HAROLD RIDLEY’S BRILLIANT INNOVATION
A transformative surgery that continues to save the vision of millions every year.

ALSO IN THIS ISSUE
MERoV Study
Results Preview
Factors linked to pseudoaccommodation and cataract surgery revealed.
Treatment at a Crossroads
Growing number of patients with comorbid cataract and Fuchs’ dystrophy creates surgical challenges.
SIDICS for a More Sustainable OR Cat packs shown an effective and helpful way to reduce waste and carbon footprints.
Welcome to the Future of Glaucoma Laser Therapy.
Introducing the Eagle™ by BELKIN Vision
Accessible First-Line Glaucoma Care for All
Automation
Delightfully simple navigational guidance using an intuitve touch screen
Precision
120 automated treatments enabled by
delivered directly to the trabecular meshwork
Efficiency
Ergonomic patientand doctor- friendly set up for streamlined positioning and treatment


Visit us at the ESCRS Winter Meeting - Booth #B02
׳׳׳׳׳׳׳׳׳׳׳׳

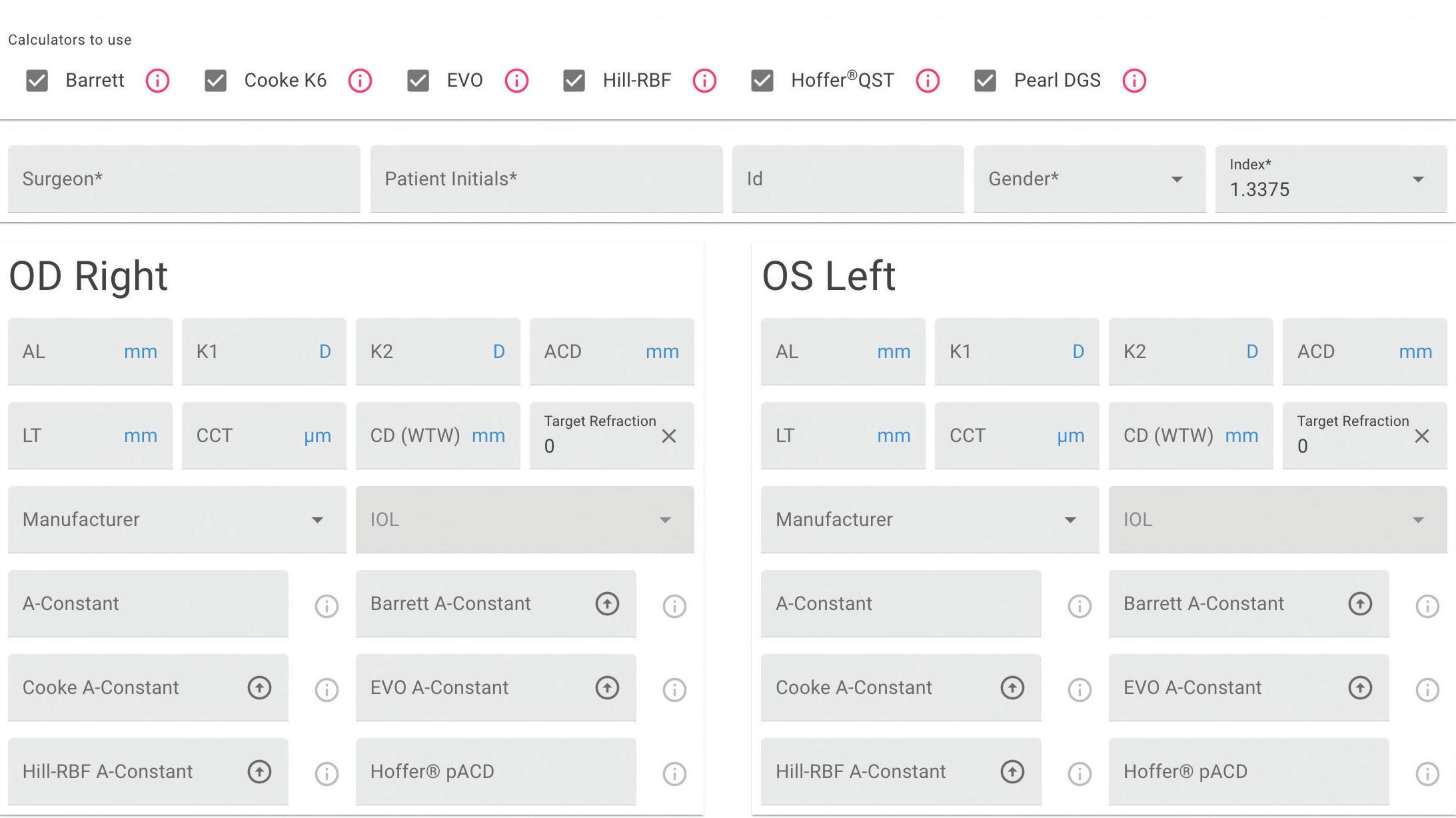

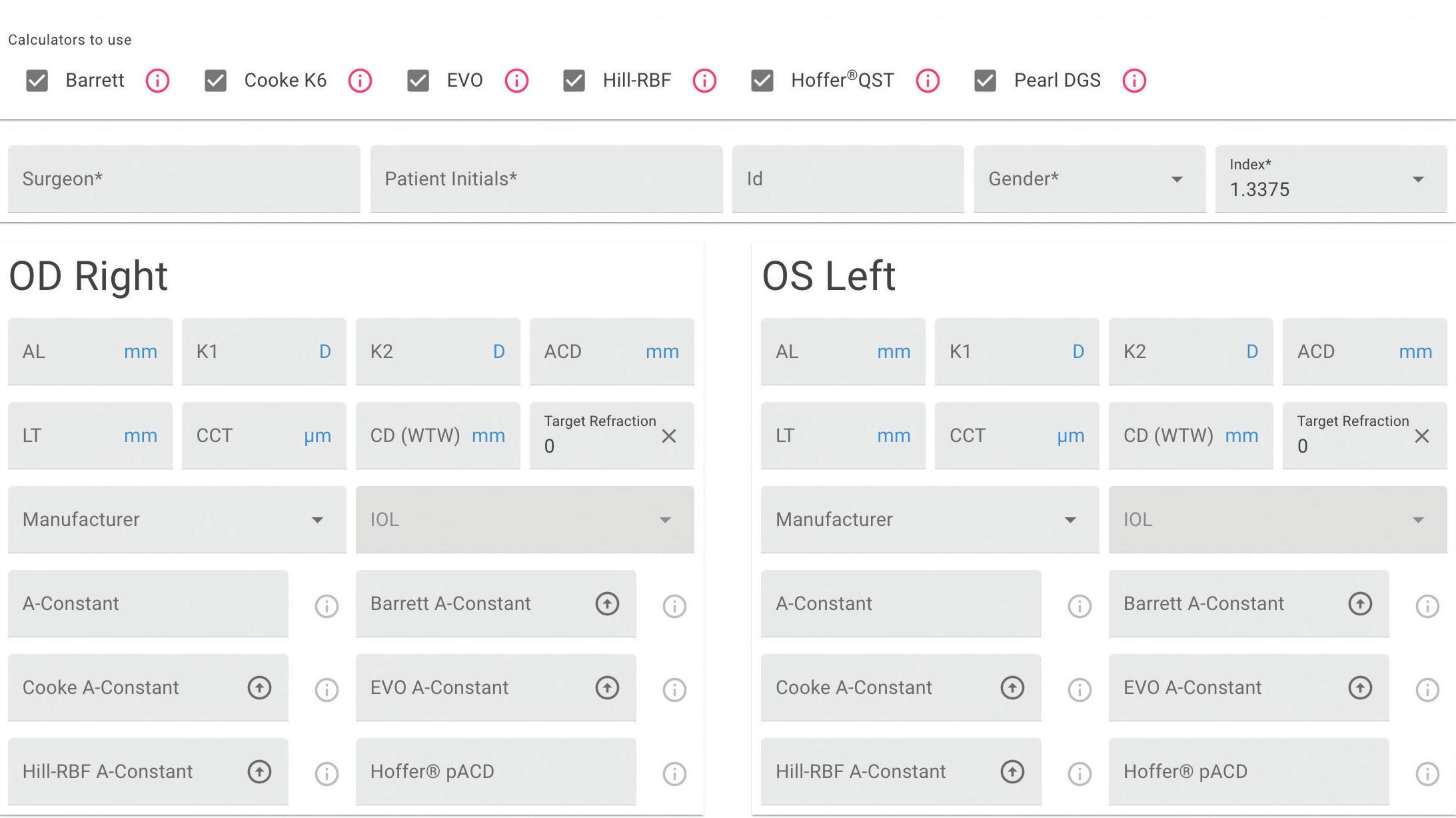
This first-of-its-kind web application for IOL power calculations uses multiple modern formulas simultaneously, and suggests lens constants for a wide range of IOL models .
IOL Calculator is now live on the ESCRS website!
Find out
Our
more at iolcalculator.escrs .org/

08 Cover
Harold Ridley’s Brilliant Innovation
A transformative surgery that continues to save the vision of millions every year.
04 Editorial: Happy Birthday to IOL Surgery!
06 Inside ESCRS: Webinar Examines Impact of Investors on Ophthalmology
07 ESCRS Update
CATARACT & REFRACTIVE
12 Gazing into a Lenticule-Based Future
Béatrice Cochener-Lamard MD, PhD
14 MERoV Study Results Preview
Mayank Nanavaty MBBS, DO, FRCOphth, PhD
15 Will Marking Go Digital?
Tim Schultz MD, FEBO
16 Lenticule Extraction Gaining Fans?
Rohit Shetty MD, PhD and Walter Sekundo MD, PhD
18 What is the Best Option for Hyperopia?
Michael C Knorz MD and Pavel Stodůlka MD, PhD
20 It’s in the Bag
Marie-José Tassignon MD, PhD, FEBO
21 Refractive Surgery for Myopia
Roger Zaldivar MD, MBA
22 Intraoperative Aberrometry in the Balance
David Piñero Llorens OD, PhD
CORNEA
26 Six Essentials to Iris Repair
Soosan Jacob MS, FRCS, DNB
28 Best Practices in Cataract Surgery
Allan R Slomovic MSc, MD
29 Treatment at a Crossroads
Björn Bachmann MD, PhD
GLAUCOMA
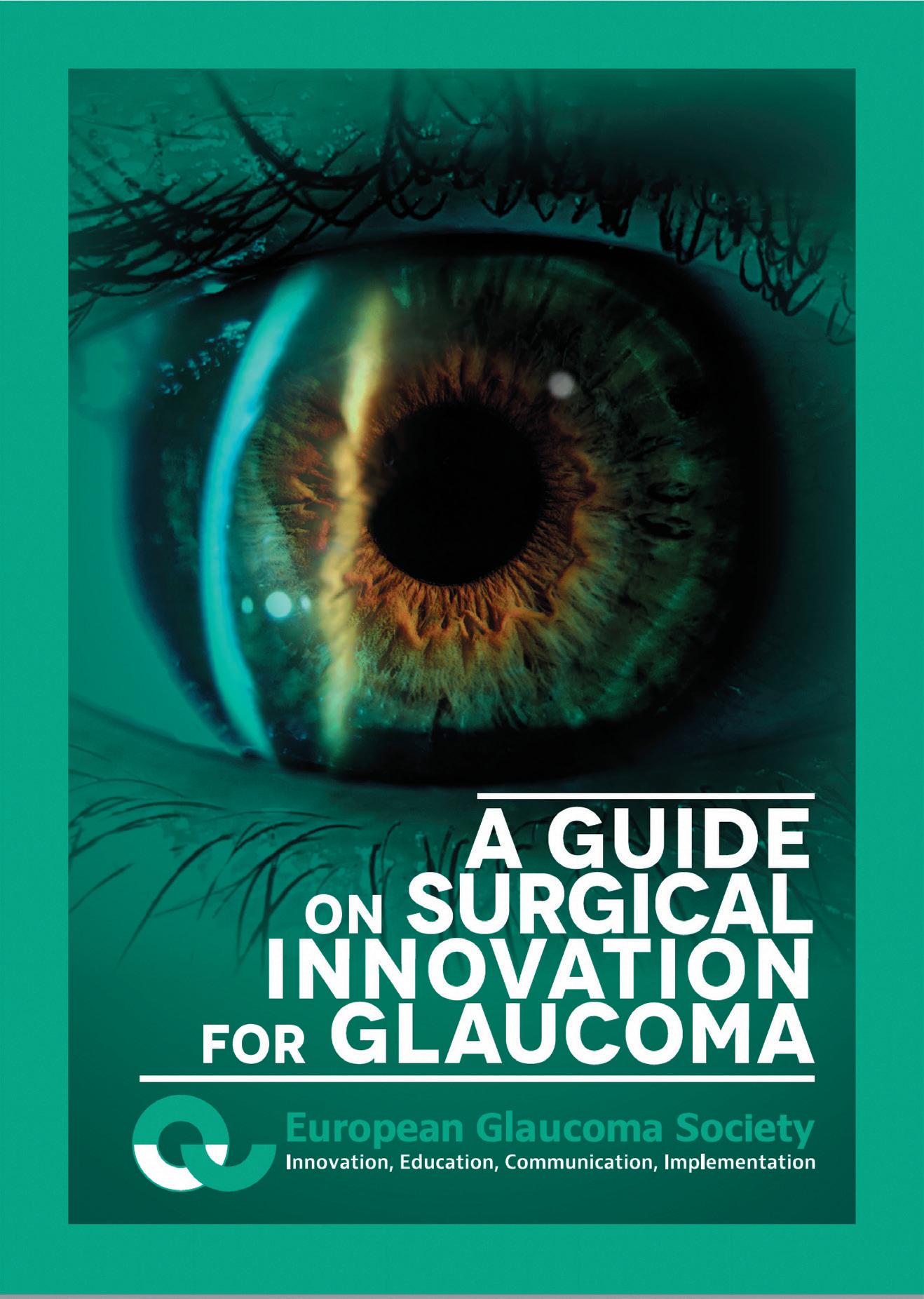
30 Charting the Glaucoma Course
Antonio Maria Fea MD, PhD; Verena Prokosch MD, PhD; Carlo Enrico Traverso MD
RETINA
32 Oral Treatment for Stargardt Disease
Carel Hoyng MD, PhD
33 MDR Requirements Affect All Ophthalmic Surgeons
José-Carlos Pastor MD, PhD
34 Vitreoretinal Surgery for Managing Uveitis
Shwu-Jiuan Sheu MD
DIGITAL OPHTHALMOLOGY
36 Putting Digital Under the Microscope
Matteo Ripa MD and Kfir Azoulay
37 Boarding the Smart Future
David Smadja MD
SUSTAINABILITY
38 Updating the Hippocratic Ideal Sjoerd Elferink MD
40 SIDICS for a More Sustainable OR Nicolas Winklmair MD
2 EUROTIMES | FEBRUARY 2024




Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Soosan Jacob
Timothy Norris
Colour and Print
W&G Baird Printers
Advertising Sales Roo Khan
Tel: +44 203 530 0100 | roo.khan@wearemci.com
® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983


3 2024 FEBRUARY | EUROTIMES Learn more about EuroTimes or connect with ESCRS at ESCRS.org
Supported by an independent medical education Included with this Issue The Future of Refractive Surgery — Lenticule Extraction, Phakic IOLs, and Beyond Belkin Direct SLT Simplifies Open-Angle Glaucoma Laser Treatment 48 Citation Index 49 Upcoming Events 32 37 29 12 30
Happy Birthday to IOL Surgery!
This year, 2024, will mark 75 years since the first intraocular lens implantation by British surgeon Sir Harold Ridley MA, MD, Cantab, FRCS (1906–2001). The number of patients who have benefited from this innovation must number in the many millions, and it continues to grow. It is now considered among the most common and safest of all forms of surgery.
In our cover story, Howard Larkin explores how Dr Ridley’s revolutionary invention launched a cascade of surgical techniques and technical innovations that make cataract surgery what it is today.
Dr Ridley’s profound insight was born out of the ocular trauma of a combat pilot he was treating during the Second World War. The first surgery involved an IOL made of rigid polymethylmethacrylate (PMMA) implanted through a large incision in the posterior chamber about three months after extracapsular cataract extraction. The operation was performed without modern lighting and microscopy, viscoelastics, phacoemulsification, and modern biometry.
As Dr Rupal Trivedi and colleagues recount in their excellent overview of Dr Ridley’s career,1 the response to the revolutionary idea of implanting a prosthetic plastic lens into the eye was met with widespread opprobrium by the medical establishment. Dr Ridley anticipated this and kept his work secret for a few years after the first surgery. Even so, his initial
presentation of the first IOL results at the Oxford Conference in 1951 caused a storm of harsh criticism. It was not until late in his career that his contributions were widely honoured, including his election to the Royal Society, London, in 1986 and knighthood in 2000.
The combination of daring and innovation represented by Dr Ridley’s invention has come to characterize the field of ophthalmology, with examples ranging from the introduction of viscoelastic devices and phacoemulsification to ever-improving IOL designs, modern biometry, and better operating microscopes.
Without Dr Ridley’s tireless work, the ESCRS would not exist. Along with Peter Choyce and others, Harold Ridley was a founding member of the European Intraocular Implant Club (EIIC) in 1966. It later became the International Intraocular Implant Club in 1981, and from these roots sprang the ESCRS. Our Society is based on the original principles of the EIIC of promoting research and encouraging the open exchange of ideas in the field of cataract surgery.
These ideals continue to inform our own conferences. We hope you will be able to visit, learn, and contribute at our Winter Meeting in Frankfurt (16–18 February) and the Annual Congress in Barcelona (6–10 September).
For citation notes, see page 48.
EDITORIAL BOARD

Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)

Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)
Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
EDITORIAL
4 EUROTIMES | FEBRUARY 2024
Thomas Kohnen Chief Medical Editor
José Güell Medical Editor
Paul Rosen Medical Editor
Apply for the
John Henahan Writing Prize
Burnout is a chronic issue in ophthalmology, leading a growing number to abandon the field early in their careers. What should be done to reduce unnecessary stress in training and practice, allowing for a successful long-term career?
Young ophthalmologists are invited to submit their answer to that question in an 800-word essay for the John Henahan Writing Prize. The author of the winning essay will receive a €500 bursary and a specially commissioned trophy, awarded during the 2024 ESCRS Congress in Barcelona, Spain. The winning essay will be published in EuroTimes.
The competition is open to ESCRS members (including the free membership available to trainees) age 40 or younger on 1 January 2024.

