





It’s summer. While hospitals are bracing themselves for surges in ERs and further staffing shortages, Doug Ford and his government are taking an extra-long break, with all signs pointing to an early election call.
After six years of Doug Ford, how healthy is Ontario’s public health care system?
If you’re a patient who’s had to access care, you’ve waited longer than you ever have - in ERs, for tests and procedures, or to be seen by a specialist. Too many of you don’t have a family doctor. You struggle to get adequate home care. You can’t find a long-term care bed. You’re shocked to learn that your ER is closed sometimes, or your community hospital is disappearing.
If you’re a nurse or a health-care professional, the staffing shortage is a daily challenge. It’s getting much harder to meet the standards of care you were trained for. You see first-hand how privatization is undermining the public system, and you’re afraid that equal access to care is a vanishing ideal.
That’s just six years of Doug Ford. Imagine another four.








By Leora Goldreich
Primary care providers are the backbone of our healthcare system. For patients seeking medical attention, family physicians are often the first line of contact, providing a comforting face to navigate the complex and often confusing maze that we call ‘Ontario’s healthcare system’. And yet, Ontario is facing a family medicine crisis. Physician Assistants (PAs) are one solution to this crisis.
Earlier this year, the Ontario College of Family Physicians urgently called on the Ontario Government to provide support for family doctors and patients. According to their statement, over 516,000 Torontonians do not have access to a family doctor, and this number is expected to increase to nearly 1 million by the year 2026 (Ontario College of Family Physicians [OCFP], 2024). Across Ontario, this statistic is forecasted to grow to 4.4 million in two years’ time as family physicians retire or switch specialties (OCFP, 2024). According to the college, Ontario’s family medicine crisis can be attributed to several challenges in retaining primary care physicians, including overwhelming time spent on administrative tasks and lack of team supports. Last month, the Ontario Government announced plans for a pilot program where primary care providers will utilize new digital health avenues, including artificial intelligence, to help ease the administrative burden and leave more time for medicine (Ontario Newsroom, 2024). But the
AUGUST 2024 ISSUE
EDITORIAL: July 5
ADVERTISING:
Display – July 26 | Material – July 30
Monthly Focus:
Paediatrics/Ambulatory Care/Neurology/ Hospital-based Social Work: Paediatric programs and developments in the treatment of paediatric disorders including autism. Specialized programs offered on an outpatient basis. Developments in the treatment of neurodegenerative disorders (Alzheimer’s, Parkinson’s etc.), traumatic brain injury and tumours. Social work programs helping patients and families address the impact of illness.
Annual Paediatric Supplement
college notes that more needs to be done to ensure all Ontarians have access to primary care. In addition to easing the administrative burden, the college recommended creating a team-based model of primary care in which family doctors work closely alongside a team of other expert providers to free up the physician’s time for patients who need it most (OCFP, 2023). In such a context, PAs can serve as a crucial support by expanding access to primary care and improving patient outcomes. PAs are highly trained medical professionals who work with physicians to complete patient assessments, diagnose medical conditions, formulate treatment plans, prescribe medication, and work collaboratively to empower patients with health education and counselling (Jones et al., 2021). PAs have been working in primary care medicine in the U.S. for nearly 60 years. Here in Canada, PAs were integrated into the Canadian Armed Forces in the 1980s and into the civilian healthcare system starting with Manitoba in 1999, Ontario in 2007, and other provinces were quick to follow, including British Columbia, Newfoundland and Labrador, and Prince Edward Island most recently in 2023. Since their introduction into Canada’s healthcare system, PAs have had a significant impact on improving access to primary care and easing family physician burden. In primary care, PAs can manage approximately 75 per cent of visits. (Schweitzer & Record, 1981).
Continued on page 6
EDITORIAL: Aug. 9
ADVERTISING: Display – Aug. 23 | Material – Aug. 27
Monthly Focus:
Emergency Services/Critical Care/Trauma/ Emergency/Online Education: Innovations in emergency and trauma delivery systems. Emergency preparedness issues facing hospitals and how they are addressing them. Advances in critical care medicine.
Online Education Focus & Special Focus Emergency Care
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher
Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

By Lise Diebel
If you know someone with diabetes, you may have noticed them wearing an insulin pump. It may even be a high-tech version, consisting of a continuous glucose monitor and computer program that calculates how much insulin they need to keep blood glucose levels in check and automatically deliver dosages.
It’s advanced technology by today’s standards. But what if there was an even better, more accurate way to ensure consistent, correct dosages in medications like insulin, or blood-thinners warfarin and heparin by using artificial intelligence (AI) that teaches itself?
A study by the Hamilton Health Sciences (HHS) CREATE (Centre for Data Science and Digital Health) team explored this, opening the door to use this type of AI in health-care research. “Our results were very promising, and have caught the attention of the wider scientific community,” says Dr. Ted Scott, vice president of innovation and partnerships for HHS.
Medications like insulin, warfarin and heparin need to be dosed just right or they can trigger serious health issues. Warfarin, for example, prevents blood clots, but too small a dose and patients are at risk of a stroke. Too much, and they could start bleeding spontaneously because their blood becomes too thin.
Artificial intelligence that uses reinforcement learning could help advance health-care technology for such patients, says Dr. Jeremy Petch, director of CREATE. Staffed with experts in software engineering, AI and data sciences, CREATE works with hospital clinicians including physicians to develop new ideas and create digital solutions that fundamentally reimagine how health care is delivered. CREATE also works with organizations in both the public and private sector, from local start-ups to national agencies and international bodies.

