Exploding the REGULATORY LANDSCAPE

Ophthalmic industry scrambles to adapt to new European medical device regulations.
ALSO IN THIS ISSUE
EuroTimes Has a New Look!
We’ve redesigned EuroTimes to be easier to read and more visually enticing.
Delivering Aid to Conflict
Zones
Dr Ogilvie-Graham reveals how innovative strategies adaptable to specific situations are key to successful delivery.
Lessons from a Prolific Career
Dr Sheraz Daya shares top insights from his experience in refractive surgery.
FEBRUARY 2023 | VOLUME 28 | ISSUE 1
PRIORITISING SAFE AND EFFECTIVE OUTCOMES COMPARABLE TO CATARACT SURGERY ALONE1
LOWESTREPORTED ECL=ENDOTHELIAL CELL LOSS; PAS=PERIPHERAL ANTERIOR SYNECHIAE.
NO REPORTS
RATES OF SIGNIFICANT ECL (>30%) & PAS IN ANY MIGS PIVOTAL TRIAL1
OF HYPOTONY, SIGNIFICANT HYPHEMA, OR CHOROIDAL HEMORRHAGE OR EFFUSION1
0.01 DECIBEL MEAN CHANGE IN VISUAL FIELD MEAN DEVIATION FROM BASELINE AT 24 MONTHS IN THE PIVOTAL TRIAL1
99 % OF EYES WERE WITHIN 1 DIOPTER OF TARGET** 2

72 % REDUCTION IN THE PERCENTAGE OF PATIENTS WITH SEVERE OSD SYMPTOMS 3

disease changes in
micro-bypass
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only.
• This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. Glaukos®, iStent®, and iStent inject® W are registered trademarks of Glaukos Corporation. All rights reserved. ©2023 PM-EU-0208
 **Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface
eyes after trabecular
stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.
**Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface
eyes after trabecular
stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.
EuroTimes Has a New Look!
Ophthalmologists know the importance of seeing clearly.
So we’ve redesigned EuroTimes to be easier to read and more visually enticing. We’re incorporating more graphics and using colour more strategically; we’re also adding more content about ESCRS and making the connection between EuroTimes and ESCRS more noticeable. Check out these and other changes in this issue—and see what a difference a new look can make!

2 Contents 06 Cover Exploding the Regulatory Landscape Ophthalmic industry scrambles to adapt to new European medical device regulations. GLOBAL 12 Delivering Aid to Conflict Zones Tom Ogilvie-Graham, Managing Director of the ESCRS UKRAINE 14 ESCRS Support for Ukraine Continues Oliver Findl MD, President of the ESCRS CATARACT & REFRACTIVE 10 Patient Safety is Paramount Concern in Regulation Overhaul José-Carlos Pastor MD, PhD 16 Lessons from a Prolific Career Sheraz M Daya MD 17 Complications with Trypan Blue Alexander Ionides MD 18 Calculating for Unusual Eyes Giacomo Savini MD 20 Micromonovision with Non-Diffractive Enhanced Monofocal IOL Elizabeth M Law PhD, MSc, MCOptom 22 Learning from Experience Liliana Werner MD, PhD CORNEA 24 Vision Correction with Corneal Inlays Michael C Knorz MD 26 COVID Through the Eye? Time Will Tell Uri S Soiberman MD 28 Intracorneal Ring Segments for Keratoconus David Touboul MD, PhD GLAUCOMA 30 New EGS Patient Project Stelios Georgoulas MD, PhD, MSc, FEBO, FRCOphth, PGDCRS 31 Treating with More Precision Ananth C Viswanathan MD, PhD RETINA 32 Finding an AMD Holy Grail Frank G Holz MD 34 Sun, Snow, and AMD Aaron Y Lee MD, MSCI PAEDIATRIC OPHTHALMOLOGY 36 How Young is Too Young? Paolo Nucci MD, FEBO 37 Keratoconus in Younger Patients Beatrice E Frueh MD EUROTIMES | FEBRUARY 2023 February 2023 | Vol 28 Issue 1
Publishers Barbara Calderwood
Mariska van der Veen
Mark Wheeler

Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
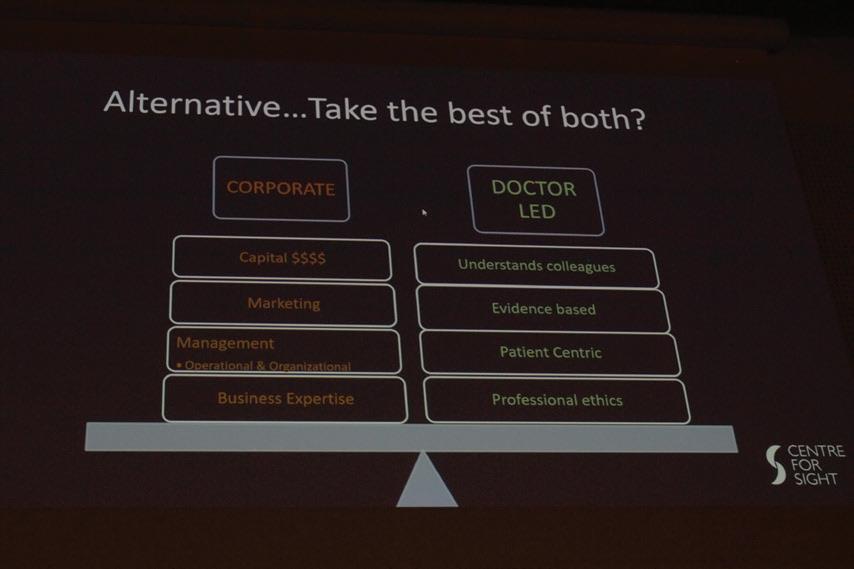
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Mariska van der Veen
Contributing Editors




Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Soosan Jacob
Leigh Spielberg
Colour And Print
W&G Baird Printers
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 roo.khan@wearemci.com
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes
ISSN 1393-8983





Learn more about EuroTimes or connect with ESCRS at ESCRS.org



3
38 BioOphthalmology: Targeting Bruch’s Membrane 40 Industry Briefs 43 JCRS Highlights 44 Leadership and Business Innovation: Who Owns Ophthalmology? 46 Inside ESCRS: Do You Know Where Your Cat Pack Comes From? 48 Book Review: There is Always More to Learn About Cataract Surgery 49 Upcoming Events Included with this Issue A Corneal Refractive Update on Lenticule Extraction Technology and Outcomes 10 12 30 18 16 2023 FEBRUARY | EUROTIMES ALSO IN THIS ISSUE
Spectres Haunting Europe
PAUL ROSEN FRCOPHTH, MBA



Aspectre is haunting Europe—a new regulatory environment that will affect every ophthalmologist working in the EU and beyond.
This issue of EuroTimes features two articles by contributing editor Dermot McGrath considering issues associated with the European Union’s new Medical Device Regulation (MDR) policy change—the biggest shake-up of the regulatory environment in the past 20 years—with a particular focus on the impact on the ophthalmic industry, ophthalmologists, and patients.
Many companies have been underprepared or underestimated the requirements of the new certification process, particularly in terms of collecting clinical data, starting a frantic scramble to obtain certification for countless legacy devices before the grace period was due to expire in May 2024. Certifying bodies are unable to cope with the demand, raising mass withdrawals of what will be uncertified products. Critics say the MDR will stifle innovation and increase costs with no guarantee of enhanced patient safety. Following a backlash, the EU Health Commissioner has proposed an extension of the deadline by a few years and cancelled the requirement for products currently on the market to be thrown out.
We would all support appropriate regulation to protect patients first and foremost, but the doctors using the devices and the manufacturers developing and selling them, too. However, any regulation must not stifle innovation and allow for the continued use and development of low monetary value, low margin but high clinical value products. We
need a form of “grandfather rights” for the orphan products we rely on for safer surgery (e.g., trypan blue), which major manufacturers do not necessarily support.
It is worth remembering what brought about the changing MDR regulations: a series of several high-profile scandals involving medical devices. A second article in this issue reviews these in detail, including toxic vitreoretinal PFO and silicone oils that left scores of people blind or severely debilitated, and how the MDR will hopefully help prevent reoccurrence.
Another very real spectre is also haunting Europe, that of the Russian invasion of Ukraine, now entering its second year. ESCRS Managing Director Tom Ogilvie-Graham features in an article discussing the realities of providing medical aid in a conflict zone.
The ESCRS will continue to support Ukraine, providing much-needed medical and surgical supplies as well as educational opportunities and financial benefits for Ukrainian ophthalmologists. We are very grateful for the continuing support we are receiving from the industry and our members. For more information on contributing, please see page 14.
EDITORIAL BOARD
INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)
Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)
Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell
EDITORIAL
Paul Rosen
4
EUROTIMES | FEBRUARY 2023
The ESCRS will continue to support Ukraine.
FULL PAGE AD NOW OPEN! Applications for the Peter Barry Fellowship 2023 are The Fellowship of €60,000 will allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year. The application deadline is 2 May 2023. For more information: escrs.org/education/grants-awards/peter-barry-fellowship
Exploding the REGULATORY LANDSCAPE
6 EUROTIMES | FEBRUARY 2023 COVER ARTICLE
industry scrambles to adapt to new European medical device regulations.
Ophthalmic
Arising from a series of damaging healthcare scandals and a widespread recognition of the need to overhaul a system no longer fit for purpose, the new European Union Medical Device Regulation (EU MDR No. 2017/745) and In Vitro Diagnostic Regulation (IVDR) represent the most significant overhaul of the EU medical device regulatory environment in more than 20 years.
Governing the production and distribution of all medical devices in the EU, the MDR entered into full force on 26 May 2021 after a one-year delay related to the COVID-19 pandemic. While the implementation of certain MDR provisions was initially to extend to May 2024 for medical devices approved under previous regulatory directives, the EU Health Commissioner proposed an additional extension following a backlash.
The implications for the ophthalmic industry in Europe are wide-reaching. The designation of medical devices encompasses a broad range of products. Surgical instruments, artificial tears, viscoelastics, intraocular lenses, corneal and scleral implants, glaucoma stents, and laser and phaco systems, among others, will all have to adhere to the new regulations or face eventual market withdrawal.
Many experts believe the stricter MDR demands will result in longer certification times and increased costs with no guarantee of improved patient safety—the ostensible reason for MDR’s introduction in the first place. In addition, the current lack of infrastructure to process device applications, and the fact many device manufacturers severely underestimated the work involved, has led to a massive backlog.
7 2023 FEBRUARY | EUROTIMES
DERMOT M CGRATH REPORTS
“Despite everyone’s best efforts, it is clear that not all products will get certified in time,” said industry veteran James V (Jim) Mazzo. “While there are mechanisms that can provide ways to maintain the flow of products to hospitals and patients until bottlenecks are resolved, if needed, the EU could also delay the implementation of some requirements.”
Time running out
As a board member of the Medical Device Manufacturers Association (MDMA), Mazzo said the medical technology industry supports responsible regulation, but the clock is running out for many device manufacturers to get their products certified in time.
“We want to make sure the regulations as implemented will be reasonable, and any dislocations will be temporary,” he emphasised. “Maintaining patient access to medical devices is critical. The EU Commission should eliminate unnecessary disruptions and impediments to achieving this goal, even if this means prioritizing or pausing the implementation of certain regulations.”
Tim Clover, CEO of ophthalmic products manufacturer Rayner, said the cost to obtain certification has been substantial, with the more stringent requirements for clinical data under the MDR stretching the resources of many companies.
“New product registrations are now much longer and require significant clinical studies—which are becoming harder to undertake, especially on older products. We hired a much bigger regulatory affairs and eye science team, invested significantly, and can confirm that all our products will be certified under MDR,” he explained. “Smaller companies or even bigger companies with small product lines will certainly withdraw products from Europe. My understanding is only 15% of the 500,000 products on the market are currently approved. The net effect will be reduced choice, higher prices, and longer innovation cycles.”
Kris Morrill, Founder and President at Medevise Consulting, said companies of all sizes massively misinterpreted the seismic shift MDR represented for the medical device industry. Notified bodies, the organisations designated in European countries to assess the conformity of certain products before market placement, are obligated to be much stricter postMDR in all aspects of certification.
“Many companies wrongly assumed having good relations with their notified body over many years would automatically carry over into the new environment,” she said. “And they were shocked when they realised this wasn’t the case. The big players have a bit more of an advantage because they can spend money to fix the situation, whereas smaller companies don’t necessarily have the resources to do so.”
Clinical data challenges
One of the key challenges, Morrill said, is the MDR puts far greater emphasis on clinical data collection than the previous regulatory process. The result is many companies lack clinical data for their legacy devices.
“In ophthalmology, very few clinical studies were ever conducted to bring products to the market. It was very unusual for companies to do. They would do them for the FDA but
would usually skip Europe,” she observed. “It is also extremely difficult to design studies for some technologies such as phacoemulsification systems because there are so many variables involved. So, figuring out what needs to be done to obtain certification is a major challenge even for bigger companies.”
Steven Bridges, an expert in European healthcare policy, said ophthalmic surgeons may not realise the full impact until they can no longer obtain a product they’ve used for years.
“If something is not fixed in the next six months, surgeons will start to increasingly find that a product they like to use isn’t on the shelf anymore. They may have to use an alternative they find less ergonomically pleasing or with less impressive clinical outcomes in their experience,” he said.
Although drawn up with enhanced patient safety in mind, politicians and policymakers did not necessarily understand the vast scale of the medical device sector and the tens of thousands of products. To try to limit the potential impact of forced product withdrawals, Bridges advised ophthalmologists play their part by raising awareness of the issues.
“Ophthalmic surgeons can bring it to the attention of their hospital CEOs or raise it with anybody they know in government about how important it is to patient outcomes that they have these ophthalmic devices on hand. [They can stress] Europe is competitive in how quickly devices come to market safely and appropriately,” he said.
Stifling innovation?
The fear of Europe losing a competitive edge through tighter regulation has been consistently flagged by business leaders

8 EUROTIMES | FEBRUARY 2023 COVER ARTICLE
If something is not fixed, surgeons will increasingly find a product they like isn’t on the shelf anymore.
ever since the EU Commission first mooted the need for stricter controls.
“The EU will always be an attractive market for industry. However, during the transition stages of the MDR, the EU market could lose some of its competitiveness and attractiveness,” suggested Mazzo. “We hope those dislocations will be temporary and addressed through streamlined regulations and processes.”
The concerted effort to ensure legacy devices attain certification may also obscure the damaging impact the MDR may have on new devices.
“Many of these new devices could be innovative and of great potential benefit to patients,” Bridges emphasised. “We are so focused on not losing legacy devices that we forget about the next generation of products.”
For ophthalmologists, a major concern is no longer having access to the latest technologies as companies shift market focus outside Europe.
“Europe will be at a competitive disadvantage,” said Arthur Cummings MD, an ophthalmologist based in Dublin, Ireland. “My practice will be at a disadvantage—and so will my patients, with a smaller choice of products for their needs. Price increases are also inevitable in this hyperinflationary period, and there are additional supply chain challenges to consider.”
The knock-on effect may be lower reimbursement rates for physicians as health systems try to curtail the overall costs of providing care. “Physicians are often the soft target, and they seldom put up much resistance,” Dr Cummings said.
Greater protection for patients?
While greater patient protection is a virtuous goal, Dr Cummings felt the EU may have overreached with the MDR. “I have a feeling the baby has been thrown out with the bathwater, and the pendulum may have swung too far,” he posited. “In the long term, the lack of innovation and timely access to appropriate technologies and therapies may be an issue with equally negative impact on patient care.”
Clover is also not entirely convinced the MDR will offer enhanced safety. “I’ve never seen any safety targets, which is odd since this is why it was introduced. I’m also not sure a large gap exists between the US and EU safety which could make this a waste of time, leading to slower innovation and substantially higher costs,” he said. “Ultimately hospitals and governments will pay for the MDR, so expect a period of rapid medical device price inflation for the next three years. Since the PIP breast implant scandal in France initiated the process, it’s worth noting the MDR would not have prevented it since it was already illegal under the MDD.”
Not everyone felt, however, that Europe will lose a competitive advantage once companies adapt to the reality of the MDR.
“It still takes twice as long to get on the market in the US for implantable devices,” said Morrill. “It’s easier for companies to blame the regulators and present a doomsday scenario of Europe losing competitiveness than admit they didn’t do their due diligence in terms of planning for the MDR.”
Morrill advises companies to embrace change and seize the opportunity the MDR represents.

