football medicine & performance Legal • Education • Recruitment • Wellbeing www.fmpa.co.uk Issue 43 Summer 2023 Women’s World Cup Special Edition: The Female Sleep Paradox: Why Many Female Players Have Sleep As A Foe When It Should Be A Friend Flipping The Script On Women’s ACL Injury Prevention & Management Hormonal Contraceptives & Football Pregnancy In Football, A Blanket Ban? Menstrual Cycle: Practical Considerations For The Team Physician The official magazine of the Football Medicine & Performance Association
Enigma Legal provides legal services and advice to managers, coaches and professionals working within the sports industry, its unique structure utilising a panel of expert barristers all with extensive experience of the sports industry, most notably their work with the League Managers Association.

Enigma Legal lawyers are tried and trusted to work in a flexible, agile and responsive way, demonstrating their understanding of the unique demands of the sports industry. A creative and pragmatic approach will ensure that Enigma Legal offers real value to the FMPA Membership.
www.enigmalegal.com
admin@fmpa.co.uk
CEO MESSAGE
The FMPA Conference recently returned as a face-to-face event for the first time in four years. Hosted at Leicester City’s King Power Stadium, the event delivered a terrific education programme enjoyed by a full quota of delegates and trade exhibitors. With a noticeably younger wave of delegates from across all disciplines, it was encouraging to see such an enthusiastic and appreciative audience readily engaging with the speakers throughout the day.
There is no question that the FMPA Conference remains a firm fixture in the football calendar and we are therefore delighted to announce that the 2024 Conference and Awards are to return at the end of this season. The date has been set for the 23 rd May 2024 which is highlighted on our forthcoming wall planner. Fortunately for everyone, this season is back on a normal footing which means our event will not collide with holidays this time round. The event structure will be a return to the traditional format of a single day education programme and an evening awards event with the venue to be announced.
Every year, a cohort of Conference programme contributors and speakers, as well as facilitators, combine to create an event that is relevant and of real value to our audience.
The FMPA are fortunate to have so many members who are prepared to offer support, commitment, and their valuable time to the association and this year was no exception. Every one of our members brought unique skills, experiences, and perspectives to the table and it is through their collective efforts that we were able to accomplish such a successful event.
I am certain that next year will be no exception.
Salmon Eamonn Chief Executive Officer Football Medicine & Performance Association

3 www.fmpa.co.uk

FROM THE EDITORS

As the rise of the Women’s game continues and in preparation for the Women’s World Cup in Australia and New Zealand, we look forward to growing the support, education and opportunities for all medical and performance staff working in Women’s football. Therefore, we are proud to release a special edition on the Women’s World Cup for our 43rd Edition of the Football Medicine & Performance Editorial.
Beth Mead, Vivianne Miedema, Alexia Putellas, Leah Williamson. Four players who were named in the Guardian’s list of Top 20 female footballers in the world in 2022. Concerningly, for the football medicine and performance community, the same four players have sustained career-threatening ACL injuries within the last 12 months. The experience of these players (and many other well-known female players), and their public profile, means that there is a greater urgency than ever before to address female players’ risk of ACL injuries. For this edition, we have brought together some of the world’s leading clinicians and researchers who are trying to solve this and many more issues within the women’s game – including technology advancements (Dr Katrine Okholm Kryger), pelvic floor (Emma Brockwell), pregnancy considerations (Dr Eva Ferrer), Dr Rita Tomas (menstrual cycle influence) and the gendered approach to performance support (Dr Joanne Parsons).
Our aim for this edition is to inspire higher quality research and improved standards in the Women’s game. It is only through doing so that we can ensure the game continues to grow and its leading players remain healthy despite an increasingly demanding fixture schedule.

We hope you enjoy the 43rd edition of Football Medicine & Performance and can take away key learnings that can be applied across your clinical practice.
 Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
5 www.fmpa.co.uk
Sean Carmody Fadi Hassan Andrew Shafik
ABOUT
ASSOCIATE EDITORS
REVIEWERS
Football Medicine & Performance Association 43a Moor Lane, Clitheroe, Lancs, BB7 1BE


T: 0333 456 7897 E: info@fmpa.co.uk W: www.fmpa.co.uk
FMPA_Official Officialfmpa fmpa_official LinkedIn: Football Medicine & Performance Association



FMPA_Register FMPARegister fmpa_register

Chief Executive Officer Eamonn Salmon eamonn.salmon@fmpa.co.uk







Commercial Manager Angela Walton angela.walton@fmpa.co.uk


Design Oporto Sports www.oportosports.com
Photography Alamy, FMPA, Unsplash
Cover Image Physios check on Lauren Hemp of England who collided with Antonia of Brazil resulting in a facial injury. Womens Finalissima, England versus Brazil, Wembley Stadium, London. 6th April, 2023


Photo: Alamy
Football Medicine & Performance Association. All rights reserved. The views and opinions of contributors expressed in Football Medicine & Performance are their own and not necessarily of the FMPA Members, FMPA employees or of the association. No part of this publication may be reproduced or transmitted in any form or by any means, or stored in a retrieval system without prior permission except as permitted under the Copyright Designs Patents Act 1988. Application for permission for use of copyright material shall be made to FMPA. For permissions contact admin@fmpa.co.uk
Ian Horsley Lead Physiotherapist
Dr Jon Power Director of Sport & Exercise Medicine
Dr Dáire Rooney Doctor
Dr Andrew Butterworth Senior Lecturer Frankie Hunter Lead Sports Scientist
Dr Manroy Sahni Medical Doctor
Eleanor Trezise Medical Student
Matthew Brown Academy Sports Scientist
Callum Innes Medical Doctor
Kevin Paxton Strength & Conditioning Coach
Dr Avinash Chandran Director
Mike Brown Head of Physical Performance Jake Heath Elite Sports Specialist Podiatrist
Lisa Edwards Sports Therapist
Dr Jose Padilla MD Sports Medicine Specialist
Dr Daniela Mifsud Doctor & Physiotherapist
Dr Danyaal Khan Academy Doctor
09 The Female Sleep Paradox: Why Many Female Players Have Sleep As A Foe When It Should Be A Friend David Thorne & Dr. Chris James


14 Flipping The Script On Women’s ACL Injury Prevention & Management


Dr. Joanne L. Parsons, Dr. Sheree Bekker, Dr. Stephanie E. Coen
18 Hormonal Contraceptives & Football


Dr. Tessa R. Flood, Professor Kirsty J. ElliottSale
23 Is Technology In Football Adjusted For Women?
Dr. Katrine Okholm Kryger
28 Pelvic Floor Considerations: A Potential Game Changer For Women’s Football?


Emma Brockwell
37 Pregnancy In Football, A Blanket Ban?
Eva Ferrer
42 Menstrual Cycle: Practical Considerations For The Team Physician
Rita Tomás
49 The Effects Of The Menstrual Cycle On Both Training & Match Day Physical Performance Using Subjective & Objective Measures
Lisa Edwards
09 23 49 28
7 www.fmpa.co.uk 14 37 18 42
CONTENTS FEATURES

THE FEMALE SLEEP PARADOX: WHY MANY FEMALE PLAYERS HAVE SLEEP AS A FOE WHEN IT SHOULD BE A FRIEND
Introduction
Sleep issues are significantly more common amongst athletes than the general population, partly due to the bodily and mental stress associated with performing at a high level, and the environmental demands of having to consistently travel and perform during evening matches1 However, there are also experiences specific to women that can compound these factors that influence sleep quality.
From the pain associated with menstrual cramps to the impact of hormones on melatonin production, female players will have additional risk factors to contend with in New Zealand & Australia this summer.

The Female Sleep Paradox
Several studies have found that women generally have better quality sleep patterns for athletic recovery. They spend more time in deep restorative sleep2, allowing them to recover quicker physically and create
memories more readily. However, despite them spending more time in deep sleep, women paradoxically also more frequently report poor subjective sleep quality3 and are 55% more likely to report sleep disturbances than their male athlete counterparts4
Subsequently, the prevalence of insomnia is particularly high in women5, partly attributable to menstrual cramps (dysmenorrhea), endometriosis, hormonal fluctuations, and pregnancy. Despite sleep being considered as a potential performance advantage for female athletes, it can very quickly become a weakness without specialist individualised education and intervention.
Endometriosis
Endometriosis is a condition which results in the presence of endometrial glands and stroma like lesions outside of the uterus, and is a condition that affects women of any age. In 2022, England captain Leah
Williamson spoke out about the impact endometriosis has had on her life, and how following her diagnosis in 2021 she worried that the condition could have led to her missing key matches during England’s European Championship victory on home soil. These worries came from the ‘agonising’ pain she endured.
Endometriosis is characterised by particularly debilitating period pains, pelvic pains, cramps and uncomfortable bowel movements. Endometriosis is relatively prevalent affecting approximately 10% of women of reproductive age6
When it comes to sleep, research consistently shows that women with a diagnosis of endometriosis can expect:
• More sleep disturbances7
• Longer sleep onset latency7
• Worse subjective sleep quality8, with one study finding a 30% difference between
FEATURE / DAVID THORNE (BSC, MSC) & DR. CHRIS JAMES (BSC, MSC, DCLINPSY) - SLEEP ATHLETIC
9 feature www.fmpa.co.uk medicine & performance football
Germany’s Alexandra Popp
those with and without endometriosis9
• And, subsequently, greater daytime sleepiness10
Crucially, it is those with the greatest pain intensity that have the biggest sleep problems10. This is as expected, with the pain of endometriosis making it difficult to relax enough to create sleep onset while also causing women to consistently wake up throughout the night. This is a finding that is showcased across the board with people who experience chronic pain11
The challenge for female footballers is that sleep and endometriosis can form a vicious cycle. Research has found that poor sleep quality one night generally leads to greater pain sensitivity the following day, making endometriosis symptoms even more debilitating12. These worsened endometriosis symptoms then lead to even worse sleep that night, and the vicious cycle continues. The result is fatigue being twice as common in individuals with endometriosis than in their control group counterparts13. Fatigue in turn impacts player performance as poor decision making occurs and sub-optimal physical intensity ensues. Further more fatigue secondary to poor sleep quality impacts recovery through overreach injuries and muscle fatigue accumulation.
On top of pain broadly impacting on sleep quality, endometriosis has also been associated with a sleep medical condition called Restless Leg Syndrome. This sleep
condition is already more common amongst elite athletes, but research also suggests that those with endometriosis are 2 and a half times more likely to experience Restless Leg Syndrome (RLS) than the general population14 This could be due to the strong relationship between RLS and iron deficiency15, and women with endometriosis being at greater risk of iron deficiency through heavier menses and the iron unavailability associated with endometriosis-related chronic inflammation.
For women playing in this year’s world cup that are struggling with endometriosis symptoms, there are a few things to keep in mind that could help with their pain and/or RLS symptoms and their impact on sleep:

