
SEPTEMBER 2023 | VOLUME 28 | ISSUE 7 EuroTimes takes a look at the tremendous potential of AI in ophthalmology, as well as the potential pitfalls. VIEW OF ALSO IN THIS ISSUE
Prize Essays
ophthalmologists
AI’s potential to improve eye care and possible concerns
IOL Power
for Short Eyes
support software may more accurately predict refractive outcomes.
OSD, eye infections,
retinal disease. OPEN-EYED AN AI
Henahan
Young
discuss
AI-Enabled
Calculations
Decision
Climate Change Hard on Eyes Expect increased rates of
and


ADVERTISEMENT
https://congress.escrs.org/


2 Contents 18 Cover An Open-Eyed View of AI Reaping the benefits will require good data and careful design and oversight. 04 Editorial: AI—Proceed with Caution Oliver Findl MD, ESCRS President 06 Inside ESCRS: Debate to Show Less Can Be More 08 ESCRS at a Glance: ESCRS Membership by Country 09 ESCRS Abroad: ESCRS Supports Cataract Project in Nepal 10 Henahan Prize Finalists SUSTAINABILITY 14 Climate Change and Eye Health 16 Links in Eye Care Delivery and Climate Change DIGITAL OPHTHALMOLOGY 21 Emerging Ophthalmic AI Applications 22 AI-Enabled IOL Power Calculations for Short Eyes Douglas D Koch MD CATARACT & REFRACTIVE 24 Pharmacotherapy for Dim Light Vision Disturbances Mitchell Brigell PhD and Jay Pepose MD, PhD 26 Small-Aperture IOL for Complex Corneas Robert Edward T Ang MD 28 Assessing Transepithelial Surface Ablation Benefits Jesper Hjortdal MD, PhD 29 Getting the Maximum from Mini-Monovision Fernando Llovet MD, PhD and Zeki Yiğit Karaca MD 30 Striving for Perfection in LASIK Mark Lobanoff MD 32 Improving Refractive Outcomes After Cataract Surgery Eduardo Martínez-Enríquez PhD 34 EVO ICL for Low Myopia Erik L Mertens MD 36 Femto-LASIK Sets High Bar for Myopic Correction Miguel A Teus MD, PhD September 2023 | Vol 28 Issue 7 EUROTIMES | SEPTEMBER 2023
Functional Vision with Monofocal-plus IOL Filomena Ribeiro MD, PhD, FEBO CORNEA
António
Vision
Winners
Dohlman
Gerrit
Melles
and Reza Dana
MSc, MPH 42 Healing Persistent Corneal Epithelial Defects Dipak Panigrahi MD GLAUCOMA 44 Intraocular Travoprost Implant L Jay Katz MD and Gabriella Szekely PhD RETINA 46 Managing Refractory Scleritis Ian Yeung MD
38
40
Champalimaud
Award
Leonor Beleza; Claes
MD, PhD;
RJ
MD, PhD;
MD,
Publishers
Carey Earle
Mariska van der Veen
Mark Wheeler
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Nicola Lodge
Contributing Editors

Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Soosan Jacob
Timothy Norris
George Liu
Colour and Print

W&G Baird Printers
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.

Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.

ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983


3 Learn more about EuroTimes or connect with ESCRS at ESCRS.org 21 14 46 44 28 ALSO IN THIS ISSUE 48 Leadership and Business Innovation ESCRS Launches Leadership and Business Innovation Weekends 50 Industry News 51 JCRS Highlights 52 Industry Insight Glaukos Rising 54 Citation Index 57 Upcoming Events ALSO IN THIS ISSUE Included with this Issue ESCRS Clinical Trends Survey 2022 Results Medicontur: Premium IOL Solutions ESCRS Clinical Trends Survey 2022 Results
2023 SEPTEMBER | EUROTIMES
AI—Proceed with Caution
It seems the only thing spreading faster than artificial intelligence application development is the hype surrounding it. Ophthalmology is at the forefront of using its potential in the clinical setting. Early indications show it can facilitate better screening of retinal disease, smooth workflows, and free up time for ophthalmologists to do what they do best— patient care.
In our cover story, Howard Larkin takes an open-eyed view of AI. There are many types of AI, but those used in healthcare are predominantly deep learning variants of machine learning. The article looks at one of the main issues facing AI in ophthalmology—the limitations of how the data train these applications. The quality of any computer output depends on the quality of the data going in, raising questions of erroneous output and inherent bias. Success with AI will require careful work at these early stages to validate its use in the clinic.
A related article reviews several AI tools now in use or soon to enter the clinic, including Dora (Ufonia), an automated system for making follow-up calls to patients after cataract surgery shown to reduce routine clinician activity by up to two-thirds. Also in the pipeline, an AI-enabled IOL power calculator that may more accurately predict refractive outcomes in short eyes.
This issue also includes three of the top essays from young ophthalmologists in the 2023 Henahan Prize writing contest, the theme of which was “What is the potential role of AI in ophthalmology, and what are the negative implications and caveats?”. Each of these essays raises fascinating possibilities and caveats for the future of ophthalmology. The essayists look at the technology’s vast potential as well as the barriers, risks, and potential social effects. The winner will be announced at this year’s annual Congress in Vienna.
It is impossible to contain the AI debate in this small space. The upcoming ESCRS Congress in Vienna provides many opportunities to get a better understanding of AI in the clinic. Starting with iNovation Day, there will be a session on the digital OR that will include a discussion of digital visualisation, integrated diagnostic information, and artificial intelligence decision making support. Later in the meeting, a special session on AI in ophthalmology will feature an in-depth discussion by researchers around the world. On the “Smart and @active Monday,” there is an entire digital track with three main sessions highlighted by symposia on the continents going digital: the digital operating room, automated robotic eye surgery, and the newest from artificial intelligence.
Additionally, ESCRS is funding research in this field with the “Digital Research Award,” the fourth “pillar” of grants for supporting research next to the established Clinical Research, Pioneer Research, and Systematic Review Awards.
There are real concerns about the potential hazards of unchecked AI development in the human sphere. The creators of AI have recently issued a “Statement of AI Risk,” voicing many concerns up to and including the extinction of the human race. Signatories including Sam Altman, the CEO of OpenAI (the company that developed ChatGPT), Google DeepMind CEO Demis Hassabis, and Apple co-founder Steve Wozniak are advocating more attention be spent on potential societal risk and the creation of a framework to follow AI development.
It may be too late to put a red light on AI development, and it may be inadvisable to green light every potential use. Rather, we should proceed with caution, ensuring whatever we use is in the best interests of our patients.
EDITORIAL BOARD
Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)
Oliver Findl (Austria)
Nino Hirnschall (Austria)


Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)


Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell Medical Editor
Paul Rosen Medical Editor
EDITORIAL
4
EUROTIMES | SEPTEMBER 2023
Oliver Findl MD, MBA is Chief of the Department of Ophthalmology at Vienna Hanusch Hospital and President of the ESCRS.

belkin-vision.com Introducing Eagle™ by BELKIN Vision Intuitive Glaucoma Care Designed for ALL Ophthalmologists Accessible First-Line Glaucoma Care for All Welcome to the Future of Glaucoma Laser therapy
Debate to Show That Less Can Be More
Younger ophthalmologists to face off against seniors in discussion about sustainability.
BY STUART HALES, EXECUTIVE EDITOR
Boxing matches typically favour those with more—more strength, more stamina, more tenacity, more skill. At the upcoming ESCRS Annual Congress in Vienna, a boxing ring will serve as the backdrop for a debate about sustainability—and the winners will be those who can present the best argument for using less.
The “ESCRS Arena” at the Congress will be the setting for pro-con discussions on a variety of topics, including combined glaucoma surgery (MIGS versus trabeculectomy), myopia treatment (LASIK versus ICL), and cataract surgery timing (delayed sequential versus immediate sequential). The debate about sustainable practices in cataract and refractive surgery will pit younger ophthalmologists such as Sjoerd Elferink and Sarah Schimansky against more experienced practitioners such as Burkhard Dick and Ike Ahmed.
“Oliver (Findl) asked me to organise it, and it made me think—the seniors are the role models,” Dr Elferink says. “They are the ones presenting at congresses; they are the ones presenting to the audience. But what if we flip it around, so now the young ophthalmologists are challenging the seniors about this topic?”
The debate will be moderated— perhaps “refereed” would be a more appropriate term—by Ben LaHood, who practices in Australia and hosts podcasts such as The Second Look and Ophthalmology Against the Rule.
“Ben is a funny guy, and he was very enthusiastic to join and is committed to sustainability,” Dr Elferink says. “If you look at the poster, he’s the one at the bottom. Ben and I wanted to make a classical wrestling poster. He purchased special referee attire for this photo shoot.”
“Is anyone actually doing anything to improve sustainability in ophthalmology, or is it all just talk?! Join us ringside in the ESCRS Arena on Sunday to witness some of the most renowned international surgeons being asked the tough questions from the next generation of ophthalmologists and find out whether they are saving the planet... or saving themselves.”

6 INSIDE ESCRS
EUROTIMES | SEPTEMBER 2023
Keen to see progress
Dr Elferink readily acknowledges sustainability cuts across all generations and that many experienced ophthalmologists are as keen to see progress in this area as their younger colleagues. “I invited some very well-known seniors, and they all said yes,” he notes. “There were even some that had other sessions taking place and they said, ‘I’ll have one of my residents do that one, and I’ll join the sustainability debate.’”
The arena debate is not the only Congress programme addressing sustainability issues. On the same day (Sunday), a two-hour symposium titled “Making Eye Surgery Greener” will discuss topics such as reducing operating room waste, lessons from low- and middle-income countries, and the risks of reusing certain surgical devices. The next day, a one-hour session titled “The Cost and Savings in Sustainable Ophthalmology” will feature presentations by four leaders in this area.
The entire Congress, for that matter, will be a laboratory for sustainable practices. In keeping with its “Mission Zero” vision to host events that produce no landfill waste and zero net carbon emissions, ESCRS will recycle waste at the convention centre and donate leftover food to a local food security charity. ESCRS is also estimating CO2 emissions for the Congress and purchasing offset credits from the following projects:
• Aqua Clara water filters (Kenya)
• Solar water heating (Asia)
• Orb rooftop solar panels (India)
• Clean water and cooking (Guatemala)
“In 2023, we are working together with interested parties to support our event participants’ wellness, the local and global communities we visit and support, to protect and replenish affected
ecosystems, and to inspire more regenerative actions all round,” says Dr Findl, president of ESCRS. “We invite everyone to join us in this journey because we can achieve an exponentially more positive impact together.”
On the leading edge
Although the push for sustainable practices within ESCRS is coming from several directions, younger ophthalmologists are at the forefront. The ESCRS Young Ophthalmologists for Sustainability (YOFS) are leaders in the move to develop a sustainable cataract pack, now shepherded by ESCRS through the SIDICS (Sustainability Index for Disposables in Cataract Surgery) Project.
“We saw there were such major differences in cat packs in such small countries as the Netherlands or Austria, so we did a European inventory, and it appeared there were also major differences in other countries,” he says. “The aim was to develop an ESCRS-endorsed cat pack that has the least materials you need to perform a safe and good operation.”
Dr Elferink notes the cat pack project is just one example of how ophthalmology in general is on the leading edge of adopting sustainable practices within the healthcare profession.
“What I hear when I speak to other medical doctors in the Netherlands is that we as ophthalmologists are definitely pioneering,” he says. “Hopefully, ophthalmology will inspire our fellow medical specialists. So, ideally, key opinion leaders like David Chang and Oliver Findl might be invited to speak to other medical societies and say, ‘This is what we’ve done in ophthalmology,’ and maybe some of this kind of thinking could transfer.”
ESCRS Launches Cat Pack Tool
Wondering how your cataract pack affects the environment? ESCRS has launched an online tool to help you find out.
The tool is the result of the SIDICS Project, an ESCRS-led initiative to create metrics to evaluate the overall sustainability of cat packs. Use this fourstep process to see how your packs compare with the ESCRS benchmark recommendation and where there is a potential for CO2 savings.
1. Enter the number of cataract packs you order annually.
2. Choose items for your pack from the list to see its CO2 footprint and how it compares with the ESCRS benchmark.
3. Adjust the components and learn how much CO2 you save.
4. Use the final list for ordering cat packs in the future.
Note for industry: You can add your own product alternatives and their CO2 information to see how it changes the carbon footprint of cataract packs.
7
2023 SEPTEMBER | EUROTIMES
The “ESCRS Arena” at the Congress will be the setting for pro-con discussions on a variety of topics.
ESCRS Membership by Country
8
Belgium • 255 Germany • 547 Poland • 112 Spain • 275 Brazil • 128 India • 161 Portugal • 139 Switzerland • 194 Egypt • 118 Italy • 311 Romania • 159 Turkey • 180 Finland • 246 Morocco • 181 Saudi Arabia • 115 United Kingdom • 452 France • 143 Netherlands • 414 Serbia • 91 United States • 110 ESCRS AT A GLANCE EUROTIMES | SEPTEMBER 2023 Countries with highest member totals in 2022.
ESCRS Supports Cataract Project in Nepal

Partnership with Ridley Eye Foundation delivers care in remote mountainous areas.
BY ANGIRA SHRESTHA MD
Nepal is a small (147,000 km²), landlocked country in Asia known for its diverse culture, stunning mountain ranges, and rich history. Most of Nepal’s roughly 30 million people live in rural and remote areas and do not have easy access to healthcare services, including eye care. Several other factors are making this problem worse, including a shortage of medical specialists in rural areas, a lack of basic supplies, and financial and cultural barriers.
Some charitable organisations are partnering with healthcare institutions in Nepal to expand access to medical care for these rural populations. For example, the Ridley Eye Foundation (REF), established in 1967 by the pioneer ophthalmologist who invented intraocular lens surgery, is providing free cataract surgery in the remote Nepalese communities along the Himalayan Range.
As much as 80% of preventable blindness in the mountainous areas of Nepal is due to cataracts, but access to cataract surgery is difficult in remote, high-altitude communities.1 Additional challenges to cataract surgery are the medical cost, the loss of earnings while travelling, and a lack of public information on its availability.
Salambu field camp
Dhulikhel Hospital is an independent, non-profit institution conceived as a cost-effective and compassionate provider of quality healthcare services in remote areas. Dhulikhel has been operating 17 outreach centres that provide 24-hour services through its staff, who reside in the centres as part of their communities.
In February 2023, with the generous support of ESCRS, the REF partnered with Dhulikhel Hospital to establish a field surgical camp at Salambu in the Bagmati Province in the foothills of the Himalayas northeast of Kathmandu. The Salambu camp triaged 277 patients and operated on 38 of them.
One of the patients was Mr Hom Bahudur Gurung, a 44-year-old man born with Down syndrome. Deaf and barely able to speak, he was raised by his brother and sister-in-law. He never attended school; over time, he slowly became less active and could only walk by supporting himself on walls.