“This is not going away, and we’ve got to learn to live with it. So, is it not better to learn how to work within that environment and do what needs to be done? At the end of the day, companies [will] be in a better position to have clinical data they can use for marketing and promote their clinical results,” she said. “People often fail to understand that just because you have to do something for the MDR doesn’t mean you can’t use it for other things.”
Steven Bridges is an independent public affairs professional based in Brussels, Belgium. steve@bridges.be
Tim Clover is CEO at Rayner, a UK-based manufacturer of ophthalmic medical products. timclover@rayner.com
Arthur Cummings MD is Consultant Eye Surgeon and Medical Director, Wellington Eye Clinic and Consultant Ophthalmologist at The Beacon Hospital, Dublin, Ireland. abc@wellingtoneyeclinic.com
9 2023 FEBRUARY | EUROTIMES
James V Mazzo is Executive Chairman of Neurotech, a retinal implant company and an advisor for Avellino Labs, a biotechnology and genetic science company. mazjim@me.com
Kris Morrill is Founder and President at Medevise Consulting based in Strasbourg, France. kris@medevise-consulting.com
Patient Safety is Paramount Concern in Regulation Overhaul
EU makes major policy changes where everyone stands to gain.
DERMOT M CGRATH REPORTS
The new EU Medical Device Regulation (MDR) policy should lead to greater patient protection and renewed confidence in the certification process for a wide range of ophthalmic products and devices on the market, according to José-Carlos Pastor MD, PhD.
“The scandals that occurred in recent years with certain medical devices must be avoided at all costs—firstly and most importantly for the benefit of our patients’ health and secondly for the reputation of European companies and what CE marking means,” he told EuroTimes
Although the French PIP breast implant controversy is often cited as one of the main reasons for tightened regulations, ophthalmology has had its fair share of device scandals in recent years, Dr Pastor said.
These included multiple cases of acute intraocular toxicity reported in several European countries with at least three different products after uneventful vitreoretinal surgery.
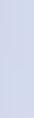
In Spain alone, some 117 cases of toxicity were reported following surgery with AlaOcta perfluoro-n-octane (PFO; Alamedics)—with patients commonly experiencing low visual acuity the day after surgery, optic nerve atrophy, and acute retinal necrosis, sometimes leading to retinal holes, relapse of retinal detachments, and retinal vascular occlusion (see https://escrs.org/eurotimes/extreme-vision-loss/ for more information).
Dr Pastor said toxicity issues with other products routinely used in vitreoretinal surgery, such as silicone oils and internal limiting membrane dyes, have also occurred in recent years.

10 EUROTIMES | FEBRUARY 2023 CATARACT & REFRACTIVE
A step in the right direction
Against this background, he believes the MDR, while not perfect, represents a step in the right direction.
“Some products may be discontinued, and some companies may have problems, but patient safety must be the primary goal of policymakers, manufacturers, and healthcare providers,” he said. “Like all rules, it may have aspects to improve and that, in certain situations, may have exceptions.”
One of the main challenges with the MDR is that the regulations may not be sufficiently flexible to differentiate between devices of vastly different complexity and function, explained Dr Pastor, citing the filter paper strips routinely used to perform Schirmer testing as an example.
“If MDR regulation is strictly applied, its accuracy and repeatability would need testing in clinical trials,” he said. “Their cost is currently around €0.24 per strip, and if companies have to pass those costs on to the final product, the market may not accept the final price. So, we really do need to find a solution for this and many other similar examples.”
Although still too early to judge the true impact of the MDR, Dr Pastor said it was important for ophthalmologists to regain confidence in the integrity of CE marking for safety.
“The scandals with medical devices in ophthalmology have created a certain rupture in confidence about the CE
117 cases
In Spain alone, some 117 cases of toxicity were reported following surgery with AlaOcta perfluoro-n-octane (PFO; Alamedics).
mark. Physicians need to be able to take for granted the safety of the products they use,” he said. “For instance, we have had some chemists manufacturing products who have proposed clinical ophthalmologists should also become experts in chemistry to better select the products we apply to our patients. Obviously, this is not the way to proceed.”
Stricter reporting
Under the MDR, stricter reporting responsibilities for companies and a EUDAMED database to share information concerning adverse events across all EU member states should help prevent a recurrence of the PFO incidents and similar cases.
When problems arose in the past, companies tended to minimise the extent of the problem or even blame the ophthalmologists for misusing the product—as with the contaminated PFO case.
“When mandated by the Spanish Agency of Medicines to analyse the possible causes of the contamination, the companies never provided us with critical data to interpret what happened,” Dr Pastor said.
The non-obligation for healthcare providers to report suspected adverse effects in all EU countries exacerbated the problem.
“Although we knew there were cases in more countries, they were not initially reported, which allowed one manufacturing company to expand the idea that toxicity was ‘a Spanish problem,’” he said.
The MDR reinforces companies’ legal responsibility and requires they have sufficient financial coverage for their potential liability.
“In the case of Alamedics, the company went bankrupt. And patient compensation, at least for those in Spain, had to be addressed mostly by the state with public funds from taxpayers. The CEO was hired again by another company and specialised in giving talks to retinologists about the ‘adverse effects’ of medical devices,” he said.
As an additional measure, Dr Pastor stressed the need for notified bodies to have specialised scientific advisors capable of evaluating whether both preclinical and clinical data a company presents really cover the safety and clinical efficacy needs it demands for that specific product.
11 2023 FEBRUARY | EUROTIMES
José-Carlos Pastor MD, PhD is a full professor and Chairman at the Hospital Clinico Universitario of Valladolid, Spain, and Advisor to the Spanish Agency for Medicine and Medical Devices (AEMPS). pastor@ioba.med.uva.es
Some products may be discontinued, and some companies may have problems, but patient safety must be the primary goal of policymakers, manufacturers, and healthcare providers.
Like all rules, [MDR] may have aspects to improve and that, in certain situations, may have exceptions.
Delivering Aid to Conflict Zones
Innovative strategies adaptable to specific situations are key to successful delivery of medical aid in regions of social unrest and war.
The successful delivery of medical aid to conflict zones requires adaptability to local conditions and a trustworthy and efficient distribution network. However, it always remains a learning process because each conflict zone is different, stresses Dr Tom Ogilvie-Graham.
“You meet a lot of people with a lot of experience in delivering medical aid in different places,” he said, “And there is a danger that you draw too much on your experience and lose that adaptability to the particular circumstances.”

He noted his involvement in bringing medical aid to conflict zones or immediately post-conflict zones in about 12 different areas. For approximately five years, he was in Palestine as the CEO of the Order of St John’s Eye Hospital Group—based in Jerusalem, where it has been since 1882. The hospital also had clinics in Hebron and Gaza and has provided remote villages with mobile outreach clinics.
“Although the distances are not that great on the West Bank, the problems of getting access are pretty severe, which also involves ferrying more difficult cases to Jerusalem for definitive treatment,” he said.
Working with a disrupted system
While Palestine presents difficulties with delivering medical aid, it has a well-established home base that has been there year on year, decade after decade. In Ukraine, by contrast, there is a disrupted economy and healthcare system, with a disappearance of nearly 200 clinics and the loss of staff.
Dr Ogilvie-Graham noted healthcare systems in conflict zones are often broken or inherently corrupt. Ukraine’s corruption prevention agency is currently dealing with 78 incidents of attempted profiteering from humanitarian aid since February 2022. Medical aid is particularly vulnerable to corruption because of its high value. He cited an instance in Iraq where he found the material they delivered to a medical facility only two days earlier was now on sale in the local bazaar.
Working through well-established, international medical aid NGOs will provide safeguards against corruption, he said. However, in conflict zones, they are often incapable of delivering specialist support where and when it is most needed. Currently, 80% of medical supplies to Ukraine come from small organisations such as ESCRS, 17% from individuals,
12 EUROTIMES | FEBRUARY 2023 GLOBAL
ROIBEÁRD O’HÉINEACHÁIN REPORTS
and only 3% from international organisations such as the Red Cross.
Dr Ogilvie-Graham noted that at an early stage of its involvement, ESCRS had the good fortune to team up with Lyubomyr Lytvynchuk MD, PhD, a vitreoretinal surgeon based in Giessen, Germany. He has provided ESCRS with a well-established network for the distribution of medical aid in Ukraine. And since he is based in the EU, he has been able to reduce the difficulties involved in importing medical materials.
“I am 100% pleased with Lyubomyr, and I believe we have made the right choice. We want to continue working with him as well as our sister society in Ukraine, of course,” he said. “ESCRS has also invited the European Society of Reconstructive Surgeons (ESOPRS), the world society of oculoplastic recon structive surgeons (WSOPRS), and EURETINA to join in this initiative so we can provide ophthalmic support beyond anterior segment surgery.”
Acquiring funding and resources
Dr Ogilvie-Graham noted ESCRS’s industry partners responded very generously to its specific requests, with more than €1 million worth of equipment distributed so far. ESCRS set up a fund in March 2022 and allocated €100,000 from its own reserves to wards Ukrainian support. Many sister societies and some ESCRS members have also contributed to this fund. ESCRS has also absorbed all related adminis tration costs into its overall budget.
Future ESCRS strategies in Ukraine may include initiatives such as telemedicine and an internation al trauma consultancy network. Telemedicine is unlikely to be of much value right now because the physicians in Ukraine’s remaining medical facilities have been dealing with the conflict since 2014. How ever, in the longer term, establishing a worldwide network of consultants could be useful—particu larly in areas such as reconstructive surgery where improvement is necessary.
In the meantime, the ESCRS is contributing to Ukrainian ophthalmic surgeon training by offering 20 observerships in host institutions across Europe, the United States, and New Zealand. It gave travel grants of €1,000 each to observership candidates to attend the 40th ESCRS Congress in Milan. The ESCRS also offered free Congress registration to 600 Ukrainian surgeons, and 300 attended in person.
“One should never underestimate the effect of mo rale,” he observed. “The fact that a European organi sation is doing something practical has an enormous effect, and the word goes around that our colleagues in Ukraine are not on their own.”
Dr Ogilvie-Graham is the managing director of ESCRS and is based in Rome. He delivered his talk at the ORBIS symposium at the 40th Congress of the ESCRS in Milan. tog@md.escrs.org
New Design Innovations that Incorporate Operator and Patient Comfort with Gentle Measurements

• Fully-automatic measurement
• Gentle voice guidance (available in 9 languages)
• Reliable tono/pachymeter
• Flexible and space-saving design
• A variety of options to meet your needs
Non Contact Tono/Pachymeter
www.nidek.com ET 93 x 266mm
ESCRS Support for Ukraine Continues

The ESCRS continues to support our Ukrainian colleagues as the war extends into its second year. Most recently, we have been coordinating the delivery of a generous donation from Dr Lee at iCare whilst Jurek Zych, the managing director of MDT Poland, has offered to supply Ahmed valves at cost price. We are also finalising observerships for one Ukrainian trainee to go to Utah, United States, and two to Auckland, New Zealand.
The 40th ESCRS Congress in Milan was very well attended by Ukrainian surgeons. The ESCRS offered free registration, and this offer was very warmly received, with 300 Ukrainian delegates attending in person and 180 virtually. The Society also provided travel bursaries for 20 Ukrainian trainees and hosted an exclusive reception.
The War Trauma session in Milan had strong support from Ukrainian speakers who were able to share their considerable knowledge and experience in this field. As the keynote speaker, Professor Ferenc Kuhn provided exceptional insight and contributed enormously to the discussion. The case studies on blast injuries alone, emphasising how frequently bilateral, complex polytrauma presents among civilians as military patients, was a stark reminder of just how damaging the war is in human terms and how impressively our Ukrainian colleagues are responding.
As the war unfortunately enters its second year, the ESCRS will endeavour to continue providing targeted support for Ukrainian surgeons. We know this will be put to the best possible use.
Our Society has established a fund to accept financial donations we will direct exclusively to support ophthalmology-related relief efforts arising from this conflict. We can accept donations to the fund from ESCRS members, industry partners, and fellow societies.
We can accept these donations through bank transfer. If you are an ESCRS member and wish to contribute, simply log in at https://donate.escrs.org using your membership details to access information on how to donate, which is a straightforward process.
For industry partners or fellow societies, please email escrs@mci-group.com for information on how to make your donation.
Oliver Findl MD, President of the ESCRS
14 EUROTIMES | FEBRUARY 2023 UKRAINE



15 2023 FEBRUARY | EUROTIMES
Our Society has established a fund to accept financial donations we will direct exclusively to support ophthalmology-related relief efforts arising from this conflict.
Drs Oliver Findl and Volodymyr Melnyk
Ferenc Kuhn at the War Trauma session
Trauma session at ESCRS Congress in Milan
Reception for Ukrainian ophthalmologists at the Milan conference
Lessons from a Prolific Career
Sheraz Daya shares insights from his long and broad experience.
CHERYL GUTTMAN KRADER REPORTS
During his decades-long career in ophthalmology, Sheraz M Daya MD has been an innovator and pioneer in refractive surgery. He reviewed his journey in the field and the lessons he learned in a keynote lecture—offering the following observation on the totality of his experience: “Surgical trends are like a fashion show—they come and go.”
Excimer laser experience
Dr Daya was introduced to refractive surgery more than 30 years ago when he learned radial keratotomy (RK) while completing a cornea fellowship. He performed RK after starting practice in the United States. Considering the multiple problems and complications associated with the incisional procedure, he was glad to be able to abandon it when he moved to England, where the excimer laser was available.
The surgeon performed his first LASIK procedure in the United Kingdom in 1994, recalling he experienced multiple flap issues while using a variety of mechanical microkeratomes in the early days of the procedure.
“The complications bothered me, and fortunately I could handle them because I was a corneal surgeon. I learned you have to be brave, and if you are going to be brave, you have to be prepared,” Dr Daya said.
He added this lesson reinforced itself when he encountered a horrifying complication involving perforation with iris prolapse when performing LASIK on top of a corneal graft.
“From then on, I always had a suture kit ready for any LASIK procedure just in case,” he said.
The introduction of the Orbscan (Bausch + Lomb) led to a new understanding of the effect of corneal shape and ectasia on refraction after penetrating keratoplasty (PK). With this knowledge, Dr Daya instead intervened with wedge resection rather than astigmatic keratotomy in many cases where the source of the problem was in the host cornea. It also led him to realise astigmatism remained in post-PK eyes after attempts to correct it with LASIK because the periphery was not ablated. From that observation, he adopted bitoric ablations and devised an effective approach for treating mixed astigmatism.
Studying the persistence of topically applied mitomycin-C (MMC) in the eye using an animal PRK model, Dr Daya and colleagues found the antimetabolite remained in the aqueous humour for up to six hours. The observation raised concern about the potential for long-term ocular toxicity, and he has continued avoiding the use of MMC for fear of contributing to what might be a public health problem. In response, he developed the transepithelial PRK approach on the Bausch + Lomb platform. It’s now incorporated in the Teneo (Technolas) laser software and works without the need for any nomogram change.
“A study of the technique is about to start in the United States, and hopefully, it will be approved for use there soon,” Dr Daya said.
Ignoring the gurus
Challenging the dogma LASIK should not be used to treat high levels of hyperopia, Dr Daya said the solution for achieving good outcomes requires creating a slow gradient of change by treating flat corneas and using a large optical zone (>6.7 mm), considering angle kappa, and avoiding an excessively deep ablation that might involve peripheral corneal nerve bundles.
In a very brief foray into conductive keratoplasty to treat hyperopia, Dr Daya said he found it induced a considerable amount of cylinder. He concluded that if the procedure can cause astigmatism, its best use may be treating astigmatism.
An early adopter of the PermaVision (Anamed Inc) synthetic corneal inlay to treat hyperopia, the innovator said he was excited by the good outcomes achieved early after surgery. However, on seeing evidence of an inflammatory reaction after evaluating inlays
CATARACT & REFRACTIVE 16 EUROTIMES | FEBRUARY 2023
explanted from eyes that developed reticular haze, he learned another lesson—the cornea does not like anything but itself.
He subsequently avoided introducing synthetic corneal inlays but went on to perform the first case of TransForm Corneal Allograft implantation in the United Kingdom.
“So far, there have been no cases of haze, and the results are stable during follow-up to three years,” Dr Daya reported.
He began implanting phakic IOLs in 2002 and learned when using the iris-fixated Artiflex lens (while a great option, he added) that patients need to be monitored closely for the potential of rapid endothelial cell loss. He avoided using any angle-supported lenses for similar reasons.
“Like others, I came to the conclusion that if a lens is too close to the cornea, it is not good.”
That same year, he also began performing refractive lens exchange on relatively clear lenses. Through his journey using different types of presbyopia-correcting IOLs, Dr Daya found patients implanted with a zonal refractive lens were unhappy with their quality of vision. Complaints were understood by reviewing their aberrometry outcomes that showed the lens could cause a coma and other unwarranted aberrations, leading Dr Daya to abandon refractive technology in favour of diffractive lenses.
Noting that he has not performed SMILE, Dr Daya said the advantages of the newest femtosecond laser used for the procedure have given him more confidence in trying it.
He concluded his lecture by summing up his philosophy in one sentence: “Disregard the naysayers, ignore the gurus, and follow the evidence.”
COMPLICATIONS WITH TRYPAN BLUE
CHERYL GUTTMAN KRADER REPORTS
The likelihood of an anterior capsule (AC) tear during phacoemulsification cataract surgery is significantly higher in cases using trypan blue for AC staining, according to a large retrospective review. It also found AC tear development is associated with a significantly increased rate of posterior capsule (PC) tear with vitreous loss.
Alexander Ionides MD reported the findings, which analysed electronic phacoemulsification cataract surgery records from a large, multicentre NHS teaching hospital trust. The researchers identified 140,930 cases of phacoemulsification performed from January 2011 to January 2021. Trypan blue was used in 1,541 (1.1%) of the 140,930 cases.
The tear occurred in 98 (6.4%) of the 1,541 cases performed with trypan blue and 1,756 (1.3%) of the 139,391 cases where the stain was not. Comparing the trypan blue group with and the group without, the 5-fold increase in AC tear rate in the former group was highly statistically significant (P <.0001).
Researchers concluded having absolute numbers regarding AC and PC tears allows surgeons to have more accurate data to provide to patients when obtaining informed consent for phacoemulsification. Dr Ionides acknowledged, however, several limitations, including the potential for selection bias and those inherent to a retrospective design.
“There may be many reasons for our finding, including trypan blue was perhaps used in more complicated cases with an increased risk of a complication anyway. [It’s also] a retrospective electronic database study. Therefore, it relies on accurate data entry and all the problems that can entail.”
Dr Ionides and colleagues Drs Osvaldo Berger and Benjamin Riley were interested in investigating whether intraoperative use of trypan blue affected the AC tear rate based on anecdotal impressions the stain affects the material properties of the anterior capsule.
“Some surgeons feel trypan blue alters the elasticity of the anterior capsule, while basic science laboratory studies have conflicting findings. We wondered if the anterior capsule stained with trypan blue is in fact more brittle and if there was an increased likelihood it would tear,” he explained.
A secondary study objective examined the risk of developing an extension of an anterior capsule tear to the posterior capsule. Data analysis showed the risk of PC tear with vitreous loss was more than 10-fold higher in eyes with an AC tear compared to those without (P <.0001).
Within the entire case series, 2,231 eyes developed a posterior capsule tear with vitreous loss. The PC tear subgroup comprised 246 (14.0%) of the 1,754 eyes with an AC tear and 1,985 (1.3%) of the 139,078 eyes without an AC tear.
17 2023 FEBRUARY | EUROTIMES
The study was presented at the 40th ESCRS Congress in Milan, Italy.
Alexander Ionides MD is a consultant ophthalmic surgeon, Moorfields Eye Hospital, London, UK. a.ionides@nhs.net
Dr Daya presented at the AAO 2022 Refractive Surgery Subspecialty Day in Chicago, US.
Sheraz M Daya MD is the Medical Director, Centre for Sight, London, UK. sdaya@centreforsight.com
Calculating for Unusual Eyes
Better predictability with new IOL calculation formulas.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Eyes with unusual optical dimensions are at a higher risk for refractive surprise following cataract surgery, but newer intraocular lens calculation formulas can reduce that risk, said Giacomo Savini MD.

