What is the Future of Ophthalmology Training in Europe?
Shifts from the pandemic and inconsistent training standards make young ophthalmologists feel less than confident. Add-on

Climate Change and the Eyes Changing ocular epidemiology and increased prevalence of poverty-related blindness are likely consequences of climate change.
Trauma of War Laid Bare Ukrainian ophthalmologists relay the extent of their challenges treating in a war zone.
MARCH 2023 | VOLUME 28 | ISSUE 2
ALSO IN THIS ISSUE
IOLs Bring Added Benefits
Primary and secondary implantation procedures offer advantages to alternatives.
https://congress.escrs.org/

BINKHORST MEDAL LECTURE
Jorge L Alió MD, PhD, FEBOphthal will speak on “Corneal Regeneration: The Future of Corneal Surgery.” Dr Alió is a professor and chairman of ophthalmology at the University Miguel Hernández de Elche in Alicante, Spain, and a leader in the emerging topic of corneal regeneration. He conducted the first worldwide clinical trial for the treatment of corneal dystrophies and particularly keratoconus with autologous mesenchymal stem cells, and he has published a series of important scientific papers on this innovative type of corneal surgery.
SMART AND @CTIVE MONDAY
A new addition to the ESCRS Congress, Smart and @ctive Monday will feature “brushups” on retinal surgery, glaucoma surgery, and oculoplastics, a medical writing workshop for young ophthalmologists, an ophthalmic anaesthesia symposium, a surgical video session, and practice management sessions. A “digital track” will offer a “Continents Going Digital” symposium, symposia on automating eye surgery and the digital operating room, and talks and panel discussions about artificial intelligence in ophthalmology.

HERITAGE LECTURE
Marie-José Tassignon, MD, PhD, FEBOS-CR will speak about “The Enigma of the Anterior Interface.” Dr Tassignon is the emeritus head and chief of the department of ophthalmology of the Antwerp University Hospital and University of Antwerp. The first female president of ESCRS (2004–2005), Dr Tassignon developed bagin-the-lens cataract surgery for the paediatric population and holds 10 patents (three earned since 2019). She has been published more than 370 times in peer-reviewed journals and is the author of 27 book chapters and two full textbooks in ophthalmology.
iNOVATION DAY
Building on the success of the inaugural iNovation® Day in 2022, ESCRS is hosting the second iNovation Day on Friday, 8 September. Sessions will focus on the most urgent clinical needs and barriers to success in anterior segment care and how new technologies may address those barriers and clinical needs within the next 5–10 years. Of special interest is a new feature, “The Innovators Den: EyeCare Pioneers,” which will highlight entrepreneurs who have personally developed unique ideas to address some of the biggest unmet needs of Congress attendees.

2 Contents GLOBAL 14 Climate Change and the Eye Robert J Casson MB.BS (Hons), MBiostats, DPhil, FRANZCO UKRAINE 16 Trauma of War Laid Bare in Ukraine Focus Session Andrii Ruban MD, PhD; Ihor Novytskyy MD, PhD; Volodymyr Melnyk MD, PhD; Natalia Grubnyk MD; Ferenc Kuhn MD, PhD CATARACT & REFRACTIVE 18 Add-on IOLs Bring Added Benefits Oliver Findl MD and Michael Amon MD, PhD 20 Capsular Tension Rings and Toric IOLs Daniel Schartmüller MD 22 New IOL Underscores Importance of Peripheral Vision Pablo Artal PhD CORNEA 24 Rethinking Fuchs’ Dystrophy Gerritt RJ Melles MD, PhD 26 Studies Shed Light on Long-Term Cross-Linking Outcomes Riccardo Vinciguerra MD 28 Corneal Regeneration Jie Zhang PhD 30 Better Before or After? Irit Bahar MD, MHA and Jennifer Li MD 32 Endothelial Cell Injection Shigeru Kinoshita MD, PhD GLAUCOMA 34 Surgery for Patients with Symptomatic Cataract and Ocular Hypertension Andrew J Tatham MD and Simonetta Morselli MD 36 Use IOLs with Caution Filomena Ribeiro MD, PhD RETINA 38 Gene Therapy in the Real World Dominik Fischer MD, DPhil, FEBOphth 40 New Prospects for Inherited Retinal Disease Ben Shaberman MA, MS 08 Cover What is the Future of Ophthalmology Training in Europe? Shifts from the pandemic and inconsistent training standards make young ophthalmologists feel less than confident. EUROTIMES | MARCH 2023 March 2023 | Vol 28 Issue 2
Publishers Barbara Calderwood
Mariska van der Veen
Mark Wheeler
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Mariska van der Veen
Contributing Editors
Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Soosan Jacob
Leigh Spielberg
Colour and Print
W&G Baird Printers
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 roo.khan@wearemci.com
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes

ISSN 1393-8983
Learn more about EuroTimes or connect with ESCRS at ESCRS.org



3 04 Editorial: Onwards to Portugal 05 ESCRS at a Glance: 40th Congress of the ESCRS in Numbers 06 Inside ESCRS: The FEBOS-CR Exam: A Stepping Stone to Greater Accomplishment? 42 BioOphthalmology: How Should We Read Clinical Trials? Designing, executing, and interpreting randomised clinical trials. 44 Leadership and Business Innovation: Young Ophthalmologists Need Business and Management Skills 46 Industry News 47 JCRS Highlights 48 ESCRS Eye Journal Club: ICL—The Lasso Formulas 49 Upcoming Events 18 14 2023 MARCH | EUROTIMES
Onwards to Portugal
FILOMENA RIBEIRO, PRESIDENT-ELECT OF THE ESCRS
We will be gathering this month in Vilamoura, Portugal, for what may be the largest Winter Meeting the ESCRS has ever held. It is a welcome return to near normal after we were obliged to convert our previously scheduled get-together in Vilamoura to a virtual format during the depths of the COVID pandemic. We are happy to be able to continue the tradition of holding the meeting in a special setting, allowing a unique combination of a high-level programme and the warm welcome of my country, Portugal.

The 2023 Winter Meeting will be in collaboration with the Sociedade Portuguesa Oftalmologia (SPO) and the Portuguese Groups of Cataract and Refractive Surgery, Ocular Surface, Cornea and Contactology (CIRP). This cooperative effort will translate into joint free paper sessions, a Live Surgery Session, and a separate track in Portuguese for our local colleagues. There will also be a joint Portuguese-Brazilian symposium.
The conference format for Vilamoura will be fully faceto-face, with no virtual access. The recent annual congress in Milan has shown the growing appetite for meeting, learning, and socializing at conferences.
The sizable ESCRS programme begins with a full Cornea Day. Attendees can choose from a selection of symposia, free paper sessions, instructional courses, and posters throughout the three-day meeting. A full selection of wet labs is also on the menu. We are happy to welcome members of the European Society of Ophthalmic Nurses and Technicians (ESONT), who will have a special session.
Young ophthalmologists have many options during the conference. During COVID, many trainees had their studies
EDITORIAL BOARD
INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)

Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)
Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)
disrupted by the isolation required for public health, missing opportunities for live or even simulated surgical training. This, in turn, made applying for fellowships and future employment even more difficult than it had been, adding to a uniquely stressful time to be entering the ophthalmology profession. Our lead story by Dr Clare Quigley looks at the challenges facing ophthalmology training in Europe.
Once young ophthalmologists qualify to practice, they may find themselves unprepared for the commercial realities of an ophthalmology clinic. A column in this issue addresses this challenge, discussing ways young ophthalmologists can learn business and management skills.
With the arrival of March, the Ukraine war sadly enters its second year. Writer Dermot McGrath looks at the toll of that war and reminds us of the many challenges faced by our Ukrainian colleagues.
The ESCRS continues to support our colleagues in the war zone. We are very grateful for the continuing support we are receiving from the industry and our members. If you are an ESCRS member and wish to contribute, simply log in at https://donate.escrs.org
I hope to see you in Vilamoura! EuroTimes will offer comprehensive coverage of the proceedings in future issues.
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)


Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
 Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell
Paul Rosen
Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell
Paul Rosen
4 EUROTIMES | MARCH 2023 EDITORIAL
5 2023 MARCH | EUROTIMES ESCRS AT A GLANCE 6% 3% 68% 4% 19% 1% 13’874 PARTICIPANTS 7’175 DOCTORS 5 MAIN SYMPOSIA 4 RESEARCH SYMPOSIA 378 FREE PAPERS 104 WET LABS 332 HEALTHCARE PROFESSIONALS 697 NURSES/TECHNICIANS 867 DOCTORS/HCPS (VIRTUAL) 4’803 INDUSTRY MEMBERS =50 PARTICIPANTS 1473 947 825 662 656 588 529 515 484 303 129 COUNTRIES ITALY GERMANY UNITED KINGDOM UKRAINE SWITZERLAND UNITED STATES NETHERLANDS SPAIN FRANCE ROMANIA COUNTRIES REPRESENTED CONGRESS OVERVIEW TOP 10 COUNTRIES 401 PRESENTED POSTERS
26 VIDEOS IN THE LIBRARY CHALLENGING VIDEO CASES 205 PARALLEL ROOMS
40TH CONGRESS OF THE ESCRS IN NUMBERS
THE FEBOS-CR EXAM: A STEPPING STONE TO GREATER ACCOMPLISHMENT?
Given the already high bar to becoming an ophthalmologist, taking exams for subspecialties might seem excessive. But those who have sat for and passed the FEBOS-CR exam—an assessment of the knowledge and skills needed by cataract and refractive (CR) surgeons to perform difficult cases—say the test is worth the time and effort.
“Although it was challenging to take the exam when nobody had done it before, I think it was a great experience,” says Julio Ortega-Usobiaga MD, PhD, who sat for—and passed—the exam, which was developed by the ESCRS in conjunction with the European Board of Ophthalmology (EBO). “This exam proves you have a vast knowledge of this subspecialty. In addition, you must show, in English, that you can explain complex surgical cases and scientific literature before a board of eminent colleagues.”
Dr Ortega-Usobiaga is one of just 25 ophthalmologists who have earned the FEBOS-CR honorific. Nearly 150 ophthalmologists have applied to take the exam since its inception in 2017, and of those, only 57 were invited to sit for it.
The FEBOS-CR exam is one of a handful of European ophthalmic subspecialty exams, along with glaucoma, paediatric, and strabismus; others are in development. The goal of these exams is to harmonize ophthalmic education in Europe and define the expected level of knowledge and skills a subspecialist should acquire to solve complex, difficult cases.
“The level should be advanced, since the final goal is getting a structured fellowship programme in different fields of ophthalmic subspecialists in Europe,” says Marie-José Tassignon MD, PhD, who led the development of the exam and chairs the FEBOS-CR exam committee. “Successful candidates have shown high skills in education and surgical skills within their subspecialty and should be able to run clinical trials. This explains why the application process is a bit more daunting for the primarily surgically oriented subspecialisations like FEBOS-CR.”
Dr Ortega-Usobiaga concurs, saying the exam serves as proof of excellence in a specialised field that historically has lacked credentials to signify accomplishment.
“There is a clear pathway to be a physician in most countries,” he says. “There is also another pathway to be an ophthalmologist and even another
to achieve a PhD. But there is not a clear path to be a subspecialist in most countries.”
To provide a “clear path,” EBO began to approach subspecialty scientific societies in Europe and request their assistance in creating exams. EBO reached out to the ESCRS in 2016 and asked for assistance in organising the FEBOS-CR exam.
“The ESCRS membership is composed of high-volume cataract surgeons in academic and private settings,” says Dr Tassignon. “This is the perfect mix out of which a committee can be created of colleagues who will define the curriculum considered to best fit what is expected of a candidate who potentially will finish a fellowship education and who can, in turn, eventually further evolve to become a trainer of fellowship programmes.”
Rudy Nuijts MD, PhD, who chairs the ESCRS Education Committee (which is responsible for the FEBOS-CR exam), confirms the ESCRS is committed to continuing this project, with a final goal of harmonizing criteria for defining fellowship standards across Europe.
“Currently, there are no formulated criteria, or consensus on a definition of criteria is lacking,” he says. “The ultimate goal of the ESCRS is to add value to the personal skills of its members that are recognized throughout Europe.”
The 2023 exam will be administered in September at the ESCRS Annual Congress in Vienna. The application deadline is March 10; as part of the application process, candidates must submit a recommendation letter, a video of a complex case they operated on, and a completed CV/application that lists their surgical, teaching, and publication experience.
This year will mark the fourth round of FEBOSCR exams; the exam was not given in 2020–2022 because of the COVID-19 pandemic. Dr Tassignon hopes the exam serves not just as a barometer of surgical achievement but as a stepping stone to greater accomplishment.
“There is much more to learn than surgical skills and knowledge to become an excellent ophthalmologist,” she says. “There is also leadership, planning, team building, research, etc. Much awaits those who have the ambition to grow in their profession and who would like to find the solution to currently unanswered pathological conditions.”
6 EUROTIMES | MARCH 2023 INSIDE ESCRS
The ESCRS membership is composed of highvolume cataract surgeons in academic and private settings.

7 2023 MARCH | EUROTIMES
What is the Future of
Ophthalmology
Training in Europe?
Shifts from the pandemic and inconsistent training standards make young ophthalmologists feel less than confident.

COVER ARTICLE 8 EUROTIMES | MARCH 2023
CLARE QUIGLEY MD REPORTS
Ophthalmology surgical training programmes in Europe are inconsistent across the continent, with general dissatisfaction among trainees and more than a few young ophthalmologists (YOs) feeling unprepared to perform surgery.


