MARCH/APRIL 2024 • COVERING THE I-4 CORRIDOR AdventHealth Invests in Helping Physicians Feel Whole





















CELEBRATING DOCTORS’ WEEK AdventHealth.com OUR DOCTORS PIONEER WHAT OTHERS PRACTICE.
advances
clinical
us. 24-CFD-01906
AdventHealth physicians are dedicated to enhancing patient care through innovative therapies, technological
and
breakthroughs. It’s an extraordinary commitment that continues to push the boundaries of what is possible in health care. We thank our doctors for their trailblazing work that continues to inspire the healing power of the human spirit in all of

Living whole means being physically healthy, mentally well, spiritually connected and socially content. It’s about fulfilling potential and overcoming challenges.
As the pioneer and leading practitioner of whole-person care for more than 150 years, AdventHealth has grown to become one to the largest health care providers in the United States with more than 92,000 professionals working to extend the healing ministry of Christ across nine states. Within Florida, AdventHealth employs over 57,000 team members and 4,000 physicians and advanced practitioners.
AdventHealth believes helping physicians feel whole is essential to fulfilling its mission and has implemented numerous innovative initiatives in recent years designed to:
• Promote physician leadership, recognition and governance.
• Foster physician well-being.
• Ease physician workload and stress through the use of carefully vetted artificial intelligence (AI) tools.
– PARKINSON’S
ONE OF THE MOST

FLORIDA MD - MARCH/APRIL 2024 1 DEPARTMENTS 2 FROM THE PUBLISHER 8 DERMATOLOGY 9 MARKETING YOUR PRACTICE 10 PULMONARY AND SLEEP DISORDERS 12 HEALTHCARE LAW 14 ORTHOPEDICS 16 PEDIATRICS contents MARCH/APRIL 2024 COVERING THE I-4 CORRIDOR
COMMONLY
NEUROLOGICAL CONDITIONS 20 YOUR PATIENT
NOT HAPPY WITH THEIR KNEE OR HIP REPLACEMENT. WHAT’S NEXT?
SESSION 2 - NEGOTIATING LEASES 4 COVER STORY
18 WHEN THE TREMOR ISN’T ESSENTIAL
DISEASE:
MISDIAGNOSED
IS
22
PHOTO: PROVIDED BY ADVENT HEALTH
PHOTO: PROVIDED BY ADVENT HEALTH
Iam pleased to bring you another issue of Florida MD. Sometimes a patient may have the opportunity to participate in a clinical trial. Sometimes a patient may need specialized treatment that is not available in Central Florida. And sometimes there’s no money for that patient to get to those places. Fortunately there is Angel Flight Southeast to get those patients where they need to go. I asked them to tell us about their organization and how you, as physicians, can help. Please join me in supporting this truly wonderful organization.
Best regards,
 Donald B. Rauhofer Publisher
Donald B. Rauhofer Publisher


ANGELS ON EARTH HELP PATIENTS GET TO LIFESAVING MEDICAL TREATMENT
Everyone knows angels have wings! But did you know in Florida and many parts of the nation they have engines and tails with dedicated volunteers who donate lifesaving services every day? Leesburg, Fla.-based Angel Flight Southeast is a network of approximately 650 pilots who volunteer their time, personal airplanes and fuel to help passengers get to far-from-home medical care. A member of the national Air Charity Network, Angel Flight Southeast has been flying passengers since 1993.
Almost all of its passengers are chronic-needs patients who require multiple, sometimes 25-50 treatments. Passengers may be participating in clinical trials, may require post-transplant medical attention or are getting specialized treatment that is not available near home. Each passenger is vetted to confirm medical and financial need and is often referred to Angel Flight Southeast by medical personnel and social workers.
Angel Flight Southeast “Care Traffic Controllers” arrange flights 24 hours a day, 365 days a year. In the event of a transplant procedure, the Care Traffic Controllers have precious minutes to reach out to its list of volunteer pilots who have agreed to be prepared on a moment’s notice to fly a patient to receive his or her potentially lifesaving organ.
The organization is completely funded through donations by individuals and organizations. A typical Angel Flight Southeast pilot donates $400 to $500 in services-per-trip. In fact, Angel Flight Southeast has earned the Independent Charities of America Seal of Approval as a good steward of the funds it generates from the public. Each $1 donated generates more than $10 worth of contributed services by Angel Flight Southeast.
The charity always seeks prospective passengers, volunteer pilots and donations. For additional information, please visit https://www.angelflightse.org or call 1-888-744.8263.
ADVERTISE IN FLORIDA MD
For more information on advertising in Florida MD, call Publisher Donald Rauhofer at (407) 417-7400, fax (407) 977-7773 or info@floridamd www.floridamd.com
Email press releases and all other related information to: info@floridamd.com
PREMIUM REPRINTS
Reprints of cover articles or feature stories in Florida MD are ideal for promoting your company, practice, services and medical products. Increase your brand exposure with high quality, 4-color reprints to use as brochure inserts, promotional flyers, direct mail pieces, and trade show handouts. Call Florida MD for printing estimates.
Publisher: Donald Rauhofer
Photographer: Donald Rauhofer / Florida MD
Contributing Writers: JJohn “Lucky” Meisenheimer, MD, Daniel T. Layish, MD, John Meisenheimer, VII, MD, Sonda Eunus, MHA, Julie Tyk, JD, Paul J. Watkins, George Haidukewych, MD, Frank Ricci
Art Director/Designer: Ana Espinosa
Florida MD is published by Sea Notes Media,LLC, P.O. Box 621856, Oviedo, FL 32762. Call (407) 417-7400 for more information. Advertising rates upon request. Postmaster: Please send notices on Form 3579 to P.O. Box 621856, Oviedo, FL 32762. Although every precaution is taken to ensure accuracy of published materials, Florida MD cannot be held responsible for opinions expressed or facts expressed by its authors. Copyright 2024 Sea Notes Media. All rights reserved. Reproduction in whole or in part without written permission is prohibited. Annual subscription rate $45.
FLORIDA MD - MARCH/APRIL 2024 2
FROM THE PUBLISHER

AdventHealth Invests in Helping Physicians Feel Whole
By Staff Writer
Living whole means being physically healthy, mentally well, spiritually connected and socially content. It’s about fulfilling potential and overcoming challenges.
As the pioneer and leading practitioner of whole-person care for more than 150 years, AdventHealth has grown to become one to the largest health care providers in the United States with more than 92,000 professionals working to extend the healing ministry of Christ across nine states. Within Florida, AdventHealth employs over 57,000 team members and 4,000 physicians and advanced practitioners.
AdventHealth believes helping physicians feel whole is essential to fulfilling its mission and has implemented numerous innovative initiatives in recent years designed to:
• Promote physician leadership, recognition and governance.
• Foster physician well-being.
• Ease physician workload and stress through the use of carefully vetted artificial intelligence (AI) tools.
BATTLING THE BURDEN OF BURNOUT — BEYOND RESILIENCE
National physician burnout surveys reveal nearly half of all physicians in the U.S. say they are feeling burned out which has been defined as long-term, unresolved, job-related stress leading to exhaustion, cynicism, depersonalization and decline in a sense of personal accomplishment.
While the concept of burnout is not new, it grew significantly during the COVID-19 pandemic and remains high today. In
fact, the Medscape Physician Burnout & Depression Report: “We Have Much Work to Do” released in January 2024 compiled the input of over 9,000 U.S. physicians across 29 specialty areas and revealed:
• Forty-nine percent of physicians said they felt burned out, and 20% said they were depressed.
• Eighty-three percent of doctors surveyed cited professional stress as the primary contributor to their burnout and/or depression.
• The number of work-related bureaucratic tasks was cited as the primary reason for burnout (62%). Spending too many hours at work (41%) and lack of respect from administrators, employers and coworkers (40%) also were contributing factors.
• Physicians in emergency medicine reported the highest burnout rates (63%) followed by OB/GYNS, oncologists, pediatricians and family physicians.
“I often frame physician burnout as death by 1,000 cuts,” explains AdventHealth Apopka Chief Medical Officer Omayra Mansfield, MD, MHA, FACEP, who oversees physician experience and well-being for AdventHealth’s Central Florida Division. “It typically isn’t one incident but an accumulation of stressors or injuries over time.”
Dr. Mansfield also shares that too often health care organizations and leaders have simply told physicians to build resilience as a solution to their burnout.

FLORIDA MD - MARCH/APRIL 2024 4 COVER STORY
AdventHealth Medical Group providers meet up to practice meditation and mindfulness.
PHOTO: PROVIDED BY ADVENT HEALTH