“The latest generation of IOL calculation formulas reduces the risk of refractive surprises, especially if you have optimised constants,” he said. “And our wish is that new biometers will include the formulas so we can have them on the printout, which would make everything easier.”
Influence of risk factors on formulas
Dr Savini noted keratometry values of less than 42.0 D or more than 46.0 D increase the risk of refractive surprises with many of the older IOL calculation formulas. Using the SRK/T, prediction accuracy sharply diminishes as the K value deviates from average values (42.0–44.0 D), with myopic errors in eyes with steep corneas and hyperopic errors in flat corneas.
The accuracy of other formulas is also influenced by keratometry values, although to a lesser degree. In eyes with flat K, using Holladay 1 and 2 can result in a hyperopic error, but using Haigis can result in a myopic error. In eyes with steep keratometry, using Haigis and Olsen can result in a hyperopic error.
All eyes with values less than 2.75 mm or more than 3.50 mm in anterior chamber depth (ACD) are at increased risk of refractive surprises. Using the old formulas in such eyes— which don’t account for ACD—can result in myopic error in eyes with shallow ACD and hyperopic error in eyes with deep ACD. The Barrett and Haigis formulas reduce this risk because they account for ACD, as do EVO, Kane, and Hoffer QST, he explained.
In eyes with an axial length shorter than 22.0 mm, only around half of cases will achieve postoperative refraction within 0.50 D of the target value with all the older formulas.
That compares to around three-fourths of eyes with more average proportions. There also appear to be no significant differences between the formulas in predictive accuracy.i
Dr Savini cited recent research showing that the latest generation formulas have greater predictive accuracy in short eyes—including Kane, Naeser 2, Olsen, VRF-G, Castrop, Okulix, and Pearl-DGS.ii–iii
Old formulas with no axial length adjustment tend to result in hyperopic errors in long eyes and tend to result in myopic errors with axial length adjustment. Barrett, Olsen, and Haigis achieve the highest accuracy in long eyes.iv Better outcomes with newer formulas include Barrett Universal II, EVO 2.0, and Hoffer QST.v
“The ESCRS IOL calculator is a good option because it only requires users to enter the data once. And it will perform the calculation from seven formulas that have all shown greater accuracy than standard IOL formulas available on biometers, as well as the Barrett II formula,” Dr Savini said. “However, even with the newer formulas, and even among average eyes, one in four or five will have a postoperative error of more than half a dioptre.”
This paper was presented at the 40th Congress of the ESCRS in Milan.
giacomo.savini@startmail.com
i Gokce et al, JCRS, 2017; 43: 892.
ii Voytsekhivskyy et al, Curr Eye Res, 2021; 12: 1832.
iii Wendelstein et al, BJO, 2022; 106: 795.
iv Melles et al, Ophthalmol, 2018; 125: 169.
v Shammas et al, JCRS, 2022; 48(10): 1113–1120.
18 EUROTIMES | FEBRUARY 2023 CATARACT & REFRACTIVE
Giacomo Savini MD is an ophthalmologist in private practice in Bologna, Italy, and a researcher at the GB Bietti Foundation – IRCCS in Rome, Italy.

10–12 MARCH 2023 TIVOLI MARINA, VILAMOURA ALGARVE 27 th ESCRS WINTER MEETING PORTUGAL 20 23 wintermeeting.escrs.org REGISTRATION NOW OPEN
Micromonovision with Non-Diffractive Enhanced Monofocal IOL
Lens using positive spherical aberration yields spectacle independence for some.
HOWARD LARKIN REPORTS
Most patients implanted bilaterally with a new non-diffractive enhanced monofocal intraocular lens targeting micromonovision ended up with good distance and intermediate vision, and many achieved spectacle independence.
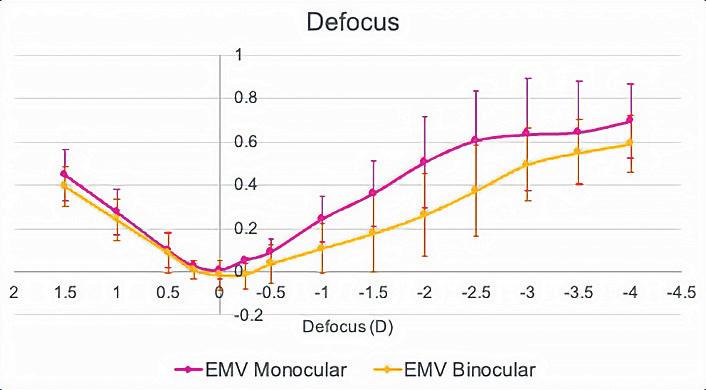
The results came from a retrospective study of the first 30 patients bilaterally implanted with the Rayner RayOne EMV IOL, which uses positive spherical aberration to stretch the focal distance. Patients were assessed 12 to 15 months postoperatively. Mean age was 69 years, reported Elizabeth Law PhD, MSc, MCOptom.
Dominant eyes were targeted for emmetropia, and non-dominant eyes for -0.75 D to -1.25 D. Patients’ previous experience with monovision determined the myopia level targeted in the non-dominant eye. Those without monovision experience were targeted closer to -0.75 D, while those with experience closer to -1.25 D, Dr Law said.
Good distance vision
In the dominant eye, mean uncorrected distance visual acuity was 0.12 ± 0.10 logMAR (or about 20/25), while it was a little better than 0.30 (0.28 ± 0.14, or about 20/40) in the non-dominant eye. Binocular uncorrected distance vision was 0.07 ± 0.06 logMAR. Mean corrected distance vision was better than 0.0 (or 20/20) monocularly and binocularly, Dr Law reported. However, “nobody wore spectacles for distance vision even though it was slightly better corrected, and none were unsatisfied.”
The study allowed patients with up to 1.0 D corneal astigmatism to be implanted, which may explain why mean distance vision improved with correction, Dr Law said.
“Perhaps we were not quite stringent enough in treating astigmatism in these patients.”
69 years
Patients were assessed 12 to 15 months postoperatively. Mean age was 69 years, reported Elizabeth Law PhD, MSc, MCOptom.
Intermediate and near vision
Not surprisingly, mean uncorrected intermediate vision was significantly better in the non-dominant eye and binocularly than in the dominant eye, coming in at better than 0.2 (0.18 ± 0.14) in the non-dominant eye and binocularly (0.15 ± 0.12), and a little better than 0.4 in the dominant eye. As expected with micromonovision approach, near performance was slightly less than intermediate, with a mean of about 0.3 (0.32 ± 0.16) in the non-dominant eye and binocularly (0.28 ± 0.16), and about 0.5 for the dominant eye (0.53 ± 0.10).
The binocular defocus curve was also better than monocular performance, yielding a mean uncorrected visual acuity of better than 0.2 from +0.75 D to -1.50 D for the micromonovision approach, Dr Law said. There were no reports of dysphotopsias in the group.
“We certainly have achieved an extended range of focus,” she said. “A lot of our patients are spectacle independent.” She disclosed she is doing a longer-term study of the same lens, sponsored by Rayner.
Dr Law presented her findings at the 40th Congress of the ESCRS in Milan.
Elizabeth M Law PhD, MSc, MCOptom, is lead optometrist and researcher at Southend University Hospital, Mid and South Essex NHS Trust, and BMI Southend Private Hospital, both in the United Kingdom. elizabeth.law6@nhs.net
20 EUROTIMES | FEBRUARY 2023 CATARACT & REFRACTIVE
Spherical aberration extends depth of focus in non-diffractive lens.
Learn more at ESCRS.org

21 2023 FEBRUARY | EUROTIMES
To be the leading community and trusted source for science, education, and professional development in the fields of cataract and refractive surgery.
Learning from Experience
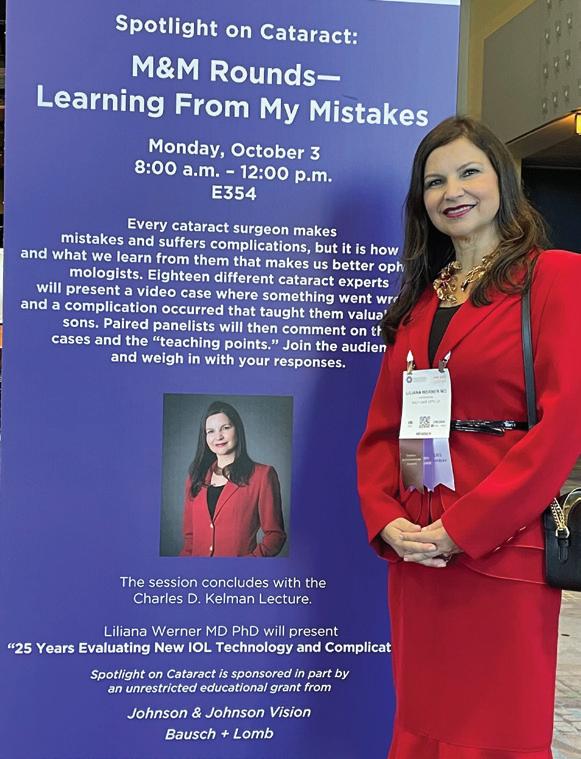
Liliana Werner recalls 25 years of ophthalmology findings in AAO Kelman Lecture.
HOWARD LARKIN REPORTS
As a PhD student a quarter century ago, Liliana Werner MD, PhD made an important discovery about a Teflon coating applied to polymethyl methacrylate (PMMA) intraocular lenses (IOLs). In vitro, the highly hydrophobic coating showed significant antiadhesive and antiproliferative action against lens epithelial cells (LECs), presumably discouraging posterior capsule opacification (PCO).
“However, when we implanted the coated IOLs in rabbit eyes, it became quite evident other factors may play a role in PCO prevention, such as the IOL design,” Dr Werner said in her Charles D Kelman Lecture “25 Years Evaluating New IOL Technology and Complications” at the American Academy of Ophthalmology 2022 annual meeting in Chicago, US. She is the first woman selected to deliver the prestigious talk.
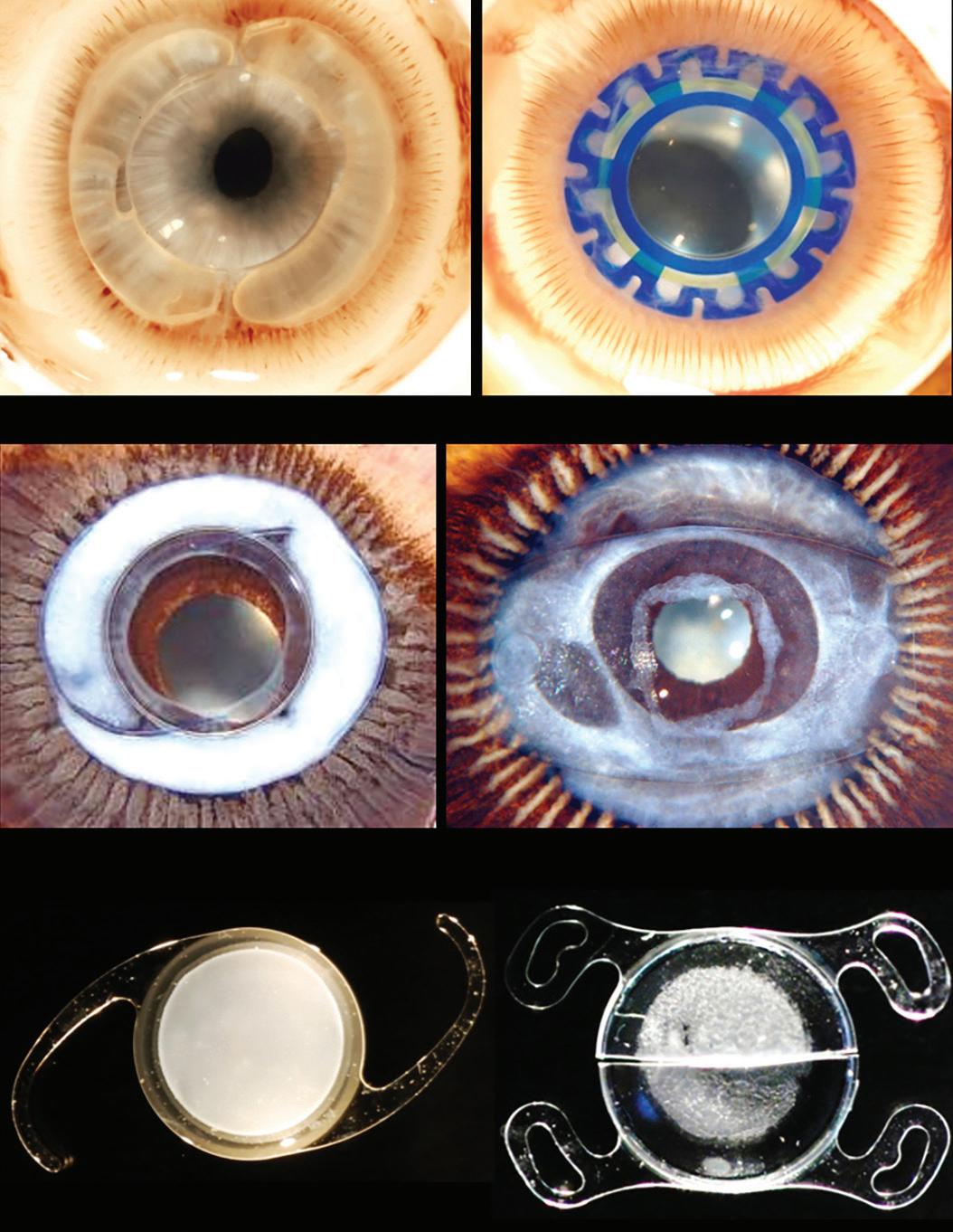
The discovery proved just the start of a series of pioneering studies using in vivo animal models, cadaver eyes, and explanted IOLs (Figure 1) that often yielded surprising findings. Insights generated by the work of Dr Werner and her colleagues guided much of the materials, design, and implantation methods seen in today’s most advanced techniques and devices.
Controlling PCO
After earning her PhD with a thesis based on discouraging PCO with antiadhesive materials, Dr Werner joined David J Apple MD’s ophthalmic pathology lab, where one of the first studies she was involved with tested the opposite hypothesis—promoting the adhesion of the capsule with a monolayer of LECs to bio-adhesive IOL surfaces could prevent further cell proliferation. Similar research later helped bring down PCO even with microincision IOLs notorious for high rates, she said.
With standard IOLs, though, a square edge on the posterior surface proved to play the most prominent role in PCO prevention, Dr Werner said. Cadaver eyes demonstrated that lenses with sharp posterior edges discouraged PCO regardless of material.
Dr Apple’s six factors to prevent PCO summarised this research. Three factors are surgery-related: hydrodissection-enhanced cortical clean-up, in-the-bag IOL fixation, and capsulorhexis smaller than the IOL optic diameter. And the other three are IOL-related: biocompatible materials to reduce LEC proliferation stimulation, contact between the IOL optic and the posterior capsule, and a square IOL optic edge. Using these allows for the capsule to shrink-wrap around the optic of lenses with a more standard design.
However, further research with a bag-filling dual-optic silicone lens showed keeping the bag open and expanded allowed for circulation of aqueous humour within the capsular bag, Dr Werner said. Recently, an open-bag silicone modular accommodating lens showed no PCO in a rabbit model and out to 12 months in human patients.
On the other end of the spectrum, the bag-in-lens—in which the twin capsulorhexes edges fit into a groove around the IOL optic—also completely prevents PCO by sequestering residual LECs in the closed bag around the periphery.
22 EUROTIMES | FEBRUARY 2023 CATARACT & REFRACTIVE
Figure 1: The bulk of Dr Werner’s work involves pre-clinical in vivo studies in rabbit eyes (top) and studies using human eyes obtained postmortem (middle) and IOLs explanted all over the world (bottom).
Other studies are necessary to fully understand the aetiology and manifestations of this complication.
Explanted IOLs
Dr Werner has participated in many studies of explanted IOLs, notably looking for reasons some hydrophilic acrylic lenses tend to calcify. Multiple factors may be at play, some related to manufacturing and packaging using silicone products and others patient-related.

