Piecing Together a Solution

ALSO IN THIS ISSUE
Monofocal Plus
Finding the Balance
Enhanced monofocals may be the future standard of care in cataract patients.
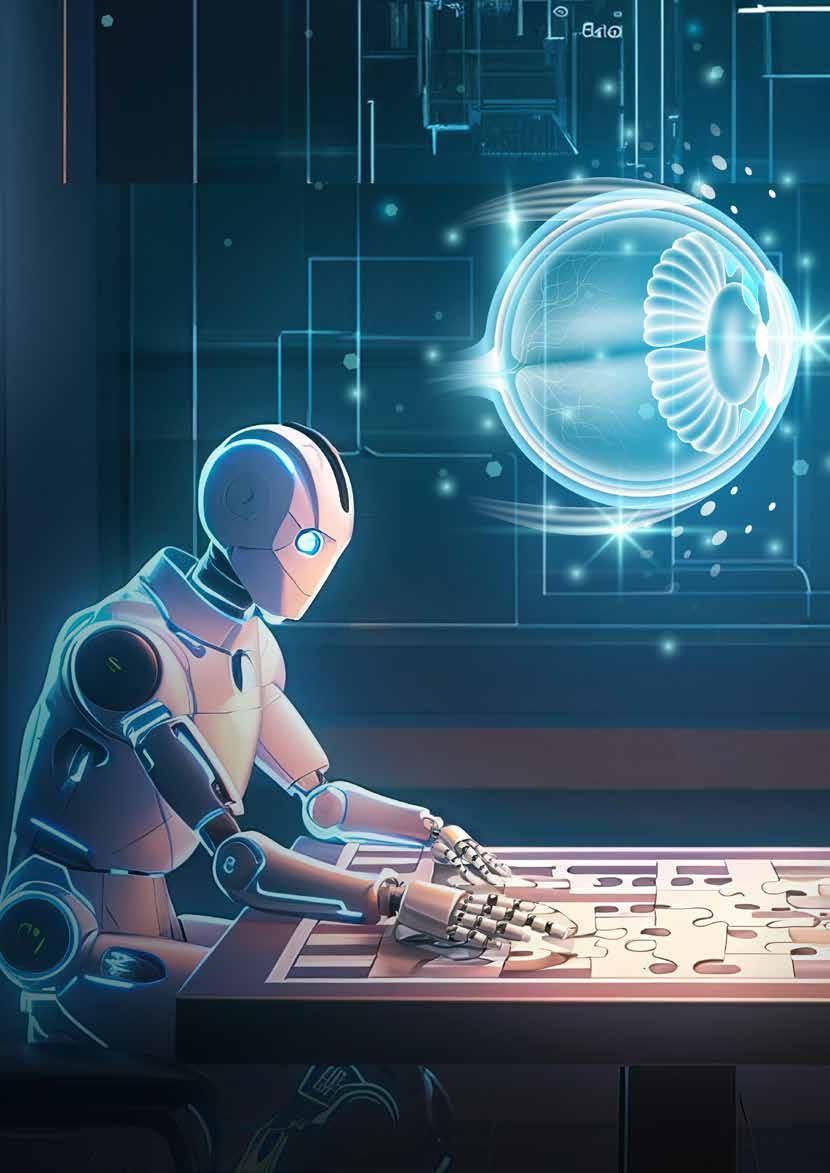
What is the best use of robotics and AI in cataract and refractive surgery?
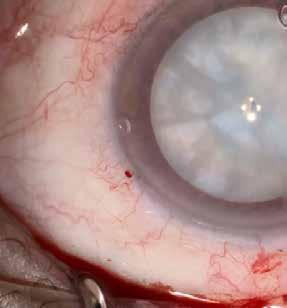
Improving Preoperative Prediction of PCR Machine learning models show promise, outperforming existing scoring systems.
Semaglutide Shows DR Changes
Retrospective registry-based trial examines impact on diabetic eye disease over two years.
MARCH 2024 | VOLUME 29 | ISSUE 2
Welcome to the Future of Glaucoma Laser Therapy.
Introducing the Eagle™ by BELKIN Vision
Accessible First-Line Glaucoma Care for All
Precision
120 automated treatments enabled by
delivered directly to the trabecular meshwork
Automation
Delightfully simple navigational guidance using an intuitve touch screen
Efficiency
Ergonomic patientand doctor- friendly set up for streamlined positioning and treatment


Visit us at the ESCRS Winter Meeting - Booth #B02
׳׳׳׳׳׳׳׳׳׳׳׳


www.escrs.org

2 Contents EUROTIMES | MARCH 2024 04 Editorial: Robotic Surgery and the Human Touch 06 Inside ESCRS: Library of Short Videos Complements Educational Offerings 07 ESCRS Update: New President’s Vision, Interview Series, FEBOS-CR Exam DIGITAL OPHTHALMOLOGY 12 Ophthalmic Imaging Gets Robotic Enhancement Anthony N Kuo MD 13 A Guide to the AI Revolution Ursula Schmidt-Erfurth MD CATARACT & REFRACTIVE 14 Laser Refractive Surgery for High Myopia John So Min Chang MD and Edward Manche MD 16 AI Applications in Diagnostic Imaging Michael F Chiang MD 17 The Future of FLACS Alexander C Day MD, PhD 18 The Modern Era of Refractive Surgery Victor Derhartunian MD
Advances in Toric IOL Alignment H Burkhard Dick MD, PhD
Growing Options Optimise Outcomes in Cataract Surgery
Findl MD, MBA and Thomas Kohnen MD, PhD, FEBO
Improving Preoperative Prediction of PCR Rudy MMA Nuijts MD, PhD; Ron JMA Triepels PhD; Maartje HM Segers MD; and Mor M Dickman MD, PhD 26 Monofocal Plus Finding the Balance Filomena Ribeiro MD, PhD, FEBO CORNEA 28 Overcoming Issues Limiting DMEK Access and Success Victor A Augustin MD 29 Tech Advances Microbial Keratitis Care Maria A Woodward MD, MS
Knowing Iris Repair: Pupilloplasty Soosan Jacob MS, FRCS, DNB RETINA
Optogenetic Therapy for Stargardt Disease Michael Singer MD 33 Semaglutide Shows DR Changes Zeeshan Haq MD 34 New Subspecialty Could Improve Care Bertil Damato MD, PhD PAEDIATRIC OPHTHALMOLOGY 36 Defusing the Ticking Time Bomb of High Myopia Andrzej Grzybowski MD, PhD 38 Advancements for Paediatric Amblyopia Courtney L Kraus MD SUSTAINABILITY 40 Tackling Waste in Retinal Surgery Redmer van Leeuwen MD, PhD and Francesc March de Ribot MD, PhD
Cover Piecing Together a Solution What is the best use of robotics and AI in cataract and refractive surgery? March 2024 | Vol 29 Issue 2
20
22
Oliver
24
30
32
08





Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983


3 Learn more about EuroTimes or connect with ESCRS at ESCRS.org
2024 MARCH | EUROTIMES 20 12 ALSO IN THIS ISSUE 42 Industry News 45 JCRS Highlights 46 Citation Index 49 Upcoming Events ALSO IN THIS ISSUE
Robotic Surgery and the Human Touch
Will robotics and artificial intelligence replace the ophthalmic surgeon? Timothy Norris explores this question in our lead story. The answer is yes, no, and maybe, depending on the surgical procedure discussed.
Robotic-assisted surgery is becoming well established in the retina field. A robotic hand, holding instruments guided by a surgeon, can perform precise, micron level, delicate surgery without the least tremor. It is also suitable for highly targeted gene therapy delivery to the back of the eye.
Robotics and AI are also integrated in many aspects of refractive laser surgery—as much as laser could be considered a form of robotic surgery—already a core part of this kind of eye surgery.
But what about cataract surgery? Cataract surgery is different. Most cataract operations take place whilst the patient is fully awake, their senses heightened by a mix of fear and anxiety. Particularly in the anterior segment, high levels of standardisation with low rates of complications have led to low levels of interest among cataract surgeons. One exception, femtosecond laser-assisted cataract surgery (FLACS), is an amazing technical achievement, but it has yet to prove more cost effective than standard surgery. It also remains to be seen if industry, the other piece in the puzzle, will support the development of robotic platforms for cataract surgery.
Exploring the topic further, other articles in this issue provide updates on the role of AI in ophthalmic surgery. A robotic alignment system for posterior segment OCT now
in development does not require positioning the patient at a headrest or the assistance of a trained technician. One version welcomes the patient, guiding them to the imaging area. This approach can help reduce COVID risk and difficulties with patient tremors.
Another article looks at AI IOL calculation formulas and their potential for evaluating more challenging eyes. Here, the online ESCRS IOL calculator helps keep track of the growing number of AI-based formulas.
The 2020 prompt for the Henahan Prize asked, “Will clinicians be replaced by a robot to perform cataract surgery?” In Dr Jennifer Kim’s winning essay, she reminds us cataract surgery is a human interaction, citing the example of her own grandmother’s surgery.
Her grandmother recalled lying stiff on the operating table, waiting for her cataract procedure to start. As her surgeon entered the operating theatre, he immediately picked up on her anxiety from the awkward silence in the air and tightly crossed hands pressed into the middle of her chest. Instead of placing the eye drape, he paused and spoke directly to her—asking whether she wanted the radio on and reassuring her it would be okay to move or cough as long as she gave the surgeon a little notice. Throughout the 15-minute procedure, he constantly spoke to her and put her at ease. She remains forever grateful to the surgeon. This view from the patient’s perspective reminds us of the importance of the human touch.
EDITORIAL BOARD

Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)

Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)


Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)
Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
EDITORIAL
4
EUROTIMES | MARCH 2024
Thomas Kohnen Chief Medical Editor
José Güell Medical Editor
Paul Rosen
Medical Editor

Need a quick introduction or refresher about a surgical procedure? Have a tip to share about a technique or approach you use that makes surgery easier?
The ESCRS 100 is the place to go. It’s a library of short (roughly 100 seconds), high-quality instructional videos about all fields of cataract and refractive surgery.
More than a dozen videos have already been created, and additional videos are being uploaded each month. Current videos include the following topics:
• Secondary IOL implantation
• Extracapsular cataract extraction
• Scleral fixation
• Single-thread, single-knot sewing machine suture for iridodialysis repair
MAKE EVERY SECOND COUNT
—PUT THE ESCRS 100 VIDEO SERIES ON YOUR LIST OF MUST-WATCH EDUCATIONAL RESOURCES !
ESCRS 100
HTTPS://WWW.ESCRS.ORG/EDUCATION/EDUCATIONAL-RESOURCES/ESCRS-100/
Library of Short Videos Complements Educational Offerings
BY STUART HALES, EXECUTIVE EDITOR
When it comes to videos, less is often more.
That’s the takeaway from a 2018 study of the impact of video length on retention of course material. The study authors found that students who watched short videos reported greater long-term retention of the material they learned than students who watched longer videos.1
ESCRS is taking advantage of these study findings by launching a series of short videos—roughly 100 seconds in length—on topics related to cataract and refractive surgery. More than a dozen videos already have been uploaded to the ESCRS website, and more are added each month.
“The ESCRS 100 videos are intended to show best practice cases and thus serve as a basis for surgical training,” says Dr Alja Crnej, co-leader of the ESCRS 100 project. “In this way, well-founded knowledge can be acquired in a relatively short time using modern media.”
The videos uploaded thus far address topics such as secondary IOL implantation, extracapsular cataract extraction, and single-thread, single-knot sewing machine suture for iridodialysis repair. Submitted videos are categorized in one of the following topics:
• Astigmatic correction in cataract surgery
• Capsular complications and management
• Capsulorhexis
• Cataract surgery after refractive surgery
• Extracapsular cataract extraction
• Hydrodissection and hydrodelineation
• Incision construction
• Irrigation and aspiration
• Mature cataract and capsule dye
• Non-chopping techniques
• Ophthalmic viscosurgical devices
• Phaco chop
• Presbyopia
• Secondary IOL implantation
• Small pupil
• Surgical management of cataract in glaucoma patients
• Sutured intraocular lenses
• Suturing in cataract surgery
• Zonular instability and endocapsular tension rings
“The aim is to focus on specific aspects and deal with a very specific topic,” says Dr Stefan Palkovits, cochair of the project. “In that regard, we are creating 100-second videos to show and explain a definite step during a procedure or a difficult situation and its solution.”
Intended for all generations
The videos are a project of the ESCRS Education Committee and are intended to share a quick “how to” tip or trick to solve a problem or complication that may arise during surgery. The videos can be used as standalone resources or to complement more formal education initiatives.
“The ESCRS 100 videos can be used as standalone education tools, but in the future, the videos will also become part of a larger ESCRS learning platform, which is currently being developed,” says Dr Crnej. “The ESCRS 100 videos might act as an entry point. The other parts of the learning platform will be linked to make it easier to find further relevant content, such as full videos, lectures, or presentations.”
The videos are intended for surgeons at all stages of their career, although currently, they are not differentiated on the ESCRS website by skill level or years of practice.