“Resilience is defined as the capacity to withstand or recover quickly from difficulties,” says Dr. Mansfield. “Our efforts must be about so much more than that. Even the most durable bone in the body is susceptible to a stress fracture due to repetitive force and overuse. To help our physicians feel truly whole, we must recognize the daily insults and help them heal.”
COLLABORATING TO CREATE A CULTURE FOCUSED ON FEELING WHOLE
AdventHealth believes in viewing its physicians through the same service standards they apply to caring for their patients:
• Keep Me Safe
• Love Me
• Make It Easy
• Own It
In addition, AdventHealth recognizes that achieving improvement in physician well-being must be a collaborative, organizational effort. To that end, AdventHealth regularly engages physicians throughout the system to provide feedback, share ideas and evaluate opportunities.
“It is important that our work is physician-generated and physician-led,” explains Dr Mansfield. “We want to empower our physicians to speak up about the challenges and obstacles they face. We may not be able to fix everything, but we can certainly help remove some of the rocks in their shoes. Our goal is to create an environment where our physicians can thrive, and in doing so, allow them to successfully provide the most exception care for our patients and communities.”
Double board-certified radiation oncologist and lifestyle medicine specialist Amber Orman, MD, who serves as the first-ever chief wellness officer for AdventHealth Medical Group, agrees.
“When I first took on this role in 2021, during the COV-
ID-19 pandemic, we focused initially on physicians’ well-being,” says Dr. Orman. “While this is still an essential part of my work, we quickly expanded our focus to organizational well-being. We recognize that creating a supportive work environment that fosters wholeness is essential.”
EMPOWERING PHYSICIANS BY ENHANCING ENGAGEMENT, BUILDING COMMUNITY AND FOSTERING LEADERSHIP
AdventHealth’s whole-person approach isn’t just about healing what’s wrong, it’s also about celebrating what’s right and encouraging personal and professional growth.
Physician Recognition Program
“As we engaged our physicians in identifying new opportunities to enhance their experience and well-being, the need for positive recognition kept rising to the top so we created a program to celebrate the wins,” shares Dr. Mansfield.
With the “Physician Serving in Excellence” recognition program, Dr. Mansfield and her team created a QR code that all AdventHealth physicians can easily access. It links to three simple questions:
• What physician should be recognized?
• Which AdventHealth campus do they work at?
• Why should they be recognized?
Physicians are then recognized in an appropriate, individualized way — it could be at a medical staff meeting or in private. The physician receives two lapel pins — one to wear and one to “pay it forward” to another physician they would like to acknowledge for a job well done.
“This program has really caught on and fostered a positive, caring culture of lifting each other up,” says Dr. Mansfield. “In fact, it has been so successful here in Florida that AdventHealth
FLORIDA MD - MARCH/APRIL 2024 5 COVER STORY
AdventHealth providers and staff celebrate interventional radiologist Donald Joe “D.J.” Perry, MD, who was recently named a “Physician Serving in Excellence” as part of AdventHealth’s ongoing physician recognition campaign.
PHOTO: PROVIDED BY ADVENT HEALTH
has implemented it company-wide across all nine states where we have facilities.”
Dr. Mansfield also shares positive patient comments gathered through the system’s Press Ganey surveys with both individual providers and hospital leadership.
“These efforts have really helped to show our physicians that we see them and appreciate them.”
Physician Team Leadership Program
AdventHealth has also implemented a Physician Team Leadership Program. A partnership between the AdventHealth Leadership Institute and Harvard Business Publishing, it is designed to equip physicians with leadership skills to help address evolving and unexpected challenges throughout the health care industry.
Over six months, a cohort of 50 AdventHealth physicians, leaders and clinicians participate in a series of in-person and virtual learning sessions that cover a variety of topics:
• How to lead authentically to promote trust and psychological safety.
• How to use powerful questions to connect meaningfully.
• How to lead effectively where volatility, uncertainty, complexity and ambiguity co-exist in a rapidly changing landscape.
The program concludes with a four-day experience at Harvard University in Boston that focuses on improving patient outcomes and lowering costs amidst the competitive forces driving health care. Physicians who complete the Physician Team Leadership Program also earn Continuing Medical Education (CME) credits.
Enhancing Physician Engagement and Governance Models within AdventHealth Medical Group
As a group of employed physicians, AdventHealth Medical Group (AHMG) believes in seeking physician feedback to guide positive change. This led to several changes in recent years, in-
cluding improving contracts, providing additional CME opportunities, addressing staffing and workflow issues, adjusting the vacation policy and ensuring appropriate technology.
“These are all things that left unaddressed can cause moral injury over time,” explains Dr. Orman. “Our goal is to find, fix and communicate progress along the way. We want our physicians to feel valued and heard.”
AHMG has also changed its governance structure to give physicians and advanced practice providers (APPs) more opportunities to participate in administrative leadership.
“This not only gives clinicians a stronger voice at the leadership table but also promotes value,” shares AHMG Orlando Chief Physician Executive Eric Deshaies, MD, MBA. “The medical group structure has quality represented by clinicians and cost control represented by the business executives.”
IMPROVING PHYSICIAN WELL-BEING
AdventHealth has also invested in a variety of programs designed to support the mental, emotional and spiritual wellness of its physicians.
Center for Physician Well-being
AdventHealth’s Center for Physician Wellbeing offers various types of virtual and in-person counseling to meet the needs of physicians, advanced practice providers and their family members. This includes individual counseling, martial or couples counseling, family counseling and group therapy designed to help participants learn interventions and strategies to reduce symptoms, improve functioning and develop coping skills.
AdventHealth recognizes that physicians are often reluctant to seek formal counseling services out of privacy concerns or fear of judgement by colleagues. As a result, they are working to not only destigmatize seeking mental health support, but also ensure physicians’ privacy and make it easy for them and their families to access the services they need to feel whole and thrive in both their personal and professional lives.

All credentialed AdventHealth physicians are eligible for six free counseling sessions per year, which are also redeemable by family members. Additional services include coaching and workshops where physicians can give and receive support from fellow providers.
HEAL: Healer Wellness Summits and Chats
In addition to the Center for Physician Wellbeing, Dr. Orman has applied her expertise in the field of lifestyle medicine to create two additional resources that are designed to help physicians and advanced practitioners thrive:
FLORIDA MD - MARCH/APRIL 2024 6 PHOTO: PROVIDED BY ADVENT HEALTH COVER STORY
Double board-certified radiation oncologist and lifestyle medicine specialist Amber Orman, MD, who serves as AdventHealth Medical Group’s chief wellness officer, leads a recent “HEAL: Healer” session designed to help providers make positive lifestyle changes to improve their health and well-being.
• HEAL: Healer Wellness Summits — HEAL stands for Healthy Eating Active Lifestyle and is based on a program Dr. Orman designed to educate and inspire cancer patients to make positive life changes to improve their health. The day-long, quarterly events feature a variety of speakers who address topics like burnout, mindfulness, acupuncture, yoga and plant-forward nutrition.
• HEAL: Healer Chats — These virtual, hour-long monthly discussions include wellness and lifestyle information from both Dr. Orman and guest speakers. They are designed to help physicians set personal lifestyle goals while also building community. Some of this year’s topics include personal relationships, nutrition, yoga, mindfulness, physical movement, sleep, work relationships and managing conflicts, cancer, gratitude, managing stress and communication.

Additional AdventHealth Medical Group Wellness Events and Initiatives
AdventHealth Medical Group offers additional opportunities to its employed physicians that promote wellness such as support groups for those with similar interests, lifestyle-based education for CME credits, family-focused events, a trail club, and Cabana: a mental health app designed specifically for health care professionals.
“We believe in caring for our care team, and there are no onesize-fits-all solutions,” shares Dr. Orman. “We want to offer a variety of opportunities that make it easy for our physicians to invest in themselves while also building supportive bonds with each other.”
HARNESSING ARTIFICIAL INTELLIGENCE TO EASE PHYSICIAN WORKLOAD
Since bureaucratic tasks like charting and paperwork are one of the leading contributors to burnout, AdventHealth is planning to introduce artificial intelligence (AI) technology to make daily clinical operations and functions more efficient while also providing physicians more focused face time with their patients. AdventHealth has established a companywide AI Advisory Board that consists of clinical leaders from multiple disciplines to guide these efforts.
One example currently being implemented is an ambient listening tool used during physician/patient visits so that the doctor focuses solely on talking to the patient while the AI tool transcribes the relevant information for the patient’s record and documentation in a confidential, HIPAA-compliant manner. After the visit, the doctor simply reviews, adjusts as needed and signs off on the visit.
“We only implement AI tools after a thorough vetting and with support from those who will be using the technology,” explains AdventHealth Central Florida Division Chief Clinical Officer Victor Herrera, MD, who chairs AdventHealth’s companywide AI board. “By having these conversations in a facilitated environment, we can help leaders make sense of the noise and better support a responsible path forward. We want to leverage AI in a way that helps our physicians do their jobs and enhances the high-quality, personalized, whole person care we provide. These technologies come with the promise of revolutionizing healthcare and we have the responsibility of accelerating their adoption, but we need to make sure we do it in a way that is ethical and responsible. I like to think about it as staying safe in the fast lane”
A LONG-TERM COMMITMENT
Looking ahead, AdventHealth is further exploring ways to provide programs and foster well-being for physicians that are both employed within the medical group as well as credentialed on medical staff.
“Despite the obstacles and challenges we all face as physicians, we can still feel happy, healthy and whole. Finding ways to support our physicians efficiently, respectfully and adequately is essential, sacred work,” shares Dr. Orman
Dr Mansfield concurs. “As an organization, we believe in loving each other well, healing wounds when we can, helping each other grow toward our goals and aspirations, and accompanying one another along the journey so we can live our lives in community and service.”

FLORIDA MD - MARCH/APRIL 2024 7
A group of AdventHealth providers visit Freight Farm, a hydroponic farm inside a freight-shipping container, created to provide fresh leafy vegetables to hospital staff and guests and to encourage the community to consume fresh produce and get back in touch with nature.
PHOTO:
PROVIDED BY ADVENT HEALTH
COVER STORY
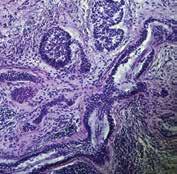
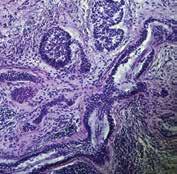
Not All Basal Cell Carcinomas Are Created Equal
By John “Lucky” Meisenheimer, MD and John Meisenheimer, VII
Occasionally a patient will tell me their “doctor friend” recommended that they don’t need treatment for a basal cell carcinoma because it will never hurt you. “Doc, he said it’s only a basal cell carcinoma.” Dermatologists fully recognize this as a genuinely cringe-worthy statement. You don’t need to see too many people missing various parts of their facial anatomy to know this advice is blatantly wrong. Even in this modern time of medical miracles, people still die from neglected basal cell carcinomas. When pressed for the name of their “doctor friend,” it usually comes up as I don’t remember their name, or it ends up being “Doctor Google.”
It is true a superficial basal cell carcinoma on the torso probably would take years and years for it to cause any sort of significant morbidity to a patient. But, on the other hand, even a small basal cell on the torso will continue to grow if left untreated slowly. What might have been a simple, inexpensive procedure now, a decade later, has turned into a monster of aggravation, discomfort, and cost.
Although metastatic disease risk is low with basal cell carcinomas, it is certainly not zero. Several people die each year from basal cell carcinoma. Even more, patients can have disfiguring bouts with cancer losing various parts of anatomy such as nose, ears, eyes, etc. What a lot of patients and even some physicians are not aware of is that not all basal cell carcinomas are created equal. There are several different histologic growth patterns. These varying histologic types can each behave differently and require different treatment plans.


