the 38th Congress of the ESCRS

It is a tremendous privilege to be presenting the Ridley lecture this year. Although this is one of the greatest individual honours that I’ve ever received, I wanted to use my lecture to highlight what I consider to be the greatest team of cataract surgeons – those at the Aravind Eye Care System in Southern India – and some of the most important lessons that they’ve taught us during the last two decades.
Aravind is a network of more than 10 regional centres with six main large hospitals. My collaboration with their cataract surgeons started with my first visit there in 2003. They have become the global model for reducing the backlog of cataract blindness in underserved societies, by using revenue from paying patients to subsidise cataract surgery at little or no cost to the indigent (which accounts for 60% of their total surgical volume). This is the first and most important lesson – that we can use this type of cost-recovery model to reduce and eventually eliminate global cataract blindness.
At the centre of their approach is the use of sutureless, manual, small-incision cataract surgery (MSICS). This is an extracapsular procedure where an undivided nucleus can be manually extracted through a funnel-shaped 8mm scleral tunnel incision that does not require suturing. A non-foldable PMMA IOL, costing less than $5.00 USD, is implanted through this incision. To restore vision to as many indigent cataract patients as possible, surgery is performed in an assembly line fashion to maximise efficiency, while minimising cost, and yet maintaining high-quality outcomes.
Compared to MSICS, phacoemulsification is much more expensive in terms of capital investment, maintenance and repair, and consumables per case. Furthermore, we showed in a study at the Madurai Aravind hospital that the complication rate was much higher with phaco than MSICS when the surgeon has less experience. In addition, indigent populations have a huge burden of ultra-brunescent and mature cataracts, which increases the risk of complications with phaco. Therefore in eyes with very advanced and complicated cataracts, MSICS would probably be safer than phaco for many surgeons. In fact, I use MSICS in my own practice for the most advanced cataracts that I encounter in the United States.
Another important innovation of the Aravind group is that they found a way of putting a square edge on to PMMA lenses at a cost of $1 USD. Posterior capsule opacification (PCO) is an inconvenience for patients in the West since it can be easily treated with a YAG-laser capsulotomy. However, for patients living in rural areas in developing countries, limited healthcare access makes PCO one of the leading causes of visual impairment. We performed a nineyear, long-term study that showed that when patients underwent implantation of a squareedged PMMA IOL in one eye and a round-
edged PMMA IOL in the other, the eye with the square-edged lens had dramatically less PCO compared to the fellow eye. Aravind is one of the largest suppliers of IOLs for developing countries, and as a result of this study, all of their PMMA IOLs now have a square edge – which is lesson #3.
A fourth compelling lesson from Aravind is that intracameral moxifloxacin is safe and effective for endophthalmitis prophylaxis. ESCRS sponsored a landmark study with intracameral cefuroxime but vancomycin was the most commonly used antibiotic for intraocular prophylaxis in the US, until it was determined to be the cause of HORV. We authored the largest, single-institution study of intracameral antibiotic prophylaxis, comparing the endophthalmitis rates with and without intracameral moxifloxacin in two million consecutive cataract surgeries at Aravind. The endophthalmitis rate dropped from 0.07% in those who didn’t receive moxifloxacin compared to only 0.02% among those who did. Lacking a large randomised trial, this type of big data registry study offers the best available evidence in my opinion.
The last compelling lesson is that our innumerable operating room regulations in the West mandating single-use of most of our supplies, pharmaceuticals, and devices may be of unproven benefit in reducing infection rates. In addition, they add significantly to the cost and carbon footprint of cataract surgery. Studies carried out of Aravind have shown that their carbon footprint for one phaco is 20 times lower than for one phaco in the UK. That is largely because Aravind re-uses devices, pharmaceuticals and supplies such as irrigating solution, IA tubing, metal blades and cannulas, and they don’t change gowns or gloves between cases. Their robust electronic data registry allows them to continually monitor their infection rates and outcomes and they have learned that re-using these supplies and devices does not affect the outcome. After adopting intraocular moxifloxacin routinely, their endophthalmitis rate is actually lower than that of the AAO IRIS registry (0.04%), but of course intraocular antibiotic prophylaxis is not used by many Americans due to lack of a commercially approved product.
David Chang was interviewed by Roibeard O’hEineachain, Contributing Editor, EuroTimes
EUROTIMES | SEPTEMBER 2020 26 VIRTUAL MEETING PREVIEW
I wanted to use my lecture to highlight what I consider to be the greatest team of cataract surgeons – those at the Aravind Eye Care System in Southern India
Clinical research
Congress
Clinical research is the future of ophthalmology. This year’s ESCRS Clinical Research Symposia, to be held 3 October live from the ESCRS Virtual Congress 2020, highlight four current areas of vital advances.
“The programme is mainly researchbased, to address what’s new, what is coming in the future, what is not implemented yet, or implemented only in a few clinics to make it more widely known,” said ESCRS Research Committee Chair Jesper Hjortdal MD, PhD, DMSc. Currently, the plan is for presenters to meet in person in Amsterdam, though circumstances may require some presenters to appear remotely.
Delegates will participate virtually – but not impersonally. All attendees will be able to ask questions online in real time, and each of the four symposia will be followed by a 30-minute interactive discussion including audience questions. “It may attract even more attendees because people do not have to fly in and pay for hotels,” said Dr Hjortdal, who is also clinical professor at Aarhus University, Denmark, and medical director of the Danish Cornea Bank.
As always, this year’s topics result from consultations by the ESCRS Clinical Research Committee, which also identifies research projects for ESCRS support.
Dr Hjortdal briefly discussed the four topic areas and why they were chosen.
ARTIFICIAL INTELLIGENCE
While still in their early days, machine learning and other AI approaches are increasingly pervasive and powerful in ophthalmology, and in medicine and society generally, Dr Hjortdal noted. The symposium will examine both the roots of AI and how it can be used for clinical research as well as some specific applications in use and development.
The breadth of these AI applications is impressive. One presentation examines developing machine learning-accessible electronic health records to enable AI-powered registry studies that could leverage clinical data from millions of patients. Another explores digital eye testing in cataract and refractive care, which could improve patient care and convenience by enabling telemonitoring of patients after surgery.
Current anterior segment AI applications to be presented include IOL power calculation formulae using deep machine
learning programmes that increase predictive accuracy, particularly for very long and very short eyes that give conventional formulae fits. AI is also in use for detecting corneal ectasia and, importantly, risk of ectasia. A new application for classifying corneal dystrophies will also be discussed.
Biomarkers, including both chemical and physical indicators of pathological states and biological processes, are another technology exploding across the ophthalmic and general medical landscape. Detecting a specific protein or combination of proteins is making it possible to identify more precisely the causes of a wide range of inflammatory diseases, making it possible to better tailor treatments, Dr Hjortdal said.

