Nemours






Children with complex conditions that affect the esophagus, stomach, intestines, pancreas, liver, biliary tract, colon, or rectum do better with a team of pediatric sur geons who partner in care. To mark the next evolution in care, The Nemours Children’s Digestive Disorders and Gastrointestinal Surgery Center brings together pediatric colorectal surgeons, gastroenterologists and urologists with expertise in the full range of conditions.

Our team of nationally recognized physicians and surgeons are experts in all aspects of GI disorders. The center was created to deliver convenient, coordinated access to experts in gastroenterology, pediatric surgery, nutrition and social work- all in one loca tion. The goal? To provide the best options closer to home in Central Florida and the Southeast region to better serve patients and families. This center allows us to serve yet another segment of the patient population in Florida.

pleased to bring you another issue of Florida MD. I can only imagine the emotional and physical trauma that a woman goes through when she has a mastectomy. The procedure affects not only her body, but her mind and her self-esteem. Now add in the inability to not be able to reconstruct her breasts and give that part of her life back, because she’s uninsured or under insured, and it becomes an unthinkable crushing blow. Fortunately there is My Hope Chest to help women who are unable to afford reconstructive surgery. I asked them to tell us about their organization and how you, as physicians, can help. Please join me in supporting this truly wonderful organization.
Best regards,
Donald B. Rauhofer Publisher

In 2010, more than 22,000 uninsured women lost their breasts to cancer and were left disfigured, deformed and feeling “less than whole.” How many years has this figure been growing?
Many organizations raise funds for research, education and “awareness” of breast cancer. Most have no idea there lies a huge gap in assistance for delayed reconstruction and co-pays for survivors wanting this surgery.
My Hope Chest is the ONLY national 501c3 non-profit organization focused on funding breast reconstruction for the uninsured and under insured survivors. Our services “pick up” where other breast cancer organizations leave off… providing the “final step in breast cancer treatment. ”

My Hope Chest is about addressing the needs of survivors now. Through wonderful surgeon partnerships we are able to transform the lives of breast cancer survivors who otherwise have no hope of reconstruction. We hope to hear from you to learn how we can work together to eliminate our wait list and take action to help every woman who desires reconstruction after mastectomy and feel restored in body, mind and spirit.
• Surgeons to create awareness for My Hope Chest and to identify new clients
• Doctors of Distinction- Surgeon partners nationwide to join our program.
• Corporate partners, interested in Win-Win, Commercial- coventure marketing campaigns promoting their product or service by sharing our vision to make sure there is always coverage for reconstruction surgery.
For additional information on how you can help or refer a patient please go to www.MyHopeChest.org.
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: John “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, Julie A. Tyk, JD, Benjamin K. Rhee, MD, George J. Haidukewych, MD, Naina Mehta, MD, Sonda Eunus, MHA, Michael Patterson NHA, OTR/L, CEAS, John Meisenheimer, VII

Art Director/Designer: Ana Espinosa
Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762.
Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2022, Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.
Ten years on and we’re turning the tide for children.
Since opening one decade ago, Nemours Children’s Hospital, Florida has been part of a sea change in children’s health. Bringing unique programs to millions of central Florida families, providing innovative care to our region’s most medically challenged children, and ensuring a pipeline of pediatric providers across the state. While we celebrate how far we’ve come, it’s not even close to how far we’ll go to ensure every child’s world is a place for them to thrive.

The ripple effects of better health.
 By Staff Writer
By Staff Writer
Nemours Children’s Hospital, Florida celebrates its 10th anni versary this October after opening its doors in Lake Nona Medi cal City 2012 with a focus on sophisticated medical treatment, research and education in Central Florida.
From the beginning, we have cared for children and adoles cents in pediatric gastroenterology (GI) and pediatric surgery. To mark the next evolution in care for children and teens, we are thrilled to introduce the Nemours Children’s Digestive Disorders and Gastrointestinal Surgery Center.
The GI Surgery Center is a team of nationally recognized physicians and surgeons who are experts in all aspects of GI disor ders. Our GI and surgery teams have come together to provide comprehensive, multidisciplinary care using the most up-to-date and innovative diagnostic and therapeutic approaches for kids.
The GI Center has created a care model designed to deliver convenient, coordinated access to experts in gastroenterology, pediatric surgery, nutrition and social work — all in one loca tion.
The goal is to provide the best options closer to home in Cen tral Florida and the Southeast region to better serve patients and families, including those who travel to Florida for care.
And, as part of Nemours Children’s Health, the GI Surgery Center draws on the integrated resources of one of the country’s largest pediatric health care systems, which has cared for children and adolescents for more than 80 years.
We continue to grow our team of expert providers to improve access for patients. This growth effort, combined with a full complement of highly skilled support staff, permits us to expand the subspecialties offerings in pediatric GI and GI surgery.
We have sought after and recruited specially trained physicians that give us the opportunity to improve our GI Center’s capa bilities in conditions like Hirschsprung disease, anorectal mal formations, inflammatory bowel diseases, complex esophagealaerodigestive conditions, and a variety of other areas that were underrepresented. This allows us to serve yet another segment of the patient population in Florida.
We offer a wide range of care for patients with anorectal mal formations and other issues such as Hirschsprung disease. The GI Surgery Center experts work with parents and experts early (including colleagues in our Center for Fetal Care and many other referring community physicians) to provide initial diagno sis, prenatal support and delivery, surgical consultations, treat ment and procedures, recovery care, and lifelong support.
Many of these children require expertise in diagnosis and sur gical management as early as possible, and it’s critical that they continue with lifelong follow-ups to monitor for disease compli cations and focus on the best quality of life for patients
The GI Surgery Center provides care for chil dren with inflammatory bowel disease (IBD), including children with Crohn’s disease and ul cerative colitis. Our team consists of IBD and childcare specialists, each with a unique role in making treatment as easy as possible for young patients and their families. Our team offers the full spectrum of services, including:
• personalized nutrition counseling
• careful monitoring of growth and development
• age-appropriate psychological and social sup port
• preparation and education for college, travel and work
complete transitional care services for young adults


Our team also specializes in the diagnosis and management of hereditary polyposis disorders and GI cancer syndromes. This requires a multidisciplinary team of specialists managing the sur veillance, treatment and counseling of patients to help reduce cancer risk and improve quality of life. Our team can provide regular, advanced endoscopic surveillance and colorectal surgery of the digestive tract as part of the ongoing care plan. Esophageal, Aerodigestive Disorders and Feeding
The GI team offers unsedated transnasal esophagoscopy (TNE) that eliminates the need for an IV or anesthesia. Transnasal esophago gastroduodenoscopy (TNEGD) will be coming soon to Orlando.