I am sure there are enough tips and tricks out there for an indefinite number of the videos.
“The videos are intended for all ‘generations’ of doctors,” says Dr Palkovits. “When more videos are posted online, we will distinguish those for young doctors from those for more experienced surgeons. But many times, even experienced doctors can learn some valuable information from basic videos.”
6 INSIDE ESCRS EUROTIMES | MARCH 2024


ESCRS Update
New ESCRS President Lays Out Vision
Dr Filomena Ribeiro announced that education, inclusivity, and innovation will be the focus of her agenda as president of the European Society of Cataract & Refractive Surgeons during 2024–2025.
“Our collective vision for ESCRS centres on fostering a robust educational environment,” she stated in a 15 January message to ESCRS members. “Our aim is not merely to meet the demands of everyday clinical practice, but to exceed them.”
Dr Ribeiro is the 18th president of ESCRS, succeeding Oliver Findl. She is the third woman to hold the position and second ESCRS president from Portugal.
In addition to establishing an overarching theme for her tenure, Dr Ribeiro set forth five key initiatives for her presidency:
• Encouraging environmental and social responsibility, with a strong emphasis on equity and inclusivity
• Celebrating the history of ESCRS and its contributions to ophthalmology
• Strengthening connections with ophthalmological societies worldwide
• Introducing new formats and opportunities for sharing experiences, fostering connections, and making meaningful contributions
The conversation between Dr Roger Zaldivar and Dr Oliver Findl will touch on the possibility of remote operating room consultations, the emerging role of artificial intelligence, and the influence of 3D visual operating systems on surgeon ergonomics and long-term health. The interview will also address the challenges of integrating these technologies into everyday cataract practice and propose possible solutions.
The videos, also available as ESCRS podcasts, will present as follows:
• Part 1: Impact of the Digital Operating Room on Everyday Practice
• Part 2: 3D Visual Operating Systems and Augmented Reality
• Part 3: Pathways to Implementing Digital Operating Room Technology
Applications Open for FEBOS-CR Exam
Cataract and refractive surgeons interested in sitting for the FEBOS-CR subspecialty exam have until Friday, 29 March, to submit their application materials and the non-refundable €150 deposit.
Drs Crnej and Palkovits hope the video library continues to grow throughout 2024 and beyond. There is no numerical goal in mind, just a desire to provide as many learning tools as possible.
“We really do hope for a huge library of videos,” says Dr Crnej. “I am sure there are enough tips and tricks out there for an indefinite number of the videos. We just need to keep asking surgeons to share their tips and tricks, since the preparation of the videos is additional work on top of everyone’s busy routine.”
• Developing and promoting research and education projects
“As we embark on this journey together, I encourage you to actively participate, share your insights, and collaborate with us,” she concluded. “Together, we can create a vibrant community dedicated to advancing excellence in cataract and refractive surgery, with a focus on education, inclusivity, and innovation.”
Interview Series Looks at Digital Operating Room
A three-part ESCRS video interview series will explore the transformative effects of the digital operating room, emphasizing its impact on visualization, data integration, and workflow efficiency.
The exam, developed by ESCRS and the European Board of Ophthalmology (EBO), certifies the expertise and advanced knowledge of experienced cataract and refractive surgeons. Along with exams for glaucoma, paediatric ophthalmology, and strabismus, the cataract and refractive exam is designed to harmonize ophthalmic education in Europe and define the expected level of knowledge and skills a subspecialist should acquire to solve complex, difficult cases.
The FEBOS-CR exam is open to cataract and refractive subspecialists from UEMS member countries; ESCRS membership is not required. Candidates must be independent surgeons with a varied case mix who regularly deal with complex situations and are willing to be challenged by a rigorous theoretical examination and interviews with opinion leaders in European and worldwide ophthalmology.
7 2024 MARCH | EUROTIMES
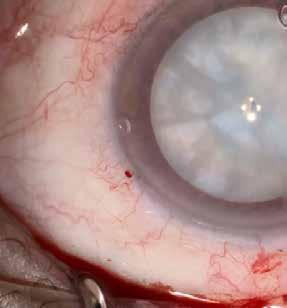
At top, still image from phaco chop video by Vladimir Pfeifer; at bottom, still image from white cataract aspiration video by José Güell.
COVER ARTICLE 8 EUROTIMES | MARCH 2024

Piecing Together a Solution
What is the best use of robotics and AI in cataract and refractive surgery?
BY TIMOTHY NORRIS
It has been a long journey since Karel Čapek first mentioned the word “robot” in his 1920 science fiction play R.U.R. and John McCarthy coined the term “artificial intelligence” in 1956. Concepts like automation and machine learning were decades or even a century from being something real, let alone conceivable for physicians at the time. The fervent thoughts of science fiction visionaries such as Gene Roddenberry and George Lucas flirted with the idea but could not fully grasp its complexity. What was then something related to starships and distant galaxies is now something real, something close, and considered one of the potential greatest turning points for medicine and surgery.
Automation is indeed a recent and revolutionary concept, integrating AI and robotics in everyday practice, from patient flow to prognosis, from diagnosis to treatment and surgery. However, the fundamental nature of revolution may exact a price that some are not willing to pay.
9 2024 MARCH | EUROTIMES
Is robotics really worth it?
The launch of the da Vinci system at the start of the new millennium set a milestone for medical robotics, rapidly becoming a valuable option for microsurgery. According to JeanPierre Hubschman MD, the success of this kind of technology was just the beginning.
“The da Vinci system has already revolutionised laparoscopic surgery, and since then, it has been redesigned and commercialised for other applications like general, paediatric, and cardiac surgery, with more than 7,000 platforms adopted worldwide,” he said. “This is a technology that can really provide some outstanding performance by enhancing surgeons’ manoeuvrability and precision, translating into improved outcomes with shorter hospital stays and fewer complications. It is a solution that may open the door for new surgical techniques, and that will eventually lower the cost of surgery.”
Despite the success in many different surgical fields, the da Vinci system was unable to break through in ophthalmology. A possible explanation for this could be that eye surgery is already a precise and minimally invasive microsurgery with low complication rates and exceptional precision. “It is not a good system for eye surgery,” Marc de Smet MD, PhD said. “Da Vinci has proved its efficiency in urology because a certain degree of precision is needed when you want to avoid vessels. But we are talking about the precision in the millimetre range, not precision in micrometre range as eye surgery demands.”
Particularly in the anterior segment, high levels of standardisation with low rates of complications have led to a general lack of interest in robotics among cataract surgeons, whereas refractive surgery has already used it since the late 1980s. “A robotic system does not necessarily have arms,” Dr de Smet explained. “Laser is indeed a form of robotic surgery. Therefore, robotics is already a core part of eye surgery.”
Automation is already a reality for refractive surgery, explained Diego de Ortueta MD, PhD. “We have devices that collect a lot of information from the patient and calculate the best outcomes. However, not every system—not even transPRK—can be performed without the help of a surgeon.”
Who needs robots?
However, from the point of view of cataract surgery, interest is dwindling. Dr de Ortueta noted this is also due to the negative outcomes in cost-effectiveness of femtosecond-assisted cataract surgery (FLACS). “There is scarce evidence in the literature showing FLACS to be better than the standard procedure. Maybe in the future that could be better, but right now it is not, and the costs are much higher,” he said. “The main point is this: if we are so good at doing surgery, why should we let a robot do our surgery instead?”
On the other hand, the demand for the high levels of precision provided by a robotic arm found fertile ground in the field of vitreoretinal surgery, especially when considering subretinal injections. “If we want to hit a bleb size of 0.1 mm, the maximum volume that we can inject is only 0.1 microlitres. I would challenge anyone to be able to know where to stop injecting at that volume,” Robert MacLaren noted. “If you want to inject an 800,000-euro gene therapy treatment subretinally, you have to do everything possible to be sure that you
are doing it safely. One of the greatest advantages of having a robotic system would be to slow the infusion rate to minimise the risk of retinal stretch. The advantage of using a robot as a delivery system is to increase precision at a point you can avoid reflux—thus reducing the risk of an immune response, while also reducing the quantity of drug in your syringe.”
Into the black box
The astonishing, and in some respects controversial, boom of AI has deeply affected every aspect of our daily living. Ophthalmology is no exception. It is one of the medical fields that saw the earliest application of artificial intelligence in advanced imaging, and the potential for further developments is indeed high.
Soon it will help surgeons make the right decision, plan surgeries, assess and even execute different surgical steps.
“AI is changing the way we do everything, from ChatGPT to Autopilot, it is all around us,” Dr Hubschman pointed out. “It is a technology that is going to deeply change medicine and surgery. It has the ability to accumulate an unlimited amount of knowledge, identify new trends, and solve complex problems. Soon it will help surgeons make the right decision, plan surgeries, assess and even execute different surgical steps.”
“If you want a procedure or a task to work well in a robot, you have to program the robot with a good mathematical algorithm telling the robot what movements it needs to make,” Dr de Smet said. “AI can take information from multiple operations, giving good results with just a hundred different cases. Right now, it can provide us with the best parameters. And in the future, it will probably help identify the best starting point for surgery—or, in the distant future, eventually doing the surgery for us.”
“The biggest problem is that a surgeon understands what the machine does but not the calculations inside the black box. Who or what will decide in the end what could be the best option for the patient?” Dr de Ortueta asked. “In the future, all of this could be fully automated, but an AI making decisions would have clear ethical issues. For example, what if automation would answer more to the logic of the industry than the needs of the surgeon, suggesting SMILE every time instead of the best option for the patient? As ABBA says, ‘the winner takes it all,’ as the industry may decide things that we surgeons are not capable of fully understanding.”
Waiting for the leap of faith
When speaking of partial automation of surgery, the relationship between the physician and the industry is complex. Despite
10 COVER ARTICLE EUROTIMES | MARCH 2024
robotics becoming a growing reality in medicine, its presence in anterior and posterior ocular microsurgery is still scarce.
“For years I’ve debated why investors do not come forward in the field of robotics,” Dr de Smet said. “Essentially, a company must take a leap of faith before the others will be willing to follow. There is a lot of work that must go into the making of a robotic system, and it takes quite a while to get something that properly works. Then you must sell enough units, and only then you get to a point where suddenly investors and money become available.”
According to Dr de Ortueta, this reluctance of the ophthalmic industry may also be driven by scepticism in the medical community. “If a device starts performing worse than the surgeon itself, would it be worth investing? Perhaps when the number of patients will increase to the point that we will not have sufficient resources to treat them all, and maybe when technology will be able to provide a certain degree of safety and efficacy, things will start to change.
“We will eventually end up with full automation of surgery, but right now, we would have to deal with higher rates of complications compared to standard cataract surgery. Industry will preferably invest in other fields of medicine like urology, where these rates are already much higher.”

Things are only recently starting to slowly move in the right direction. Dr de Smet reported the University of California, Los Angeles, has developed a commercial application for cataract, with companies in Israel and Lyon, France, doing the same. “Other platforms for general surgery, like Medtronic, are already challenging da Vinci,” he said. “So, I think that it is coming, I just don’t know when all will finally take off, but it is sure that a big change is coming.”
Jean-Pierre Hubschman MD is Co-Founder and CEO at Horizon Surgical Systems, California, US. jphubschman@horizonsurgicalsystems.com
Marc de Smet MDCM, PhD, FRCSC is Founder and Executive Director of Microinvasive Ocular Surgery Clinic (MIOS) and CMO of PrecEyes (a Zeiss Company). mddesmet1@mac.com
Diego de Ortueta MD, PhD is Medical Director at the Augenlaserzentrum Recklinghausen, Germany. Diego.de.Ortueta@augenzentrum.org
Robert MacLaren MB, ChB, DPhil is a Professor of Ophthalmology at the University of Oxford, UK. robert.maclaren@eye.ox.ac.uk

11 2024 MARCH | EUROTIMES
BIOMECHANICS MEETS TOMOGRAPHY HEY CORVIS ST I just took a look at the tomography. These values call for caution. I don’t think I would operate. HI PENTACAM The biomechanics looks good, though. The cornea is very stable. I don’t see any problem with operating. O.K. TOGETHER NOW Tomography and corneal biomechanics together make the decision easier: Surgery could be an option. Corvis® ST meets Pentacam®: Combined measurement results for a safe decision on surgery Benefit from the combination of biomechanical data from the Corvis® ST and tomographic data from the Pentacam®. Provide surgical care to more patients safely! Follow us! www.oculus.de www.corneal-biomechanics.com Eurotimes ESCRS-Motiv Biomechanics 178x130 e 01.24.indd 1 26.01.2024 18:33:23
Ophthalmic Imaging Gets Robotic Enhancement
Robotics technology offers potential for autonomous imaging.
CHERYL GUTTMAN KRADER REPORTS
The development of robotics-driven alignment technology for ophthalmic imaging platforms enables the capture of high-quality images, even in challenging situations, with the added benefit of providing a contactless, operator-free examination, said Anthony Kuo MD.
To date, Dr Kuo and colleagues—including Drs Joseph Izatt, Ryan McNabb, and Pablo Ortiz in the departments of ophthalmology and biomedical engineering at Duke University and Dr Mark Draelos (now in the department of robotics at the University of Michigan)—have created and tested a robotically aligning system for posterior segment optical coherence tomography (OCT). However, he said the robotics technology could readily be applied to other imaging devices used in ophthalmology.
The system acquires images without patients having to lean against chin and forehead rests for stabilisation and without needing a trained technician onsite to position the patient and perform the scan. It therefore addresses the needs for equipment sanitisation and physical distancing that came to the forefront during the COVID-19 pandemic.
Using multiple cameras for near real-time tracking combined with open and closed loop control of the OCT imager fixed to the robotic arm, the system automatically detects the eye, maintaining proper alignment during the scan by compensating for patient head and eye motion. Dr Kuo highlighted its ability to track and adjust for patient motions by showing its performance in obtaining a quality scan from a patient with retinal pathology despite tremors from Parkinson’s disease.
“The robotically aligned imaging and motion compensation even allow for rudimentary OCT angiography,” he added.
Other versions of the system can provide verbal instructions and feedback to patients, recognising subjects when they enter the room and directing them to the imaging device. Once the face-tracking camera locates the face, pupil cameras triangulate the pupil location so the OCT beam is properly projected. Then, patients can initiate the scan by depressing a foot pedal. Once completed in the first eye, the system automatically switches to scan the fellow eye. To finish the session, the patient receives instruction to release the foot pedal.
Initially tested in younger adults with healthy retinas, the system was found to perform well by comparing the quantitative and qualitative measurements it provided with those acquired through clinician-operated OCT.1 Additional modifications helped to make the platform more patient-friendly and compatible for use in a clinical research population.
“Changes accounted for the diverse characteristics of patients encountered in daily practice, including differences related to age, ethnicity, and gender,” Dr Kuo said.
Further system testing initially set an examiner in the same room who made sure the scan capture was successful. Realising examiners could perform their functions remotely through a digital connection, subsequent testing placed the examiner at a satellite clinic 10 kilometres from where the imaging was taking place.
Dr Kuo also recommended two additional articles relating to this research for those interested in learning more.1,2
Dr Kuo spoke at AAO 2023 in San Francisco, US.
For citation notes, see page 46.
Anthony N Kuo MD is an Associate Professor of Ophthalmology and Assistant Professor of Biomedical Engineering at Duke University, Durham, North Carolina, US. anthony.kuo@duke.edu