For details, please see the dedicated page on our website https://www.escrs.org/eurotimes/john-henahan-writing-prize
Webinar Examines Impact of Investors on Ophthalmology
BY STUART HALES, EXECUTIVE EDITOR
Young ophthalmologists in Europe can look forward to a busy career, thanks in large part to an ageing populace. According to Eurostat, cataract surgery was performed 4.32 million times in the European Union in 2021, making it the most common surgical procedure in the consortium’s 27 countries.1
The growth in cataract surgery and other procedures has been accompanied by a rising desire among private investors to include ophthalmology in their healthcare portfolios. To address some of the questions surrounding investor interest in ophthalmology, ESCRS hosted a webinar on 21 November titled “Who Owns Ophthalmology?” Moderated by Sheraz Daya and Artemis Matsou, the webinar explored how ophthalmologists can retain their independence while engaging with industry in a constructive and positive manner.
Daya, founder and medical director of the Centre for Sight in the UK, laid the groundwork for the webinar by positioning ophthalmology within the overall healthcare business environment. “The business of ophthalmology is ever changing,” he said. “What we want to discuss today are the options that are evolving. And that discussion principally starts with what do we, as ophthalmologists, want?”
Vincent Qin, a consulting surgeon in Belgium, followed with an overview of private investment and its impact on the work and careers of ophthalmologists. He cautioned that the interests of private investors and those of ophthalmologists are not always aligned.
“For private equity groups, profit is paramount,” he said. “They’re looking for a return on their investment, and their ultimate goal usually is to flip the practice within five years. So they’re not necessarily making business decisions with the same
motivations as the physicians who are working in these practices.”
The motivations of ophthalmologists, Qin explained, can vary greatly, especially by age and career stage.
“The older ophthalmologists usually are pleased with the arrangements because they’re close to retirement and want an exit strategy,” he said. “But there is significant concern among younger ophthalmologists because they have 30 or 40 years to go, and now they find they might have less of a say in the control of their practice.”
A sense of control
Because of the profit-seeking nature of private investors, doctors in investor-owned ophthalmology practices can expect to perform more surgeries than their counterparts in public settings. In the UK, for example, the number of private clinic groups backed by private equity has grown exponentially. As a result, the number of cataract cases outsourced to the private sector has skyrocketed—as has the workload for surgeons.
“In the UK, the private sector has embraced a very high-efficiency, high-throughput model in their clinics where they only operate on outpatients,” said Victor Chua, an ophthalmologist and senior partner at Mansfield Advisors, a healthcare consulting firm. “They select surgeons who can perform 25 cataracts per day. You have to ask yourself, is that the kind of job I would like to have?”
Increasingly, young surgeons entering the workplace may answer that question in the negative.
“I think young people today have a healthier attitude towards life in general,” said Arthur Cummings, consultant eye surgeon at the Wellington Eye Clinic and consultant ophthalmologist at the Beacon Hospital in Dublin, Ireland. “They want to be good family members and involved fathers and mothers. I

The interests of private investors and those of ophthalmologists are not always aligned.
think what may happen is they’ll say, ‘I’ll work in a public setting now or work for a big company as an employee, get some experience and develop my own my skill set, and when my kids don’t need all my time anymore, then maybe I’ll go out and do my own thing.’”
Ultimately, the deciding factor in whether ophthalmologists opt for private practice and seek investors is whether they can retain a sense of control and/or ownership over their work arrangements.
6 EUROTIMES | FEBRUARY 2024 INSIDE ESCRS

“We don’t want to lose our sense of control,” said Artemis Matsou, a consultant ophthalmic surgeon at Queen Victoria Hospital in East Grinstead, UK. “We’ve been training for many years, and we’ve reached the stage as young ophthalmologists where we are ready to go out there in the market, but we don’t want to lose our sense of autonomy, decision making, and choice. I think that scares a lot of young people.”
“To get new doctors you have to offer life-work balance,” said Joern Joergensen, chief executive of Denmark-based EuroEyes. “I think making them a partner is very crucial. You should not have employees; you should really try to make them partners.
“I think we have a model in EuroEyes where we can do that. When we are going to take over a practice, I don’t wish to intervene there. They have full autonomy. That way, we can talk doctor to doctor. It’s much, much easier than talking to a banker.”
For citation notes, see page 48.
ESCRS UPDATE
ESCRS Releases Joint Paper on Reducing Surgical Waste
In 2022, ESCRS partnered with the American Society of Cataract & Refractive Surgery (ASCRS) and the American Academy of Ophthalmology (AAO) to form EyeSustain, a global platform for incorporating sustainability into ophthalmology.
Recently, ESCRS teamed with ASCRS, AAO, and EyeSustain to write a position paper encouraging industry and regulators to move towards electronic instructions for use (e-IFUs) rather than continue to include a set of paper IFUs with surgical products. This would reduce paper waste significantly and enable surgeons to access IFUs of the newest version available.
“We believe that requiring a paper IFU is outdated and environmentally detrimental,” the report states. “This is particularly important for IOLs, given the common practice where IOLs are stored under consignment in surgical facilities. Some infrequently used IOLs may sit on shelves for long periods of time, allowing the enclosed paper IFU to become outdated.”
The report notes, however, that several countries still require printed IFUs, posing a “major obstacle” to e-IFU adoption.
The paper, “Reducing Ophthalmic Surgical Waste through Electronic Instructions for Use (eIFU),” is available on the ESCRS website.
Applications Now Open for the 2024 Peter Barry Fellowship
ESCRS is now accepting applications for the Peter Barry Fellowship, which commemorates the significant contributions made by the late Barry to ophthalmology and the Society.
The Fellowship of €60,000 allows a trainee to work at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year. The Fellowship is awarded at each ESCRS Annual Congress and begins the following year.
Applicants must be a European trainee ophthalmologist, 40 years of age or under on the closing date for applications, and have been an ESCRS trainee member for 3 years by the time of starting the fellowship.
Applicants must first complete the online Peter Barry Fellowship application form found at https://www.escrs.org/education/grants-awards/peter-barry-fellowship/. Applications for 2024 will close on 2 March.
7 2024 FEBRUARY | EUROTIMES

HAROLD
RIDLEY’S BRILLIANT INNOVATION
A transformative surgery that continues to save the vision of millions every year.
One day, perhaps in 1947, a routine list of operations was performed. At the end, a student who had never before seen a cataract said, ‘It’s a pity you can’t replace the cataract with a clear lens.’ He was told that this was not usual, though many people, including myself, had suggested this project. However, no one had the temerity to take action.
– Sir Harold Ridley, inventor of the intraocular lens
 BY HOWARD LARKIN
BY HOWARD LARKIN
Following this encounter, Mr Ridley, as he then was, went forward with the first intraocular lens (IOL). He met with John Pike of Rayner and Keeler and, between them, realised the basic ideas of the project. Mr Ridley had been impressed during World War II by the apparent lack of inflammation caused by fragments of aircraft clear canopies when found in the eyes of injured crew. Pike asked his friend John Holt of Imperial Chemical Industries in the UK to create clinical quality and hopefully biologically inert polymethylmethacrylate (PMMA).
The design he chose for the first IOL mimicked the shape of the human lens. It was inserted into a patient’s eye behind the pupil and hopefully into the capsular bag after an extracapsular cataract extraction. The actual date of the first implantation is not entirely clear. It may have been 29 November 1949, but it was removed and inserted as a secondary operation on 8 February 1950. It produced a gross refractive error of -14 D due to the IOL power calculation conducted in air, not liquid. The error was quickly corrected in subsequent implantations, and the operation promised the first “cure for aphakia,” as Harold Ridley put it.
9 2024 FEBRUARY | EUROTIMES
Mr Ridley wanted to keep his invention a secret until he had sufficient clinical data. However, one of his implanted patients, when going for a follow-up visit, went to see another ophthalmologist with the surname Ridley by mistake. With his secret out, Mr Ridley decided to go public at the Oxford Ophthalmological Congress in July 1951. He brought two of his patients, one with 6/6 vision unaided, to the meeting so colleagues could examine them. At the meeting was Sir Stewart Duke Elder, the doyen of British ophthalmology at the time, who refused to look at Ridley’s patients or watch the coloured movie of one of the implant procedures. This very negative attitude was mirrored by many senior ophthalmologists across the world.
Lacking haptics for support and weighing many times more than current IOLs, the earliest lenses tended to dislocate, sometimes months or even years after surgery. Despite this, some of the early IOLs continued to give good vision 20 years after implantation. About 15% of Ridley lenses were eventually explanted. Stabilising the implant was a problem that took more than 40 years to adequately solve.
Other frequent complications of early IOL surgery included postoperative infections, haemorrhage, inflammation, corneal oedema, peripheral anterior synechiae, raised intraocular pressure, capsule and lens opacification, and residual refractive error.
Focusing on the problems rather than trying to find solutions, much of the global academic ophthalmic establishment vehemently opposed ocular implants for several decades.
However, the status quo was not acceptable. “Spectacles for aphakia were horrendous—they magnified and distorted the image, and many patients never really adapted to them. The gross anisometropia made uniocular surgery impossible to rehabilitate,” said David J Spalton, who, as a trainee in the mid-1970s, was among the last to assist Harold Ridley in an implant procedure.
Implants restored normal vision, and “there was a lot to be said for that. It was just a matter of getting the design and techniques right for it,” Professor Spalton said.
To bring together those interested in lens implantology, Mr Ridley and Peter Choyce, a very early IOL pioneer, formed the Intraocular Implant Club (IIC) in 1966. The founder members of what became the International Intraocular Implant Club (IIIC) came from many countries. In the US, it took another decade before Harold Ridley was recognised for his accomplishments at a meeting of the American Academy of Ophthalmology in 1976. For Mr Ridley, the greatest of all his achievements by way of scientific recognition was admission to The Royal Society of London in 1986. Public recognition eventually came after lobbying of a prime minister’s wife when he was knighted in 2000.
Along the way, enterprising surgeons, researchers, and manufacturers made most of the technical innovations. “It was driven by individuals who put a lot of time and thought into the complications and how you would avoid them,” Prof Spalton said.
“It’s truly remarkable to witness the ongoing evolution of these technologies, underscoring our commitment to providing tailored solutions for each patient’s unique visual

needs. Continuous progress in the field not only enhances our surgical capabilities but, more importantly, significantly improves the quality of life for those seeking visual correction after cataract surgery,” incoming ESCRS President Professor Filomena Ribeiro said.
Advancing IOL design
Early lessons prompted continual improvement in IOL design, said Richard Packard MD. To solve the problem of posterior lens dislocation, Dr Ridley designed anterior chamber lenses, prompting many other surgeons to design angle-supported lenses in the early 1950s.
“Universally, they failed. Not immediately, because there were enough endothelial cells to cope with it, but […] they didn’t understand that the edges of the lenses and the haptics were gradually destroying the back of the cornea,” Mr Packard explained. Implant pioneers including Dr Joaquin Barraquer in Barcelona ended up explanting half or more of their anterior chamber lenses.
In the late 1950s, Dr Cornelius Binkhorst designed what Mr Packard described as the first “successful” IOL, the iris-fixated four loop lens, for use with intracapsular extractions. “He determined that the only way IOLs would work was to be separated enough from vital tissues not to cause problems.”
These and similar lenses continued to be implanted until posterior chamber lenses finally overtook them in the late 20th century. Indeed, Mr Packard’s first IOL in December 1978 was a Fyodorov Mark 1 iris-fixated lens, implanted at London’s Charing Cross Hospital after he served as a senior resident at Moorfields, where he never saw an IOL. The day he arrived at Charing Cross, an IOL and phacoemulsification course was underway.
“This was like Saul’s conversion on the road to Damascus. I’d never seen anything like it,” he said.
Around the same time, Roberto Bellucci MD began doing cataract surgery in Italy, where cryoextraction remained the standard of care until the mid-1980s. “I remember Mr [Eric] Arnott giving a lecture about his lens at my university, but my professor was not convinced. He used to say: ‘If the surgery is for your mother, do an intracap! If it is for your mother-in-law, put an intraocular lens in!’ It was very hard to overtake this scepticism, and innovation was pushed by doctors working mainly outside the universities, like Lucio Buratto in Milan and Egidio Dal Fiume in Ravenna.” In 1985, he implanted his first IOL, a Worst Medallion sutured to the iris.
In the 1960s, Prof Binkhorst pioneered using the capsular bag left behind in extracapsular procedures to stabilise the
10 EUROTIMES | FEBRUARY 2024 COVER ARTICLE

IOL. His two-loop iridocapsular lens optic sat in front of the iris with haptics anchored in the bag. This eventually led to a resurgence of posterior chamber designs, such as Dr Steve Shearing’s 1977 J-loop PC IOL. Based on the Barraquer anterior lens design, it was the first of a new generation of posterior lenses that did not extend into the anterior chamber. The 1960s also saw the introduction of theoretical lens power calculation formulas, pioneered by Prof Svyatoslav N Fyodorov.
Cataract surgery technologies advanced rapidly: This included the invention of phacoemulsification by Charles Kelman, the development of capsulorhexis by Drs Howard Gimbel and Thomas Neuhann, and Prof Robert Stegmann’s innovation of viscoelastics. Subsequent innovations included foldable acrylic IOLs, UV blocking IOLs, and toric IOLs. The procedure also became safer with improved anaesthesia and endophthalmitis prophylaxis.
The cumulative impact of all these technologies was a movement away from intracapsular and even extracapsular procedures to phacoemulsification. This reduced hospital stays from several days to overnight and eventually made cataract surgery mainly an outpatient procedure.
On the horizon are accommodative lenses and even robotic surgery, Oliver Findl MD said. Over the course of his career, “the technology has changed, but in the end, it is still a person doing the procedure. I wonder if in 30 years it will still be a person doing it.”
Development Timeline of IOL and Key Related Technologies
1930s Harold Ridley discusses IOL concept with mentor Cyril Hudson; no lenses were made
1940s Ridley observes Perspex (PMMA) fragments in WWII pilots’ eyes are biologically non-reactive 1949: Ridley designs and implants first IOL, made of PMMA and manufactured by Rayner, as “cure for aphakia”
1950s Early anterior chamber IOLs by Ridley, Strampelli, Choyce, Barraquer, and others; Many subsequently explanted due to corneal damage and uveitis-glaucoma-hyphaemia 1951: Ridley presents first paper on IOL implants, sparking opposition that would last decades, despite many successes
1960s Introduction of iris-fixated lenses, including Binkhorst 4-loop
1965: Binkhorst 2-loop capsule-fixated iris lens reduces corneal and inflammatory complications, foreshadowing capsular bag lens placement
1966: Intraocular Implant Club founded with Ridley the first president
1967: Charles Kelman and Anton Banko invent phacoemulsification
1970s More iris-stabilised lenses, return of posterior chamber IOLs
1975: John Pearce implants tripod posterior chamber lens
1977: Steven Shearing introduces posterior chamber in-the-bag lens with flexible J-loops
1980s IOL acceptance grows
1980: Viscoelastic Healon introduced
1982: Tom Mazzocco patents folding silicone IOL for insertion through 3.0 mm incision
1986: John Pearce implants 2-zone multifocal IOL
1987: 3M releases diffractive IOL
1990s Foldable and multifocal lens designs proliferate
1990: First foldable hydrophobic acrylic lens implanted
1991: Hoya markets first blue-filtering IOL in Japan
1992: AMO introduces Array refractive multifocal IOL
1992: Kimiya Shimizu implants first toric IOL
1998: Staar markets foldable toric lens
David J Spalton FRCS, FRCP, FRCOphth is an ophthalmologist in London, UK, and a former ESCRS president. profspalton@gmail.com
Richard B Packard MD, FRCS, FRCOphth, FEBOS-CR is an ophthalmologist in London, UK. eyequack@vossnet.co.uk
Filomena Ribeiro MD, PhD, FEBO is head of ophthalmology at Hospital da Luz Lisboa, Portugal, and ESCRS president. filomenajribeiro@gmail.com
Paul Ursell MBBS, MD, FRCOphth is an ophthalmologist in London, UK, and president of the UKISCRS. paul@cataract-doctor.com
Roberto Bellucci MD is an ophthalmologist in Verona, Italy, and former ESCRS president. roberto.bellucci52@gmail.com
Oliver Findl MD, MBA, FEBO is chair of ophthalmology at Hanusch Hospital, Vienna, Austria, and immediate past president of ESCRS. oliver@findl.at
1998: Square-edge IOL optic shown to inhibit PCO
2000s Multifocals proliferate; early attempts at accommodating IOLs reach market
2003: Alcon adds blue light-filtering lens, US FDA clears Crystalens accommodating IOL
2006: Synchrony accommodating IOL CE marked
2006: Rayner introduces M-flex T toric multifocal IOL
2010s Extended depth of focus and enhanced monofocal IOLs reach market
2014: Tecnis Symfony extended depth of focus lens CE marked
2019: Eyhance enhanced monofocal lens CE marked
2020s Huge selection of multifocal, extended depth of focus, and enhanced monofocal IOLs available; accommodating lenses on the horizon
2024 FEBRUARY | EUROTIMES 11