Hom Bahudur was brought to Salambu by his brother and sister-in-law. At presentation, his vision was only a perception of light in both eyes. He had bilateral white mature cataracts. A B-scan of both eyes was normal. After preoperative evaluation, he was scheduled for cataract surgery under general anaesthesia (GA), as he was very reluctant to leave his guardians to go to the operating theatre.
Bilateral small incision cataract surgery (SICS) was performed. After the surgery, his hands were tied with elastoplast because he was trying to remove his eye guards and bandages and rub his eye. When his eye guards and bandages were removed the next day, he went up to a mirror and saw himself. The smile on his face was priceless.
A week later at his postoperative follow-up, we couldn’t get his exact visual acuity, but he could now walk comfortably and even dance with happiness. He then went to the window and was clearly looking to find his house amongst the hills surrounding Dhulikhel.
Our work with REF has allowed us to take surgery to patients like Hom Bahudur rather than forcing them to travel to the hospital for surgery. We are proud of our partnership with REF—and through our skill and their encouragement, we are at long last able to reach the unreachable in the remote and impoverished communities of the Himalayas.
We are hugely grateful to the ESCRS for their support of this camp. The camp could not have been established otherwise, and 277 people would have remained blind or become blind—a result that would have been wholly preventable.
For citation notes, see page 54.
Dr Shrestha is senior ophthalmic surgeon at Dhulikhel Community Hospital in Nepal.
9 ESCRS ABROAD
2023 SEPTEMBER | EUROTIMES
The AI Conundrum: Unleashing Potential or Awakening the Terminator?
BY YARROW SCANTLING BIRCH MD
The year is 2079. The artificially intelligent (AI) machines have won—the once sacred doctor-patient relationship has decayed under the weight of ruthless standardisation. Time, a once cherished human resource for building understanding, has been replaced by AI-driven algorithms that economise on human interaction. Empathy has become an antiquated notion, trampled under the boots of scientific progression. As an ophthalmologist of the future, you work virtually to moderate the activity of numerous clinical rooms, hearing synthetic conversations, and witnessing the replacement of human touch with the sterility of a robotic handshake.
The revolution
As we enter the Fourth Industrial Revolution, technologies capable of surpassing human intelligence are emerging. AI encompasses data-driven computer systems that use algorithms and machine learning to rapidly process large quantities of data and solve complex problems. Deep learning (DL), a variant of machine learning, is inspired by the cortical architecture of our own brains. DL employs deep neural networks (DNN) to analyse inputs through interconnected artificial neurons across multiple layers.
A wealth of pixelated information
AI in ophthalmology shows promising potential in detecting retinal disease and glaucoma, the leading causes of blindness in Western society. Optical computed tomography (OCT) scans use infrared light to capture detailed retinal structures and is becoming the gold standard ophthalmic imaging tool. DNNs can digest the wealth of pixelated data on OCT into lower-level inputs. These DNNs can outperform ophthalmic experts in the diagnosis of various retinal conditions and have been developed into autonomous commercial AI systems, such as IDx-DR (LumineticsCore). Similar advancements have been
made in detecting early glaucoma. Integrating AI systems in front-of-house triage and screening services has the potential to improve accessibility and affordability of eye care, as well as alleviate work from busy eye clinics. Moving forward, AI needs to expand beyond ophthalmic imaging to other ocular biomarkers such as the oculome, which holds promise for the early detection of systemic disease. This would unlock an era of personalised and whole-system medicine.
Black box learning
The lack of transparency in AI poses a significant challenge. DNNs resemble enigmatic black boxes, making it difficult to unravel their inner workings. This obscurity compromises the principle of nonmaleficence, as AI models generate outputs without clear rationales and erode trust in their validity.
An unexpected revelation occurred when Google researchers developed a DNN model to predict cardiovascular risk, only to discover that gender could be identified from fundus photographs alone. This surprised the researchers due to the seemingly implausible nature of such a hypothesis, but equally, there was no means to investigate the underlying reasoning behind this output.
Collaboration, regulation, and bias
Commercial interests are driving an unregulated arms race in AI innovation with no consideration for potential harm. In ophthalmology, there are numerous patented algorithms but few fully approved regulatory devices on the AI market. Given these AI models thrive off large quality data sets, it appears wasteful that data sharing and collaborations are not being forged amongst medical technology firms. This results in greater bias within individual AI models, less standardisation of diagnostic inputs, and less generalisability to larger populations. Efforts like the EU’s AI Act aim to establish legal legislation for AI products and address issues regarding safety and bias, but these are not keeping up with the progress of AI technology.
The issue of privacy is crucial as ophthalmic images used to train AI models can be reverse-engineered to reveal confidential information. Patient autonomy is maximised when patient-derived data is obtained with informed consent, lawfulness, and compliance with data regulations. However, the use of patient-derived data for commercial ventures remains a major challenge and may create future disputes.
Liability is another ethical challenge. AI engineers responsible for developing algorithms impacting clinical care should bear equal responsibility for adverse outcomes from AI errors,
10 EUROTIMES | SEPTEMBER 2023 HENAHAN PRIZE FINALISTS
In the immortal words of the Terminator, we embark on a future where AI machines and ophthalmologists will stand side by side to deliver outstanding patient care.
especially if the technology is claimed to be autonomous. This remains a major argument for why eye care professionals still need to oversee AI decision-making and will not be replaced anytime soon. AI models still lack the ability to contextualise information within the wider clinical picture and undertake nuanced decision-making.
Conclusions
Currently, AI has the potential to revolutionise the screening and diagnostic workflow within ophthalmology. However, as we navigate this new revolution, it is crucial for humanity to take an active role in steering the trajectory of AI research. AI has the potential to open Pandora’s box, both unleashing immense potential, but also raising ethical dilemmas regarding transparency, commercial bias, and ownership of confidential
data. Taking a moment to pause and ensure AI legislation keeps up pace with technological advancements will allow us to establish ethical frameworks to safeguard humans. In the immortal words of the Terminator, we embark on a future where AI machines and ophthalmologists will stand side by side to deliver outstanding patient care.
Dr Birch submitted this essay to the John Henahan Writing Prize essay contest, answering the prompt “What is the potential role for AI in ophthalmology, and what are the negative implications and caveats?”. It was rated in the top 5 of 41 essays submitted by the medical editorial board of EuroTimes . Dr Birch is a firstyear trainee at Whipps Cross Hospital, Barts Health NHS Trust, London, UK. yarrow.scantling-birch@nhs.net
The Symphony of AI in Ophthalmology
BY SIYIN LIU MD
Medicine is at a critical inflection point for artificial intelligence (AI). With a whopping 3,327 new AI companies in the mix and a projected $37 billion splurge on AI by 2025, this tech is drastically transforming every industry, including healthcare.
Ophthalmology, with its rich imaging data, presents an ideal setting for training algorithms in image recognition, segmentation, and disease detection. Current focus lies on prevalent ophthalmic conditions like diabetic retinopathy (DR), age-related macular degeneration (AMD), and glaucoma, leveraging large, standardised imaging data sets. The COVID pandemic accelerated the integration of AI into tele-ophthalmology, exemplified by the FDA-approved autonomous diagnostic device for DR, enabling point-of-care diagnosis without human oversight. Challenges exist in AI research for anterior segment diseases due to non-uniform slit-lamp images and limited data sets. Nevertheless, recent advancements demonstrate AI’s potential in the anterior segment, including early detection of keratoconus, post-refractive surgery ectasia screening, and diagnosis of infectious keratitis.
AI in ophthalmology has primarily focused on image-based deep learning. Yet, the adoption of electronic health records has unveiled the untapped potential of unstructured free-text data. Natural Language Processing (NLP) and algorithmic rule-based text extraction techniques have shown promise in leveraging this data to enhance care delivery and for big data analysis, predictive modelling, cohort identification, and stratification. NLP also standardises specialised ophthalmic terminology, facilitating interactions among healthcare providers and patients. With predictions that 85% of customer interactions will be managed without human agents by 2025,
NLP-based chatbots hold tremendous potential in triaging symptoms, monitoring treatment adherence, and providing support in areas with limited ophthalmology services.
AI chasm
A core challenge in applying AI is the clinical validation of recently developed concepts and tools. Clinical AI research faces limitations due to retrospective design, leading to biased algorithms “overfitted” to specific data sets. The conventional approach of pitting AI against clinicians may not demonstrate real-world performance, as its realistic application likely involves interaction between clinicians and algorithms. Clinicians, the end users, must grasp AI’s strengths and limitations to foster mutual learning. Envisioning AI’s role in high-risk real-time situations like surgery, where surgeons adapt their approach on the fly, is challenging.
AI regulatory approval is another challenging obstacle. Many algorithms rely on complex and opaque mathematical models, often referred to as “black boxes.” The lack of transparency raises concerns about data mishandling and understanding of the algorithms’ inner workings. Agencies like the FDA/EMA require extensive transparency in scientific methods, but researchers and companies may hesitate to expose proprietary algorithms publicly due to potential financial risks. Further, without a clear understanding of algorithmic processes, AI may struggle to gain patients’ trust and approval. Would it be worse for patients to be misdiagnosed by a human or a machine? What if the algorithm had demonstrated superior performance in research settings? Ultimately, trust and confidence in algorithmic decision-making play a pivotal role.
11
2023 SEPTEMBER | EUROTIMES
Overall, more rigorous work is needed to combat the disparity between AI hype and application in healthcare, the so-called “AI chasm.”
The glass cage
The integration of AI into healthcare runs the risk of stripping medicine of its human touch. With advancing algorithms, we may see clinics where machines take the lead, like a macular clinic where an OCT machine decides on intravitreal anti-VEGF injections for AMD without ophthalmologist involvement. Even with fancy AI voice synthesizers like Siri, the empathy and intuition of the doctor-patient relationship diminishes. After all, to these machines, patients are reduced to mere data points where efficiency and cost-effectiveness are the sole measures of success. Further, overreliance on AI-powered automated diagnosis or treatment decisions may stunt the clinicians’ development of critical thinking and decision-making skills, which may, with time, add them to the list of skills lost due to technology.
Biases embedded in the training data can perpetuate inequalities by providing inaccurate or inadequate recommendations for certain groups or populations. With training data predominantly derived in the Western world, algorithms may struggle to effectively generalise to diverse groups. Unchecked, AI can reinforce and amplify existing disparities in healthcare outcomes. Also, the ethical implications of data ownership and privacy protection arise in an era of round-
the-clock data collection from gadgets and wearables. Algorithms may exploit this data and stigmatise the chronically ill or those who don’t fit the “healthy lifestyle” mould, potentially leading to unjust financial and health penalties, such as reduced access to insurance.
The rise of AI
We are told AI-powered healthcare is not about replacing ophthalmologists, but rather augmenting their knowledge and expertise. The integration of genomic data, lifestyle factors, and imaging will lead to AI-powered decision support systems that can guide targeted therapies and tailored interventions. Although AI’s current capabilities fall short of the hype, overcoming challenges could unlock its potential in achieving the holy grail of personalised medicine. Yet, the question remains whether the rise of AI leads to the “machinification” of medicine.
Dr Liu submitted this essay to the John Henahan Writing Prize essay contest, answering the prompt “What is the potential role for AI in ophthalmology, and what are the negative implications and caveats?”. It was rated in the top 5 of 41 essays submitted by the medical editorial board of EuroTimes . Dr Liu is Specialty training year 4 at UCL Institute of Ophthalmology, London, UK. siyin.liu@ucl.ac.uk
What is the Potential Role of AI in Ophthalmology?
BY ARUN JAMES THIRUNAVUKARASU MD
Ophthalmology is at the forefront of medical artificial intelligence (AI) innovation. Through deep learning— where artificial neural networks are trained to process unstructured data such as images and text—many models have been validated for use with fundus photography, optical coherence tomography (OCT), and electronic patient records to augment diagnosis, management planning, and risk stratification.1 Opportunities abound, but risks and limitations must be considered and ameliorated to ensure that AI benefits patients and practitioners.
Opportunities for development
Some AI tools have already undergone validation and acceptance by regulatory authorities such as the US FDA or EU MDR. Progress has been greatest in models for diabetic retinopathy (DR) screening, such as IRIS and IDx-DR.1 For these tools, the aim for development is cost-effective and clinically successful implementation. Economic modelling and systems analysis suggest these models are best used alongside clinicians rather
than as a replacement—negative marginal revenue was recorded following autonomous deployment of IDx-DR in the US, but semi-automation (AI triage followed by human assessment) was shown to be cheaper than autonomous deployment or humans working without AI in Singapore.2,3 Benefits of implementation are likely to be greater where human resources are more strained, such as in lower-income countries where access to ophthalmologists is more limited: Cybersight and ARDA have been used to good effect for DR screening of hundreds of thousands of patients in India, Rwanda, and Thailand.4,5 Further work is necessary to identify how other models should be incorporated into ophthalmology services.
However, even where there is better access to care, resources are strained, with waiting lists ballooning around the world in the wake of the COVID pandemic. 6 Deployment of AI systems may help address these issues. Large language models (LLMs) exhibit limited ophthalmological knowledge and are unlikely to be deployed as autonomous agents, but they can serve to improve the efficiency of
12 EUROTIMES | SEPTEMBER 2023
PRIZE FINALISTS
HENAHAN
cognitive work by rapidly assimilating information from disparate sources such as clinic notes, correspondence, and investigations. 7,8 As multimodal LLMs such as GPT-4 (OpenAI, San Francisco, California, US) and PaLM 2 (Google LLC, Mountain View, California, US) emerge, functionality is set to increase—models can now cope with the rich variety of image-based ophthalmological investigations in addition to large volumes of text. Multilingual models may reduce the requirement for translators and improve communication, improving the equity of service provision with patients of different backgrounds. 9 If doctors can delegate time-consuming administrative work to AI assistants, more time can be used to treat patients, improving quality of care and alleviating service pressures.
Conclusion
AI systems offer exciting opportunities to automate repetitive cognitive tasks in ophthalmology, such as assimilation, interpretation, and production of data relating to clinical documentation, investigation results, and management planning.1 Automatic DR screening has demonstrated this potential as validated models with regulatory approval are changing clinical practice internationally. Models corresponding to a wide range of other diseases and input modalities are well-established, and implementation is expected to result in significant changes to how eye care is delivered. Policymakers must engage closely with stakeholders to ensure that risks and limitations are mitigated so AI systems work for the greatest possible benefit.
For citation notes, see page 54.
Dr Thirunavukarasu submitted this essay to the John Henahan Writing Prize essay contest, answering the prompt “What is the potential role for AI in ophthalmology, and what are the negative implications and caveats?”. It was rated in the top 5 of 41 essays submitted by the medical editorial board of EuroTimes . Dr Thirunavukarasu is an Academic Foundation Doctor at the University of Oxford, UK. ajt205@cantab.ac.uk
Risks and limitations
There are a wide range of barriers to AI development in ophthalmology. AI introduces new risks and concerns requiring discussion: cybersecurity (Are AI models using patient data safely, away from adversarial attack?), medicolegal issues (Who takes responsibility for decisions made or contributed to by AI?), and the evolving patient-ophthalmologist relationship as computer systems begin to play a larger role in decision making. Other barriers to implementation are more general. Quality of care is of paramount importance, and robust validation is essential to ensure that models are implemented based on true benefit rather than mere hype. There is room for improvement here, as a 2020 systematic review found just one randomised control trial testing deep learning systems against ophthalmologists, despite an exponentially growing literature base.10 Financial, infrastructural, and human resource demands are significant for AI systems, particularly for initial implementation, and it is necessary to consider whether other interventions may represent a more cost-effective means of improving patient outcomes.
These multifaceted considerations are complicated. To ensure that a fair and optimal outcome is reached for all stakeholders, it is critical that patients and practitioners are consulted. Policymakers must retain neutrality when working with innovators who often have conflicts of interest. Technological limitations must be acknowledged—AI is not a panacea—and evidence-based decisions made regarding precisely where models should (and should not) be deployed. These decisions also depend on ethical considerations, as society must reach a consensus on how AI systems should be incorporated into healthcare systems.
THE JOHN HENAHAN WRITING PRIZE
What is the potential role of artificial intelligence (AI) in ophthalmology, and what are the negative implications and caveats?
Earlier this year, young ophthalmologists were invited to submit their answer to that question in an 800-word essay for the John Henahan Writing Prize. The competition was open to ESCRS members (including the free membership available to trainees) age 40 or younger on 1 January 2023.
The three accompanying essays are finalists for the 2023 Henahan Writing Prize. The author of the winning essay will receive a €500 bursary and a specially commissioned trophy, to be awarded during the 2023 ESCRS Congress in Vienna, Austria.
13
2023 SEPTEMBER | EUROTIMES
Quality of care is of paramount importance, and robust validation is essential to ensure that models are implemented based on true benefit rather than mere hype.
Climate Change and Eye Health

Threats arise from direct and indirect pathways.
CHERYL GUTTMAN KRADER REPORTS
The impact of climate change on health is a leading global issue but seems somewhat underappreciated within the eye and vision community, said Dr Michael Chiang, Director of the National Eye Institute, in his introduction to a session on climate change and challenges in global eye health at ARVO 2023 in New Orleans, Louisiana, US.
Corroborating Dr Chiang’s comment, Dr Nisha Acharya cited a recent review article on the impact of air pollution and climate change on eye health in which the authors found a paucity of relevant publications.1 She also highlighted that many online resources focusing on the health effects of climate change lacked content relating to the eye.
Dr Acharya added there is information indicating that climate change and air pollution have direct adverse effects on several ocular conditions.2 Speaking during the same session, Dr Hugh Taylor and Professor Serge Resnikoff opined that the greatest climate change ramifications on eye health would occur via an indirect effect involving climate change’s impact on population migration.
Citing predictions from various models, Dr Taylor said climate change may lead at least 143 million people to move within their own country by 2050, while another source
estimates for every one-degree-Centigrade rise in temperature, at least 1 billion people will be displaced.2–3 Analyses of between-region flows indicate a massive migration of people from equatorial countries northward.
“As a result, we are going to have real problems in the provision of eye care,” predicted Dr Taylor.
“Although there has been progress in the past 20 to 30 years in reducing the prevalence of blindness and vision loss, the number of affected individuals continues to increase with population growth. We must think about how we will address existing unmet needs and what will happen if there is a vast migration of people from underserved regions to high-income areas. Then we also need to consider what we can do in our own behaviours, practices, and activities to reduce carbon emissions.”
Prof Resnikoff also proposed the impact of migration on health systems is the most important issue surrounding climate change and eye health. Referring to the World Health Organization’s health system strengthening agenda and framework describing health systems in six building blocks, he said the financing block will be the most significantly impacted by population migration.
14 EUROTIMES | SEPTEMBER 2023
SUSTAINABILITY
“My suggestion is research on health systems’ resilience and the development of new paradigms for financing, including eye health financing, is of critical importance,” Prof Resnikoff said.
Outlining direct risks
















Depletion of the ozone layer is not the primary threat of climate change, but allowing more ultraviolet radiation (UVR) to penetrate the earth’s atmosphere does have consequences for eye health, Dr Acharya said.
“Increased exposure to UVR is associated with increased risks of ocular surface conditions, including pterygium, ocular surface squamous neoplasia, and cataract,” she observed. “These consequences make sense, and there are data to support the associations.”


Some evidence also shows risks for both cataract and ocular surface diseases expand with increased exposure to air pollutants.4

“There are some mixed results on the effect of air pollution on cataract, so this [needs] further research,” Dr Acharya said. “However, there are studies showing a positive association between increasing levels of particulate matter in the air and a higher rate of cataract development.”
More data are available on associations between air pollution and the development of ocular surface diseases. In addition, researchers from Australia reviewing preclinical studies investigating smoke exposure effects on ocular surface tissues and cells showed the consequences include true biological changes consistent with observed increases in clinical complaints.4
Through its effect on environmental threats, such as extending the length of wildfire and allergy seasons, global warming can also increase exposure to exogenous irritants, thereby increasing ocular surface disease risk. Furthermore, because relative humidity decreases as temperature increases, global warming can cause or worsen dry eye disease.
Yet as another consequence, climate change can impact the incidence and spread of ocular infectious diseases, particularly tick- and mosquito-borne diseases.
“With climate change, these infections might begin to spread across the planet, no longer respecting their traditional geographic boundaries,” Dr Acharya said.
Evidence also points to associations between exposure to higher concentrations of particulate matter 2.5 in the air and increased risks of uveitis, diabetic retinopathy, age-related macular degeneration, and open-angle glaucoma.5–8




































For citation notes, see page 54.

Serge Resnikoff MD, PhD is Professor of Ophthalmology, Brien Holden Vision Institute, Sydney, Australia. s.resnikoff@brienholdenvision.org



Hugh Taylor MD is Professor of Ophthalmology Emeritus, University of Melbourne, Australia. h.taylor@unimelb.edu.au



Nisha Acharya MD, MS is Director of the Uveitis and Ocular Inflammatory Disease Service, University of California San Francisco, US. nisha.acharya@ucsf.edu


15 2023 SEPTEMBER | EUROTIMES
Links in Eye Care Delivery and Climate Change
Exploring the relationship shows strategies are needed for both mitigation and adaptation.
CHERYL GUTTMAN KRADER REPORTS
As large contributors to greenhouse gas emissions, healthcare systems have a major impact on climate change, which already negatively impacts healthcare delivery. Breaking the cycle requires ophthalmologists and associated stakeholders to implement strategies for reducing their carbon footprint and adapting to climate change, emphasised Dr Cassandra Thiel.
“If global healthcare were a country, it would be the fifth largest contributor to carbon emissions in the world,” she said. “We need to mitigate our greenhouse gas emissions to reduce the negative impact the care we provide has on the population, health, and the environment. But we also have to think about preparing for the consequences of climate change-related events that interfere with our ability to deliver care. By rethinking how things are done, we have an opportunity to impact climate change and improve care. And adaptations in our health systems will enable recovery from climate shocks and perhaps leave them operating better than before.”
Improving sustainability
Focusing on the carbon footprint of cataract surgery (one of the most commonly performed operations), Dr Thiel reviewed findings from studies examining emissions related to surgical supply manufacturing, distribution, and waste. These findings show substantial differences in waste generated through cataract surgery conducted in high-income versus low-income countries, indicating opportunities exist for increasing resource efficiency without compromising outcome quality.