12 EUROTIMES | MARCH 2024 DIGITAL OPHTHALMOLOGY
A Guide to the AI Revolution
Strict EU regulations guide AI use in clinical ophthalmology.
TIMOTHY NORRIS REPORTS
The dramatic development of artificial intelligence (AI) has posed a global challenge for institutions and healthcare professionals alike, raising the need for regulations and ethical guidelines for what is being referred to as an “unstoppable revolution.”
In the field of ophthalmology, this revolution has already found its way with the posterior segment—specifically in retina. According to Professor Ursula Schmidt-Erfurth MD, this progress is driven by OCT use in diagnostics and imaging.
“There are good attempts in the use of AI in cataract, refractive, and glaucoma. However, at this very moment the state of the art resides in the posterior segment in the OCTbased image analysis,” she explained. “Using deep learning algorithms, it is possible to localise, classify, and quantify relevant biomarkers with semantic segmentation for detecting pathological features and anomalies. Today, imaging hardware can provide, detect, and differentiate much more medical information than even the most trained expert can do.”
The European Union updated the regulations regarding medical devices in 2017, involving medical AI in the new approval process.
“The latest regulation is the MDR 2017/745/EU, in substitution of the MDD that was basically a self-assessment. It is a

huge step towards secure medical products,” Prof Schmidt-Erfurth explained. “The precautionary principle also applies to this technology, but it is defined separately as part of the risk management of a medical device under ISO 14971, in which the manufacturer should mitigate any suspected risk of causing harm. From design to implementation, everything is covered.”
While its use sparked controversies in all other fields outside of medicine, in ophthalmology, AI is considered by many an empowering technology—while others view AI as something that still must be deeply understood.
“We are talking about a CDSS—a clinical decision support system that empowers the doctor’s decision. It does not make a decision alone,” Prof Schmidt-Erfurth pointed out.
Imaging hardware can provide, detect, and differentiate much more medical information than even the most trained expert can.
The technology removes the subjectivity and variability in clinical routine by simultaneously improving workflow and substantially replacing it with precise measurements.
“For me, the real ethical dilemma is for the current routine not being able to provide the best diagnostics for every patient. AI helps to get rid of this conundrum and finally improve outcomes,” she said. “We are not using AI for an autonomous diagnosis, but we are giving the eye doctor the measurements to make a truly educated and timely treatment decision.”
According to Prof Schmidt-Erfurth, many concerns focus on the black box concept and liability in case of misdiagnosis. “In OCT-based analysis, there is no black box: everything is clear; nothing is hidden,” she said.
Some technologies, such as self-driving cars, were already there 20 years ago but needed the legal framework to ensure the driver was responsible for their mistakes. “This is no different if we consider AI and the physician, but with radically different technology. OCT makes no collisions because everything is clear, more accessible, and the doctor is in optimal control,” she concluded.
13 2024 MARCH | EUROTIMES
Ursula Schmidt-Erfurth MD is Chair of the Department of Ophthalmology at the Medical University of Vienna and advisor for RetInSight, Austria. ursula. schmidt-erfurth@meduniwien.ac.at

Laser Refractive Surgery for High Myopia
LASIK and SMILE each have advantages but excellent results attainable with either.
CHERYL GUTTMAN KRADER REPORTS
While LASIK and lenticule extraction with SMILE are both known to deliver excellent visual results, finding differences between the two procedures requires drilling down to take a more detailed look at available data.
Doing so definitively shows LASIK results in faster visual recovery, according to Edward E Manche MD.
“LASIK has the fastest visual recovery of any keratorefractive procedure,” Dr Manche said. “The speed of visual recovery after SMILE has improved with use of lower femtosecond laser energy settings, but even with that modification, visual recovery is still faster after LASIK.”
On the other hand, there are reasons to prefer SMILE, according to John So Min Chang MD.
“SMILE seems to have better refractive predictability than LASIK; some studies show refractive stability is better after SMILE, and SMILE has additional advantages of eliminating flap concerns and causing less postoperative dry eye.”
Time to achieving 20/20 UCVA
Providing evidence to support his conclusion, Dr Manche cited data from selected studies, beginning with results from the clinical trials that led to US FDA approval of SMILE for treating spherical myopia and myopic astigmatism. In the spherical myopia trial, only 63% of eyes achieved 20/20 or
better UCVA at one week. By one month, the percentage was still just 79%, and it only rose to 83% by three months. The myopic astigmatism study results showed 20/20 or better UCVA was achieved by only 44% of eyes at one week, 66% at one month, and 83% at three months.
Dr Manche noted multiple prospective studies directly compared LASIK and SMILE, and he discussed three trials that used different LASIK approaches.
One study published in 2016 compared wavefrontoptimised LASIK to SMILE and included about 200 eyes with a mean preoperative spherical equivalent (SEQ) of about -5.2 D in both groups.1 SMILE was performed with a laser energy setting of 180 nJ, which was the manufacturer’s recommendation when the study was conducted. On the first day postoperative, 20/20 UCVA was achieved by 73% of LASIK-treated eyes compared to 55% of those treated with SMILE. By one week and throughout follow-up to month six, UCVA was 20/20 or better in 95% of LASIK-treated eyes, only reaching that level in the SMILE group at month three.
A more recent study performed by Dr Manche and colleagues compared wavefront-guided LASIK with SMILE in 80 eyes (40 patients) with a mean SEQ of about -3.9 D.2 The energy settings for SMILE ranged from 130 to 160 nJ. By day one after surgery, 95% of LASIK patients saw 20/20 UCVA
14 CATARACT & REFRACTIVE EUROTIMES | MARCH 2024
versus only 49% in the SMILE group. In this study, the SMILE-treated eyes caught up to the LASIK group by month one when 89% achieved 20/20 or better UCVA.
Another study compared topography-guided LASIK versus SMILE with the procedures performed in fellow eyes of 30 patients.3 Mean SEQ for eyes in this study was about -4.0 D, and the laser energy setting for SMILE was 125 nJ. At one day postoperative, UCVA was 20/20 or better in 100% of LASIK-treated eyes but only 60% of eyes treated with SMILE. At one week, 86% of SMILE-treated eyes achieved 20/20 or better UCVA.
Benefits with SMILE
In his review of the literature, Dr Chang observed that in addition to evidence showing SMILE has better predictability and stability than LASIK, various studies found statistically significant differences favouring SMILE for resulting in better mean BCVA, less change in corneal spherical aberration (SA), and better corneal biomechanics.
Focusing on results from analyses of data for patients treated at his centre, Dr Chang reported better predictability with SMILE was the only statistically significant difference found between the two procedures. Data on mean postoperative SEQ showed more overcorrection after LASIK than with SMILE (+0.45 D and +0.29 D, respectively).
The review included 202 eyes of 124 patients treated with SMILE and 201 eyes of 120 patients treated with LASIK. Preoperative SEQ was greater than or equal to -6.0 D in all eyes. He reported finding no statistically significant differences between groups in mean postoperative UDVA, BCVA, or cylinder. Induction of SA was slightly greater after LASIK compared with SMILE (mean change 0.11 and 0.05 microns, respectively), with a trend towards statistical significance.
“Other studies comparing the two procedures for correcting mild and moderate myopia have also reported less SA induction with SMILE,” Dr Chang said.
In addition, an analysis of enhancement rates for a cohort of almost 2,000 eyes treated for any level of myopia over a recent two-year period showed no statistically significant difference between the two procedures. All SMILE cases were performed with the VISUMAX 800 laser. Enhancement rates were 0.18% for SMILE and 0.23% for LASIK.
Drs Chang and Manche spoke at AAO Refractive Surgery Subspecialty Day 2023 in San Francisco, US.
For citation notes, see page 46.
John So Min Chang MD is Director of the Guy Hugh Chan Refractive Surgery Centre of Hong Kong Sanatorium & Hospital, Hong Kong. John.SM.Chang@HKSH.com
Edward Manche MD is Professor of Ophthalmology at the Byers Eye Institute, Stanford School of Medicine, Palo Alto, California, US. lasik.manche@stanford.edu
15 2024 MARCH | EUROTIMES
One-stop-shop Registries in Ophthalmology registries.ESCRS.org EuReCCa European Registry for Childhood Cataract Surgery EUREQUO European Registry of Quality Outcomes for Cataract and Refractive Surgery ECCTR European Cornea and Cell Transplantation Registry Accountability. Benchmark. Patient Care. Research. Outcomes & Risks. ESCRS_Registries_Ad_HPV.indd 1 11/17/21 2:40 PM
AI Applications in Diagnostic Imaging
Accelerating the path to progress by identifying and addressing existing barriers.
CHERYL GUTTMAN KRADER REPORTS
Advances in diagnostic imaging have transformed clinical practice in ophthalmology by providing quantitative rather than qualitative information. Now, researchers are looking to use artificial intelligence (AI) to improve diagnostic accuracy and consistency of image interpretation. Achieving this goal, however, requires attention to several issues, said Michael F Chiang MD.
One key challenge for developing useful AI-enabled diagnostic systems relates to the fact the algorithm performance improves as the task narrows. In the real world, however, diagnosis involves many parallel tasks, as clinicians need to integrate data from images with their clinical findings and account for the possibility that patients can have multiple comorbid diseases.
“AI systems are improving rapidly but have yet to reach this level of sophistication,” Dr Chiang said.
To be robust and avoid bias, AI-enabled image diagnostic systems must also be trained on large, diverse data sets to ensure their application is generalisable to the diverse populations encountered in practice. However, the data being used in the research world where AI systems are being developed is often homogenous because it is extracted from a population representing a single centre or geographic region.

Recognising the importance of building large, AI-ready data sets to avoid bias, the National Institutes of Health (NIH) has become involved and established a programme known as Bridge2AI that is providing $130 million in funding across four “data generation” groups. A team led by ophthalmologists at the University of Washington in Seattle is one of the recipients of the funds from this NIH-sponsored project, Dr Chiang said.
Data sharing and collaboration for knowledge discovery are also critical for developing AI-enabled diagnostic systems, and this depends on having imaging devices that adopt imaging standards.
“The problem, however, is that in many existing ocular imaging devices, the data are often locked in proprietary formats and therefore cannot be easily exchanged or retrieved,” Dr Chiang said. He provided some personal examples from his career in academia of how this issue impeded clinical productivity and research.
Addressing the need for conformance to DICOM standards, representatives from three US agencies—the Food and Drug Administration, Office of the National Coordinator for Health Information Technology, and the National Eye Institute—held a workshop in May 2022 focused on improving interoperability among ocular imaging modalities and devices. The meeting led to the identification of knowledge gaps, barriers to progress, and potential approaches for overcoming obstacles.
“Levers that can be pulled to advance the field are described in a published position statement.1 In a nutshell, I am not enthusiastic about funding future studies using ocular imaging devices which do not conform to the DICOM standard because they would not represent the best research or clinical care.”
Noting the need for all stakeholders to work together, Dr Chiang said he was heartened by seeing the community of ocular imaging device vendors appears to be working towards platforms that conform to DICOM standards. Still, he encouraged users of ocular imaging devices to insist on adherence to standards through their interactions with vendors in the device industry.
Dr Chiang spoke at AAO 2023 in San Francisco, US.
For citation notes, see page 46.
Michael F Chiang MD is director of the National Eye Institute, National Institutes of Health, Bethesda, Maryland, US. michael.chiang@nih.gov
16 CATARACT & REFRACTIVE EUROTIMES | MARCH 2024
The Future of FLACS
Multiple issues constrain potential for achieving benefits and greater adoption.
CHERYL GUTTMAN KRADER REPORTS
Available evidence from systematic reviews and large European randomised controlled trials shows no clinically relevant differences in key outcomes achieved after femtosecond laser-assisted cataract surgery (FLACS) versus traditional phacoemulsification,1–4 said Alexander C Day MD, PhD.
Looking to the future, the likelihood that technological innovation will make FLACS better than phacoemulsification faces significant challenges considering the current lack of industry interest in upgrading lasers for FLACS, the scope of required development, and the remaining research questions.
“Currently, femtosecond lasers for FLACS are functioning as expensive devices for capsulotomy and astigmatic keratotomy,” Dr Day said.
“They perform only a few of the steps needed to complete cataract surgery, and only do some of these well. And manufacturers have made limited investment in the last five years towards further research and development of FLACS.”
The high cost of the lasers is another significant drawback for FLACS currently and presents an obstacle to its adoption in the future.
“We know from studies that FLACS is not cost-effective, which will continue to be a huge problem for the next step— [possibly robotising] the procedure,” Dr Day said.
While providing an evidence-based critique of FLACS, Dr Day prefaced the information by noting he remains a FLACS user. Unlike many cataract surgeons who have put their femtosecond lasers aside, he still thinks FLACS has distinct advantages and uses it in about one-third of his private patient cases, particularly for those having an extended depth of focus or multifocal IOL or where there is a low amount of corneal astigmatism correctable by femtosecond laser astigmatic keratotomy rather than a toric lens.
Nevertheless, he acknowledged data are needed to demonstrate that FLACS has a benefit compared with conventional phacoemulsification for improving outcomes for patients choosing a multifocal or extended depth of focus IOL.
“It is accepted that compared to manual capsulorhexis, the laser creates capsulotomies more precise in size and shape. And it is thought that a more perfect capsulotomy with centration on the visual axis might be critical for achieving better visual results and possibly less dysphotopsias when implanting advanced technology lenses,” said Dr Day.
“However, there are no comparative studies on outcomes with these lenses implanted after FLACS or manual surgery, and a key question is whether we even need the laser for capsulotomy,” said Dr Day, citing a study showing that after manual capsulorhexis, modern IOLs maintain good centration unless the capsule opening is severely malformed.5
Novel but non-essential applications
Certain femtosecond lasers used for FLACS are equipped with various features that may be considered “nice to have” but are not essential, Dr Day said.
For example, when used in cases needing astigmatic correction, some lasers can automatically align astigmatic incisions on the steep axis or create alignment marks on the cornea or capsule that remain visible at follow-up.
In addition, the laser can be used to perform a primary posterior capsulotomy, which is very technically demanding if done manually. Not all eyes need to be treated for posterior capsule opacification, and should the need arise, can be successfully treated with Nd:YAG capsulotomy.
“Is this just trying to find use for a technology that we don’t really need?” Dr Day said.
Dr Day spoke at the 2023 ESCRS Congress in Vienna.
For citation notes, see page 46.
Alexander C Day MD, PhD is a Consultant at Moorfields Eye Hospital and Associate Professor, UCL Institute of Ophthalmology, London, England, UK. alex@alexday.co.uk
17 2024 MARCH | EUROTIMES
The Modern Era of Refractive Surgery
New technologies for screening and treatment qualify more patients for intervention.
CHERYL GUTTMAN KRADER REPORTS
Advances in both preoperative diagnostics and treatment technologies are helping overcome barriers to refractive surgery and broaden the pool of patients who can undergo a safe and successful procedure, according to Victor Derhartunian MD.
“Overall, we now have a refractive surgery solution for 99.9% of patients,” he said. “We just need to choose the right patient for the right procedure.”
Currently, LASIK and femto-LASIK remain the gold standard for refractive surgery, but LASIK use is limited by patient concerns about the potential for flap-related complications along with postoperative problems with dry eye and visual symptoms.
Concerns about dry eye appear justified based on the results of a poll of attendees at the session where Dr Derhartunian spoke and the 2022 ESCRS Clinical Surgery Trends survey. However, according to surgeons who completed the latter questionnaire, dry eye occurs less often after lenticule extraction than following LASIK.
“LASIK has a greater impact on corneal nerve anatomy compared to lenticule extraction, and dry eye symptoms are less severe and usually faster to recover after a lenticule extraction procedure,” said Dr Derhartunian.
Newer diagnostics technologies that offer automated screening for dry eye with measurement of noninvasive tear breakup time and other objective disease-related signs are helping to identify patients at greatest risk for dry eye problems after LASIK.
“These patients can be offered lenticule extraction or phakic IOL implantation that could possibly even avoid exacerbating dry eye after surgery,” he said.
The risk of developing corneal ectasia after surgery represents another issue that limits patients from undergoing LASIK. However, advances in diagnostics have also improved the precision of screening for keratoconus and identifying eyes at risk for post-LASIK corneal ectasia. These developments include the shift from the use of Placido topography to Scheimpflug imaging, improved software for cornea analysis with Scheimpflug imaging, anterior segment OCT with epithelial mapping, and the introduction of artificial intelligence-based techniques.
“If we recognise through the use of good diagnostics that an eye is at risk for ectasia after LASIK, we can decide not to do any surgery or choose a phakic IOL,” Dr Derhartunian said.
Improving outcomes of LASIK alternatives
Stating lenticule extraction is a safe, effective, and predictable treatment for high myopia and myopic astigmatism that will
hopefully soon be approved for hyperopia, Dr Derhartunian said improvements in the pioneering femtosecond laser system used for lenticule extraction enabling centration and cyclorotation control are leading to better visual quality outcomes after this type of surgery. Now, lenticule extraction will also be an option using femtosecond lasers marketed by three other companies.
Phakic IOLs not only offer a refractive surgery option for eyes at risk for ectasia or dry eye after LASIK, he said, but they also expand the range of refractive surgery candidates because they can be used to treat higher degrees of myopia, astigmatism, and hyperopia along with presbyopia.
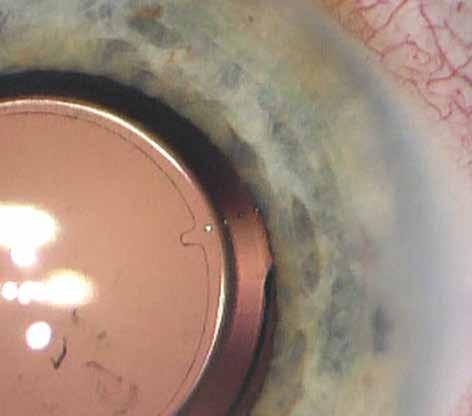
Today, only two options remain for phakic IOL implantation—the iris-fixated lens (Artisan) and the sulcus-supported implant (ICL). Outcomes with these devices have also improved due to changes in lens design and use of diagnostics that guide sizing and predict vault.
Dr Derhartunian presented at the 2023 ESCRS Congress in Vienna.
Victor Derhartunian MD is in private practice at EyeLaser Clinics in Vienna, Austria; Zurich, Switzerland; and SwissLaser Clinics in Poland. VD@EyeLaser.at

