

JANUARY/FEBRUARY 2023 • COVERING THE I-4 CORRIDOR Encompass Health Hospital Rehabilitation of Altamonte Springs Providing Superior Outcomes Through Connected Care

As a nationwide leader in rehabilitation services, Encompass Health Corp., formerly HealthSouth Corp., has been known in the medical community for over three decades. In 2015, the company, already present in the state of Florida, expanded to Central Florida, bringing an exemplary level of post-acute care to the region with the opening of Encompass Health Rehabilitation Hospital of Altamonte Springs in 2014. The hospital is part of a nationwide network of 130 inpatient rehabilitation hospitals and 220 home health locations and 58 hospice locations.

As Encompass Health, the hospital and its staff remain dedicated to guiding each patient through recovery and are committed to helping patients regain their independence. By building a solid reputation for its comprehensive approach to rehabilitation of patients, including those dealing with traumatic injuries that require extensive rehabilitation services, Encompass Health Altamonte Springs provides options that benefit patients with acute care needs and their families committed to getting them back home, getting them back their independence and living life to its fullest.

FLORIDA MD - JANUARY/FEBRUARY 2023 1 DEPARTMENTS 2 FROM THE PUBLISHER 8 DERMATOLOGY 9 MARKETING YOUR PRACTICE 10 HEALTHCARE LAW 12 PULMONARY AND SLEEP DISORDERS 14 PEDIATRICS contents JANUARY/FEBRUARY 2023 COVERING THE
CORRIDOR 16 CANNABIS DEMONSTRATES IMPROVEMENT IN OPIOID ADDICTION OUTCOMES 17 OSTEOPOROSIS IN MENOPAUSE 19 ADVANCEMENTS IN DIGESTIVE HEALTH 4
I-4
COVER STORY
PHOTO: ENCOMPASS HEALTH
PHOTO: DONALD RAUHOFER / FLORIDA MD
ON THE COVER: Encompass Rehabilitation Center of Altamonte Springs
Iam pleased to bring you another issue of Florida MD. I can only imagine the emotional and physical trauma that a woman goes through when she has a mastectomy. The procedure affects not only her body, but her mind and her self-esteem. Now add in the inability to not be able to reconstruct her breasts and give that part of her life back, because she’s uninsured or under insured, and it becomes an unthinkable crushing blow. Fortunately there is My Hope Chest to help women who are unable to afford reconstructive surgery. I asked them to tell us about their organization and how you, as physicians, can help. Please join me in supporting this truly wonderful organization.
Best regards,
Donald B. Rauhofer Publisher


MY HOPE CHEST — Making Women Whole Again
In 2010, more than 22,000 uninsured women lost their breasts to cancer and were left disfigured, deformed and feeling “less than whole.” How many years has this figure been growing?
Many organizations raise funds for research, education and “awareness” of breast cancer. Most have no idea there lies a huge gap in assistance for delayed reconstruction and co-pays for survivors wanting this surgery.
My Hope Chest is the ONLY national 501c3 non-profit organization focused on funding breast reconstruction for the uninsured and under insured survivors. Our services “pick up” where other breast cancer organizations leave off… providing the “final step in breast cancer treatment. ”

My Hope Chest is about addressing the needs of survivors now. Through wonderful surgeon partnerships we are able to transform the lives of breast cancer survivors who otherwise have no hope of reconstruction.
We hope to hear from you to learn how we can work together to eliminate our wait list and take action to help every woman who desires reconstruction after mastectomy and feel restored in body, mind and spirit.
Wish List
• Surgeons to create awareness for My Hope Chest and to identify new clients
• Doctors of Distinction- Surgeon partners nationwide to join our program.
• Corporate partners, interested in Win-Win, Commercial- coventure marketing campaigns promoting their product or service by sharing our vision to make sure there is always coverage for reconstruction surgery.
For additional information on how you can help or refer a patient please go to www.MyHopeChest.org.
ADVERTISE IN FLORIDA MD
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
PREMIUM REPRINTS
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: John “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, Shyam Varadarajulu, MD, Jyothsna Bandaru, MD, Ramamoorthy Nagasubramanian, MD, Julie Tyk, JD, Sonda Eunus, MHA, Michael Patterson NHA, OTR/L, CEAS, John Meisenheimer, VII
Art Director/Designer: Ana Espinosa Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762. Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2023 Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.
FLORIDA MD - JANUARY/FEBRUARY 2023 FROM THE PUBLISHER
2

FLORIDA MD - JANUARY/FEBRUARY 2023 3 or call (844) 212-5321 to learn more. Visit neulinehealth.com/providers THE BEST EEG CLINICAL CARE FROM THE COMFORT OF HOME NeuLine Health is a neurodiagnostic services provider that performs convenient, at-home Ambulatory EEG testing for patients with neurological-related medical conditions. We are dedicated to serving qualified healthcare providers and their patients with best-in-class neurodiagnostic testing, nationwide. In-home testing puts the mind at ease, leading to a more accurate picture of neurological activity. Testing through NeuLine Health typically costs 3X less than inpatient care. Scheduling with NeuLine Health is fast and convenient, leading to faster answers on the next steps in your treatment. 01 02 03 Convenience & Comfort Affordability Rapid Results Leading the Wave IN EXCEPTIONAL EEG CARE
Encompass Health Hospital Rehabilitation of Altamonte Springs – Providing Superior Outcomes Through Connected Care
By Staff Writer
As a nationwide leader in rehabilitation services, Encompass Health Corp., formerly HealthSouth Corp., has been known in the medical community for over three decades. In 2015, the company, already present in the state of Florida, expanded to Central Florida, bringing an exemplary level of post-acute care to the region with the opening of Encompass Health Rehabilitation Hospital of Altamonte Springs in 2014. The hospital is part of a nationwide network of 130 inpatient rehabilitation hospitals and 220 home health locations and 58 hospice locations.
As Encompass Health, the hospital and its staff remain dedi-
cated to guiding each patient through recovery and are committed to helping patients regain their independence. By building a solid reputation for its comprehensive approach to rehabilitation of patients, including those dealing with traumatic injuries that require extensive rehabilitation services, Encompass Health Altamonte Springs provides options that benefit patients with acute care needs and their families committed to getting them back home, getting them back their independence and living life to its fullest.
Based on 2016 data, Encompass Health accounts for 22 percent of licensed beds in the nation and provides rehabilitation services for 29 percent of Medicare patients. In November 2018, Encompass Health Altamonte Springs expanded its services to reach even more patients. The hospital added 20 new beds, giving it a total of 70. It also recently opened a new dialysis unit with four beds, allowing those in need of dialysis to continue their therapy and work toward their individual goals. The hospital has seen over 1,800 patients since it opened its doors in the fall of 2015 and received a reaccreditation by The Joint Commission as a facility of care.
For Dr. Eliam Fuentes, medical director of Encompass Health Altamonte Springs, it was not surprising; “Since our opening we have helped so many patients providing excellent rehabilitation care for many strokes, Parkinson’s, and other catastrophic injuries.”
Dr. Fuentes, began seeing patients at HealthSouth Altamonte Springs in 2014, after doing his residency in Cleveland, Ohio. He was drawn to the endless possibilities that would result in bringing an established hospital system to a growing and aging community. “Being such a large corporation, Encompass Health has rehab down to a science, we have resources and each hospital can function and operate and focus on specialties needed in our patient population.”
“THE UPSWING OF MEDICINE”
Encompass Health Altamonte Springs employs a staff of more than 100 who are quick to point out what sets their teams and their services apart. First is clearing up the misconception, that because “rehabilitation” is in the hospital name,