“There is a lot of dissatisfaction and a lot of discrepancy across European training programmes in ophthalmology,” was Dr Vincent Qin’s stark assessment during a roundtable discussion on postgraduate training available in Europe at the 40th ESCRS Congress in Milan.
Currently, there is no parity in the quality of ophthalmology training across Europe. As a starting point, training duration varies widely, from as short as two years in countries such as Ukraine to seven years in the United Kingdom and Ireland. There is a general tendency towards longer training duration in western compared to eastern Europe, as shown in a survey published in a 2022 issue of the Eye. i
9 2023 MARCH | EUROTIMES
As well as training duration, opportunities available for cataract surgery training vary considerably. Dr Qin, a consultant ophthalmic surgeon in Belgium, highlighted that the minimum number of cataract surgeries stipulated by national training programmes varies from zero to 350 across Europe. Overall, a minority of ophthalmology trainees surveyed reported satisfaction with their surgical training.ii
“The deficient surgical training is reflected in the degree of satisfaction of the participants who responded to the survey,” said Dr Miguel González-Andrades, chair of the European Society of Ophthalmology YO section and the corresponding author of the manuscript. “Only 16% were completely or very satisfied with their acquired surgical competences, and 42% indicated they were completely unsatisfied with their surgical competencies.”

Young ophthalmologists expressed their concerns at the Milan roundtable event.
“YOs in Europe are mainly concerned about their surgical training, especially after the impact the pandemic had on ophthalmology services and training,” said Dr Artemis Matsou, consultant ophthalmic surgeon in the United Kingdom. “We have had limited access to surgery, and in countries where residency training lasts four years, residents spent at least half of their training with no access to surgery.”
Pandemic problems

Inequalities in training access compounded after the pandemic for different reasons, although this should be of limited duration as we learn to live with COVID.
“The lack of face-to-face conferences during the pandemic also meant we did not have access to wet labs and simulation
10 EUROTIMES | MARCH 2023
Only 16% were completely or very satisfied with their acquired surgical competences, and 42% indicated they were completely unsatisfied with their surgical competencies.
training—which was another big hit in surgical training. This has had a domino effect, as YOs are now finding it more difficult to get into fellowship training due to high competition,” Dr Matsou commented.
The core of the problem may be a lack of defined training standards in some European countries.
“It seems [that in some countries] there is no clear structure in YO surgical training. There is wide variation even within the same country,” she said. “The majority of YOs don’t feel confident to operate independently immediately after their residency. This is just regarding cataract surgery, as nearly no other type of surgery is being taught—other than some basic eyelid procedures and sometimes strabismus.”
Possible solutions

So, what is the solution to improve surgical training standards across Europe? International agreement about what constitutes ophthalmology training is a potential starting point.
Dr Matsou suggested guidelines or recommendations on minimum surgical training from a society such as the ESCRS and with agreement from individual national societies as a start. Simulation training, with better access for trainees and more frequent wet labs, would also be valuable. Finally, she proposed increased awareness of fellowship programmes in other countries and more opportunities to apply for bursaries, as self-funded trainees struggle to cover these costs.
Patient safety underlines the urgency of this issue. Within EU member states, doctors—including ophthalmologists— can migrate freely to practise their profession. But when a fully trained ophthalmologist equates to a competent cataract surgeon in one country and an ophthalmologist with no surgical experience in another, problems arise.


“It is essential for national governments as well as governing bodies to establish a European training curriculum common to all national teaching committees,” Dr González-Andrades said. “It is evident from our data that there is deficient surgical training since a considerable proportion of the respondents are far from achieving the minimum standards set by some of the countries.”
A great idea in theory, current ESCRS President Dr Oliver Findl shared the complications of putting it into practice. “I believe it will be very difficult to harmonise surgical training across Europe due to the significant differences in health systems.”
As an example, he said the Austrian public health system only funds cataract surgeries performed in public hospitals. For this reason, ophthalmologists practicing outside of hospitals—of which there are many—do not perform any surgery but instead comprehensive ophthalmology, medical retina, and other non-surgical subspecialties.
“In the past, I have trained numerous residents in cataract surgery, but they then decided to go into practice (for all kinds of reasons), and they never again performed surgery,” Dr Findl explained. “To train someone who may never again perform surgery due to the local health system may be seen as unethical since it is well-known that complication rates are highest in the initial, steep part of the learning curve— and patients are the ones exposed. It may also [appear]
11 2023 MARCH | EUROTIMES
risky, maybe even unethical, having a young, licensed surgeon perform surgery on their own outside of a hospital setting, having performed (in the best case) 350 cataract procedures during their training. We all know that significantly more surgical experience is necessary to do surgery safely without a more senior backup surgeon.”
Surgical and medical split?
Whilst cataract surgery is the bread-and-butter procedure of ophthalmic surgeons, the need for every ophthalmologist to be surgically trained is under question. Recent years have seen a great increase in demand for medical retina specialists, ushered in by the advent of anti-VEGF therapies. An overall ageing of Europe’s population has increased the prevalence of age-related macular degeneration, glaucoma, and cataract.
With this increasing demand for medical ophthalmology services, Dr Yvonne Delaney, Dean of Postgraduate Education at the Irish College of Ophthalmologists, proposes to split ophthalmologist training into medical and surgical streams.

The ESCRS stresses the need for a clear purpose for such a programme: whether it should be so comprehensive as to produce independent cataract surgeons of a sufficiently high standard or a basic training programme preparing doctors for a fellowship in cataract surgery or another subspecialty. The latter option moves away from the assumption all ophthalmologists must be able to do cataract surgery to be considered a fully qualified ophthalmologist—towards the model proposed by Dr Delaney.
The long-term impact of removing cataract surgery from training centres and university hospitals to the private sector is unknown. What is clear is training opportunities and funding are at risk of significant reduction, creating additional challenges for YOs.


Vincent Qin MD, MBA, MPH, FEBO, SSL. vincent.qin@live.be
Miguel González-Andrades MD, MSc, PhD. mgandrades@gmail.com
Artemis Matsou MD, MRCP(UK), FEBO, PgDip CRS. artmatsou@gmail.com
i–ii Anaya-Alaminos, R., Rassmussen, M.L., Fung, S.S.M. et al. “Comparative analysis of European residency programs: benchmarking and harmonizing ophthalmology training in Europe”. Eye (2022). https://doi.org/10.1038/s41433-022-02040-3
12 EUROTIMES | MARCH 2023 COVER ARTICLE
Applications for the Peter Barry Fellowship 2023 are

NOW OPEN!
The Fellowship of €60,000 will allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year.
The application deadline is 2 May 2023. For more information:
13 2023 MARCH | EUROTIMES
escrs.org/education/grants-awards/peter-barry-fellowship
Climate Change and the Eye
Changing ocular epidemiology and increased prevalence of poverty-related blindness are likely consequences of climate change.
Climate change may directly alter global ocular disease patterns, but the societal effects of extreme weather and rising sea levels will have the most devastating impact on ocular health, according to Professor Robert J Casson MB.
“The direct effects of climate change on ocular health will be relatively minor and remain largely speculative,” he said. “Nevertheless, the indirect effects are likely to be catastrophic.”
The scientific community has been aware of global warming since 1859 when John Tyndall began the discussion of climate change resulting from greenhouse gases in the atmosphere, and later Svante Arrhenius, who described the effect of carbon dioxide on the earth’s surface temperature in 1896. Its anthropogenic nature likewise became clear during the 20th century.

The world has been getting warmer since accurate measures began—and increasingly so in recent decades. In the early years of the current century, Frank Luntz, an American Republican party political propagandist, popularised the term “climate change” because he said “global warming” sounded too scary.
“Luntz was right about one thing,” Prof Casson said. “That global warming is scary. In fact, the World Health Organization has described global warming as the single biggest health threat facing humanity.”
An evaluation of climate change’s threat to ocular health requires consideration of both the direct and indirect effects of global warming, he noted. Direct effects might include some temperature-dependent or seasonal pathogenic component, such as seasonal allergic conjunctivitis or posterior vitreous detachment and associated retinal detachment, where dehydration is a risk factor.
A rise in world temperature will lead to people spending more time outdoors, Prof Casson posited, resulting in increased exposure to ultraviolet light that could raise the incidence of cortical cataract. More outdoor activity might also lead to a reduction in myopia.
Changes in vector-borne diseases are amongst the direct effects of climate change. There is already considerable
14 EUROTIMES | MARCH 2023 GLOBAL
ROIBEÁRD O’HÉINEACHÁIN REPORTS
The World Health Organization has described global warming as the single biggest health threat facing humanity.
evidence that climate change is altering the seasonal distribution of disease vectors, such as flies carrying trachoma and mosquitoes carrying malaria and dengue. However, malaria’s spread will probably have negligible impact on global eye health because its ocular complications are rare.
The indirect effects of global warming on ocular health will most likely result from extreme weather events and rising sea levels that will create a catastrophic and worsening cycle of water shortages, food shortages, natural diseases, and poverty. Research has shown a strong association between poverty and visual impairment. Below an income threshold of 10,000 USD per capita, Prof Casson said, the prevalence of blindness increases.
“Two-hundred years ago, 90% of the world’s population was in abject poverty. Now that figure is around 10%. Alleviating that last 10% will be a challenge,” he concluded. “But of all things, it is likely to have the most profound effect on reducing the prevalence of visual impairment. However, in the presence of climate change, we may see an unravelling of all that good work and a reversal of the trend of poverty reduction and age-related visual impairment.”
Prof Casson spoke at the virtual 2022 World Ophthalmology Congress.
The First Piece for Myopia Management, The Key Piece for Success

· Simply add it to your practice and your platform is ready for Myopia Management.


· Easy. Quick. Accurate.

· Visualize progression and treatment outcomes.
www.nidek.com

15 2023 MARCH | EUROTIMES
Robert J Casson MB.BS (Hons), MBiostats, DPhil, FRANZCO is Professor of Ophthalmology at the University of Adelaide and Vice Chair of Sight for All, North Adelaide, South Australia, Australia. robert.casson@adelaide.edu.au
Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol 2018;96(3):301-309. doi:10.1111/aos.13603
Optical Biometer
AL-Scan M
NEW
Trauma of War Laid Bare in Ukraine Focus Session
Surgeons deal with many complex challenges.
DERMOT MCGRATH REPORTS
Ukrainian ophthalmologists face a daunting array of challenges—medical, organisational, and logistical—trying to provide sight-saving care for its military and civilian population on the front line of its ongoing war with Russia.
The extent of these challenges, and the horrific toll on the Ukrainian people in devastating eye injuries incurred during the conflict, were described in graphic detail in a special session on ocular trauma at the 40th Congress of the ESCRS in Milan.

Andrii Ruban MD, PhD discussed the challenges of treating patients in a war zone, with specialised ophthalmic equipment often destroyed or damaged and a shortage of trained medical and support personnel, making it extremely difficult for clinics to function properly. He noted the medical challenges are primarily associated with the severity of operating on combat-related eye injuries.
“We encounter a high level of complex ocular polytrauma and a high level of association of ocular injuries with other head, neck, face, or systemic injuries,” he said. “There are delays in being able to treat patients due to the conditions of war and difficulties with evacuation. And the patients often have other life-threatening injuries that need to be treated first.”
The advanced fragmentation weapons used in modern conflicts result in a high rate of ocular trauma, Dr Ruban noted.
“Blast injuries are the most horrific thing I have ever encountered,” he said. “One in every three patients is blind in one eye, and one in every ten is blind in both eyes. The surgery is very challenging and requires knowledge of the anterior and posterior segments and oculoplasty skills as well.”
All of these factors, he added, can take a mental toll on the treating surgeon.
“The challenges for the ophthalmic surgeon are also psychological; There is a lot of stress, overload from working around the clock in difficult conditions, and dealing with the absence of family and friends while facing traumatic situations every day.”
The nature of the ocular injuries facing surgeons in Ukraine was described in detail by Ihor Novytskyy MD, who reported on 48 eyes of 42 patients treated at Lviv Military Hospital. The injuries included, among others, corneal trauma, iris damage, traumatic cataract, vitreous haemorrhage, intraocular foreign bodies, and retinal detachments.
“The majority of the eyes had combined damage of the different structures of the eye,” he explained. “Eleven patients had blunt trauma injuries, and 31 patients had penetrating eye injuries. Many of these patients will need to be reoperated in the future.”
Focusing on reconstructive surgery for combat eye injuries, Natalia Grubnyk MD pointed out that although February 2022 is considered the official start of the war with Russia, the conflict actually started with the annexation of Crimea by Russian forces in 2014. She expressed gratitude for ESCRS support—adding the supplies of ophthalmic equipment, including an endoscope, to the hospital where she works in Odesa has proven very helpful in treating eye injuries. She noted reconstructive vitreoretinal surgery timing remains a major problem due to difficulties evacuating and transporting patients, as well as the need for polytrauma treatment in other hospitals.
16 EUROTIMES | MARCH 2023
UKRAINE
Discussing cases of traumatic cataract in the Ukrainian military, Volodymyr Melnyk MD, PhD noted obtaining the best results in cataract surgery usually involves a combination of criteria difficult to obtain in a conflict scenario: a minimal corneal incision between 2.0 to 2.5 mm, undamaged capsular bag and ciliary band, and no penetration of vitreous into the anterior chamber, followed by IOL implantation corresponding to the patient’s needs at the greatest extent possible.
“Obviously it is not the same for all cases of traumatic cataract, but we still try to do our best for our patients to ensure they obtain the best outcome possible under difficult circumstances,” he said.
Traps to avoid
Ferenc Kuhn MD, PhD also underlined this point, discussing common traps to avoid when dealing with traumatic cataract. The initial traps are essentially diagnostic, he said.
“We have to be sure this is really a cataract and not perform cataract surgery unless the diagnosis is absolutely certain,” he stressed. “A second, more complicated diagnostic dilemma entails knowing whether the posterior capsule is intact or not, which goes unrecognised intraoperatively in about half of all operated eyes.”
Another key difference is traumatic cataract patients are invariably younger than standard cataract cases, which means a strong adherence between the posterior capsule and the anterior hyaloid, as well as between the anterior hyaloid and the peripheral retina.
“The risk, if phacoemulsification is employed, is that you may aspirate vitreous and put traction on the peripheral retina,” Dr Kuhn said. “The only way to really know if the vitreous has prolapsed is to use triamcinolone, which is not typically what cataract surgeons do.”
Andrii Ruban MD, PhD
President of the Ukrainian Vitreoretinal Society.
Ihor Novytskyy MD, PhD
Professor of Ophthalmology, Lviv National Medical University, Ukraine. inovytskyy@gmail.com
Volodymyr Melnyk MD, PhD
The Head of the Society of Ukrainian Ophthalmic Surgeons. suo.org.ua@gmail.com
Natalia Grubnyk MD
Ferenc Kuhn MD, PhD is a noted authority on ocular trauma with teaching positions in the United States, Poland, and Serbia. fkuhn@mindspring.com
Meet us at the ESCRS Winter Meeting 2023 :
Booth 33
MR-6000 Multifunction Unit
Get to know its excellent features
+ 6 in one: Ref, Kerato, Tono, Pachy, Topo, Dry Eye
+ Measurement cone interchange in just 4 seconds
+ Pupil and cornea ø measurement

+ Auto-alignment and auto-measurement
+ Quick refraction mode

+ Corrected IOP
tomey.de
17 2023 MARCH | EUROTIMES
Add-on IOLs Bring Added Benefits
Supplementary (“add-on”) IOLs designed for implantation into the sulcus provide a reversible solution for refractive enhancement after cataract surgery or when implanted during the primary surgery in a “duet” procedure to correct presbyopia, Oliver Findl MD told a recent conference.
Polypseudophakia was first described in 1993 and involved piggybacking a second standard IOL in the capsular bag to treat high hyperopia. However, postoperative problems such as interlenticular membrane formation—with opacification
and hyperopic defocus—meant a second IOL placement into the ciliary sulcus. But this technique was done using an IOL intended for implantation in the capsular bag, which resulted in complications including pigment dispersion, inflammation, elevated IOP, and haemorrhage.