With reinforcement learning, AI mimics the trial-and-error process that humans use for learning. Algorithms with a reward-and-punishment pattern learn from mistakes in order to find the best ways to achieve positive outcomes.
“It’s the same paradigm of AI that led to computers beating humans in games like chess,” says Petch. “Through trial and error, AI discovers optimal strategies.”
Other types of AI learning are already used in health care, but reinforcement learning using AI has traditionally been avoided, in part because it requires vast amounts of data.
But there’s enormous potential, says Petch, and the CREATE team was able to study reinforcement learning by accessing huge amounts of data from warfarin studies through partnerships with Harvard and Duke universities in
the United States, Uppsala University in Sweden and PHRI, a joint research institute of HHS and McMaster University, a global leader in large clinical trials.
Through this partnership, CREATE gathered the largest data sample ever assembled for the purpose of studying warfarin dosing. “We wanted to explore whether AI could do a better job of helping to get the dose just right on a continual basis,” says Petch.
And while the study focused on warfarin, its results could apply to other conditions, such as diabetes, where constant monitoring of medications is essential for accurate dosing.
“For these patients and their doctors, it’s a never-ending dance to stay at just the right range for optimal dosage management,” says Petch. “For example, foods high in vitamin K, like broccoli, can counteract the blood-thinning effects of warfarin, causing them to bounce in and out
of the therapeutic range. The same is true for someone with diabetes, who may go in and out of the glycemic range if their blood sugar levels aren’t carefully managed.”
Harvard, Duke, Uppsalla and PHRI had run randomized control trials for alternative medications to warfarin. These studies included control groups of patients that continued taking warfarin as their standard of care for comparison’s sake against new drugs being tested. Those control groups were what interested the CREATE team, because they provided data from hundreds of thousands of encounters with doctors responsible for monitoring the warfarin-taking study participants and adjusting their warfarin dosages as needed.
Using this data, the CREATE team was able to use reinforcement learning to train an AI model to recommend warfarin dose changes. It turned out that AI did very well – providing dosage recommendations at the same level as the very best, most highly skilled physicians involved in the studies.
“By simply observing this enormous cycle of data, AI showed that it could learn to dose warfarin as well as the very best, most experienced and highly skilled clinicians who specialize in this area,” says Petch.
Until the CREATE study, no one had rigorously shown that reinforcement learning with AI may have an important place in health care.
“Our study has opened that door,” says Petch. “As well as showing the potential to develop a whole new and better approach for dosing these kinds of medications, we’ve helped establish that using this paradigm of AI can work in health care with enough data. That’s what really interested us and the wider scientific community.” n H
Astudy from the University of Saskatchewan’s College of Medicine provides a picture of anti-Black racism in medical school at a Canadian university. The study is published in CMAJ (Canadian Medical Association Journal).
“Our findings provide empirical evidence to reveal the extent and specific nature of racism in a Canadian medical school; we suspect Black students in many other medical schools experience similar racism,” writes Dr. Jacob Alhassan, University of Saskatchewan, Saskatoon, Saskatchewan, with coauthors. This racism stems from historical, anti-Black policies, which endure in subtle and pernicious forms in today’s medical system and medical education.
Based on interviews conducted at the medical school between May and July 2022, the study revealed 5 central themes describing experiences with, and exposures to, racism in medical education that can worsen as learners progress through the medical system. Anti-Black racism negatively affects medical learners – for example, repeatedly question-
Continued from page 4
ing their competence fosters self-doubt and low confidence in their medical abilities – as well as patients.
“Experiences of racism are encountered through microaggressions and uncomfortable encounters, blatant comments, the medical curriculum, and medicine’s inherent hierarchical structures. Intersecting oppressions (e.g., being Black and a woman) compound experiences of anti-Black racism and, as learners progress in medical education, racist experiences may worsen,” the authors write.
They suggest that the medical system needs to reorient its perspectives and practices as part of an ongoing process. This should include a yearly review of medical curriculum to ensure that Black representations are appropriate and accurate.
“[M]uch of this discussion highlights the need for decolonization of medicine and an examination of how the structure of medical education contributes to racist encounters between Black learners and medical faculty,” write the authors. “Although some form of hierarchy can be useful
In a study evaluating the efficacy of PA utilization in Canada, around 95 per cent of physicians working with PAs said that having a PA in their clinic allowed them to increase the number of patients seen per day and improve clinic efficiency overall (n = 83; Burrows et al., 2023). Around 90 per cent of physicians working with PAs noted that PAs helped to improve the quality of care provided to patients and around 88 per cent indicated that having a PA on their team improved their own overall well-being (n = 84; Burrows et al., 2023). As a PA student, I am humbled to be joining a community of providers committed to en-
hancing healthcare access in Canada.
Clearly, PAs have an important role to play in helping restore Ontario’s family medicine landscape. Despite their proven value, PAs continue to face barriers, including limited recognition, regulatory challenges, and sustainable funding models. It is incumbent upon our healthcare institutions, policymakers, and stakeholders to address these challenges and welcome PAs as part of the primary healthcare team to maximize their contribution to patient care. Investing in Ontario’s PAs means supporting family doctors and protecting the health of Ontario’s most vulnerable. n H
Leora Goldreich (Goldstein) BSc., MSc. is a Physican Assistant Student in Toronto.
for role modelling and maintaining order in the clinical setting, many of the negative experiences described by Black medical learners show that a toxic combination of hierarchy, power, and prestige can breed unaccountability, expressed in blatant racism.”
In a commentary on a related topic, authors emphasize that Canada’s Black population is very diverse and that this diversity – and associated unique experiences of anti-Black racism and racial discrimination – should be recognized in health research and health care.
“Ignoring the diverse identities and social positions of Black people can lead to overgeneralized findings that fail to recognize nuanced intersections
with anti-Black racism that drive inequities in health and health care,” writes Khandideh K.A. Williams, McGill University, Montréal, Quebec, with coauthors.
“Without acknowledging the within-group diversity of Canada’s Black communities, health care policies and interventions aimed at addressing anti-Black racism are unlikely to make much of a difference,” they conclude.
“Variegated racism: exploring experiences of anti-Black racism and their progression in medical education” and “Embracing Black heterogeneity: the importance of intersectionality in research on anti-Black racism and health care equity in Canada” were published June 10, 2024. n H
With wildfires becoming more frequent and extensive in Canada, it’s important for people to understand the health risks of wildfire smoke.
An article in CMAJ (Canadian Medical Association Journal) aims to provide information for clinicians and people in Canada as wildfire season is upon us.
“As climate change causes more frequent and severe wildfires, wildfire smoke becomes a larger health problem,” says Dr. Mehdi Aloosh, assistant professor, Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, and medical officer of health of Windsor–Essex County, Ontario. “Communities need to be aware and prepared to reduce the harmful health effects of wildfire smoke, and health care practitioners play a crucial role in this effort.”
1. Exposure to wildfire smoke is linked to negative health outcomes, including respiratory conditions, such as asthma, and heart issues.
3. The Air Quality Health Index (AQHI) is a useful tool to communicate risk of wildfire smoke. The AQHI scale measures air quality on a scale of 1–10, and a level of more than 7 indicates that at-risk people, including those with respiratory and chronic diseases, older adults, pregnant people, and children, should minimize time spent outdoors in strenuous activity.
4. Health care providers can help people understand health risks. Clinicians should discuss the risks of wildfire smoke with at-risk patients, the usefulness of the AQHI, and the value of indoor air filtration, and ensure patients with respiratory conditions have updated action plans and an adequate supply of medications.
5. Reducing exposure will reduce health risks. Staying indoors and using high-efficiency particulate air cleaners, and when outside wearing well-fitted N95 or KN95 masks can reduce exposure to fine particles by more than 90 per cent.
“Wildfire smoke” was published June 17, 2024. n H
2. Wildfire smoke can be more toxic than other types of air pollution. The fine particulates in wildfire smoke can travel more than 1000 km, enter the body, generate free radicals, and cause inflammation in body organs.
Recent study reveals that the risk of developing type 2 diabetes is increased in women who first get gestational diabetes during a second pregnancy, and that it increases even more for those who get it during two consecutive pregnancies.
One in 10 Canadian adults has type 2 diabetes, a disease that damages blood vessels and can lead to heart disease, stroke, kidney disease and even blindness.
Women with gestational diabetes – temporary diabetes during pregnancy – are at higher risk for future type 2 diabetes later in life. But from one pregnancy to the next, how does this risk evolve? A new study from the Research Institute of McGill University Health Centre (RI-MUHC) shows that women who have gestational diabetes for the first time in a second pregnancy have a 76 per cent higher risk of future type 2 diabetes than women with gestational diabetes in the first pregnancy but not in the second. Women with gestational diabetes in both pregnancies are at the highest risk, more than 3.5 times higher than
those with gestational diabetes only in their first pregnancy. The study authors hope that the results of the study recently published in JAMA Network Open will enable women to benefit from personalized advice to reduce their risk of developing type 2 diabetes.
“Around 10 per cent of pregnancies are affected by gestational diabetes overall. Our study shows that future diabetes risk differs in relationship to which pregnancy is affected by gestational diabetes and how many gestational diabetes pregnancies there are. We can help mothers personalize risk estimates with this and other information, so that they can make informed choices about when and how to take action on prevention,” says Dr. Kaberi Dasgupta, senior author of the study and Senior Scientist in the Metabolic Disorders and Complications Program at the RI-MUHC
Using data from Quebec health administrative and birth and death registries, the researchers built a study group of 431,980 women with two deliveries between 1990 and 2012. They did not have diabetes before or between their pregnancies. The researchers looked at whether they had developed diabetes by 2019.
More than 10,000 women had gestational diabetes only in their first pregnancy, more than 16,000 had it only in their second, and more than 8,000 had it in both pregnancies (respectively, 10,920 women (2.5%), 16,145 women (3.7%) and 8255 women (1.9%)). Overall, more than 12,000 developed type 2 diabetes.
Compared with women who had never had gestational diabetes, those who had gestational diabetes during
Many health-care providers are ill-equipped
McGill study finds only 13 per cent of those surveyed received training on child maltreatment and its effects on pain assessment
Many health-care professionals are ill-equipped to assess pain in children who have suffered abuse, a new study by McGill researchers suggests. This can lead to inadequate pain treatment, making the physical and emotional effects of abuse even worse.
“Our findings show a critical need for training programs for health-care providers about the effects of child maltreatment,” said Matthew Baker, the study’s lead author and a PhD stu-
“OUR FINDINGS SHOW A CRITICAL NEED FOR TRAINING PROGRAMS FOR HEALTH-CARE PROVIDERS ABOUT THE EFFECTS OF CHILD MALTREATMENT,”
dent in the School/Applied Child Psychology program at McGill.
The researchers surveyed 100 health-care providers in Canada and the United States, using an online questionnaire. They found only 13 per cent had received training on child maltreatment and its effect on assessing pain in children with a history of abuse. Those who had received con-
tinuing education on child maltreatment were more likely to consider its impact on a child’s pain reports and adapt their assessments accordingly.
“With so few providers trained, it’s vital to raise awareness and improve education on how abused children present in health-care settings in order to enhance their treatment outcomes,” Baker said. n H
their first pregnancy had over 4 times the risk of future type 2 diabetes (4,35), those with gestational diabetes in the second pregnancy only had more than 7.5 times the risk (7,68), and those with gestational diabetes in both pregnancies had a nearly 16 times higher risk (15,8).
“Our results suggest that women who had gestational diabetes in their first pregnancy, but not in their second, were probably able to change their eating habits and increase their physical activity between the two pregnancies. We can now tell them that they have also lowered their risk of future diabetes, which could encourage them to maintain their healthy life habits,” explains Joseph Mussa, first author of the paper and PhD candidate in the Department of Epidemiology and Biostatistics at McGill University.
“On the other hand, women diagnosed with gestational diabetes in a second pregnancy have moved to an increased level of risk. We need to help them manage this risk. We also need to provide women who have had two occurrences of gestational diabetes with urgent support to improve their health and reduce their risk,” adds Dr. Dasgupta, who is also a professor at McGill University’s Faculty of Medicine and Health Sciences and an internist at the MUHC.
The researchers performed several analyses, taking into account various known risk factors for type 2 diabetes. As expected, having gestational hypertension, giving birth to a baby with a high weight for gestational age, or having a partner with diabetes, were associated with an increased risk of the mother developing type 2 diabetes. The risk was also increased for women with mood disorders, drug or alcohol addiction, thyroid problems, arthritis or respiratory problems. n H
t’s estimated that 70 per cent of people with asthma or COPD go undiagnosed. This is the first study to prove that treating those people makes a real difference to their health and quality of life.” -Dr. Shawn AaronFinding and treating people with undiagnosed asthma or chronic obstructive pulmonary disease (COPD) improved their health and reduced their healthcare visits for respiratory symptoms in the year after diagnosis, according to a world-first clinical trial published in the New England Journal of Medicine.
“I Dr.
“It’s estimated that 70 per cent of people with asthma or COPD go undiagnosed.” said study lead Dr. Shawn Aaron, a senior scientist and lung specialist at The Ottawa Hospital and professor at the University of Ottawa. “This is the first study to prove that treating those people makes a real difference to their health and quality of life.”
How did the research team find undiagnosed cases?
To find people with undiagnosed asthma and COPD, the research team called random phone numbers at 17 study sites across Canada from 2017 to 2023. An automated call asked whether any adults in the household had unexplained shortness of breath, wheezing, prolonged cough or were coughing up mucus in the past six months.
The 26,905 people who reported these symptoms completed questionnaires. Those most likely to have asthma or COPD did a spirometry breathing test, the gold standard for diagnosis.
A total of 595 people were diagnosed with either asthma or COPD, and 508 agreed to participate in a randomized controlled trial to compare different types of care.
Half the people in the trial were randomly assigned to usual care (care provided by their primary care provider or a walk-in-clinic), while the other half were treated by a lung specialist and asthma/COPD educator (a specially-trained nurse or respiratory therapist).

