According to recent numbers, Ontario has the lowest number of registered nurses per capita in the country. Ontario also ranks dead last in the amount spent on health care per person. Underfunding and short staffing - that’s Doug Ford’s approach to public health care.
Behind the numbers there are the real people who are being failed by our health-care system. The family waiting for hours in the hospital ER because of the staffing crisis. The nurse who reluctantly abandons the profession she loves, to escape unbearable burnout and moral distress. The housebound senior in crisis because there aren’t enough home-care resources to provide the services he needs. And on and on.
Doug Ford says his government is transforming health care - but it’s not for the better. Numbers don’t lie, and neither do the stories. It’s time for change.










Michael’s-led research calls for screening program for ‘ticking time bomb’ abdominal aortic aneurysm

By Ivy Oandasan and Ivy Bourgeault
very day we hear stories about the primary care crisis in Canada and the urgent need for a solution. Primary care is the first point of contact into the health system for routine healthcare needs.
More than six million Canadians are not able to access a regular primary care provider. This number continues to balloon.
Many family physicians are retiring, some reducing clinic hours, and others focusing their practices to address specific conditions. Coupled with a decreased interest in choosing family practice as a specialty, more communities are left vulnerable to the realities of limited access to primary care.
So, what’s the solution? Governments are celebrating the opening of new medical schools, new nurse practitioner-led clinics and announcing increased scope of practice for pharmacists to manage minor ailments. Unfortunately, these piecemeal initiatives – focused on access alone – will not solve the problems of primary care.
A patchwork quilt only works when the pieces are put together into a collaborative design.
We need a primary care system designed to be coordinated, comprehensive and accessible. And we need a primary care health workforce committed to collaboration to make this happen.
A new way of working is needed.
Every person in Canada should have access to a primary care team, who can manage health issues faced by
OCTOBER 2024 ISSUE
EDITORIAL: Sept. 6
ADVERTISING:
Display – Sept. 27 | Material – Oct. 1
Monthly Focus:
Mental Health and Addiction/Patient Safety/ Research/Infection control: New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
Infection Control Supplement – National Infecton Control Week
a patient collaboratively. Whoever is the first point of contact in the health system should ensure that a patient is treated or referred to another team member in a coordinated and seamless manner.
There is an inherent accountability built in being part of a team, whether co-located or not, to deliver holistic patient care. Without greater access enabled through coordinated team-based care, the health of Canadians will continue to suffer.
As a family physician and a health workforce researcher, we co-led the Team Primary Care: Training for Transformation initiative in partnership with over 20 primary care practitioner groups and 100 healthcare organizations across Canada to begin to stitch together a quilt of solutions. This taxpayer funded initiative had over 800 participants call on our governments to make sure future investments in primary care include coordinated training to enable Canadians access to a primary care team.
Another complementary taxpayer funded project, OurCare, collected the perspectives of thousands of people across the country calling for standards to define what every person in Canada should expect from primary care. These include being able to receive culturally safe care, from a primary care clinician, who works with others in a team, providing ongoing care, connected to community and social services, and accountable to the communities served.
Continued on page 6
2024 ISSUE
EDITORIAL: Oct. 4
ADVERTISING:
Display – Oct. 25 | Material – Oct. 31
Monthly Focus:
Emergency Services/Critical Care/Trauma/ Emergency: Innovations in emergency and trauma delivery systems. Emergency preparedness issues facing hospitals and how they are addressing them. Advances in critical care medicine.
Emergency Care Focus
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries
accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario. The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

By Kent Anjo
team of researchers at North York General Hospital (NYGH) is studying a video recording of a surgery. In the video, a surgical resident navigates an unusually narrow pelvic cavity as part of a reconstruction procedure. When the resident runs into difficulty, they speak up and the surgeon responds in a reassuring tone to calmly guide them with the support of the OR team.
The recording is an example of what psychological safety can look like in the OR, where a resident feels safe enough to speak up when they have trouble because they know they will receive helpful guidance instead of criticism. These types of environments can encourage open communication, learning and ultimately better patient outcomes.
“Relationship dynamics within surgical teams are just as important as technical skills when it comes to delivering quality patient care,” says Patricia Trbovich, PhD and Badeau Family Research Chair in Patient Safety and Quality Improvement at NYGH and an Associate Professor at the Institute of Health Policy, Management and Evaluation at the University of Toronto.
“However, until recently we haven’t studied the complexity of team dynamics within surgical teams and developed a way to objectively identify and assess relational concepts like psychological safety.”
Dr. Trbovich is leading this research with NYGH surgeon Dr. Usmaan Hameed using data from Operation Room Black Boxes (ORBBs). ORBBs provide unprecedented access to understanding what occurs during surgery through a network of cameras, microphones and sensors installed in an operating room.
ORBB data can range from a patient’s vital signs to video and audio recordings of a surgical team working and laparoscopic views inside a patient. This type of information is commonly used to minimize risks and improve patient outcomes by focusing on technical performance.

In contrast, researchers working alongside Dr. Trbovich and Dr. Hameed are analyzing ORBB data to pinpoint behaviours that often go unnoticed or are taken for granted but play a key role in helping surgical teams work smoothly, especially during unexpected situations.
The team recently published some of their findings in the medical journal Annals of Surgery and found surgical team members from different professions will respond differently during periods of uncertainty, with these differences supporting successful outcomes.
“Nurses ramped-up their backup behaviour by anticipating the team needs and offering their assistance,” explains Taylor Incze, a graduate researcher on the study. “In contrast, surgeons and medical trainees amplified their psychological safety-related skills like voicing a concern and blameless problem-solving.”
“Negative reactions to uncertainty in the OR among surgical team members can stifle communication, increase
stress and lead to potentially adverse outcomes,” adds Dr. Hameed, who is also one of the study’s co-authors.
“What our research is showing is the ability to safely recover during an unexpected situation is heavily dependent on effective teamwork. By exploring these dynamics, we can move clos-
er to ensuring that all surgical teams can perform at their best, even under the most challenging conditions.”
The research team is also using ORBB data to explore other opportunities to improve surgical safety with funding from Natural Sciences and Engineering Research Councils of Canada and the Canadian Institutes of Health Research. This includes identifying and categorizing all the contributing factors to an adverse surgical event, including workflows in the OR, the layout of equipment and tools, and even policies.
The NYGH team hopes to use their findings to support improvements in quality, safety and efficiency and to inform training programs for surgery teams. They have also approached other hospitals including Sunnybrook Health Sciences and Unity Health in Toronto, the Mayo Clinic in Minnesota and Stanford Medicine in California to analyze and code their ORBB data with a unique focus on team interactions.
“We are really on the cusp of something big in terms of how we study surgical safety and teamwork and I am thrilled that we are doing it right here at North York General,” says Dr. Trbovich.
“By systematically analyzing surgical team interactions, we can understand communication and behavioural patterns that support successful outcomes and reveal what is currently invisible.” n H
Despite increased funding for cataract surgeries to private, for-profit clinics, access to surgery fell nine per cent for lower-income people, according to new research published in CMAJ (Canadian Medical Association Journal).
“Unexpectedly, despite new public funding for operations provided in private for-profit surgical centres, which was intended to fully cover all overhead costs and remove the need to charge patients, this disparity did not decrease, but instead grew during the funding change period,” says lead author Dr. Robert Campbell, a clinician–scientist in the Department of Ophthalmology at Queen’s University and a senior adjunct scientist at ICES.
The COVID-19 pandemic created backlogs for cataract surgery and, to increase access without the need for
Continued from page 4
patients to pay, the provincial government provided funding to private clinics in 2020.
The study, conducted by researchers at ICES, Queen’s University, and the University of Toronto, included 935 729 cataract surgeries performed in Ontario between January 2017 and March 2022. Researchers looked at differences in socioeconomic status of patients who underwent surgery at publicly funded hospitals and patients who accessed surgery at private, for-profit centres before the additional funding (up to February 2020) and after (March 2020–2022).
The majority of cataract surgeries (81%) were performed in public hospitals, with the remaining 19 per cent performed in private, for-profit surgical centres. Over the 6-year study period, more people in the highest socioeconomic bracket (23%) received surgery
Both Team Primary Care and OurCare initiatives launched appeals to the public asking them to urge their governments to support a vision for an integrated primary care system where “access alone” is not enough. We call for a primary care workforce who can provide a full complement of primary care services collaboratively in supported teams.
No one government, no one healthcare practitioner group, no one group of educators, regulators, accreditors or leaders can solve the primary care crisis alone. We need an all-hands-ondeck approach, and we need it now.
The recent $25 billion bilateral agreements signed between the federal and provincial/territorial governments as part of “Working together to improve health care for Canadians” is a unique and timely opportunity for this
kind of primary care system design. The agreements state that each province and territory must draft action plans to describe how they will use federal funds, identify and measure targets, and report annually on their progress.
It is critical that our governments build on the insights gleaned and partnerships developed from these two tax-payer funded projects which would enable a good return on investment into primary care redesign – especially given primary/family health care is identified by the federal government as a key area of shared priority.
We need partners to bring those of us with evidence-informed solutions to fix Canada’s healthcare system together. We’re interested in collectively solving the crisis in primary care with design solutions. Who else will join us? n H
Dr. Ivy Oandasan is a Professor with the Department of Family and Community Medicine at the University of Toronto and is Director of Education at the College of Family Physicians of Canada.
Dr. Ivy Bourgeault is a Professor in the School of Sociological and Anthropological Studies at the University of Ottawa and leads the Canadian Health Workforce Network.
in private clinics than patients in the lowest income bracket (14%). In-hospital surgeries were evenly distributed across socioeconomic brackets. Cataract surgeries in private, for-profit centres increased from 16 per cent in the pre-pandemic period to 23 per cent in the period after the funding increase. Surgical rates in private, for-profit centres rose 22 per cent for patients in the highest socioeconomic bracket, but rates fell nine per cent for patients in the lowest socioeconomic group.
To improve access for patients across all socioeconomic levels, policy changes are needed to ensure transparency and a lack of conflicts of interest.
“Patient protection requires the removal of all conflicts of interest among surgeons, including centre ownership and incentive plans aimed at pro-
moting the sale of add-on services. Patients need clear, non-conflicted information regarding the availability of publicly funded options without additional fees within both public and private for-profit centres,” write the authors.
They suggest creating a single waitlist for all private surgical clinics and public hospitals in an area, rather than separate lists for public hospitals and for-profit centres.
“Addressing the factors underlying this incongruity is vital to ensure equitable access to surgery and maintain public confidence in the cataract surgery system.”
“Public funding for private for-profit centres and access to cataract surgery by patient socioeconomic status: an Ontario population-based study” was published August 26, 2024. n H
With tick-borne viruses such as Powassan virus increasing in Canada, clinicians should consider these infections in patients with encephalitis, as a case study shows in CMAJ (Canadian Medical Association Journal).
Although rare, Powassan virus is serious, with a death rate of 10 per cent –15 per cent in people with encephalitis, and it can cause lingering health effects after infection. The virus can transmit within 15 minutes of tick attachment, and symptoms can develop one-to-five weeks later.
In this case study, a 9-year-old child with up-to-date vaccinations was admitted to hospital after a visit to an emergency department for fever, neck stiffness, and headache that developed 1 week after a camping trip in northern Ontario.
Physicians conducted extensive testing for a range of illnesses including Epstein–Barr virus, Lyme disease, bacterial meningitis, and more. They also sent serology samples for testing at the Public Health Ontario laboratory, but the results were not available for sever-
al weeks. The eventual diagnosis, confirmed after the child was discharged, was Powassan virus.
Cases of encephalitis from Powassan virus and other tick-borne illnesses have been increasing in the last 20 years, and the authors emphasize that the consideration of these is important. Recent travel to an endemic region, outdoor activity such as hiking and camping, and possible exposure to animals or ticks are important in helping diagnose.
“Given the nonspecific clinical features, laboratory investigations, neuroimaging findings of encephalitis, as well as the effects of climate change on tick-borne infection rates, broad arbovirus serology testing should be considered for patients presenting with encephalitis, particularly in the summer and fall,” writes Dr. Zachary Blatman, a senior pediatric resident physician at CHEO, Ottawa, Ontario, with coauthors.
“Powassan virus encephalitis in a 9-year-old” was published August 26, 2024. n H
With the recent listeria cases and food recalls in the news in Canada, it is important to understand the disease’s serious health effects in pregnancy, including fetal death. An article in CMAJ (Canadian Medical Association Journal) highlights important things to know about listeriosis, a foodborne bacterial illness that is 20 times more common in pregnancy.
1. When listeriosis spreads beyond the gastrointestinal system in pregnant people, it can be deadly for fetuses.
– The rate of fetal loss or neonatal death in pregnant people with invasive listeriosis is 29 per cent .
– Symptoms may include gastrointestinal symptoms, aches, fever, severe respiratory distress, and sepsis, although infection with Listeria monocytogene can also be asymptomatic.
2. Pregnant people should avoid foods at high risk of listeria contamination.
– These include unpasteurized dairy products, luncheon meats, meat spreads, and prepared salads.
– SYMPTOMS MAY APPEAR 2-3 MONTHS AFTER INGESTION
3. Investigation of asymptomatic people who may have consumed contaminated products is not necessary.
– Symptoms may appear 2-3 months after ingestion as the incubation period for listeriosis is up to 70 days.
4. Patients with mild gastrointestinal or flu-like symptoms and possible exposure to L. monocytogenes but no fever can be managed with blood tests and oral amoxicillin.
5. In patients with fever and possible exposure to L. monocytogenes, immediate blood cultures should be taken and high-dose ampicillin
started along with electronic fetal heart rate monitoring.
“Most importantly, pregnant people should be aware whether they have been recently exposed to contaminated foods,” recommends Dr. Jeffrey Wong, reproductive infectious diseases physician at BC Women’s Hospital and coauthor of the article. “While there are foods traditionally linked
with listeria, Health Canada product recalls alert people to foods contaminated with L. monocytogenes. Many recently recalled foods do not fall within high-risk foods. If a pregnant person is exposed, they should monitor for symptoms and seek medical advice if they become symptomatic.”
“Listeriosis in pregnancy” was published August 26, 2024. n H
Canada’s Pharmacare Act, Bill C-64 is merely a fillthe-gaps approach rather than a universal public program and should be amended, argue authors of a commentary published in CMAJ (Canadian Medical Association Journal)
Bill C-64, which will cover contraceptives and diabetes medications, is currently awaiting final approval by the Senate.
“A fill-the-gaps pharmacare system will not give Canada the institutional capacity needed to fairly and efficiently provide universal access to appropriately prescribed, affordably priced, and equitably financed medicines in a global context of powerful players and growing challenges regarding the reasonableness and transparency of pharmaceutical pricing,” writes Steven Morgan, professor at University of British Columbia, Vancouver, BC, with Matthew Herder, professor of law and medicine at Dalhousie University, Halifax, Nova Scotia.
“NATIONAL PHARMACARE THAT WOULD FUNCTION LIKE AND INTEGRATE WITH CANADA’S EXISTING MEDICARE SYSTEM HAS BEEN ADVISED AND DESIRED FOR DECADES.”
In Canada, there are currently more than 100 public drug plans and thousands of private plans. Prescription drugs account for almost half (45%) of health care spending by private insurance plans.
A fill-the-gaps plan will continue the country’s fragmented pharmaceutical buying practices, which increase drug costs. It will also add administrative complexity and higher premiums that will especially affect lower-income households, as private insurance plans will finance nearly half of the costs of the fill-the-gaps plan.
Further, Bill C-64 fails to clarify the powers, functions, and responsi-
bilities of the Canadian Drug Agency. The omission of these key details is a missed opportunity to ensure that national pharmacare remains accountable, first and foremost, to Canadians.
“National pharmacare that would function like and integrate with Canada’s existing medicare system has been advised and desired for decades. Although the preamble of Bill C-64 promises this, as written it will not deliver such a system and should therefore be amended,” the authors urge.
“Pharmacare Act does not prescribe universal, public pharmacare” was published August 12, 2024. n H