• Physical exercise is a protective factor against endometriosis. As Leah Williamson highlighted, her endometriosis flared up after getting a hamstring injury. Research suggests that regular physical exercise improves levels of immune and anti-inflammatory markers and reduces menstrual flow, which can then decrease the symptom weight for athletes16. Regular exercise can also enhance melatonin secretion, which subsequently helps endometriosis sufferers with insomnia symptoms17
• On top of exercising, which is of course a natural part of elite athletes’ lives anyway, melatonin supplementation might be a way to kill two birds with one stone. Clinical trials have found that treatment of 10mg of melatonin for 8 weeks, when compared with placebo in women with endometriosis,
reduces daily pain, stomach cramps, painful urination, and improves sleep quality18. It is important to note that this study was not within the athletic population, though.
• As well as supplementing melatonin, as iron deficiency is strongly associated with endometriosis, and subsequently with RLS, female athletes at the World Cup should also consider discussing with their doctor about the need for iron supplementation.
• And finally, Leah Williamson described how the threat of a painful period provided additional stress and anxiety. Painful menses triggers additional stress and anxiety which in turn may result in insomnia, meaning that an individual who has a diagnosis of endometriosis might not only have poor sleep when they are in pain. Ruminating on the potential pain could be enough to worsen sleep onset, and potentially induce endometriosis symptom flare ups. Working with a clinically trained psychologist, especially those who specialise in sleep, can help tackle these psychological triggers for poor sleep.
Pregnancy
Another factor that influences the sleeping experiences of female athletes is pregnancy. Remarkably, a FIFPro report from 2017 which surveyed 3,295 women footballers found that only 2% were mothers19. Although this report didn’t survey any male players, we can expect this percentage to be significantly higher in the male population, in part because they don’t have to take time out of their career to carry a child. This is a particular issue because less than 40% of female players are offered childcare support and this means almost half of women footballers believe they would have to leave the game early if they wanted to start a family. This is supported by the view of leading coaches, with Emma Hayes describing the lack of childcare support offered to female players as a disgrace.
Therefore, due to the scarcity of women’s footballers who are mothers, we will spend less time talking about the impact that pregnancy has on sleep. That said, it’s important to highlight that there are multiple partum-related factors that impact on sleep:
• Sleep issues during pregnancy are highly common with almost half (46%) of women reporting poor sleep, and sleep issues become more common as women move from the second to the third trimester20.However, it is to be noted that even in the second trimester, over 1/4 of women (285) slept less than 7 hours per night21 and in the first trimester more than half of women report insomnia symptoms despite normal sleep duration22
• Although total sleep time increases during the first trimester, subjective sleep quality is altered as early as the first trimester
• Sleep then worsens throughout pregnancy with the end of pregnancy being associated
feature 10 info@fmpa.co.uk
with greater sleep fragmentation because of a number of variables21: snoring, respiratory effort-related arousals, restless leg syndrome, and lower back pain.
• Restless leg syndrome is potentially the most common sleep disorder associated with pregnancy, with systematic analyses suggesting a prevalence of between 26 and 30% for gestational restless leg syndrome23 With athletes already being at risk of restless leg syndrome, and women being twice as likely to experience restless leg symptoms compared to men, this is a key area that needs tackling. Residual postpartum RLS correlated with lower ferritin23, which again highlights the importance of supplementing iron as a way of tackling RLS’ impact on women’s sleep experiences.
Hormones, Cramps and the Menstrual Cycle
The primary sleep-regulating areas in the brain are filled with estrogen and progesterone receptors24, which is why it’s unsurprising that hormonal fluctuations in women have a significant impact on sleep quality. This is something that takes effect as young as after a woman’s first menstrual bleeding with research demonstrating that girls are 2.75 times more likely to develop insomnia when compared to boys25
The biggest hormone-driven sleep changes seem to be during the pre-menstrual fluctuation of progestogens and estrogens rather than during the follicular or luteal phases, with one study finding no difference in objective sleep data throughout these phases other than a higher percentage of restorative REM sleep in the follicular phase compared to the luteal phase26. However, due to non-hormonal factors associated with stages of the menstrual cycle that include bleeding, research shows a worsening of subjective indicators of sleep quality and efficiency, and total sleep time during the menstrual phases too27
Research shows that the sleep issues associated with the menstrual cycle are likely present in elite female athletes, too. During the menstrual phase, female athletes can expect to experience a decrease in the proportion of sleep time spent in restorative slow wave sleep27. The primary drivers of poor sleep quality during hormonal fluctuations is likely the increase in core body temperature seen when progesterone levels are elevated28
Pain during the menstrual cycle is an extremely common experience for women. Research by Women’s Health Concern suggests that over 80% of women will experience period pain at some point in their life. What this means is there is likely a time when women are more vulnerable to poor sleep quality through worse sleep onset
(struggling to relax and get to sleep), more sleep awakenings during the night, and a greater likelihood of waking up earlier than they want.
The tournament in New Zealand and Australia lasts a month. We can expect a significant proportion of players to experience menstrual cycle-related sleep issues during this tournament, purely based on their natural body clocks. What this means is that players and medical teams need to be prepared for the impact this could have by:
• Educating players on how they can prevent the menstrual cycle from significantly impacting their sleep, including sleeping in the foetal position for cramps, wearing loose fitting clothes and making sure their bedroom is cool so they don’t get too hot, and potentially increasing total sleep time for the few days before and during the menses phase
• Have sleep experts screen squads to identify players who are vulnerable to the impact of the menses phase on their sleep, and develop tailored strategies to help players effectively wind down before bed and optimise sleep/recovery during these more challenging periods
• It’s important for players to know how they can best be kind to themselves when struggling with their menses and that they
can expect slightly worse during the menses phase. If players feel ready and equipped to tackle hormone changes, pain and slightly worse sleep when it comes by, they’re less likely to allow stress and anxiety to be another factor impacting their sleep.

What we should be doing
Part of medical and performance teams’ work with female athletes is helping them understand that there are unique factors associated with being a woman that could impact on their sleep, and they need to be fully prepared for this.
The first step in empowering female athletes to deal with the potential sleep challenges is to educate. Athletes and staff need to better understand the womanspecific factors that can negatively impact on the sleep quality of players, and part of this is creating a team culture where female athletes feel safe to talk about these issues. Previous research has shown that female athletes vary in how comfortable they are talking to male coaches about these issues29, and this is where representation becomes huge. If female athletes are not supported by staff which allow them to feel comfortable to discuss these issues whilst also being aware of the challenges these athletes face, then this population of athletes will continue to suffer in silence.
11 medicine & performance football www.fmpa.co.uk
England’s Leah Williamson
The second step is to measure the origin of symptoms. Without effective measuring of sleep, and the factors influencing sleep, it is impossible to provide tailored and targeted interventions for female athletes. For one athlete they might be struggling to sleep during their menstrual cycle because of cramps, for another it could be elevated progesterone levels leading to heightened body temperature. Without effective sleep screening and 1:1 consultation with players, both players could be given the same treatment for sleep disruption and perhaps only one would benefit. Crucially, there’s an overreliance in sports on wearable technology for sleep. Technology showing a player’s sleep stages without qualitative understanding and expert understanding offers little-tono value when trying to improve a player’s sleep quality. The sleep stage data might provide information on poor sleep patterns, but it would not provide information on psychological symptoms, restless leg syndrome or changes in breathing patterns. For this reason, medical and performance staff need to properly screen for sleep issues. This will help facilitate tailored interventions and guidance for each player.