Our pediatric GI team offers expert diagnosis and treatment for a full spectrum of digestive issues from minor problems to complex, chronic conditions. The team works with families and other Nemours Children’s specialists to develop a personalized care plan that best suits the needs of each individual patient.
We utilize an approach to the whole child that provides the most effective support for children to thrive and overcome con ditions that can impact their entire lives.
When GI procedures are needed, we can offer innovative en doscopy and advanced testing.
We offer comprehensive care for children with complex aerodi gestive disorders including complex airway surgery. The GI Surgery Center team helps to evaluate, diagnose, and treat con ditions, then work with patients to develop care plans which ad dress a wide variety of complex airway conditions that impact a developing child’s ability to swallow, speak and breathe. We are also the only pediatric program in the Southeastern United States to offer unsedated transnasal esophagoscopy with biopsies (TNE; Unsedated Transnasal Endoscopy. The TNE procedure involves no IV needle, no sedation and is approximately 60% lower cost to families.
We offer highly skilled general surgeons who are experienced in performing advanced surgical treatments to care for GI patients, including mini mally invasive and robotic surgery.

Outcomes with robotic surgery are comparable and often better than with open surgical procedures, related to greater precision and visualization when compared to open sur gery — and greater than open surgery with respect to parent satisfaction re garding cosmesis and re covery. The robotic arm’s movements have a greater range of motion and can rotate 370 degrees. The ro botic camera provides for magnified, high-definition
A surgical console provides precise movements and enhanced magnifi cation of the surgical area.
visualization of the surgical area and has three-dimensional ca pabilities that are superior to the human eye.

We have the advantage of working together with the largest pediatric radiology group in the country at Nemours Children’s. This allows us to have access to the most advanced imaging mo dalities for our patients, including 3-D modeling. Our radiolo gists can use MRI imaging to print a 3-D model of the pathol ogy and surrounding structures and provide us with a model of what to expect intra-operatively.
We also have access to a virtual reality module that allows us to visualize the patient’s pathology and virtually “practice” the opera tion until we are confident of our approach. This collaboration with radiology, as well as other colleagues in our institution, allow us to provide the best outcomes, even for our tiniest patients.

The GI Center works closely with the pathology and labora tory medicine specialists at Nemours Children’s. The team’s three pathologists are board-certified in anatomic, clinical, and pedi atric pathology and have extensive experience in pediatric pa thology, including pediatric gastrointestinal diseases, hepatology, oncology and neuropathology. They have also published and presented research at national and international medical confer ences covering IBD, Hirschsprung disease, cholestatic liver dis ease, and non-alcohol fatty liver disease in children.
Our pathologists work closely with the GI Center team, and, to ensure clinical pathological correlation, present interesting
and challenging cases at our weekly GI conferences. Also, our clinical laboratory performs clinical testing 24/7 to ensure rapid, accurate testing results. It supports testing in three major areas that include hematology, clinical chemistry and microbiology.
Our involvement in academics and research has dramatically changed over the years We have significantly expanded our re search programs allowing our more faculty to be actively involved in research and publications. Our physicians have hundreds of peer-reviewed publications, national expert presentations, and millions of dollars in external research funding. Our team also offers clinical trials for leading-edge, innovative therapies and we have also grown the research infrastructure that supports the work.
We have always seen the benefit of partnering with our col leagues to determine how to build upon our services. Our team works with several hospitals and other types of organizations to help strengthen our presence in local communities.
It is our intent to work closely with our referring physicians to provide the best services possible. We look forward to being trusted collaborators to ensure the best possible outcomes for their patients and families.

A recent study published in the JAMA NETWORK asked the age-old question; Is there an Association between Marijuana Ex posure and Pulmonary Function over 20 years? The study can be found via the link below:
Association Between Marijuana Exposure and Pulmonary Function Over 20 Years | Adolescent Medicine | JAMA | JAMA Network