For example, staining and tear film analysis may not yield the precise results needed to identify the causes of dry eye which may be revealed through protein analysis, Dr Hjortdal said. Similarly, chemical biomarkers can detect viral infections.
On the physical biomarker side, development of criteria for definitively diagnosing keratoconus will be presented. Beyond the eye, measurement of retinal nerve layer thickness may be a biomarker for neurodegenerative diseases, such as multiple sclerosis and Wilson disease. Detection of these physical biomarkers, as well as chemicals associated with specific disease states, overlaps AI to a certain extent. Biomarkers potentially may be found in any procedure specimen, so storing and analysing fluids and other debris from procedures can be an important way of identifying new biomarkers. The biomarkers journey from clinic to laboratory back to the clinic will also be discussed.
Advent of the femtosecond laser and more recently SMILE® intrastromal lenticular surgery technology are revolutionising both refractive and therapeutic surgery, Dr Hjortdal said. A range of recent innovations in the field will be discussed.
On the refractive side, lenticule extraction or implantation may be the future for correcting hyperopia. Intrastromal lenticule rotation may help address mixed astigmatism. Stromal implants may also be useful for treating corneal disease and for treating ectasia. Bioengineered and synthetic stromal lenticules may also soon be available.
PRESBYOPIA TREATMENT
Closer to the current clinical realm, the day’s final clinical research symposium will address current treatments for presbyopia. General topics will include a discussion of current understanding of accommodation and how it influences the design and use of presbyopia correcting technology. Measuring outcomes and how well they meet actual patient needs will also be discussed.
On the treatment side, recent advances in pharmacologic, laser and corneal inlay procedures will be presented. Discussions will include improving outcomes in high correction corneal refractive procedures, Dr Hjortdal added. New crystalline lens treatment approaches will be included as well.
Overall, Dr Hjortdal expects a highquality programme from prominent researchers worldwide, who accepted what has become a prestigious invitation to participate. “I know when I was first invited, I was a little bit proud,” Dr Hjortdal said.
EUROTIMES | SEPTEMBER 2020 27 VIRTUAL MEETING PREVIEW
symposia will highlight a variety of important new and upcoming breakthroughs in the field of ophthalmic research
2020 The Lens
Main symposium highlights state-of-the art in lens-based refractive surgery. Cheryl Guttman Krader reports
The Saturday afternoon main symposium during the 38th Congress of the ESCRS features an international faculty of experts in cataract refractive surgery who will be presenting on topics pertinent to the theme “20/20 in 2020: The Lens”.
Filomena Ribeiro MD, PhD, Lisbon, Portugal, and Roberto Bellucci MD, Verona, Italy, are co-chairing the session. Dr Bellucci said that while the virtual format creates new challenges for meeting organisers and presenters, there is a positive side to an online meeting.
“The COVID-19 pandemic has impacted the medical community in many ways, including the approach to education, and perhaps the 2020 Winter Meeting in Marrakech will be the last ESCRS meeting held in the pre-COVID format,” he remarked.
“However, ESCRS is ready to carry on its tradition of excellent education in the form of a webcast virtual meeting that will have the potential to reach a wider audience than ever. While we all regret not meeting in person, I believe we can transform the ‘problem’ into an opportunity.”
Continuing, he drew a parallel between the session content and its online delivery.
“The ‘20/20’ main symposia, which include the session on the lens and another on cornea-based refractive surgery, were conceived to provide updates on the most recent techniques in cataract and refractive surgery. Now, speakers will deliver the information using the most innovative communication method available,” Dr Bellucci said.
In planning the symposium, Dr Bellucci said that he and Dr Ribeiro were tasked with having to choose a finite number of topics and from among a long list of experts in the field.
“I believe we have put together a very interesting programme featuring speakers who are renowned for their work in lensbased surgery,” he said.
The symposium is beginning with a talk on “The quest for emmetropia”. It is being given by Giacomo Savini MD, Bologna, Italy, who will discuss biometry, IOL power calculation, and how to reduce the
pseudophakic refractive error to <0.5D.
“Minimising postoperative refractive error is of utmost importance in cataract surgery today. Especially as we are operating on more post-LASIK patients who enjoyed spectacle independence for decades and want to maintain it after cataract surgery,” said Dr Bellucci.
In the next talk, “Correcting astigmatism”, Adi Abulafia MD, Jerusalem, Israel, will explain methods to address another modifiable factor that can limit postoperative unaided vision.
“Far from considering it useful for pseudo-accommodation, we will learn how to minimise astigmatism by appropriately evaluating the anterior and the posterior corneal surfaces,” Dr Bellucci said.
The question, “Restoring accommodation with IOLs: have we made progress?” will be addressed in a talk by Gerd U Auffarth MD, PhD, Heidelberg, Germany. Dr Auffarth will discuss pseudoaccommodation and the most recent optic technologies using novel modalities to exploit the distribution of incoming light.
“I think we will hear that we are probably close to obtaining seamless vision in the pseudophakic state, which is an option that is becoming increasingly attractive for middle-aged patients looking for spectacle independence,” Dr Bellucci said.
Continuing with the topic of IOL optics, Scott M MacRae MD, Rochester, NY, USA, will review “Lens refractive indexing”. Dr McRae will share his views on this approach and results being achieved with new types of refractive IOLs that are modified using laser energy.
The focus of the last portion of the symposium is on optical disturbances and quality of vision. Even patients with full uncorrected vision may experience dysphotopsia that can prompt them to ask
for lens exchange, noted Dr Bellucci.
“The presentation ‘Pseudophakic dysphotopsia’ by Gre Luyten MD, PhD, Leiden, The Netherlands, is important for surgeons because it will describe both preventive and corrective strategies for these optical disturbances as well as the potential for their occurrence with newer optical designs that increase the depth of focus of monofocal IOLs,” he said.
Concluding the session, Béatrice Cochener-Lamard MD, PhD, Brest, France, will speak about “Quality of vision: Beyond 20/20”, as a critical determinant of patient satisfaction. Dr Cochener-Lamard noted that there have been spectacular advances in cataract surgery over the past two decades that have elevated the procedure to the rank of true refractive surgery. With the refinements that have occurred, “Super vision”, which considers vision quality in addition to 20/20 visual acuity, has become the targeted outcome for cataract surgery, Dr Cochener-Lamard said.
In her talk, she will discuss the many metrics by which quality of vision is characterised as well as the importance of optimising the ocular surface. “The ideal outcome is to offer patients a level of satisfaction such that they “forget their eyes” throughout their daily activities,” she said.
Dr Bellucci said that at the end of the symposium, it will be clear why lens-based surgery is increasingly popular as a method for refractive correction.
“In conjunction with the cornea refractive symposium, the lens symposium will provide a comprehensive review of the latest practical information on patient selection and surgical methods. These sessions fulfill the purpose of ESCRS symposia, which is to provide good scientific content that is readily understood by practitioners and easy to implement into their daily routines,” Dr Bellucci said.

20/20 in
EUROTIMES | SEPTEMBER 2020 28 VIRTUAL MEETING PREVIEW
Minimising postoperative refractive error is of utmost importance in cataract surgery today
Roberto Bellucci MD
2020 The Cornea
Main symposium speakers discuss definitions, metrics, and surgical techniques. Cheryl Guttman Krader reports
Cornea-based techniques for vision correction will be highlighted during the 38th Congress of the ESCRS Sunday morning main symposium. The session is titled “20/20 in 2020: Cornea” and is chaired by Béatrice Cochener-Lamard MD, PhD, and Vikentia Katsanevaki MD, PhD.

Dr Cochener-Lamard noted that the evocation of 2020 lent itself nicely to craft a title using a word play on “20/20 visual acuity” for a programme reviewing past and forthcoming advances in cornea-based approaches to refractive surgery.
“Refractive surgery was born with the application of incisional corneal surgery and then advanced and expanded with the introduction of procedures using the micron precision excimer laser followed by intrastromal strategies and most recently by femtosecond laser lenticule extraction,” said Dr Cochener-Lamard, Professor and Chair of Ophthalmology, University Hospital of Brest, France.
“Over the years we have seen patient outcomes benefit because of technological advances in energy delivery that improve treatment profiles and imaging techniques for centration optimisation, pupillary shift correction, cyclotorsion compensation for astigmatic treatments, and laser guidance, including by topography or aberrometry.”
Aberrometry ushered in a new era in laser vision correction. Introducing the language of optical aberrations and treatment targeting more than mere spherocylindrical correction, it also focused attention on evaluating vision quality as a performance, said Dr Cochener. “Rather than simply correcting a refractive error and providing 20/20 visual acuity, we now expect that patients will maintain optimal visual performance in
all living conditions, day and night. This defines ‘Super vison’ that is the topic for the first presentation in our session by Jesper Hjortdal MD, PhD, Aarhus, Denmark, who will emphasise that vision be measured both objectively and qualitatively.”
Nino Hirnschall MD, PhD, Vienna, Austria, will discuss modern techniques for refractive evaluation, with particular reference to recent automated measurement platforms. He will also describe the different scales of visual acuity and the optimal conditions for assessment.
“Objective measurements of vision quality” is the topic for a talk given by the renowned expert in optics, Pablo Artal PhD, Murcia, Spain. Dr Artal will demonstrate how optical aberrations impact visual performance and discuss ways to measuring and modulate them.
In a presentation titled “From guided ablation to small lenticule extraction”, Liem Trinh MD, Paris, France, will review the literature on topographically-guided LASIK and SMILE®, the femtosecond laserbased technique of lenticule extraction.
Dr Cochener-Lamard observed that understanding of the link between the geometric profile of the cornea (ie, asphericity) and treatment-induced optical aberrations (eg, spherical aberration and coma) gave rise to topographically-guided and wavefrontguided treatments, respectively, which aim to optimise the quality of vision.
“These techniques targeted improved visual performance under mesopic conditions by preserving preoperative asphericity and not increasing or even decreasing preoperative optical aberrations. They also led to presbyLASIK that accentuated corneal prolaticity for a gain in depth of field.”
Discussing SMILE, Dr Trinh will review its theoretical advantages compared with LASIK along with its outcomes and limitations.
“Whereas refractive correction by lenticule extraction is currently available using a single manufacturer’s femtosecond laser platform, the technique is currently being developed by competitor companies, which indicates a definite interest in this approach,” Dr Cochener-Lamard said.
Still in an early stage of development, intrastromal implantation of a lenticule to remodel the cornea is being evaluated as a method of correcting hyperopia or even presbyopia with placement of a lenticule featuring an aspheric profile. Numerous studies are also being undertaken using intrastromal lenticule implantation as a means to reinforce a keratoconic cornea. Mario Nubile MD, PhD, Pescara, Italy, a pioneer in this area, will provide an inventory of current investigations in his talk titled “New perspectives of intrastromal implantations”.
Dr Cochener-Lamard said that in creating an agenda for the symposium, issues emerging for patients after keratorefractive surgery could not be ignored. In the final presentation, Thomas Kohnen MD, PhD, Frankfurt, Germany, will describe reprocessing, remote adjustments, corneal enhancement and cataract management after corneal refractive surgery. Dr Kohnen will demonstrate the complementary nature of corneal and intraocular strategies and present data from studies investigating the ability to achieve the expected result.
Dr Kohnen said: “There is not one correct strategy for restoring spectacle independence after previous corneal surgery. Rather, there is a wide range of surgical options, and intraocular lenses should be available, which, if completed with precise anamnesis, preoperative examination and calculation, take into account the individual needs of the patient and lead to a high level of postoperative satisfaction and spectacle independence.”
Dr Cochener-Lamard observed that innovation is also reflected in the virtual format of the symposium and in the entire 38th Congress of the ESCRS.
20/20
in
EUROTIMES | SEPTEMBER 2020 29 VIRTUAL MEETING PREVIEW
Rather than simply correcting a refractive error and providing 20/20 visual acuity, we now expect that patients will maintain optimal visual performance...
Béatrice Cochener-Lamard MD, PhD
Making the most out of a virtual ESCRS