Finally, female athletes should be encouraged to lean into their sport. Poor sleep quality and
the pain associated with endometriosis, the menstrual cycle, and pregnancy can all make football feel like a chore. However, research suggests that women who regularly exercise have a significantly better sleep quality, so players should be reminded that their sport is actually a protective factor against poor sleep quality30
Okay, but why does good sleep quality even matter for female athletes?
As well as the significant performance, recovery and wellbeing gains seen in footballers who have better sleep quality, research suggests that extending sleep can help reduce inflammation, which has a significant impact on the likelihood of developing the negative symptoms associated with menstruation such as menstrual cramps31
Conclusion
There’s a female sleep paradox. Female athletes can make sleep-related recovery a strength but currently for many it is a weakness. Several players are struggling with their sleep in silence during pregnancy as they’re not being properly supported by the footballing world. There’s a growing awareness that endometriosis is a relatively common experience for female athletes, but
there isn’t currently a discussion surrounding its vicious cycle with sleep and how this subsequently impacts performance and recovery.
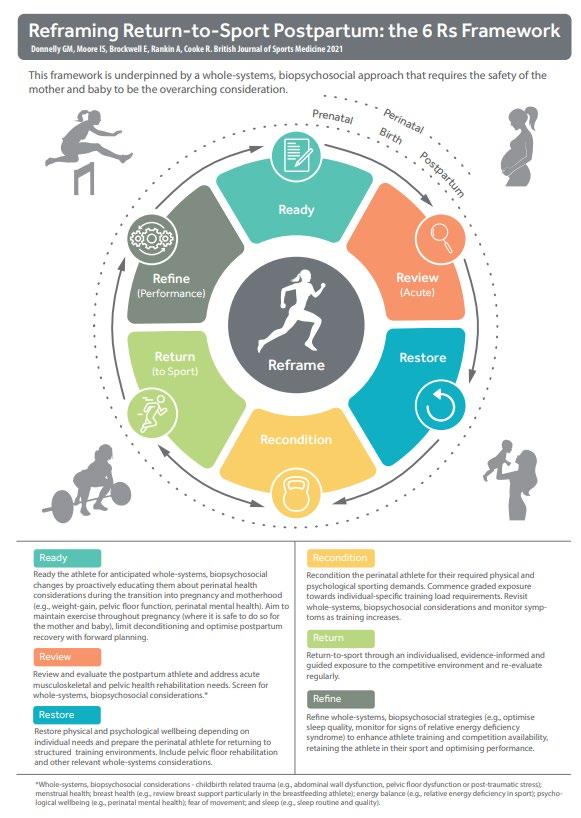
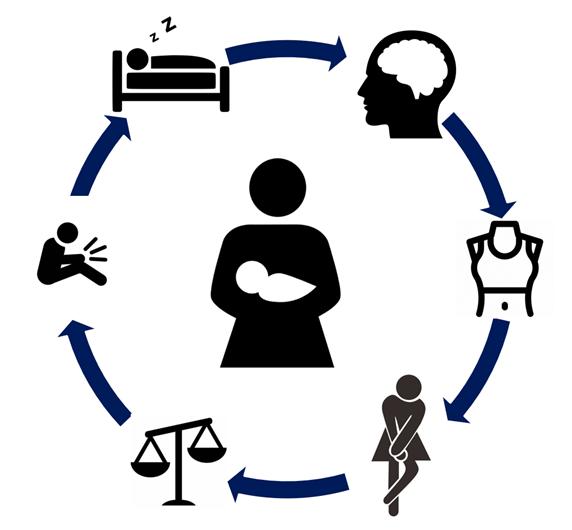
The numerous factors impacting sleep quality can be conceptualised as multiple ‘vicious cycles’. Our ‘vicious flower’ diagram illustrates this (see figure 1 below). More practically, this can also be used to help the athlete make sense of their sleep problems, and key maintaining factors (‘petals’) can be targeted, thereby breaking these negative cycles.
Finally, in a tournament that lasts as long as the average woman’s menstrual cycle, medical and performance teams need to be considering the impact of the menstrual cycle on all their players’ sleep quality. The reality is that many athletes do not recognise they have sub-optimal sleep or they have become resigned to it. This suboptimal sleep is impacting female players’ performance, recovery and mental health/ wellbeing. Furthermore, the only genuinely viable way to tackle this is through specialist sleep screening and assessment of players, together with individually tailored sleep support delivered by clinically trained sleep experts.
feature 12 info@fmpa.co.uk
Figure 1: The ‘vicious flower’: Key factors maintaining sleep issues in women athletes
References
1. Walsh, N. P., Halson, S. L., Sargent, C., Roach, G. D., Nédélec, M., Gupta, L., ... & Samuels, C. H. (2021). Sleep and the athlete: narrative review and 2021 expert consensus recommendations. British journal of sports medicine, 55(7), 356-368.
2. Bixler, E. O., Papaliaga, M. N., Vgontzas, A. N., LIN, H. M., Pejovic, S., Karataraki, M., ... & Chrousos, G. P. (2009). Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. Journal of sleep research, 18(2), 221-228.
3. Koikawa, N., Shimada, S., Suda, S., Murata, A., & Kasai, T. (2016). Sex differences in subjective sleep quality, sleepiness, and health-related quality of life among collegiate soccer players. Sleep and Biological Rhythms, 14(4), 377-386.
4. Benjamin, C. L., Curtis, R. M., Huggins, R. A., Sekiguchi, Y., Jain, R. K., McFadden, B. A., & Casa, D. J. (2020). Sleep dysfunction and mood in collegiate soccer athletes. Sports Health, 12(3), 234-240.
5. Zeng, L. N., Zong, Q. Q., Yang, Y., Zhang, L., Xiang, Y. F., Ng, C. H., ... & Xiang, Y. T. (2020). Gender difference in the prevalence of insomnia: a metaanalysis of observational studies. Frontiers in Psychiatry, 11, 577429.
6. Giudice, L. C., & Kao, L. C. (2004). Endometriosis. Lancet (London, England), 364(9447), 1789–1799.
7. Youseflu, S., Jahanian Sadatmahalleh, S., Roshanzadeh, G., Mottaghi, A., Kazemnejad, A., & Moini, A. (2020). Effects of endometriosis on sleep quality of women: does life style factor make a difference?. BMC Women’s Health, 20(1), 1-7.
8. Nunes, F. R., Ferreira, J. M., & Bahamondes, L. (2015). Pain threshold and sleep quality in women with endometriosis. European Journal of Pain, 19(1), 15-20.
9. Davie, S., Hamilton, Y., Webb, L., & Amoako, A. A. (2020). Sleep quality and endometriosis: A group comparison study. Journal of Endometriosis and Pelvic Pain Disorders, 12(2), 94-100.
10. Maggiore, U. L. R., Bizzarri, N., Scala, C., Tafi, E., Siesto, G., Alessandri, F., & Ferrero, S. (2017). Symptomatic endometriosis of the posterior culde-sac is associated with impaired sleep quality, excessive daytime sleepiness and insomnia: a case–control study. European Journal of Obstetrics & Gynecology and Reproductive Biology, 209, 39-43.
11. Youseflu, S., Jahanian Sadatmahalleh, S., Roshanzadeh, G., Mottaghi, A., Kazemnejad, A., & Moini, A. (2020). Effects of endometriosis on sleep quality of women: does life style factor make a difference?. BMC Women’s Health, 20(1), 1-7.
12. Loring, M., Kabelac, Z., Munir, U., Yue, S., Ephraim, H. Y., Morris, S. N., ... & Katabi, D. (2019). Assessing pain and sleep patterns in endometriosis: a pilot study using passive radio sensors. Journal of Minimally Invasive Gynecology, 26(7), S89.
13. Ramin-Wright, A., Schwartz, A. S. K., Geraedts, K., Rauchfuss, M., Wölfler, M. M., Haeberlin, F., ... & Leeners, B. (2018). Fatigue–a symptom in endometriosis. Human reproduction, 33(8), 1459-1465.
14. Tempest, N., Boyers, M., Carter, A., Lane, S., & Hapangama, D. K. (2021). Premenopausal Women With a Diagnosis of Endometriosis Have a Significantly Higher Prevalence of a Diagnosis or Symptoms Suggestive of Restless Leg Syndrome: A Prospective Cross-Sectional Questionnaire Study. Frontiers in Endocrinology, 12, 599306.
15. Earley, C., Jones, B. C., & Ferré, S. (2022). Brain-iron deficiency models of restless legs syndrome. Experimental neurology, 114158.
16. Ricci, E., Viganò, P., Cipriani, S., Chiaffarino, F., Bianchi, S., Rebonato, G., & Parazzini, F. (2016). Physical activity and endometriosis risk in women with infertility or pain: systematic review and meta-analysis. Medicine, 95(40).
17. Taheri, M., & Irandoust, K. (2018). The exercise-induced weight loss improves self-reported quality of sleep in obese elderly women with sleep disorders. Sleep Hypn, 20(1), 54-9.
18. Yang, H. L., Zhou, W. J., Gu, C. J., Meng, Y. H., Shao, J., Li, D. J., & Li, M. Q. (2018). Pleiotropic roles of melatonin in endometriosis, recurrent spontaneous abortion, and polycystic ovary syndrome. American Journal of Reproductive Immunology, 80(1), e12839.
19. Koukiadaki, A., & Pearson, G. (2017). 2017 FifPro Global Employment Report: Working Conditions in Professional Football.
20. Silvestri, R., & Aricò, I. (2019). Sleep disorders in pregnancy. Sleep Science, 12(3), 232.
21. Reid, K. J., Facco, F. L., Grobman, W. A., Parker, C. B., Herbas, M., Hunter, S., ... & Zee, P. C. (2017). Sleep during pregnancy: the nuMoM2b pregnancy and sleep duration and continuity study. Sleep, 40(5).
22. Kızılırmak, A., Timur, S., & Kartal, B. (2012). Insomnia in pregnancy and factors related to insomnia. The Scientific World Journal, 2012.
23. Manconi, M., Ulfberg, J., Berger, K., Ghorayeb, I., Wesström, J., Fulda, S., ... & Pollmächer, T. (2012). When gender matters: restless legs syndrome. Report of the “RLS and woman” workshop endorsed by the European RLS Study Group. Sleep Medicine Reviews, 16(4), 297-307.
24. Curran-Rauhut, M. A., & Petersen, S. L. (2002). The distribution of progestin receptor mRNA in rat brainstem. Gene Expression Patterns, 1(3-4), 151-157.
25. Calhoun, S. L., Fernandez-Mendoza, J., Vgontzas, A. N., Liao, D., & Bixler, E. O. (2014). Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep medicine, 15(1), 91-95.
26. Driver, H. S., Dijk, D. J., Werth, E. S. T. H. E. R., Biedermann, K., & Borbély, A. A. (1996). Sleep and the sleep electroencephalogram across the menstrual cycle in young healthy women. The Journal of Clinical Endocrinology & Metabolism, 81(2), 728-735.
27. Hrozanova, M., Klöckner, C. A., Sandbakk, Ø., Pallesen, S., & Moen, F. (2021). Sex differences in sleep and influence of the menstrual cycle on women’s sleep in junior endurance athletes. Plos one, 16(6), e0253376.
28. Driver, H. S., Werth, E., Dijk, D. J., & Borbély, A. A. (2008). The menstrual cycle effects on sleep. Sleep medicine clinics, 3(1), 1-11.
29. Brown, N., Knight, C. J., & Forrest, L. J. (2021). Elite female athletes’ experiences and perceptions of the menstrual cycle on training and sport performance. Scandinavian journal of medicine & science in sports, 31(1), 52-69.
30. Yang, S. Y., Lan, S. J., Yen, Y. Y., Hsieh, Y. P., Kung, P. T., & Lan, S. H. (2020). Effects of exercise on sleep quality in pregnant women: a systematic review and meta-analysis of randomized controlled trials. Asian Nursing Research, 14(1), 1-10.
31. Bruinvels, G., Hackney, A. C., & Pedlar, C. R. (2022). Menstrual cycle: the importance of both the phases and the transitions between phases on training and performance. Sports Medicine, 52(7), 1457-1460.
13 medicine & performance football www.fmpa.co.uk
FLIPPING THE SCRIPT ON WOMEN’S ACL INJURY PREVENTION & MANAGEMENT