What they discovered was that “occasional and low cumulative marijuana use was NOT adverse effects on pulmonary function”. In other words, cannabis smoke – unlike tobacco smoke – doesn’t have such a drastic impact on lung function despite having some of the same chemical profile in smoke.
The study performed was called CARDIA, which is a longi tudinal study designed to measure risk factors for coronary ar tery disease in a cohort of black and white women and men (n = 5115) aged 18 through 30 years and healthy at enrollment in 1985. Participants were sampled from 4 US communities with out selection for smoking behaviors and comprise a broad crosssection of typical tobacco and marijuana use patterns.
Each study center (Oakland, Chicago, Minneapolis, and Bir mingham), participants underwent a baseline examination and 6 follow-up examinations, with 69% retention at year 20. Pul monary function testing was performed at years 0, 2, 5, 10, and 20. For this investigation, we included all visits for which pulmo nary function, smoking behavior, secondhand smoke exposure, height, and waist circumference were available.
Current intensity of tobacco use (cigarettes smoked per day) was assessed at each examination. These data, along with baseline examination data on past years of smoking, were used to estimate cumulative lifetime exposure to cigarettes in terms of pack-years, with 1 pack-year of exposure equivalent to 7300 cigarettes (1 year × 365 days/y × 1 pack/d × 20 cigarettes/pack). Misclassification of smoking exposure by self-report, measured by comparisons with serum cotinine levels, is uncommon.
Current intensity of marijuana use (episodes in the last 30 days) was also assessed at each examination. Using baseline examination data on past lifetime exposure to marijuana, current intensity of marijuana use, and another question designed to assess number of joints or filled pipe bowls smoked per episode we calculated total lifetime exposure to marijuana joints in joint-years, with 1 joint-year of exposure equivalent to 365 joints or filled pipe bowls smoked (1 year × 365 days/y × 1 joint/d), as described previously.
The 5115 CARDIA participants recruited in 1985-1986 con tributed 20 777 total visits that included pulmonary function testing. Of these, 959 visits were excluded for lack of complete information on smoking behavior, 114 for lack of height or waist measurements, and 1 for an unknown visit date, leaving 19 703 visits (95%) with complete data from 5016 participants (98%). Participants contributed 3.9 visits/participant on average; attri tion was more common in tobacco smokers but not associated with marijuana use. FEV and FVC varied across participants, in creased slightly with age through the late 20s, and declined slowly thereafter.
More than half of participants (54%; mean age at baseline, 25 years) reported cur rent marijuana smoking, tobacco smoking, or both at 1 or more examinations. Smok ing patterns differed by race and sex, with black women most likely to smoke tobacco only, white men most likely to smoke marijuana only, and black men most likely to smoke both. Tobacco smokers tended to have lower education and income and to be slightly shorter and less ac tive, whereas marijuana smokers tended to be taller and more ac tive. The median intensity of tobacco use in tobacco smokers was substantially higher (8-9 cigarettes/d) than the median intensity of marijuana use in marijuana smokers (2-3 episodes in the last 30 days). Although marijuana and tobacco exposures were strongly correlated, our sample included 91 participants with no tobacco exposure and more than 10 joint-years of marijuana exposure (contributing 153 observations of pulmonary function), 40 (56 observations) of whom had more than 20 joint-years of exposure.
The findings suggest that occasional use of marijuana for these or other purposes may not be associated with adverse consequences on pulmonary function. It is more difficult to estimate the potential effects of regular heavy use, because this pattern of use is relatively rare in our study sample; however, our find ings do suggest an accelerated decline in pulmonary function with heavy use and a resulting need for caution and moderation when marijuana use is considered.
While this study is good news, smoking cannabis for medical purposes is not the most efficient way to consume medicine. A lot of cannabinoid effects are lost when cannabis is burned to be smoked. A similar, but better way to consume cannabis is via vaporizer or vape pen. The cannabis not being burned but heated into a vapor, which maintains all of the cannabinoids in order to be available for absorption into the body. Furthermore, more accurate dosing of cannabis can be found via edibles or tinctures, which allow a patient to have a measured amount of cannabinoids (THC, CBD, THCA, CBG, CBN, etc.) to build confidence and certainty in the reaction of cannabis medicine on the body.
Michael Patterson NHA, OTR/L, CEAS is CEO of US Cannabis Pharmaceutical Research and Development LLC. (uscprd.com). He is a healthcare executive with 25+ years experience in: Cannabis-Hemp investment, Law, Regula tion, Compliance, Operations, & Management, Skilled Nursing, Pharmacy, Laboratory, Assisted Living, Home Healthcare, & Healthcare Analytics. He is a subject matter expert in the Global Cannabis and Hemp Industry with Gerson Lehrman Group (glg.it) & Guidepoint. He is an editorial board member of the American Journal of Medi cal Cannabis, licensed Nursing Home Administrator, & li censed Occupational Therapist in 4 states.

 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
When you mention skin cancer to the general public or even to the medical community, most folks think of the three big celebrities: basal cell carcinoma, squamous cell carcinoma, and melanoma. I like to refer to having occurrences of all three types of skin cancer in one patient as hitting the trifecta of skin cancer; unfortunately, there is no big payout with this trifecta. Excessive sun exposure is typically the common denominator. What is less known is there are other cancers of the skin besides the big three, and these can kill you as well. What I like to call “the fourth skin cancer” is the Merkel Cell Carcinoma. Not as famous as the big three, but Merkel cell carcinoma still should be treated with respect when it makes it rare appearances.

Merkel Cell carcinoma, like other skin cancers, has a predisposition for appearance in sun-exposed areas such as the face or some times the hands or digits. They usually do not appear in younger individuals and tend to arise more frequently in those with immuno deficiency. Merkel cell carcinomas present as a nonspecific papule or nodule. Because it can initially be misdiagnosed as a benign cyst, the actual pathology of the tumor may be delayed. Additionally, Merkel cell carcinoma is typically asymptomatic in the beginning, and this also adds to delay in diagnosis as many patients are not concerned until the fast-growing tumor reaches a large size.
The problem with Merkel cell carcinoma is that it is a highly aggressive type of skin cancer, and like melanomas, with enough growth and time, it can metastasize. Merkel cell carcinomas are treatable, and the treatment of choice is excision, the earlier, the better. Once a Merkel cell carcinoma has metastasized, it becomes a problematic tumor to treat, although new therapies are available that hold some promise. Recent studies suggest that 97% of Merkel Cell carcinomas have a common virus expression (Merkel cell polyomavirus). How this oncovirus may cause, Merkel cell carcinoma is currently unknown. Fortunately, patients that have Merkel cell carcinoma are not infectious.
If you observe a growth on the skin and you think to yourself, well, it doesn’t look like a basal or squamous cell carcinoma or mela noma; therefore, it’s probably benign always think of the other skin cancer, Merkel cell carcinoma. Happily, I have not had any of my patients that have had a trifecta of skin cancer also get Merkel cell carcinoma. In this scenario, I would have to name it the superfecta of skin cancer and not a title I would want to bestow on anyone.


