OU SURGERY: AN ENDLESS EVOLUTION








In our Spring/Summer issue, we share the incredible basic science, translational science, and clinical innovation our department faculty are contributing to academic surgery. As the field of surgery evolves so does our department and we highlight the amazing accomplishments since the beginning of this year.
We are constantly striving to improve and innovate which keeps us at the forefront in the world of surgical advancements.
Finally, I would like to congratulate our graduates who will continue OU surgery’s legacy as they begin their fellowships and practices
Thank you for your interest in our newsletter and I hope you find it informative.
Barish H. Edil, MD Professor & ChairTo learn more about the University of Oklahoma and the Department of Surgery, visit https://medicine.ouhsc.edu/Academic-Departments/Surgery

The Department of Surgery contains many divisions including:
Cardiac, Thoracic & Vascular Surgery
General Surgery, Trauma
& Critical Care
Pediatric Surgery
Plastic & Reconstructive Surgery
Surgical Oncology
Transplant Surgery
Education Research
To improve the health of all people, to deliver excellent innovative patient care, advance the science of medicine, and to educate physicians and surgeons for the future.


Administration
BarishH.Edil,MD Professor/Chair
JessicaCapetillo
Executive Assistant & Senior Administrative Manager
WarrenChurchill,MBA,CPA Senior Clinical Business Administrator
HeatherDees
Lead Accountant
NikkiKnaggs Business Analyst
MarySheets Senior Accountant
ElisabethSlay Media Coordinator
LisaSuriano
Senior Clinical Department Business Manager
PiperBrown Surgery Scheduler
AcademicClinicalFaculty
HaroldBurkhart,MD Professor/Division Chief
KlayBuckley Clinician Educator
JoshuaGierman,MD Associate Professor
LacyHarville,MD Assistant Professor
LaurenHerget
Perfusionist Pediatric Cardiac
MeganHolmesPA-C Clinician Educator
AlexHickey
Perfusionist Pediatric Cardiac
ConstantineIonan Clinician Educator
MichaelMassoni Clinician Educator
YukiNakamura,MD
Assistant Professor
EdRaines,MD
Adult Cardiac Surgeon
J.MatthewReinersman,MD
Assistant Professor
JoniSchroeder,PA
Clinician Educator
BerkeleyStevens Clinician Educator
CarmenTaylor,APRN Clinician Educator
DavidVint Clinician Educator
EmilyWilhelm,APRN Clinician Educator
AcademicClinical SupportStaff
JenniferBurks
Administrative Manager
KristenEarnhardt
Staff Assistant Pediatric Cardiac Surgery
ShellyJones
Financial Coordinator/Administrative Assistant
NashonaRagland
Administrative Manager
CrystalTaylor Resident Coordinator/ Administrative Assistant
GeneralSurgery/ Trauma/CriticalCare
AcademicClinicalFaculty
RoxieAlbrecht,MD
Tenured Professor of Emeritus
Ann-MarieAlexander,PA Clinician Educator
GraceBedford,NP Clinician Educator
IrynaBilga,PA Clinician Educator
ScottBlair,DO Assistant Professor
MaryMargaretBrandt,MD Professor
AmandaCelii,MD Assistant Professor
AlisaCross,MD Associate Professor
MeganCuoco,PA Clinician Educator
MarielleDelRosario,PA Clinician Educator
LauraFischer,MD Associate Professor
KenzeeGambrell,PA Clinician Educator
JasonLees,MD Interim Division Chief
FernandoMier,MD Assistant Professor
CeliaQuang-Blair,MD Assistant Professor
AlexanderRaines,MD Associate Professor
AshleyRichey,NP Clinician Educator
JessiSiler,PA Clinician Educator
EmilySkinner,PA-C Associate Professor
CarleeSteele,NP Clinician Educator
CaitlinStenberg,APRN Clinician Educator
JacobSteverson,PA-C Associate Professor
RonaldTaylor,PA-C Clinician Educator
RachaelThies,NP Clinician Educator
FrankWood,MD Assistant Professor
AcademicClinical
SupportStaff
LeslieMasse Administrative Assistant
BrookeTheriault, Administrative Assistant
AcademicClinicalFaculty
CatherineHunter,MD Professor/Division Chief
JeremyJohnson,MD Associate Professor
AlessandraLandmann,MD Assistant Professor
CameronMantor,MD
Professor/Vice Chair of Operations
NikolaPuffinbarger,MD Associate Professor
AlexRuiz-Elizalde,MD Associate Professor
StephanieScofield Clinician Educator
SupportStaff
SherrySpence Administrative Assistant
SusanCloer
Financial/Administrative Coordinator
AcademicClinical ResearchSupportStaff
CamilleSchlegel,BS Staff Research Assistant
Plastic& ReconstructiveSurgery
AcademicClinicalFaculty
SuhairMaqusi,MD Associate Professor/Division Chief
GuilhermeBarreiro,MD Assistant Professor
ChristianEl-Amm,MD Professor
MarkMims,MD Assistant Professor
NicoleOwens,NP Clinician Educator
ErinPoole,NP Clinician Educator
AcademicClinical
SupportStaff