Silicone lens calcification occurs on the posterior optic surface in eyes with asteroid hyalosis. They often reaccumulate, even after partial removal with Nd:YAG laser. The impact on light scatter, light transmission, and modulation transfer function are clinically significant, requiring explantation, Dr Werner said.
Opacification of silicone lenses within a few hours of implant occurred thanks to industrial cleaning and fumigant chemical contamination, which Dr Werner found may have been caused by improper storage. Analysis of some lenses explanted due to toxic anterior segment syndrome (TASS) revealed the presence of ointment used after implantation coating the corneal endothelium and the silicone IOL optic.
Dr Werner examined hydration-related issues in hydrophobic acrylic lenses in which fluid-filled vacuoles known as glistenings form. However, she said glistenings and subsurface nanoglistenings do not affect light scatter and light transmittance enough to require explant in most cases. More recent hydrophobic acrylic lenses with higher water content, ranging up to 4.9%, are much less subject to this phenomenon.
“I could confirm that some of these materials are glistening-free,” she said.
Analysis of explants due to late in-the-bag dislocations showed an association with pseudoexfoliation, uveitis, myopia, pars plana vitrectomy, and other conditions causing progressive zonular weakening rather than any IOL material or design issue. Lenses implanted with a capsule tensioning ring may dislocate sooner, though this may partially be due to the selection of patients with existing zonular problems and additional stress during implantation of the ring itself, Dr Werner noted.
This year Dr Werner and team published on dead bag syndrome, in which the capsular bag becomes diaphanous, floppy, and unable to support the IOL. Analysis of the specimens included in this first study showed scarce or no LECs or proliferative or fibrotic capsule changes, but delamination of the capsule at the zonular attachments.
“Other studies are necessary to fully understand the aetiology and manifestations of this complication,” she commented.
In conclusion, Dr Werner outlined three lessons she learned from 25 years of research on IOL design, materials, and technique. First, keep an open mind because today’s idea may become the next disruptive technology. Second, use a thorough scientific process to ensure clinical practice can safely adopt new ideas. Third, constant vigilance is required to detect and learn from IOL complications, so reporting and analysing them is essential to protect patients—the goal of her life’s work in ophthalmology research.
iLEARN
ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
23 2023 FEBRUARY | EUROTIMES
Liliana Werner MD, PhD is professor of ophthalmology and visual sciences and co-director of the Intermountain Ocular Research Center at the Moran Eye Center of the University of Utah, Salt Lake City, US, and associate editor of the Journal of Cataract and Refractive Surgery . liliana.werner@hsc.utah.edu
Vision Correction with Corneal Inlays
Technique remains a work in progress despite a long history of attempts.
CHERYL GUTTMAN KRADER REPORTS
The first implantation of a synthetic corneal inlay for vision correction was in 1972, but all the devices developed since then have failed to deliver satisfactory results. Could allografts do better?

“It is time to try something different,” said Michael C Knorz MD.
The synthetic corneal inlays used for vision correction can be divided into three generations, categorised by material. The first synthetic corneal inlays were polymethylmethacrylate, and both the vision and safety outcomes with these devices were unsatisfactory. Corneal melts developed in some eyes, and although the inlays are removable, the inlay procedure was not reversible because corneal scarring remained.
The next generation of corneal inlays were hydrogel devices. This group included the 5-mm PermaVision inlay (Anamed) introduced in 1999 for the treatment of hyperopia—available
for two years—and the 6-mm Cougar inlay from 2000, available for just six months.
Presenting his personal experience using the PermaVision inlay, Dr Knorz said that after an initial overshoot, the refractive outcomes were fairly stable during two-year follow-up. However, the refractive predictability was not very good. At one and six months postoperatively, the achieved refraction was within 0.5 D of attempted in only about two-thirds of eyes and within 1.0 D in about 80% of eyes.
In addition, the device had an unacceptable safety profile. Fifteen percent of eyes lost two or more lines of BSCVA, and multiple complications developed at relatively high rates. Inlay decentration greater than or equal to 1 mm occurred in 19% of eyes, and haze occurred in 86%. Twenty-nine percent of patients reported moderate halos and glare. Severe halos and glare affected 38% of patients.
CORNEA 24 EUROTIMES | FEBRUARY 2023
After an initial overshoot, the refractive outcomes were fairly stable during two-year follow-up.
“Almost half of the inlays had to be explanted,” Dr Knorz said.
Follow-up at the slit lamp showed the inlay appeared to be well-tolerated early after implantation, but deposits were visible at the edges by 6 months, and the device basically encapsulated by 12 months. The implants were removable, but the topography changed from its preoperative state, and corneal scars were present.
The third generation of synthetic inlays were developed for presbyopia treatment: the polyvinylidene difluoride KAMRA (AcuFocus), the Raindrop hydrogel (ReVision Optics, recalled in 2019), and the hydrophilic acrylic Flexivue (Presbia). Only Flexivue is still on the market, available in a limited number of countries.
Discussing the KAMRA inlay, Dr Knorz said it was implanted in more than 20,000 eyes after receiving US FDA marketing approval. The procedure was associated with satisfactory vision results, and many patients who received it kept it. Dr Knorz and colleagues examined the outcomes of ten patients who underwent KAMRA removal and found the topography was reversible in 60% of cases.
“The flip side is that 40% of eyes had a permanent change in topography, and we saw persisting scars that caused scattering of light,” Dr Knorz said.
60%
Dr Knorz and colleagues examined the outcomes of ten patients who underwent KAMRA removal and found the topography was reversible in 60% of cases.
Will allografts do better? Clinical trials are investigating several allograft corneal inlays, including the TransForm corneal allograft (Allotex) prepared from sterile human donor corneas and PEARL (PrEsbyopic Allogenic Refractive Lenticule), which uses lenticules obtained from SMILE procedures.

Dr Knorz presented at the 40th ESCRS Congress in Milan.
Michael C Knorz MD is a professor of ophthalmology at the University of Heidelberg, Germany. He is also the Medical Director of the FreeVis LASIK Centre in Mannheim, Germany. knorz@eyes.de
ESCRS Academies
Committee representatives of ESCRS organise and present sessions at meetings organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies promoting and sharing benefits across both memberships.
escrs.org/education/academies/
COVID Through the Eye? Time Will Tell
Current information shows eye as an uncommon site of pathology.
CHERYL GUTTMAN KRADER REPORTS
Although SARS-CoV-2 RNA has been detected in tear and conjunctival samples from patients with COVID-19, ocular findings in patients with the virus are uncommon, showing it unlikely the eye is a portal for the infection, current research indicates.
“We do not see a lot of eye disease in patients with COVID-19. However, ophthalmologists do not see many patients at the time of acute illness,” noted Uri S Soiberman MD.
“It is very possible that COVID-19 could cause conjunctivitis, and eye disease is more prevalent in severely ill patients. Perhaps SARS-CoV-2 also causes secondary inflammation in the eye or very late-onset disease. These are unanswered questions. Only time will tell.”
The lack of relevant studies with large numbers of patients has hampered a better understanding of the potential for SARS-CoV-2 to cause eye disease. An early paper from China reported 12 of 38 patients hospitalised for COVID-19 had conjunctivitis.
“Most likely, however, the patients had chemosis only, which is something expected in severely ill patients,” Dr Soiberman said.
One paper reviewing 500 patients admitted to the hospital for COVID-19 pneumonia found that fewer than 10% had ocular surface signs or symptoms. Based on findings from a literature review of 28 papers, conjunctivitis appears to be the most common COVID-19-related eye disease, but its prevalence is likely below 5%, Dr Soiberman said.
The eye as an entry point
Discussing literature addressing whether the eye is a portal for SARS-CoV-2 infection, Dr Soiberman noted some conflicting information from studies investigating the presence of viral RNA in ocular surface cells.
An early case report from the Wilmer Eye Institute (Johns Hopkins University, Baltimore, Maryland, US) showed SARSCo-V-2 detected by real-time polymerase chain reaction (RTPCR) in ocular surface swabs from a patient with COVID-19, while a large study from another institution found ocular surface specimens from patients who died of COVID-19 tested positive for the virus. The latter group also showed SARSCoV-2 could infect cultured human embryonal stem cell-derived ocular epithelium, suggesting the ocular surface could be a portal for viral entry.


However, another group reported negative RT-PCR virus testing in a series of postmortem eyes of patients who died from COVID-19, and researchers using RT-PCR to test tear and conjunctival secretions in patients with confirmed COVID-19 pneumonia reported a positive result in only about 3% of cases.
An early study conducted in China, Dr Soiberman said, showed a lower proportion of inpatients with confirmed COVID-19 wore eyeglasses daily for more than eight hours compared to the general population, suggesting the eye could be a portal of viral entry. In addition, studies show ocular surface cells express the surface receptors necessary for SARSCoV-2 binding and internalisation.
Stronger evidence for SARS-CoV-2 possibly infecting human conjunctiva comes from a study where researchers transduced fresh conjunctival tissue from healthy patients with the virus in an ex vivo model. After 48 hours, the fixed specimens stained positive for the SARS-CoV-2 nucleoprotein.
“Although this finding suggests the eye is a portal, the staining was mainly in the deeper layer of the conjunctiva versus in the superficial layer, as we might expect. In addition, the increase in COVID-19 transcript 48 hours after transfection was not that dramatic,” said Dr Soiberman.
“Furthermore, some animal studies suggest the conjunctiva is not the site of penetration into the body. Instead, the entry occurs through autoinoculation from the conjunctiva to the respiratory mucosa.”
CORNEA 26 EUROTIMES | FEBRUARY 2023
Dr Soiberman presented at AAO 2022 in Chicago, US.
Uri S Soiberman MD is an assistant professor of ophthalmology at the Wilmer Eye Institute, Johns Hopkins University, Baltimore, Maryland, US. usoiber1@jhmi.edu
Although this finding
suggests
the
eye
is a portal, the staining was mainly in the deeper layer of the conjunctiva versus in the superficial layer, as we might expect.
Our IOL Calculator is now live on the ESCRS website!

This first-of-its-kind web application for IOL power calculations uses multiple modern formulas simultaneously, and suggests lens constants for a wide range of IOL models. Find out more at iolcalculator.escrs.org/
27 2023 FEBRUARY | EUROTIMES
Intracorneal Ring Segments for Keratoconus
Implants offer benefits with good safety.
CHERYL GUTTMAN KRADER REPORTS
The use of intracorneal ring segments (ICRS) to reduce corneal steepening and astigmatism associated with keratoconus has grown since first proposed by Joseph Colin MD in 2000. Performed worldwide in more than 500,000 eyes, several companies are now marketing intracorneal rings/ring segments for treating keratoconus.
“Experience confirms the procedure is safe, and the rings are very well-tolerated in the long-term. In addition, a meta-analysis of published reports of more than 4,500 eyes found ring implantation has a large positive effect for improving both uncorrected and corrected distance visual acuity. Currently, ring insertion cannot be considered as a refractive surgery procedure for keratoconus,” said David Touboul MD, PhD.
“Still, further technological refinements and combined strategies are pending to make this modality even more reliable and efficient for targeting emmetropia. More and more often, ring implantation is being combined with cross-linking, phototherapeutic keratectomy, phakic IOLs, or IOLs to limit progression of keratoconus and treat anisometropia.”
Mechanisms and outcomes
Ring insertion into the deepest layers of the corneal stroma induces a local curvature inflexion, resulting in corneal flattening. This effect amplifies with the device’s increasing thickness and is inversely proportional to the corneal diameter at the implantation site.
Although corneal biomechanics would be expected to change with the corneal curvature induced by the rings, biomechanics parameters measured with various elastographic devices are unchanged.
“Stress redistribution should occur and could explain a trend seen in some studies for the rings to inhibit keratoconus progression,” Prof Touboul said. “However, inhibition of eye rubbing by patients who fear the manipulation will cause ring extrusion may also play a role in limiting disease progression.”
He noted the keratometric outcome of the surgery is more predictable in eyes with low keratoconus stages than in those with more advanced disease. Functionally, however, eyes with stage 2 and 3 keratoconus derive greater benefit since eyes with forme fruste or stage 1 have better visual function at the time of surgery and greater risk for BCVA loss.
Surgical planning
Nomograms for ICRS implantation are mostly based on anterior topographic pattern and refraction, which are controversial and imperfect for failing to consider many parameters.
“The most important things to know are corneal flattening is increased by symmetrical implantation, greater ring
thickness, narrower channels, more superficial implantation, and the smaller diameter in the cornea where the device is implanted decreases,” he explained. “Astigmatism is reduced by making the incisions on the steepest meridian, inserting rings on the flattest meridian, and using the smallest arc length.”
He noted symmetrical implantation also addresses defocus and aspheric aberration, while asymmetrical implantation addresses comatic aberration. Combining ring insertion with topoguided photokeratectomy can also dramatically decrease coma if enough tissue is available. Additionally, newer ring designs are useful for correcting coma and astigmatism.
Satisfactory safety
Research so far indicates the overall rate of complications with ring insertion is less than 5%. The problems include keratitis, epithelial ingrowth, extrusion, hydrops, migration/decentration, and breaks.
“To the best of our knowledge, no large studies had follow-up longer than 5 years after implantation. But to date, there is no epidemic of ring exchange, migration, or extrusion after almost 20 years of use worldwide,” Prof Touboul said.
Extrusion risk factors include superficial ring implantation, excimer laser enhancement, eye rubbing, and atopy. Although late extrusion is very rare, he cautioned it is a concern.
“Extrusion can occur spontaneously with few symptoms, and it must be treated quickly with ring removal. Corneoplastic patching has been tried, but it is not easy,” he said.
Ring implantation for keratoconus has also been associated with photic optical aberrations, especially in patients with large pupils implanted with rings at a small diameter in the cornea. Patients usually describe the symptoms as very different from the halos or glare experienced the night before ring surgery and typically tolerate them well, thanks to neuroadaptation.
Literature reports the removal of less than 5% of implanted rings. The procedure is easy if done within the first few months after implantation and allows for exchange with or without a new channel. Later removal is more challenging but usually beneficial, even though fibrosis around the ring may prevent complete restitution of the previous corneal shape.
“Ring placement will not compromise the ability to perform deep anterior lamellar keratoplasty if it becomes necessary,” he added.
CORNEA 28 EUROTIMES | FEBRUARY 2023
Prof Touboul presented at the 40th Congress of the ESCRS in Milan.
David Touboul MD, PhD is an ophthalmologist at the University Hospital of Bordeaux, France. david.touboul@chu-bordeaux.fr
Research. Education. Innovation.
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

New EGS Patient Project




Europe-wide survey of glaucoma patients indicates shortcomings in care.