A guide for young ophthalmologists seeking to get all they can from a new experience. Sorcha Ní Dhubhghaill reports
It goes without saying that the past six months have changed everything; How we work, how we learn and of course how we come together as a profession. And while at the start of this pandemic, October seemed like a safe month for a conference, it is increasingly clear that that is unlikely. And while we all hope for things to look better and brighter by then, we cannot be sure. To ensure the safety of all participants, Professor Rudy Nuijts, President of the ESCRS, along with the ESCRS Executive, have decided to hold the annual ESCRS meeting as an online rather than a live event.
The annual ESCRS meeting is the biggest gathering of the year for European Ophthalmologists and so this news comes as a bit of a blow, in particular for the young ophthalmologist (YOs). The YOs usually flock to the practical sessions and wet labs for a chance to practice new techniques with the advice of a master in the field. It’s hard not to be a bit disappointed – but on the plus side, none of the sessions will be booked out!
The show must go on as always, there’s a silver lining. For there are a number of benefits to an online meeting format that you may not have considered. Rest assured that registration — open in August this year — with greatly reduced registration fees is still well worth it. So, make a cup of tea (or treat yourself to a glass of wine if it’s not too early) and prepare to enjoy the first ESCRS meeting you can attend, from home, in your comfiest sweatpants. And you get to save all that money on airfare and accommodation.
The programme kicks off on Friday 2 October with the opening of the 3D interactive exhibition. You will be able to make a profile for yourself and “visit” the booths before the academic sessions start. The session starts with an update on the COVID-19 situation for ophthalmologists as well as a tribute to those working to stem the tide of the pandemic.
This is followed by the official opening of the congress and the Ridley Medal lecture which will be given by Dr David Chang — a trailblazer in innovative ophthalmic surgery. The title of his lecture is “Five Compelling Lessons from the Greatest Team of Cataract
Surgeons” and I am not sure I have ever read a more compelling title for the young ophthalmologist. Who is this team? What did they learn? This one is surely not to be missed.
After that you can pick between the JCRS symposium, the ESCRS/EuCornea session or the ESCRS/WSPOS symposium — feel free to drop by the paediatric session and I can tell you about the learning curves of special intra-ocular implants. Here’s the best part: even if you miss the sessions the first time around, you will be able to catch them afterwards. I attended the virtual World Ophthalmology Congress (WOC) online this year and I am still logging in to watch the sessions from time to time. So, you really don’t have to miss a thing.
The Saturday sessions start at 8:30am — or later if you want. The benefit of catching it live is that you will be able to ask the presenters questions in real time. You don’t even have to stand up and find the microphone, you can just fire questions from your laptop. All questions welcome.
The ESCRS/EURETINA programme has a really practical theme, cataract surgery in patients with AMD. Something we see rather frequently so if you want to adapt your approach to treat these patients better, make sure to tune in. The next main symposium covers “what to do when the unexpected happens” and offers practical advice on how to turn a mess into a success. The YO session
follows this up and gives some crucial advice on the basics from the experiences of other young ophthalmologists.
Sunday starts when you want it to start — but again if you are an early bird you can participate in the video symposium on surgical complications (where you can vote live), the YO programme or the myopia workshop. At lunch-time you can follow the industry satellite meetings but you may have to bring your own lunch this time. The future of cataract surgery and the glaucoma workshops are the main highlights of the afternoon and should bring you to the closing of the congress.
Like in most professions, COVID has forced us to adapt and the ESCRS is making this pivot to provide the best content in the safest way. The online congress will let you follow everything you want at the pace that suits you, in your own home. It may also help some of our colleagues that could not afford to attend in person the chance to join in and they will be most welcome. So, bookmark the link and follow everything you want to, without worrying about being too late or the room being too crowded.
Sorcha Ní Dhubhghaill MB PhD MRCSI(Ophth) FEBO is an Anterior Segment Ophthalmic Surgeon at the Netherlands Institute for Innovative Ocular Surgery (NIIOS) and Antwerp University Hospital
EUROTIMES | SEPTEMBER 2020 30 VIRTUAL MEETING PREVIEW
Oliver Findl, Chairman of the ESCRS Young Ophthalmologists Committee
Diagnosing OSD with AI
Artificial intelligence deep learning algorithm makes accurate determinations by assessing OCT images. Cheryl Guttman Krader reports
Amulti-disease predicting artificial intelligence (AI) deep learning algorithm shows excellent accuracy, sensitivity, and specificity for autonomous detection of both dry eye disease (DED) and Fuchs’ endothelial corneal dystrophy (FECD), reported researchers at the 2020 ASCRS Virtual Meeting.
The AI software was developed by researchers at Bascom Palmer Eye Institute, University of Miami, Florida, USA. It processes images captured using an ultra-high resolution anterior segment optical coherence tomography (AS-OCT) platform (Envisu R2210, Bioptigen).
The findings from prospective evaluations of its performance for diagnosing the two ocular surface conditions were presented by Collin Chase BSc and Taher K Eleiwa MD, MSc.
DETECTING DED
The availability of an AI platform for diagnosing DED would be a valuable addition for clinicians, said Mr Chase.
“DED affects up to 25% of patients seen in ophthalmology clinics. Although there are currently a number of traditional tests and newer modalities used for its diagnosis, as noted by the members of the Dry Eye Workshop II, there is no gold standard,” he said.
“Artificial intelligence and deep learning networks can help us to discover patterns that exist within medical imaging but that are not obvious to the naked eye. Given the difficulty of diagnosing DED without conducting multiple timeconsuming tests, we believe that our autonomous algorithm that is coupled with AS-OCT images could be helpful.”
Mr Chase said that the group was interested in using AS-OCT images to develop the AI system for diagnosing DED, considering previous research that found OCT-identified features in the corneal epithelial layer were prevalent in eyes with DED. In addition, OCT has been reported to detect DED through quantification of ocular surface adhesiveness and tear meniscus measures.
“In this black box process, we are not
teaching the system what features to look at but rather asking it to discover features on its own. As we had hoped, we found that the AI was looking at the epithelial layer and the ocular surface,” he told the virtual session.
The AI algorithm for DED was trained and tested using a total of 27,180 images from 151 eyes of 91 patients. Its performance was then tested in a prospective study that included 32 eyes with DED and 28 healthy eyes.
All of the patients in the prospective study underwent testing for DED with a tear breakup time, Schirmer’s test, corneal fluorescein staining, conjunctival lissamine green staining and the Ocular Surface Disease Index. Eyes were categorised as healthy if none of the DED tests was abnormal and they had no corneal ICD-10 diagnoses. Eyes were assigned a clinical diagnosis of DED if they had an ICD10 diagnosis of DED and at least two abnormal DED tests.
The deep learning model was very successful for diagnosing DED and differentiating DED eyes from the healthy controls. It correctly diagnosed 29 of the 32 eyes with DED and 25 of the 28 healthy eyes. In a receiver operating characteristic (ROC) curve analysis for DED, the test had an area under the curve of 0.993, 96.9% sensitivity and 95.8% specificity, Mr Chase reported.
A prediction score was also calculated for each group of eyes based on the percentage of images diagnosed as DED. The mean DED prediction score was 0.83 for the DED group and 0.11 for the healthy eyes (p<.01).
DIAGNOSING FECD
In a recently published paper, Dr Eleiwa and colleagues reported that the ultra-high resolution OCT platform detected in vivo
characteristics of FECD and could be used for both diagnosis and severity grading.
“We found that in healthy eyes, the endothelium/Descemet’s membrane is visualised as a band formed by two smooth regular hyperreflective lines with a hyporeflective space in between. In eyes with FECD, however, the posterior line showed a wavy irregular appearance with areas of focal thickening, which is considered tomographic visualisation of guttae,” he explained.
The researchers conducted a prospective case-control study that used 7,380 AS-OCT images from 15 eyes with FECD and 28 controls to evaluate the performance of the AI algorithm for diagnosing FECD. The ROC curve analysis showed that the AI algorithm was able to autonomously diagnose FECD with an AUC of 0.999, 100% sensitivity and 97.8% specificity. It had a mean FECD prediction score of 0.92 for the FECD eyes and just 0.01 in the healthy controls (p<.01).
Dr Eleiwa said that prospective studies are now required to evaluate the utility of the AI algorithm to predict FECD, especially after cataract surgery. He noted that current tools for diagnosing FECD have limitations. In particular, they fall short of detecting the natural course of FECD and for predicting its progression, especially after cataract surgery.
“Slit-lamp examination can miss subtle oedema, specular microscopy can have sampling errors that render its measurements inaccurate and pachymetry gives an isolated measurement of central corneal thickness that is not always representative of cornea oedema or FECD severity,” Dr Eleiwa noted.
Collin Chase: collinchase14@miami.edu
Taher K Eleiwa: tahereleiwa87@gmail.com
EUROTIMES | SEPTEMBER 2020
CORNEA 31
Artificial intelligence and deep learning networks can help us to discover patterns that exist within medical imaging but that are not obvious to the naked eye
Collin Chase BSc
Protecting corneal endothelial cells
Emerging therapies may improve graft survival, reduce transplant need. Howard Larkin reports
Gene and cell technologies now in development would protect corneal endothelial cells (EC) from dying, potentially extending the life of donated corneas in eye banks and improving endothelial graft survival, Thomas A Fuchsluger MD, PhD, told the 37th Congress of the ESCRS in Paris, France.
The innovative technologies might even reduce the need for transplantation by protecting patients’ own endothelium in vivo, said Dr Fuchsluger, who is chairman and professor of ophthalmology at Rostock University Hospital, Germany.