By Sarah Ripplinger
The emergency department’s role in providing life-saving care can extend into longer-term treatment plans for people with opioid use disorder (OUD). Vancouver Coastal Health Research Institute researcher Dr. Jessica Moe and clinical pharmacy specialist Dr. Katherin Badke researched emergency department health care worker perceptions on connecting people with OUD to the first-line treatment, buprenorphine/ naloxone (Suboxone).
“Emergency departments provide immediate, front-line access and are therefore ideal locations to identify people who are at risk of overdose, and to initiate interventions to provide support and mitigate that risk profile,” says Moe. “Our study builds on findings that there exists an opportunity to expand screening and patient engagement in this area.”
“Our team is building the knowledge base to positively impact clinical practice in the area of emergency department OUD identification and intervention.”
In one British Columbia study, around 60 per cent of individuals who experienced a drug overdose had visited the emergency department at least once within the year prior to their overdose event. However, there is presently no formal procedure to screen for and identify people with OUD, which puts someone at risk of overdose, states Moe.
Moe and Badke’s study, published in BMC Health Services Research, cites context-specific factors identified by 37 emergency department health care workers who participated in the study, including emergency physicians, nurses, pharmacists and social workers.
The research team conducted and drew from interviews and focus groups on OUD identification and patient engagement in emergency department settings to identify key themes regard-
ing the provision of take-home buprenorphine/naloxone kits to people with OUD.
Buprenorphine/naloxone, also known by the brand name Suboxone, is a partial opioid agonist medication given to people with OUD to replace the need for more harmful and potentially deadly opioids, such as unregulated fentanyl. The medication is given to patients at the Vancouver General Hospital emergency department as a take-home kit.
“The kit allows people to take the medication at home at their convenience,” explains Badke. “While other treatments are also available, buprenorphine/naloxone has a track record of being a safer and more convenient option for people with OUD.”
Regular opioid use builds dependence in the brain and body, making stopping a monumental feat for people with OUD. A United States study found that the initiation of buprenorphine/naloxone in the emergency department was able to retain 78 per cent of participants in addictions treatment programs within the first month, compared to X% in a control group who received referral to addictions care alone, without buprenorphine/naloxone.
The study team identified key themes from participant feedback, including difficulty carving out time and space in understaffed and resource-strained emergency departments for confidential discussions with patients about OUD and treatment options. “There are so many patients in emerg and so many things that I’m doing,” said a pharmacist participant. A participant who is identified as a nurse echoed this sentiment, stating that the much-needed, in-depth discussions surrounding OUD treatment are often cut short due to competing

Emergency departments provide immediate, front-line access and are therefore ideal locations to identify people who are at risk of overdose, and to initiate interventions to provide support and mitigate that risk profile.
demands, such as needing to attend to other emergency situations.
A social worker who participated in the study identified a need to spend time building rapport with people with OUD to successfully introduce concepts surrounding treatment.
Providers highlighted multidisciplinary collaboration as a strength that can enable teams to complete multiple, time-sensitive tasks necessary to provide patients with buprenorphine/ naloxone in a fast-paced emergency department setting.
Patient receptivity and ability to absorb information were also cited by study participants as both opportunities for engagement as well as barriers. A nurse participant noted that a person with OUD’s prior awareness and understanding of buprenorphine/ naloxone facilitated treatment initiation. Conversely, a physician participant shared an example of a patient who was too drowsy from opioid use to consent to initiating buprenorphine/ naloxone.
Likewise, study participants’ familiarity with buprenorphine/naloxone
was noted as being either a supporting factor or a barrier to its initiation, which coincided with many participants favouring the idea of ongoing OUD and buprenorphine/naloxone initiation training. This was supported by the belief among many participants that the emergency department is an essential first point of contact to discuss buprenorphine/naloxone with the target patient population.
“Where else in the health care system do we see people at all hours of the day, seven days a week?” asks Moe. “This is a low-barrier setting where the health care system can offer people with OUD support that could save their lives.”
“Our study demonstrates the incredible work that emergency department providers do every day – despite unprecedented strains – to support patients at risk of overdose during a public health emergency,” says Moe. “Our team’s resilience, commitment and empathy are true points of pride and must be matched by greater resources and supports to optimise the impact of what we do.” n H
new, first of its kind Canadian study suggests flash glucose monitors* can help improve health and reduce healthcare resource utilization (HRCU) for people living with diabetes.1
Presented at the American Diabetes Association’s (ADA) 84th Scientific Sessions this past June, findings from the FRONTIER study are significant, given that 5.8 million people in Canada live with diabetes.2 For many people living with diabetes, daily self-management of glucose levels is critical to reducing serious, potentially life-threatening complications that can lead to hospitalization.3,4 This means that beyond the physical and mental impacts on individuals, diabetes complications impose significant costs on an already stretched healthcare system. According to Diabetes Canada, the national cost of treating diabetes jumped from $14 billion in 2008 to just under $30 billion in 2019.5
Led by Dr. Stewart Harris and Dr. Alexandria Ratzki-Leewing of Western University, as well as Dr. Remi Rabasa-Lhoret of Université de Montréal, the FRONTIER study used data from the Institute for Clinical Evaluation Sciences (IC/ES) and real-world practice data, which were analyzed for more than 45,000 Ontarians diagnosed with type 1 or type 2 diabetes who met specific criteria.
“Our population-based study design allowed us to examine flash glucose monitor* use in a different way,” says Dr. Ratzki-Leewing. “For years, we’ve understood the benefits of this technology on diabetes management. The ability to study its effects on a much larger population, with a more comprehensive scope of people,
Mean
before and after starting
helps validate that understanding and strengthen the case for the tool’s use by all people living with diabetes.”
The FRONTIER study examined two key measures: glycated hemoglobin (HbA1c) levels, an average of an individual’s glucose levels over a 2- to 3-month period, and healthcare resource utilization (HRCU), defined as the overall incidence of emergency department (ED) visits and hospitalizations. HbA1c levels were recorded 12 months before the first claim of a flash glucose monitoring system* and at the end of a 24-month follow-up period. HRCU data were collected from 12 months prior to the use of the technology and during the last 12 months of the follow-up period.1
As Harris, Ratzki-Leewing, Rabasa-Lhoret, and their colleagues found, the effect of flash glucose monitor* use on diabetes outcomes was undeniable. After adopting flash glucose monitoring*, HbA1c levels improved by 0.6 per cent for the under 66-year-old cohort and 0.3 per cent for the over 66-year-old cohort, regardless of their type of diabetes and treatment regimen (figure 1).1
Additionally, the overall incidence of ED visits dropped by 15 per cent for the under 66 cohort and 9 per cent for the over 66 cohort, whereas overall hospitalizations dropped by 11 per cent and 9 per cent, respectively, after using a flash glucose monitor* (figure 2).1
“These data give us proof that tools like flash glucose monitors* reduce
healthcare utilization, support daily diabetes management and improve health outcomes,” says Dr. Harris. “For healthcare providers, like myself, it means having a tool to empower our patients to help control their glucose levels and reduce their risk of complications. And for our patients, it means having a companion that helps them make the hundreds of diabetes-related decisions they make every day.”
The results also clearly demonstrate the broad systemic benefits of flash glucose monitors*. Ontario is the first province to provide public coverage for flash glucose monitors* for people managing their diabetes with any insulin. Other provinces also offer reimbursement for these tools to individuals who meet specific criteria.††
“With more awareness, coupled with continually expanding reimbursement, Canadians, and the healthcare system, stand to benefit. Removing barriers to access is so important and it’s encouraging that many private and public reimbursement programs now cover flash glucose monitoring systems*,” adds Dr. Rabasa-Lhoret. “The evidence is clear – this technology supports people living with diabetes as well as the overall healthcare system.” n H
2. Reduction in ED visits and hospitalizations overall, with DKA, and with hypoglycemia after starting
*Examples of flash glucose monitoring systems include Abbott’s FreeStyle Libre 2. The FreeStyle Libre 2 flash glucose monitoring system is indicated for measuring interstitial fluid glucose levels in people aged 4 years and older with diabetes mellitus. Always read and follow the label/insert. † Data collected from the FreeStyle Libre system. FreeStyle Libre 2 has the same features as the FreeStyle Libre system, with the addition of optional real-time glucose alarms. Study data are applicable to both products. ††Please check EasytoFreeStyle.ca for more information on public coverage in Canada for the FreeStyle Libre 2.
1. Harris, S.B., Ratzki-Leewing, A. et al. “FRONTIER – Flash Glucose Monitoring Use in Ontario Among Patients with DM in the ICES Database – Evidence from Real World Practice.” Data presented at the American Diabetes Association 84th Scientific Session, June 21-24, 2024. 2. Diabetes Canada. “Estimated Prevalence and Cost of Diabetes.” Accessed August 7, 2024. https://www.diabetes.ca/advocacy – policies/advocacy-reports/national-and-provincial-backgrounders/diabetes-in-canada 3. Benoit, Stephen R et al. “Trends in Emergency Department Visits and Inpatient Admissions for Hyperglycemic Crises in Adults With Diabetes in the U.S., 2006-2015.” Diabetes care vol. 43,5 (2020): 1057-1064. doi:10.2337/dc192449 4. McCoy RG, Lipska KJ, Van Houten HK, Shah ND. “Association of Cumulative Multimorbidity, Glycemic Control, and Medication Use With Hypoglycemia-Related Emergency Department Visits and Hospitalizations Among Adults With Diabetes.” JAMA Netw Open. 2020;3(1):e1919099. doi:10.1001/jamanetworkopen.2019.19099 5. Diabetes Canada. “New Data Shows Diabetes Rates And Economic Burden On Families Continue To Rise In Ontario” Accessed August 7, 2024. https://www.diabetes.ca/media-room/press-releases/newdata-shows-diabetes-rates-and-economic-burden-on-families-continue-to-rise-in-ontario.
www.hospitalnews.com
Humber River Health (Humber), situated in one of Toronto’s most diverse communities, consistently demonstrates its commitment to innovation and excellence in healthcare. This dedication is especially evident in their Apotex Emergency Department (ED), the busiest in Ontario, serving almost 140,000 patients annually. Despite the high volume and complexity of cases, Humber has set provincial benchmarks for quality care, driven by a culture of innovation and the strategic implementation of digital health technologies.
In response to the growing challenges of managing patient flow and hospital resources, Humber is introducing an artificial intelligence (AI)-enabled online queuing system. This optional innovative tool will advise low-acuity patients whether they should come to the ED immediately or enter the queue from home, reducing unnecessary congestion and optimizing resource utilization. The system uses AI and machine learning to predict patient queues and determine advanced time slots based on urgency and resource availability. By timing their arrival for less emergent cases, patients can minimize wait times and receive timely care.
At Humber, the focus on innovation stems from a continuous drive to provide patients with better access to care closer to home. This ethos was central to a recent study conducted by Humber River Health’s Research Institute. The study aimed to assess the community’s willingness and ability to use digital technologies, ensuring that the AI queuing system being implemented would meet the specific needs of the patient population.
The Research Institute’s study recruited patients visiting the Apotex Emergency Department to participate in a survey examining access to, use of, and attitudes toward digital