Gazing into a Lenticule-Based Future
New and emerging platforms and applications predicted to drive growth for lenticule-based refractive surgery.
CHERYL GUTTMAN KRADER REPORTS
Femto-LASIK remains the gold standard for refractive surgery, but an increase in uptake of lenticule-based procedures may be on the horizon driven by recent femtosecond platform developments, according to Béatrice Cochener-Lamard MD, PhD
Providing predictions about the landscape of refractive surgery in 2030, Prof Cochener-Lamard said, “Looking into my crystal ball, I think lenticule-based surgery has a promising future and may become competitive with LASIK, but I cannot tell if lenticule-based surgery will replace LASIK. I do guarantee, however, that PRK will not become obsolete because there will continue to be specific indications for choosing a surface ablation procedure.”
Factors that could lead to the expansion of lenticular procedures in the future include the introduction of cyclotorsion compensation (like on the VISUMAX 800 laser), the anticipated approval of software for the VISUMAX 800 to treat hyperopia/hyperopic astigmatism, and the availability of lenticule-based procedures to treat myopia/myopic astigmatism using other femtosecond laser platforms—e.g., SILK with the Elita laser, Smartsight with the ATOS laser, and CLEAR with the FEMTO LDV Z8 and FEMTO Z8 NEO lasers.
“Finally, with these new platforms, a product (SMILE) is becoming a concept, and it might attract more surgeons to try lenticule-based refractive surgery,” Prof Cochener-Lamard said.
She noted that compared with the VisuMax, the VISUMAX 800 features ergonomic enhancements to provide time-saving benefits and make the procedure more comfortable for patients and surgeons. The laser also introduces new surgeon support functions, including aids for centration and cyclotorsion adjustment. Most importantly, it has a fourfold faster pulse frequency than the VisuMax.
“The beauty of the VISUMAX 800 is it makes lenticule extraction a much faster procedure.”
The safety, efficacy, predictability, and stability of SMILE for hyperopia/hyperopic astigmatism were proven in a multicentre 12-month study in which Prof Cochener-Lamard was an investigator.1 Even though the procedures were performed using the VisuMax laser without cyclotorsion control, good results were achieved treating patients with up to 4.0 D of astigmatism. Study results also showed patients were subjectively happy with their outcomes and had less halo and glare compared to reports for hyperopic LASIK.
12 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE

There are caveats, however. “The results are en couraging, but we still wonder about stability over the longer term, and for a variety of reasons, SMILE for hyperopia is more challenging than SMILE for myopia,” she added.
Another dimension of lenticular surgery
Looking ahead, Prof Cochener-Lamard discussed the emergence of lenticular implantation procedures (addi tion keratoplasty) that use tissue removed from myopic SMILE or a corneal button. Applications in development within this category could include treatment of keratec tasia, aphakia, pathological corneal thinning, and even hyperopia and presbyopia.
“Feasibility has been demonstrated with respect to bioavailability, but the predictability of refractive out comes needs to be refined,” she said. “In addition, work is still needed on lenticule preservation methods that will guarantee the best behaviour when the tissue is reused.”
Prof Cochener-Lamard spoke at the 2023 ESCRS Congress in Vienna.
For citation notes, see page 48.
Non Contact Tono/Pachymeter
Non
New Design Innovations that Incorporate Operator and Patient Comfort with Gentle Measurements
• Fully-automatic measurement*1
• Gentle voice guidance (available in 9 languages)*1
• Reliable tono/pachymeter*2
• Flexible and space-saving design
• A variety of options to meet your needs
Béatrice Cochener-Lamard MD, PhD is Professor and Head of the De partment of Ophthalmology, CHU Morvan Brest – UBO University, Brest, France. beatrice.cochener-lamard@chu-brest.fr





13 2024 FEBRUARY | EUROTIMES
/
Contact Tonometer
*1 Available for the NT-1p and NT-1 *2 Pachymetry is available for the NT-1p. For the NT-1, the corrected IOP is displayed by entering the patient‘s central corneal thickness. www.nidek.com ET 93 x 266mm
MERoV Study Results Preview
Short eyes, low myopia, and low spherical aberration show the formula for pseudoaccommodation following cataract surgery.
ROIBEÁRD O’HÉINEACHÁIN REPORTS

Acombination of low myopic spherical equivalent, lower total eye spherical aberration, shorter preoperative axial length, and smaller pupil size increases the chance of achieving pseudoaccommodation with a monofocal intraocular lens (IOL), according to the findings of the ESCRS-funded Monofocal Extended Range of Vision (MERoV) study.
“Of the four factors we identified in our study, the only modifiable factor is the spherical aberration of the IOL, which can impact the total eye spherical aberration,” lead study author Mayank Nanavaty PhD told EuroTimes. “Therefore, if the patient has a shorter preoperative axial length and a smaller pupil size, then the surgeon can aim for a low myopic spherical equivalent and select an IOL with appropriate asphericity to reduce the total eye asphericity to almost zero.”
The prospective, non-blinded, non-randomised, single-eye cohort study sequentially recruited 412 patients, among whom 301 were available for follow-up at three to nine months. All underwent phacoemulsification and implantation of RayOne IOL (Rayner), a monofocal and aspherically neutral single-piece hydrophobic acrylic lens. The study’s inclusion criteria were uneventful cataract surgery with the postoperative potential for 20/40 (0.3 logMAR) uncorrected distance visual acuity (UCDVA) or better, no significant macular pathology, and willingness to participate in follow-up at three months.
9.6%
The study showed 29 patients (9.6%) achieved pseudoaccommodation
The criteria for pseudoaccommodation were a UCDVA of 20/40 (0.3 logMAR) or better, measured with the ETDRS logMAR chart at 4 m, and a near distance visual acuity (UCNVA) of J5 (0.3 logMAR) or better, measured using a Salzburg Reading Desk at 40 cm. All eyes underwent assessment of mesopic pupil size, keratometry, corneal topography, and wavefront aberrometry with the iTrace aberrometer (Tracey Technologies) and optical biometry with the IOLMaster (Zeiss) or, in those with very dense cataracts, A-scan ultrasound biometry (Accutome).
The study showed 29 patients (9.6%) achieved pseudoaccommodation, with a median UCDVA of 0.12 logMAR and a median UCNVA of 0.3 logMAR. Among those who did not, the median UCDVA was 0.14 logMAR, and median UCNVA was 0.5 logMAR.
Multivariate logistic regression modelling identified preoperative axial length, spherical equivalent, total eye spherical aberration, and mesopic pupil size as statistically significant factors influencing pseudoaccommodation. Comparing those with and without pseudoaccommodation, the respective median values were 23.4 mm and 23.7 mm for axial length, -0.39 D and 0.00 D for spherical equivalent, 0.018 mm and 0.022 µm for total eye spherical aberration, and 3.62 mm and 4.10 mm for mesopic pupil size. The study’s authors noted previous research has shown a correlation between smaller pupil size and reduced spherical aberration, leading to greater contrast sensitivity. Research has also shown that similar amounts of forward movement of an IOL in response to the eye’s natural accommodative reflex may lead to greater defocus in shorter eyes than in longer eyes.
The authors plan further research into accommodation involving different IOL types and may also investigate the effects of binocular summation and the influence of photopic pupil size and factors affecting reading comprehension.
The study has been accepted by the Journal for Cataract and Refractive Surgery and will be published in 2024.
14 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE
Mayank Nanavaty MBBS, DO, FRCOphth, PhD is based at Sussex Eye Hospital, University Hospitals Sussex NHS Foundation Trust, Brighton, UK. mayank.nanavaty@nhs.net

Will Marking Go Digital?
Digitising workflow and marking could improve toric IOL performance.
TIMOTHY NORRIS REPORTS
Although the implantation rate of toric IOLs around the globe is growing, one surgeon out of three is still hesitant to implant this kind of lens in eyes with moderate astigmatism, due to the risk of poor results from misalignment.
According to Tim Schultz MD, this is more of a problem of workflow, and digital marking could be a key to avoiding it.
“One surgeon out of three may not opt for a toric IOL for an eye with a 2.5 D of cylinder. These surgeons are not using toric IOLs because with 10-degree misalignment, we have a 30% reduction of the IOL functionality,” he said. “So, would perfect marking make a perfect result? No, there is much more behind this. We must address the whole workflow, and many problems can come from every step.”
While Dr Schultz said digitalising the workflow can be helpful to avoid errors with manual data entry, it is something to manage with care.
“We can have big variations in our measurements,” he explained. “Using an online calculator can lead to some errors, even if the calculator comes from a reliable source.”
The next step is axis calculation.
“Even in the biggest calculators, a 5- to 10-degree deviation occurs in 20% of cases. It is huge,” Dr Schultz said.
Yet manual markers also come with a price.
“If you ask a surgeon what the best marker is, they will reply, ‘The marker I use is the best,’” Dr Schultz said. “However, there are different kinds of markers with different advantages and disadvantages, especially regarding accuracy, and they all have one problem in common: globe rotation.”
There are several types of digital marking methods already available to surgeons. “Digital drawing is a superb, underrated option, but it is time consuming,” he observed. “Intraoperative measurements are helpful in IOL alignment, but you must enter the patient’s full biometry. Digital overlay is the big top, with automated data in a closed system with good usability, but it also has a high cost. Finally, intraoperative marking has two systems—the camera and the laser—that can do very thin lines on the cornea. This is the game changer.”
According to Dr Schultz, the literature shows slightly better results from digital marking than manual.
“In the trials, very well-performed markings will end up with something around a 4- or 5-degree margin of error. With the laser marking, the margin error is 2 or 3 degrees on average,” Dr Schultz said. “Of all the errors that can come up in the workflow, globe rotation is surely one of the most important. Having some laser markings that can remain visible after surgery—helping to find the correct position during and after surgery—shows how digital marking has an exciting potential to improve surgery. We will see how computer vision and artificial intelligence can further help us.”
Dr Schultz presented at the 2023 ESCRS Congress in Vienna.
15 2024 FEBRUARY | EUROTIMES
Tim Schultz MD, FEBO is Head of Glaucoma and Eye Research Institute at the University Eye Hospital of Bochum, Germany. tim.schultz@kk-bochum.de
Lenticule Extraction Gaining Fans?
New lasers expand options and indications.
CHERYL GUTTMAN KRADER REPORTS
The 2022 ESCRS Clinical Trends Survey showed only 12% of respondents use femtosecond intrastromal lenticule extraction as a treatment for patients interested in refractive surgery. Will the availability of a new femtosecond laser (ELITA), approval of the indication for two existing lasers (Z8 and ATOS), and the anticipated approval of an indication for treatment of hyperopia/hyperopic astigmatism using the VISUMAX 800 laser affect adoption rates?
Together, these features address the needs of patients concerned about flap displacement, dry eye, speed of recovery, and quality of vision after LASIK.
New laser debut
According to Rohit Shetty MD, PhD, lenticule extraction performed using the new ELITA laser in a procedure dubbed “SILK” (Smooth Incision Lenticule Keratomileusis) is characterised by several unique features. First, the intrastromal lenticule has a novel biconvex shape. In addition, the procedure is unlikely to cause irregularity of Bowman’s membrane, and it has minimal effects on spherical aberration (SA), corneal epithelium, and corneal nerves.
“Together, these features address the needs of patients concerned about flap displacement, dry eye, speed of recovery, and quality of vision after LASIK,” Dr Shetty said.
He pointed out that achieving a smooth, wrinkle-free Bowman’s membrane is important for visual quality.
“Outcomes after lenticule extraction depend not only on the quality of the laser and the surgeon’s skill but also on its effects on the corneal tissue,” he said. “Bowman’s membrane irregularity after lenticule removal can result in irregular optics that can be a major cause of poor vision and patient dissatisfaction.”
Creating a biconvex-shaped lenticule profile, demonstrated via a 3.0 D reconstruction of anterior segment OCT maps, strongly impacts quality of vision because it accounts for minimal postoperative change in SA. In an analysis of 125 eyes treated with SILK, mean change in SA at 3 months postoperatively was just 0.02 microns.
“Minimal change in SA is associated with good depth perception and gives patients good night vision,” Dr Shetty said.

He added the procedure also has implications for good depth of focus, as evidenced by data showing the refractive and aberrometric status during accommodation in eyes undergoing SILK was close to that of emmetropic eyes.
Dr Shetty also proposed any impact on corneal nerves is minimised in the SILK procedure, perhaps because the ELITA laser operates at a low energy level and because of the lenticule’s unique shape. He reported corneal nerve regeneration occurs relatively quickly after the surgery.
“Better and faster nerve regeneration likely means less dry eye and better wound healing, resulting in a more regular corneal epithelium,” he said. “A better tear film and smoother corneal surface translate into better optical and visual outcomes.”
Expanding the indication
Data from an international multicentre registration trial demonstrating the efficacy and safety of SMILE for hyperopia/hyperopic astigmatism have been submitted to support CE mark receipt.1 With approval, this procedure will provide an excellent new option for laser vision correction, said Walter Sekundo MD, PhD.
The registration trial used the VisuMax laser to create lenticules. However, when the software for hyperopia and hyperopic astigmatism treatment is released, it will be available only for the next-generation VISUMAX 800.
16 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE

Dr Sekundo explained that multiple modifications to the procedure improved the hyperopic lenticule extraction outcomes performed with the original VisuMax laser over time. However, the suction loss rate in the registration trial was unacceptably high at 1.34% and related to the treatment time of about 35 seconds.
“The solution to this problem is to use the VISUMAX 800. We showed a porcine eye model took 12 seconds to cut the hyperopic lenticule,” Dr Sekundo said.
“Since I began using the VISUMAX 800 in October 2021, I have not had a single case of suction loss during SMILE pro procedure.”
The VISUMAX 800 also offers cyclotorsion adjustment and a patented computer-assisted centration function, which addresses the heightened need for excellent centration in hyperopic treatments.
Summarising other results from the registration trial, Dr Sekundo reported that 69% of the 219 eyes targeted for plano distance achieved UCVA of 20/20 or better at 12 months. Only 1.2% of the 374 eyes in the total cohort lost two or more lines of corrected distance VA.
“I remind you that loss of corrected VA is more common with a hyperopic versus myopic laser treatment, and so these are excellent results,” Dr Sekundo said.
Some undercorrection was seen in the predictability analysis, and it was more significant in eyes treated for higher levels of hyperopia. The commercially released software will incorporate a nomogram adjustment based on this finding.
“Even so, the achieved refraction was within 0.5 D of intended in 81% of eyes, which is slightly better than LASIK and an excellent result for a hyperopic treatment,” Dr Sekundo said.
“Refractive stability was good overall. While there was some regression between 3 and 12 months, it unclear if the shift is the result of late epithelial healing or progression of presbyopia.”
Dr Shetty and Dr Sekundo spoke during the 2023 ESCRS Congress in Vienna.
For citation notes, see page 48.
Rohit Shetty MD, PhD is Chairman of Narayana Nethralaya Eye Institute, Bangalore, India. drrohitshetty@yahoo.com
Walter Sekundo MD, PhD is Professor and Chair, Department of Ophthalmology, Philipps University of Marburg, Germany. sekundo@med.uni-marburg.de
17 2024 FEBRUARY | EUROTIMES
What is the Best Option for Hyperopia?
Two renowned surgeons engaged in a thought-provoking debate in Vienna.
TIMOTHY NORRIS REPORTS
During the 2023 ESCRS Congress in Vienna, close to where the famous boxing arena saw two surgeons fighting one against the other on divisive topics, a single, brief showdown at the JCRS symposium between two illustrious surgeons took place between Pavel Stodůlka MD, PhD and Michael Knorz MD.