 FEATURE / DR JOANNE L PARSONS, DR SHEREE BEKKER, DR STEPHANIE E COEN
FEATURE / DR JOANNE L PARSONS, DR SHEREE BEKKER, DR STEPHANIE E COEN
Introduction
Despite 30 years and tens of thousands of research studies, there are still significant differences in sports injury rates between women and men. Concussion and ankle sprain rates remain twice as high in girls/ women1,2, and ruptures of the anterior cruciate ligament (ACL) – which have occurred with alarming frequency in the last year– occur up to six times more frequently than in boys/ men.3,4 Severe injuries like ACL rupture can remove athletes from play for months, result in early development of osteoarthritis5, early knee replacement6, and negatively impact lifelong physical activity participation.7 To start making tangible change, we need to steer away from the overwhelming focus on biological and sex-based explanations (e.g. anatomical characteristics, hormone levels) that are part of current sports injury approaches (Table 1), and instead seriously consider the role of the social and material environments that shape the athlete in highly gendered ways (Figure 1).8
Where are we now?
Since the first recognition of higher ACL injury rates in women in the 1990s, the search for risk factors has focused largely on sex-based explanations such as anatomy (e.g., femoral notch and ligament size; ligament laxity) and physiology (e.g., muscle strength and activation patterns; hormones/menstruation) (Table 1). These factors are largely thought of as intrinsic or internal to the athletes – in other words, they are the athlete’s responsibility to ‘fix’ (if indeed they can be ‘fixed’ at all). However, despite all the work that has occurred over the last 30 years, ACL injury rates for women at all levels of play have either increased or stayed the same4,16 Injury rates are anywhere from 2-6 times higher in women compared to men17-19
Once an ACL injury has occurred, there is some evidence that women are not offered a surgical option as often as men20. If they do have reconstructive surgery, women
demonstrate greater knee laxity, lower patient reported knee function, a lower chance of returning to sport, and a more frequent need for revision surgery after their surgery, compared to men21. Again, investigations into the reasons for these disparities continue to take a sex-based biological approach.
How can we look at things differently?
Our research8 suggests that sport practitioners need to move beyond biology to consider ACL (and other sport injuries) from both social and biological viewpoints. By looking at the list of risk factors for ACL injury (Table 1) we can provide plausible explanations for how sport environments may influence risk. For example, resistance training is key to increasing strength and optimising strength ratios, but we know that girls and women often do not view resistance training and increasing muscle mass
Q angle
‘Intrinsic’ risk factors
Navicular drop
Knee valgus (static and dynamic)
Notch size
Ligament size
Tibial slope angle
Foot pronation
Body Mass Index
Body composition
Menstrual phase
Muscle strength
Hormone concentrations
Muscle strength ratios
Muscle stiffness
Physical fitness
Previous ACL injury
Skill level
Neuromuscular control
Proprioception
Personality
Sports played
Stress response
Race
Sex
Family history of ACL injury
‘Extrinsic ‘ risk factors
Meteorological conditions
Playing situation
Playing surface
Opponent behaviour
Rules
Unanticipated events during play
Referee behaviour
Coaching behaviour
Footwear
Knee braces
Table 1: Summary of factors currently categorised in the literature as ‘intrinsic’ or ‘extrinsic’ that place an athlete at higher risk of non-contact ACL injury9-15
feature 14 info@fmpa.co.uk
Women are injury prone
(e.g. women as menstrual cycles or Q-angles)
Women are made injury prone Focus largely on women’s bodies Consider social and environmental factors
(e.g. stereotypes that disadvantage women)
Marginal gains
(e.g. menstrual cycle monitoring)
Meaningful gains
(e.g. gender equitable environments)
as socially acceptable due to societal norms about ‘desirable’ femininity22-25
They also experience resistance training environments as highly gendered and unwelcoming to women25. How can we say, then, that muscle strength, strength ratios, activation patterns, and physical fitness are all intrinsic risk factors when the programs and environments (i.e., gyms) required to address those factors are heavily gendered in ways that disadvantage women’s participation?
It is plausible that even anatomical characteristics (size of the ACL, shape of the femoral notch), which are recognized risk factors for ACL injury, could be influenced by external environments. The foundation of the rehabilitation and strength and conditioning professions is the principle of tissue adaptability – soft tissue and bone will adapt and remodel according to the forces placed upon them. This means that bone and ligament size and shape could conceivably be influenced by gendered environments that do not encourage women to train and compete as intensely or as often or from as early an age as men.
In the treatment environment, comparing the poorer post-surgical outcomes of women (e.g., more laxity, lower function, lower chance of returning to sport) to that of men assumes that their rehabilitation and training environments were equivalent, which we have suggested is not true. Also, it is widely known that in most parts of the world women still carry the bulk of childcare and domestic
responsibilities. That means women and men very likely have different constraints on their time and ability to complete their rehabilitation programs, which will heavily influence their surgical outcomes and ability to return to play. There are numerous recent examples of how women’s resources, support, and environments are inferior to those of men. From not getting paid while on maternity leave, to relying on inadequately staffed medical teams at a professional level, to playing on sub-standard field conditions, there are constant reminders of how gendered beliefs and expectations influence the way people are treated, the opportunities they have, the activities they participate in, and ultimately their health.
How can you use these ideas to improve things in your practice now?
First – understand how sex and gender relate to each other:
> Sex refers to a complex blend of physical and physiological characteristics (e.g., hormones, genes, anatomy), while gender refers to identities, roles, and structures that are formed by society which may or may not align with sex. Neither sex nor gender is binary.26
> Sex/gender is increasingly being used as a term to recognize the ‘entanglement’ of biological and social factors in expressions of sex and gender.27 It acknowledges the dynamic processes and interactions through which “body-based characteristics…are shaped by gendered social interactions”.28
Now you can reflect on where in the following four sport environments you can intervene:
Pre-sport environment
Gendered play develops different physical skill sets, and the ability to demonstrate and control particular movement patterns are key to injury prevention. Early experiences set the stage for what girls understand as acceptable behaviors and roles.
> Encourage all children to participate in a wide range of activities, and especially encourage girls towards more active play
> Do not use phrases such as “you throw like a girl”
Training environment
Strength training environments are often not welcoming to girls and women. Girls and women are inundated with messages from society about body norms and what they ‘should’ look like.
> Evaluate whether there are gendered messages or imagery in weight-training or clinic spaces. What kind of posters or pictures do you have up, and what message are they sending, either implicitly or explicitly?
> Have a knowledgeable woman coach in weight-training spaces who can be a positive role model
> Focus on an athlete’s goals, performance gains, physical and mental health, not appearance, which is often gendered in nature when commented on
Figure 1: To flip the script on women’s ACL injury, we need to move away from a biological based default and think about how gendered environments may be playing a role
15 medicine & performance football www.fmpa.co.uk
Competition environment
By its very nature, sport places girls/ women and boys/men in different playing situations. The nature and type of sports thought appropriate for women and men are often different.
> Work towards ensuring girls/women and boys/men have equal opportunity to participate in all sports at all ages
> Challenge different rules for girls/ women and boys/men that imply gendered expectations and abilities that disadvantage women (e.g., tennis matches for women are 3 sets; men are 5 sets)
Treatment environment
Gendered assumptions permeate healthcare, and sports medicine is no different. Post-ACL injury outcomes are different for women and men.
> Reflect on how you manage and treat women and men who have ruptured their ACL. Is there a difference, and can you justify it based on observations and assessments and not just assumptions?