technology. The results were promising, with nearly all patients having access to digital devices and internet, and expressing positive attitudes toward technology. These findings indicated that patients are willing and able to use everyday technologies, suggesting minimal barriers to adopting the AI-enabled online queuing system.
“The culture at Humber is one where we are continuously leveraging technology to support our teams and the community we serve,” said Dr. Peter Voros, Vice President of Clinical Programs at Humber. “It is important to us that we listen to the needs of our community, and we are confident that this tool will help improve the patient experience.”
Central to Humber’s ability to manage such a high volume of patients efficiently is the state-of-theart Command Centre. This “mission-control” allows staff to keep a constant watch on patients, even
when they are on the move. In the Command Centre, a specialized team scans real-time data displayed across a wall of monitors, known as tiles. Each tile is dedicated to a specific aspect of hospital or patient data, including emergency room wait times and NICU patient vitals, to assess patient risk. Any concerns are flagged and immediately sent to various departments, which work collaboratively to address them.
The Emergency Department Tiles in the Command Centre provide a live feed of the ED as well as a bird’s eye view of capacity, waiting lists, and patients waiting to be moved to the appropriate level of care. All of the data collected by the Command Centre is fed back to medical teams across different platforms, including their handheld devices, ensuring patients receive better, faster, and safer care.
Humber River Health has long been recognized as one of the safest hospitals in Canada. Despite having the busiest ED in Ontario, Humber boasts 66 per cent fewer cases of hospital harm than the provincial average, a 10 per cent
year-over-year reduction in sepsis cases, and a 40 per cent year-over-year decrease in code blues – medical emergencies that can include heart attacks or respiratory distress.
At Humber River Health, innovation is not just a luxury but a necessity. The forthcoming implementation of the AI-enabled online queuing system exemplifies their commitment to providing the highest quality care through advanced technology and innovative practices. Humber remains focused on collaboration with community partners, listening to patient needs, and continuously improving the delivery of care.
“Without constant innovation, there is no way we can do what we do today. We are constantly seeing more patients with greater needs within existing budgets, and this allows us to provide better, safer care,” emphasized Dr. Voros.
Humber River Health is proud to work closely with its community partners to coordinate and manage care effectively, in the most appropriate settings, leading to the best outcomes for patients. The organization recognizes the pivotal role digital technologies play in improving patient access to healthcare and supporting the effective and efficient delivery of healthcare services. The challenges faced by the community in Northwest Toronto, including high unemployment rates and a shortage of primary care physicians, underscore the importance of these innovative solutions.
Through these efforts, Humber River Health continues to light new ways in healthcare, demonstrating that even in the face of significant challenges, excellence and innovation can thrive. This commitment to research-driven, patient-centric innovation ensures that Humber River Health remains at the forefront of delivering high-quality, equitable healthcare to its community. n H
By Kaitlin Jingco
Recent advancements in cancer treatment have lengthened and improved patients’ lives, but the increased complexity in care can be challenging to navigate – especially for marginalized communities.
“It’s almost like cancer care becomes someone’s full-time job. They’re so busy going to appointments for scans, for tests, for treatments, that they don’t have time to do anything else,” says Dr. Lisa Hicks, malignant hematologist at St. Michael’s Hospital. “When you’re already struggling to manage your day-to-day, navigating care becomes almost insurmountable.”
To address this, an interdisciplinary team led by Hicks and medical oncologist Dr. Ronita Lee received $200,000 in funding from the Canadian Partnership Against Cancer for a new pilot project supported by Ontario Health
– Care for All: An initiative to help marginalized patients engage with, and benefit from, cancer treatment.
The goal of the program is to provide a sustainable infrastructure that will enable oncology care teams to identify and address the unique, unmet needs of vulnerable patients with cancer.
“Often the patients with the highest needs are the people who don’t speak up,” says Hicks, adding that when people are dealing with homelessness, mental illness and cultural and language barriers, they may not have the capacity to advocate for themselves. “That’s what this initiative is really about. It’s about, ‘How can we get the services and assistance to those who need it most?’”
“Cancer can be challenging for patients physically, emotionally, mentally,” adds Lee. “We want to help patients navigate their cancer care and offload some of that burden, as cancer therapy itself is only part of the treatment.”
To start, the team, which will include oncologists, nurses, social workers, administrative champions and patient representatives, will conduct a mixed methods study to better understand the needs of marginalized people with cancer.
That information will help guide the development of interventions. The team isn’t certain exactly what it will look like – it could be a guide to connect people to existing resources, it could lead to new resources being created, it could be a reorganization of existing processes (likely, it will be all of those things) – but they do know some of the key issues that will need to be addressed.
“Cancer has a financial impact on our patients, so I expect there will be a financial piece,” says Hicks, citing the cost of drugs, child care and transportation, as well as the loss of income from being off work, as some of the reasons. “When we’re talking about patients who are already living in poverty, that can be crushing.”


Hicks says there will likely also be aspects to assist with transportation; support cancer-related dietary needs, especially for those dealing with food insecurity; coordinate appointments so that patients don’t have to go to the hospital so frequently; and help patients with various cultural and language needs.
Some care providers and services are already addressing these barriers, but Hicks and Lee say there’s opportunity for them to be done better and in a more coordinated way.
“Locally, the goal is to create an infrastructure that provides lasting benefits to patients,” says Hicks. The hope is that infrastructure will be adaptable for other centres that are caring for patients with intersectional vulnerabilities.
“We see people falling through the cracks,” says Hicks of cancer care. “We’re seeing a ton of advances, but if we don’t act, not everyone is going to benefit.” n H
By Dave Yasvinski
Dr. Cesar Marquez-Chin has been preparing for the future ever since he watched Star Wars for the first time.
Growing up in Mexico City, the University Health Network (UHN) scientist spent countless hours at the local movie theatre, watching and rewatching his favourite science fiction movies play out on the silver screen, where his young mind opened up to infinite possibilities.
“For me, science fiction is like going to school,” Dr. Marquez-Chin says. “I know that sounds ridiculous, but when I see things on the screen, I get a lot of inspiration. It makes me wonder, ‘How would I do this? Is this even possible?’ I love movies; they transport me to a different planet. I think I watched Star Wars seven times when it came out.”
His emerging enthusiasm for technology would soon be tempered by tragedy. On the morning of September 19, 1985, a powerful 8.1-magnitude earthquake rocked the Mexico City area, killing more than 10,000 people and injuring 30,000 others.
“It was an awful situation,” Dr. Marquez-Chin says. “As you can imagine,

after that event, the number of people with disabilities on the street grew exponentially. I think that planted a seed of interest in the field of rehabilitation engineering.”
Now, Dr. Marquez-Chin is part of the Neural Engineering and Therapeutics (NET) Team at the KITE Research Institute, where he’s devel-
Dr. César Marquez-Chin weighs in on the real-life viability of a few other popular cyborgs we know and love.
Robocop
In this 1987 movie, a police officer killed in the line of duty is resurrected with the help of cyber technology to become the ultimate crime-fighting machine.
“Robocop is the ultimate cyborg, even beyond Luke Skywalker,” he explains. “The fact that you can control such a complex mechanism with just brain activities – that’s pretty cool, but I don’t know how you would do it. How would you extract all those signals to drive the artificial body? At the same time – and this is something that no one ever thinks about –what kind of battery would you use to power it?”
Dr. Marquez-Chin compares Robocop’s body to an electric car, noting that a good portion of the weight of the car is batteries, which would make the logistics of powering a human body a challenge. He also points to
oping the kind of futuristic technology he might have seen at the movies back in Mexico. Even better, his work combines his love of sci-fi with his interest in rehab.
the method through which information is transferred into the brain in the Matrix – via a giant plug at the base of the skull and questions how it would work for a real-life cyborg.
“If you’re recording information from so many sites, what type of connector do you need? That’s a real challenge for people who work in this field: How do you get information to and from the brain?”
Terminator
Although many of us think of the Terminator franchise when cyborgs are mentioned, Dr. Marquez-Chin questions the practicality of the concept.
“The Terminator is just a robot with a suit over it, which could help the aspect of appearance – so you wear a prosthetic device, for example, and the device looks like a natural hand,” he explains. “But how would you give maintenance to it when you need to have surgery, if you have this biological sleeve over top of it? I’m not sure that’s very practical from my perspective.”
His current research aims to restore a person’s ability to move voluntarily after suffering from one of the two main causes of paralysis: stroke or spinal cord injury. The technology works by retraining the brain to make the body move again without the ongoing aid of assistive devices, such as a wheelchair. It relies on a brain-computer interface that identifies when the body is trying to move and electrical stimulation to help the nervous system make it happen.
Dr. Marquez-Chin’s work couldn’t come at a better time. According to a study by the Heart and Stroke Foundation, there are 108,707 stroke occurrences in Canada every year (or one every five minutes), all with the potential to cause some degree of paralysis. There are also more than 85,000 Canadians currently living
brain-computer interface detects the intention to move by analyzing brain activity in real time. When it identifies that the person is attempting movement, it triggers functional electrical stimulation that actually helps the person produce the movement.”
Ultimately, the goal is to help patients live as independently as possible by restoring their own ability to move.
It’s not lost on Dr. Marquez-Chin that his research often mirrors the science fiction films he enjoyed all those years ago. Some of the technology, he says, isn’t as far-fetched as one might think.
The Matrix, for example, takes the concept of the brain-machine interface to the next level by fully immersing humanity in a virtual world created by machines. The interface that enables this illusion not only extracts massive amounts of information from Neo – or anyone else connected to the Matrix –it also injects information directly into their brains to allow them to touch

“That’s really interesting because some of those technologies are actually in development,” Dr. Marquez-Chin says. “Not at that level, but a cochlear implant, for example, uses a microphone that basically translates sound into pulses that stimulate your brain so you can hear. We also have visual prostheses in which people who are blind can see colours or broad figures. So, it’s really tricky, but maybe one day.”
Another work of fiction that may be flirting with reality is Blade Runner, a movie set in a dystopian future riddled with synthetic humans. “Blade Runner is very unique in the sense that it’s all biological,” Marquez-Chin says. “They’re basically clones that are given an expiry date. But what’s interesting is the notion of implanting memories.”
While he doesn’t think we’ll see evil replicants running around any time soon, Dr. Marquez-Chin says there are researchers at UHN who are trying to
understand how memories are created at the neuronal level. “This is very important because it will allow us to potentially create new interventions for people with memory problems, such as people with Alzheimer’s disease. Whether it’s a form of prevention or treatment, that’s another thing. We’re not quite there yet in terms of implanting memories.”
As for his own real-life sci-fi exploits at KITE, the results have been encouraging and Dr. Marquez-Chin’s team has witnessed important changes in people who have not traditionally responded well to therapy. The closest parallel to his work is probably found in that galaxy far, far away.
In the Star Wars movies, Luke Skywalker requires a robotic hand replacement after an unsettling encounter with Darth Vader’s lightsaber. “That notion of using signals from the nervous system to control an external device aligns with what we’re trying to do,” he says. “It’s funny to think that when I was little, maybe I was already working on this.” n H
By Christina Cindric
rip. Drip. Drip.
DSimon is lying in a hospital bed after a successful abdominal surgery. Listening to the steady drip of the intravenous (IV) pump, he wonders whether he’s getting the right medication. What’s worse, he wonders, “what if the dose is wrong? What happens then?”
He resigns himself to the fact that he has to put his trust in the health care professionals taking care of him. Surely, the doctor has prescribed the right medication, the pharmacist verified it correctly and the nurse programmed the equipment properly.
And for patients like Simon, this is true at most hospitals, most of the time.
However, as the Enlightenment poet Alexander Pope’s quote goes, “to err is human,” and human error is unfortunately a risk across the health care system when it comes to manually programming an IV pump.
To help address this risk, Mackenzie Health has added an additional level of assurance that patients are getting the right medication at the correct dose, at the rate and time they need it.
In April, the organization became the first health care provider in Canada to launch a technology that allows for the sharing of two-way information between the IV pump and the patient’s electronic medical record (EMR), providing additional safeguards to ensure patients receive the right medication every time.
This new technology, known as BD Alaris™ EMR interoperability, was introduced at both Mackenzie Richmond Hill Hospital and Cortellucci Vaughan Hospital. It replaces the need for health care profes -
sionals to manually program pumps while sending infusion safety information back into the Epic EMR. This significantly reduces the risk of administration errors and provides a more accurate infusion record in the EMR.
A study published in the American Journal of Health-System Pharmacy found that interoperability and this type of connectivity between technology, equipment and workflows can result in an 86 per cent reduction in the average number of keystrokes needed to manually program an infusion.
By scanning a patient’s wristband, medication barcode and infusion pump, the care team can connect a patient’s electronic medication order to their IV pump and verify that it will deliver the right medication and dosage to the right patient at the right time.

