

Lake Nona Hospital
the Standard for High-Quality, Patient-Centered Care
2023 •
I-4 CORRIDOR
UCF
Setting
MAY/JUNE
COVERING THE
The Best Nurses in Orlando.
choose well.
The only hospital in Orlando designated a Magnet Hospital for adult acute care by the American Nurses Credentialing Center (ANCC), Orlando Health
Orlando Regional Medical Center provides the highest level of emergency and specialty services provided by an expert and compassionate clinical team.
OrlandoHealth.com/ORMC

Since opening two years ago, UCF Lake Nona Hospital has lived up to the high expectations that were set for Lake Nona’s only full-service hospital. Created through a unique partnership between the University of Central Florida and HCA Healthcare, the nation’s most extensive health system, UCF Lake Nona Hospital has established a new standard of healthcare for the whole family.
The technologically advanced hospital has been growing faster than projected, running ahead of expectations in all areas. The medical staff has grown to more than 450 affiliated physicians, including specialists in primary care, cardiology, colorectal surgery, thoracic surgery, general surgery, gastroenterology, orthopedic surgery, pulmonology, nephrology, OB/ GYN, gynecological oncology, infectious disease, neuro health sciences, spine and urology.
Before the hospital began construction in 2018, no other facilities in the Lake Nona area were designed to serve the adult patient population: Nemours Children’s Hospital and Orlando VA Medical Center, the two primary hospitals in the area, provided care for children and veterans respectively. To serve the region’s unmet need, the UCF Lake Nona facility opened with 64 inpatient beds and a 20-bed emergency department, with ample capacity for expansion in future years.


FLORIDA MD - MAY/JUNE 2023 1 DEPARTMENTS 2 FROM THE PUBLISHER 8 DERMATOLOGY 9 MARKETING YOUR PRACTICE 10 PULMONARY AND SLEEP DISORDERS 12 PEDIATRICS 18 ORTHOPEDICS contents MAY/JUNE 2023 COVERING THE I-4 CORRIDOR 16 MIGRAINES ARE MUCH MORE THAN JUST HEADACHES 20 MITIGATING THE RISKS OF CERVICAL INSUFFICIENCY 4 COVER STORY
BY
PHOTO: PROVIDED
UCF LAKE NONA HOSPITAL
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
ON THE COVER: UCF Lake Nona Hospital
Iam pleased to bring you another issue of Florida MD. Mother’s Day is supposed to be one of happy times spent with family. Unfortunately, for some women and children in central Florida, home life is anything but happy. They suffer an existence fraught with domestic violence and mental and/or sexual abuse. Accordingly, I have asked Harbor House of Central Florida to inform us about some of the programs they have and some of the services they offer that bring healing and hope, to women and children who are trapped in abusive relationships or have suffered physical trauma. If you suspect that one of your patients may be a victim, please pass along the information discussed below. I hope you will join me in supporting Harbor House and the good work that they do to save women’s lives.
Best regards,
Donald B. Rauhofer Publisher


Domestic violence is a pattern of controlling behavior that may include physical, economic, emotional, psychological, cyber –amongst other forms of abuse – by an intimate partner or family member. It can happen to anyone of any race, age, sexual orientation, religion, or gender. Harbor House of Central Florida works to prevent and eliminate domestic violence in Orange County and the City of Orlando by providing lifesaving services to survivors, implementing best practices, and educating and engaging the community in a united front.
Since the inception of the domestic violence movement in the 1970s, Harbor House has been highly regarded as one of the most comprehensive programs, impacting the lives of more than 15,000 women, children and men annually. It’s also the only domestic violence organization in the region that includes an onsite kennel to ensure no family member is left behind in an abusive household. The Paws for Peace Kennel broke barriers for survivors and allows them to come into shelter with their pets.
Harbor House, Orange County’s only state certified domestic violence service provider, is mostly known for its temporary emergency shelter, however, its work is well outside of its campus walls. In addition to providing a safe shelter, Harbor House also provides a 24hour bilingual confidential crisis hotline, counseling, safety planning, legal advocacy, a pet shelter, support groups, youth programs – amongst many other services.
Last year, Harbor House offered nearly 104,500 services, provided nearly 31,000 community referrals, conducted 343 domestic violence trainings, and answered nearly 5,400 hotline calls. In 2021, these numbers are pacing higher as survivors are finding the courage to step forward for help and as our community continues to talk about this global epidemic.

As a healthcare professional and business leader, you can have a profound impact on the lives and wellbeing of your employees in the workplace, while reducing healthcare costs, absenteeism, and lost productivity due to stress and injuries from domestic abuse. As most of you know, most of the our community’s costs that result from domestic violence are related to medical expenses and are extremely draining on the healthcare system.
Harbor House works with local businesses throughout Central Florida to implement domestic abuse workplace safety policies, train employees and establish a company go-to person in the organization to be familiar with available resources.
For more information and to join Harbor House and community partners to eliminate domestic violence in our community, visit harborhousefl.com, call 407-886-2244, email info@harborhousefl.com, or contact via Facebook.
Harbor House Hotline: 407-886-2856 Statewide Domestic Violence Hotline: 800-500-1119
ADVERTISE IN FLORIDA MD
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
PREMIUM REPRINTS
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: John “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, John Meisenheimer, VII, MD, Benjamin Service, MD, Cole Douglas Greves, MD, Brian C. Kellogg, MD, Jaivir S. Rathore, M.D., Vaishnavi Sharma (M.B;B.S Candidate, England), Sonda Eunus, MHA
Art Director/Designer: Ana Espinosa Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762. Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2023 Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.
FLORIDA MD - MAY/JUNE 2023 FROM THE PUBLISHER 2
The ripple effects of better health.

Ten years on and we’re turning the tide for children.
Since opening one decade ago, Nemours Children’s Hospital, Florida has been part of a sea change in children’s health. Bringing unique programs to millions of central Florida families, providing innovative care to our region’s most medically challenged children, and ensuring a pipeline of pediatric providers across the state. While we celebrate how far we’ve come, it’s not even close to how far we’ll go to ensure every child’s world is a place for them to thrive.
Well Beyond Medicine Go well beyond at Nemours.org/Beyond
An Official Sponsor of the USTA National Campus
UCF Lake Nona Hospital – Setting the Standard for High-Quality, Patient-Centered Care
By Staff Writer
Since opening two years ago, UCF Lake Nona Hospital has lived up to the high expectations that were set for Lake Nona’s only full-service hospital. Created through a unique partnership between the University of Central Florida and HCA Healthcare, the nation’s most extensive health system, UCF Lake Nona Hospital has established a new standard of healthcare for the whole family.
The technologically advanced hospital has been growing faster than projected, running ahead of expectations in all areas. The medical staff has grown to more than 450 affiliated physicians, including specialists in primary care, cardiology, colorectal surgery, thoracic surgery, general surgery, gastroenterology, orthopedic surgery, pulmonology, nephrology, OB/GYN, gynecological oncology, infectious disease, neuro health sciences, spine and urology.
Before the hospital began construction in 2018, no other facilities in the Lake Nona area were designed to serve the adult patient population: Nemours Children’s Hospital and Orlando VA Medical Center, the two primary hospitals in the area, provided care for children and veterans respectively. To serve the re-
gion’s unmet need, the UCF Lake Nona facility opened with 64 inpatient beds and a 20-bed emergency department, with ample capacity for expansion in future years.
The hospital benefits from the expertise, clinical knowledge and practices available across HCA Florida Healthcare’s network of 50 hospitals, 570 affiliated sites of care, 11,000 physicians and 77,000 colleagues and over 7 million patient encounters annually.
Overall the HCA Healthcare network encompasses to 182 hospitals supported by approximately 2,300 ambulatory sites of care in 20 states and the United Kingdom.
This enterprise supports the physical, mental, professional and financial health of its 294,000 colleagues and invests in a variety of benefits and resources to help improve their overall well-being, so they can provide comprehensive and compassionate patientcentered care for the communities it serves.
In the two years since it began serving the Lake Nona community, UCF Lake Nona Hospital has earned high marks for quality patient satisfaction. Since opening in March 2021, hospital departments have consistently ranked among the nation’s top 10 percent in patient satisfaction scores. Currently the hospital’s surgical services department is ranked first out of all HCA Healthcare hospitals for patient experience, and in the 99th percentile in Press Ganey, the industry’s leading human experience platform.
“This feedback reflects the voices of our patients,” said Wendy H. Brandon, FACHE, CEO of UCF Lake Nona Hospital. “These high scores are simply unheard of in healthcare.”