There are several categories of pulmonary hypertension. WHO Group I includes patients with idiopathic pulmonary hypertension, familial pulmonary hypertension, drug and toxin related (fen-phen) portopulmonary hypertension, HIV related pulmonary hypertension and pulmonary arterial hypertension associated with connective tissue disorders (such as scleroderma). WHO Group II pulmonary hypertension is often referred to as pulmonary venous hypertension. This includes patients with left ventricular systolic or diastolic dysfunction or valvular heart dis ease. Essentially, the WHO Group II category includes patients who have an elevated pulmonary capillary wedge pressure and/ or elevated left ventricular end diastolic pressure. WHO Group III pulmonary hypertension consists of patients with COPD, interstitial lung disease, or other conditions in which hypoxia causes vasoconstriction. The remainder of this article will focus on WHO Group IV pulmonary hypertension (chronic thromboembolic pulmonary hypertension or CTEPH). Although WHO Group IV patients are relatively rare, it is crucial to identify them because this is the only type of pulmonary hypertension which is potentially surgically curable.
After acute pulmonary embolism, most patients will recover and have normal pulmonary hemodynamics, gas exchange, and exercise tolerance. It is believed that 1-4% of patients with acute pulmonary embolism will go on to develop CTEPH within two years. It is not clear why some patients with acute pulmonary embolism develop CTEPH. Risk factors include hypercoagulable states, myeloproliferative syndromes, splenectomy and chronic indwelling central venous catheters. Patients with CTEPH pres ent with dyspnea, which can have a gradual onset. Many patients with CTEPH will not have a known previous diagnosis of acute pulmonary embolism. As with other patients with pulmonary hypertension, patients with CTEPH may not show findings on physical exam until pulmonary hypertension is in the late stages. Findings include a right ventricular lift, jugular venous disten tion, fixed splitting of the second heart sound, hepatomegaly, ascites, and peripheral edema. Patients with CTEPH may have “flow murmurs” heard over the lung fields because of turbulent flow through partially obstructed or recanalized pulmonary arter ies. These tend to be accentuated during inspiration.
Acute pulmonary embolism is the trigger for CTEPH. In some patients this triggers a small vessel vasculopathy (for unclear rea sons) that contributes to the extent of pulmonary hypertension. This may explain why up to 35 percent of patients who undergo succesful pulmonary thromoendarterectomy can have some de gree of postoperative pulmonary hypertension.
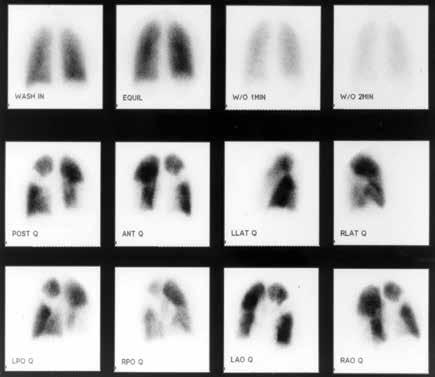
Although VQ scanning has become less commonly used for diagnosis of acute pulmonary embolism this remains the initial imaging study of choice in patients with pulmonary hypertension
to separate “small vessel” variants (Idio pathic pulmonary arterial hypertension) from “large vessel” disease (CTEPH) A normal VQ scan essentially excludes the diagnosis of CTEPH. A scan with one or more mismatched segmental defects is suggestive of the diagnosis. However, it is important to note that VQ scan can often under state the extent of central pulmonary vascular obstruction. Once the VQ scan is found to be abnormal then further testing should be undertaken (such as CT angiogram and/or pulmonary angiography). The angiographic findings in CTEPH are distinct from those of acute pulmonary embolism. They can include pouch de fects and pulmonary artery webs. Patients with severe pulmonary hypertension have been found to tolerate performance of angiog raphy as well as VQ scan without significant complication rate.
The surgery for CTEPH is quite different from surgical inter vention for an acute pulmonary embolism. Surgery for CTEPH is called a pulmonary thromboendarterectomy (PTE), which requires median sternotomy and cardiopulmonary bypass. It requires an often tedious intimal dissection of fibrotic recannal ized thrombus from the native pulmonary arterial wall. IVC filter placement is usually recommended before pulmonary thrombo endarterectomy. These patients can have a complicated postop erative course and this type of surgery is only done at a few spe cialized centers in the country. The center which is best known for this type of surgery is the University of California (San Di ego). Patients who have undergone PTE are typically maintained on lifelong anticoagulation. To be a candidate for this surgery, a patients must have central, surgically accesible chronic thrombo emboli. A significant postoperative complication is pulmonary artery steal, which refers to redistribution of pulmonary arterial blood flow from well-perfused segments into the newly opened segments resulting in ventilation perfusion mismatch and hypox ia. This redistribution of flow resolves over time. Approximately, 30% of PTE patients can develop reperfusion pulmonary edema. The perioperative mortality of pulmonary thromboendarterecto my can be in the range of 2-3% in experienced centers. Outcome is clearly better in high voluime centers (more than fifty PTE sur geries/year). Approximately 5000 thromboendarterectomy pro cedures have been performed worldwide, 3000 at UCSD alone.
Surgery for CTEPH is clearly the best therapeutic option. However, there are some patients with CTEPH who are inoper able or who have persistent or recurrent pulmonary hyperten sion after undergoing pulmonary thromboendarterectomy. There is now a medical therapy available for these patients. Riociguat (Adempas) was approved by the FDA in October 2013. It is a member of a new class of compounds-soluble guanylate cyclase stimulators. In the multicenter study by Ghofrani et al that was published in the New England Journal of Medicine in July 2013,
261 patients were randomized prospectively to re ceive riociguat versus placebo. Riociguat was shown to significantly improve exercise capacity and pul monary vascular resistance. Side effects include systemic hypotension. Prior smaller studies have also shown some benefits to medical therapy in CTEPH (inoperable or with post-operative PH) with oral agents such as bosentan and sildanefil, in haled iloprost and subcutaneous treprostinil. Medi cal therapy has also been used as a “bridge” before PTE.
Although relatively rare, CTEPH is an important cause of PH since it is potentially curable with pul monary endarterectomy. This surgery should only be performed in very experienced, specialized cen ters. PTE surgery should always be the treatment of choice for CTEPH. However, medical therapy can have a role as a bridge to PTE,in patients who are not surgical candidates or in those who have persistent pulmonary hypertension despite under going PTE.

I
Daniel Layish, MD, graduated
University Medical School in 1990. He then completed an In ternal Medicine
St.Louis, Missouri and a Pulmonary/Critical Care/ Sleep Medicine

has been a member of the Central Florida
may be
According to the Agency for Healthcare Research and Qual ity, more than 790,000 knee and 450,000 hip replacements are performed in the United States each year. While these numbers declined somewhat over the past year due to obvious reasons and events related to the pandemic, experts project a significant up ward trend in medically indicated joint replacement surgeries over the next 10 years.
More than 85-90 percent of patients who undergo total knee or hip arthroplasty (TKA/THA) surgery experience a favorable outcome, with a decrease in pain, an increase in mobility and an overall improved quality of life. And with advances in technology, patients can expect their replacement joint to function well for 20 years or longer. But not all joint replacement surgeries are suc cessful. Complications and failures can occur, and patients who expected dramatic pain relief and function after a knee or hip re placement may present with persistent pain, as well as consider able frustration and unhappiness.
About a third of patients will still have some aches and pains following knee or hip replacement. Early problems can be due to technical factors involving the surgery, inadequate rehab, or more serious problems such as infection or loosening. Problems can also occur years after surgery as the ceramics and plastics start to wear through. A joint replacement that had previously been functioning well for several years can suddenly start hurting or swelling.
The most common complaints following TKA include swelling, activity-related pain and mechanical symptoms, like a crunching behind the kneecap and even clicking when the patient walks. With THA, common painful symptoms include persistent pain around the tendon or bursa on the side of the hip.

