SEPTEMBER/OCTOBER 2023 • COVERING THE I-4 CORRIDOR
Nemours Children’s Health
Redefining Care for Children with Ear Differences and Deafness



SEPTEMBER/OCTOBER 2023 • COVERING THE I-4 CORRIDOR
Nemours Children’s Health
Redefining Care for Children with Ear Differences and Deafness


Imagine being born missing a piece of yourself. To feel “incomplete”, “defective”, “different”. These are some of the terms microtia patients often report and feel, prompting them to search for reconstructive options. The lack of the external ear from birth, more often than not leads to the lack of the middle ear and associated hearing loss, threatening difficulty in communication in addition to the feeling of loss. Or consider the world of silence a newborn infant born deaf arrives in, or a child born with hearing enters upon losing their audition ability—sight but no sound, feelings but no hearing. The lack of hearing creates a vulnerabilities and barrier to, social opportunities, educational pursuits and career choices for an aspiring child.
“We aim to provide restorative care to patients with ear differences and deafness in a truly unique way. Our team of plastic surgeons and ENT surgeons has devised a completely integrated, interdisciplinary approach in treating children with microtia,” says Angelo A. Leto Barone, MD, a craniofacial and pediatric plastic surgeon at Nemours Children’s Health.
Dr. Leto Barone’s vision inspired the development of the Nemours Ear, Hearing and Communication Center (NEHCC), which he co-directs with Cedric Pritchett, MD, an otolaryngologist and head and neck surgeon who specializes in pediatric hearing loss and hearing restoration.


Iam pleased to bring you another issue of Florida MD. I can only imagine the emotional and physical trauma that a woman goes through when she has a mastectomy. The procedure affects not only her body, but her mind and her self-esteem. Now add in the inability to not be able to reconstruct her breasts and give that part of her life back, because she’s uninsured or under insured, and it becomes an unthinkable crushing blow. Fortunately there is My Hope Chest to help women who are unable to afford reconstructive surgery. I asked them to tell us about their organization and how you, as physicians, can help. Please join me in supporting this truly wonderful organization.
Best regards,
Donald B. Rauhofer Publisher
In 2010, more than 22,000 uninsured women lost their breasts to cancer and were left disfigured, deformed and feeling “less than whole.” How many years has this figure been growing?
Many organizations raise funds for research, education and “awareness” of breast cancer. Most have no idea there lies a huge gap in assistance for delayed reconstruction and co-pays for survivors wanting this surgery.
My Hope Chest is the ONLY national 501c3 non-profit organization focused on funding breast reconstruction for the uninsured and under insured survivors. Our services “pick up” where other breast cancer organizations leave off… providing the “final step in breast cancer treatment. ”

My Hope Chest is about addressing the needs of survivors now. Through wonderful surgeon partnerships we are able to transform the lives of breast cancer survivors who otherwise have no hope of reconstruction. We hope to hear from you to learn how we can work together to eliminate our wait list and take action to help every woman who desires reconstruction after mastectomy and feel restored in body, mind and spirit.
Wish List
• Surgeons to create awareness for My Hope Chest and to identify new clients
• Doctors of Distinction- Surgeon partners nationwide to join our program.
• Corporate partners, interested in Win-Win, Commercial- coventure marketing campaigns promoting their product or service by sharing our vision to make sure there is always coverage for reconstruction surgery.
For additional information on how you can help or refer a patient please go to www.MyHopeChest.org.
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: John “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, Julie A. Tyk, JD, Naina Mehta, MD, MHA, John Meisenheimer, VII, MD, Jaivir S. Rathore, MD, Julia Fink, DO, Firas Abdul, MD, Sonda Eunus, MHA, CMPE

Art Director/Designer: Ana Espinosa
Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762. Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2023 Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.

 By Staff Writer
By Staff Writer
Imagine being born missing a piece of yourself. To feel “incomplete”, “defective”, “different”. These are some of the terms microtia patients often report and feel, prompting them to search for reconstructive options. The lack of the external ear from birth, more often than not leads to the lack of the middle ear and associated hearing loss, threatening difficulty in communication in addition to the feeling of loss. Or consider the world of silence a newborn infant born deaf arrives in, or a child born with hearing enters upon losing their audition ability—sight but no sound, feelings but no hearing. The lack of hearing creates a vulnerabilities and barrier to, social opportunities, educational pursuits and career choices for an aspiring child.
Dr. Leto Barone’s vision inspired the development of the Nemours Ear, Hearing and Communication Center (NEHCC), which he co-directs with Cedric Pritchett, MD, an otolaryngologist and head and neck surgeon who specializes in pediatric hearing loss and hearing restoration.
“Led by Nemours’ guiding principal ‘Well Beyond Medicine’, NEHCC offers holistic care from functional and cosmetic reconstructive options to hearing augmentation services, speech and language therapy, genetic analysis, ophthalmological and individualized optometry solutions, psychological support and social work support,” according to Dr. Pritchett.
Two Programs, One Big Symbiotic Team – Meet NICEAR and NHEAR.
The NICEAR program, directed by Dr. Leto Barone from the Division of Pediatric Plastic Surgery, focuses on reconstructive efforts customized for each patient.
“No two patients are the same, which is why we don’t believe in a ‘one size fits all’ approach to microtia care,” says Dr. Leto Barone. “We study and discuss with our patients the best surgical technique (either using the patient’s own rib cartilage, cadaveric cartilage, porous polyethylene implants, or prosthetics) combined with the best hearing aiding solution to meet the individual needs of each patient. This work is made possible thanks to the attentive care of the NICEAR coordinator, Amanda D’Ambra, NP, who coordinates all patient evaluations in addition to all other providers, including audiologists, and speech language pathologists”.
The center has strong research, educational and social components. Our research team focuses on augmented reality and 3D printing use for preoperative planning and intraoperative navigation, medical device innovation and development of new surgical techniques, and rigorous speech evaluation in children
with microtia and atresia.
As part of our educational mission, we offer seminars to educate students, residents, and family with the understanding that “knowledge is power, allowing patient families to make a more informed decision to determine what is best for their child,” states Dr. Leto Barone. The center also hosts social events and national microtia and atresia support groups. This brings together our patient families in an effort to show each of these children with craniofacial differences that they are not alone.