“IT’S ESTIMATED THAT 70 PER CENT OF PEOPLE WITH ASTHMA OR COPD GO UNDIAGNOSED.”
Individuals treated by a lung specialist and educator were prescribed inhalers to treat their asthma or COPD and were taught how to use them. Some were given action plans to help them manage disease flare-ups themselves. They were provided with smoking cessation treatment, exercise and weight counselling, and pneumonia and flu vaccines if appropriate.
Ninety-two per cent of patients seen by a lung specialist and asthma/COPD educator started new medications for asthma or COPD, compared to 60 per cent of patients who received usual care.
Treating undiagnosed asthma, COPD leads to fewer healthcare visits
The researchers found that patients seen by a lung specialist and asthma/ COPD educator averaged 0.53 healthcare visits per year for respiratory symptoms in the year after diagnosis, compared to 1.12 visits in the usual care group.
In addition, patients seen by a lung specialist and asthma/COPD educa-
tor saw their average score on the St. George’s Respiratory Questionnaire rise by 10.2 points, compared to 6.8 points for the usual care group. A fourpoint rise means an improvement in health and quality of life.
“In the real world, not everyone can see a lung specialist,” explains Dr. Aaron. “The good news is that as long as a patient gets diagnosed and treated, their symptoms will improve. The people in our study who went to primary care providers and walk-in clinics had great outcomes, and those who went to a lung specialist and asthma/COPD educator had excellent outcomes.”
“The asthma diagnosis makes a big difference. I’ve noticed an increase in energy. I have two small kids now and I can keep up with them. I sleep better because I used to regularly wake up struggling to breathe.” – study participant Jazzminn HeinJazzminn Hein was 24 years old and had recently given birth to her first child when she got the call invit-
ing her to join the study. Carrying a few loads of laundry up the stairs or talking on the phone for 10 minutes would leave her breathless. She didn’t see the downside to getting a breathing test.
“For years I told doctors about this elephant on my chest and struggling to breathe. They said it was my anxiety, that I was having panic attacks.” remembers Jazzminn. But it wasn’t panic attacks. It was asthma. Asthma that she’d likely had since grade school. A daily inhaler turned her symptoms around.
“The asthma diagnosis makes a big difference,” she says. “Your muscles need oxygen, and when you can’t breathe properly it makes you sore and tired all the time. I’ve noticed an increase in energy. I have two small kids now and I can keep up with them. I sleep better because I used to regularly wake up struggling to breathe.”
Asthma affects eight per cent of Canadian adults and can develop at any age, while COPD affects eight per cent of Canadians over the age of 60.”If you have breathing symptoms like mine, go to your doctor or a walk-in clinic and ask for a spirometry test,” recommends Jazzminn. “The worst that can happen is that you’ll have wasted your time. But if you do have a respiratory disease and get it properly treated, you’ll be able to do things you hadn’t realized you missed.”
Dr. Aaron agrees with Jazzminn. He thinks the best way to catch more cases of undiagnosed asthma and COPD is for patients to advocate for themselves. His past research found that even early stages of these diseases are linked with worse quality of life, greater healthcare use and decreased work productivity.
“Many people know to ask for breast cancer and colon cancer tests when they see certain signs. Ideally, they’d ask for a spirometry test when they notice symptoms of chronic respiratory diseases,” says Dr. Aaron. “People don’t have to put up with these breathing problems when there is effective treatment available.” n H
Marilyn Jackson recalls waking up, breathless, with a terrible cramp in her leg.
“I’m going to die, I remember thinking.”
The 87-year-old has since learned that her shortness of breath was due to heart failure. With the help of a few medications, Marilyn is breathing easy now and living independently.
“I clean my house, do errands using my walker and see friends and family a lot,” says Marilyn, an avid piano player and former downhill skier on Canada’s national team. “I’ve always been active, so it’s a relief to have such a simple plan that allows me to do the things I want to.”
Heart failure, which occurs when the heart is damaged or weakened, has no cure, but can be effectively treated with the right medication and lifestyle modifications, says Dr. Stephanie Poon, Director, Sunnybrook’s Heart Function Clinic. Currently over 800,000 Canadians are living with heart failure.
“Our goal is to provide patients like Marilyn, and their families, with strategies to greatly improve their quality of life,” says Dr. Poon.
She notes that some patients are prescribed puffers and antibiotics for months before a correct diagnosis is made. “Those are really missed opportunities, where people aren’t receiving the correct treatment, and the disease progresses. The result is that rates of heart failure are rising. And this is amid the reality that heart failure is deadlier than many common forms of cancer.”
She urges people experiencing shortnwess of breath, swelling in their legs or abdomen and fatigue, to seek testing for heart failure. A blood test called natriuretic peptide (NP) levels, also known as BNP or NT-pro BNP, is a reliable diagnostic tool. Elevated NP levels indicate that symptoms may be related to heart failure, prompting further investigation by a physician.
Sunnybrook’s Heart Function Clinic has incorporated the Medly app into their model of care, enabling patients to record daily weight, blood pressure, heart rate, and symptoms.
In turn, patients receive instant electronic feedback on how to adjust their medications or alerts based on personalized thresholds and care plans.
Marilyn Jackson

A nurse practitioner uses a web-based dashboard to assess patients’ health status and respond to alerts generated through the app.
“By enabling early interventions in response to symptom changes, the Medly app can result in dramatic improvements to patients’ health and reductions in hospitalizations,” says Dr. Poon.


For Marilyn, the combination of medication and ensuring she drinks roughly two litres of water a day has made a massive difference. “If I could say anything from my experience, it’s to not delay seeking care if you’re not feeling right,” adds Marilyn. “There are treatment options that can be as simple as taking medication.” n H
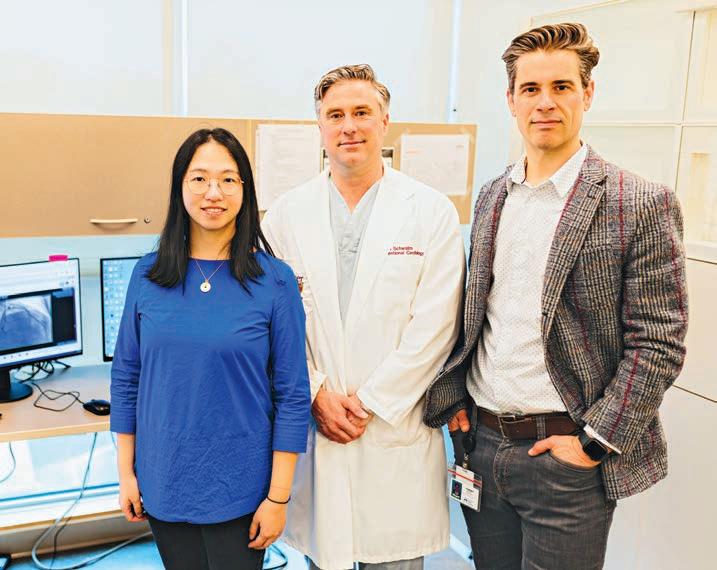
By Lise Diebel
Anew Hamilton Health Sciences (HHS) study will harness the power of artificial intelligence (AI) to help determine which cardiac patients need an invasive procedure to check for life-threatening artery blockages to the heart, and which patients who would benefit from a simpler, non-invasive test using CT scanning.
The two-year randomized control trial, where participants are assigned into the research study group or a control group, is expected to launch in June and involve up to 150 patients from HHS Hamilton General Hospital (HGH) and Niagara Health’s St. Catharines Hospital site.
“Very few randomized control trials of AI are happening in health care, so this is considered a landmark study,” says Dr. J.D. Schwalm, an interventional cardiologist at HGH and director of HHS’ Centre for Evidence-Based Implementation (CEBI), established to advance health care through research and education. CEBI partnered with HHS Centre for Data Science and Digital Health (CREATE) for this trial, and research leading up to it. The trial received funding from Hamilton Academic Health Sciences Organization and the Population Health Research Institute, a joint institute of HHS and McMaster University.
Based on previous research including a study of patient data going back 12 years, this AI tool is expected to be faster and better at ensuring patients are directed to the best test for their condition. For example, the AI tool will recommend patients for an invasive coronary angiogram if they have a higher chance of blockage in their heart arteries based on their medical information. The AI tool can also identify patients who likely don’t have a blockage, and will recommend them for CT scanning. This tool has the potential to improve patient outcomes, advance health equity and lower the cost of health care.
“Ultimately we want to scale this AI tool provincially, if we can prove through this latest study that it delivers what we believe it can,” says
Dr. Tej Sheth supervises an invasive coronary angiogram in the Heart Investigation Unit at HHS Hamilton General Hospital