> Ask your athlete patients about their nonsport gendered roles like childcare and unpaid work at home. How does it affect their ability to play and rehabilitate?
Conclusion
ACL injury rates have not changed in 30 years despite tens of thousands of studies. The overwhelming focus on biological explanations may be a reason for this failure. Considering gender an external environmental influence will encourage us to ask new questions and move towards improving outcomes for girls and women.
For more information on this topic, see the following resources:
1. Our open access paper
2. Podcast where we discuss our paper
3. Blog where we discuss our paper
4. Interview with Flo Lloyd-Hughes on the Counter Pressed podcast



5. Interview with Kathleen McNamee, Emma Byrne, and Karen Duggan on the COYGIG Pod
Associate Professor and Physiotherapist, University of Manitoba
Dr Joanne L Parsons
Dr Sheree Bekker Associate Professor, Department for Health, University of Bath
Dr Stephanie E Coen Associate Professor, School of Geography, University of Nottingham
feature 16 info@fmpa.co.uk
References
1. Cheng J, Ammerman B, Santiago K, et al. Sex-based differences in the incidence of sports related concussion: systematic review and meta-analysis. Sports Health. 2019;11(6):486-491.
2. Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123-140.
3. Lindenfeld TN, Schmitt DJ, Hendy MP, et al. Incidence of injury in indoor soccer. Am J Sport Med. 1994;22(3):364-371.
4. Montalvo AM, Schneider DK, Yut L, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med. 2019;53(16):1003- 1012.
5. Allen K, Thoma L, Golightly Y. Epidemiology of osteoarthritis. Osteoarthr Cartil. 2022;30(2):184-195.
6. Suter LG, Smith SR, Katz JN, et al. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adulthood. AC & R. 2017;69(2):201-208.
7. Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? Arthritis Rheum. 2011;63(11):3372-3382.
8. Parsons JL, Coen SE, Bekker S. Anterior cruciate ligament injury: towards a gendered environmental approach. Br J Sports Med 2021;55(17):984-990.
9. Cameron KL. Commentary: time for a paradigm shift in conceptualizing risk factors in sports injury research. J Athl Train 2010;45:58–60.
10. Price MJ, Tuca M, Cordasco FA, et al. Nonmodifiable risk factors for anterior cruciate ligament injury. Curr Opin Pediatr 2017;29:55–64.
11. Shultz SJ, Schmitz RJ, Benjaminse A, et al. ACL research retreat VII: an update on anterior cruciate ligament injury risk factor identification, screening, and prevention. J Athl Train 2015;50:1076–93.
12. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the HUNT Valley II meeting, January 2005. Am J Sports Med 2006;34:1512–32.
13. Griffin LY. Prevention of noncontact ACL injuries. Rosemont, Illinois: American Academy of Orthopaedic Surgeons, 2001.
14. Shultz SJ, Schmitz RJ, Nguyen A-D. Research Retreat IV: ACL injuries--the gender bias: April 3-5, 2008 Greensboro, NC. J Athl Train 2008;43:530–1.
15. Williams JM, Andersen MB. Psychosocial antecedents of sport injury: Review and critique of the stress and injury model. J Appl Sport Psychol 1998;10:5–25.
16. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: national collegiate athletic association injury surveillance system data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016 Nov 1;26(6):518-23.
17. Bram JT, Magee LC, Mehta NN, Patel NM, Ganley TJ. Anterior cruciate ligament injury incidence in adolescent athletes: a systematic review and meta-analysis. Am J Sports Med. 2021 Jun;49(7):1962-72.
18. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019 May;54(5):472-82.
19. Lin CY, Casey E, Herman DC, Katz N, Tenforde AS. Sex differences in common sports injuries. PM&R. 2018 Oct 1;10(10):1073-82
20. Collins JE, Katz JN, Donnell-Fink LA, et al. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med 2013;41:544–9.
21. Tan SHS, Lau BPH, Khin LW, et al. The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions: a systematic review and meta-analysis. Am J Sports Med 2016;44:242–54.
22. Coen SE, Rosenberg MW, Davidson J. “It’s gym, like g-y-m not J-i-m”: exploring the role of place in the gendering of physical activity. Soc Sci Med 2018;196:29–36.
23. Coen SE, Davidson J, Rosenberg MW. ‘Where is the space for continuum?’ Gyms and the visceral “stickiness” of binary gender. Qual Res Sport Exerc Health 2020:1–17.
24. Coen SE, Davidson J, Rosenberg MW. Towards a critical geography of physical activity: emotions and the gendered boundary-making of an everyday exercise environment. Trans Inst Br Geogr 2020;45:313–30.
25. Parsons JL, Ripat J. Understanding the experiences of girls using a high school weight room. PHE Journal 2020;86.
26. Canadian Institutes of Health Research, Institute of Gender and Health. What is gender? What is sex? 2014. Available: http://www. cihr-irsc.gc.ca/e/48642.html
27. Springer KW, Mager Stellman J, Jordan-Young RM. Beyond a catalogue of differences: a theoretical frame and good practice guidelines for researching sex/gender in human health. Soc Sci Med 2012;74:1817–24.
28. Fausto-Sterling A. Sex/gender: Biology in a social world. Routledge, 2012.
17 medicine & performance football www.fmpa.co.uk
HORMONAL CONTRACEPTIVES & FOOTBALL
DR TESSA R FLOOD PHD, PROFESSOR KIRSTY
What are hormonal contraceptives?
Hormonal contraceptives (HC) contain exogenous [external] synthetic hormones that act via negative feedback on gonadotrophic hormones resulting in the chronic downregulation of the hypothalamic-pituitary-ovarian axis and endogenous [internal] ovarian sex hormones. The long-term reduction of endogenous oestrogen and progesterone [the ovarian sex hormones] removes the cyclic fluctuations in these hormones associated with the phases of the menstrual cycle. By inhibiting the production of the ovarian hormones, HC reduce the chance of pregnancy by thickening cervical mucus, thinning the lining of the endometrium, and inhibiting ovulation. HC are designed to prevent pregnancy but are also used for a variety of other reasons, for example: to alleviate symptoms of dysmenorrhea (painful periods), lighten or prevent bleeding, prevent acne, reduce variation in cycle lengths, and to treat other medical issues. When discussing athletic performance and contraceptive choices, it is important to remember that it is a women’s right to choose to take HC.
How common is hormonal contraceptive usage?
J ELLIOTT-SALE PHD
HC are estimated to be used by around 49% of athletes1 in the United Kingdom (UK) and around 30% of the general population2. In a recent audit of the Women’s Super League in the UK, 28% of players reported current hormonal contraceptive use with 43% being previous users.
What are the most common types of hormonal contraceptives?
Common types of HC in the UK include the combined contraceptive pill (OCP), progestogen-only pill (mini-pill), patch, vaginal ring, implant, injection, and intrauterine systems. The use of these HC within sport depends on numerous factors, including the location [country] of the athlete. In the UK combined monophasic OCPs are available from pharmacies by prescription and are the most common type of HC used. Table 1 shows the contraceptive types and brand names available in the UK.
A cis gendered naturally menstruating women (cycle length 21-35 days) will experience menstruation (also known as menses or having their period) once per menstrual cycle. A period is the shedding of the endometrium layer, which has been built and sustained to allow a fertilised egg to embed. Many women taking HC still bleed; however, these are called withdrawal bleeds and occur due to the fluctuations in synthetic hormones. Withdrawal bleeds do not represent physiological menstruation. As Table 1 shows, many women taking HC stop getting a regular bleed and the effects of HC on bleeding patterns are highly individual. Parker et al.,3 reported that, in 21 elite female Women’s Super League players using HC, 29% (n=6) still got a regular withdrawal bleed and 29% (n=6) stopped bleeding, with the other 42% having infrequent bleeds. Athletic populations have reported using the OCP to manipulate the timing of or omit the withdrawal bleed to reduce the perceived and actual impact of this bleed on performance1
Pills
Monophasic combined pill
e.g., Microgynon®, Yasmine®, Rigevidon®, Levest, Lucette
Monophasic combined pill (28-day preparations)
e.g., Microgynon® 30 ED, Femodene® ED
Phasic [bi or tri] combined pill
e.g., Logynon
Phasic [bi or tri] combined pill (28-day preparations)
e.g., Logynon® ED, Qlaira®**
Progestogen-only pill
e.g., Norgeston, Cerazette
Cyclic Contraceptives
Vaginal ring
e.g., NovaRing
Patch
e.g., Evra
Long-Acting Reversible Contraceptives
Implant
e.g., Nexplanon®
Injection
e.g., Depo-Provera, Noristerat
Intrauterine System (IUS)
e.g., Mirena®, Jaydees®, Levosert®, Kyleena®
Ethinylestradiol & Progestogen
21 pills per packet (constant hormonal exposure)
7-day pill free break
Yes, in the 7-day break (lighter)
May experience spotting
Ethinylestradiol & Progestogen 28 pills per packet (21 active, 7 inactive) Yes, in the 7 inactive pills
Ethinylestradiol & Progestogen
Ethinylestradiol & Progestogen
21 pills per packet (3 sections with different concentrations of hormones) 7-day pill free break
28 pills per packet (3 or 4 sections with different concentrations of hormones)
Contains active and inactive pills
Progestogen 28 pills per packet, no break between pill packets
Ethinylestradiol & Progestogen
Ethinylestradiol & Progestogen
Each ring lasts 21 days 7-day break
Each patch lasts 7 days (use for 21 days) 7-day break
Progestogen 3 years
Progestogen One injection every 8-13 weeks
Progestogen 3-5 years (depending on brand)
Yes, in the 7-day break (lighter)
May experience spotting
Yes, in the inactive pills
Less Frequent (lighter, less heavy)
May experience spotting
Yes, in the 7-day break (lighter)
Yes, in the 7-day break
Stop or less frequent (lighter)
Irregular or stop (heavier or lighter)
Stop or less frequent (heavier 3-6 months)
*Please note, this is just the general advice on withdrawal bleeds, however, this response is highly individual and can differ both between and within women.
** Qlaira contains 26 active pills and 2 inactive, Logynon® ED contains 21 active and 7 inactive pills
FEATURE
/
Institute of Sport, Manchester Metropolitan University, UK
Type Synthetic Hormones How do you take them? Withdrawal Bleed* Oral Contraceptive
Table 1: Contraceptive types and further information
feature 18
info@fmpa.co.uk
How do hormonal contraceptives work?


HC change the hormonal profile; natural/endogenous oestrogen and progesterone are supressed and are replaced by synthetic ethinylestradiol and progestogen. Figure 1 shows a graphical representation of hormonal profiles that occur when using HC in comparison with a women’s natural menstrual cycle. It is important to note that the amount of synthetic hormone in each brand of contraceptive is different (Table 2) and hence the side effects and impact of HC on an individual can vary. The impact of HC on women are highly individual and there is not a one size fits all option.
Symptoms and Performance
Players taking HC do not have the same hormonal patterns as naturally menstruating women (i.e., eumenorrheic women) therefore players should not experience ‘phased based symptoms’ (i.e., symptoms that correspond with phases of the menstrual cycle). Indeed, HC are often used to minimise or alleviate symptoms of the menstrual cycle. As such, players should try different types of HC if they are experiencing symptoms as it might be that they have not found their best fit yet. Parker et al.,3 showed that negative symptoms (e.g., mood swings, weight gain) were higher in progestogen-only HC compared to combined HC (63 vs.
Figure 1: Example hormonal profiles for different contraceptive types in comparison with the menstrual cycle. Please note this is a graphical representation not measured values.
19 medicine & performance football www.fmpa.co.uk
23%). Progestogen-only contraceptives are prescribed when combined contraceptives are contra-indicated or can be due to personal preference. Their higher rates of self-reported symptoms, compared with combined contraceptives, should be considered when both types are an option. In a recent survey around 40% of athletes who take a monophasic OCP perceived [thought] that their physical performance was reduced during the pill free week in comparison with pill taking weeks, which corresponds to withdrawal bleeding and increased symptomology4
How do hormonal contraceptives affect female footballers?