The Nemours Hearing Enhancement, Augmentation and Restoration team at its core is defined by the collaboration of otolaryngologists, audiologists, and speech language pathologists. In addition to this triad, we provide a complementary partnership of psychology, social work, and occupational and physical therapy. According to Dr. Pritchett, “our goal is to enable and optimize a family’s desire to communicate with their child with hearing differences—most commonly, but not exclusively, directed at spoken language development and mastery.”
The NHEAR approach is based on:
• A timely and accurate diagnosis of hearing loss
• Understanding individual etiology and establishing appropriate expectation for performance
• A collaborative partnership with stakeholders in the child’s language growth and development – from parents to educational caregivers to community caretakers
This process supports the parent’s choice in their child’s hearing and communication health, while empowering them with up-todate knowledge on options and advances.
“Over the last nearly decade, our team has treated hundreds of children with hearing losses of all types—conductive, sensorineural and mixed in nature. Our team is proficient in the basic diagnostic techniques of behavioral pediatric audiometry as well as advanced electrophysiologic testing like auditory brainstem testing and evoked auditory cortex potential testing. These strategic tools are employed to pursue optimal access to quality sound in a timely manner,” says Dr. Pritchett. “We are experienced in the numerous types of implantable devices, including cochlear implants and bone-anchored hearing aids (osseointegrated implants), and facile with the delicate work of reconstructing the ossicular chain of the middle ear—either by native bone or titanium implants, using either microscopic or endoscopic techniques.”
The experienced team is comfortable with diagnosing and managing the uniqueness of conditions creating atypical hearing environments for the developing brain, such as auditory neuropathy and single-sided deafness. It has excelled in auditory habilitation for prelingual and perilingual deafness with Listening and Spoken Language (LSLS) certified speech language pathologists. This approach recognizes that children with hearing differences often have other challenges like balance difficulties, that benefit from the collaborative support of professionals in physical and occupational therapy, audiology and neurology.
Maintaining rigorous clinical curiosity is an important component of achieving superior clinical excellence in the work we do. Our team is engaged in many scholarly pursuits, with published manuscripts and numerous abstracts and presentations at regional and national meetings on relevant topics in the field. These research projects range from clinical outcomes, such as hearing out-
comes in children with congenital cytomegalovirus and performance of cochlear implant recipients with auditory neuropathy; to health services research, such as exploring barriers to care in pediatric cochlear implantation; to translational research, such as diagnostic assay design of point-of-care testing for congenital cytomegalovirus (the largest non-genetic cause of congenital hearing loss).
Built upon the energy, expertise and commitment of its team, the interdisciplinary foundation of the NEHCC program is the shared vision of Dr. Leto Barone and Dr. Pritchett. The surgical partnership of Aftab Patni, MD; Adele Evans, MD, Brian Kellogg, MD, has been crucial, as has collaboration with the following leaders:
Chelsea Clancy, AuD
Lynn O’Boyle, AuD
Yeraldi Geronimo, MA, CCC-SLP
Megan Nelson, MA, CCC-SLP, LSLS, Cert AVT
Vanessa Batzan, MA, CCC-SLP

Anais Andara, PA-C
Michelle Steward, APRN
Mahshid Roohi, APRN
Cristina Ortiz, MSW, LCSW
Amanda D’Ambra, APRN
Sandra Giraldo, BA

Evette Pizarro
We believe that success is not only measured in accomplishing a novel or innovative intervention, but also in what percentage of the eligible pediatric population are given appropriate access to quality, timely standard-of-care surgical intervention. We’re committed to dialogue and advocacy in collaboration with community partnership to achieve positive outcomes for the patients we serve.
With providers, educators, parents and thought leaders working together we can and will transform the health of children by going beyond medicine and improving the health of the world in which every child lives.

 By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII, MD
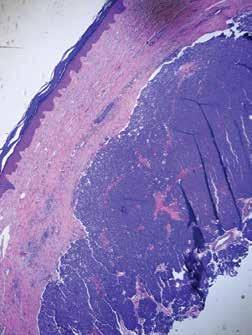
When you mention skin cancer to the general public or even to the medical community, most folks think of the three big celebrities: basal cell carcinoma, squamous cell carcinoma, and melanoma. I like to refer to having occurrences of all three types of skin cancer in one patient as hitting the trifecta of skin cancer; unfortunately, there is no big payout with this trifecta. Excessive sun exposure is typically the common denominator. What is less known is there are other cancers of the skin besides the big three, and these can kill you as well. What I like to call “the fourth skin cancer” is the Merkel Cell Carcinoma. Not as famous as the big three, but Merkel cell carcinoma still should be treated with respect when it makes it rare appearances.

Merkel Cell carcinoma, like other skin cancers, has a predisposition for appearance in sun-exposed areas such as the face or sometimes the hands or digits. They usually do not appear in younger individuals and tend to arise more frequently in those with immunodeficiency. Merkel cell carcinomas present as a nonspecific papule or nodule. Because it can initially be misdiagnosed as a benign cyst, the actual pathology of the tumor may be delayed. Additionally, Merkel cell carcinoma is typically asymptomatic in the beginning, and this also adds to delay in diagnosis as many patients are not concerned until the fast-growing tumor reaches a large size.
The problem with Merkel cell carcinoma is that it is a highly aggressive type of skin cancer, and like melanomas, with enough growth and time, it can metastasize. Merkel cell carcinomas are treatable, and the treatment of choice is excision, the earlier, the better. Once a Merkel cell carcinoma has metastasized, it becomes a problematic tumor to treat, although new therapies are available that hold some promise. Recent studies suggest that 97% of Merkel Cell carcinomas have a common virus expression (Merkel cell polyomavirus). How this oncovirus may cause, Merkel cell carcinoma is currently unknown. Fortunately, patients that have Merkel cell carcinoma are not infectious.
If you observe a growth on the skin and you think to yourself, well, it doesn’t look like a basal or squamous cell carcinoma or melanoma; therefore, it’s probably benign always think of the other skin cancer, Merkel cell carcinoma. Happily, I have not had any of my patients that have had a trifecta of skin cancer also get Merkel cell carcinoma. In this scenario, I would have to name it the superfecta of skin cancer and not a title I would want to bestow on anyone.