ROIBEÁRD O’HÉINEACHÁIN REPORTS























The European Glaucoma Society (EGS) has initiated a new patient project designed to seek glaucoma patient views and foster a more patient-centred approach to treating their disease.
“We started this project for many reasons,” explained Stelios Georgoulas MD, PhD, MSc, FEBO, FRCOphth, PGDCRS. “We want to better understand our patients’ needs and how these differ across Europe. Currently, patients are significantly underrepresented in decisions taken for them. We, therefore, aim to increase patients’ involvement and public awareness and identify unmet needs.”
At the time of Dr Georgoulas’ presentation, the EGS had received responses from 402 patients from 20 of 27 European countries. Roughly two-thirds of the respondents were UK residents; the next highest proportion of patients were from Germany and France. The respondents ranged in age from 21 and 90 years, with most between 60 and 70 years old.
Dr Georgoulas noted that 353 (85.1%) respondents said they had received a glaucoma diagnosis, while the rest were either glaucoma suspects or ocular hypertension patients.
Among the glaucoma patients, 79.3% used drops, 43.2 % had laser treatment sometime during their treatment, and 45.6% had ocular surgery as part of their treatment.
Regarding the psychological impact of the glaucoma diagnosis, most patients reported no impact. However, 98 respondents said they experienced negative psychological impact, including 24 who mentioned fear of blindness, 24 who mentioned anxiety, and 14 who mentioned depression.
In terms of satisfaction with their glaucoma knowledge, 81% of respondents said they were satisfied. However, they also complained that due to lack of simple explanations of their condition and restricted access to consultants, they had to independently source the information. Patients reported the information they received in hospitals focused only on clinical aspects of treatment but not secondary prevention and behavioural aspects.
Most respondents (83.8%) said they were satisfied with their level of glaucoma care. The negative aspects mentioned included long wait times between appointments, long wait times in hospitals, and rushed consultations. In addition,
30 EUROTIMES | FEBRUARY 2023 GLAUCOMA
some patients did not think they were offered all options regarding their treatment. Some also complained about the lack of specialised centres for childhood glaucoma in some parts of Europe.
Some of the common challenges associated with treatment reported by the respondents with a glaucoma diagnosis included struggling to stabilise their disease (20.9%), difficulty with the side effects of their eyedrops (15%), and difficulty remembering to apply their medications (13.4%).
Dr Georgoulas noted one surprise finding regarding local patient support organisations. Although many are available throughout Europe—and four out of five respondents believe such organisations would be useful—only around half were aware of their existence, and about a third received information or participated in the events.
This study was presented at the virtual World Ophthalmology Congress.
TREATING WITH MORE PRECISION
ROIBEÁRD O’HÉINEACHÁIN REPORTS


Genomic analys is offers the prospect of personalised glaucoma management, said Ananth C Viswanathan MD, PhD, but achieving that goal will involve a gradual process involving big data and empirical outcomes.
“It is already changing our practice, and we are on a journey where it will change our practice for the benefit of our patients.”
He noted the evidence base for genotype analysis in glaucoma management is still in its early stages. A review of the literature he co-authored with Anthony P Khawaja indicated genetic testing on a population level is not currently justified.i Furthermore, the latest EGS guidelines advise against offering routine genetic testing to POAG patients.
“It might seem genomics does not have a great deal to do with glaucoma management, but evidence is rapidly accumulating that genomic information can be very helpful,” Prof Viswanathan explained.
As an example, he cited a study involving participants of the Ocular Hypertension Treatment Study (OHTS). It showed the risk allele in the TMCO1 gene (related to intraocular pressure) had a higher hazard ratio for conversion to glaucoma than any of the previously identified risk factors, including central corneal thickness, vertical cup-to-disc ratio, visual field defect, and IOP itself.ii
“The OHTS risk calculator has now been modified to take account of this. That means if you use the calculator, you are using genomic information,” he said.
Another approach uses a multi-trait analysis of glaucoma risk variants across the genome, putting them together to form a polygenic risk score (PRS). A study involving optic nerve photographs of 67,040 UK Biobank participants showed those in the top PRS decile had a 15-fold increased risk of developing advanced glaucoma compared to the bottom decile.iii

Precision Medicine
Prof Viswanathan noted genomic analysis will be a valuable tool in developing precision medicine, an approach to disease treatment and prevention that considers the variability in an individual’s genes, environment, and lifestyle.
“We are already using genomics for biomarkers to guide our management of the condition in a number of areas—all of which have a crucial role in glaucoma management.”
He explained its development as an iterative process, starting with a broad stratum of diagnostic and prognostic groups. Then, as information accumulates on how risk factors influence disease and treatment outcomes, treatment protocols gradually refine.
“It is not as if we are going to go from nothing to full precision medicine by the flick of a switch,” he observed. “It will develop gradually.”
This paper appeared at the virtual World Ophthalmology Congress.
Ananth C Viswanathan MD, PhD is based at NIHR Biomedical Research Centre, Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, London, UK.
i Khawaja et al, Nat Eye, 2018; 32: 877–883.
ii Scheetz et al, Ophthalmology, 2016; 123(12): 2527–2536.
iii J E Craig et al, Nat Genet, 2020; 52: 160–166.
Stelios Georgoulas MD, PhD, MSc, FEBO, FRCOphth, PGDCRS is a consultant ophthalmic surgeon at Cambridge University Hospitals, UK. He specialises in adult and childhood glaucoma and cataract surgery. stylianos.georgoulas@addenbrookes.nhs.uk
Finding an AMD Holy Grail
Ongoing European study searches for intermediate AMD markers.
DR GEARÓID TUOHY REPORTS
With 700 patients enrolled and well underway, the European MACUSTAR project aims to develop novel clinical endpoints for those with intermediate age-related macular degeneration (iAMD).
There is a significant unmet need for treatment options in both early and intermediate AMD. While there are some valuable treatments for late-stage non-neovascular AMD (i.e., geographic atrophy)—using particular agents to slow the progression of the disease—the “holy grail” for a therapy in the ophthalmic community is a process to intervene earlier in the pathology, preventing the later stages of the disease and, thus, minimising visual loss.
The MACUSTAR project will characterise the functional deficits in iAMD and develop and validate functional, structural, and patient-reported outcome measures. Additional goals include investigating risk factors for progression from iAMD to late AMD, according to Frank Holz MD.
As there may be no universally accepted clinical endpoints for early or intermediate stages of the disease, Professor Holz commented that accomplishing this goal might be challenging. Designing, using, and measuring the “right endpoints,” therefore, will be imperative for MACUSTAR.
“Measuring a patient with intermediate AMD with BCVA would not be helpful, as it may maintain for a long period
until it crashes into late-stage disease development,” he explained. “So we need other endpoints accepted by the regulatory authorities to test interventions in these earlier stages.”
MACUSTAR investigators across Europe are assessing methods for structural, functional, and patient-reported outcome tests; reliable test/retest processes; and how the community can differentiate between different neighbouring disease states and how these may change over time.
The project covers this gap in the research work to develop key outcomes supported by expert academic, clinical, and commercial organisations. MACUSTAR will follow more than 700 AMD patients over three years, using state-of-theart imaging techniques, vision testing, and patient-reported outcome measures that capture the disease’s impact on quality of life.
The continent-wide project has 20 clinical sites to date. Each site collects data including mean and point-wise retinal sensitivities on scotopic/mesopic fundus-controlled perimetry, low-luminance visual acuity (LLVA), low luminance deficit, Moorfields Acuity Chart visual acuity, dark adaptation absolute threshold and rod intercept time, and several more assays. Sites also collect patient-reported low-luminance functioning.
One of MACUSTAR’s valuable research outcomes so far is further validation of the “Vision Impairment in Low Luminance (VILL) questionnaire”, which captures visual functioning and vision-related quality of life (VRQoL) under low luminance, low-contrast conditions relevant to AMD.
The relevance of this work only increases as other existing patient-reported outcome instruments do not fulfil regulator development requirements or sufficiently capture AMD patients’ difficulties. The new VILL questionnaire now supports the psychometric performance of patients, including internal consistency, item fit, subscale structure, test/retest reliability, and construct validity in a multinational, multilanguage setting. Prof Holz noted this research could impact clinical research, practice, and policy in the future.
The Innovative Medicines Initiative (IMI), with support from the European Commission and the European Federation of Pharmaceutical Industries and Associations (EFPIA), funds the €16.2M project—scheduled to complete in spring 2024 after running for approximately 6.5 years.
For more information on MACUSTAR, please visit www.macustar.eu
RETINA 32 EUROTIMES | FEBRUARY 2023
Prof Holz spoke at the 22nd EURETINA Congress in Hamburg.
Frank G Holz MD is Chair of the Department of Ophthalmology at University Hospital Bonn, Germany. frank.holz@ukb.uni-bonn.de
ESCRS AT A GLANCE
We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With over 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.
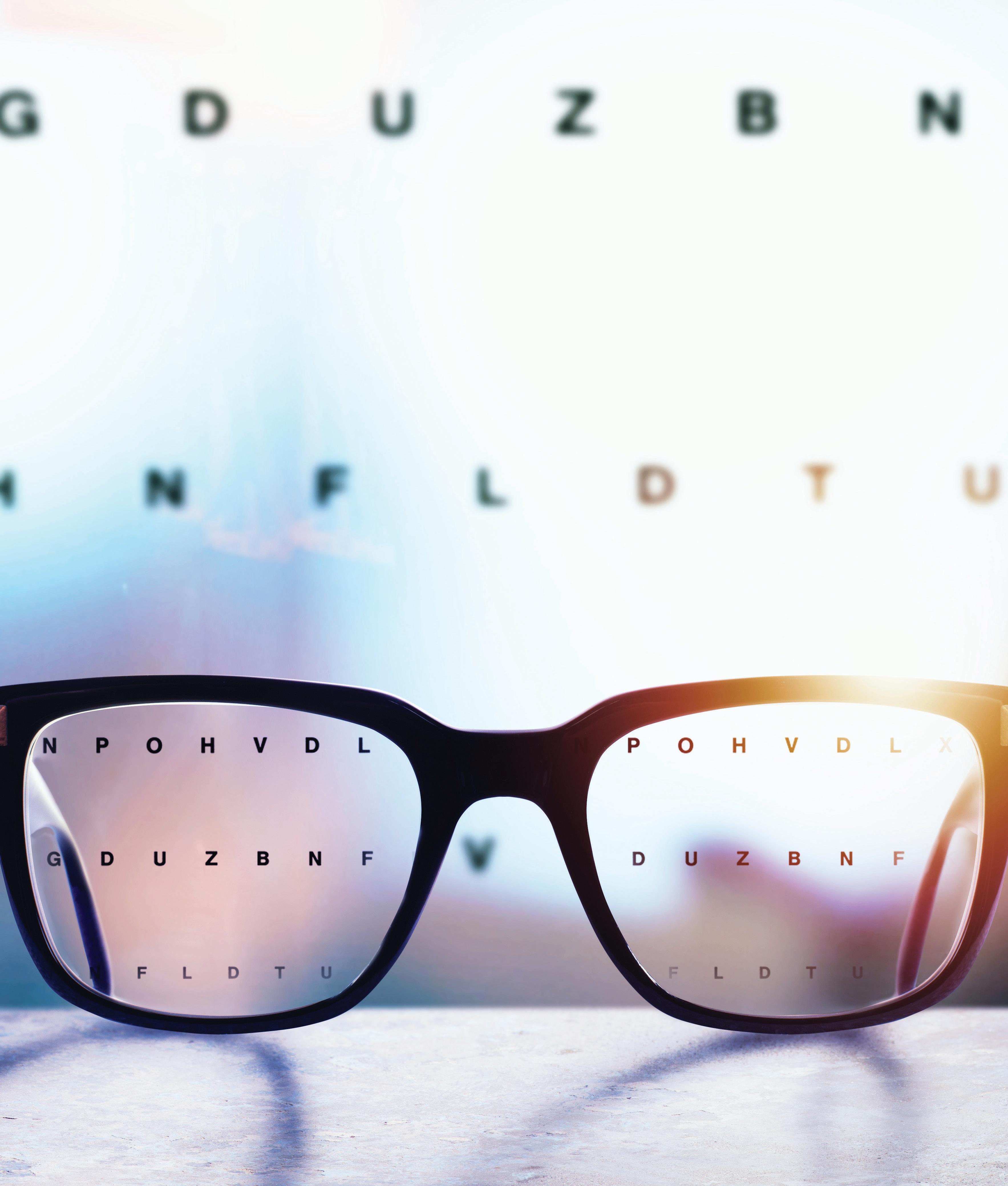
Sun, Snow, and AMD
“Big Data” sheds light on environmental factors and AMD.
DR GEARÓID TUOHY REPORTS
An American study involving nearly ten million people reveals some intriguing findings on the potential role of environmental factors and the risk for age-related macular degeneration (AMD).

Aaron Y Lee MD, MSCI presented research analysing environmental data to assess these risk factors. The study investigated natural environmental exposures with exudative and non-exudative AMD across the United States, particularly environmental data obtained from public sources, including the US Geological Survey, National Renewable Energy Laboratory, National Oceanic and Atmospheric Administration, and Environmental Protection Agency.
Essentially, there was no bigger “big data” than everything under the sun, and this study showed sunlight and latitude were significantly associated with active exudative AMD. Two pollutant variables—ozone and nitrogen dioxide—also showed positive associations. While the statistical outcomes were relevant, clinical relevance of the associations may require further assessment
The study reviewed the types of environmental factors associated between participants in four groups: no AMD, dry AMD (non-exudative AMD), inactive wet AMD (inactive exudative AMD), and active wet AMD (active exudative AMD). Dr Lee collected almost ten million participants from the IRIS database, which provides large-scale, population-level data across the United States, capturing disease diagnoses, patient demographic information, and multiple ocular health metrics.
The literature shows both genetic and environmental factors likely to contribute to AMD development and progression. Sunlight, or solar irradiation, is measured in Global Horizontal Irradiance (GHI), which is all radiation striking a flat surface from the sun. This solar irradiance is measured in watts per metre squared in SI units.
Describing key demographic data for each patient group, Dr Lee said of the patients included without AMD, the majority were female (58%), the most common race was White (69%), the mean age was 68 years, and interquartile range (IQR) was 62 to 74. Pseudo/aphakic patients (21%) were less common than phakic patients, and patients with a history of smoking (37%) were less common than non-smokers.
“Compared with the study population, the patients with non-exudative AMD, inactive exudative AMD, and active exudative AMD had a higher proportion of women (60%, 58%, and 59%, respectively),
RETINA 34 EUROTIMES | FEBRUARY 2023
The literature shows both genetic and environmental factors likely to contribute to AMD development and progression.
Whites (80%, 83%, and 87%, respectively), pseudo/ aphakic patients (33%, 37%, and 37%, respectively), and smokers (43%, 50%, and 55%, respectively),” Dr Lee said. “And they tended to be older (mean age 75 years, IQR, 69 to 80; 77 years, IQR, 71 to 81 years; and 77 years, IQR, 72 to 81, respectively).