Opinions and clinical experiences were donned as gloves. A couple of very clever jabs, none below the belt, and some direct hits occurred here and there as the crowd cheered. The theme was refractive options for hyperopia between 2 and 9 dioptres, with Dr Knorz in support of lenticular options and Dr Stodůlka in favour of corneal refractive procedures.
Two different points of view emerged, placing patient happiness first on one side, and the rate of unhappy patients on the other.
“I will never do any corneal laser surgery over +3.0 D,” Dr Knorz said. “The reason is that about 15 years ago, I did a study for 1.0 to 3.0 D, 3.0 to 6.0 D, and 6.0 to 9.0 D, published in the Journal of Refractive Surgery, and the outcome was clearly inferior over 6.0 D with plenty more unhappy patients.”
“I think you are absolutely right [about] 10 years ago,” Dr Stodůlka replied, “but laser technology has really evolved over these years. I think LASIK for +4.0 D and +5.0 D is successful. And with SMILE, it is going to be even better: in 100 procedures, I have not seen a single unhappy patient.”
“Maybe you needed 100 patients with +6.0 D on the study, and I guarantee you would have 10% unhappy patients in that case,” Dr Knorz answered.
After the discussion, both contenders doubled down.
“I was more in favour of the intraocular solution for hyperopia from 2 to 9 dioptres, and apparently I am not a proponent of doing all on the cornea alone,” Dr Stodůlka said. “So, for patients who are older than 40, we do intraocular surgery and refractive lens exchange—typically with trifocal lenses, or it can be monofocal, monovision, EDOF, etcetera.
“For the younger patients, we still perform LASIK, and we hope we will soon be able to clinically perform hyperopic SMILE. I was part of the first international study, on more than 100 eyes, and the patients were very, very happy. The optical zones are large, and the results were exciting,” he said. “Hyperopic SMILE is going to take off quite soon.”
Hyperopic SMILE is going to take off quite soon.
Dr Knorz’s defensive stance was perfectly in line with the German guidelines. “In Germany, we have a guideline that says you should not perform laser refractive surgery for more than +3.0 D of hyperopia. The reason for this is when
18 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE
you do higher ablations, even with moderate ablation algorithms, you create a lot of corneal aberrations [that] lead to significant visual disturbances in about 5 to 10% of patients,” he said. “So, we are not questioning the high success rate for those 90 to 95% happy patients. But we are concerned about the 5 to 10% of unhappy patients because, unlike the intraocular approach, they cannot be undone. That’s why one conclusion of my talk is you should not do LASIK, or SMILE, or PRK for more than +3.0 D of hyperopia.”
“I think the part where we do not have the same strategy was the young hyperopes with hyperopia higher than 3.0 D,” Dr Stodůlka said. “Professor Knorz would not perform LASIK or any kind of corneal refractive surgery. He fears the aberrations with the recent technologies of the latest generation of excimer lasers. With thicker flap and LASIK extra and with SMILE, we have very nice results—and we have happy patients, so that was a little bit different approach.”
“My main point of disagreement with Dr Stodůlka, who I really highly regard as a very good surgeon, is his focus on the success for the patient, while my focus is on the
problem some patients may experience,” Dr Knorz said. “In our EuroEyes clinic, we perform more than 1,000 cases every year, and if you do these numbers and have 5% of unhappy patients, you will find yourself with a really significant number.”
“We both agreed that [in patients] over 40, we should only do refractive lens exchange because the hyperopic patient has no risk of retinal detachment,” Dr Knorz said. “The hyperopic patient has small eyes, shallow angles with high risk of glaucoma—all these things get better with a refractive lens exchange in addition to actually making them spectacle independent. On this we completely agree.”
Michael C Knorz MD is medical director of the FreeVis LASIK Center Mannheim, EuroEyes Group, Germany. knorz@eyes.de
Pavel Stodůlka MD, PhD is founder, chief surgeon, and CEO of Gemini Eye Clinics in the Czech Republic and Vienna, Austria. stodulka@lasik.cz
ESCRS Academies
Committee representatives of ESCRS organise and present sessions at those meeting organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually. These sessions provide useful education as well as collaboration between societies memberships.
19 2024 FEBRUARY | EUROTIMES
escrs.org/education/academies/
It’s in the Bag
ESCRS Heritage Lecture explores the enigma of the anterior hyaloid.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
The anterior hyaloid has remained a matter of controversy since its earliest description in terms of its relationship with other parts of the intraocular anatomy, its strength, and its distinction from the posterior capsule. Research now confirms its actual nature and role in separating the anterior segment from the vitreous cavity, said Marie-José Tassignon MD, PhD in her Heritage Lecture at the 2023 ESCRS Congress in Vienna.
“Most illustrations tend to leave out the anterior hyaloid,” she noted. “But it is important because the anterior hyaloid is the membrane that separates the anterior segment from the posterior segment. And it is not the posterior capsule.”
Descriptions of the anterior hyaloid date back to the late nineteenth century, possibly the eighteenth. The hyalo-capsular ligament—“Wieger’s ligament”—that fastens the anterior hyaloid to the periphery of the posterior lens capsule was first demonstrated by Germain Wieger in 1883. In his 1887 medical thesis, Emil Berger created anatomical illustrations of the space between the anterior hyaloid and the posterior capsule, now known as Berger’s space (BS).1, 2
However, textbooks continued to describe Berger’s space as somehow “virtual” in nature. Professor Tassignon noted that in 1999, Jan Worst invited her to Groningen, Netherlands, to collaborate in research demonstrating it possible to use a staining technique to visualise BS. Further research conducted with the fluorophotometer (Fluorotron) developed by José Cunha-Vaz showed fluorescein injected into the anterior chamber primary posterior capsulorhexis did not diffuse into the vitreous so long as there was no damage to the anterior hyaloid.
Prof Tassignon noted the presence of Berger’s space can also be easily demonstrated by gently puncturing the posterior capsule with a lateral capsule-dragging approach and injecting an ophthalmic viscosurgical device underneath. If the anterior hyaloid is intact, the OVD will spread homogeneously until it reaches Wieger’s ligament. In addition, Prof Tassignon and her associates were able to demonstrate the presence and dimensions of BS and the anterior hyaloid face intraoperatively using an optical coherence tomography (OCT) system attached to the Opmi Lumera 700/Rescan microscope (Zeiss).3
These findings were important in confirming the safety of Prof Tassignon’s bag-in-the-lens (BIL) intraocular lens (IOL). Designed to prevent posterior capsule opacification, the lens is implanted after posterior capsulorhexis for implantation and clasps the anterior and posterior capsule in a groove between its plate-like haptics.
“Based on all these accumulations of knowledge, we were able to implement the ideal adult BS dimensions in the ideal Gullstrand eye model, which should be 8.0 mm to 9.0 mm,” Prof Tassignon said. “Definitely big enough to accommodate a lens of 7.5 mm, and that is why the diameter of the BIL is 7.5 mm.”

She added that while she has not conducted comparative studies, the BIL does not appear to endanger the retina. She has observed no excess in retinal detachment, and among normal eyes with no ocular nor systemic comorbidity factors implanted with the lens, there have been no instances of macular oedema.
She also noted that as a patient ages, their eyes become increasingly prone to anterior vitreous detachment, just as with posterior vitreous detachment. This can be demonstrated by a “spaghetti-like” diffusion of OVD injected beneath the posterior capsule.
A pathology of the hyaloid and posterior capsule, called anterior vitreolenticular interface dysgenesis (AVLID), appears to play a role in paediatric cataract, Prof Tassignon said. The condition arises from a repair mechanism from the lens epithelial cells in the capsular bag and the hyalocytes from the vitreous face that transform into fibroblasts, creating opaque plaques.
“In such cases, one option is to place the anterior capsule, anterior hyaloid, and posterior capsule within the groove of the lens, restoring the kind of attachment of the anterior hyaloid as it is in nature,” she added.
For citation notes, see page 48.
Marie-José Tassignon MD, PhD, FEBO is emeritus chair and chief of the department of ophthalmology at the University Hospital of Antwerp, Belgium. She is a past president of the ESCRS.
20 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE
Refractive Surgery for Myopia
Posterior chamber phakic IOL offers a safe and accurate option for growing candidate pool.
CHERYL GUTTMAN KRADER REPORTS
Implantation of the posterior chamber phakic implantable collamer lens (ICL) offers a very accurate and safe option for improving visual acuity in eyes with all levels of myopia, according to Roger Zaldivar MD.
“By 2050, 50% of the world’s population will be myopic, including about 1 billion people with more than 6.00 D of myopia. Piggybacking on these data, consider that about 6 million people drop out of contact lens wear each year,” he said.
“I encourage surgeons who have not implanted the ICL to think about using it. In my opinion, it will be the refractive procedure that will have the most growth in the next couple of years.”
List of attributes
Made of a collagen co-polymer with its biocompatibility established through a 30-year track record, he noted the current version of the ICL with its central port allows for both greater safety and faster surgery compared to previous iterations.
“The central port was a game changer,” Dr Zaldivar said. “It eliminated the need to perform a peripheral iridectomy and revolutionised the procedure’s safety profile. Today, the whole surgical procedure takes less than five minutes.”
Compared with all other surgical treatments, the ICL also has the highest safety and efficacy index. Dr Zaldivar cited an analysis of a large cohort of eyes stratified into three groups according to baseline refraction that showed mean CDVA improved from baseline in all groups—but the magnitude of improvement increased as the degree of baseline myopia increased.1
“We found some eyes treated for >10.00 D of myopia gained four or more lines of CDVA,” Dr Zaldivar said.
Consistent with its efficacy and safety profile, the ICL has garnered high levels of patient satisfaction.
“Even among low myopes, who are perhaps the most difficult patients to make happy, we found 92% rated their satisfaction as ‘10’ (the highest level), and the other 8% graded satisfaction as ‘9’,” Dr Zaldivar said.
Patient selection and procedure tips
The ICL is available in powers ranging from -1.00 D to -18.00 D. Based on its clinical performance, Dr Zaldivar said he is now comfortable offering it to patients aged up to 52 years, whereas his previous cut-off was 45 years.
Appropriate patients would have demonstrated stable refraction and an anterior chamber depth ≥3.00 mm. Shown through the use of a very high-frequency digital ultrasound robotic scanner that the ICL rests on the ciliary body in ~80% of eyes, Dr Zaldivar said he has developed a new formula based on ultrasound measurement that accurately predicts ICL vault, building his confidence in achieving a safe outcome.2
Offering surgical tips, Dr Zaldivar said creating a generous main incision and using the Zaldivar ICL Manipulator for implantation help avoid flipping the IOL. He also recommended using a specific 2% methylcellulose product (OcuCoat) for filling the anterior chamber and being careful when aspirating viscoelastic at the end of the procedure.
“Aspirate gently in a circular pattern over the lens, and do not over-aspirate in the centre because the turbulence created could induce cataract by pushing fluid through the central hole.”
Dr Zaldivar spoke during the 2023 ESCRS Congress in Vienna. For citation notes, see page 48.
Roger Zaldivar MD, MBA is CEO of the Instituto Zaldivar in Mendoza, Argentina. zaldivarroger@gmail.com

21 2024 FEBRUARY | EUROTIMES

Intraoperative Aberrometry in the Balance
IA can boost the predictability of refractive correction but adds time to surgery.
TIMOTHY NORRIS REPORTS
More predictable refractive outcomes and significant clinical benefits in challenging cases (such as toric IOL implantation in patients with low levels of corneal astigmatism) can be achieved using intraoperative aberrometry (IA), according to David Pablo Piñero Llorens PhD.
“IA measures the refractive state of the eye during cataract surgery, guiding surgeons in real time for IOL power selection and positioning, as well as detecting corneal curvature changes,” Dr Llorens said. “At present, the Optiwave Refractive Analysis (ORA, Alcon) is the only model that can be purchased; it is connected to a software with its own exclusive closed database. There is another model that is not available commercially at the moment.”
According to Dr Llorens, several variables can affect the accuracy of IA measures, lowering the repeatability.
“The intracameral presence of viscosurgical devices can affect the measurement of IOL power,” he explained. “In addition, ocular surface irregularity and intraocular pressure can also play a role, as well as the lid speculum and its position, because it puts some pressure on the globe and can make some modifications to the geometry of the cornea and other structures of the anterior chamber.”
Moreover, IA comes with one issue that must be addressed. “As you can imagine, the main inconvenience is the increase in surgery length: this can lead to less surgical efficiency. We must prepare the eye for this measurement, the device for the analysis, and look at the data. On average, the use of an IA increases the overall time by 3 minutes and 45 seconds compared to normal surgical time.”
Yet one of IA measurement’s major benefits, the potential optimisation of surgical outcomes, carries a controversial aspect.
“Many studies have demonstrated that the use of the currently available generation formulas should seem sufficient to produce clinical outcomes with toric IOLs as good as we can achieve with IA.”
One of the most difficult challenges comes with IA and FLACS use in low corneal astigmatism.
“Compensation with toric IOLs will have a lower predictability of refractive correction, with a significant contribution of posterior corneal astigmatism and a significant impact of small IOL misalignments or rotations. However, the combination of FLACS and IA to optimise the position and calculation of a toric IOL may allow a very efficacious correction of pre-existing low to moderate corneal astigmatism,” he said.
“Intraoperative aberrometry can be useful to improve the predictability of refractive correction with toric IOLs—especially in eyes with corneas with low astigmatism—but some factors must be controlled for an accurate procedure, such as lid speculum and OVD.”
Dr Piñero Llorens spoke during the 2023 ESCRS Congress in Vienna.
David Piñero Llorens OD, PhD is Associate Professor of the Department of Optics, Pharmacology, and Anatomy at the University of Alicante, Spain. david.pinyero@ua.es
22 EUROTIMES | FEBRUARY 2024 CATARACT & REFRACTIVE

23 2024 FEBRUARY | EUROTIMES Educational Resources Advanced FEBOS-CR Exam/Diploma (Cataract and Refractive Surgery) ESCRS iLearn • ESCRS Research Portals • Important Publications
EuroTimes Podcasts • ESCRS on Demand • JCRS Online Case Reports The Video Journal of Cataract, Refractive, and Glaucoma Surgery escrs.org/education/educational-resources
ESCRS

SET YOUR SIGHTS ON FRANKFURT! Register now!
Mark your calendar now for the 2024 ESCRS Winter Meeting 15–18 February in Frankfurt!
The ESCRS Winter Meeting is a unique opportunity for ophthalmologists, researchers, and industry representatives to exchange ideas and insights about the latest advances and challenges in cataract and refractive surgery, whilst also providing an ideal setting to network with colleagues and forge new connections.
Review the Winter Meeting Programme
The 2024 Winter Meeting programme is now available online at https://wintermeeting.escrs.org/ programme/. It has been crafted for an immersive experience that promises to deepen your knowledge, expand your professional network, and shape the future of refractive expertise through its two main tracks, Intraocular Refractive Surgery and Corneal Refractive Surgery, running in parallel to the DGII Programme.
Register Now to Secure Your Space
Registration for the 2024 Winter Meeting is now open! Register at https://wintermeeting.escrs.org/ registrations/ to ensure you take advantage of all the Winter Meeting has to offer, from symposia and free paper sessions to instructional courses and wetlabs to the young ophthalmologists programme. New networking features will also be offered.