There are several categories of pulmonary hypertension. WHO Group I includes patients with idiopathic pulmonary hypertension, familial pulmonary hypertension, drug and toxin related (fen-phen) portopulmonary hypertension, HIV related pulmonary hypertension and pulmonary arterial hypertension associated with connective tissue disorders (such as scleroderma). WHO Group II pulmonary hypertension is often referred to as pulmonary venous hypertension. This includes patients with left ventricular systolic or diastolic dysfunction or valvular heart disease. Essentially, the WHO Group II category includes patients who have an elevated pulmonary capillary wedge pressure and/ or elevated left ventricular end diastolic pressure. WHO Group III pulmonary hypertension consists of patients with COPD, interstitial lung disease, or other conditions in which hypoxia causes vasoconstriction. The remainder of this article will focus on WHO Group IV pulmonary hypertension (chronic thromboembolic pulmonary hypertension or CTEPH). Although WHO Group IV patients are relatively rare, it is crucial to identify them because this is the only type of pulmonary hypertension which is potentially surgically curable.
After acute pulmonary embolism, most patients will recover and have normal pulmonary hemodynamics, gas exchange, and exercise tolerance. It is believed that 1-4% of patients with acute pulmonary embolism will go on to develop CTEPH within two years. It is not clear why some patients with acute pulmonary embolism develop CTEPH. Risk factors include hypercoagulable states, myeloproliferative syndromes, splenectomy and chronic indwelling central venous catheters. Patients with CTEPH present with dyspnea, which can have a gradual onset. Many patients with CTEPH will not have a known previous diagnosis of acute pulmonary embolism. As with other patients with pulmonary hypertension, patients with CTEPH may not show findings on physical exam until pulmonary hypertension is in the late stages. Findings include a right ventricular lift, jugular venous distention, fixed splitting of the second heart sound, hepatomegaly, ascites, and peripheral edema. Patients with CTEPH may have “flow murmurs” heard over the lung fields because of turbulent flow through partially obstructed or recanalized pulmonary arteries. These tend to be accentuated during inspiration.
Acute pulmonary embolism is the trigger for CTEPH. In some patients this triggers a small vessel vasculopathy (for unclear reasons) that contributes to the extent of pulmonary hypertension. This may explain why up to 35 percent of patients who undergo succesful pulmonary thromoendarterectomy can have some degree of postoperative pulmonary hypertension.
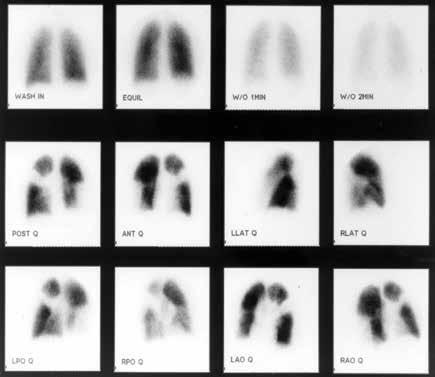
Although VQ scanning has become less commonly used for diagnosis of acute pulmonary embolism this remains the initial imaging study of choice in patients with pulmonary hypertension
to separate “small vessel” variants (Idiopathic pulmonary arterial hypertension) from “large vessel” disease (CTEPH) A normal VQ scan essentially excludes the diagnosis of CTEPH. A scan with one or more mismatched segmental defects is suggestive of the diagnosis. However, it is important to note that VQ scan can often understate the extent of central pulmonary vascular obstruction. Once the VQ scan is found to be abnormal then further testing should be undertaken (such as CT angiogram and/or pulmonary angiography). The angiographic findings in CTEPH are distinct from those of acute pulmonary embolism. They can include pouch defects and pulmonary artery webs. Patients with severe pulmonary hypertension have been found to tolerate performance of angiography as well as VQ scan without significant complication rate.
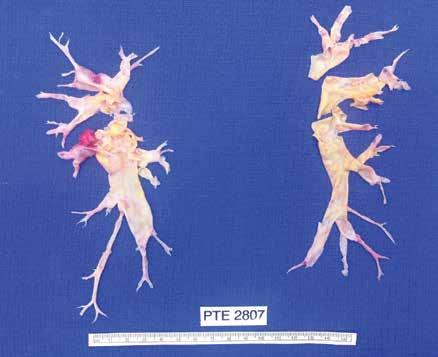
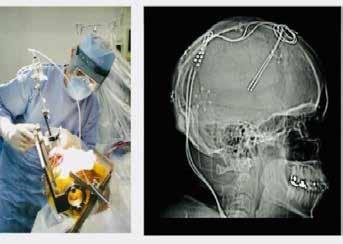
The surgery for CTEPH is quite different from surgical intervention for an acute pulmonary embolism. Surgery for CTEPH is called a pulmonary thromboendarterectomy (PTE), which requires median sternotomy and cardiopulmonary bypass. It requires an often tedious intimal dissection of fibrotic recannalized thrombus from the native pulmonary arterial wall. IVC filter placement is usually recommended before pulmonary thromboendarterectomy. These patients can have a complicated postoperative course and this type of surgery is only done at a few specialized centers in the country. The center which is best known for this type of surgery is the University of California (San Diego). Patients who have undergone PTE are typically maintained on lifelong anticoagulation. To be a candidate for this surgery, a patients must have central, surgically accesible chronic thromboemboli. A significant postoperative complication is pulmonary artery steal, which refers to redistribution of pulmonary arterial blood flow from well-perfused segments into the newly opened segments resulting in ventilation perfusion mismatch and hypoxia. This redistribution of flow resolves over time. Approximately, 30% of PTE patients can develop reperfusion pulmonary edema. The perioperative mortality of pulmonary thromboendarterectomy can be in the range of 2-3% in experienced centers. Outcome is clearly better in high voluime centers (more than fifty PTE surgeries/year). Approximately 5000 thromboendarterectomy procedures have been performed worldwide, 3000 at UCSD alone.
Surgery for CTEPH is clearly the best therapeutic option. However, there are some patients with CTEPH who are inoperable or who have persistent or recurrent pulmonary hypertension after undergoing pulmonary thromboendarterectomy. There is now a medical therapy available for these patients. Riociguat (Adempas) was approved by the FDA in October 2013. It is a member of a new class of compounds-soluble guanylate cyclase stimulators. In the multicenter study by Ghofrani et al that was published in the New England Journal of Medicine in July 2013,
261 patients were randomized prospectively to receive riociguat versus placebo. Riociguat was shown to significantly improve exercise capacity and pulmonary vascular resistance. Side effects include systemic hypotension. Prior smaller studies have also shown some benefits to medical therapy in CTEPH (inoperable or with post-operative PH) with oral agents such as bosentan and sildanefil, inhaled iloprost and subcutaneous treprostinil. Medical therapy has also been used as a “bridge” before PTE.
Although relatively rare, CTEPH is an important cause of PH since it is potentially curable with pulmonary endarterectomy. This surgery should only be performed in very experienced, specialized centers. PTE surgery should always be the treatment of choice for CTEPH. However, medical therapy can have a role as a bridge to PTE,in patients who are not surgical candidates or in those who have persistent pulmonary hypertension despite undergoing PTE.

I would like to express my gratitude to Dr. Peter Fedullo (University California San Diego) for his review of this manuscript and providing the photographs.
Daniel Layish, MD, graduated magna cum laude from Boston University Medical School in 1990. He then completed an Internal Medicine Residency at Barnes Hospital (Washington University) in St.Louis, Missouri and a Pulmonary/Critical Care/ Sleep Medicine Fellowship at Duke University in Durham, North Carolina. Since 1997, he has been a member of the Central Florida Pulmonary Group in Orlando. He serves as Co-director of the Adult Cystic Fibrosis Program in Orlando. He may be contacted at 407-841-1100 or by visiting www.cfpulmonary.com.


Ask any patient and they can tell you that regardless of the benefits they expect to receive from a planned surgical procedure, they are dreading post-operative pain during their recovery. They may accept this as an inevitable part of their treatment, but that doesn’t lessen their stress and anxiety.
The potential habit-forming aspects of some opiates are a big concern. So, the development of a new procedure to block pain receptors with minimal medication is a major step forward. This approach can lead to less stress and anxiety before surgery and faster recoveries afterwards.
Cryoneurolysis is the technical term for the process. The word is a mouthful for a fairly straightforward procedure.