Schwalm, adding that the team is also in the process of validating this model at the provincial level with data from ICES, an independent, non-profit research corporation.
“The province, in its Auditor General report, found that there’s a need for system-level improvements to ensure patients don’t undergo unnecessary and costly treatments,” says Dr. Ted Scott, HHS vice president of innovation and partnerships. “This new trial, and the work leading up to it, illustrate the power of AI when it is implemented using evidence-based methods to improve patient care and drive system efficiencies.”
An invasive coronary angiogram procedure is considered the gold standard for diagnosing coronary artery disease, caused when vessels supplying blood to the heart get narrowed, clogged or completely blocked by plaque. It involves inserting a cathe-
ter into the patient’s groin or arm as a route to the heart via the arteries.
Then a special dye is released into the bloodstream for contrast, and an x-ray is taken to show doctors how blood is flowing and identify any blockages which can be opened with a stent as part of the procedure, or in a separate surgery called coronary artery bypass grafting.
The problem is, all patients suspected of having coronary artery disease are sent for an invasive coronary angiogram, even though many were found to not have any significant blockage, or to have a minor condition that could be treated with medication instead of stenting or bypass surgery. In other words, many patients were undergoing this unnecessary invasive procedure.
There’s also some risk with this procedure, though it’s rare. Provincially, about one in 1,000 patients will have a bad outcome that could include a stroke, heart attack or death. HGH and St Catharines perform over 10,000 of these invasive procedures each year.
A study of Hamilton and Niagara patients found that 44 out of 100 patients who underwent an invasive coronary angiogram could have avoided the procedure, says Dr. Jeremy Petch, who leads the team of digital data and tech experts at CREATE, as the centre’s director. The remainder of patients had an obstruction and needed a stent to open clogged arteries.
Meanwhile, the process for deciding who qualifies for an invasive coronary angiogram was found to be biased against women. “About 40 per cent of patients who get this procedure are women, yet women are 40 per cent less likely to be diagnosed with an obstruction than men,” says Petch. “This means that they’re being exposed to the risks of an invasive coronary angiogram with less chance of benefit than men, so we have a gender inequity on our hands.”
Back in 2018, Schwalm led a research trial called CarDIA that looked at using a non-invasive imaging test called coronary CT angiography instead of an invasive coronary angiogram to check for blockages. When provided to the right patients, the CT scan is a lower risk, highly accurate test that costs the health-care system less.
As part of the CarDIA study, Schwalm led the introduction of a centralized triaging system, where he and interventional cardiologist Dr. Tej Sheth reviewed cases, recommending an invasive coronary angiogram where a blockage was suspected so that stenting could be done, or the CT test for patients who were less likely to have a blockage.
While successful at getting more patients to the right test, the triaging process was labour intensive. So Schwalm approached CREATE to see if AI could be introduced for faster and more accurate triaging.
Led by Petch and data scientist Shuang Di, CREATE looked at anonymous data from 27,000 Hamilton and Niagara cardiac patients going back 12 years, and used the AI tool to predict whether these patients should have been sent for an invasive coronary angiogram or CT scanning.
Instead of 44 per cent of patients recommended for an invasive coronary angiogram when this procedure could have been avoided, the number dropped to just 14 per cent through this AI modelling. “No test is perfect, but the reduction was dramatic,” says Petch.
The CREATE team was also able to train the AI algorithm so it learned to avoid the historical gender bias. “It performs equally well for men and women,” says Petch.
And by using AI, it’s estimated that the HGH cardiac team can avoid one bad outcome, such as a stroke, heart attack or death per year. There’s also
a cost savings, since an invasive coronary angiogram costs approximately $1,600, compared to a cardiac CT scan which costs $600.
“Even when we account for patients needing both tests, because they were sent for CT scanning and then identified as also needing the invasive
coronary angiogram and stenting, this translates, conservatively, to $600,000 in savings in Hamilton every year,” says Petch.
“When you think about cost savings provincially, there’s potential to save the Ontario health care system $6 million to $10 million a year.” n H



By Danae Theakston
Southlake Regional Health Centre is setting new benchmarks that will bring leading edge cardiac care to the forefront of Ontario’s healthcare landscape. With a steadfast commitment to excellence, Southlake is not only elevating the standards of cardiac care, but also spearheading innovative medical procedures and expanding its reach with new clinics.
Southlake, which is home to the Regional Cardiac Care Program, is no stranger to innovation. Over the years, some of the best clinicians, nurses and medical staff have made significant advancements in cardiac care at the hospital. Building on those lessons, Southlake is taking what it has learned to strengthen care across the region.
In recent months, Southlake has enhanced its cardiac care capabilities by expanding the scope of the program to ensure it continues to meet the needs of Southlake’s patients and partners. One of the first steps was appointing Christopher Overgaard, MD, as Southlake’s first Chief, Department of Cardiac Health.
“We want to better own our role to improve the system as a true regional partner committed to working in a collaborative manner to deliver leading edge care,” said Dr. Overgaard, Chief, Department of Cardiac Health, South-

lake. “In this new role, I will work together with members of the program and our partners in the community to elevate the Regional Cardiac Care Program to ensure that patients in some of Ontario’s fastest growing communities have access to innovative, life-saving care when they need it most.”
With a renewed focus on elevating cardiac care, the dedicated team at Southlake has thrived, pioneering new procedures that will improve patient experiences and care. In a recent, ground-breaking achievement, Southlake successfully performed a first-in-Ontario medical procedure
that represented a significant leap forward in the treatment of atrial fibrillation (AF).
AF, a common and serious heart rhythm disorder, has seen significant advancements in treatment options, thanks to emerging ablation technologies. Pulsed Field Ablation (PFA), is at the forefront of these developments, offering new hope for patients.
PFA involves delivering electric fields to ablate or disrupt cardiac tissues through irreversible electroporation. This process induces electric fields that alter cellular membrane potentials, redistributing charged species and disrupting cell membrane integrity. As a result, the targeted cells undergo apoptosis and die, leading to a controlled and precise ablation process.
Southlake has pioneered the clinical use of Farapulse PFA, becoming the first centre to use this technology in Ontario. With this new technology, Southlake has seen a reduction in procedure times from one hour to just under 30 minutes over the first seven procedures. Additional elements of the procedure have also found enhanced safety and efficiencies.
“Pulsed Field Ablation represents a significant advancement in the treatment of atrial fibrillation, offering precision, safety, and efficiency,” said Yaariv Khaykin, MD, Electrophysiologist, Southlake. “As more clinical data emerges and technology evolves, PFA could become the preferred method for AF ablation, providing better outcomes for patients worldwide.”
This pioneering procedure demonstrates Southlake’s leadership in adopting innovative medical solutions and enhancing patient care.
Southlake’s advancements in cardiac care also go beyond new procedures. The organization is delivering leading edge care, close to home with the opening of a new Cardio-Oncology Clinic. The clinic, a joint effort by Southlake’s Regional Cardiac and Cancer Programs, represents an important improvement in access to integrated cardio-oncology care, which was previously unavailable in this region.
The clinic will help patients with suspected or confirmed cardiac complications because of cancer treatment, those needing evaluation before cancer therapy or stem cell transplants, longterm heart monitoring for childhood cancer survivors, and other cases referred by oncologists. Led by Andrew Elagizi, MD, a cardiologist who subspecializes in the management of cardiac complications from cancer treatment, this clinic ensures patients receive the care they need, close to home.
Southlake’s unwavering dedication to elevating cardiac care, pioneering medical procedures, and expanding its reach with new clinics underscores its role as a leader in Ontario’s healthcare sector. These advancements not only enhance patient care but also set new standards for medical excellence in the region. n H
Humber River Health recognizes that modern challenges are best met with modern solutions, and understands the importance of collaboration with like-minded organizations to advance health access, enhance efficiency, and improve patient outcomes.
To this end, Humber River Health partnered with TeleVU and OBIO®, two organizations focused on healthcare innovation, and successfully completed the Innovative Model of Care Project.
Leveraging TeleVU’s augmented reality and artificial intelligence tool, TelePresence, and the BioVU Remote Patient Monitoring (RPM) platform, this groundbreaking initiative has created a transformative real-time, remote cardiac care model designed to elevate patient care, improve clinic efficiency, and reduce patient wait times and backlogs.
The TelePresence platform employs smart glasses and connected devices to facilitate real-time, interactive communication between Humber’s cardiac technicians and cardiologists. By enabling remote assistance during patient

procedures, the platform saves time, heightens hospital workflow, and improves care delivery by allowing staff to manage cardiac patients in real-time.
Whether additional consultations during procedures or interpreting devices like pacemakers and ICDs, TeleVU optimizes time and capacity by allowing healthcare professionals to manage more patients safely in both the cardiac device clinic and the procedure room, even after hours.
“The collaboration with TeleVU and OBIO®, and leveraging these innovative augmented reality and artificial intelligence technologies has enabled us to further enhance our cardiac care model,” said Dr. Douglas