INNOVATIVE AND AT THE FOREFRONT OF CHANGE
UCF Lake Nona Hospital is transforming medical care by providing some of the most advanced technological tools and procedures. Recently, the learning-focused hospital became HCA Healthcare’s first Care Transformation and Innovation Hub (CT&I) to change how care is delivered to meet today’s demand for better, more efficient, and more effective patient care.
“The uptick of demand for healthcare services, coupled with accelerated progress in the digital space, creates an opportunity to transform the way we deliver care for the ultimate benefit of our patients,” Brandon said. “The designation as an
FLORIDA MD - MAY/JUNE 2023 4 COVER STORY
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
Sheila O’Ben’s health improved significantly following surgery with Dr. Keith Kim at UCF Lake Nona Hospital. “When I look in the mirror, I just can’t believe it’s me,” she said.
Innovation Hub through HCA Healthcare is a great honor, and our team is ready for the challenge of taking the delivery of healthcare excellence to the next level.”
CT&I builds on HCA Healthcare’s legacy of innovation and aims to transform the future of patient-centered care. The CT&I team is working to identify, build and roll out new technology solutions and process innovations that will create better outcomes and experiences for care teams and patients.
The work being done is designed to enhance the patient experience, create more face time between providers and patients, and improve both quality and safety in the delivery of healthcare. CT&I also works alongside HCA Healthcare nurses to better understand current processes and help generate insights to inform future innovations.
FLORIDA’S ONLY LEED GOLD HOSPITAL

This spring UCF Lake Nona Hospital earned LEED Gold certification, the first and only hospital in Florida to achieve this green building designation. LEED (Leadership in Energy and Environmental Design), developed by the U.S. Green Building Council, (USGBC), is the most widely used green building rating system in the world and an international symbol of excellence.
“Sustainability is a growing priority and we are excited about this recognition by the USGBC,” Brandon said. “It’s a major milestone and testimony to the cumulative efforts and innovative work of our HCA Healthcare project team.”
The designation recognizes the hospital’s commitment to sustainable building products and energy-saving operations, including:
• Systems that reduce water use, including sinks, toilets and showers, that conserve 767,908 gallons of water per year –equivalent to nearly 6 million bottles of drinking water
• Native landscaping that reduces water consumption by nearly 600,000 gallons of water each year
• High efficiency LED lighting and other systems that save over 21% in annual energy costs, as compared to standard design and construction practices
• On-site recycling, recycled and sustainable building materials, and the fact that 75% of the building waste during the hospital’s construction was recycled
Through design, construction and operations practices that improve environmental and human health, LEED-certified buildings are helping to make the world more sustainable. In the U.S. alone, building account for almost 40% of national CO2 emissions, but LEED-certified buildings have 34 % lower CO2 emissions, consume 25% less energy and 11% less water, and have diverted more than 80 million tons of waste from landfills.
“This is an exceptional accomplishment for both UCF and HCA,” said Amy Pastor, USGBC Central Florida Board chair. “You are among the best and you will be known worldwide for this.”

“LEED was created to make the world a better place and revolutionize our buildings and communities by providing everyone with access to healthy, green and high performing buildings,” said Peter Templeton, president and CEO of USGBC. “UCF Lake Nona Hospital is a prime example of how the innovative work of project teams can create local solutions that contribute to making a global difference.”
CARING FOR FAMILIES FROM DAY ONE
In just two years since opening its state-of-the-art Family Birthing Unit, UCF Lake Nona Hospital has welcomed 2,000 babies to Lake Nona. Featuring modern, suite-style facilities, the new unit is designed to provide a more comfortable, supportive, and private experience for expecting parents and their families.
At the Family Birthing Unit, mothers can labor, deliver and recover in boutique specialty birthing suites, which come equipped with everything the family needs for a safe birth. The spacious rooms feature a range of amenities for patients and visitors, room service, WiFi, 55-inch smart TVs with streaming services, and space for one guest to stay overnight.
For overnight births and those requiring around-the-clock care, the Family Birthing Unit is staffed 24 hours a day and seven days a week by a dedicated obstetric team who can provide care until the patient’s personal physician arrives. Parents with specific birth preferences, including low-intervention births, can be accommodated as well.
As part of UCF Lake Nona Hospital’s commitment to supporting parents before, during and after a birth, the Family Birthing
FLORIDA MD - MAY/JUNE 2023 5 COVER STORY
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
On Earth Day U.S. Green Building Council’s Amy Pastor awarded UCF Lake Nona Hospital Florida’s only LEED Gold hospital certification. “You are among the best and you will be known worldwide for this,” she said.
Unit offers maternity, childbirth, breastfeeding and newborn care classes for the whole family, including siblings.
LIFE-CHANGING WEIGHT LOSS SURGERY
The hospital is also the site of life-changing care for bariatric patients who qualify for weight loss surgery. Sheila O’Ben went from 289 pounds to just 145 after undergoing gastric bypass surgery a year ago at UCF Lake Nona Hospital.
Obesity, characterized by a BMI of 30.0 or higher, is a common disease that impacts more than one in four adults statewide. This widespread public health risk is expected to become more prevalent over time, according to the Florida Department of Health.
Living with obesity can be limiting and isolating in daily life, and it can also lead to a range of related complications, such as joint pain, difficulty breathing, cholesterol problems, hypertension, sleep apnea and fatigue. Adults with obesity are at a higher risk for severe weight-related illnesses like type 2 diabetes, heart disease and cancer, as well as an increased risk of premature death.
Surgery is not a stand-alone treatment for obesity, and UCF Lake Nona Hospital’s bariatric team works collaboratively with the patient to select an appropriate treatment option based on health and lifestyle needs. As part of the treatment process, patients are screened for eligibility and counseled extensively about nutrition, exercise and supplementation requirements to ensure a safe procedure and a healthy recovery.
After visiting her primary care physician recently, O’Ben said her doctor couldn’t believe the change in her health. She has been able to discontinue multiple prescriptions, including cholesterol

and acid reflux medications, due to her successful weight loss.
“I’m doing fantastic and living a normal life. It’s awesome to see family members who haven’t seen me in a while. They have to look twice and barely recognize me,” she said.
LIFE-CHANGING AND TRANSFORMATIVE MEDICINE
The hospital has brought life-changing technological advancements to Central Florida for many patients. It was the first Orlando-area facility to offer MRI-guided focused ultrasound for the advanced treatment of essential tremor (ET).
Central Florida’s first focused ultrasound patient Patricia Hawley was one of the more than 10 million Americans (an estimated 3% of the population) who live with ET, making it the most common movement disorder in the nation. Her involuntary shaking posed substantial hurdles in the normal activities of her daily life. As a school teacher Hawley had lost the ability to write years earlier and was no longer able to keep her daily journal.
“For patients who qualify, MRI-guided focused ultrasound provides an incision-less treatment option, performed on an outpatient basis with short recovery time and often immediate results,” said Dr. Nizam Razack, a neurosurgeon at UCF Lake Nona Hospital who performs the procedure. “This procedure can help restore independence and provide relief for individuals suffering from debilitating and progressive tremors within hours of treatment.”
The procedure, which was approved by the FDA in 2016 and by the Centers for Medicare and Medicaid Services (CMS) in July 2020, presents minimal risks, making it a strong alternative to existing surgical treatment options. Lake Nona is home to a large population of older adults, who are at a higher risk of being diagnosed with ET or Parkinson’s tremor, and noninvasive treatment options such as focused ultrasound can significantly improve independence, ability and quality of life.
“I am so happy and cannot believe the difference! After 15 years, I can write again,” Hawley said.
Innovation in medicine is a driving principle for UCF Lake Nona Hospital, and another new advancement is needle knee arthroscopy. Pioneered by orthopedic surgeon Dr. Vonda Wright and other UCF Lake Nona Hospital orthopedic surgeons, this new technology uses imaging sensors, LED light and image management to allow patients a less invasive arthroscopic surgery, during which they can stay awake under local anesthesia.
“This technology allows the patient to be a partner in their medical care as they see their joints in real-time and understand the treatment, minimizing patient risk and optimizing recovery in musculoskeletal surgery,” said Dr. Wright. “Needle arthroscopy is a game changer using only small points of entry, no general anesthesia, very little pain medications, no need for opioids, the procedure leads to extremely rapid recovery.”
Shorter downtime, less scars and fast recovery means returning to normal activity sooner, and in some instances, patients walk out of the hospital following the procedure.
FLORIDA MD - MAY/JUNE 2023 6 COVER STORY
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
Above, essential tremor patient Patricia Hawley holds her pre- and post-operative, before/after writing samples. These images were taken two hours apart from the incisionless surgery, and Hawley left the hospital shortly after this outpatient procedure.
As the hospital begins its third year of caring for the Lake Nona community, its leader reflects with gratitude for all her team has accomplished together.