For example, analyses performed using environmental life cycle assessment showed a phacoemulsification procedure at Aravind Eye Centre in India emits about 5% of the greenhouse gases of one in the United Kingdom.1,2
“Cataract surgery is much more efficient at Aravind than in developed countries, and Aravind’s outcomes are just as good,” Dr Thiel said. “Therefore, we know cataract surgery can be done differently yet safely.”
Similarly, results from a study analysing data obtained with “Eyefficiency,” a cataract surgical services auditing tool Dr Thiel and colleagues developed to help units improve their surgical productivity and reduce costs, waste generation, and carbon footprint, showed significant variations in measured endpoints between centres located in different geographic regions.3
“Often, we found that lower-income countries lacking the resources to spend a lot on supplies already implemented very efficient ways to perform cataract surgery and do it well,” she said. “These are [lessons] practices can use to improve value by reducing costs and minimising their envi-

16 EUROTIMES | SEPTEMBER 2023
SUSTAINABILITY
ronmental footprint while still providing high-quality care.”
To assist US surgeons in making changes prioritising sustainability, Dr Thiel and colleagues created decision flowcharts for selecting interventions related to supplies and pharmaceuticals used in cataract surgery.4
“‘Do we need to use it?’ is the first question you should ask about every supply and pharmaceutical you have in your procedure room,” she said.

“If the answer is no, then consider if you can remove it from your custom packs. If a supply is needed, ask if it has to be single use, and for necessary drugs, consider if any part is being wasted after surgery.”
Dr Thiel also discussed EyeSustain as a resource for information on reducing surgical waste and ophthalmology’s carbon footprint (eyesustain.org). As part of its mission to make ophthalmic care and surgery more sustainable, EyeSustain’s leadership reaches out to manufacturers and regulators to achieve changes.
Steps for climate change resiliency
Strategies for adapting to and coping with the potential for hazardous impacts of climatic events are harder to specify, Dr Thiel said, because they can be unique to individual institutions, de-


pending on such issues as existing infrastructure and the likely threats. The process for becoming more climate change resilient begins with assembling a diverse team of relevant stakeholders who will then work to characterise valued and crucial assets, the risks to those assets from a possible climatic event (e.g., wildfires, hurricanes, floods), the likelihood of any such event, and the resulting consequences.
Energy sourcing has been one such focus of adaptation strategies. Solar panel installation is a step facilities have taken to ensure power is available if a climatic event shuts down the grid, but it has additional benefits. For facilities where grid operation is not always reliable, having a constant power supply might lengthen equipment lifespan. In addition, solar panels represent an environmentally friendly, clean energy source. While strategies for reducing and reusing supplies are part of the framework for climate change mitigation, they are also relevant for adaptation because they lessen the impact of a non-functioning supply chain.
“Overall, the main theme is rethinking how we are doing things by asking, ‘Do they have to be done that way?’,” she concluded.
For citation notes, see page 54.
17 2023 SEPTEMBER | EUROTIMES
(Left) Total solid waste from one US phaco and total solid waste from 93 phacos at Aravind in India.
Dr Thiel spoke at ARVO 2023 in New Orleans, Louisiana, US.
Cassandra Thiel PhD is an Assistant Professor, Departments of Population Health and Ophthalmology, New York University and NYU Langone Health, New York, US. Cassandra.Thiel@nyulangone.org
VIEW OF OPEN-EYED AN AI

Reaping the benefits will require good data and careful design and oversight.
BY HOWARD LARKIN
18 EUROTIMES | SEPTEMBER 2023
On two occasions I have been asked, ‘Pray, Mr Babbage, if you put into the machine wrong figures, will the right answers come out?’... I am not able rightly to apprehend the kind of confusion of ideas that could provoke such a question.” – Charles Babbage, inventor of the digital programmable computer, from Life of a Philosopher (London, 1864).
In 1837, Charles Babbage designed a programmable mechanical calculating device that is the conceptual model for most electronic digital computers today. With the above quote, he also articulated a computer truism later formulated as “GIGO”—garbage in, garbage out. In other words, the quality of any computer output depends on the quality of the data and programming going in.
And so it remains, even in the realm of artificial intelligence (AI). AI is any computer application that does something normally thought to require human intelligence, Dr Pearse A Keane, an ophthalmologist and professor of artificial medical intelligence, told EuroTimes. However, AI deep learning models go beyond traditional computer programs by independently identifying relationships among data points not prespecified by programmers. Further, they can be programmed to learn and adjust their algorithms based on new information. This gives AI enormous and unforeseeable transformational potential on par with the advent of personal computers—and ophthalmology is at the forefront, he said.
But whether they are narrowly focused, supervised applications trained on labelled ocular images or other curated data sets, or unsupervised or generative applications powered by
large language models (LLM) accessing hundreds of billions of words, images, recordings, or medical records, AI-enabled programs are still computer programs. As such, they require careful design, testing, training, and ongoing supervision to work reliably and accurately—at least for now.

“We have seen a lot of hype around AI. The interesting and scary thing is progress is accelerating—even in the last few months—that is really blowing everyone’s mind outside healthcare. It will be absolutely huge,” Dr Keane said. “But we need to balance enthusiasm with caution for anything used in healthcare.”
So, just as ophthalmologists wouldn’t send a referral note or answer a patient question using only what the electronic medical record provides or diagnose glaucoma progression based on automated visual field analysis alone, the output of any AI system, no matter how sophisticated, always should be carefully evaluated and edited, said Dr Ranya Habash, co-chair of AI for the American-European Congress of Ophthalmic Surgery.
“No one is asserting that we should let algorithms treat our patients without oversight. In fact, that’s exactly the opposite,” Dr Habash said. “We can allow AI to perform the tedious tasks to help us be more efficient; then, we oversee the output to make sure things are accurate before they go out. It’s our responsibility and an obligation.”
Model drift and hallucinations
There are many types of AI, but those used in healthcare are predominantly deep learning variants of machine learning. They use neural networks to
19 2023 SEPTEMBER | EUROTIMES
“
iteratively identify, examine, and statistically test correlations among data points based on images or other digital data such as biometry measurements or text.
The goal is to develop models capable of predicting likely diagnoses or outcomes in patients outside the training data set used, such as screening for diabetic retinopathy or selecting the appropriate IOL power for cataract surgery. LLMs may also help draft documentation, patient communication, surgical plans, reports, and papers, or even assist in resolving diagnostic dilemmas.
Because these statistical models are empirical, their predictive power depends heavily on the make-up of their data

“hallucinations”—or a confident presentation of wildly wrong information. Generative AI systems making up references or describing how the Golden Gate Bridge moved to Egypt are examples. LLMs are being revised to reduce or eliminate these problems. But he advised always checking the text for accuracy before signing off on it.
The clinician’s role
While most clinicians will not participate directly in developing AI applications, these tools will likely become ubiquitous soon, Dr Keane said. Practising clinicians will not only use such applications—many will likely provide clinical data for updating them through electronic systems.
As AI applications become available, clinicians need to educate themselves on appropriate use, Dr Keane said. “Learn how to identify their strengths and weaknesses. In a certain type of patient, an algorithm might not be so accurate—that is the kind of learning we will need.” For example, an algorithm developed on average axial lengths may not be as accurate as one developed specifically for shorter eyes.
training sets. In general, the larger and more representative the training set is of the general patient population, the more accurate the model will be for clinical use.
Typically, only part of the sample data set trains the models, with the resulting algorithm tested for accuracy on the remaining portion. Tweaking and rerunning the model occurs at this stage. But before its use in practice, it should also be clinically validated with other methods, Dr Keane said.
Testing for approved AI medical devices is stringent, and devices in clinical use should meet that standard, he added. AI-trained devices currently approved by the US Food and Drug Administration (FDA) are locked, meaning they do not learn, and the model doesn’t change. The agency is developing regulations to accommodate machine learning by requiring a prospective plan to revise and test models without further approval.
Data quality is also critical, Dr Mark Lobanoff told EuroTimes. But clinical data gathered from large groups of practices can be unreliable due to differences in when and how it is collected, even the calibration of test equipment.
In his work with Bausch + Lomb developing AI applications for eyeTELLIGENCE, an ophthalmology software platform, Dr Lobanoff addresses the issue by using a subgroup of data known to be meticulously collected. Models, such as those calculating IOL power or detecting glaucoma progression, are developed using this set and then tested in the larger, less curated data set to find tweaks to improve performance.
Clinical validation involves running beta versions alongside existing methods and comparing the outcomes the models predicted with those achieved using the existing methods. Only then will the AI models be ready for clinical use, which Dr Lobanoff said is about two years off for eyeTELLIGENCE.
Dr Lobanoff said care also must be taken using generative LLMs, such as ChatGPT. “We don’t always really understand what AI is doing, how it finds a solution.” This can lead to
Awareness of the importance of collecting accurate data is also critical, Dr Lobanoff said, noting precise postoperative manifest refractions are particularly needed to evaluate cataract procedures. This could drive culture changes in practices to collect such information more regularly and rigorously, benefitting these practices with better AI models. “Accuracy means a happier patient.”
20 COVER ARTICLE EUROTIMES | SEPTEMBER 2023
Pearse A Keane MD is an ophthalmologist at Moorfields Eye Hospital, London, UK, and professor of artificial medical intelligence at University College London. p.keane@ucl.ac.uk
Ranya Habash MD is an ophthalmologist and assistant professor of ophthalmology at Bascom Palmer Eye Institute, Miami, US. ranya@habash.net
Mark Lobanoff MD is an ophthalmologist and founder and president of OVO LASIK + LENS, a private clinic; founder and CEO of Phorcides, a LASIK software firm. mlobanoff@gmail.com
No one is asserting that we should let algorithms treat our patients without oversight. In fact, that’s exactly the opposite.
Emerging Ophthalmic AI Applications
Ophthalmology is in the vanguard of medical specialties adopting AI for clinical use. Here’s a short list of some of the applications entering the clinic.

In April 2018, the IDx-DR system for automatically assessing and recommending referral or continued screening for diabetic retinopathy (DR) became the first AI-enabled diagnostic medical device capable of independent diagnosis approved by the US FDA. Several additional DR and retinal disease diagnostic systems have been approved since, and several more are CE marked and available outside the US.
Non-DR ophthalmic AI devices that already exist or have potential include:
IOL power calculators – Improving cataract surgery outcomes requires getting the intraocular lens power just right. Tests have shown they rival, if not exceed, traditionally designed power calculators. They have the advantage of being customisable for eyes that are difficult to calculate, including short, long, and post-refractive surgery. Cataract IOL power calculators now in use include the Hill-RBF, Zeiss AI, Kane, Pearl-DGS, and Barrett Universal II.
Predictive analytics – Predictive analytics is another powerful way AI can support clinical care. Applications in development include devices for detecting, measuring, and predicting glaucoma progression.
Aiding complex diagnoses – Large language model AI has had success helping physicians with diagnostic dilemmas. They can do a good job of summarising observations and steering clinicians towards unusual diagnoses they may not have considered.
Oculomics – AI drives oculomics, which finds biomarkers in the eye for non-ocular diseases. It already has helped identify retinal biomarkers for several neurological ones, including multiple sclerosis, Parkinson’s disease, and Alzheimer’s disease. Ocular biomarkers also have been found for psychiatric, cardiovascular, haematological, nutritional, respiratory, autoimmune, infectious, and retinal conditions, as well as drug toxicity.
Documenting patient visits – Several medical records firms are already incorporating AI to prepare patient visit summaries, reducing time spent writing them out manually or by pull-down menu.
Patient education and communication – Dora (Ufonia) is an automated system for making follow-up calls to patients after cataract surgery. In tests, it has been shown as accepted by most patients and preferred by many, reducing routine clinician activity by up to two-thirds. The similarly named but distinct AskDora (Myma Healthcare) answers clinic phones and provides information on hours, locations, and services. It can also schedule appointments, reducing staff time. EPIC is rolling out ChatGPT-enabled patient education tools to answer patient questions.
Augmented and virtual reality and the metaverse – VR training allows surgical trainees to immerse themselves in the procedure and even examine anatomy features from any angle. It can also support patient education. An FDAcleared NovaSight device for treating amblyopia uses eye tracking and image processing to blur vision as an alternative to eye patching.
21 2023 SEPTEMBER | EUROTIMES DIGITAL OPHTHALMOLOGY
AI-Enabled IOL Power Calculations for Short Eyes





An artificial intelligence-enabled intraocular lens (IOL) power calculator that applies real-world patient diagnostic measurements to specific IOL models may more accurately predict refractive outcomes in short eyes than most of the best current formulas, according to Dr Douglas D Koch.
The Zeiss AI IOL calculator is the first AI-based formula specific to individual IOL models, Dr Koch said, noting optimising IOL constants based on population-level data is misleading if the cohort is not representative of the population at large or if the constant varies throughout. Short eyes, post-refractive surgery eyes, and keratoconus eyes are among such inconsistent cohorts.
However, using AI to factor in a broad range of biometry and refractive data recorded before and after surgery with optical data specific to each unique IOL model appears to improve refractive prediction accuracy, though only for IOL models for which the AI formula has been specifically trained.
Short eye study
To test the Zeiss AI calculator’s performance in small eyes, Dr Koch with Dr Warren Hill and colleagues at Baylor College of

Medicine and Carl Zeiss Meditec conducted a test involving 278 eyes implanted with one of three monofocal IOL models: the SN60WF (Alcon), the Tecnis ZCB00 (Johnson & Johnson), and the enVista (Bausch + Lomb). Mean axial length of the eyes was 21.56 mm ± 0.41, ranging from 19.77 mm to 22.00 mm, and statistical analysis showed a non-Gaussian distribution.










The team tested each of the 15 IOL power calculation formulas for predicted and achieved refraction accuracy. Paired comparisons were made of the top 7 formulas based on percentages with outcomes within ± 0.5 D of target. At 0.41 D, the mean absolute error for the Zeiss AI calculator was the lowest of the 7, reaching statistical significance for the Kane, Barrett, and Pearl DGS formulas but not for the K6, Hill-RBF, or EVO. Root mean square absolute error results were similar, with the K6 value lower than the Barrett value.

22 EUROTIMES | SEPTEMBER 2023
Training with IOL model-specific, real-world data may improve accuracy. HOWARD LARKIN REPORTS DIGITAL OPHTHALMOLOGY Internal use 3. Refine prediction 3. IOL-model-specific AI training based on real clinical data 17 July 2023 ZEISS 1 Real pre-op biometry Measured residual SE Predict residual SE and IOL SE power on real eyes 1. Learn the physics 2. Predict post-op IOL position Simulated realistic eyes Paraxial ray-tracing AI Predict residual SE and IOL SE power on model eyes Real pre-op biometry Real post-op ACD AI Predict post-operative IOL position (PLP) 500,000 model eyes generated General AI IOL-optimized AI
IOL-model-specific AI training based on real clinical data
For the future, you can build a larger database of eyes with various parameters.
To ensure quality, anonymised data for the calculator are collected automatically from the Zeiss Veracity surgical planner with strict filtering criteria, including testing visual acuity using a 6M lane. Data have already been collected on more than 100,000 eyes, and six IOL models have more than 1,000 eyes, Dr Koch said.



“For the future, you can build a larger database of eyes with various parameters, including anterior chamber depth, lens thickness, and corneal diameter, optimised for each IOL model,” he said. “Using optics with paraxial ray tracing to frame where you are working and, from there, building up the models using real-world data … is a really promising approach.”
The First Piece for Myopia Management, The Key Piece for Success
· Simply add it to your practice and your platform is ready for Myopia Management.
· Easy. Quick. Accurate.
· Visualize progression and treatment outcomes.
Douglas D Koch MD is professor and Allen, Mosbacher, and Law Chair in Ophthalmology at the Baylor College of Medicine, Houston, Texas, US. dkoch@bcm.edu
Dr Koch consults with Alcon, Carl Zeiss Meditec, and Johnson & Johnson Vision.
Find out more at ESCRS Booth #B304, Hall B

www.nidek.com

23 2023 SEPTEMBER | EUROTIMES Internal use Mean Absolute Errors (MAE) 0.41 0.43 0.44 0.44 0.44 0.45 0.37 0.38 0.39 0.40 0.41 0.42 0.43 0.44 0.45 0.46
* * *
K6 Hill-RBF Kane EVO Barrett Pearl-DGS
* Internal use Root Mean Square Absolute Error (RMSAE) 0.55 0.53 0.58 0.59 0.60 0.60 0.60 0.48 0.50 0.52 0.54 0.56 0.58 0.60 0.62 Zeiss
*Zeiss AI had smaller MAE than Kane, Barrett, and Pearl-DGS (adjusted P<0.05)
AI K6 Hill-RBF Kane EVO Barrett Pearl-DGS
* * * * ** **
*Zeiss AI had smaller RMSAE than Kane, Barrett, and Pearl-DGS
**K6 had smaller RMSAE than Barrett
Dr Koch presented at the inaugural Digital Ophthalmic Society Digital Day of the 2023 ASCRS annual meeting in San Diego, US.
Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol 2018;96(3):301-309. doi:10.1111/aos.13603
M
AL-Scan
Optical Biometer NEW
Mean Absolute Errors (MAE)
Root Mean Square Absolute Errors (RMSAE)
Pharmacotherapy for Dim Light Vision Disturbances
Study suggests topical phentolamine improves visual function.
CHERYL GUTTMAN KRADER REPORTS
Apivotal trial investigating phentolamine 0.75% ophthalmic solution (Nyxol, Ocuphire Pharma) for improving visual function in patients with dim light vision disturbances (DLD) met its primary endpoint, and planning is underway for a second phase 3 study.