“The idea then emerged to design an IOL optimised for sulcus implantation into the pseudophakic eye,” Dr Findl explained.
Currently, there are three commercially available add-on IOL models for refractive indications: Reverso (Cristalens), Sulco-
18 EUROTIMES | MARCH 2023 CATARACT & REFRACTIVE
CHERYL GUTTMAN KRADER REPORTS
Primary and secondary implantation procedures offer advantages to alternatives.
flex (Rayner), and 1stQ AddOn (Medicontour). All are made of biocompatible hydrophilic acrylic and feature a 6.5-mm optic that gives good overlap with the IOL in the bag while avoiding iris optic capture. In addition, they have round optic edges to minimise dysphotopsia risk, a concave posterior surface to avoid contact with the IOL in the bag, and haptics designed to provide good centration, rotational stability, and uveal clearance. Available optic designs include aspheric monofocal, refractive and diffractive multifocal, toric, and multifocal toric.
Published data from clinical and cadaver eye studies show the add-on IOLs are associated with good refractive outcomes and safety profiles. A study of the Sulcoflex IOL showed its centration was better than that of the in-the-bag IOL. A bench study comparing optical quality of a single trifocal in-the-bag IOL with a trifocal add-on IOL plus an in-the-bag monofocal IOL found no difference between the two systems.
Consistent with the good visual outcomes, studies evaluating the add-on IOLs also show good and stable centration. However, a study of eyes implanted with a toric add-on IOL found rotation in 10% of cases.
“A toric add-on IOL can be suture fixated in the sulcus. However, this is a little tricky, and surgeons would prefer not to have to do that,” Dr Findl said.
Surgical planning and performance
In cases of secondary implantation to correct postoperative ametropia ±7.0 D of target, the IOL power calculation is simple as the patient’s current refraction can serve as the base, he noted. The patient’s spherical equivalent is multiplied by 1.5 in cases of hyperopia or by a factor of 1.2 for myopia. The R-vergence formula, which incorporates values for keratometry and anterior chamber depth in addition to the spherical equivalent, can serve as an alternative.
Dr Findl observed implanting the add-on IOL is also straightforward. In a duet procedure, after the primary IOL is implanted into the bag and viscoelastic removed from inside the capsule bag, more viscoelastic is placed under the iris to open the sulcus. An injector or forceps delivers the add-on IOL through a 2.4-mm or slightly smaller incision. Once positioned, viscoelastic is aspirated, with special attention directed to removing the material from the interface between the two lenses.
Implanting an add-on IOL in a secondary procedure to correct ametropia or explanting or exchanging an existing add-on IOL are also easier and less risky procedures than exchanging an IOL in the capsular bag.
“If a patient with a multifocal add-on IOL is troubled early on by dysphotopsia or a lack of neuroadaptation, surgeons simply need to reopen the incision and remove the lens,” Dr Findl said. “The add-on lens can also be easily removed years later if needed because of pathological changes, such as the development of age-related macular degeneration or diabetic macular oedema.”
Dr Findl presented during the AAO 2022 Refractive Surgery
Subspecialty Day meeting in Chicago, US. He spoke on behalf of Michael Amon MD, PhD, Vienna, Austria, inventor of a commercially available add-on IOL platform.
Oliver Findl MD is the Chair of the Department of Ophthalmology, Hanusch Hospital, Vienna, Austria. He is current president of the ESCRS. oliver@findl.at
Michael Amon MD, PhD is Head of the Department of Ophthalmology
Academic Teaching Hospital of St. John Chair for Ophthalmology at Sigmund Freud Private-University in Vienna, Austria. amon@augenchirurg.com
19 2023 MARCH | EUROTIMES
The idea then emerged to design an IOL optimised for sulcus implantation into the pseudophakic eye.
Image credit: Michael Amon MD, PhD, 2023.
Capsular Tension Rings and Toric IOLs
CTR may not affect rotation but may increase tilt and decentration.
Capsular tension rings (CTR) are designed to increase the stability of intraocular lenses in the capsular bag, particularly in eyes with weak or damaged zonules. However, a study of rotation, tilt, and decentration of a plate haptic IOL found no overall difference in rotation between lenses implanted with or without a CTR, while tilt and decentration were actually higher in the CTR group.
Daniel Schartmüller MD and colleagues conducted a prospective randomised study involving 130 eyes of 65 patients. Each patient randomly received an 11.00-mm Zeiss 409M plate haptic IOL and an Ophtec CTR 276 13/11 in one eye, and the lens only in the fellow eye. All patients were in treatment for bilateral, age-related cataract and had no other relevant ocular disease.

Regarding rotation, no lens in the CTR group rotated more than 5 degrees in the first hour after surgery, while four non-CTR lenses did, with one rotating nearly 24 degrees. Mean rotation was 1.3 degrees in the CTR group and 2.1 degrees in the non-CTR group, though the difference was not statistically significant. Mean rotation was also similar between the two groups at one week, one month, and six months after surgery, though there were more outliers in the non-CTR group at one month.


130 eyes
of 65 patients. Each patient randomly received an 11.00-mm Zeiss 409M plate haptic IOL and an Ophtec CTR 276 13/11 in one eye, and the lens only in the fellow eye. All patients were in treatment for bilateral, age-related cataract and had no other relevant ocular disease.
“There was no difference in mean absolute rotation, but there was a significantly lower proportion of outliers in the CTR group,” Dr Schartmüller said. “There was no correlation between absolute overall rotation and lens thickness, axial length, and lens equatorial diameter. A decrease in rotation in the CTR group was observed within the first postoperative hour.”

20 EUROTIMES | MARCH 2023 CATARACT & REFRACTIVE
HOWARD LARKIN REPORTS
Mean6.66°±2.77° Min1.5° Max 17.7° Temporal Mean5.55°±1.60° Min2.50° Max9.20° Temporal p=0.009 +CTR -CTR
Lens Tilt at 6m
IOLs tilted more with CTRs than without.
Fibrosis increases tilt and decentration

Lens decentration and tilt were secondary results, he add ed. Both were measured in absolute terms and compared with measurements of tilt and decentration of the crystal line lens before surgery.
Six months after surgery, mean absolute decentration in the CTR group was 0.28 mm and in the non-CTR group 0.24 mm, which was not statistically significant. Howev er, compared with preoperative measurements, the CTR group was significantly more decentred at a mean of 0.29 mm compared to 0.18 mm in the non-CTR group. The decentration increased at one month and six months after surgery as capsular shrinkage set in, Dr Schartmüller said.
Mean tilt in the CTR group was 6.66 degrees compared with 5.55 degrees in the non-CTR group six months after surgery, a statistically significant finding the group found. Tilt increased more in the CTR group as the capsule shrunk. There were also more outliers in the CTR group, with lenses tilted up to 17.7 degrees in the same period.
“We see a negative impact on decentration and tilt when using a capsular tension ring with an 11.00-mm plate haptic IOL,” he concluded.
Dr Schartmüller was awarded first prize in the cataract category for this poster at the 2016 ESCRS Congress in Copenhagen and presented as the “best of the best” at the 40th Congress of the ESCRS in Milan.
Compact and Comprehensive Powerful but Handy
• More powerful and effective phacoemulsification with torsional ultrasound oscillation
• Improved fluid dynamics and anterior chamber stability
Product/model name: Ophthalmic Surgical System CV-9000R www.nidek.com

21 2023 MARCH | EUROTIMES
NEW
Daniel Schartmüller MD is an ophthalmologist and researcher at Medical University of Vienna, Austria. daniel.schartmueller@meduniwien.ac.at
Torsional Technology
ET 93 x 266mm
New IOL Underscores Importance of Peripheral Vision

Inverted meniscus design now in clinical trials.
Anew inverted meniscus-shaped intraocular lens (ArtIOL, Voptica SL) successfully reduces oblique astigmatism and provides improved peripheral vision compared to a standard IOL, according to Pablo Artal PhD.
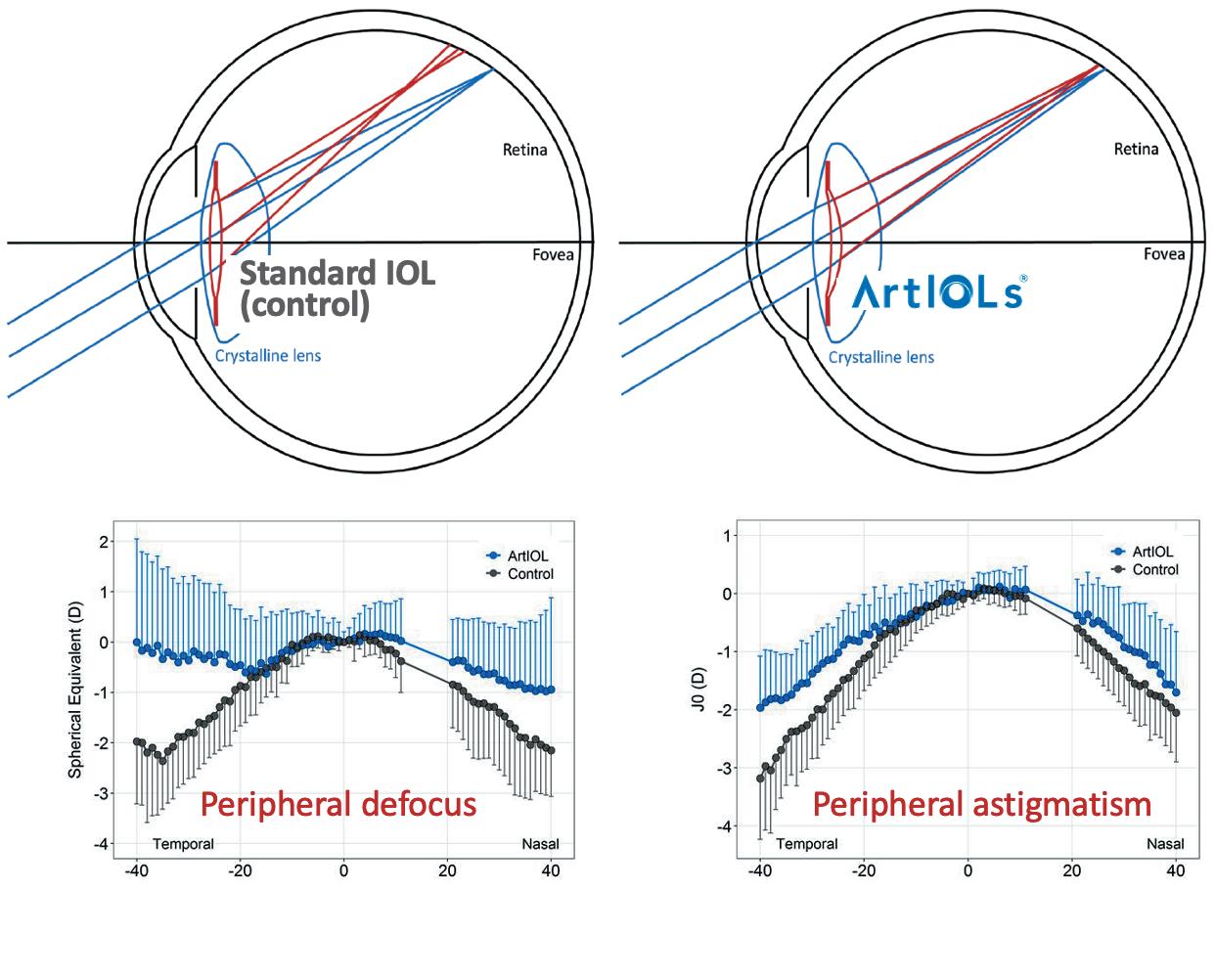
“Current IOLs typically degrade the optical quality at the peripheral retina, thereby compromising quality of vision,” he said. “The inverted meniscus IOL more closely mimics the optics of the natural crystalline lens, reduces astigmatism, and improves peripheral vision, which may help to improve safety and quality of life after cataract surgery.”