As mentioned before, a superficial basal cell carcinoma is probably not going to cause a great deal of physical damage unless neglected for long periods. There are other types of basal cell carcinomas; morpheaform and sclerosing basal cell carcinomas with infiltrating growth patterns. These cancers left untreated can cause a significant amount of morbidity in shorter periods measured in months, not years. Aggressive basal cell cancers can also become neurotropic, meaning that they “wrap” around a nerve and can track down its length. Neurotropism can be particularly dangerous, especially if this is on the face and affecting a nerve that happens to pass through a foramen into the brain. Clearly, not a good scenario.
Basal cell carcinomas, limited to the skin, tend to be very amenable to treatment in a variety of different ways. Even as a Mohs surgeon I can think of at least half a dozen different ways that I have treated basal cell carcinomas. Not all basal cell carcinomas need Mohs surgery. Each case of basal cell carcinoma should be evaluated individually and in consideration as to the best method of treatment based on its histologic growth pattern, location, and physical condition of the patient.
The great news about basal cell carcinoma, even though it is the most common type of skin cancer and millions are treated each year, only a tiny percentage of these end up causing death in patients. When someone says I would much rather have a basal cell carcinoma than a melanoma, there is a caveat; if you die from a basal cell carcinoma, you are just as dead as if you were to die from melanoma. Happily, most of the time, with early diagnosis and treatment, you don’t have to die from either. Basal cell carcinoma is called cancer for a reason. Give it its respect that it is due, or otherwise, you may regret saying, “oh, you don’t have to worry about it, it’s only a basal cell carcinoma.”
Lucky Meisenheimer, M.D. is a board-certified dermatologist specializing in Mohs Surgery. He is the director of the Meisenheimer Clinic – Dermatology and Mohs Surgery. John
VII is an MD practicing in Orlando.




FLORIDA MD - MARCH/APRIL 2024 8 DERMATOLOGY
Meisenheimer,
PHOTO: JOHN MEISENHEIMER, VII, MD
Pathology of an infiltrative basal cell carcinoma.
Infiltrative Basal Cell carcinoma of the forehead.
Superficial Multifocal BCC.
Nodular basal cell carcinoma.
PHOTO: JOHN MEISENHEIMER, VII, MD
Neurotropic basal cell carcinoma.
Sclerosing basal cell carcinoma.
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
PHOTO: JOHN MEISENHEIMER, VII, MD
Is Your Online Reputation Costing You Patients?
By Sonda Eunus, MHA, CMPE
What does your online reputation say about your practice? If you have a negative online reputation, you are missing out on new patients every day. Most medical practices now get the majority of their new patients through Google and other search engine queries, such as “Pediatrician in Orlando”. If your practice appears in these searches, the most common next step for a potential new patient would be to check out your reviews – what are other patients saying about your practice? It has been reported that 90% of consumers read online reviews before visiting a business and that online reviews influence 67% of purchasing decisions (Bright Local). For this reason, it is incredibly important to pay attention to the rating and reviews that your practice has on search engines, social media platforms, and local online business directories.
However, despite the importance of cultivating a positive online reputation, only 33% of businesses report actively collecting and asking for reviews (1). One great process to set in place at your practice is asking for patient reviews after each patient visit. It can be as simple as training your front office staff to ask each patient how their visit went while checking them out, and if they receive favorable feedback then they can ask the patient to please leave a review on Google or Facebook about their experience. If they receive negative feedback, this feedback should be taken very seriously, and management should be notified as soon as possible so that the issue can be mitigated before the patient decides to post a negative review.

Setting up an automated text or email campaign that asks each patient for their feedback after their appointment is also a great way to improve your online reputation as well as to correct any issues that may be occurring at your practice. When you receive feedback from patients, you are then able to prompt them to leave a public review on Facebook, Google, Yelp, Healthgrades, or other applicable review platforms. However, you must be aware that legally, you are not allowed to only direct people with favorable feedback to leave reviews, which is known as review-gating – so if you are implementing an automated system like this, just make sure that you are aware of this limitation. There are online reputation management platforms which allow you to customize the messages that people see when they leave negative feedback as opposed to positive feedback, but both of those messages must still offer the option to leave a public review. However, if you create your message in such a way as to communicate to the patient who may leave negative feedback that you are working hard on resolving the issue and that someone will be in touch shortly, that may prevent them from leaving a public negative review.
When you receive a public review on Google, Facebook, or other review sites, make sure that you respond to it – either by thanking them for a good review or by asking them to contact you to discuss how you can improve their experience. Do not argue or try to defend yourself online – try to speak about it with them privately, fix the issue, and ask them to remove the review if possible. When you receive great reviews, make sure to cross-share them on your various social media platforms. You should also create a “Reviews” page on your website and add all great reviews to this page. This instantly adds credibility to your website.
Finally, make sure that when you look over the feedback and reviews that you receive, you are paying attention to what the negative reviews are saying – this is a great opportunity to identify current process challenges and improve your patients’ experience at your practice. Need help managing your practice’s online reputation? Visit www.lms-plus.com to see how Leading Marketing Solutions can help.
Sonda Eunus is the CEO of Leading Marketing Solutions, a Marketing Agency working with Medical Practices and other Businesses to help them identify the best marketing strategies for their business, create a strong online presence, and automate their marketing processes for a better return on their Marketing budget. Learn more about Leading Marketing Solutions at www.lms-plus.com.
FLORIDA MD - MARCH/APRIL 2024 9 MARKETING YOUR PRACTICE
What’s New in the Treatment of Mild Obstructive Sleep Apnea and Primary Snoring?
By Tabarak Qureshi, MD FCCP
THE FIRST FDA-AUTHORIZED DAYTIME THERAPY: EXCITEOSA®
SNORE... SNORE… SNORE…
We all know of someone who snores, but when people are informed of their snoring, the typical response is denial and disbelief. The truth of the matter is that snoring is extremely common, but most people don’t understand why it happens.
Snoring is generated when the upper airway/pharyngeal muscles relax and as air flows through a relaxed posterior airway. In some people with a crowded posterior airway, these sounds and vibrations result in mild obstructive sleep apnea (OSA), which is identified by having an AHI (apnea hypopnea index) between 5-15 events/hour. The repeated airway obstructions result in sleep disruption, blood pressure swings, and recurrent nocturnal asphyxia and hypoxia resulting in increased sympathetic nervous system activation during sleep. Traditionally, there has not been any significant treatment modality for primary snoring. Mild OSA has been treated primarily with auto-CPAP/PAP or mandibular advancement devices along with lifestyle modifications (weight loss, drinking, and smoking cessation). The most notable change is noted in the upper airway and the genioglossus muscle. This collapsibility is higher in mild OSA compared to primary snoring. In non-snorers, there is an ability to prevent collapsibility of the upper airway and have functional mechanisms that prevent collapse.
The genioglossus is considered the largest muscle of the airway and the most important dilatory muscles during sleep onset. With sleep onset, there is rapid reduction in pharyngeal and tongue muscle contractility. Over time the respiratory stimulus and genioglossus activity progressively increase during stable non-REM sleep. However, a notable number of individuals fail to effectively increase genioglossus activity or achieve inadequate tongue muscle activation to overcome the obstruction prior to the arousal. Therefore, there is a failure of the tongue muscles to generate an appropriate protective response from a neural drive or responsiveness perspective.
The first proof of concept of daytime stimulation of the tongue was presented by Wiltfang in 1999 (28). He demonstrated using a TENS like stimulation during daytime for two weeks resulted in a significantly reduced respiratory disturbance index (RDI), from 13.2/hour to 3.9/hour, oxygen desaturation index improved as did minimum oxygen saturation from 75% to 88%. In another prospective placebo controlled randomized trial of daytime tongue stimulation vs TENS type stimulation the number of snoring epochs decreased significantly (from 63.9±23.1 epochs per hour to 47.5±31.2; P<.05).
EXCITEOSA®:

The eXciteOSA device targets the intrinsic and extrinsic pharyngeal and tongue muscles by delivering neuromuscular electrical stimulation to the tongue with the purpose of increasing muscle responsiveness and preventing excessive relaxation. The device has three components:
1. Washable flexible electrode mouthpiece with an electrode array that fits onto the tongue.
2. Rechargeable control unit that attaches to the mouthpiece via a USB connection.
3. Smartphone App that manages the functions of the device. The mouthpiece is placed in the mouth, on the tongue with the two electrodes located above and two below the tongue. Therapy consists of a series of pulse bursts with rest periods for 20 minutes during the wakefulness state for a period of 6 weeks. With daily use of eXciteOSA, the tongue muscle function improves to prevent the backward collapse of the tongue and hence obstruction of the airway.
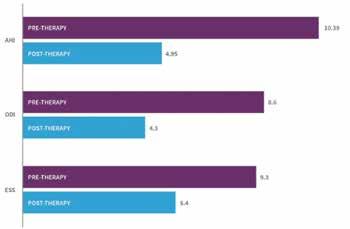
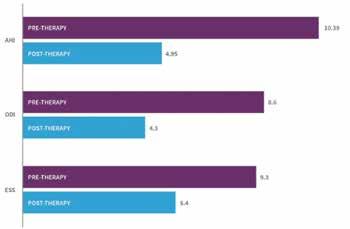
CLINICAL TRIALS DATA
The original trial was a prospective multicenter trial of individuals with primary snoring or mild OSA. Snoring was assessed by the bed partner reporting on a visual analog scale-VAS (ranging from 1-10, 10=unbearable snoring). The snorers sleep quality was recording using the Pittsburgh Sleep Quality Index (PSQI) pretreatment (2 weeks before start of therapy), during treatment phase (6 weeks recorded in last two weeks) and post treatment (2 weeks after stopping therapy).
27 individuals completed the trial (8 women and 19 men), average age 44 years (age range 2568 years), BMI 29.7 (range 20.7-35) and AHI 9 (range 2.5-15).

