What’s the Diagnosis – Case 180 1
What’s the Diagnosis – Case 180 2

What’s the Diagnosis – Case 180 3

What’s the Diagnosis – Case 180 4

What’s the Diagnosis – Case 180 5
What’s the Diagnosis – Case 180 6
What’s the Diagnosis – Case 180 7

What’s the Diagnosis – Case 180 8

What’s the Diagnosis – Case 180 9

What’s the Diagnosis – Case 180 10

What’s the Diagnosis – Case 180 11

What’s the Diagnosis – Case 180 12

What’s the Diagnosis – Case 180 13
What’s the Diagnosis – Case 180 14

What’s the Diagnosis – Case 180 15

What’s the Diagnosis – Case 180 16
What’s the Diagnosis – Case 180 17

What’s the Diagnosis – Case 180 18

What’s the Diagnosis – Case 180 19

What’s the Diagnosis – Case 180 20

What’s the Diagnosis – Case 180 21

What’s the Diagnosis – Case 180 22

What’s the Diagnosis – Case 180 23

What’s the Diagnosis – Case 180 24

What’s the Diagnosis – Case 180 25

What’s the Diagnosis – Case 180 26
What’s the Diagnosis – Case 180 27

What’s the Diagnosis – Case 180 28
What’s the Diagnosis – Case 180 29
What’s the Diagnosis – Case 180 30

What’s the Diagnosis – Case 180 31

What’s the Diagnosis – Case 180 32
What’s the Diagnosis – Case 180 33
What’s the Diagnosis – Case 180 34
What’s the Diagnosis – Case 180 35
What’s the Diagnosis – Case 180 36