“Mackenzie Health is committed to continually improving the way we deliver safe, quality care to our patients,” says Mary-Agnes Wilson, Executive Vice President, Chief Operating Officer and Chief Nursing Executive at Mackenzie Health. “We are on a journey to zero harm, embracing the philosophy that even one error is one too many. This new, connected IV pump technology helps enable the safe administration of medication and ultimately better outcomes for those who trust us with their care.”

Top: Alexander, a nurse at Mackenzie Health, scans a medication barcode to verify that the IV pump will deliver the right medication and dosage to the patient he’s caring for.
Left: Intravenous (IV) medication pumps using BD Alaris™ EMR interoperability technology were introduced at Mackenzie Richmond Hill Hospital and Cortellucci Vaughan Hospital in April 2024.
Making investments like this is part of Mackenzie Health’s commitment to the principles of High Reliability Organizing (HRO) – principles used in industries like aviation and nuclear where the stakes are high and errors can lead to catastrophic outcomes. Mackenzie Health is committed to providing health care workers with the tools, processes and skills they need to reduce errors and prevent events that can cause harm to patients and employees, ensuring every patient receives reliable and consistent care, every time.
“In 2017 when purchasing additional smart infusion pumps in ad-
By Christina Cindric, Senior Communications Consultant and Public Affairs Lead, Mackenzie Health
vance of opening our second hospital, we made the decision to continue investing in a single platform that would allow us to leverage additional interoperability features in the future,” said Purvi Desai, Vice President, Digital Health and Chief Information Officer. “Enabling these additional features that allow for two-way information flow between IV pumps and our electronic medical record creates efficiency, adds safeguards to the process and ultimately allows our clinicians to do what they do best –spend more time taking care of their patients.” n H
By Marlene Leung
t’s been seven months since Daniel Hook had successful surgery at St. Michael’s Hospital to treat an abdominal aortic aneurysm (AAA), a condition where there is swelling or ballooning in the aorta. Known as a “ticking time bomb” because it can grow undetected for years, AAA is usually deadly if the aortic aneurysm ruptures or bursts.
Hook’s AAA was discovered by clinicians at St. Michael’s, who performed an emwergency surgery on him in 2022 to remove a blood clot from his leg. The care team monitored the AAA until it was large enough to warrant surgery and, in December 2023, scheduled the 63-year-old for a minimally-invasive aneurysm repair in Operating Room 20 per cent one of the hospital’s new hybrid ORs.
On the day of the surgery, Vascular Surgeon Dr. Charles de Mestral and colleagues treated the AAA with an endovascular stent to relieve pressure from the aorta. The stent was inserted and placed into Hook’s aorta via a needle puncture in the groin – or as Hook recalls “two quick pokes in my hip.”
After a brief two-night hospital stay, Hook returned home.
“I started being active when I got home. I started going for daily walks and following my doctor’s directions,” he said, noting that since his surgery he’s quit smoking, cut out alcohol and caffeine and is working on reducing his sugar intake. “I feel happy, like I can be active again.”
Hook will continue to receive follow-up care from St. Michael’s, including annual ultrasounds of his abdomen to monitor the stent. He says while he was initially very nervous to have a second surgery after the removal of his blood clot, he always felt very safe with his care team.

but it’s at risk of bursting,” he said. “If it bursts, most people don’t survive. Most people don’t make it to the hospital, and survival rates are not high for those who do make it in time to get an emergency surgery.”
De Mestral is among a group of researchers who are calling for the creation of provincial AAA screening programs.
Despite existing recommendations for aneurysm screening, there are currently no established screening programs in Canada.
Earlier this year, de Mestral and his research team published a study in the Canadian Medical Association Journal that found that AAA screening is cost-effective and results in fewer AAA-related deaths.
Based off models, the study found that screening adults 65 and older reduced AAA-related deaths by 84.9 per cent among males and 81 per cent among females. Screening for AAA was increasingly cost-effective in populations with higher AAA prevalence.
“I got a lot of strength from the wonderful people at St. Michael’s. I was overwhelmed by how everybody was there for me. I had no reservations, no hesitations. I feel very positive about the whole experience,” he said.
De Mestral was also happy with the outcome. “This was a textbook minimally-invasive abdominal aortic aneurysm repair with a rapid recovery. As our first case in the new hybrid OR suite, it could not have gone more smoothly,” he said.
In addition to top-of-the line OR equipment, de Mestral also credits the successful surgery to collaborative pre-operative planning of all AAA repair cases by vascular surgery and interventional radiology colleagues and, to a strong OR team of anesthesiology, nursing and medical imaging professionals, as well as trainees.
In Canada, about 20,000 people are diagnosed with AAA every year. Risk factors for AAA include a family predisposition, as well as smoking, high blood pressure, high cholesterol and hardened arteries. AAAs are much more common in men. The size of an AAA is closely linked to the risk of it bursting.
The main treatment for an AAA is to manage risk factors and monitor the aneurysm risk with regular ultrasounds of the aorta. Surgery is recommended only once the risk of the AAA bursting exceeds the risk of surgery. Early detection and monitoring provides the opportunity to fix the AAA before it bursts, says de Mestral.
“The concern is that an aortic aneurysm rarely causes any symptoms,
“Our results support one-time ultrasonography screening for AAA in Ontario for males aged 65-75 years, consistent with current screening recommendations. Screening for females aged 65-75 years is likely cost-effective despite lower prevalence rates,” the study concluded. “Given our findings, the implementation of provincial AAA screening programs should be seriously considered.”
De Mestral said Ontario Health is currently looking to establish an aneurysm screening program, and data from this study will help move the development of the provincial program along.
“The research is well tied-in to policy,” he said. “Often research is done with the hopes that it will inform practice. We know that the data from our study are actively being used in the planning of an AAA screening program in Ontario. That’s pretty exciting.” n H
On November 30, 2024, Unity Health will launch its new electronic patient record (EPR) system, transforming communication and information sharing between patients, families and their care teams.
Called Project Connect, this major clinical transformation project will improve the way that clinical teams deliver care and empower patients to play a more significant role in their care journey.
The new system is powered by Epic Systems and was informed by over 500 staff, physicians, patients, and Patient & Family Partners who sit across several work groups and advisory councils. These groups are making sure the system is designed to meet the needs of Unity Health patients and teams.
Caroline Assouad, an EPR Applications Specialist Inpatient with a background in nursing, is working with clinicians in the obstetrics departments
at St. Michael’s Hospital and St. Joseph’s Health Centre to ensure their Epic module, called Stork, meets their workflows and needs prior to go-live.
“We need to build one system, so harmonization of policies, order sets and workflows across the organization is key,” says Assouad, who meets with clinical experts to review the module and then edits it to fit their specific needs. “I really enjoy the sort of problem solving that building the system requires.”
At Providence Healthcare, where most clinical and corporate processes are paper based, this project marks a major change in practices and workflows.
It’s a lot of work, says Olga Krasik, a Clinical Nurse Educator at Providence, but it’s also really exciting.
“The new EPR system will relieve nurses of more of the administrative burdens and give them more time to do what they do best – provide excellent patient care,” says Krasik.
Across Unity Health, clinicians say they’re looking forward to seamless information sharing with patients and fellow clinicians, whether they’re sharing laboratory test results, diagnostic images or medication information. The ease of information sharing also promises to improve patient safety.
“Clear, automated tracking of medication, treatments and diagnoses allows everyone on a patient’s care team to obtain the same information,” says Krasik. “It’s a great way to help us reduce the number of potential errors.”
Alina Lalani, a Clinical Pharmacy Specialist and Leader at St. Joseph’s, says that while communication and information sharing within each site will improve, the new system will also make it easier to seamlessly transfer patients between sites.
“The current practice for transfer of information is to download and share our documentation which is labor intensive and not always consistently
Did you know: Today, healthcare workers have 1.5 times the number of lost-work days than the average Canadian worker?
Prioritizing employee health and safety should be top of mind for all employers.
That’s where a Joint Health and Safety Committee (JHSC) shines. A JHSC is foundational in creating a safer and healthier workplace, helping achieve compliance and excellence in occupational health and safety. Made up of worker and employer representatives, the goal of a JHSC is to be mutually committed to improving health and safety in the workplace. Every Ontario business with 20 or more regular employees is required to have a JHSC in place with a minimum of two certified members who have completed training with an approved provider.
The Public Services Health and Safety Association (PSHSA) is here to help you on your journey to workplace health and safety. We understand that everyone learns differently, which is why we offer flexibility in how learners approach their JHSC certification. Learners
done,” says Lalani. “Epic will allow seamless conversations between our teams across sites which will reduce our workload overall.”
Though Project Connect is a clinical transformation project, it will also transform processes for some corporate and support services teams. For instance, the Patient Transport teams at Unity Health will be able to receive transport requests on their mobile devices, eliminating the need for colleagues to monitor a central intake email and dispatch team members upon request.
“This improvement will lead to quicker responses to patient needs and smoother overall operations,” says Punya Ross, Manager of Environmental, Patient Food and Transport Services at Providence. “It’ll give us more time to focus on what’s most important – patient care.”
More information about Project Connect is available on the Unity Health Toronto website. n H
can choose to learn on their own with self-paced eLearning or can attend sessions led by a knowledgeable instructor either in-person or virtually. For larger groups of learners, we also offer private training delivered just for you and your organization.
JHSC training is delivered in two parts. For Part 2 training, PSHSA offers general sessions for all workplaces, as well as specialized certifications tailored to our sectors. These specialized healthcare sessions are facilitated by our health and safety consultant using their sector-specific expertise. This experience allows the course content to align more closely with healthcare, using examples and references tailored to the challenges learners face in their jobs.
Within this training, learners are joined by others within that sector, allowing them to engage with peers, share learning and working experiences, and benefit from the collective knowledge of workers across Ontario.
Help lower the lost-work days average across Canada tomorrow by keeping workers safe today with an effective JHSC.
t the beginning of this year, St. Joseph’s became one of Canada’s first academic community hospitals to deploy AI to improve patient care and streamline staff and physician workloads.
CHARTwatch, which was deployed in partnership with Signal 1, a Canadian health AI startup, is one of over 50 AI and analytics innovations developed by the Data Science & Advanced Analytics (DSAA) team at Unity Health. Our network has deployed more AI solutions into clinical practice than any other Canadian hospital. These innovations are designed to save lives and improve care across the network.
CHARTwatch started at St. Michael’s on the General Internal Med
data like test results and vital signs to predict the level of support a patient will need. It can tell us which patients are at risk of getting more sick.
Since deployment at St. Michael’s, unplanned mortality has decreased by over 20 per cent. The same is expected to happen at St. Joseph’s.
Alice Feruelo, a Registered Nurse and Team Leader on the Medicine unit at St. Joseph’s, says this unique tool has made nurses feel more confident in their patients’ conditions and has given them back time to dedicate to other necessary tasks.
For Feruelo and other registered nurses like Emme Rose Villanueva, CHARTwatch has started conversations among the team and helped them learn about risk factors they

“It’s so much easier for us to tell who is high risk now,” says Feruelo.
Bringing CHARTwatch to St. Joseph’s was a collaborative project. Data engineers, clinical informatics specialists, data scientists, system administrators, physicians, nurses and project managers, among others, came together to bring it to life.
“From a technical perspective, the data sources and technologies at St. Michael’s and St. Joseph’s are different, so we had to make some adjustments,” says Chloe Pou-Prom, Senior
The team trained the AI tool on a new model using data from patients previously admitted to the General Internal Medicine unit at St. Joseph’s. From a clinical perspective, the team tailored the system to fit the needs of the St. Joseph’s community hospital patient care environment.
While it’s still in its earliest phases, everyone agrees that the results seem clear: AI is preventing potentially life-threatening events before they happen and creating an even better system of care as it spreads across our