Several viral and non-viral vectors have proven effective in delivering genes and proteins that slow cell death of EC in donated corneas, said Dr Fuchsluger. These include lentiviruses, optimised adeno-associated viruses and calcium phosphate nanoparticles. This could help reduce the approximately 30% loss of corneas due to EC deterioration in eye banks, as well as the 25% loss after transplantation.
Similarly, magnetic nanoparticles have successfully penetrated and treated EC in explanted corneas, protecting them from early failure, Dr Fuchsluger noted. If this technique is successful when injected into the anterior chambers of living patients, it could avoid the need for transplants.
“This is an unmet need in ophthalmology,” he said.
BLOCKING CELL DEATH
EC apoptosis is triggered internally through mitochondrial action in response to stresses including oxidation and DNA damage, and externally through surface receptors receiving death ligands including Fas and TNFR1. The protein Bcl-xL has been found to block both apoptosis pathways, Dr Fuchsluger said. Transfecting genes that express Bcl-xL into ECs is effective in reducing cell death and maintaining EC physiological morphology and function.
In a 2011 study, Dr Fuchsluger and colleagues used a lentivirus to transfect
genes for Bcl-xL into donor EC. A baculovirus that causes EC to express the broad-spectrum anti-apoptotic protein p35 was also tested. Both extended EC cell life and morphology well beyond untreated cells out to 11 weeks under eye bank storage conditions (Fuchsluger TA et al. Gene Ther. 2011 Aug;18(8):778-87. Fuchsluger TA et al. Human Gene Ther. 2011; 22:549-558).
Experiments with HIV transfection showed a preference for EC over stromal cells and may be a possible vector. Trials with various adeno-associated viruses (AAV) found AAV-2 and AAV-9 most efficient for gene transduction, making them a potential alternative vector to the much larger lentivirus. (Fuchsluger TA et al. Klin Monbl Augenheilkd. 2011(June);228(6):498-503.)
Efficiency of AAV transfection was further increased using a selfcomplementary approach that doubled the transfected DNA strand, Dr Fuchsluger said. The approximately two-week expression achieved with this method might make it useful for protecting EC immediately after transplantation, which is when the greatest loss occurs, Dr Fuchsluger said. (Gruenert et al. PLOS ONE March 29, 2016.)
NON-VIRAL VECTORS
Among transfection solutions more elegant than viral vectors are calcium phosphate nanoparticles, Dr Fuchsluger said.
“They are cheap to produce, they can be stored on the shelf and you can produce them so they are custom designed for mammalian cells.”
Techniques include coating the calcium phosphate particle surrounding the DNA to be inserted with etoposide, which increases cellular uptake, delaying apoptosis in more cells, Dr Fuchsluger added.
“You can get up to about one in every six cells, which is a lot for a nonviral vector,” he noted (Hu J et al. Acta Biomateriala 2012;8:1156-1163).
Dr Fuchsluger is currently working with nanoparticles to transfect siRNA designed to downregulate two proapoptotic proteins. He reported a 25% reduction in Bak expression and 20% cut in Bax in experimental corneal tissue, which should translate into less EC selfdestruction.
IN VIVO TREATMENT
Magnetic nanoparticles could be used to protect EC in patients with failing endothelium, possibly avoiding the need for transplantation, Dr Fuchsluger said. The particles surround a magnetic core with DNA to be transfected and lipoplexes to aid adherence and penetration. The technique has decreased EC apoptosis up to 56% (Czugala et al. Nanomedicine. 2016 Jul;11(14):1787-800). In future practice, the particles would be injected into the anterior chamber and drawn into contact with the corneal endothelium using a magnetised contact lens.
Talks are under way with German regulators to launch phase I clinical trials of these technologies, Dr Fuchsluger reported.
Thomas A Fuchsluger: sekretariat.uak@med.uni-rostock.de
EUROTIMES | SEPTEMBER 2020 CORNEA 32
They are cheap to produce, they can be stored on the shelf and you can produce them so they are custom designed for mammalian cells
Thomas A Fuchsluger MD, PhD
VIR TUAL EVENT 26th September 2020
11th EuCornea Congress
Artificial intelligence for KERATOCONUS DIAGNOSIS
Deep learning improves detection of mild ectasia. Howard Larkin reports
Despite the accuracy of Placido-disk based corneal topography and tomography imaging for diagnosing keratoconus, post-LASIK ectasia remains a challenge, occurring at least 0.033% (10/30,000) of cases. “Therefore, a better evaluation is required to detect keratoconus, especially in the early stages,” said Eyüp Özcan MD, at the ASCRS Virtual Annual Meeting 2020.
To that end, Dr Özcan and colleagues at the Bascom Palmer Eye Institute, University of Miami, Florida, USA, developed an artificial intelligence tool to autonomously assess corneal images for keratoconus signs. While autonomous systems exist for diagnosing diabetic retinopathy, glaucoma, age-related macular degeneration and retinopathy of prematurity, no autonomous system has been reported for keratoconus, he added.
HIDDEN FEATURES
Using techniques of deep learning based on analysis of thousands of training images, the AI tool identifies hidden features in the data set that may be missed by unaided human analysis, Dr Özcan said. His group built on existing criteria in anterior segment OCT imaging for detecting keratoconus features (Sandali, O et al. Ophthalmology 2013; 120(12):24032412), and applied it to detect keratoconus autonomously using high-definition OCT images generated by a Bioptigen Envisu R2210.
Data from labelled training images were assessed by a deep neural network. The resulting algorithm, Bascom Palmer AI 1.0, was then applied to assess 7,740 images from 43 eyes of 23 patients with keratoconus and 5,040 images of 28 eyes in 28 patients without keratoconus. Results were compared with diagnoses provided by board-certified corneal specialists at Bascom Palmer.
While one eye of a keratoconus patient was diagnosed as healthy, the fellow eye of that patient was correctly identified with keratoconus.
“So, the algorithm was able to correctly differentiate all patients with keratoconus from healthy subjects and thus achieving accuracy, sensitivity and specificity of 100%,” Dr Özcan reported. Similarly, it correctly diagnosed 42 out of 43 keratoconic eyes, achieving accuracy of 97.9%, sensitivity of 95.3% and specificity of 94.6%.
MORE DATA: INCREASED ACCURACY
Separately, Renato Ambrósio Jr. MD, PhD, Adjunct Professor of Ophthalmology of the Federal University of the State of Rio de Janeiro (UNIRIO), Brazil, reported on a machine learning approach to further optimise the current integrated Scheimpflug tomography and biomechanics index (TBI). The seminal TBI study included one eye randomly selected from 480 healthy patients, from 204 keratoconus cases, and 94 eyes with typical or normal topography from patients with very asymmetric ectasia (VAE-NT). To further enhance the
accuracy of ectasia detection, a large cohort of cases from the International Corneal Tomography and Biomechanics Group included one eye randomly selected from 1,679 healthy patients, from 1,084 keratoconus cases and 543 VAENT cases. Expanding the data does allow for optimising the AI methods. This study was done with the BrAIN Med (Brazilian Artificial Intelligence Networking in Medicine; www.brain.med.br).
A random forest (RF) method based on 16 clinical features increased the sensitivity in detecting abnormality in normaltopography eyes in very asymmetrical ectasia cases from 75.7% to 85.6%, with a higher specificity of 90.5%, compared to 89.1%. For the clinical ectasia cases, the new RF also augmented sensitivity from 98.4% to 99% and specificity from 98.5% to 99.2%.
“The aim of the TBI is to provide an objective metric for epitomising the susceptibility for ectasia progression, which goes beyond but not over detecting keratoconus,” explained Prof Ambrósio.