Known as LYNX-1, the study randomised 145 adults with DLD 1:1 to phentolamine or vehicle, one drop into both eyes at or near bedtime for 14 nights. The primary efficacy endpoint analysis showed that at day 8, the percentage of patients achieving a ≥3-line improvement in mesopic low-contrast distance visual acuity (mLCVA) was significantly greater in patients using phentolamine than the control group (13% vs 3%; P <0.05). The research team also saw a significant difference favouring phentolamine over vehicle in the percentage of patients with a ≥3-line improvement in mLCVA at day 15 (21% vs 3%; P <0.01).
“Over 40% of patients in the phentolamine group gained two or more lines in mLCVA at days 8 and 15, and subjectively, patients were very happy with their outcome,” said Dr Mitchell Brigell, head of clinical development and strategy at Ocuphire Pharma.
Higher-order aberrations in the cornea and ocular scatter cause the photic phenomena and decreased mesopic vision patients with DLD experienced. Phentolamine, a non-selective α-adrenergic agonist, addresses the underlying aetiology by causing pupil constriction, thereby blocking out-of-focus peripheral light rays. In LYNX-1, pupil diameter was reduced by a mean of about 1 mm in the phentolamine group compared to vehicle (P <0.0001).
40%
Over 40% of patients in the phentolamine group gained two or more lines in mLCVA at days 8 and 15, and subjectively, patients were very happy with their outcome.
“The pupil does not get so small that night-time vision becomes impaired. Therefore, phentolamine differs from cholinergic miotic drugs, for which the labelling includes a warning to use caution when driving at night or performing hazardous activities in poor lighting,” said Dr Brigell.
“In addition, phentolamine reduces pupil size solely by inhibiting the iris dilator muscle. Unlike cholinergic miotics that cause ciliary muscle contraction, we believe our drug is unlikely to cause brow ache/headache, retinal tears, or retinal detachment.”
Instillation site pain and irritation (13% and 9%), dysgeusia (11%), and conjunctival hyperaemia (9%) were the most common adverse events in the phentolamine group.
Although conjunctival hyperaemia was infrequent and mostly mild, the bedtime dosing regimen aimed to limit any cosmetic concerns relating to this reaction. Users still benefit the next day when instilling phentolamine at night because it has a very long half-life and duration of action, Dr Brigell noted.
LYNX-1 enrolled subjects with a pupil diameter ≥5 mm under mesopic conditions in at least one eye, mLCVA of 20/100 Snellen or worse and self-reported DLD, regardless of known or unknown aetiology. They were stratified for randomisation by iris colour (light/dark). Dr Brigell added the second pivotal trial will apply findings from analyses to identify characteristics associated with a treatment response to refine eligibility criteria.
“The promising results in our study indicate phentolamine holds potential to be a first option for treating DLD,” Dr Jay S Pepose concluded.
24 CATARACT & REFRACTIVE EUROTIMES | SEPTEMBER 2023
Dr Brigell presented at ARVO 2023 in New Orleans, Louisiana, US.
Mitchell Brigell PhD is head of clinical development and strategy at Ocuphire Pharma, US. mbrigell@ocuphire.com
Jay Pepose MD, PhD is Chief Medical Advisor at Ocuphire and Medical Director, Pepose Vision Institute, St Louis, Missouri, US. jpepose@peposevision.com
ESCRS IN A SNAPSHOT
We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With more than 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.

25 2023 SEPTEMBER | EUROTIMES
Small-Aperture IOL for Complex Corneas


Reduced aperture size may mitigate visual impact of optical aberrations.


Corneas with complex optical aberrations generally present a challenge for cataract surgery—especially presbyopia-correcting intraocular surgery. In addition to extending depth of focus, implanting small-aperture intraocular lenses (IOLs) can reduce the impact of ocular aberrations on visual quality, according to Dr Robert Ang.
He characterised complex corneas as those with irregular astigmatism and higher-order aberrations (HOA), such as spherical aberration and coma that degrade visual quality and acuity and complicate cataract surgery, particularly IOL power calculations.
Corneal complexity may occur naturally, though natural HOAs seldom exceed 0.6 microns, Dr Ang observed. Complex corneas also can result from disease (such as keratoconus) or trauma and are often surgically induced through corneal refractive procedures or keratoplasty.
Small-aperture IOLs, he added, are particularly attractive for such patients because they filter out the generally more severe peripheral effects of aberrations and extend depth of focus without inducing additional aberrations, as do other presbyopia-correcting lenses.
Post-refractive surgery success
Dr Ang said he has been implanting the small-aperture IC-8 Apthera IOL (Bausch + Lomb, AcuFocus) in cataract patients since 2014 and discovered early on how effective it can be for post-refractive surgery patients.
“We kind of incidentally figured out the astigmatism is masked with the IC-8.”
He often uses a scleral tunnel approach to avoid weakening corneas with peripheral defects.
Dr Ang conducted a prospective study of 16 post-refractive surgery cataract patients followed for 12 months. Each was implanted with the IC-8 in one eye targeting -0.75 D and a monofocal IOL targeting plano in the fellow eye.
“It’s like a modified monovision, which is similar to the US FDA approval.”
Twelve months after surgery, mean manifest spherical equivalent was -0.550 D ± 0.704 in the IC-8 eye and -0.135 D ± 0.660 in the monofocal eye. Of the 13 IC-8 eyes, 12 achieved 20/25 or better in uncorrected distance visual acuity, 10 achieved it for intermediate vision, and 9 for near vision. Binocularly, all patients achieved 20/25 or better in corrected distance vision, 12 for intermediate, and 10 for near vision.
No IC-8 eyes lost distance-corrected vision compared with the monofocal eyes, while the mean IC-8 defocus above 20/32
Reduced Aperture = Reduced Aberrations
Reduced Aperture = Reduced Abberrations
• Reducing the aperture size of an optical system mitigates the effects of optical aberrations like coma, astigmatism and spherical aberration*
Reducing the aperture size of an optical system mitigates the effects of optical aberrations like coma, astigmatism and spherical aberration*


26 CATARACT & REFRACTIVE EUROTIMES | SEPTEMBER 2023
HOWARD LARKIN REPORTS
Internal use *Vega F, et al. J. Europ. Opt. Soc. Rap. Public. 8, 1307 (2013) Kasper T, et al. J Cataract Refract Surg 2006; 32:78-84 Coma Spherical Aberration Astigmatism Coma Spherical Aberration Astigmatism Optical Aberrations Optical Aberrations with a Small Aperture
We kind of incidentally figured out the astigmatism is masked with the IC-8.
Uncorrected Visual Acuities at 12 Months
Uncorrected Visual Acuities at 12 Months

Mean MRSE at 12 Months
IC-8 IOL eye -0.550 D ± 0.704
Fellow eye -0.135 D ± 0.660
The IC-8 IOL eye achieving 20/25 or better:
• UCDVA: 92.3% of patients (12/13)
• UCIVA: 76.9% of patients (10/13)
• UCNVA: 69.2% of patients (9/13)
Binocular achieving 20/25 or better:
• BCDVA:100% of patients (13/13)
• DCIVA: 92.3% of patients (12/13)
• DCNVA: 76.9% of patients (10/13)
was -2.41 D compared to -1.54 D for the monofocal eyes. Quality of vision was also excellent, with mesopic contrast sensitivity similar between IC-8 and monofocal eyes with or without glare. The incidence and severity of visual symptoms—including glare, halo, starbursts, dim vision, and eye dryness— were low.
“Your first experience [with the IC-8] may be on complex corneas because you cannot put other premium IOLs in this group,” Dr Ang said.

With experience, surgeons may gain confidence in the IC-8 as a premium monovision option in normal corneas. However, he advised against implanting the lens in patients with dilated pupils of less than 6.0 mm due to difficulties visualising the retina.
Dr Ang presented at the Refractive Surgery Subspecialty Day of the 2023 ASCRS annual meeting in San Diego, US.
Robert Edward T Ang MD is a senior consultant and head of cornea and refractive surgery, and research and training at the Asian Eye Institute, Makati City, Philippines. angbobby@hotmail.com
27 2023 SEPTEMBER | EUROTIMES
Internal use
2 20/20 20/25 20/32 20/40
Assessing Transepithelial Surface Ablation Benefits
Epi-on
Transepithelial surface ablation offers a safe, effective, and predictable method of refractive correction in topography-guided photorefractive keratectomy (PRK) and phototherapeutic keratectomy (PTK) procedures, according to Dr Jesper Hjortdal.

In traditional PRK procedures, the corneal epithelium is mechanically removed, most often alcohol assisted, to enable the excimer laser to reshape the cornea. Although successfully deployed for more than 30 years, PRK recovery time is typically longer than LASIK, primarily due to the healing of the corneal epithelium. This prompted the evolution of PRK without epithelial removal to provide theoretically faster healing, faster visual recovery, and better predictability, Dr Hjortdal said.
He noted transepithelial ablation presents its own unique challenges for the surgeon.
“The corneal epithelium is thicker towards the periphery, where the excimer laser is less efficient. The ablation rate of the epithelium is different than the stroma,” he said. “To ensure a controlled stromal ablation, we can increase the number of excimer laser spots in the periphery, use online measurements of the epithelial thickness profile, or use a platform with laser nomograms specifically designed to perform transepithelial PRK.”
He did point out very few randomised controlled trials in the scientific literature compare the two approaches.
A recent meta-analysis by Alasbali included 12 experimental and interventional studies from 2011 to 2021 comparing PRK with and without epithelium, but only two of those studies were randomised controlled trials.1
In terms of visual outcomes, Alasbali found no difference between PRK with epithelium (TPRK) and without epithelium (PRK) for uncorrected distance visual acuity (UDVA) and
spherical equivalent refraction. Corneal haze results were also similar in both procedures. However, there was a faster healing time for TPRK than PRK.
“My interpretation of the study conclusion based on the forest plots indicate the traditional outcome measures are comparable after PRK with and without epithelium, but epithelial healing may be faster after PRK with epithelium,” Dr Hjortdal said.
A contralateral randomised controlled study revealed the visual and refractive outcomes were similar with or without epithelium.2 Furthermore, although the time to complete re-epithelialisation was similar, the epithelial healing rate was faster in conventional PRK, considering the initial corneal epithelial defect area. Patients also experienced less pain and discomfort in the first postoperative day.
Deploying transepithelial ablation can also reduce visual symptoms after complicated SMILE procedures—though Dr Hjortdal added it was important to use mitomycin C after the ablation to reduce the risk of haze development.
The transepithelial approach provided a viable treatment option for a young patient diagnosed with homozygous granular corneal dystrophy type II at six years old.
“She has had repeated transepithelial ablations over many years,” Dr Hjortdal explained. “We always use mitomycin C. She is 17 years of age now, and her visual acuity is 0.4.”
Dr Hjortdal presented at the 2023 ESCRS Winter Meeting in Vilamoura, Portugal.
For citation notes, see page 54.
28 EUROTIMES | SEPTEMBER 2023 CATARACT & REFRACTIVE
Jesper Hjortdal MD, PhD is Clinical Professor at Aarhus University Hospital, Denmark. jesphjor@rm.dk
and epi-off appear to produce similar outcomes.
DERMOT MCGRATH REPORTS
Getting the Maximum from Mini-Monovision
New IOLs designed for monovision could provide more patient satisfaction. DERMOT MCGRATH REPORTS
Implantation of an enhanced monofocal intraocular lens with mini-monovision provides good visual and refractive outcomes and a high level of patient satisfaction, according to Dr Fernando Llovet.
“The RayOne EMV (Rayner) provides excellent distance vision and a high quality of overall vision,” he said. “Spectacle independence was achieved for all patients for far and intermediate distances.”
The RayOne EMV was specifically developed to enhance patient outcomes achieved with monovision, Dr Llovet explained. The lens provides up to 2.25 D of extended depth of vision with a 1.00 D offset, improving intermediate vision compared to monovision achieved with standard monofocal lenses and reducing dysphotopsia compared to diffractive IOL designs. Its design has an aspheric anterior surface and unique inner optic zone, which induces controlled positive spherical aberration to extend depth of field without compromising visual acuity under low-light conditions.
Dr Llovet’s prospective multicentre interventional case series included 80 eyes of 40 patients who underwent delayed sequential bilateral cataract surgery and RayOne EMV IOL implantation. The target refraction was -1.00 D in the non-dominant eye and emmetropia in the dominant eye. The primary outcomes were binocular uncorrected distance visual acuity (UDVA) at 4 m, binocular uncorrected intermediate visual acuity (UIVA) at 66 cm, and binocular uncorrected near visual acuity (UNVA) at 40 cm at one, three, and six months postoperatively. A Spanish version of the CAT-QUEST 9SF questionnaire assessed the patient-reported outcomes (PROMs).
Reporting the mean binocular logMAR UDVA, UIVA, and UNVA were 0.08 (± 0.11), 0.22 (± 0.19), and 0.50 (± 0.10), respectively, at three months postoperatively, Dr Llovet added mean manifest refraction spherical equivalent was -0.05 (± 0.34 D) and -0.85 (± 0.50 D) for the dominant and non-dominant eye respectively. Based on the CAT-QUEST 9SF at the three-month follow-up, all respondents reported spectacle
independence for intermediate and distance, with 29% not requiring glasses for near tasks. All patients also reported satisfaction with their vision, with 86% indicating no difficulty driving at night. There were no adverse events reported during the follow-up period.
Mini-monovision was also the topic of a separate presentation by Dr Zeki Yiğit Karaca, who compared the defocus curves of the Tecnis Eyhance IOL (Johnson & Johnson) at different spectacle-induced mini-monovision levels and emmetropia.
Dr Karaca’s study evaluated 36 eyes of 18 patients implanted with bilateral Eyhance lenses at least three months before the measurement date. The Multifocal Lens Analyzer (Q Vision) obtained one emmetropic and two different spectacle-induced bilateral defocus curves, whose set-ups the team then compared.
The study found near vision could be increased more than twofold without affecting binocular distance vision when the non-dominant eye refraction was set at -1.00 D. When the non-dominant eye refraction was -0.50 D, intermediate vision increased, yet no significant increase in near vision.
“While planning monovision with the Eyhance IOL, aim for -1.00 D in the non-dominant eye to achieve significantly better near vision,” Dr Karaca concluded. “However, patients should be informed they may still need reading glasses, especially for small letters.”

29 2023 SEPTEMBER | EUROTIMES
Dr Llovet and Dr Karaca presented at the 2023 ESCRS Winter Meeting in Vilamoura, Portugal.
Fernando Llovet MD, PhD is Medical Director of Clínica Baviera, Madrid, Spain. fllovet@clinicabaviera.com
Zeki Yiğit Karaca MD is an ophthalmology resident at Medipol University, Istanbul, Türkiye. DrYigitKaraca@gmail.com
Striving for Perfection in LASIK
Combining topography and astigmatism data helps achieve 20/15 in most eyes.
For years, Dr Mark Lobanoff eagerly awaited topography-guided LASIK to make its way from Europe to the United States. Reproducibility and independence from pupil size are among the advantages over earlier wavefront-guided ablation approaches.
But when Alcon’s Contoura Vision topography-guided LASIK finally arrived, his results were not as good as expected. While 88% of eyes in the FDA approval trial reached 20/20 or better uncorrected and 59% reached 20/15 or better, Dr Lobanoff’s early cases saw 73% and 26%, respectively. Similarly, Dr A John Kanellopoulos reported 61% and 22%, respectively.
Behind the discrepancy was the manufacturer’s recommendation to base topographic corrections on manifest refractions, Dr Lobanoff said. While this worked well in the near-perfect corneas allowed into the FDA trial, it didn’t work as well on real-world corneas with significant higher-order aberrations. Topographically correcting corneas with less than 4 microns of corneal astigmatism does not significantly change the cornea’s refractive power, whereas removing 24 microns does, he explained.
What’s needed is an approach that addresses the reasons why a patient’s manifest and measured anterior corneal astigmatism differ. So, ever striving for LASIK perfection, Dr Lobanoff developed the Phorcides Analytic Engine.
Multiple factors
A decision support software package available for free to any surgeon, Phorcides calculates a topographic ablation solution based on multiple factors. It predicts the effects of combining topographic treatment with anterior corneal cylinder power. The software also considers significant contributions from posterior corneal and lenticular astigmatism. Dr Lobanoff measures the posterior cornea with Scheimpflug imaging.
Developing it required expertise in topographic analysis, leading Dr Lobanoff to contact geographic imaging software producers as potential partners.
“I approached 10 companies, and 9 of the 10 said I was crazy and didn’t want to talk to me. One company said I was crazy, but they would talk to me.”
Getting the right skill set was critical, Dr Lobanoff added. “I finally found a programmer with a background in physics, so he could understand the optical physics we were talking about and the software programming. It took me a while, but once we found that correct individual, we really could make progress and take off.”
The resulting software generates a topographic ablation solution in about 10 seconds, with excellent results.
In a study involving 130 eyes treated for myopia in four centres, 100% achieved 20/20 or better uncorrected, 89%
30 CATARACT & REFRACTIVE EUROTIMES | SEPTEMBER 2023
HOWARD LARKIN REPORTS y = 1.012x -0.0361 R² = 0.9883 -9 -8 -7 -6 -5 -4 -3 -2 -1 0 -9 -8 -7 -6 -5 -4 -3 -2 -1 0 0%0% 0% 10% 20% 30% 40% 50% 60% < -2.00 -2.00 -1.51 % Of Eyes Postoperative 28% 89% 100% 2% 45% 100% 0% 20% 40% 60% 80% 100% 20/12.5 or better20/15 20/20 Cumulative % Of Eyes Cumulative Snellen Visual Acuity (20/x or better) Postop UDVA Preop CDVA Pre #REF! -3.60 -6 -5 -4 -3 -2 -1 0 1 Mean ±SD Spherical Equivalent Refraction (D) Spherical Equivalent Attempted vs Achieved Spherical Equivalent Refractive Astigmatism Uncorrected Distance Visual Acuity Change in Corrected Stability of 0.0%0.0% 0% 10% 20% 30% 40% 50% 60% Loss or More % Of Eyes Undercorrected Overcorrected 130 eyes 3 months postop 3 130 eyes (plano target) 3 months postop 3 3 Achieved Spherical EquivalentRefraction Attempted Spherical Equivalent Refraction (D) 99% 1% 0% 0% 0%0%0% 45% 18% 11% 15% 5% 4% 2% 1% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% 110% ≤ 0.25 0.26 to 0.50 0.51 to 0.75 0.76 to 1.00 1.01 to 1.25 1.26 to 1.50 1.51 to 2.00 2.01 to 3.00 % Of Eyes Refractive Astigmatism (D) Postop Preop 130 eyes 3 months postop ≤0.50 D: 100% ≤1.00 D: 100% mean: -3.60±1.79 D range: -0.50 to -8.25 D A B C D E F
20/15 or better, and 28% 20/12.5 or better. Mean correction was -3.60 ± 1.79 D, ranging from -0.5 to -8.25 D, and 99% had 0.25 D or less residual cylinder.1
Similarly, a Phorcides topo-guided LASIK study by Dr Sloan W Rush saw 58.7% of 92 eyes in 46 patients reached 20/12.5 uncorrected, 98.9% 20/20 monocularly, and 100% 20/16 or better binocularly.2