By Anna McClellan
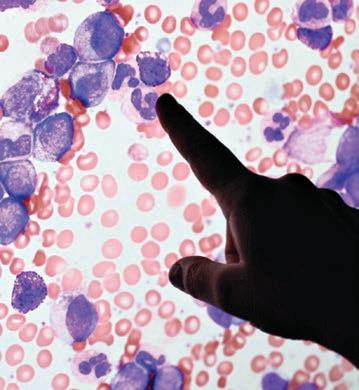
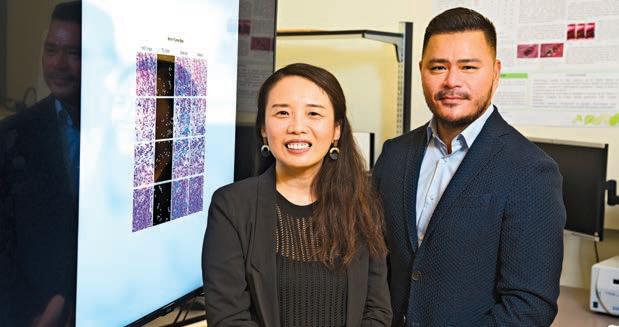
dvancements in technology play a crucial role in health care breakthroughs and holds significant potential for the future. Researchers at Sunnybrook are using emerging artificial intelligence (AI) technologies to advance the diagnosis, treatments and outcomes of some of the world’s most debilitating diseases.
Oral cancer is a form of head and neck cancer, affecting more than 5,000 Canadians per year. Progression of the disease can drastically affect the way an individual eats and speaks. Dr. Jesse Chao, scientist in the Odette Cancer Research Program at Sunnybrook Research Institute (SRI) and Canada Research Chair in Precision Cancer Diagnostics and Artificial Intelligence, is developing new AI software to better detect cancerous cells in the mouth and lymph nodes which will support early detection, staging, and prognosis, leading to improved patient outcomes. Using samples from over 500 patients with oral cancer, Dr. Chao and his team are training AI software to automate the image analysis of microscopy data. The software first identifies regions in the tissue and pinpoints areas likely to contain tumours, it then confirms the presence of cancerous cells. Pathologists often have to go
through numerous slides and use many different dyes and stains to determine an oral cancer diagnosis. “Automating this process enhances diagnostic quality, advances early detection, supports personalized treatments and ultimately improves patient outcomes,” explains Dr. Chao.
Currently Dr. Chao and his lab are applying this model to detect instances of oral cancer, however, with further research Dr. Chao hopes the software will play a role in the diagnosis of other forms of cancer too.
Dr. Jesse Chao, scientist at Sunnybrook Research Institute and Canada Research Chair in Precision Cancer Diagnostics and Artificial Intelligence.
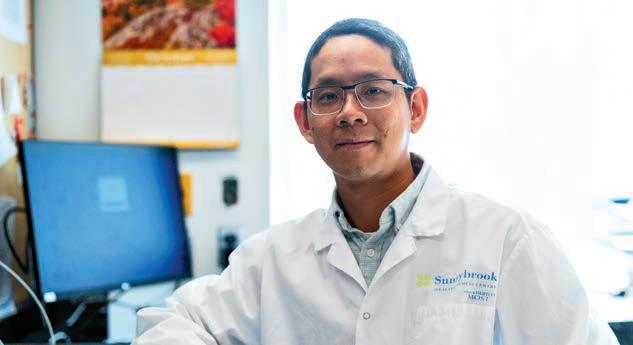
An intracerebral hemorrhage (ICH), or brain bleed, is a form of stroke and occurs by a spontaneous artery rupture or traumatic brain injury. ICH is the deadliest types of stroke, accounting for one in six acute strokes. Dr. Bradley MacIntosh, senior scientist in the Hurvitz Brain Scienc-

es Research Program, and his lab are using deep-learning AI tools to support acute stroke imaging and aid in the treatment of patients suffering the deadliest types of stroke.
Timely diagnosis and treatment play a critical role in stroke patient outcomes and in order to provide care for patients suffering from a brain bleed, clinicians need to know the size of the bleed and where it is located.
The MacIntosh lab has built an AI tool called VIOLA to analyze, detect, and outline locations of hemorrhages visible on computed tomography (CT) scans of patients who have had a stroke. The VIOLA tool searches CT scans and automates these measurements, saving time and potentially improving patient outcomes.
“The VIOLA tool can provide clinicians with an accurate analysis and measurement of a brain bleed, enabling faster care and ultimately increasing the likelihood of recovery for stroke patients,” says Dr. MacIntosh.
Breast cancer is one of the most common types of cancer affecting women in Canada, with about 1 in 8 women developing it in their lifetime. Dr. William Tran, radiotherapist and senior scientist in the Odette Cancer Program and Dr. Fang-I Lu, a breast pathologist at Sunnybrook, have teamed up to develop an AI tool to improve radiation therapy treatment for breast cancer patients.
The team’s technology maps the tumour immune microenvironment, the complex ecosystem of cells surrounding the breast’s tumour, to measure the probability of a tumour’s response to high-dose radiation treatment in women with high-risk breast cancer. The project involves taking thousands of tumour images and complex computational methods to recognize biomarkers associated with the tumour-killing effects of radiation treatment. Dr. Lu explains, “the ability to predict a tumour’s response to certain types of therapy has the potential to support more personalized and effective treatment plans for patients with advanced breast cancer.”
Radiation therapy is a common type of treatment for many cancers, but can also damage healthy cells in the body.
“Our AI-based prediction model will help spare patients who are unlikely to benefit from radiation treatment from the short and long-term side effects associated with exposure to that type of therapy,” adds Dr. Tran. n H




OCTOBER 15-17, 2024
TORONTO, CANADA




A significant impetus for bringing the conference to Canada is the country’s strong medical technology innovation environment, and we’re very excited about the interest shown by the Canadian MedTech sector. In fact, the MedTech Campus will feature a Canadian Pavilion – which had to be expanded due to overwhelming interest. In addition to the Canadian Pavilion, there are also off-site tours being planned to showcase innovation adoption, collaboration, and R&D opportunities in Canada.

With special discounted registration rates for the healthcare provider community, we would warmly welcome our partners in this
sector to join us at the conference to learn about the latest in medical technology innovations that can help you enhance patient care and address the health care challenges you face. It also provides a tremendous platform to network with MedTech innovators and discuss potential partnership opportunities.
We look forward to welcoming you at The MedTech Conference October 15-17 as we celebrate “Medtech in Motion” and explore new avenues for growth, innovation, and partnership.
Nicole Dekort is President and CEO, MEDEC Canada, Official Event Partner



TWO OPTIONS TO ATTEND:
Visit
themedtechconference.com/ register to learn more about our Hospital buyer registration options (for those that qualify)
HOSPITAL BUYERS
Must complete application
HOSPITAL AND HEALTH SYSTEM OFFICIALS
One Day Rate for $500




The MedTech Conference is the can’t-miss event where innovators from every part of the medtech industry come together to break through current limitations and showcase what they do best – put the future of health care in motion and ultimately keep patients moving.
The conference brings top industry executives and thousands of global innovators together in Toronto.
Medical devices, diagnostics, imaging and digital technologies are making a significant impact on the lives of people around the globe. These advances are being made by scientists, entrepreneurs, academics, investors, and an entire community of MedTech leaders and innovators.
The MedTech Conference is where innovators from every part of the MedTech industry come together to break free from current limitations and showcase what do what they do best – put the future of health care in motion… and keeping patients moving.
Network with thousands of MedTech professionals and discover innovative companies sharing next-level tech, explore our cutting edge education program, and connect with an incredible network of decision makers. Join us in Toronto, Canada, from October 15-17, with specialized programming on the 14th.
Visit themedtechconference.com for more information.
We believe that people can only live their healthiest lives on a healthy planet.
Leading Global MedTech Organization Hosting Toronto Event this October:


©2024 Medtronic.


n Access to global MedTech leaders. This unique gathering offering access to thousands of thought leaders MedTech leaders under one roof, including thousands of CEOs and MedTech subject matter experts and key decision-makers from around the world.
n Patient-centric solutions. The MedTech campus exhibit space features advancements that enhance patient care, improve accessibility and promote inclusivity in health care delivery.
n Global innovation. Innovators and entrepreneurs from the most recognizable companies from 40 countries and the most promising startups showcase their latest technologies here.
n Interactive company stages. The perfect setting for learning about groundbreaking

ideas that support the development of lifechanging technologies – and a chance to meet and network with more than 1,400 MedTech companies from 40 countries.
n Valuable insights. A carefully crafted MedTech program that covers critical industry topics and trends from leading experts.
n Investment opportunities. More than 200 qualified investors attend the conference to find breakout MedTech devices for potential funding.
n Network with Toronto’s research and innovation community. The host city is a hub for research and innovation, particularly in the field of life sciences and medical technology – and it is home to a vibrant venture capital and private equity scene, with numerous investors interested
in funding health care and MedTech startups.
There’s no better place to hear perspectives and gain valuable insight into today’s and tomorrow’s MedTech industry trends. Attendees can expect dynamic conversations focused on key topics, including artificial intelligence in health care, emerging regulatory and reimbursement pathways, the ways in which M&A activity is impacting health care delivery and wearable innovations for chronic condition management.
By examining the critical industry issues and opportunities in every facet of our field, we’ll enhance our ability to deliver solutions for the world’s ever-evolving health care needs.
STERIS is a leading global provider of products and services that support patient care with an emphasis on infection prevention. WE HELP OUR CUSTOMERS CREATE A HEALTHIER AND SAFER WORLD by providing innovative healthcare, life sciences and dental products and services. Our commitment is to help Customers solve their biggest challenges, leverage opportunities for growth, and advance the care of patients.
Every day, healthcare facilities of all sizes rely on the quality and assurance of STERIS. We’ve built our reputation by listening and delivering on the most critical infection control and surgical needs in clinical settings. STERIS brings this experience to Surgery Centres to provide a complete offering stretching beyond the Medical Device Reprocessing Area (MDRA), Operating Room (OR), and Endoscopy Suite. We partner to understand where you are today, create a plan together, and provide comprehensive product & service offerings supporting throughput for the OR, GI / Endoscopy and MDRA environments.
Designing your surgery centre can bring many challenges. Lean on our experience to help you optimize your facility for the highest productivity. Services range from simple equipment placement and single room layouts to entire department design, including OR, Endoscopy Suite, and MDRA design.
Maintenance & Repair Specialists. STERIS helps keep healthcare equipment operating at peak performance. Our equipment repair services minimize unnecessary downtime. From technical support to on-site trainings, our dedicated team of 100+ Service Technicians help you increase productivity and ultimately improve patient outcomes.
Supporting a Strong Department. Developing Future Leaders. STERIS University has you covered from point-of-use to storage and everything in between. Department Managers and Technicians learn current standards and best practices on Device Processing and Infection Prevention, while earning continuing education credits. Visit university.steris.com.
To learn more about how STERIS can help you, call STERIS Canada Sales ULC at 800-661-3937 or visit www.steris.com/healthcare-canada.

Elevate your endoscope reprocessing with the first and only automated endoscope reprocessor that provides Liquid Chemical Sterilization (LCS) along with a validated cleaning claim*.
Elevate your endoscope reprocessing with the first and only automated endoscope reprocessor that provides Liquid Chemical Sterilization (LCS) along with a validated cleaning claim*.
Efficient automated cleaning. Effective liquid chemical sterilization. Elevated infection prevention.
Efficient automated cleaning. Effective liquid chemical sterilization. Elevated infection prevention.
The enspire™ 3000 Cleaning and Liquid Chemical Sterilant Processing System. Endoscope reprocessing reimagined…for the highest standard of care.
The enspire™ 3000 Cleaning and Liquid Chemical Sterilant Processing System. Endoscope reprocessing reimagined…for the highest standard of care.
*Does not apply to duodenoscopes.
*Does not apply to duodenoscopes.
TO LEARN MORE ABOUT THE ENSPIRE 3000 visit www.steris.com
TO LEARN MORE ABOUT THE ENSPIRE 3000 visit www.steris.com