JasmineAshford Administrative Assistant
YolandaBoyer Administrative Assistant





 Transplant Surgery
Transplant Surgery

S U R G E R Y
V A S C U L A R
C A R D I A C
T H O R A C I C

 Story
Story
and photo by Elisabeth Slay
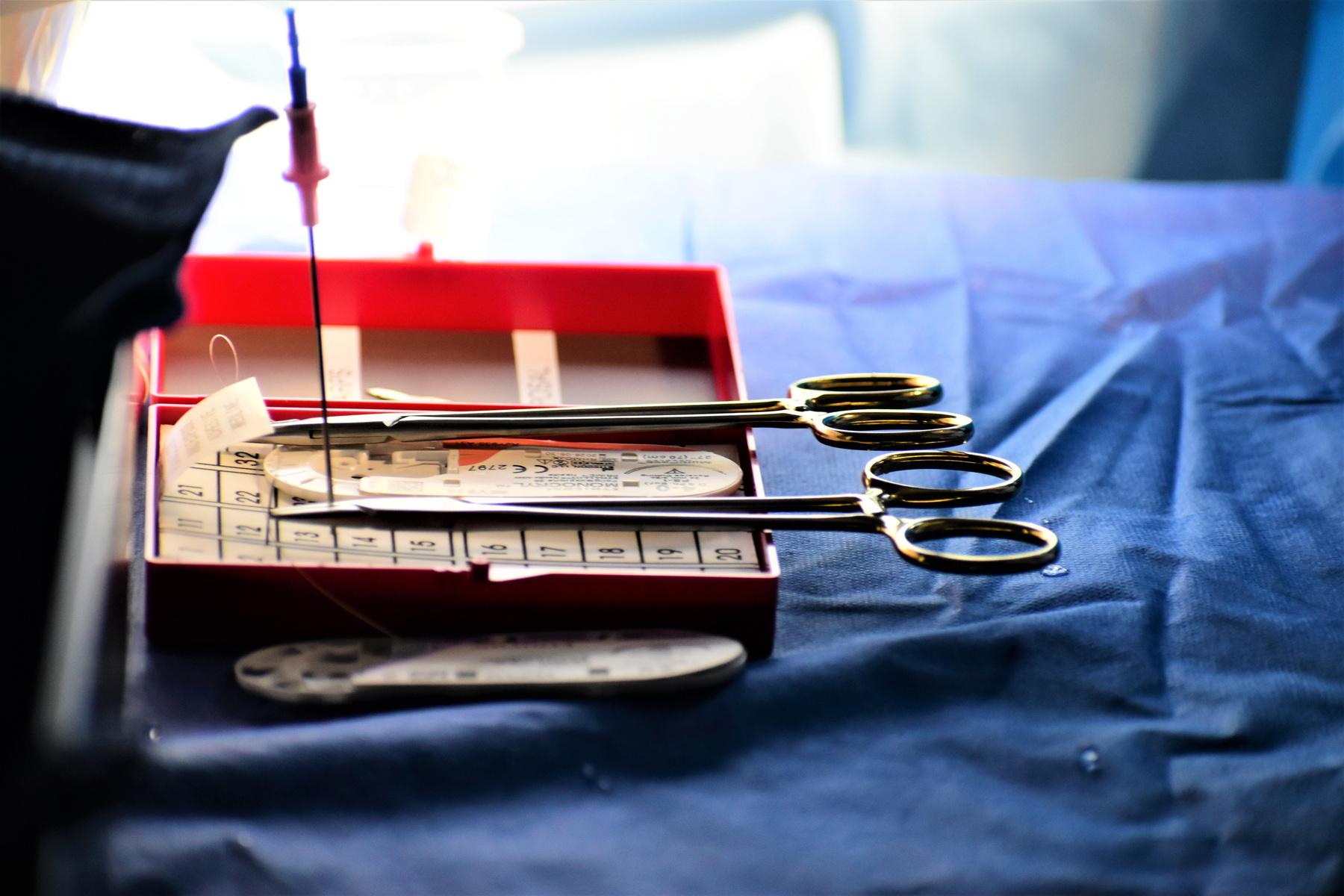
“It’s pretty different compared to what we’ve used in the past Basically, it’s for patients who have lung nodules that are a concern for lung cancer,” Dr Reinersman said “It allows us to biopsy the nodules when they’re smaller ”
He explained it’s often difficult to biopsy these nodules as they’re in challenging areas to operate on or too small to accurately biopsy forcing surgeons to wait until the nodules increase in size
“We were limited to having radiologist biopsy the nodules from the outside where they put the patients in a CAT scan and put a needle in the patient from the outside and that can be successful if the nodule is on the outside of the lung but if it’s deeper there’s a higher risk of complications,” he said
Thoracic & Cardiovascular Surgeon Dr. Matthew Reinersman can better navigate the depths of the lung with Intuitive’s new robotic-assisted bronchoscopy platform: the Ion Endoluminal System.These complications include bleeding or hemothorax which is when there is air outside of the lung in between the lung and the chest wall “The risk of that happening with the Ion, because we do it through the inside of the lung, is much lower and we’re able to do the biopsy and potentially stage their lymphoid,” Dr Reinersman said
Staging is when a pathologist determines if cells are cancerous and biopsies allow the surgeons to determine how far the disease has spread in the body if the cells are positive.
By utilizing the Ion, Dr Reinersman explained pathologists have the ability to give him “real-time results” and then the surgical team can “use a different scope and look at a” patient’s lymph nodes, and “potentially get the diagnosis and the staging in one anesthesia ”
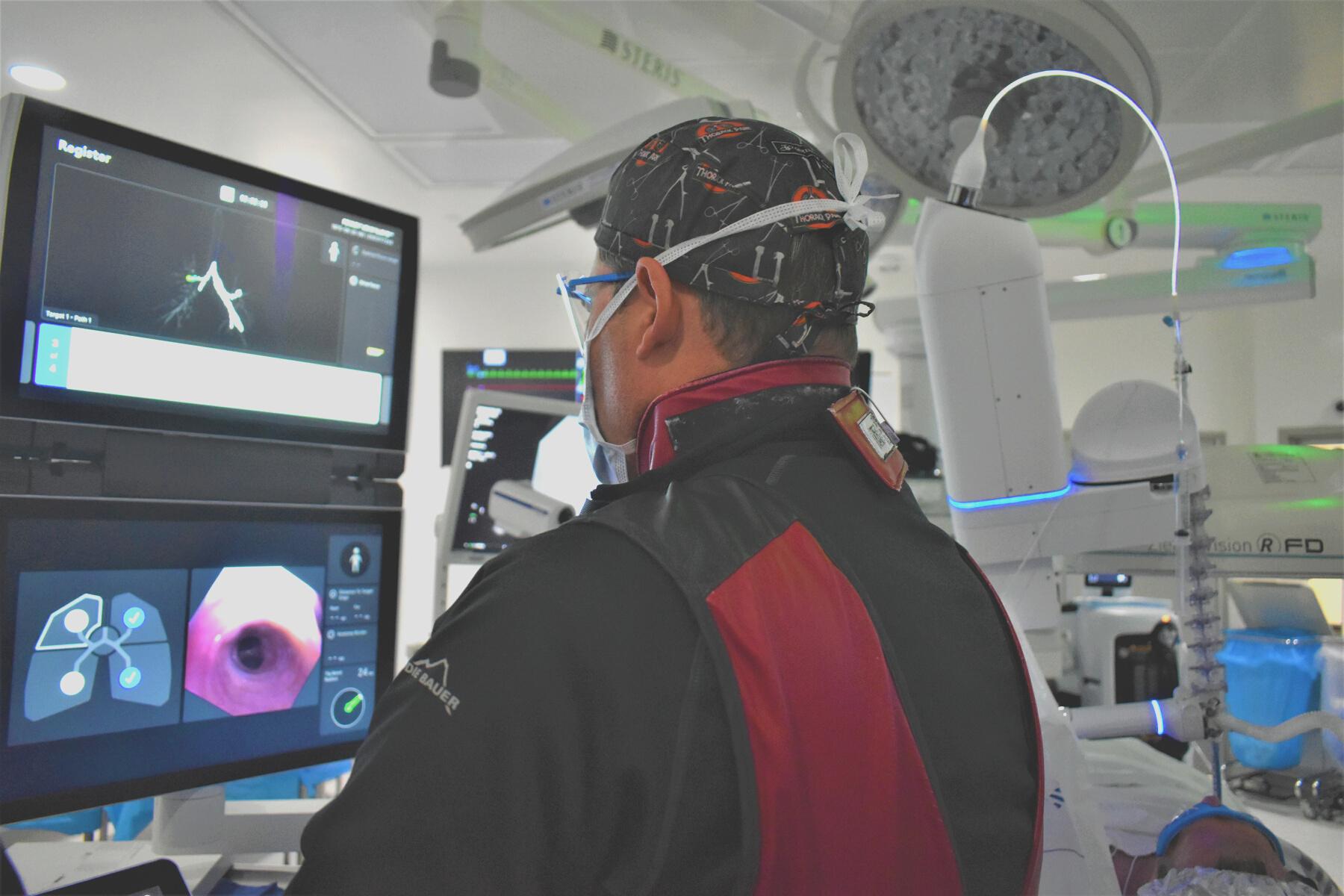
Essentially the Ion is a rolling cart with numerous screens and a control panel attached to an arm that connects to a patient’s body through a treaclier tube. The arm is magnetically connected to the treaclier tube and there is a camera attached to another arm that navigates through the patient’s body The camera is controlled by a portable panel connected to the system

“What we do is we get a CAT scan of the patient and we load that into a special computer and we generate a map of the inside of their lungs to the nodule,” Reinersman said. “It’s basically a GPS roadmap and the Ion creates a plan of which pathway to go down to get to the nodule inside the lungs.”
When a clear path is determined, Dr Reinrsman explained the map appears on the screens of the Ion as a three-dimensional image of the patient’s lung and the nodule “We used to do an electromagnetic navigational biopsy which would generate a magnetic field and you’d have to have the operating room mapped out a certain way,” he said.
This technique was useful for certain nodules but made it difficult to resect a nodule if it was deep within the lung “In that case, you’d have to remove the whole lobe which would be problematic especially if it turns out it’s not cancerous,” he said Dr Reinersman explained the Ion was acquired about two years ago.
The electromagnetic navigational biopsy only had a 65 percent success rate.
"We’d be taking these patients to determine through a biopsy if they had lung cancer and it was frustrating because you could determine it more than half the time but that’s not enough and we were putting people through potentially unnecessary procedures.”
The Ion is more precise and efficient than an electromagnetic navigational biopsy. The technology is just so fascinating with the Ion because the way the other ones worked is that you were limited on a standard bronchoscope,” he explained.
“A standard bronchoscope isn’t very long and it’s big, so it can only go about a third of the way into the airway So, then these systems would give you a roadmap but you’d only see so much, and then you’d have to hope you were going down the right pathway to the nodule.”
With the Ion, Dr. Reinersman explained he has better access to a visual of the lung and the pathway to the nodule
“The camera is under robotic control so you can drive it all the way to the edge of the lung,” he stated. “So, it’s really a huge revolutionary step forward in navigating inside the lung and getting to pathology.”
To learn how to use the Ion, Dr Reinersman said one should already have knowledge of performing bronchoscopies.
“For the most part here at OU we have it so that the only persons that can get credentialed to use it are those who’ve completed a thoracic surgery fellowship or have completed an interventional pulmonary fellowship,” he said “So, you need a lot of extra training and Intuitive sends you to a special course.”
In this course, trainees learn how the machine works and then perform practice procedures on pigs. In total, there are about 30 hours of extra training to learn how to use the Ion.

“It surprises me how far you’re able to get out into the very edge of the lung,” he said. “And just how powerful it is to be able to get anywhere in the lung and be able to biopsy something that is less than a millimeter in size.”
Dr. Reinersman is amazed at how much access the Ion gives to a patient’s lung and the detailed images of any nodule no matter the size.
“My hope is that it will allow us to be on the forefront of innovation when it comes to lung cancer and allow us to be recognized nationally or internationally as a center that is involved in these advances early,” he said “It’s unique for surgeons to do this ”


G E N E R A L
T R A U M A
C A R E
C A L
C R I T I
To further the effort of endless evolution at the University of Oklahoma Health Sciences Center Department of Surgery, Trauma and Critical Care Surgeon Dr. Amanda Celii has led the implementation of the Whole Blood Program into the General Surgery, Trauma, and Critical Care Division
Dr. Celii explained the OU Whole Blood Program is the first of its kind in Oklahoma and one of a few in the entire nation.
“When Trauma patients are bleeding, we have to give them components of blood, so packed red blood cells (PRBC), fresh frozen plasma (FFP), platelets, and Cryoprecipitate (Cryo) to help give them blood back and stop additional bleeding from coagulopathy,” she said “We have to keep the ratios very balanced, however with whole blood, we can give our patients more blood before it’s been broken down into its components, so it has everything in one unit.”