FLORIDA MD - JANUARY/FEBRUARY 2023 4 COVER STORY
Dedicated physical therapists are key to providing focused care to patients.
PHOTO: ENCOMPASS HEALTH
that it is the same as a skilled nursing facility. The hospital also provides access to independent physicians specialized in rehabilitative medicine including Dr. Fuentes, and Dr. Dana Kuriakose.
“At a skilled nursing facility a patient’s stay is a lot longer and they have approximately three to five hours of rehabilitation a week. At Encompass Health Altamonte Springs, we are a hospital and as such we are regulated to do three hours of therapy a day for five days each week,” explains Dr. Kuriakose.
The secret to the hospital’s success, he added, is its staff and the fact that it is 100 percent dedicated to rehabilitation. The therapy is intentional, focused, multi-disciplinary and effective. With an average length of stay of about 12 days, compared to 38.5 days at a skilled nursing home, Dr. Fuentes said Encompass Health can also get patients back to their home, which is better for the patient and more cost-efficient. For 2017, the company had a 79.4% discharge rate back to the community outperforming the Uniform Data System for Medical Rehabilitation average of 75.9%.
The therapy gym, located in the center of the hospital, is a focal point of a patient’s time at the hospital and boasts the most advanced equipment. Patients can move easily from one modality to the next during their multiple visits to the gym each day. Modalities include partial weight bearing equipment, to gate training, to IREX, a new modality that is a virtual reality therapy system which uses immersive video gesture control.
“The biggest thing to educate our patients about is that they’re not going to spend all day in bed. The goal here is to be out of bed, in the gym and working toward independence. For some that is terrifying and for some that is a welcome change,” says Dr. Kuriakose. “We almost take a second seat as a physician, because the real goal is to get their therapies and ultimately transition them home.”
THE ENCOMPASS HEALTH PATIENT
Most Encompass Health Altamonte Springs patients are admitted from local acute care hospitals, although some are referred from home or other long-term care facilities. Patients admitted to Encompass Health Altamonte Springs face complex situations resulting from stroke, spinal cord injuries, amputations, traumatic brain injuries, ALS and neurologic cases. The hospital is also one of the few facilities in Central Florida certified in LSVT programs designed for Parkinson’s disease. In addition, the hos-
pital current holds disease-specific care certification from The Joint Commission for its stroke rehabilitation program.
For all patients though, regardless of their injury, there is a common denominator. Patients and their families must be committed and able to handle the intense rehabilitation they will undergo at Encompass Health Altamonte Springs.

“If you have a complex patient with many medical comorbidities, it is a challenge to do therapies outpatient or at home,” explains Dr. Fuentes. “Most patients cannot endure home therapies and some think they can’t tolerate three hours of therapy, but many can and they do.”
Before a patient is admitted, he or she undergoes pre-admission screening. Nurses do a CMS guideline screening, patients are then evaluated by a physiatrist and physical and occupational therapists.
“Every patient is exposed to multiple therapies. Patients engage in physical therapy and we see how they perform. If they can tolerate it, it’s a good predictor of their success in an inpatient rehabilitation facility,” says Dr. Fuentes.
PLANNING DISCHARGE AT ADMITTING
For Encompass Health Altamonte Springs patients, discharge planning begins at admission and includes patients and their families and caregivers every step of the way. “We work as a team. From day one, we establish realistic goals that involve patients, family, and the whole team. The whole idea is to set up a rehabilitation plan that includes the patient, and an interdisciplinary team aimed to guarantee a safe discharge home,” says Dr. Fuentes.
FLORIDA MD - JANUARY/FEBRUARY 2023 5 COVER STORY
Patients participate in a variety of exercises which help strengthen motor skills.
PHOTO: ENCOMPASS HEALTH
This includes case managers planning ahead for everything from durable medical equipment to dialysis treatments, so that when patients can return home they have everything that they need to sustain their rehabilitation success. And if further care is needed after discharge, patients can choose to continue that high level of care they received in the hospital at home. In addition to inpatient rehabilitation, Encompass Health also has a home health and hospice segment available after discharge if needed.
PATIENT OUTCOMES
For patients, being part of an acute care facility means that they will move around and benefit from it. Encompass Health Altamonte Springs prides itself on extremely low infection rates, half the benchmark for national rehabilitation hospitals.
“This is exceptional, especially considering we are working with post-surgical patients,” says Dr. Fuentes. “It is not only about function. As physiatrists we are trained in wound care, and our hospital is blessed to have a great wound care program that handle complex wounds on a regular basis.”
THE “TEAM CONFERENCE”
At Encompass Health Altamonte Springs, the multi-disciplinary team is charged with executing a road map that will get patients out of their hospital bed and return home. The hospital has all the specialties of an acute hospital including infectious disease and cardiology to name a few. These specialists, comprising the team, meet two to three days per week in what is called the “team conference.” Working cohesively as a group in these “team conferences” they ensure that patients are getting all of the services they need to get them home faster, healthy and infection free.
At the table you will find the entire team including the physician, a pharmacist, physical therapist, occupational therapist, speech therapist, registered dietitian, nurse and a case manager. The first team conference takes place within the first week of admission after the patient has fully been assessed. Together the 15-20 members of the team come up with one solidified idea to make a patient more functional with the ultimate goal is to start addressing a patients needs early on.
“These meetings help us to coordinate patients’ needs better,” says Dr. Fuentes. “Every portion is so valuable and will help the patient turn the corner.”
PHYSIATRISTS - THE QUALITY OF LIFE SPECIALISTS
Physiatry is a specialty that began during war time, caring for the military during the first and second World Wars. The physiatrists at Encompass Health Altamonte Springs point out that, while not as well known in the United States as in other countries, it is a specialty that is growing exponentially.
“As a specialty, physical medicine & rehabilitation focuses on function. We treat neurological and musculoskeletal conditions which can limit independence” says Dr. Fuentes.
For those who have made their careers in physiatry, such as Drs. Fuentes and Kuriakose, it is a specialty of the heart. Each has a unique path that led them to this field.
Dr. Fuentes did his residency at Case Western Reserve University at the MetroHealth Rehabili-

FLORIDA MD - JANUARY/FEBRUARY 2023 6 COVER STORY
The goal at Encompass Health is to get patients out of bed and working toward their independence.
PHOTO: ENCOMPASS HEALTH
tation Institute of Ohio, where spent part of his residency at the trauma hospital and at the Veterans’ Hospital in Cleveland treating traumatic brain injuries and spinal cord injuries. For him, overseeing a patient’s rehabilitation from a devastating injury and observing their strength, and the strength of their families recommitted him to the specialty.
Dr. Fuentes understands firsthand the life changing effects of rehabilitation. At the age of two, his daughter suffered a stroke and became a patient at the Encompass Health hospital in Puerto Rico.
“I changed my career goals after that. Other specialties don’t have the ability to see the direct results of treating complex issues. My daughter was completely dependent when she became a patient at Encompass Health Puerto Rico. And now, here we are years later, she is a normal teenager and has recovered completely. I often share this story with my patients. It helps us create a rapport. I don’t presume to know what ever patient is feeling, but I’ve been there in a hospital, crying and I have been in their shoes.”
For Dr. Kuriakose, the specialty is incredibly rewarding because she can oversee a patient’s progress. “We get to see patients over a long period of time, their progression and as they move back into the community.”
It was while in residency at Harvard that she treated Boston Marathon bombing victims and witnessed firsthand the strong sense of support within the rehabilitation community.
“This support is invaluable for patients. I consider it a privilege to be a part of the team that gives them the physical and emotional tools to regain their independence.”
WHY ENCOMPASS HEALTH?

At Encompass Health Altamonte Springs, the physiatrists and therapy teams work in tandem, providing an acute rehabilitation facility that offers patients the ability to be monitored and have their therapy directed from all angles. This aids in overall positive outcomes and patients return to an independent, albeit perhaps new normal, life.