REGISTER NOW: https://wintermeeting.escrs.org/registrations/

Experience a Conference Like No Other
Prepare to immerse yourself in a groundbreaking experience at the ESCRS 2024 Winter Meeting in Frankfurt. You’ll experience a host of innovative initiatives that will revolutionize your conference journey. Spaces are limited, so secure your spot early to ensure you don’t miss out on these exclusive opportunities.
Collaborative Innovation in Action
Experience the unique “unconference” format, where you wield the power to shape sessions based on your interests. Dive into participant-driven discussions, ignite collaborations, and innovate within an open, dynamic environment. Be at the forefront of the agenda-setting process, fostering an engaging and personalized experience.
Share, Engage, and Learn
Participate in intimate roundtable discussions offering the perfect setting to share your ideas, experiences, and expertise with peers on relevant conference topics.
Guided Exhibition Tours with ESCRS Experts
Join guided exhibition tours led by members of the ESCRS Executive Committee. Gain firsthand insights and knowledge from industry veterans while exploring the latest advancements. It’s an ideal opportunity for young ophthalmologists to glean wisdom from seasoned professionals.
Escape Room Challenge: A Unique Learning Adventure
Embark on an immersive adventure in our Escape Room. Work together with your peers to solve intricate medical cases. You’ll foster teamwork, critical thinking, and problem-solving skills in an engaging and interactive setting.
Spotlight Theatre: Cutting-Edge Industry Presentations
Engage with exhibitors showcasing their latest innovations in an interactive Spotlight Theatre. Witness firsthand the advancements that are shaping the future of refractive surgery.
New Conference Tracks: Intraocular and Corneal Refractive Surgery
Ready to elevate your expertise in refractive surgery? Experience our new conference tracks focused on Intraocular and Corneal Refractive Surgery. Take a deep dive into these themed tracks covering essential topics across the entire educational programme.
Six Essentials to Iris Repair
In the first of a multi-part series, Dr Soosan Jacob describes an introduction to the basics of iris repair.
DR SOOSAN JACOB REPORTS
Iris repair is an integral part of many ocular surgeries, and every anterior segment eye surgeon should learn a few basic techniques. Usually performed as part of anterior segment reconstruction, it is sometimes also required of cataract surgeons, e.g., in case of iris damage following continual iris prolapse in intraoperative floppy iris syndrome. Complex surgeries that require peripheral anterior synechiolysis or release of posterior synechiae may also necessitate iridoplasty techniques.
In addition, sometimes one may need to operate on a patient with cataract co-existent with pre-existing iris damage—either as part of a pathology (e.g., iridocorneal endothelial syndrome) or secondary to post-traumatic/iatrogenic iris damage. In all these situations, it is beneficial to be well-versed in basic iris repair techniques. This multi-part series on iris repair will cover everything about the topic.
Iris anatomy
The iris consists of the pupillary and ciliary zones, with the thickest part the collarette (lying 2 mm around the pupil) and the thinnest the iris root. The circular sphincter pupillae and the radial dilator pupillae constrict and dilate the pupil, respectively. The pupillary ruff is the dark border of the pupil and formed by the posterior pigment epithelium wrapping around the pupillary margin. The anterior ciliary and long posterior ciliary arteries anastomose in the ciliary body (CB) to form the major and minor arterial circles that lie in the anterior part of the CB and along the pupillary border and are joined by radial vessels weaving
through the iris stroma. The formed radial network can bleed into the anterior chamber (AC) during surgical iris trauma.
Synechiolysis
Peripheral anterior synechiolysis is sometimes needed in patients with prior surgery or other pathology. The iris should be carefully examined for signs of neovascularisation, atrophy, or prior defects. In every synechiolysis case, care should be taken to keep the AC pressurized, which may be done using viscoelastic or an AC maintainer and working through small incisions. Pressurization of the chamber is important to rapidly tamponade any possible bleeding from the iris. Hypotony will delay clotting and keep blood oozing for longer. Synechiolysis should be done gently by viscodissection, and if this proves difficult, then with either the rounded viscoelastic cannula or a blunt rod. Rough manoeuvres should be avoided as this can lead to iris tears, iridodialysis, and even Descemet’s detachment.
Posterior synechiolysis is required in some cases, especially post-uveitic cataracts. These can also often be released by gentle viscodissection. However, the pupil may remain non-dilating, and if additional procedures (such as cataract extraction, IOL explantation, or vitrectomy) are needed, some other pupillary dilatation technique such as mini-sphincterotomies, iris hooks, B-Hex, or Malyugin ring may be needed. Some of these cause iris tears and need iris repair, while others are gentler on the sphincter and do not need additional procedures.

Iridectomy
Though iridectomy is not a type of iris repair, it is sometimes required in combination with anterior segment reconstruction surgeries and often required during glaucoma, corneal, or vitreoretinal procedures. A peripheral iridectomy is best done in the superior periphery but may be required inferiorly to prevent a pupillary block when air or silicone oil is left in the eye. It may be done preoperatively using a YAG laser but also intraoperatively using a vitrector in I/A-cut mode with a very
LEGEND FOR FIGURE:
Figure: A) Post-uveitic peripheral anterior synechiae. B, C) Iris membrane dissection with a sharp 23-gauge needle. This fibrous membrane can be removed, freeing up the iris below for reconstruction. D) Iridectomy with a vitrector.
CORNEA 26 EUROTIMES | FEBRUARY 2024
low cut rate and vacuum of about 300 mmHg. It is done after constricting the pupil using intracameral miotics.
In pseudophakic eyes, Fang et al. have described a technique of introducing a sharp needle (with its tip bent to 45 degrees) posterior to the iris that is bellowed upwards with viscoelastic.1 The bend is held horizontally to prevent iris snag and, once in position, turned anteriorly to engage the iris while applying posterior pressure with an iris repositor. The puncture is then enlarged with a microscissor. The approach should be from a comfortable angle for both instruments. Techniques that involve cutting the iris directly below the base of an incision run the risk of a poorly positioned iridectomy and iris base damage.
Iris membranes
The iris is a pro-inflammatory structure and iris membranes can often form, especially after severe episodes of intraocular inflammation. These membranes are fibrotic with varying levels of vascularisation and can hold the iris fixed in different positions. Membrane peeling can be done from over the iris using a combination of instruments. The sharp point of a 23-gauge needle can be inserted under the membrane, and the membrane gently dissected off the iris. Microforceps and microscissors can also be used to cut fibrous strands and remove them. Often, the entire iris then becomes mobile and free if not excised during any previous surgery. This freed iris tissue can then be pulled into position for iridoplasty.
Pupillary fibrous membrane
Sometimes a pupillary membrane may be found occluding the pupil, especially if associated with pre-existing uveitis, rubeosis, trauma, or post-surgical inflammation. This may be peeled off using microforceps or, if difficult, cut and removed using a combination of microforceps and microscissors or even a vitrector. In case of phakic eyes, care should be taken not to damage the lens. Sometimes, a fibrous band may encircle the pupillary aperture, and this can also be removed using microforceps.
iLEARN
ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
Management of iris defects without intraocular surgery
Iris defects may exist from a previous surgery or trauma. This may result in photophobia, difficulty looking at light, polyopia, stray light, etc. Iris defects may be managed conservatively using tinted glasses or aniridic contact lenses, which have a clear central optic zone and a coloured periphery. Focal corneal tattoos may also be helpful in certain situations—e.g., if a peripheral iridectomy or an iridodialysis is not covered by the lid, causing symptoms. It can also be used for traumatic iris defects and aniridia. Tattoo application can be superficial or intra-lamellar into a femtosecond laser-created channel.
The next article in this series on iris repair will deal with pupilloplasty techniques. Stay tuned!
For citation notes, see page 48.
Soosan Jacob MS, FRCS, DNB is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.

27 2024 FEBRUARY | EUROTIMES

Best Practices in Cataract Surgery
Perform surgical planning only after managing ocular surface disease.
CHERYL GUTTMAN KRADER REPORTS
Diagnosis and management of existing ocular surface disease (OSD) before cataract surgery is critical for maximising patient satisfaction and outcomes after the cataract procedure, said Allan R Slomovic MD.
“Failure to detect and manage OSD prior to cataract surgery can result in postoperative refractive surprises due to inaccurate keratometry and biometry data and worsening of dry eye disease,” he explained.
“The ophthalmologist’s role is to optimise the ocular surface before and after surgery and to set realistic expectations. Explain to patients that they have two separate problems— their cataract and their OSD—and the OSD must be treated first to get optimum results from the cataract surgery.”
Dry eye disease (DED) is the most common OSD encountered in the typically older population of patients undergoing cataract surgery, noted Dr Slomovic, citing a study reporting 80% of cataract patients had at least one abnormal tear test result suggestive of OSD.1
The potential consequences of not treating DED before cataract surgery include delayed visual recovery, refractive surprises, patients unhappy because of DED symptoms and suboptimal vision, and even an increased risk for infection. Highlighting the importance of treating DED preoperatively, Dr Slomovic detailed a study he conducted showing a sixweek regimen of topical lifitegrast 5% resulted in significant improvements in DED-related signs and symptoms along with biometry changes affecting planned IOL power by 0.5 D in 33% of eyes.
He also called attention to considering the potential adverse effects of topical medications typically prescribed for patients undergoing cataract surgery and cautioned against using NSAIDs postoperatively in patients with significant DED.
“Multiple papers also report corneal melting in patients treated with NSAIDs after cataract surgery, and I have personally seen that NSAIDs in this setting can result in corneal ulcers, melting, and even perforation,” Dr Slomovic said, adding that he chooses to use a steroid alone for these patients.
Pterygium, epithelial basement membrane dystrophy (EBMD), and Salzmann’s nodular corneal degeneration are also seen fairly frequently in patients presenting for cataract surgery. All these conditions cause astigmatism, and both EBMD and Salzmann’s nodules can cause reduced vision.
“Understanding best practices for managing a patient with pterygium requires knowledge that the pterygium affects the ocular surface in three ways,” Dr Slomovic said.
“It causes flattening of the cornea in the area of the pterygium, results in irregular with-the-rule astigmatism, and increases higher-order aberrations.”
He shared another study he conducted showing pterygium excision resulted in reduced topographic and refractive astigmatism, allowing for more accurate biometry, and was associated with improved best-corrected visual acuity and reduced higher-order aberrations.
“Remove the pterygium with a conjunctival autograft before cataract surgery, and then wait six to eight weeks for the ocular surface to heal before performing biometry,” Dr Slomovic recommended.
Similarly, he advised treating EBMD or a Salzmann’s nodule before cataract surgery by performing a superficial keratectomy and waiting six to eight weeks for healing.
“We have seen that both the axis and amount of astigmatism changed significantly after superficial keratectomy,” Dr Slomovic said.
Dr Slomovic spoke at Cornea Day before the 2023 ESCRS Congress in Vienna. He acknowledged the assistance of his daughter, Jacqueline Slomovic MD, an ophthalmology resident, in preparing the presentation.
For citation notes, see page 48.
Allan R Slomovic MSc, MD is Marta and Owen Boris Endowed Chair in Cornea and Stem Cell Research and Professor of Ophthalmology, University of Toronto, Canada. allan.slomovic@utoronto.ca
28 EUROTIMES | FEBRUARY 2024
CORNEA
Treatment at a Crossroads
Multiple unknowns challenge surgical decisions treating comorbid cataract and Fuchs’ dystrophy.
CHERYL GUTTMAN KRADER REPORTS
Ahigh prevalence of cornea guttata among persons 55 years and older, combined with the expected increase in the size of the older population, suggests the number of patients with comorbid cataract and Fuchs’ endothelial corneal dystrophy (FECD) is significant and will continue to grow, observed Björn Bachmann MD, PhD.
Determining the proper approach to treating these patients requires surgeons first consider whether both cataract surgery and endothelial keratoplasty (EK) are necessary.
“Answering this question can be difficult, however, because existing classification systems for cataract and FECD do not always correlate well with the visual impairment patients are experiencing,” Dr Bachmann said.
“Making the decision to do cataract surgery by itself or just EK is also challenging because there are no good parameters for predicting whether the untreated condition will get worse.”
He added it is important not to do EK if it is not necessary, considering the need for long-term steroid treatment to minimise the risk of graft rejection.
“Even though the regimen may be tapered to just one drop daily, patients need to be on steroids for two years, and that is a long time.”
Weighing the options
Ultimately, surgical management of patients with both cataract and FECD can be approached by performing combined surgery or with a staged approach that begins with either the cataract procedure or Descemet membrane endothelial keratoplasty (DMEK) followed by the other procedure either as a planned intervention or if it seems necessary. Each approach has advantages and disadvantages and requires special attention to IOL power calculation.
For patients with pronounced corneal oedema and cataract, combined surgery offers the benefit of rapid success, but
achieving an accurate refractive outcome in these cases can be challenging. According to a recent study, using a keratometry value adjusted for the abnormal posterior-to-anterior corneal curvature radii ratio after DMEK can reduce the risk of a hyperopic shift after the combined procedure, Dr Bachmann said.1
He suggested a sequential approach beginning with cataract surgery as suitable for patients with mild or subclinical corneal oedema, adding it could avoid DMEK if the patient is satisfied after cataract surgery. However, if the IOL calculation does not anticipate DMEK and the transplant is needed, the eye will end up hyperopic following DMEK. As another consideration, there are no proven measures for determining risk for endothelial decompensation after cataract surgery, although a recently described risk prediction model may be helpful.2
Regarding sequential surgery beginning with DMEK, Dr Bachmann suggested this approach is suitable for younger patients with corneal oedema/opacification and a clear lens or for patients with cataract and massive opacification that prohibits visualisation during cataract surgery. However, there is the potential for harm to the transplanted endothelium by subsequent cataract surgery, and no trials are investigating the accuracy of IOL calculations after phakic DMEK. He suggested surgeons refer to a readily available online platform (http://www.eomy.kr/kadjiolcalc/) to help choose the IOL power after DMEK.
Dr Bachmann spoke during Cornea Day before the 2023 ESCRS Congress in Vienna.
For citation notes, see page 48.
Björn Bachmann MD, PhD is Professor of Ophthalmology, University of Cologne, Germany. bjoern.bachmann@uk-koeln.de

2024 FEBRUARY | EUROTIMES 29
Charting the Glaucoma Course
Tips on IOP control devices with the EGS Guide on Surgical Innovation.
TIMOTHY NORRIS REPORTS
Following the introduction in the last decade of many surgical options for the management of intraocular pressure (IOP) in open-angle glaucoma (POAG), the European Glaucoma Society (EGS) has produced a new reference book— the aptly named A Guide on Surgical Innovation in Glaucoma. As stated by the EGS itself, the guide answers the need to gather evidence and provide recommendations to support clinicians in making decisions, as well as proposing a core outcome set to enable benchmarking across studies on surgical innovation.
Introduced during the 2023 ESCRS Congress in Vienna, the new guidelines served as a backbone for the Glaucoma Day symposium held on day one of the Congress.
A plethora of treatments
“I think the EGS decided to make us a little more aware of what we are all doing with all these kinds of new devices and procedures,” Antonio Fea MD, PhD said during the symposium. “So, in terms of MIGS and bleb-forming devices, what are our options?”
Along with the non-device-based treatments, Dr Fea clarified the many differences between microinvasive glaucoma surgery (MIGS) and microinvasive bleb surgery (MIBS) devices, divided into three main categories.
“Some devices address the Schlemm’s canal, trying to increase the outflow facility following Goldman’s equation. There are suprachoroidal devices using alternative pathways and are completely independent of IOP. Finally, there are the subconjunctival devices that are really relying on the Hagen Poiseuille equation. These are all different from a clinical perspective,” he said.
In the end, choosing the right device wisely makes the patient and yourself happy.
“In the trabecular and suprachoroidal devices, you have a cataract-like follow up, while the bleb-forming devices may need revisions and needling due to fibrosis.”
According to Dr Fea, the devices addressing the Schlemm’s canal, like iStent (Glaukos) and Hydrus (Alcon), while being very fast to implant and less disruptive of the anatomy, are usually also less effective in terms of IOP lowering and less predictable between individual patients.
“On the other hand, the suprachoroidal devices still have a phaco-like follow up, but with potential complications such as IOP spikes,” he explained. “Finally, the subconjunctival MIGS, with the ongoing fight between the two big guys (Preserflo [Glaukos] and Xen), are one of the more effective in this arena.”
Dealing with the elephant
According to Verena Prokosch MD, PhD, IOP in glaucoma is like an elephant jumping on the lamina cribrosa—IOP lowering is the only thing that really makes the difference.
“Every millimetre of mercury really counts,” she said.
Dr Prokosch went on to observe things have drastically changed for the better in the last five decades.
“Nowadays, we have many different devices and options on our hands, so now the question is, how much IOP lowering do we get?” Dr Prokosch asked.
30 EUROTIMES | FEBRUARY 2024 GLAUCOMA
As cited in the Guide on Surgical Innovation, there is consensus a 3-mmHg reduction is a clinically relevant measure—best achieved using IOP control devices rather than phaco alone, as shown in pivotal studies.
The HORIZON study showed a 34% increase in IOP reduction with the Hydrus implant and cataract surgery when compared to phaco alone. The COMPASS trial with the CyPass Microstent, now off-market, showed a 25% increased reduction compared to phaco, and in the US IDE trial, the iStent inject the difference with phaco alone was 22%.
The right choice for the best MIGS device also depends on the patient.
“It is important to look at the target IOP and how much risk we want to have. This depends not only on the guidelines but also on factors like the rate of progression of the disease, the situation of the other eye, family history and the life expectancy of the patient, and if there is a combination with phaco,” Dr Prokosch explained.
“In the end, choosing the right device wisely makes the patient and yourself happy, and to know how much IOP lowering it provides is quite important—as is, in terms of IOP lowering, the less you risk, the less you get.”
To combine or not to combine
According to Carlo Traverso MD, “the evidence is out” for what is the best device and the best technique to use for specific patients.
“Whenever the clinical condition allows it, sequential surgery with phaco performed initially should be considered,” he said, quoting the new book. “This is pretty generic, but also very wise. Often in clinical management, we are loaded with things to worry about, and simple approaches are forgotten.”
If preoperative IOP is high or advanced disease is present, a bleb-forming device as a standalone procedure or in combination with phacoemulsification surgery should be preferred to MIGS.
“If you have advanced disease, your target IOP is lower, and there is no chance you get that with a trabecular gadget,” he stressed.
Antonio Maria Fea MD, PhD is an ophthalmologist, head of glaucoma at the ocular clinic, and aggregate professor at the University of Turin, Italy. antoniomfea@gmail.com
Verena Prokosch MD, PhD is Professor at the University of Cologne, Germany. verena.prokosch-willing@uk-koeln.de
Carlo Enrico Traverso MD is head of the Ophthalmology Department at the Policlinico Ospedale San Martino, Professor at the University of Genoa, Italy. carlo.enrico.traverso@unige.it