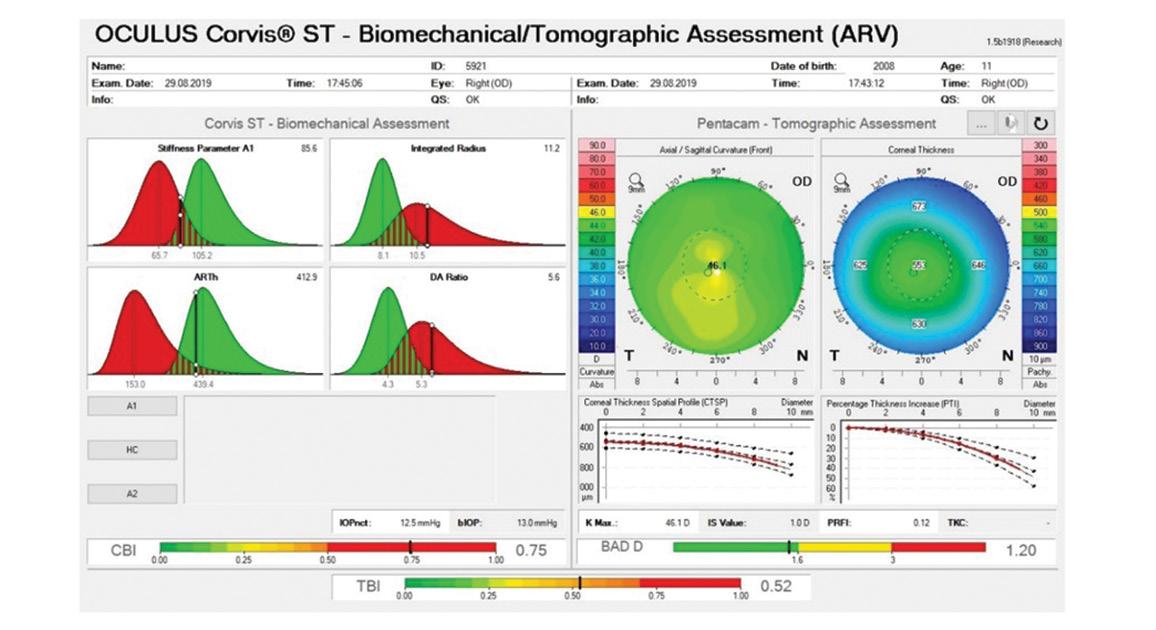
“We have to be very careful with internal cross-validation methods when programming AI, which requires a large data set. Indeed, external validation tests are always to be considered, and further enhancements with continuously more massive training sets should be expected. Also, improvements should come with the integration of additional parameters including wavefront data, axial length, epithelial thickness data is part of the plan, along with the correlation with genetics and finite element analysis,” added Prof Ambrósio. “This is truly a revolution in evolution,” he concluded.
Prof Ambrósio (dr.renatoambrosio@gmail.com) is a consultant for Oculus and a founder of the BrAIN Med.
Eyüp Özcan: ozcan_eyup@hotmail.com
EUROTIMES | SEPTEMBER 2020 CORNEA 34
The Integrated TBI display from a patient with DCVA (distance vision correction) of 20/20+ with high susceptibility for (forme fruste) keratoconus
Courtesy of Eyüp Özcan MD
Biomarker explosion
Howard Larkin reports
New chemical and biological markers constantly being identified are proving to be powerful clinical tools for ophthalmologists. Found in tears, ocular tissues and other fluids, these biomarkers are essential to understand the evolving causes of long-known diseases so they can be more accurately diagnosed, and more effectively managed and treated, Rohit Shetty DNB, FRCS, PhD, of Maastricht University, The Netherlands, and GROW Research Laboratories, Bangalore, India, told the 37th Congress of the ESCRS in Paris, France.
For example, keratoconus has often been considered a noninflammatory disease because it does not follow the classic progression of heat, redness, swelling and pain followed by loss of function. Biomarker analysis tells a different story, Dr Shetty said. Tear sample analysis showed elevated expression of matrix metalloproteinase-9 (MMP9) and other inflammatory cytokines in eyes with keratoconus.
This suggested treatment with cyclosporin A – which led to reduced MMP9 and cytokine levels, and slowed progression in 20 previously progressing patients (Shetty R et al. IOVS 2015 Feb 3;56(2):738-50). Moreover, following patients over time revealed that progressing patients showed a higher level of MMP9 and cytokines such as IL-4 and IL-8 than nonprogressing patients did.
“If you see these markers it could mean progression, and help decide on treatment, with cyclosporine to manage ocular surface inflammation,” Dr Shetty said.
Conversely, lower levels of lysyl oxidase (LOX) and collagen have been found in the cone of keratoconus patients. Higher levels of LOX correlate with better outcomes in crosslinking, and lower levels of LOX in tears correlates with progression, Dr Shetty noted. Reduced LOX and collagen levels may predispose clinically healthy eyes to ectasia after corneal refractive surgery, making it a good biomarker for screening patients before surgery (Shetty R et al. J Refract Surg. 2019;35(1):6-14). Other markers may help predict postsurgery corneal haze.
Recently discovered tear film biomarkers for other ocular diseases include TNFα, IL-6, IL-8, IL-17, MMP9 for dry eye; fibrotic markers for pterygium; inflammatory mediators for blepharitis; IgE for allergies; VEGF, lipocalin 1, lactotransferrin, lacritin, lysosome C and lipophilin A for diabetic retinopathy; and IL-1β, IL-6, IL-12, TNFα, S100As and MMPs for glaucoma. Tear biomarkers also exist for metabolic diseases, autoimmune and neurological disorders, including multiple sclerosis and Alzheimer’s, and for various cancers. Tear film biomarkers are also associated with gut microbiome as well, Dr Shetty added.
Tools for using biomarkers are entering the clinical realm, and will include chips that can detect multiple markers, said Dr Shetty, who is developing such a device.
Noting that biomarkers may be present in any tissue or fluid that is discarded during surgery, Dr Shetty recommended saving these samples from surgery for future analysis, as it has helped him in his research.
“Anything that you throw in the bin may hold biomarkers,” he said.
Rohit Shetty: drrohitshetty@yahoo.com
• ESCRS Research Portals (Find details of ESCRSSponsored research)
• Astigmatism Double Angle Plot Tool (JCRS)
• JCRS Online Case Reports
• Landmark Articles
• ESCRS Eurotimes Podcasts
• ESCRS Player Videos
• ESCRS On Demand
• ESCRS iLearn
• EBO-ESCRS Exam and more...
EUROTIMES | SEPTEMBER 2020 CORNEA
Traces in tears and tissues improve disease diagnosis, prognosis and management.
Visit education.escrs.org Ready when you are.
Continue your education all year with our range of online resources
35
European Union Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
the ECCTR Registry Join Track
your Surgical Results
www.ecctr.org
ECCTR is a project funded by the ESCRS with initial support from the EU
Who should do MIGS?
Should minimally invasive glaucoma surgery (MIGS) be limited to glaucoma specialists? Florent Aptel MD, PhD, argued that it should in a debate at ESCRS Glaucoma Day 2019 in Paris, France.
Glaucoma and ocular hypertension are complex, lifelong diseases with multiple potential causes, and may progress rapidly or not at all depending on individual patient risk factors, said Dr Aptel, who is professor at Grenoble-Alpes University and University Hospital, Grenoble, France.
And while MIGS has expanded options for early and intermediate cases, treatment decisions must always consider long-term implications, particularly any limits on future treatment. Some procedures are also technically complex, sometimes complicated by the use of antifibrotics such as mitomycin C. Therefore, “surgery is not the first treatment option”, Dr Aptel said, noting that 80-to90% of patients can be controlled with medication.
Glaucoma patients also must be followed long-term to assess and quantify progression to determine the need for additional treatment, Dr Aptel added. This is a complex and subtle task, particularly for slowly progressing patients, and requires expert evaluation of both structural and functional parameters.
Often, multiple surgical, laser and medical interventions are needed, and they may need maintenance such as needling – cataract surgery is not always appropriate, Dr Aptel said. Cataract surgeons with short-term patient relationships are not in a position to assess long-term needs and complex options, he added. “Clearly, only glaucoma surgeons are able to assess progression and decide what to do with surgery.”
However, there are simply not enough glaucoma surgeons to address the growing global need for treatment, noted Alain Bron MD, professor at University Hospital, Dijon, France. He noted that worldwide, blindness due to glaucoma increased 62% and visual impairment 83% between 1990 and 2010. (Bourne R et al, Plos ONE 11(10):e0162229.) At the same time, the number of glaucoma surgeons has declined, with those performing trabeculectomy in France falling from 713 to 610 in just three years ending in 2014. (Bron AM et al. BJO, 2017;101:1500-1504.)
Dr Bron argued that the transition to combining MIGS with cataract surgery is already well under way, with MIGS surgery growing exponentially in recent years.
“Should we keep glaucoma surgery in the ghetto of glaucoma specialists? In my opinion, no, because glaucoma is for everybody,” Dr Bron said.
Alain Bron: alain.bron@chu-dijon.fr.
EUROTIMES | SEPTEMBER 2020 GLAUCOMA
Careful planning and follow-up are more important than who does the surgery. Howard Larkin reports
36
Cataract surgeons with shortterm patient relationships are not in a position to assess longterm needs and complex options
Florent Aptel MD, PhD
Saturday 26th September
The current pandemic caused by the COVID-19 virus has created upheaval in all aspects of our personal and professional lives.
We at WSPOS believe that with every challenge comes opportunity and this challenge now presents us the opportunity to deliver a new and exciting programme to a global audience via a virtual platform.