For Dr. Fuentes and his colleagues, time spent at the inpatient rehabilitation hospital is a critical component to a patient making important strides in his or her recovery.
“I would advise them to trust our care and providers. We have the best therapy teams, we have the best nursing teams and we have an excellent team of doctors dedicated to our patients.”
With the commitment of its staff, therapists and physicians, Encompass Health Altamonte Springs continues to spread its wings, and reach those with acute rehabilitation needs, providing patients with a road to recovery in order to return home, to a new normal and regain a level of independence despite their injuries.
FLORIDA MD - JANUARY/FEBRUARY 2023 7 COVER STORY
Therapists review multi-disciplinary patient treatment plans.
ENCOMPASS HEALTH REHABILITATION HOSPITAL OF ALTAMONTE SPRINGS
SOUTH STATE ROAD 434 ALTAMONTE SPRINGS, FL 32714
NUMBER: 407.587.8600
PHOTO: ENCOMPASS HEALTH
831
PHONE
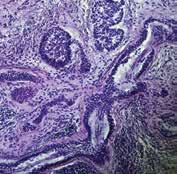
Not All Basal Cell Carcinomas Are Created Equal

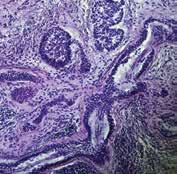


 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
Occasionally a patient will tell me their “doctor friend” recommended that they don’t need treatment for a basal cell carcinoma because it will never hurt you. “Doc, he said it’s only a basal cell carcinoma.” Dermatologists fully recognize this as a genuinely cringe-worthy statement. You don’t need to see too many people missing various parts of their facial anatomy to know this advice is blatantly wrong. Even in this modern time of medical miracles, people still die from neglected basal cell carcinomas. When pressed for the name of their “doctor friend,” it usually comes up as I don’t remember their name, or it ends up being “Doctor Google.”
It is true a superficial basal cell carcinoma on the torso probably would take years and years for it to cause any sort of significant morbidity to a patient. But, on the other hand, even a small basal cell on the torso will continue to grow if left untreated slowly. What might have been a simple, inexpensive procedure now, a decade later, has turned into a monster of aggravation, discomfort, and cost.
Although metastatic disease risk is low with basal cell carcinomas, it is certainly not zero. Several people die each year from basal cell carcinoma. Even more, patients can have disfiguring bouts with cancer losing various parts of anatomy such as nose, ears, eyes, etc. What a lot of patients and even some physicians are not aware of is that not all basal cell carcinomas are created equal. There are several different histologic growth patterns. These varying histologic types can each behave differently and require different treatment plans.
As mentioned before, a superficial basal cell carcinoma is probably not going to cause a great deal of physical damage unless neglected for long periods. There are other types of basal cell carcinomas; morpheaform and sclerosing basal cell carcinomas with infiltrating growth patterns. These cancers left untreated can cause a significant amount of morbidity in shorter periods measured in months, not years. Aggressive basal cell cancers can also become neurotropic, meaning that they “wrap” around a nerve and can track down its length. Neurotropism can be particularly dangerous, especially if this is on the face and affecting a nerve that happens to pass through a foramen into the brain. Clearly, not a good scenario.
Basal cell carcinomas, limited to the skin, tend to be very amenable to treatment in a variety of different ways. Even as a Mohs surgeon I can think of at least half a dozen different ways that I have treated basal cell carcinomas. Not all basal cell carcinomas need Mohs surgery. Each case of basal cell carcinoma should be evaluated individually and in consideration as to the best method of treatment based on its histologic growth pattern, location, and physical condition of the patient.
The great news about basal cell carcinoma, even though it is the most common type of skin cancer and millions are treated each year, only a tiny percentage of these end up causing death in patients. When someone says I would much rather have a basal cell carcinoma than a melanoma, there is a caveat; if you die from a basal cell carcinoma, you are just as dead as if you were to die from melanoma. Happily, most of the time, with early diagnosis and treatment, you don’t have to die from either. Basal cell carcinoma is called cancer for a reason. Give it its respect that it is due, or otherwise, you may regret saying, “oh, you don’t have to worry about it, it’s only a basal cell carcinoma.”
Lucky Meisenheimer, M.D. is a board-certified dermatologist specializing in Mohs Surgery. He is the director of the Meisenheimer Clinic – Dermatology and Mohs Surgery. John Meisenheimer, VII is a medical student at USF.

FLORIDA MD - JANUARY/FEBRUARY 2023 8 DERMATOLOGY
PHOTO: JOHN MEISENHEIMER, VII
Pathology of an infiltrative basal cell carcinoma.
Infiltrative Basal Cell carcinoma of the forehead.
Superficial Multifocal BCC.
Nodular basal cell carcinoma.
PHOTO: JOHN MEISENHEIMER, VII
Neurotropic basal cell carcinoma. Sclerosing basal cell carcinoma.
PHOTO: JOHN MEISENHEIMER, VII
PHOTO: JOHN MEISENHEIMER, VII
PHOTO: JOHN MEISENHEIMER, VII
PHOTO: JOHN MEISENHEIMER, VII
Is Your Online Reputation Costing You Patients?
By Sonda Eunus, MHA, CMPE
What does your online reputation say about your practice? If you have a negative online reputation, you are missing out on new patients every day. Most medical practices now get the majority of their new patients through Google and other search engine queries, such as “Pediatrician in Orlando”. If your practice appears in these searches, the most common next step for a potential new patient would be to check out your reviews – what are other patients saying about your practice? It has been reported that 90% of consumers read online reviews before visiting a business and that online reviews influence 67% of purchasing decisions (Bright Local). For this reason, it is incredibly important to pay attention to the rating and reviews that your practice has on search engines, social media platforms, and local online business directories.
However, despite the importance of cultivating a positive online reputation, only 33% of businesses report actively collecting and asking for reviews (1). One great process to set in place at your practice is asking for patient reviews after each patient visit. It can be as simple as training your front office staff to ask each patient how their visit went while checking them out, and if they receive favorable feedback then they can ask the patient to please leave a review on Google or Facebook about their experience. If they receive negative feedback, this feedback should be taken very seriously, and management should be notified as soon as possible so that the issue can be mitigated before the patient decides to post a negative review.
Setting up an automated text or email campaign that asks each patient for their feedback after their appointment is also a great way to improve your online reputation as well as to correct any issues that may be occurring at your practice. When you receive feedback from patients, you are then able to prompt them to leave a public review on Facebook, Google, Yelp, Healthgrades, or other applicable review platforms. However, you must be aware that legally, you are not allowed to only direct people with favorable feedback to leave reviews, which is known as review-gating – so if you are implementing an automated system like this, just make sure that you are aware of this limitation. There are online reputation management platforms which allow you to customize the messages that people see when they leave negative feedback as opposed to positive feedback, but both of those messages must still offer the option to leave a public review. However, if you create your message in such a way as to communicate to the patient who may leave negative feedback that you are working hard on resolving the issue and that someone will be in touch shortly, that may prevent them from leaving a public negative review.
When you receive a public review on Google, Facebook, or other review sites, make sure that you respond to it – either by thanking them for a good
review or by asking them to contact you to discuss how you can improve their experience. Do not argue or try to defend yourself online – try to speak about it with them privately, fix the issue, and ask them to remove the review if possible. When you receive great reviews, make sure to cross-share them on your various social media platforms. You should also create a “Reviews” page on your website and add all great reviews to this page. This instantly adds credibility to your website.

Finally, make sure that when you look over the feedback and reviews that you receive, you are paying attention to what the negative reviews are saying – this is a great opportunity to identify current process challenges and improve your patients’ experience at your practice. Need help managing your practice’s online reputation? Visit www.lms-plus.com to see how Leading Marketing Solutions can help.
Sonda Eunus is the CEO of Leading Marketing Solutions, a Marketing Agency working with Medical Practices and other Businesses to help them identify the best marketing strategies for their business, create a strong online presence, and automate their marketing processes for a better return on their Marketing budget. Learn more about Leading Marketing Solutions at www.lms-plus.com.