18 CATARACT & REFRACTIVE EUROTIMES | MARCH 2024
Apply for the
John Henahan Writing Prize
Burnout is a chronic issue in ophthalmology, leading a growing number to abandon the field early in their careers. What should be done to reduce unnecessary stress in training and practice, allowing for a successful long-term career?
Young ophthalmologists are invited to submit their answer to that question in an 800-word essay for the John Henahan Writing Prize. The author of the winning essay will receive a €500 bursary and a specially commissioned trophy, awarded during the 2024 ESCRS Congress in Barcelona, Spain. The winning essay will be published in EuroTimes.
The competition is open to ESCRS members (including the free membership available to trainees) age 40 or younger on 1 January 2024.
For details, please see the dedicated page on our website https://www.escrs.org/eurotimes/john-henahan-writing-prize

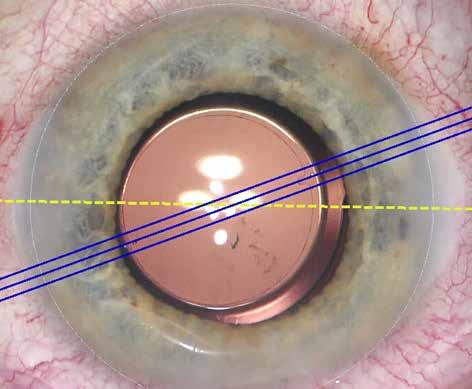
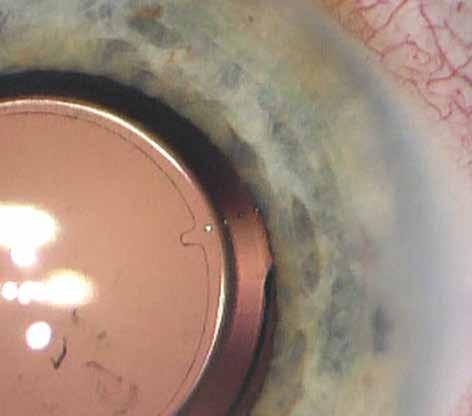
Advances in Toric IOL Alignment
Biomorphometric approaches offer high precision and increase efficiency.
CHERYL GUTTMAN KRADER REPORTS
Aprospective clinical study evaluating two biomorphometric systems for intraoperative guidance of toric IOL positioning show both were associated with very low misalignment, said H Burkhard Dick MD, PhD.
“Cataract surgeons agree that the future will be digital and biomorphometric decision-making will play a major, if not a decisive, role in our procedures,” he said. “Compared to manual marking of the reference axis, biomorphometric-guided alignment techniques definitely improve surgical workflow and appear to be a step towards achieving higher patient satisfaction after cataract surgery. Other companies have also introduced biomorphometric approaches for toric IOL alignment that take us away from reliance on preoperatively marking the reference axis.”
The study included 28 eyes of 23 patients who underwent cataract surgery performed by a single surgeon with implantation of a single type of toric IOL.1 Mean preoperative cylinder for the group was about 2.2 D.
The study was designed to compare the performance of two commercially available biomorphometric methods for toric IOL alignment—an image-guided system (CALLISTO eye Z ALIGN, Zeiss) in which the reference and target axes are superimposed into the surgical microscope while scleral and limbal blood vessels are matched with a preoperatively captured image, and a femtosecond laser-assisted capsular marking system (IntelliAxis-L, Lensar) that creates markings on the capsule during capsulotomy and compensates for cyclorotation by matching a preoperatively captured iris image with the intraoperative image through iris registration.
“Both systems compensate for cyclorotation that can occur when patients change from an upright position,” Dr Dick said.
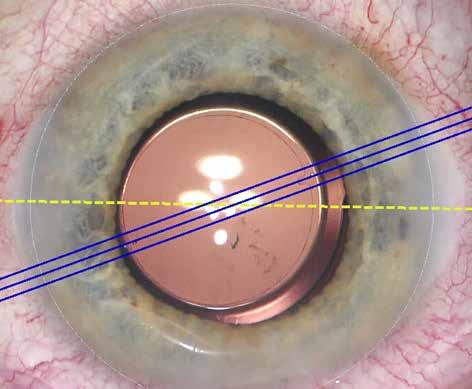
The two systems were applied simultaneously in each case. The final toric IOL alignment was guided by the capsular markings. Misalignment from intended axis was analysed as the study outcome and determined based on analysis of images from an intraoperative surgical video and postoperative slit lamp images.
20 EUROTIMES | MARCH 2024
CATARACT & REFRACTIVE
Toric IOL alignment based on data injection (Callisto).
The results showed mean misalignment was very low with both methods, but it was significantly less using the capsular marking system compared to the digital marking approach (1.71° versus 2.64°; P = 0.016). The greater precision of the femtosecond laser-assisted method may be attributed to its potential to avoid parallax error, which is partly explained by the fact the alignment marks made with the laser are approximately the same level as the toric IOL, Dr Dick explained.
Refractive and functional outcomes were excellent. Mean postoperative uncorrected distance visual acuity was 0.14 logMAR, and mean postoperative refractive astigmatism was 0.3 D.
“Our study was not designed to compare refractive and visual acuity results associated with the two methods, and it is questionable whether the lower probability of misalignment with the capsular marking approach would have led to significant differences,” Dr Dick said.
He noted that previous studies have shown the superiority of the femtosecond laser-assisted and digital marking methods of toric IOL alignment with manual marking.
“To our knowledge, this is the first study that compared two biomorphometric methods for toric IOL alignment.”
Dr Dick spoke at the ESCRS Symposium during Refractive Surgery Subspecialty Day at AAO 2023 in San Francisco, US.
For citation notes, see page 46.
H Burkhard Dick MD, PhD is Professor and Chairman, Department of Ophthalmology, Ruhr University, Bochum, Germany. burkhard.dick@kk-bochum.de
•
•

•
•
•




21 2024 MARCH | EUROTIMES Non Contact Tono/Pachymeter Non Contact Tonometer / New Design Innovations that Incorporate Operator and Patient Comfort with Gentle Measurements
Fully-automatic measurement*1
Gentle voice guidance (available in 9 languages)*1
Reliable tono/pachymeter*2
Flexible and space-saving design
A variety of options to meet your needs *1 Available for the NT-1p and NT-1 *2 Pachymetry is available for the NT-1p. For the NT-1, the corrected IOP is displayed by entering the patient‘s central corneal thickness. www.nidek.com ET 93 x 266mm
Toric IOL alignment based on capsular marks (IntelliAxis).

Growing Options Optimise Outcomes in Cataract Surgery
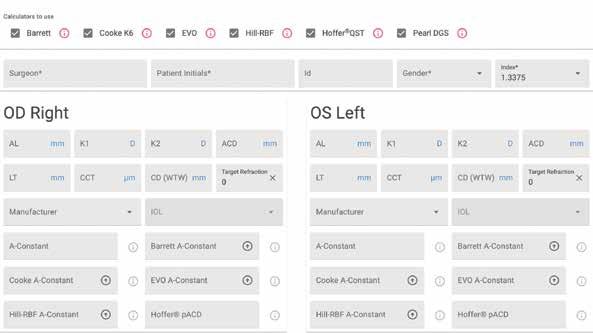
Understanding the promise and potential problems of AI-based IOL formulas.
CHERYL GUTTMAN KRADER REPORTS
The array of IOL power formulas has expanded through an influx of new options based on artificial intelligence (AI) or incorporating some AI elements. Studies evaluating the performance of these AI-driven formulas show they hold potential promise for providing more accurate refractive outcomes and might be especially useful in more challenging situations where refractive outcomes tend to be more unpredictable, i.e., when applied in cases involving short, long, or post-refractive surgery eyes.
However, more studies evaluating AI-driven formulas are needed because they are still considered “young technology”, said Thomas Kohnen MD, PhD.
Further advances might depend on the remaining need to unlock the solution for attaining improved prediction of effective lens position (ELP), according to Oliver Findl MD.
“We know the refractive outcome is probably the most critical of all outcome parameters for achieving patient satisfaction after cataract surgery,” he said. “Available modern formulas perform very well in normal eyes, but consistently achieving the target refraction is more challenging in short and long eyes, where the main issue is accurate prediction of IOL position after surgery.”
Until there are advances such that IOL power can be consistently selected to achieve the targeted refractive outcome, perhaps the formulas should be renamed IOL power estimation formulas, Dr Kohnen observed.
“Calculation may be the wrong descriptive term because it implies that we always get the right target, but we don’t,” he explained. “Rather, what we have with current formulas is mostly an approximation or estimation.”
Classifying the AI options
The proliferation of AI-driven IOL formulas is highlighted in a forthcoming article in the Journal of Cataract & Refractive Surgery authored by Drs Giacomo Savini, Ken Hoffer, and Thomas Kohnen, outlining a new classification system for IOL power formulas. Their scheme groups them into three broad categories: vergence, AI, and raytracing. The AI category includes the Hill RBF, Karmona, and Nallasamy formulas. However, subdivision of the vergence and raytracing formulas based on additional features shows the inclusion of formulas with AI elements.
The only “AI” formula within the raytracing category is the Zeiss AI IOL calculator, but the vergence category includes five—namely the thick lens PEARL-DGS and the 3C Calculator, Hoffer QST, Kane, and Ladas AI, which are all thin lens formulas.
Published studies reviewed by Drs Findl and Kohnen highlight good predictive accuracy of the AI-driven formulas. The differences in performance were sometimes small and perhaps not clinically relevant. However, when considering outcomes across the full spectrum of short, normal, and long
22 EUROTIMES | MARCH 2024 CATARACT & REFRACTIVE
eyes, the AI-based approaches appear to provide the best results overall, Dr Kohnen said.
Discussing the need for better prediction of ELP, Dr Findl also cited a study that found strategies using deep learning algorithms outperformed a traditional multilinear regression technique.
Easing the planning burden
As the number of IOL power formulas continues to grow—and with many options accessible only online and not on instruments surgeons use routinely for preoperative biometry— checking and comparing the results generated by different formulas can become tedious and time-consuming. The online ESCRS IOL calculator represents a useful tool addressing this challenge because it allows surgeons to efficiently access results from multiple modern IOL formulas after inputting data just one time into a single entry form.
“The ESCRS calculator is a convenient tool that includes the most recent and better IOL formulas and is something cataract surgeons may want to use in their daily routine, especially in the more difficult cases involving short and long eyes,” Dr Findl said.
Launched in September 2022 at the ESCRS Congress, the calculator originally included only standard non-toric IOL power calculation formulas. Recently, however, a toric calculator was added, and work is underway to create an option for IOL calculations in eyes with a history of corneal refractive surgery.
Acknowledging the problems
Excitement about the potential for achieving improved refractive results by using AI to develop IOL power formulas must be tempered by consideration of the issues accompanying its use, Dr Kohnen said.
The need for a huge amount of data underlies one challenge, accompanied by concerns about security to protect the safety of digital patient data. In addition, transparency is needed for gaining user trust, but transparency is not yet there.
“With AI, we have a black box situation because it is not known how the results were reached,” Dr Kohnen said. “Improvements are needed for understanding the decision-making process of the AI models.”
Drs Findl and Kohnen spoke at the ESCRS Symposium during AAO Refractive Surgery Subspecialty Day 2023 in San Francisco, US. Oliver Findl MD, MBA is Chief of the Department of Ophthalmology, Hanusch Hospital, Vienna, Austria. ofindl@gmail.com
Thomas Kohnen MD, PhD, FEBO is Professor and Chair of the Department of Ophthalmology, Goethe University, Frankfurt, Germany. kohnen@em.uni-frankfurt.de

ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
23 2024 MARCH | EUROTIMES
iLEARN
Improving Preoperative Prediction of PCR
Machine learning models show promise, outperforming existing scoring systems.
CHERYL GUTTMAN KRADER REPORTS
Posterior capsule rupture (PCR) occurs in approximately 1% of cataract surgery cases and is a feared event because of its potential sight-threatening consequences.
Now, work is underway leveraging data reported to the European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO) to see if a machine learning model could improve preoperative identification of patients at increased risk of PCR.1
Research conducted so far indicates such artificial intelligence-based classifiers outperform existing scoring systems and, therefore, if implemented in the clinic, may reduce the number of cases of PCR, said Rudy MMA Nuijts MD, PhD.
“Identification of patients at high risk for PCR is important so that these difficult cases can be assigned to experienced operators and for providing better communication to patients about their surgical risk,” said Dr Nuijts. “Existing scoring systems for PCR risk assessment are based on a subjective weighting of known risk factors. We were interested in seeing if data-driven risk assessment would estimate the probability of PCR more reliably and objectively.”
Three different probabilistic classifiers were constructed to estimate the probability of PCR before surgery. They included two discriminative models—a logistic regression model and a multi-layer perceptron network—and a generative model known as a Bayesian network, which has the advantage that it can deal with missing data, Dr Nuijts said.
“Analysing data for PCR risk prediction is challenging because PCR is rare, there is an exponential number of feature combinations, and, as in all registries, we have missing data.”
All the classifiers were trained using data from about 2.8 million cases of cataract surgery performed between January 2008 and December 2018. Performance of the classifiers was determined by calculating area under the precision-recall curve (AUPRC). The results showed the multi-layer perceptron
network performed best followed by the Bayesian network and then the logistic regression model. The mean AUPRC for the three classifiers was 13.10, 8.05, and 7.31, respectively.
Analysing data for
PCR risk
prediction is challenging because PCR is rare.
“The multi-layer perceptron performs better than subjective grading systems published in the literature,” Dr Nuijts said. “In addition, compared to a random classifier that has no knowledge of the patient or procedure, the machine learning classifiers are about 7 to more than 12 times better in generating the probability.”
24 CATARACT & REFRACTIVE EUROTIMES | MARCH 2024
0 20 40 60 80 100 0 20 40 60 80 100 Recall(%) Precision(%) BayesianNetwork LogisticRegression Multi-LayerPerceptron
Figure 1. The PR curves of the classifiers. The shaded areas highlight the two standard deviation error bands around the mean precision.
Analysis of an independence graph generated by the Bayesian network model was also performed to characterise direct and indirect risk factors for PCR. Direct risk factors included preoperative best-corrected visual acuity, year of surgery, operation type, anaesthe sia, target refraction, other ocular comorbidities, white cataract, and corneal opacities.
Going forward, further work aims to validate and compare the machine learning models using data from other registries, such as the American Academy of Oph thalmology’s Intelligent Research in Sight (IRIS) regis try. Once the model is validated, Dr Nuijts envisioned the ideal situation as relevant information, including measurements from diagnostic systems, would auto matically be entered into the electronic medical record, where they would be available to be processed in the probabilistic classifier.
“This would be the most efficient and beneficial way for surgeons to have an idea of the risk of PCR for any individual patient,” Dr Nuijts said.
Dr Nuijts spoke at the ESCRS Symposium during AAO Refractive Surgery Subspecialty Day 2023 in San Francisco, US. He acknowledged his co-authors—Dr Ron Triepels, Dr Maartje Segers, and Dr Mor Dickman.
For citation notes, see page 46.

Rudy MMA Nuijts MD, PhD is Professor of Ophthalmology, Vice-Chairman, and Director of the Cornea Clinic and the Center for Refractive Surgery at the University Eye Clinic, Maastricht, Netherlands. rudy. nuijts@mumc.nl
Ron JMA Triepels PhD is assistant professor at the Department of Data Analytics and Digitalization of Maastricht University, Maastricht, Netherlands. r.triepels@maastrichtuniversity.nl
Maartje HM Segers MD is a PhD candidate at the University Eye Clinic, Maastricht University Medical Center+, Maastricht, Netherlands. maartje. segers@mumc.nl
Mor M Dickman MD, PhD is associate professor at the University Eye Clinic, Maastricht, Netherlands, and clinical co-director of the ESCRS registries. mor.dickman@mumc.nl
25 2024 MARCH | EUROTIMES
escrs.org/eurotimes/ supplements/ Explore IOL solutions and demystify common misunderstandings with insights into a refractive future that offers more improved postoperative outcomes—exclusively on the ESCRS website. SUPPLEMENT YOUR IOL KNOWLEDGE
Monofocal Plus Finding the Balance
Enhanced monofocals may be the future standard of care in cataract patients.
ROIBEÁRD O’HÉINEACHÁIN REPORTS
New enhanced monofocal intraocular lenses (IOLs) provide a higher degree of functional vision than standard monofocal IOLs—without additional risk. The lenses are, therefore, promising candidates as the standard of care for cataract patients, said Filomena Ribeiro MD, PhD.
She noted cataract patients generally receive some treatment for presbyopia, either in the form of multifocal spectacles or contact lenses, or IOLs that offer varying degrees of multifocality or extended depth of focus. Both approaches have risks and benefits. In the case of the IOLs, there can be the risk of halos and dysphotopsias. For spectacles, there can be an increased incidence of falls. Multifocal spectacles contribute to one of three falls among the elderly, likely due to poor vision at intermediate distances.
A study of 40 cataract patients monitored with a Vivior headset over 36 hours showed activities involving intermediate vision comprised around a third of their waking hours.1 The evolution of multifocal and extended depth of focus (EDOF) IOLs has reflected an increased appreciation of the importance of intermediate distance vision: trifocals now direct 30% of light to the intermediate focus compared to less than 20% in some earlier models.
The risk/benefit profile of multifocal and EDOF IOLS compared to standard monofocal IOLs is largely the compromise between spectacle independence and quality of vision. Enhanced monofocal IOLs aim to reduce that compromise to a minimum while providing around a line of additional intermediate visual acuity.
“What we really need is to find the best balance between functional vision and quality of vision for patients to perform all their daily activities,” Prof Ribeiro said. “If we increase a little bit the primary or secondary spherical aberration—or a mix of both—we can increase the depth of field, [providing] more intermediate vision without a perceived loss of quality of vision.”
The enhanced monofocal IOLs available today include the Tecnis® Eyhance (Johnson & Johnson), the Isopure (BVI Physiol), and the RayOne (Rayner). The Eyhance combines negative spherical aberration with an increase of central curvature, the Isopure uses negative aberration customised top dioptric power, and the RayOne uses positive spherical aberration.
In the numerous studies published to date, enhanced monofocal IOLs showed a similar distance visual acuity and better uncorrected intermediate visual acuity compared to standard monofocal IOLs while providing similar contrast sensitivity and a similarly low incidence of halos and glare. On that basis, they could become the standard of care for
cataract. Achieving that status will require agreement with regulatory bodies and support from professional organisations with consensus statements based on scientific evidence, including clinical and patient-reported outcomes and cost-effectiveness studies, Prof Ribeiro noted.
“We still need more studies, but the trend is that in the near future, enhanced monofocals could be the new standard of care.”
Prof Riberio presented at the ESCRS eConnect Webinar “Evidence-based overview of current premium IOL technologies.”
For citation notes, see page 46.

26 CATARACT & REFRACTIVE EUROTIMES | MARCH 2024
Filomena Ribeiro MD, PhD, FEBO is the head of the Department of Ophthalmology, Hospital da Luz, Lisbon, and President of the ESCRS. filomenajribeiro@gmail.com

The FEBOS-CR Subspecialty Exam 2024 is
now open for applications.

Have your knowledge and expertise in cataract and refractive surgery tested and o icially acknowledged by sitting the EBO-ESCRS Subspecialty Exam. Successful candidates will be awarded the Fellow of the EBO Subspecialty Cataract & Refractive Surgery Diploma (FEBOS-CR). This diploma is recognised as proof of advanced knowledge and competence in this field.
The exam will take place at the ESCRS Annual Congress in Barcelona. Application deadline is Friday, 29 March 2024.
Apply Now




Overcoming Issues Limiting DMEK Access and Success
Synthetic endothelial corneal layer offers alternative for treating chronic corneal oedema.
CHERYL GUTTMAN KRADER REPORTS
Implantation of an artificial corneal layer (EndoArt, EyeYon Medical) effectively reduces central corneal thickness and restores central corneal transparency in eyes with chronic corneal oedema associated with endothelial dysfunction. Victor A Augustin MD reported this conclusion based on the results of up to four years of follow-up in more than 100 eyes.
“Descemet membrane endothelial keratoplasty (DMEK) is the gold standard for treating endothelial diseases. However, its use may be limited by a shortage of donor grafts, and it is associated with other disadvantages and risks,” said Dr Augustin.
“As an alternative to DMEK, use of the artificial DMEK layer could help treat chronic corneal oedema temporarily or permanently, especially in countries with limited access to donor tissue or in eyes with features that make DMEK technically difficult or at risk for early failure.”












The artificial corneal replacement is CE certified and has the US FDA breakthrough device designation and Green Channel fast-track priority approval from China’s NMPA. The domeshaped implant matches the curvature of the posterior cornea. It is made of an optically clear, flexible, biocompatible, biostable hydrophilic copolymer and measures 50 microns thick and 6 mm in diameter. First implanted in 2019 under a first in-human study protocol, the device serves as a waterimpermeable barrier on the posterior corneal surface where it impedes transfer of aqueous humour into the central cornea.
Implantation of the artificial corneal layer is easier than a DMEK graft. The device is introduced using an IOL injector and positioned onto the posterior corneal surface using an air bubble technique. Anterior segment OCT can help guide placement in difficult anterior chambers, and fixation with a single suture mitigates risk for early detachment, Dr Augustin said.
Images from selected patients who had failed DMEK, were considered likely to fail DMEK, or who refused DMEK showcased the ability to achieve durable reduction of central corneal thickness and maintenance of central corneal clarity post-implantation. Insight into the mechanism of the device’s adhesion was provided in a case involving a patient who had undergone removal of the artificial corneal layer due to stromal fibrosis followed by penetrating keratoplasty.


“We have seen with anterior segment OCT that the implant becomes completely attached, but we still don’t know that much about the mechanism of the adhesion. Histological evaluation of the removed tissue in this case showed the implant was incorporated with the host tissue by fibroblasts and matrix tissue,” Dr Augustin said.
A case of a patient with Fuchs’ endothelial corneal dystrophy who refused DMEK because of religious reasons showed the potential for improving visual acuity after implanting the artificial corneal layer. Visual acuity in this eye improved from 20/800 to 20/40 at six months after the surgery.


“Many patients receiving the implant had poor visual potential because of significant comorbidities,” he said. “Because of corneal oedema in the periphery, this patient did not achieve the same good result possible after DMEK. However, she still had a nice improvement in VA.”
Dr Augustin spoke at AAO 2023 in San Francisco, US.


Victor A Augustin MD is a senior physician in the department of ophthalmology, University of Heidelberg, Heidelberg, Germany. vaugustin@web.de, victor.augustin@med.uni-heidelberg.de
CORNEA 28 EUROTIMES | MARCH 2024

Tech Advances Microbial Keratitis Care
Effective algorithms for detection, diagnosis, and monitoring expected to reduce clinician burden and improve patient care.
CHERYL GUTTMAN KRADER REPORTS
Applying artificial intelligence (AI) to evaluate images of corneal ulcers holds potential for improving detection of microbial keratitis, differentiating the pathogenic cause, and monitoring response to intervention, reports Maria Woodward MD.
Discussing the intended goal of research underway developing AI in this realm, she explained it is not to replace the job of clinicians. Instead, she expects it could increase the efficiency and accuracy of clinical decision-making and thus allow practitioners to provide better patient care.
“I hope to dissuade some fears about applying AI for microbial keratitis diagnosis and management and inspire some use,” Dr Woodward said.
“To ophthalmologists who fear how it will impact their practice, I would say there is no need for an existential crisis because we will still be very needed. Just as an electrocardiogram is a tool used by cardiologists, AI interpretation of microbial keratitis can be a tool that can help us manage our patients better.”
Breaking down the functions
Decision-making for patients presenting with a corneal ulcer can be broken down into three components—detection of an infectious lesion, diagnosing its cause, and monitoring disease course over time. Those components dovetail respectively with the three domains of AI algorithms described as classification, object detection, and segmentation.
Research has already been done cultivating AI algorithms for determining whether a corneal ulcer is infectious or non-infectious, and progress is being made in developing algorithms that can differentiate/classify the causative organism.
“I would argue that the use of AI-enabled systems for deciding whether an ulcer is infectious or non-infectious probably has greater applicability for workers in community health or primary care settings,” Dr Woodward said.
“However, as AI algorithms get better, they could also be useful for helping ophthalmologists determine the organism type of microbial keratitis.”
Currently, however, the detection and classification algorithms are in the efficacy stage of development and not at the stage where they have demonstrated effectiveness and are ready for use in the clinic, she added.
Dr Woodward said that recognising how much variability exists among clinicians in how they measure morphologic features, her interest has focused on developing AI segmentation algorithms. Research conducted in collaboration with colleagues at Aravind Health System in India led to the development of a semiautomated algorithm for image-based analysis shown to reduce clinician-dependent variability in measurement of corneal ulcer size. Now, in work funded by the National Institutes of Health with Dr Sina Farsiu at Duke University (North Carolina, US) and others, a deep learning algorithm capable of measuring features of the ulcer over time is being developed.
“The goal of this work is to link the features to function and outcomes,” Dr Woodward said.
“With the ability to measure features we can determine disease severity. And when we are able to measure features over time, we can determine if patients are getting better, worse, or staying the same. This information can help clinicians decide about initial intervention and need for its modification, and it can also have value for guiding clinical trial design, including drug efficacy studies.”
Dr Woodward spoke at AAO 2023 in San Francisco, US.
Maria A Woodward MD, MS is Associate Professor, Ophthalmology and Visual Sciences, University of Michigan, Ann Arbor, US. mariawoo@umich.edu
29 2024 MARCH | EUROTIMES

Knowing Iris Repair: Pupilloplasty
This second of the series on iris repair covers everything pupilloplasty.
DR SOOSAN JACOB MS, FRCS, DNB
The iris plays an important visual function, modulating entry of light as well as controlling the effect of higher-order aberrations. In addition, an abnormally positioned iris can result in complications such as glaucoma or an increased risk of corneal graft rejection. The iris also plays an aesthetic role, especially in light-coloured irides.
Pupilloplasty can be done for visual purposes to decrease glare or reduce the effect of HOAs, for anatomical reasons to create a taut iris diaphragm and prevent peripheral anterior synechiae, or for aesthetic reasons, e.g., to correct an ectopic pupil or close an iris defect in light-coloured irides.
Iris reconstruction should therefore be an essential skill for all anterior segment surgeons. In the second of this multi-part series on iris repair, we will discuss various pupilloplasty techniques, some which can also be used for haptic fixation to the iris.
Most iris reconstruction techniques use a 10-0 or 9-0 Prolene suture on a long, thin, and curved CI-4 needle, though a long and straight needle may also be used if curved is unavailable. Pupilloplasty is difficult in phakic eyes for fear of damage to the crystalline lens from the needle passes and are also not preferred because of the difficulty during a subsequent cataract extraction. Thus, if pupilloplasty is required, it is preferable to do a cataract surgery and implant the IOL first.
McCannel suture
Introduced in 1976, the McCannel suture technique uses a 10-0 Prolene suture on a long needle introduced through the limbus and passed through the approximated first and second iris edges and out the limbus on the other side. The suture on either side of the iris is then retrieved with a Sinskey or
Kuglen hook passed through a paracentesis created between the two limbal sites and a single or double knot is slowly and gently tightened to approximate the iris edges. Further knots are then thrown. The McCannel suture has the disadvantage of traction on the iris towards the paracentesis while tightening the knots that may not be tight enough.
Siepser sliding knot
Siepser modified the McCannel suture in 1994 by introducing the sliding knot to make tightening easier and less traumatic to the iris. It gives a tighter knot and better approximation of the iris. Here, the knot is tied outside the eye and then drawn in to be tightened over the iris.
A long, thin, curved needle on a 10-0 Prolene suture is passed from the limbus through the first and second limbs of the iris and then railroaded into a 26-gauge needle passed into the anterior chamber (AC) through a limbal paracentesis and thus brought out. A Sinskey or Kuglen hook is passed through the paracentesis and the initial length of the suture before the first pass through the iris is hooked and brought out through the paracentesis in the form of a loop. The trailing segment is then passed over and under one side of the retrieved loop to create the knot.
Osher’s modification
Professor Robert Osher’s modification of the Siepser knot created two consecutive slip knots around a carefully untwisted, retrieved suture loop—the first one tightened after passing the cut end twice around the strand emanating from the iris, followed by retrieval of the loop again to create one locking knot.
30 EUROTIMES | MARCH 2024
CORNEA