“It has been exciting to see UCF Lake Nona Hospital achieve the vision we all had from the beginning of the hospital of the future, delivering high-quality, patient-centered care with the latest technology,” Brandon said.
“A new era of healthcare has arrived, and I couldn’t be prouder of our colleagues who made it possible.”

FLORIDA MD - MAY/JUNE 2023 7 UCF LAKE NONA HOSPITAL SERVICES: 6700 LAKE NONA BOULEVARD ORLANDO, FL 32827 689-216-8000 HCAFloridaHealthcare.com/ UCFLakeNonaHospital NEPHROLOGY NEUROHEALTH SCIENCES ORTHOPEDICS PULMONOLOGY ROBOTIC SURGERY SPINE CARE UROLOGY WOMEN’S CARE ONCOLOGY FOCUSED ULTRASOUND CARDIOLOGY COLORECTAL SURGERY 24/7 EMERGENCY CARE GASTROENTEROLOGY GENERAL SURGERY GYNOCOLOGIC ONCOLOGY IMAGING INFECTIOUS DISEASE MATERNITY BARIATRICS
COVER STORY
HCA Healthcare’s legacy of innovation continues at UCF Lake Nona Hospital as CT&I teams identify, build and roll out solutions and process innovations to create better outcomes for patients and care teams.
PHOTO: PROVIDED BY UCF LAKE NONA HOSPITAL
Not All Basal Cell Carcinomas Are Created Equal


 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
Occasionally a patient will tell me their “doctor friend” recommended that they don’t need treatment for a basal cell carcinoma because it will never hurt you. “Doc, he said it’s only a basal cell carcinoma.” Dermatologists fully recognize this as a genuinely cringe-worthy statement. You don’t need to see too many people missing various parts of their facial anatomy to know this advice is blatantly wrong. Even in this modern time of medical miracles, people still die from neglected basal cell carcinomas. When pressed for the name of their “doctor friend,” it usually comes up as I don’t remember their name, or it ends up being “Doctor Google.”
It is true a superficial basal cell carcinoma on the torso probably would take years and years for it to cause any sort of significant morbidity to a patient. But, on the other hand, even a small basal cell on the torso will continue to grow if left untreated slowly. What might have been a simple, inexpensive procedure now, a decade later, has turned into a monster of aggravation, discomfort, and cost.
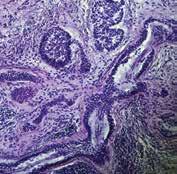
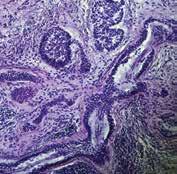
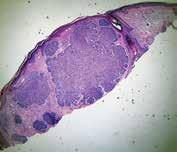
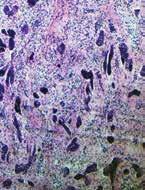
Although metastatic disease risk is low with basal cell carcinomas, it is certainly not zero. Several people die each year from basal cell carcinoma. Even more, patients can have disfiguring bouts with cancer losing various parts of anatomy such as nose, ears, eyes, etc. What a lot of patients and even some physicians are not aware of is that not all basal cell carcinomas are created equal. There are several different histologic growth patterns. These varying histologic types can each behave differently and require different treatment plans.
As mentioned before, a superficial basal cell carcinoma is probably not going to cause a great deal of physical damage unless neglected for long periods. There are other types of basal cell carcinomas; morpheaform and sclerosing basal cell carcinomas with infiltrating growth patterns. These cancers left untreated can cause a significant amount of morbidity in shorter periods measured in months, not years. Aggressive basal cell cancers can also become neurotropic, meaning that they “wrap” around a nerve and can track down its length. Neurotropism can be particularly dangerous, especially if this is on the face and affecting a nerve that happens to pass through a foramen into the brain. Clearly, not a good scenario.
Basal cell carcinomas, limited to the skin, tend to be very amenable to treatment in a variety of different ways. Even as a Mohs surgeon I can think of at least half a dozen different ways that I have treated basal cell carcinomas. Not all basal cell carcinomas need Mohs surgery. Each case of basal cell carcinoma should be evaluated individually and in consideration as to the best method of treatment based on its histologic growth pattern, location, and physical condition of the patient.
The great news about basal cell carcinoma, even though it is the most common type of skin cancer and millions are treated each year, only a tiny percentage of these end up causing death in patients. When someone says I would much rather have a basal cell carcinoma than a melanoma, there is a caveat; if you die from a basal cell carcinoma, you are just as dead as if you were to die from melanoma. Happily, most of the time, with early diagnosis and treatment, you don’t have to die from either. Basal cell carcinoma is called cancer for a reason. Give it its respect that it is due, or otherwise, you may regret saying, “oh, you don’t have to worry about it, it’s only a basal cell carcinoma.”
Lucky Meisenheimer, M.D. is a board-certified dermatologist specializing in Mohs Surgery. He is the director of the Meisenheimer Clinic – Dermatology and Mohs Surgery. John Meisenheimer, VII is a medical student at USF.