Dr Artal explained that interest in the eye’s optical quality has traditionally focused on the central fovea area of the retina, with little attention paid to the peripheral retina.
“The reality is peripheral vision is extremely important for driving and many activities in daily life,” he said. “Our natural eye has pretty good resolution in the centre and less so in the periphery, but this low-resolution information is still extremely useful for our day-to-day activities.”
The optics of the natural eye are compromised at the periphery, but Dr Artal noted this is rarely perceptible.
“We all have around 5.0 D to 7.0 D of astigmatism at 40 degrees, but we don’t complain about it as the photoreceptors and neural sampling limits our vision. So, our natural eye is beautifully adapted to our retinal capabilities,” he said.
Making the most of peripheral vision
Standard biconvex IOLs provide a wrong field curvature with additional defocus blur and increased peripheral astigmatism compared with the optics in a normal eye with the crystalline lens intact. This leads to compromised vision and a potential increased risk of falls, poor object recognition, and driving difficulties.
“We have to bear in mind the peripheral optics were already bad in a normal eye. Therefore, it is even worse in a pseudophakic eye,” Dr Artal said.
To address this issue, Dr Artal developed the ArtIOL—a single-piece, foldable lens with a square-edge design and UV and blue light filter delivered through a 2.2-mm incision.
“It’s a standard lens in all respects—apart from the inverted meniscus design,” he said, adding optical bench testing of the lens has shown promising results in its ability to correct the optics of the pseudophakic eye and improve peripheral vision. A recent clinical study reported patients implanted with the ArtIOL showed reduced amounts of peripheral defocus and astigmatism compared to patients implanted with standard biconvex IOLs. A better contrast sensitivity in the periphery was also reported for the patients implanted with ArtIOLs.
More than 2,000 ArtIOLs have been implanted already, Dr Artal said, with excellent results for the patients. He concluded that as the population ages and the prevalence of cataracts increases, developing better IOLs that improve overall vision, including peripheral vision, will be important for maintaining independence and quality of life.
22 EUROTIMES | MARCH 2023 CATARACT & REFRACTIVE
Dr Artal presented at the 40th Congress of the ESCRS in Milan.
Pablo Artal PhD is a professor of optical physics at the University of Murcia, Spain. pablo@um.es
DERMOT MCGRATH REPORTS
The results and schematics on peripheral defocus and astigmatism in a group of patients with ArtIOLs and standard IOLs.
Images obtained in a model eye with a standard biconvex lens and ArtIOL.
Research. Education. Innovation.
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Rethinking Fuchs’ Dystrophy
New ideas on its aetiology, characteristic features, and relationship with POAG.
CHERYL GUTTMAN KRADER REPORTS
Renowned cornea specialist Gerritt RJ Melles MD, PhD was having difficulty reconciling teachings found in textbooks with clinical observations regarding corneal perfusion and hydration mechanisms, corneal endothelium’s role in maintaining stromal imbibition pressure, and the aetiology of primary open-angle glaucoma (POAG) development.
In the 79th Jackson Memorial Lecture delivered at the American Academy of Ophthalmology annual meeting, he proposed Fuchs’ dystrophy should not be considered an endothelial disease. Instead, he suggested it may be a mucopolysaccharide disorder.

Dr Melles also speculated similarities in the pathogenesis of POAG and Fuchs’ dystrophy, wherein both might develop as remedy responses to some factor that triggers an overreaction without inflammation. Proposing Fuchs’ dystrophy is characterised by an imbibition pressure level that is too high (too negative), he introduced the idea it may actually be a “corneal glaucoma”.
“Reframing Fuchs’ dystrophy in this different way might actually be the gateway to understanding POAG aetiology,” Dr Melles said.
He reviewed several clinical situations that are inconsistent with the concept that corneal physiology and nutrition are maintained via a localised fluid circulation over the endothelial cell layer in which there is active outflow through the endothelial cell pump that creates a negative imbibition pressure within the corneal stroma that in turn allows for passive leakage of aqueous into the cornea.
Diagrammatic representation of (top) the corneal hydration mechanism as described in the literature, with active outflow through the endothelial cell pump that creates a (negative) imbibition pressure within the corneal stroma, which in turn allows for passive leakage of aqueous into the cornea; and (bottom) the dynamic and static corneal hydration mechanisms as suggested by clinical observation, potentially consisting of a horizontal flow of nutrients and depositions originating from the limbal vascular arcade. Image NIIOS.

“It seems a very ineffective way to perfuse the cornea,” he noted.
As an alternative, he proffered the existence of a much more sophisticated system to explain corneal nutrition, hydration, and transparency. He suggested combined dynamic and static flow mechanisms—described respectively by horizontal perfusion from the limbal vascular arcade into the cornea— provide nutrition regardless of the endothelial condition and vertical control of imbibition pressure, maintaining transparency and involving the mucopolysaccharide rods that run throughout the cornea to its surface.
CORNEA 24 EUROTIMES | MARCH 2023
Reframing Fuchs’ dystrophy in this different way might actually be the gateway to understanding POAG aetiology.
AC-OCT image of a cornea one week after DMEK. Note that the corneal centre has cleared (dashed lines), while the paracentral to peripheral areas are still oedematous due to partial graft detachment (arrows) or the relative short postoperative time interval. This cornea may illustrate how an area with normal pachymetry values (normal imbibition pressure) can border adjacent areas with various degrees of oedema (imbibition pressure low or zero). Image NIIOS.

Dr Melles presented new perspectives on the interaction between the cornea and IOP and the pathomechanism for POAG, starting with a consideration of the relationship between IOP and imbibition pressure.
He offered ideas to explain what he termed “the paradox of Fuchs’ dystrophy”, i.e., imbibition pressure is normal despite an absent or compromised endothelial layer and the mechanism for guttae formation.
“If there is a link between the imbibition pressure and IOP, there must be a similar feedback loop controlling them in a similar way,” Dr Melles said, tying the new perspectives together. “It would stand to reason that if we understand how the imbibition pressure is controlled, that may open the door to understanding how IOP is controlled and why you get POAG.”
As a caveat, however, he indicated at the start and the end of his lecture that his new ideas should not be considered the definitive word. He prefaced the material by noting that his presentation would include a lot of “buts, ifs, maybes, and things that are very speculative.”
Observing Professor Fuchs seemed to have “missed” the endothelium, Dr Melles asked, “What are we missing today that we will be mocked for in 100 years when they ask, ‘Why didn’t they think of…fill in the blank?’”
Diagrammatic representation of a “vertical” mucopolysaccharide rod organisation, possibly explaining clear and oedematous areas within the same cornea. Because the oedema is always confined to the area overlying an endothelial defect, the corneal stroma should contain a barrier to a horizontal flow of fluid. In the absence of an anatomical structure, the mucopolysaccharide rods could be organised in such a way that horizontal fluid dispersion cannot occur, for example through separated mucopolysaccharide bundles. Image NIIOS.
He invited attendees to access his complete essay describing his new perspectives in detail and the clinical observations on which they are based by visiting his organisation’s homepage at www.niios.com under JML lecture.

25 2023 MARCH | EUROTIMES
Gerritt RJ Melles MD, PhD is Director, Netherlands Institute for Innovative Ocular Surgery, Rotterdam, Netherlands. melles@niios.nl
Studies Shed Light on Long-Term Cross-Linking Outcomes
New software helps evaluate progression.
DERMOT MCGRATH REPORTS
Long-term studies of corneal cross-linking (CXL) for keratoconus treatment are providing clinicians with valuable information about the enduring safety and efficacy of different CXL protocols while underscoring the need for better definitions of disease progression, according to Riccardo Vinciguerra MD.

Reviewing the evidence from the studies with more than 10 years of follow-up, Dr Vinciguerra said CXL using the standard Dresden protocol is safe with low to intermediate progression rates.
“Based on the current evidence, we can confidently tell our patients older than 18 years old that the treatment is safe and well tolerated over the long term, with a progression rate below 10%,” he said.
One of the key issues in comparing outcomes from different studies is the lack of an agreed definition of keratoconus progression.
“There is a lack of consensus regarding the definition of progression—even preoperatively—never mind after CXL,” Dr
Vinciguerra noted. “We have a difference in the repeatability of measurements for assessing progressive disease at different stages, and this difference is accentuated after CXL treatment.”
More recently, the integration of the Belin ABCD progression display system in the native Pentacam® (Oculus) software has helped clinicians evaluate disease progression before and after CXL.
The ABCD software evaluates average anterior (A) and posterior curvature (B) values in a 3-mm optical zone centred on the thinnest point of the cornea and in the thinnest
CORNEA 26 EUROTIMES | MARCH 2023
We can confidently tell our patients older than 18 years old that the treatment is safe.
34% 21%
pachymetry (C). The software also shows 80% and 95% confidence intervals (CI) for normal and keratoconic populations. The “D” value is Snellen corrected distance visual acuity, entered manually in the Pentacam software.
The ABCD Progression Display graphically presents each parameter and shows when statistical change above measurement noise is reached using colour-coded maps. A recent upgrade to the system enabled the addition of confidence intervals for post-CXL changes to the progression display.
“Our definition for progression after CXL was at least two out of three of the following criteria: progression of A parameters more than 95% CI compared to baseline; progression of B more than 95% CI compared to baseline; and reduction of minimal pachymetry of at least seven microns compared to baseline and 95% CI,” he said.
Using these criteria, two out of 27 eyes of 22 patients (7.4%) showed significant progression with a mean follow-up of 11 years. Dr Vinciguerra said the study showed the value using a combined progression system that evaluates anterior and posterior curvature and thickness map together with the knowledge of the testing system noise level.

Epi-off CXL also achieved good safety and efficacy in 38 eyes of 24 paediatric patients with up to 14 years of follow-up.
“Based on the same criteria for failure using the ABCD Progression Display, 34% of the cases progressed,” he said. “However, the figure was only 7.1% if considering only the anterior curvature (A values) and our results are broadly in line with those of Mazzite [et al.] who reported a 24% progression rate over 10 years in paediatric patients.”
Dr Vinciguerra also presented data for transepithelial iontophoresis-assisted CXL (I-CXL) in 19 eyes of 19 patients and a maximum of seven years of follow-up.
“Our study showed I-CXL was able to stop K progression in most cases with 21% progression rate. However, it is important to note that if we had based our definition on the event of repeat CXL or transplant, only one patient would have progressed, and based on a change of 1.0 D of Kmax, only two patients would have progressed,” he said.
27 2023 MARCH | EUROTIMES
Dr Vinciguerra presented at the 40th Congress of the ESCRS in Milan.
Riccardo Vinciguerra MD is an ophthalmologist and scientific responsible at the the Humanitas San Pio X Hospital, Milan, Italy, as well as a research collaborator at Biochemical Engineering Group, University of Liverpool, United Kingdom. vinciguerra.riccardo@gmail.com
Based on the same criteria for failure using the ABCD Progression Display, 34% of the cases progressed.
The study showed I-CXL was able to stop K progression in most cases with 21% progression rate.
Corneal Regeneration
Umbilical cord stem cells a potentially limitless source of corneal endothelial cells.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Advances in stem cell culture techniques could make human umbilical cords a valuable asset in treating corneal endothelial disease, said Jie Zhang PhD.
Dr Zhang noted in research she and her associates have carried out at the New Zealand National Eye Centre, cultured umbilical cord stem cells show promise as an alternative source for corneal endothelial cells.
“We are optimistic about the future of umbilical cord stem cells for corneal regeneration,” she said. “Improved isolation methods have resulted in reliable cultures, and we have demonstrated the potential to generate multiple corneal cell types from one piece of tissue.”
So far, their research shows umbilical cord mesenchymal stem cells and human umbilical vein endothelial stem cells can potentially differentiate into keratocytes and corneal endothelial cells. Unlike donor corneas, umbilical cords are usually discarded after birth, providing an abundant supply for use. Moreover, the cells are immunologically naïve and proliferate well.
A human option
One study led by Ms Annany Parvathi isolated umbilical cord cells obtained from Wharton’s jelly, a gelatinous substance within the umbilical cord, with all the characteristics of mesenchymal stem cells (MSCs). Flow cytometry showed the cells expressed positive markers for MSCs and no negative markers, which immunochemistry and gene expression analysis confirmed, Dr Zhang said.
When the team injected the cultured umbilical cord MSCs into the stroma of decellularised human corneal buttons, the cells migrated and repopulated the buttons. Moreover, three months after implantation, the cells expressed keratocyte genes as well as negative MSC markers, suggesting a shift away from MSC phenotype towards keratocyte phenotype.
Human umbilical vein endothelial cells (HUVECs) may provide another source for corneal endothelial cells, Dr Zhang noted. Research carried out by Ms Amnol Sandhu has developed a technique to culture a high yield of HUVECS with their characteristic cobblestone morphology and positive markers for endothelial cells.
Moreover, when cultured in conditioned media from a corneal endothelial cell line, the cells differentiated into rounder ones resembling corneal endothelial cells. They also had positive markers for zonula occludens-1 (ZO-1), a tight junction protein essential for the corneal endothelium’s barrier function.
“The results suggest HUVECs have the potential to be differentiated into corneal endothelial cells if we work on the culture a bit more,” Dr Zhang added. “Ms Sandhu is now working on identifying the factors in conditioned media that drove the differentiation and hopefully coming up with a more targeted differentiation approach.”
Five phase 2 and 3 trials using umbilical cord mesenchymal stem cells for retinitis pigmentosa and neuromyelitis optica treatment and one phase 2 trial using cord blood red blood cell concentrates for retinopathy of prematurity are underway.

“Further studies are required to determine safety and efficacy of umbilical cord stem cells for corneal disease.”



An alternative option
Yet another potential source of corneal endothelial cells are the transition zone cells from limbal rims, obtainable from corneas of donors of any age, Dr Zhang said. She noted research performed by Dr Hannah Au MBChB and Dr Jane Shi MBChB found a 62% success rate in culturing the cells. They have also found they can expand, or passage, the cultures two to six times more than endothelial cells, potentially yielding enough cells for 5,000 epithelial keratopathy patients from one donor cornea.
Transition zone cells express two essential corneal endothelial proteins, the tight junction protein ZO-1 and sodium potassium ATPase, and the neural crest protein nestin, consistent with adult stem cells for the corneal endothelium.
CORNEA 28 EUROTIMES | MARCH 2023
We are optimistic about the future of umbilical cord stem cells for corneal regeneration.
After three to six months in base culture, they spontaneously become endothelial-like. But to be of practical use, the cells would need to differentiate into endothelial cells at an earlier passage.
The team compared eight cell culture treatment protocols to find a speedier process for achieving the desired cell differentiation. The cell culture treatments involved combinations of Rho-kinase inhibitors and differentiation inducers.