To date, around 6% of the research in sport and exercise science has been conducted exclusively on women5. Women account for approximately 34% of the participants studied between 2014 and 2020 when you also include studies that have used both men and women. These statistics highlight how little research is conducted on women and, as such, how little we know about female athletes and women footballers. Most studies in women have failed to account for hormonal fluctuations of the menstrual cycle or for HC.
Review papers are a type of scientific article that summarise previous research on a particular topic. In addition, they often comment on how good [research quality] the studies were. They can be useful for getting a broad overview on a topic and a sense of how much confidence practitioners should have in the findings from previous studies.
A recent review paper6 - published in 2020 - included 30 studies comparing performance in women taking OCPs and naturally menstruating women (n=597 participants) and 24 studies comparing pill phase and pill free phase in women taking OCPs (n=221 participants). A review on chronic adaptations to strength
training7 - published in 2019 - consisted of 2 studies comparing women taking OCPs and naturally menstruating women (n=59 participants). In a review on recovery following exercise induced muscle damage8 – published in 2022 - comparing women taking OCP and women with a natural menstrual cycle 4 studies were included (n=66 participants). As illustrated by the small number of studies included in these reviews more research is needed in women on sex-specific factors including the effects of HC on sport and exercise outcomes so that we can use these data to provide evidence-based practice for use in elite women’s football.
Performance
Data6 - from multiple research studies that compared performance (strength and endurance outcomes) changes in women taking OCP between the pill and pill-free days and between OCP users and naturally menstruating women - concluded that there was no difference in performance between the pill phase and the pill-free phase6. In comparison to naturally menstruating women a ‘trivial’ [extremely small] reduction in performance was seen in OCP users. However, the real life implications of these findings are likely to be (i) small and
therefore not meaningful and (ii) will not affect every OCP user6. While, using OCPs might exert a slightly negative impact on performance the size and inconsistency of this effect between studies and between women, support consideration of an individual’s response and requirements of each player.
Chronic Resistance Training
A recent review paper compared the effect of OCPs on chronic strength adaptations between naturally menstruating women and women taking an OCP7. In the two studies reviewed, no differences were seen between the OCP users and naturally menstruating women following +10-weeks of resistance training. Since this paper was published, additional studies have also showed no differences in strength adaptations9–11. One study suggested impairment in muscle gain with OCP use but that this impairment was not large enough to impact strength adaptations in comparison with naturally menstruating women12
Recovery
Four studies have compared recovery from exercise induced muscle damage in women taking OCPs and naturally menstruating women8. Collectively their data showed
Brand Ethinylestradiol (concentration) Progestogen type Progestogen (concentration) Generation Microgynon® 30 mcg Levonorgestrel 0.15 mg 2nd Levest 30 mcg Levonorgestrel 0.15 mg 2nd Millinette 30 ® 30 mcg Gestodene 0.075 mg 3rd Yasmine ® 30 mcg Drospirenone 3.0 mg 4th Lucette® 30 mcg Drospirenone 3.0 mg 4th
feature 20 info@fmpa.co.uk
Table 2: Example Monophasic Combined Oral Contraceptive pills available in the UK for each generation.
that recovery was slightly impaired in OCP users compared with naturally menstruating women. This impairment was shown by a potential for lowered muscle strength, elevated markers of muscle damage, and greater perceived muscle soreness. However, the size and variability of the effect between studies and between women, support consideration of an individual’s response and requirements of each player.
Quality of the research
As well as a lack of research in women, there is also an absence of high quality [credible] research. In the recent review on exercise performance in women taking OCP6, 64% of papers were deemed medium or low quality. These studies had hormonal contraceptive specific methodological issues. For example, some studies grouped different HC together, despite the different hormonal profiles as shown in Figure 1. This makes it difficult to see the effect different HC have on performance, strength, or recovery. In addition, the review papers above7,8 didn’t examine the methods regarding hormonal contraceptive specific methodological issues (i.e., types/ brand of HC) which can make it difficult to
References
draw robust conclusions for players and practitioners. It is also important to consider that all the studies listed above have focused on OCP use and none of the other types listed in Table 1. Due to differences in these contraceptive methods, we cannot generalise findings in OCPs to other HC.
Relevance for practitioners
- From a practical viewpoint, the group effects seen in performance and recovery are ‘trivial’ and variable across studies and between women and therefore warrants no general guidance on HC in sport.
- Each player should consider all relevant factors (physical, emotional, practical, financial and health related aspects) including their own response to and requirement for HC and that individuals do not solely make their decision to use or not use HC based on the findings in the literature.
Why don’t we know more?
In 2023, with many players choosing to use HC it is frustrating that we do not more about how HC impact performance. One of the difficulties faced with the range of HC available to women (Table 1) is the differences in type of hormone and
concentration of these hormones. Within OCPs for example, there are four different generations of OCP, each generation has a different synthetic progestogen and concentration. Table 2 highlights the differences between monophasic OCP brands. Second generation OCPs are used majority of research as they have the highest prevalence.
Conclusions
The main take home messages are,
• Many players choose to use HC as a convenient method to provide contraception.
• In many cases, this reduces or alleviates menstrual cycle related symptoms and eliminates or lightens bleeding making it a popular choice in sport.
• Research suggests that performance is stable across OCP phases, but that more high-quality research is needed into different types of HC to provide guidelines for practitioners and players.
• Whilst there is some evidence for decreased performance and recovery in comparison to athletes with a natural menstrual cycle, this reduction is ‘trivial’ and highly variable between women and the use of HC should be made on what is best overall for that player.
1. Martin D., Sale C., Cooper SB., Elliott-Sale KJ. Period Prevalence and Perceived Side Effects of Hormonal Contraceptive Use and the Menstrual Cycle in Elite Athletes. Int J Sports Physiol Perform. 2018;13(7):926-932. doi:10.1123/ijspp.2017-0330
2. Cea-Soriano L, Garcia Rodriguez LA, Machlitt A, Wallander MA. Use of prescription contraceptive methods in the UK general population: a primary care study. BJOG An Int J Obstet Gynaecol. 2014;121(1):51-53. doi:10.1111/1471-0528.12465
3. Parker LJ, Elliott-Sale KJ, Hannon MP, Morton JP, Close GL. An audit of hormonal contraceptive use in Women’s Super League soccer players; implications on symptomology. Sci Med Footb. 2022;6(2):153-158. doi:10.1080/24733938.2021.1921248
4. Ekenros L, von Rosen P, Solli GS, et al. Perceived impact of the menstrual cycle and hormonal contraceptives on physical exercise and performance in 1,086 athletes from 57 sports. Front Physiol. 2022;13(August):1-13. doi:10.3389/fphys.2022.954760
5. Cowley ES, Olenick AA, McNulty KL, Ross EZ. “Invisible Sportswomen”: The Sex Data Gap in Sport and Exercise Science Research Women Sport Phys Act J. 2021;29(2):146-151. doi:10.1123/WSPAJ.2021-0028
6. Elliott-Sale KJ, McNulty KL, Ansdell P, et al. The Effects of Oral Contraceptives on Exercise Performance in Women: A Systematic Review and Meta-analysis. Sport Med. 2020;50:1785–1812. https://doi.org/10.1007/s40279-020-01317-5
7. Thompson BM, Drover KB, Stellmaker RJ, Sculley D V., Janse de Jonge XAK. The effect of the menstrual cycle and oral contraceptive cycle on muscle performance and perceptual measures. Int J Environ Res Public Health. 2021;18(20). doi:10.3390/ijerph182010565
8. Glenner-Frandsen A, With C, Gunnarsson TP, Hostrup M. The Effect of Monophasic Oral Contraceptives on Muscle Strength and Markers of Recovery After Exercise-Induced Muscle Damage: A Systematic Review. Sports Health. 2022;XX(X):1-10. doi:10.1177/19417381221121653
9. Romance R, Vargas S, Espinar S, et al. Oral Contraceptive Use does not Negatively Affect Body Composition and Strength Adaptations in Trained Women. Int J Sports Med. 2019;40(13):842-849. doi:10.1055/a-0985-4373
10. Sung ES, Han A, Hinrichs T, Vorgerd M, Platen P. Effects of oral contraceptive use on muscle strength, muscle thickness, and fiber size and composition in young women undergoing 12 weeks of strength training: a cohort study. BMC Womens Health. 2022;22(1):1-10. doi:10.1186/s12905-022-01740-y
11. Dalgaard LB, Jørgensen EB, Oxfeldt M, et al. Influence of Second Generation Oral Contraceptive Use on Adaptations to Resistance Training in Young Untrained Women. J Strength Cond Res. 2022;36(7):1801-1809. doi:10.1519/JSC.0000000000003735
12. Riechman SE, Lee CW. Oral Contraceptive Use Impairs Muscle Gains in Young Women. J Strength Cond Res. 2022;36(11):3074-3080 doi:10.1519/JSC.0000000000004059
21 medicine & performance football www.fmpa.co.uk

IS TECHNOLOGY IN FOOTBALL ADJUSTED FOR WOMEN?
FEATURE / DR KATRINE OKHOLM KRYGER*
Introduction
Women’s football is and has been experiencing rapid growth at both elite and amateur level. In parallel, the sports technology market is growing. Technology is a necessity in football to develop designs for player uniforms, balls, boots, monitoring, etc. However, the standard product in football has traditionally been designed with the male player as a starting point and women’s football has most often used the same design for lack of an alternative. This article summarises a recently published article led by the Dr Katrine Okholm Kryger (Associate Professor, St Mary’s University, Twickenham, England). The article has coauthors from both the world of research and the world of football - including Leah Williamson (captain of the Lionesses and Arsenal WFC) as well as employees from the English national team and Women’s Super League clubs.
This summary focuses specifically on player clothing, football boots, pitches,
and balls as well as tracking equipment. The original article also discusses other topics such as sports bras, apps to track the player’s menstrual cycle, medical equipment, and sports-friendly menstrual pads/tampons. If these are interested, we refer to the article:
Okholm Kryger, K, Thomson, A, Tang, A, Brown, N, Bruinvels, G, Rosenbloom, C, Carmody, S, Williamson, L, Datson, N, Jobson, E, and Mehta, R. Technology in elite women’s football. Progressions made and barriers faced. Sports Engineering, 25
It is common knowledge that football technology is designed with a ‘default’ focus on men. This fact is not specific to football and is seen in many other professions such as aerospace, where toilets and spacesuits were only recently adapted for female astronauts1,2. Technology in football is a huge industry and has been developed for decades for men, while women’s football has used the same kits, balls, boots, etc. without consideration or adaptation to body shape and needs. This came with fit and
discomfort issues as mentioned recently by female footballers in the media, who demand adjustments for them and their specific needs3–5. We, therefore, reviewed essential products used by football player, with a specific focus on the needs of women’s football.
What about the football kit?
The major sports brands first introduced a kit adapted to the women’s fit in 2019 for the FIFA World Cup. However, one specific aspect of the kit still provokes debate – the colour of the players’ shorts3. The female players at the club usually play in the same colour scheme as their male counterparts, but players have expressed dissatisfaction with this in the media. Their concern stems from the concern of bleeding through light shorts during menstruation. This debate is not unique to football and has been discussed in other sports such as tennis and rugby as well6,7. Consequently, several teams (e.g., Manchester City and the England women’s national team)

23 feature www.fmpa.co.uk medicine & performance football
have announced changes so that female players no longer need to wear brightly coloured shorts. The authors argue that this is an easy modification to apply in both amateur and elite clubs, and suggest that clubs should consider a darker shorts colour for women and girls’ teams when next negotiating with sponsors on kits.