Your specialist for easy-to-use high-tech solutions.
TOMEY is committed to maximum quality, service, and innovation. This leads to early prevention, accurate diagnoses, and examinations that are as comfortable as possible.
Get to know our products in the fields of:
+ Cataract & Cornea
+ Glaucoma & Retina
+ Refraction
+ Refraction Units & Furniture
31 2024 FEBRUARY | EUROTIMES
ESCRS Winter Meeting TOMEY product guide
Booth B15 Hall 5.1

Oral Treatment for Stargardt Disease
Mixed results in phase 2 trial investigating remofuscin.
CHERYL GUTTMAN KRADER REPORTS
Aphase 2 study investigating oral remofuscin treatment for recessive Stargardt disease 1 (STGD1) failed to meet its primary endpoint assessing efficacy for reducing the amount of lipofuscin in retinal pigment epithelial (RPE) cells. However, questions were raised about the chosen metric for measuring lipofuscin (quantitative fundus autofluorescence [qAF]) after it was found to have high test-retest variability,1 and results for secondary endpoints supported the benefit of remofuscin for slowing retinal thinning and maintaining visual function compared to placebo, reported Carel Hoyng MD, PhD.
“After assessing the repeatability of qAF imaging for patients in this study, we concluded that we picked the wrong primary endpoint,” he said. “Since there is no treatment for STGD1, perhaps remofuscin may be accepted for fast approval.”
The active ingredient in remofuscin is soraprazan, a small molecule originally developed as a potential treatment for gastro-oesophageal reflux disease (GERD) based on evidence that it inhibited gastric acid secretion. Oral soraprazan was found to be safe and well-tolerated when investigated in clinical trials for GERD, but it failed to demonstrate efficacy. Results from investigations conducted in primates and a mouse model of advanced STGD showed soraprazan had activity for removing lipofuscin from RPE cells and suppressed retinal thinning, Dr Hoyng said.2,3
“STGD1 is the most common retinal dystrophy caused by a single gene,” he explained. “Causative mutations in the ABCA4 gene lead to accumulation of lipofuscin within the photoreceptor cells and eventually within the RPE. Subsequently, the accumulation of lipofuscin results in degeneration of RPE cells and photoreceptors—that results in loss of visual acuity.”
Clinical trial design and results
STARTT, the phase 2 study investigating remofuscin for STGD1, was a multicentre, randomised, double-masked, placebo-controlled study funded by the European Commission. It enrolled 87 adults (age 18 years and older) with at least two ABCA4 mutations and onset of STGD1 prior to age 45 who had best corrected visual acuity (BCVA) between 49 and 83 letters and a qAF value greater than or equal to 300 units.
Patients were randomised 2:1 to treatment with remofuscin 20 mg or placebo once daily. At the end of one year, patients were invited to continue in the trial for another year.
The better eye was evaluated as the study eye, but data were also analysed for the fellow eye. Changes from baseline for all endpoints were evaluated after both one and two years—except when qAF indicated an increased treatment effect after two years of remofuscin treatment compared with the end of the first year.
Secondary endpoints investigating potential remofuscin effects for preserving retinal structure included central subfield retinal thickness, total retinal macular volume, outer nuclear layer thickness (five subfields), and ellipsoid zone loss area— and all showed a tendency towards treatment efficacy, Dr Hoyng said. Results from functional testing assessing change from baseline in BCVA and mesopic microperimetry mean sensitivity also favoured remofuscin versus placebo.
Dr Hoyng spoke during the 2023 EURETINA Congress in Amsterdam.
For citation notes, see page 48.
Carel Hoyng MD, PhD is Professor of Ophthalmology, Radboud University Medical Center, Nigmegen, Netherlands. carel.hoyng@radboudumc.nl
32 EUROTIMES | FEBRUARY 2024
RETINA
MDR Requirements Affect All Ophthalmic Surgeons
Ophthalmology needs to come to grips with medical devices under new EU regulations.
DERMOT MCGRATH REPORTS
All surgeons should familiarise themselves with the Medical Device Regulation (MDR) that entered into force in May 2021 and signal any safety incidents connected with the use of a medical device to the relevant health authorities, according to José-Carlos Pastor MD, PhD.
“MDR is really complex, but the key points are that all medical devices require clinical evaluation and investigation with the same ethical, methodological, and patient protection principles as clinical drug trials,” he said. “The products from clinical research must be provided free of charge by the sponsor, and any clinical trials must be covered by insurance.”
Prof Pastor focused his talk on the surveillance measures in place to flag any issues of concern with any medical device.
“Healthcare professionals or patients who become aware of a serious incidence must report it to the country’s health authorities. Health facilities must appoint a surveillance officer to comply with established procedures,” he explained. “The clinical sites must also have a record, preferably electronically, of the Unique Device Identification (UDI) of implanted devices IIa, IIb, and III.”
He noted the vast majority of implanted devices used in ophthalmology—including contact lenses, IOLs, surgical lasers, scleral and corneal implant instrumentation and sutures—come under class IIa or IIb.
What constitutes a serious incident?
The question frequently arises as to what constitutes a serious incident which warrants reporting, Prof Pastor explained. Although the MDR itself lacks a clear definition of the difference between an “incident” and a “serious incident,” a European Union medical devices working group has since clarified the terminology. A “serious incident” is defined as one with the potential to lead to significant health or public health outcomes and may have resulted in or contributed to the death or temporary or permanent serious deterioration in the health of the patient or user.
There are three main criteria governing basic reporting criteria for a serious incident: an incident has occurred, the incident directly or indirectly led or might lead to any of the outcomes of a serious incident, and a causal relationship between the serious incident and the device has been established, is reasonably possible, or suspected. Any incident which meets all three of the above conditions is considered a serious incident and should be reported, he said.
In Spain, Prof Pastor and his team have been working with ophthalmological societies and opinion leaders to propose a list of possible serious events to help colleagues make decisions concerning MDR reporting.
The Spanish Vitreoretinal Society (SERV) has proposed a list of possible serious incidents, including those arising from the use of irrigation solutions, such as cataract formation, endothelial decompensation, or unusual inflammatory reactions.
“We should also be aware that some surgeons use low concentrations of povidone-iodine in the infusion liquid to treat or prevent infectious endophthalmitis,” he said. “They are anecdotal but could cause inflammatory reactions and endothelial toxicity, and they must be taken into account.”
A wide range of criteria for reporting issues with silicone oil use—including vision loss, unusual inflammation, sustained IOP rise, and retinal structural changes, among others—have been identified and should be considered when an incident occurs, Prof Pastor said.
He also advised caution when using so-called facilitators of silicone oil removal such as F4H5, noting there is currently little scientific basis for their safety.
Caution is also advised with perfluorocarbon liquids (PFCLs) use, which can cause inflammatory reactions and a direct toxic effect, while problems may also occur with internal limiting membrane dyes and perfluorocarbon gases.
Summing up, Prof Pastor urged practitioners to be thorough in the traceability of any medical devices they use.
“If possible, keep a record of the duration of your surgeries and the most important surgical steps,” he concluded. “Also, in case of reasonable doubt, it is preferable to report the incident involving a medical device to the health authorities.”
This presentation was given at the 2023 EURETINA Congress in Amsterdam.
José-Carlos Pastor MD, PhD is a full professor and chairman at the Hospital Clínico Universitario de Valladolid, Spain, and Advisor to the Spanish Agency for Medicine and Medical Devices (AEMPS). pastor@ioba.med.uva.es

33 2024 FEBRUARY | EUROTIMES
Vitreoretinal Surgery for Managing Uveitis
Multidisciplinary approach expands options for uveitis management.
DERMOT MCGRATH REPORTS
Vitreoretinal (VR) surgery has emerged as an important therapeutic and diagnostic tool in uveitic patients, allowing surgeons to adopt a multidisciplinary approach for better management of uveitis, according to Shwu-Jiuan Sheu MD.
“VR surgeries provide more choice in the management of uveitis,” she said. “Microincision vitrectomy (MIVS) makes the procedure easier, harbours fewer complications, and delivers greater patient comfort.”
In diagnostic approaches, pars plana vitrectomy (PPV) can serve as a valuable tool to identify infection and enable the surgeon to explore potential alternative diagnoses in atypical cases, rapidly progressing cases, and eyes with limited or no response to standard treatment and masquerade syndrome, Professor Sheu said.
Therapeutic PPV is indicated in managing uveitis complications, including hypotony, epiretinal membrane formation, retinal detachment, and vitreous haemorrhage.
“Vitrectomy also helps to clear visual opacities and decrease inflammation in cases of persistent inflammation,” she said.
Another advantage is that compared to vitreous tap, PPV can obtain larger sample volumes, avoid vitreous traction, and allow the surgeon to directly proceed to therapeutic vitrectomy after vitreous sampling.
The most common aetiologies for diagnostic PPV are infection and neoplasm, but surgeons also need to be on the lookout for masquerade syndromes, which often simulate chronic idiopathic uveitis and respond poorly to corticosteroid treatment. Intraocular lymphoma is the most common malignant form, and Prof Sheu emphasised the importance of rapidly sending vitreous biopsy samples for laboratory analysis to confirm the diagnosis.
Prof Sheu added it was vital to achieve optimum control of inflammation before PPV is recommended for non-emergent therapeutic indications and complications of uveitis.
“Previous experience suggests aggressive control of perioperative inflammation using topical, regional, and systemic steroids with or without systemic-sparing immunomodulatory therapy for at least three months,” she said. “Recent studies have shown PPV is effective even if complete control of intraocular inflammation is not achieved prior to the surgery—the timing depends on how urgent the operation is.”
PPV can also function as a potent anti-inflammatory tool when used appropriately.
“It may decrease inflammation in eyes with non-infectious uveitis by presumably removing the inflammatory cytokines,”
Prof Sheu explained. “PPV and lensectomy are used for control of inflammation in lens-associated uveitis. PPV was reported to be an alternative to immunomodulatory therapy, where 44% can be stopped after PPV and possibly reduce the recurrence of intermediate, posterior, and panuveitis.”
VR surgeries provide more choice in the management of uveitis.
Postoperative endophthalmitis is the most common indication for PPV in an inflamed eye, said Prof Sheu, noting modern MIVS in exogenous endophthalmitis with much better initial vision than light perception is regarded as safe and with a low rate of complications.
“The timing and indication of MIVS PPV should also be earlier than those suggested by the EVS study,” she added.
Uveitis is also an independent risk factor for retinal detachment (RD). For RD after acute retinal necrosis, there is a high risk of proliferative vitreoretinopathy (PVR) with multiple holes in an atrophic thinned retina and ischemic optic neuropathy presence.
“For these cases, MIVS PPV with silicone oil tamponade is the treatment of choice,” she said.
In epiretinal membrane in uveitis, PPV is indicated if the patient has sight-threatening macular oedema or if progression occurs despite maximal medical treatment.
The overall complication rate of PPV in uveitic eyes is between 42% to 54%, said Prof Sheu, with hypotony, vitreous haemorrhage, retinal detachment, epiretinal membrane, and cataract among some of the more commonly encountered complications.
“There is generally more risk in those associated with systemic risk factors,” she said in closing. “We must carefully weigh the benefits and risks of the surgery for the individual patient.”
Prof Sheu delivered the Kreissig Lecture at the 2023 EURETINA Congress in Amsterdam.
Shwu-Jiuan Sheu MD is currently chief of ophthalmology at Kaohsiung Medical University Hospital in Taiwan and professor at Kaohsiung Medical University. She previously worked as chief of Kaohsiung Veterans General Hospital and Professors of National Yang-Ming University and National Defense Medical University in Taipei. sjiuansheu@gmail.com
RETINA 34 EUROTIMES | FEBRUARY 2024

https://escrs.org/special-interest-groups/yos/
35 2024 FEBRUARY | EUROTIMES YOUNG OPHTHALMOLOGISTS ESCRS
Putting Digital Under the Microscope
Digital scopes offer advantages that may be further enhanced.
HOWARD LARKIN REPORTS
Digital microscopes offer a range of advantages over standard operating microscopes for anterior segment surgery. These include better ergonomics, teaching opportunities, enhanced visualisation, reduced risk of phototoxicity and photophobia, and interconnectivity with other devices and digital networks.
Digital microscopes come in three varieties, each with its advantages and disadvantages, said Kfir Azoulay. Retrofitted conventional scopes replace optical viewing systems with digital cameras, which saves money but eliminates the optical option. Hybrid microscopes combine optical and digital viewing options but are not optimised for either. Full digital microscopes are designed for digital visualisation—allowing more illumination options—but have no optical backup and may be more expensive.
Heads-up 3D surgery
Ergonomics are a major advantage of digital microscopes. Bending over a surgical microscope for hours at a time can promote back, neck, and other musculoskeletal injuries. “Every inch forward results in a 10-pound increase in the relative weight on the spine,” said Matteo Ripa MD. Viewing the surgery on a 3D video screen through polarised glasses or a digital headset allows a “heads-up” posture, reducing that risk.
Digital microscopes are excellent for teaching, added Dr Ripa, who has published a systematic review and meta-analysis comparing 3D heads-up digital and standard microscopes for cataract surgery.1 Trainees, assistants, and observers can watch surgery in real time in the operating theatre or remotely. “Better surgical view means better surgical understanding.”
The devices offer deeper depth of field, reducing the need to change focus frequently; better depth resolution, allowing better visualisation of small details; and better depth perception, Dr Ripa said.
Less light needed
Digital microscopes require less light in the patient’s eye, translating to quicker recovery after surgery, according to two studies Dr Ripa reviewed.2,3
These systems also can use light not visible to the naked eye to enhance contrast, augment areas of interest, and suppress irrelevant areas. Adding OCT adds another visualisation dimension, and digital scopes are set up to support it, Azoulay said.
In addition, digital surgical guides can be overlaid on a digital scope. Intraoperative measurements may also be performed to guide surgery. Integrating digital scopes with
other digital devices can significantly enhance workflow, Azoulay said. “The optical microscope is an island in the OR. The digital microscope interfaces seamlessly with the entire ecosystem.” And with the rise of AI, digital scopes are primed to use predictive technologies that might alert surgeons to impending risks such as posterior capsule ruptures, he added.
But all that matters little if outcomes are compromised by using a digital microscope, which Dr Ripa found in his meta-analysis are not.
Best-corrected visual acuity, incidence rate of intraoperative complications, and surgical duration were not statistically different between digital and standard scopes, Dr Ripa reported. One study found surgery times were longer during the first 25 procedures with a digital scope and shorter during the last 25, suggesting a learning curve. Similarly, complications declined with experience.
Dr Ripa and Azoulay presented at the 2023 ESCRS Congress in Vienna.
For citation notes, see page 48.
Matteo Ripa MD, PhD candidate, is an ophthalmologist at William Harvey Hospital, East Kent Hospitals University NHS Foundation Trust, Ashford, UK; and Universitario A Gemelli IRCCS and Catholic University, both in Rome, Italy. matteof12@gmail.com
Kfir Azoulay is head of corporate strategy at Heidelberg Engineering, Baden-Württemberg, Germany. kfir.azoulay@heidelbergengineering.com
36 EUROTIMES | FEBRUARY 2024 DIGITAL OPHTHALMOLOGY