FLORIDA MD - MAY/JUNE 2023 8 DERMATOLOGY
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
Pathology of an infiltrative basal cell carcinoma.
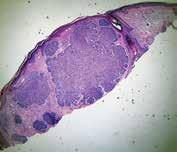
Infiltrative Basal Cell carcinoma of the forehead.
Superficial Multifocal BCC.
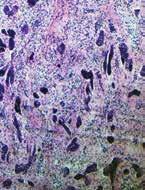
Nodular basal cell carcinoma.
Neurotropic basal cell carcinoma. Sclerosing basal cell carcinoma.
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
What Does Your Branding Say About Your Medical Practice?
By Sonda Eunus, MHA, CMPE
Your brand is the identity that you create for your practice. It is crucial to identify the core values that you want your brand to represent, because this is how it will be perceived by your target audience and the community at large.
Here are some questions to consider when building your brand:
• How do you want your practice to be perceived?
• What core values do you hold most important to your WHY?
• What does your brand look like? Colors, fonts, and shapes matter.
• What does your brand sound like?
When choosing your brand colors, be aware of the following color associations:
• Red — Red stands for passion, excitement, and anger. It can signify importance and command attention.
• Orange — Orange stands for playfulness, vitality, and friendliness. It is invigorating and evokes energy.
• Yellow — Yellow evokes happiness, youth, and optimism, but can also seem attention-grabbing or affordable.
• Green — Green evokes stability, prosperity, growth, and a connection to nature.
• Light Blue — A light shade of blue exudes tranquility, trust, openness. It can also signify innocence.
• Dark Blue — Dark blue stands for professionalism, security, and formality. It is mature and trustworthy.
• Purple — Purple can signify royalty, creativity, and luxury.
• Pink — Pink stands for femininity, youth, and innocence. It ranges from modern to luxurious.
• Brown — Brown creates a rugged, earthy, old-fashioned look or mood.
• White — White evokes cleanliness, virtue, health, or simplicity. It can range from affordable to high-end.
• Gray — Gray stands for neutrality. It can look subdued, classic, serious, mysterious, or mature.
• Black — Black evokes a powerful, sophisticated, edgy, luxurious, and modern feeling.
(www.99designs.com)
WHAT IS YOUR BRAND’S PERSONALITY?
Think of your Business brand as a person. What is this person’s personality like? How does he or she dress, talk, and act in public? Here are just a few examples of a personality that your brand
may have:
• Serious and Professional
• Warm and Friendly
• Cool and Quirky
• Funny and Playful
However, you choose to represent your brand, make sure that it is authentic to who you are. For example, if you are playful and like to crack jokes, infuse your marketing with humor and you will find that people respond positively to jokes, memes, and quotes that are applicable to them. For example, for pediatric practices, we have found that moms just can’t get enough of memes that make fun of their kids! You can add some (goodnatured) jokes and memes to your social media posts and you will see some great engagement.
Similarly, if you want your brand to be viewed as serious and professional, you will want to consistently share valuable and informative content that educates your audience. You can choose to do so by looking for speaking opportunities to help build credibility and position you as the expert in your field, making educational videos and sharing them on your website, Youtube, and social media, or by writing educational articles and contributing to reputable publications.
If you’re going for warm and friendly, you will want to be seen engaging with your social media followers, being active in Facebook groups and other online groups, hosting community events, supporting great causes, etc.
If cool and quirky is your thing, you want to stand out from your competitors. You can use some colors that are not typical for your industry, create and share some fun videos, such as “funny (HIPAA-compliant) things that patients say”, paint your waiting room to inspire awe upon arrival, etc.
Keep in mind that for any brand personality, it is important to keep it consistent across your website content, social media posts, marketing materials, and any other communication that you may have with your audience.
Sonda Eunus is the Co-Founder of Pro Medical Marketing – an Internet Marketing Agency specializing in Medical practices. She has a Masters’ in Healthcare Management and is a MGMA Certified Medical Practice Executive. She has been heavily involved in operating her family’s Pediatric practices from an early age. She is passionate about helping medical practices grow and does so by sharing her experience in her writing, speaking, and consulting. Learn more about Sonda and Pro Medical Marketing at www.promedicalmarketing.com.

FLORIDA MD - MAY/JUNE 2023 9
MARKETING YOUR PRACTICE
Idiopathic Pulmonary Fibrosis – Current Approach to Therapy
By Daniel T. Layish, MD

Idiopathic pulmonary fibrosis (IPF) is also known as usual interstitial pneumonitis (UIP). There are estimated to be 48,000 new diagnoses of IPF per year in the United States, with 40,000 deaths per year.
About two thirds of patients with IPF pass away within five years of diagnosis. For many years, combination therapy with prednisone and azathioprine had been used. However, the PANTHER trial revealed convincingly that combination therapy with prednisone and Imuran actually resulted in greater mortality, more hospitalizations, and more serious adverse events than placebo. Therefore, combination therapy with azathioprine and prednisone is no longer recommended. For a while, treatment of IPF had been essentially supportive including supplemental oxygen, pulmonary rehabilitation and vaccination against Streptococcus pneumoniae and influenza. Lung transplant can also be considered when appropriate.
Pirfenidone (Esbriet) is an antifibrotic agent, which has now been shown in several clinical trials to reduce disease progression and improve progression free survival in patients with IPF. Pirfenidone inhibits the synthesis of transforming growth factor Beta, which plays a role in cell proliferation and differentiation.
There have been two previous phase III trials of Pirfenidone that seem to have conflicting results. One study (published in 2010) showed that Pirfenidone slows disease progression while another study (published in 2011) did not meet its end point. However, this last study did have some trends that were in a positive direction; this resulted in the FDA requesting the “ Assessment of Pirfenidone to Confirm Efficacy and Safety in Idiopathic Pulmonary Fibrosis Study” (ASCEND). The result of this study was published in the New England Journal of Medicine. In the ASCEND study, 278 patients with IPF were randomized to receive Pirfenidone 2403 mg per day for 52 weeks. 277 patients were randomized to receive Placebo. The primary endpoint was forced vital capacity and secondary end points included 6-minute walk test distance, progression free survival, dyspnea, overall mortality and disease specific mortality.The proportion of patients who had an absolute reduction of at least 10% in predicted forced vital capacity (FVC) or who died was 47.9% less in the Pirfenidone group as compared to the Placebo group. In addition, the average decrease in FVC from baseline was lower in the Pirfenidone group versus the Placebo group (235 versus 428 mL). Furthermore, the proportion of patients who had no decline in FVC was 132% higher in the Pirfenidone group than in the Placebo group and there was also less decline in the 6-minute walk distance in the Pirfenidone group compared to the Placebo group as well as better progression free survival. However, there was no significant difference in dyspnea score and all cause mortality or disease specific mortality between the two groups.
There has been a pooled analysis of data from all three Pirfenidone trials, which revealed that the overall risk for death at 52 weeks was lower in the Pirfenidone group versus the placebo
group with a hazard ratio of 0.52. In this pooled analysis Pirfenidone improved both all cause mortality and disease specific mortality. The most common side effects included gastrointestinal and skin related adverse effects, but these rarely led to treatment discontinuation. Unfortunately, patients on Pirfenidone do not necessarily perceive improvement and Pirfenidone is certainly not a cure for this serious illness. Nevertheless, it appears to be a good option for slowing down the progression of this serious condition.
Another new option for treating UIP/IPF is Nintedanib (OFEV®) This is a tyrosine kinase inhibitor that targets growth factors including the vascular endothelial growth factor receptor, fibroblast growth factor receptor and platelet derived growth factor receptor. In May 2014, Luca Richeldi et al published the results of two 52 week randomized, double blind phase 3 studies of nintedanib (150 mg twice/day) versus placebo in the New England Journal of Medicine. 1066 patients were enrolled in a 3:2 randomization. The adjusted annual rate of change in FVC was negative 115 ml with Nintedanib versus negative 240 ml with placebo. Diarrhea occurred in over 60 percent of patients on Nintedanib but led to discontinuation in less than five percent.
The most frequent serious adverse reactions reported in patients treated with OFEV® (more than placebo), were bronchitis (1.2% vs. 0.8%) and myocardial infarction (1.5% vs. 0.4%). However, in the predefined category of major adverse cardiovascular events (MACE) including myocardial infarction, fatal events were reported in 0.6% of OFEV® treated patients and 1.8% of placebo-treated patients. Therefore, the clinician must weigh the risk/benefit ratio of using this medication in a patient with known coronary artery disease (or cardiovascular risk factors) carefully.
In conclusion, IPF/UIP is a relatively common and progressive pulmonary disorder. Pirfenidone and Nintedanib are two new agents that appear to slow down the progression of this disease. Further research needs to be done to identify agents that can reverse pulmonary fibrosis. Since Nintedanib and Pirfenidone seem to have similar efficacy, most clinicians choose one over the other based on side effect profile and dosing considerations.
References available upon request
Daniel Layish, MD, graduated magna cum laude from Boston University Medical School in 1990. He then completed an Internal Medicine Residency at Barnes Hospital (Washington University) in St.Louis, Missouri and a Pulmonary/Critical Care/Sleep Medicine Fellowship at Duke University in Durham, North Carolina. Since 1997, he has been a member of the Central Florida Pulmonary Group in Orlando. He serves as Co-director of the Adult Cystic Fibrosis Program in Orlando. He may be contacted at 407-841-1100 or by visiting www.cfpulmonary.com.
FLORIDA MD - MAY/JUNE 2023 10 PULMONARY AND SLEEP DISORDERS
The Natural Way to Solve your Allergy, Sinus and Respiratory Discomfort.

Relieve Symptoms of:
• Acne
• Allergies
• Asthma
• Cold & Flu
• Cystic Fibrosis
• Dermatitis
• Ear Infections

• Eczema
• Sinusitis
100% NATURAL TREATMENT

Kerri and Clay: “My son’s allergy medicines were causing terrible side effects. Now that we have been coming to The Salt Room we have been able to control his symptoms with salt therapy.”