FLORIDA MD - MARCH/APRIL 2024 10 PULMONARY
Eight primary snorers and 19 had mild OSA.
Results revealed bed partner reported snoring reduced by 52% (p<0.001) with over 80% declaring a reduction of >40%. The change remained statically significant for primary snores and mild OSA patients (VAS reduction 6.6 to 3.6 p<0,001).
Another multicenter clinical trial was undertaken at London University hospital along with other sites in Europe. The objective was to validate the objective measures and assess the reproducibility of the subjective outcomes of the previous study. This was cohort of mild OSA (HST using WatchPAT®) and primary snorers. Two consecutive night studies were conducted before and after the 6-week period. This was supplemented with partner VAS, Epworth Sleepiness Scale (ESS), and PSQI.
125 patients were recruited and 115 (50 primary snorers and 65 mild OSA patients) completed the trial. The average age was 46 (range 24-79 years), 73 males and 42 females, average BMI 27 (range 20-34). For the study population the mean objective percentage of sleep time snoring at >40dB, reduced significantly by 41% (p<0.001). 90% of the participants recorded an objective reduction in their snoring. Clinically significant reduction in snoring time was also reported at snoring intensities of 45dB and 50dB with an improvement of 52% (p<0.001) and 54% (p<0.001) respectively. In mild OSA, 79% showed an average reduction in AHI of 52% (p<0.001) and the post therapy AHI normalized to 4.95. Statistically significant improvements were noted in ESS and PSQI scores as well (p<0.001).
Oral pooling of saliva was most common side effect, with a
small percentage reported tongue discomfort, tooth discomfort, filling sensitivity, gagging, metallic taste and jaw tightness. Prevalence of these symptoms reduced in the six weeks of therapy.
DISCUSSION AND CONCLUSION
Daytime neuromuscular electrical stimulation (NMES) therapy for correction of nighttime airway obstruction is a novel, innovative and probably unconventional therapeutic strategy. The ability to control nighttime sleep disordered breathing without wearing a nighttime device makes this an attractive treatment modality. NMES involves the application of electrical current to induce muscle contractions and has been shown to activate the muscle to a greater extent than voluntary muscle actions. It has
been known to activate motor units that are not otherwise activated. NMES has been shown to change the myofibrillar protein expression to induce a phenotype shift from fatigue prone to fatigue resistant with the strengthening of the cytoskeleton. NMES has been shown to result in metabolic shift from glycolytic to oxidative profiles, increasing intracellular defense against harmful oxygen species, reverse the degeneration of pre and postsynaptic tongue neural morphology associated with ageing and a shift to a higher contractile tension.
eXciteOSA offers a simple and effective method of addressing the above-mentioned process and has been shown to benefit individuals with primary snoring and mild OSA. eXciteOSA provides a targeted retraining tool to stimulate the tongue and the biggest dilatory muscle of the airway – the genioglossus muscle. The clinical trial demonstrated significant reductions in all of the relevant objective measures, 90% of the study population showed reduction in snoring, 79% of the mild OSA population showed a 50% reduction in AHI and ODI resulting in reduction in ESS and PSQI.
Tongue muscle training using eXciteOSA has proven to be effective in reducing multiple indices associated with sleep disordered breathing. Additional studies have been published and accepted for publication and currently underway. eXciteOSA provides a “no nighttime wearable” safe option of therapy for patients and overcomes many of the risks and disadvantages of currently available treatment options.
For more information on this novel daytime therapy option, visit the eXciteOSA website: eXciteOSA.com or email info@signifiermedical.com.
Bibliography available upon request.
Tabarak Qureshi, MD FCCP practices at Central Florida Pulmonary Group. He is Chairman-Division of Pulmonary Medicine at AdventHealth, Director of ICU AdventHealth Altamonte Springs and Director of the Sleep Lab at Central Florida Pulmonary Group.




FLORIDA MD - MARCH/APRIL 2024
FloridaMDMagazine.com Your Medical Business Resource Practice Management Advice Financial Information Pod Cast Interviews with Specialists and Professionals Check out our website at www.floridamd.com! PULMONARY
Understanding Exculpatory Clauses
By Julie A. Tyk, JD.
An exculpatory clause purports to deny an injured party the right to recover damages from a person negligently causing his injury. Cain v. Banka, 932 So. 2d 575 (Fla. 5th DCA 2006). They are disfavored in the law because they relieve one party of the obligation to use due care and shift the risk of injury to the party who is probably least equipped to take the necessary precautions to avoid injury and bear the risk of loss. Applegate v. Cable Water Ski, L.C., 974 So. 2d 1112, 1114 (Fla. 5th DCA 2008). Such clauses are strictly construed against the party seeking to be relieved of liability. Sunny Isles Marina, Inc. v. Adulami, 706 So. 2d 920 (Fla. 3d DCA 1998). Thus, exculpatory clauses are enforceable, only where, and to the extent, that the intention to be relieved from liability is made clear and unequivocal. Tatman v. Space Coast Kennel Club, Inc., 27 So. 3d 108, 110 (Fla. 5th DCA 2009). The wording must be so clear and understandable that “an ordinary and knowledgeable person will know what he is contracting away.” Id. (quoting Gayon v. Bally’s Total Fitness Corp., 802 So. 2d 420 (Fla. 3d DCA 2001)).
The seminal Florida case on exculpatory clauses is the Florida Supreme Court case of Sanislo v. Give Kids The World, Inc., 157 So. 3d 256 (Fla. 2015). Give Kids the World, Inc. (“GKTW”) provided free vacations to seriously ill children and their families. When applying for the vacation, the Sanislos executed a “wish request” form that contained a waiver of liability, also known as an exculpatory clause. When the parents arrived at the resort village they again signed a liability release form, also an exculpatory clause. The language of the exculpatory clause is reprinted below for reference:
I/we hereby release Give Kids the World, Inc. and all of its agents, officers, directors, servants, and employees from any liability whatsoever in connection with the preparation, execution, and fulfillment of said wish, on behalf of ourselves, the above named wish child and all other participants. The scope of this release shall include, but not be limited to, damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physical and emotional), entertainment, photographs and physical injury of any kind....
I/we further agree to hold harmless and to release Give Kids the World, Inc. from and against any and all claims and causes of action of every kind arising from any and all physical or emotional injuries and/or damages which may happen to me/us....
Sanislo at 258-259.
While participating in a horse-drawn wagon ride, a rear pneumatic lift designed to allow those in wheelchairs to participate failed, and Ms. Sanislo was injured. The Sanislos brought suit and GKTW filed a motion for summary judgment arguing that the signed releases precluded an action for negligence. The Sanislos filed a motion for partial summary judgment against GKTW’s affirmative defense of release. The trial court granted the Sanislo’s
motion and denied GKTW’s motion. The jury found for the Sanislos and GKTW appealed. Id.

The Fifth District reversed, finding the lower court erred in denying GKTW’s motion for summary judgment because the release signed by the Sanislos was unambiguous and did not contravene public policy. It ruled the exculpatory clause barred the negligence action despite the lack of a specific reference to “negligence” or “negligent acts” in the exculpatory clause.
The Fifth District reasoned that exculpatory clauses are effective if the wording of the exculpatory clause is clear and understandable so that an ordinary and knowledgeable person would know what he or she is contracting away, and that the court had previously rejected “‘the need for express language referring to release of the defendant for “negligence” or “negligent acts” in order to render a release effective to bar a negligence action.’ ” On the public policy argument, the Court said the relative bargaining power of the parties should not be considered because it was outside of the public utility or public function context and the Sanislos were not required to request a vacation with GKTW or go on the vacation. Id.
In affirming the Fifth District’s decision, the Supreme Court wrote that the conflict for the Court’s resolution was “whether an exculpatory clause is ambiguous and thus ineffective to bar a negligence action due to the absence of express language releasing a party from its own negligence or negligent acts.” Id. at 260.
The Florida Supreme Court wrote:
.... we are reluctant to hold that all exculpatory clauses that are devoid of the terms “negligence” or “negligent acts” are ineffective to bar a negligence action despite otherwise clear and unambiguous language indicating an intent to be relieved from liability in such circumstances. Application of such a bright-line and rigid rule would tend to not effectuate the intent of the parties and render such contracts otherwise meaningless.
Id. at 270.
The Court found that the GKTW liability release form released GKTW and all of its agents, officers, directors, servants and employees from “any liability whatsoever in connection with the preparation, execution and fulfillment of said wish…” The release then provided that the scope of the agreement included “damages or losses or injuries encountered in connection with transportation, food, lodging, medical concerns (physical and emotional), entertainment, photographs and physical injury of any kind . . . .” The Court found that the release clearly conveyed that GKTW would be released from any liability, including negligence, for damages, losses, or injuries due to transportation, food, lodging, entertainment and photographs. Id.
FLORIDA MD - MARCH/APRIL 2024 12 continued
24 HEALTHCARE LAW
on page
Early Recognition Can Save Patients’ Hips
By Andrew Carbone, MD
It’s easy for us to imagine the scene. A young adult athlete, such as a hockey goalie or a ballerina, sits with their physician in the examination room reviewing several X-rays on a screen that show an apparently healthy hip.
The physician tells the patient that they have sustained an injury to the joint. The soft tissues will heal with time and the pain can be managed, but arthritis could possibly develop in the future.
While just two decades ago, this may have been the end of the conversation, young adults should no longer accept that arthritis and a deteriorating joint is the inevitable result of a hip injury. Fortunately, a major paradigm shift is underway. Supported by extensive data and increasingly effective arthroscopic techniques, we can recognize the underlying pathologies resulting from hip injuries and treat them now. Such early intervention may possibly delay or obviate the need for total hip replacement in the future and might even prevent the joints from developing arthritis altogether.
THE CHALLENGE –Traditionally, arthritis has been divided into two categories: primary and secondary. Primary arthritis basically means arthritis with no known origin. Secondary arthritis includes arthritic conditions of known medical origin, such as rheumatoid or inflammatory arthritis and infectious or septic arthritis. In the 1970s, 80s and even the 90s, we lacked the diagnostic tools to be more precise than this. But today, with increased awareness, improvements in advanced imaging, better understanding of synovial biomarkers, and other technology available, we can invest greater effort in determining the precise causes of the pre-arthritic condition and treat the underlying pathology.
These pathologies may include femoroacetabular impingement, acetabular labral tears, excessive femoral or acetabular anteversion or retroversion, inadequate femoral head coverage (Acetabular Dysplasia), or hip microinstabiltiy. In some cases, the injury that brings the patient to the physician’s office may reveal another pathology such as generalized ligamentous laxity, or even some connective tissue disorders like Ehlers-Danlos Syndrome.
These conditions may result in an earlier than normal onset of arthritis of the hip if left untreated. Ultimately, the goal is to change the mindset of both patients and providers alike – that osteoarthritis is not a disease, but rather a symptom or side effect of an untreated predisposing hip condition.
THE PARADIGM SHIFT – The focus of hip preservation is the idea that we don’t treat hip pain patients like pre-arthritic patients; we treat them like they have actual pathologies that need to be treated. A growing body of evidence shows us that early intervention can improve hip function, reduce pain, and possibly delay or even prevent the onset of arthritis.
But as with many advances that result in a paradigm shift,