Ng, Humber River Health. “This partnership aligns seamlessly with Humber River Health’s commitment to driving innovation for improved patient experiences and outcomes.”
With the BioVU RPM platform, Humber River Health’s commitment to patient-centered care extends beyond the hospital. Working in conjunction with the TelePresence platform, BioVU enables healthcare professionals to monitor vital signs remotely, allowing for a comprehensive assessment of cardiac devices implanted in patients without the need for relocation.
By enabling the cardiology team to conduct comprehensive remote assessments, BioVU plays an integral role in improving the health of the community. A patient’s care team can assess their condition and identify potential complications early on, minimizing the need for unnecessary in-person ap-
Enrollment has commenced for a groundbreaking national study that will help revolutionize cardiovascular care. Anyone who has or may have a cardiovascular condition is welcome to participate.
“VIRTUES equips healthcare providers with the up-to-date medical information about each patient, offering specific recommendations and various options to ensure the best possible care,” explains Dr. Anthony Tang, Scientific Director, and CEO of CANet. “The platform also educates patients on the rationale behind these recommendations, fostering a deeper understanding of their treatment.”
VIRTUES is holistic digital health solution designed around Care Sets, each focusing on a specific condition.
pointments, reducing emergency room visits and inpatient admissions, and ensuring patients have peace of mind when they leave the hospital.
“Integrating TeleVU’s telepresence technology into our workflow has propelled us to new heights in delivering efficient, high-quality care,” said Dr. Irving Tiong, Humber River Health. “Innovations like BioVU place the patient at the center of their care, empowering them with the tools to manage their health effectively.”
The success of this project underscores Humber River Health’s dedication to challenging the status quo and leveraging technology to transform healthcare delivery. With the foundation laid for broader adoption, the future looks promising for patient care, hospital workflow streamlining, and optimal healthcare resource allocation.
With values of compassion, professionalism, and respect at the forefront, Humber River Health continues to light new ways in healthcare, continually seeking new methods to provide the community with the best care. n H
For patients with co-morbidities— multiple concurrent conditions— several Care Sets can be enabled simultaneously, working together to provide comprehensive treatment. New Care Sets can be added at any time, ensuring the platform’s continuous growth and adaptability.
The goal is to improve and optimize patient-specific guideline-based therapy, outcomes, and health-care providers’ efficiency.
“Our healthcare system in Canada faces sustainability challenges, and many patients struggle to receive adequate care due to geographic barriers, especially in rural regions,” says Dr. Ratika Parkash, Associate Scientific Director at CANet. “VIRTUES has the potential to reach every Canadian, regardless of location, ethnicity, or other barriers.”
VIRTUES is a transformative initiative aimed at providing the highest quality cardiovascular care for everyone.
By Zhiting (Tina) Zhou, Xinyue (Iris) Zhao, and Certina
Chemotherapy (also known as chemo) is a treatment method that uses drugs to treat cancers, either by killing the cancer cells or by stopping them from dividing. Chemo medications may be administered as monotherapy (i.e., a single agent), but very often multiple agents are combined to ensure therapeutic efficacy. Chemo may be given by different routes of administration, such as, by mouth, via injection, or under the skin, etc., depending on the types and stages of cancer. Although adverse effects may vary based on the selection of drugs, common side effects of chemo include the following.
Nausea and vomiting occur in 30-90 per cent of patients receiving chemo, and 40-60 per cent of patients continue to experience symptoms of nausea and vomiting despite using preventative medication.
• Risk factors of CINV include high-emetogenic chemo (i.e., medications with a high risk of causing nausea and vomiting in most patients), female gender, patients with a history of motion sickness, pregnancy-related nausea and vomiting, and poor CINV control of the previous chemo cycle.
• Types of CINV: Each type would require different prevention and treatment regimens.
– Acute CINV occurs within the first 24 hours of chemo.
– Delayed CINV occurs more than 24 hours after chemo for up to one week.
– Anticipatory CINV occurs prior to chemo as a psychological response.
– Breakthrough CINV occurs despite preventative treatment.
• Prevention of CINV is an important component in patient care, as CINV
has a significant physical and emotional impact on cancer patients, such as, decreasing the patient’s quality of life and their willingness to continue chemo. Prevention would generally involve the following drug categories and they can be used alone or in combination, depending on the emetogenicity (the potential of causing nausea and vomiting) of the specific chemo that is being administered.
– Serotonin 5-hydroxytryptamine-3 (5-HT3) receptor antagonists (e.g., ondansetron, palonosetron)
– Neurokinin-1 (NK-1) receptor antagonists (e.g., aprepitant, fosaprepitant)
– Glucocorticoids (e.g., dexamethasone)
In terms of non-pharmacological options to manage CINV, it is recommended for patients to eat smaller meals, stay well hydrated, avoid foods with heavy smells and other triggers.
Febrile neutropenia (FN) is a serious condition often associated with chemo. It occurs when a patient develops a fever while their blood neutrophil (i.e., a type of white blood cells) count is critically low, which can potentially lead to life-threatening infections. Cancer patients undergoing chemo who develop a fever should be promptly assessed. It is important for patients to perform regular temperature checks and seek immediate medical attention if their temperature reaches or exceeds 38°C for one hour or 38.3°C under any circumstances.
• Risk factors of FN include patients who are undergoing dose-dense chemotherapy (i.e., chemo drugs are given with less time between treatments than in a standard chemo treatment plan), receiving bone marrow radiation, or having previously experienced FN.
• Prevention of FN with granulocyte-colony stimulating factor (G-CSF) should be considered when chemo is initiated. There are two types of G-CSF, short-acting and long-acting (e.g., filgrastim and pegfilgrastim), both of which are equally effective and administered via subcutaneous injection. The choice of G-CSF agent will depend on the type and frequency of the chemo cycle. Common side effects include bone and musculoskeletal pain, nausea, fatigue, and fever. Since G-CSF is self-administered at home, it is important for healthcare providers to provide patients with detailed counseling on storage, injection techniques, and proper disposal of sharps. At the same time, patients should always consider the 5 Questions to Ask About Your Medications (https://www.ismp-canada.org/ medrec/5questions.htm) during a clinical encounter with their healthcare providers, which will help them better informed of their medications.
Mucositis is another common side effect that refers to the inflammation of the oral mucosa (i.e., the soft tissue membrane that lines the structures in the mouth) caused by chemotherapy. It typically presents as erythema (i.e., red-
ness) or ulcerations of the oral mucosa, resulting in oral pain that makes it difficult for cancer patients to open their mouths, eat, and drink, which may significantly impact their quality of life. • Prevention of mucositis: Oral Care Prior to the initiation of chemotherapy, inform patients the importance of oral care to prevent mouth complications. Patients should brush their teeth using a soft-bristled toothbrush to prevent irritation and gum bleeding. They should also avoid using alcohol-containing mouthwash. Instead, they can rinse their mouth with a salt and/or baking soda solution several times after brushing, eating, before bedtime, and as needed.
• Management of mucositis: Pain Relief
Benzydamine, lidocaine 2 per cent viscous, and “Pink Lady” or Magic mouthwash are first-line options to be applied as needed. If severe pain persists despite topical treatments, acetaminophen or occasionally opioids can be used. However, it is important to note that acetaminophen may mask febrile neutropenia (FN), therefore, patients should check their body temperature before taking the medication. The above highlights some of the key considerations on safe medication use when managing three common side effects of chemotherapy. Readers are encouraged to consult further resources if they are interested to learn more about chemotherapy as well as prevention and management of chemo induced side effects. Selected resources are as follows:
• Canadian Cancer Society: Treatments – Side Effects – https://cancer.ca/en/ treatments/side-effects
• Cancer Care Ontario: Symptoms & Side Effects of Chemotherapy - https:// www.cancercareontario.ca/en/cancer-treatments/chemotherapy/symptoms-side-effects
• BC Cancer: Clinical Resources –http://www.bcancer.bc.ca/health-professionals/clinical-resources n H
By Lise Diebel
An imaging device developed by an Ontario start-up company is being studied at Hamilton Health Sciences (HHS) to see if it can better identify early signs of pressure injuries, with a focus on people with darker skin pigmentation. This patient population is more difficult to assess with the current, standard tools involving a visual inspection. As a result, pressure injuries may not be identified as early as they could be.
dren’s Hospital that showed considerably more pressure injuries in patients with darker skin pigmentation, says Ari Collerman, chief of interprofessional practice at HHS, and the study’s lead.
A pressure injury, also called a pressure ulcer or bedsore, is damage to skin and tissue under a bony part of the body that has been pressed against a surface, such as a mattress or wheelchair. They happen when patients aren’t able to shift their weight, and the skin starts to break down. Due to pressure, less blood gets into these areas and over time a wound can occur. It can start as a red area and progress to a very serious wound exposing cartilage or bone. If left untreated, pressure injuries can lead to sepsis, a life-threatening condition caused by an out-of-control response to an infection.