FLORIDA MD - JANUARY/FEBRUARY 2023 9 MARKETING YOUR PRACTICE
Social Media – Five Things Physicians Should Never Post
 By Julie A. Tyk, JD
By Julie A. Tyk, JD
As an example, Alaska dentist, Seth Lookhart, made national headlines for filming a video of himself riding a hoverboard while extracting a patient’s tooth. Dr. Lookhart filmed the procedure on a sedated patient without authorization and forwarded the video to several people. A lawsuit was filed by the State of Alaska in 2017 charging Dr. Lookhart with “unlawful dental acts”, saying his patient care did not meet professional standards. The lawsuit goes on to further allege Dr. Lookhart joked that performing oral surgery on a hoverboard was a “new standard of care,” citing phone records that were obtained. Dr. Lookhart has also been charged with medical assistance fraud for billing Medicaid for procedures that were not justified, unnecessary, and theft of $25,000 or more by diverting funds from Alaska Dental Arts. On Friday, January 17, 2020, Dr. Lookhart was convicted on 46 counts of felony medical assistance fraud, scheming to defraud, misdemeanor counts of illegally practicing dentistry and reckless endangerment. Dr. Lookhart was sentenced to serve 20 years with eight suspended, leaving 12 years of active time.
A doctor in Rhode Island was fired from a hospital and reprimanded by the state medical board. The hospital took away her privileges to work in the emergency room for posting information online about a trauma patient. The doctor’s post did not include the patient’s name, but she wrote enough that others in the community could identify the patient, according to a board filing.

The popularity of social media has exploded in recent years. According to a recent PEW report, 70% of Americans use social media. Before jumping on the bandwagon, healthcare professionals are advised to be mindful of the possible ramifications of posting information on social media sites. There are numerous legal issues that can arise when healthcare providers use social media, including issues related to patient privacy, fraud and abuse, tax-exempt status, and physician licensing. The Federation of State Medical Boards has issued the Model Guidelines for the Appropriate Use of Social Media and Social Networking in Medical Practice, which contains the “industry standards” for cyber security, online behavior, and patient privacy. Physicians should familiarize themselves with these guidelines.
Five things which physicians should never post to social media.
cial media to share any health information that could be linked to an individual patient, such as names, pictures, and physical descriptions, without the patient’s consent. The American College of Physicians recommends that doctors be especially aware of the implications for patient confidentiality when using social media. There have been cases of physicians losing their medical license after posting an image on social media that violated patient confidentiality. Always obtain permission from the patient in writing if you intend to use an image featuring any body part. Avoid talking about specific patients at all on social media unless you have permission to do so. Even if there is no chance that a patient could be identified by what you write on social media, it is considered un professional to discuss the specifics of their condition. Also be careful when taking photographs of yourself while in your practice. There have been cases where medical professionals have accidentally includ ed the image of the patient behind them while taking a ‘selfie’. Make sure there are no patient health records on display when taking photos in the medical practice and no patients are included in photographs unless they want to be.
3. Your Personal Information: The American College of Physicians (ACP) and the Federation of State Medical Boards (FSMB) recom mend that doctors create separate social media accounts for their pro fessional and personal lives. They also suggest that the professional profile be more visible than any personal one.
4. Opinions on Controversial Issues: Any controversial topic or “hot button” topic should be avoided as much as possible, including anything to do with religion, politics, racism, abortion, and gun control. Moreover, healthcare providers that are exempt from taxation under Section 501(c)(3) of the Internal Revenue Code are prohibited from intervening in political campaigns and from seeking to influence legislation as a substantial part of their activities. This restriction may extend to advertising on or sponsoring social media sites that support a political candidate or particular pieces of legislation.
1. Inaccurate Medical
Information:
Medical professionals should avoid republishing, sharing, “liking,” or “retweeting” news stories about medical treatments unless they have completely read the story and have verified its accuracy. If a user finds inaccurate medical information through your social media channel, it can reflect very poorly upon you and your practice. Healthcare professionals also need to be careful about providing medical advice to patients using social media. If a patient receiving the medical advice from a doctor through social media is located in a state in which the doctor is not licensed, the doctor giving the advice risks liability under state licensing laws.
2. Do Not Post Anything that Violates Patient Confidentiality: Friending patients on social media sites may pose risks under Health Insurance Portability and Accountability Act (HIPAA) and state privacy laws. The fact that an individual is a patient of a healthcare provider falls within the types of health information that these laws are designed to protect. As a rule, healthcare providers should not use so-
5. Complaints or Rants: It is unprofessional to use social media platforms to complain or rant about your professional situation. Everything you write on social media may one day come back to haunt you. A patient might realize that you were complaining about them on social media.
A medical malpractice claim can have far reaching implications. The Health Care Practice Group at Pearson Doyle Mohre and Pastis, LLP, is committed to assisting Clients in navigating and defending medical malpractice claims. For more information and assistance, please contact David Doyle and Julie Tyk at Pearson Doyle Mohre & Pastis, LLP.
Julie A. Tyk, JD, is a Partner with Pearson Doyle Mohre & Pastis, LLP. Julie concentrates her practice in medical practice defense litigation, insurance defense litigation and health care law. She has represented physicians, hospitals, ambulatory surgical centers, nurses and other health care providers across the state of Florida, and may be contacted by calling (407) 951-8523; jtyk@pdmplaw.com.
FLORIDA MD - JANUARY/FEBRUARY 2023 10 HEALTHCARE LAW
C M Y CM MY CY CMY K
CLOSE TO HOME EXPERTISE AT
ORLANDO REGIONAL MEDICAL CENTER.
When you choose Orlando Health, you choose board-certified expertise no matter which of our state-of-the-art facilities delivers your care. At Orlando Health - Orlando Regional Medical Center, the region’s only Level One Trauma Center, we deliver care and treatment in cardiology, orthopedics, neurology, oncology, digestive issues and more. For close to home expertise from Central Florida's most trusted team, choose Orlando Health.
ChooseOrlandoHealth.com/ORMC
CARE AT ORMC:
• Orlando Health Digestive Health Institute

• Orlando Health Heart & Vascular Institute
• Orlando Health Jewett Orthopedic Institute
• Orlando Health Neuroscience and Rehabilitation Institute
• Emergency Care • General/Robotic Surgery
• Warden Burn Center
FLORIDA MD - JANUARY/FEBRUARY 2023 11
My Chart N ow Avail able 100 Top Hospitals® is a registered trademark of IBM Watson Health™.
Chronic Thromboembolic Pulmonary Hypertension
By Daniel T. Layish, MD