Originally whole blood usage was p military during the 1970s and 1980 said.
However, the practice fell out of fav component therapy, or the act of b whole blood into its components, in
According to Blood Bank Medical D Hope Hastings, whole blood was cr limited use because of incompatibl it has returned as a practical treatm
“The unique factor for low titer O w that donors are specifically tested f anti-B titers, so only those donors w considered ‘low titer’ are eligible to specialized blood product,” Dr Has “Due to the low antibody levels, it is utilized across different ABO types
Getting this product to patients in the early stages of treatment has improved the survival rate and decreased the need for additional blood transfusions Dr Celii added

The program started over a year ago and Dr Celii said in that time she, Dr Hastings and others involved in the program’s development have honed their criteria for whole blood usage and further built the program.
“This past November we partnered with the Emergency Medical Services Authority (EMSA) to start a rotational system so they can carry whole blood pre-hospital to administer to trauma patients even before they get to the hospital,” Dr. Celii states.

The surgeon and her team meet monthly to discuss the program’s whole blood usage, wastage, and all cases to ensure safety protocols are followed In the last year, the program has had only four units of whole blood wastage, Dr. Celii added
At a conference in San Antonio, Texas, Dr. Celii learned about whole blood programs and their implementation She worked alongside OU Health’s Blood Bank and with Dr Hastings “We wouldn’t have been successful without Dr Hastings’ support and help to build this program and this team over the last year and a half,” Dr. Celii added.
Dr. Hastings stated the Blood Bank worked closely with the trauma team to determine how to use low titer O+ whole blood and change their process for our high-risk trauma patients
“Because this was a completely new product to OU Health, we had to build it from the ground up in the blood bank, which includes building and validating it in the laboratory information system, writing policies, purchasing and validating coolers, training the blood bank staff, and working with the Oklahoma Blood Institute to determine how and when we would receive

the product,” Dr Hastings explained Dr Celii feels this program solidifies the department as an innovative leader in trauma
“I hope to continue its expansion to more prehospital providers and agencies so that we can have whole blood reach our rural areas to help improve the survival of our rural trauma patients,” Dr Celii said
The Blood Bank and the trauma team will continue to collaborate with each other and additional entities to improve patient care
“Without the teamwork, the program would not have been successful,” Dr. Hastings said. “The trauma team goes above and beyond to minimize wastage and excel at blood stewardship Our blood bank staff works tirelessly to assist in the care of some of Oklahoma’s most critically ill patients ”
The medical professional feels the Whole Blood Program has completely changed the way in which adult trauma patients receive blood at OU Health.
“Low titer whole blood has been a huge success for Oklahoma Seconds saved truly save a life,” she said


L D C A R E
I N F A N T A N D C H I
S U R G E R Y
R E S E A R C H
The advancement of child medical care both in and out of the operating room are a priority in the Pediatric Surgery Division at the University of Oklahoma College of Medicine
Division Chief Dr. Catherine Hunter was awarded a $2 5 million R01 grant in April from the National Institutes of Health for her research regarding necrotizing enterocolitis (NEC). This prestigious award will run for five years.
NEC affects 5-10 percent of all babies in the neonatal intensive care unit. It is thought to occur as a result of an immature gastrointestinal tract and abnormal patterns of bacterial colonization. In its most severe forms, it carries an 80 percent mortality rate
In addition to our clinical work, we study NEC in our research laboratory
We have been fortunate to have received support from the Oklahoma Adult Stem Cell Research Institute as well as the Children’s Health Foundation We have developed a human enteroid model, which is a mini sphere of the intestine that I can grow in a test tube to study the disease,” she said “We use many high-end molecular techniques to better our understanding and drive the field forward to find a cure for NEC ”

Dr. Hunter explained she and her collaborators have worked to try and cure NEC “We’ve had fabulous collaborations here and we’ve worked very closely with the Division of Neonatology within the Department of Pediatrics,” Dr. Hunter said There have been other researchers who have also recently received NIH funding in this realm at Oklahoma Children’s, which provides the Division with terrific momentum Dr. Hunter explained.
“We are truly taking a multidisciplinary approach. I think this work has the potential to have a hugely positive impact on our patients and teams,” she said “NIH funding is less common in the state of Oklahoma compared with some other locations, so it’s very exciting to get these types of awards for our state as well as for our division, department, and hospital.
Dr. Hunter stated she and her colleagues will continue to move the Pediatric Division toward the future. “We have a responsibility to provide the best care to our patients locally and regionally but I think especially with some of our research work this allows us to impact entire patient populations and have a voice on a national platform which I think is pretty exciting,” she stated.
In April of 2023, Division Chief of Pediatric Surgery Dr. Catherine Hunter became the first surgeon-scientist within the University of Oklahoma College of Medicine Department of Surgery to receive an R01 grant from the National Institutes of Health.
Dr Hunter was awarded a $2 5 million grant for her research on the molecular pathogenesis of necrotizing enterocolitis (NEC) and neonatal sepsis
NEC is an abnormal response to bacteria in the gastrointestinal tract that typically impacts premature babies.
“Our central hypothesis is that the response of the intestinal barrier in premature infants to injury is altered and is characterized by changes in epithelial ROCK signaling, aberrant tight junction regulation, increased inflammation, sepsis, and epithelial cell death,” Dr Hunter said
Dr. Hunter explained this grant will help fund this research which will be conducted in her lab on campus. “Our major goals are to test this hypothesis by determining whether inhibition of tight
 Story and photo by Elisabeth Slay
Story and photo by Elisabeth Slay
junction protein expression and redistribution or caveolin-1-mediated endocytosis prevents paracellular permeability increases, inflammatory responses, and epithelial cell death in experimental sepsis and NEC,” she said.

According to Department of Surgery Chair Dr. Barish Edil, Dr Hunter composed various articles that established the foundation of the grant “I found these articles to demonstrate elegant work and vision as she continues to study this disease process that impacts the neonatal population,” Dr Edil stated
Dr. Hunter has researched NEC for several years and hopes the grant will serve as a means to help develop a better understanding of the disease’s function.