WORLD WIDE CONNECT 2020
Join us as we CONNECT with the world!
Registration and programme information now available on our website. Give us 24 Hours and We’ll Give you the World! www.wspos.org/world-wide-connect-2020/
Paediatric Ophthalmology and Strabismus
World Society of




For more information, visit: annualmeeting.ascrs.org Submissions open August 17, 2020 – ﹐ 2021 ASCRS Annual Meeting August 13–17 San Francisco, CA Featuring ASCRS Subspecialty Day August 13
IN US!
J
Crisis sparks online growth
Video
consultations can help patients and doctors in numerous ways. Dermot McGrath reports
With tele-ophthalmology already gaining traction in recent years as an effective eyecare delivery modality worldwide, the COVID-19 pandemic has served to further amplify this trend, according to Ken K. Nischal MD, FRCOphth.
In a special webinar (see https://youtu.be/8MDKupy6xhA) organised by the World Society of Paediatric Ophthalmology and Strabismus (WSPOS), Dr Nischal, Chief of the Division of Paediatric Ophthalmology, Strabismus, and Adult Motility at the UPMC Children’s Hospital of Pittsburgh, United States, outlined some of the key features and benefits of a teleophthalmology service for paediatric patients.
“The future is here. I do not think that tele-ophthalmology is going to go away and we would be well advised to become familiar with it as we seek to make the best use of the resources we have available to us in caring for our patients in the current crisis,” he said.
Tele-ophthalmology services can be provided primarily in two ways – synchronously or asynchronously, explained Dr Nischal.
Synchronous tele-ophthalmology enables real-time interaction between participants for consultations using standard telemedicine technologies such as video-conferencing.
“The clinic usually sets up the appointment at a designated time, or the patient may have 24/7 on-demand access to a carer. The carer is not necessarily an ophthalmologist – for instance it is a paediatrician who will handle the demands in the AnywhereCare system used at Pittsburgh,” he said.
More familiar to most ophthalmologists is asynchronous tele-ophthalmology, the classic “store-and-forward” method, where data is captured by the patient and transmitted for review at a later time.
“For instance, we get parents sending us pictures of their child’s eye for retinopathy of prematurity (ROP) or diabetic retinopathy (RP). We also use it to garner opinions from patients and other doctors,” he said.
Implementing an effective synchronous tele-ophthalmology service can be challenging, explained Dr Nischal.
“You obviously need a certain amount of equipment in terms of the video platform, bandwidth etc. You also need specific informed consent and declaration from parents, so that they fully understand that this is not the same as face-to-face consultation and that you have the requisite documentation to protect yourself. It is a new way of interaction, so we need to remember to look at the camera when talking to the patient. It is also important to understand the clinic flow to use the resources efficiently,” he said.
Dr Nischal said that there would be a growing need for “at home” testing capability or via specialised satellite centres.
To this end, there are several applications and devices available to assist in testing and monitoring patients remotely, he said.
“For visual acuity, there are a variety of web-based or smartphone apps; for strabismus, there is the 9 Gaze app; for fundoscopy, there are smartphone adapters. We now also have a mobile device for visual field assessment which has been developed by Olleyes,” he said.
Ken K. Nischal: nischalkk@upmc.edu

EUROTIMES | SEPTEMBER 2020 PAEDIATRIC OPHTHALMOLOGY
Free Membership Membership to WSPOS is available for FREE on www.wspos.org
Society of Paediatric Ophthalmology and Strabismus Contact Info: WSPOS, Temple House, Temple Road, Blackrock, Co. Dublin, Ireland Tel: +353 1 288 3630 Fax: + 353 1 209 1112 Email: wspos@wspos.org Join our society and become part of one of the largest networks of paediatric ophthalmologists in the world. You’ll gain access to our wide library of videos, including our “Masters in Surgery” archive and also get the chance to collaborate on our global case report
At WSPOS, we believe that “Expertise Resides ALL Over the World” 39
World
quiz.
47,863 *
* Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk Results from the EuroTimes Readership Study 2017
readers say it's
80 %
of
an interesting read
Reach NUMBER 1!
LEIGH SPIELBERG MD Books Editor

BOOK Reviews
PUBLICATION
CLINICAL STRATEGIES IN THE MANAGEMENT OF DIABETIC RETINOPATHY

EDITORS
FRANCESCO BANDELLO ET AL
Summaries and insights
PUBLICATION
OPTICAL COHERENCE TOMOGRAPHY IN GLAUCOMA: A PRACTICAL GUIDE
EDITORS
AHMET AKMAN ET AL
PUBLISHED BY SPRINGER
A FULL-FLEDGED INTRO AND GUIDE TO USING OCT
PUBLISHED BY SPRINGER
As the diabetic epidemic spreads across the globe, diabetic retinopathy will follow, destroying the vision of millions. Despite the advent of anti-VEGF, the refinement of laser treatment and the increased insight into the disease’s pathogenesis, the complexity and chronicity inherent in its treatment will continue to hamper efforts to save sight.
It was with this in mind that I picked up the Second Edition of Clinical Strategies in the Management of Diabetic Retinopathy: A Step-by-Step Guide for Ophthalmologists (Springer). Edited by Francesco Bandello et al, the book addresses all aspects of the disease. It offers both summaries of well-established knowledge and insight into more recent studies.
Chapter 1 introduces the reader to diabetic retinopathy by way of epidemiology, risk factors and pathophysiology. This provides a framework in which to work. Clinical Strategies is then divided by disease subtype, each of which requires a different approach.
Chapter 2 covers non-proliferative diabetic retinopathy, which the general ophthalmologist is likely to see on a daily basis. What I found most interesting in this chapter was the demonstration of the usefulness of newer imaging modalities, in the evaluation of this early stage, such as ultrawide-field angiography.
Next up is diabetic macular oedema (DME) in Chapter 3. DME, which arises from the breakdown of the blood-retinal barrier, leads to devastating central visual loss. The strength of this text is to efficiently compare the treatment modalities available for DME and offer recommendations as to which ones should be used, and when.
In Chapter 4, proliferative diabetic retinopathy (PDR) is addressed. It is comprehensively illustrated, showing examples of how to approach particular disease states, both diagnostically and therapeutically. Particularly useful are flow charts of therapeutic algorithms for the management of PDR. This advice continues in both Chapter 5, which presents a treatment update for PDR, and Chapter 6, on advanced PDR.
This 280-page book is appropriate for general ophthalmologists, medical & surgical retina fellows and established retina specialists who are looking to update and polish their knowledge in this exciting time for DRP treatment.
EVERY CONDITION YOU’RE LIKELY TO ENCOUNTER
For those looking for a “day-to-day guide on the diagnosis and management of routine to complex retinal disorders,” The Retina Illustrated (Thieme) might be the one. This 400-page text is an imagebased overview of just about every retinal condition the general ophthalmologist is likely to encounter during his or her career. Edited by Justis P. Ehlers, the text is a good mix of photo-based atlas and textbased reference book. It covers each disease in three or four pages in a highly-organised fashion.

Particularly useful is the section on chorioretinal infectious and inflammatory disorders. Including common entities like toxoplasmosis and rare ones like West Nile retinopathy, the excellent photographs help the practitioner make a diagnosis and start management. Also included are rare, difficult-to-classify conditions such as choroidal folds, and newer ones such as pachychoroid, in this case in the context of central serous chorioretinopathy.
Glaucoma follow-up is highly dependent upon imaging, and optical coherence tomography (OCT) has taken a prominent role. Optical Coherence Tomography in Glaucoma: A Practical Guide (Springer), edited by Ahmet Akman et al, provides a full-fledged introduction and guide to the clinical use of OCT for managing patients with glaucoma.

I learned a lot from Part II: How to Interpret OCT Results. Many examples are shown of findings in glaucomatous eyes with varying stages of severity, as well as scans with artifacts and anatomical variations. OCT analysis of nonglaucomatous optic neuropathies, as well as the evaluation of progression, are covered. This book is appropriate for general ophthalmologists, glaucoma fellows and anyone looking to incorporate OCT into their glaucoma practice.

PUBLICATION
BASICS OF VITRECTOMY
EDITORS
RAJVARDHAN AZAD ET AL
PUBLISHED BY THIEME
POSTERIOR SEGMENT SURGERY IN STRAIGHTFORWARD PROSE
Basics of Vitrectomy (Thieme), by Rajvardhan Azad et al, is a quick, 200-page introduction to posterior segment surgery. Readable in an hour or two, due to its small size and large number of surgical images, the text covers the surgical material in very broad strokes. Topics like macular surgery and rhegmatogenous retinal detachment are covered in a few pages, quickly familiarising the reader with the subjects without delving into detail. The book’s strength is its straightforward prose and avoidance of statistics, footnotes and references to studies.
The book is most appropriate for ophthalmology residents preparing for their vitreoretinal rotation, or even for medical students preparing to spend a day or two shadowing a vitreoretinal surgeon in the operating room.
EUROTIMES | MONTH YEAR
This book is appropriate for general ophthalmologists, as a quick reference guide for diagnostic puzzles; and for retina fellows, who will enjoy its learning-friendly format and its use of the most recent imaging modalities.
If you have a book you would like to have reviewed please send it to: EuroTimes, Temple House, Temple Road, Blackrock, Co Dublin, Ireland
BOOK REVIEWS 41
PUBLICATION THE RETINA ILLUSTRATED EDITORS JUSTIS P. EHLERS PUBLISHED BY THIEME
EUROTIMES | SEPTEMBER 2020
FDA CLEARANCE OF CATALYS COS 6.0 SOFTWARE
Johnson & Johnson Vision has announced the Food and Drug Administration (FDA) 510(k) clearance of a new software for the CATALYS Precision Laser System.
INDUSTRY NEWS
Following in great footsteps
Andreas Bosshard, co-owner and former managing director of Oertli Instrumente AG, has handed over the chairmanship of the board to Andreas Schmidheini.