There are several categories of pulmonary hypertension. WHO Group I includes patients with idiopathic pulmonary hypertension, familial pulmonary hypertension, drug and toxin related (fen-phen) portopulmonary hypertension, HIV related pulmonary hypertension and pulmonary arterial hypertension associated with connective tissue disorders (such as scleroderma). WHO Group II pulmonary hypertension is often referred to as pulmonary venous hypertension. This includes patients with left ventricular systolic or diastolic dysfunction or valvular heart disease. Essentially, the WHO Group II category includes patients who have an elevated pulmonary capillary wedge pressure and/ or elevated left ventricular end diastolic pressure. WHO Group III pulmonary hypertension consists of patients with COPD, interstitial lung disease, or other conditions in which hypoxia causes vasoconstriction. The remainder of this article will focus on WHO Group IV pulmonary hypertension (chronic thromboembolic pulmonary hypertension or CTEPH). Although WHO Group IV patients are relatively rare, it is crucial to identify them because this is the only type of pulmonary hypertension which is potentially surgically curable.
After acute pulmonary embolism, most patients will recover and have normal pulmonary hemodynamics, gas exchange, and exercise tolerance. It is believed that 1-4% of patients with acute pulmonary embolism will go on to develop CTEPH within two years. It is not clear why some patients with acute pulmonary embolism develop CTEPH. Risk factors include hypercoagulable states, myeloproliferative syndromes, splenectomy and chronic indwelling central venous catheters. Patients with CTEPH present with dyspnea, which can have a gradual onset. Many patients with CTEPH will not have a known previous diagnosis of acute pulmonary embolism. As with other patients with pulmonary hypertension, patients with CTEPH may not show findings on physical exam until pulmonary hypertension is in the late stages. Findings include a right ventricular lift, jugular venous distention, fixed splitting of the second heart sound, hepatomegaly, ascites, and peripheral edema. Patients with CTEPH may have “flow murmurs” heard over the lung fields because of turbulent flow through partially obstructed or recanalized pulmonary arteries. These tend to be accentuated during inspiration.
Acute pulmonary embolism is the trigger for CTEPH. In some patients this triggers a small vessel vasculopathy (for unclear reasons) that contributes to the extent of pulmonary hypertension. This may explain why up to 35 percent of patients who undergo succesful pulmonary thromoendarterectomy can have some degree of postoperative pulmonary hypertension.
Although VQ scanning has become less commonly used for diagnosis of acute pulmonary embolism this remains the initial imaging study of choice in patients with pulmonary hyperten-
sion to separate “small vessel” variants (Idiopathic pulmonary arterial hypertension) from “large vessel” disease (CTEPH) A normal VQ scan essentially excludes the diagnosis of CTEPH. A scan with one or more mismatched segmental defects is suggestive of the diagnosis. However, it is important to note that VQ scan can often understate the extent of central pulmonary vascular obstruction. Once the VQ scan is found to be abnormal then further testing should be undertaken (such as CT angiogram and/or pulmonary angiography). The angiographic findings in CTEPH are distinct from those of acute pulmonary embolism. They can include pouch defects and pulmonary artery webs. Patients with severe pulmonary hypertension have been found to tolerate performance of angiography as well as VQ scan without significant complication rate.
The surgery for CTEPH is quite different from surgical intervention for an acute pulmonary embolism. Surgery for CTEPH is called a pulmonary thromboendarterectomy (PTE), which requires median sternotomy and cardiopulmonary bypass. It requires an often tedious intimal dissection of fibrotic recannalized thrombus from the native pulmonary arterial wall. IVC filter placement is usually recommended before pulmonary thromboendarterectomy. These patients can have a complicated postoperative course and this type of surgery is only done at a few specialized centers in the country. The center which is best known for this type of surgery is the University of California (San Diego). Patients who have undergone PTE are typically maintained on lifelong anticoagulation. To be a candidate for this surgery, a patients must have central, surgically accesible chronic thromboemboli. A significant postoperative complication is pulmonary artery steal, which refers to redistribution of pulmonary arterial blood flow from well-perfused segments into the newly opened segments resulting in ventilation perfusion mismatch and hypoxia. This redistribution of flow resolves over time. Approximately, 30% of PTE patients can develop reperfusion pulmonary edema. The perioperative mortality of pulmonary thromboendarterectomy can be in the range of 2-3% in experienced centers. Outcome is clearly better in high voluime centers (more than fifty PTE surgeries/year). Approximately 5000 thromboendarterectomy procedures have been performed worldwide, 3000 at UCSD alone.
Surgery for CTEPH is clearly the best therapeutic option. However, there are some patients with CTEPH who are inoperable or who have persistent or recurrent pulmonary hypertension after undergoing pulmonary thromboendarterectomy. There is now a medical therapy available for these patients. Riociguat (Adempas) was approved by the FDA in October 2013. It is a member of a new class of compounds-soluble guanylate cyclase stimulators. In the multicenter study by Ghofrani et al that was published in the New England Journal of Medicine in July 2013,
FLORIDA MD - JANUARY/FEBRUARY 2023 12 PULMONARY AND SLEEP DISORDERS
261 patients were randomized prospectively to receive riociguat versus placebo. Riociguat was shown to significantly improve exercise capacity and pulmonary vascular resistance. Side effects include systemic hypotension. Prior smaller studies have also shown some benefits to medical therapy in CTEPH (inoperable or with post-operative PH) with oral agents such as bosentan and sildanefil, inhaled iloprost and subcutaneous treprostinil. Medical therapy has also been used as a “bridge” before PTE.
Although relatively rare, CTEPH is an important cause of PH since it is potentially curable with pulmonary endarterectomy. This surgery should only be performed in very experienced, specialized centers. PTE surgery should always be the treatment of choice for CTEPH. However, medical therapy can have a role as a bridge to PTE,in patients who are not surgical candidates or in those who have persistent pulmonary hypertension despite undergoing PTE.

I would like to express my gratitude to Dr. Peter Fedullo (University California San Diego) for his review of this manuscript and providing the photographs.

Daniel Layish, MD, graduated magna cum laude from Boston University Medical School in 1990. He then completed an Internal Medicine Residency at Barnes Hospital (Washington University) in St.Louis, Missouri and a Pulmonary/Critical Care/ Sleep Medicine Fellowship at Duke University in Durham, North Carolina. Since 1997, he has been a member of the Central Florida Pulmonary Group in Orlando. He serves as Co-director of the Adult Cystic Fibrosis Program in Orlando. He may be contacted at 407-841-1100 or by visiting www.cfpulmonary.com.

FLORIDA MD - JANUARY/FEBRUARY 2023 13 PULMONARY AND SLEEP DISORDERS
Example of chronic clots removed during pulmonary thromboendarterectomy.
Example of the large perfusion defects seen on V/Q scan in a patient with CTEPH.
Pulmonary angiogram showing lack of blood flow to the right middle lobe and the right lower lobe from CTEPH.
Clinical Trials For Children With Cancer
By: Ramamoorthy Nagasubramanian, MD