Within seven days of treatment, the transition zone cells treated with a combination of the Rho-kinase inhibitor Y-27632 and the TGF-B inhibitor SB-431542 had rapidly become less fibroblastic in appearance compared to cells in cultures receiving other treatments or no treatment. The cells also scored highest in circularity and had reduced expression of nestin and an increased expression of corneal endothelial proteins.
“This suggests a differentiation of cells towards corneal endothelial cells, and the results suggest transition zone cells have the potential to become an alternative source of corneal endothelial cells,” Dr Zhang said.



Dr Zhang presented her paper at the 40th Congress of the ESCRS in Milan.
Jie Zhang PhD is based at the New Zealand National Eye Centre, Department of Ophthalmology, University of Auckland, New Zealand. jie.zhang@auckland.ac.nz


The new OS 4 marks the beginning of the next generation of retina, glaucoma and cataract surgery. The all-in-one platform has received numerous exciting features that provide even more comfort, precision and safety.


Laser integration: More safety, fully automated user protection filter
Light: 45% more power*, maximum visibility


Pedal: Multifunctional with over 100 setting options
Phaco: Speedier readiness, greater controllability





User comfort: Even more userfriendly and communicative





Make the difference –with the new OS 4: www.oertli-instruments.com


29 2023 MARCH | EUROTIMES
EYE SURGERY. SWISS MADE.
Not available for sales in the US *Oertli data on file
FEATURE
OS 4TM THE NEXT GENERATION NEW
Better Before or After?
Differing perspectives on the potential risks and benefits underlie opposing views on appropriateness of treating corneal neovascularisation prior to keratoplasty.
CHERYL GUTTMAN KRADER REPORTS
Ophthalmologists know corneal neovascularisation increases the risk of graft rejection and failure after penetrating keratoplasty. Available evidence documenting the various treatments for inducing regression of existing corneal vessels are at least partially effective. Yet, treating corneal neovascularisation before keratoplasty remains controversial among cornea specialists who hold differing views.
In a recent debate, Irit Bahar MD, MHA acknowledged there is no gold standard approach for treating corneal neovascularisation. She observed that some methods are still experimental, so long-term follow-up and prospective studies are mandatory. However, Dr Bahar said she typically treats it before keratoplasty because she believes it simple, safe, and at least partially effective for inducing blood vessel regression and improving graft outcomes.
“Even partial regression is better than none, especially when the risk of the treatment is low and the side effects are negligible,” she said. “And I promise you that the vessels will not disappear by simply ignoring them.”
Lack of data?
Taking another view, Jennifer Li MD said she does not treat corneal neovascularisation before keratoplasty, citing the lack of long-term data and safety concerns.
“Most of what has been tried had limited and variable success long-term. In particular, there are limited data for newer or combination therapies, and some of the potential side effects of the various options terrify me,” she said.
“If the benefit of the treatment [for inducing vessel regression] lasts only three to six months, how much effect will we see that it has long term?”
CORNEA 30 EUROTIMES | MARCH 2023
Rationale for treating
Dr Bahar noted the long list of treatments tried over the years to induce corneal blood vessel regression before transplantation indicates there is no ideal method. However, each has induced some vessel regression and some to improve highrisk corneal graft surgery outcomes.
As an example, Dr Bahar cited a report describing five patients treated with corneal cross-linking before penetrating keratoplasty—among whom there were no cases of revascularisation, graft opacification, or immune rejection during 4 to 42 weeks of follow-up.
Graft survival results better than expected were also reported by investigators reviewing their experience with fine needle diathermy combined with subconjunctival bevacizumab. Very recently, promising results were obtained using mitomycin intravascular chemoembolisation to treat corneal neovascularisation.
For more than a decade, Dr Bahar said she has been injecting bevacizumab 2.5 mg/0.1 mL per affected quadrant at the limbus at the end of the graft procedure in high-risk cases. She reported that in a series of 20 patients, vessel regression was observed in all eyes, 19 grafts remained transparent for 24 months, and no side effects were observed.
In a recent case, she injected mitomycin-C into superficial vessels before placing ligation sutures over the two main feeder vessels because she observed only partial vessel bleaching. She presented images showing an “impressive outcome” after two months.
Reasons not to treat
Dr Li reviewed the efficacy and safety of various corneal neovascularisation treatments to support her reasons for not treating corneal vessels beforehand. Any benefit of laser thermal cauterisation, she said, is limited mainly to efferent vessels. A 37% recanalisation rate at three months has also been reported. The inherent destructiveness of the thermal procedure risks collateral damage to the cornea, limbal stem cells, crystalline lens, and iris. It also risks damage that can promote collateral vessel development.
She said photodynamic therapy appears to be the most effective of the laser treatment options and is relatively safe. However, it also induces a rebound effect secondary to enhanced VEGF expression and is very expensive and time-consuming.
A frequent need for retreatment is also a limitation of fine needle diathermy, which can be associated with significant adverse events and the potential to stimulate new vascularisation. Treatment with anti-VEGF agents has gained attention based on their use for retinal vascular diseases. But Dr Li warned of a limited window for therapeutic utility because they are not effective in clearing mature blood vessels.
“VEGF inhibitors used topically have limited penetration and so are not very effective on deeper vessels,” she said. “Subconjunctival injection is invasive, has limited effect on vessels in the central cornea, and associated with a 35% recurrence rate in one study. In addition, adverse events can occur, including corneal stromal cytotoxicity with thinning and melting.”
Adding intravascular mitomycin treatment of corneal vessels has featured heavily on the Cornea Society’s online resource, Dr Li agreed the preliminary results are very promising.
“However, data on this modality is very limited,” she said. “There are questions about whether it can be used with corneal transplantation, and there is the potential for some severe adverse events with mitomycin.”
The debate took place at the AAO annual meeting in Chicago, US.
31 2023 MARCH | EUROTIMES
Irit Bahar MD, MHA is Chief of the Department of Ophthalmology, Rabin Medical Center, Petah Tiqwa, Israel, and Full Professor of Ophthalmology at Tel Aviv University, Israel. iritbahar@gmail.com or iritba2@clalit.org.il
Jennifer Li MD is Director, Cornea and External Disease Service and Professor, Department of Ophthalmology, UC Davis Health Eye Center, Sacramento, California, US. jyhli@ucdavis.edu
Even partial regression is better than none, especially when the risk of the treatment is low and the side effects are negligible.
Endothelial Cell Injection
Cultured cell therapy a promising alternative to keratoplasty procedures for endothelial failure.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Eyes with corneal dystrophies that undergo a promising cell therapy can achieve clear corneas with endothelial cell density superior to that achieved with endothelial keratoplasty procedures or penetrating keratoplasty, reports Shigeru
Kinoshita MD, PhD.
“We think CHCEC injection therapy may be the future for corneal endothelial failure,” he said.
The therapy involves intracameral injection of mature-differentiated cultured human corneal endothelial cells (CHCEC) derived from very young donor allogeneic cells in combination with the Rho-kinase inhibitor, Y-27632. With this technique, one donor cornea makes it possible to create enough CHCECs for 300 eyes.
The cells are also cultured with Y-27632, which promotes the proliferation of the mature corneal endothelial cells most suitable for restoring the corneal endothelium. Prof Kinoshita and his team have refined their technique to ensure nearly 100% of cells in the cultures are of the mature effector cell type.
A preliminary clinical trial using CHCEC suspensions with lower percentages of mature cells yielded satisfactory results in corneal clarity and endothelial cell loss. However, eyes receiving the suspensions with more than 90% mature cells had faster rehabilitation and much higher endothelial cell density.
In the first trial, 11 eyes of 11 bullous keratopathy patients underwent intracameral injection of CHCECs, in which less than 90% of cells were of the pure type. By 24 weeks after injection, 10 of 11 eyes had restoration of corneal transparency with a CHCEC density of greater than 1,000 cells/mm2. At three years, 10 eyes had clear corneas with improved BCVA, and the mean endothelial count of 1,257 cells/mm2 at five years was close to that reported in eyes undergoing Descemet membrane endothelial keratoplasty (DMEK) or Descemet stripping automated endothelial keratoplasty (DSAEK).
To perform the cell injection procedure, Prof Kinoshita and his team first placed the eye under local anaesthesia before removing the central corneal epithelium by mechanical rubbing. Making a 1.6-mm incision at the limbal corneal junction, they gently scraped any abnormal material on Descemet’s membrane with a silicone cannula irrigation needle.
After injecting the Y-27632 solution into the anterior chamber, they fixed the incision site with a 10-0 nylon suture and, using a syringe with a 26-gauge needle, injected a 300 microlitre suspension containing a million CHCECs through the limbus and into the anterior chamber. Patients were asked to lie face down for three hours after the procedure.

Prof Kinoshita noted the team performed the CHCEC injection procedure in 65 eyes, including 20 patients with a broadened range of indications, such as corneal endothelial failure after the penetrating keratoplasty. Phase II and phase III trials involving 27 patients are complete. Aurion Biotechnologies Japan submitted the official documents, including his group’s clinical data, to the Pharmaceuticals and Medical Devices Agency (PMDA)—the Japanese equivalent of the FDA—and hope to receive approval soon.
Seven eyes underwent intracameral injection of suspensions of cultures in the second trial, in which more than 90% of cells were very mature. At four weeks follow-up, corneal epithelial oedema completely cleared in all seven eyes, compared to only four of the 11 eyes by that time in the first trial. Additionally, endothelial cell density was more than 3,000 cells/mm2 at 24 weeks, with little decay over three years.i
“We’ve never seen such high endothelial cell density after DSAEK, DMEK, or penetrating keratoplasty,” he said.
i M Ueno et al, American Journal of Ophthalmology , 2022; 237: 267–277.
CORNEA 32 EUROTIMES | MARCH 2023
Prof Kinoshita presented his research at the 40th Congress of the ESCRS in Milan.
Shigeru Kinoshita MD, PhD is Professor and Chair of Frontier Medical Science and Technology for Ophthalmology at Kyoto Prefectural University of Medicine, Kyoto, Japan. fmstoph@koto.kpu-m.ac.jp
We think CHCEC injection therapy may be the future for corneal endothelial failure.
33 2023 MARCH | EUROTIMES Educational Resources Advanced FEBOS-CR Exam/Diploma (Cataract and Refractive Surgery) ESCRS iLearn • ESCRS Research Portals • Important Publications ESCRS EuroTimes Podcasts • ESCRS on Demand • JCRS Online Case Reports The Video Journal of Cataract, Refractive, and Glaucoma Surgery escrs.org/education/educational-resources
Surgery for Patients with Symptomatic Cataract and Ocular Hypertension
Glaucoma experts debate phacoemulsification alone versus adding MIGS.
 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS
The availability of an array of minimally invasive glaucoma surgery (MIGS) procedures raises the question of whether surgeons should add one of these modalities when performing phacoemulsification for a patient with symptomatic cataract and ocular hypertension (OHT).
In a pro/con discussion, Andrew J Tatham MD spoke in favour of phacoemulsification alone, while Simonetta Morselli MD argued for adding MIGS to standard phaco surgery.
Phacoemulsification alone
Opening the session, Dr Tatham named six reasons surgeons should perform phacoemulsification alone. He explained the risk for progression to glaucoma is low for most patients, and IOP lowering may not be needed. If it is, it may be achieved with phacoemulsification alone or subsequently with nonsurgical options (medications or selective laser trabeculoplasty [SLT]). In addition, the long-term efficacy of MIGS is uncertain, and it is not without risks.
“Keep calm and play the long game,” Dr Tatham advised. “Lifetime risk of glaucoma is often low for patients with OHT, and there is a lack of evidence to support performing MIGS in patients with cataract and OHT.”
He cited findings from the landmark Ocular Hypertension Treatment Study (OHTS) to support his reasons, indicating a low risk of OHT progressing to glaucoma.
“At 5 years, more than 90% of untreated patients in the OHTS did not have glaucoma, and at 13 years, almost 80% of patients allocated to observation still did not have glaucoma,” he said.
As a caveat, Dr Tatham noted the need to individualise target IOP and treatment. While calculators for estimating glaucoma risk help, it is imperative to remember the information is an estimate only of the likelihood of developing glaucoma.
“It might be early glaucoma that is not visually significant and not affecting quality of life,” Dr Tatham said.
The OHTS is among other studies and systematic reviews providing evidence phacoemulsification alone can lower IOP. For example, in a subset of OHTS eyes that underwent phacoemulsification, IOP reduced by an average of 4 mmHg or 17% at follow-up at three years.
Furthermore, systematic reviews show the IOP reduction after phacoemulsification in eyes with primary open angle glaucoma (POAG) is modest and declines over time. Similarly, the European Glaucoma Society (EGS) guidelines state reductions in IOP and medications with phacoemulsification in eyes with OAG are typically small. EGS guidelines also do not recommend cataract surgery alone as an intervention to control OAG.
“However, the guidelines do not comment at all on cataract surgery in OHT,” Dr Tatham said.
Discussing the limited information on long-term efficacy of MIGS, Dr Tatham observed that five years is the longest follow-up for randomised controlled trials. Real-world data are available, however, and he cited a study of patients followed for seven years after implantation of two first-generation iStents (Glaukos) combined with phacoemulsification. While IOP reduction sustained over time, the average number of medications used increased.
“The most interesting thing in this study is that 27% of patients died during the follow-up, emphasising it is important to incorporate life expectancy into glaucoma care,” Dr Tatham said.
“We need to avoid cost and side effects of excessive treatment and remember MIGS is only FDA-approved for patients with mild to moderate POAG.”
To highlight the risks, Dr Tatham mentioned the market withdrawal of the CyPass Microstent (Alcon), found to cause significant endothelial cell loss in patients followed out to five years.
“A limited number of MIGS studies have reported endothelial cell loss beyond two years,” Dr Tatham observed.
Reasonable IOP-lowering alternatives
If patients need IOP lowering after undergoing phacoemulsification alone, Dr Tatham advised SLT as a good option. It has a strong recommendation from the EGS as a first-choice OAG treatment. And after three years in the LiGHT study, SLT was shown effective for maintaining target IOP without medication in 74% of eyes and appeared to reduce the need for filtering surgery.
Topical therapy is also a viable modality.
“Drops get bad press, but a European survey of 793 glaucoma patients found most were satisfied with topical therapy,” he explained. “Admittedly, 91.5% of patients were on monotherapy and 25% were using tear substitutes.”
Although Dr Tatham provided multiple reasons why surgeons should perform phacoemulsification only for patients with symptomatic cataract and OHT, he suggested MIGS might have a role if the individual’s glaucoma risk is very high and other circumstances exist.
“If a patient has all of these factors—very high IOP, SLT was not effective, inability to instill drops, drop intolerance, and field loss in the fellow eye—perhaps MIGS is reasonable,” he said.
Safety and efficacy of MIGS
Reviewing the dual procedure, Simonetta Morselli MD identified factors that could favour adding MIGS to cataract surgery, but noted there are cons to consider.
Dr Morselli defined MIGS as a minimally invasive procedure that reduces IOP with an ab interno approach without
34 EUROTIMES | MARCH 2023
GLAUCOMA
conjunctival dissection. Angular MIGS provides aqueous humour deflux through the trabecular meshwork and Schlemm’s canal using implanted stent(s) or tissue removal.
“As defined, angular MIGS is effective, quick, and safe. We can customise its approach to the patient’s preoperative condition, and the postoperative course of phacoemulsification plus MIGS is similar to cataract surgery alone,” said Dr Morselli, listing the “pros” for the dual procedure.
Identifying the “cons”, she said “MIGS is expensive, can be uncomfortable for the surgeon and the patient, and has a slow learning curve due to the challenge of achieving adequate angle visualisation.”
Her discussion focused on the positive experience her institution gained performing angular MIGS procedures with phacoemulsification in eyes with OAG and angle closure glaucoma due to cataract. The patients had mild to moderate glaucoma, and the indications for adding MIGS were to reduce medication use and address medication compliance issues.
Dr Morselli’s group has the longest and largest experience with the iStent inject®. She reported that among 70 patients followed for 12 to 18 months, IOP was reduced by an average of 20%, and 50% of eyes required no postoperative IOP-lowering therapy.