“Really, some spectacular results,” Dr Lobanoff concluded. Dr Lobanoff presented at the Innovators Session of the 2023 ASCRS annual meeting in San Diego, US.
For citation notes, see page 54.
Mark Lobanoff MD is founder and president of OVO LASIK + LENS, a private clinic; founder and CEO of Phorcides, a LASIK software firm; and CEO of American Corneal Consultants, a research organisation, all based in Minneapolis, Minnesota, US. mlobanoff@gmail.com
31 2023 SEPTEMBER | EUROTIMES -0.0361 0.9883 -9 -8 0%0% 0% 0% 8% 59% 32% 0%0%0%0% 0% 10% 20% 30% 40% 50% 60% < -2.00 -2.00 to -1.51 -1.50 to -1.01 -1.00 to -0.51 -0.50 to -0.14 -0.13 to +0.13 +0.14 to +0.50 +0.51 to +1.00 +1.01 to +1.50 +1.51 to +2.00 > +2.00 % Of Eyes Postoperative Spherical Equivalent Refraction (D) 100% 20/20 better) UDVA CDVA Pre 3 (130) 6 () #REF! 1 (130) -3.60 +0.10 +0.08 -6 -5 -4 -3 -2 -1 0 1 Mean ±SD Spherical Equivalent Refraction (D) Time After Surgery (months) Achieved Spherical Equivalent Refractive Accuracy Change in Corrected Distance Visual Acuity Stability of Spherical EquivalentRefraction 0.0%0.0% 1% 53% 40% 6% 0% 0% 10% 20% 30% 40% 50% 60% Loss 3 or More Loss 2Loss 1No Change Gain 1Gain 2Gain 3 or More % Of Eyes Change in Snellen Lines of CDVA Undercorrected 130 eyes 3 months postop ±0.50 D: 100% ±1.00 D: 100% 130 eyes 3 months postop 2 or more lines lost 0.0% 130 eyes 3 months postop % changed > 0.50 D 1-3 mo = 0% Refraction (D) 2% 1% 2.01 to 3.00 Postop Preop 100% 100% 1.79 D -8.25 D B D F
-0.0361 0.9883 -9 -8 0%0% 0% 0% 8% 59% 32% 0%0%0%0% 0% 10% 20% 30% 40% 50% 60% < -2.00 -2.00 to -1.51 -1.50 to -1.01 -1.00 to -0.51 -0.50 to -0.14 -0.13 to +0.13 +0.14 to +0.50 +0.51 to +1.00 +1.01 to +1.50 +1.51 to +2.00 > +2.00 % Of Eyes Postoperative Spherical Equivalent Refraction (D) 100% 20/20 better) UDVA CDVA Pre 3 (130) 6 () #REF! 1 (130) -3.60 +0.10 +0.08 -6 -5 -4 -3 -2 -1 0 1 Mean ±SD Spherical Equivalent Refraction (D) Time After Surgery (months) Achieved Spherical Equivalent Refractive Accuracy Change in Corrected Distance Visual Acuity Stability of Spherical EquivalentRefraction 0.0%0.0% 1% 53% 40% 6% 0% 0% 10% 20% 30% 40% 50% 60% Loss 3 or More Loss 2Loss 1No Change Gain 1Gain 2Gain 3 or More % Of Eyes Change in Snellen Lines of CDVA Undercorrected 130 eyes 3 months postop ±0.50 D: 100% ±1.00 D: 100% 130 eyes 3 months postop 2 or more lines lost 0.0% 130 eyes 3 months postop % changed > 0.50 D 1-3 mo = 0% Refraction (D) 2% 1% 2.01 to 3.00 Postop Preop 100% 100% 1.79 D -8.25 D B D F -0.0361 0.9883 -9 -8 0%0% 0% 0% 8% 59% 32% 0%0%0%0% 0% 10% 20% 30% 40% 50% 60% < -2.00 -2.00 to -1.51 -1.50 to -1.01 -1.00 to -0.51 -0.50 to -0.14 -0.13 to +0.13 +0.14 to +0.50 +0.51 to +1.00 +1.01 to +1.50 +1.51 to +2.00 > +2.00 % Of Eyes Postoperative Spherical Equivalent Refraction (D) 100% 20/20 better) UDVA CDVA Pre 3 (130) 6 () #REF! 1 (130) -3.60 +0.10 +0.08 -6 -5 -4 -3 -2 -1 0 1 Mean ±SD Spherical Equivalent Refraction (D) Time After Surgery (months) Achieved Spherical Equivalent Refractive Accuracy Change in Corrected Distance Visual Acuity Stability of Spherical EquivalentRefraction 0.0%0.0% 1% 53% 40% 6% 0% 0% 10% 20% 30% 40% 50% 60% Loss 3 or More Loss 2Loss 1No Change Gain 1Gain 2Gain 3 or More % Eyes Change in Snellen Lines of CDVA Undercorrected 130 eyes 3 months postop ±0.50 D: 100% ±1.00 D: 100% 130 eyes 3 months postop 2 or more lines lost 0.0% 130 eyes 3 months postop % changed > 0.50 D 1-3 mo = 0% Refraction (D) 2% 1% 2.01 to 3.00 Postop Preop 100% 100% 1.79 D -8.25 D B D F
Improving Refractive Outcomes After Cataract Surgery

OCT-based parameters and AI increase ELP prediction accuracy.
CHERYL GUTTMAN KRADER REPORTS
Better estimation of the effective lens position (ELP) continues to present a hurdle for achieving more accurate refractive outcomes after cataract surgery. A new method for ELP estimation using geometrical features quantified from preoperative swept-source (SS) OCT images combined with machine learning algorithms shows promise for overcoming this obstacle.
“The main novelty and important aspect of our approach is it includes information on the geometry of the crystalline lens that can now be obtained using SS-OCT for preoperative imaging,” Dr Eduardo Martínez-Enríquez told EuroTimes
“Moving ahead, we are trying to further improve the model’s performance using a larger data set and additional parameters describing lens geometry.”
Conducted at the Flaum Eye Institute, Rochester, New York, US, the project used data from OCT images obtained with the IOLMaster 700 (Zeiss) pre- and postoperatively in 61 eyes of 31 cataract surgery patients. Most eyes were implanted with an AcrySof IOL (54%, Alcon), but others received the Clareon (Alcon) and EnVista (Bausch + Lomb) IOLs.
Custom algorithms performed surface segmentation, distortion correction, and registration to obtain 3D cornea, crystalline lens/IOL, and retina geometry. Four models incorporating different combinations of preoperative geometrical features were tested for ELP predicting capabilities using the
actual postoperative position of the IOL as the ground truth. Parameters in the four models included radius of curvature of the anterior cornea (RAC), standard axial length (AL), IOL model implanted, AL using custom indices of refraction for the different structures of the eye, axial measurements (anterior chamber and vitreous chamber depths; cornea and crystalline lens thickness), and radius of curvature of the anterior and posterior surfaces of the crystalline lens.
One thousand independent experiments were run, and a Gaussian process regression model was trained and evaluated for each experiment using five-fold cross-validation. Model performance was then compared with outcomes using the SRK/T and Haigis formulas.
The mean of absolute estimation error was 256 µm using SRK/T (200 µm using Haigis) and ranged from 119 to 197 µm for each model. The differences compared to SRK/T and Haigis were statistically significant for models including axial measurements and radius of curvature of the crystalline lens surfaces.
Analyses of maximum error across subjects and the number of eyes with an error greater than 200 μm also showed better results using each of the models than the SRK/T and Haigis formulas. Values for maximum error across subjects were 1.30 mm for SRK/T, 904 µm for Haigis, and between 474 and 671 µm for the models. SRK/T use resulted in an error greater than 200 µm in 32 eyes but in only 10 or 11 eyes with two of the four models.
32 EUROTIMES | SEPTEMBER 2023
CATARACT
& REFRACTIVE
The model that displayed the best performance incorporated RAC, IOL type, axial measurements, and radius of curvature of the anterior and posterior surfaces of the crystalline lens.
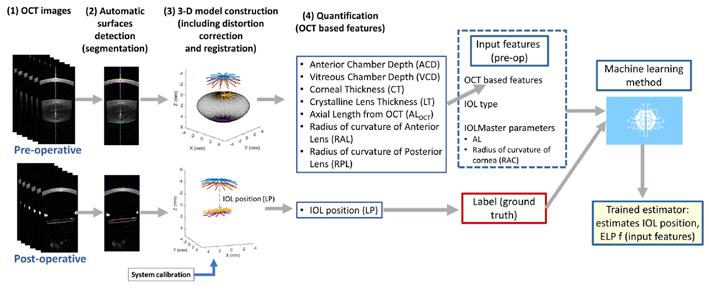
Dr Martínez-Enríquez noted an ELP estimation method is not limited to data acquired with the IOLMaster 700. Rather it could be implemented using values from other OCT devices able to obtain the necessary parameters.
The new GONIO ready ® changes the way of your Glaucoma Surgery
Two-handed MIGS surgeries are now possible for the first time! The OCULUS GONIO ready® seamlessly integrates with the microscope giving surgeons the freedom to utilize both hands during MIGS.
• Single-use for excellent optical quality

• Unique Flex System for maintained contact with the cornea
• More safety for surgeons and patients


Contact the OCULUS team or your local distributor for more information and a no-obligation trial.
Satellite Symposium at ESCRS!
Sunday, 10 September, 9:30 – 10:30 h, Strauss 1 Pentacam ® AXL Wave / Corvis ® ST / Myopia Master ®
Speakers: Huy Tran, Vietnam| Renato Ambrósio, Brazil Riccardo Vinciguerra, Italy | Gerd Auffarth, Germany
33 2023 SEPTEMBER | EUROTIMES
oculussurgical com /gonioready +49 6 41 2005-298 855-SDI-BIOM (Toll Free, US Only) The availability of products and features may vary by country. OCULUS reserves the right to change product specifications and design.
Dr Martínez-Enríquez presented at 2023 ARVO in New Orleans, Louisiana, US.
Eduardo Martínez-Enríquez PhD is a researcher with the Spanish National Research Council, Madrid, Spain. eduardo.martinez@io.cfmac.csic.es
EVO ICL for Low Myopia
Reversible procedure may be suitable corneal surgery alternative for some patients.
Offering excellent safety, visual outcomes, and a design that eliminates the need for a peripheral iridotomy, the EVO/EVO+ Visian ICL (implantable collamer lens; Staar Surgical) may be a viable option to correct low myopia in some patients, according to Dr Erik L Mertens.
Dr Mertens defined low myopia as a spherical equivalent refraction of -0.5 D to -6.0 D when ocular accommodation is relaxed. In Europe, the EVO/EVO+ ICL is indicated for myo pia from -0.5 D to -20.0 D at the spectacle plane, with toric cor rection available up to 6.0 D cylinder in phakic patients aged 21 to 60 years. Minimum indicated anterior chamber depth (ACD) is 2.8 mm in Europe and 3.0 mm in the US, which also limits lens refractive power to -3.0 D to -15.0 D with 4.0 D or less cylinder in patients aged 21 to 45 years. An open angle is also needed.
Preventing endophthalmitis



Because the EVO is implanted intraocularly, endophthalmitis is a risk. Dr Mertens prevents it by applying povidone-iodine before and after surgery and injecting intracameral cefuroxime.
“I’ve never seen a case of endophthalmitis so far.” Citing a 2009 study that found three cases of endophthalmitis in 19,000 ICL implantations, he noted the two cases with follow-up recovered completely.1
“Even if you have an endophthalmitis [case], it doesn’t have to be a catastrophe in ICL surgery.”
Sizing and predicting lens vault
Accurately predicting ICL vault is essential to choose a size that maintains sufficient clearance to prevent cataract formation or interference with the corneal endothelium, iris, or angle. Dr Mertens presented results from the Least Absolute Shrinkage and Selection Operator (LASSO) vault prediction formulas he helped develop with researchers at the University of Leuven, Belgium. Whether using OCT or IOLMaster data or both, the LASSO formulas more accurately predicted lens vault in White patients, including those with low and moderate myopia, than the manufacturer’s nomogram or the Nakamura 1 or 2 formulas commonly used to size ICLs.2
Predictability and safety
EVO ICL refractive predictability is very high, Dr Mertens said. In 306 cases followed for at least three years that he implanted, achieved refractions tracked predicted refractions very closely, yielding an R2 value of 0.9992.
“The most important factor is you have to do a perfect preoperative refraction,” he said, adding results in published studies are similar.
Safety is also high. A review of studies including 4,196 eyes followed for up to five years found just one case of pupillary
block due to retained viscoelastic and no cases of cataract formation or pigmentary dispersion.3
In addition, the lens carries no risk of ectasia, making it a great option for thin corneas, and since the EVO ICL is removable, it leaves all surgical options open for the future.
“The EVO ICL is a valuable option for all myopes with adequate anterior chamber depth,” Dr Mertens concluded.

Dr Mertens presented at the Refractive Surgery Subspecialty Day of the 2023 ASCRS annual meeting in San Diego, US.
For citation notes, see page 55.
Erik L Mertens MD, FEBO, FWCRS, PCEO is founder, medical director, and ophthalmic surgeon at Medipolis,
Antwerp, Belgium. e.mertens@medipolis.be
34 CATARACT & REFRACTIVE EUROTIMES | SEPTEMBER 2023
HOWARD LARKIN REPORTS Internal use LASSO Cumulative Predictive Accuracy 20% 30% 40% 10% Cumulative Predictive Accuracy Internal use 90% 100% 80% 20% 30% 40% 50% 60% 70% 10% ±300µm ±200µm ±100µm 68% 62% 57% 92% 73% 73% 100% 81% 78% LASSO (all features) NK2 OCOS Cumulative Predictive Accuracy Internal use Predictability-Efficacy y = 1.0042x + 0.0131 R² = 0.9992 -16 -14 -12 -10 -8 -6 -4 -2 0 2 -16 -11 -6 -1 Personal unpublished data 306 eyes F-U > 3 years

35 2023 SEPTEMBER | EUROTIMES Educational Resources Advanced FEBOS-CR Exam/Diploma (Cataract and Refractive Surgery) ESCRS iLearn • ESCRS Research Portals • Important Publications ESCRS EuroTimes Podcasts • ESCRS on Demand • JCRS Online Case Reports The Video Journal of Cataract, Refractive, and Glaucoma Surgery escrs.org/education/educational-resources
Femto-LASIK Sets High Bar for Myopic Correction
Debate continues over relative merits of femto-LASIK and SMILE. DERMOT
Despite the growing popularity of lenticule extraction procedures such as SMILE in recent years, femtosecond LASIK (FS-LASIK) is still considered the gold standard for myopia correction in normal corneas, according to Dr Miguel A Teus.

“We now have more than 20 years of experience with FS-LASIK, with its safety and efficacy well established by numerous studies in the scientific literature,” he said. “SMILE is also a very good procedure, with similar safety and refractive outcomes to FS-LASIK, and it may be particularly suitable for young patients with moderate myopia, those with risk of ocular trauma and who accept a slower visual recovery and a slightly lower uncorrected visual acuity.”
In a broad overview of the current options for laser vision correction, Dr Teus said surface ablation still has a role in the refractive surgeon’s arsenal.
“Surface ablation or PRK is still the technique of choice in thin corneas, asymmetric topography, epithelial dystrophy, and low myopia,” he said.
Using the femtosecond laser for flap creation further improved LASIK outcomes compared to those achieved with a mechanical microkeratome.
“The femtosecond laser obtains a planar, thinner, and more predictable flap than the meniscus-shaped flap obtained with a mechanical microkeratome,” Dr Teus explained. “The advantages are less biomechanical impact, lower incidence of intraoperative complications, and more flap adherence.”
The scientific literature also reflects this, he added, with several meta-analyses showing FS-LASIK provides fast visual recovery, similar efficacy and safety, better predictability, and lower induction of higher-order aberrations than MK-LASIK for myopia correction.
36 EUROTIMES | SEPTEMBER 2023
MCGRATH REPORTS
CATARACT & REFRACTIVE
Lenticule extraction
For lenticule extraction, most published studies pertain to SMILE procedures using the VisuMax platform (Carl Zeiss Meditec).
“SMILE benefits include avoidance of flap-related complications, theoretically fewer dry eye symptoms, and improved biomechanical stability,” he said. “The downsides include a steeper learning curve, potential complications related to lenticule dissection and removal, increased risk of treatment decentration, delayed visual recovery, and limited
less corneal nerve fibre and branch densities, less nerve fibre length, and significantly more nerves with sprouting than SMILE eyes after 4 years postoperatively.2 However, researchers still observed nerve regeneration activity after 2.7 years for both SMILE and LASIK, and the sub-basal nerve plexus had not returned to a normal level after 5.5 years with both techniques.
For corneal sensitivity, SMILE performed better than LASIK at 1 and 3 months but returned to baseline values in both groups at 12 months.3 Another study showed similar OSDI scores with FS-LASIK and SMILE during the follow-up period.4
“No eye had severe OSDI scores. The patient-reported dry eye symptoms improved after both FS-LASIK and SMILE procedures, so SMILE does not seem significantly better for dry eye prevention,” he said.
Biomechanical stability
SMILE preserves more anterior corneal stromal fibres in biomechanical stability—believed to have the greatest tensile strength in normal corneas.
“Some studies have shown a lower corneal biomechanical impact after SMILE, but others have found no significant differences between SMILE and FS-LASIK,” Dr Teus said. “The biomechanical advantages of SMILE seem modest in normal corneas.”
He noted a reported incidence of ectasia of 0.15% after SMILE from a cohort of 7,024 eyes with 12 months follow-up, whereas FS-LASIK reported prevalence rates between 0.02% and 0.6%.5
“The main risk factor is abnormal preoperative topography,” he said. “There are the same exclusion criteria for LASIK and SMILE, so SMILE is not the solution if the eye is a risk for ectasia with LASIK.”
For visual rehabilitation, SMILE has slower visual recovery than FS-LASIK at 1 and 3 months but no significant differences at 6 or 12 months postoperatively.
“This is perhaps due to higher corneal optical density with SMILE in the early postoperative period due to higher surgical manipulation and trauma,” he said.
Although SMILE has demonstrated good efficacy and safety for low myopia, Dr Teus warned the surgery could be more challenging.