WHY DO CHILDHOOD CANCER CLINICAL TRIALS MATTER?
Simply put, clinical trials save lives. In fact, childhood cancer research and clinical trials have fueled one of the great success stories in modern medicine — a pediatric cancer survival rate of more than 80%. Despite these advances, cancer is still the leading cause of death by disease in children. What’s more, all childhood cancers combined receive only 4% of U.S. federal cancer research funding. We have more work to do.
HOW HAVE CLINICAL TRIALS IMPROVED CANCER CARE IN KIDS?
Treating cancer in kids is not the same as adults. We’re looking at not only treating the disease today, but also protecting children from treatment side effects for optimal development, health, and quality of life for decades to come. Pediatric cancer clinical trials have helped us develop safer, more effective treatments for kids and strategies to better manage symptoms and side effects. Thanks to advances in cancer clinical trials and research, a child with cancer today compared to even 10 years ago has a much different experience through treatment and beyond.
WHAT DO I NEED TO KNOW ABOUT CHILDHOOD CANCER CLINICAL TRIALS?
Clinical trials, which are available at leading pediatric cancer centers, offer a level of care that kids can’t get everywhere. One of the largest clinical trial networks is the Children’s Oncology Group (COG). Funded by the National Cancer Institute, and part of the larger National Clinical Trials Network, the COG involves more than 200 hospitals and research centers in the U.S. and abroad and offers more than 100 clinical trials. There are also other networks and consortiums related to specific cancers. Membership in groups like the COG is important because childhood cancer is so rare, and we can make a larger impact when we come together.
WHAT ARE THE TYPES AND PHASES OF CLINICAL TRIALS?
Clinical trials can test treatments, preventions, diagnostics and screenings, as well supportive care aimed at improving outcomes and quality of life. They also study how genes influence diseases and patterns of disease across groups of people. Phase 1 trials are smaller and are the first to study safety, dosage and delivery on human subjects. Phase 2 trials study effectiveness. Phase 3 trials are much larger and test if treatments work better or have fewer side effects than current best practices. The whole process can take 10 years or more.
WHY DO PARENTS OR GUARDIANS ENROLL CHILDREN IN CLINICAL TRIALS?
There are many reasons. For some, especially those with rare disease, clinical trials may provide the most advanced, latest care available. This can mean a better chance for kids to live and live longer, and why many choose to enroll in Phase 1 and 2 trials. Some participate for the close, constant health monitoring.
Others may participate for the potential for treatment cost savings.
WHAT ARE THE BARRIERS TO CHILDHOOD CANCER CLINICAL TRIAL ENROLLMENT?
Compared to adults, cancer in children is rare. About 16,000 children under age 20 are diagnosed with cancer in the U.S. each year. Sometimes, strict eligibility requirements mean fewer participants can enroll. Lack of awareness, finances, logistics and even cultural differences can also affect enrollment. Pediatric cancer centers with large clinical trial participation actively invest in resources to reduce these barriers, so that more kids can have a better chance to live.
HOW CAN I HELP?
Clinical trial enrollment directly affects outcomes for kids with cancer. The more children we can enroll, the faster we can advance promising treatments so that kids everywhere have access to lifesaving care. As a trusted care provider, you can help raise awareness about the importance, and particularly the availability, of childhood cancer clinical trials in our area. Talk to your parents about the benefits of participating and refer them to a pediatric cancer center with active involvement in large cancer research networks.
WHAT ARE WAYS TO IMPROVE OPPORTUNITIES FOR CLINICAL TRIALS?
It’s unacceptable that society’s most underserved children — from racial and ethnic minority groups — are more likely to die of childhood cancer than their non-minority peers due to lack of access to care. So, Nemours Children’s Health decided to do something about it.
To create a more equitable care environment for patients, we’ve worked intentionally to identify and minimize all barriers to research and clinical trial participation. To measure the impact of these efforts, our program tracks and reports weekly on three essential data elements:
1. Total clinical trial enrollments
2. Clinical trial enrollments across racial and ethnic groups and compared to population estimates, and
3. Screen failures (eligible but not enrolled) across racial and ethnic groups, as well as primary language spoken.
Our objective is to enroll all eligible patients in available clinical trials. We measure our program against national benchmarks published each year in the COG Report Card. What we’ve learned along the way is that by understanding the factors that contribute to underrepresentation in research and clinical trials, clinicians can create targeted strategies to increase engagement.
For example, by translating our research consent forms into different languages common in our catchment areas, we’ve elimi-
FLORIDA MD - JANUARY/FEBRUARY 2023 14 PEDIATRICS
Our Center for Cancer and Blood Disorders ranks second in the U.S. for accruals to pediatric clinical trials, enrolling patients on 291 trials in 2021.
Offering hundreds of cancer clinical trials each year, and we are among the national leaders in participation in symptom management and prevention research.
nated patient screening failures due to language barriers. This is especially relevant considering that half of our clinical trial enrollments identify as Hispanic or non-white, a significant proportion of whom required consent in a language other than English.
Today, the Nemours Children’s Center for Cancer and Blood Disorders boasts the nation’s second largest pediatric clinical trial program of its kind — and the largest in Florida. We’re one of only two pediatric programs nationwide to be recognized as a National Cancer Institute Community Oncology Research Program (NCORP)
Ramamoorthy Nagasubramanian, MD, is chief of Hematology/Oncology at Nemours Children’s Hospital, Florida. Dr. Naga has been caring for Nemours Children’s hematology/oncology patients since 2007. He did his early medical training in India at Apollo Hospitals. He moved to Chicago for a residency in pediatrics and completed a double fellowship in pediatric hematology/oncology and clinical pharmacology at University of Chicago hospitals. Dr. Naga is the principal investigator of clinical trials in pediatric cancer, sickle cell anemia and hemophilia. Call (407) 650-7715 or visit Nemours.org to find out more or schedule an appointment.
FLORIDA MD - JANUARY/FEBRUARY 2023 15 PEDIATRICS
44 51 51 60 67 75 84 96 97 112 140 156 195 231 273 291 296 Nemours Children’s Health
Cannabis Demonstrates Improvement in Opioid Addiction Outcomes
 By Michael Patterson, NHA, OTR/L, CEAS
By Michael Patterson, NHA, OTR/L, CEAS
Cannabis demonstrates improved treatment outcomes for people suffering from opioid addiction and reduced risk from accidental fentanyl exposure, according to research published in the December 2020 issue of the Drug and Alcoholic Dependence Journal. The link to the article is below.
Cannabis use is associated with reduced risk of exposure to fentanyl among people on opioid agonist therapy during a community-wide overdose crisis - ScienceDirect
The study was performed by University of British Columbia and BC Center on Substance Abuse (BCCSU). The study included 819 participants, with 53 percent either intentionally or accidentally using fentanyl despite being treated for opioid addiction with treatments like methadone or buprenorphine/naloxone. The researchers found that participants who had urine tests positive for THC were about 10% less likely to have fentanyl-positive urine which puts them at a lower risk for overdoing on the opioid.


Dr. Eugenia Socías, the study’s lead author and clinician-scientist at BCCSU, said the “findings suggest that cannabis could have a stabilizing impact for many patients on treatment, while also reducing the risk of overdose.”
Previous BCCSU research found that individuals on opioid agonist treatments, such as methadone, who reported using cannabis on a daily basis were 21% more likely to continue addiction treatment at six months than non-cannabis users, the report says. BCCSU is set to work with the Canadian Institutes of Health Research on further evaluating the role of cannabis as a potential adjunct therapy to opioid agonist treatments.
Canadian researchers have found that without access to and rapid expansion of take-home naloxone, overdose prevention services, and opioid analog treatments, the number of overdose deaths in B.C. would be 2.5 times higher than current levels; but patient retention on these medications remains a challenge despite more individuals with opioid-use disorder being connected to treatments, the report says.
ANALYSIS
This study provides positive data linking cannabis use with decreased effect of opiates. It helps validate cannabis as a viable treatment for opiate dependence.
This is extremely important because the US opioid crisis has picked up momentum under the distraction of the Coronavirus pandemic. Eighteen states and Washington, D.C. have reported a 10% increase in opioid related deaths from 2019 to 2020. According to Addictioncenter.com, drug overdoses rose 4.6% in 2020 to 70,890 cases in the USA.
In the US, more individual states are adding qualifying conditions for medical cannabis related to opiate dependency. Cannabis has never killed anyone in human history, and therefore safer than many prescription medications, including opiates. The more data we collect on the benefits of cannabis for opiate addiction, the more momentum is gained to push to recognize cannabis as a legal medicine under US federal law.
Michael Patterson NHA, OTR/L, CEAS is CEO of US Cannabis Pharmaceutical Research and Development LLC. (uscprd.com). Mr. Patterson is a healthcare executive with over 25 years experience in the following areas: Cannabis-Hemp investment, Law, Regulation, Compliance, Operations, and Management, Skilled Nursing, Pharmacy, Laboratory, Assisted Living, Home Healthcare, and Healthcare Analytics. Michael is a subject matter expert in the Global Cannabis and Hemp Industry with Gerson Lehrman Group (glg.it) and Guidepoint. Mr. Patterson is an editorial board member of the American Journal of Medical Cannabis, licensed Nursing Home Administrator, and licensed Occupational Therapist in 4 states..
FLORIDA MD - JANUARY/FEBRUARY 2023 16
www.floridamd.com
Osteoporosis in Menopause
By Jyothsna Bandaru, MD, FACP

INTRODUCTION:
Osteoporosis is a generalized skeletal disorder characterized by impaired bone strength, that increases the risk of fractures, most importantly of the spine and hip.