“Our analysis confirmed previous reports that demographic factors such as sex and ethnicity are strongly correlated with AMD because many of these factors were significantly correlated in all three models,” he reported. “Our analysis further revealed significant associations between several environmental variables and the risk of active exudative AMD, including latitude, solar irradiance, and pollution.”
The environmental associations differed between the AMD subtypes, with the risk of developing any AMD versus no AMD significantly associated only with inches of winter snow and ozone, and the risk of developing any exudative AMD versus all non-exudative AMD not significantly associated with any environmental factors. In environmental pollutant assessments, the study also indicated a contribution of the risk of developing AMD, particularly ozone and nitrogen dioxide.
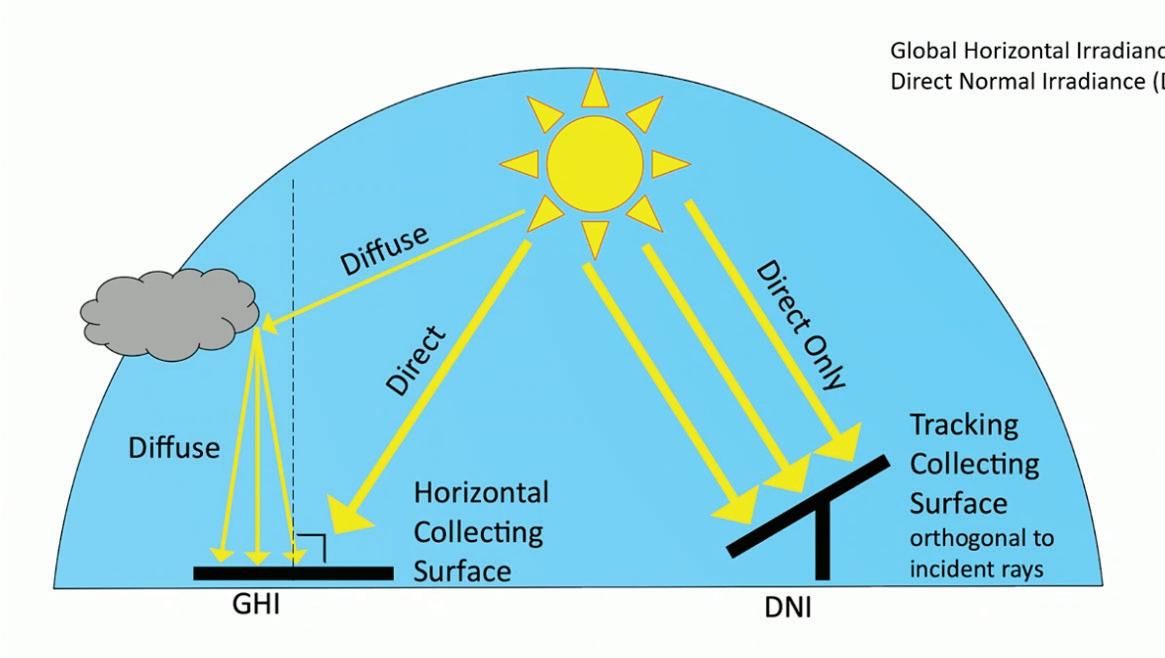
“The deleterious effects of these pollutants arise, in part, from inducing oxidative stress in affected tissues,” he noted. “This mechanism may also contribute to disease progression in AMD, and the findings presented here highlight several promising directions for further research aimed at identifying the mechanisms that contribute to AMD.”
Dr Lee presented his findings at the 22nd EURETINA Congress in Hamburg.
& ASTIGMATISM CORRECTION REINVENTED











35 2023 FEBRUARY | EUROTIMES
The schematic indicates the Global Horizontal Irradiance (GHI) and the Direct Normal Irradiance (DNI), presented by Dr Aaron Lee.
1)
paper: Evaluation of a new toric IOL optic by means of intraoperative wavefront aberrometry (ORA system): the effect of IOL misalignment on cylinder reduction. By Erik L. Mertens, MD Medipolis Eye Center, Antwerp, Belgium 2) The misalignment tolerance and the use of segments instead of concentric rings reduces photic phenomena, helping patients to adapt more naturally to their new vision. 3) The central zone of 1.4 mm in diameter is larger than most available mIOLs and allows a wider tolerance so that the visual axis passes through the wider central segment avoiding visual disturbances. 4) In cases of tilt or misalignment, the patient can still benefit from good near and far vision, as the segmented zones allow a balanced far/near light distribution in a steady optical platform. OPHTEC | Cataract Surgery REDUCE GLARE & HALOS1 TOLERATE THE KAPPA ANGLE2 TOLERATE DECENTRATION 3 TOLERATE MISALIGNMENT 4 CTF/TCT optic designed to:
Aaron Y Lee MD, MSCI is an assistant professor, department of ophthalmology, University of Washington, Seattle, US. aylee@vision.wustl.edu
Broader Toric meridian designed to be more tolerant of misalignment. White
PRESBYOPIA
How Young is Too Young?
The challenge of congenital cataract surgery.
CLARE QUIGLEY MD REPORTS
Delivering the keynote lecture at the World Society of Paediatric Ophthalmology and Strabismus Subspecialty Day in Milan, Italy, Paolo Nucci MD, FEBO discussed congenital cataract surgery, important paradigm shifts, and his current approach.
He began with a case illustrating the impact congenital cataract surgery may have on a patient. A six-month-old child underwent a late operation for a congenital cataract. The operating surgeon implanted a multifocal lens in the sulcus. The resulting poor vision led to a referral to Prof Nucci for rehabilitation. He removed the lens implant, and the corrected vision improved from 20/400 to 20/200 with the help of occlusion therapy directed by the orthoptist. Unfortunately, the child had a severe trauma to the good eye, which was eviscerated. So, what happened to the bad eye? Following this catastrophic injury, the child’s vision unexpectedly improved, reaching 20/50.
“Maybe we know less than we believe about congenital cataract,” Prof Nucci proposed. “The first question is whether the time window for unilateral and bilateral surgery is appro-
priate. Many ophthalmologists follow a strict time window of four to six weeks of age, but this could be revised later with important benefits to operated children. The problem with aphakic glaucoma is strictly related to earlier surgery. Maybe four to six weeks is a little bit early.”

He currently employs a strict patching regime to stretch surgery time, shifting the window for congenital cataract surgery to 8 to 12 weeks in unilateral and 10 to 14 weeks in bilateral.
“Keep in mind the child has interrupted waking hours and sleeps a lot,” Prof Nucci advised.
Parental monitoring, he said, is crucial, and patching should be part time, carried out for a portion of the time the infant is awake. Monitoring is harder during the neonatal stage, as waking hours are so few.
Prof Nucci suggested creating nuances for each step of congenital cataract surgery, including dilation, the main incision, and the rhexis approach. An off-label intracameral preparation that includes tropicamide, phenylephrine, and lidocaine (Mydrane®, Thea Pharmaceuticals) can dilate. He recently
36 EUROTIMES | FEBRUARY 2023 PAEDIATRIC OPHTHALMOLOGY
published how he found it provides good dilation in infants without safety concerns and is completely reversible with intracameral acetylcholine.i
In constructing incisions, Prof Nucci spares the superior cornea, carrying out cataract surgery from a temporal approach to help preserve different options for future glaucoma surgery for these patients, which one in four will go on to have.
Many surgeons can be nervous to perform capsulorhexis on infants due to the more elastic nature of the paediatric lens capsule, but Prof Nucci counselled going forward with this step.
“If you use the correct dilation and correct viscoelastic, I can say the capsulorhexis is very, very easy,” he emphasised. “Aim for a smaller capsulorhexis. Aim for a small opening in the capsule [because it] will be larger than your target. A high molecular weight viscoelastic is required. Giving care and attention to the forces at play allows a controlled manual rhexis. The movement is always centripetal.”
Regarding when to implant a lens, Prof Nucci advised between ages eighteen months and two years and using a posterior approach with a 2.5 mm to 3.0 mm port.
And what about a primary implant at a very young age? It’s a procedure he doesn’t recommend in infancy.
“The number of complications when I do this surgery under age six months is relevant. Also, there is no possibility to accurately calculate the lens.”
Prof Nucci also does not advocate for multifocal lens implantation in young children.
“We should aim for a hyperopic target. Perfect centration is quite difficult. Movement and tilt, even after months from surgery of a multifocal lens cause problems. Also, children’s eyes have unpredictable axial growth, and their reading distance is closer than that of adults,” he explained. “The one advantage, which is of course not an advantage at all, is children don’t complain. So, when problems such as glare, loss of contrast, and low vision quality arise, the ophthalmologist may not hear about it.”
KERATOCONUS IN YOUNGER PATIENTS
DERMOT MCGRATH REPORTS
Although a general screening for keratoconus in the paediatric population is not warranted, a targeted screening may be indicated in the groups at greatest risk, according to Beatrice E Frueh MD.
“It might make sense to screen certain groups, such as children whose parents or other family members have keratoconus, some ethnic groups, children with Down syndrome, and children with more than two dioptres of astigmatism,” she said.
“Keratoconus is rare in children, but we should be aware young children compensate better for vision loss and may not complain about it,” Dr Frueh explained. “Progression of the disease is much faster in paediatric populations, so early detection is important. Furthermore, we have a viable treatment option in cross-linking, which has shown safe and effective in halting the progression of the disease in paediatric patients.”
Discussing the known risks for keratoconus development, Dr Frueh said surgeons need to consider genetic and ethnic factors.
The reported prevalence of keratoconus in adults is 1 in every 2,000 individuals (0.05%). About 10% of paediatric patients diagnosed with keratoconus have a positive family history of the disease. Some ethnicities are affected more than others, with studies finding a higher incidence of 0.9% to 3.3% among people in Asia and the Middle East. One study from the United Kingdom showed those of Asian origin (Pakistan, India, Bangladesh) living in the English Midlands had a 4.4 higher incidence of keratoconus than the overall population. Another study of 522 patients ranging from 6 to 21 years old in Saudi Arabia found a prevalence of 4.79%.
Studies have found varying frequencies of keratoconus in persons with Down syndrome. A study from Norway drawing on national patient registry data found a prevalence of 5.5% in this subgroup which is around 30 times the estimated keratoconus prevalence in the general Norwegian population. Another recent study in which 98 athletes with Down syndrome attending the 2017 New Zealand Special Olympics National Summer Games were screened found between 30% to 39% had keratoconus, depending on the criteria used.
While screening is a proven means of identifying an unrecognised disease in individuals without signs or symptoms, Dr Frueh said there are some disadvantages associated with its deployment.
i Nucci P, Lembo A, Caputo R, Dellavalle A, Serafino M, Schiavetti I, Pichi F, “Efficacy and safety of intraoperative use of tropicamide 0.02%/phenylephrine 0.31%/ lidocaine 1% intracameral combination during pediatric cataract surgery”. Intl Ophthalmol, 2022 Sep 2. doi: 10.1007/s10792-022-02501-4. Epub ahead of print. PMID: 36053475.
“It is time-consuming and expensive to implement, and there is always a risk of overdiagnosis,” she said. “Patients may ignore symptoms later on if the results are normal.”
Summing up, Dr Frueh said there was a convincing case for targeted screening in the population groups she highlighted.
“Retinoscopy is a valid alternative to topography and tomography for screening. We should also remember that screening can be negative in young children, but keratoconus may still develop later,” she concluded.
37 2023 FEBRUARY | EUROTIMES
Dr Frueh presented at the 40th Congress of the ESCRS in Milan.
Beatrice E Frueh MD is an ophthalmologist at University Hospital Bern, Switzerland. beatrice.frueh@insel.ch
Paolo Nucci MD, FEBO is Full Professor of Ophthalmology at University of Milan and Director of the Nucci Eye Clinic in Milan, Italy. paolo. nucci@unimi.it
TARGETING BRUCH’S MEMBRANE
Three therapeutic approaches targeting Bruch’s membrane under evaluation.
BY DR GEARÓID TUOHY
Speaking at the 22nd EURETINA Congress in Hamburg, Germany, Dr Maximillian Pfau discussed three therapeutic approaches targeting Bruch’s membrane: vitamin A supplementation, removal of Bruch’s membrane deposits, and a surgical bypass process using a choroid Bruch’s membrane RPE patch.
Bruch’s membrane provides a structural support and attachment for the retinal pigment epithelium (RPE), a semi-permeable filtration barrier that provides metabolic exchange between these layers. Nutrients pass from the choriocapillaris through Bruch’s membrane to reach the RPE and the photoreceptors. Cellular breakdown products may travel in the opposite direction. Diffusion through Bruch’s membrane depends on the local concentration of salts, glucose, and pH.
The membrane is 2 µm to 4 µm thick for adults and can change in thickness, ultrastructure, and histochemistry with age and disease. Changes are associated with the accumulation of material thought to derive from the highly metabolically active RPE, where it functions as the “household calvary” to degrade photoreceptor outer segment (OS) shed tips. The undigested end products are collected by phagocytosis and subsequently fuse with long-term phagosomes and the breakdown materials. These are then recycled and extruded through the basal surface of the RPE into Bruch’s membrane before diffusing into the choroidal circulation. With age and disease, the level of waste materials may lead to drusen formation in age-related macular degeneration and other disorders.
Adding vitamins
One approach Dr Pfau told delegates was a supplementation strategy that essentially pushes vitamin A through the choroid and Bruch’s membrane, even in the context of degenerating layers, to provide as much vitamin A as possible via elevating blood levels. Sorsby fundus dystrophy patients in Philadelphia,
Pennsylvania, US, first received this therapy, whereby vitamin A supplementation used approximately 50,000 units for one month—and it provided significant improvements in the dark adaptation (DA) kinetics.
A similar approach using vitamin A for late-onset retinal degenerative (L-ORD) patients showed a comparable improvement in DA kinetics. A further study with Pseudoxanthoma elasticum (PXE) patients, with a progressive calcification of elastic fibres, also showed moderate vitamin A levels could improve similar DA kinetics.
In healthy aged eyes and eyes with early AMD, a landmark trial by Cynthia Owsley and colleagues demonstrated small improvements are attainable with high-dose vitamin A supplementation. And while the effect size of the study was small and many of the eyes in the cohort had relatively healthy retina,
38 EUROTIMES | FEBRUARY 2023
BIOOPHTHALMOLOGY
With age and disease, the level of waste materials may lead to drusen formation in age-related macular degeneration and other disorders.
patients showed a number of improvements. Lastly, Dr Pfau mentioned a current study with an intermediate-AMD group—conducted at the US National Eye Institute (NEI, PI: Catherine A Cukras MD, PhD)—using a moderate and high dose supplementation with vitamin A is expected to publish its results soon.
Cleaning up the mess
A second strategy is a potential therapeutic treatment aimed at clearing up Bruch’s membrane with a deposit removal approach, using both an exogenous and endogenous process.
The endogenous strategy (“stimulating repair”) applies a nanosecond laser treatment to up-regulate proteases and thin the membrane. LEAD study (NCT01790802) results reported no significant effect on slowing AMD progression for the relevant endpoints (adjusted hazard ratio [HR], 0.61 [0.33–1.14], p = 0.122). Dr Pfau added that the post-hoc analyses of the trial
suggest a therapeutic window for using laser treatment depending on the stage of disease.
The exogenous process, on the other hand, uses apolipoprotein (apo) A-I mimetic peptides (e.g., L-4F). These short helical peptides (18 amino acids; molecular weight, 2.31 kDa) may emulate anti-atherogenic properties of apoA-I (243 amino acids, 28.3 kDa), and these amphipathic peptides sequester lipids for travel through aqueous environments. The L-4F has reported binding with high-affinity oxidized phospholipids and fatty acid hydroperoxides in cellular membranes and is well tolerated by humans, providing an attractive strategy for targeting Bruch’s membrane lipids and soft drusen. This approach targets thinning the Bruch’s membrane and, in preliminary preclinical work, has shown the clearing up of neural lipid, esterified cholesterol, and membrane attack complex.
Dr Pfau reported this particular mimetic peptide approach is not under clinical consideration this year, but others have potential in the future. Regardless, this was just one peptide, and there may be new or improved compounds in the pipeline.
A last resort
The last strategy is what Dr Pfau commented as the “last and most drastic” therapeutic option—a surgical bypass.
“It’s mostly obsolete these days, and is a strategy for having a full choroid/ Bruch’s membrane/RPE patch, explanting that from the peripheral retina and moving it below the fovea to save the fovea from further degeneration.”
Prof Bernd Kirchhof, now retired, presented this surgical approach approximately 15 years ago in Cologne, Germany. One follow-up patient had an intact patch with a reasonable visual acuity measurement of 0.4 logMAR, indicating some level of function.
There are multiple approaches targeting the barrier at Bruch’s membrane. Short-term vitamin A supplementation may be effective to restore rod-mediated dark adaptation, which the results of an ongoing trial should reveal in due course.
“For the vitamin A trials, there is clearly a signal there, but it’s a little
Vitamin A supplementation can provide significant improvements in dark adaptation kinetics.
Post-hoc analyses suggest a therapeutic window for using laser treatment.
bit difficult to understand [the data],” Dr Pfau told delegates. “They enrolled patients with different disease stages, and it’s unclear at what disease stage vitamin A provides the best benefit or if it is more for a short diagnostic test.”
The LEAD clinical study did not provide an effective outcome for nanosecond laser treatment to date, although there may be an appropriate therapeutic window for this approach. Notably, such a new trial examining nanosecond laser again is currently in the planning stages. For the apoA-I mimetic peptides, again, the outcome to date has only progressed to the preclinical stages, but new iterations in lab studies could address peptides in the future.
Finally, autologous transplantation of a choroid Bruch’s membrane RPE patch is successful for selected patients. “But there is no evidence that the benefit on average outweighs complications,” Dr Pfau concluded.
39 2023 FEBRUARY | EUROTIMES
Maximilian Pfau MD, PhD is the Head of the Visual Neurophysiology Platform, Institute of Molecular and Clinical Ophthalmology Basel (IOB), Switzerland. maximilian.pfau@iob.ch, maximilian.pfau@nih.gov
The L-4F provides an attractive strategy for targeting Bruch’s membrane, well tolerated by humans.
Rayner creates outcomes app
Rayner announced the global launch of RayPRO+, a free smartphone app that collects patient-reported outcomes for up to three years after cataract surgery. Patients register in the surgeon’s office—where the surgeon records the type of lens implanted—and then answer a few questions on their satisfaction, spectacle independence, dysphotopsia, and follow-up procedures. Using the RayPRO+ dashboard the surgeon can then analyse the responses and trends about patients, clinics, and IOLs. The company suggests the app can be used for several purposes, including peer comparison, clinical studies, and promotion of surgical services to new patients.
www.rayner.com
Ocular corticosteroid nanoemulsion
Salvat Laboratories announced the submission of NDA documentation for a new drug application to the US FDA for approval of Clobetasol. It would be the first ocular corticosteroid formulated in a nanoemulsion for inflammation and pain in patients undergoing eye surgery. The Spanish company has created a proprietary nanoemulsion technology it says enhances drug penetration and bio-adhesion while enhancing patient comfort. In clinical trials, the drug had no rebound effect two weeks after treatment. The product does not need to be shaken because the nanoemulsion ensures a consistent concentration.
Svt.com
OK for Omlonti
Santen announced US FDA approval of Omlonti® (omidenepag isopropyl ophthalmic solution) 0.002% eyedrops for reducing elevated intraocular pressure in patients with primary open-angle glaucoma or ocular hypertension. Omidenepag isopropyl, the active pharmaceutical ingredient, is a relatively selective prostaglandin EP2 receptor agonist, which increases aqueous humour drainage through the conventional (or trabecular) and uveoscleral outflow pathways. It is currently the only product with this pharmacological action, the company said.
santen.com
Nidek launches non-contact tono/ pachymeter
Nidek has launched an innovative non-contact tonometer/pachymeter, the NT-1p. The device automates reliable non-contact tonometry and pachymetry. After the patient puts their chin on the chinrest, the NT-1p recognises the eye position automatically and starts measuring without a user prompt.
The product offers flexibility via a variety of options. There are models with and without joysticks. The newly designed joystick’s four-direction button provides seamless movement of the measurement device, while the addition of handheld control and tablet control software allows for remote operation. nidek.com
New dry eye treatment advances
Aldeyra Therapeutics took a step closer to US FDA approval of reproxalap, its novel drug candidate intended for dry eye disease treatment. The company submitted a new drug application (NDA) based on extensive clinical trial data. This would be the first approval of a RASP (reactive aldehyde species) modulator, a family of small molecule targets that affect a broad array of protein mediators.
www.aldeyra.com
40 EUROTIMES | FEBRUARY 2023
INDUSTRY BRIEFS