there has been skepticism and resistance in some quarters. I compare this to how arthroscopic surgery was viewed many years ago. For a long time, some physicians considered shoulder arthroscopy to be “an instrument of the devil” by very prominent shoulder surgeons. For example, if you were doing a labral repair arthroscopically, some argued that you were doing harm to the patient and that of course would be a terrible thing. But then our arthroscopy techniques steadily improved. The result has been a total shift away from open surgical labral repairs for shoulder instability. In fact, the role for open shoulder labral repairs is so limited today that the technique is not often taught in surgical residency or fellowship anymore.
With hip surgery, it’s similar. Early articles were published with nearly the same headlines, comparing hip arthroscopy to the “devil’s tool.” Open surgery on the hip for dysplasia, for example, has been around for some time. Whereas hip arthroscopy has been around only since the early 2000s. But now that paradigm has started to change. Now, we are able to combine open surgery with arthroscopic techniques. The results are promising, but they have taken time to gather. Part of this is due to the nature of hip preservation. Unlike surgery to the shoulder or the knee, for example, in hip surgery, the benefits for the patient may not always be immediately clear. Instead, we are trying not only to improve function and reduce pain now, but potentially prevent a disease that’s possible to happen 10 to 20 years from now. Now that we have been doing this work for nearly 20 years, longer term data has begun to demonstrate that hip arthroscopy improves a patient’s pain and function. And while it is likely too early to truly know hip arthroscopy’s effect long term, as we continue to improve our techniques and study our patients, I am confident we will start to see stronger evidence for delayed and possibly reduced rates of hip osteoarthritis.
UNDERDIAGNOSED – Education is key in hip arthroscopy because many times the underlying pathology goes undiagnosed. For example, often a patient will present with vague groin pain or maybe a tightness they experience when they are trying to stretch out. Sometimes this pain radiates to other areas, such as the buttocks, or the hip. Then it often gets written off as a muscle pull or lower back pain. But unlike those conditions, it never really goes away. The patient gets X-rayed, but the X-ray looks healthy. Eventually, the patient gets frustrated and that’s typically when we are consulted; because, if you are 21 years old, you should not be experiencing hip pain. And if you do, that’s something that needs to be addressed.
FLORIDA MD - MARCH/APRIL 2024 14
ORTHOPEDICS
Dr. Andrew Carbone is a dual fellowship-trained orthopedic surgeon and sports medicine physician at the Orlando Health Jewett Orthopedic Institute.
At the Orlando Health Jewett Orthopedic Institute, we are seeking to raise awareness among young adult athletes that hip-related pain is not normal and the cause of it should be carefully investigated and identified. And if it is determined not to be a temporary condition, such as a muscle strain, we should review the possible treatment options, which may include arthroscopy. Orlando Health Jewett Orthopedic Institute is the first orthopedic specialty hospital in Florida, and we’ve assembled a team of distinguished experts to address these kinds of cases. When a patient comes here, they aren’t seeing just one doctor and getting just one opinion, they are seeing several doctors and getting several perspectives at once. We form a kind of collective in which we can share our views and challenge each other. In addition to this, we are part of the Academic Network of Conservational Hip Outcomes Research group (ANCHOR). ANCHOR is a multicenter, clinical research group of physicians and scientists who are investigating adolescent and adult hip disorders. We are focused on improving patient care through research, education and mentorship. This collaboration enables us to learn from thousands of data points and patient outcomes.
BOTTOM LINE – If you have a young adult patient who has experienced an injury to their hip or is presenting with unusual pain, don’t dismiss it, investigate it. Find out why this is happening, and let’s get it treated. It might save that patient a lot of pain and difficulty not just now, but many years from now.
Dr. Andrew Carbone is a dual fellowship-trained orthopedic surgeon and sports medicine physician at the Orlando Health Jewett Orthopedic Institute. His expertise is in sports medicine, and he frequently collaborates with athletes across many sports. This includes enthusiasts who play sports in their leisure time as part of an active lifestyle. Dr. Carbone is proficient in a wide array of procedures including:
• Arthroscopic hip labral repair for treatment of femoroacetabular impingement
• Complex primary and revision hip arthroscopy including labral reconstruction for treatment of recurrent labral tears
• Shoulder arthroscopy for rotator cuff tears, shoulder instability and biceps injuries
• Knee arthroscopy for treatment of meniscal and cartilage injuries
• Ligament reconstruction for knee injuries
• Minimally invasive robotic hip replacement
• Minimally invasive treatment of gluteal and hamstring tears
Dr. Carbone stays informed on the latest medical research and science so he can offer his patients the most comprehensive information and care. He takes time to answer all of their questions so they feel comfortable about their treatment options.
DR. CARBONE’S TRAINING
He earned a bachelor’s degree in neuroscience and behavioral biology from Emory University in Atlanta. Dr. Carbone received his medical degree from New York Medical College in Valhalla, where he was inducted into the Alpha Omega Alpha national medical honor society. He then stayed in New York for an orthopedic surgery residency at The Mount Sinai Hospital.
He completed a sports medicine fellowship at the Cedars-Sinai Kerlan-Jobe Institute in Los Angeles and another fellowship in hip preservation at the American Hip Institute & Orthopedic Specialists in Des Plaines, Illinois. He received specialized training in open and arthroscopic hip preservation techniques, treatment of gluteal and hamstring injuries, and minimally invasive robotic hip replacement procedures.
ABOUT DR. CARBONE
Dr. Carbone is a member of the American Orthopaedic Society for Sports Medicine, American Academy of Orthopaedic Surgeons, Arthroscopy Association of North America and International Society of Hip Preservation. He is also a peer reviewer for The American Journal of Sports Medicine.
His research has been published on topics including arthroscopic capsular repair, batter’s shoulder, shoulder arthroplasty and femoroacetabular impingement syndrome, a condition in which the bones at the hip joint rub together due to one or both bones being irregularly shaped.
He has a particular interest in the arthroscopic treatment of sports-related injuries of the hip, knee and shoulder. During his medical studies, he spent a year researching the biologic and mechanical pathways involved in tendon to bone healing and how sports-related injuries affect cartilage health and contribute to the development of osteoarthritis.
He constantly reviews the latest research, allowing him to extend to his patients the most comprehensive information and care available to ensure they are comfortable with their treatment options.
An avid sports fan, Dr. Carbone previously served as the assistant team physician for the Los Angeles Dodgers and Los Angeles Angels. He served as the associate team physician for the Anaheim Ducks, Los Angeles Galaxy, Los Angeles Sparks, Pepperdine University and West LA College.
Outside of work, he enjoys spending quality time with his wife and children, playing golf, and exploring new places through travel.
FLORIDA MD - MARCH/APRIL 2024 15
ORTHOPEDICS
Caring for Chest Wall Problems in Kids - Giving Them Back Comfort, Confidence and a Chance to Soar
By: Kellianne Kleeman, MD
Chest wall disorders can significantly impact a child’s life. Unfortunately, many children are told that their defect is merely cosmetic based on a superficial examination of their chest. However, the external appearance of the defect doesn’t always tell the whole story. Even in cases that seem mild, many children experience symptoms that can significantly affect their quality of life. Pectus excavatum, in particular, can cause functional limitations that are objectively measurable. Along with plummeting self-confidence, children often experience exercise intolerance, presyncope, palpitations, and dyspnea. When children aren’t offered the treatment they need, they’re forced to adjust their lives around their limitations. Axel’s story is a perfect example of this scenario. Axel’s Story – Pectus Excavatum
From a young age, Axel’s family had noticed the unusual appearance of his chest. They took him to see a few different providers, but they were told that his chest was not responsible for his symptoms, and it was only a cosmetic defect. It wasn’t until Axel needed a checkup and couldn’t get into his regular pediatrician that his mom searched for another pediatrician. At that appointment, Axel asked his mom once again to mention his chest, and although hesitant due to their past experiences, she brought it up. This pediatrician immediately noticed that something was wrong and referred them to Dr. Kellianne Kleeman, a pediatric cardiothoracic surgeon at Nemours Children’s Hospital, Florida.
Dr. Kleeman mapped out a detailed care plan that included preoperative testing to determine his degree of functional impact and planning a minimally invasive surgery to repair his pectus excavatum.
Axel says, “When Dr. Kleeman showed us the picture in clinic—that was the first time I saw my dad cry. Growing up, I couldn’t keep up with other kids, it was hard to breathe. I had to quit things I enjoyed—like baseball, which I loved. I thought it was my fault, and not that there was something wrong with me because I was always told I was okay, physically. I was also self-conscious about the way my chest looked, and always wore a T-shirt, even in the pool. Now, I feel comfortable and confident. The pain isn’t as bad as I thought it would be, and I was



able to go home already after one day.”
Axel is excited to test his new limits. He can’t wait to see how long he can run and try everything he once believed he couldn’t do.
Axel’s mom leaves encouraging words for families going through a similar situation: “Listen to your kids, listen to them. Advocate for them, and don’t make the same mistake I made by waiting. It doesn’t hurt to get a second or third opinion. The doctors here, you see them care, their attention to detail, there’s not a single bad thing I can say about them. Everyone was amazing.”
NEMOURS CHILDREN’S CHEST WALL INSTITUTE, CENTRAL FLORIDA
The Nemours Children’s chest wall disorders team helps children feel better, inside and out. We offer the latest nonsurgical and surgical treatments for pectus excavatum (sunken chest), pectus carinatum (pigeon chest) and other complex chest wall problems.