Sorting out what is a normal discomfort for a prosthetic joint and what is a more serious problem is not always straightforward. What may seem like a minor ache or pain could be a sign of a more serious underlying problem. Problems such as instability or loosening of the knee or hip, or even more unusual problems like corrosion or metal sensitivity, can be easily misdiagnosed; ruling out infection and instability is critical.
The optimal plan of care for those patients who continue to experience ongoing joint pain after TKA or THA is an evaluation referral with an orthopedic specialist. Specialized tertiary referral centers like Orlando Health Jewett Orthopedic Institute offer expert specialist care and advanced technology, including leadingedge imaging, such as MRI scanning with metal artifacts suppres sion, to diagnose reasons for persistent symptoms after a knee or hip replacement.
Sometimes patients have unreal istic expectations of their replace ment, because of what they’ve been told or seen on TV or social media. Expecting the joint to be normal versus artificial is a common source of dissatisfaction. They may not follow proper rehab or activity levels. These patients require a comprehensive evaluation of their overall fitness level, including other joints like the shoulders and ankles. Patients need to focus on total body fitness and understand what a replacement joint can and cannot do.
An overall aging population, a rise in the prevalence of risk factors such as obesity, and the popularity of maintaining active lifestyles not only contribute to the increasing number of joint re placement surgeries, but also the inevitable consequential increase in complications or failed joint replacements. We also have seen an increasing number of joint replacements in a younger patient population whose active lifestyles place added stress and wear on their original and replacement joints. With normal use and activ ity, every joint replacement implant begins to wear over time, and excessive activity or weight may increase the rate of this normal wear, causing the replacement joint to loosen and become painful.
Evaluation by an orthopedic specialist may determine that a painful knee or hip replacement does need any further surgical intervention. It may simply be something that indicates additional physical therapy, weight loss or activity modification. But there is an increasing number of patients who will require a joint replace ment revision (redo).
Revision, or redo, surgery is a complex procedure that involves removing and replacing the original joint implant, usually due to a complication from the initial replacement.
Overall, complication rates following TKA or THA surgery are low. Serious complications, such as a joint infection, occur in fewer than 1-2 percent of patients. Instability can occur in 2-3 percent of knee replacements, and 2-3 percent of hip replacements can have a dislocation or similar problem. These percentages are small, but given the large number of surgeries performed, it adds up to a significant number of people experiencing undue discom fort and pain.
Typically, more women than men undergo knee replacement, with hip replacements being about even between men and women. Overall, men place more wear on replacement joints than women, due both to more body weight and slightly more activity, resulting in a slightly higher need for revision surgery.
Data from Medicare shows that the average rate of revision sur gery within 90 days is 0.2 percent but increases to 3.7 percent
within 18 months. These are usually due to infection or mechanical complications of the implant. While surgical techniques and implant designs and materials continue to advance, implant surfaces can wear down and the components can loosen over time. Research suggests that long-term wear and loosening affects 6 percent of people after 5 years and 12-15 percent after 10 years.
Only a handful of centers in Florida specialize in diagnosing and treating conditions associated with problematic joint replacements. Specialists with the Orlando Health Jewett Orthopedic Institute perform hundreds of successful revisions of knee and hip replacements every year for patients throughout Florida and the Southeast.




These complex, long procedures can be challenging and require multidisciplinary and subspecialty care, including infectious disease experts and plastic surgeons, as well as advanced surgical, intensive care, recovery and rehabilitation facilities that provide a higher level of care. Backed by all the resources of the Orlando Health system, Orlando Health Jewett Orthopedic Institute offers this advanced level of care. And, expected to be completed in 2023, a new, state-of-the-art orthopedic complex on Orlando Health’s downtown Orlando campus will usher in the next generation of orthopedic care.
Ultimately, the basic message for your patients is “Don’t give up hope!” An orthopedic surgeon who specializes in complex knee and hip revision work can provide a comprehensive evaluation to determine how to best correct a persistent joint replacement problem.
Internationally recognized for joint replacement surgery and trauma, George J. Haidukewych, MD, serves as Orlando Health’s director of orthopedic trauma and chief of complex joint re placement, practicing at the Or lando Health Jewett Orthopedic Institute. Dr. Haidukewych spe cializes in total hip and total knee replacements as well as orthope dic trauma. He brings extensive experience in the management of failed and infected total hip and total knee replacements and in reconstruction of the joints after trauma. Up to half of his practice is dedicated to solving these chal lenging problems from around the Southeast. Dr. Haidukewych completed his residency training at the Mayo Clinic in Rochester, Minnesota, as well as a fellowship at Florida Orthopaedic Institute in the Tampa Bay area..