Educational Resources Advanced FEBOS-CR Exam/Diploma (Cataract and Refractive Surgery) ESCRS iLearn • ESCRS Research Portals • Important Publications ESCRS EuroTimes Podcasts • ESCRS on Demand • JCRS Online Case Reports The Video Journal of Cataract, Refractive, and Glaucoma Surgery escrs.org/education/educational-resources

Access the latest articles, presentations, podcasts, webinars, and videos. Find where and when the latest events, meetings, and conferences are happening. ESCRS.org
Research | Education | Innovation
Data modelling with decision trees and multiple regression analysis identified the contributions personality traits made. Low neuroticism and high extraversion were the primary personality contributors for men, while in women, all traits contributed. Women had higher expectations for postoperative distant acuity than men (0.1 vs 0.2 logMAR) to present high satisfaction. Both groups showed openness, conscientiousness, and extraversion as contributors to optimal satisfaction.
N Panagiota et al., “Impact of personality on the decision process and on satisfaction rates in pseudophakic presbyopic correction”, 48(12): 1433–1439.

43 2023 FEBRUARY | EUROTIMES EYE SURGERY. SWISS
Not available for sales in the US *Oertli data on file
MADE.
WHO OWNS OPHTHALMOLOGY?
As investors move in, surgeons may be well advised to band together.
 BY HOWARD LARKIN
BY HOWARD LARKIN
In the wake of COVID-19, ophthalmology is undergoing a profound shift in practice patterns. Private equity companies and large clinic groups are rapidly buying up independent, surgeon- or partnership-owned practices. Many acquirers are international, including Ramsay of Australia and Aier of China, or regional, such as Miranza in Spain, Artemis Augenkliniken in Germany, Optegra in the UK, and EuroEyes across Europe.
It’s not hard to see the attraction. Over the past two decades, rapid—and expensive—technology advances have made ophthalmology one of the most capital-intensive of medical specialties, leaving new surgeons hard-pressed to strike out on their own and retiring surgeons unsure of how they can cash out. And COVID-19 shutdowns showed just how vulnerable even established practices are to financial shocks.
“So, the question is, do we jump on the consolidation train, or do we continue as we are?” asked Sheraz M Daya MD in the Practice Management programme at the 40th Congress of the ESCRS in Milan.
For Dr Daya, the answer comes down to why he founded his private clinic—to care for patients the way he felt best, work in an enjoyable environment without compromise, and master his destiny. Compared with public practice or working itinerantly in corporate-owned clinics, he sees ophthalmologist-owned or directed clinics as better able to achieve critical quality goals, including safety, timeliness, effectiveness, efficiency, equity, and patient-centeredness.
But quality also depends on consistent execution, which requires access to capital, business knowledge, leadership skills, and effective operational management. These are strengths experienced corporate managers can bring.
“I think there can be a happy marriage between the corporate role—who bring money, marketing skills, knowledge of
management and building teams, and business expertise—and doctors, who understand colleagues and the value of giving patients what they need based on evidence and professional ethics,” Dr Daya said. “They can work together toward the same goals.”
Motives matter
Dr Daya pointed out private equity investors generally are not interested in patient care, per se, but in making profits buying and selling companies, which he finds unsustainable. But if a group came along that was interested in partnering to solve the problems of public health systems and financing, “I’d be there in a flash, because then we’d be seeing eye-to-eye. I’m optimistic things will change.”
In many ways, the current private equity boom echoes the practice management company wave in the US in the 1990s, said Kris Morrill, a management consultant. After buying practices for 15 to 20 times annual revenues, most of these deals collapsed. The firms had no experience running medical practices, and the theorised economies of scale never materialised. That most of the deals were transacted in stocks instead of cash was only reason some doctors didn’t lose their practices. “It was a Ponzi scheme,” she said. However, some firms currently consolidating ophthalmic practices are not traditional private equity operations but have demonstrated a commitment to improving clinical practice efficiency and effectiveness—bringing the management expertise needed to add value to physicians’ clinical ethos. But these
44 EUROTIMES | FEBRUARY 2023
LEADERSHIP AND BUSINESS INNOVATION
So, the question is, do we jump on the consolidation train, or do we continue as we are?
firms may be unable to generate this added value needed to sell off to a bigger company, which is the typical private equity model. Still, “they may be a viable option for [ophthalmologists] looking for an exit strategy,” Ms Morill said.


For those planning to stay on, Ms Morrill advises getting ready for changes. “It’s not yours anymore. That’s the part of this that sometimes gets lost,” she said. “At the end of the day, you are answering to somebody else.” Surgeons used to calling their own shots should think long and hard before committing to such an arrangement, and due diligence is required.
A third way
Yet, scale and management skills are needed to successfully address the quality and access issues presented by hybrid public/private systems, Dr Daya said. He believes the solution is for surgeons to band together rather than move from hospital to hospital as freelancers.
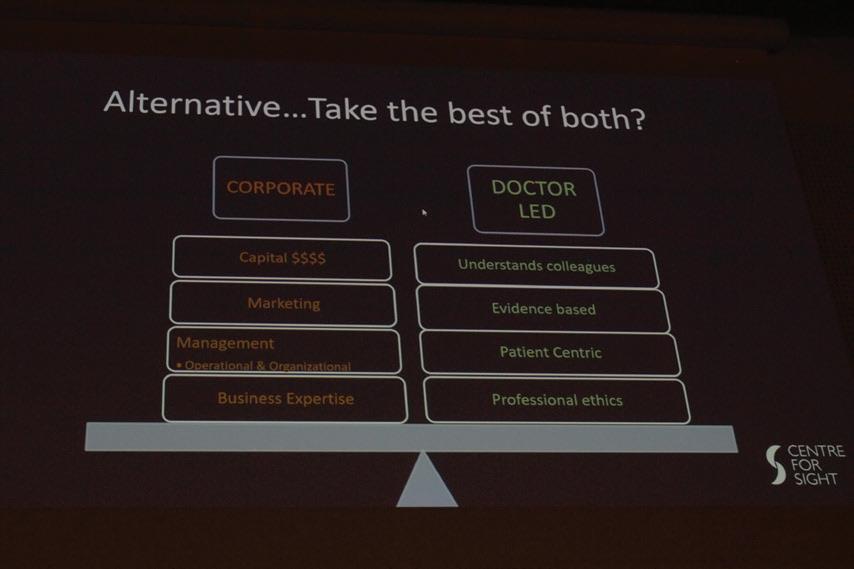
“If doctors could very single-mindedly start to work with each other and pull in the [management] resources available, I think they would fly. The paradigm has changed, and we need to change with it,” Dr Daya said.
“With the money sloshing around that they don’t have a home for, and the problem that exists, there is a marriage that could be made.”
45 2023 FEBRUARY | EUROTIMES
Sheraz M Daya MD, FACP, FACS, FRCS(Ed), FRCOphth, is founder and medical director of Centre for Sight, based in London, UK, and a leading researcher and practitioner in cataract, refractive, and corneal surgery, stem cell transplantation, and tissue engineering.
Kris Morrill is founder and lead consultant with Medevise Consulting, based in Strasbourg, France.
DO YOU KNOW WHERE YOUR CAT PACK COMES FROM?
The modern cataract pack (“cat pack”) is a case study in the benefits of customisation and efficiency. Everything an eye surgeon might need—gowns, gloves, drapes, cotton-tipped applicators, eye spears, gauze, instrument wipes, label sheets, resealable bags, syringes, cassettes and tubing, phaco needles, disposable blades, syringes, cannulas, and so on—are included, matched to the machines in use and the surgeon’s preferences.
But what the cat pack saves in staff time, it more than wastes in terms of environmental impact. Items that go unused or used just once, heavy packaging materials, plastics that are difficult to recycle—the cat pack has them all.
“We did a study that looked at the cat packs used in Austria because Austria is a small country and has relatively few operating centres, so we know them all,” says Dr Oliver Findl, president of the ESCRS. “Essentially what we’ve seen is that there’s a huge variability in the size of these cat packs. We’ve calculated that if we all were to go down to the average of the lowest third of the packs in Austria, we would reduce the carbon footprint of our packages by about one-third. And it would actually be cheaper, so it’s a win-win from a cost and sustainability point of view.”
Achieving those wins is the goal of the SIDICS (Sustainability Index for Disposables in Cataract Surgery) Project, an ESCRS-led initiative aiming to create metrics to help cataract surgeons evaluate the overall sustainability of cat packs. The project kicked off with a workshop at the 2022 ESCRS Congress in Milan, attended by ophthalmologists with an interest in sustainability as well as representatives of companies that sell cat packs. Leading the workshop (and the SIDICS Project) was SDI*Rating, a firm based in Vienna that developed a scientifically based methodology to capture industry-relevant sustainability indicators and present them in a single number ranging from 0 to 100.
“The SIDICS project is about providing the same quality of medical care with fewer materials and less waste and, therefore, more sustainably,” says Erek Stoisser, co-founder of SDI*Rating. “The first challenge is the speed with which we can initiate this transformation. There’s quite a high number of stakeholders, which makes this process relatively slow. The second challenge is the lack of standardisation of procedures and resources used. For example, the weight of the surgical kit varies by 236%, while the patient care remains the same.”
Over the course of the year, SDI*Rating will work with the ESCRS to develop a sustainability index that will enable cataract surgeons to evaluate their cat packs. Findl hopes to unveil the index at the 2023 ESCRS Congress in Vienna.
“The idea is to have a sustainability index, let’s say from 0 to 100, where 100 would be the most sustainable pack you can imagine, and 0 will be really devastating to the environment,” says Dr Findl. “Part of that index will be a rating of the company as a whole. Do they have photovoltaic panels? Do they have electric cars? What is the mix of their electric power origin?
“The bigger part of the index will be the pack itself,” he adds. “Where is the drape produced, and how is it produced? What is the supply chain like? And at the end of the day, what you get at is, how sustainable is this pack?”
The annual carbon footprint of cataract surgeries in Europe is equivalent to that of 410,000 cars per year. Reducing the size and weight of cat packs and reusing more of their components—as is done in India, for example—can significantly reduce their carbon footprint.
“What we’re doing is looking at how you can benchmark your cat pack,” Dr Findl says. “You could just say, ‘I have a package that works well for me.’ But you might want to see a benchmark and whether your pack is close to that because you want to have a sustainable cat pack or cassette and tubing. So you would ask your producer to fill out the rating form, they would complete it, and you could see where your cat pack rates on the scale.”
When finalised, the sustainability index will represent a significant milestone in the effort to reduce the environmental impact of cataract surgery. The challenge then will be to persuade ophthalmologists to use the index to encourage manufacturers to develop more sustainable cat packs.
“It is important that ESCRS continues this conversation once the index is developed, making sure hospitals use it and the exchange with industry keeps happening,” Stoisser says. “Generating greater awareness of sustainability issues among all stakeholders and highlighting further ways the eye care industry can be improved is the key to ensure long-term systemic change. This way, doctors will become more aware of the impact their purchasing decisions have, and the industry will be encouraged to design more sustainable products.”
46 EUROTIMES | FEBRUARY 2023
An ESCRS project aims to shrink the carbon footprint—and the cost—of cataract packages.
INSIDE ESCRS

47 2023 FEBRUARY | EUROTIMES
The SIDICS project is about providing the same quality of medical care with fewer materials and less waste and, therefore, more sustainably.
THERE IS ALWAYS MORE TO LEARN ABOUT CATARACT SURGERY
BY LEIGH SPIELBERG MD
It can be tempting for experienced surgeons to assume they have nothing left to learn. After all, after thousands of successful procedures, what could possibly be missing? Why spend valuable time buried in the depths of yet another textbook when life—at home and in the clinic—has so much else to offer?
And yet, well-written texts can offer the reading surgeon insight into the knowledge and experience of the surgeon who took the time to distil it into readable form.
It is this distillation that makes books such as Cataract Surgery: Advanced Techniques for Complex and Complicated Cases worth one’s time. Published in Springer’s Essentials in Ophthalmology series—and edited by the Jorge L Alió, H Burkhard Dick, Robert H Osher—this 500-page text approaches cataract surgery with a wide-angle lens while still delving into fine detail. Such is the experience of this trio that it would surprise me if there were anyone who could not learn something from nearly every chapter.
Fortunately, the book does not start with the standard, “Cataract is defined as a clouding of the crystalline lens” introduction. Instead, it opens with a chapter on surgical risk evaluation. The authors encourage a well-organised and highly developed approach.
“When surgeons fail to identify key risk factors in cataract evaluation, it is more likely due to systemic flaws rather than a lack of knowledge or skill in examination,” they observed. “A high level of knowledge about risk factors for complicated cataract surgery is only as good as your system of evaluation.”
This sets the overall tone: a systematic approach emphasising thought and organisation rather than speed and numbers. Considering the volume of patients modern “high-volume” cataract surgeons see, this is easier said than done. It is, however, refreshing to read the high-volume surgeons who authored this text still adhere to the premise extra time taken for in-depth evaluation is not only mandatory but worthwhile for more complex and potentially risky cases.
The chapters in this edition are titled very explicitly, increasing usefulness for those surgeons looking to brush up on a specific topic. Each is dedicated to a specific challenge, like phakic intraocular lens bilensectomy, cataract surgery in the
vitrectomised eye, floppy iris syndrome, artificial iris implantation, and MIGS in special cases.
The text itself often introduces a section with a pleasingly direct statement, sharpening the reader’s focus and getting straight to the issue. Regarding phakic intraocular lenses, the authors said, “all pIOLs will be explanted at some point,” implying surgeons will likely face this possibility sooner or later and should prepare.