What’s the Diagnosis – Case 180 37
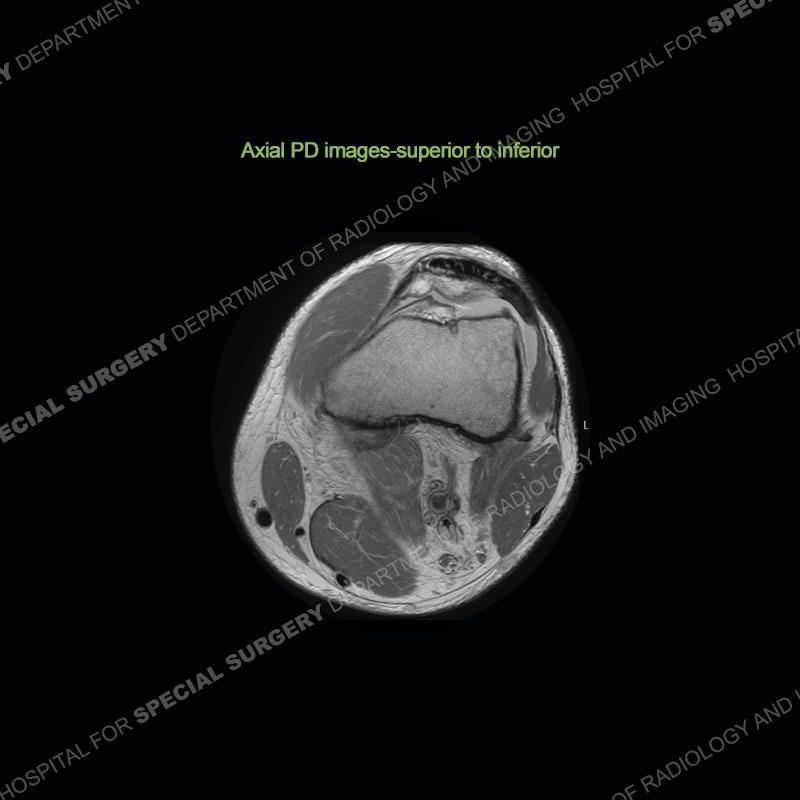
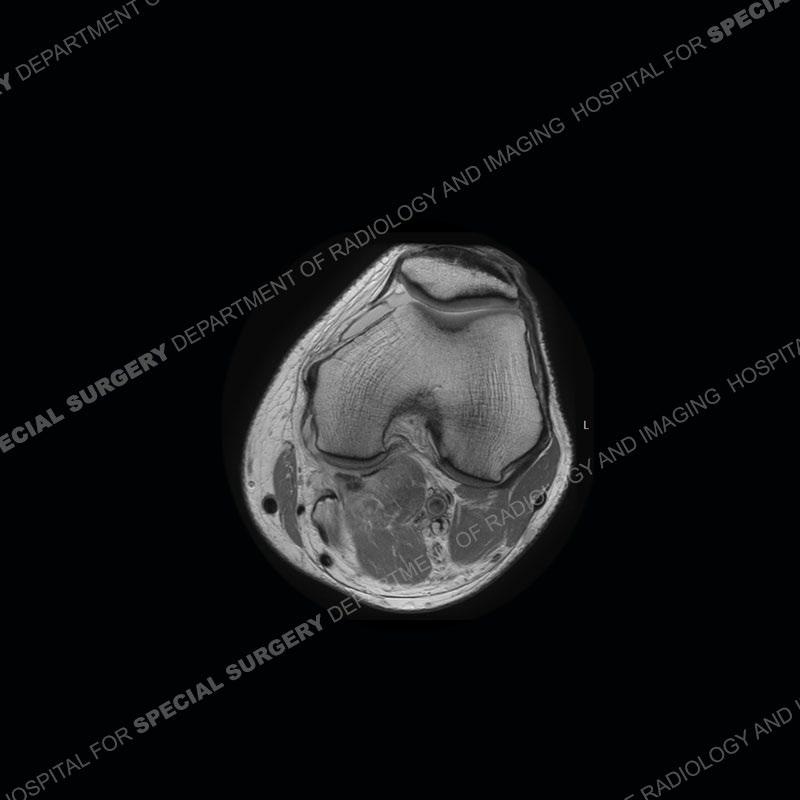
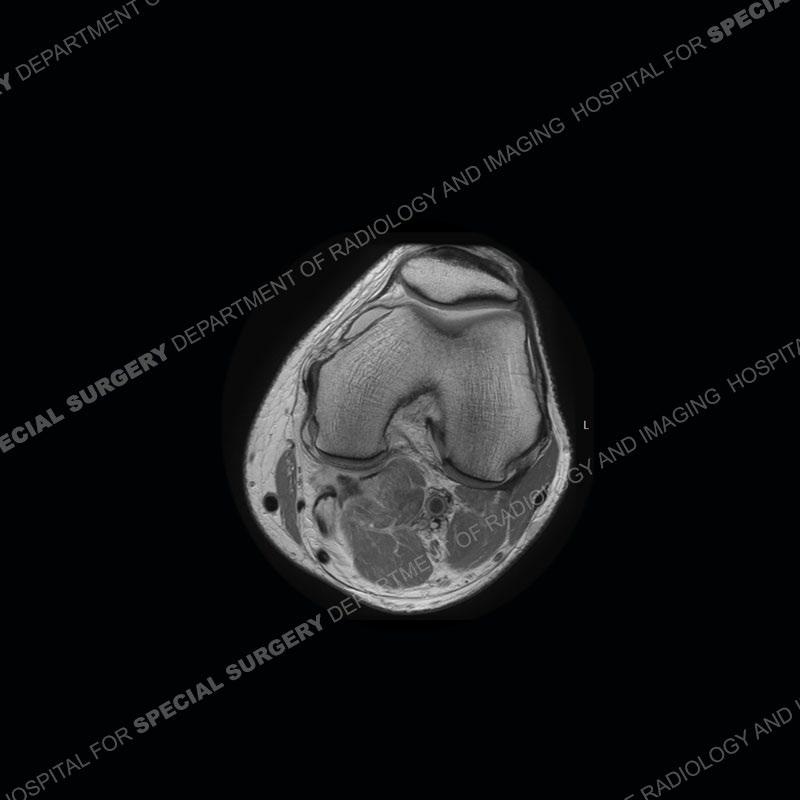
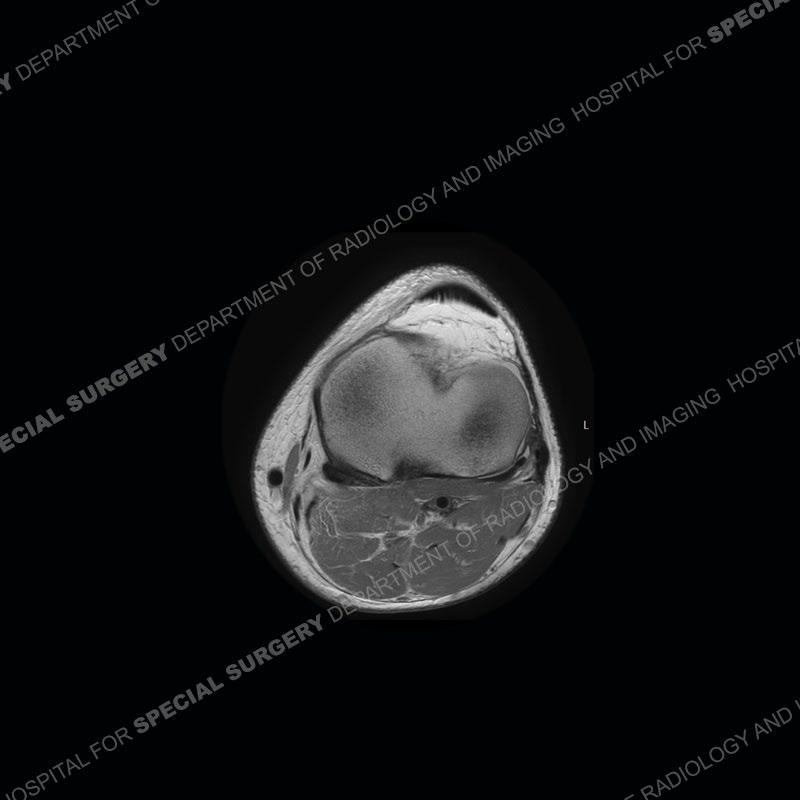
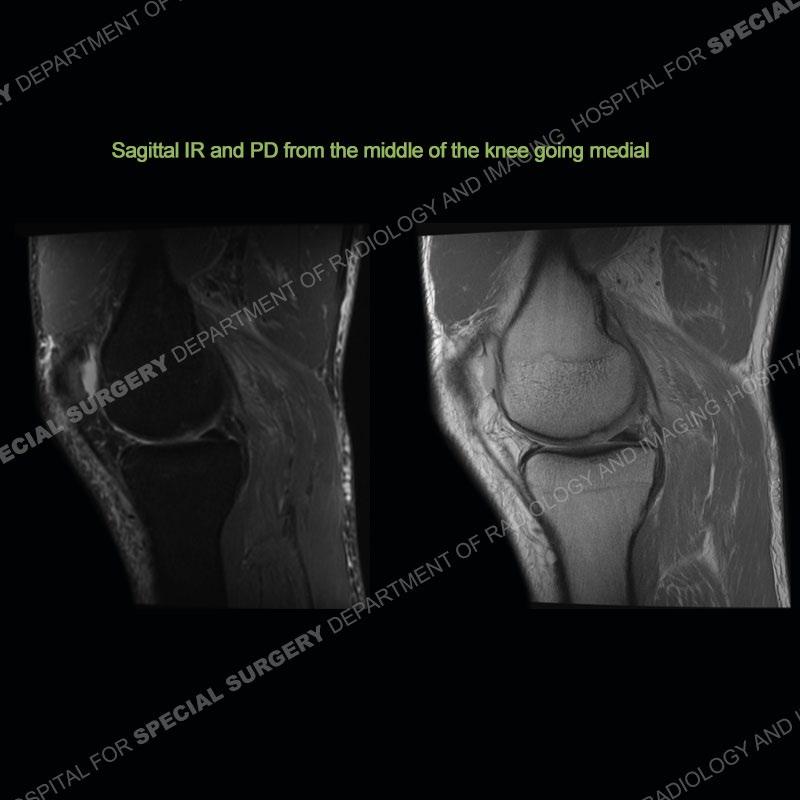
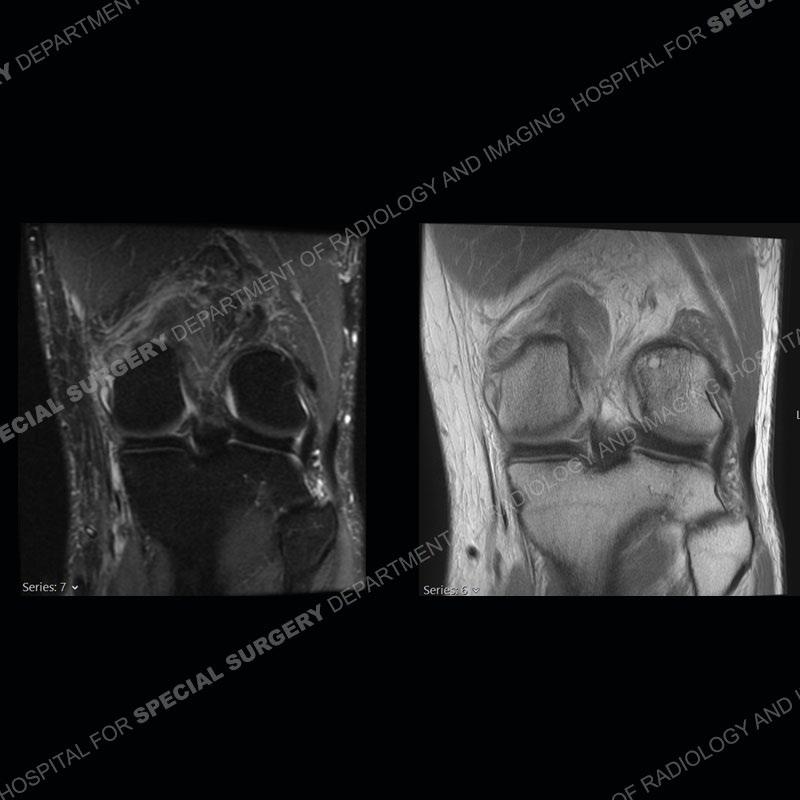
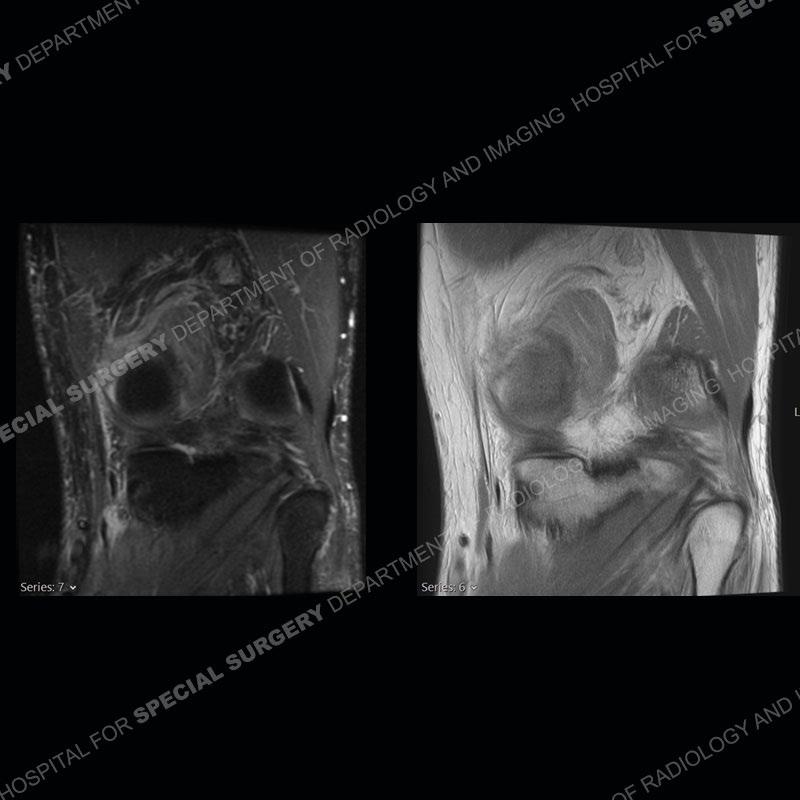