“Preventing hospital-acquired pressure injuries and sepsis are strategic priorities for HHS, as is equity, diversity and inclusion,” says Dr. Ted Scott, vice president of innovation and partnerships for HHS. “We welcome the opportunity to test technology new to Canada that helps improve health equity for our patients.”
Current practice in hospitals across North America is for health-care providers to visually check for risk of pressure injuries using something called the Braden Scale, which rates a patient’s risk of skin breakdown by how it appears as well as discomfort or pain, exposure to moisture, the patient’s ability to reposition their body, friction against the skin, and nutrition.
The MIMOSA Pro can identify signs below the skin’s surface that ar-
en’t yet visible to the naked eye, capture the images and upload them into the hospital’s secure health records system so they can be tracked over time.
McMaster Children’s Hospital was connected with MIMOSA through its partnership with the Coordinated Accessible National (CAN) Health Network – a national organization working to scale Canadian innovation across Canada.
The CAN Health Network is supporting a project between MCH and MIMOSA that will look at whether the MIMOSA Pro is more effective than the Braden Scale in detecting early signs of pressure injuries, including in darker skin pigmentation. The project is set to launch in June.
Continued on page 16

By Marlene Leung
New research led by Unity Health Toronto that examines how fibroblast cells in the body are activated to cause fibrosis and organ scarring has been published in the prestigious scientific journal Nature Reviews Molecular Cell Biology. Fibrosis and organ scarring are leading causes of death, with data suggesting they are responsible for up to 45 per cent of deaths in the developed world.
Fibrosis is a process by which fibroblast cells in our body produce an excess amount of a protein mixture called extracellular matrix (ECM). ECM contains proteins including collagen, elastin and fibronectin and can be thought of as a sort of “glue” at the organism level that connects the different organs of our body while respecting their boundaries.
Typically, fibroblasts produce ECM to help support tissue structures and to help repair tissue that has been injured or wounded. For example, under
normal circumstances, when you cut yourself, fibroblasts will travel to the site of the cut or wound, proliferate and produce ECM to help heal the cut. With fibrosis, however, fibroblasts receive certain signals which activate them to overproduce ECM. This excess ECM, in particular the excess collagen, can result in the formation of scar tissue which can impair organ function. Fibrosis can occur in any tissue or organ in the body, including the lungs, liver, kidney and heart, and is associated with many common diseases – often as an end-stage condition.
The new research review summarizes some of the signals and molecular mechanisms that play a role in activating fibroblasts to produce excess ECM. The researchers also discuss the heterogeneous nature of fibroblasts, and how their vast heterogeneity can impact the healing process.
“This review tries to untangle some of our knowledge and understanding – or misunderstanding of fibroblasts and fibroblast activation,” said Dr. Bo-
ris Hinz, corresponding author of the study and scientist at the Keenan Research Centre for Biomedical Science at St. Michael’s Hospital.
“We generally talk about activation of fibroblasts from a dormant state in normal healing and fibrosis. But the cells activated to make new ECM were neither really dormant, nor are they all fibroblasts,” said Hinz. “We wanted to understand which cells in particular are activated. What types of activations take place – for example, ‘What are the key signals that activate these fibroblasts and how?’”
PhD student Fereshteh Sadat Younesi helped lead the review. Younesi is a member of Hinz’s lab and is a student at the Research Training Centre at St. Michael’s Hospital.
“One key signal arises from the mechanical cues present in the stiffened environment of fibrotic regions. When tissues undergo fibrosis, they become way
stiffer than normal because of these fibroblasts going into overproduction and rearranging the ECM,” Younesi said.
“Those fibroblasts can feel the stiffness around them, which keeps them switched on, even after the initial injury has healed. These mechanically induced fibroblasts exacerbate the fibrotic area with their persistent activity.”
Hinz said once researchers have a better understanding of the signals and mechanisms involved in fibroblast activation, they can develop therapies and interventions to interrupt the process and stop the overproduction of ECM, thus halting fibrosis.
“We need a cure for fibrosis. Scientists have known about fibrosis for roughly a century and there still is no cure,” Hinz said. “With only two currently approved drugs, we can only stop fibrosis in some organs – at best. An end goal would be to instruct the scar-making cells to remove excess ECM with pharmaceutical guidance. This is where the science is going and this is the ultimate dream.” n H
Continued from page 15
During early discussions with MIMOSA leadership, the technology wasn’t yet available in Canada. “It hadn’t been Health Canada approved, although it was a Canadian innovation,” says Collerman, adding that HHS worked with the vendor to support the application to, and approval by, Health Canada.
“It takes a large team from various areas of the hospital working together to make this type of study possible.”
HHS teams supporting the study include MCH; quality and performance; skin, wound and ostomy; interprofessional practice; and innovation.
“If we have positive results, we’ll purchase additional devices and make them
part of our routine care for patients who may be at risk,” says Collerman.
The study team is finalizing which hospitals across HHS sites will take part in the study. Ten units from several sites have volunteered, so there’s keen interest in testing this technology, says Collerman.
Patients will be tested with both the Braden Scale and MIMOSA Pro to see if there’s a difference in early detection. The study team plans to use Epic, the hospital’s state-of-the-art hospital information system, to store and track data, comparing the two tools.
“All patient populations will be included in the study, but we’re especially interested in our patients with darker skin pigmentation,” says Collerman. n H

Through several focused strategies and a dedicated team effort, London Health Sciences Centre (LHSC) has improved cancer surgery wait times at the Verspeeten Family Cancer Centre by 50 per cent over the past year for non-urgent and non-emergent patients.
“We know how hard it is for patients with cancer and their families to wait for surgery and we needed to do everything we could to improve our times,” says Dr. Michael Ott, Department Head, Oncology, LHSC. “This involved finding new ways to maximize our current resources and improve efficiencies – like improving our referral systems, optimizing our data used in making decisions, and dedicating more operating room time for cancer surgeries.”
The impact of these efforts is clear. As of March 2024, 90 per cent of all oncology patients receive their surgery

within the targeted wait time, according to the urgency of their diagnosis.
Dr. Ott notes that, “We won’t settle until every patient gets care within the
: Dr. Michael Ott, Department Head of Oncology at LHSC
appropriate target wait time, and we continue to improve.”
While patients identified as high priority have largely been seen within

the recommended surgical wait time, this reduction in wait times is even more impactful because these improvements positively impact patients who are more likely to encounter extended waits across the health-care system.
“These improvements reflect our commitment to providing timely and efficient care to a growing number of patients across southwestern Ontario,” says Dr. Kevin Chan, Corporate Medical Executive, LHSC.
LHSC is home to the regional cancer centre responsible for providing inpatient and outpatient cancer care, including surgery, radiation therapy and chemotherapy, as well as a full range of support services and the advancement of groundbreaking research. We remain committed to investing resources to further enhance the patient experience – from diagnosis to treatment. n H

eam-building and face-toface meetings were limited during the COVID-19 pandemic. However, the long-term care team was committed to implementing evidence-based practices and sharing their learnings across long-term care homes.
“We were working with challenging circumstances when we were developing this study in the fall of 2020,” says Janice Sorensen, research lead, LongTerm Care and Assisted Living. “We thought, let’s do it virtually.”
T Anew report from UHN recommends residential highrise buildings with a high proportion of older adults have a dedicated home care team who can care for multiple clients within the same complex.
The policy paper from UHN’s NORC Innovation Centre says instead of care providers – such as personal support workers (PSWs) – travelling from client to client performing piecemeal work, they be able to work fulltime or part-time shifts with minimal travel and provide care of varying duration and frequency based on client needs.
Streamlining services for older adults in one place will “provide home care that’s client-centered, efficient and better for workers,” says the recently released A Home Care Model for Naturally Occurring Retirement Communities in Ontario from UHN’s NORC Innovation Centre.
NORC stands for naturally occurring retirement community. In Toronto, 489 buildings housing approximately 70,000 older adults have been identified as NORCs, each having at least 50 older adults and 30 per cent or more residents over the age of 65.
A STUDY LED BY DR. AKBER MITHANI, REGIONAL MEDICAL DIRECTOR, JANICE
Multidisciplinary quality improvement teams were created with dedicated people, including nurs -
es, physicians, residents and family partners. The teams collaborated via online communication and col -
laboration platforms, Zoom and Slack.
Quality Improvement Coaches, Dr. Adriaan Windt and Angela Tecson, guided the teams through weekly virtual huddles. Using adapted quality improvement tools, the coaches helped the teams transform their 46 change ideas into 16 quality improvement projects for prevention, preparation and response to COVID-19 outbreaks in long-term care homes. The projects also addressed staff recognition and family visitation concerns.
In the streamlined model set out in the report, staff would be able to see more clients per day without compromising service delivery, yielding significant productivity gains.
If implemented across all NORCs in Ontario, the analysis finds that this model could provide more than 750,000 hours of additional PSW services worth nearly $26.8 million annually at no additional costs.
“Home care ends up being your community,” says Eugene, a report participant who receives home care.
Eugene hopes for a more streamlined approach to care that fosters a stronger connection between PSWs and residents of NORCs, bringing a deeper sense of “home” back into home care.
The NORC program at UHN leverages the naturally occurring densities of older adults in these buildings to provide place-based services and often integrates health, social and physical supports directly within the community to make it easier for people to age in place.
In 2022-23, PSWs delivered nearly 3.5 million hours of home care services in Ontario’s NORCs, valued at more than $120 million. UHNs NIC
analysis found that approximately 85 per cent of NORCs are receiving PSW services from two or more home care agencies.
“It’s no surprise that our community care providers are experiencing burnout,” says Melissa Chang, Director of Operations and Sustainability at UHN’s NORC Innovation Centre. “They can’t continue to be spreading themselves this thin and we are seeing people leave the industry because of the stress.”
A NORC-based home care model would involve assigning a lead home care agency for each NORC building with a high enough clientele. In cases of buildings with fewer home care clients, several NORC buildings in close proximity could be grouped together under the responsibility of a single, lead agency.
A single responsible agency can solve some of the issues raised by older adults who use publicly-funded home care, the report says. Care coordination under this model could be done much more efficiently, directly through the lead agency.
With clear accountability and a funding model that allows for flexibility, assessing any new home care needs,
scheduling home care staff and coordinating each client’s care could all be done closer to home, at the level of the NORC, it says.
This means care decisions would be made by someone who knows each client and their needs, and communication between home care agencies and users are streamlined, which can help develop trust and more consistent service.
A lead agency also allows for home care to be more easily integrated with the rest of the local health care system such as through Ontario Health teams.
The report from UHN follows adoption of a NORC motion at Toronto City Council last fall.
The motion urged both the federal and provincial governments to explore working with UHN’s NORC Innovation Centre to build greater system capacity for innovation, research, and knowledge of targeting the large number of apartment, condo, and coop buildings that over time, have become home to a high-density of older adults. n H