She reported outcomes for follow-up of one year in 10 patients who had MIGS with the Omni system (Sight Surgical). In this cohort, mean IOP reduction was also 20%, and 80% of eyes required no additional therapy for IOP lowering.
The group also has experience with high-frequency deep sclerectomy, which is limited to 11 patients. At three months, IOP was reduced by an average of 10% without any eyes needing additional therapy. However, Dr Morselli noted HFDS is a painful procedure and requires more intensive medication to control inflammation.
Referring to the outcomes she reported for the iStent inject, Omni Surgical System, and HFDS, Dr Morselli said, “The literature supports our good results.”
She mentioned the Trabectome system, excimer laser trabeculostomy, and Hydrus Microstent (Ivantis) are other angular MIGS options, citing published data showing good and stable outcomes after follow-up ranging from two to three years.
The debate took place during the Glaucoma Day session of 40th Congress of the ESCRS in Milan.
Andrew J Tatham MBChB Hons, FRCOphth, FRCSEd, FEBO, AFHEA is a Consultant Ophthalmic Surgeon, Princess Alexandra Eye Pavilion, Edinburgh, Scotland, United Kingdom. andrewjtatham@gmail.com
Simonetta Morselli MD is chief of the department of ophthalmology at San Bassiano Hospital, Bassano del Grappa, Italy. simonetta.morselli@gmail.com
The Gamechanger for ophthalmic surgeons


Pentacam ®
AXL Wave
Essential to refractive practice for 20 years
Thanks to the streamlined measurement workflow and application-oriented overview screens you further improve your time efficiency. Plus, with tons of studies and a huge user community to support data validity, you are always on the safe side. Optimized workflows, satisfied patients and best possible clinical results are all achieved quickly and reliably and without long training periods.
No risk, just fun – the Pentacam® AXL Wave
www.pentacam.com/axl-wave

35 2023 MARCH | EUROTIMES
IT ʼ S TIME TO CHANGE
Meet us at ESCRS Winter Meeting Booth: 31 Visit our Symposium at CIRP Friday, 10th March, 12:00 h Room: VEGA ROOM
Use IOLs with Caution
Presbyopia-correcting IOLs in glaucoma patients involves a multifaceted decision.
 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS
For patients with glaucoma seeking reduced spectacle dependence after cataract surgery, offering a presbyopia-correcting intraocular lens (IOL) should be on a case-by-case basis taking into account multiple patient- and IOL-related features, advises Filomena Ribeiro MD, PhD.
“Cataract and glaucoma often coexist, and patients with both conditions are seen with increasing frequency. Glaucoma has been considered a contraindication for using a presbyopia-correcting IOL. However, this is a controversial because high-level evidence is lacking,” said Professor Ribeiro.
“Multifocal IOLs should be used with caution in patients with glaucoma but perhaps considered in those with early, stable disease with a low risk of progression. Other IOL options can provide patients with more functional vision.”
Careful preoperative evaluation
The decision to implant a presbyopia-correcting IOL is partly guided by whether the preoperative examination identifies issues with the potential to affect functional outcomes. Attention should be paid to the ocular surface condition, recognising that dry eye is common in glaucoma patients. The examination should also look at structural features of the anterior segment that can be affected, including anterior chamber depth and symmetry, as well as the irido-corneal angle, pupil, and iris.
In addition to the stage of glaucoma, surgeons should examine the possibility a multifocal IOL can affect interpretation of tests used to monitor glaucomatous progression and the potential for disease development following cataract surgery. Without these considerations, the risk increases for glaucoma progressing to a point requiring filtering surgery that can induce astigmatism, or a patient with pseudoexfoliation glaucoma could develop zonular laxity that will affect IOL stability.
Evaluations should also include visual function measurements to determine if the patient would benefit from a multifocal IOL or suffer relevant compromise due to existing reduced contrast sensitivity. Noting visual acuity is not a good indicator of visual function in patients with early glaucoma, Prof Ribeiro said the evaluation should rely more on contrast sensitivity, with mesopic the most relevant.
“We know contrast sensitivity is compromised even in patients with ocular hypertension and early-stage glaucoma, and published studies show contrast sensitivity with and without glare is worse after implantation of a diffractive multifocal IOL than a monofocal IOL,” she said. “However, [studies also show] contrast sensitivity in normal subjects over sixty years old is not that different.”
Central retinal sensitivity will determine whether a patient will benefit from a multifocal IOL. Furthermore, mean deviation values are reduced by multifocal IOLs, although there is a lack of information on the effects of newer trifocal and EDOF designs.

Prof Ribeiro noted microperimetry’s use in assessing the central visual field. It has also shown strong correlations with structural parameters obtained by OCT and offers slightly better reproducibility.
“Of course, [microperimetry] is not the perfect examination. In the future, new functional assessment methods can complement structural information provided by OCT,” she said.
Multifocal alternatives
Prof Ribeiro suggested newer enhanced monofocal IOLs might be an option for giving patients more functional vision for daily activities without further reducing contrast sensitivity. An addon multifocal IOL that can be explanted in the future, leaving the patient with an in-the-bag monofocal lens, is another possibility.
“We do not yet have evidence to support this approach, but it is being studied,” she said.
36 EUROTIMES | MARCH 2023 GLAUCOMA
Prof Ribeiro spoke at Glaucoma Day during the 40th Congress of the ESCRS in Milan.
Filomena Ribeiro MD, PhD is the Head of the Department of Ophthalmology, Hospital da Luz, Lisbon, Portugal. filomenajribeiro@gmail.com
Fundus-driven perimetry can detect retinal sensitivity to light stimuli on the central retina.
Multifocal IOLs should be used with caution in patients with glaucoma.
ESCRS AT A GLANCE
We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With more than 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.


37 2023 MARCH | EUROTIMES
Gene Therapy in the Real World
Treatment shows safety and effectiveness for patients with rare inherited retinal degeneration.
DR GEARÓID TUOHY REPORTS
The two-year interim results following the treatment for LCA2-RPE65 patients provide valuable real-world safety and effectiveness data for voretigene neparvovec (VN; Luxturna®, Spark Therapeutics), according to Dominik Fischer MD, DPhil, FEBOphth.

Voretigene neparvovec is the first ocular gene therapy approved for treating the rare inherited retinal degeneration caused by a bi-allelic RPE65 mutation. The disease causes progressive vision loss and ultimately leads to complete blindness.
183 eyes from 103 patients (data cut off 8/21) interim analysis:
• n=10 to n=51 per time point for FST
• mean at baseline -5dB
• increase within first month
• increase sustained
Prof Fischer’s real-world study “PERCEIVE” is the first global (ex-US) registry evaluating long-term safety and effectiveness for a gene therapy. PERCEIVE is a prospective, longitudinal, multicentre, multinational, observational project collecting phase IV participants for a 10-year duration. The enrolment period is for 5 years, from 2019 to 2024, with a follow-up period for a further 5 years, from 2024 to 2029. Collected data includes demographic data, adverse events (AEs), medical records, patient-reported outcomes (PROs), caregiver-reported outcomes (CROs), medical history, ocular characteristics, IRD diagnoses, ophthalmic examinations (VA, VF, FST, and OCT), and information on pregnancy outcomes.
The phase III VN data, supported by Spark Therapeutics, showed 31 participants of the pivotal trial randomly assigned to intervention (n = 21) or control (n = 10), leaving a modified-ITT (intention-to-treat) population of 20 intervention and 9 control participants. After 12 months, a mean bilateral multi-luminance mobility test (MLMT) change score reported a value of 1.8 (SD 1.1) in the intervention group versus 0.2 (1.0) in the control group. This primary endpoint’s 1.6 difference (MLMT assay, 95% CI 0·72−2·41, p = 0·0013) led to US FDA approval in December 2017 and EMA approval in November 2018. In addition, the original publication reported no serious, product-related adverse events or deleterious immune responses.i
Following the real-world data for the VN treatment, Prof Fischer showed a total 106 patients enrolled in PERCEIVE by August 2021, 103 patients of which received VN (183 eyes). The mean patient age was 19.5 years, with a 2- to 51-year range. Half of the patients were adults, and half were female. Patients came from 15 countries, the majority of which were from Germany, France, and Italy. Most eyes (80.7%) had an outer nuclear layer present, assessed by OCT. Data recorded on the ellipsoid zone line was intact in 32% eyes, disrupted in 53.9%, and absent in 14 .1%. In addition, the mean BCVA at
baseline was 1.14 logMAR, with a range of 0.2 to 2.6 logMAR. Research has not observed any clinically meaningful change in the mean BCVA over time.
In terms of visual function, assessed by full-field stimulus testing (FST, white light), the mean FST at baseline was -4.56 dB, and its increase had clear changes from month one to year two, showing FST improvements of -16.59 dB, -18.24 dB, 15.84 dB, and 13.67 dB (Figure 1).
“Following the FST, which is a light sensitivity threshold test, almost 100 patients have approximately a 20 dB gain,” Prof Fischer reported, “meaning they are about 10 times more light sensitive now than after the treatment, compared to before, which would be complete night blindness. This nicely reflects what we have seen from the pivotal phase III trials.”
Ocular AEs were reported in 35 patients (34.0%), affecting a total of 50 treated eyes (75 events), with chorioretinal atrophy appearing the most common. However, the benefit for the PERCEIVE study is simply “a numbers game”. Given LCA2RPE65 is a rare disorder, any individual centre in one or two cities only collects a handful of patients each.
Prof Fischer encouraged clinical investigators to contribute to the data by enrolling their patients in the study.
“We will certainly recognise the contribution, and this will really help us and our patients understand how to prepare for such a treatment.”
RETINA 38 EUROTIMES | MARCH 2023
Prof Fischer provided this update at the 22nd EURETINA Congress in Hamburg.
Dominik Fischer MD, DPhil, FEBOphth is a consultant ophthalmic surgeon based at the Nuffield Laboratory of Ophthalmology, University of Oxford, UK. Dominik.Fischer@eye.ox.ac.uk
Mean ± SD Change in FST (dB)
i Russell et al, The Lancet, 2017; 390: 849–860.
-35 Month 6Year 1 -30 -25 -20 -15 -10 -5 -0 5 10 -16.6 -18.2 -15.8 -13.7 n=42 n=10 n=13 Month 1 n=51 Year 2
ESCRS Educational Forum is supported by multiple industry partners to provide independent didactic education on selected therapeutic areas. The platform combines presentations from ESCRS Winter and Annual Congresses, selected EuroTimes articles, videos, and webinars to provide an in depth overview on current clinical outlooks.
escrs.org/education/forum/