These and other osteoporosis- related fractures occur most commonly in the older postmenopausal women and are often lifealtering events; however, the bone loss leading to osteoporosis, is most marked during the menopause transition and early menopause.
Younger post-menopausal women with wrist fracture, who have osteopenia or normal BMD, are at increased risk for future fractures, even if they do not have osteoporosis at the time of fracture.
PATHOPHYSIOLOGY:
In adults, there is a constant change of bone tissue, through a process called bone remodeling, where old bone is resorbed (removed) by osteoclasts and replaced by new bone by osteoblasts.
In young healthy women, the resorption and formation components of bone remodeling are balanced; the amount of old bone resorbed is replaced with an almost equal amount of new bone. As a result, bone mass is usually quite stable in healthy premenopausal women.
However, at the time of menopause, in response to estrogen deficiency, bone resorption becomes more rapid exceeding the ability of osteoblasts to replace new bone, resulting in bone loss. The imbalance in remodeling continues into advanced age, when an additional deficit in osteoblast function limits the rate of additional bone formation.
As bone loss occurs in the trabecular component of bone, especially in the spine and ends of long bones, the once thick and numerous trabeculae become thinned and perforated and often completely resorbed, leaving empty spaces in the place where bone tissue existed. The imbalance in bone remodeling can be accentuated by very sedentary lifestyle, often resulting in increased bone loss in elderly inactive women.
DIAGNOSING OSTEOPOROSIS:

The measurement of BMD by dual energy X-ray absorptiom-
etry (DXA) is the principal clinical tool to assess skeletal health. T-scores are used to make the diagnosis of osteoporosis in postmenopausal women.
The Z-score has limited value in postmenopausal women but is the preferred method of expressing BMD values in premenopausal women.
WHO defines osteoporosis in postmenopausal women as a BMD T-score value of –2.5 or lower, at the lumbar, femoral neck or total hip by DXA testing, whereas T-score of –1 to –2.49 is considered as osteopenia.
The diagnosis of osteoporosis is made in premenopausal women who have BMD Z-score of –2.0 and a history of fragility fracture.
Other methods of bone mineral density assessment include quantitative CT, densitometric measurements of the heel or fingers, and noninvasive ultrasound measurements at several skeletal sites.
PREVALENCE:
Between 40%- 50% postmenopausal women experience an osteoporosis related fracture during their lifetimes.
Vertebral fractures are associated with acute and chronic pain, height loss, and deformity and adversely affected ambulation, pulmonary function, and ability to perform routine chores.
Fear of falling after having a fracture limits socialization and physical activity, contributing to the effect of fractures on development of frailty.
RISK FACTORS:
Advanced age
Thinness
BMD in healthy women is strongly correlated with body weight. So thin women have lower BMD compared to heavy women. Genetic differences - In general, US Asian women have lower BMD than white women, whereas BMD in black women is generally higher.
Smoking - Possible explanations include women who smoke are generally thinner, have earlier menopause and lower serum estra-
FLORIDA MD - JANUARY/FEBRUARY 2023 17
diol levels than nonsmokers.
History of fracture, prior fragility fracture
Low BMD
Age
Excessive alcohol intake
Parental history of hip fracture
Diseases and drugs – DM2, obesity, proton pump inhibitors
FRAX is the 10-year probability of hip fracture or major osteoporotic fracture (hip, proximal humerus, distal radius and symptomatic spine fractures). FRAX is appropriate for use in postmenopausal women aged 40 to 90 years.
INDICATION FOR BMD TESTING:
All postmenopausal women with medical causes of bone loss, hx fragility fracture, or age>= 65
CLINICAL EVALUATION OF WOMEN WITH OSTEOPOROSIS:
A complete medical evaluation, including a detailed history of other diseases and medications, previous fractures and family history, a thorough physical examination and routine laboratory testing should be performed in all patients with osteoporosis before initiating therapy.
MANAGEMENT OF OSTEOPOROSIS:
• Comprehensive fall prevention programs, including home safety, exercises to promote strength and balance, correcting visual impairment, and appropriate use of walking aids may reduce fall frequency but have not been shown to reduce fracture risk.
• Correcting the deficiencies of calcium and vitamin D.
• In otherwise healthy postmenopausal women, including those with osteoporosis, the average serum 25-OH D level is about 20ng/ml.
• In fall-prone elderly patients, who were losing weight, higher protein intake was associated with reduced fall frequency.
• Magnesium deficiency is uncommon in healthy patients with normal diets. Although providing magnesium supplements to patients with malabsorption may be warranted, routine magnesium supplementation cannot be recommended.
• In a small randomized clinical trial in postmenopausal women, adding vit K2 to risedronate had no effect on BMD or fractures.
• There is no compelling evidence for beneficial effects of boron, zinc, black cohosh, berberine, or dehydroepiandrosterone (DHEA) on bone density or fracture risk in postmenopausal women.
PHARMACOLOGIC THERAPY:
North American osteoporosis guidelines suggest treating the patients with low BMD with 10-year fracture probability of major osteoporosis fracture of 20% or more, or hip fracture risk of 3% or higher. No treatment “cures” osteoporosis.
The beneficial skeletal effects of most osteoporosis drugs wane
quickly on stopping treatment. Hence, long-term treatment is required for this chronic disorder.
Beginning estrogen more than 10 years beyond menopause is not recommended due to safety concerns on CV health. The beneficial skeletal effects of estrogen abate within a few months of stopping therapy. Switching from estrogen to alendronate (or other bisphosphonates or denosumab) prevents the rebound in remodeling and rapid bone loss.
Raloxifene is an option for younger postmenopausal women with osteoporosis at risk for vertebral fracture, but no concern for hip fracture, without risk factors for venous thrombosis, vasomotor symptoms, and with concerns on breast cancer risk.
The four drugs in the class of bisphosphonates (alendronate, risedronate, ibandronate, zoledronic acid) are aminobisphosphonates, which are more potent than the original bisphosphonates. Ibandronate reduced spine fracture risk, but no overall effect on nonvertebral or hip fracture risk.
Diffuse bone, muscle or joint pain of unknown mechanism are described with both oral and IV bisphosphonates.
Poor oral hygiene and invasive dental procedures are risk factors for osteonecrosis of the jaw (ONJ).
Patients on bisphosphonate therapy for more than 3 years should be cautioned to report new thigh or groin pain, so that appropriate radiology evaluation can be undertaken.
Bone mineral density in the hip region plateaus and then remains stable after about 5 years of bisphosphonate therapy. After 5 years of treatment in women at high fracture risk, switching to denosumab might result in additional gains in BMD.
Skin rash and infection occurred more frequently with denosumab than placebo.
As with stopping estrogen, switching to a bisphosphonate is suggested if denosumab therapy is stopped.
Because of possible association with increased cancer risk, nasal calcitonin is marketed with caution in American prescribing information.
Teriparatide is a recombinant 1-34 N-terminal fragment of PTH. Adverse events with teriparatide include transient hypercalciuria, hypercalcemia, dizziness, and muscle pain. Switching to a bisphosphonate or denosumab is advised to preserve or improve BMD, when stopping therapy.
Abaloparatide is a synthetic analog of parathyroid hormonerelated peptide (PTHrP). Both these agents carry a blackbox warning about potential risk of osteosarcoma due to studies in rats.
Monitoring renal function with bisphosphonate use and serum calcium with teriparatide use is suggested.
In summary, rapid bone loss which almost always occur in postmenopausal women can lead to osteoporosis and subsequently high fracture risk. The benefit-risk ratio for denosumab, bisphosphonates, raloxifene is very favorable during the first several years of therapy. Continued on page 20
FLORIDA MD - JANUARY/FEBRUARY 2023 18
Advancements in Digestive Health
By Shyam Varadarajulu, MD