Condon’s modification
Dr Garry Condon modified the Siepser knot by using forceps to wrap one side of the loop around the suture, just as in a simple double throw knot.
Single-pass, four-throw pupilloplasty
Dr Amar Agarwal modified this further by using only a single pass and four throws. A paracentesis is created at the site through which the needle will emerge after the second iris pass. Any pre-existing paracentesis sufficiently close may also be used instead.
The first limb of the iris to appose is held with a microforceps that passes through this paracentesis. A 10-0 Prolene suture on a long, thin, curved CIF-4 needle or a straight STC-6 needle is passed trans-limbally through the iris root, sufficiently close to the edge to prevent undue iris bunching but with sufficient gap to prevent cheese-wiring. The needle is then carefully released and allowed to rest freely. Followed by a 30-gauge needle passed through the paracentesis, taking care not to engage corneal tissue.
The second limb of the iris is held firmly by a microforceps passed through a second paracentesis, and the 30-gauge needle is passed through the iris, again close to its edge. The needle on the 10-0 Prolene suture is docked into this 30-gauge needle and railroaded out through the paracentesis. A
two ends of the suture on either side of the limbus are then pulled in opposite directions—this internalizes the knot and tightens it over the iris, bringing the two limbs of the iris together. Advantages include ease of surgery and the ability to use either limb of the externalized loop.
Pinhole pupilloplasty (PPP)
As described by Dr Agarwal, the pupil is made pinhole sized to remove the effect of HOAs and improve visual acuity in eyes with high amounts of irregular astigmatism.
Open-sky pupilloplasty
A pupilloplasty is often needed in combination with a penetrating keratoplasty. In this case, an open-sky pupilloplasty may easily be done. A short, curved needle on a 10-0 nylon suture is often easier to pass than the long, curved needle attached to the 10-0 Prolene suture. Care should be taken to avoid excess pulling to avoid any tug on the ciliary body in the open-sky state.
Complications
There must be enough stretch in the iris to bring the limbs together from either side. If pulled without sufficient laxity for the two limbs to appose, the suture can cheese-wire through the iris, or the iris can detach from its root, creating an iridodialysis and bleeding into the AC. Excessive stretch can also result in iris stromal tears, iris hole creation, etc. Extensive manipulation can result in postoperative iritis.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
31 2024 MARCH | EUROTIMES
Kuglen or Sinskey hook draws a loop of the initial pass of the suture out through the paracentesis. The free end of the suture is then cut and looped four times around the externalized loop. The
Figure:
A–C) The 10-0 Prolene and the 30-gauge needle are, respectively, passed through the limbs of the iris on either side. The long needle on the 10-0 Prolene suture is railroaded into the 30-gauge needle and externalized through the paracentesis. D) A loop of the suture is pulled out through the paracentesis. E) The cut end of the suture is thrown four times around the loop. F) Pulling apart the two suture ends on either side results in the knot sliding in and tightening the two limbs of the iris snugly.
Optogenetic Therapy for Stargardt Disease
Single intravitreal injection shows promise for improving vision and quality of life.
CHERYL GUTTMAN KRADER REPORTS
The 48-week follow-up in the 1-year phase 2 STARLIGHT trial shows optogenetic treatment with MCO-010 (sonpiretigene isteparvovec) in patients with severe vision loss from Stargardt disease was well-tolerated and associated with improvements in visual function, including visual acuity, visual field, and patient-reported outcome measures, reported Michael Singer MD.
“But it’s not important what I tell you [about the study results],” Dr Singer said. “What really counts is what patients have to say.”
To make his point, he showed an excerpt from a videotaped interview with a study participant who described seeing colours more vividly, no longer needing magnification to read some text on her mobile phone, and the ability to recognise characters on television by face structure rather than voice.
“Every little bit of vision is better than what I had before,” the patient said.
Study design and data
Delivered as an intravitreal injection, MCO-010 is an adeno-associated virus 2-packaged optogenetic therapy that targets bipolar cells and sensitises them to light.
“The important thing about this therapy is that it has the potential to treat all outer retinal degenerative diseases—including geographic atrophy, irrespective of genotype,” Dr Singer said.
STARLIGHT enrolled six patients with a documented clinical or genetic diagnosis of Stargardt disease who had BCVA 1.3 to 1.9 logMAR in the study eye. Three patients had centre-involving degeneration (macular phenotype), and three had peripheral-involving panretinal disease. The patients were given a single intravitreal injection of MCO010 1.2E11 gc (genome copies) into one eye and received oral steroid for inflammation prophylaxis in a 20-day tapering regimen.
Safety was assessed as the primary endpoint in STARLIGHT, and there were no serious adverse events. Three eyes developed intraocular inflammation that was no worse than grade 2, controlled with topical and/or oral steroids, and resolved by 12 months. There were no cases of endophthalmitis, retinitis, choroiditis, or vasculitis.
“MCO-010 was previously investigated as a treatment for retinitis pigmentosa in the RESTORE trial1, and it is nice to see the favourable safety and efficacy results achieved in RESTORE were mirrored in this population of patients with Stargardt disease,” Dr Singer said.






perimetry; for both efficacy measures, patients with macular disease achieved improvements in their results that were clinically meaningful and better than their counterparts with peripheral retina involvement. In the overall cohort, BCVA improved from baseline to week 48 by a mean of 5.5 ETDRS letters and by 13 ETDRS letters in testing using a wearable magnifier. Among the three patients with the macular phenotype, two gained ≥7 letters—all three gained >30 letters using a magnifier.
Visual field mean defect improved by a mean 2.6 dB overall, with three patients in the macular degeneration phenotype showing a mean benefit 5.2 dB. Data from the validated Michigan Retinal Degeneration Questionnaire, which were analysed as exploratory endpoints to understand the potential treatment effect on quality of life, showed all patients had improved scores in the colour and contrast and reading domains.
“These are the kinds of measures patients with low vision really care about,” Dr Singer said.
Dr Singer spoke at the 2023 EURETINA Congress in Amsterdam.
For citation notes, see page 46.
RETINA 32 EUROTIMES | MARCH 2024
Michael Singer MD is Clinical Professor of Ophthalmology at the University of Texas Health Science Center, San Antonio, US. msinger11@me.com
Semaglutide Shows DR Changes
Retrospective
registry-based trial examines semaglutide treatment impact on diabetic eye disease.
CHERYL GUTTMAN KRADER REPORTS
Aretrospective observational study including data from 96,432 eyes of patients with diabetes who predominantly had no or minimal diabetic retinopathy (DR) found that most eyes had neither worsening of their DR status nor experienced vision-threatening complications related to DR within two years after starting treatment with subcutaneous semaglutide.
“Semaglutide treatment for type 2 diabetes has been associated with an increased risk of DR complications. More data on its impact on diabetic eye disease would be useful for informing screening guidelines, monitoring schedules, and patient counselling,” said Zeeshan Haq MD. “The major strength of our research is it is based on a relatively large real-world population. However, while it seems to provide some reassuring news about the effect of semaglutide on diabetic eye disease, the findings must be considered in the context of our study’s limitations. Further study on this issue is needed. For now, we recommend diabetic patients considering semaglutide treatment should consult their primary and eye care providers regarding their individual situation.”
The retrospective study extracted data from the American Academy of Ophthalmology’s Intelligent Research in Sight Registry (IRIS). The patients included had type 2 diabetes, were started on subcutaneous semaglutide between January 2013 and December 2021, and had a minimum follow-up of three months.
At baseline, 71.8% of eyes had no or background DR, 18.4% had mild or moderate non-proliferative DR (NPDR), and 9.8% had severe NPDR or proliferative DR. At the two-year time point after initiation of semaglutide, DR status worsened in 2.2% of eyes with no or background DR and in 3.5% of eyes with mild or moderate NPDR. DR status improved in 58.7% of eyes with severe NPDR or PDR at baseline.
Diabetic macular oedema was diagnosed in 0.35% of eyes at the two-year time point, and PDR developed in 0.97% of
eyes that did not have PDR at baseline. Rates for DR-related vision threatening complications at the two-year time point were 0.10% for vitreous haemorrhage, 0.02% for traction retinal detachment, and 0.04% for neovascular glaucoma.
Dr Haq told EuroTimes he and his co-authors plan to perform additional analyses to address potential confounding that was not controlled for in the research they presented. For example, the initial analyses did not consider the potential effects of any existing anti-VEGF treatment on DR status or any relationship to semaglutide dose.
The latter issue is important, considering that in the past few years, the US FDA approved the use of higher doses of subcutaneous semaglutide for treating chronic weight management in adults who are obese or overweight with a weight-related condition.
Dr Haq said results from the ongoing prospective, randomised placebo-controlled FOCUS study have the potential to provide information that is less susceptible to the biases associated with retrospective observational research. FOCUS is a five-year study investigating the long-term effects of semaglutide on DR in people with type 2 diabetes. Eligible patients have Early Treatment Diabetic Retinopathy Study scores ranging from no DR to PDR (levels 10 to 75), BCVA greater than or equal to 30 ETDRS letters, and no history of ocular or intraocular treatment for DR or diabetic macular oedema within six months of screening or anticipated need for such treatment within three months after randomisation.
33 2024 MARCH | EUROTIMES
Dr Haq and colleagues presented their research in a poster at AAO 2023 in San Francisco, US.
Zeeshan Haq MD is a retina specialist at Retina Consultants of Minnesota, Edina, Minnesota, US. zeeshan.haq7@gmail.com
New Subspecialty Could Improve Care
OncoVR subspecialists bring dual knowledge of vitreoretinal surgery and ocular oncology.
CHERYL GUTTMAN KRADER REPORTS
The diagnosis and treatment of intraocular tumours often require vitreoretinal surgery, and these procedures are best performed by an “OncoVR subspecialist”—a vitreoretinal surgeon with special expertise in ocular oncology, according to Bertil Damato MD, PhD.
“When vitreoretinal surgeons become part of the ocular oncology team, they understand the potential problems that can occur with different surgical approaches used for tumour diagnosis and treatment,” Professor Damato said. “And thanks to their understanding of oncology, OncoVR surgeons can develop novel techniques that lead to better outcomes for patients.”
Providing examples highlighting the benefits that OncoVR surgeons bring to patient care, Prof Damato said these subspecialists have the knowledge and experience to obtain larger tumour samples with a smaller biopsy, ensuring a sufficient specimen is available for diagnostic and prognostic testing while minimising risk for complications.
“When performing transretinal tumour biopsy that leaves a hole in the retina, some vitreoretinal surgeons are unhappy unless they turn the procedure into a big operation that includes total vitrectomy, endolaser retinopexy, and gas tamponade. I have been fortunate, however, to work with others who were persuaded to unlearn standard vitreoretinal principles and perform the biopsy without those procedures, knowing retinal detachment is very rare after transretinal tumour biopsy,” Prof Damato explained.
“Furthermore, risks of inadequate sample acquisition, post-biopsy haemorrhage, and tumour seeding are very rare if the operation is done by an OncoVR expert.”
He added obtaining a sufficient sample in cases of uveal melanoma is critical to allow genetic testing that provides prognostic information, which enhances patient counselling, allows screening for metastatic disease to be targeted at highrisk patients, and provides information on tumour biology, which helps with treatment decisions.
Impact of surgical expertise
Discussing the value OncoVR surgeons bring to therapeutic intervention for patients with intraocular tumours, Prof Damato said their knowledge and skills help safely perform endoresection to treat choroidal melanomas adjacent to the optic nerve, a procedure he developed to avoid radiotherapy and the inevitable radiation-induced optic neuropathy leading to severe visual loss.
Prof Damato also described the development of therapeutic vitrectomy, which he introduced with colleagues at the

University of California, San Francisco, as a technique that improves outcomes of systemic chemotherapy for vitreoretinal lymphoma with dense vitreal infiltrates.
In addition, he provided several examples illustrating how an OncoVR surgeon has the expertise to successfully perform complex salvage procedures unique to ocular oncology, such as treatment for residual or recurrent choroidal melanoma. He outlined how the expertise of an OncoVR surgeon enhances the prevention and management of complications and side effects resulting from other forms of eye-conserving treatment, such as rhegmatogenous retinal detachment after exoresection and toxic tumour syndrome after radiotherapy of choroidal melanoma.
Prof Damato spoke on this topic at the 2023 EURETINA Congress in Amsterdam.
Bertil Damato MD, PhD is a Consultant Ocular Oncologist at St Erik Eye Hospital, Stockholm, Sweden, and Moorfields Eye Hospital, London, UK. bertil.damato@gmail.com
RETINA 34 EUROTIMES | MARCH 2024

35 2023 MONTH | EUROTIMES YOUNG OPHTHALMOLOGISTS ESCRS
https://escrs.org/special-interest-groups/yos/