Before getting too deep into the procedure, let’s first think about how your central nervous system works. At the risk of oversimplifying an extremely complex system, you have nerves that control muscles and nerves that transmit sensations to the brain. The network of nerves that transmit sensations to the brain are composed of the individual nerve endings or receptors and the system of fibers that connect those nerves to the brain. These fibers act as a sort of network of pipes carrying information from the receptors.
What we do in cryoneurolysis is to freeze specific nerves without affecting that system of pipes. This technique allows us to, in effect, switch off those nerves. The nerves stop sending signals to the brain, and the patient stops feeling pain from those specific nerves.
In practice, it works like this. Let’s suppose a patient has a severely arthritic knee, and joint replacement surgery is scheduled. The patient can go to the anesthesiologist several weeks before the surgery for pre-operative cryoneurolysis treatment. There, the doctor uses an ultrasound device to view and identify the specific nerves that are involved. Then, after administering a local anesthesia, the doctor uses a thin probe – basically a needle with a sealed tip – into which a pulse of nitrous oxide creates a tiny iceball at the tip of the probe. Using the ultrasound device, we can see the nerves and precisely guide the probe so this tiny ice-ball forms around each specific nerve, freezing it without damaging the surrounding tissue or the network of nerve pipes. Without the nerve receptors sending sensations to the brain, the patient immediately stops feeling pain from those nerves. This decreases the patient’s pre-operative and post-operative discomfort, reducing the burden of medication. Typically, the nerve receptors regenerate within several months, and by that time the patient will have healed from the surgery.
At Orlando Health Jewett Orthopedic Institute, we have already begun using this technique on some knee-replacement patients, and the results have been very reassuring. Patients have less pain going into surgery and their recovery times are faster because
they are able to be more mobile following surgery. Using this technique, we’re able to add another tool to help patients after a total knee replacement surgery. Many of our patients, already scheduled for an outpatient procedure in which they can go home on the same day as the surgery, now have an option that will further reduce their pain. It’s a game-changer.
We have even had patients for whom cryoneurolysis has been the treatment, not just a component of the treatment. We recently treated an 80-year-old patient who was mentally sharp, but in our judgement was too frail to undergo surgery. However, the pain she was experiencing due to arthritis had severely limited her quality of life. She was unable to walk unassisted, and every step was painful.
After cryoneurolysis treatment, her pain was substantially relieved, and her mobility was restored. In fact, she is even able to now walk without her walker.
It’s important to note that cryoneurolysis only addresses the patient’s pain and not the underlying problems caused by the arthritis. But since surgery was not an option, the elimination of the patient’s pain, and doing it without any of the side effects that might come with other pain treatments, was a terrific outcome.
I had first learned about this technique a couple of years ago, but it wasn’t until we established our new practice within Orlando Health Jewett Orthopedic Institute that we have been able to focus on this. It’s one of the advantages of being in a practice with a singular focus. Everyone who works in the Institute is working one-hundred-percent on our coordinated approach to patient health, patient experience and patient outcomes. It’s a very exciting and rewarding time to not only be practicing anesthesiology, but to be helping patients receive the most up to date care in Central Florida.
 By Julia Fink, DO
By Julia Fink, DO
More and more young athletes today are participating on competitive sports teams year-round instead of multiple sports through different seasons. This change in athletic competition has led to an increase in overuse injuries in the pediatric population. The cause of these overuse injuries can be attributed to a combination of an underdeveloped musculoskeletal system, increased duration and intensity of competition as well as early sports specialization. One type of overuse injury that can have a detrimental impact on sports preformation and overall health are stress fractures. Stress fractures are due to abnormal stresses being placed on the trabecular bone resulting in microfractures. Due to lack of adequate rest and recovery or underlying abnormalities in bone metabolism, these microfractures are unable to heal and remodel and can propagate over time. Continued repetitive loads exceeding the body’s normal intrinsic bone healing can eventually lead to complete fracture through the affected bone. The most common site for stress fractures is the anterior tibia but can also occur in the femoral shaft, femoral neck and posterior ribs. Stress fractures can occur on the compression side or the tension side of bones. Stress fracture on the compression side can be effectively treated without surgery due to stability and adequate blood supply. However, stress fractures that occur on the tension side of a bone have poor healing potential and usually require surgical intervention.
Stress fractures are commonly confused with tibial stress syndrome, also known as shin splints. Shin splints differ from stress fractures in that shin splints are an inflammation of the superficial portion of the bone called the periosteum. The underlying periosteum becomes inflamed from the repetitive pull of the muscles originating in the anterior or posterior compartment of the lower leg. Patients most commonly report vague pain that runs along the middle to distal aspect of the tibia, usually worse with the beginning of exercise but improved with prolonged activity. Radiographs may be normal in these patients but are often obtained to rule out stress fracture. Treatment for shin splints involves modifying activities until the pain subsides which can involve decreasing running distance, performing cross-training exercises and avoiding running on hills or hard, uneven surfaces. Physical therapy can also be used as an adjunctive treatment to help with stretching and strengthening especially of the ankle invertors and evertor muscles.
Two major risk factors for the development of stress fractures are rapid increases in high intensity activity and abnormalities in normal bone metabolism. High intensity athletes as well as new military recruits are subject to rapid increase in training intensity especially during conditioning periods and basic training. Pediatric and adolescent muscles are underdeveloped and subsequently subject to early fatigue causing compensatory
gait changes with increased stresses applied to the bone. This loss of the body’s ability to absorb shock from fatigued muscles combined with poor mechanics and improper training regimens can also cause overloading of these deconditioned muscles ultimately resulting in overuse injuries. 90% of a child’s bone mass is attained by the age of 18. Essential vitamins, such as Vitamin D and calcium, play a vital role in a child’s developing skeleton. Athletes that are at risk of suboptimal bone mass and stress fractures include distance runners, gymnasts and elite dancers. These sports require lean body mass and are often associated with disordered eating habits and irregular menstrual cycles in young female athletes. There has been a dramatic increase in the number of healthy children and adolescents who are at risk of vitamin D deficiency. Lifestyle changes that place children at risk for Vitamin D deficiency include lack of outdoor activities, increased screen time and poor diets. Inadequate oral intake of Calcium and Vitamin D, lack of outdoor physical activity and abnormal estrogen levels can disrupt normal body homeostasis needed for appropriate bone growth and remodeling.
Patients with lower extremity stress fractures most commonly present with complaints of pain in the anterior tibia, hip or thigh, worse with running or increased physical activity. Overtime pain can occur even with simple daily activities like walking or at rest. Symptoms usually develop insidiously and unrelated to a known injury. Evaluation by a physician begins with a detailed history of symptoms and physical exam. Plain radiographs are also obtained which may demonstrate cortical thickening or stress fracture. There may be radiographic markers of bone healing, such as periosteal reaction and consolidation within 3 weeks of injury. If plain radiographs are negative, MRI is a sensitive imaging modality to help evaluate location of stress fractures as well as to assess the growth plate and surrounding soft tissues. MRI can demonstrate subtle findings with exquisite detail of bone edema and fracture to confirm diagnosis without radiation exposure to the child. First line treatment for compression sided stress fractures is protected weight bearing on the affected extremity for 4-6 weeks or until pain resolves. NSAIDs such as Aspirin, Aleve and Advil are usually avoided due to the potential to slow bone healing by inhibiting pro fracture healing inflammation. Tension sided stress fractures are less likely to heal with conservative management and likely require operative fixation. Treatment also consists of a progressive return to play to avoid recurrence of stress fracture.
The most important factor for preventing stress fractures in
Continued on page 12
young athletes and children is to recognize risk factors early. A healthy diet of essential vitamins and protein should be emphasized in young athletes as well as in young children for complete normal development of their skeleton. Children of all ages should also participate in at least 60 minutes of physical activity per day; this regular physical activity also helps to promote the development of bone strength. Coaches, parents and athletic trainers can help identify athletes and children at risk for overuse injuries and stress fractures as well as encourage adequate recovery and rest. Young athletes should be encouraged to seek treatment to prevent complications or need of surgical intervention from their overuse injuries.
Julia V. Fink, DO, is a board-certified orthopedic surgeon and sports medicine specialist at Nemours Children’s Hospital. A national champion collegiate softball player herself, Dr. Fink has been recognized by the American Orthopedic Society for Sports Medicine with a STOP Award, which recognizes outstanding research related to youth sports injury prevention, treatment, or rehabilitation. She attended medical school at the Philadelphia College of Osteopathic Medicine’s Georgia campus prior to her residency in orthopedic surgery at Jack Hughston Memorial Hospital in Phenix City, Alabama. She continued her training with a fellowship at Children’s Healthcare of Atlanta at Scottish Rite in Georgia. In addition to injury prevention, Dr. Fink is passionate about leadership, inclusion, and career development. She works with young athletes in the community and in school settings to offer her care for sports physicals, scoliosis screenings and other preventive services. Dr. Fink also volunteers for camps and provides physician sports coverage and she’s active in research.
Your brand is the identity that you create for your practice. It is crucial to identify the core values that you want your brand to represent, because this is how it will be perceived by your target audience and the community at large.
Here are some questions to consider when building your brand:
• How do you want your practice to be perceived?
• What core values do you hold most important to your WHY?
• What does your brand look like? Colors, fonts, and shapes matter.
• What does your brand sound like?
When choosing your brand colors, be aware of the following color associations:
• Red — Red stands for passion, excitement, and anger. It can signify importance and command attention.
• Orange — Orange stands for playfulness, vitality, and friendliness. It is invigorating and evokes energy.
• Yellow — Yellow evokes happiness, youth, and optimism, but can also seem attention-grabbing or affordable.
• Green — Green evokes stability, prosperity, growth, and a connection to nature.
• Light Blue — A light shade of blue exudes tranquility, trust, openness. It can also signify innocence.
• Dark Blue — Dark blue stands for professionalism, security, and formality. It is mature and trustworthy.
• Purple — Purple can signify royalty, creativity, and luxury.
• Pink — Pink stands for femininity, youth, and innocence. It ranges from modern to luxurious.
• Brown — Brown creates a rugged, earthy, old-fashioned look or mood.
• White — White evokes cleanliness, virtue, health, or simplicity. It can range from affordable to high-end.
• Gray — Gray stands for neutrality. It can look subdued, classic, serious, mysterious, or mature.
• Black — Black evokes a powerful, sophisticated, edgy, luxurious, and modern feeling.
(www.99designs.com)
Think of your Business brand as a person. What is this person’s personality like? How does he or she dress, talk, and act in public? Here are just a few examples of a personality that your brand
may have:
• Serious and Professional
• Warm and Friendly
• Cool and Quirky
• Funny and Playful
However, you choose to represent your brand, make sure that it is authentic to who you are. For example, if you are playful and like to crack jokes, infuse your marketing with humor and you will find that people respond positively to jokes, memes, and quotes that are applicable to them. For example, for pediatric practices, we have found that moms just can’t get enough of memes that make fun of their kids! You can add some (goodnatured) jokes and memes to your social media posts and you will see some great engagement.
Similarly, if you want your brand to be viewed as serious and professional, you will want to consistently share valuable and informative content that educates your audience. You can choose to do so by looking for speaking opportunities to help build credibility and position you as the expert in your field, making educational videos and sharing them on your website, Youtube, and social media, or by writing educational articles and contributing to reputable publications.
If you’re going for warm and friendly, you will want to be seen engaging with your social media followers, being active in Facebook groups and other online groups, hosting community events, supporting great causes, etc.
If cool and quirky is your thing, you want to stand out from your competitors. You can use some colors that are not typical for your industry, create and share some fun videos, such as “funny (HIPAA-compliant) things that patients say”, paint your waiting room to inspire awe upon arrival, etc.
Keep in mind that for any brand personality, it is important to keep it consistent across your website content, social media posts, marketing materials, and any other communication that you may have with your audience.
Sonda Eunus is the Co-Founder of Pro Medical Marketing – an Internet Marketing Agency specializing in Medical practices. She has a Masters’ in Healthcare Management and is a MGMA Certified Medical Practice Executive. She has been heavily involved in operating her family’s Pediatric practices from an early age. She is passionate about helping medical practices grow and does so by sharing her experience in her writing, speaking, and consulting. Learn more about Sonda and Pro Medical Marketing at www.promedicalmarketing.com.