Our Chest Wall Institute at Nemours Children’s Hospital, Florida is led by experts in cardiothoracic surgery. Our
FLORIDA MD - MARCH/APRIL 2024 16 PEDIATRICS
CT Scan – pre op
Chest X-Ray – post op
Axel and mom, Maite
Kaitlin Frindt, PA-C, Dr. Kleeman, Axel, Maite
program brings together a whole team of specialists, advanced approaches, and treatments you can’t find everywhere.
PROGRAMS & SERVICES
Team-based approach to personalized care with a multidisciplinary chest wall clinic, offering:
• Non-interventional treatments such as chest-wall specific physical therapy, nutrition optimization, and behavioral therapy to improve coping skills, confidence, or periprocedural anxiety
• Chest wall mentorship and support programs for patients with chest wall defects
• Specialized diagnostic workup including chest-wall specific echocardiographic measurements and cardiopulmonary exercise testing protocols
• Imaging protocols to minimize radiation and provide optimal images for 3-D modeling and virtual surgical planning as well as patient surveillance
• Multiple bracing and orthotics options including custom-made braces for the treatment of pectus carinatum and mixed defects
• Vacuum bell treatment of pectus excavatum in patients as young as 5 years old, with the goal of avoiding the future need for surgery
• The most advanced surgical technology and techniques to improve outcomes, including mandatory external sternal elevation, use of titanium bars, placement of multiple bars, customized pre-made implant modeling for minimally invasive repair of pectus excavatum
• Aggressive approach to pain control with cryoablation of intercostal nerves in addition to an enhanced recovery pathway and multimodal pain control, allowing patients to go home the day after surgery and avoid the use of postoperative narcotics
Our approach is based on each child’s needs, offering a personalized treatment plan.
“Kids are often told that their chest wall defect is “just cosmetic.” But research shows that the Haller index and the external appearance of the chest does not correlate with the degree of physiologic impact of the defect on cardiopulmonary function and does not predict who will benefit most from treatment or surgery. Every patient with a chest wall defect should have a full evaluation by a chest wall specialist.
I believe that everyone deserves the chance to live life to the fullest. Chest wall defects can have a profound impact on a child’s life. Every child deserves a full evaluation and compassionate, personalized care with a thoughtful and comprehensive treatment plan.
We want all patients with chest wall defects to get the treatment they deserve!” – Dr. Kleeman
Kellianne Kleeman, MD is an experienced cardiothoracic surgeon who is board-certified and leads the Chest Wall Institute at Nemours Children’s Hospital in Florida. She joined the Nemours Cardiac Center in September 2021 to provide exceptional cardiac care to patients throughout the state of Florida.
Dr. Kleeman earned her medical degree at the University of Michigan, after she graduated with honors from Vanderbilt University. She then went on to complete her cardiothoracic surgical residency at the University of Michigan. Following this, she underwent advanced training in congenital and pediatric cardiothoracic surgery at Mott Children’s Hospital at the University of Michigan.

Dr. Kleeman is passionate about outcomes research related to surgical treatment of chest wall disorders and improving access to quality treatment for chest wall patients. Her primary interest lies in caring for children with chest wall disorders, and she strives to empower them to live up to their potential.
During her free time, Dr. Kleeman enjoys traveling with her husband and two children.
TO REFER A PATIENT
• Call Appointment Scheduling: 407.650.7715 – then select Option 1 to be connected to our access center representative to assist.
• Submit referrals via fax: 407.650.7124
• Submit electronic referrals through Nemours.org/Nemourslink (requires access to Nemours PCP portal)
• Recommend the Nemours Cardiac Center, and their families call into our main scheduling at 407.650.7715.
• Email chestwallinstitute@nemours.org


FLORIDA MD - MARCH/APRIL 2024
17
PEDIATRICS
Kellianne Kleeman, MD
Axel Post Op Axel at post op checkup with Cynthia Cardwell, RN
When The Tremor Isn’t Essential –Parkinson’s Disease: One of the Most Commonly Misdiagnosed Neurological Conditions
By Jaivir S. Rathore, M.D, F.A.E.S & Idha Sood, M.B;B.S
A COMPREHENSIVE ARTICLE, ON THE OCCASION OF WORLD PARKINSON’S DAY • APRIL 11, 2023
WHAT IS PARKINSON’S DISEASE?
Parkinson’s disease (PD) is the second-most common neurodegenerative disease after Alzheimer’s dementia. More than 10 million people worldwide and nearly one million people in the U.S. are living with PD. This number is expected to rise to 1.2 million by 2030. Nearly 90,000 people in the U.S. are diagnosed with PD each year. The incidence of PD increases with age, but an estimated four percent of people with PD are diagnosed before age 50. Men are 1.5 times more likely to have PD than women. Within the US; Florida has the second highest population of people living with PD. It is a slowly progressive disorder which often first presents with a resting hand tremor. The patient can then develop other cardinal features of bradykinesia, rigidity and postural instability. Autonomic symptoms like constipation, poor sense of smell, excess salivation due to poor swallowing can be present years before the patient develops the classic PD symptoms. In some patients there can be signs of cognitive decline which could be part of “Parkinson’s Plus” or Parkinson’s dementia.
WHAT CAUSES PARKINSON’S DISEASE?
PD results from loss of dopaminergic neurons in the pars compacta of substantia nigra of basal ganglia which is responsible for subcortical control of motor activity. In most cases the exact cause is unknown (Idiopathic Parkinson’s Syndrome, IPS), up to 15% cases may have genetic components, most common being LRRK2, GBA and PRKN (associated with young onset PD). In some cases it has also been linked to exposure to certain pesticides, herbicides, and industrial chemicals. One such compound called MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) accumulates in the mitochondria and generates free radicals, which can cause damage to basal ganglia and hence lead to PD. Latest research is also suggestive of alpha synuclein aggregation playing a role in the pathogenesis of PD. The earliest histopathological changes are hence seen in the myenteric plexus of the gastrointestinal tract, which then progresses to involve the dorsal motor nucleus of the vagus nerve and sleep centers in the ponto-medullary brainstem.
Many known figures in the world history have been affected by Parkinson’s disease including Pope John Paul II, Adolf Hitler, Mao Zedong, Michael J Fox and notably world heavyweight boxing champion Muhammad Ali, in his case repeated hits to his head is considered a risk factor to cause “dementia pugilistica” a neurode generative condition with Alzheimer’s like dementia. Neurode generation is a serious issue for boxing or for any traumatic brain injury for that matter.
WHAT ARE THE EARLY SIGNS OF PARKINSON’S DISEASE?


Patients typically have constipation, poor sense of smell and REM sleep disorder preceding the motor symptoms by around 10-15 years. Patients most commonly present with the earliest symptom of tremor. The tremor is usually present at rest and sometimes has classic pin rolling features involving the thumb and the index finger; it can disappear for some time while doing a task but returns when the patient is distracted. In cases where PD is not tremor dominant, patients usually present with the cardinal features of “overall slowness” or bradykinesia, mask facies, muffled speech (hypophonia), small handwriting (micrographia) etc. Patients can take a long time to do their usual daily activities and walk slowly. When prompted about mood or sleep issues, patients might elaborate on feeling depressed and can give a history of movements in their sleep, likely REM sleep disorder. Other autonomic features that a patient of PD might have include urinary retention, erectile dysfunction and orthostatic hypotension. Patients with advanced disease can also present with memory decline due to the neurodegenerative changes of the brain.
On examination, patients have the characteristic cog-wheel rigidity which can be elicited by slow rotatory movements of their wrists. Patients can appear to be stiff, they have shortened stride while walking and arm swing is typically reduced asymmetrically. They walk with a stooped posture and have to take multiple short steps to turn around. On pulling them back suddenly, called the posterior pull test, patients take a lot of steps to catch themselves or may even fall.
HOW DOES PARKINSON’S DISEASE PROGRESS?
In classic PD cases, the patient has tremor of one hand in stage 1. This can progress to the other hand in stage 2. Stage 3 is characterized by mild balance problems, which can worsen causing falls in stage 4 needing cane or a walker to walk and if it continues to worsen, in stage 5 patients can be wheelchair or bed bound. Not all patients progress to stage 5 and brain imaging such as (Dopamine Transporter, DaT) scan is not usually a good prognostication tool.
WHAT MIMICS PARKINSON’S DISEASE?
The PD tremor is most commonly mistaken for an essential
FLORIDA MD - MARCH/APRIL 2024 18
tremor and it remains refractory of usual treatment of propranolol, primidone etc. In such situations, emphasis should be put on looking out for other clinical features of PD like bradykinesia and gait disturbances.
Progressive supranuclear palsy (PSP) can have similar features of bradykinesia, rigidity and gait disturbances but patients may also have vertical gaze paralysis and falling en-block while sitting which is not a feature of PD and MRI Brain of PSP patient may show midbrain atrophy which is described as “Hummingbird” sign.
Patients of Lewy Body Dementia (LBD) have many features of Parkinson’s but those symptoms usually tend to occur after dementia symptoms. In contrast dementia is progressively developed later in the course of disease in PD patients due to overall neurodegeneration. In addition, LBD patients have very vivid visual hallucinations along with wide mood fluctuation which are not a feature of PD, however PD dementia patients may get hallucination or psychosis which is treated with pimavanserin. Ischemic or hemorrhagic stroke, mass lesions, hydrocephalus and Wilson’s disease can be excluded using imaging techniques such as MRI brain.
HOW IS PARKINSON’S DISEASE DIAGNOSED?
The diagnosis of PD is primarily a clinical one. A comprehensive examination and proper staging of PD can be done using Unified Parkinson’s Disease Rating Scale (UPDRS) which is a gold standard tool to measure not only the severity and progression of PD but also helpful in monitoring the response to medications. While evaluating the patient it is also imperative to go over their list of medications to exclude the possibility of drug-induced PD. Traditional antipsychotic medications are most implicated in such a condition.