Boarding the Smart Future
Navigating the surge of AI-based tools targeting increased efficiency and better outcomes.
CHERYL GUTTMAN KRADER REPORTS
While multiple artificial intelligence (AI)-based applications are already relevant for refractive surgeons, users must understand how these programs work and their limitations, advises David Smadja MD.
“We are being flooded by AI today, and there is no doubt that AI can help to improve efficiency, safety, and accuracy in refractive surgery,” Dr Smadja said. “We must be careful, however, not to over-rely on AI. Although the AI wave is here, we need to learn how to surf it.”
He proposed that busy refractive surgeons wanting to improve practice workflow and save time with surgical planning and patient care without compromising outcomes may find AI a valuable assistant in several ways. For example, a recently developed AI-enabled automated eye health platform collects and interprets subjective symptoms from the patient, conducts a comprehensive ophthalmic exam, and generates a report with guidance on choosing the best approach for individual patients.
Many teams have demonstrated good accuracy for AI approaches that predict subjective refraction based on a single aberrometry imaging acquisition. As another time-saving application, AI could be applied to develop questionnaires to triage a need for postoperative follow-up.
“We have all faced the situation where a patient calls a few days after PRK, wondering if blurry vision is normal,” Dr Smadja said. “What if the patient could use a smart tool at home that could answer the question automatically and either reassure the patient or raise a red flag that a visit is needed?”
AI-based programs are also helping refractive surgeons interpret data collected to screen patient appropriateness for refractive surgery. Discussing this application, Dr Smadja referred to the challenges of reviewing complex topography readouts where surgeons need to recognise patterns, detect abnormal values, and determine whether the latter are real or acquisition artefacts.
“We still have difficulty discriminating if a normal cornea is a keratoconus suspect or if what appears to be an early keratoconus is a normal eye,” he noted.
Yet while most corneal imaging tools provide AI-based scoring systems for guiding these decisions, Dr Smadja
cautioned the need for understanding normality is relative because the determination depends on the algorithm’s training database, the features of which can vary across different patient populations.
“Normal ranges need to be adapted to the population seen in your clinical practice,” Dr Smadja said.
Other AI-based algorithms can guide patient selection for different refractive surgery procedures, integrating all clinical and demographic data for an individual or providing guidance for achieving the targeted refractive outcome. In addition, software created using AI can help to identify whether a patient is at risk for postoperative myopia regression, thereby allowing counselling about the possible need for a future enhancement.
We must be careful, however, not to over-rely on AI. Although the AI wave is here, we need to learn how to surf it.
Finally, refractive surgeons wanting to publish their research can find AI as a useful and time-saving aid for manuscript preparation.
“AI can help create a better manuscript—one standardised to the journal’s specifications by performing reference verification and checking for issues such as proper grammar, clarity, and formatting,” Dr Smadja said.
Dr Smadja spoke at the 2023 ESCRS Congress in Vienna.
David Smadja MD is the Director of Refractive Surgery, Hadassah Medical Center, Tel Aviv, Israel, and president of the Israeli Society of Refractive Surgery. smadj.david@gmail.com
37 2024 FEBRUARY | EUROTIMES
Updating the Hippocratic Ideal
Cataract surgery can become more sustainable.
TIMOTHY NORRIS REPORTS
Small changes could make a big difference in making cataract surgery more environmentally friendly, according to Sjoerd Elferink MD.
“It is always good to kick off with a banana,” he said. “You might think a banana grown across the ocean must have a high environmental footprint. However, when you look closely into its details, a banana does not need a hothouse to grow—and it comes with its own packaging. It is not bad at all.”
By considering similar small details, cataract surgery can have a lower impact on the environment, peeling off waste on the path of a greener surgery.
The total carbon emissions of cataract surgery differ between 39 and 150 kilogrammes, which Dr Elferink said can be reduced and balanced with many different expedients. “There are many ways to make cataract surgery more sustainable, and you can already start next Monday.”
A strategy for sustainability is the core part of the #StartNextMonday campaign promoted by the ESCRS Young Ophthalmologists for Sustainability (YOFS).
“Start with energy use,” Dr Elferink said. “Enabling OR ventilation just 30 minutes prior to the operation will be enough to clean the air. Furthermore, to meet the requirement for a class-2 OR, you will need only 20 air changes per hour.”
Optimising surgical materials is also an essential way to reduce carbon footprint.
“You can replace your full body drape with a face drape only, cover the armrest with your gown, use medical sponges only when your hands are visibly dirty, and use only alcohol-based hand scrub. Re-evaluate the content of your cataract custom pack. You can save an enormous amount of waste and money this way,” Dr Elferink said.
“Finally, we as doctors should advocate for dietary changes,” he said. “The latest IPCC report urged for an accelerated food transition. The mitigation potential is enormous because we could cut yearly carbon equivalent emission by 25% by just eating less meat. Physicians do have an important role in this—a 50% reduction in red meat reduces mortality up to 20% and will benefit both patients and the environment.”

38 EUROTIMES | FEBRUARY 2024 SUSTAINABILITY
There are many ways to make cataract surgery more sustainable, and you can already start next Monday.
With this level of involvement, Dr Elferink believes it should lead to an ethical re-evaluation of what it means to be a doctor.
“What we need is a new oath of Hippocrates because we as doctors have a really important role. Something similar recently happened in the Netherlands. Our code of conduct was changed with a new bullet point: ‘You are aware of the relationship between health, climate, and environment, you are committed to a sustainable healthcare sector and healthy living environment’. This is really our way to change the vicious circle of climate change,” he concluded. “It is crucial to realise that if everything is at stake, everything is possible.”
For more information on ESCRS Young Ophthalmol ogists for Sustainability, please visit www.escrs.org/ special-interest-groups/yos/yofs/.
Dr Elferink presented at the 2023 ESCRS Congress in Vienna.
Sjoerd Elferink MD is a cataract surgeon at the Flevoziekenhuis Hospital of Almere, Netherlands. sjoerd.elferink@gmail.com
Since its founding in 2007, the European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO) has grown to encompass three registries that contain data for more than 4 million surgeries.
In 2022, the Registries Steering Group worked to integrate additional data from national registries sharing common data models and centrally from individual sites committed to quality improvement enrolled in the registries.
39 2024 FEBRUARY | EUROTIMES
DOWNLOAD YOUR FREE COPY TODAY: Scan for more information on ESCRS Young Ophthalmologists for Sustainability
SIDICS for a More Sustainable OR
Reducing the environmental burden of cataract surgery worldwide.
Twenty to thirty million lens extraction surgeries are performed worldwide annually, with up to 5 kg of waste and 130 kg of carbon dioxide equivalents per single phacoemulsification. In the global effort to respond to climate change, reducing the environmental impact of cataract surgery has become a more urgent concern.
For Nicolas Winklmair MD, optimisation of cataract packages (cat packs) can be an effective and helpful way to reduce waste and carbon footprints in cataract surgery—an objective easier to achieve thanks to the efforts of the European Society of Cataract and Refractive Surgeons.
“If all departments were to reduce the product volumes and drape sizes to the average lower third already in use in the country, we’d be able to reduce cat pack-associated waste by about 37% and the associated carbon emissions by about 34%,” Dr Winklmair said, referencing a study he and others published in the Journal of Cataract & Refractive Surgery that analysed and compared 55 different custom package sets used in Austria in 2021.1
“Starting from this study, we brought the analysis up to the European level, sending emails to all ESCRS members, asking them for their cat pack product lists and data on the number of surgeries performed annually,” he said. “Thanks to the Young Ophthalmologists for Sustainability group (YOFS), we were able to collect data from 44 different surgical centres from 12 different countries and 9 different suppliers.”
The main goal of this research was to find the lowest common denominator of cat packs used in Europe and remove all reusable and unnecessary instruments from the package. “What we ended up with is now the suggested ESCRS sustainable cat pack,” Dr Winklmair said. “Compared to the standard package currently used at the Hanusch Hospital in Vienna, this cat pack is not only lighter and environmentally more friendly but 19% cheaper.”
With the sustainable cat pack as a benchmark, ESCRS and YOFS created the new Sustainability Index for Cataract
37%
If all departments were to reduce the product volumes and drape sizes to the average lower third already in use in the country, we’d be able to reduce cat pack-associated waste by about 37%
Surgery (SIDICS), a calculator easily accessible on the ESCRS website. Using SIDICS, surgeons can obtain valuable information on the environmental burden of their surgical activity.
“Once filled with all the required information, you will end up with the product list page, giving the summary and an estimate of the annual carbon footprint and water demand of the cat pack you entered, along with some suggestions for the optimisation potential,” Dr Winklmair said. “For example, the standard package generates 74 tonnes of carbon equivalent per year compared to the 50 tonnes of the benchmark pack. After reassessing all these products, you can download your product list to talk to your peers and your supplier about reimbursing.”
This new tool is one of many steps to reduce the environmental burden in ophthalmology. “With further iterations, we will conduct more detailed assessments of the product’s life cycle, further helping to advocate for policy changes and collaborating with suppliers for more sustainable production,” Dr Winklmair concluded.
Dr Winklmair presented at the 2023 ESCRS Congress in Vienna. For citation notes, see page 48.
Nicolas Winklmair MD is a researcher at the Vienna Institute for Research in Ocular Surgery Medizinische Universität Wien and Hanusch Hospital of Wien, Austria. nickwinklmair@gmail.com

You can find out at sidics.escrs.org/
SUSTAINABILITY
TIMOTHY NORRIS REPORTS
40 EUROTIMES | FEBRUARY 2024
How does your cat pack stack up?
ESCRS IN A SNAPSHOT

We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With more than 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.
41 2024 FEBRUARY | EUROTIMES
ESCRS WELCOMES NEW PRESIDENT
EuroTimes spoke with Filomena Ribeiro MD, PhD, FEBO, incoming president of the ESCRS, about her goals and aspirations during the next two years. She is head of the department of ophthalmology at Hospital da Luz, Lisbon, Portugal.
You are not the first Portuguese president or the first female president, but you are the first Portuguese female president, so congratulations on that distinction!
Thank you. I am honoured to follow Professor José Cunha-Vaz, who was ESCRS president in 2000. It is also wonderful to follow Marie-José Tassignon (2004) and Béatrice Cochener-Lamard (2018) in this position.
When did you first realise you wanted to be an ophthalmologist?
As long as I can remember, I wanted to be a doctor. When I began my medical training in Lisbon, I felt that what I really liked was surgery. So, my first thought was about general surgery. But then, once I had the experience of doing eye surgery, I knew I should be an ophthalmologist. It was such a beautiful experience performing eye surgery.
How did you become involved with the ESCRS?
I became active in the ESCRS in 2016 when I served as the Portuguese coordinator for the ESCRS Congress in Lisbon. Professor Cochener-Lamard provided a lot of mentoring as I became more involved with the ESCRS and became very interested in promoting all the goals of the Society.
When Rudy Nuijts became president in 2020, the COVID pandemic broke out, presenting many challenges to the ESCRS and the field of ophthalmology. Then, when Oliver Findl became
president in 2022, he also had the pandemic to deal with, along with Ukraine and climate change. You have all those things to deal with, plus artificial intelligence, robotics, economic issues, and more. Are you ready for this?
Yes, it’s true. We are facing big challenges today, and these things directly affect the field of ophthalmology and our organisation. We have become a world Society, among the biggest in the world, and as such, we have to face the challenges facing the world in general. The ESCRS strategic plan provided us with a very good instrument that helped us prepare to face all these big issues. For example, we were in the process of developing digital ways of communication to provide educational opportunities to all Society members, which proved useful when the pandemic struck.
Are there any ESCRS projects you are personally interested in?
Education is my number one concern. We will continue to expand our learning opportunities for our members at our conferences and online. Our programmes span across continents, providing a platform for pioneering research, advanced surgical techniques, and continuous professional development.
Among the many challenges I would like to help with is the need to provide eye care in low- and middle-income nations. The ESCRS is collaborating with several groups to provide local teaching resources in underserved countries in different parts of Africa. The shift towards building local capacity is a cornerstone of ESCRS’s charitable strategy. For example, we are collaborating with Eyes of the World in Mozambique in a programme guaranteeing the right to eye

42 EUROTIMES | FEBRUARY 2024 NEWSMAKER
An interview with incoming president Filomena Ribeiro.
health through equitable access to public health with a human rights and gender approach. I’m Portuguese, so I have an affinity with that country. We want to make sure women have equal access to sight-saving eye care. I will be there next year to see the progress of this project.
What can we look forward to in 2024?
I want to encourage our members to attend our conferences, the Winter Meeting in Frankfurt in February, and our Annual Congress in Barcelona in September. The Vienna Congress was a tremendous success both from an educational and a social point of view. It is such a pleasure to be able to meet and mingle in person again. We will continue to try some new concepts in presentation at these conferences as we did in Vienna. For example, in Frankfurt, we will focus on immersive learning experiences for residents and promoting fresh education and networking opportunities. We will have a new interactive ‘unconference’ format for sessions to allow members to share ideas during the presentations. We will also continue the emphasis on innovative and interesting formats in Barcelona.
In 2024, we are strengthening our commitment to sustainability by placing a strong emphasis on social responsibility and promoting inclusivity through various initiatives. We are collaborating with our partners to work towards zero waste to landfill, zero net carbon emissions, and becoming a role model for social responsibility. We are implementing measures to support the wellness of our attendees, contribute to local and global causes, restore ecosystems, and foster sustainability leadership in our industry.
Our vision for sustainability is ambitious but achievable, as we are not alone in this journey. We are collaborating with other organisations, institutions, and experts to learn from best practices and share our experiences. We are also engaging with our members, partners, and stakeholders to solicit their feedback and suggestions on how we can improve our sustainability performance.
I hope our readers will be able to attend these events and will also explore many of the expanding educational opportunities we are creating online.

43 2024 FEBRUARY | EUROTIMES
JOIN the leading community and trusted source for SCIENCE, EDUCATION, AND PROFESSIONAL DEVELOPMENT in the fields of cataract and refractive surgery. Learn more about membership at escrs.org Sign up as an ESCRS member now for €150 per year and save €100 on your 2023 Annual Congress registration fee!