The recently created Orlando Health Digestive Health Institute offers a comprehensive digestive disease program with areas of expertise including luminal gastroenterology, pancreatology, inflammatory bowel diseases, motility and hepatology. As president of the Orlando Health Digestive Health, I am excited about our new state-of-the-art facility in downtown Orlando, which will provide dedicated space to deliver care ranging from general GI procedures to subspecialized care for complex digestive disorders, as well as an opportunity to be at the leading edge of research with clinical trial that will bring innovation and treatment options not available elsewhere.
The new facility will house the Center for Advanced Endoscopy, Research and Education (CARE), featuring purpose-built space for advanced endoscopic services, together with the personnel and technical expertise needed for impactful clinical research and teaching. The dedicated area will be outfitted with the latest technologies to optimize clinical outcomes and maximize research productivity, including sophisticated endoscopic and fluoroscopic equipment, capability for artificial intelligence, and specific areas for observation and education.
SPECIALIZED POEM PROCEDURE
One of those advanced services is peroral endoscopic myotomy (POEM). This specialized endoscopic procedure addresses swallowing disorders such as achalasia, spastic esophageal conditions and esophagogastric junction outflow obstruction. Orlando Health is one of only five hospital systems in Florida to provide POEM treatment.
This advanced, minimally invasive therapeutic procedure to treat motility disorders of the esophagus is performed orally using high-definition upper endoscopes. This allows physicians to make mucosal incisions and subsequent submucosal tunneling to permanently relax tight esophageal muscles and open narrowed parts of the esophagus. No external cuts are required.
“POEM gives us a very controlled method of cutting from inside the esophageal cavity for solving these complex disorders in a safe, effective manner,” says Ji Young Bang, MD, a board-certified gastroenterologist and director of clinical research at the Orlando Health Digestive Health Institute Center for Advanced Endoscopy, Research & Education. An internationally recognized researcher in interventional endoscopy, Dr. Bang brings extensive experience in POEM to Orlando Health, having completed 150 of these procedures since 2017.
While POEM was developed specifically for one digestive disorder, it forms a foundation for other procedures like submucosal tunneling endoscopic resection (STER), endoscopic submucosal dissection and gastric peroral endoscopic myotomy (G-POEM). Each of these procedures differ slightly, but they are all a part of our arsenal of very advanced, complex endoscopy procedures that we can now offer to patients.
A STANDARDIZED TREATMENT APPROACH
As an example of our passion for effecting meaningful contributions to research, Orlando Health Digestive Health Institute physicians are among the authors of a recently published journal article highlighting results from a study involving a new protocol to help standardize treatment options and improve clinical outcomes for patients who require endoscopic drainage of pancreatic fluid collections (PFC).1
Results from a retrospective, observational study of prospectively collected data among patients with symptomatic PFCs demonstrated significantly higher rates of endoscopic treatment success in patients treated with a combination of lumen-apposing metal stents (LAMS) and selective plastic stents (the Orlando Protocol) versus those treated with plastic stents alone. Additionally, the need for rescue surgery was significantly higher in patients treated with plastic stents alone compared with those treated using the Orlando Protocol. These results promise to bring a much-needed measure of standardization to PFC treatment.
Traditionally, transluminal plastic stents have been placed to facilitate drainage in the endoscopic management of PFC. But today, LAMS are increasingly used instead of plastic stents, largely because of three distinct advantages LAMS offer: better drainage due to their larger diameter, less risk of peritoneal leakage and perforation due to their apposing nature, and technically easier stent deployment. Despite these advantages, there has been a lack of data validating the use of LAMS over plastic stents in patients with PFCs. By introducing a measure of standardization in PFC management, the Orlando Protocol can help to improve clinical outcomes in this complex group of patients.
Evidence supporting the Orlando Protocol is further strengthened by several additional considerations. These include significantly shorter procedural duration times for index interventions, which is an important advantage given the critically ill status of most patients, who likely cannot endure longer procedures. The Orlando Protocol also appears to be particularly useful for a subset of patients suffering from disconnected pancreatic duct syndrome, who have higher PFC recurrence rates. Utilizing the protocol can facilitate better drainage and reduce PFC recurrence in these patients, thereby reducing disease morbidity.
As one of the study authors, I can confidently state that this is the first time in the medical literature where a treatment protocol was validated prospectively for index interventions, reinterventions and follow-up, thereby standardizing the management approach outside of a clinical trial setting for patients with PFCs.
These are just two examples of the elevated level of services that the Orlando Health Digestive Institute will provide as a national and international destination for care.
References available by request
Continued on page 20
FLORIDA MD - JANUARY/FEBRUARY 2023 19
Continued from page 19
Shyam Varadarajulu, MD, is a board-certified gastroenterologist and president of the Orlando Health Digestive Health Institute. He specializes in advanced endoscopy for the treatment of complex digestive disorders at the institute’s Center for Advanced Endoscopy, R.esearch & Education. Dr. Varadarajulu is a sought-after researcher, educator and lecturer. He is widely published in peer-reviewed journals and reference textbooks, and is currently editor of the textbook ENDOSONOGRAPHY and a reviewer for more than 30 professional journals. After earning his medical degree at Madras Medical College in India, Dr. Varadarajulu completed his residency in internal medicine at St. Mary’s Hospital in Rochester, New York, followed by fellowships in gastroenterology at the University of Connecticut and advanced endoscopy at the Medical University of South Carolina.
Continued from page 18

Dr. Bandaru, MD FACP received her medical doctorate from Loyola Medicine Macneal Hospital, Illinois. She is trained in Internal Medicine and Primary Care and has experience working in community settings, treating adult patients with diverse pathology. She is passionate about Women’s Health.
With her intriguing experiences with postmenopausal women’s issues, she is looking forward to NAMS NCMP certification. She is a Member of the American College of Physicians (Florida Chapter). Dr. Bandaru has been honored with the prestigious Fellowship of the American College of Physicians (FACP) as an acknowledgment of her ongoing individual service and contributions to the practice of medicine.

FLORIDA MD - JANUARY/FEBRUARY 2023 20
EDITORIAL CALENDAR

Florida MD is a monthly medical/business digital magazine for physicians..
Florida MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD
It is hard to be aware of everything happening in the rapidly changing medical profession and doctors want to know more about new medical developments and technology, procedures, techniques, case studies, research, etc. in the different specialties. Especially when the information comes from a local physician specialist who they can call and discuss the column with or refer a patient. They also want to read about wealth management, financial issues, healthcare law, insurance issues and real estate opportunities. Again, they prefer it when that information comes from a local professional they can call and do business with. All advertisers have the opportunity to have a column or article related to their specialty or profession.
JANUARY – Digestive Disor ders
Diabetes
FEBRUARY – Car diology
Hear t Disease & Stroke
MARCH – Or thopaedics
Men’s Health
APRIL – Sur gery
Scoliosis
MAY –
Women’s Health
Advances in Cosmetic Sur gery
JUNE – Aller gies
Pulmonar y & Sleep Disorders
JULY – Neurology / Neuroscience
Advances in Rehabilitation
AUGUST – Spor ts Medicine
Robotic Sur gery
SEPTEMBER – Pediatrics & Advances in NICUs
Autism
OCTOBER – Cancer
Dermatology
NOVEMBER – Urology
Geriatric Medicine / Glaucoma
DECEMBER – Pain Management
Occupational Therapy
Please call 407.417.7400 for additional materials or information.
2023
Stroke rehabilitation— Life-changing results
For stroke survivors, rehabilitation can be one of the most important parts of recovery. Our hospital offers innovative, customized therapy programs to improve function and strength, getting patients back into the community for the activities they love most.
Learn more at ehc.rehab/floridamd

18
©2019:Encompass Health Corporation:1520729AHA 831 South State Road 434 Altamonte Springs, FL 32714 407.587.8600
The Joint Commission DiseaseSpecific Care Certification in Stroke Rehabilitation


















 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII



 By Julie A. Tyk, JD
By Julie A. Tyk, JD






 By Michael Patterson, NHA, OTR/L, CEAS
By Michael Patterson, NHA, OTR/L, CEAS