Education Forum
New Prospects for Inherited Retinal Disease
Emerging gene-agnostic therapies offer hope of preservation and restoration of vision in eyes with retinal degeneration.
Several new gene-agnostic, vision-preserving and restoring treatments for inherited retinal disease could soon enter clinical practice.
Three of these treatments demonstrate this potential: One is an orally administered antioxidant n-acetylcysteine for RPE Usher syndrome and potentially other conditions. A gene therapy, a second, causes cone photoreceptors to express a protein normally produced by the rod-derived cone viability factor (RCVF). The third, an optogenetic therapy, helps retinal ganglion and bipolar cells mimic photoreceptor function in eyes that lost all rods and cones.
Research indicates oxidative stress exacerbates retinal degeneration. In studies Peter Campochiaro conducted using animal models of retinal degenerative disorders, administration of the powerful antioxidant n-acetylcysteine preserved function and reduced photoreceptor loss. N-acetylcysteine is already FDA-approved for a few indications, including acetaminophen overdose.
A company called Nacuity Pharmaceuticals is conducting a clinical trial using a form of n-acetylcysteine called NACA, modified to increase its bioavailability. So far, the trial has recruited Australian patients with Usher syndrome. The company plans to report some results early in 2023, and if favourable, will begin recruiting patients in the United States.
“What we’re excited about is this is a pretty non-invasive and gene-agnostic oral medication. We’ve invested $7.5 million thus far, and we invest in a company if there is a return on our investment,” said Ben Shaberman, Vice President of Science and Communication for Foundation Fighting Blindness, whose organisation contributed funding to the research. “We don’t give that out to investors—we take that money and plough it back into research. So, this is a way to keep research moving forward.”
Preserving cones after rod collapse
The Foundation Fighting Blindness Retinal Degeneration (RD) Fund has also contributed to the research behind two new gene-agnostic therapies for retinal degeneration. One of the treatments, developed by SparingVision, is designed to preserve cone receptors by transfecting the remaining retinal cells with the gene RCVF.
Company founders José Sahel and Thierry Léveillard had shown in previous research that RCVF, which ordinarily is generated by rods, plays an essential role in the metabolism and function of cone receptors. Most IRDs originate in genetic defects of the rods—the subsequent death of cones may result in part from the absence of RCVF. The
FDA approved SparingVision’s Investigational New Drug application (IND) in December 2022 as a gene therapy approach in RP treatment.
“This is targeting cone preservation; they will target RP and I’m guessing Usher syndrome and other approved diseases. This has been in development for decades and we have invest ed nearly €7.5 million just in SparingVision, the company that is moving it into the clinic,” Mr Shaberman said.
Optogenetics for eyes with no photoreceptors
Another company the foundation’s RD fund helped launch is Vedere Bio, founded by John Flannery and Ehud Isacoff. The company has developed an optogenetic treatment for eyes that have lost all their photoreceptors. The treatment involves using an adeno-associated virus vector to transfect bipolar cells and retinal ganglion cells with the genes for opsins. The opsins cause the cells to behave as photoreceptors and provide patients with some rudimentary vision.
Other companies have used the same approach, and early clinical reports have included the case of a patient who was completely blind but observed his dog at play after undergoing the therapy. However, those approaches use microbial proteins that require high-intensity light to function properly—obligating patients to use special goggles to amplify the incoming light signal. In contrast, Vedere Bio’s approach uses a medium-wave green cone opsin that works better in natural light, so patients do not require special goggles.
Vedere Bio was acquired by Novartis in September 2020. The company’s leadership and research team has since launched Vedere Bio II, which has developed an optogenetic treatment using a green cone opsin with a chemical photoswitch.
The Foundation Fighting Blindness is the largest non-governmental source of research funds for inherited retinal degenerative diseases. It raises funds through pri vate individual contributions, corporate philanthropy, and community-based fundraising activities. The foundation launched the Retinal Degeneration Fund in 2018, a venture philanthropy fund that puts returns on investments back into research. So far, the RD fund has invested more than $100 million in 12 companies.

RETINA 40 EUROTIMES | MARCH 2023
ROIBEÁRD O’HÉINEACHÁIN REPORTS
Ben Shaberman spoke at the Retina 2022 congress in Dublin, Ireland.
Ben Shaberman MA, MS is Vice President of Science and Communication for Foundation Fighting Blindness, Maryland, US. bshaberman@fightingblindness.org
Research | Education | Innovation
Access the latest articles, presentations, podcasts, webinars, and videos. Find where and when the latest events, meetings, and conferences are happening.

41 2023 MARCH | EUROTIMES
ESCRS.org
HOW SHOULD WE READ CLINICAL TRIALS?
Designing, executing, and interpreting randomised clinical trials.
BY DR GEARÓID TUOHY
While a large body of details is required to master the mechanics of a clinical trial, it is just as important to ensure researchers consider the “big picture” of clinical research, Professor Timothy Jackson told a recent conference.

In a presentation discussing the design, execution, and interpretation of randomised clinical trials, he stressed the importance of thinking about papers and bringing critical appraisal to clinical research—rather than just absorbing the facts.
Clinical trials are any form of planned experimental study designed to evaluate the effect of a treatment on a clinical outcome. There are two distinct study designs: observational and experimental. Prof Jackson focused on the latter, outlining the process of designing and executing a clinical trial of either a drug or a medical device.
There are four phases of clinical trials. Phase I, often referred to as “first-in-man”, is an experimental study for a new drug or regimen routinely used by “healthy” volunteers, ranging somewhere between 20 and 80 participants. The primary aim is to find a dose with an acceptable level of safety, including the biological and pharmacological effects of a treatment.

For phase II, researchers may recruit an estimated 20 to 300 patients (and controls), including patients diagnosed with a specific condition, to obtain a preliminary efficacy estimate. These trials collect data in each trial arm to potentially design a larger subsequent trial. Phase IIA is routinely used to specify the dose, while phase IIB aims to evaluate efficacy and ongoing safety.
Phase III studies generally comprise large, multicentre randomised clinical trials with a control group ranging from 300 to 3,000 patients. Studies in phase III routinely present a formal hypothesis in advance, the types of statistical tests planned, and the outcomes to collect. The design should confirm preliminary evidence accumulated from previous exploratory studies showing a drug is both effective and has an acceptable safety profile in the intended indication and target patient population.
The fourth phase of a clinical trial transpires after the approval of a drug or device is made available on the market. These studies continue monitoring efficacy and safety on a broader population consistent with the approved labelling and may expand to other groups, such as paediatric patients or perhaps pregnant patients.
Go with PICO
“PICO” is a useful mnemonic tool for formulating efficient questions: Population, Intervention, Comparison/ Control, and Outcome. The “population” aims to define the characteristics of the patient groups included in the study—defining basic inclusions and exclusions such as age, gender, and disease severity. If the inclusions and exclusions are too tightly or selectively defined, the subsequent results may not be generalisable for a useful population.
The “intervention” describes the specific treatment studied—a drug, device, or regimen—and considers
42 EUROTIMES | MARCH 2023 BIOOPHTHALMOLOGY
the treatment delivery method: monthly injection, a slow-release formulation, etc. The treatment or intervention the comparator or control group receives, whether a placebo or an active comparator, or “standard of care”, defines the “comparison”.
Finally, the “outcome” is where the “rubber meets the road”. It is critical to consider how measurements are collected, ensure they are appropriate and clinically relevant, and examine what functional outcomes are useful for the patient. Prof Jackson also noted it essential to define the primary and secondary endpoints, whereby the primary endpoint meets “approval” with at least 90% power and accepted by independent market regulators, and the secondary endpoints have designated use.
He also emphasised PROMs— patient-reported outcome measures. While these are routinely considered secondary endpoints, they are extremely important in the context of novel treatments and comparing other available options.

As an example PICO question, a search could identify an interventional RCT clinical trial (the study design) of an AAV gene therapy (the intervention) for a specific retinitis pigmentosa patient (the population) to improve the disorder (the outcomes), given no other available treatments (the comparison).
A clear methodology should be available when executing a study so an independent evaluator can assess the given protocol and ensure everything follows the plan. They can subsequently show how the study went, and if not to plan, why and how researchers addressed the deviations.

Bias awareness
Prof Jackson emphasised the concern of bias in trial design. Many common sources of bias need active monitoring, including selection bias, performance bias, attrition bias, and reporting bias. And in reading any paper, he stressed, ask if bias strengthens or weakens the results in the context of the “bigger picture”.
At the results stage, it is essential to consider what is meant by statistical significance versus clinical significance.
Phase I aims to find a dose with an acceptable level of safety.
Phase II helps specify dose, efficacy and ongoing safety, and helps build the case for a larger subsequent trial.
Phase III confirms preliminary evidence, particularly in the intended indication and target population.
Phase IV transpires after approval, expanding efficacy with a broader population.
For example, if a paper reports a treatment difference for a logMAR of 0.1 visual acuity, compared to a treatment difference for a logMAR of 0.3 visual acuity, then with all other things equal, the latter logMAR 0.3 difference may likely be relevant for a patient.
Prof Jackson spoke at the 22nd EURETINA Congress in Hamburg.
ChB, FRCOphth
t.jackson1@nhs.net
43 2023 MONTH | EUROTIMES
Timothy L Jackson PhD, MB
is a Professor of Retinal Research and Consultant Ophthalmic Surgeon at the School of Life Sciences and Medicine, King’s College London, UK.
YOUNG OPHTHALMOLOGISTS NEED BUSINESS AND MANAGEMENT SKILLS
BY HOWARD LARKIN
In professional life, as in business, you seldom get what you deserve—you get what you negotiate. And negotiating success in ophthalmology requires cultivating business and management skills right from the start, particularly if you want your own practice, Daniel Kook MD, PhD said in the ESCRS Leadership and Business Innovation Programme at the 40th Congress of the ESCRS in Milan.
The cost and complexity of running a practice drive a growing share of young ophthalmologists into employment, Dr Kook said. Starting a practice is risky and involves taking on heavy administrative burdens and complex legal and tax obligations. Plus, it can take up to two years of planning and another two years operating before breaking even.
But the rewards are worth it, Dr Kook said. Independence means self-determination that promotes trusting patient relationships and providing the care you think best. It also offers opportunities for balancing work and life needs, financial growth, and skill building. Based on his experience launching a practice in April 2020, he outlined several essential areas requiring skill and knowledge for successful negotiation.
Business and finance
Business planning is one. A clear understanding of the potential market, its competitors, and how to serve and address them creates the foundation for building a practice. Many business planning programs are available online, Dr Kook noted.

Real estate is another. It’s essential to find and choose a location easily reachable for you and future patients, as well as a facility that’s accessible and attractive. Space planning and environmental analysis also are required.
Another requirement is financial planning. Dr Kook’s financial plan,
which he developed with help from a colleague’s consulting firm in 2019, assumed realistic sales over a two-year ramp-up starting in 2020. He figured the total cost would be €600,000. That included €100,000 to convert the offices he rented, €110,000 for furnishings, €200,000 for imaging equipment, €30,000 for information technology, and €30,000 annually for marketing.
Ongoing costs included €80,000 annually for staff, €40,000 for rental, his own projected living expenses, and €7,000 annually on a €700,000 loan that delayed repayment for two years.
“In Germany, rates were 1% at the time; now, they are a lot higher,” Dr Kook said.
Don’t forget to save for any future tax, pension, or other delayed payment obligations, he added.
“One of the biggest mistakes you can make is you don’t take this into account, and two years later, when the bill is due [in Germany], you have no money to pay it.”
Certifications and marketing
New practices may also need a range of technical certifications, requiring qualification courses for the surgeon or
44 EUROTIMES | MARCH 2023 LEADERSHIP AND BUSINESS INNOVATION
Everybody is already a leader in one or more aspects of their lives. Effective leadership makes life much easier.
designated staff. Depending on location and services offered, these may include hygiene, laser protection, data protection, ultrasound, intravitreal injections, and quality management for special contracts.
One last area Dr Kook touched on as needed knowledge was marketing skills. These include setting up and maintaining a practice home page, search engine optimisation, target group identification, print media, online advertorials, social media, brochures, business cards, and information meetings.
That is a lot of complex material, but there is no need to reinvent the wheel, he advised. Networking with like-minded colleagues through professional exchange groups lets you learn from their experience and avoid classic pitfalls.
“Sometimes you stay awake at night wondering what’s going on, what will you do tomorrow,” Dr Kook said. But realise building a practice takes time and patience.
While Dr Kook planned for two years without a revenue gain, he achieved it after about nine months and has since surpassed his five-year goals.
“Questioning yourself doesn’t get you there. Just do it.”
Growing in leadership
Whether in a private, public, or hospital practice, leadership is another essential element for ophthalmology success, said Nic J Reus MD, PhD, adding influencing others to help accomplish a common task is one definition.


Other descriptions range from helping patients make treatment decisions and running operating rooms to running hospitals or research departments to guiding national and international organisations. All require managing the time and resources supplied or controlled by others.
Change management also requires leadership. Adopting a new lens
implant or curtailing post-surgery eye shield use requires complex coordination of clinicians, administrators, and outside parties, Dr Reus observed.
Leadership involves setting direction, defining problems, building commitment, and motivating and sustaining efforts. Dr Reus recommended developing these skills early through acting as a trainee representative on committees and progressively taking responsibility for running clinics.
“You grow in your role as an ophthalmologist.”
Formal programmes are available to help residents develop leadership skills. These include training on personal leadership, managing complexity, influencing and conflict management, understanding finances, and quality improvement.
“Everybody is already a leader in one or more aspects of their lives. Effective leadership makes life much easier,” Dr Reus concluded.

45 2023 MARCH | EUROTIMES
Daniel Kook MD, PhD owns Prof Kook & Partner, a private ophthalmology practice in Gräfelfing, near Munich, Germany. daniel.kook@med.unimuenchen.de, info@profkookundpartner.de
Nic J Reus MD, PhD is an independent ophthalmologist at Amphia Hospital, Breda, the Netherlands. nreus@amphia.nl
NIDEK launches Fully Assisted Refraction System for TS-610
Nidek announced the launch of the innovative Fully Assisted Refraction System (FARS), an optional kit for the TS-610 NIDEK Tabletop Refraction System for performing subjective refractions that integrates the chart and refractor into a single unit.
FARS is used to determine the full refractive correction based on patient response using objective data or spectacle prescription as the starting point. The kit consists of a joystick controller and FARS application software. Gentle voice guidance prompts the patient to respond to questions with the controller. A Windows computer or tablet displays the test progress and times as the refraction progresses. A staff member can check progress even if they do not accompany the patient.
Nidek.com

Two-handed MIGS now possible for the first time
The new GONIO ready® by Oculus allows surgeons performing MIGS to attach the gonio lens to the microscope rather than holding it with one hand, which gives them two free hands for the surgery.
“Being able to use both hands for the MIGS operation opens new possibilities for surgeons and adds a degree of safety for both the surgeon and the patient. Our new GONIO ready will benefit anyone already using a gonio lens,” said Christian Kirchhübel, Oculus CEO.
With the GONIO ready, the gonio lens is attached to the microscope via an adapter with a flexible “swan neck”, referred to as the Flex System, which avoids any additional pressure against the patient’s eye. The system is flexible enough to be moved around during MIGS yet sufficiently resistant to movement so as not to be inadvertently displaced. The lens is designed for single use.