 By Julie A. Tyk, JD.
By Julie A. Tyk, JD.
An exculpatory clause purports to deny an injured party the right to recover damages from a person negligently causing his injury. Cain v. Banka, 932 So. 2d 575 (Fla. 5th DCA 2006). They are disfavored in the law because they relieve one party of the obligation to use due care and shift the risk of injury to the party who is probably least equipped to take the necessary precautions to avoid injury and bear the risk of loss. Applegate v. Cable Water Ski, L.C., 974 So. 2d 1112, 1114 (Fla. 5th DCA 2008). Such clauses are strictly construed against the party seeking to be relieved of liability. Sunny Isles Marina, Inc. v. Adulami, 706 So. 2d 920 (Fla. 3d DCA 1998). Thus, exculpatory clauses are enforceable, only where, and to the extent, that the intention to be relieved from liability is made clear and unequivocal. Tatman v. Space Coast Kennel Club, Inc., 27 So. 3d 108, 110 (Fla. 5th DCA 2009). The wording must be so clear and understandable that “an ordinary and knowledgeable person will know what he is contracting away.” Id. (quoting Gayon v. Bally’s Total Fitness Corp., 802 So. 2d 420 (Fla. 3d DCA 2001)).
The seminal Florida case on exculpatory clauses is the Florida Supreme Court case of Sanislo v. Give Kids The World, Inc., 157 So. 3d 256 (Fla. 2015). Give Kids the World, Inc. (“GKTW”) provided free vacations to seriously ill children and their families. When applying for the vacation, the Sanislos executed a “wish request” form that contained a waiver of liability, also known as an exculpatory clause. When the parents arrived at the resort village they again signed a liability release form, also an exculpatory clause. The language of the exculpatory clause is reprinted below for reference:
I/we hereby release Give Kids the World, Inc. and all of its agents, officers, directors, servants, and employees from any liability whatsoever in connection with the preparation, execution, and fulfillment of said wish, on behalf of ourselves, the above named wish child and all other participants. The scope of this release shall include, but not be limited to, damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physical and emotional), entertainment, photographs and physical injury of any kind....
I/we further agree to hold harmless and to release Give Kids the World, Inc. from and against any and all claims and causes of action of every kind arising from any and all physical or emotional injuries and/or damages which may happen to me/us....
Sanislo at 258-259.
While participating in a horse-drawn wagon ride, a rear pneumatic lift designed to allow those in wheelchairs to participate failed, and Ms. Sanislo was injured. The Sanislos brought suit and GKTW filed a motion for summary judgment arguing that the signed releases precluded an action for negligence. The Sanislos filed a motion for partial summary judgment against GKTW’s affirmative defense of release. The trial court granted the Sanislo’s
motion and denied GKTW’s motion. The jury found for the Sanislos and GKTW appealed. Id.
The Fifth District reversed, finding the lower court erred in denying GKTW’s motion for summary judgment because the release signed by the Sanislos was unambiguous and did not contravene public policy. It ruled the exculpatory clause barred the negligence action despite the lack of a specific reference to “negligence” or “negligent acts” in the exculpatory clause.
The Fifth District reasoned that exculpatory clauses are effective if the wording of the exculpatory clause is clear and understandable so that an ordinary and knowledgeable person would know what he or she is contracting away, and that the court had previously rejected “‘the need for express language referring to release of the defendant for “negligence” or “negligent acts” in order to render a release effective to bar a negligence action.’ ” On the public policy argument, the Court said the relative bargaining power of the parties should not be considered because it was outside of the public utility or public function context and the Sanislos were not required to request a vacation with GKTW or go on the vacation. Id.
In affirming the Fifth District’s decision, the Supreme Court wrote that the conflict for the Court’s resolution was “whether an exculpatory clause is ambiguous and thus ineffective to bar a negligence action due to the absence of express language releasing a party from its own negligence or negligent acts.” Id. at 260.
The Florida Supreme Court wrote:
.... we are reluctant to hold that all exculpatory clauses that are devoid of the terms “negligence” or “negligent acts” are ineffective to bar a negligence action despite otherwise clear and unambiguous language indicating an intent to be relieved from liability in such circumstances. Application of such a bright-line and rigid rule would tend to not effectuate the intent of the parties and render such contracts otherwise meaningless.
Id. at 270.
The Court found that the GKTW liability release form released GKTW and all of its agents, officers, directors, servants and employees from “any liability whatsoever in connection with the preparation, execution and fulfillment of said wish…” The release then provided that the scope of the agreement included “damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physical and emotional), entertainment, photographs and physical injury of any kind . . . .” The Court found that the release clearly conveyed that GKTW would be released from any liability, including negligence, for damages, losses, or injuries due to transportation, food, lodging, entertainment and photographs. Id.
The determination of whether an exculpatory clause is en-
forceable will be determined by the Judge as the enforceability of a pre-injury release is a question of law. The enforceability therefore, will depend on the Judge assigned to the matter. Physicians should not assume that because a patient signed a liability release form the patient does not have a viable cause of action. Physicians should consult with an experienced attorney who can examine the facts of the case and help you determine the best path forward. The Health Care Practice Group at Pearson Doyle Mohre and Pastis, LLP is committed to assisting Clients in navigating and defending medical malpractice claims. For more information and assistance, please contact David Doyle and Julie Tyk at Pearson Doyle Mohre & Pastis, LLP.