“The grant will be used to continue to drive the field forward and try and identify why some babies develop NEC as well as to try and prevent this disease,” she said
Dr Hunter explains that it is important to learn as much as possible about NEC so she and others in her specialty can develop better treatments and preventive measures against the disease.
“I research this disease because it affects about five percent of all of our newborns in the Neonatal Intensive Care Unit And of those that get NEC, up to 80 percent require surgery Sadly, even after having everything possible done, there can be negative outcomes including death or resultant short gut syndrome,” Dr Hunter said
Dr. Edil explained it is a great accomplishment to receive the type of funding Dr. Hunter was awarded.
“Dr. Hunter is a wonderful example of a physicianscientist,” Dr Edil said “An R01 is an amazingly difficult accomplishment that takes years of work; many strive for it, but a small minority of surgeons achieve it ”
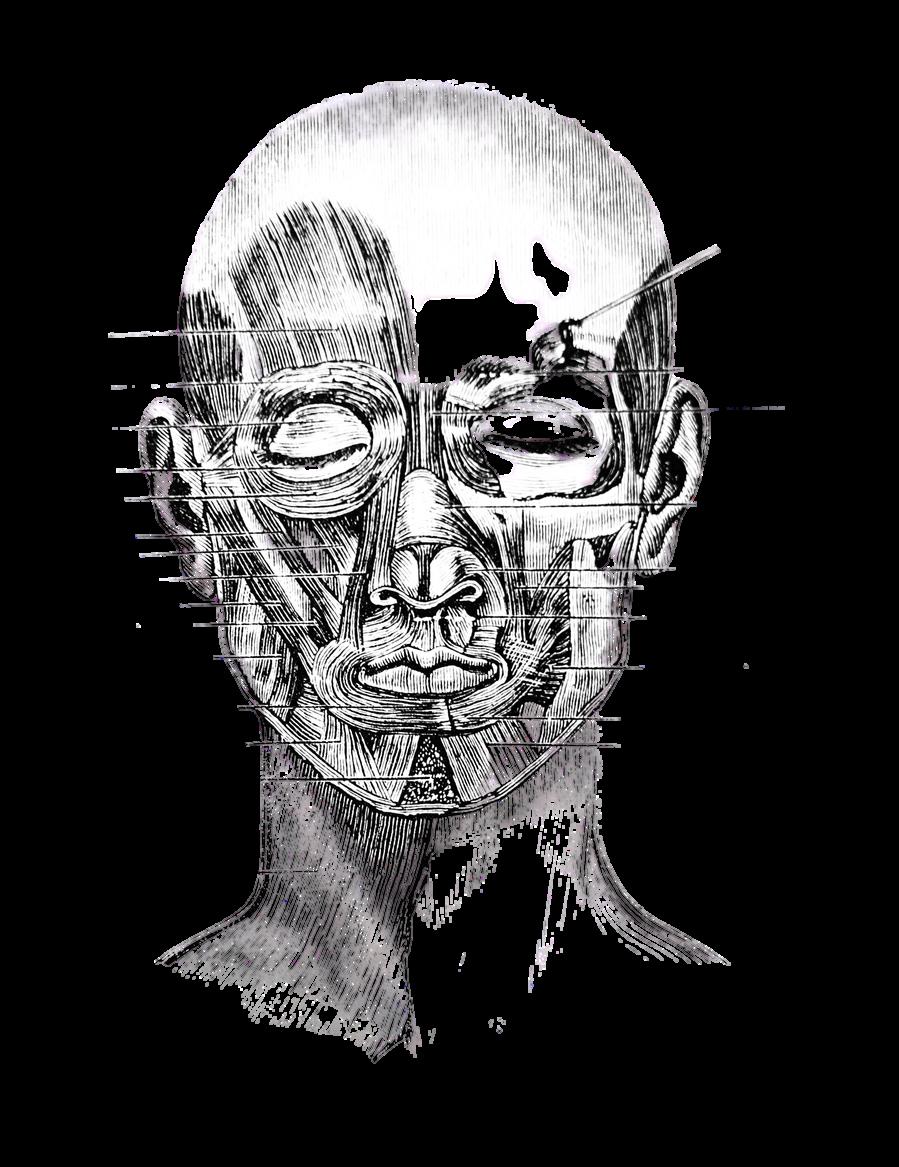
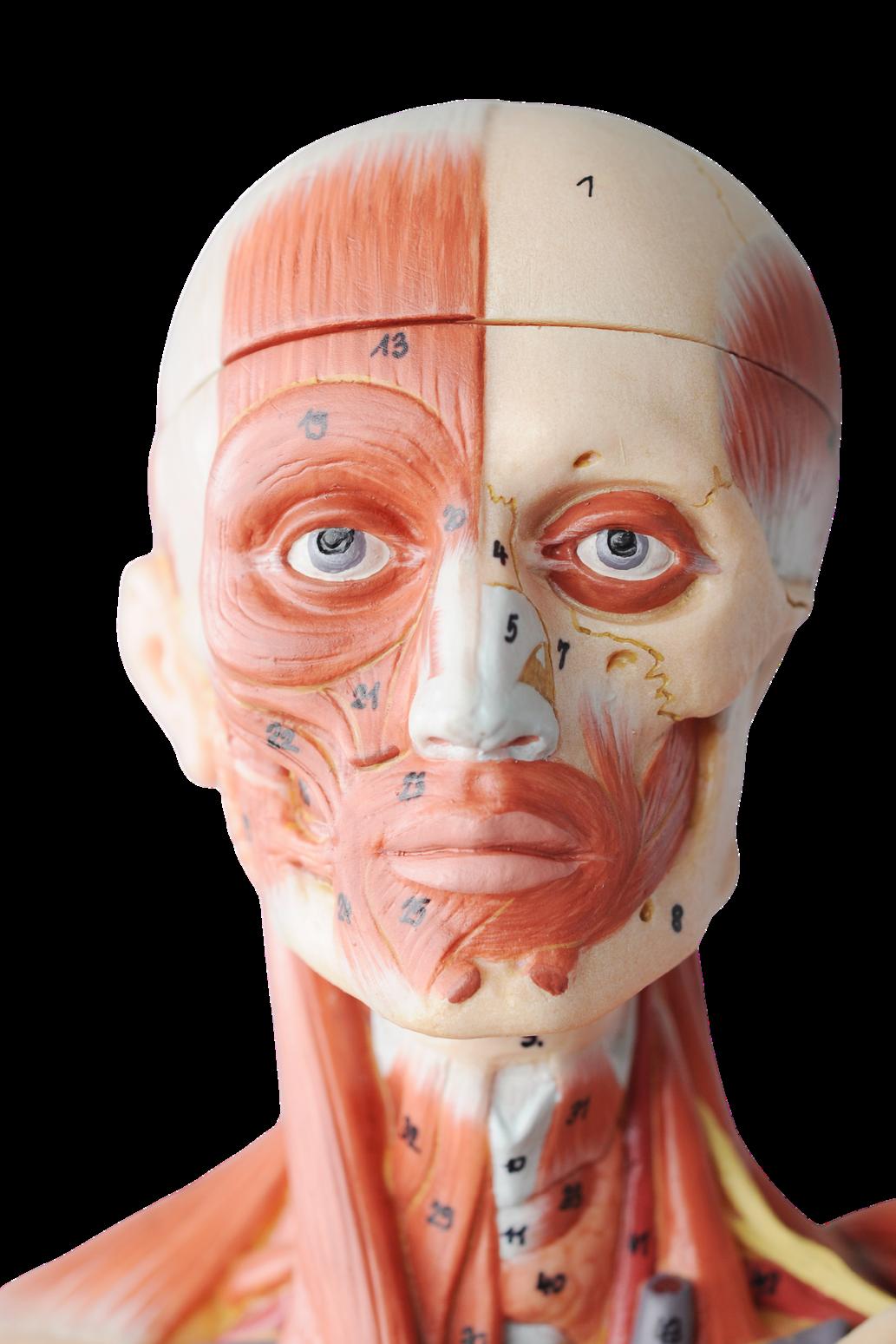
Through the eyes of the Surgical Enhanced Visualization System (SEViS) surgeons access CT Scan imaging directly overlaid on a patient’s body, making it easier to prepare for difficult operations.
According to Pediatric Plastic Surgeon and co-creator of SEViS, Dr. Christian El Amm, the SEViS system is housed in a pair of goggles that allow surgeons to see detailed images of any part of a patient’s body, including the bones, muscles, organs, and blood vessels
“The device is part of what’s being called augmented reality in surgery or extended reality and what we have done is turned it into a navigation software to assist surgeons with their surgeries and procedures,” Dr. El Amm said.
Dr El Amm explained this technology helps providers better perform their surgical tasks as they have quicker access to medical data

“Instead of pausing surgery and turning to the computer monitor and training to pull up what they need the surgeons have what they need right there in front of them using just a voice command,” Dr El Amm said.
The device is operated through voice command technology, similar to Siri, and rather than needing a controller, the operator of the device simply uses hand motions
“The surgeons wear the headset during surgery and the headset can be flipped up or down when needed It does not obstruct your view like the traditional Virtual Reality goggles,” he said.

Inspired by the original basic mapping technique surgeons use when determining where to make incisions, SEViS provides opportunities for precision, accuracy, and safety

“So far in cranial facial surgery we’ve found it to decrease the injury to major blood vessels in the brain and it may decrease the amount of blood loss in surgery,” he said. “That’s what we’re studying.”
In the last year, Dr El Amm explained the use of SEViS expanded to other specialties including Trauma and Critical Care and more
“It may help trauma surgeons find and fix rib fractures using smaller incisions. For General Surgery the goggles may help with liver procedures. For Urology, they may help with tumor procedures and tumor resections. For Anastasia, they may help with the performance of nerve blocks," He stated
Additionally, the medical professional explained SEViS can be utilized in Neurosurgery with challenging tumors and Orthopedic Surgery with hip reconstructive surgery
SEViS originally began as a research project in 2018 and the concept was further developed in 2019.
“We had a working prototype in 2020-2021. In 2022 we started expanding its use in other specialties,” Dr. El Amm said.
Dr. El Amm and others in the Craniofacial Imaging Lab have been researching and developing new imaging tools since 2006
“We did three-dimensional modeling, threedimensional simulations, and studies on 3D scans,” Dr El Amm said “Then it expanded to 3D printing and virtual reality models ”

In 2016, when augmented reality technology was more accessible Dr El Amm and his team discussed developing a virtual surgical planning system.
“In 2018, with the help of Dr James Tomasek, who supported us with a grant for a collaborative study with Baker Hughes, an initial prototype was created Then we spent another year and a half in the lab developing it,” Dr El Amm stated
Xironetic, a company started by Dr. El Amm and others, is licensing the patented technology, and the Imaging Lab is always updating and advancing the SEViS.
“We’re always developing ideas but the main ideas come from the surgeons who tell us how to use it,” he said. “The surgeons ask the questions and then the technology finds the answers.”
Since the expansion, Dr El Amm explained SEViS has been used in 100 different operations
As the department continues to gather data and a better understanding of the device, Dr El Amm and his team feel optimistic the technology will become more of a helpful tool for other specialties
“The SEViS goggles are helping make surgery faster, safer, and better for patients,” Dr. El Amm said.
A new initiative.
Story by Elisabeth Slay Archived photoIn collaboration with various organizations, OU Health started an initiative in May in which head and neck surgeons from Ukraine are invited to learn about different surgical techniques from Oklahoma reconstructive surgeons

According to reconstructive surgeon Dr. Mark Mims, the purpose of this initiative is to supply Ukrainian surgeons with the tools to provide quality care to those injured in the ongoing war and the nation overall.
“Currently in Ukraine, there are over 13,000 injured civilians and soldiers, many with devastating head and neck injuries,” Dr Mims said “At this time, Ukrainian surgeons do not have the training to manage these severe injuries ”
The American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS), Razom for Ukraine, and INgenius are working together with OU Health to bring Ukrainian neck and head reconstructive surgeons to the University of Oklahoma Health Sciences Center to train for a month
Initially, Dr Mims explained, the AAFPRS humanitarian organization Face-to-Face was doing one to two-week mission trips to Ukraine to treat the worst of civilian and soldier injuries
“However, we have identified the need to provide more sustainable and locally-based expertise in order to better treat these patients,” Dr. Mims said. “To
accomplish this, we at OU are the first U S center to pilot a formal educational program that will bring Ukrainian surgeons for an in-depth training experience in complex head and neck reconstructive techniques ”