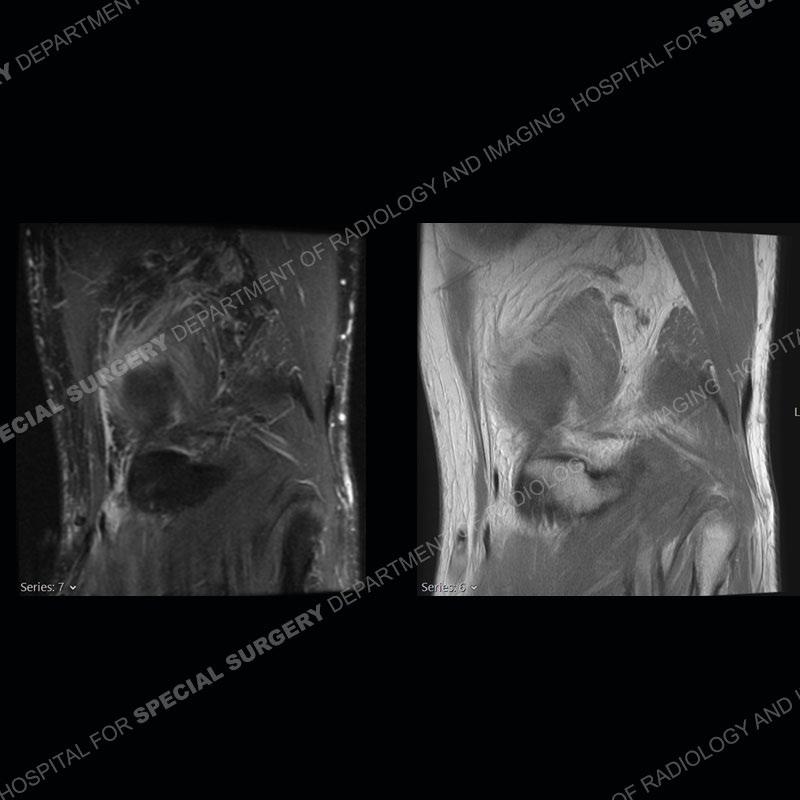
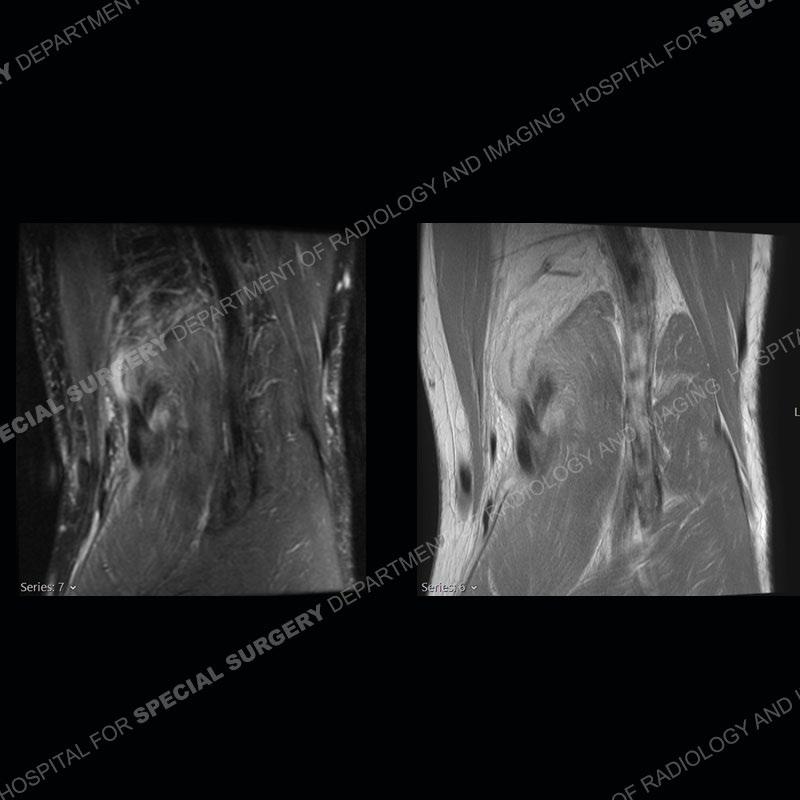
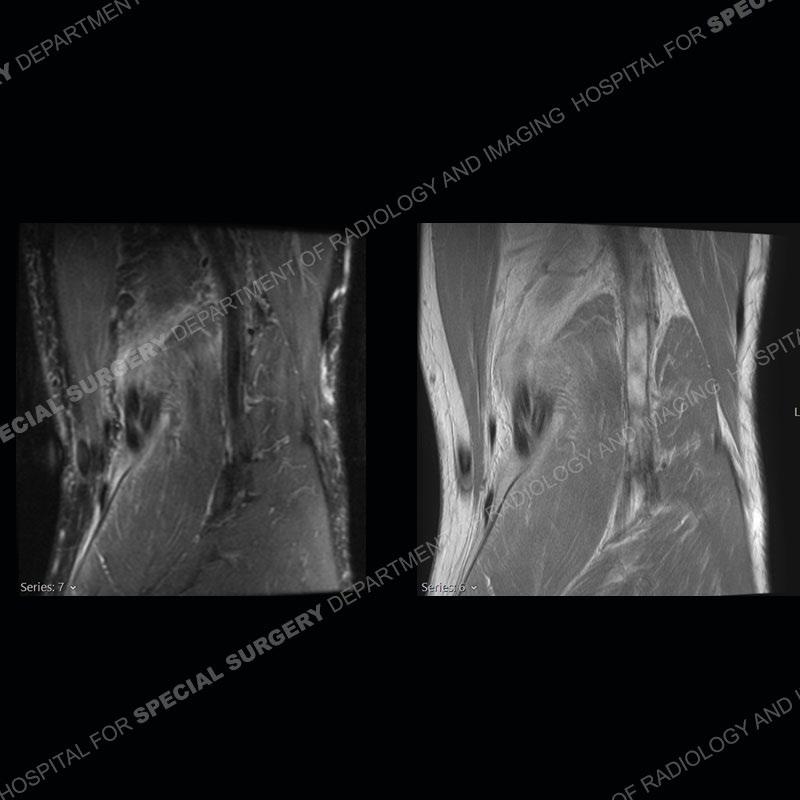
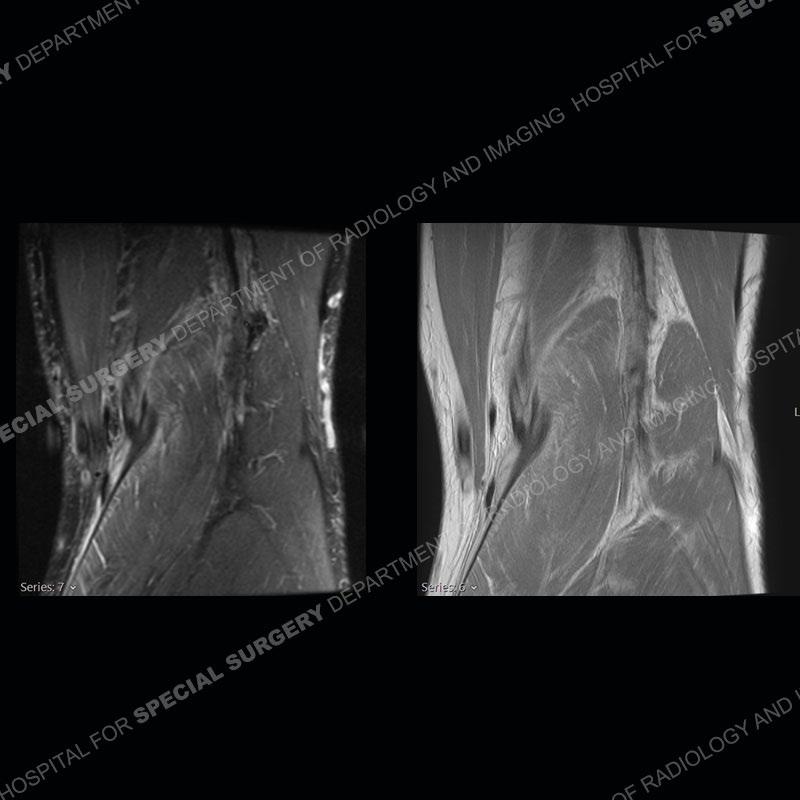
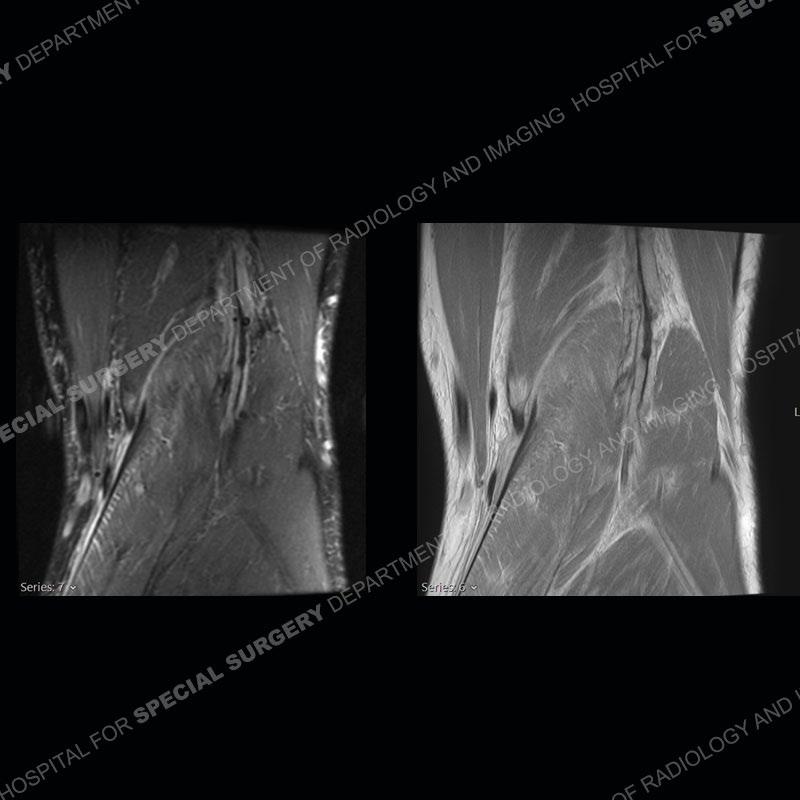
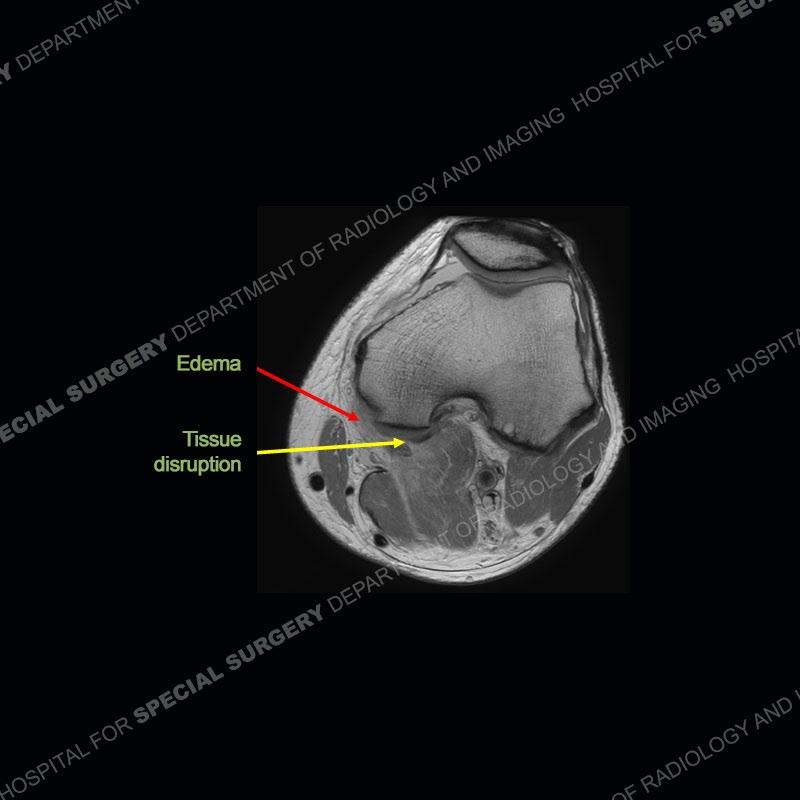
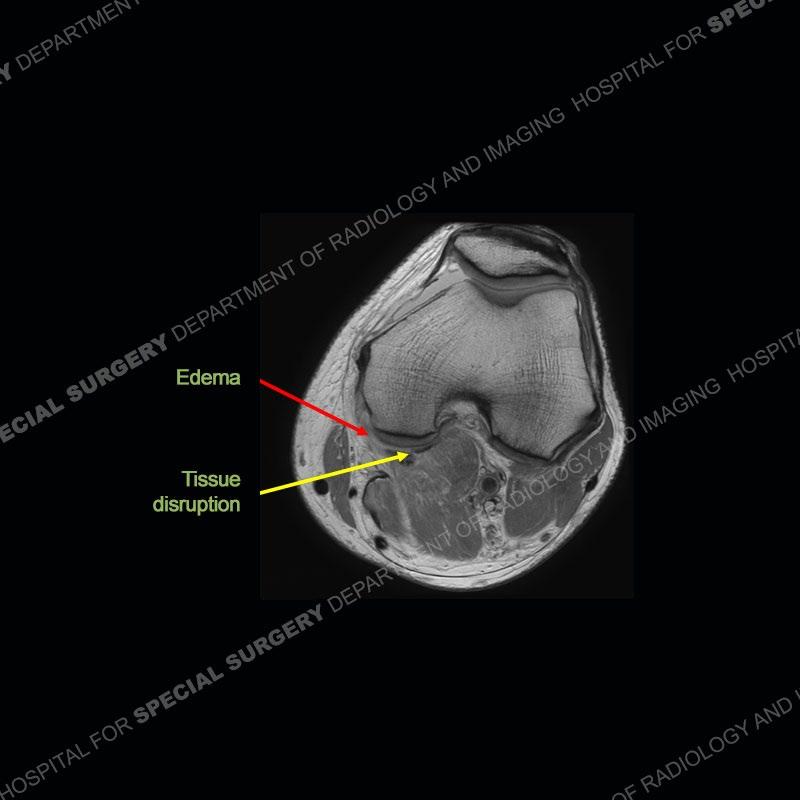
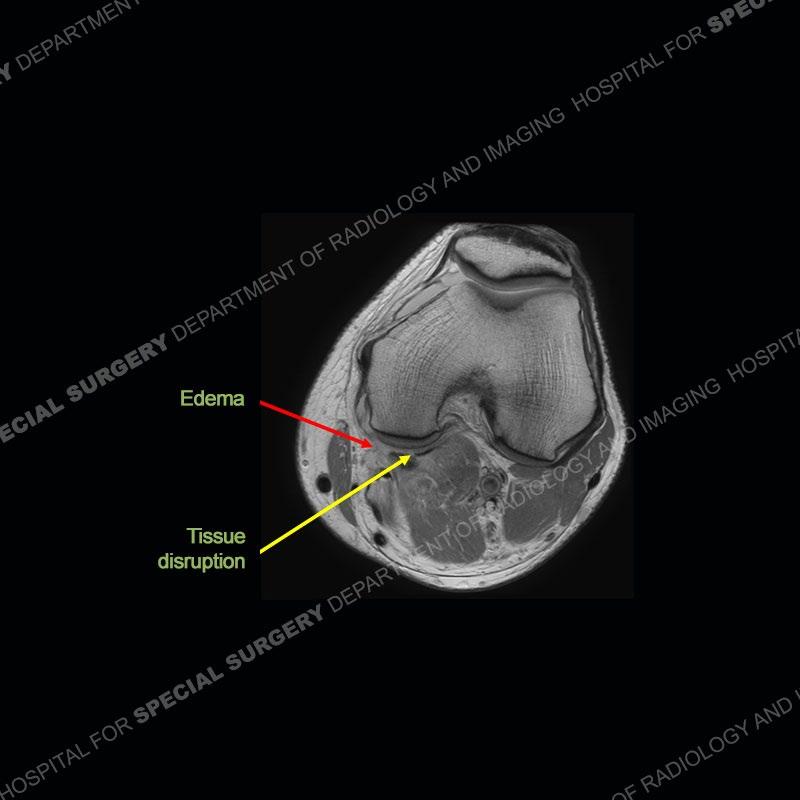
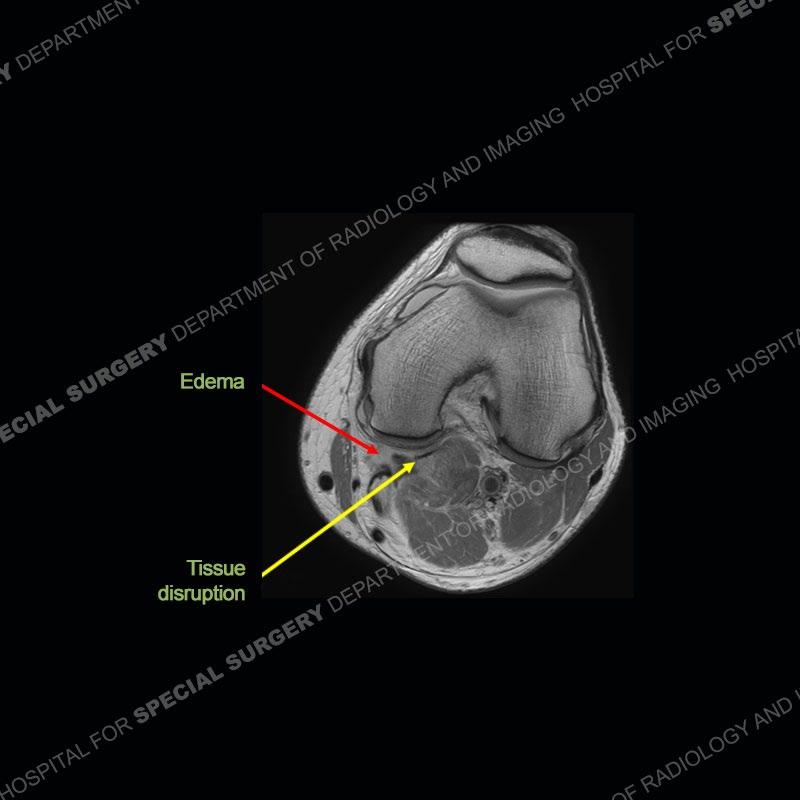