Defusing the Ticking Time Bomb of High Myopia
Every
dioptre matters when reducing high myopia risk.
DERMOT MCGRATH REPORTS
If current trends continue, one out of every two people on the planet will be myopic by 2050. Even more worryingly, a significant proportion of these will be highly myopic with all the associated problems in terms of ocular morbidity, disease, and vision loss, according to Andrzej Grzybowski MD, PhD.
High myopia is a key risk factor for conditions such as myopic macular degeneration, staphyloma, cataract, and glaucoma, among others.
The good news, however, is ophthalmologists and health authorities are not powerless in the fight to stem the tide of the coming epidemic, said Professor Grzybowski.
“It is important to highlight as a starting point that due to the environmental risk factors, myopia is partly preventable,” he said. “As doctors and retina experts, we should be the source of this knowledge in our societies—otherwise, the transfer of this knowledge to parents, schools, and the general public will be much longer.”
Prof Grzybowski said a range of treatments such as atropine, soft contact lenses with myopia control features, orthokeratology, and repeated low-level red light (RLRL) therapy are available and may be deployed in tandem with measures encouraging children to spend more time outdoors and limit near work.
“We do have methods, even if they are not perfect, to help control myopia. As retina specialists, we do not deal with the issue that often, but we should be aware and refer parents to the paediatric ophthalmologists who can provide the appropriate treatment,” he said. “I think we need to emphasise the message that every dioptre matters.”
Surveying the current methods available to control myopia in Europe, Prof Grzybowski said pharmacological approaches have focused largely on atropine in different concentrations while popular optical methods include orthokeratology, contact lenses and special eyeglasses such as Defocus Incorporated Multiple Segments (DIMS), and Highly Aspherical Lenslet Target (HALT) technologies.
We do have methods, even if they are not perfect, to help control myopia.
For atropine, the pivotal LAMP study clearly showed 0.05% atropine was more effective than lower concentrations such as 0.01% and 0.025%, Prof Grzybowski noted.1 Other studies have also confirmed the safety and effectiveness of atropine in controlling myopia in children—although one recent randomised trial of children in the United States found no difference in the outcomes achieved with nightly drops of 0.01% atropine compared to placebo.2
Other issues with atropine relate to the fact it has to be provided by a compounding pharmacy, which means the content of the compounded drops is not always very reliable.
“We know that it is effective in higher doses, but that is the point at which usually some side effects appear,” he said. “And despite years of research, the underlying mechanism
36 EUROTIMES | MARCH 2024
PAEDIATRIC OPHTHALMOLOGY

by which atropine halts or delays the progression of myopia is still not known.”
A recent review of 12 randomised controlled trials publications by Prof Grzybowski and co-workers concluded that low-dose atropine of 0.01% was not effective in reducing axial length progression in two studies, whereas 0.05% atropine showed good efficacy.3
“Spectacles (HAL and DIMS) and contact lenses (MiSight and Biofinity) may confer a comparable treatment benefit compared to atropine to slow myopia progression,” they concluded.
There is also increasing interest in combination treatments, said Prof Grzybowski, with a growing body of evidence in the scientific literature suggesting an additional benefit from combining atropine with orthokeratology or glasses to slow the progression of myopia.
One particularly promising treatment to emerge in recent years is RLRL therapy, which can be done at home for just three minutes twice a day, five days a week, using a special device.
The treatment achieved up to 87.7% myopia control efficacy in a randomised controlled trial with a high level of patient compliance and no observed side effects or adverse events. The effect was sustained over time, with 75% myopia control efficacy after two years and a sustained effect on myopia progression after withdrawal of the RLRL treatment.
Prof Grzybowski presented at the European Association for Vision and Eye Research (EVER) symposium session on high myopia at the EURETINA Congress in Amsterdam.
For citation notes, see page 46.
Andrzej Grzybowski MD, PhD is Professor of Ophthalmology, Head of the Institute for Research in Ophthalmology, Poznan, Poland, and President of the European Association for Vision and Eye Research. ae.grzybowski@gmail.com

GLOBAL REACH
As a renowned authority in the field of cataract and refractive surgery, ESCRS facilitates global connections amongst ophthalmic professionals, fostering collaboration and the exchange of knowledge.
Our events span across continents, providing a platform for pioneering research, advanced surgical techniques, and continuous professional development.
Using the interactive map on our website, we invite you to explore our global presence by viewing upcoming events and academies.
Join us to network with esteemed experts, access the latest advancements, and contribute to the enhancement of eye care on a worldwide scale.
escrs.org/meetings-and-events/global-reach/
37 2024 MARCH | EUROTIMES
Advancements for Paediatric Amblyopia
Digital dichoptic therapeutics offer new tools, but do not supplant conventional options.
CHERYL GUTTMAN KRADER REPORTS
Currently available digital dichoptic therapy platforms for paediatric amblyopia can be associated with better patient compliance than patching but will not completely replace conventional therapies such as spectacles, patching, or atropine penalisation, according to Courtney L Kraus MD.
High rates of residual amblyopia in children treated with patching or atropine penalisation raised interest in whether a dichoptic approach involving digitally presented binocular stimulation could be more effective. Despite two different dichoptic game-based approaches having poor compliance and disappointing results in Pediatric Eye Disease Investigator Group studies, investigation persisted, exploring alternative platforms using media children were already used to consuming to be more engaging and hold greater promise.
Positive results achieved in prospective controlled trials investigating two digital dichoptic therapeutics—Luminopia and CureSight (NovaSight)—led to their FDA approval. The latter system also has the CE mark.
Luminopia is a video-based technology in which the child watches media on a virtual reality (VR) headset. The goggles create dichoptic masking and contrast reduction to encourage the brain to synergise and use the two eyes together while strengthening the synaptic connections to the amblyopic eye.
The VR system used with continued glasses was compared with full-time glasses in a 12-week clinical trial that found mean VA improvement was significantly greater in the dichoptic group (1.8 versus 0.8 lines).1 Compliance with the VR device was 88%, and no serious safety issues emerged.
With CureSight, the child views videos on a tablet while wearing coloured eyeglasses that alter the image in the non-amblyopic eye by foveal blur. This system also uses eye tracking to determine where the non-amblyopic eye is foveating.
In a 16-week trial, CureSight was found to be non-inferior to patching for improving VA.2 The study groups had similar stereoacuity improvements and safety, but compliance was significantly higher in the dichoptic group compared to patching (91% versus 83%).
Caveats to consider
When asked about her treatment approach for paediatric amblyopia, Dr Kraus explained she is not about to fully replace patching with dichoptic digital therapy any time soon but has found an increasing number of children where it presents an attractive alternative. Neither dichoptic system is approved for use in children younger than four years, and the VR headset is not even feasible with very young children since proper

fitting requires the wearer to have an interpupillary distance of at least 52 mm.
Importantly, use of these systems must be balanced against concerns relating to digital media consumption by children. For example, the American Academy of Pediatrics recommends children aged two to five years be limited to no more than one hour per day of digital media use. In the clinical trials, they were used for 60 or 90 minutes a day, five or six days a week.
“How do we rationalise these treatments, especially considering children may still need to consume some sort of digital media for school or just relaxing?” Dr Kraus asked.
“Furthermore, I prescribe four to six hours a day of patching for some children. The equivalent amount of digital therapeutic time is not established, and I am not comfortable recommending more than one hour a day, especially in young children.”
Dr Kraus spoke at the 2023 AAO meeting in San Francisco, US.
For citation notes, see page 47.
38 EUROTIMES | MARCH 2024 PAEDIATRIC OPHTHALMOLOGY
Courtney L Kraus MD is Associate Professor of Ophthalmology, Wilmer Eye Institute, Johns Hopkins University, Baltimore, Maryland, US. Ckraus6@jhmi.edu
ESCRS Educational Forum is supported by multiple industry partners to provide independent didactic education on selected therapeutic areas. The platform combines presentations from ESCRS Winter and Annual Congresses, selected EuroTimes articles, videos, and webinars to provide an in-depth overview on current clinical outlooks.

Education Forum
escrs.org/education/forum/

Tackling Waste in Retinal Surgery
Intravitreal injections are one of the most common procedures in ophthalmology, but they come with significant environmental consequences in waste generation and carbon emissions. Although improved sustainability in retinal disease treatment is definitely achievable, it requires awareness and optimization of each clinic’s protocols and routines to make a tangible difference, according to Redmer van Leeuwen MD, PhD.
“To achieve waste reduction in intravitreal injections we need to apply the three ‘Rs’: rethink, reduce, and recycle,” he said. “First, we have to ask if this intravitreal injection is meaningful and necessary. The most sustainable injection is the one you can skip. To reduce, we have to ask if we really need all these disposables. Be critical and take on the challenge with the manufacturer and get them to reduce plastic packaging, which is thrown away every time. And finally, we need to recycle, as waste separation saves money and increases awareness.”
Dr van Leeuwen explained his own epiphany in sustainability came in 2019 when his clinic in Utrecht mandated a move from reusable equipment to single-use disposable packs. “Initially, it went smoothly without any major objections, but there was a huge amount of waste, and I refused to continue with that approach,” he said.
Part of the solution came from recycling paper and plastic packaging that came as part of the disposable surgical packs, while significant waste reduction came after selecting a new disposable pack with the manufacturer.
The upshot of these measures was a more than 50% reduction in total waste per injection, a 75% reduction in hospital waste and carbon footprint, and a 30% reduction in costs, Dr van Leeuwen said.
To try to extend the benefits of such an approach to other hospitals and clinics in the Netherlands, Dr van Leeuwen and Sjoerd Elferink founded the Dutch Working Group on Sustainable Ophthalmology and published best practice guidelines on administering intravitreal injections in a safe and sustainable way.
“Based on the guidelines of EURETINA and the American Academy of Ophthalmology, we made a list of evidence-based protocol for intravitreal injections, which has now been adopted as standard practice by the Dutch Ophthalmic Society,” he said.
The list divides surgical equipment into three categories: essential, optional, and superfluous. Essential equipment includes face masks, gloves, anaesthetic eye drops, povidone iodine drops, and sterile eyelid speculum; optional equipment includes marker/calliper, cotton buds for applying iodine, and non-sterile gauze and non-sterile fluid for removing iodine and eye ointment; superfluous equipment includes drape, cotton swap for anaesthesia and massage, forceps, cap, jacket, tablecloth, and antibiotics pre- and post-injection.
Beyond intravitreal injections, other concrete measures can help reduce the environmental impact of retinal surgery, said Francesc March de Ribot MD, PhD.
“We don’t have to try to reinvent the wheel,” he said. “There are small steps we can take immediately, following some of the guidance available to make our surgeries more sustainable, economic, and environmental.”
One such measure is to stop continuous operating theatre ventilation and only enable it 30 minutes before surgery, which can generate up to €2,000 a year in electricity savings.
40 EUROTIMES | MARCH 2024
Reducing waste from intravitreal injections is an achievable goal.
SUSTAINABILITY
DERMOT MCGRATH REPORTS

Another simple measure is to save water by using alcohol solutions instead of sponges for hand disinfection.
“This can save up to 50 litres of water per surgery, which is a major impact,” he said. “And this does not increase the risk of infections, as alcohol hand rub provides superior disinfection for a longer duration.”
Reducing topical drug waste is another simple measure that can make a real impact on sustainability, added Dr March de Ribot. “Studies have shown that preoperative drugs in multidose containers are safe to use on multiple patients if proper guidelines are followed and patients requiring a topical medication not used for other patients should be allowed to bring that partially used medication home for postoperative use,” he said.
Using a lighter, perhaps reusable face drape instead of a full body drape should also be considered, as 20% of the waste during eye surgery is due to the plastic face drape, Dr March de Ribot added.
“Bigger drapes are not safer but create more anxiety for the patient,” he noted. “Face drapes allow better ventilation, less hypercapnia, gas consumption, and claustrophobia and are more comfortable for the patient.”
Taking such small measures to save electricity, water, and medications and reduce waste can translate into significant savings annually for every clinic or hospital, Dr March de Ribot concluded.
This article is based on presentations given at the EURETINA Congress in Amsterdam.

Redmer van Leeuwen MD, PhD is an ophthalmologist and vitreoretinal surgeon at University Medical Center Utrecht, Netherlands. r.vanLeeuwen@umcutrecht.nl
Francesc March de Ribot MD, PhD is an ophthalmologist at the University Hospital of Girona, Italy. march.professor@gmail.com
To be the leading community and trusted source for science, education, and professional development in the fields of cataract and refractive surgery.
41 2024 MARCH | EUROTIMES
Learn more at ESCRS.org
New monofocal-plus IOL from Ophtec
Ophtec has launched its new “monofocal plus” Precizon Go intraocular lens. The new non-diffractive lens has a modified aspheric anterior surface designed to provide distance and enhanced intermediate vision without inducing dysphotopsias such as glare or halos. Precizon Go received CE marking in September 2023. The company said the lens is now available in the EU, South Africa, and South Korea, with more countries set for introduction in H1-2024.
www.ophtec.com
Travoprost insert approved
The US FDA had approved the new drug application from Glaukos for iDose TR (travoprost intracameral implant) 75 mcg, indicated for the reduction of intraocular pressure in patients with ocular hypertension or open-angle glaucoma. The 1.8 mm titanium implant has a nanoporous, ethylene-vinyl acetate membrane that allows continuous elution of preservative-free travoprost directly into the anterior chamber. It is implanted through the trabecular meshwork and back wall of Schlemm’s canal, anchored directly into scleral tissue. In two phase III clinical trials, 81% of patients receiving the implant maintained target IOP levels at 12 months. Glaukos designed iDose TR to be removed and replaced, but the FDA only granted approval for a single administration per eye. The company says it will soon meet with the FDA to explore expansion of the implant’s use to include repeat administration.
www.glaukos.com
FDA grants clearance to new laser for selective laser trabeculoplasty
Belkin Vision reported the US FDA 510(k) application gained clearance for its Eagle laser for performing a new automated, noncontact, one-second procedure called direct selective laser trabeculoplasty (DSLT) in the treatment of primary open-angle glaucoma. The company says the Q-switched, 532 nm-wavelength, frequency-doubled Nd:YAG laser allows delivery of laser energy directly through the limbus to the trabecular meshwork, automatically defines the target location, and applies the laser treatment sequence and has an eye tracker to compensates for eye movement. Therefore, it does not require gonioscopy lens use. The company says the laser’s ease of use may enable a larger number of eye care professionals to perform the procedure.
www.belkin-vision.com
New anti-VEGF implant meets primary and secondary endpoints
EyePoint Pharmaceuticals reports its new sustained-release anti-VEGF implant candidate, EYP-1901, has met its primary endpoint and all secondary endpoints in the Phase II DAVIO 2 trial of neovascular age-related macular degeneration (AMD) treatment. At both 2 mg and 3 mg doses, EYP-1901 demonstrated statistical non-inferiority change in best corrected visual acuity (BCVA) compared with the aflibercept control, with a favourable safety profile and no EYP-1901-related ocular or systemic serious adverse events. EYP-1901 combines vorolanib, a selective tyrosine kinase inhibitor, with EyePoint’s bioerodible Durasert E technology. Vorolanib blocks all VEGF isoforms but does not inhibit Tie-2, associated with vascular stability. EyePoint says it has plans for a pivotal trial of EYP-1901 for neovascular AMD later in 2024.
www.eyepointpharma.com
42 INDUSTRY NEWS EUROTIMES | MARCH 2024