Julie A. Tyk, JD, is a Partner with Pearson Doyle Mohre & Pastis, LLP. Julie concentrates her practice in medical practice defense litigation, insurance defense litigation and health care law. She has represented physicians, hospitals, ambulatory surgical centers, nurses and other health care providers across the state of Florida. She may be contacted by calling (407) 951-8523; jtyk@pdmplaw.com..


We hear more about autism these days, leading many people to conclude that there are more and more cases each year. In fact, today we estimate that one in 54 children may be diagnosed as autistic, compared to one in 150 children back in 2000 and just one in 2,000 children in the 1980s. Is the incidence of autism really more than doubling every 20 years?
As a neurodevelopmental pediatrician, I don’t believe the incidence of autism is truly increasing exponentially, but it is our screening and diagnosis of autism that has been expanding. We define autism as a developmental disorder characterized by difficulty in social interaction and communication associated with restricted or repetitive patterns of thought and behavior.
Currently there is no medical test to diagnose autism, such as a blood test. But our screening processes and diagnostic tools have expanded. Often, the first step in diagnosing a child with autism lies with the pediatrician. They assess the child soon after the first birthday to see if they’re meeting milestones and interacting appropriately. If the physician or family suspects autism, the child is referred to a specialist for an official diagnosis, based on an evaluation using the Diagnostic and Statistical Manual of Mental Disorders, fifth addition (known as the DSM-5). In the state of Florida, this diagnosis must be made by a specialist – a developmental pediatrician, a neurologist, a psychologist or a psychiatrist, in order for the insurance companies to provide approval for the appropriate therapy, applied behavioral analysis (ABA), that the child needs.
In the past, a child may have been given the diagnosis of mental retardation, now more commonly known as intellectual impairment. In the case of a higher functioning child, the child may previously have been considered to be just quirky and different, and may have been diagnosed with the term Asperger’s. Today that same child may be considered autistic, based on the expanding criteria. A diagnosis of autism addresses a combination of two things: intelligence and behavior. The terms “high functioning” and “low functioning” refer to intellectual ability or intelligence. The terms “low,” “moderate” and “severe” refer to their autistic behaviors. We see autistic people at all levels of intelligence and behavior. For instance, many may remember the character from the Rain Man film of the 1980s, who would be considered super high functioning for his intelligence – a savant even. Yet, his behavior was more severe.
While we don’t know what causes autism, we do know that boys are up to four times as likely to be diagnosed as girls. We also know that genetics are very much involved. In fact, parents with one autistic child are 10 to 20 percent more likely to have a second child diagnosed. If one identical twin is diagnosed as autistic, there is as high as a 90 percent chance the second twin is also autistic.
As our screening and diagnostic tools for autism have expanded, our knowledge of treatment options for autism remains the same. Despite the numerous claims that there is a cure for autism, such as medications, mega-vitamins, gluten-free and casein-free diet, hyperbaric oxygen chambers or colonic cleanses, none have demonstrated success in curing or treating autism. After years of experience with autism, the medical community can say that behavioral therapy is the only treatment to have shown significant success.
It’s important to note that while medication may not be an effective treatment for autism, many people with autism have comorbid conditions, such as anxiety or depression, attention deficit hyperactivity, seizures, sleep issues and sometimes more significant behaviors of self-injury and aggression, where medications may have some benefit.
When it comes to treatment, we have seen significant success with applied behavioral analysis or ABA, an evidence-based treatment strategy used to reduce challenging behaviors and increase socially appropriate behaviors. ABA therapy is an intensive therapy administered by a board-certified behavioral analyst (BCBA)/ registered behavior technician (RBT) – up to 40 hours per week, which may be offered in the home or in a clinical setting. The therapy consists of an intensive, structured teaching program in which social and communication behaviors are broken down and rehearsed in their simplest elements. Other forms of therapy, such as floor time and circles of communication have also been shown to provide beneficial effects and can be practiced at home. Here the parent gets down at the child’s eye level and, through play, makes continuous social communication and interaction, back and forth, creating circles of communication which help the child understand that there’s a world out there in which he or she can interact.
Studies show that the earlier ABA therapy begins, the earlier we can see improvement. Our developmental window is the first six years of life. We see cases where treatment begins as early as 2 years of age and the child is ready for regular kindergarten by the age of 5 or 6. Sadly, the process of diagnosis and qualifying for treatment can be slow. In many cases, we see that it may take more than six months to see a specialist for a diagnosis and then up to a year to find availability with an ABA therapist, underscoring the need for early intervention. We recommend referring children to a specialist as early as possible to ensure that autism is diagnosed promptly and treatment may begin.
Special training is also available for parents and family mem-
bers, which I highly recommend. In fact, siblings often turn out to be the best therapists for their sibling with autism. So often children learn better from other children than an adult. Involving siblings in the therapy can also make the siblings feel more a part of the solution rather than resenting the autistic sibling for the extra attention required from parents. This special training for family members is an excellent tool to supplement ABA therapy or to be used while a family is awaiting ABA therapy approval or availability.
Autism is a fascinating field of study. We continue to learn more about the condition and ways to improve functionality. In fact, I’m currently working with a group of ear, nose and throat specialists, and gastroenterologists on a study to determine if nasopharyngeal microbiomes may be a marker for autism, advancing the thought that the olfactory nerve is the closest in proximity to brain tissue that can be easily accessible. This may provide evidence of changes within the brain, specific to children with autism, which can then be used a marker aiding in the diagnosis of autism. I look forward to learning more and to continuing my work serving autistic children and their families.
If you suspect a child has autism, consider scheduling an appointment with a specialist as early as possible to maximize treatment opportunities.
Naina Mehta, MD, is a neurodevelopmental pediatrician at the Orlando Health Arnold Palmer Hospital for Children Pediatric Behavioral Health and Developmental Center. She is board certified in neurodevelopmental disabilities. Dr. Mehta has co-published studies involving meditation, yoga and breathing practices for children and youth with ADHD and learning disabilities. She offers parents both personal experience and professional training in managing behavioral issues with their children. She is currently leading a research study with ENTs and gastroenterologists on nasopharyngeal microbiome as a possible autism marker.