In clinically uncertain cases nuclear imaging DAT-SPECT scan may be helpful, however routine use of this test should be discouraged. A clear clinical improvement after levodopa treatment provides the best confirmation of PD.
HOW IS PARKINSON’S DISEASE TREATED?
There is no cure for PD at this time, however since the pathogenesis of PD involves loss of dopaminergic neurons, the primary mode of treatment is replenishing the dopamine levels with medications such as levodopa with carbidopa, which may also be used in combination with other classes of medications including Dopamine Agonists, COMT Inhibitors, MAO-B Inhibitors, and Anticholinergic agents. Treatment is individualized to the patient and adjusted over time based on symptoms, side effects and tolerability. Dopamine agonists like pramipexole, or ropinirole can be used in younger patients with the advantage of lesser side effects. If a patient primarily has tremor only, amantadine or anticholinergics may be used. In advanced stages of PD, patients may have psychosis with visual or auditory hallucinations and delusions. Pimavanserin, a serotonin 5-HT2 receptor antagonist is the only FDF approved treatment for psychosis associated with PD.
Most PD medications provide good improvement in symptoms for the first 3 to 6 years, but with the natural progression of the disease, results can decline with time. Levodopa-Carbidopa can have the “on-off” phenomenon where symptoms may worsen during the “off” periods. Apomorphine, a dopamine agonist, is the only FDA approved medication which can be used for symptom control during the off periods.

PD being a multi system disease requires a multi system ap proach. Patients can benefit a lot with physical therapy, like LS VT-BIG (Lee Silverman Voice Treatment), which encompasses physical therapy to improve their gait and balance coupled with speech therapy to address the hypophonia which can be pres ent. Patients should be encouraged to have an active lifestyle.
FLORIDA MD - MARCH/APRIL 2024 19
Typical Dopamine Transporter Ligands Single Photon Emission Tomography (DaT-SPECT) scan findings in patients with Idiopathic Parkinson’s Syndrome (IPS) showing reduced striatal DAT availability compared with a normal finding. The reduction is often left/right asymmetrical, usually more pronounced in the hemisphere contralateral to the clinically dominant side. The posterior “tail” of the putamen is almost always most strongly affected. The motor symptoms of IPS manifest only after a DAT loss of about 50% in the putamen. The atypical neurodegen erative parkinsonian syndromes, especially Progressive Supranuclear Palsy (PSP) and Multiple System Atrophy (MSA) of the parkinsonian type show similar patterns of findings on DAT-SPECT as IPS.
IMAGE COURTESY DTSCH ARZTEBL INT 2019 BUCHERT, R ET AL.
Continued
Deep Brain Stimulation (DBS) is a promising and underutilized advanced treatment for people who experience disabling tremors, wearing-off spells, and medication induced dyskinesias.
on page 24
Your Patient Is Not Happy with Their Knee or Hip Replacement. What’s Next?
By George J. Haidukewych, MD
According to the Agency for Healthcare Research and Quality, more than 790,000 knee and 450,000 hip replacements are performed in the United States each year. While these numbers declined somewhat over the past year due to obvious reasons and events related to the pandemic, experts project a significant upward trend in medically indicated joint replacement surgeries over the next 10 years.
More than 85-90 percent of patients who undergo total knee or hip arthroplasty (TKA/THA) surgery experience a favorable outcome, with a decrease in pain, an increase in mobility and an overall improved quality of life. And with advances in technology, patients can expect their replacement joint to function well for 20 years or longer. But not all joint replacement surgeries are successful. Complications and failures can occur, and patients who expected dramatic pain relief and function after a knee or hip replacement may present with persistent pain, as well as considerable frustration and unhappiness.
About a third of patients will still have some aches and pains following knee or hip replacement. Early problems can be due to technical factors involving the surgery, inadequate rehab, or more serious problems such as infection or loosening. Problems can also occur years after surgery as the ceramics and plastics start to wear through. A joint replacement that had previously been functioning well for several years can suddenly start hurting or swelling.
The most common complaints following TKA include swelling, activity-related pain and mechanical symptoms, like a crunching behind the kneecap and even clicking when the patient walks. With THA, common painful symptoms include persistent pain around the tendon or bursa on the side of the hip.
WHAT DO YOU DO IF YOUR PATIENT EXPERIENCES PERSISTENT PAIN AFTER JOINT REPLACEMENT SURGERY?
Sorting out what is a normal discomfort for a prosthetic joint and what is a more serious problem is not always straightforward. What may seem like a minor ache or pain could be a sign of a more serious underlying problem. Problems such as instability or loosening of the knee or hip, or even more unusual problems like corrosion or metal sensitivity, can be easily misdiagnosed; ruling out infection and instability is critical.
The optimal plan of care for those patients who continue to experience ongoing joint pain after TKA or THA is an evaluation referral with an orthopedic specialist. Specialized tertiary referral centers like Orlando Health Jewett Orthopedic Institute offer expert specialist care and advanced technology, including leadingedge imaging, such as MRI scanning with metal artifacts suppression, to diagnose reasons for persistent symptoms after a knee or hip replacement.
Sometimes patients have unrealistic expectations of their replacement, because of what they’ve been told or seen on TV or social media.

Expecting the joint to be normal versus artificial is a common source of dissatisfaction. They may not follow proper rehab or activity levels. These patients require a comprehensive evaluation of their overall fitness level, including other joints like the shoulders and ankles. Patients need to focus on total body fitness and understand what a replacement joint can and cannot do.
An overall aging population, a rise in the prevalence of risk factors such as obesity, and the popularity of maintaining active lifestyles not only contribute to the increasing number of joint replacement surgeries, but also the inevitable consequential increase in complications or failed joint replacements. We also have seen an increasing number of joint replacements in a younger patient population whose active lifestyles place added stress and wear on their original and replacement joints. With normal use and activity, every joint replacement implant begins to wear over time, and excessive activity or weight may increase the rate of this normal wear, causing the replacement joint to loosen and become painful.
Evaluation by an orthopedic specialist may determine that a painful knee or hip replacement does need any further surgical intervention. It may simply be something that indicates additional physical therapy, weight loss or activity modification. But there is an increasing number of patients who will require a joint replacement revision (redo).
WHEN IS REVISION SURGERY NECESSARY?
Revision, or redo, surgery is a complex procedure that involves removing and replacing the original joint implant, usually due to a complication from the initial replacement.
Overall, complication rates following TKA or THA surgery are low. Serious complications, such as a joint infection, occur in fewer than 1-2 percent of patients. Instability can occur in 2-3 percent of knee replacements, and 2-3 percent of hip replacements can have a dislocation or similar problem. These percentages are small, but given the large number of surgeries performed, it adds up to a significant number of people experiencing undue discomfort and pain.
Typically, more women than men undergo knee replacement, with hip replacements being about even between men and women. Overall, men place more wear on replacement joints than women, due both to more body weight and slightly more activity, resulting in a slightly higher need for revision surgery.
Data from Medicare shows that the average rate of revision surgery within 90 days is 0.2 percent but increases to 3.7 percent
FLORIDA MD - MARCH/APRIL 2024 20
within 18 months. These are usually due to infection or mechanical complications of the implant. While surgical techniques and implant designs and materials continue to advance, implant surfaces can wear down and the components can loosen over time. Research suggests that long-term wear and loosening affects 6 percent of people after 5 years and 12-15 percent after 10 years.
Only a handful of centers in Florida specialize in diagnosing and treating conditions associated with problematic joint replacements. Specialists with the Orlando Health Jewett Orthopedic Institute perform hundreds of successful revisions of knee and hip replacements every year for patients throughout Florida and the Southeast.
These complex, long procedures can be challenging and require multidisciplinary and subspecialty care, including infectious disease experts and plastic surgeons, as well as advanced surgical, intensive care, recovery and rehabilitation facilities that provide a higher level of care. Backed by all the resources of the Orlando Health system, Orlando Health Jewett Orthopedic Institute offers this advanced level of care. And, expected to be completed in 2023, a new, state-of-the-art orthopedic complex on Orlando Health’s downtown Orlando campus will usher in the next generation of orthopedic care.
Ultimately, the basic message for your patients is “Don’t give up hope!” An orthopedic surgeon who specializes in complex knee and hip revision work can provide a comprehensive evaluation to determine how to best correct a persistent joint replacement problem.
Internationally recognized for joint replacement surgery and trauma, George J. Haidukewych, MD, serves as Orlando Health’s director of orthopedic trauma and chief of complex joint replacement, practicing at the Orlando Health Jewett Orthopedic Institute. Dr. Haidukewych specializes in total hip and total knee replacements as well as orthopedic trauma. He brings extensive experience in the management of failed and infected total hip and total knee replacements and in reconstruction of the joints after trauma. Up to half of his practice is dedicated to solving these challenging problems from around the Southeast. Dr. Haidukewych completed his residency training at the Mayo Clinic in Rochester, Minnesota, as well as a fellowship at Florida Orthopaedic Institute in the Tampa Bay area.