Congenital or acquired urological conditions that affect the kidney, ureter, bladder and genitourinary system can happen to anyone, including children. As a pediatric urologist, I have performed many procedures to treat and resolve these issues. Techniques have ranged from complex surgeries that required larger incisions to less-invasive manual laparoscopic procedures. More recently, robot-assisted (RA) surgeries, where surgeons em ploy innovative robotic technologies to enhance precision, lessen scarring, shorten (or even eliminate) hospital stays and reduce recovery time, have gained a great deal of attention.
Conversations about RA surgeries have typically focused on adult procedures, starting with prostatectomies. However, RA surgery has become increasingly common in pediatric cases, with clinical outcomes that rival traditional techniques. Because children are smaller than adults, RA surgery requires more cus tomization in pediatric cases. That’s where the innovation comes in. Over the past couple of decades, highly experienced pediat ric surgeons have created and mastered the customization of RA surgery protocols for use in pediatric cases.
RA surgeries are not new. They have been performed for de cades. But the accolades have become more transparent in recent years as technologies have become more widely used. Here, we’ll discuss RA surgery through the da Vinci® surgical system.
The da Vinci surgical system has been around for 25 years and counting. Introduced in 1997, it became the first robotic surgi cal platform to be commercially available in the United States. In 2000, it was cleared by the FDA for use in general laparoscopic surgery.
The system provides surgeons with an advanced set of instru ments to use when performing surgery. There are three primary parts to the system:
• The surgeon console: Where the surgeon sits and guides in struments while viewing high-definition 3D images of the pa tient’s anatomy.
• The patient cart: Positioned alongside a patient’s bed, it con tains the camera and instruments the surgeon is controlling from the console. The system will translate a surgeon’s hand movements in real time, bending and rotating the instruments on the patient cart, while performing the procedure with a greater range of motion than available to the natural human hand.
• The vision cart: Facilitates communications between all the components and provides support for the 3D high-definition vision system.
Because RA surgeries are more sophisticated, they also can require more precise (and demanding) phys ical movement than traditional inci sion or manual laparoscopic surgeries. With traditional modes of surgery, the instruments can go in-and-out. They can rotate around the axis of how surgeons’ put the instrument into mo tion. They can go up-and-down and side-to-side. But the sur geon cannot articulate the wrist — there is only so much range of motion one can perform. With RA surgery, there is a greater range of motion, better articulation and better depth perception. In the urology field this is a huge benefit. When one can articu late the wrist and employ better vision, the task of sewing tissues becomes much easier.
At Orlando Health Arnold Palmer Hospital for Children, we currently utilize RA surgery in about 40 to 50 cases per year and have the ability to support from 100 to 120 per year.
There are a number of reasons for why the use of robotic surgery is on the rise, including quicker recovery rates and less reliance on pain medications. In fact, only 40 percent of the children we have treated with RA surgery have needed any nar cotic pain relief; and, 100 percent went home just with scripts of ibuprofen for pain relief.
These two major points are also beginning to catch the atten tion of health insurers, nationwide. More precise surgical proce dures, with reduced recovery time and lower narcotic pain relief, equate to better overall outcomes physically and financially, for patients, providers and payers alike.
When utilizing robotic surgery, the procedures between adult and pediatric patients are similar, but they’re performed on a miniaturized scale. While some surgical instruments do come in sizes that can be larger or smaller, they’re not specifically designed to be applied as adult or child sized — robotic or oth erwise. This means there’s a fair amount of customization that takes place when performing a RA surgery on a pediatric patient. But it’s never left to chance. Protocols have been in long use.
Early on, surgeons were concerned over a perceived change in tactile feedback when performing RA surgery. What was found over time, however, was that many experienced surgeons dis played a highly developed skill to ‘feel with their eyes;’ they were able to observe changes in tissue reaction, color and so forth through vision, which translated into tactile response and feed back.
Taking into consideration areas of adjustment that include space limitations when working in a smaller body cavity and pres sure, it goes without saying that an RA surgery procedure could be customized to make accommodations based on whether your patient is an adult or a child. Pediatric surgeons took note and developed customized RA surgery protocols.

Historically, surgeons made larger incisions through skin and muscle to get clear views of areas of concern. More invasive inci sion surgeries are still performed when necessary. But, when per forming RA surgery, the incisions are much smaller and the pro cedures are more minimally invasive, resulting in quicker healing and recovery times.
Some common RA pediatric urological procedures include:
• Partial and total nephrectomy
• Pyeloplasty

• Cyst removal
• Ureteral implantation
While the premise of RA surgery offers surgeons — and pa tients — enhanced precision, wider articulation and control, and better vision while performing delicate and complex pro cedures (and all the recovery benefits), it’s vital for referring physicians to vet the experience of pediatric surgeons. Surgeons are certified to perform RA surgery after five procedures. Be cause optimal precision comes with experience, it’s important to discuss experience and outcomes with the specialist you con sider.
Benjamin K. Rhee, MD, FACS, is a pediatric urologist with Orlando Health Arnold Palmer Hospital for Children and board certified by the American Board of Urology. He specializes in robotic pediatric urology surgery using the da Vinci® Surgical System and has performed more than 1,000 pediatric RA surgeries. Dr. Rhee may be contacted at (321) 843-9017.

We hear more about autism these days, leading many people to conclude that there are more and more cases each year. In fact, today we estimate that one in 54 children may be diagnosed as autistic, compared to one in 150 children back in 2000 and just one in 2,000 children in the 1980s. Is the incidence of autism re ally more than doubling every 20 years?
As a neurodevelopmental pediatrician, I don’t believe the in cidence of autism is truly increasing exponentially, but it is our screening and diagnosis of autism that has been expanding. We define autism as a developmental disorder characterized by dif ficulty in social interaction and communication associated with restricted or repetitive patterns of thought and behavior.
Currently there is no medical test to diagnose autism, such as a blood test. But our screening processes and diagnostic tools have expanded. Often, the first step in diagnosing a child with autism lies with the pediatrician. They assess the child soon after the first birthday to see if they’re meeting milestones and interacting ap propriately. If the physician or family suspects autism, the child is referred to a specialist for an official diagnosis, based on an evaluation using the Diagnostic and Statistical Manual of Mental Disorders, fifth addition (known as the DSM-5). In the state of Florida, this diagnosis must be made by a specialist – a develop mental pediatrician, a neurologist, a psychologist or a psychiatrist, in order for the insurance companies to provide approval for the appropriate therapy, applied behavioral analysis (ABA), that the child needs.
In the past, a child may have been given the diagnosis of mental retardation, now more commonly known as intellectual impair ment. In the case of a higher functioning child, the child may previously have been considered to be just quirky and different, and may have been diagnosed with the term Asperger’s. Today that same child may be considered autistic, based on the expand ing criteria. A diagnosis of autism addresses a combination of two things: intelligence and behavior. The terms “high functioning” and “low functioning” refer to intellectual ability or intelligence. The terms “low,” “moderate” and “severe” refer to their autistic behaviors. We see autistic people at all levels of intelligence and behavior. For instance, many may remember the character from the Rain Man film of the 1980s, who would be considered super high functioning for his intelligence – a savant even. Yet, his be havior was more severe.
While we don’t know what causes autism, we do know that boys are up to four times as likely to be diagnosed as girls. We also know that genetics are very much involved. In fact, parents with one au tistic child are 10 to 20 percent more likely to have a second child diagnosed. If one identical twin is diagnosed as autistic, there is as high as a 90 percent chance the second twin is also autistic.
As our screening and diagnostic tools for autism have expanded, our knowledge of treatment options for autism remains the same. Despite the numerous claims that there is a cure for autism, such as medications, mega-vitamins, gluten-free and casein-free diet, hyperbaric oxygen chambers or colonic cleanses, none have demonstrated success in curing or treating autism. Af ter years of experience with autism, the medical community can say that behavioral therapy is the only treatment to have shown significant success.
It’s important to note that while medication may not be an effective treatment for autism, many people with autism have comorbid conditions, such as anxiety or depression, attention deficit hyperactivity, seizures, sleep issues and sometimes more significant behaviors of self-injury and aggression, where medications may have some benefit.
When it comes to treatment, we have seen significant success with applied behavioral analysis or ABA, an evidence-based treat ment strategy used to reduce challenging behaviors and increase socially appropriate behaviors. ABA therapy is an intensive thera py administered by a board-certified behavioral analyst (BCBA)/ registered behavior technician (RBT) – up to 40 hours per week, which may be offered in the home or in a clinical setting. The therapy consists of an intensive, structured teaching program in which social and communication behaviors are broken down and rehearsed in their simplest elements. Other forms of therapy, such as floor time and circles of communication have also been shown to provide beneficial effects and can be practiced at home. Here the parent gets down at the child’s eye level and, through play, makes continuous social communication and interaction, back and forth, creating circles of communication which help the child understand that there’s a world out there in which he or she can interact.
Studies show that the earlier ABA therapy begins, the earlier we can see improvement. Our developmental window is the first six years of life. We see cases where treatment begins as early as 2 years of age and the child is ready for regular kindergarten by the age of 5 or 6. Sadly, the process of diagnosis and qualifying for treatment can be slow. In many cases, we see that it may take more than six months to see a specialist for a diagnosis and then up to a year to find availability with an ABA therapist, underscoring the need for early intervention. We recommend referring children to a special ist as early as possible to ensure that autism is diagnosed promptly and treatment may begin.
Special training is also available for parents and family mem
bers, which I highly recommend. In fact, siblings often turn out to be the best therapists for their sibling with autism. So often children learn better from other children than an adult. Involving siblings in the therapy can also make the siblings feel more a part of the solution rather than resenting the autistic sibling for the extra attention required from parents. This special training for family members is an excellent tool to supplement ABA therapy or to be used while a family is awaiting ABA therapy approval or availability.