“Kudos to our coaches who developed some long-term care adaptive quality improvement tools to be at a very attainable level,” says Janice. “Everyone involved, whether resident or staff member, was on the same page to walk that quality improvement journey together.”
The virtual quality improvement collaborative approach worked well, with all but one of the projects completed within the study period.
The study found that quality improvement infrastructure and virtual supports can help conduct timely projects to improve pandemic response in long-term care homes during emergencies when in-person communication is not possible.
Crucial takeaways from the study are that flexibility and customizing approaches for each long-term care

home are essential with consideration for staff time availability and capacity.
Also, multidisciplinary teams, including family members or residents, provide valuable and diverse perspectives to inform projects.
“As we reflect on the challenges during the pandemic and the outcomes of our study, it’s evident that
investing in quality improvement initiatives is paramount,” says Janice.
The study was part of the ‘Implementation Science Teams – Strengthening Pandemic Preparedness in Long-Term Care’ programme led by Healthcare Excellence Canada, co-funded by Michael Smith Health Research BC and the BC Ministry
of Health and supported by Health Quality BC.
Although the study was limited to six long-term care homes, the adaptive quality improvement tools and lessons learned have informed ongoing quality improvement initiatives in long-term care homes across the Fraser Health region. n H


















By Wendy Glauser
Ross Durant was volunteering at his church just over a decade ago when he noticed he was dripping sweat. “I felt like an elephant was sitting on my chest,” recalls the former insurance underwriter. As it turned out, Durant, now 91, had suffered a heart attack.
Fellow volunteers gave him an Aspirin and called 911. At the hospital, doctors treated his heart with medications, and weeks later, he underwent surgery to reduce the risk of another attack. He then went through a sixmonth rehab program at the Toronto Rehabilitation Institute, where he learned more about diet and exercise, as well as how to measure his heart rate by holding his two fingers to the side of his neck.
Now, over 10 years later, Durant has found an easier way to track metrics and activities relevant to his heart health: through an Apple Watch. He’s one of 1,000 people with cardiovascular disease being followed over a fiveyear period for KITE’s Health Metrics and Clinical Events study, also known as “HERACLES.”
The study aims to understand how data picked up by Apple Watch – including heart rate, exercise levels and more – relate to long-term heart health outcomes. In addition to having access to Apple Watch data once participants have shared their consent, the researchers conduct in-clinic checkups before, during and after the study. Participants undergo electrocardiograms and stress tests to measure the heart’s electrical activity at rest and during exercise, as well as fitness, blood pressure and weight checks.
HERACLES builds upon an initial study of 300 people in cardiac rehab conducted by the team that explored the relationship between watch metrics and other objectively measured fitness levels. These are the first studies examining Apple Watch’s potential role in cardiac rehab.
While wearables have helped people improve and monitor their health for years now – whether through tracking steps, sleep patterns or heart rate numbers – there haven’t been many formal studies on how devices can help in medical settings.
“The potential for this tech, however, is enormous. In the future, wearables like Apple Watch could help doctors know when to intervene,” says Dr. Paul Oh, a Senior Scientist at KITE and Medical Director of the Cardiovascular Prevention and Rehabilitation Program at the University Health Network.
“For example, if someone’s heart function is getting worse, maybe we’ll see that their activity pattern has been going down for days or weeks, or that their resting heart rate has been going up, indicating underlying physical stressors,” he adds.
As Dr. Oh explains, routine medical checkup visits represent “a tiny fraction” of people’s lives, while in cardiac therapy, “we are asking people to be active throughout the day, and we want a picture of overall day-to-day health.” A wearable helps providers support patients between appointments and provides the everyday encouragement and reminders that rehab therapists could only dream of being able to offer.
The results are promising so far, with 90 percent of participants evaluated after one year either increasing or maintaining their VO2 max – a measure of how much oxygen the participants take in and use during exercise. It’s an indicator of the overall function of their heart and lungs.
Lisa Cotie, a kinesiologist and researcher at KITE, says that many patients appreciate the reassurance of the watch, including that they can see whether they’re exercising within their “Goldilocks” target heart rate –meaning they’re pushing their hearts

enough to get stronger, but not too much that they overexert themselves.
“Especially after graduating from cardiac rehab, a lot of people are craving the extra monitoring and knowing that we at the cardiac rehab centre are connected with them in some way,” she says.
Jessica Nooyen, a research manager at KITE, sees the watch as a self-empowerment tool.
“People feel like they have more control over their health. In terms of health literacy, we’ve noticed an increase in understanding as to what parameters like heart rate and VO2 max mean, and what to look out for,” she explains. “You could talk about these things in cardiac rehab, but to actually see it displayed on your watch provides you with immediate feedback and a great opportunity for learning.”
Durant’s Apple Watch records his daily walks, strength-training exercises, and estimated cardio fitness levels during exercise. More than anything, the watch keeps him honest. He
Dr. Paul Oh is a Senior Scientist at KITE and Medical Director of the Cardiovascular Prevention and Rehabilitation Program at the University Health Network.
makes sure he closes his three Activity rings every day – which means he’s met his goals of burning a predetermined number of calories through activity, exercising for a predetermined number of minutes and standing up at regular intervals to counter the ill health effects of sitting. (Calories are calculated based on the person’s age, gender, weight, height, activity and heart rate.)
Some of his friends and family members also have an Apple Watch, and many of them have a “friendly competition” going on where they see who can complete their rings fastest each day. If his sister completes her rings before him, “I’ll get a little text, and it’ll have a little barb in it,” he says.
While Durant has had to get some tech support from his grandchildren on using the watch, in general, he finds the Apple Watch makes it easier for him to follow his heart health. “In rehab, one of the first things you learn is to check your pulse in exercise, using two fingers on your neck and counting,” he says. “The watch takes the grunt work out of it. It’s all there on your wrist.” n H
new study from UHN’s Toronto General Hospital Research Institute (TGHRI) has identified the impact of frailty on hospitalized patients with interstitial lung diseases (ILD).
Interstitial lung diseases are a group of lung disorders that cause progressive scarring and declining lung function.
Every year, between three per cent and 14 per cent of patients with ILD suffer acute exacerbations flare-ups (AEILD), which are associated with high morbidity and mortality. Identifying risk factors is crucial for predicting outcomes, allocating resources, assessing transplant eligibility and optimizing recovery.
“Frailty is a syndrome characterized by the reduced reserve of energy to maintain functions and cope with stressors that happens as we age,” says Dr. Dmitry Rozenberg, a scientist at TGHRI, assistant professor in the Temerty Faculty of Medicine at the University of Toronto (U of T) and senior author of the study.
“Frailty is often associated with greater risks in chronic lung diseas-
“FRAILTY IS A SYNDROME CHARACTERIZED BY THE REDUCED RESERVE OF ENERGY TO MAINTAIN FUNCTIONS AND COPE WITH STRESSORS THAT HAPPENS AS WE AGE”
es and has also been associated with diminished quality of life and transplant-free survival in patients with chronic respiratory diseases.”
Although it is known that frailty can be an indicator of outcome for patients with ILD and that approximately half of ILD patients experience frailty, the implications of frailty during acute exacerbations of ILD have remained largely unexplored.
“Our study aimed to understand the association between frailty and various aspects of AE-ILD, including clinical characteristics, physical function, hospital outcomes and post-AE-ILD recovery,” says Dr. Marine Van Hollebeke, former postdoctoral researcher at UHN and co-first author of the study.