“The very thin lenticule required for low myopia correction may suffer from retained fragments during removal. We, therefore, need to enlarge the optical zone to 7 mm and set a thicker lenticule thickness than needed for the refractive correction, meaning more corneal tissue is removed for these low myopes compared to excimer laser surgeries.”
retreatment options.”
Although dry eye has often been touted as a theoretical advantage of SMILE over FS-LASIK, Dr Teus said that the evidence is not so clear cut.
A 2022 meta-analysis showed SMILE had lower corneal nerve damage and better reinnervation within 3 months postoperatively.1 Another study found FS-LASIK eyes had
For citation notes, see page 55.
37 2023 SEPTEMBER | EUROTIMES
Dr Teus presented at the 2023 ESCRS Winter Meeting in Vilamoura, Portugal.
Miguel A Teus MD, PhD is Professor of Ophthalmology at the Department of Surgery, Medical, and Social Sciences, University of Alcalá, Madrid, Spain. miguel.teus@uah.es
Femtosecond LASIK (FS-LASIK) is still considered the gold standard for myopia correction in normal corneas.
Functional Vision with Monofocal-plus IOL



Improving intermediate-range vision may improve patients’ lives.
HOWARD LARKIN REPORTS
On average, presbyopic patients spend more than twice as much time involved in activities requiring near and intermediate vision than distance-vision activities and in mesopic conditions 34% of the time, according to a study by Professor Filomena Ribeiro and colleagues.1 An ESCRS clinical survey also shows these patients are most likely to complain about the lack of intermediate-range vision after receiving presbyopia-correcting intraocular lenses (PCIOLs).2
Because they provide good intermediate vision with minimal loss of contrast sensitivity, monofocal-plus may help solve the problem, Prof Ribeiro said. But before choosing a presbyopiacorrecting IOL, she emphasised assessing patients’ daily visual demands.
To evaluate the clinical outcomes of pa2ents who underwent cataract surgery with the implanta2on of a monofocal IOL designed to improve both distance and intermediate vision (TECNIS EyhanceTM, J&J Vision)
Cataract pa'ents without other pathology
To evaluate the clinical outcomes of pa2ents who underwent cataract surgery with the implanta2on of a monofocal IOL designed to improve both distance and intermediate vision (TECNIS EyhanceTM, J&J Vision)

Follow-up = 4 weeks
visual acui'es for distance, intermediate and near, defocus curve, contrast sensi'vity and pho'c phenomena
Cataract pa'ents without other pathology

Follow-up = 4 weeks phenomena
Characterization of Daily Visual Habits of Cataract Refractive Surgery
Characterisation of Daily Visual Habits of Cataract Refractive Surgery Candidates
Characterization of Daily Visual Refractive Surgery Candidates
Characterization of Daily Visual Habits of Cataract Refractive Surgery Candidates
“The impact of intermediate vision on quality of life has not only personal consequences but social and economic [ones].”
Changing designs
The need for better intermediate vision has prompted a shift in light-splitting in trifocal PCIOLs, away from sharp peaks at distance and near and towards more light at intermediate range. Extended depth of focus (EDOF) PCIOLs alone provide better intermediate vision but give less near assistance, though more than a monofocal IOL.
Combining a trifocal with an EDOF in the fellow eye is another way surgeons have tried to improve intermediate focus while maintaining a full range of continuous vision, Prof
TECNIS Eyhance™: Our experience
38 CATARACT & REFRACTIVE EUROTIMES | SEPTEMBER 2023
Filomena Ribeiro| 2022 Hospital da Luz RESULTS ! Mean percentage of -me with digital screens was 18.98% (SD: 10.48; median: 19.00% Range:2% to 48%). ! Mean percentages of time dedicated to distance, intermediate and near vision:
Candidates ! Mean percentages of -me performing ac-vi-es under photopic, mesopic and scotopic condi-ons: Filomena Ribeiro| 2022 RESULTS ! Mean percentage of -me with digital screens was 18.98% (SD: 10.48; median: ! Mean percentages of time dedicated to distance, intermediate and near vision:
! Mean percentages under photopic
HOSPITAL DA LUZ Filomena Ribeiro MD, PhD,FEBO|ESCRS Amesterdam 2020
Functional ability must be the main outcome of cataract surgery and the main objective of the intervention.
HOSPITAL DA LUZ Filomena Ribeiro MD, PhD,FEBO|ESCRS Amesterdam 2020
Our experience 42.5% ±14.96 27.3% ±11.93 30.2% ±9.36 29.28% ±17.03 37.08% ±23.20 33.65% ±13.84
TECNIS Eyhance™:
RESULTS Distance Intermediate Near Photopic Mesopic Scotopic Mean percentages of time dedicated to distance, intermediate, and near vision: Mean percentages of time performing activities under photopic, mesopic, and scotopic conditions: Filomena Ribeiro| 2022 Hospital da Luz RESULTS ! Mean percentage of -me with digital screens was 18.98% (SD: 10.48; median: 19.00% Range:2% to 48%). ! Mean percentages of time dedicated to distance, intermediate and near vision:
! Mean percentages of -me performing ac-vi-es under photopic, mesopic and scotopic condi-ons: Mean percentage of time with digital screens was 18.98% (SD: 10.48; median: 19.00% Range: 2% to 48%).
TECNIS Eyhance™: Our experience
Ribeiro said. Both multifocal and EDOF PCIOLs provide less contrast sensitivity and more photic phenomena, including glare and halos, than monofocals.
Monofocal-plus lenses are the latest entrant. They use changes in curvature or spherical aberration to extend the depth of focus slightly, Prof Ribeiro said. In her experience, the lenses are more tolerant of refractive error and extend intermediate vision to about 2.0 D of defocus above 20/40.
Restoring function
Contrast sensitivity and photic phenomena for monofocal-plus IOLs are similar to a plain monofocal IOL. An addition of about one line of intermediate vision means patients report much less difficulty seeing prices and using computers than with monofocal IOLs, she added.
A meta-analysis of monofocal-plus studies concluded they effectively improved unaided intermediate vision with similar distance vision to conventional monofocal IOLs without degrading optical quality.3
“Functional ability must be the main outcome of cataract surgery and the main objective of the intervention,” Prof Ribeiro said.
Monofocal-plus lenses can improve it, and transitioning is easy, requiring no additional chair time, she said. There is no learning curve, and, if anything, there is more tolerance for residual refractive error, making them a good option in cases where biometry or IOL power—or pathology— are in doubt.
Highlighting the potential for considering monofocal-plus IOLs as the standard of care in the future, Prof Ribeiro stressed the necessity of further studies comparing their performance with conventional monofocal IOLs.
Prof Ribeiro presented at the 2023 ASCRS annual meeting in San Diego, US.
For citation notes, see page 55.
39 2023 SEPTEMBER | EUROTIMES 55,00 50,00 45,00 40,00 35,00 30,00 25,00 20,00 15,00 10,00 5,00 0,00 1,5 cpd 18 cpd C ontrast Sens i t i v i ty 3,0 cpd 6,0 cpd 12,0 cpd Spatial Frequency (cycles per degree) Tecnis 1 (n=30) Eyhance (n=30) HOSPITAL DA LUZ Filomena Ribeiro,MD,PhD,FEBO Mesopic CSF with glare
experience 100 90 80 70 60 50 40 30 20 10 0 N on e Mild M o d e r at e S e v e re N on e Mild M o d e r at e S e v e re N on e Mild M o d e r at e S e v e re % o f patients Tecnis
HOSPITAL DA LUZ Filomena Ribeiro,MD,PhD,FEBO Halos Starburst Glare
TECNIS Eyhance™: Our
1 (n=30) Eyhance (n=30)
Filomena Ribeiro MD, PhD, FEBO is head of ophthalmology at Hospital da Luz, Lisbon, Portugal, associate editor of the Journal of Cataract and Refractive Surgery , and president-elect of the ESCRS. filomenajribeiro@gmail.com
António Champalimaud Vision Award Winners
CHERYL GUTTMAN KRADER REPORTS
Dr Claes H Dohlman and Dr Gerrit RJ Melles were celebrated as recipients of the 2022 António Champalimaud Vision Award during a special session at ARVO 2023.

In opening remarks, Leonor Beleza said the Champalimaud Foundation was honoured and proud to recognise the two European physician-scientists whose work embodied the spirit of the United Nations Vision for Everyone resolution and opened new paths for treating those affected by corneal disease worldwide, giving sight back to millions of people.
New concepts on the corneal endothelium
In his award lecture, Dr Melles reflected on the question, “How would nature see our corneal triumphs?”.1 He introduced new concepts on corneal physiology and Fuchs’ endothelial corneal dystrophy that he developed, recognising discrepancies between conventional teachings and clinical observation.
“More and more, I have come to believe the literature and textbooks do not agree with clinical observation,” Dr Melles said. “Clinical observation is something you cannot fake, and in the end, it is the truth.”
Dr Melles began his talk by challenging attendees to look at the cornea in a slightly different way after hearing his presentation. He discussed a new concept to describe corneal endothelial flow mechanisms involving a vertically oriented static flow and a horizontal dynamic flow perfusing the endothelium from limbus to limbus.
The artificial cornea and other accomplishments
Dr Dohlman, who turned 100 years old in September 2022, appeared in a video presentation to summarise 50 years of translational work on the Boston Keratoprosthesis (B-KPro) artificial cornea. He recognised the award he was receiving was based on work done by his teams at Massachusetts Eye and Ear Hospital, Schepens Research Institute, and Harvard University in Boston.
The award recipient described the B-KPro as “a relatively new procedure” when considered in the history of attempts to create an artificial cornea. Its development began in the 1960s, and to date, about 20,000 B-KPros have been implanted worldwide.
After outlining selected design features and their value for improving outcomes, Dr Dohlman noted that certain complications remain a limiting factor in providing patients with good vision.
He also outlined evidence to support the idea Fuchs’ dystrophy is not an endothelial disease but rather a corneal glaucoma characterised by an exceptionally high imbibition pressure level. Dr Melles suggested the name may be a “framing error” that implies the condition is “an endothelial problem.” Regarding Fuchs’ dystrophy as a corneal glaucoma may not only be the correct perspective, he said, but understanding the mechanism underlying the corneal disorder may also be the key to understanding the mechanism of primary open-angle glaucoma.
“The long-term sensitivity to secondary glaucoma, particularly in connection to any severe injury or corneal surgery, is concerning. Secondary glaucoma is, of course, irreversible,” he said.
He outlined how animal experiments led to the idea glaucoma development was mediated by intraocular inflammation with its associated increases in inflammatory cytokines, especially tumour necrosis factor alpha (TNFα). Preclinical research from his team also showed treatment with monoclonal antibodies directed against TNFα protected against retinal ganglion cell death, a major hallmark of glaucoma.
CORNEA 40 EUROTIMES | SEPTEMBER 2023
Drs Dohlman and Melles recognised for contributions to research and treatment of corneal disease.
The sensitivity to secondary glaucoma, particularly in connection to any severe injury or corneal surgery, is concerning.
Dr Dohlman further posited rapid inflammation inside the eye after trauma and surgery has been underestimated as a major factor in long-term glaucoma development. Monoclonal antibodies should have great promise in preventing complications after surgery and trauma, which is no longer a minor matter.

Dr Reza Dana concluded the session with a tribute to Dr Dohlman.
Listing just some of Dr Dohlman’s accomplishments, Dr Dana recognised him for establishing the first cornea subspecialty clinic and training programme founded in science. He also highlighted how the environment created by Dr Dohlman and the generations of scientists he assembled led to major innovations that transformed ophthalmology.
Dr Dana went on to enumerate some of the contributions, including understanding the pathophysiology and management of herpetic keratitis; understanding the concept of stem cells for epithelial healing; the first clinical application in any tissue of stem cell transplantation; viscoelastic use in ocular surgery; cultivation of endothelial cells leading to cutting-edge technological alternatives to conventional transplants; development of drugs for ocular allergy; new contact lens technologies; elucidation of the pathophysiology of dry eye and the development of new treatments for dry eye; development of drug-eluting contact lenses and new biomaterials; expansion of corneal
epithelial cells for clinical applications; new surgical techniques for refractive surgery; and development of novel treatments for reversing corneal scarring.
“Let us ask, ‘Where would we be today without these contributions?’” Dr Dana said.
ARVO 2023 took place in New Orleans, Louisiana, US.
For citation notes, see page 55.
Leonor Beleza is president of the board of directors of the Champalimaud Foundation.
Claes Dohlman MD, PhD is Professor of Ophthalmology, Emeritus, Harvard Medical School, Boston, Massachusetts, US. claes_dohlman@meei.harvard.edu
Gerrit RJ Melles MD, PhD is Director of the Netherlands Institute for Innovative Ocular Surgery, Rotterdam, Netherlands. melles@niios.nl
Reza Dana MD, MSc, MPH is Claes H Dohlman Professor of Ophthalmology, Harvard Medical School, Boston, Massachusetts, US. reza_dana@meei.harvard.edu
41 2023 SEPTEMBER | EUROTIMES
JOIN the leading community and trusted source for SCIENCE, EDUCATION & PROFESSIONAL DEVELOPMENT in the fields of cataract and refractive surgery. learn more about membership at escrs.org
Healing Persistent Corneal Epithelial Defects

Novel antisense oligonucleotide shows promise.
CHERYL GUTTMAN KRADER REPORTS
Lufepirsen ophthalmic gel (Nexagon ®, Amber Ophthalmics) showed promising efficacy and safety in a phase 2 study treating persistent corneal epithelial defects (PCEDs), a rare disease resulting from ocular chemical and/or thermal injury, according to Dr Dipak Panigrahi.
The treatment is an unmodified antisense oligonucleotide thought to address the underlying pathogenic inflammatory mechanisms associated with PCED.
“Inflammation is a major contributor to the PCED disease process, subverting homeostatic mechanisms needed for healing and thus favouring rapid progression of advanced corneal defects towards corneal ulceration, corneal melt, and ultimately corneal transplant,” he told EuroTimes
“Lufepirsen is thought to quell inflammation by downregulating pathogenically elevated connexin 43 protein translation, thereby enabling the cornea to regain its homeostatic balance that favour the ability to heal. We restore the eye’s ability to heal itself by minimising inflammasome activation.”
The phase 2 study, conducted in the United States and India, planned to enrol 108 subjects but stopped after an
interim analysis of data from the first 35 patients revealed a strong efficacy signal for subjects suffering from PCED secondary to chemical and/or thermal injuries. The data also corroborated previous findings on lufepirsen safety. The 35 participants included 22 adults and 13 paediatric patients (7 to 75 years) with a PCED refractory to standard of care, mean corneal defects measuring 52.5 mm2 on average, and Dua grades ranging from I to VI, with the majority (54%) grade IV or greater.
Participants were randomised 1:1:1 to lufepirsen ophthalmic gel 0.06%, lufepirsen ophthalmic gel 0.006%, or vehicle
CORNEA 42 EUROTIMES | SEPTEMBER 2023
We restore the eye’s ability to heal itself by minimising inflammasome activation.
Representative patient for the Nexagon trial. The photo demonstrates corneal epithelial healing (of what was a non-healing persistent epithelial defect), as demonstrated by fluorescein staining under slit lamp illumination.
administered under a bandage contact lens on days 1, 2, and 14. The primary efficacy endpoint assessed corneal epithelial recovery, defined as complete corneal re-epithelialisation within the treatment period and maintained for at least 28 continuous days. The efficacy endpoint was achieved in 66.7% of subjects treated with both lufepirsen concentrations compared to just 27.3% in the control group. Greater improvement in visual acuity was also observed in the lufepirsen groups compared to controls, although these results did not achieve statistical significance.
participants are representative of patients seen in the clinic with PCED related to chemical and/or thermal injury,” Dr Panigrahi said. “Our investigators were encouraged by the observed treatment benefits, especially considering the di verse demographics and advanced stages of PCED lesions in the study subjects. They did not expect to see the kind of responses they witnessed. We are excited to broaden our study population and further establish lufepirsen’s value in patients with this rare disease, an area of tremendous unmet medical need.”
Lufepirsen gel was generally well-tolerated, with 19 of 22 subjects experiencing mild or moderate adverse events (AEs). Further, investigators considered 21 of 33 subjects’ AEs unrelated to the study drug.
Further development