Football is global and a multicultural sport, with players representing different cultural and religious backgrounds. If a woman wishes to, she can play with a sports hijab. However, this has not always been the case as hijabs were only incorporated into FIFA’s laws in 20148,9. Before this, when FIFA banned the use of a hijab at the time, several incidences had taken place, including one in 2011 where the Iranian national team was forced to lose in a qualifying match for the 2012 Olympics. The ban was reasoned as a concern of increased risk of head and neck injuries, despite the fact that there had never been a reported injury from the use of the hijab8. As a result, the sports technology companies Capsters and Resport proved the safety of wearing sports hijabs during football using scientific evidence. The authors use this example to highlight the importance of using and collaborating with sports technology to ensure that football is for everyone.

What about football boots?
Today, there are no football boots designed specifically for women on offer among larger boot brands10. Women have a different foot shape than men11 and whilst a football boot’s fit is tight around the foot to allow for optimal agility, it is especially essential that the fit is optimal
to reduce the risk of blisters and more serious injuries such as Achilles tendon problems and overload or stress fracture in the forefoot bones10,11. In addition, the number, shape, length and location of studs under the boot are essential for a player to be able to move optimally on the pitch i.e., neither sliding on the ground nor getting stuck to the side. Hence, outsoles are designed to match a surface type (i.e., soft, firm, or artificial grass). However, these guidelines are based on males and not adapted to women’s body weight, muscle mass and increased risk of cruciate ligament injuries10,12,13. Therefore, the advice for now is that women try to find the best fit and choose football boots
based on how they feel they interact with the pitch. Therefore, players should preferably have two to three pairs of boots with different grips, which they can choose from on the day, so that it suits the pitch they are playing on. Women’s boots will be launched by the big manufacturers for the 2023 World Cup.
What about pitches and balls?
Women play on the same pitches and with the same balls as men. There are no major concerns from research or the football world about this, although it is different from many other sports where the game is adjusted between sexes such as in basketball (ball size), handball (ball size) or volleyball (net height). Instead, the concern of the football world and by the authors is focused on pitch quality 14–17. The Women’s Super League is often played in stadia shared with men’s teams from lower leagues who play on Saturday, leading to an eroded and worn-out playing surface for the women’s match played on the following day. Since the quality of the pitch is essential for the quality of the game as well as the players’ risk of injury, it is worrying that the women often do not play on optimally curated pitches.
What about tracking equipment?
Measurement (tracking) is part of everyday life, especially at elite level. Both women and men are usually equipped with, GPS and heartrate measuring devices to analyse their performance. The current standard values used in men’s football are well established, whilst the women’s game
feature 24 info@fmpa.co.uk
still lacks research and consensus 18 Female players express that the equipment is often uncomfortable to wear, such as the GPS device. This sits in a tight vest fitted for a male body, which a female would need to put on over the sports bra. This can alter the fit and, therefore, affect data quality. In addition, the heartrate monitor, which often is a band worn around the waist under the chest can interfere with the band from the sports bra. The authors stress that these are further indicators of a lack of adaptation to the female athlete and a problem yet to be solved.
Key takeaways
• The football world and technology in football have for many years had men’s football as the ‘default’.
References
• Women need adapted technology to optimise performance and minimise the risk of injury.
• Women do not want to play in white/ light coloured shorts.
• Sports hijabs are now allowed as a safe option on the pitch, helping football inclusion and diversity.
• Today, football boots are not adapted to the shape of women’s feet or traction needs, though women’s specific boots are soon to be launched.
• Women are often given lower priority in the provision of pitches and pitch quality, which can affect the quality of play and the risk of injury.
• GPS and heart rate monitors are often uncomfortable and poorly placed on women, which increases the uncertainty in data collected.
Podcasts https://open.spotify.com/ episode/0mRaBeijIJ5c65JcrYy189
https://www.bbc.co.uk/programmes/ p0dp06zy
*Dr Katrine Okholm Kryger Medical Researcher, FIFA, Zurich, Switzerland; Faculty of Sport, Allied Health and Performance Science, St Mary’s University, Twickenham, London UK; Sport and Exercise Medicine, Queen Mary University of London, Sport and Exercise Medicine, London, UK; UEFA Fitness4Football Advisory Group, UEFA, Nyon, Switzerland
1. Benson E, Rajulu S. Complexity of Sizing for Space Suit Applications. In: Duffy VG, editor. Digital Human Modeling. Berlin, Heidelberg: Springer; 2009. p. 599–607. (Lecture Notes in Computer Science).
2. Kahlenberg B, Corroll D, Cristea O, Urquieta E, Bissada N, Jones J. Urologic Innovation in the Spaceflight Environment: Challenges, Opportunities, and Future Directions. Med Res Arch. 2021;9(9):1–18.
3. Garry T. FA to consider white shorts U-turn after England’s women raise period fears. The Telegraph [Internet]. 2022 Jul 9 [cited 2022 Aug 4]; Available from: https://www.telegraph.co.uk/football/2022/07/09/fa-consider-white-shorts-u-turn-englands-women-raiseperiod/
4. Garry T. Why footwear gender gap must be tackled [Internet]. The Telegraph. 2021 [cited 2022 Aug 4]. Available from: https://www. telegraph.co.uk/football/2021/04/23/footwear-gender-gap-must-tackled/
5. Kessel A. If the boot doesn’t fit then female footballers should have an alternative. The Guardian [Internet]. 2018 Jun 20 [cited 2022 Aug 4]; Available from: https://www.theguardian.com/sport/blog/2018/jun/20/boot-fit-female-footballers-marketing-mens
6. Weaving C. Breaking Down the Myth and Curse of Women Athletes: Enough is Enough, Period. Women Sport Phys Act J. 2017 Apr 1;25(1):43–9.
7. Findlay RJ, Macrae EHR, Whyte IY, Easton C, Whyte) LJF (née. How the menstrual cycle and menstruation affect sporting performance: experiences and perceptions of elite female rugby players. Br J Sports Med. 2020 Sep 1;54(18):1108–13.
8. Prouse C. Harnessing the hijab: the emergence of the Muslim Female Footballer through international sport governance. Gend Place Cult. 2015 Jan 2;22(1):20–36.
9. Al Saied N, Creedon P. Chapter 4: Women’s Sports and Fashion in Arab Gulf Countries. In: Fuller LK, editor. Sportswomen’s Apparel Around the World: Uniformly Discussed [Internet]. Cham: Springer International Publishing; 2021 [cited 2022 Feb 28]. p. 69–82. (New Femininities in Digital, Physical and Sporting Cultures). Available from: https://doi.org/10.1007/978-3-030-46843-9_5
10. Thomson A, Wannop JW, Okholm Kryger K. “HEY COACH/DOCTOR/ PHYSIO/PODIATRIST/ DAD/MUM: WHAT FOOTBALL BOOT IS BEST FOR ME”? Aspetar Sports Med J. 2021;10:268–72.
11. Hoey C, Wang A, Raymond RJ, Ulagenthian A, Okholm Kryger K. Foot morphological variations between different ethnicities and sex: a systematic review. Footwear Sci. 2022 Dec 15;0(0):1–17.
12. Thomson A. Same same, but different? Should football boot selection be a consideration after ACLR. Aspetar Sports Med J. 2020;9:50–5.
13. Montalvo AM, Schneider DK, Silva PL, Yut L, Webster KE, Riley MA, et al. ‘What’s my risk of sustaining an ACL injury while playing football (soccer)?’ A systematic review with meta-analysis. Br J Sports Med. 2019 Nov;53(21):1333–40.
14. Mears AC, Osei-Owusu P, Harland AR, Owen A, Roberts JR. Perceived Links Between Playing Surfaces and Injury: a Worldwide Study of Elite Association Football Players. Sports Med - Open. 2018 Aug 20;4(1):40.
15. Roberts JR, Osei-Owusu P, Mears AC, Harland AR. Elite Players’ Perceptions of Football Playing Surfaces: A Qualitative Study. Res Q Exerc Sport. 2020 Apr 2;91(2):239–51.
16. Alba M. U.S. Soccer Star Abby Wambach: Playing on Turf a ‘Nightmare’ [Internet]. NBC News. 2015 [cited 2022 Aug 4]. Available from: https://www.nbcnews.com/storyline/artificial-turf-debate/us-soccer-star-abby-wambach-playing-turf-nightmare-n371906
17. Hill J. Why FIFA Is Snubbing Its Top Women Stars [Internet]. ABC News. 2014 [cited 2022 Aug 4]. Available from: https://abcnews. go.com/Sports/fifa-snubbing-top-women-stars/story?id=25948778
18. Harkness-Armstrong A, Till K, Datson N, Myhill N, Emmonds S. A systematic review of match-play characteristics in women’s soccer. PLOS ONE. 2022 Jun 30;17(6):e0268334.
25 medicine & performance football www.fmpa.co.uk
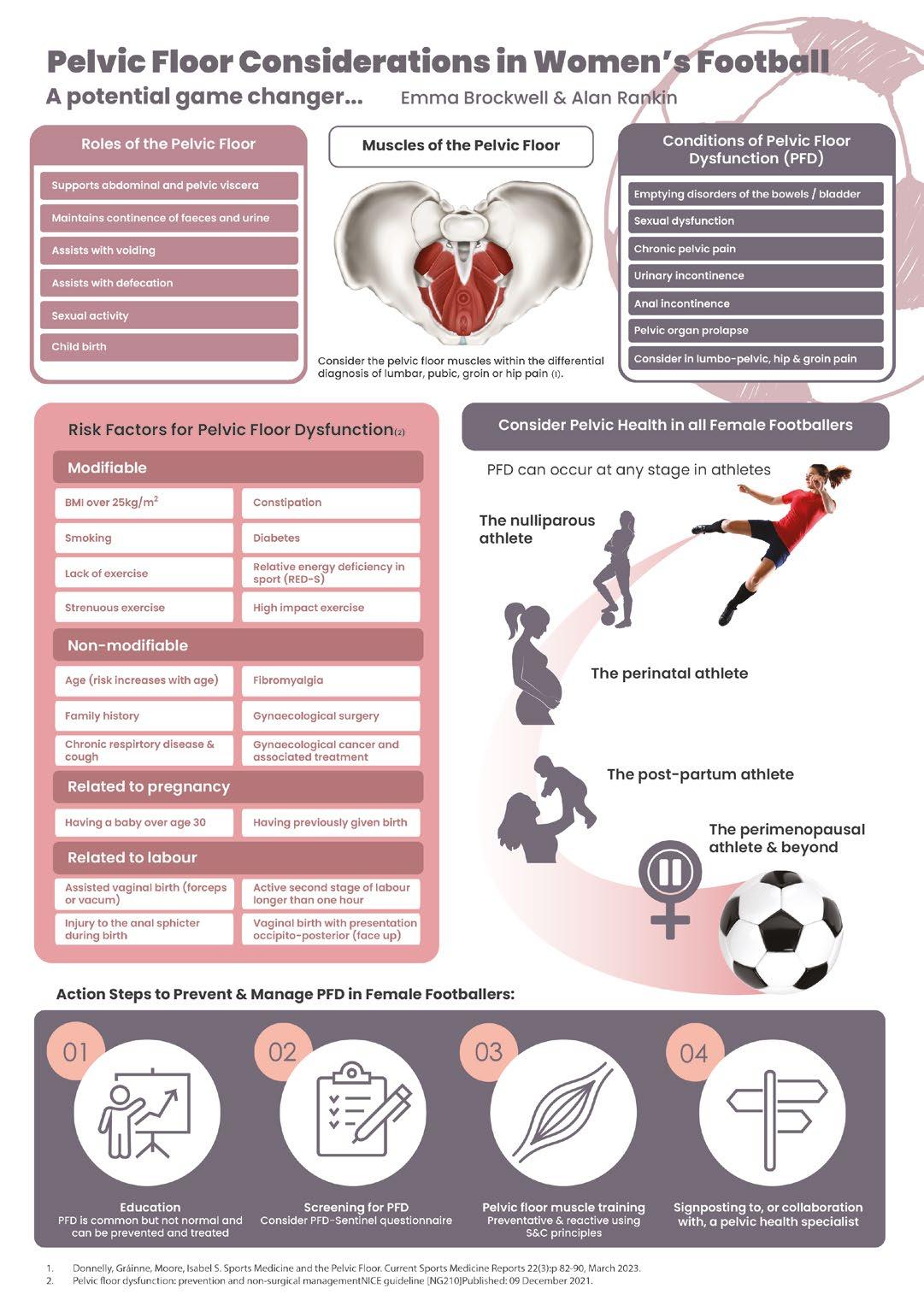
PELVIC FLOOR CONSIDERATIONS A POTENTIAL GAME CHANGER FOR WOMEN’S FOOTBALL?