AUGUST FOCUS: Paediatrics/Ambulatory Care/ Neurology/Hospital-based Social Work: Paediatric programs and developments in the treatment of paediatric disorders including autism. Specialized programs offered on an outpatient basis. Developments in the treatment of neurodegenerative disorders (Alzheimer’s, Parkins on’s etc.), traumatic brain injury and tumours. Social work programs helping patients and families address the impact of illness.
Annual Paediatric Supplement and Added Distribution to CHC Members (+8,200)

Advertising Booking Deadline July 26th
Material Deadline July 30th
For more info email advertising@hospitalnews.com
Dr. Van Hollebeke was co-supervised by Dr. Rozenberg and Dr. W Darlene Reid, Senior Scientist at UHN’s KITE Research Institute, a professor at U of T, and co-author on the study.
The team analyzed retrospective data spanning from January 2015 to October 2018.
They examined 89 patients hospitalized with AE-ILD, 31 of them being identified as having frailty based on a previously developed index. This indicates that frailty is prevalent, being present in one-third of patients admitted with AE-ILD.
“We found that patients with frailty tended to be older, had a higher burden of comorbidities – for example, diabetes or cardiovascular disease, exhibited reduced physical function prior
to hospitalization, and decreased independence,” says Dr. Karan Chohan, former medical student at U of T and co-first author of the study.
“Patients with frailty also had more major medical complications – 32 per cent of patients with frailty versus 10 per cent without – and required more multidisciplinary support during hospitalization.”
However, the study also showed that frailty was not associated with one-year mortality when factoring in lung transplantation, which is a life-saving procedure.
This study underscores the importance of identifying frailty in ILD patients, as it may help health care providers better understand prognosis, allocate resources more effectively, and tailor care plans to address the specific needs of individuals.
Future research will evaluate if frailty can be modified prior to or during hospitalization with AE-ILD and whether offering rehabilitation strategies during or after hospitalization can improve hospital and post-discharge outcomes. n H



SEPTEMBER FOCUS: Technology and Innovation in Healthcare/Artificial Intelligence (AI)/ Patient Experience/Health Promotion
Online Education:
New treatment approaches to mental health and addiction. An overview of current research initiatives Programs and initiatives focused on enhancing the patient experience and family centered care. Programs designed to promote wellness and prevent disease including public health initiatives, screening and hospital initiatives.
Annual Medtech Technology Supplement & Distribution To Conference Attendees. Plus: Annual Online Education Focus
Advertising Booking Deadline August 23rd
Material Deadline August 27th For more info email advertising@hospitalnews.com

OCTOBER FOCUS: Mental Health and Addiction/Patient Safety/Research/Infection control:
New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
Annual National Infection Control Week (Oct.14-18) Supplement

Advertising Booking Deadline September 27th
Material Deadline October 1st For more info email advertising@hospitalnews.com
Lung problems plagued David Shoots since his youth. It would take buying a dream cottage as an adult for him to finally piece together the puzzle behind his poor health: a rare, but life-threatening, fungal infection known as chronic pulmonary aspergillosis (CPA).
As a teen, David grew up in a home that frequently flooded, causing mould to flourish. Later, his lungs collapsed at different times. He received surgery, which helped his condition, but no clear answers about the cause.
After marrying and having kids of his own, David bought a cottage in Bruce County as a second home for his Brantford-based family. The cottage had a musty odour but, at the time, no one thought twice about it. That is until David got really sick.
“One summer, I started having symptoms like a pneumonia. The fever, chest pain, night sweats and coughing wouldn’t go away – even after being hammered with antibiotics and steroids,” David recalls.
Doctors, too, were stumped by David’s symptoms and the CT scans showing shadowing on his lungs. Unable to provide him with a clear cause for his illness, David started to seek out his own answers.
“I don’t even know why but I started looking into mould exposure,” he says. “And the more I looked into it, the more I thought, ‘that could actually be the problem.’ That’s when I contacted Dr. David Denning at the University of Manchester.”
In hearing David’s story, Dr. Denning – a world-renowned expert in fungal diseases – connected with his specialists in Canada over email, validating his concerns. To be certain, David visited St. Joe’s Firestone Institute for Respiratory Health for testing. There, under the care of respirologist Dr. Gerard Cox, David was finally able to get the answers he needed.
Dr. Cox diagnosed David with CPA, a condition caused by a common mould that lives indoors and outdoors. While most people breathe aspergillus spores every day without getting sick, for some, like David, it can lead to a lung infection requiring a powerful antifungal drug to treat.

Because aspergillosis is rare – an estimated 1.8 per cent of Canadians are affected by serious fungal infections – it often goes undiagnosed. Unfortunately, aspergillosis also doesn’t go away.
“The medication doesn’t cure the infection but keeps it at bay,” David says. “And while I’ve been doing better ever since, I still have problems, like bad bronchiectasis where my lungs can’t clear phlegm naturally. But I’m well enough to live a relatively closeto-normal life. And when I have a flareup, Dr. Cox is my doc and I know he’ll take care of me.”
Today, David credits Dr. Cox and his team for not only taking years of debilitating symptoms seriously, but also for saving his life. In many climates outside of Canada where mould runs rampant, chronic aspergillosis is a “hidden disease” that often gets misdiagnosed. Deaths are attributed to tuberculosis instead, David says.
That’s why David shares his story widely – to raise awareness about the realities of fungal infections. And that’s why, over the years since David was diagnosed, his Hyundai dealership in Brantford has donated nearly $30,000 to St. Joe’s to help advance research into lung health. His hope is
that, one day, respiratory researchers will find better treatments or a cure for aspergillosis, as well as other diseases of the lung.
“I have to be very cautious because of COVID-19,” David says. “I avoid breathing in any particles of any kind. I can’t go into a dusty barn, and I definitely can’t go outside if there are air quality issues, like smoke from the recent wildfire events.”
“But there’s a lot of people who have it a lot worse, like people living with lung cancer. So, that’s why I donate to St. Joe’s. Because the Hospital was there for me when I was looking for answers. And through more research, doctors like Dr. Cox will be

able to provide other patients with the answers they need, too. I’m so thankful that Dr. Cox took the time to figure out my case.” n H
For decades, St. Joe’s Firestone Institute for Respiratory Health, a partnership with McMaster University, has been a world leader in the treatment of lung diseases like asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis. The goal of the Institute is to conduct research that increases the understanding of respiratory health and disease though collaborative clinical studies that aim to enhance patient care at the Hospital. The Institute’s reputation as a leader in respiratory health is not only evident in the volume of high-quality, peerreviewed studies it produces, but also by putting into practice new and innovative treatments that enhance the care of the patients St. Joe’s serves.
By Catherine Danko
Acyclist is struck by a car and in critical condition.
In the Emergency Department (ED), a call goes out – “Code Shock” – bringing together a range of health care professionals to aid in decision-making to provide care to the critically ill patient, who is in a life-threatening condition due to severe blood loss.
This was the simulated scenario of the new emergency protocol – which goes live on Monday, June 17 at both Toronto Western (TWH) and Toronto General (TGH) hospitals.
It will standardize and streamline the care of patients who present to the EDs requiring rapid resuscitation and specific interventions related to trauma and undifferentiated shock.
Code Shock brings together an immediate in-person response team made up of professionals from emergency, anesthesia, critical care, respiratory care therapy awnd general surgery, as well as additional support as required from JDMI, Blood Bank and bed flow.
It is designed to support the clinical team in identifying patients requiring timely trauma and shock intervention and ensuring the necessary resources are available to provide optimal care through coordination and clear decision-making, improving the timeliness of emergency interventions, quality of care and patient safety.
“The EDs at UHN treat some of the sickest patients in the province, and sometimes this requires the rapid deployment and formation of a multidisciplinary team,” says Dr. Thomas Forbes, Surgeon-in-Chief, Sprott Department of Surgery at UHN.
“This is what Code Shock is about, experts working in teams for the benefit of our patients.”
The development of the protocol was a recommendation from a serious safety event which occurred in 2023. This led to the development of a Code Shock working group, who built the protocol.
In early June, the EDs at both TWH and TGH practiced a mock Code
Shock where members of the multidisciplinary immediate response team practiced providing care to a patient requiring hypotensive resuscitation – a resuscitation strategy that uses fluids and blood products during the early stages of treatment for hemorrhagic shock, a life-threatening condition caused by severe blood loss.
“Simulation is important because we want to make sure what’s on paper is impactful and safe for patients and providers in real life,” says Dr. Alia Dharamsi, Director of Simulation at UHN.
“A mock simulation allows us to identify latent safety threats or gaps within the protocol, as well as improve the team’s communication, which in turn supports understanding and role clarity.”
One advantage of the mock trials was that they were physically performed in the EDs – rather than a simulation room – allowing for staff who work outside the department an opportunity to orient themselves within the walls of the usual care space, using the standard equipment when Code Shock is called in the future.
“Most staff who will be attending a Code Shock won’t have ever met or worked with each other before and will be expected to perform in a high-stress, high-acuity patient resuscitation scenario,” says Dr. Alyssa Louis, a critical care physician at TWH.
“The simulation helps us to analyze team dynamics and identify how people might work together in the future, allowing us to identify opportunities for improvement.”
The protocol does not replace rapid transfer for trauma patients to a Level 1 Trauma Centre – such as St. Michael’s Hospital – which is strongly equipped to provide care for patients suffering from major traumatic injuries such as falls, motor vehicle collisions or gunshot wounds.
The Code Shock team will ensure there is support for the multisystem trauma patient while awaiting trans-

fer. For patients who do not meet the clinical criteria for transfer, such as a patient presenting with undifferentiat-
ed shock and the cause is unclear, the Code Shock team will be the first to respond. n H
Catherine Danko works in communications at University Health Network.









Do you have employees or retirees not covered by the hospital's benefits?
HCP is a voluntary group plan designed for your part-time, casual, contract and temporary employees and retirees. All you have to do is communicate the opportunity to your employees and we handle the rest, including enrollments, premium collection, and claims administration.
It's really that easy!
Plan offerings for your employees:
Three benefit packages available (Signature, Supreme & Standard)
Signature Package (Life, LTD and ADD&D ONLY) for those who already have health benefits through a spouse or other group plan
Competitive extended health plans & two optional dental plans
BONUS $1000 LTD offering for eligible employees under 35
Get in touch with us today to learn more about our plans and HR support programs 1-866-768-1477 x2208 or mdesousa@healthcareproviders.ca