Tuesday October 15
12:00 pm–1:30 pm
MedTech in Motion:
Shaping the Future of Health Care Innovation
The landscape of health care is being transformed by advances in technology, artificial intelligence, and data analytics, revolutionizing patient care, disease management, and overall wellbeing. In this session, leading CEOs will share insights on the latest innovations and trends in MedTech that are reshaping the health care industry.
The Lifetime Achievement Award will be presented during this keynote.
Moderator:
Joanne Wuensch, Managing Director, Citi
Speakers: Peter Arduini, President and CEO, GE HealthCare
Michael Mahoney, Chairman and Chief Executive Officer, Boston Scientific
Roy Jakobs, CEO, Philips
Wednesday October 16
12:00 pm–1:30 pm
Champions of Resilience: Martina Navratilova and Chris Evert on Leadership, Rivalry and the Patient Journey
Join us for an inspiring keynote with tennis legends Martina Navratilova and Chris Evert. Renowned for their storied rivalry, they will share insights on leadership, resilience, and perseverance.
Learn how their competitive spirit and health challenges have shaped their approach to adversity.
FOR A FULL LIST OF HOSPITAL BUYERS AND PURCHASERS THAT ARE ATTENDING VISIT:
SPONSORED CONTENT
By Krista Balenko
Canada Health Infoway (Infoway) is an independent, not-for-profit organization funded by the federal government, dedicated to advancing digital health across Canada. Through the Shared Pan-Canadian Interoperability Roadmap (“Roadmap”), Infoway is leading efforts to achieve seamless and secure data exchange within the healthcare system. Recognizing the critical role of clinical leaders in this transformation, Infoway has launched the Infoway Centre for Clinical Innovation in Digital Health (CIDH). The CIDH aims to foster innovation and collaboration among healthcare professionals to accelerate the adoption of interoperable digital health solutions, ultimately improving patient
outcomes and modernizing healthcare delivery in Canada.
As its first major initiative, the CIDH introduced the Connected Care Innovation Grant, which aims to empower clinical leaders by providing project funding to advance grassroots initiatives focused on digital health interoperability. This year, ten recipients from across the country, including organizations in British Columbia, Alberta, Saskatchewan, Quebec, and Ontario, were awarded grants. Notably, three of these organizations serve Indigenous communities, emphasizing the need for and importance of improving healthcare delivery and access for diverse and underserved populations.
The awarded projects span a variety of healthcare settings, from commu-
nity clinics, hospitals and provincial agencies to universities and non-profit organizations. These initiatives are designed to enhance the delivery of care through the integration of advanced digital health technologies, ultimately improving patient outcomes and supporting healthcare providers in their daily practice.
Looking ahead, the CIDH will continue to support the advancement of digital health through the upcoming Connected Care Innovation Scholarship program, aimed at clinical learners who are pursuing further education in digital health interoperability.
By investing in our clinical leaders and students, we strengthen the backbone of our healthcare infrastructure,
ensuring that it can effectively adapt to evolving healthcare needs. The CIDH and its initiatives not only align with the strategic goals and priority initiatives of the Roadmap, but also aims to support clinicians at every stage of their career, empowering them to better care for patients and drive the modernization of Canada’s healthcare system in a way that meets their needs.
Through these initiatives, Infoway is committed to ensuring that healthcare providers have the tools they need to deliver connected, efficient, and patient-centered care across Canada. To learn more, please visit us at https://www.infoway-inforoute.ca or contact us at interoperabilty@infoway-inforoute.ca n H
Nov. 18-19, 2024
Jo in ind u st ry ex per ts and di g ital health leade r s to driv e inte rop erab ilit y and hel p
c ha r t the p ath for a healthie r s y ste m and a healthie r Canada .
Westin Ottawa Register now to secure your discounted rate!

Don’t miss this opportunity to hear from two of the greatest athletes as they discuss the essence of resilience and the patient journey.
Moderator:
Sally Jenkins, Sports Columnist, Washington Post
Speakers:
Martina Navratilova
Chris Evert
Thursday, October 17
8:15 a.m.–9:30 a.m.
FDA CDRH Town Hall
An exclusive peek into FDA’s Center for Devices and Radiological Health (CDRH) during the Thursday morning CDRH Town Hall. This is a rare
opportunity to interact directly with senior office leaders from CDRH. After they provide an update on the CDRH strategic plan and priorities, panelists will answer specific questions from the audience. Take advantage of this session and get answers to all of your burning questions directly from CDRH.
Moderator:
Janet Trunzo, Senior Advisor to the President and Senior Executive Vice President Technology and Regulatory Affairs, AdvaMed
Speakers:
Daniel Caños, Director, Office of Clinical Evidence and Analysis,
Office of Product Evaluation and Quality, Center for Devices and Radiological Health (CDRH), Food & Drug Administration (FDA)
Owen Faris, Acting Director, Office of Product Evaluation and Quality, CDRH, FDA
Jeffrey Shuren, CDRH Center Director Emeritus, Office of the Commissioner, FDA
Michelle Tarver, Acting Director, CDRH, Office of the Center Director, FDA
Troy Tazbaz, Director, Digital Health Center of Excellence, FDA



Canada’s AgeTech enthusiasts and leading minds in technology and aging are set to gather in Edmonton, Alberta, this October for the envisAGE Forum and AGEWELL Annual Conference. These premier events span research, innovation, and real-world application in the dynamic field of AgeTech in Canada.
Co-hosted by AGE-WELL and MEDTEQ+, the envisAGE 2nd Annual Forum will take place on October 23, alongside the AGE-WELL Conference. The envisAGE Forum focuses on the commercialization and integration of AgeTech solutions into practical benefits for older adults and caregivers.
On October 23 and 24, the 2024 AGE-WELL Annual Conference will navigate the theme of Shared Visions, Shared Futures: Transforming Aging
Together. Participants will explore the latest research and discourse on contemporary issues from global and Canadian thought leaders.
envisAGE forum keynote Christopher Kunney, an expert in health information technology and digital transformation, will offer insights into adopting new technologies.
Closing keynote speaker, Dianne Buckner, host of “CBC Dragons’ Den,” will share her expertise on turning ideas into reality, aligning with the Forum’s theme: Innovation in Motion for Quality Aging.
In a landmark collaboration in 2023, AGE-WELL, Canada’s primary network for technology and aging, and MEDTEQ+, a pan-Canadian consortium for industrial research and innovation in health care technologies, teamed up to focus on elevating Canada to the forefront of AgeTech. At the Forum, envisAGE

co-leads will announce the selection of the first eight collaborative projects to receive envisAGE funding, coaching, and support and launch the second call for innovations.
The two-day AGE-WELL Conference will conclude with the National Impact Challenge: Solutions for Healthy Aging, recognized for spotlighting stellar startups in the
AgeTech sector. Eager contestants from across the nation will pitch their innovative solutions, all geared towards enriching the lives of older Canadians and their caregivers.
The challenge winner, selected for their potential to make a positive societal impact, will secure $25,000 in cash alongside in-kind prizes to support the advancement of their enterprise.
These two AgeTech events provide delegates from many sectors with a unique opportunity to explore an ecosystem rich with expertise, networking and funding opportunities. Join a diverse group of participants including: researchers, academics, entrepreneurs, investors, health care leaders, older adults and caregivers interested in improving the quality of life of Canadians.
Learn more and register today! agewell-nce.ca and envis-age.ca n H
On October 23 and 24, the 2024 AGE-WELL Annual Conference will navigate the theme of Shared Visions, Shared Futures: Transforming Aging Together. The event showcases a multi-disciplinary program of research and innovation from across the country and provides a forum for networking and collaboration among partners.
On October 23, the envisAGE Annual Forum: Innovation in Motion for Quality Aging, hosted by MEDTEQ+ and AGE-WELL, will spotlight small and medium-sized enterprises (SME) and startup-driven innovation in partnership with health and community-based organizations.

October 23-24, 2024
Edmonton, Alberta
Early Bird Deadline: September 6, 2024
for just

We’ve reimagined the exhibit hall into an immersive, innovative experience designed for companies of all sizes and attendees from any background and career stage. The Campus transforms the traditional exhibit space into a vibrant, bustling hub where the future of MedTech comes to life.
Showcase your innovative technology in an exciting environment, generate buzz, and position your company among peers and competition. Experience cutting-edge innovations hands-on, network with industry peers, and enjoy surprise pop-up events.
Enjoy these exciting features of the Campus all week long:
n NEW! Tech in Motion Hub: Established companies showcase technology and product demos in an immersive area spotlighting diabetes, in-home & connected care, digital health and women’s health.
n CEOs Unplugged Stage: Hear candid commentary, insights, and expertise from top MedTech industry leaders.
n Innovation Pavilion: We’ve partnered with the NIH, etc. to bring you a dedicated space for startups and innovators to showcase new tech and network with potential investors and industry leaders.
n Career Hub: Providing the next generation of MedTech professionals a chance to experience the MedTech Conference through specialized programming, cultivated networking experiences, and direct access to MedTech companies.
n Exhibit Hall: Discover the newest in medical technology on the exhibit hall floor. It’s the perfect place to find part-
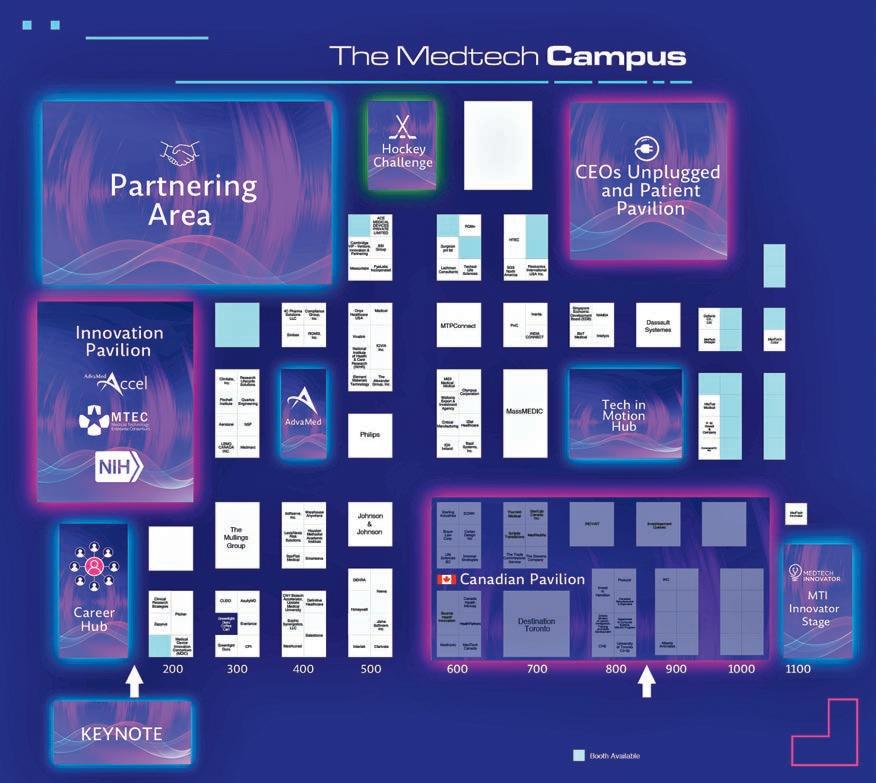
ners who share your vision and connect with businesses showcasing their latest innovations.
n Patient Stories: Hear firsthand accounts from patients whose lives were changed by the latest MedTech innovations.
n Hockey Challenge: Get ready to showcase your skills and compete in our exciting hockey challenge right on the Campus floor.
n MedTech Innovator Stage: Highlights the most innovative companies in sector-based sessions, presenting their technologies and value propositions, and moderated by leading corporate executives and investors.
n Efficient 1×1 Partnering: Schedule meetings and benefit from one-to-one matchmaking and arrive in Toronto with a plan.
1. NEW MedTech Campus: Discover the newest in medical technology on our newly revamped MedTech Campus exhibit. It’s the perfect place to find partners who share your vision and connect with businesses showcasing their latest innovations. Dive in, build meaningful relationships, and find tools to elevate your company’s journey in health care.
2. Networking & Connection: Daily receptions and networking breaks bring you together with distinguished professionals from across the entire MedTech landscape – investors, policymakers, academics, top executives and visionaries from promising startups. Make connections that will help you keep MedTech in motion.
3. Education: The 100+ cross-cutting sessions give you the opportunity to delve deep into key topics like digital health and artificial intelligence in health care; health
equity and climate change; supply chain disruptions and government regulations. You’ll find fresh perspectives and actionable insights to inform your decision-making.
4. MedTech Innovator Showcase: AdvaMed and The MedTech Conference are proud to partner with MedTech Innovator – the global competition and accelerator – so you can learn how the most innovative, emerging companies translate their desire to make a difference into solutions that transform lives. Explore details.
5. Investor Forum: The Investor Forum is tailored for discerning investors, offering curated content and bridging connections with emerging companies. Attendees have access to daily highlights, including plenary and panel discussions, plus networking events. Special sessions are also available, designed to cater to the needs and interests of investors. Explore the investor forum.
6. Partnering: The MedTech Conference is the perfect place to find your next gamechanging connection. Here, investors find innovative entrepreneurs, policymakers converse with CEOs about enhancing health care access, and like-minded companies come together. Join us and tap into our exclusive partnering program for personalized meetings with potential collaborators. Expand business development.
Visit themedtechconference.com/register to learn more about our Hospital buyer registration options (for those that qualify)
HOSPITAL BUYERS
Must complete application
HOSPITAL AND HEALTH
SYSTEM OFFICIALS
One Day Rate for $500