Ultimately the main goal of this project is to create “a paradigm shift in how complex head and neck injuries are treated in Ukraine,” Dr. Mims explained
The medical professional has followed the war in Ukraine since it began and was inspired by “the strength and resiliency of the Ukrainian people in the face of such adversity,” he stated.
“For those that have read the reports or seen the photographs of the horrific injuries and conditions they have experienced, it is impossible to not be drawn to find ways to support efforts in their war-torn country,” Dr Mims said “I consider myself very fortunate to be in a position where I can contribute through this initiative.”
The surgeon explained he was the only one to volunteer to create a program such as this after the idea was proposed by Face-to-Face surgeons at the AAFPRS meeting in September of 2022
So far, three surgeons from Ukraine have participated in the program Two of the surgeons are from Kyiv Regional Hospital and one is from Chernihiv.
“Four more surgeons from Western Ukraine will come at the end of the summer or early fall We hope this will become a recurring experience until we can train enough surgeons that they will be able to provide internal training within Ukraine,” Dr Mims said The surgeons will train at OUHSC for a month.
One to two half-days per week they will participate in proctored cadaver dissections covering free tissue transfer techniques as well as other head and neck reconstructive techniques,” Dr Mims stated “These sessions will be led by faculty members in ENT, plastic surgery, OMFS, and oculoplastics ”
He also said that Kerecis is providing a four-hour training in their product in the cadaver lab. When the surgeons aren’t in the cadaver lab, they will be observing live cases in the operating room. They will also round with the team on these cases to see how initial postoperative management is performed Dr Mims explained the first three surgeons chosen to participate in the program were selected by members of the Fact-to-Fact team during their missions in Ukraine.
“We are currently working on an application process that would allow any Ukrainian surgeon to apply to participate in this program,” he said “We hope to identify those surgeons who will have the biggest impact not only in patient care but also in the ability to train other Ukrainian surgeons ”
According to Dr. Mims, this project is e by donations both monetary and in-ki provide housing, transportation, cell p training expenses for the surgeons, to barrier to entry for them,” Dr Mims sa
We have had a very generous donor w seed funds, allowing us to take the pr ground.” To maintain the program, the funds will continue to be raised throu events, social media, and additional o “Companies such as Leica, Stryker, Ke have provided in-kind donations, inclu instrumentation and biologic products “We are also collaborating with non-go organizations such as Razom for Ukra to help cover costs of airfare and other needs ”
The hope for the program is to help Ukrainian surgeons become independent in “the practice of complex head and neck reconstructive techniques,” Dr Mims said

“This will allow their patients across the country with extreme head and neck deformities to receive the care they need to restore them to a better quality of life,’ Dr Mims said “We also hope to foster a long-term relationship with the surgeons and the centers where they work so that we may collaborate in future clinical and research activities ”
Dr. Mims would like to thank those collaborating on this project including the surgeons, the department chairs, the media and marketing team, philanthropy, the cadaver lab staff, and the administrative roles for their assistance and hard work in making this initiative a reality
For more information regarding the project contact Dr. Mims at mark-mims@ouhsc.edu or visit https://giving.ouhealth.com/helpshealukraine.



Department of Surgery Surgical Oncology Division is advancing the field of medicine in various ways, including technology, surgical services, and clinical and basic science research
According to Division Chief Dr. Ajay Jain, the evolution of the Division came to a head in 2019 when it was officially recognized as an extension of the Department.
“Before there were surgeons, but as a division, we now have very specialized expertise,” Dr. Jain said. Dr. Jain explained there are various branches of the Division each one providing an enhancement to the treatment and care of cancer patients
After becoming a National Cancer Institute in 2016, receiving a National Accreditation Program for Breast Cancer in May, and its National Rectal Cancer Program of Excellence Accreditation in February, the Division has become a leading cancer program dedicated to furthering advancements in surgical oncology.
“
We over the last decade have really started offering minimally invasive colon surgery and rectal surgery with the (Da Vinci Surgical System) and treatment of metastatic disease that presents at the same time or after primary colorectal cancer,” Dr. Jain said. Dr. Jain explained that the ability to offer minimally invasive surgeries decreases mobility, infection, metastases, and other complications “Two-thirds of patients with colorectal surgery will go on to develop metastases
Our program enables us to treat the whole patient including treatment for liver and lung metastases,” Dr Jain said In February, the Surgical Oncology Division received its National Rectal Cancer Program of Excellence Accreditation “We are the only one in the state of Oklahoma and in a multi-state region to have this accreditation,” Jain said “It means we offer the highest standard of care for rectal cancer ” According to Dr Jain, the greatest tool in the evolution of the Division is research.
Dues to all its accreditations and specialty services, the department extends beyond medical services and has the ability to conduct various forms of research including clinical trials. “As a cancer program, we have more pancreatic cancer R01-funded research than any program in the country,” Dr. Jain said.
The use of robots in a surgical setting was initially theorized in 1967, but it would take another 30 years for the first fully developed multipurpose surgical robotic system to be created Currently, the most common and available surgical system is “Intuitive Surgical Inc.'s Da Vinci Surgical System, which is found in operating rooms across the globe,” including the OU Department of Surgery.

In 2000, the Da Vinci Surgery Center became the first robotic surgery system approved by the FDA. According to Colorectal Surgeon Dr. Steven Carter, the Da Vinci is “a surgical system that basically allows us to make small incisions and have three-dimensional viewing with wrist articulation that allows us to do really complex surgeries that we could not do with the laparoscope before ”
Dr Carter explained that the Da Vinci is specifically useful for deep pelvic surgery The medical professional said he was one of the first surgeons in the Department to utilize the Da Vinci and the first robotic surgery performed at OU was around 2014.
Story and photo by Elisabeth Slay"(Robotic surgery) has really taken off in the last five years,” Dr. Carter said. “Initially we were doing a handful of robotic surgeries here and there but now with all of us I think we’re doing more in a week than we would have done in a year back in 2014.”
Various surgeries are performed with the Da Vinci including hernia repairs, complex pelvic surgeries such as ileoanal anastomosis or j-pouches, esophagectomies, gallbladder repairs, and more.

Currently, there are about seven Da Vinci Surgical System machines utilized by the Department of Surgery Dr Carter said the department has the latest model of the system which is about five years old
There are numerous ways in which the Da Vinci has improved the medical field but perhaps the most beneficial is the postoperative treatment of patients.
Dr. Carter explained surgeries performed in the past would have a week’s worth of recovery time for patients whereas now patients “wake up the next day and go home It’s just amazing,” Carter stated
Prior to the invention of the Da Vinci and other robotic surgical systems, Carter explained the use of the laparoscope made it difficult to perform complex surgeries. “The old fashion way was laparoscopy and you really couldn’t do anything in the pelvis area well.”
The Da Vinci, however, enables a surgeon to make small incisions and have positive resections and successful cancer surgeries “It lets the patients wake up with just little poke holes and it’s a really nice surgery,” Dr. Cater said.
Those utilizing the Da Vinci are able to structures, nerves, and other areas of the body that aren’t accessible during open surgery. “It’s just amazing,” Dr. Carter said
Surgeons use this device to operate and control the

Medical professionals who work with the Da Vinci spend a considerable amount of time training and learning how to operate the various parts of the machine.

Dr. Carter explained doctors are required to take a course in which they learn the inner workings and uses of the robot “You have to be an expert in your (practice) and then you go to the course to learn how the machine works and safety stuff and then you do surgeries with a proctor ”
Practice makes perfect when becoming acquainted with the Da Vinci. “You have to do surgeries on your own several times to become really proficient at it,” Dr. Carter confirmed.
These days, Dr Carter explained, the training process for the Da Vinci is simpler as residents have opportunities to utilize the machine in during their residency and eventually become experts on the robot through that hands-on learning.
“Now we teach them how to do it and they are so much more advanced than we are,” Dr Carter said. Dr. Carter explained the Da Vinci is on a rotating boon that moves fluidly throughout the operation.
“There are arms on the robot and it connects to these ports that go in the patient’s abdomen,” Dr Carter said “There’s a console in the room and you can sit at it and control all these arms while you’re in the console ”
Dr. Carter is an expert on the use of the Da Vinci Surgical System as he has completed around 400 different surgeries with the machine.
“The patients just do better It’s the difference between waking up with a two-foot incision on your stomach versus six eight-millimeter incisions It’s a dramatic change,” Dr Carter said
L I V E R A N D K I D N E Y

In 2022 the University of Oklahoma Health Sciences Center Transplant Division reached a record high for the number of transplants it performed
According to Division Chief Dr. Tomasz Kozlowski, last year was the best year in organ transplantation across the country.
“We transplanted more than 42,000 patients which is a record high for the United States in the history of organ transplantation,” Dr. Kozlowski said. “That reflects a record high of transplantation at the OU Health Transplant Institute.”
Dr. Kozlowski said the division transplanted 97 organs which is a first for the division “Fifty of those 97 transplants were liver transplants which is also a record high number with absolutely outstanding outcomes,” Dr Kozlowski said.