A phase 2/3 trial is now underway to investigate the firstin-class medication for healing PCEDs of broader aetiologies. Conducted at centres in multiple countries, the study will compare the same two concentrations of lufepirsen gel against the vehicle but enrol patients with PCED of any aetiology, excluding those with infectious or postsurgical causes.
ESCRS Academies
Committee representatives of ESCRS organise and present sessions at meetings organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies promoting and sharing benefits across both memberships.
escrs.org/education/academies/
Dr Panigrahi presented at ARVO 2023 in New Orleans, Louisiana, US.
Dipak Panigrahi MD is chief medical officer, Amber Ophthalmics, San Diego, US. dpanigrahi@amberophthalmics.com
Intraocular Travoprost Implant
Sustained-release device provides safe and durable IOP control.
 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS
Anew drug-eluting implant (iDose TR®, Glaukos) has shown promising results in ongoing Phase 3 pivotal trials.
The microinvasive intraocular titanium implant elutes a proprietary formulation of travoprost. Its IOP-lowering benefit was comparable to twice-daily topical treatment with timolol 0.5%. The novel implant also demonstrated favourable safety and tolerability profiles, reported Dr L Jay Katz.
“The intraocular implant, which continuously releases minute amounts of travoprost and delivers a therapeutic level to the target site over an extended period, addresses the side effect and compliance issues associated with topical drops,” he told EuroTimes . “Because of its efficacy, safety, and benefits, we are very optimistic the travoprost intraocular implant could open a whole new era in the treatment of glaucoma.”
Two parallel pivotal trials randomised 1,150 patients equally into three treatment groups to receive one of two iDose TR implant models (slow- and fast-eluting) or topical timolol. In February 2023, Glaukos filed a New Drug Application for iDose TR with the US Food and Drug Administration.
Patients enrolled in the pivotal studies had open-angle glaucoma or ocular hypertension. A majority of patients in all treatment groups were using one or two topical IOP-lowering medications at the time of screening.
The primary efficacy IOP endpoint changed from baseline to day 10, week 6, and month 3 in IOP measured at 8:00 a.m. and 10:00 a.m. Across both studies, mean IOP reduction ranged from 6.6 to 8.5 mmHg in the slow-eluting iDose TR arms and 6.5 to 7.7 mmHg in the timolol control arm. The trials plan to follow patients for 36 months. So far, data analysed from visits completed after 12 months showed 93% of slow-release iDose TR subjects remained well-controlled on the same or fewer IOP-lowering topical medications compared to screening after a single administration of iDose TR, versus 67% of timolol control subjects. A majority of patients in the iDose TR arm, 81%, were off all topical medications.
Iritis was the most common ocular adverse event in the iDose TR arms (5.5% and 6.2%). Rates of ocular or conjunctival hyperaemia ranged from 1.1% to 2.6%. Mean endothelial cell density was stable in the iDose TR arms through month 12, and there were no cases of clinically significant endothelial cell loss, periorbital fat atrophy, iris discolouration, or serious corneal adverse events.
“The side effect profile of the iDose TR implant compared very favourably with topical timolol,” Dr Katz said. “Importantly, hyperaemia, periorbital fat atrophy, and eyelid and iris discolouration that are common with topical prostaglandin analogue treatment were seen at much lower rates or not at all.”
The efficacy and durability of the implant’s IOP-lowering effect are consistent with findings of another study conducted to determine the in vivo drug elution rate, aqueous humour concentrations of travoprost-free acid (the active agent), and residual travoprost remaining in the device over time. The study included 210 patients with open-angle glaucoma or ocular hypertension who received a slow-eluting implant. Participants were divided into cohorts to undergo device explantation, aqueous humour sampling, and new implant insertion at prespecified follow-up times between 3 and 24 months.
Aqueous humour analyses showed the concentration of travoprost-free acid reached a steady state by 3 months at a level higher than needed for IOP-lowering efficacy, was maintained at 12 months, and was adequate to elicit IOP lowering based on comparison with data reported for travoprost delivered topically and with an intracameral implant. Explant analysis showed they still contained about 50% of their initial travoprost load after 12 months in patients’ eyes.
“The finding on the remaining drug gives us a strong indication the IOP-lowering effect of the slow-eluting implant might be durable for up to 24 months at least,” Dr Gabriella Szekely said.
The study also provides insight into the safety/tolerability of the explantation/exchange procedure, with very encouraging findings, she said. So far, a single case of hyphaema that resolved within seven days was the only test article-related adverse event observed.
44 GLAUCOMA EUROTIMES | SEPTEMBER 2023
Surgical technique
The implant is placed in an ab interno procedure performed under topical anaesthesia and using a gonioprism to visualise the nasal angle. It is delivered with a dedicated instrument through a temporal clear cornea incision after filling the anterior chamber with a cohesive ophthalmic viscosurgical device and placed into the back wall of Schlemm’s canal. It features an anchor at its tip that securely fixes the device into the scleral wall.
“The implantation procedure is similar in some respects to some MIGS procedures, but the travoprost implant placement is done with a ‘straight in’ motion and does not require the type of multidirectional manipulations needed for some MIGS devices,” said Dr Katz.
“Our positive safety data bear out the idea the scleral anchor is a key element of the implant’s design. Preventing the device from moving around inside the eye is important for avoiding inflammation or corneal endothelial contact.”
The study update was presented at ARVO 2023 in New Orleans, Louisiana, US.
L Jay Katz MD is Director Emeritus Glaucoma Service Wills Eye Hospital and Professor of Ophthalmology, Sidney Kimmel Medical College, Philadelphia, Pennsylvania, US, and Chief Medical Officer, Glaukos, Aliso Viejo, California, US. jkatz@glaukos.com

Gabriella Szekely PhD is Vice President, Research & Development, Glaukos, Aliso Viejo, California, US. gszekely@glaukos.com
apEye –
Let‘s talk about apEye and CASIA2 at the ESCRS:
Booth B506
Revolutionising eye prostheses with CASIA2




At ESCRS we’ll introduce apEye: A 3D-printed artificial eye prosthesis that owes its unique true colour and the natural appearance of the iris to high-resolution scans from the TOMEY Cornea/Anterior Segment OCT CASIA2.
Learn all about the ground-breaking Light Source Technology in CASIA2 and apEye –products that will revolutionise the market.
45 2023 SEPTEMBER | EUROTIMES
CASIA2 at tomey.de
Managing Refractory Scleritis
Case series supports biologic therapy with adalimumab.
Subcutaneous adalimumab (Humira, AbbVie) can be an effective therapeutic option for patients with non-infectious scleritis refractory to conventional therapy, according to a recent retrospective analysis.
The review included 15 adults treated at Moorfields Eye Hospital, London, UK. All patients were on prednisone and had tried a variety of immunosuppressants but were unable to maintain quiescence if prednisone was tapered to <5 mg per day.
Analyses of data from six months of follow-up showed adalimumab had a steroid-sparing benefit. Researchers saw a statistically significant reduction in the mean daily prednisone dose from 21.0 mg to 6.6 mg. The proportion of patients maintained on ≤10 mg of prednisone per day increased significantly from 46.7% to 93.3%, while those maintained on ≤5 mg prednisone per day increased from 26.7% to 53.3%.

Endpoint analyses for disease control showed vision improved in 27% of patients and was stable in the remaining patients. Four patients experienced scleritic flares, which translated into a reactivation rate of 0.62 flare-ups per patient year.
“In theory, adalimumab is an attractive option for refractory scleritis, but its use is limited by an absence of data from randomised controlled trials and cost,” said Dr Ian Yeung. “We were fortunate to have experience using adalimumab in a reasonably sized cohort that allowed us to assess its outcomes.
“Older guidelines on managing inflammatory eye diseases recommend the long-term maintenance dose of prednisone not exceed 10 mg per day, and more recent guidance advises an even lower long-term target, ideally 5 mg per day or less. We hope the findings of our review add valuable data that will encourage more clinicians to consider using adalimumab as an effective steroid-sparing treatment for their patients with refractory scleritis,” he told EuroTimes.
Adalimumab is a fully humanized anti-tumour necrosis factor-α monoclonal antibody. The biologic medication used at Moorfields is an adalimumab biosimilar. It is administered at home by subcutaneous injection, beginning with an 80 mg loading dose at week zero, then 40 mg every two weeks from week one onwards. Injection frequency was increased to weekly after 3.5 months in one patient whose scleritis remained active.
Treatment with adalimumab had an acceptable safety profile. Adverse events recorded in four patients included oral and genital thrush, pain on injection, headache, nausea, and a single episode of bleeding gums.
“One of the patients who experienced a flare was the same person who developed thrush, and the flare occurred after adalimumab was withheld for approximately 6 weeks. Three of the four flares (i.e., 75%) occurred 6 to 10 weeks after adalimumab initiation,” Dr Yeung reported.
93.3%
The proportion of patients maintained on ≤10 mg of prednisone per day increased significantly from 46.7% to 93.3%.
53.3%
Those maintained on ≤5 mg prednisone per day increased from 26.7% to 53.3%.
A few patients did not have their scleritis fully controlled or their prednisone tapered to <5 mg per day while on adalimumab and thus were switched to a different biologic. The others remained on adalimumab.
“Soon we will have a two-year follow-up for the patients who continued adalimumab and plan to conduct an audit of their outcomes for presentation at a future meeting,” he said. “We also plan to conduct an audit of the patients who switched to a different biologic.”
RETINA 46 EUROTIMES | SEPTEMBER 2023
Dr Yeung presented at ARVO 2023 in New Orleans, Louisiana, US.
Ian Yeung MD is an associate specialist in the medical retina and uveitis service at Moorfields Eye Hospital, London, UK. i.yeung@nhs.net
CHERYL GUTTMAN KRADER REPORTS
ESCRS Leadership, Business & Innovation
ESCRS LEADERSHIP & BUSINESS INNOVATION MASTERCLASS,
SUNDAY, 10 SEPTEMBER. STRAUSS 3, 08.30–18.00
The Fine Art of Juggling
Ophthalmologists must be master jugglers. Most of these skills are learned on the job with no formal training. The expectation is they will manage them all and do them well. In this interactive and didactic workshop, ESCRS Consultant Kristine Morrill and an expert panel will cover topics including Finding the Hidden CEO, Managing Money, and Encouraging Creativity.
08.30–08.40 Welcome
Paul Rosen, Chair ESCRS Leadership and Business Innovation Committee, Consultant Ophthalmic Surgeon, Oxford Eye Hospital, Oxford University Hospital Foundation Trust, UK; and



Kristine Morrill, ESCRS Consultant and Founder and President, Medevise.

08.40–10.00 The Hidden CEO
Omid Kermani, Co-Founder Augenklinik am Neumarkt, Germany; and



Daniel Kook, Co-founder, Prof Kook & Partner, Germany.
10.00–10.30 Discussion/coffee break
10.30–11.30 Money Management—Balancing Profitability with Patient Care
John Bolger, London.
11.30–11.45 Discussion
11.45–12.45 HR: Mistakes We’ve Made and How We Learned from Them Paul Rosen and Kris Morrill
12.45–13.30 Lunch Break
13.30–14.30 Panel: Ophthalmologist as Inventor— Taking Something from Idea to Reality
Florent Constantini, Founder, GlassPop, France.
Nick Pennington, Associate Medical Director, Ufonia, UK.
Robert McClaren, UK, Ophthalmologist and Founder, Nightstar/Biogen.


14.30–14.45 Discussion
14.45–15.30 Understanding the EU Regulatory Environment
Michael Mrochen, Founder and CEO, IROC Science, Switzerland.
15.30–16.00 Discussion/coffee break
16.00–17.00 Panel: Embracing Your Creative Side
Damien Gatinel, Chief, Anterior Segment, France.
Detlef Holland, Co-Founder, Augenzentrum One, Germany.
Florian Auerbach, Founder, Private Practice, Germany.


17.00–17.30: Discussion/Wrap Up Faculty, Paul Rosen, and Kris Morrill

47 2023 SEPTEMBER | EUROTIMES
ESCRS LAUNCHES LEADERSHIP AND BUSINESS INNOVATION WEEKENDS

Frankfurt programme will feature interactive education on leadership and finance.
The ESCRS Leadership and Business Innovation weekend programme returns—this year, in Frankfurt, Germany, on Saturday and Sunday, 7 and 8 October 2023. The twoday programme will focus on Leadership and Finance, delivered by keynote ESCRS speakers and leading business innovation consultants.
“This will be a unique learning opportunity for ophthalmologists,” said Dr Paul Rosen, Chairperson of the ESCRS Leadership and Business Innovation Committee. The weekend is the first of a series the committee plans through 2024.
The Saturday session will be devoted to “Principles of Leadership and Innovation for Ophthalmologists.” The second session on Sunday will discuss “Practical Tools for Ophthalmologists in Planning and Managing Financial Resources and Creating Value.” Both sessions will feature a combination of keynote lectures on these topics and practical exercises for delegates to help them put their learning into practice.
“On the first day, we will examine the skills needed for ophthalmologists who wish to become leaders and innovators in their public and private practices. Among the topics we will discuss are leadership values and leadership culture, leadership and innovation from concept to implementation, and avoiding physician burnout,” Dr Rosen said. The Sunday session will focus on finance, discussing cost management, raising funds, preparing business plans, and market analysis and segmentation.
“All ophthalmologists are very skilled clinicians,” said Dr Rosen, “but they will face challenges in dealing with the complex issues of leading teams in private and public practice. We need to learn how to be creative in our day-to-day
work, as in the future, telehealth and artificial intelligence will profoundly affect every aspect of ophthalmic practice.”
Expert faculty
The Frankfurt programme facilitators are Dr Karl Thomas and Mr Matt Jensen.
Dr Thomas, based in Dublin, Ireland, has acted as a mentor at various innovation and entrepreneurship events. He also provides coaching support to startups and business leaders, focusing on developing people who think differently in the field of innovation and creating future leaders who understand the value of communication, collaboration, critical thinking, and creative problem solving.
Matt Jensen is the principal and founder of Matt Jensen Marketing. Mr Jensen was previously CEO at Vance
Thompson Vision in Sioux Falls, South Dakota, US. He now runs his own marketing and communications firm with extensive expertise in eye care. He is also an international speaker on customer experience design in business and healthcare.
The ESCRS faculty includes Professor John Marshall, Drs Paul Rosen, Daniel Kook, Artemis Matsou, Arthur Cummings, David Lockington, and Ms Celine Reibel, who will show how they have successfully led teams in their public and private practices and introduced innovative ideas into these practices.
Registration for the weekend at the Hilton Frankfurt Hotel costs €750. Early registration is advised, as the course is limited to 30 delegates. For further details, visit www.escrs.org
48 LEADERSHIP AND BUSINESS INNOVATION
EUROTIMES | SEPTEMBER 2023
We need to learn how to be creative in our day-to-day work, as in the future, telehealth and artificial intelligence will profoundly affect every aspect of ophthalmic practice.
FACULTY
ESCRS LEADERSHIP & BUSINESS INNOVATION WORKSHOPS





MONDAY, 11 SEPTEMBER. STRAUSS 3, 09.00–17.00


CHAIRMAN
PAUL ROSEN, UK
• BUSINESS SKILLS FOR YOUNG OPHTHALMOLOGISTS


• MASTERING THE ART OF NEGOTIATION
MODERATORS: ROD SOLAR, UK
• BUILDING AND DEVELOPING YOUR PRIVATE PRACTICE







• VALUE-BASED HEALTHCARE
• SUSTAINABILITY IN OPHTHALMOLOGY
LAURA LIVESEY, UK

• GETTING AN OPHTHALMOLOGICAL BUSINESS BACK ON ITS FEET DURING WARTIME
• MANAGING PATIENT FLOW IN A BUSY OPHTHALMOLOGICAL PRACTICE
• MARKET LEADERSHIP: HOW THREE REFRACTIVE SURGEONS 3X’ED THEIR PRACTICES IN THE LAST THREE YEARS

49 2023 SEPTEMBER | EUROTIMES
A Matsou, Greece
D Kook, Germany
D Chang, US
N Reus, The Netherlands
B Lahood, Australia
O Findl, Austria
V Qin, Belgium
P Stodulka, Czech Republic
Sheraz Daya, UK
J Buratto, Italy
R Nuijts, The Netherlands
F van den Biggelaar, The Netherlands
C Reibel, France
Eyenuk AI approved for use with multiple retinal cameras
The US FDA has granted clearance for the use of Eyenuk’s EyeArt® v2.2.0 artificial intelligence (AI) system with the Topcon NW400 retinal camera for automatic detection of diabetic retinopathy (DR). Since the AI system already had clearance for detecting DR with Canon CR-2 AF and Canon CR-2 Plus AF cameras, the new clearance decision makes the EyeArt the first and only AI system to be FDA-approved for use with multiple retinal cameras by different manufacturers. This latest FDA clearance for the EyeArt v2.2.0 system is based on clinical data from a prospective multi-centre clinical trial that demonstrated 94.4% sensitivity and 91.1% specificity for more than mild DR detection, and 96.8% sensitivity and 91.6% specificity for vision-threatening DR detection. In the European Union, the EyeArt system is the only AI system approved under MDR Class IIb to detect DR, age-related macular degeneration, and glaucomatous optic nerve damage in a single test.
www.eyenuk.com
FDA pauses approval of high-dose aflibercept
Regeneron Pharmaceutical’s high-dose version of Eylea®, aflibercept 8 mg, has hit a snag in its approval process in the US for treating patients with wet age-related macular degeneration, diabetic macular oedema, and diabetic retinopathy. The US FDA has issued a Complete Response Letter (CRL) for the Biologics License Application (BLA) for the 8 mg aflibercept preparation, which is designed for three- and four-month dosing. The CRL is solely due to an ongoing review of inspection findings at a third-party filler, namely the production facility Catalent Inc. The CRL did not identify any issues with the clinical efficacy or safety, trial design, labelling or manufacturing of aflibercept 8 mg, and the FDA has requested no additional clinical data or trials. Regulatory filings for aflibercept 8 mg are under review in Europe and Japan.
www.regneron.com
Ocular tissue substitute granted FDA clearance
EverPatch, Corneat Vision’s synthetic biocompatible tissue substitute for ophthalmic surgeries, has received 510(k) clearance from the US FDA. Designed as an alternative to processed donor tissue, the EverPatch is composed of a sterile, non-woven polymer matrix that integrates with surrounding tissue to reinforce the sclera, thereby aiding the physical reconstruction of the ocular surface. The company notes EverPatch is significantly thinner than processed patch tissue and provides better handling as it does not “cheesewire” when sutured. They add the non-biodegradable polymer matrix material also has the potential for wider use in soft tissue reinforcement, biomechanical integration of implants with surrounding tissue, fabrication of membranes, and concealment of implants and sensors.
www.corneat.com
50 INDUSTRY NEWS
EUROTIMES | SEPTEMBER 2023
PERILS OF AI IN MEDICAL PUBLISHING

In a frontpiece editorial, Dr William J Dupps Jr highlighted the perils of generative artificial intelligence (AI) in academic publishing. The article noted the double-edged nature of this emerging technology. On the one hand, it provides a useful tool in research and the dissemination of knowledge; on the other, it poses serious ethical challenges. Among these is the danger of inadvertent plagiarism. How can authors using AI know whether the work the software generates is truly original, leaving original authors without their due credit?
Secondly, even when putting plagiarism aside, how can an “author” of an AI-generated manuscript acknowledge the AI contribution without bringing their credibility into question?
Aside from ethics, there is the question of AI’s impact on the quality of academic papers. The reliability, validity, and relevance of AI-generated manuscripts can be difficult to evaluate and peer review, particularly given the nonhuman nature of the generated content and its susceptibility to errors, bias, and misinformation. Essentially, how can AI be relied on to check its work since it answers to no one and has no personal reputation to maintain?
These challenges underline the need for clear and consistent guidelines for using AI in academic publishing, such as declaring and explaining its use, acknowledging its limitations, and verifying its sources. Robust and transparent mechanisms are necessary for detecting and addressing AI-related misconduct, such as plagiarism, fabrication, or falsification. Moreover, researchers who use AI tools need to critically assess their outputs with an awareness of the potential risks, benefits, and ethical considerations involved.
Dr Dupps shared this cogent discussion of AI’s risks and benefits was, in fact, generated by the AI engine ChatGPT seconds after he typed “perils of generative AI in academic publishing” as a prompt in the “Compose” section of the Microsoft Edge sidebar and selected “Blog” for the writing style

However, he noted one thing the AI-generated composition left out of the discussion was the potential erosive impact AI could have on the intellectual prowess of authors themselves. This is particularly true in the case of education and academic publishing. Education is about the cultivation of the intellect and growth in character only achieved through honest effort. Academia, for its part, places originality, innovation, attribution, and intellectual property at its core.
“At a time in history when technology can increasingly be confused with personhood, the value of the people and the human processes that birthed these technologies should always be the measure against which policy is measured,” Dr Dupps concluded.
Dupps WJ, Journal of Cataract & Refractive Surgery, 49(7): 655–656.