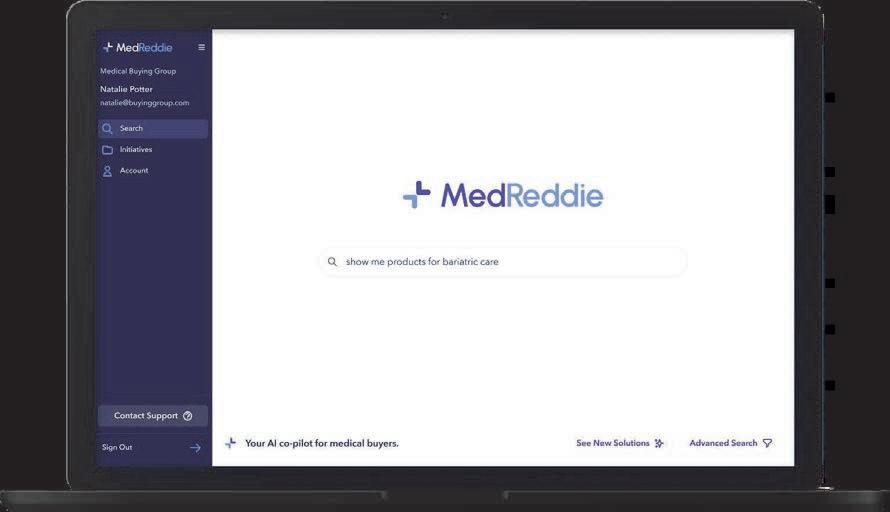

1. Partnering with health systems to overcome their biggest challenges: Shortages of healthcare workers pose challenges globally, with the results ranging from extended wait times, communication gaps, higher costs and care coordination issues. Even when enough staff can be found, training and established norms are often weaker than before the pandemic. For MedTech, traditionally focused on innovation and minimizing manufacturing costs, the industry is now presented with an opportunity to help be a part of the solution for one of the biggest issues facing healthcare. This panel will explore the ways in which MedTech is working with hospital systems to thrive in difficult times through use of AI and robotics, engineering simpler technologies, training surgeons and staff, developing labor-saving solutions to workflow
problems and helping support alternative sites of care delivery.
2. Navigating the Intersection: Digital Health Innovations and Market Access Strategies:
In this session, we will delve into the dynamic intersection of digital health innovations and market access strategies.
3. Unlocking Commercial Payer Reimbursement for Innovative Technologies The societal benefits of medical innovation are clear. Given the escalating complexity, cost, and resource needs of medical advancements, all stakeholders face financial headwinds: payers in controlling costs, hospitals staying…
4. Value Pathways for Drug/Diagnostic/ Digital Product Combinations: Innovators are increasingly looking to combine different types
For the list of the program, visit themedtechconference.com
of products to enhance their overall value. This can be drug delivery devices, drug diagnostic pairings or incorporation of digital tools.…
5. CMS' Goldilocks Dilemma With CED: Getting Their Coverage with Evidence Development Policy Just Right: CMS's controversial Coverage with Evidence Development (CED) policy has come under fire as a potential impediment to patient access. While many device companies arguably have benefitted from the policy's…
6. Navigating US Healthcare Reimbursement: Bringing Digital Health Technologies to Market: Digital technologies, including mobile medical apps, clinical decision support software, artificial intelligence, and machine learning, are transforming healthcare. With applications ranging from general wellness to medical devices, reimbursement strategies.








By Lijeanne Lee
It was a dramatic first for both the patient and his care team.
Just 27 days after arriving at UHN’s West Park Healthcare Centre, Yevhen Shlemkyvych, 21, a below-knee double amputee patient who had never walked, took his first steps.
And, for the rehabilitation care team – including a physiatrist, physiotherapists, rehabilitation assistants and prosthetists – it marked the first
time they treated a patient who had never experienced walking and had to be taught the mechanics such as using his knees and exploring a new range of motion.
“It’s really remarkable to see his progress,” says Dr. Steven Dilkas, physiatrist for Amputee & Musculoskeletal Services at West Park. “This is all new to him – being upright, putting on shoes for the first time and learning to tie his shoelaces.”
Growing up in Western Ukrainian, Yevhen was born with a condition that
rendered his legs unusable. At home and when he was out in public but thought no one was looking, he moved on his knees with pads for protection, dragging his feet behind.
With limited infrastructure in his village to accommodate wheelchairs, he was largely housebound.
Yevhen was advised to wait until he turned 18 to undergo a double amputation and be fitted with prostheses. But by the time that day came, the Russo-Ukrainian War prevented him from having the procedure.
After immigrating to Canada a year ago, Yevhen was referred to a surgeon, underwent bilateral amputations and arrived at West Park in May. Over the course of his stay, which ended earlier in July, he worked with West Park’s Amputee Rehabilitation and Prosthetics & Orthotics Services.
As Yevhen had never walked before, the rehabilitation care team had to explain the mechanics. They guided him through strengthening muscles he had never fully used, taught him how to utilize his knees and their range of
By Stephanie Hatzifilalithis, Rachel Savage and Paula Rochon
In an episode of the popular Netflix show “Grace and Frankie,” Frankie (played by the formidable Lily Tomlin) is navigating a world built for speed over safety alongside her friend Margaret, who is experiencing mobility challenges. Frankie and Margaret, as pedestrians in their later years, face the daily gauntlet of impatient drivers and short crosswalk signal times.
Frankie brings the municipal authorities out to reevaluate the timing of the crossing signal to make it more suited to older people and those with mobility challenges. While her advocacy on the show is successful, changes to Canada’s built environment are slow, few and far between.
It’s time Canada built cities and towns for an aging population. A thoughtfully and intentionally designed built environment can significantly impact the well-being and independence of everyone – especially older adults.
The World Health Organization’s (WHO) age-friendly cities framework highlights the need for features like longer crosswalk signals to make aging in the community easier and more accessible. A great example is Singa-
pore’s Green Man Plus Scheme, which prioritizes pedestrian safety.
Imagine a busy intersection. Those in need of longer crossing times can tap their regular transit card on a reader near the traffic light. That tap activates “Green Man Plus,” extending the crossing signal time. Over 1,000 crossings across Singapore are equipped with Green Man Plus, offering peace of mind for countless residents.
The good news is that Canada is moving toward the global trend of finding ways for older people to stay at home longer. The National Seniors Council of Canada recently released a report on supporting Canadians to age at home, recommending expanding support for age-friendly communities and investing in safe and innovative options designed to help older persons to age in their community of choice.
One opportunity for rapid advancement would be working with naturally occurring retirement communities – or NORCs for short. NORCs are geographic areas with a high concentration (typically 30 per cent or more) of people aged 65 and older.
In Ontario alone, an analysis done by the NORC Innovation Centre shows that there are an estimated 2,000 NORCs in high-rise buildings
that are home to 200,000 older Ontarians. This is more than the number of residents in Ontario’s long-term care and retirement homes combined.
NORCs with limited access to essential services, poorly maintained sidewalks and lack of benches and public restrooms on long stretches can discourage active participation in our communities.
In a recent paper published by Women’s Age Lab at Women’s College Hospital, we saw several neighbourhood-level variables associated with a significantly increased likelihood of long-term care home wait-list status. Without convenient and safe public transportation, community centres, parks, well-lit streets and walkable areas to public squares to encourage people to gather, loneliness and isolation rates are bound to rise with age.
NORCs present a unique opportunity for governments to act now.
Studies have shown a direct link between walkable neighbourhoods and increased physical activity, a reduced risk of chronic diseases and loneliness. By prioritizing age-friendly design features both inside and outside NORCs, we can enable residents to stay connected and at home longer.
It’s time we built our communities for all ages.
The eminent Professor of Geriatric Medicine, Bernard Isaacs, said, “design for the young and you exclude the old; design for the old and you include the young.” Investing in an age-friendly built environment isn’t just the right thing to do, it’s also economically sound. A well-designed physical environment can have a positive impact on health, lead to a decrease in healthcare utilization for older adults and aid independence.
The benefits of age-friendly environments are vast, from sparking creativity to strengthening communities and reducing healthcare costs. Such environments shape societies and cultures. It’s about creating change and vibrant geographic havens with accessible destinations where all residents can thrive.
The call to action is clear, as highlighted in a recent Toronto City Council Motion: we must prioritize universal design and utilize opportunities such as NORCs to adapt and modify Canada’s built environment. It’s about fostering a healthier, happier future for all with simple solutions like the Green Man Plus Scheme.
One tap at a time. n H
motion, and helped him find his new centre of gravity after his prostheses – which were fitted at West Park –significantly increased his height.
“It was hard. The prostheses were very heavy at first, but they seem lighter now,” says Yevhen, describing his first steps through a Ukrainian translator, Stefania Lehkyj, who was also one of his physiotherapists. “I knew over time, I would be able to walk.”
Wearing blue Saucony runners, his first pair of shoes, Yevhen is now able to walk and go up and down the stairs with two canes. With continued training, he looks forward to the day he can walk without aides.
Since his first step, Yevhen’s perspective on life has changed literally and figuratively. With his new legs, he is taller, which he says offers a much better view. Life opportunities are also beginning to open.

“With my legs, I feel normal,” Yevhen says. “I can be amongst people now. I can find a job.”
“With my legs, I feel normal,” says Yevhen Shlemkyvych, a below-knee double amputee patient who was fitted with prostheses at UHN’s West Park Healthcare Centre, learned to walk and took his first steps there. “I can be amongst people now.”
The West Park team has been in awe of his progress over the weeks and is optimistic for this future.
“It’s an inspiring story,” says Dr. Dilkas. “I’m thankful for what we do here, the team and all of their efforts.” n H
























































Exceptional processes and technology are essential to delivering exceptional quality healthcare – and Scarborough Health Network (SHN) is at the forefront of a significant technology transformation putting healthcare workers and its 850,000-strong patient population at the centre.
On July 1, 2024, SHN became the first Ontario hospital to launch the largest scope of health human resources (HHR) technology upgrades with an integrated suite of best-in-class technologies, in just 18 months. In what can only be described as the perfect blend of science and art, SHN leveraged a strategic vision and people-focused model to propel the organization forward as it builds on essential human capital management (HCM) solutions to support rapid growth and level up employee experiences.
The suite of software and hardware is impressive, including:
• Workday – powerful HHR application, which supports data tracking, employee accounts with individualized dashboards and information (i.e. payroll, benefits, etc.), talent acquisition and a seamless recruiting experience, managing access and compliance for learning and on improved employee experience;
• UKG – a flexible and functional, cloud-based solution for managing scheduling, timecards, pay, and accruals;
• UKG timeclocks – electronic time capture devices installed at key locations across SHN hospitals that support strategic scheduling and the automation of pay based on schedules; and
• Vocantas – a call-out system to support frontline shift coverage and manage absence reporting. Additionally, SHN has put in place a new Scheduling and Workforce Optimization Office to support staffing organization-wide. This team works directly with program and unit managers to strategically schedule hospital staff and fill unplanned gaps. The integration of these systems and structures is designed to stream-

line operations, improve workforce efficiency, and foster a supportive work environment that enables healthcare professionals to focus on what they do best: providing top-tier care to patients and families.
“Exceptional quality care starts with empowering the people who deliver it,” said David Graham, President and CEO, SHN.
“By optimizing HHR through artificial intelligence (AI) and machine learning technology, we are ensuring our people can devote more time and energy to compassionate and inclusive patient care, and setting a new benchmark for healthcare innovation in Ontario.”
This holistic approach to workforce management underscores SHN’s dedication to creating an environment where staff feel supported and valued, including improving their work-life balance.
“The integration of these innovative systems is transforming our care continuum, through ensuring optimal staffing levels to improving efficiencyempowering our people to focus on addressing the unique healthcare needs in Scarborough,” said Amanda Firth,
SHN’s Manager of Critical Care and HCM Change Champion. “By reducing manual and timely administrative labour to ensuring we have the right people, available at the right times, we can ultimately reduce wait times, improve patient satisfaction, and enhance overall patient outcomes.”
In today’s healthcare environment, trained professionals are in high demand and short supply. Anticipating the significant workplace growth needed to maintain the highest standards for quality and patient safety as Scarborough’s population evolves, SHN’s milestone project is setting the stage for its growing workforce with AI-driven recruitment tracking.
Recognized as one of Canada’s Most Admired Corporate Cultures in 2023, SHN is committed to building up its team of people. The new system design is directly aligned with SHN’s recruitment campaign, Where the World Comes to Work, which highlights Scarborough and SHN as places where diverse cultures, ethnicities, genders,
faiths and life experiences come together. Now candidates can easily filter their career interests, access SHN’s employee referral program, personalize job applications, and introduce themselves directly to the recruiter.
“SHN serves some of the most vulnerable populations in the country,” said Michele James, Executive Vice President, People and Transformation, SHN.
“Equity, diversity and inclusion are core to our recruitment strategy, and with the new Workday system, we will provide a better application experience for all applicants including those from diverse backgrounds who are excited to start their journey at SHN and make a difference in Scarborough.”
Over the last 50 years, Scarborough’s population, the Ontario healthcare system, and Scarborough’s three hospitals have all changed dramatically, a trend that is forecasted to continue well into future generations.
The strategic deployment of these HCM systems supports SHN’s ability
to adapt to the ever-changing healthcare needs of Scarborough, and builds upon the Network’s 2021 implementation of the Epic clinical information system and integrated MyChart Central East Ontario patient portal – in partnership with hospitals across the region. Together, these systems are empowering SHN’s people and teams with the tools they need to access real-time patient care and workforce information, promoting stronger collaboration across the region, and enabling patients to access their records and manage appointments as active partners in their care.
Ultimately, SHN’s investments into these best-in-class technologies are investments into quality, patient’s safety, and our people, the foundational pillars of SHN’s Strategic Plan 20242029. With the HCM implementation successfully underway, SHN is now focusing on optimizing the new technology to advance SHN’s award-winning corporate culture through achievable objectives across HR, talent, payroll and workforce management. n H
By Shauna Mazenes
It was almost two years ago, early in Dr. Klaudia Nowak’s medical career, that she received an urgent call in the middle of the night.
With a patient on the operating table and the surgeons standing by, she had 30 minutes to diagnose a sample of human brain tissue. Her conclusions could alter the course of brain surgery.
“Needless to say, I was quite nervous,” Dr. Nowak, a gastrointestinal pathologist at UHN, says of the diagnosis, which was made more difficult because the sample was frozen and distorted.
However, thanks to digital pathology, the biopsy was scanned and
CONVERTING GLASS SLIDES INTO VIRTUAL IMAGES ALLOWS FOR FASTER, MORE PRECISE DIAGNOSES. NOW, 29 NORTHERN ONTARIO HOSPITALS ARE GETTING ACCESS TO THESE SERVICES.
converted into a virtual image. Dr. Nowak sent it to a neuropathology colleague, the pair viewed it in real-time, and their diagnosis led the neurosurgery team to stop the procedure before it started.
This is just one example of the many ways digital pathology has revolutionized patient care at UHN.
Now, UHN, the first multi-centre hospital in Canada to fully adopt
digital pathology, is expanding it to 29 partner hospitals in Northern Ontario – giving these communities equitable access to enhanced laboratory medicine services.
“Digital pathology is bringing us to places we could have never even imagined five years ago,” says Dr. George Yousef, Medical Director of the Laboratory Medicine Program at UHN.
Continued on page 39