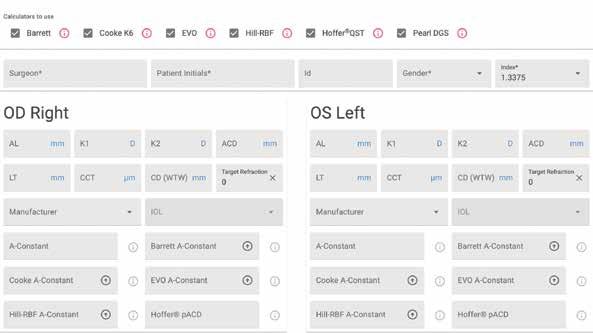

This first-of-its-kind web application for IOL power calculations uses multiple modern formulas simultaneously, and suggests lens constants for a wide range of IOL models .
IOL Calculator is now live on the ESCRS website!
Find out more
Our
at iolcalculator.escrs .org/
Research Education Innovation

ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

PILOCARPINE DROPS IMPROVE NEAR VISION
A pooled analysis of the GEMINI 1 and 2 phase 3 randomised trial results indicates topical treatment with pilocarpine HCl 1.25% provides presbyopes with similar improvements in near visual acuity, whether or not they have a history of laser vision correction. The studies showed that, in 39 patients with previous LASIK or PRK, the proportion gaining three or more lines of distance corrected near visual acuity (DCNVA) at 30 days of treatment was 16.7% at 15 minutes and 41.7% at one hour, gradually falling to 8.3% by 10 hours. Among 336 non-LASIK/PRK participants, the proportion gaining three or more lines of DCNVA was 16.8% at 15 minutes, 39% at one hour, and 10.5% at 10 hours. C Lievens, et al. “Pilocarpine HCl 1.25% for treatment of presbyopia after laser vision correction: pooled analysis of two phase 3 randomized trials (GEMINI 1 and 2),” 50: 57–63.
ELECTRONIC INSTRUCTION FOR USE BROCHURES REDUCE CARBON FOOTPRINT
If all intraocular lens (IOL) manufacturers transitioned from paper instruction for use brochures (IFUs) to electronic IFUs, the amount of paper used annually in cataract surgery could be reduced by 128 tonnes, with a 120-tonne reduction in carbon dioxide emissions and the preservation of more than 2,000 trees, according to the findings of an experimental study. The authors weighed a selection of IOL IFUs to determine an average to compare to the electronic IFUs. They based their estimate of the paper IFUs’ current cumulative weight on the number of cataract surgeries performed annually in Europe and the US (8.7 million) and their estimate of the potential environmental benefits of universal electronic IFU use on shorter paper documents, which include a link or QR code for access on the internet.
B Stern, et al. “Paper waste from instructions for use brochures in cataract surgery implant packaging in Europe and the United States,” 50: 72–77.
MORE EQUITABLE DEMOGRAPHIC ENROLMENT NEEDED
High-quality, US-registered cataract trials enrol acceptable proportions of female participants, yet they underreport race and ethnicity, according to the findings of a cross-sectional database study. From 864 cataract-related studies, the analysis identified 100 completed randomised clinical trials, registered on clinicaltrials.gov, that employed double or greater masking and had results published through the registry or in a scholarly journal. Of those trials, 97 reported sex demographics. Using the Global Burden of Disease database as the reference for the sex-based cataract prevalence, the study’s authors calculated the pooled participation-to-prevalence ratios for female sex in the trials—arriving at a value of 0.89, which lies within values constituting sufficient study enrolment. However, the absolute female enrolment was only 28.16%. In addition, only nine trials reported ethnicity and only 26 reported race. Among participants in trials that reported race, 84.44% were Caucasian.
B Ka-Lok Tao. “Diversity in Enrollment to Clinical Trials for Cataract Medicine and Surgery: A Meta-Analysis,” DOI: 10.1097/j. jcrs.0000000000001395.

45 JCRS HIGHLIGHTS
Learn more about membership at escrs.org Sign up as an ESCRS member now
€150 per year and save €100 on your 2023 Annual Congress registration fee!
JOIN the leading community and trusted source for SCIENCE, EDUCATION, AND PROFESSIONAL DEVELOPMENT in the fields of cataract and refractive surgery.
for
2024 MARCH | EUROTIMES
Cited in this Issue
Library of Short Videos Complements Educational Offerings
Page 6
1. Slemmons K, Anyanwu K, Hames J, et al. 2018. “The Impact of Video Length on Learning in a Middle-Level Flipped Science Setting: Implications for Diversity Inclusion,” Journal of Science Education and Technology, 27(5): 469–479. https://doi. org/10.1007/s10956-018-9736-2
Ophthalmic Imaging Gets Robotic Enhancement
Page 12
1. McNabb R, Ortiz P, Roh KM, et al. “Contactless, autonomous robotic alignment of optical coherence tomography for in vivo evaluation of diseased retinas,” Res Sq [Preprint]. 2023 Jan 9:rs.3.rs-2371365.
2. Draelos M, Ortiz P, Qian R, Viehland C, McNabb R, Hauser K, Kuo AN, Izatt JA. “Contactless optical coherence tomography of the eyes of freestanding individuals with a robotic scanner,” Nat Biomed Eng. 2021 Jul; 5(7): 726–736. doi: 10.1038/ s41551-021-00753-6. Epub 2021 Jul 12. PMID: 34253888; PMCID: PMC9272353.
3. Song A, Roh KM, Lusk JB, Valikodath NG, Lad EM, Draelos M, Ortiz P, Theophanous RG, Limkakeng AT, Izatt JA, McNabb RP, Kuo AN. “Robotic Optical Coherence Tomography
Retinal Imaging for Emergency Department Patients: A Pilot Study for Emergency Physicians’ Diagnostic Performance,” Ann Emerg Med. 2023 Apr; 81(4): 501–508. doi: 10.1016/j. annemergmed.2022.10.016. Epub 2023 Jan 18. PMID: 36669908; PMCID: PMC10038849.
Laser Refractive Surgery for High Myopia
Page 14
1. Liu M, Chen Y, Wang D, et al. “Clinical Outcomes After SMILE and Femtosecond Laser-Assisted LASIK for Myopia and Myopic Astigmatism,” Cornea, 2016; 35(2): 210–216.
2. Chiang B, Valerio GS, Manche EE. “Prospective, Randomized Contralateral Eye Comparison of Wavefront-Guided Laser In Situ Keratomileusis and Small Incision Lenticule Extraction Refractive Surgeries,” Am J Ophthalmol. 2022; 237: 211–220.
3. ClinicalTrials.gov. Identifier: NCT05611294. Personal communication: Majid Moshirfar MD.
AI Applications in Diagnostic Imaging
Page 16
1. Goetz KE, Reed AA, Chiang MF, et al. “Accelerating Care: A Roadmap to Interoperable Ophthalmic Imaging Standards in the United States,” Ophthalmology. 2023 Nov 6:S0161-6420(23)00713-
3. doi: 10.1016/j.ophtha.2023.10.001. Epub ahead of print.
The Future of FLACS
Page 17
1. Schweitzer C, Brezin A, Cochener B, et al; FEMCAT study group. “Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked
randomised superiority and cost-effectiveness trial,” Lancet 2020; 395(10219): 212–224.
2. Day AC, Burr JM, Bennett K, et al; FACT group. “Femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery (FACT): a randomized noninferiority trial,” Ophthalmology. 2020; 127(8): 1012–1019.
3. Roberts HW, Wagh VK, Sullivan DL, et al. “A randomized controlled trial comparing femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery,” J Cataract Refract Surg. 2019; 45(1): 11–20.
4. Narayan A, Evans JR, O’Brart D, et al. “Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery,” Cochrane Database Syst Rev. 2023; 6(6): CD010735.
5. Findl O, Hirnschall N, Draschl P, Wiesinger J. “Effect of manual capsulorhexis size and position on intraocular lens tilt, centration, and axial position,” J Cataract Refract Surg. 2017; 43(7): 902–908C.
Advances in Toric IOL Alignment
Page 20
1. Schultz T, Hoffmann S, Dick HB. “Comparison of toric intraocular lens alignment between femtosecond laser-assisted capsular marking and digital marking,” J Cataract Refract Surg. 2023; Oct 17. Epub ahead of print.
Improving Preoperative Prediction of PCR
Page 24
1. Triepels RJMA, Segers MHM, Rosen P, et al. “Development of machine learning models to predict posterior capsule rupture based on the EUREQUO registry,” Acta Ophthalmol. 2023; 101(6): 644–650.
Monofocal Plus Finding the Balance
Page 26
1. Ribeiro F, Ferreira TB, Silva D, Matos AC, Gaspar S, Piñero DP. “Analysis of Daily Visual Habits in a Presbyopic Population,” J Ophthalmol. 2023 Apr 8; 2023:6440954. doi: 10.1155/2023/6440954. PMID: 37089413; PMCID: PMC10118895.
Optogenetic Therapy for Stargardt Disease
Page 32
1. Boyer et al., “Efficacy and safety of MCO-010 optogenetic therapy for vision restoration in patients with severe vision loss due to retinitis pigmentosa: a phase 2b randomized, sham-controlled, multi-center, multi-dose, double-masked clinical trial (RESTORE),” IOVS, June 2023, 64(8).
Defusing the Ticking Time Bomb of High Myopia
Page 36
1. Yam, et al. Ophthalmology, 2019 Jan; 126(1): 113–124.
2. Repka MX, et al. JAMA Ophthalmol. 2023 Aug 1; 141(8): 756–765.
3. Grzybowski, et al. Front Public Health. 2023; 11: 1125000.
46 CITATION INDEX
EUROTIMES | MARCH 2024
Advancements for Paediatric Amblyopia
Page 38
1. Xiao S, Angjeli E, Wu HC, et al; Luminopia Pivotal Trial Group. “Randomized Controlled Trial of a Dichoptic Digital Therapeutic for Amblyopia,” Ophthalmology. 2022 Jan; 129(1): 77–85. Erratum in: Ophthalmology. 2022; 129(5): 593.
2. Wygnanski-Jaffe T, Kushner BJ, Moshkovitz A, Belkin M, Yehezkel O; CureSight Pivotal Trial Group. “An Eye-Tracking-Based Dichoptic Home Treatment for Amblyopia: A Multicenter Randomized Clinical Trial,” Ophthalmology. 2023; 130(3): 274–285.
ESCRS Academies
Committee representatives of ESCRS organise and present sessions at those meeting organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies memberships.
47 2024 MARCH | EUROTIMES
escrs.org/education/academies/
ESCRS IN A SNAPSHOT
We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With more than 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.
Upcoming Events
April 5–8
2024 ASCRS Annual Meeting
Boston, United States
May 5–9
2024 ARVO Annual Meeting
Seattle, United States
May 24–26
2024 EuCornea Annual Congress
Paris, France
June 1–4
2024 European Glaucoma Society Congress Dublin, Ireland
September 6–10
2024 ESCRS Congress
Barcelona, Spain

April 5
May


Sep
24
6 49 2024 MARCH | EUROTIMES
INTERVENE EARLIER WITH ISTENT INJECT® W
DELAYING GLAUCOMA DISEASE PROGRESSION1-8
40 %
IOP REDUCTION AFTER 5 YEARS FOLLOW-UP 2
81
DECIBEL MEAN CHANGE IN VISUAL FIELD MEAN DEVIATION FROM BASELINE AT 24 MONTHS IN ISTENT INJECT-TREATED EYES IN A PIVOTAL TRIAL 8
0 ,01 8
YEAR STUDY WITH 2 ISTENTS DEMONSTRATED SUSTAINED PROTECTION AGAINST VISUAL FIELD LOSS, AS WELL AS PRESERVATION OF BEST CORRECTED VISUAL ACUITY, CUP TO DISC RATIO AND RETINAL NERVE FIBER LAYER THICKNESS 5
16 WITH 4-8 YEARS FOLLOW-UP
STUDIES
2,6 %
POWERFUL PREDICTABLE PROVEN
OF 778 PATIENTS IN A META-ANALYSIS OF STANDALONE ISTENT INJECT EYES REQUIRED SECONDARY
INCISIONAL SURGERY DURING FOLLOW-UP6

+40
PUBLICATIONS DEMONSTRATE ISTENT TECHNOLOGIES PROTECT AGAINST VISUAL FIELD LOSS†
4 %
OF 125 PATIENTS IN REAL WORLD STUDY OF STANDALONE AND COMBINED
1%
OF 186 EYES IN A RANDOMISED CONTROLLED TRIAL WENT ON TO REQUIRE SECONDARY INCISIONAL SURGERY DURING 3 YEARS FOLLOW-UP 7
ISTENT INJECT CASES REQUIRED A SECONDARY PROCEDURE DURING 5 YEARS OF FOLLOW-UP 2
2-7
† Data on file. 1. Berdahl, J., Voskanyan, L., Myers, J. S., Katz, L. J., & Samuelson, T. W. (2020). iStent inject trabecular micro-bypass stents with topical prostaglandin as standalone treatment for open-angle glaucoma: 4-year outcomes. Clinical & Experimental Ophthalmology, 48(6), 767-774. 2. Hengerer, Fritz H., Gerd U. Auffarth, and Ina Conrad-Hengerer. “iStent inject Trabecular Micro-Bypass with or Without Cataract Surgery Yields Sustained 5-Year Glaucoma Control.” Advances in Therapy (2022): 1-15. 3. Ferguson, Tanner J., et al. “iStent trabecular micro-bypass stent implantation with phacoemulsification in patients with open-angle glaucoma: 6-year outcomes.” Clinical Ophthalmology (Auckland, NZ) 14 (2020): 1859. 4. Ziaei, Hadi, and Leon Au. “Manchester iStent study: long-term 7-year outcomes.” Eye 35.8 (2021): 2277- 2282. 5. Salimi, Ali, Harrison Watt, and Paul Harasymowycz. “Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results.” Eye and Vision 8.1 (2021): 1-12. *Consistent cohort. 6. Healey, Paul R., et al. "Standalone iStent trabecular micro-bypass glaucoma surgery: A systematic review and meta-analysis." Journal of Glaucoma 30.7 (2021): 606-620. 7. Samuelson TW, on behalf of the iStent inject Pivotal Trial Study Team. Three-Year Effectiveness and Safety of 2nd-Generation Trabecular Micro-Bypass (iStent inject). Paper at the Annual Meeting of the American Academy of Ophthalmology (AAO). Virtual Meeting: November 13-15 2020. 8. Samuelson, Thomas W., et al. "Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results." Ophthalmology 126.6 (2019): 811-821. iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject ® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject ® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject ® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject ® W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject ® W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.”
• There are no known compatibility issues with the iStent inject ® W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of
intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. © 2023 Glaukos Corporation. Glaukos, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation PM-EU-0237
RATE OF SSIs
C O NTROLLINGIOP1-5 PROTECTINGAGAINST V F L SSO 48
LOW
OF PATIENTS
FOLLOW-UP
%
BELOW 15MMHG AFTER 5 YEARS
2