It’s not about counting the days. It’s about making the days count.Featuring specialized programs and services for children to seniors, and a proud Level 5 We Honor Veterans program provider. (866) 269-4240 I reflectionslsc.org


Parkinson’s disease (PD) is the second-most common neurodegenerative disease after Alzheimer’s dementia. More than 10 million people worldwide and nearly one million people in the U.S. are living with PD. This number is expected to rise to 1.2 million by 2030. Nearly 90,000 people in the U.S. are diagnosed with PD each year. The incidence of PD increases with age, but an estimated four percent of people with PD are diagnosed before age 50. Men are 1.5 times more likely to have PD than women. Within the US; Florida has the second highest population of people living with PD. It is a slowly progressive disorder which often first presents with a resting hand tremor. The patient can then develop other cardinal features of bradykinesia, rigidity and postural instability. Autonomic symptoms like constipation, poor sense of smell, excess salivation due to poor swallowing can be present years before the patient develops the classic PD symptoms. In some patients there can be signs of cognitive decline which could be part of “Parkinson’s Plus” or Parkinson’s dementia.
PD results from loss of dopaminergic neurons in the pars compacta of substantia nigra of basal ganglia which is responsible for subcortical control of motor activity. In most cases the exact cause is unknown (Idiopathic Parkinson’s Syndrome, IPS), up to 15% cases may have genetic components, most common being LRRK2, GBA and PRKN (associated with young onset PD). In some cases it has also been linked to exposure to certain pesticides, herbicides, and industrial chemicals. One such compound called MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) accumulates in the mitochondria and generates free radicals, which can cause damage to basal ganglia and hence lead to PD. Latest research is also suggestive of alpha synuclein aggregation playing a role in the pathogenesis of PD. The earliest histopathological changes are hence seen in the myenteric plexus of the gastrointestinal tract, which then progresses to involve the dorsal motor nucleus of the vagus nerve and sleep centers in the ponto-medullary brainstem.
Many known figures in the world history have been affected by Parkinson’s disease including Pope John Paul II, Adolf Hitler, Mao Zedong, Michael J Fox and notably world heavyweight boxing champion Muhammad Ali, in his case repeated hits to his head is considered a risk factor to cause “dementia pugilistica” a neurode generative condition with Alzheimer’s like dementia. Neurode generation is a serious issue for boxing or for any traumatic brain injury for that matter.
Patients typically have constipation, poor sense of smell and REM sleep disorder preceding the motor symptoms by around 10-15 years. Patients most commonly present with the earliest symptom of tremor. The tremor is usually present at rest and sometimes has classic pin rolling features involving the thumb and the index finger; it can disappear for some time while doing a task but returns when the patient is distracted. In cases where PD is not tremor dominant, patients usually present with the cardinal features of “overall slowness” or bradykinesia, mask facies, muffled speech (hypophonia), small handwriting (micrographia) etc. Patients can take a long time to do their usual daily activities and walk slowly. When prompted about mood or sleep issues, patients might elaborate on feeling depressed and can give a history of movements in their sleep, likely REM sleep disorder. Other autonomic features that a patient of PD might have include urinary retention, erectile dysfunction and orthostatic hypotension. Patients with advanced disease can also present with memory decline due to the neurodegenerative changes of the brain.
On examination, patients have the characteristic cog-wheel rigidity which can be elicited by slow rotatory movements of their wrists. Patients can appear to be stiff, they have shortened stride while walking and arm swing is typically reduced asymmetrically. They walk with a stooped posture and have to take multiple short steps to turn around. On pulling them back suddenly, called the posterior pull test, patients take a lot of steps to catch themselves or may even fall.
In classic PD cases, the patient has tremor of one hand in stage 1. This can progress to the other hand in stage 2. Stage 3 is characterized by mild balance problems, which can worsen causing falls in stage 4 needing cane or a walker to walk and if it continues to worsen, in stage 5 patients can be wheelchair or bed bound. Not all patients progress to stage 5 and brain imaging such as (Dopamine Transporter, DaT) scan is not usually a good prognostication tool.
The PD tremor is most commonly mistaken for an essential
tremor and it remains refractory of usual treatment of propranolol, primidone etc. In such situations, emphasis should be put on looking out for other clinical features of PD like bradykinesia and gait disturbances.
Progressive supranuclear palsy (PSP) can have similar features of bradykinesia, rigidity and gait disturbances but patients may also have vertical gaze paralysis and falling en-block while sitting which is not a feature of PD and MRI Brain of PSP patient may show midbrain atrophy which is described as “Hummingbird” sign.
Patients of Lewy Body Dementia (LBD) have many features of Parkinson’s but those symptoms usually tend to occur after dementia symptoms. In contrast dementia is progressively developed later in the course of disease in PD patients due to overall neurodegeneration. In addition, LBD patients have very vivid visual hallucinations along with wide mood fluctuation which are not a feature of PD, however PD dementia patients may get hallucination or psychosis which is treated with pimavanserin. Ischemic or hemorrhagic stroke, mass lesions, hydrocephalus and Wilson’s disease can be excluded using imaging techniques such as MRI brain.