Jessica L.:
looked and felt better after just one session. His cough wasn’t as bad. I felt he could breathe so much better.”
Joseph Cannizzaro, MD: “I have been recommending The Salt Room for years. It has helped my patients with respiratory nuisances and skin problems, reducing symptoms while we address the root cause to improve their long-term quality of life.”

FLORIDA MD - MAY/JUNE 2023 11
::
GIFT CERTIFICATES ARE AVAILABLE FUSION OF SCIENCE & NATURE
DRUG FREE
407.862.1163 l 357 Wekiva Springs Rd., Longwood l www.SaltRoomLongwood.com Located inside Cannizzaro Integrative Pediatric Center. Offering relief to all ages. ANTI-BACTERIAL | SIDE EFFECT FREE | ANTI-INFLAMMATORY
“My son
22q11.2 Deletion Syndrome
By Brian C. Kellogg, MD, Chief of Plastic and Craniofacial Surgery, Nemours Children’s Health

Q: WHAT IS 22Q11.2 DELETION SYNDROME?
A: 22q11.2 deletion syndrome (22qDS) is a common microdeletion disorder of variable expressivity that results in multi-organ system dysfunction. Patients may present with heterogenous combinations of cardiac anomalies, genitourinary anomalies, endocrinopathies, immunodeficiencies, overt or submucous cleft palate, velopharyngeal dysfunction (hypernasal speech), hematologic problems, gastrointestinal problems, developmental delays, neuropsychiatric illness and characteristic facial features. Several previously described disorders, including DiGeorge syndrome, velocardiofacial syndrome, conotruncal anomaly face syndrome, Opitz G/BBB syndrome and Cayler cardiofacial syndrome, are now recognized as different manifestations of 22qDS. The incidence of 22qDS is estimated to be around 1 in 4,000. It is the second most common cause (behind Down syndrome) of congenital heart disease and developmental delays, and it is the most common genetic cause of structural anomalies of the palate.
Q: WHAT CAUSES 22QDS?
A: 22qDS is caused by a microdeletion on the long (q) arm of the 22nd chromosome. It has an autosomal dominant inheritance pattern with variable expressivity, but 90-95% of cases are believed to result from de novo mutations. 22qDS has not been linked to any extrinsic or environmental factors during fetal development.
Q: WHAT ARE THE SIGNS AND SYMPTOMS OF 22QDS?
A: Congenital heart anomalies are often the earliest sign that a patient may have 22qDS. Further investigation into other organsystems and genetic testing can confirm the diagnosis. Other patients may escape diagnosis in the neonatal period only to present to a specialist later in life with very specific complaints, such as hypernasal speech. Specific signs and symptoms affecting different organ-systems that may be present include:
General: 22q facies (short forehead, hooded eyelids, upslanting palpebral fissures, prominent ears, malar flatness, bulbous nasal tip, small nasal alae, generalized hypotonia, multiple congenital anomalies, polyhydramnios, learning disabilities
Cardiac: Any congenital heart anomaly, especially conotruncal (tetralogy of Fallot, truncus arteriosus, interrupted aortic arch, transposition of the great vessels, etc.)
Endocrine: Hypoparathyroidism, hypocalcemia, growth hormone deficiency, hypothyroidism
Palate: Submucous cleft palate, overt cleft palate, high-pitched cry, nasal regurgitation, recurrent otitis media, hearing loss, hypernasal speech (velopharyngeal dysfunction)
Hematologic: Intrinsic platelet dysfunction, thrombocytopenia, easy bleeding, splenomegaly
Immunologic: Humoral and cell-mediated immunodeficiencies, may manifest as recurrent infections
GI: GERD, dysmotility/dysphagia, cholelithiasis, imperforate anus,
malrotation, Hirschprung’s disease
Genitourinary: Any structural GU anomaly, unilateral renal agenesis, multicystic dysplastic kidneys
Skeletal: Scoliosis, C-spine anomalies
Development: Failure to thrive, short stature, expressive and receptive language delays, gross motor delays, learning disabilities
Neuropsych: Attention deficit or autism spectrum in young children, anxiety or depression, schizophrenia or other psychotic disorders in teens/adults
Q: HOW IS 22QDS DIAGNOSED?
A: Genetic testing is required to confirm the diagnosis. Fluorescent in situ hybridization (FISH) or chromosomal microarray are two commonly employed modalities.
Q: HOW IS 22QDS TREATED?
A: Patients require a multitude of tests at the time of diagnosis. Per care guidelines, many of these assessments must be repeated at regular intervals. For example, children with 22qDS only require an immunologic evaluation at the time of diagnosis and once again in preschool years (unless specific concerns arise). However, guidelines recommend thyroid studies annually.
Due to the multi-system nature of 22qDS, these patients are most effectively managed in the setting of an interdisciplinary team experienced in treating patients with 22qDS and wellversed in the care guidelines. Care coordination is crucial when working with children with 22qDS because of the large number of specialists who are involved and the complexity of the child’s care. Studies have shown that interdisciplinary team care leads to significantly improved adherence to care guidelines.
Q: WHAT ARE THE OUTCOMES FOR CHILDREN WITH 22QDS?
A: Outcomes for children with 22qDS are highly variable based on the systems involved and the degree to which they are affected. 22qDS can affect any system of the body, which is why early detection and treatment is so important. While there is no cure for 22qDS, therapies and medical interventions can help address its associated symptoms.
There is still very little information available for this population. Most 22qDS clinics are housed in pediatric institutions, so a transition to adult care should be carefully planned as these patients near adulthood.
Brian C. Kellogg, MD, serves as the chief of plastic and craniofacial surgery as well as the director of the Cleft Lip and Palate Program at Nemours Children’s Health. He completed a fellowship in pediatric plastic and craniofacial surgery at Nationwide Children’s Hospital after an integrated residency in plasticsurgeryatUniversityofSouthFlorida.Dr.Kelloggearnedhis medical degree at University of Cincinnati College of Medicine.
FLORIDA MD - MAY/JUNE 2023 12
PEDIATRICS



FLORIDA MD - MAY/JUNE 2023 13 GIVE HELP Volunteer • Donate • Learn More Harbor House provides safe shelter, legal advocacy, injunctions, relocation assistance and hope. HELP YOUR PATIENTS Do you see patients whose partners physically harm, insult, threaten or verbally abuse them? Help is Here. Download our free app RECOGNIZE | RESPOND | REFER H.I.T.S. tool is included to identify if your patient is experiencing domestic abuse Visit HarborHouseFL.com • Call 407-886-2244 CONNECT WITH US 24-HOUR HOTLINE: 40 7- 88 6 - 28 5 6 • STATEWIDE: 1-800-50 0 -1119 www.HarborHouseFL.com
Pulmonary Rehabilitation
By Daniel T. Layish, MD, FACP, FCCP, FAASM