OCTOBER FOCUS: Mental Health and Addiction/Patient Safety/Research/Infection control:
New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
Annual National Infection Control Week (Oct.14-18) Supplement
Advertising Booking Deadline September 27th
Material Deadline October 1st For more info email advertising@hospitalnews.com

NOVEMBER FOCUS: Emergency Services/ Critical Care/Trauma/Emergency: Innovations in emergency and trauma delivery systems. Emergency preparedness issues facing hospitals and how they are addressing them. Advances in critical care medicine. Focus Emergency Care
Advertising Booking Deadline October 25th
Material Deadline October 29th For more info email advertising@hospitalnews.com


DECEMBER FOCUS: Medical Imaging /Year in Review/Future of Healthcare/Accreditation/ Hospital Performance Indicators: Overview of advancements and trends in healthcare in 2024 and a look ahead healthcare for 2025. An examination of how hospitals are improving the quality of services through accreditation. Overview of health system performance based on hospitals performance indicators and successful initiatives hospitals have undertaken to measure and improve performance. A look at medical imaging techniques for diagnosis, treatment and prevention of diseases. + SPECIAL FOCUS: ANNUAL RADIOLOGY SUPPLEMENT
Advertising Booking Deadline November 22nd
Material Deadline November 26th For more info email advertising@hospitalnews.com
By Fatima Hashemi-Sabet, Ziyi Xiao, Sheena Ye, Uroosa Abbas, and Certina Ho
JJ.S., a 55-year-old female, presented to her oncology clinic for her third cycle of chemotherapy. During a routine consultation, she mentioned that she had been taking antioxidant supplements (Vitamin C 1000 mg, Vitamin E 400 IU) daily, recommended by a friend, to “boost her immune system” and combat any chemotherapy side effects. While antioxidant vitamins, such as Vitamin C and Vitamin E, are generally considered safe, their use (or potential overuse) during chemotherapy raised concerns for J.S’s oncology healthcare team.
Chemotherapy is a commonly used term for cancer treatments that do not involve surgery or radiation. Many chemotherapy drugs can be described as “cytotoxic” which translates directly to “toxic to living cells”. Cancer is a disease in which cells of the body undergo uncontrolled growth, harming the body. In cancer treatment, cytotoxic agents are used for their toxicity to kill these fast-growing cells. However, non-cancerous or “normal” cells are also at risk of experiencing toxicity, which can be manifested as side effects of chemotherapy, for example, hair loss, vomiting, diarrhea, and the development of mouth sores.
Antioxidants are nutrients that help fight damage to our cells. The way that cells process oxygen results in the production of unstable molecules, called free radicals, which can damage our cells and DNA. Over time, a build-up of free radicals may lead to diseases, such as cancer. The body’s cells can repair or prevent free radical damage by naturally making antioxidant enzymes and
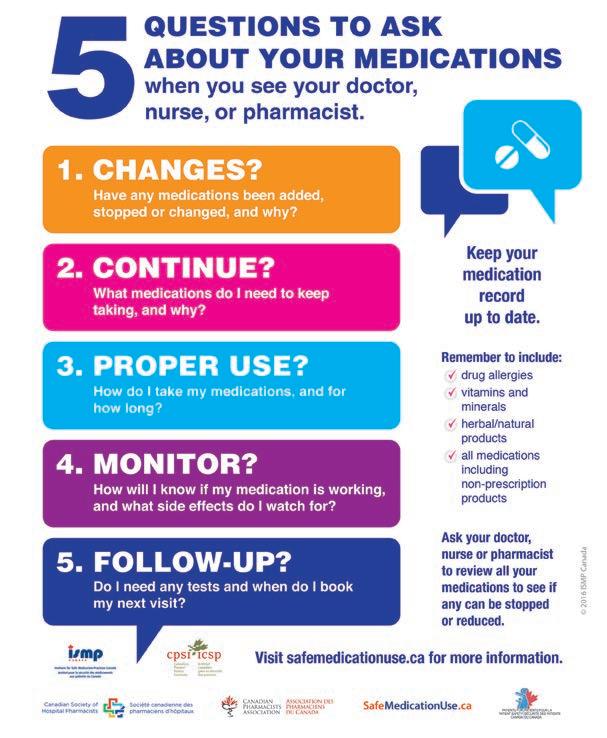
consuming antioxidants from a variety of food sources. Some of these common antioxidants include Vitamin C, Vitamin E, and Selenium. Overall, antioxidants help protect our cells from the daily damages they face.
Current research shows that the action of antioxidants may not translate into long-term benefits during cancer treatment. The side effects of antioxidants, including interactions, may be difficult to predict as there is no
standardized dose or specific type(s) of antioxidant(s) that are recommended alongside the use of chemotherapy. On one hand, patients treated with chemotherapy that reduces the patient’s antioxidant levels may require antioxidant supplements after treatment. Antioxidant supplements may reduce the frequency and severity of side effects associated with chemotherapy. Therefore, it is possible that antioxidant use might facilitate the administration of higher and more effective doses of certain types of chemotherapy. However, it is important to note that with-
in the context of different types/stages of cancers, various chemotherapy agents may have different effects and impacts on the antioxidant levels in a patient’s body. For example, Bortezomib, an anticancer medication that is used for multiple myeloma (cancer associated with a type of white blood cells), interacts with the antioxidant components in green tea, which may inhibit the therapeutic efficacy of Bortezomib, leading to ineffective cancer treatment.
As the recipient of care, patients should always consider the five questions to ask about their medications (see Figure 1)) during a clinical encounter with their healthcare providers. Patients should always be well informed of their medications, including vitamins, supplements, and natural health products. They can discuss and ask their pharmacist or healthcare team about their vitamins, supplements, and natural health products. This can help their healthcare team identify potential interactions and manage them appropriately.
With regards to J.S., her healthcare team discussed the possible interactions between high-dose antioxidants and chemotherapy; and advised her to stop the supplements. Dietary levels of antioxidants are considered safe during chemotherapy and cancer treatment. It is important to maintain a healthy and well-balanced diet. J.S. is recommended to focus on a balanced diet with natural antioxidants from fruits and vegetables, which will provide a safer, more moderate level of antioxidant activity without interfering with her cancer treatment.n H
Pathologists, the doctors who diagnose cancers and infectious diseases, have traditionally done so by examining a biopsy on a glass slide under a microscope. In digital pathology, glass slides are converted into virtual images on a computer screen, allowing for faster, more precise diagnoses while eliminating the manual work of a microscope.
In the past, if a general pathologist needed a second opinion from a specialist they didn’t have, the glass slide would have to be shipped in the mail to the appropriate hospital for analysis. This process could take weeks, with the possibility of the slides breaking with the biopsy in it, posing serious safety risks.
Now, Dr. Yousef says, the flexibility of digital pathology can bypass geographic barriers around the world, speeding up consultation and diagnosis from weeks to days, days to hours, or even hours to minutes.
Bringing the infrastructure for digital pathology to Timmins Cluster Lab Services Program, Kenora Rainy River Regional Laboratory Program and the Sault Area Hospital – an initiative called “We The North” –will give more remote communities access to UHN’s specialized pathologists, which acts as an effective solution to the understaffing challenges particularly prominent in these areas.
Northern expansion will not only enable faster diagnoses, but better metrics and data for communities that have been historically underrepresented in medical research.
The Lake of the Woods Hospital in Kenora recently began stocking new medications in their pharmacy to treat diseases that are common in the community – something Dr. Nowak says is a direct result of the high-quality, detailed pathology reports from UHN’s Laboratory Medicine Program.
“It’s amazing how we can collaborate with our northern partner sites to bring about change in the manner patients are treated,” says Dr. Nowak, who serves as the Anatomical Pathology Director for the Kenora Rainy River Regional Laboratory Program.
“We can now use AI to significantly improve our capabilities and take patient care to the next level, something we call precision medicine,” Dr. Yousef says.
AI can help identify specific genetic disease patterns in biopsies and eventually develop algorithms to predict the best course of treatment for the patient based on their condition, he says.
Dr. Yousef adds that having access to digital files of human biopsies allows for the full engagement of a multidisciplinary team in a patient’s treatment plan, which wasn’t previously possible in pathology. Now that everything is electronic, he says, oncologists, pathologists and surgeons can sit down together and have a complete view of everything related to the patient.
“It truly is a new era of pathology – a holistic approach to patient care,” Dr. Yousef says.
For Dr. Rumina Musani, digital pathology is more than just teamwork. For her patients, it can make the difference in a life and death situation.
“The ability for technologists to communicate immediately with pathologists can save lives as far as leukemia goes,” says Dr. Musani, a pathologist specializing in hematology at UHN.
One of the most urgent diagnoses hematologic pathologists face is called acute promyelocytic leukemia. A patient may be hemorrhaging all over their body and can die if they don’t start treatment immediately.
Dr. Musani remembers being a young pathologist on call and having to physically go into the hospital in the middle of the night to make that and other urgent diagnoses, trips that wasted valuable time. She adds that biopsies or blood smears aren’t always easy to read and often don’t present how they do in the textbooks.
“Not being able to access second opinions back then were very scary, high-pressure situations,” she says.
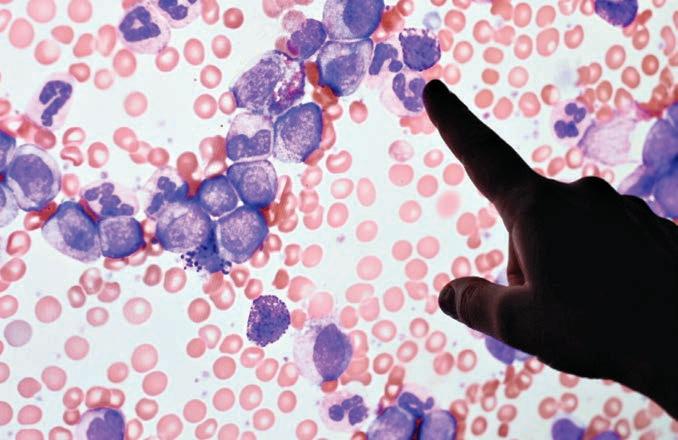
She adds it’s a big step for hospitals in Northern Ontario, who didn’t previously have access to specialized hematology pathologists.
“It’s really a good feeling when you’re able to find something that was missed, but to know you also helped save a patient’s life,” she says.
UHN is looking ahead to even bigger collaboration and recently signed with the Mayo Clinic to expand digital pa-
thology into the United States. The next step is expansion in Israel and Brazil.
However, Dr. Yousef says digital pathology is a very expensive innovation that needs philanthropy to keep moving forward.
“We’re leading the way in Canada at UHN, but the idea is to create a global hub for digital pathology,” he says.
“International collaboration will help build the case.” n H
Shauna Mazenes works in communications at University Health Network.

Artificial intelligence (AI) also plays a key role in digital pathology, making diagnoses faster and more precise than the human eye.
Now, being able to get a high quality second opinion in urgent cases is not only critical for safety of the patient, but for the development of a young pathologist, she says.
“Being able to consult your colleagues builds confidence,” says Dr. Musani. “Being alone creates fear.”