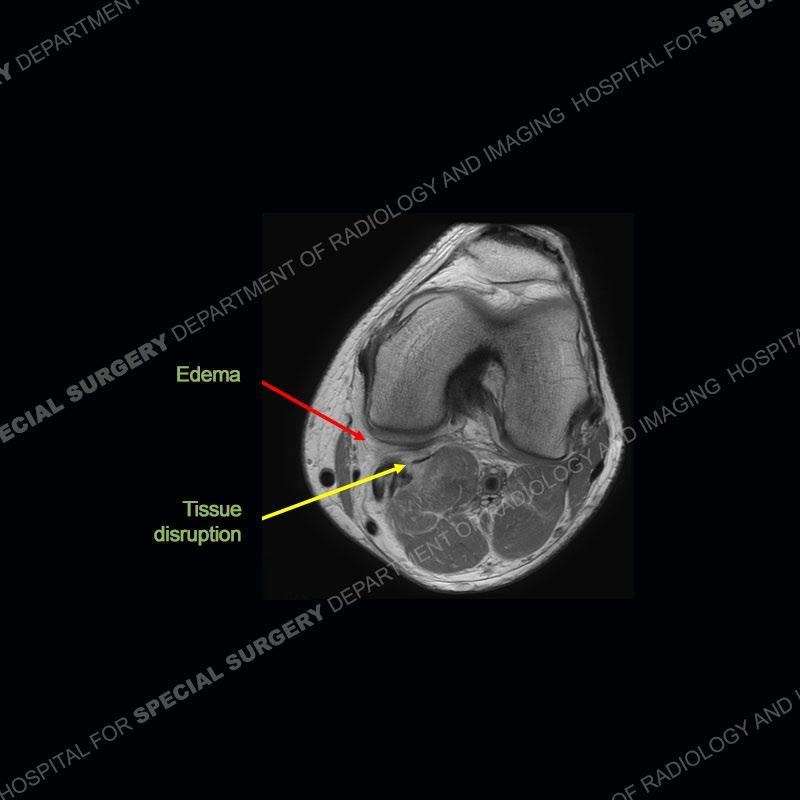
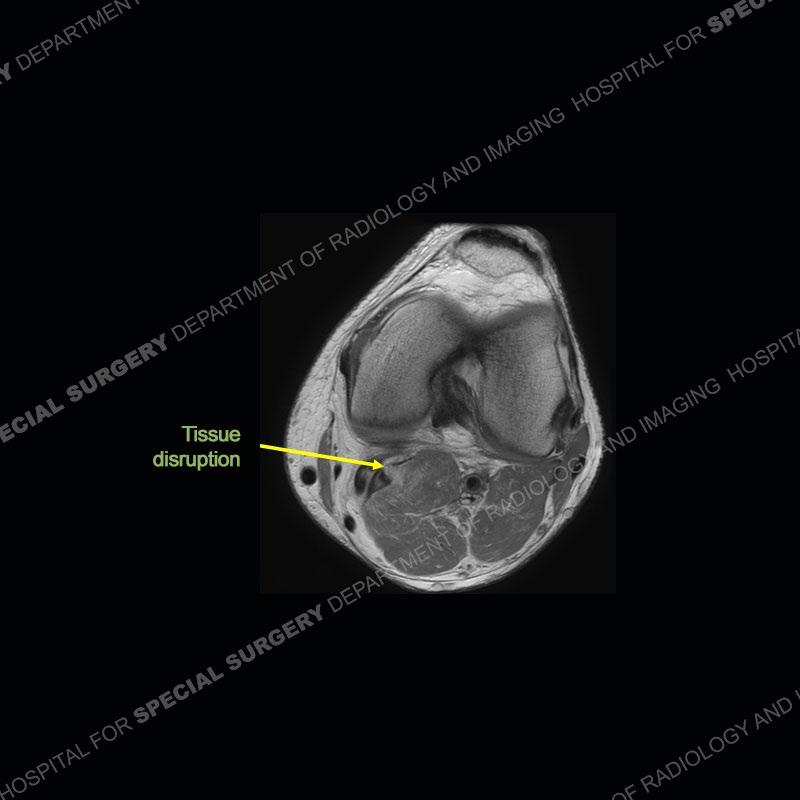
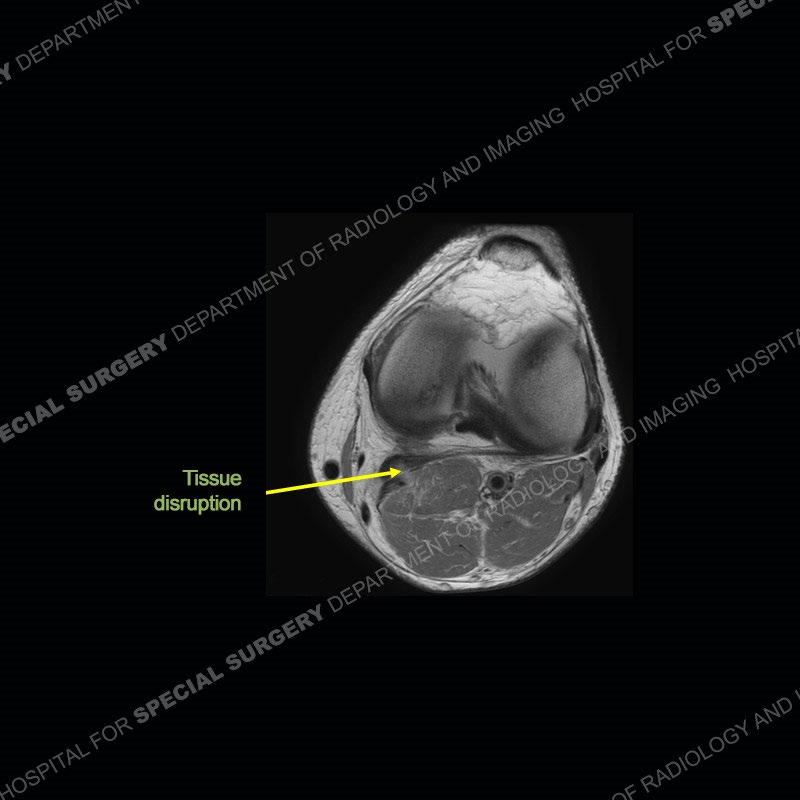
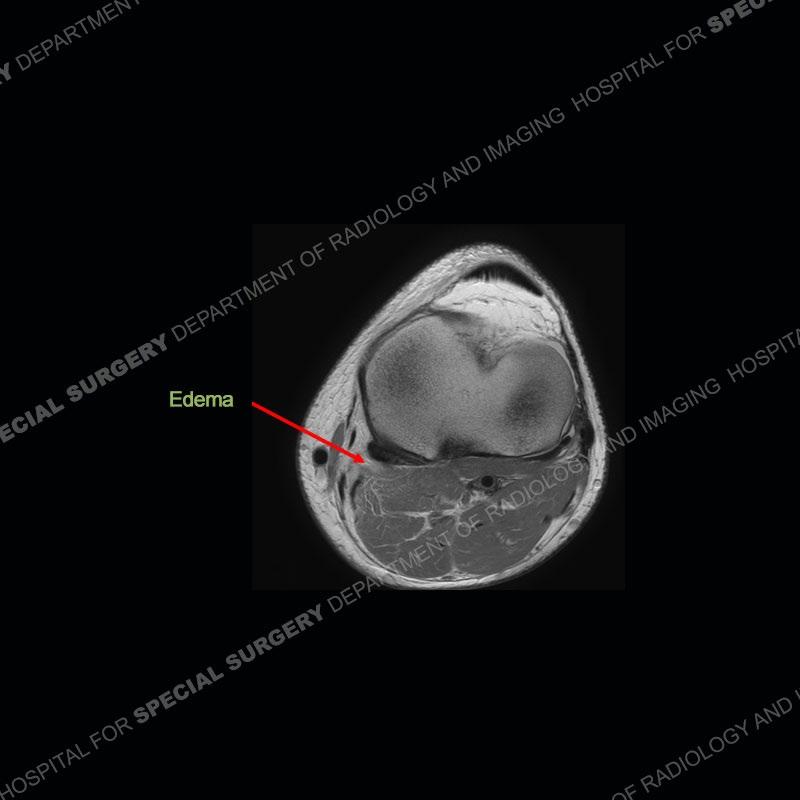
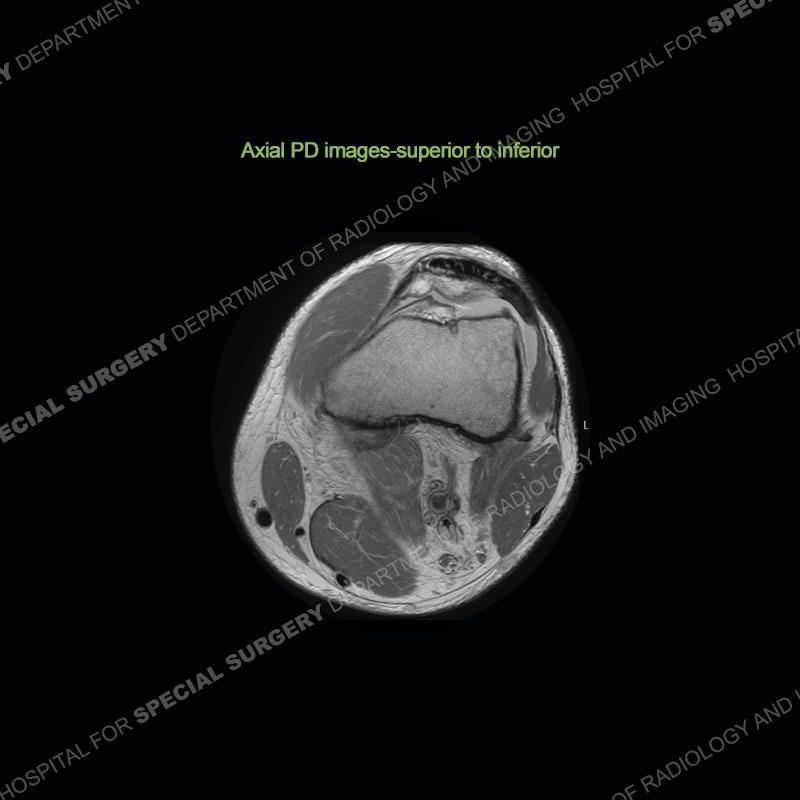
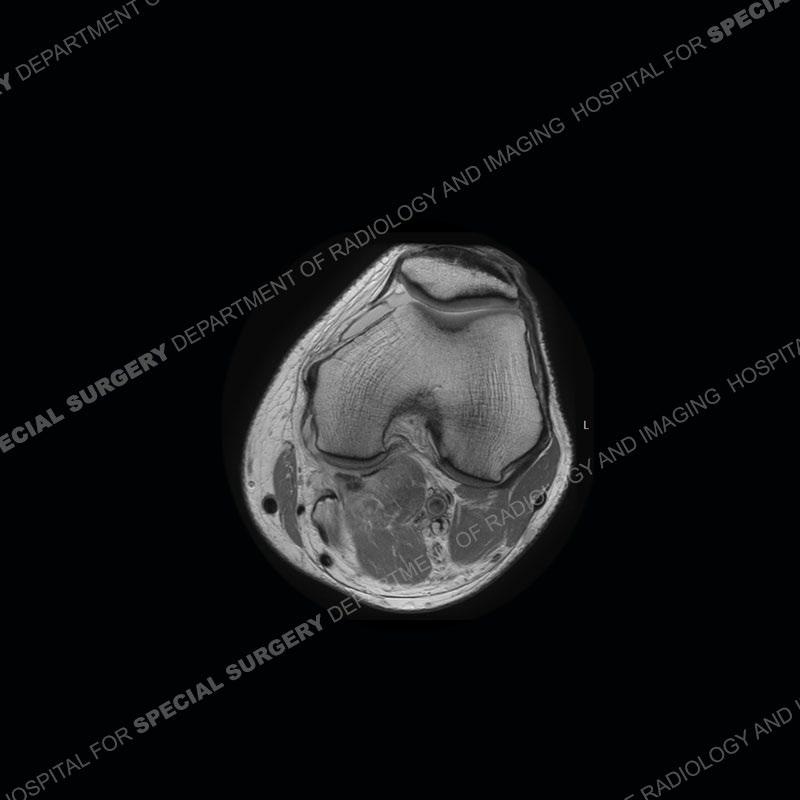
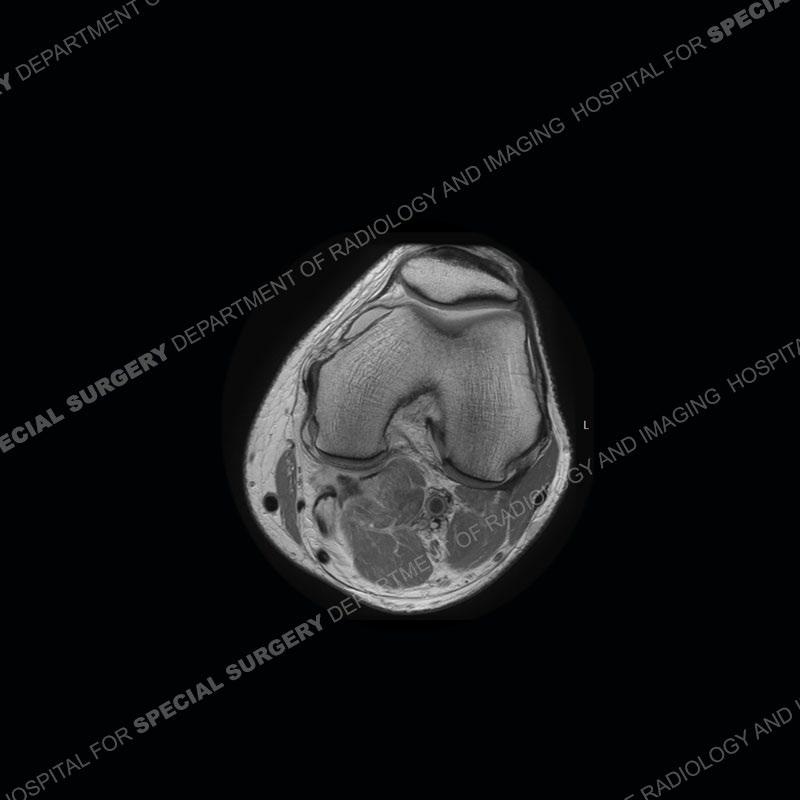
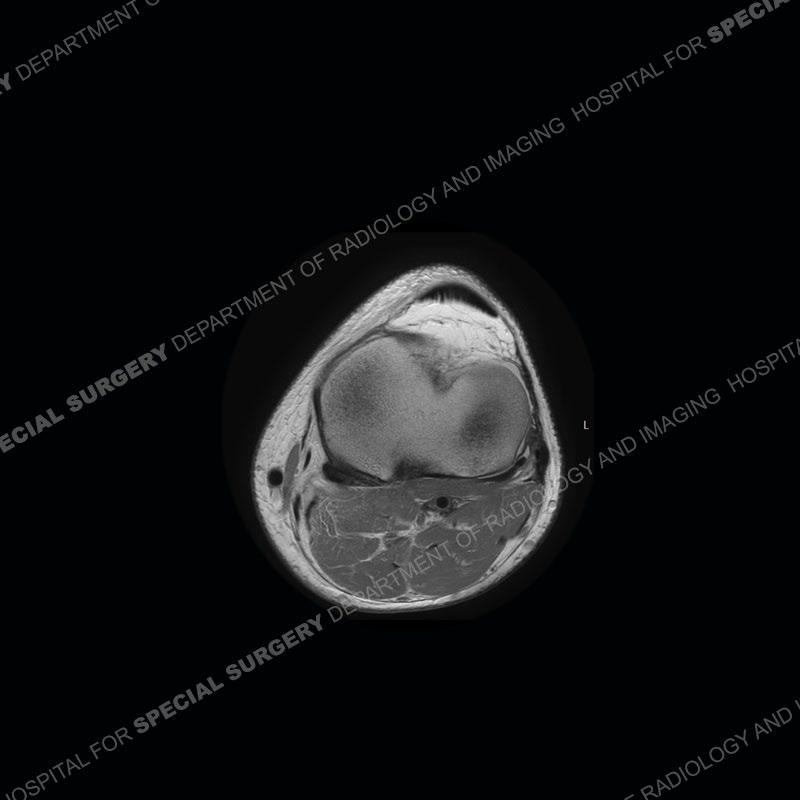