Pulmonary rehabilitation can benefit patients with a wide variety of lung diseases including COPD, pulmonary fibrosis, cystic fibrosis, and sarcoidosis (among other chronic respiratory illnesses). Pulmonary rehabilitation does not replace standard medical and/or surgical treatments for these lung diseases. Rather, it supplements and complements standard therapy.
Patients with COPD (and other chronic lung diseases) develop shortness of breath with activity. This leads to the tendency to avoid activity, which in turn leads to deconditioning. It is felt that one of the main benefits of pulmonary rehabilitation is to break the cycle of deconditioning. Pulmonary rehabilitation programs typically include two or three outpatient sessions per week for 10 to 12 weeks. Typically, a pulmonary rehab program will include aerobic exercise, strength training, patient education in management of lung disease - including nutrition, energy conservation, medication compliance, bronchial hygiene, and breathing strategies. The component of group support is also felt to be a significant contributor to the success of these programs. The group support motivates the patient to attend the pulmonary rehab sessions. It also allows the patient to realize that there are other people suffering from chronic respiratory illness and to see how they are able to overcome these obstacles. Pulmonary rehabilitation is considered to be critical both before and after lung transplantation. Occasionally, a patient will have such a significant functional and symptomatic improvement after pulmonary rehab that transplant can be delayed.
Pulmonary rehabilitation programs are typically multidisciplinary in nature and may include a respiratory therapist, registered nurse, exercise physiologist, nutritionist, physical and/ or occupational therapists. The staff is trained to encourage the patient’s self management and coach them to adopt healthier habits through lifestyle modification. To enroll in a pulmonary rehabilitation program requires a medical referral. Pulmonary rehabilitation is covered by most third party payors. Pulmonary rehabilitation is appropriate for any stable patient with a chronic lung disease who is disabled by respiratory symptoms.
The pulmonary rehab program should involve assessment of the patient’s individual needs and creation of a treatment plan that incorporates realistic goals tailored to each patient. Evidence based analysis consistently reveals improvement in health related quality of life after pulmonary rehabilitation as well as improved exercise tolerance. Pulmonary rehabilitation has been shown to improve the symptom of dyspnea and increase the ability to perform activities of daily living. Pulmonary rehabilitation has also been shown to reduce health care utilization (including frequency of hospitalization) and decreases length of stay (when hospitalization is required). Pulmonary rehabilitation has not been demonstrated to improve survival.
The benefit from a pulmonary rehabilitation program may decline over time if the individual does not maintain their con-
ditioning. Some pulmonary rehabilitation programs will therefore include a “graduate” or maintenance program after the patient finishes the initial program.
Patients who develop shortness of breath often become anxious which in turn exacerbates the sensation of dyspnea and this can become a vicious cycle. Pulmonary rehabilitation can be very helpful in addressing this problem. Sometimes pulmonary rehabilitation will require supplemental oxygen with exercise. Although the strongest evidence regarding pulmonary rehabilitation programs is in the setting of COPD, it has been shown to be beneficial in a variety of disease states. Pulmonary rehabilitation has been shown to be a cost effective tool in the fight against chronic lung disease. It is currently felt to be underutilized.
Daniel Layish, MD, graduated magna cum laude from Boston University Medical School in 1990. He then completed an Internal Medicine Residency at Barnes Hospital (Washington University) in St.Louis, Missouri and a Pulmonary/Critical Care/Sleep Medicine Fellowship at Duke University in Durham, North Carolina. Since 1997, he has been a member of the Central Florida Pulmonary Group in Orlando. He serves as Co-director of the Adult Cystic Fibrosis Program in Orlando. He may be contacted at 407841-1100 or by visiting www.cfpulmonary.com.
FLORIDA MD - MAY/JUNE 2023 14
PULMONARY AND SLEEP DISORDERS
NeuLine Health is a neurodiagnostic services provider that performs convenient, at-home Ambulatory EEG testing for patients with neurological-related medical conditions.

We are dedicated to serving qualified healthcare providers and their patients with best-in-class neurodiagnostic testing, nationwide.
03
Scheduling
NeuLine Health is fast and convenient, leading to faster answers on the next steps in your treatment.
FLORIDA MD - MAY/JUNE 2023 15 Visit neulinehealth.com/providers or call (844) 212-5321 to learn more.
CLINICAL CARE
THE COMFORT
HOME In-home testing puts the mind at ease, leading to a more accurate picture of neurological activity.
Convenience & Comfort Testing through NeuLine Health typically costs 3X less than inpatient care.
Affordability
THE BEST EEG
FROM
OF
01
02
with
Rapid Results
Migraines Are Much More Than Just Headaches! A Comprehensive Review On The Occasion of Migraine Awareness Month of June
By Jaivir S. Rathore, MD, FAES & Vaishnavi Sharma (MBBS Candidate, Hull York Medical School, UK)


WHAT IS A MIGRAINE?
A migraine is a complex neurological disease, not “just a headache” that has a significant impact on the lives of those that suffer from it. The pain is caused by the activation of nerve fibers within the wall of brain blood vessels traveling inside the meninges. It is recognized as the leading cause of years lived with disability in people under the age of 50 years. It directly affects more than 1 billion people worldwide and is the 3rd most prevalent disease and has a massive socioeconomic impact. Migraines are three times more common in women than men but are equally disabling in both genders and is the second leading cause of disability worldwide. Migraine often starts at puberty and mostly affects adults in their productive years but can also affect children and the elderly. It affects someone in nearly 1 in 4 American households, with an estimated 40 million people suffering from migraine headaches. Those with migraine have 2-3 times the rate of depression, 5 times the rate of anxiety and 2.5 times the rate of suicide when compared to the general population.
A migraine is usually a throbbing pain on one side of the head lasting 4 to 72 hours. Associated features include sensitivity to light or sound, nausea, vomiting, dizziness etc. Visual disturbances such as kaleidoscopic flashing colors or “squiggly or zigzag lines” may be present as well. There are several types of migraines including migraine with or without aura or even without a headache (acephalgic migraine). About 15% of the worldwide population suffers from some type of migraine. Migraine and chronic headaches are the second highest cause of short-term absence for non-manual employees and amongst the five top reasons for patient visits to the emergency department.
WHAT CAUSES MIGRAINES?
The pathophysiology of migraine is explained by cortical and subcortical spreading depression (CSD) which is an electrophysiological phenomenon of spreading wave of hyper-excitation (spreading depolarisation) across the brain’s surface followed by a period of reduced blood-flow (hypoperfusion) and suppressed neural activity (spreading depression). The aura phase that precedes migraine headache in about 20–30% of migraineurs may be a direct consequence of the events of CSD. Some studies have shown sub cortical spreading depression may be the basis for neuroanatomical and functional (central hypersensitivity) changes observed in migraine patients. The mechanism of CSD involves complex molecular changes in cortical upregulation of genes involved in inflammatory processing (e.g. for cyclooxygenase-2, tumor necrosis factor-α, interleukin-1β, galanin, or metalloproteinases). Metalloproteinase activation produces leakage of the blood–brain barrier, which leads to the release of a variety of molecules (e.g. potassium,
nitric oxide, adenosine) that may then sensitize the dural perivascular trigeminal afferents. CSD is reported to activate dural nociceptors; specifically, migraine with aura is initiated by waves of CSD that lead to delayed activation of the trigeminovascular pathway, thus linking a central event with peripheral nociceptive pathways. It is known that genetics and environmental factors play a role. Current cutting-edge research is investigating the role of serotonin and calcitonin gene related peptide (CGRP) in migraines.
ARE THERE TRIGGERS FOR MIGRAINES?
Absolutely! Migraines have a number of triggers. Hormonal changes in women such as fluctuations in estrogen, hormonal medications such as the combined oral contraceptives, drinks including alcohol and those containing excessive caffeine, sensory stimuli such as bright or flashing lights, loud noise and strong smells or even lack of sleep or hunger can trigger migraines. Other triggers include stress, increased physical activity, sudden weather changes, foods such as aged cheeses and salty processed food and food additives such as the sweetener aspartame and the preservative monosodium glutamate (MSG). Risk factors that make individuals more at risk of migraines include a family history of migraines and female sex.
WHAT ARE THE EARLY SIGNS OF A MIGRAINE?
The early signs of a migraine can differ amongst different individuals. In-fact, some patients can experience no warning signs. Common symptoms occurring days to hours before a migraine include an aura, fatigue, neck stiffness, food cravings or changes in appetite, increased urge to urinate and increased thirst. A migraine aura can present in many different ways including visual phenomena such as seeing bright lights, temporary vision loss, pins and needles sensation in limbs, weakness or numbness in certain areas of the body (hemiplegic migraine) and difficulty speaking. Mood changes such as irritability, sadness or excitement can also occur prior to a migraine.
HOW DOES A MIGRAINE PROGRESS?
After the early signs as noted above, patients may experience the phase characterized by one sided throbbing or pounding headache with associated symptoms including nausea, vomiting, sensitivity to light and sound and dizziness. This phase is variable in duration lasting from a couple of hours to multiple days (status migrainosus if 72 hours or more). The final phase occurs after the
FLORIDA MD - MAY/JUNE 2023 16
headache has receded. Patients may suffer from fatigue, poor concentration and mood fluctuations during this period.
WHAT MIMICS MIGRAINES?
Tension headaches can be mistaken for migraines. They feature a dull ache that is bilateral and is characteristically a band-like pressure around the head. They do not have an aura like migraines and a migraine is usually not a bilateral headache, at least to begin with.
Cluster headaches are another type of headache that can be mistaken for a migraine. The pain is incredibly severe in a cluster headache and patients often describe this as the worst headache of their life. The pain typically occurs around the eye. There is redness, swelling and lacrimation.
Sinus headaches are headaches that occur due to inflammation of the mucous membranes of the paranasal sinuses and usually coincide with infections or a history of sinus problems. This typically presents with frontal pressure pain which is worse on bending forward.
HOW DO YOU DIAGNOSE MIGRAINES?
The diagnosis of migraine is mostly clinical based on history and examination. Patients are asked about the onset and duration of the migraine, whether it is recurring, aura symptoms and any triggers for the migraine amongst other questions. Not every case of migraine needs a brain imaging but in certain cases, especially atypical ones and if there are focal neurological findings on exam, a MRI Brain may be considered. Additionally, patients are advised to maintain a headache diary where they can keep a record of the frequency, length, severity and any triggers of the headache. A headache diary can help healthcare professionals with making a diagnosis and its treatment plan.
HOW DO YOU TREAT MIGRAINES?
While there is no cure for migraines, there are several ways to manage its symptoms and reduce its intensity, frequency and associated suffering to improve the quality of life of the patients. Medications for migraines are divided into two categories including pain relieving rescue or abortive medications and preventive medications. Rescue or abortive medications includes NSAIDs (nonsteroidal anti-inflammatory drugs), triptans, opioids, oral calcitonin gene-related peptide receptor antagonist and anti-nausea drugs amongst others. Preventive medications include beta blockers, calcium channel blockers, antidepressants, anti-seizure drugs, botox injections and CGRP monoclonal antibodies. Lifestyle changes such as relaxation
techniques, developing a sleeping and eating routine, staying hydrated and exercising regularly can help control symptoms. Magnesium, manganese, vitamin B complex etc supplements are also helpful in prevention of migraines.
Botox therapy once every 3 months can reduce the frequency and intensity of migraines. Cutting edge research demonstrates that monoclonal antibodies targeting the CGRP protein, receptor and/or ligand can be effective for migraine prophylaxis as well as treatment of acute headache episodes.