BELKIN DIRECT SLT SIMPLIFIES OPEN-ANGLE GLAUCOMA LASER TREATMENT
Increased efficiency and patient comfort may help cut long waits.
Like many eye practices, Erik L Mertens MD’s Antwerp, Belgium, clinic is seeing more glaucoma patients. One of its five ophthalmologists is a glaucoma specialist with extensive research experience in selective laser trabeculoplasty (SLT) lasers, which it often uses as initial therapy.
SLT is recommended by many practice guidelines as a primary treatment
for open-angle glaucoma. Typically reducing intraocular pressure by 25% to 30%, it can delay, reduce, or even eliminate the need for eye drops in many patients. It also can be repeated.
Historically, Dr Mertens’s clinic has delivered SLT the traditional way—one laser shot at a time reflected into the trabecular meshwork through a gonio lens held by hand against the patient’s
cornea. The treatment takes about 10 to 15 minutes to set up and complete. Then, the patient goes home and comes back another day to treat the second eye.
That changed in April 2023 with the arrival of the Belkin Vision direct SLT (DSLT) system. Using a sophisticated eye tracker to keep it on target, DSLT laser light passes through the sclera without harming it directly into
44 EUROTIMES | FEBRUARY 2024
INDUSTRY INSIGHT
HOWARD LARKIN REPORTS
the trabecular meshwork. There, it is absorbed by pigment, causing a tissue response similar to SLT.
Automated DSLT not only eliminates the SLT gonio lens—and the skill needed to manipulate it—it delivers 120 shots over 360 degrees in a fraction of the time required for SLT. “The procedure itself is about six times more efficient,” Dr Mertens said. His clinic can treat about 10 patients bilaterally, or 20 eyes, per hour with DSLT compared with three to four patients in one eye each per hour with SLT.
In Dr Mertens’s practice, the results of the two procedures are similar so far. Indeed, at 12 months in the GLAUrious trial, both SLT and DSLT reduced mean IOP by a little more than 3.0 mmHg and cut topical glaucoma medication use by about 50%.1 Serious adverse events are rare, with a failure to lower IOP in one out of 15 or so patients
We can immediately treat the other eye … And they can even drive themselves home.
the most significant Dr Mertens has observed, though about half of those patients respond to a second treatment.
DSLT is more comfortable for patients, who don’t have to take pilocarpine beforehand or even sit down for the treatment, Dr Mertens said. “The patients only experience a mild sensation and some blurred vision for a minute to a minute and a half from the bright light, and we can immediately treat the other eye. … And they can even drive themselves home.”
And patients love it. “We are treating about 40% more with the laser than previously. The advantages of DSLT are very attractive to patients,” some of whom come from far away, Dr Mertens said.
Since the practice already did SLT, implementing DSLT was easy, Dr Mertens added. It is now the only type of SLT his clinic offers. “After one week of having DSLT, we sold the previous technology laser.”
Cutting backlogs
In addition to quicker procedure speed and patient comfort, the simplicity of operating the automated DSLT device could increase its availability, said Professor Gus Gazzard, who was chief investigator of the landmark LiGHT Trial (Laser in Glaucoma and ocular Hypertension trial).2
“It’s not so much the speed in the session—it is the ability to quickly train individuals who can safely and reliably deliver the treatment without six months of gonioscopy practise,” said Prof Gazzard, who is currently conducting a study of DSLT outcomes and possible practice efficiencies at Moorfields in London. Though he does not yet have results, Prof Gazzard estimates adopting DSLT will at least double clinic throughput and capacity.
This could help cut waiting lists that reach six months or more at some UK hospitals, though the backlog is much less at Moorfields, which employs op-
tometrists with advanced training and backed by ophthalmologists to do much of the SLT.
“‘Are you done?’ are the three words I hear most often” after DSLT, said Dr Neil Nathwani, a research optometrist who has performed more than 1,300 SLT procedures at Moorfields. Prof Gazzard is also interested in seeing how the device holds up in developing countries where the need is even greater.
Improving efficiency for all parties is an overall DSLT design objective for Belkin, said Andrew Webb, the firm’s chief commercial officer. CE marked and recently cleared by the US FDA, the DSLT device is being rolled out in select practices in the UK, Spain, Germany, Belgium, Poland, and soon, France.
“We are fine tuning some of the approaches,” such as enabling patient data to be loaded into the device before treatment sessions to reduce downtime between patients, Mr Webb said. The firm is also developing flexible financing arrangements to accommodate differences in payment from place to place. The goal is to make it work for everyone—providers, health systems, the company itself, and most of all, patients, he added.
For citation notes, see page 48.
This piece includes contributions from Belkin. Erik L Mertens MD, FEBO is director, founder, and ophthalmic surgeon at Medipolis, Antwerp, Belgium. E.Mertens@medipolis.be
Gus Gazzard MBBChir, MA, MD, FRCOphth is director of surgery at Moorfields Eye Hospital and professor at UCL London, UK. gusgazzard@gmail.com
Neil Nathwani is a research optometrist at Moorfields Eye Hospital, UK.
Andrew Webb is chief commercial officer for Belkin Vision, Yavne, Israel. andrew@belkin-vision.com
45 2024 FEBRUARY | EUROTIMES
Phase 2 trial commences with new cannabinoid eye drops
Skye Bioscience has enrolled the first patient in a Phase 2 double-masked, randomised, placebo-controlled study of SBI-100 ophthalmic emulsion for treating primary open-angle glaucoma (POAG) or ocular hypertension (OHT). The formulation consists of SBI-100, a novel prodrug of tetrahydrocannabinol (THC) and a proprietary nanoemulsion formulation, and is designed to enable its penetration into different eye compartments through topical administration. The company reported that in Phase 1 studies, the emulsion was safe and reduced IOP by a mean 23.9% in healthy volunteers. The Phase 2 trial will involve approximately 54 patients with elevated intraocular pressure diagnosed with POAG or OHT.
www.skyebioscience.com
EMA recommends approval for high-dose aflibercept
The European Medicines Agency (EMA) has recommended approval of 8 mg aflibercept (Eylea® HD, Bayer) in the treatment of neovascular AMD and diabetic retinopathy. Earlier this year, the US FDA issued approval for 8 mg aflibercept following the 48-week results of the PULSAR and PHOTON clinical trials for neovascular AMD and diabetic retinopathy, respectively. The trials showed non-inferior and clinically equivalent vision gains with Eylea HD at 48 weeks with both 12- and 16-week dosing regimens, compared to an 8-week dosing regimen with 2 mg aflibercept (EyleaY®, Bayer).
www.bayer.com
Amazon under fire from FDA for distribution of unapproved eye drops
The US Food and Drug Administration (FDA) issued a warning to Amazon regarding the sale of several unapproved eye drops due to the possible risk of eye infections that could result in vision loss or blindness. In a letter addressed to Amazon President and CEO Andrew Jassy, the FDA named seven ophthalmic products that, contrary to federal regulations, the company is responsible for introducing or delivering for introduction into interstate commerce. The letter states that failure to adequately address the matter could result in legal action. Furthermore, the FDA requested a response in writing from Amazon regarding the specific steps they are taking to correct the cited violations, as well as steps they will take to prevent any future violations. Amazon has since removed all the cited products, which are no longer available for purchase.
FDA issues complete response letter for dry eye drug
Aldeyra Therapeutics has received a complete response letter from the US FDA stating that its New Drug Application for dry eye treatment reproxalap did not show efficacy in treating the condition. The response letter stated an additional study was necessary to demonstrate the treatment’s efficacy. Aldeyra says they have submitted a Special Protocol Assessment for a further dry eye disease crossover clinical trial. Results from this trial, if conducted, would be expected within the first half of 2024, with the potential for an NDA resubmission in the first half of 2024 as well, pending FDA feedback and positive results from the proposed trial.
www.aldeyra.com
46 EUROTIMES | FEBRUARY 2024 INDUSTRY NEWS


GETTING COMFORTABLE WITH ANAESTHESIA
In a special editorial, Professor Robert Osher MD provided a series of recommendations to young cataract surgeons for achieving optimal anaesthesia during phacoemulsification, gleaned from his more than 40 years of practice. He emphasised the importance of tailoring the anaesthesia to each patient’s medical and emotional needs, noting the best anaesthesia is not general or local but vocal. He advised that during the initial encounter, the surgeon should note the patient’s general demeanour and sensitivity to light while undergoing biomicroscopy and indirect ophthalmoscopy. Also to be evaluated are pre-existing factors that may influence the choice of anaesthesia, such as a history of thrombocytopenia or anticoagulation therapy, which may raise haemorrhage risk. If a block is indicated, it is better to explain to the patient any risk factors, such as long axial length or previous ischemic optic neuropathy, before rather than after surgery.
Communication with the anaesthesia team is also important— surgeons should let them know about the type and degree of anaesthesia preferred. For example, he noted if the patient is going to receive a regional block, he prefers the volume for a retrobulbar block be limited to 3.5 mL, while a peribulbar block can contain 6.0 mL. However, in cases where the orbit is cavernous and the globe deeply set, a greater volume of anaesthetic to bring the eye forward may outweigh any risk of creating positive pressure. Conversely, if the orbit is tiny and the lids are tight, less volume may be desirable. In cases where subconjunctival anaesthetic balloons the conjunctiva, draining or sweeping it around the limbus to the nasal quadrants will maintain a flat temporal approach.
Surgeons should always be conscientious about maintaining patients’ comfort throughout the procedure. If they complain of pain, supplement anaesthesia with either topical drops—applied to the sclera rather than the cornea to reduce the risk of drug-induced keratitis—or intracameral anaesthesia. If a patient exhibits photophobia, it is best to turn the microscope light down and inject an intracameral agent. Prof Osher emphasised not resuming the procedure until the patient is comfortable. If a retrobulbar haemorrhage occurs, it is important to differentiate an arterial bleed from a venous bleed by retropulsing the globe, assessing proptosis, and evaluating lid mobility. In addition, intraocular pressure should be measured and documented, as well as retinal arterial perfusion, if an arterial bleed is suspected. If a venous bleed is not self-limiting, cancelling the surgery may be the best option. With any retrobulbar haemorrhage, the surgeon must explain what is happening to the patient. At the same time, the surgeon should forbid the team from making comments during surgery that may frighten the patient.
“Your choice of anaesthesia should always be supplemented with calm conversation and reassurance. The words you choose are the best drug in the anaesthesia formulary,” Prof Osher concluded. RH Osher, et al. “Feeling relaxed about anaesthesia?” 49(12): 1193–1194.

Research Education Innovation
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.
47 2024 FEBRUARY | EUROTIMES JCRS HIGHLIGHTS
Cited in this Issue
Happy Birthday to IOL Surgery!
Page 4
1. Trivedi, Rupal H; Apple, David J; Pandey, Suresh K; Werner, L; Izak, Andrea M; Vasavada, Abhay R; Ram, J, Indian Journal of Ophthalmology, 51(3): 211–216.
Webinar Examines Impact of Investors on Ophthalmology
Page 6
1. “Cataract surgeries down 4% in 2021.” Eurostat, 12 September 2023.
Gazing into a Lenticule-Based Future
Page 12
1. Reinstein DZ, Sekundo W, Archer TJ, et al. “SMILE for Hyperopia with and without Astigmatism: Results of a Prospective Multicenter 12-Month Study.” J Refract Surg. 2022; 38(12): 760–769.
Lenticule Extraction Gaining Fans?
Page16
1. Reinstein DZ, Sekundo W, Archer TJ, et al. “SMILE for Hyperopia with and without Astigmatism: Results of a Prospective Multicenter 12-Month Study,” J Refract Surg. 2022; 38(12): 760–769.
It’s in the Bag
Page 20
1. G Wieger. “Über den Canalis Petiti und ein ‘Ligamentum hyaloideocapsulare,′″ Thesis, Strasburg, 1883.
2. E Berger. “Beiträge zur Anatomie des Auges in Normalem und Pathologischem Zustande,″ Wiesbaden: Bergmann. 1887.
3. M Tassignon. “Real-Time Intraoperative Optical Coherence Tomography Imaging Confirms Older Concepts About the Berger Space,” Ophthalmic Res. 2016; 56(4): 222–226.
Refractive Surgery for Myopia
Page 21
1. Zaldivar R, Zaldivar R, Gordillo CH, Adamek P. “Visual Acuity Improvement in Low, Moderate and High Myopia After Posterior-Chamber Phakic Implantable Collamer Lens Surgery in a Large Patient Cohort,” Clin Ophthalmol. 2023; 17: 1179–1185.
2. Zaldivar R, Zaldivar R, Adamek P, Quintero G, Cerviño A. “Descriptive Analysis of Footplate Position After Myopic Implantable Collamer Lens Implantation Using a Very High-Frequency Ultrasound Robotic Scanner,” Clin Ophthalmol. 2022; 16: 3993–4001.
Six Essentials to Iris Repair
Page 26
1. A Fang, et al., BMC Ophthalmology, 2018; 18(120).
Best Practices in Cataract Surgery
Page 28
1. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. “Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation,” J Cataract Refract Surg. 2018; 44(9): 1090–1096.
Treatment at a Crossroads Page 29
1. Diener R, Treder M, Lauermann JL, Eter N, Alnawaiseh M. “Optimizing intraocular lens power calculation using adjusted conventional keratometry for cataract surgery combined with Descemet membrane endothelial keratoplasty,″ Graefes Arch Clin Exp Ophthalmol. 2022; 260(9): 3087–3093.
2. Arnalich-Montiel F, de-Arriba-Palomero P, Muriel A, Mingo-Botín D. “A risk prediction model for endothelial keratoplasty after uncomplicated cataract surgery in Fuchs endothelial corneal dystrophy,” Am J Ophthalmol. 2021; 231: 70–78.
Oral Treatment for Stargardt Disease
Page 32
1. Dhooge PPA, Möller PT, Meland N, et al.; Soraprazan Consortium. “Repeatability of Quantitative Autofluorescence Imaging in a Multicenter Study Involving Patients with Recessive Stargardt Disease 1,” Transl Vis Sci Technol. 2023; 12(2): 1.
2. Julien S, Schraermeyer U. “Lipofuscin can be eliminated from the retinal pigment epithelium of monkeys,” Neurobiol Aging. 2012; 33(10): 2390–2397.
3. Fang Y, Taubitz T, Tschulakow AV, et al. “Removal of RPE lipofuscin results in rescue from retinal degeneration in a mouse model of advanced Stargardt disease: Role of reactive oxygen species,” Free Radic Biol Med. 2022 Mar; 182: 132–149.
Putting Digital Under the Microscope
Page 36
1. Diagnostics (Basel). 2022 Sep; 12(9): 2100.
2. Rosenberg ED, Nuzbrokh Y, Sippel KC. “Efficacy of 3D Digital Visualization in Minimizing Coaxial Illumination and Phototoxic Potential in Cataract Surgery: Pilot Study,” J Cataract Refract Surg. 2021; 47: 291–296.
3. Nariai Y, Horiguchi M, Mizuguchi T, Sakurai R, Tanikawa A. “Comparison of Microscopic Illumination between a Three-Dimensional Heads-up System and Eyepiece in Cataract Surgery,” Eur J Ophthalmol. 2021; 31: 1817–1821.
SIDICS for a More Sustainable OR
Page 40
1. Winklmair N, et al., JCRS. 49(6): 628–634, June 2023.
Industry Insight: Belkin Direct SLT Simplifies Open-Angle Glaucoma Laser Treatment Page 44
1. IOVS. June 2023, 64(7): 5393.
2. Lancet. April 2019, 393(10180): 1505–1516.
48 EUROTIMES | FEBRUARY 2024 CITATION INDEX
Upcoming Events
February 15–18
2024 ESCRS Winter Meeting in conjunction with the 38th Congress of the DGII Frankfurt, Germany
April 5–8
2024 ASCRS Annual Meeting Boston, United States
May 5–9
2024 ARVO Annual Meeting Seattle, United States
May 24–26
2024 EuCornea Annual Congress Paris, France
June 1–4
2024 European Glaucoma Society Congress
Dublin, Ireland
September 6–10
2024 ESCRS Congress
Barcelona, Spain

Feb 15
May

Sep

49 2024 FEBRUARY | EUROTIMES
24
6
INTERVENE EARLIER WITH ISTENT INJECT® W
DELAYING GLAUCOMA DISEASE PROGRESSION1-8
40 %
IOP REDUCTION AFTER 5 YEARS FOLLOW-UP 2
81
DECIBEL MEAN CHANGE IN VISUAL FIELD MEAN DEVIATION FROM BASELINE AT 24 MONTHS IN ISTENT INJECT-TREATED EYES IN A PIVOTAL TRIAL 8
0 ,01 8

YEAR STUDY WITH 2 ISTENTS DEMONSTRATED SUSTAINED PROTECTION AGAINST VISUAL FIELD LOSS, AS WELL AS PRESERVATION OF BEST CORRECTED VISUAL ACUITY, CUP TO DISC RATIO AND RETINAL NERVE FIBER LAYER THICKNESS 5

STUDIES
16 WITH 4-8 YEARS FOLLOW-UP
2,6 %
POWERFUL PREDICTABLE PROVEN
OF 778 PATIENTS IN A META-ANALYSIS OF STANDALONE ISTENT INJECT EYES REQUIRED SECONDARY
INCISIONAL SURGERY DURING FOLLOW-UP6

4 %
1%
OF 186 EYES IN A RANDOMISED CONTROLLED TRIAL WENT ON TO REQUIRE SECONDARY INCISIONAL SURGERY DURING 3 YEARS FOLLOW-UP 7
+40
PUBLICATIONS
DEMONSTRATE ISTENT TECHNOLOGIES PROTECT AGAINST VISUAL FIELD LOSS†
OF 125 PATIENTS IN REAL WORLD STUDY OF STANDALONE AND COMBINED
ISTENT INJECT CASES REQUIRED A SECONDARY PROCEDURE DURING 5 YEARS OF FOLLOW-UP 2
2-7
† Data on file. 1. Berdahl, J., Voskanyan, L., Myers, J. S., Katz, L. J., & Samuelson, T. W. (2020). iStent inject trabecular micro-bypass stents with topical prostaglandin as standalone treatment for open-angle glaucoma: 4-year outcomes. Clinical & Experimental Ophthalmology, 48(6), 767-774. 2. Hengerer, Fritz H., Gerd U. Auffarth, and Ina Conrad-Hengerer. “iStent inject Trabecular Micro-Bypass with or Without Cataract Surgery Yields Sustained 5-Year Glaucoma Control.” Advances in Therapy (2022): 1-15. 3. Ferguson, Tanner J., et al. “iStent trabecular micro-bypass stent implantation with phacoemulsification in patients with open-angle glaucoma: 6-year outcomes.” Clinical Ophthalmology (Auckland, NZ) 14 (2020): 1859. 4. Ziaei, Hadi, and Leon Au. “Manchester iStent study: long-term 7-year outcomes.” Eye 35.8 (2021): 2277- 2282. 5. Salimi, Ali, Harrison Watt, and Paul Harasymowycz. “Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results.” Eye and Vision 8.1 (2021): 1-12. *Consistent cohort. 6. Healey, Paul R., et al. "Standalone iStent trabecular micro-bypass glaucoma surgery: A systematic review and meta-analysis." Journal of Glaucoma 30.7 (2021): 606-620. 7. Samuelson TW, on behalf of the iStent inject Pivotal Trial Study Team. Three-Year Effectiveness and Safety of 2nd-Generation Trabecular Micro-Bypass (iStent inject). Paper at the Annual Meeting of the American Academy of Ophthalmology (AAO). Virtual Meeting: November 13-15 2020. 8. Samuelson, Thomas W., et al. "Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results." Ophthalmology 126.6 (2019): 811-821. iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject ® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject ® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject ® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject ® W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject ® W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.”
• There are no known compatibility issues with the iStent inject ® W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of
intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. © 2023 Glaukos Corporation. Glaukos, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation PM-EU-0237
RATE
SSIs
C O NTROLLINGIOP1-5 PROTECTINGAGAINST V F L SSO 48
LOW
OF
OF PATIENTS
FOLLOW-UP
%
BELOW 15MMHG AFTER 5 YEARS
2