It’s also sprinkled with fun facts. Who knew, for example, that cataract surgery is performed in 8 per 1,000 population per year in Europe, or the worldwide need for cataract extraction is 56 million per year, while only half of those operations actually occur?
As a vitreoretinal surgeon, I particularly enjoyed the chapter on combined cataract surgery with vitrectomy. It confirmed many of my own conclusions: that combined surgery is generally advantageous, not only for the patient (one procedure required, rather than two), but also for society (it typically results in less time taken off work and allows the patient to resume normal activities more quickly).
I would have liked a more extensive discussion of lens implant options in eyes with no capsular support. Although iris fixation and sutured scleral fixation are tried and tested methods with reasonably good outcomes, they have disadvantages. New, more modern developments, such as sutureless scleral self-anchoring implants, offer the possibility of posterior segment lens implantation without the complex manoeuvres associated with intrascleral fixation, not to mention late-stage lens dislocation.
But this is just a small oversight. The text is otherwise comprehensive, smoothly written, and properly illustrated with slit-lamp and intraoperative photography, decision-making flowcharts, ocular imaging examples, and charts compiling results from the authors’ data or peer-reviewed studies.
Given the scope of the text, who should consider purchasing? This book is suitable for all cataract surgeons, from the resident in training to the phaco fellow, early-career surgeon, and even experienced senior faculty. Whether searching for an introduction to the world of cataract surgery or seeking to update your knowledge and polish your skills, Cataract Surgery: Advanced Techniques for Complex and Complicated Cases might be appropriate for you.
48 EUROTIMES | FEBRUARY 2023
BOOK REVIEW
Upcoming Events
March 10–12
ESCRS Winter Meeting 2023
Vilamoura, Portugal

April 23–27
ARVO
New Orleans, US

May 5–8
ASCRS
San Diego, US

May 22–25
Royal College of Ophthalmologists
Birmingham, UK

June 15–17
European Society of Ophthalmology (SOE)
Prague, Czech Republic
June 28–July 1
World Glaucoma Congress
Rome, Italy
Sep 8–12
41st Congress of the ESCRS
Vienna, Austria
April 23
March 10
May 5
May 22
2023 FEBRUARY | EUROTIMES 49
PROVEN PLATFORM
iStent inject® is the gold standard in Trabecular Micro-Bypass surgery, continuing the legacy of excellence set throughout 20 years of iStent ® devices. It’s backed by the most robust, diverse, and longest-term body of clinical evidence for any MIGS procedure available today, given through clinical rigor and integrity.
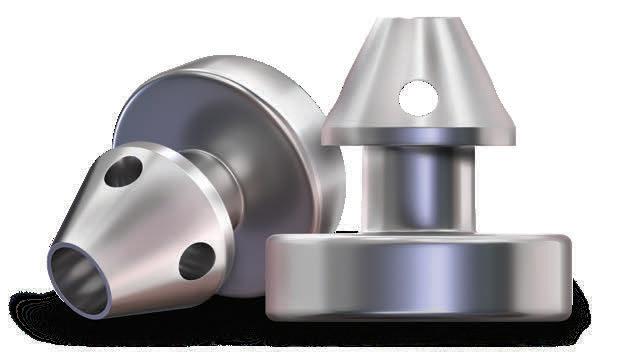
8 year study with iStent demonstrated sustained protection against visual field loss, as well as preservation of best corrected visual acuity, cup to disc ratio, and retinal nerve fiber layer thickness9
<0.01 decibel mean change in visual field mean deviation from baseline at 24 months in iStent inject-treated eyes in a pivotal trial1
4% of 125 patients in real world study of stand alone and combined iStent inject cases required a secondary procedure during 5 years of follow up4
LEGACY OF EXCELLENCE
20 Years of Data. 20K+ Eyes Studied. 20+ Countries.
38 publications demonstrate the power of iStent technologies to protect against visual field loss†
2.6% of 778 patients in a meta-analysis of stand alone iStent inject eyes went on to require secondary incisional surgery during follow up5
Only 1% of 186 eyes in a randomised controlled trial went on to require secondary incisional surgery during 3 years follow up10
Scientific evidence and clinical rigor have been at the heart of Glaukos, with the earliest publication on iStent® dating back to 2002 - years prior to the iStent ® pivotal trial. Today, this same rigor and integrity is applied to our business as we remain focused on generating strong clinical evidence.
5. Healey, Paul R., et al. “Standalone iStent trabecular micro-bypass glaucoma surgery: A systematic review and meta-analysis.” Journal of Glaucoma 30.7 (2021): 606-620. 9. Salimi, Ali, Harrison Watt, and Paul Harasymowycz. “Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results.” Eye and Vision 8.1 (2021): 1-12. 10. Samuelson TW, on behalf of the iStent inject Pivotal Trial Study Team. Three-Year Effectiveness and Safety of 2nd-Generation Trabecular Micro-Bypass (iStent inject). Paper at the Annual Meeting of the American Academy of Ophthalmology (AAO). Virtual Meeting: November 13-15, 2020. † Data on file.
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/ PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.”


• There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. © 2022 Glaukos Corporation. Glaukos, iStent inject® and iStent inject® W are registered trademarks of Glaukos Corporation. PM-EU-0163
POWERFUL. PREDICTABLE. PROVEN PROVEN
PROTECTS VISUAL FIELDS1,9
LOW RATE OF SECONDARY SURGERY INTERVENTIONS4,5,10
1. Samuelson, Thomas W., et al. “Prospective, randomized, controlled
pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results.” Ophthalmology 126.6 (2019): 811-821. 4. Hengerer, Fritz H., Gerd U. Auffarth, and Ina Conrad-Hengerer. “iStent inject Trabecular Micro-Bypass with or Without Cataract Surgery Yields Sustained 5-Year Glaucoma Control.” Advances in Therapy (2022): 1-15.




 **Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface
eyes after trabecular
stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.
**Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface
eyes after trabecular
stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941-953.








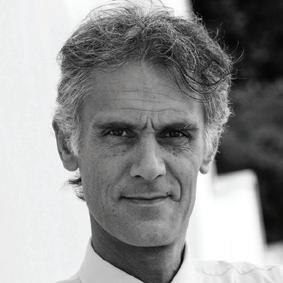











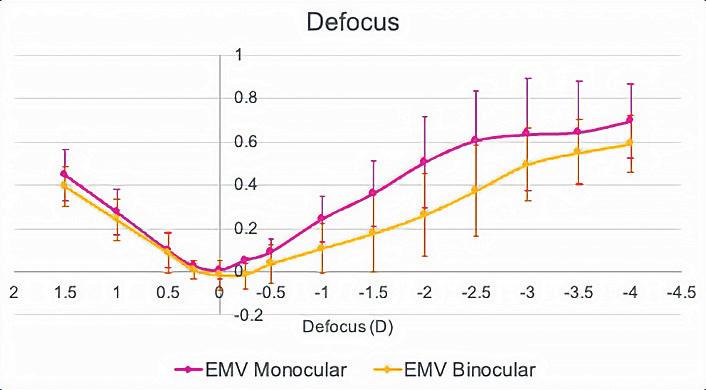

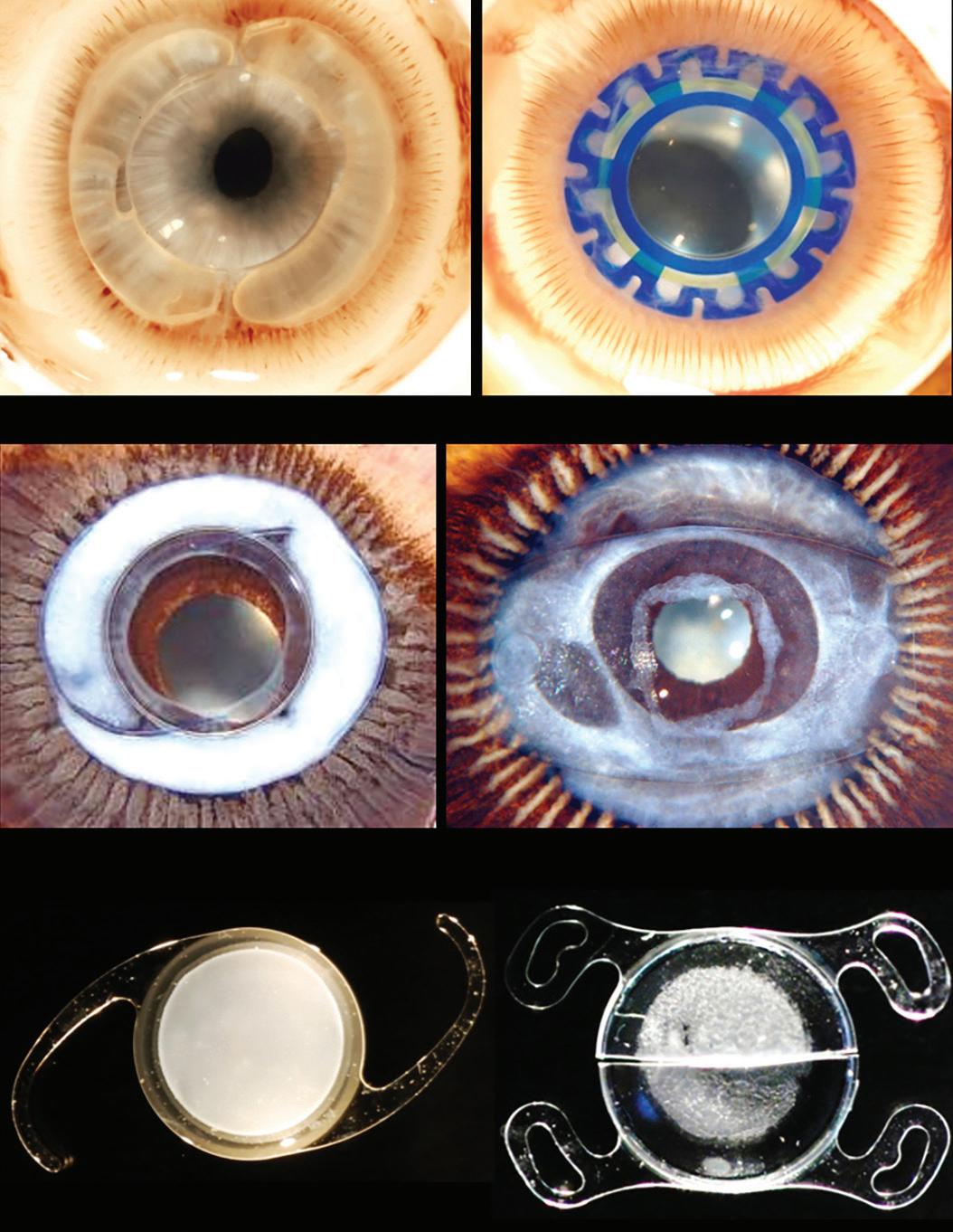

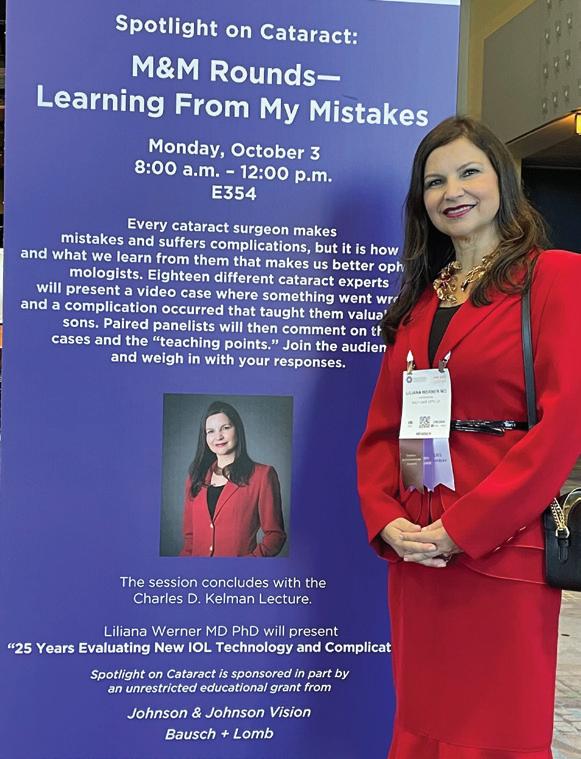




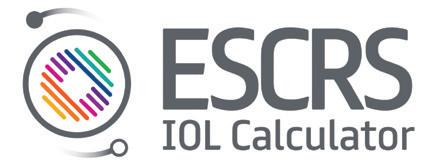
















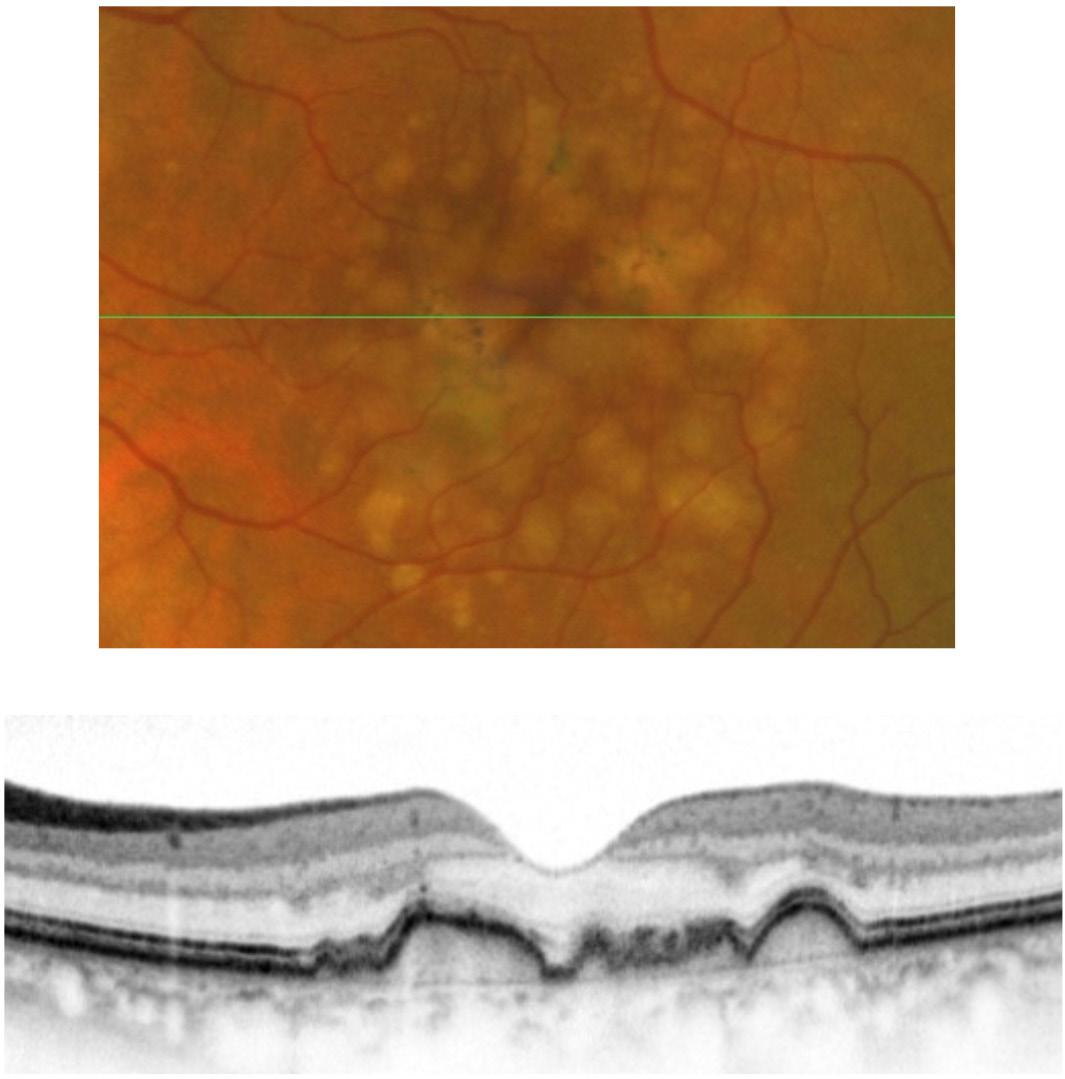





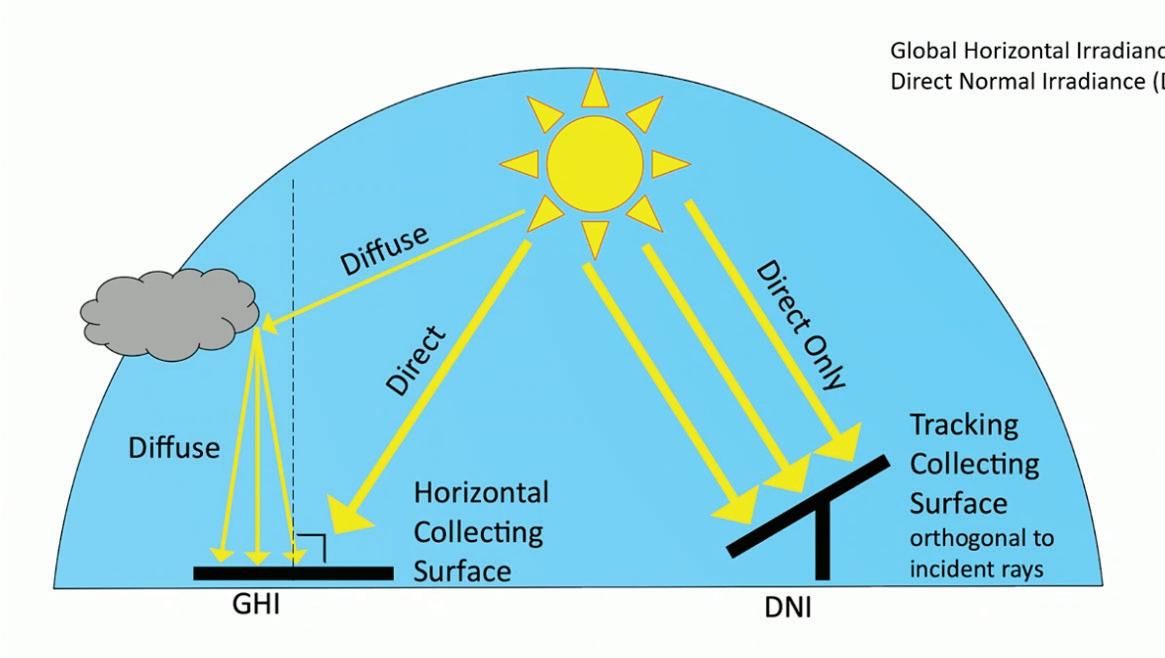













 BY HOWARD LARKIN
BY HOWARD LARKIN