Courtesy sources: American migraine foundation, International headache society, Science direct Mayo Clinic, Pubmed/NCBI/NIH and JAMA network.
Dr. Jaivir Rathore, a triple board-certified toprated neurologist trained at the Johns Hopkins and the Cleveland Clinic, Harvard University journal published neuroscientist and the Medical Director of Falcon Advanced Neurology & Epilepsy Freedom Center (FANEFC) in Orlando FL with additional clinics serving the largest retirement community of the world in The Villages FL provides comprehensive neurology care including chronic and episodic migraines. FANEFC is “Care Connected” with the Mayo Clinic, Jacksonville FL for surgical cases.
FLORIDA MD - MAY/JUNE 2023 17
IMAGE COURTESY: HTTPS://AMERICANMIGRAINEFOUNDATION.ORG/RESOURCE-LIBRARY/BOTOX-FOR-MIGRAINE/ MAGE COURTESY: HTTPS://WWW.SCIENCEDIRECT.COM/SCIENCE/ARTICLE/PII/ S1555415519302776
Augmented Reality, Mixed Reality, Virtual Reality, and the Future of Surgery: What type of headset will my surgeon wear in the operating room?
 By Benjamin Service, MD
By Benjamin Service, MD
The future of surgery will be filled with new technology and innovations with the goal of helping patients achieve better and safer outcomes. Multiple companies are pioneering the use of specialized tools, including mixed reality headsets during surgery. This is not just the future of surgery—it is the cutting edge of surgical care today! Additionally, virtual reality goggles are being used in disruptive ways to help medical students, residents, and surgeons train for surgery with complex, immersive simulations. This type of technology is transformative for how we approach not only medical education but also the entire surgical field.
Before diving into applications of these disruptive innovations, let’s get on the same page about what we’re talking about. Big picture: there are three types of “reality” that have subtle but important differences.
1. Augmented reality is when digital information is overlaid onto real objects or places in the world. The idea is that the digital information enhances the user experience to make it more engaging and memorable. Augmented reality can use a heads-up display or more frequently use a device like a cell phone to see the digital content. This type of technology, also called AR, has been used for popular cell phone games such as Pokémon™ GO and can change the way we perceive normal or objects in the real world with digital overlays. Using AR apps can be fun and very useful!
2. Mixed reality (MR) applications are like augmented reality, however, there is an opportunity to connect the digital and real world with mixed reality. When using mixed reality, the user wears a special type of goggles with a heads-up display that places the digital objects into the real world. Unlike AR, mixed reality allows you to interact with those objects. In the case of surgery, you can interact with x-rays or surgical tools. The ability to interact with both the digital and real world will have many applications in surgery. Mixed reality is actively being used by surgeons in the operating room in 2023. Using a MR headset is something like stepping “inside” of a computer. Three-dimensional anatomy is even more compelling when I can literally reach out with my hand and (digitally) touch and move the shoulder replacement in the operating room.
3. Virtual reality, also called VR, is very different. The entire experience is digital without a focus on connection to the real world. For VR experiences, the user wears a pair of “goggles” that you can’t see through–all you see are 2 small screens that show a single virtual and completely digital experience. VR can be extremely immersive. Imagine being inside of a movie where you can interact with objects in that movie, drive a car, pick up tools, or even do surgery. VR is currently being used as a training and
educational tool for high-risk situations. For example, VR is being used to help surgeons and trainees learn about surgical procedures without any risk of harm to patients and can be done anywhere, anytime. Future applications of virtual reality may be used in a variety of ways for surgeons, residents, and patients too.
Surgeons at the Orlando Health Jewett Orthopedic Institute are currently investigating the use of mixed reality in the operating room during shoulder replacement surgery. I use an augmented reality headset when performing anatomic shoulder replacement, reverse shoulder replacement, and revision shoulder replacement surgeries. The mixed reality goggles let me to see my patients’ anatomy on 3D planning software as a hologram right in the operating room! The software allows me to connect to my patients’ unique problems while performing the surgery and without physically touching any part of a computer. I work with the MR system virtually using my hands, voice, and by moving the headset itself. When using this software, the heads-up display shows the shoulder anatomy in space. I can walk completely around the 3D holographic digital shoulder image; it is like being inside of a computer! Instead of a mouse or controller, I use my hands to virtually type on a holographic keyboard, navigate menus, study the patient’s anatomy, and check the pre-planned size of the joint replacement.
The current mixed reality software allows me to connect with my patient’s problem in a unique way. In the future, this technology will also enhance accuracy and consistency by guiding surgeons to the ideal location for placing the components for a shoulder joint replacement. The goal of guided surgery is to help surgeons to achieve better outcomes by enhancing their accuracy and consistency.
Augmented reality will likely have many applications for physicians and all healthcare providers to help us better engage our patients. It could be used in many ways to help doctors have important information displayed but without the interference of a traditional computer screen or mobile device.
Virtual reality is growing in popularity not only as a gaming or social tool, but also has a valuable educational tool. Simulating surgery with VR experiences helps residents, fellows, and surgeons prepare for the operating room. Virtual reality education improves access for learners to high-quality simulation without the costs, infrastructure demands, and supply chain challenges of a cadaver lab. Another powerful feature of VR software is collaboration. Imagine virtually standing next to a surgeon (physically located in
FLORIDA MD - MAY/JUNE 2023 18
ORTHOPEDICS
another part of the world) that can interact with you and the digital environment as if they were right there with you. These simulations can bring you virtually into the operating room to participate as lead surgeon in a virtual shoulder replacement surgery! Medical education has many opportunities to expand the use of VR to help empower and educate our next generation of physicians.
Technology is advancing rapidly. Augmented reality, mixed reality, and virtual reality will likely all have a place to help doctors get better. To answer the question in the title, a mixed reality headset is not only likely to be the headset of choice in the future, but they are in use now. The current applications for these technologies are the tip of the iceberg compared to where we will be in 10 years. It is an exciting time to be a surgeon.
Benjamin Service, MD, is a fellowship-trained, board certified, orthopedic surgeon specializing in shoulder surgery, elbow surgery, orthopedic sports medicine and orthopedic trauma.
Dr. Service received his undergraduate degree in biology from Florida Atlantic University, graduating magna cum laude. He received his medical degree from the University of Florida College of Medicine and was inducted into the prestigious Alpha Omega Alpha Honor Medical Society and Gold Humanism Honor Society. He served his residency in orthopedic surgery at Orlando Health and completed his fellowship in shoulder and elbow surgery at the University of Washington. He can be reached at (321) 843-8551 or – Benjamin.service@orlandohealth.com