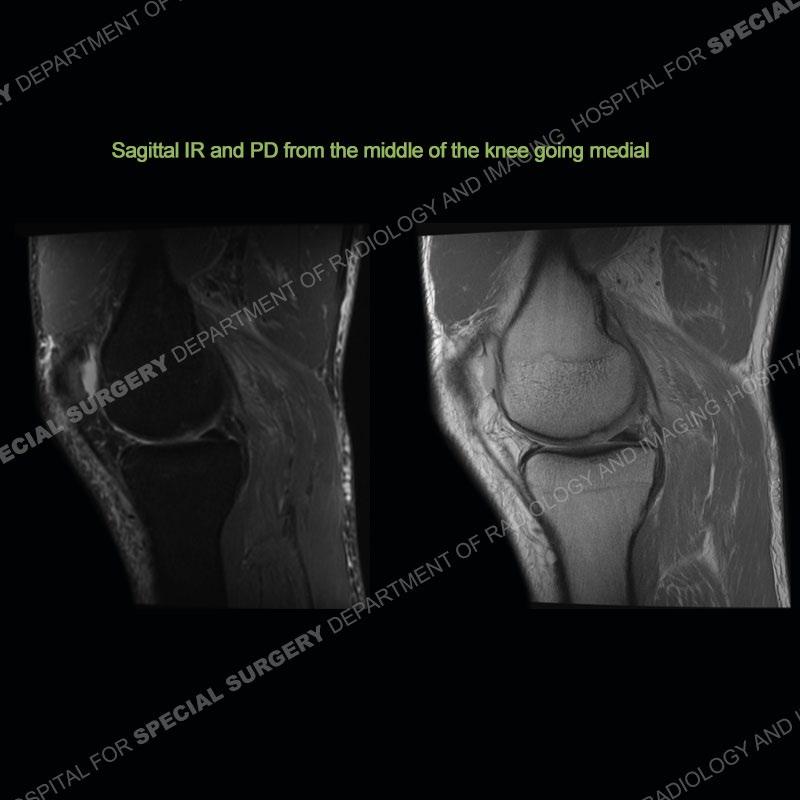
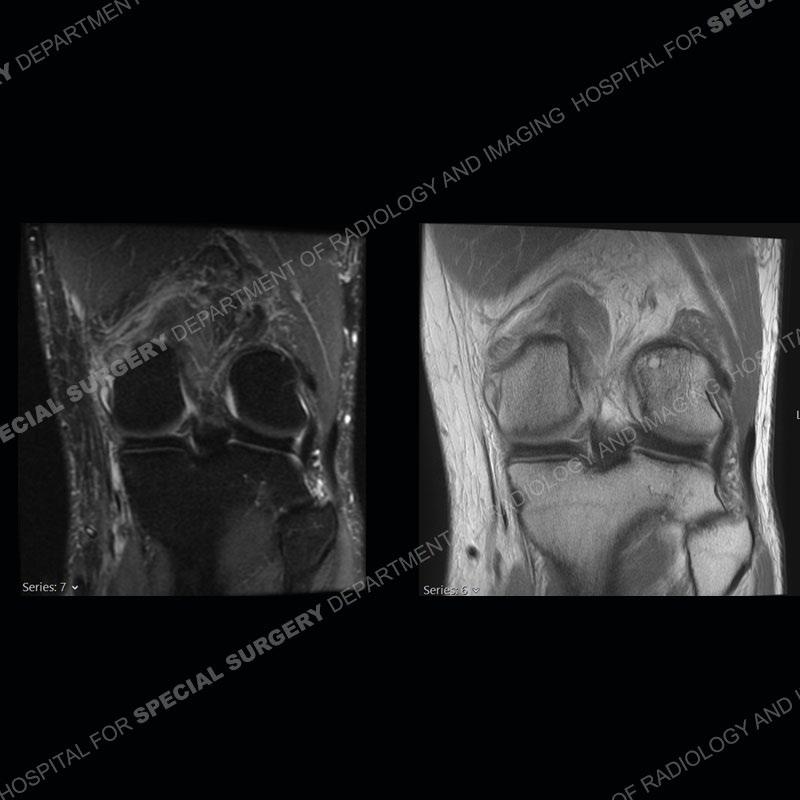
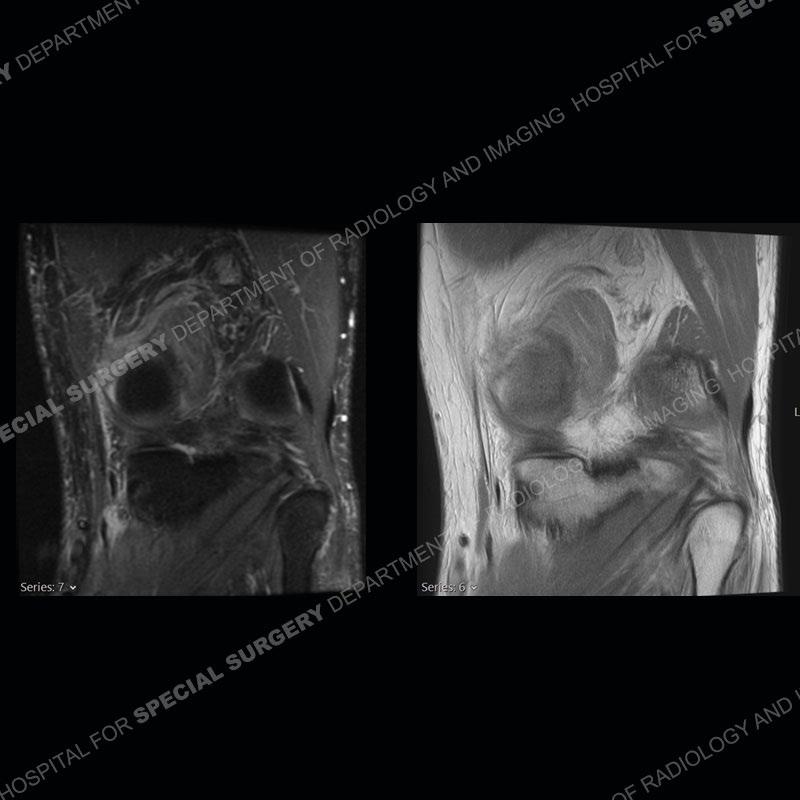
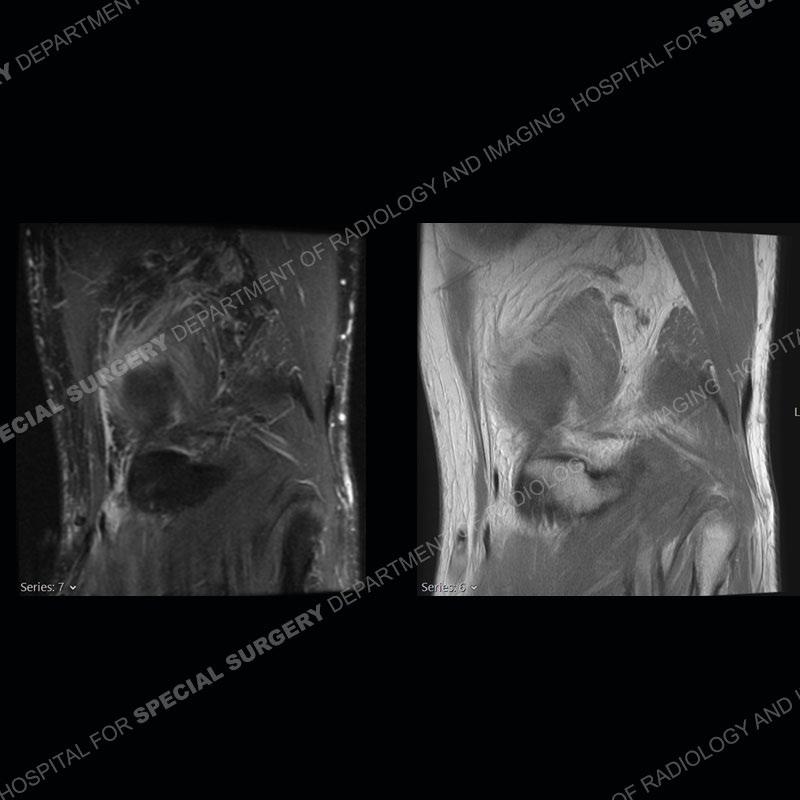
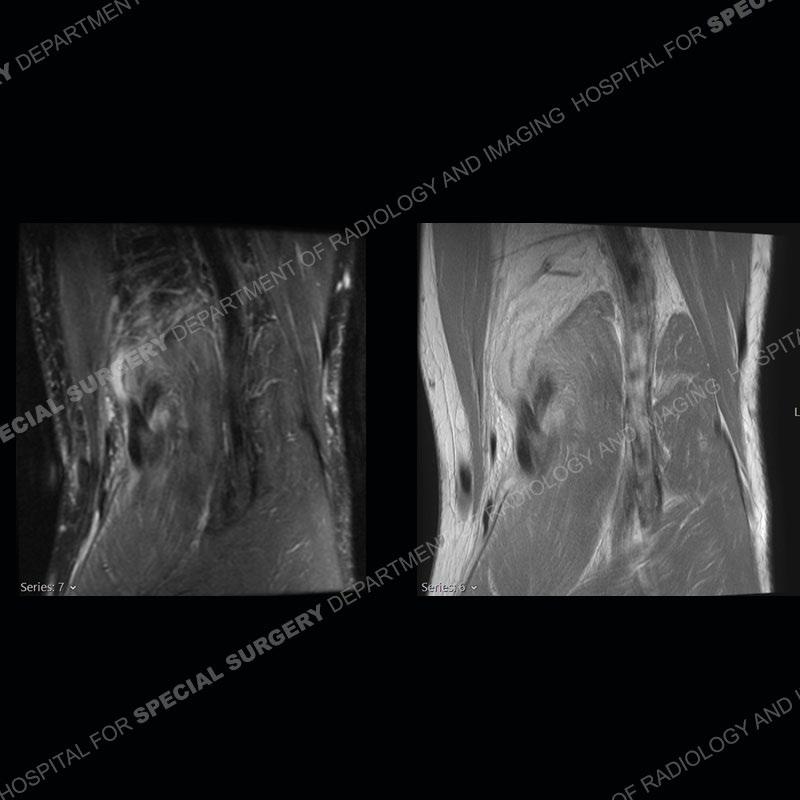
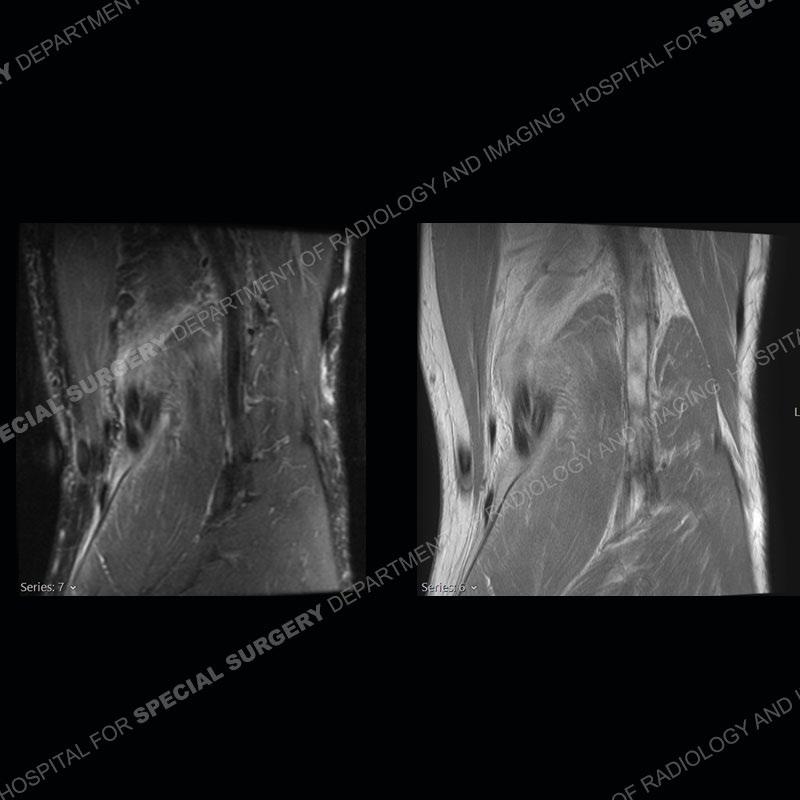
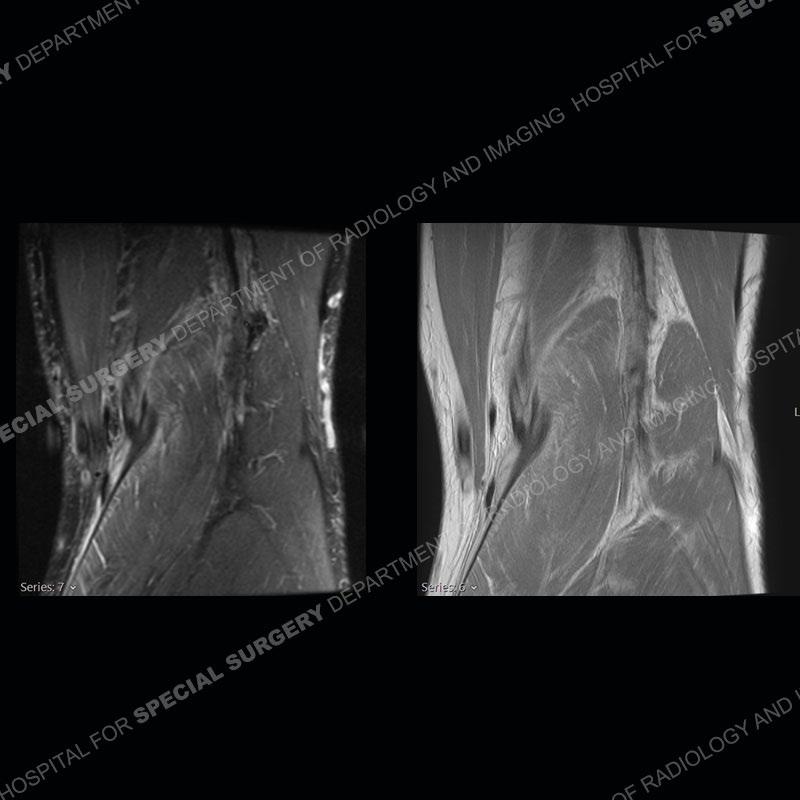
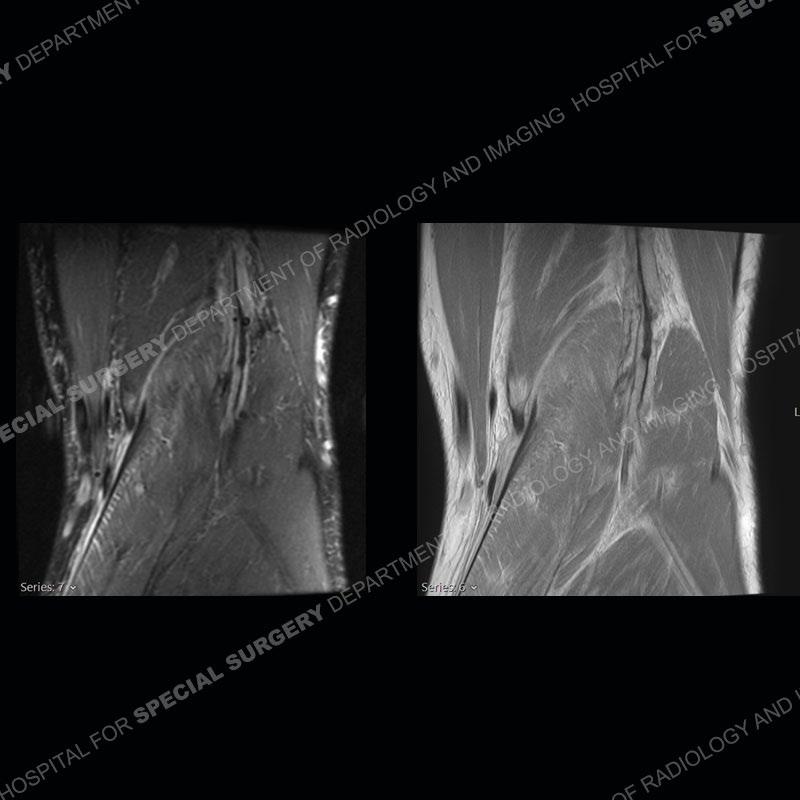