Autism is a fascinating field of study. We continue to learn more about the condition and ways to improve functionality. In fact, I’m currently working with a group of ear, nose and throat specialists, and gastroenterologists on a study to determine if nasopharyngeal microbiomes may be a marker for autism, advancing the thought that the olfactory nerve is the closest in proximity to brain tissue that can be easily accessible. This may provide evidence of changes within the brain, specific to children with autism, which can then be used a marker aiding in the diagnosis of autism. I look forward to learning more and to continuing my work serving autistic children and their families.

If you suspect a child has autism, consider scheduling an appointment with a specialist as early as possible to maximize treatment op portunities.




Naina Mehta, MD, is a neu rodevelopmental pediatrician at the Orlando Health Arnold Palmer Hospital for Children Pediatric Behavioral Health and Developmental Center. She is board certified in neuro developmental disabilities. Dr. Mehta has co-published studies involving meditation, yoga and breathing practices for children and youth with ADHD and learning disabilities. She offers parents both personal experi ence and professional training in managing behavioral issues with their children. She is cur rently leading a research study with ENTs and gastroenter ologists on nasopharyngeal mi crobiome as a possible autism marker.

 By Julie A. Tyk, JD.
By Julie A. Tyk, JD.
An exculpatory clause purports to deny an injured party the right to recover damages from a person negligently causing his injury. Cain v. Banka, 932 So. 2d 575 (Fla. 5th DCA 2006). They are disfavored in the law because they relieve one party of the obligation to use due care and shift the risk of injury to the party who is probably least equipped to take the necessary precautions to avoid injury and bear the risk of loss. Applegate v. Cable Water Ski, L.C., 974 So. 2d 1112, 1114 (Fla. 5th DCA 2008). Such clauses are strictly construed against the party seek ing to be relieved of liability. Sunny Isles Marina, Inc. v. Adulami, 706 So. 2d 920 (Fla. 3d DCA 1998). Thus, exculpatory clauses are enforceable, only where, and to the extent, that the intention to be relieved from liability is made clear and unequivocal. Tat man v. Space Coast Kennel Club, Inc., 27 So. 3d 108, 110 (Fla. 5th DCA 2009). The wording must be so clear and understand able that “an ordinary and knowledgeable person will know what he is contracting away.” Id. (quoting Gayon v. Bally’s Total Fitness Corp., 802 So. 2d 420 (Fla. 3d DCA 2001)).
The seminal Florida case on exculpatory clauses is the Florida Supreme Court case of Sanislo v. Give Kids The World, Inc., 157 So. 3d 256 (Fla. 2015). Give Kids the World, Inc. (“GKTW”) provided free vacations to seriously ill children and their families. When applying for the vacation, the Sanislos executed a “wish request” form that contained a waiver of liability, also known as an exculpatory clause. When the parents arrived at the resort vil lage they again signed a liability release form, also an exculpatory clause. The language of the exculpatory clause is reprinted below for reference:
I/we hereby release Give Kids the World, Inc. and all of its agents, officers, directors, servants, and employees from any liability whatsoever in connection with the preparation, execution, and fulfillment of said wish, on behalf of our selves, the above named wish child and all other participants. The scope of this release shall include, but not be limited to, damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physi cal and emotional), entertainment, photographs and physi cal injury of any kind....
I/we further agree to hold harmless and to release Give Kids the World, Inc. from and against any and all claims and causes of action of every kind arising from any and all physical or emotional injuries and/or damages which may happen to me/us....
Sanislo at 258-259.
While participating in a horse-drawn wagon ride, a rear pneu matic lift designed to allow those in wheelchairs to participate failed, and Ms. Sanislo was injured. The Sanislos brought suit and GKTW filed a motion for summary judgment arguing that the signed releases precluded an action for negligence. The Sanislos filed a motion for partial summary judgment against GKTW’s affirmative defense of release. The trial court granted the Sanislo’s
motion and denied GKTW’s motion. The jury found for the Sanislos and GKTW appealed. Id.
The Fifth District reversed, finding the lower court erred in denying GK TW’s motion for summary judgment because the release signed by the Sanislos was unambiguous and did not contravene public policy. It ruled the exculpatory clause barred the negligence action despite the lack of a specific reference to “negligence” or “negligent acts” in the exculpatory clause.
The Fifth District reasoned that exculpatory clauses are effec tive if the wording of the exculpatory clause is clear and under standable so that an ordinary and knowledgeable person would know what he or she is contracting away, and that the court had previously rejected “‘the need for express language referring to release of the defendant for “negligence” or “negligent acts” in order to render a release effective to bar a negligence action.’ ” On the public policy argument, the Court said the relative bargain ing power of the parties should not be considered because it was outside of the public utility or public function context and the Sanislos were not required to request a vacation with GKTW or go on the vacation. Id.
In affirming the Fifth District’s decision, the Supreme Court wrote that the conflict for the Court’s resolution was “whether an exculpatory clause is ambiguous and thus ineffective to bar a negligence action due to the absence of express language releas ing a party from its own negligence or negligent acts.” Id. at 260.
The Florida Supreme Court wrote:
.... we are reluctant to hold that all exculpatory clauses that are devoid of the terms “negligence” or “negligent acts” are ineffective to bar a negligence action despite otherwise clear and unambiguous language indicating an intent to be relieved from liability in such circumstances. Application of such a bright-line and rigid rule would tend to not effectuate the intent of the parties and render such contracts otherwise meaningless.
Id. at 270.
The Court found that the GKTW liability release form re leased GKTW and all of its agents, officers, directors, servants and employees from “any liability whatsoever in connection with the preparation, execution and fulfillment of said wish…” The release then provided that the scope of the agreement included “damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physical and emotional), entertainment, photographs and physical injury of any kind . . . .” The Court found that the release clearly conveyed that GKTW would be released from any liability, including negli gence, for damages, losses, or injuries due to transportation, food, lodging, entertainment and photographs. Id.
The determination of whether an exculpatory clause is en
forceable will be determined by the Judge as the enforceability of a pre-injury release is a question of law. The enforceability there fore, will depend on the Judge assigned to the matter. Physicians should not assume that because a patient signed a liability release form the patient does not have a viable cause of action. Physicians should consult with an experienced attorney who can examine the facts of the case and help you determine the best path for ward. The Health Care Practice Group at Pearson Doyle Mohre and Pastis, LLP is committed to assisting Clients in navigating and defending medical malpractice claims. For more informa tion and assistance, please contact David Doyle and Julie Tyk at Pearson Doyle Mohre & Pastis, LLP.
Julie A. Tyk, JD, is a Partner with Pearson Doyle Mohre & Pastis, LLP. Julie concentrates her practice in medical practice defense litigation, insurance defense litigation and health care law. She has represented physicians, hospitals, ambulatory surgical centers, nurses and other health care providers across the state of Florida. She may be contacted by calling (407)
jtyk@pdmplaw.com..