The diagnosis of PD is primarily a clinical one. A comprehensive examination and proper staging of PD can be done using Unified Parkinson’s Disease Rating Scale (UPDRS) which is a gold standard tool to measure not only the severity and progression of PD but also helpful in monitoring the response to medications. While evaluating the patient it is also imperative to go over their list of medications to exclude the possibility of drug-induced PD. Traditional antipsychotic medications are most implicated in such a condition.
In clinically uncertain cases nuclear imaging DAT-SPECT scan may be helpful, however routine use of this test should be discouraged. A clear clinical improvement after levodopa treatment provides the best confirmation of PD.
There is no cure for PD at this time, however since the pathogenesis of PD involves loss of dopaminergic neurons, the primary mode of treatment is replenishing the dopamine levels with medications such as levodopa with carbidopa, which may also be used in combination with other classes of medications including Dopamine Agonists, COMT Inhibitors, MAO-B Inhibitors, and Anticholinergic agents. Treatment is individualized to the patient and adjusted over time based on symptoms, side effects and tolerability. Dopamine agonists like pramipexole, or ropinirole can be used in younger patients with the advantage of lesser side effects. If a patient primarily has tremor only, amantadine or anticholinergics may be used. In advanced stages of PD, patients may have psychosis with visual or auditory hallucinations and delusions. Pimavanserin, a serotonin 5-HT2 receptor antagonist is the only FDF approved treatment for psychosis associated with PD.
Most PD medications provide good improvement in symptoms for the first 3 to 6 years, but with the natural progression of the disease, results can decline with time. Levodopa-Carbidopa can have the “on-off” phenomenon where symptoms may worsen during the “off” periods. Apomorphine, a dopamine agonist, is the only FDA approved medication which can be used for symptom control during the off periods.
Typical Dopamine Transporter Ligands Single Photon Emission Tomography (DaT-SPECT) scan findings in patients with Idiopathic Parkinson’s Syndrome (IPS) showing reduced striatal DAT availability compared with a normal finding. The reduction is often left/right asymmetrical, usually more pronounced in the hemisphere contralateral to the clinically dominant side. The posterior “tail” of the putamen is almost always most strongly affected. The motor symptoms of IPS manifest only after a DAT loss of about 50% in the putamen. The atypical neurodegen erative parkinsonian syndromes, especially Progressive Supranuclear Palsy (PSP) and Multiple System Atrophy (MSA) of the parkinsonian type show similar patterns of findings on DAT-SPECT as IPS.
PD being a multi system disease requires a multi system ap proach. Patients can benefit a lot with physical therapy, like LS VT-BIG (Lee Silverman Voice Treatment), which encompasses physical therapy to improve their gait and balance coupled with speech therapy to address the hypophonia which can be pres ent. Patients should be encouraged to have an active lifestyle.
Continued on page 20
Continued from page 19
Other features of PD including depression, constipation. REM sleep disorders should also be managed concomitantly. In long-standing or medically refractory cases of at least 4 years of PD, Deep Brain Stimulation (DBS) of the subthalamic nucleus (STN) or globus pallidus interna (GPI) is a great option to provide relief with disabling symptoms. In summary, early accurate diagnosis by a neurologist experienced in PD along with a multidisciplinary approach should be used for improving the symptoms and quality of life of PD patients.
Dr. Jaivir Rathore, A triple board-certified top-rated neurologist trained at the Johns Hopkins and the Cleveland Clinic, Harvard University journal published neuroscientist and the Medical Director of Falcon Advanced Neurology & Epilepsy Freedom Center (FANEFC) in Orlando FL with additional clinics serving the largest retirement community of the world in The Villages FL provides comprehensive neurology care including movement disorders such as Parkinson’s disease. FANEFC is “Care Connected” with the Mayo Clinic, Jacksonville FL for surgical cases including DBS for PD.
Final Trim: 8.125” wide x 10.75” tall
Final Trim: 8.125” wide x 10.75” tall
Binding: Saddle-stitched
Binding: Saddle-stitched
Florida MD magazine is a four-color monthly medical/business magazine for physicians in the Central Florida market.
Florida MD MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD
Cover: Sheet fed on 100 lb. gloss text
Cover: Sheet fed on 100 lb. gloss text
Body: Sheet fed on 70 lb. gloss text
Body: Sheet fed on 70 lb. gloss text
Preferred File Format: Press optimized, Acrobat PDF/X-1a compliant files are the preferred format for final artwork. We do not accept ads created in Microsoft programs.
Preferred File Format: Press optimized, Acrobat PDF/X-1a compliant files are the preferred format for final artwork. We do not accept ads created in Microsoft programs.
File Transfer: All digital files should be provided on a CD or DVD and must be accompanied by a hard copy/proof. Electronic transfers can be sent using www.YouSendIt.com.
It goes to 3,000 physicians, at their offices, in the nine-county area of Brevard, Volusia, Seminole, Orange, Lake, Osceola, Sumter, Flagler and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD magazine.
File Transfer: All digital files should be provided on a CD or DVD and must be accompanied by a hard copy/proof. Electronic transfers can be sent using www.YouSendIt.com.
Images: Images must be 300dpi, CMYK and saved in a TIFF or EPS format. Noncompliant images may not print correctly and Florida MD does not assume responsibility for any discrepancies that may occur.
CUSTOMIZE YOUR EMAIL MESSAGE
Customize your email broadcast to healthcare providers in specific counties or throughout Central Florida. Rates available upon request.
Fonts: Include all fonts with your source files. Font substitutions will be made for missing or noncompliant fonts.
Images: Images must be 300dpi, CMYK and saved in a TIFF or EPS format. Noncompliant images may not print correctly and Florida MD does not assume responsibility for any discrepancies that may occur. Fonts: Include all fonts with your source files. Font substitutions will be made for missing or noncompliant fonts.
Charges: Submit final, approved artwork only. Production charges may apply to your supplied ads if they do not comply with our specifications. Charges are billed at an hourly rate with a half-hour minimum.
Charges: Submit final, approved artwork only. Production charges may apply to your supplied ads if they do not comply with our specifications. Charges are billed at an hourly rate with a half-hour minimum.
Reach medical providers in targeted areas of Central Florida and statewide with your custom email message. Contact Florida MD for details.
Insert size: 7.875” x 10.75” or smaller. Paper stock not to exceed 100 lb. text. Inserts count as one insertion toward frequency. All single-page inserts are tipped in. Please contact Florida MD for quantity to supply or a custom layout estimate.
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.

Please call 407.417.7400 for additional materials or information.
Please call 407.417.7400 for additional materials or information.

Relieve Symptoms of:
• Acne
• Allergies
• Asthma
• Cold & Flu
• Cystic Fibrosis
• Dermatitis
• Ear Infections

• Eczema
• Sinusitis
100% NATURAL TREATMENT

Kerri and Clay: “My son’s allergy medicines were causing terrible side effects. Now that we have been coming to The Salt Room we have been able to control his symptoms with salt therapy.”




Joseph Cannizzaro, MD: “I have been recommending The Salt Room for years. It has helped my patients with respiratory nuisances and skin problems, reducing symptoms while we address the root cause to improve their long-term quality of life.”