“When we introduced the BIOM® system almost 40 years ago, it revolutionized wide-angle viewing techniques in vitreoretinal surgery. Now glaucoma specialists can look forward to the revolutionizing capabilities of the GONIO ready and how it will make their daily surgical work easier and more efficient,” said Steffen Adamowicz, Director of OCULUS Surgical. oculus.de/en

In case you missed it…
In the Heritage Lecture presented at the 40th Congress of the ESCRS, noted cataract and refractive surgery pioneer Dr Lucio Buratto discussed the evolution of cataract surgery from Ridley’s first IOL to the modern foldable lenses we use today.
46 EUROTIMES | MARCH 2023 INDUSTRY NEWS
BRIDGING THE GAP BETWEEN LAB AND CLINIC
In the editorial, Liliana Werner MD, PhD highlights JCRS’s Laboratory Science section—introduced in January 2000 as “devoted to experimental work related to cataract and refractive surgery.” The journal has since published approximately 700 articles in this section and created the Mamalis Award for the Best Laboratory Science Article, presented during the ASCRS/ESCRS annual meeting. John Zdral and associates received the first award for their article “Rotational stability of toric intraocular lenses with a newly modified capsular tension ring”, published in the April 2021 issue. Article award winners feature on a dedicated page on the JCRS website.
L Werner, “Bridging the gap between basic science and clinical practice: the Laboratory Science section”, 49(1): 1–2.




NEW COMPLEMENTARY EDOF SYSTEM

A new complementary extended depth of focus (EDOF) IOL system may yield better monocular intermediate visual acuity than the conventional trifocal lens, a new optical bench study suggests. The study compared a conventional trifocal IOL (AcrySof IQ PanOptix, Alcon) and the ARTIS Symbiose complementary IOL system (Cristalens Industrie). The patient received an ARTIS Symbiose MID with an EDOF profile favouring intermediate vision in one eye and an ARTIS Symbiose PLUS with an EDOF profile favouring near vision in the other. The MID lens produced higher MTF values than the other studied IOLs at the intermediate focus, whereas the PLUS lens outperformed the others at the near focus. The author noted the new system may yield better monocular intermediate visual acuity than the conventional lens, but further investigation is necessary.




T Naujokaitis et al., “Complementary system vs conventional trifocal intraocular lens: comparison of optical quality metrics and unwanted light distribution”, 49(1): 84–90.
NEW PRESSURE-SENSING PHACO HANDPIECE


The new pressure-sensing Sentry phaco handpiece for the Centurion Vision System phacoemulsification and aspiration system quickly detects IOP changes in the anterior chamber and stabilises IOP during surgery, a new study suggests. The study authors compared changes in anterior chamber depth (ACD) in freshly enucleated porcine eyes during intentional occlusion breaks with the Centurion Vision System with Active Sentry, Infiniti Vision System, and Constellation Vision System. Each group included five eyes, and the researchers observed and evaluated the ACD changes using the slit side view (SSV) method. The smallest ACD change occurred in the eyes where the Sentry phaco handpiece was used.


H Suzuki et al., “Effect of a new phacoemulsification and aspiration handpiece on anterior chamber stability”, 49(1): 91–96.


PRESBYOPIA & ASTIGMATISM CORRECTION REINVENTED









47 2023 MARCH | EUROTIMES JCRS HIGHLIGHTS
1) Broader Toric meridian designed to be more tolerant of misalignment. White paper: Evaluation of a new toric IOL optic by means of intraoperative wavefront aberrometry (ORA system): the effect of IOL misalignment on cylinder reduction. By Erik L. Mertens, MD Medipolis Eye Center, Antwerp, Belgium 2) The misalignment tolerance and the use of segments instead of concentric rings reduces photic phenomena, helping patients to adapt more naturally to their new vision. 3) The central zone of 1.4 mm in diameter is larger than most available mIOLs and allows a wider tolerance so that the visual axis passes through the wider central segment avoiding visual disturbances. 4) In cases of tilt or misalignment, the patient can still benefit from good near and far vision, as the segmented zones allow a balanced far/near light distribution in a steady optical platform. OPHTEC | Cataract Surgery REDUCE GLARE & HALOS1 TOLERATE THE KAPPA ANGLE2 TOLERATE DECENTRATION 3
TOLERATE MISALIGNMENT 4 CTF/TCT optic designed to:
ICL — THE LASSO FORMULAS
BY ARTEMIS MATSOU (GREECE) AND MARIO NUBILE (ITALY)
Implantable collamer lenses (ICL) have gained wide popularity as an alternative to laser refractive surgery for refractive error correction, while several studies have demonstrated their safety and efficacy. Accurate ICL sizing and vault prediction remain the main challenges, with inadequate vault comprising the leading cause of ICL exchange/explantation. An undersized ICL can increase the risk of cataract formation due to insufficient vaulting, whereas an oversized ICL may result in secondary glaucoma and endothelial cell loss. Several other ICL-sizing formulas or nomograms have been proposed in addition to the manufacturer’s official online Calculation & Ordering System (OCOS) formula, which calculates ICL size based on white-to-white (WTW) distance and anterior chamber depth (ACD).
In a recent episode of the ESCRS Eye Journal Club, we discussed the study published by Rocamora (et al.) in the Journal of Cataract and Refractive Surgery with guest speakers and ICL users Mr Allon Barsam (UK) and Prof Emilio Pedrotti (Italy). Our conversation centred on a new set of ICL sizing formulas—the LASSO suite—developed to better suit a less myopic population of Caucasian descent.
The LASSO formulas consist of the LASSO-OCT, LASSO-Biometry, and LASSO-Full models, based on preoperative parameters obtained by the respective devices and processed with the LASSO technique. The study authors concluded the LASSO suite provides a set of powerful, reproducible, yet convenient ICL sizing formulas with state-of-the-art performance in Caucasian patients—including those with low and moderate degrees of myopia. Other published formulas, they noted, predominantly tested in Asian datasets with a high proportion of highly myopic eyes.
Both speakers agreed there is a need for accurate ICL-sizing formulas offering a postoperative vault predic -
tion, a feature not currently available with the manufacturer’s formula. Indeed, the OCOS formula relies only on WTW and ACD measurements, and although it seems mostly accurate for average eyes, it is notable for its outliers. Formulas that incorporate more detailed anatomic dimensional parameters are anticipated to be more precise—a useful tool when choosing the preferred ICL size.
Mr Barsam highlighted that clinical complications of incorrect vault may not always correlate with the achieved vault, as often there are cases where vault exceeds the recommended range of 250 to 750 μm with no clinical implications. He therefore recommended judging this on an individual basis. And while the study proposes the LASSO suite as more accurate for non-Asian eyes, there is not enough information on the racial background of the studied population. Both speakers mentioned that ICLs are gaining more space in their practices, coming up 5% to 10%
currently versus laser refractive surgery—but they are less keen to widely adopt the lenses for very low refractive errors or keratoconic patients.

Guest speakers Mr Barsam and Prof Pedrotti stated interest in using the LASSO suite based on the available equipment to improve the safety of ICL implantation in their group of patients. The LASSO suite can be accessed at http://icl.emmetropia.be
Rocamora L, Orlando JI, Lwowski C, Kohnen T, Mertens E, Van Keer K. “Postoperative vault prediction for phakic implantable collamer lens surgery: the LASSO formulae”. J Cataract Refract Surg. 2022 Oct 14.

48 EUROTIMES | MARCH 2023
ESCRS EYE JOURNAL
27
CLUB, EPISODE
There is a need for accurate ICL-sizing formulas offering a postoperative vault prediction.
Upcoming Events
March 10–12
ESCRS Winter Meeting 2023
Vilamoura, Portugal

April 23–27
ARVO
New Orleans, US

May 5–8
ASCRS
San Diego, US

May 22–25
Royal College of Ophthalmologists
Birmingham, UK

May 26
EuCornea Congress
Barcelona, Spain
June 15–17
European Society of Ophthalmology (SOE)
Prague, Czech Republic
June 28–July 1
World Glaucoma Congress
Rome, Italy
Sep 8–12
41st Congress of the ESCRS
Vienna, Austria
March 10
April 23
May 5
May 22
49
2023 MARCH | EUROTIMES
PRIORITISING SAFE AND EFFECTIVE OUTCOMES COMPARABLE TO CATARACT SURGERY ALONE1
LOWESTREPORTED ECL=ENDOTHELIAL CELL LOSS; PAS=PERIPHERAL ANTERIOR SYNECHIAE.
NO REPORTS
RATES OF SIGNIFICANT ECL (>30%) & PAS IN ANY MIGS PIVOTAL TRIAL1
OF HYPOTONY, SIGNIFICANT HYPHEMA, OR CHOROIDAL HEMORRHAGE OR EFFUSION1
0.01 DECIBEL MEAN CHANGE IN VISUAL FIELD MEAN DEVIATION FROM BASELINE AT 24 MONTHS IN THE PIVOTAL TRIAL1
99 % OF EYES WERE WITHIN 1 DIOPTER OF TARGET** 2

72 % REDUCTION IN THE PERCENTAGE OF PATIENTS WITH SEVERE OSD SYMPTOMS 3

surface disease changes in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification.
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only.
• This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. Glaukos®, iStent®, and iStent inject® W are registered trademarks of Glaukos Corporation. All rights reserved. ©2023 PM-EU-0208

XXXXXXXXXXX
**Retrospective analysis of 106 patients undergoing femtosecond laser-assisted cataract surgery and the insertion of 2 iStent inject® devices. 1. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811-821. 2. Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517-524. 3. Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular
Ophthalmol Ther. 2020;9(4):941-953.













 Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell
Paul Rosen
Oliver Findl ESCRS President
Thomas Kohnen Chief Medical Editor
José Güell
Paul Rosen





























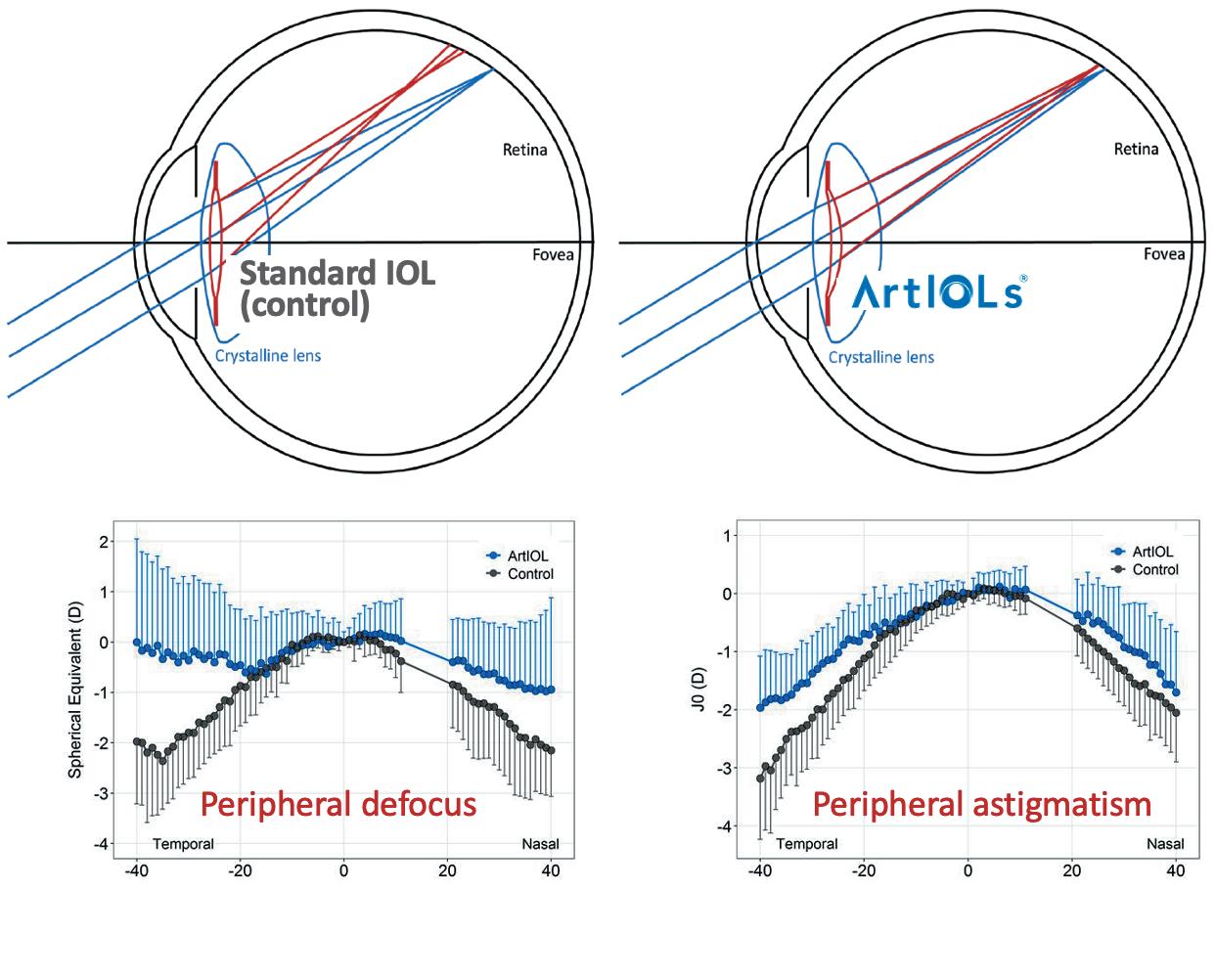


































 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS


 CHERYL GUTTMAN KRADER REPORTS
CHERYL GUTTMAN KRADER REPORTS




















