The medical professional said the division also received its recommendation letter from the Organ Procurement and Transplantation Network for its advancement and sustainable outcomes in liver transplantation for the last two years.
“The program expanded and we have a designated transplant pharmacist and a dietitian,” Dr Kozlowski said Additionally, the program has been active in various communities and maintained relationships with other hospitals in the country
“We put OU Health Transplant Institute on the map of transplant centers,” he said “We have more referrals for instate and out-of-state patients ”
Hepatology is the study of liver diseases and after a loved one experienced liver difficulties of their own, Dr Sidra Ahsan became a hepatologist and now works for the University of Oklahoma College of Medicine Department of Surgery.

“Hepatology is a very wide field. It has a lot of pathology and physiology as well. It’s any disease that affects the liver whether it be acute liver conditions or chronic liver conditions it can be metabolic disturbances,” she said
Dr Ahsan explained in the United States and specifically in Oklahoma, many liver issues are caused by alcoholassociated liver disease.
“At the same time, we’re also seeing a lot of patients with NASH which is nonalcoholic steatohepatitis which can also lead to hepatitis but with the medications available we are seeing less hepatitis now,” Dr Ahsan said
The medical professional explained many patients with NASH don’t know they have the condition. “They are not aware and it’s related to a lot of lifestyle choices, genetics, diabetes, and obesity So those are the main patients that we are seeing,” she said “At the same time, we see a lot of patients with Hepatitis B and Hepatitis C, and other diseases ” Dr Ahsan has a personal connection to hepatology that inspired her to join the field and work with those who suffer from liver conditions.
“I lost my father to Cirrhosis He was an orthopedic surgeon and he never knew he had Cirrhosis,” she explained “He had NASH and he was a diabetic at the age of 40 and when he retired at the age of 67 he had Upper GI bleeding and that’s when we found out he had NASH and later on he passed away from complications.”
The hepatologist finds her work extremely rewarding and enjoys the many different elements of the profession “With the surgical component, the role of the hepatologist is to complete the evaluation of a pretransplant patient,” she said “For transplant surgery, we work with our surgical colleagues to evaluate the patients from the medical standpoint.

At the same time, we take care of these patients in the acute phase and manage their medical conditions while they’re being evaluated for a liver transplant.”
Additionally, Dr. Ahsan said she assists patients who might already have certain liver conditions to maintain their symptoms and prevent them from developing into worsened conditions She also works with patients after their transplants and helps them maintain their health
“I find it very rewarding that a lot of patients can get a second chance at life for themselves and also for their children and family,” she said. Since 2021, Dr. Ahsan has worked with surgeons and patients at the University of Oklahoma.
“I think working together with our surgical colleagues has been really beneficial for the program and for us For us hepatologists, we can manage a disease medically but the cure for Cirrhosis is a liver transplant,” Dr Ahsan said Both components work together to provide the best care they can for liver disease patients Dr Ahsan explained


Clinical PGY3 Surgical Resident Dr Isabel Dennahy was awarded the Association for Academic Surgery /AASF Trainee Basic Science Translational Research Award and a $30,000 grant for her proposal "Novel Imaging Techniques in the Diagnosis and Treatment of Pancreatic Cancer.”
“What we’re going to be working on is developing a florescent targeted dye specifically for pancreas cancer cells, with the idea that it can be used intraoperatively to detect areas where the cancer is still present to guide resection,” Dr. Dennahy said. The surgeon explained she was inspired to pursue her proposal based on her passion for pancreatic cancer treatment and Vice Chair of Academic and Research Advancement Dr Lacey McNally’s similar studies in breast cancer
“You attach a fluorescent dye to a specific protein that will target the cancer cell,” she said “First, we need to make the protein ” Dr Dennahy will conduct her research in Dr McNally’s lab. “In her lab, there is a peptide synthesizer. You input all of the amino acids in the correct proportions to make the protein and then it synthesizes it and then you go through several steps to process it and clean it up,” she said.

"The most potential for growth."
Dr Dennahy explained that once the protein is created she will attach a CW-800 fluorescent peptide-based target dye to create the imaging technology
Following that process, Dr Dennahy and Dr McNally will begin a testing series to ensure the target marker accurately targets cancer cells in the pancreas.
“First, we are going to test it on a pancreas cancer cell line. Then, we will test it in cell lines from other organs to confirm that it binds to the pancreas and not as much in other organs so we’ll know it’ll have a good signal in one area and not the whole body,” she said.
Next, Dr Dennahy will test different lengths of the protein to see which one has the strongest signal The resident will then select the best protein and test it in cultured pancreas cancer cells from actual patient tumors and make sure that it binds well in an actual patient tumor as well as cell lines

“No one tumor is the same, and there are often differences even within the same tumor So, this will be the next step to show our protein withstands those differences,” she said. After the cell testing, Dr. Dennahy explained she will begin the next phase of testing her markers. “We’re going to be testing the markers in mice and we’re going to be doing that using a model where you inject the sample of the tumor into the mouse’s pancreas and it develops there. Then we’re going to give the mouse the marker,” she stated.
According to Dr Dennahy, things work really well in cells, but when put in the body there are many other factors to consider including the distribution, the blood supply, etcetera Should the dye become a successful marker for pancreas cancer, Dr Dennahy explained it could be used with various forms of imaging existing technical systems such as the Da Vinci Surgical Systems
“The Da Vinci Surgical Systems have the Firefly Feature which we currently use in gallbladder cases with a different kind of dye,” she said. “The dye that we’re developing now will be usable with the same technology.
Additionally, Dr Dennahy’s marker will be compatible with multi-spectral optoacoustic technology (MSOT) The resident explained that the purpose of this study is to prevent unnecessary operations or guide surgical resection to provide better care for pancreatic cancer patients “If we’re successful with what we’re doing, eventually this could be used preoperatively to get a much better idea as to whether these patients are operative candidates,” she said.
Dr. Dennahy feels pancreatic cancer research is an area with some of the most potential for growth and positive results in advancing treatments. She explained how imaging now can’t accurately differentiate between treated cancer and live cancer after patients have had chemotherapy
“That really affects whether or not those people should get an operation, or the kind of operation that would best for them,” she said The resident explained for those who need an operation this technology would help the surgeons limit how radical their resection is Dr Dennahy is especially grateful to her mentors.
“I think when I have someone as supportive as Dr. Ajay ”





S C I E N C E


Those in the Research Division of the University of Oklahoma Department of Surgery study various types of cancer According to researcher and professor Dr Min Li, his team is dedicated to studying pancreatic cancer pathogenesis and the development of new therapies to treat patients.
“Our research covers early detection, molecular mechanism, and targeted therapy of pancreatic cancer,” he said “Current projects in the laboratory include the role of zinc transporter ZIP4 in pancreatic cancer progression, the therapeutic potential for ZIP4 shRNA, the function of microRNAs in ZIP4-mediated tumor growth, signaling transduction and metabolism in pancreatic cancer, and cancer cachexia “
Dr. Li explained his group is the first to identify a key zinc transporter called ZIP4 which is “aberrantly expressed in pancreatic cancer, and promotes tumor growth, epithelial-mesenchymal transition (EMT), and metastasis, suggesting that ZIP4 serves as a novel prognostic and predictive marker for pancreatic cancer." The researcher has conducted various research projects through the years and his team’s most recent findings suggest ZIP4 promotes muscle wasting and cancer cachexia
"Also known as rapid conditioning, Dr Li said cachexia is a dysfunction in the body that causes uncontrollable weight loss independent of nutritional supplements
“Muscle wasting, adipose loss, and loss of appetite (anorexia) are prevalent in those patients. Cachexia is associated with multi-organ dysfunction and increased mortality,” he said “Currently, no effective treatment options have been approved to reverse or ameliorate cancer cachexia Novel therapeutic targets and treatmen strategies are urgently needed ”
Dr. Li explained pancreatic cancer has the highest prevalence of cachexia more than any other form of cancer. “Our recent study, Acetyl-Coenzyme A Synthetase 2 Potentiates Macropinocytosis and Muscle Wasting Through Metabolic Reprogramming in Pancreatic Cancer found that metabolic stress can induce ACSS2 expression
Furthermore, ACSS2 promotes muscle wasting through GSK3β/TRAIL axis, resulting in muscle wasting, which potentially provides nutrients to maintain tumor fitness,” he said. “ACSS2 dominates the metabolic reprogramming by orchestrating macropinocytosis and muscle wasting to support tumor progression in pancreatic cancer ”
The medical professional said targeting ACSS2 would help prevent the development of cachexia in pancreatic cancer patients “This study expanded our knowledge on the complex mechanism of cancer cell macropinocytosis under metabolic stress conditions and the release of tumor-derived factors stimulating muscle wasting in pancreatic cancer,” he stated.
Dr Li is inspired to study pancreatic cancer as it is a catchment area of the Stephenson Cancer Center and it’s one of the most fatal forms of cancer “Innovative research focusing on pancreatic cancer such as new mechanisms, and new therapies are timely and urgently needed. I am excited to take this opportunity to pursue this innovative research in pancreatic cancer,” he said.
It’s the change innovation brings that Dr Li enjoys most about conducting his research “I hope this research will lead to a better understanding of the biology of pancreatic cancer, and help to develop a new therapy for this terrible disease,” he said In recent years, Dr Li’s team has published various studies with their findings and new therapies.
“Our studies indicate that ZIP4-based therapy can sensitize the pancreatic cancer cells to chemotherapy; therefore, a combinational therapy using ZIP4 shRNA and chemotherapy may further increase the efficacy of individual treatment for pancreatic cancer,” he said.
“Our studies also elucidated the complex mechanism of cancer cell macropinocytosis under metabolic stress conditions and the release of tumor-derived factors stimulating muscle wasting and cancer cachexia in pancreatic cancer Furthermore, our recent study indicated that a combination of local phototherapy and immunotherapy induced systemic immunity against established tumors and metastases in an aggressive, preclinical pancreatic tumor model, leading to a potential clinical method for patients with advanced pancreatic cancer ”