FLORIDA MD - MARCH/APRIL 2024 21
FloridaMDMagazine.com FL MD Full Pg Ad.indd 1 4/30/10 4:16:48 PM
SESSION 2 – Negotiating Leases
By Frank Ricci, Healthcare Realty & Development Services LLC
Welcome back to our second in a series about Medical Real Estate. In the first installment we discussed locating property. In today’s chapter, we are discussing leases and important considerations for your practice. If you want to refer back to SESSION 1 in the previous issue of FloridaMD/JanuaryFebruary2024 please contact me at the email address listed below.
Assuming that you and your broker have identified a great property for your practice, the next step is negotiating the lease and the hundreds of potential clauses. We won’t discuss all of them, just some of the more relevant terms and clauses for your practice.
1. RENTAL RATE
Office space is typically quoted on a cost per square foot per year ($/SF/YR) basis. Going into negotiations with the owner or landlord, it is imperative that you have an understanding of the market, including what others are paying for similar space, incentives offered, services included, length of term, escalations, etc.
2. INCENTIVES
Most landlords offer incentives to lease space in the form of “Free Rent” or a “Tenant Improvement Allowance (TIA).” Free rent is usually 1-3 months but is very dependent upon vacancy rates in the area. Tenant improvement allowances vary considerably, depending on the rental rate offered and the condition of the building. For reference purposes, it typically costs around $25/sf to refurbish an office with new paint, carpet, etc. and can run from $80-$150/sf or more to build a new office from a shell condition. In most cases, the owner will provide a TIA but it usually does not cover the entire cost of the improvements. The remaining costs will be financed by your practice as either a lump sum, payments to the Owner or payments to a lender. If the Owner is financing only part of the cost to finish your space, negotiate the terms so that you are paying for the items with the shortest depreciable life, such as flooring and cabinets. This way you can itemize and either write off as an expense or depreciate over a short time period.
3. RENTAL ESCALATIONS
When you lease office space, you are taking a snapshot in time of market rental rates. Historically, those rents have increased over time and to address this, most Owners will incorporate a form of rent escalation. This is negotiable and may be tied to a Consumer price Index (CPI), another basket index or a fixed rate. Discuss this with your broker to negotiate escalations that are fair and appropriate for your situation.
4. LEASE TERMS, EXTENSIONS & CANCELLATIONS
The lease term is the length of the original lease and typically lasts from 5-7 years. Shorter terms are usually available for second generation space and longer terms for spaces requiring extensive
renovations or construction. Extension Clauses allow you to maintain your occupancy past the original lease term while a Cancellation Clause allows you to be relieved of further financial obligation. This can be important for a small practice where a partner dies or falls ill and the practice can no longer sustain the expense.
5. EXPENSES

Your lease should cover all of the expenses that may be incurred in the operation of your office and identify who is responsible for paying them. Here is a partial list of items of expense that should be specified:
1. Common area expenses; cleaning, maintenance, repair, replacement and other expenses to maintain the common areas, parking lot, landscaping, etc.
2. Utilities; water, sewer, trash, electric, etc.
3. Management fees; supervision, accounting, legal, leasing commissions, construction administration
4. Real estate taxes, licenses and legal fees for disputing assessments
5. Future regulatory assessments and impact fees
6. Repair and replacement of major building systems; HVAC, Elevators, roof, windows, etc.
7. Insurance; building, flood, sinkhole, liability, etc.
8. After hours use; Many multitenant buildings charge extra for after hours use and this rate can be substantial.
6. ADJACENT SPACES AND EXCLUSIVITY
A lease is a long-term obligation, especially with renewals, and considering the difficulty involved in moving a practice, it is always advantageous to include a Right of First refusal on adjacent spaces as they become available. This would allow you to expand your practice by adding programs and services without moving. Requesting an Exclusivity Clause is important if a competitor locating within your building would be detrimental to your practice.
7. RESTRICTIONS ON USE AND/OR PROCEDURES YOU MAY PROVIDE (TYPICAL ON A HOSPITAL CAMPUS)
Some professional office buildings may place restrictions on the types of procedures which can be performed on the premises. This typically involves radiology, surgery or laboratory services but can also ban certain procedures such as abortion. Be sure that any procedures necessary for your practice are permitted.
Continued on page 24

FLORIDA MD - MARCH/APRIL 2024 22


FLORIDA MD - MARCH/APRIL 2024 19 Advanced Care: Before, During and After High-Risk Pregnancy Appointments: 407.567.3000 Learn More © 2023. The Nemours Foundation. Nemours Children’s Health® is a registered trademark of The Nemours Foundation. All rights reserved. J11608 (08/23)
from page 12
The determination of whether an exculpatory clause is enforceable will be determined by the Judge as the enforceability of a preinjury release is a question of law. The enforceability therefore, will depend on the Judge assigned to the matter. Physicians should not assume that because a patient signed a liability release form the patient does not have a viable cause of action. Physicians should consult with an experienced attorney who can examine the facts of the case and help you determine the best path forward. The Health Care Practice Group at Pearson Doyle Mohre and Pastis, LLP is committed to assisting Clients in navigating and defending medical malpractice claims. For more information and assistance, please contact David Doyle and Julie Tyk at Pearson Doyle Mohre & Pastis, LLP.
Continued from page 19
Julie A. Tyk, JD, is a Partner with Pearson Doyle Mohre & Pastis, LLP. Julie concentrates her practice in medical practice defense litigation, insurance defense litigation and health care law. She has represented physicians, hospitals, ambulatory surgical centers, nurses and other health care providers across the state of Florida. She may be contacted by calling (407) 951-8523; jtyk@pdmplaw.com..
Other features of PD including depression, constipation. REM sleep disorders should also be managed concomitantly.
In long-standing or medically refractory cases of at least 4 years of PD, Deep Brain Stimulation (DBS) of the subthalamic nucleus (STN) or globus pallidus interna (GPI) is a great option to provide relief with disabling symptoms. In summary, early accurate diagnosis by a neurologist experienced in PD along with a multidisciplinary approach should be used for improving the symptoms and quality of life of PD patients.
Dr. Jaivir Rathore, A triple board-certified top-rated neurologist trained at the Johns Hopkins and the Cleveland Clinic, Harvard University journal published neuroscientist and the Medical Director of Falcon Advanced Neurology & Epilepsy Freedom Center (FANEFC) in Orlando FL with additional clinics serving the largest retirement community of the world in The Villages FL provides comprehensive neurology care including movement disorders such as Parkinson’s disease. FANEFC is “Care Connected” with the Mayo Clinic, Jacksonville FL for surgical cases including DBS for PD.
Continued from page 22

SESSION 2 – Negotiating Leases
Leasing space is an important financial and legal transaction and should not be taken lightly. It is important to have an experienced real estate broker and real estate attorney represent you. This combination of professionals provides the greatest protection at the least cost. Based upon their market experience, your broker should handle the preliminary issues, negotiate the rates and terms and prepare the deal points in a “Letter of Intent (LOI).” Once negotiated, a complete legal review should be completed by your attorney before execution.
If you address each of these seven issues, you should be able to move forward with confidence in the completion of your lease negotiations and securing your office space for your prosperous enjoyment.
Frank Ricci is president of Healthcare Realty & Development LLC and H R & D Construction Inc. and has over 30 years of medical real estate brokerage, construction and development experience. He can be reached at (407) 947-5074, or FrankR@HealthcareRealtyOnline.com or visit the company website at: www.HealthcareRealtyOnline.com.
FLORIDA MD - MARCH/APRIL 2024 24 HEALTHCARE LAW Continued

JANUARY – Digestive Disorders
Diabetes
2024
Florida MD is a monthly medical/business digital magazine for physicians..
Florida MD is emailed directly to healthcare providers in Orange, Seminole, Flagler, Volusia, Osceola, Polk, Brevard, Lake and Indian River counties. Cover stories spotlight extraordinary physicians affiliated with local clinics and hospitals. Special feature stories focus on new hospital programs or facilities, and other professional and healthcare related business topics. Local physician specialists and other professionals, affiliated with local businesses and organizations, write all other columns or articles about their respective specialty or profession. This local informative and interesting format is the main reason physicians take the time to read Florida MD.
It is hard to be aware of everything happening in the rapidly changing medical profession and doctors want to know more about new medical developments and technology, procedures, techniques, case studies, research, etc. in the different specialties. Especially when the information comes from a local physician specialist who they can call and discuss the column with or refer a patient. They also want to read about wealth management, financial issues, healthcare law, insurance issues and real estate opportunities. Again, they prefer it when that information comes from a local professional they can call and do business with. All advertisers have the opportunity to have a column or article related to their specialty or profession.
FEBRUARY – Cardiology
Heart Disease & Stroke
MARCH – Orthopaedics
Men’s Health
APRIL – Surgery
Scoliosis
MAY – Women’s Health
Advances in Cosmetic Surgery
JUNE – Allergies
Pulmonary & Sleep Disorders
JULY – Neurology / Neuroscience
in Rehabilitation
Advances
Pediatrics
NICUs Autism
– Cancer Dermatology NOVEMBER – Urology Geriatric Medicine / Glaucoma
– Pain Management Occupational Therapy Please call 407.417.7400 for additional materials or information.
AUGUST – Sports Medicine Robotic Surgery SEPTEMBER –
& Advances in
OCTOBER
DECEMBER
EDITORIAL CALENDAR
The Natural Way to Solve your Allergy, Sinus and








18
Symptoms of:
Acne
Allergies
Asthma
Cold & Flu
Cystic Fibrosis
Dermatitis
Ear Infections
Eczema
Sinusitis
Relieve
•
•
•
•
•
•
•
•
•
::
Kerri and Clay: “My son’s allergy medicines were causing terrible side effects. Now that we have been coming to The Salt Room we have been able to control his symptoms with salt therapy.”
GIFT CERTIFICATES ARE AVAILABLE FUSION OF SCIENCE & NATURE 100% NATURAL TREATMENT DRUG FREE
Respiratory Discomfort.
407.862.1163 l 357 Wekiva Springs Rd., Longwood l www.SaltRoomLongwood.com Located inside Cannizzaro Integrative Pediatric Center. Offering relief to all ages. ANTI-BACTERIAL | SIDE EFFECT FREE | ANTI-INFLAMMATORY
Joseph Cannizzaro, MD: “I have been recommending The Salt Room for years. It has helped my patients with respiratory nuisances and skin problems, reducing symptoms while we address the root cause to improve their long-term quality of life.”
Jessica L.: “My son looked and felt better after just one session. His cough wasn’t as bad. I felt he could breathe so much better.”
























 Donald B. Rauhofer Publisher
Donald B. Rauhofer Publisher