Research Education Innovation
51 JCRS HIGHLIGHTS
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.
2023 SEPTEMBER | EUROTIMES
GLAUKOS RISING
Ophthalmic innovator rises as fully integrated ophthalmic device and pharmaceutical firm.
BY HOWARD LARKIN
More than 20 years ago, Glaukos set out to transform glaucoma therapy. And with more than 1 million iStent devices implanted globally since, they have taken a giant step toward that goal. The minimally invasive trabecular meshwork microstent continuously reduces intraocular pressure (IOP) and reduces reliance on medications for glaucoma patients.
Now Glaukos is on the verge of expanding that mission with iDose TR, a minimally invasive sustained drug delivery intraocular implant. The drug-device combination is implanted in the iridocorneal angle, where it elutes a special stabilised travoprost formulation.
In clinical trials, iDose demonstrated significant IOP lowering while effectively addressing eye drop shortcomings, including ocular surface disease and patient non-adherence.
In one phase 3 study, 81% of iDose TR subjects were completely free of IOP-lowering drops at 12 months. A phase 2b study showed 69% of patients maintained IOP control after three years on the same or fewer IOP-lowering topical medications than pre-procedure. The drug delivery device showed greater IOP reduction from washout than pre-study topical prostaglandin analogues (PGAs) in two other phase 3 studies.
iDose TR also demonstrated favourable safety compared with topical PGAs. Researchers in phase 2b and 3 studies did not observe any periorbital fat atrophy and very few iris colour changes or conjunctival hyperaemia cases, nor any adverse events of corneal endothelial cell loss in the trials or an extended trial examining device exchanges for more than five years.
“We are very excited about this data,” Dr Tomas Navratil, Glaukos Chief Development Officer, said at the Eyecelerator event at the ASCRS 2023 annual meeting. The drug-device combination is in US FDA review with a target of approval by year’s end, he announced.
Branching out
But glaucoma is just one branch of the Glaukos story. Based in Aliso Viejo, California, US, the company has built an extensive product portfolio and pipeline of pharmaceutical, device, and drug-device combination products for glaucoma, corneal, and retinal diseases. Since 2018, the firm has invested more than $400 million in research and development, Dr Navratil said.
For the cornea, approved products include the iLink corneal cross-linking system with UV-activated pharmaceuticals for epithelium-off keratoconus treatment. In phase 3 development is Epioxa, a pharmaceutical for use with epi-on corneal cross-linking. For the retina, the company is making
52
EUROTIMES | SEPTEMBER 2023 INDUSTRY INSIGHT
encouraging pre-clinical development progress for its sustained delivery pharmaceutical platform designed to treat retinal vein occlusion, wet age-related macular degeneration, and diabetic retinopathy. “We are targeting year’s end for our first in-human retina clinical program,” Dr Navratil said.
Stages of growth
In the inaugural company profile segment of the Eyecelerator programme, company officials outlined Glaukos’ path from start-up to growing force in ophthalmology.
“Glaukos had a very altruistic beginning,” said company Chairman and CEO Thomas Burns, who has led the company for more than 20 years since joining in
2002. In 1998, an 18-year-old man presented with pigmentary glaucoma and bilateral vision loss to Dr Richard A Hill at the University of California, Irvine, who recommended trabeculectomy. The patient’s father (a venture capitalist) challenged Dr Hill for a better way, Burns said.
Dr Hill said he had a better way—a trabecular meshwork bypass device— but no one would listen. The venture capitalist connected him with a California Institute of Technology engineering professor. Together they designed the micro-bypass glaucoma device that would become iStent.
Yet, there were many bumps in the road along the way. Designing the microstent and implant procedure
and making them acceptable to the FDA and surgeons as a standalone procedure was an early challenge, Dr Link—one of Glaukos’ founders and former Chairman, now managing partner of Flying L Ventures—said. Dr Richard Lindstrom suggested inserting it during cataract surgery, an idea that “rang the bell,” Dr Link said. Still, it took two years from the FDA panel review to win approval for the iStent in conjunction with cataract surgery in 2012.
Investor support was essential to survive, said investor Dr Gil Kliman, managing partner of InterWest Partners. But there was no hesitation due to the strength of the idea, the technology, and the team, he said. “Many companies fail at exactly that point.”
Since then, Glaukos has invested in other ophthalmology areas. It has acquired Avedro for cornea, and DOSE Medical for its retinal research and development programme, while investing in new technologies.
This willingness to invest is another reason why top executives and investors continue supporting Glaukos, said Joseph Gilliam, the firm’s president and chief operating officer. “I’ve seen many companies who put all their eggs in one basket, for good reason.” But Glaukos’ willingness to look forward to generations two and three and other opportunities made it stand out as a good long-term prospect, he said.
53
Thomas Burns is chairman and CEO, Tomas Navratil PhD is chief development officer, and Joseph Gilliam is president and chief operating officer at Glaukos.
William J Link PhD is managing partner, Flying L Ventures.
Gil Kliman MD is managing partner, InterWest Partners, California, US.
2023 SEPTEMBER | EUROTIMES
Thomas W Samuelson MD is an adjunct professor, University of Minnesota, and a surgeon at Minnesota Eye Consultants, US. twsamuelson@mneye.com
Since 2018, the firm has invested more than $400 million in research and development.
Cited in this Issue
ESCRS Supports Cataract Project in Nepal
Page 9
1. International Centre for Eye Health. 2019. Rapid Assessment of Avoidable Blindness.
What is the Potential Role of AI in Ophthalmology?
Page 12
1. Ting DSW, et al. “Artificial intelligence and deep learning in ophthalmology.” British Journal of Ophthalmology, 2019; 103: 167–175.
2. Xie Y, et al. “Artificial intelligence for teleophthalmology-based diabetic retinopathy screening in a national programme: an economic analysis modelling study.” Lancet Digit Health, 2020; 2: e240–e249.
3. Chen EM, Chen D, Chilakamarri P, Lopez R, and Parikh R. “Economic Challenges of Artificial Intelligence Adoption for Diabetic Retinopathy.” Ophthalmology, 2021; 128: 475–477.
4. Mathenge W, et al. “Impact of Artificial Intelligence Assessment of Diabetic Retinopathy on Referral Service Uptake in a Low-Resource Setting: The RAIDERS Randomized Trial.” Ophthalmol Sci, 2022; 2: 100168.
5. Widner K, et al. “Lessons learned from translating AI from development to deployment in healthcare.” Nat Med, 2023; 1–3: doi: 10.1038/s41591-023-02293-9.
6. Toro MD, et al. “Early impact of COVID-19 outbreak on eye care: Insights from EUROCOVCAT group.” Eur J Ophthalmol, 2021; 31: 5–9.
7. Thirunavukarasu AJ. “ChatGPT cannot pass FRCOphth examinations: implications for ophthalmology and large language model artificial intelligence.” Eye News, 2023.
8. Thirunavukarasu AJ. “Large language models will not replace healthcare professionals: curbing popular fears and hype.” J R Soc Med, 2023; doi: 10.1177/01410768231173123.
9. OpenAI. GPT-4 Technical Report. Preprint at https://doi. org/10.48550/arXiv.2303.08774 (2023).
10. Nagendran M, et al. “Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies.” BMJ, 2020; 368: m689.
Climate Change and Eye Health
Page 14
1. Alryalat SA, Toubasi AA, Patnaik JL, Kahook MY. “The impact of air pollution and climate change on eye health: a global review.” Rev Environ Health, 2022 Dec 29. doi: 10.1515/ reveh-2022-0209. Epub ahead of print. PMID: 36579431.
2. Rigaud KK, et al. 2018. “Groundswell: Preparing for Internal Climate Migration.” World Bank, Washington, DC. doi: 10.1596/29461, License: CC BY 3.0 IGO.
3. Chen M, Caldeira K. “Climate change as an incentive for future human migration.” Earth Syst Dynam, 11: 875–883. doi: 10.5194/esd-11-875-2020, 2020.
4. Jaiswal S, et al. “Smoke and the Eyes: A Review of the Harmful Effects of Wildfire Smoke and Air Pollution on the Ocular Surface.” Environmental Pollution, 309 (July): 119732. doi:
10.1016/j.envpol.2022.119732. Epub 2022. PMID: 3589974.
5. Sun HY, et al. “Association Between PM2.5 Exposure Level and Primary Open-Angle Glaucoma in Taiwanese Adults: A Nested Case-Control Study.” Int J Environ Res and Public Health, 2021 Feb 10; 18(4): 1714. doi: 10.3390/ijerph18041714. PMID: 33578928; PMCID: PMC7916685.
6. Shan A, et al. “Association Between Long-Term Exposure to Fine Particulate Matter and Diabetic Retinopathy among Diabetic Patients: A National Cross-Sectional Study in China.” Int J Environ Res and Public Health, 2021 Sept; 154. doi: 10.1016/j. envint.2021.106568.
7. Ju MJ, Kim J, Park SK, Kim DH, Choi YH. “Long-Term Exposure to Ambient Air Pollutants and Age-Related Macular Degeneration in Middle-Aged and Older Adults.” Environmental Research, 204 (March): 111953. doi: 10.1016/j.envres.2021.111953.
8. Gómez-Mariscal M, de Arriba F, et al. “Do Season and Environment Have a Role in the Incidence of Anterior Uveitis Attacks?” Ocul Immunol Inflamm, 2020. 28(5): 786–790. doi: 10.1080/09273948.2019.1636092.
Links in Eye Care Delivery and Climate Change
Page 16
1. Thiel CL, Schehlein E, Ravilla T, et al. “Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility.” J Cataract Refract Surg, 2017; 43(11): 1391–1398.
2. Morris DS, Wright T, Somner JE, Connor A. “The carbon footprint of cataract surgery.” Eye (Lond), 2013; 27(4): 495–501.
3. Goel H, Wemyss TA, Harris T, et al. “Improving productivity, costs, and environmental impact in International Eye Health Services: using the ‘Eyefficiency’ cataract surgical services auditing tool to assess the value of cataract surgical services.” BMJ Open Ophthalmol, 2021; 6(1): e000642.
4. Sherry B, Lee S, Ramos, et al. “How ophthalmologists can decarbonize eye care: a review of existing sustainability strategies and steps ophthalmologists can take.” Ophthalmology, 2023 Mar 6: S0161-6420(23)00137-9. doi: 10.1016/j.ophtha.2023.02.028. Epub ahead of print.
Assessing Transepithelial Surface Ablation Benefits
Page 28
1. Alasbali T, et al., J Ophthalmol, 2022 Aug 23.
2. Hashemi H, et al., BMC Ophthalmol, 2022 Feb 11; 22(1): 68.
Striving for Perfection in LASIK
Page 30
1. Stulting RD, et al. J Cataract Refract Surg, 2022 Sep 1; 48(9): 1010–1015.
2. Rush SW, “Patient Satisfaction with Contoura Vision Topography-Guided LASIK,” ClinicalTrials.gov, classic.clinicaltrials. gov/ct2/show/NCT04903301.
54 CITATION INDEX
EUROTIMES | SEPTEMBER 2023
EVO ICL for Low Myopia
Page 34
1. Allan B, et al. JCRS, 2009; 35: 766–769.
2. Rocamora L, et al. JCRS, 2023; 49(2): 126–132.
3. Packer M. Clin Ophthalmol, 2018; 12: 2427–2438.
Femto-LASIK Sets High Bar for Myopic Correction

Page 36
1. Jiang, et al., J Refract Surg, 2022 Apr; 38(4): 277–284.
2. Liu, et al., J Refract Surg, 2020 Oct 1; 36(10): 653–660.
3. He, et al., BMC Ophthalmol, 15, 141 (2015).
4. Ma, et al., Am J Ophthalmol, 2022 Sep; 241: 248–253.
5. Brar, et al., J Refract Surg, 2021 Dec; 37(12): 800–808.
Functional Vision with Monofocal-plus IOL
Page 38
1. Ribeiro F, et al., “Analysis of Daily Visual Habits in a Presbyopic Population,” J of Ophthalmol, 2023 Apr 1–8, https://doi.org/10.1155/2023/6440954.
2. Kohnen T, et al., JCRS, 49(2): 133–141.
3. Wan KH, et al., J Refract Surg, 2022 Aug: 38(8).
António Champalimaud Vision Award winners
Page 40
1. Melles GRJ, Parker JS. “How would nature see our corneal triumphs?” 2022. https://www.niios.com/wp-content/ uploads/2022/09/2209-JML-How-would-nature-see-ourcorneal-triumphs-AAO-2022.pdf
2. Dohlman C. “The Boston Keratoprosthesis—The First 50 Years: Some Reminiscences.” Annu Rev Vis Sci, 2022 Sep 15; 8(1): 1–32.
55 2023 SEPTEMBER | EUROTIMES
more at ESCRS.org
To be the leading community and trusted source for science, education, and professional development in the fields of cataract and refractive surgery.
Learn
ESCRS LEADERSHIP & BUSINESS INNOVATION WEEKEND
HILTON FRANKFURT CITY CENTRE, GERMANY
SATURDAY OCTOBER 7–SUNDAY OCTOBER 8, 2023
ESCRS
Leadership, Business & Innovation
MODERATORS:
CHALLENGING THE NORM—REDUCING COSTS,
IMPROVING PRODUCTIVITY, AND ENHANCING PATIENT EXPERIENCE WITH GREAT LEADERSHIP AND INNOVATION
TOPICS:
• Leadership Values and Culture
• Leadership and Innovation in Ophthalmology
Matt Jensen, Principal/Founder Matt Jensen Marketing, US
• Avoiding Physician Burnout
• Leading a Team in a Private Ophthalmological Practice

• Innovating to Reduce Costs
Karl Thomas, Innovation Trainer & Consultant and Leadership Coach, Ireland


FACULTY:
Paul Rosen, Consultant Ophthalmologist, Oxford Eye Hospital, UK, and Chairperson of the ESCRS Leadership and Business Innovation Committee and Chairman of the Trustees of ESCRS


John Marshall, Frost Professor of Ophthalmology, Institute of Ophthalmology in association with Moorfield’s Eye Hospital, UK
Daniel Kook, Consultant Ophthalmologist, Gräfelfing, Germany
• Optimising Workflow to Maximise Productivity and Enhance Patient Experience
• Artificial Intelligence and Innovation in Ophthalmology
• Raising Funds
• Preparing Your Business Plan
• Market Analysis and Segmentation
• Pitching Your Business Idea to a Venture Capital Company

• Lean Business Canvas Model for a New Private Practice
Arthur Cummings, Consultant Ophthalmologist, Beacon Hospital, Dublin, Ireland

David Lockington, Consultant Ophthalmologist, Nuffield Health, Glasgow Hospital, UK

Artemis Matsou, Consultant Ophthalmologist, Queen Victoria Hospital, East Grinstead, UK
REGISTRATION €750
Celine Reibel, Responsable Relations Patients, France
https://www.escrs.org/education/leadership-business-and-innovation/ leadership-weekend-2023/ www.hilton.com/en/hotels/frahitw-hilton-frankfurt-city-centre

56 EUROTIMES | SEPTEMBER 2023
Upcoming Events
September 8–12
2023 ESCRS Annual Congress
Vienna, Austria

Sept 8
October 5–8
2023 EURETINA Congress
Amsterdam, Netherlands

Oct 28–Nov 1
German Society of Ophthalmology
Berlin, Germany

November 3–6
American Academy of Ophthalmology
San Francisco, United States

November 24–26
Italian Society of Ophthalmology
Rome, Italy
February 15
2024 ESCRS Winter Meeting
Frankfurt, Germany
Oct
57 2023 SEPTEMBER | EUROTIMES
28
3
Oct 5 Nov



Join Our Experts Panel at the ESCRS to learn more about iStent inject® W Do Not Miss your Chance to IKE AHMED FRITZ HENGERER KEVIN GILLMANN ANA MIGUEL TICIANA DE FRANCESCO FAISAL AHMED JULIÁN GARCÍA FEIJOO GOK RATNARAJAN VINCENT QIN View Important Safety Information Scan now to access the full program! Saturday 9th and Sunday 10th GLAUKOS BOOTH B204






















































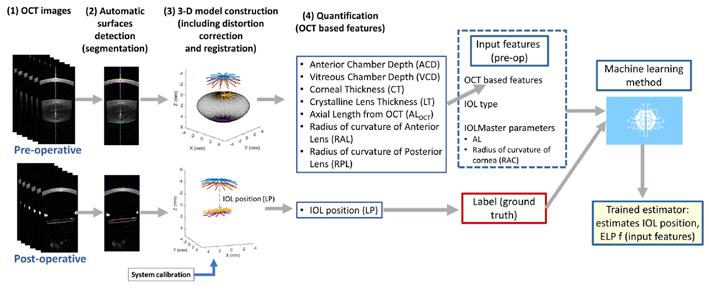
















 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS























