The researcher explained several colleagues are involved with these studies including Drs Barish Edil, Ajay Jain, and Lacey McNally “This creates multidisciplinary collaborations, and training opportunities for our junior faculty, residents, and fellows,” he said. “More importantly, it will benefit the patients diagnosed with pancreatic cancer and improve the overall clinical and research programs in the Department of Surgery “
Going forward Dr Li hopes to identify new “diagnostic and therapeutic markers in pancreatic cancer which can be translated into new clinical trials and benefit patient care at OUHSC.
The medical profession is grateful to the department and Chair of the Department Dr. Edil for creating an environment that’s supportive of growth


Retirement Party ~














20 years of service



April 14, 2023
Sushanth Reddy, MD

Associate Director - UAB General Surgery
Residency Program
Associate Director - Division of Surgical Oncology
UAB Department of Surgery

April 7, 2023
Chief of Hepatobiliary and Pancreatic Surgery

NYU Grossman School of Medicine

Vice Chair for Clinical Affairs
NYU Department of Surgery
Christopher Wolfgang, MD
April 28, 2023

The 2022-2023 Chief Residents received their Captain's Chair at the Chief Resident Farewell Breakfast on June 16, 2023.


Andrea Geddes, M.D.
General Surgery & Trauma Surgery (Faculty)
Ascension St. Francis Evanston, IL
Areej Sami, M.D.
Surgical Oncology Fellowship
Advocate Aurora Health Milwaukee, WI
Andrew Murphy, M.D.
Vascular Surgery Fellowship
Eastern Virginia Medical School
Norfolk, VA
Taylor Martin, M.D.
Surgical Critical Care Fellowship
Yale New Haven Hospital New Haven, CT
Lindsay Lindsey, M.D.
General Surgery
North Florida Surgeons Jacksonville, FL
























































& Vascular Surgery
Harold Burkhart, MD
405 Magazine 2023 OKC Metro Top Doc
Joshua Gierman, MD
405 Magazine 2023 OKC Metro Top Doc
Lacy Harville, MD
405 Magazine 2023 OKC Metro
Frank Wood, MD
Catherine J. Hunter, MD
Presentation Award, Partners in Quality College of Nursing at the University of OUHSC
Alpha Omega Alpha, Alpha Omega Alpha Honors Society Mentorship Award, OUHSC Department of Pediatrics
Jeremy J Johnson, MD
405 Magazine 2023 OKC Metro
Harold Burkhart, MD
Oklahoma University Medical Center: Co-Investigator: Tobacco Treatment Partnership, OU Medical Center (Congenital Heart Surgery) and the Oklahoma Hospital Association Private Total Direct Cost: $44000, 2017 – Present
Catherine J. Hunter, MD
Hunter, C J , "ROCK, tight junctions and prematurity in the pathogenesis of necrotizing enterocolitis and neonatal sepsis," Federal Grant, Sponsored by National Institutes of Health, Federal Grant/Contract Number: R01 DK133207-01A1
Education
Areej Sami, MD
Top Doc Faculty Senator for OU College of Medicine Faculty Senate Co-Director of Adult ECMO Russell G Postier, MD Award for Excellence in Resident Education Gold Humanism Honor Society
Brook Snyder, MD
2023- Joseph Susman Memorial Award for best presentation and manuscript, Surgical Infectious Society Annual Meeting, Westlake Village, Ca 2023- Top plenary papers session award Surgical Infectious Society Annual Meeting, Westlake Village, Ca 2023- Third place plenary presentation award, Partners in Quality Annual Meeting, Oklahoma City, Ok 2023- Plenary Top Oral Presentation Award, Pediatric Research Day Oklahoma City Ok
General Surgery, Trauma & Critical Care
Top Doc 2021 - 2022 Outstanding Teacher Award, Clinical Curriculum Subcommittee the Medical Education Committee and the Office of Faculty Affairs and Professional Development
2021-2022 Outstanding Teacher Award, University of Oklahoma Health Sciences Center
Alessandra Landmann, MD
Principle Investigator: ExGRAFT Vascular Conduit, IRB#15530, 2023 – pending
Mayo Clinic: Principle Investigator: A Prospective Study of Patients Hypoplastic Left Heart Syndrome Following Stage II Surgical Palliation, 01/2016 – Present
Total Direct Costs: $3,400,000 00 Additional Information: Score 9th percent April 1 2023March 31, 2022
Nikola K. Puffinbarger, MD
Alejandro Ruiz-Elizalde, MD
Principle Investigator: Phase I Safety Study of Autologous Umbilical Cord Blood-Derived Mononuclear Cells During Surgical Stage II Palliation of Hypoplastic Left Heart Syndrome 12/2014 – Present
Matthew Reinersman, MD
University of Oklahoma:
Principle nvestigator:Marijuana
Associated Spontaneous Pneumomediastinum, IRB#15686
Yuki Nakamura, MD
Oklahoma University Medical Center: Principle Investigator: ECMO – Thrombus Formation at Junctions, IRB#15226, 2023 –pending
Frank Wood, MD
Principle Investigator: Utilization of Cardiopulmonary Bypass in Traumatic Injuries:AAST multi-center study 2022 – present
Principle Investigator: Effects of Historical Redlining and Gun Violence in Oklahoma City, Oklahoma 2021 – present
Alexander Raines, MD (Faculty – Clinical)
405 Magazine 2023 OKC Metro
Top Doc Aesculapian Award for Excellence in Teaching
Stanton L Young Master Teacher Award
Third Place Podium for “Anecdotes drive attitude, data drives decisions: optimizing the emergency department workup prior to surgical consultations" Associate Member, Academy of Teaching Scholars, University of Oklahoma Health Sciences Center 2021 - 2022 Outstanding Teacher Award, University of Oklahoma Health Sciences Center 405 Magazine 2023 OKC Metro Top Doc 2021 - 2022 Outstanding Teacher Award, Clinical Curriculum Subcommittee, the Medical Education Committee and the Office of Faculty Affairs and Professional Development 2021-2022 Outstanding Teacher Award, University of Oklahoma Health Sciences Center 405 Magazine 2023 OKC Metro Top Doc Aesculapian Award for Excellence in Teaching
Ajay Jain, MD (Faculty – Clinical)
Teresa Shavney, MD
Greater Oklahoma City Alumnae Panhellenic Delta Delta Delta 2023 Woman of the Year CNDH Employee of the Week
Principle Investigator: Penetrating Trauma in Children During the Covid-19 Era 2021 –present
Principle Investigator: Subjective Determination of Oxygenator Function in Adult ECMO Management 2021 –present
Principle Investigator: Anastomotic Leak Following Repair and Primary Anastomosis of Blunt-Trauma
Associated Mesenteric Bucket Handle Injuries: a multi-center study 2021 – present
Hunter, C J (Principal Investigator), 7% Effort, "Defining the role of the intestinal barrier in necrotizing enterocolitis using human enteroids," Oklahoma Center for Adult Stem Cell Research Sponsored by Oklahoma Center for Adult Stem Cell Research, State
Current Funding (Total Cost per Year): $143,360 00 January 1, 2021December 31, 2023
Research
William Berry, PhD 02/2023-01/2028
R01AR080896

PDGFRB Signaling in Progressive Skin Disease
PI: Lorin E Olson
Co-I: William L Berry
Total Direct Costs: $92,595