Mr Bosshard joined Oertli Instrumente AG and took over as managing director in 1989. Heinz A. Oertli, the founder of the company, had hired Mr Bosshard, who had experience as a development, sales and marketing manager, with the intention of finding a successor. In 1992, the change of ownership took place with 30 employees at that time.
“For more than 20 years, Mr Bosshard managed the small and medium-sized company and led it from a local manufacture to an international success story in ophthalmic surgery. Under his leadership, Oertli launched five surgical platforms on to the market, developed two new surgical techniques for glaucoma and cataract surgery and successfully introduced several inventions that still shape the world of ophthalmology today,” said a company spokeswoman.
In 2010, Mr Bosshard handed over the operational management to his two sons and concentrated on his function as Chairman of the Board. Christoph Bosshard is CEO of Oertli and Thomas Bosshard is Head of Marketing & Sales.
Andreas Schmidheini, who has been on the Board of Directors of Oertli Instrumente AG since 2010, said he was impressed, by the life’s work of his predecessor: “I am aware that I am following in great footsteps, he said.” www.oertli-instruments.com
FDA ACCEPTANCE OF PMA APPLICATION
Santen has announced that the United States Food and Drug Administration (FDA) has accepted the Premarket Approval (PMA) application for DE-128 (MicroShunt) for review. DE-128 is an investigational surgical glaucoma implant designed to reduce intraocular pressure (IOP) in patients with primary open-angle glaucoma (POAG) whose IOP is not controlled when using maximum tolerated glaucoma medications.
The substantive review, which traditionally spans 180 days from the FDA’s receipt of the PMA final module, is an in-depth review following which the FDA will make a decision as to whether the PMA is approved.
“As of this year, it is expected that 3.7 million people in America will be living with POAG,” said a Santen spokeswoman. “The
prevalence of POAG is expected to rise to 4.1 million in 2025,” she said.
In the United States, DE-128 is an investigational, ab-externo, minimallyinvasive surgical glaucoma implant designed to help drain eye fluid and reduce IOP in patients with POAG whose IOP is not controlled when using maximum tolerated glaucoma medications. IOP reduction is the most effective means of preventing the progression of glaucoma and vision loss. Made of a proprietary, biocompatible material called SIBS [poly(styrene-block-isobutylene-blockstyrene)], DE-128 is a flexible, 8.5mm-long tube with planar fins to help fixate the device in the tissue and prevent leakage and migration. www.santen.com
“The new CATALYS cOS 6.0 software with advanced astigmatism management is a collaboration with Cassini Technologies B.V,” said a Johnson & Johnson Vision spokeswoman. “The new software simplifies astigmatism management workflow and increases operational efficiency. Latest advancements build on the laser cataract surgery essentials that differentiate the CATALYS System, with features such as advanced visualisation that provide full-volume, 3D, high-resolution and streaming Optical Coherence Tomography imaging as well as reliable, accurate laser incisions and premium patient experience,” she said.
“Accuracy and precision in astigmatic procedures are critical to good outcomes,” said Douglas Koch MD.

“CATALYS cOS 6.0 with advanced astigmatism management not only provides more accurate surgical alignment and automatic cyclorotation compensation that is three times better than manual markings, the workflow will make the entire process easier and faster for me.”
“Building on the launch and rollout of our TECNIS Toric II platform, the introduction of our new CATALYS cOS 6.0 software will be a powerful addition to our portfolio of astigmatism management solutions,” said Rajesh K. Rajpal MD, Chief Medical Officer and Global Head of Clinical and Medical Affairs at Johnson & Johnson Vision. www.jjvision.com
NEW CHIEF MEDICAL OFFICER
Oxurion NV, a biopharmaceutical company engaged in the development of next-generation therapies to treat diabetic eye disease, with a focus on diabetic macular oedema, has announced the appointment of Grace Chang MD, PhD, as the company’s Chief Medical Officer. Dr Chang will be responsible for leading the company’s clinical programmes for THR687 and THR-149 as Oxurion looks to build a world-leading diabetic macular oedema (DME) franchise that could provide much improved therapeutic solutions for all DME patients, said a company spokeswoman.
Dr Chang joins Oxurion from Notal Vision Inc, where she held the position of CMO and was responsible for the scientific and clinical strategy, clinical development and medical affairs programmes. She is currently an Adjunct Clinical Associate Professor in the Department of Ophthalmology, Vitreoretinal Service at the University of Southern California in Los Angeles, CA, USA. Prior to this, Dr Chang held several high-level clinical and strategic roles at Alcon Laboratories following a faculty appointment at the University of Washington. www.oxurion.com
INDUSTRY NEWS 42
EUROTIMES | SEPTEMBER 2020
Douglas Koch MD
The new Chairman of the Board Andreas Schmidheini thanks Andreas Bosshard
Hydrophobic acrylic IOL
VSY Biotechnology has announced the launch of Enova, a 100% glistening-free IOL. The company says Enova is the first 100% glistening-free hydrophobic acrylic IOL that does not require pre-hydration or storage in saline solution.

VSY say the unique composition of Enova material allows uniform hydration of specific sites to have controlled water uptake and resistance to glistening formation. Glistening study was performed at the Intermountain Ocular Research Center (Mamalis/Werner Laboratory), John A. Moran Eye Center, University of Utah and the unique composition of Enova hydrophobic acrylic IOL shows no glistening compared with other IOLs.
“Enova is the first 100% glistening-free hydrophobic acrylic IOL that requires neither prehydration nor storage in saline. Enova is packaged dry and has excellent optical and mechanical properties,” said a company spokesman. “Glass transition temperature of a polymer is the temperature where the polymer changes from a rigid material to a soft material. Having a Tg -2°C, Enova IOL has gentle and controlled unfolding process below standard operating room temperatures. Thus, no warming or special conditioning is required. Low glass transition temperature (Tg -2°C) combined with its optimised modulus of elasticity, provides a high level of flexibility and controlled unfolding,” said the spokesman. www.vsybiotechnology.com
PRECISION OCT ANALYSER
“This new swept-source-based precision OCT analyser has now received CE registration,” said a company spokesman. “Haag-Streit is delighted to introduce the exciting new Eyestar 900 in various countries. Initially devices will be obtainable in some defined markets and will be widely available in October 2020.
“The Eyestar 900’s new state-ofthe-art technology enables precise measurement, as well as topographic assessment of the front and back corneal surface and the anterior chamber, including the lens, as well as providing superior imaging of all of these structures. It also includes OCT biometry of the entire eye,” the spokesman continued.
“The device is fully-automated and enables an efficient, easy to delegate workflow, with user independent measurements. The Eyestar 900 is powered by EyeSuite, the intuitive software that enables seamless integration of the device into any practice environment. The OCT analyser also includes EyeSuite IOL cataract planning software, which enables the excellent planning of cataract interventions based on latest-generation IOL calculation methods such as Hill-RBF, Barrett and Olsen,” the spokesman concluded. www.haag-streit.com

TELEMEDICINE PLATFORM WILL HELP EYE CARE PROFESSIONALS BUILD THEIR SKILLS
Santen and Orbis International has announced a partnership to develop a suite of digital training tools that will continue to help eyecare professionals around the world build their skills. Through the three-year, global partnership, Orbis and Santen will create online courses, live surgical demonstrations and artificial intelligence (AI) focused on glaucoma, a leading cause of avoidable blindness.
“Santen values the advancements that can be made through collaboration and digital learning, and especially in times like these, this partnership will be another step forward for better eyecare for millions of patients,” said Shigeo Taniuchi, President and CEO of Santen. “Digital resources and solutions are critical to ensure doctors can
provide optimal care to their patients. This partnership combines Orbis’s innovative technology in ophthalmic training and our global industry knowledge to enhance our joint mission of improving eye health for people around the world.”
“Technology has opened so many doors in our work to end avoidable blindness. This initial step in the new partnership with Santen is very significant for Orbis because it allows us to further strengthen Cybersight offerings and reach more ophthalmologists in more countries,” said Dr Danny Haddad, Chief of Programs at Orbis International. “As we increase eyecare professionals’ access to training in their local language, we are ensuring
that more patients get the quality care they deserve.”
In a joint statement Santen and Orbis said this partnership will bring together two global leaders in eye health and ensure that eyecare professionals and their patients will continue to benefit from the latest knowledge and technology. “Virtual solutions that allow for distance learning and connection have never been more important. Amid the current public health situation with the COVID-19 pandemic, record-breaking numbers of eyecare professionals have registered for Cybersight and taken advantage of the platform’s learning opportunities,” said a spokeswoman. www.santen.com, www.orbis.org
43 INDUSTRY NEWS
EUROTIMES | SEPTEMBER 2020
The Enova glistening-free hydrophobic acrylic IOL
• Reduced Registration Fees for ESCRS Congresses

• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand
Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
5 year membership for trainees Join today. www.escrs.org
ESCRS Membership FREE
Innovating in times of crisis
Lessons learnt from New York in the COVID-19 pandemic. Dermot McGrath reports
The COVID-19 pandemic has changed the world in profound ways and ophthalmic practices will need to adapt, innovate and rethink their ways of managing patients in order to make the transition as safely and effectively as possible, according to Jeffrey
Liebmann MD.
“If we think that things are going back to the status quo before the pandemic, I think that we’re mistaken. There will always be some virus in the air over the next year or two and if we seek the old status quo, we are going to fail,” Dr Liebmann said at a special COVID-19 symposium at the World Ophthalmology Congress 2020 Virtual.
Discussing the lessons learnt in New York from the pandemic, Dr Liebmann, Director of the Glaucoma Division of Columbia University Irving Medical Centre, said that his department had implemented a number of guiding principles to help aid recovery from the COVID-19 crisis.
“The first principle is to remember to continue the clinical, teaching and research missions of the department, including the highest level of expert clinical care and surgery. Many of us who are in private practice also have teaching responsibilities to our resident trainees and medical students. We have responsibilities to our fellow researchers as well, so it is important to maintain these activities,” he said.
A SAFE ENVIRONMENT
The next important measure is to ensure a safe environment for patients, faculty and staff, said Dr Liebmann.
“We all know that ophthalmologists are at much greater risk for developing this disease and we need to maintain all of our protections in place going forward. We need to ensure strict patient screening and sterilisation protocols and minimise in-person visit frequency and examination time. We cannot have the same density of patients as before, so it also increases our working hours,” he said.
Organising the workflow and clinic space with new protocols in place for social distancing and sterilisation is a complex
task that requires a lot of thought and administrative time by physicians and other staff, added Dr Liebmann.
“To solve a lot of these problems, we need to innovate, to rethink our clinical care models and explore new opportunities. We have determined that we can safely see approximately four patients per hour per doctor to maintain social distancing between patients as they enter and leave the office setting. We have our doctors working five-hour sessions, six days a week,” he said.
To try to reduce the backlog of patients, visit stratification is very important, said Dr Liebmann.
“Some patients don’t need to come in straightaway and can have a video consultation. We also have testing and procedure days that don’t involve physicians, but where patients can come in and leave the office easily. We are also changing our diagnostic testing models and we perhaps need to do more imaging than perimetry. Sterilising a perimeter is a very difficult task and is not easily done, and it is not really clear how well patients perform perimetry with masks on. We only perform dilation when necessary,” he said.
Novel drug treatments with longer-lasting effects may also help to reduce the need for office visits going forward, he added.
Every aspect of patient care needs to be re-examined and re-adjusted where necessary.
“For example, we have instigated quicker visits, where our patients come in, have imaging, get their pressure checked
followed by a patient discussion in that order rather than going into a more convoluted approach to care. We try to minimise contact and procedures as much as possible,” he said.
MAINTAINING MORALE
Rebuilding the financial strength of the practice is important by setting targets for a phased return to full activity, said Dr Liebmann. He also stressed the importance of maintaining staff and physician morale at a time of immense stress and worry.
“We have to remember that everyone is under stress – people are losing family members. The staff are worried about getting the disease from a patient and transmitting that to their families at home. These are issues we need to address and be aware of as the physician leaders – just as we take care of patients, we also need to take care of our staff,” he said.
With every crisis also comes opportunity, concluded Dr Liebmann.
“We have an opportunity perhaps to improve our care and make lemonade from all the lemons we’ve been given. We desperately need to rethink our clinical care model. This is a good time for us to really focus on what’s important. As we rebuild our financial strength to do new things, I think we should look forward to a day of different care models that will help us greatly in the future while maintaining staff and faculty morale and engagement,” he said.
EUROTIMES | SEPTEMBER 2020 PRACTICE MANAGEMENT 45
We have to remember that everyone is under stress – people are losing family members. The staff are worried about getting the disease from a patient and transmitting that to their families at home
Jeffrey Liebmann MD
A very different world
What did the ESCRS Congress look like 30 years ago?
EuroTimes Executive Editor Colin Kerr reports
Will things ever be the same again?
2020 will be remembered as the year of the COVID pandemic but the hope remains that we can return to happier times for ophthalmologists.
The world was a very different place 30 years ago in 1990. Europe was at the centre of a major change of the political landscape and in February 1990, the Communist Party of the Soviet Union voted to end its monopoly of power.
This cleared the way for multi-party elections and an agreement was reached for a two-stage plan to re-unite east and west Germany.
The 1990s were to see the redrawing of the map of Europe with the disappearance of four established states and the birth or rebirth of 14 new states.
The world of ophthalmology was also changing and in 1990 the European Intraocular Implant Lens Council, the precursor of the ESCRS, met in Dublin, the capital of the Republic of Ireland.
Dr Peter Barry, in European Society of Cataract and Refractive Surgeons – A History, recalled the meeting.
“The then President of Ireland Patrick Hillery hosted the opening ceremony in the National Concert Hall. The fact that Mr Hillery was a physician helped, but in any case it was very impressive to have the president of the country at the opening ceremony.”
Dr Peter Barry said his memory of the year is that the
meeting, held in September in Trinity College, was blessed with beautiful weather. “The sun shone all day, every day, with clear blue skies and this helped to give our visitors a magnificent impression of the city,” he says. “Everyone was astonished that you could have such a marvellous university campus with open space and playing fields and cricket fields and conference centre right in the middle of the city. It was a wonderful event.”
The organising committee for the meeting was made up of Drs Paddy Condon and Peter Barry. “It was not like the programme committee we have nowadays,” said Dr Barry. “But it was actually efficient because you could only blame one of two people if something wasn’t working. So we were on the phone to each other morning, noon and night.”
Few of the ophthalmologists attending the 1990 EIIC meeting would have had mobile phones and even fewer would have been using email or the internet.
Thirty years on the whole world has changed because of the dramatic development of mobile communications, the world wide web and social media.
So much so that the COVID-19 pandemic has led to the convening of the first ever Virtual Congress, which will be held from October 2 to October 4 2020.
And 30 years ago, who could have predicted that?
EUROTIMES | SEPTEMBER 2020 RANDOM THOUGHTS 46
Emanuel Rosen, Peter Barry, Patrick Hillery and Patrick Condon walking through Trinity College Dublin during the EIIC Congress, 1990
Illustration by Eoin Coveney
↙ LAST CALL
SEPTEMBER 2020
SFO 2020 Congress
Virtual Meeting
5 – 6 September
https://www.sfo.asso.fr/
OAS 34th Annual Scientific Meeting
Virtual Meeting
11 – 12 September
www.eyeanesthesia.org/
11th EuCornea Congress

Virtual Meeting
26 September
www.eucornea.org
WSPOS World Wide Connect 2020

Virtual Meeting
26 September
www.wspos.org
OCTOBER
38th Congress of the ESCRS




Virtual Meeting
2 – 4 October www.escrs.org

20th Euretina Congress

Virtual Meeting
2 – 4 October www.euretina.org
NOVEMBER
BEAVRS 2020 Virtual Meeting
6 November https://beavrs.org/
NOVEMBER
AAO 2020
Virtual Meeting
13 – 15 November
https://www.aao.org
/annual-meeting
100th SOI National Congress

25 – 28 November
Rome, Italy
https://www.congressisoi.com
XXI International Congress of the Brazilian Society of Ophthalmology
26–28 November
Rio de Janeiro, Brazil
https://sistemacenacon.com.br/site/ sbo2020/mensagem
DECEMBER
14th EGS Congress
14 – 16 December


Brussels, Belgium
www.egs2020.org/
CALENDAR 47 EUROTIMES | SEPTEMBER 2020
The 14th EGS Congress will take place in Brussels, Belgium
2021
JANUARY
6th Annual Congress on Controversies in Ophthalmology: Asia-Australia (COPHy AA)
29 – 30 January
Bangkok, Thailand
http://cophyaa.comtecmed.com/
FEBRUARY
25th ESCRS Winter Meeting
19 – 21 February
Krakow, Poland www.escrs.org
10th EURETINA Winter Meeting
26 – 27 February
Vilnius, Lithuania www.euretina.org
MARCH
6th San Raffaele OCT & Retina Forum
5 – 6 March
Milan, Italy https://www.octforum2021.eu/
12th Annual Congress on Controversies in Ophthalmology: Europe (COPHy EU)
18 – 20 March
Lisbon, Portugal
http://cophy.comtecmed.com/
JUNE
AECOS 2021 European Symposium
3 – 6 June
Florence, Italy
https://aecosurgery.org/ 2021-european-symposium/
46th Meeting of the European Paediatric Ophthalmological Society (EPOS)
17 –19 June

Copenhagen, Denmark https://epos2021.dk/
JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA https://aecosurgery.org/ 2020-summer-symposium/
JULY
33rd APACRS–SNEC
30th Anniversary
Joint Meeting
29 – 31 July
Suntec City, Singapore https://apacrs-snec2020.org/
AUGUST
ASCRS Annual Meeting 2021
13 – 17 August
San Francisco, USA
https://ascrs.org/news/ascrs-news/ 2021-ascrs-annual-meeting-update
SEPTEMBER
5th International Glaucoma Symposium
3 – 4 September
Mainz, Germany https://glaucoma-mainz.de/
49th ECLSO Conference
3 – 4 September
Paris, France https://www.eclso.eu/
CALENDAR 48
The 25th ESCRS Winter Meeting will take place in Krakow, Poland
Visit player.escrs.org to view all episodes EUROTIMES | SEPTEMBER 2020
2-4 October 2020
Join us for an exciting 3 day meeting broadcast live from Amsterdam, where expert speakers, chairpersons and panellists will deliver a programme covering a range of hot topics and including lively discussion and debate. Delegates can actively participate with dynamic Q&A facilities, polling and opportunities for personal connections.
Main Symposia: Programme Highlights:
ESCRS/EuCornea Symposium: Dealing with the Traumatized Cornea
ESCRS/EURETINA Symposium: Cataract Surgery in Patients with AMD
20/20 in 2020: The Lens
20/20 in 2020: The Cornea
The Next Decade of Cataract Surgery
What to Do When the Unexpected Happens
Clinical Research Symposia
Video Symposia
Ridley Medal Lecture
Heritage Lecture
Covid-19 Sessions
Free Paper Forum
Poster Village
Instructional Courses
Satellite Meetings
The meeting will include:
? !
Sessions
In addition to the scientific programme there will be an interactive 3D Exhibition, Networking Lounges + much more! For further information and registration please visit
www.escrs.org
Interactive 3D
Networking
Live Q&A
Exhibition 4 Live Streams
Lounges