Orthopedic Doctor Orlando - Elbow Surgeon - Shoulder Specialist (orlandohealth.com)

FLORIDA MD - MAY/JUNE 2023 19
ORTHOPEDICS
Mitigating the Risks of Cervical Insufficiency
By Cole Douglas Greves, MD, FACOG

As an OB-GYN, I have a tremendous respect for the intricacies of pregnancy and childbirth.
Having a baby can be one of the most amazing and joyous experiences. But for some, it can be a difficult and anxious time. As part of a Maternal-Fetal Medicine group, I am able to help guide women and families through the stress and uncertainties of a high-risk pregnancy — understanding each woman’s unique challenges and providing the appropriate treatment at every step along the way. I also value the partnership with a woman’s primary OB-GYN, with a shared goal of a safe pregnancy and delivery, and a healthy mother and baby.
Affecting about 1 in 100 pregnancies, cervical insufficiency is defined as painless, cervical dilation in the absence of persistent uterine contractions. During pregnancy, the cervix, which is the opening of the uterus into the vagina, normally stays firm and closed until late in the third trimester. In preparation for the baby’s birth, the cervix becomes thinner and softer, shortens and dilates, creating the birth canal for the baby to pass through during delivery. Cervical insufficiency, also known as incompetent cervix, is a condition that occurs when these changes take place too early in the pregnancy. Cervical insufficiency can put expectant mothers at higher risk for pregnancy loss or premature birth.
Because these changes are usually painless, cervical insufficiency often isn’t detected until it’s too late — when it is seen on an ultrasound or when a woman experiences downward pressure in the pelvis that signals dilation and positioning of the fetus into the birth canal. Almost 25 percent of miscarriages in the second trimester are due to cervical insufficiency.
The good news is that there are treatment options available that can help prolong the pregnancy of a woman with cervical insufficiency, ideally to full term. With cerclage, a procedure that can help prevent the cervix from opening too soon, we can mitigate the risks of cervical insufficiency and hopefully keep the baby in place as long as necessary.
CAUSES OF CERVICAL INSUFFICIENCY
Since there usually is not a definitive cause and effect relationship, it’s difficult to predict who will experience cervical insufficiency. Factors that may cause the condition include:
• Biological makeup and how the cervix interacts with the hormones produced during pregnancy.
• Past cervical trauma, including injury or past cervical surgery, such as surgeries to remove pre-cancerous or cancerous cells. This has become somewhat less common in recent years, as many women are now vaccinated against the human papillomavirus (HPV) that is linked to cervical cancer.
• Genetics also may play a role. If a close family member has had cervical insufficiency, preventive measures may be advised.
The model scenario for diagnosing cervical insufficiency is to spot signs of early cervical change during the mid-pregnancy ultrasound that usually takes place at 18-20 weeks. If cervical insufficiency is suspected, a follow-up transvaginal ultrasound can provide an accurate evaluation of the cervix and its length. Based
on what is seen on the ultrasound or if there is a history of cervical insufficiency, a decision will be made either to monitor the situation or move forward with treatment.
TREATMENT OPTIONS FOR CERVICAL INSUFFICIENCY
Depending on how advanced the cervical insufficiency is, the recommended first option, particularly for a first pregnancy, could be progesterone vaginal suppositories. Progesterone is a hormone that can help stabilize the structure of the cervix and reduce inflammation, potentially preventing cervical insufficiency from progressing.
If progesterone treatment fails, the next step may be transvaginal cervical or abdominal cerclage. Cerclage is a treatment option for cervical insufficiency that can help prevent the cervix from opening too soon. The Center for Maternal-Fetal Medicine at Orlando Health Winnie Palmer Hospital for Women & Babies provides expertise in all types of cerclages and is one of few in Florida to offer transabdominal cerclage.
In a transvaginal cerclage, the weakened cervix is stitched shut and/or reinforced through the opening to the vagina. Usually performed during the 12th to 14th week of pregnancy, a transvaginal cerclage is the preferred method, if possible, since it is less invasive with no abdominal surgical incision needed. A transvaginal cerclage stitch is typically removed around 37 weeks of pregnancy in anticipation of a vaginal delivery.
A transabdominal cerclage is a surgical procedure in which the cervix is accessed through an incision in the lower abdomen. The cervix is then encircled with a stitch to reinforce it and help ensure that it remains closed during the pregnancy. For women who have no cervix or a history of incompetent cervix with previous unsuccessful vaginal cerclage placement, including those who have experienced pregnancy loss, this procedure can be performed prior to pregnancy. If performed during pregnancy, transabdominal cerclage placement will typically be done between the 9th and 14th week. Transabdominal cerclages require a Cesarean section delivery for every pregnancy going forward and are normally kept in place until a woman reaches the end of her childbearing years.
Cerclage can be very effective at helping women with cervical insufficiency maintain or prolong their pregnancies. With regular monitoring throughout the duration of the pregnancy, we can help ensure a successful progression, safe delivery, and healthy mom and baby.
Cole Douglas Greves, MD, FACOG, a board-certified clinical perinatologist, is director of the Fetal Care Center, part of the Center for Maternal-Fetal Medicine at Orlando Health Winnie Palmer Hospital for Women & Babies. Dr. Greves has more than 15 years of experience with cerclage procedures — including those placed transabdominally –which is available at only a handful of hospitals. He also has conducted extensive research in other areas and is a fre-
FLORIDA MD - MAY/JUNE 2023 20
quent presenter at medical conferences and meetings. After earning his medical degree from the University of North Dakota School of Medicine in Grand Forks, Dr. Greves completed his OB-GYN residency at Orlando Health and a fellowship in Maternal-Fetal Medicine at the University of Rochester – Strong Memorial Hospital in Rochester, New York.
202
3
EDITORIAL CALENDAR

Florida MD is a monthly medical/business digital magazine for physicians..
Florida MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD
It is hard to be aware of everything happening in the rapidly changing medical profession and doctors want to know more about new medical developments and technology, procedures, techniques, case studies, research, etc. in the different specialties. Especially when the information comes from a local physician specialist who they can call and discuss the column with or refer a patient. They also want to read about wealth management, financial issues, healthcare law, insurance issues and real estate opportunities. Again, they prefer it when that information comes from a local professional they can call and do business with. All advertisers have the opportunity to have a column or article related to their specialty or profession.
JANUARY – Digestive Disor ders
Diabetes
FEBRUARY – Car diology
Hear t Disease & Stroke
MARCH – Or thopaedics
Men’s Health
APRIL – Sur gery
Scoliosis
MAY –
Women’s Health
Advances in Cosmetic Sur gery
JUNE – Aller gies
Pulmonar y & Sleep Disorders
JULY – Neurology / Neuroscience
Advances in Rehabilitation
AUGUST – Spor ts Medicine
Robotic Sur gery
SEPTEMBER – Pediatrics & Advances in NICUs
Autism
OCTOBER – Cancer
Dermatology
NOVEMBER – Urology
Geriatric Medicine / Glaucoma
DECEMBER – Pain Management
Occupational Therapy
FLORIDA MD - MAY/JUNE 2023 21
Please call 407.417.7400 for additional materials or information.

18Hospice Palliative Care Grief Support It’s not about counting the days. It’s about making the days count. Featuring specialized programs and services for children to seniors, and a proud Level 5 We Honor Veterans program provider. (866) 269-4240 I reflectionslsc.org

















 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD






















 By Benjamin Service, MD
By Benjamin Service, MD