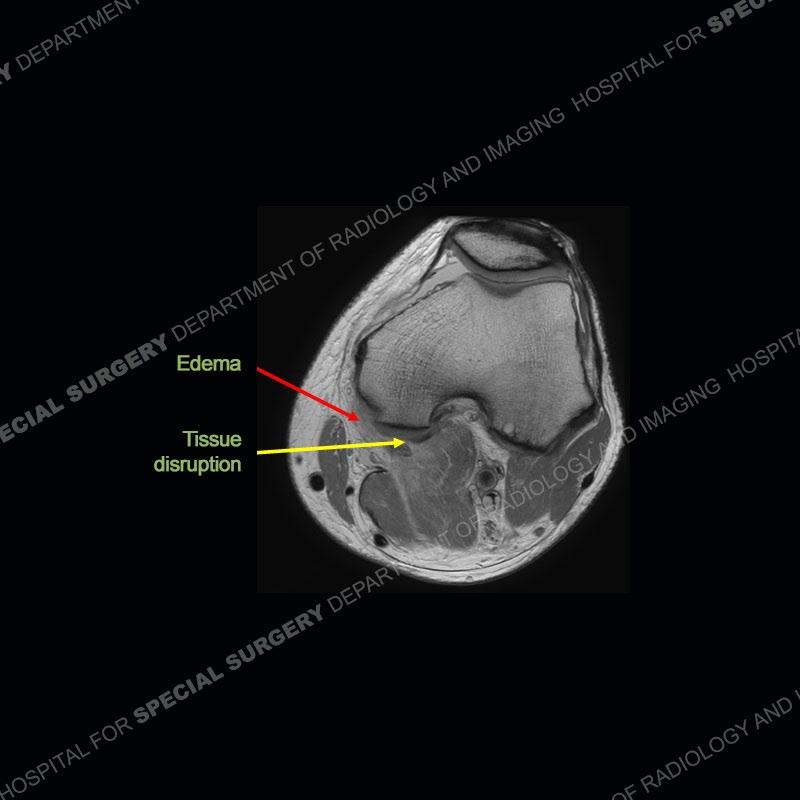
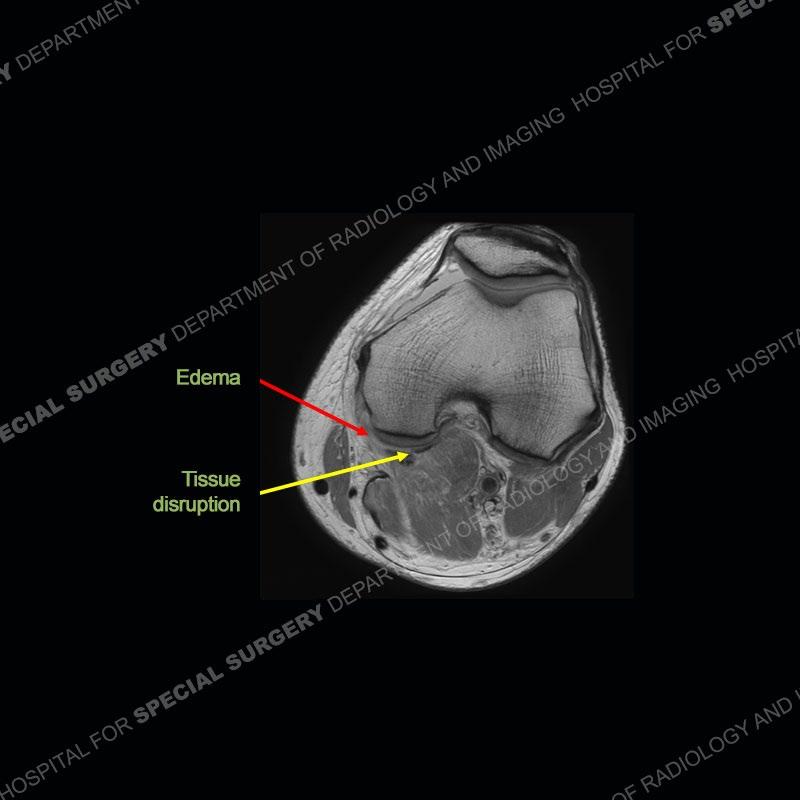
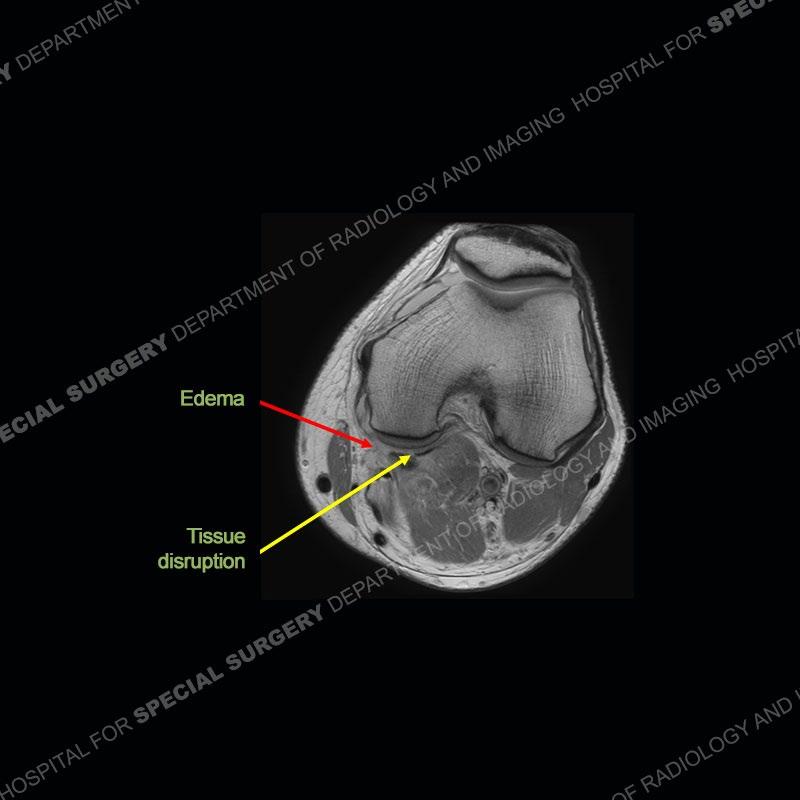
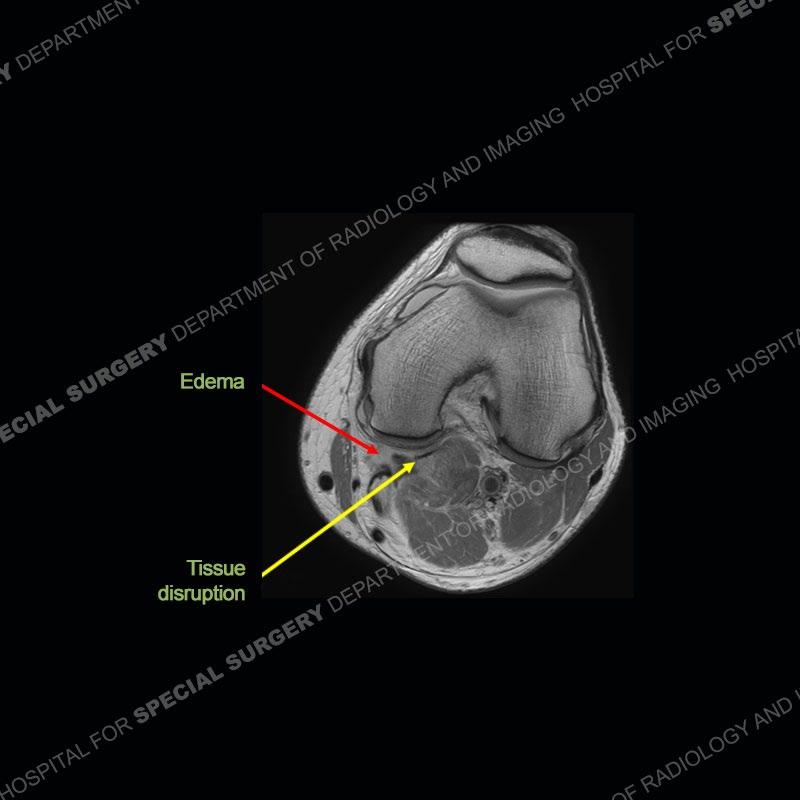
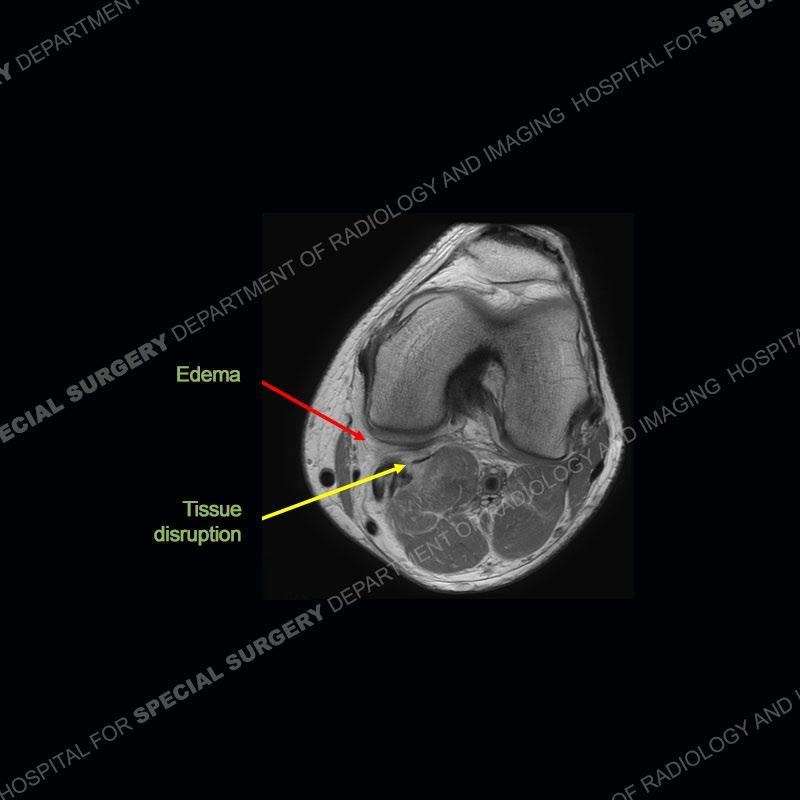
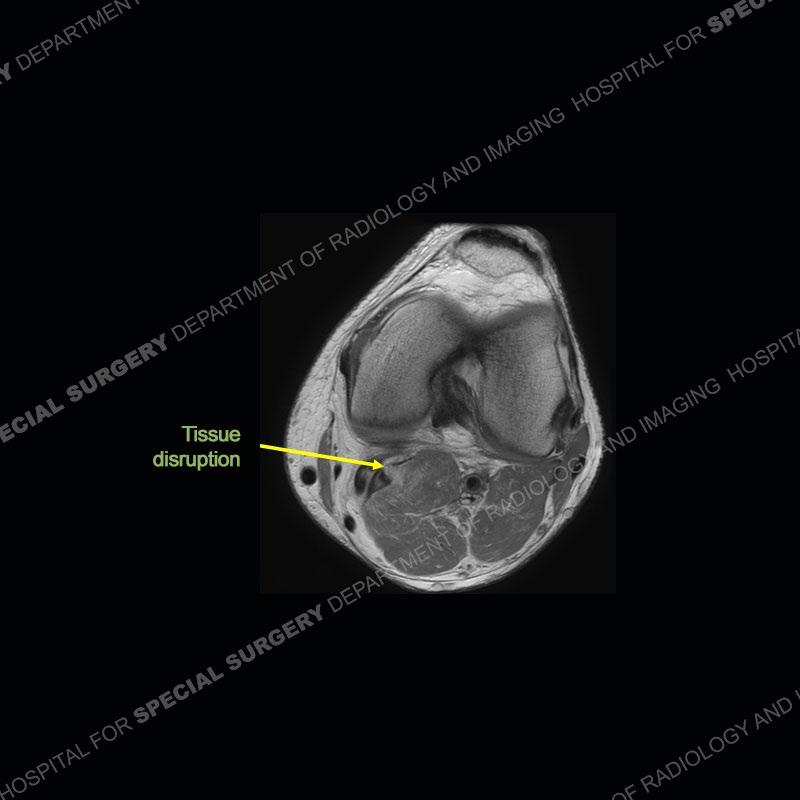
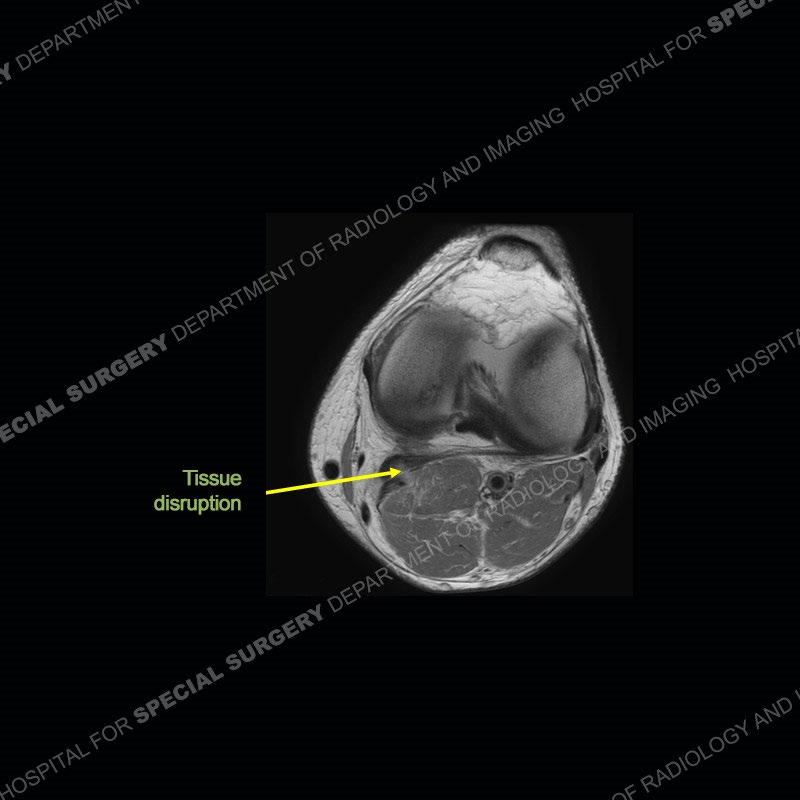
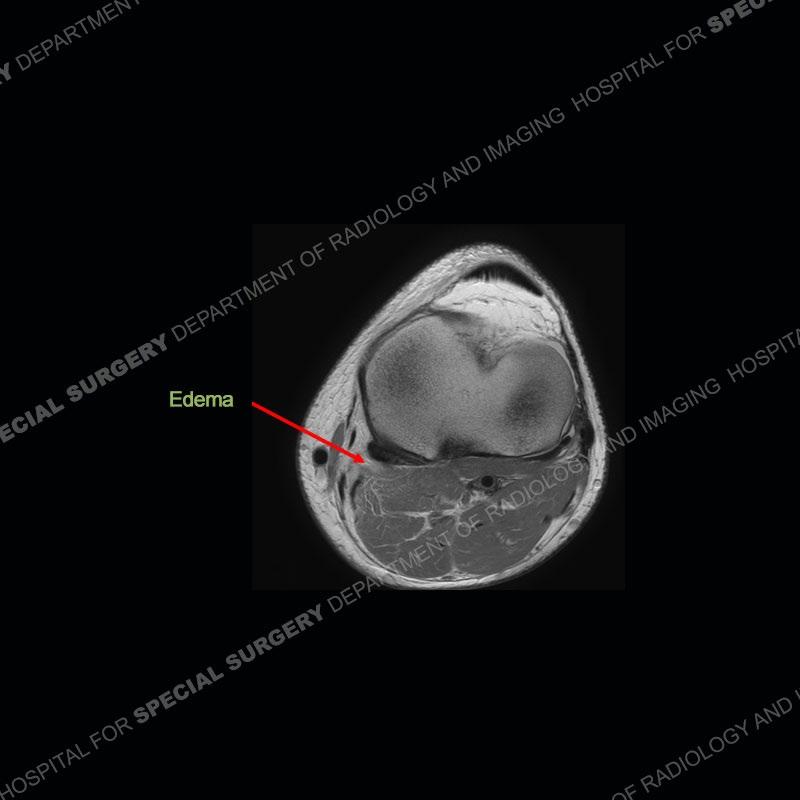
Findings
The radiographs show degenerative change of the medial compartment and a varus knee, but they are not germane to this case. No acute bony injury is present. The MRI shows edema of the posterior medial knee/soft tissue and a focal area of a partially disrupted low signal structure. The details are kept at a minimum in the findings of this case on purpose.