WT Martin, KB Snyder, AK Patterson, J Ball, KE Stewart, Z Sarwar A Raines and A Cross “Not all cholecystitis is created equal: Disparities contributing to presentation and failure of outpatient algorithm ” Oral presentation Southwestern Surgical Congress, Ojai, CA, April 2023
Catherine J. Hunter, MD
Hunter, C J , "Ethics Perspective: The changing legal landscape around abortion post-Dobbs: Impact of Pediatric Surgery", American Pedaitric Surgical Association, Orlando, Florida, Invited, Panel May 11, 2023
Leiva T, Golubkova A, Snyder K Liebe H, Schlegel C, Eckert J, Zhongxin Y, Berry W, Hunter C J “Loss of Caveolin-1 is Associated with Necrotizing Enterocolitis in Humans and Mice ” American Pediatric Surgical Association Annual Meeting, Orlando FL, May, 2023
Leiva T, Snyder K, Golubkova A, Hunter C J “Historical Review of ECMO Innovation and Outcomes ” American Pediatric Surgical Association Annual Meeting Orlando FL, May, 2023
Snyder K, Liebe H, Schlegel C, Golubkova A, Leiva T, Hunter C J “The hyperinflammatory state: increasing proclivity to develop necrotizing enterocolitis ” American Pediatric Surgical Association Annual Meeting Orlando FL May, 2023
Grand Rounds: Pediatric Surgical Considerations for the General Surgeon Hunter C J (Presenter) to Residents and Faculty April 27, 2023, Surgery, University of Illinois
Boot-camp in a Surgical Residency Program at the Association for Surgical Education
Brook Snyder, MD
The University of Oklahoma Pediatric Research Day Oklahoma City: The hyperinflammatory state: increasing proclivity to develop necrotizing enterocolitis
Western Trauma Association, Lake Louise Canada: The trauma pan scan: Advocating for use in geriatric falls
Alexander Raines, MD
C Jeffery, K Stewart, J Hayhurst, C Hall, J Regner, and A Raines “Get on board or get out of the way – Survey shows all residents have exposure to robotic surgery platforms yet no formalized curricula exist: A Southwestern Surgical Congress Multi-Center Study ” Oral presentation Southwestern Surgical Congress, Ojai, CA, April 2023.
Leiva T Cai X Schlegel C Golubkova, Snyder KB,Hunter C J “ROCK inhibition attenuates pro-apoptotic factors associated with Necrotizing Enterocolitis ” Surgical Infectious Society Annual Meeting, Westlake CA, April, 2023
Golubkova A Leiva T Snyder KB, Liebe H, Schlegel C, Hansen J, Vitiello P, Hunter C J “Oxidative injury leads to lipid radical accumulation in a human necrotizing enterocolitis enteroid model ” Surgical Infectious Society Annual Meeting, Westlake CA, April, 2023
gery, itical MD casa S n, P Choi, ate? No al hernia my ” J of ted March gery r, MD


H, Leiva T, K, Hunter nt al Clinical 3 H, Leiva T, Z, Hunter nt y (BCVI) in tims ” The TBD r, C J
Neonatal crobiome NEC 23 May 9; 390/microo , C , , Harris, r, C J , S D ersus application s to the cencenal of OI: 016/j jpeds
Liebe, H , Schlegel, C , Cai, X , Golubkova, A , Loerke, C , Leiva, T , Hunter, C J (2023) “Apical-Out Enteroids as an Innovative Model for Necrotizing Enterocolitis ” The Journal of surgical research, 283 1106-1116 PMID:
Golubkova, A , Hunter, C J (2023) “Updates and recommendations on the surgical management of NEC ” Seminars in perinatology, 47(1), 151698 PMID:
Snyder, K B * , Hunter, C J # (in press) “Bugs and the barrier: a review of the gut microbiome and intestinal barrier in necrotizing enterocolitis ” Seminars in Pediatric Surgery
Cai, X , Liebe, H L , Golubkova, A , Leiva, T , Hunter, C J (2023) “A Review of the Diagnosis and Treatment of Necrotizing Enterocolitis ”Current pediatric reviews, 19(3), 285-295 PMID: 35929629 DOI: 10 2174/157339631866622080 5110947
Golubkova A, Leiva T, Hunter C J “Necrotizing Enterocolitis is Associated with a Hyperinflammatory Response in a Human Enteroid Model ”
Annual Academic Surgical Congress Houston TX February 8, 2023
Golubkova A, Snyder K, Leiva T, Chun W, Stewart K, Stavis R, Hunter C J , Landmann A, Ivanov V “Impact of meconium exposure on bowel injury and function: 10-year review of children born with gastroschisis in Oklahoma” poster OU Health Department of Pediatrics Annual Research Symposium, Oklahoma City, OK, January 20, 2023
Abdominal Wall Hernias In NonHuman Primates, Two Cases In Western Lowland Gorillas (Gorilla Gorilla Gorilla)", Journal of Zoo and Wildlife Medicine Department of Surgery OUHSC Oklahoma City OK, Manuscript (February 2023)
Alejandro Ruiz-Elizalde, MD
Nguyen, L H , Landmann, A , RuizElizalde, A R , "Gastrojejunostomy tube placement in infants, a weight based decision to decrease complications", Academic Surgical Congress, Houston, TX, Invited, Platform Presentation (February 7, 2023)
Loerke, C , T r Z Gin ban, H , “A ontrol calcitonin ecrotizing Enterocolitis ” Surgical infections PMID: 37134209
DOI: 10 1089/sur 2022 366
Reiter A J Warner S G
Chen H Ingraham A M Hunter, C J , Freischlag, J , Raval, M V (2023)
“Translating the Value of the Academic Surgeon Into Salary, Time, and Resources The Journal of surgical research, 285, A1-A6 PMID: 36682973
DOI: 10 1016/j jss 2022 12 039
Liebe H Schlegel C Cai X
Golubkova, A , Loerke, C , Leiva, T , Hunter, C J (2023)
“Apical-Out Enteroids as an Innovative Model for Necrotizing Enterocolitis ” The Journal of surgical research, 283, 1106-1116 PMID:
10 1016/j jss 2022 11 048
Chung S Landmann A Johnson, J J , Sisk, J M “Intraoperative Extracorporeal Membrane Oxygenation Rescue of a Polytrauma Patient with a Complete Right Mainstem Bronchus Avulsion: A Pediatric Case Report International Anesthesia Research Society”, 17(3/March 2023) DOI:10 1213/XAA 00000000000 01670 (March 20, 2023) Stottlemyre, R L , Notrica, D M , Cohen, A S , Sayrs, L W , Naiditch, J , St Peter, S D , Leys, C M , Ostlie, D J , Maxson, R T , Ponsky, T , Eubanks, J W , Bhatia, A , Greenwell, C , Lawson, K A , Alder A C Johnson J J Garvey E “Hemodilution in pediatric trauma: Defining the expected hemoglobin changes in patients with liver and/or spleen injury: An ATOMAC+ secondary analysis Journal of Pediatric Surgery, 58(2), 325329 DOI: 10 1016/j jpedsurg 2022 10 04 4 (February 2023)
Salkini, A , Schwartz, R M , Makil, E S , Mir, A , Burkhart, H M , Johnson, J J , Gierman, J L “Lifesaving use of temporary balloon occlusion of an iliac artery disruption to prevent hemorrhagic shock” Pediatric Cardiology Journal, 43(8), 1934-2029 Pediatric Cardiology (December 2022)
Lacey McNally, PhD
Abhilash Samykutty, Karl N
Thomas, Molly McNally, Jordan Hagood, Akiko Chiba, Alexandra Thomas, Libby
McWilliams Bahareh Behkam
Ying Zhan, McAlister Council-
Troche, Juan C Claros-Sorto, Christina Henson, Tabitha
Garwe, Zoona Sarwar, William

E Grizzle, Lacey R McNally
Simultaneous Detection of Multiple Tumor-targeted Gold
Nanoparticles in HER2-positive
Breast Tumors Using Optoacoustic Imaging
Radiology: Imaging Cancer-
Accepted Hunter Chalfant, Morgan
Bonds, Kristina Scott, Anna Condacse, Isabel S Dennahy, W Taylor Martin, Cooper
Little, Barish H Edil, Lacey R
McNally, Ajay Jain 2023
Innovative Imaging Techniques
Used to Evaluate BorderlineResectable Pancreatic Adenocarcinoma Journal of Surgical Research 284:42-53
Tereza Husarova, William M
MacCuaig, Isabel S Dennahy, Emma Sanderson , Barish H
Edil , Ajay Jain , Morgan
Bonds, Molly McNally, Katerina Menclova Jiri Pudil
Pavel Zaruba Radek Pohnan
Christina E Henson, William
E Grizzle, and Lacey R
McNally 2023 Intraoperative imaging in hepatopancreatobiliary surgery
Surgeons at the University of Oklahoma Health Sciences Center are dedicated to excellence in education, research and patient care. We appreciate the generous support of patients and their families, alumni, physicians, friends and businesses.

Your gift can help improve a child’s health, award a resident a scholarship, or provide funds for research, equipment, computers, library materials and more. Every gift we receive makes a difference, and we sincerely thank you for your generosity.
Development Office
University of Oklahoma Health Sciences Center
P.O. Box 26901 Oklahoma City, OK 73126 405-271-2300
http://home.oufoundation.org/COMSurgery
Ifyouwouldliketocontributeanarticle,newsitemoreventnoticeforournewsletter, pleaseemail: jessica-capetillo@ouhsc.edu