Your brand is the identity that you create for your practice. It is crucial to identify the core values that you want your brand to represent, because this is how it will be perceived by your target audience and the community at large.
Here are some questions to consider when building your brand:
• How do you want your practice to be perceived?
• What core values do you hold most important to your WHY?
• What does your brand look like? Colors, fonts, and shapes matter.
• What does your brand sound like?
When choosing your brand colors, be aware of the following color associations:
• Red — Red stands for passion, excitement, and anger. It can signify importance and command attention.
• Orange — Orange stands for playfulness, vitality, and friend liness. It is invigorating and evokes energy.
• Yellow — Yellow evokes happiness, youth, and optimism, but can also seem attention-grabbing or affordable.
• Green — Green evokes stability, prosperity, growth, and a connection to nature.
• Light Blue — A light shade of blue exudes tranquility, trust, openness. It can also signify innocence.
• Dark Blue — Dark blue stands for professionalism, security, and formality. It is mature and trustworthy.
• Purple — Purple can signify royalty, creativity, and luxury.
• Pink — Pink stands for femininity, youth, and innocence. It ranges from modern to luxurious.
• Brown — Brown creates a rugged, earthy, old-fashioned look or mood.
• White — White evokes cleanliness, virtue, health, or simplic ity. It can range from affordable to high-end.
• Gray — Gray stands for neutrality. It can look subdued, clas sic, serious, mysterious, or mature.
• Black — Black evokes a powerful, sophisticated, edgy, luxuri ous, and modern feeling. (www.99designs.com)
Think of your Business brand as a person. What is this person’s personality like? How does he or she dress, talk, and act in public? Here are just a few examples of a personality that your brand
may have:
• Serious and Professional
• Warm and Friendly
• Cool and Quirky
• Funny and Playful
However, you choose to represent your brand, make sure that it is authentic to who you are. For example, if you are playful and like to crack jokes, infuse your marketing with humor and you will find that people respond positively to jokes, memes, and quotes that are applicable to them. For example, for pedi atric practices, we have found that moms just can’t get enough of memes that make fun of their kids! You can add some (goodnatured) jokes and memes to your social media posts and you will see some great engagement.
Similarly, if you want your brand to be viewed as serious and professional, you will want to consistently share valuable and in formative content that educates your audience. You can choose to do so by looking for speaking opportunities to help build credibility and position you as the expert in your field, making educational videos and sharing them on your website, Youtube, and social media, or by writing educational articles and contrib uting to reputable publications.
If you’re going for warm and friendly, you will want to be seen engaging with your social media followers, being active in Facebook groups and other online groups, hosting community events, supporting great causes, etc.
If cool and quirky is your thing, you want to stand out from your competitors. You can use some colors that are not typi cal for your industry, create and share some fun videos, such as “funny (HIPAA-compliant) things that patients say”, paint your waiting room to inspire awe upon arrival, etc.
Keep in mind that for any brand personality, it is important to keep it consistent across your website content, social media posts, marketing materials, and any other communication that you may have with your audience.
Sonda Eunus is the Co-Founder of Pro Medical Marketing – an Internet Marketing Agency specializing in Medical practices. She has a Masters’ in Healthcare Management and is a MGMA Certified Medical Practice Executive. She has been heavily involved in operating her family’s Pediatric practices from an early age. She is passionate about helping medical practices grow and does so by sharing her experience in her writing, speaking, and consulting. Learn more about Sonda and Pro Medical Marketing at www.promedicalmarketing.com.

Florida MD is a monthly medical/business digital magazine for physicians..

Florida MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD.
It is hard to be aware of everything happening in the rapidly changing medical profession and doctors want to know more about new medical developments and technology, procedures, techniques, case studies, research, etc. in the different specialties. Especially when the information comes from a local physician specialist who they can call and discuss the column with or refer a patient. They also want to read about wealth management, financial issues, healthcare law, insurance issues and real estate opportunities. Again, they prefer it when that information comes from a local professional they can call and do business with. All advertisers have the opportunity to have a column or article related to their specialty or profession.