What’s the Diagnosis – Case 180
38
What’s the Diagnosis – Case 180 39
What’s the Diagnosis – Case 180 40
What’s the Diagnosis – Case 180 41
What’s the Diagnosis – Case 180 42
What’s the Diagnosis – Case 180 43
What’s the Diagnosis – Case 180 44

What’s the Diagnosis – Case 180 45
What’s the Diagnosis – Case 180 46
What’s the Diagnosis – Case 180 47

What’s the Diagnosis – Case 180 48

What’s the Diagnosis – Case 180 49

What’s the Diagnosis – Case 180 50

What’s the Diagnosis – Case 180 51

What’s the Diagnosis – Case 180 52

What’s the Diagnosis – Case 180 53

What’s the Diagnosis – Case 180 54

What’s the Diagnosis – Case 180 55

What’s the Diagnosis – Case 180 56

What’s the Diagnosis – Case 180 57

What’s the Diagnosis – Case 180 58
Diagnosis: Partial Disruption Medial Head Gastrocnemius (MHG)
The findings were kept purposefully vague as identifying the structures early on takes away a lot of the diagnosis. An uncommon entity and one of which we do not see a lot. Enthesopathic changes and tendinosis are seen as are distal MHG injuries, but proximal tears are rarely present. This case highlights a number of points. One, it almost always comes down to anatomy. Perhaps not a structure we normally spend too much time on, except save for diagnosing a Baker’s cyst, but knowing where this structure and all structures exist in all three planes is imperative. Second, when you think you are making a “call” or finding that you have never made before, step back and think is this just the abnormal presentation of a common pathology. That situation arises much more frequently. Third, if you look at it once, twice, and probably a third time and are confident in your odd or very rare diagnosis, stick to your guns. Especially, when it comes down to anatomic structures, the proof will be in the images.
Fourth, use all imaging planes and different pulse sequences to make your diagnosis. The edema highlighted in this case can be seen as the obscuration of fat on the PD images but is much easier to perceive as the high signal on the IR pulse sequences. The actual disruption of the MHG myotendinous junction is only able to be seen on the axial images. On the sagittal and coronal images, we get a sense something is wrong but hard to be exact. Lastly, when you look at a study and something just seems off (as I would say the sagittal and coronal images do with that dark band of tissue posteriorly), listen to yourself and go through the study slowly and meticulously. Most of the time you will find you were right, and something indeed is present.

What’s the Diagnosis – Case 180
59
References

Bencardino JT, Rosenberg ZS, Brown RR, Hassankhani A, Lustrin ES, Beltran
J. Traumatic Musculotendinous Injuries of the Knee: Diagnosis with MR Imaging. RadioGraphics October 2000, 20:103-120.
Gabrielle Bergman, M.D. Proximal Gastrocnemius Tendon Pathology. Radsource. MRI Web Clinic — September 2013
What’s the Diagnosis – Case 180
60