FIFPRO, the organisation which works as a trade union to unite the voice of professional footballers and their national unions produced a report in 2020 which highlighted that ‘players are the most valuable resource for all football teams and that the athlete is central to the existence of the sport’1. Therefore, for the sport to reach its full potential the player’s potential must be fulfilled. One way of doing this is to identify and implement the best practices in health, safety and performance of the players2. Female footballers, and all those working with them are keen to make this a reality with informed, evidence-based information3. However, females remain significantly underrepresented in sport and exercise science research,4,5 and certain areas remain “wholly underappreciated”, even hidden within sports medicine.
One such area is the pelvic floor and its connected structures and conditions that can result when dysfunctional. Sitting at the base of the pelvic outlet, these structures uniquely serve multiple roles; organ support, sphincteric, lumbopelvic motor control, sexual and sump pump. When this area is not optimally working Pelvic Floor Dysfunction (PFD) can occur. Conditions of PFD include:
• Emptying disorders of the bladder and bowel
•Sexual dysfunction
• Chronic pelvic pain
• Urinary Incontinence
• Anal Incontinence
• Pelvic Organ Prolapse
Typically, PFD has been thought to only affect the perinatal and menopausal
population and not necessarily the ‘athletic female’ population. Whilst it is true that females present with higher prevalence of PFD during these key transitional periods of life, females of all ages who participate in sport / exercise have 3 times the risk of experiencing urinary incontinence for example compared to a non-athletic female6. In fact, amongst female athletes, PFD is one of the most common concerns over the lifespan of female athletes7 and yet it is not considered within key documents that support female athletes’ health8
But, what if, consideration, prevention and management of PFD could optimise and unlock the true potential of all female footballers, see them return to football postpartum better than ever before, future proof their health and in doing so empower
Muscles of the pelvic floor complex
Anterior Urogenital triangle
and inspire girls and women who follow football to take their pelvic health more seriously?
The Pelvic Floor Muscles - an overview There are many overt differences between males and females and the pelvic floor is a great example of this. The male pelvic floor is invaginated by two openings and therefore less compromised than the female’s pelvic floor, which is invaginated by three, the urethra, vagina and anus.
The pelvic floor complex sits within the bony pelvis and includes muscular tissues of the pelvic floor, their neural connections, and the fascial layers surrounding the pelvic floor muscle fibres/fascicles9. The following muscles in the table below are considered to be those that make up the perineum and pelvic floor10:
Bulbosponginosus
Bulbocavernosus
Ischiocavernosus
Superficial transverse perinei
External Urethral Sphincter
Deep transverse perinei
Posterior (anal) triangle
External anal sphincter
Levator Ani Pubococcygeus (which includes puborectalis, pubovisceralis, pubovainalis)
Iliococcygeus
Ischiococcygeus / coccygeus
FEATURE
/ EMMA BROCKWELL
Pelvic Health Physiotherapist BSc (Hons) MCSP HCPC Affiliated POGP Private Practice, Physiomum, Surrey, UK
feature 26 info@fmpa.co.uk

Images courtesy of www.netterimages.com 27 medicine & performance football www.fmpa.co.uk
The pelvic floor muscles are part of the musculoskeletal system and are comprised of predominately 70% slow twitch fibres; and 30% rapid response fibres. It has been recommended to consider pelvic floor muscles within the differential diagnoses of lumbar, pubic, groin or hip pain due in part to the shared muscle attachments of the pelvic floor muscles and groin muscles to the pubic bone and the obturator internus muscles dual functionality; forming part of the pelvic wall (and thus the wider pelvic floor muscle group) as well as being a lateral hip rotator11
Pelvic floor dysfunction - what’s the big deal?
PFD is prevalent amongst the general population with 1 in 4 women reporting symptoms12. Women participating in sport / exercise, especially high impact and strenuous exercise have a higher prevalence of PFD, with 1 in 3 leaking urine during exercise13. 63% of 12–19-year-old amateur soccer players demonstrated objective evidence of UI compared to 25% of similarly aged girls not participating in sports14, whilst a staggering 80% of young, elite, nulliparous gymnasts report symptoms of UI13. UI is not the only type of PFD to affect and impact female athletes. 80% of powerlifters experience symptoms of anal incontinence15 and 7% of triathletes experience pelvic organ prolapse16. However, studies looking at these types of dysfunctions are limited, and further research is required.
The risk factors for PFD can be seen in the table right (modified from NICE Guidelines 202117
The true impact of PFD on female athletes is hugely significant. Many female athletes who experience PFD report feeling negative emotions, predominately embarrassment, followed by fear concern and anxiety18 Strategies to manage symptoms of UI amongst female athletes include the use of pads, prevoiding and limiting fluid intake19. Studies also show that performance is affected and eventually some athletes stop or limit their activity during their sport which is of huge concern20. The societal stigma and taboo surrounding PFD trickles into the sporting world. Shame, inconvenience, fear of surgery and an inadequate knowledge of the pelvic floor and available treatment options may explain why self-disclosure rates for PF symptoms in sports / exercise settings are under reported (<10%)21 and consequently under treated.
Understanding and Managing Pelvic Floor Dysfunction in Young, Nulliparous Female Footballers
It seems highly likely that strenuous, high impact and high intensity exercise may be a risk factor for PFD. The effect of exercise on PFD is yet to be firmly concluded due to knowledge gaps but two hypotheses exist6:
Risk factor type
Modifiable
Risk Factor
Body Mass Index (BMI) over 25kg/m2
Smoking
Lack of exercise
Strenuous exercise
High impact exercise
RED(s)
Constipation
Diabetes
Non-Modifiable
Age (risk increases with age)
Family history
Gynaecological cancer and any treatments for this
Gynaecological surgery
Fibromyalgia
Chronic respiratory disease and cough
Related to pregnancy Being over 30 year when having a baby
Having given birth before their current pregnant
Related to labour Assisted vaginal birth (forceps or vacuum)
A vaginal birth when the baby is lying face up (Occipito-posterior)
An active second stage of labour taking more than 1 hour
Injury to the anal sphincter during birth
1. Exercise training strengthens the pelvic floor
2. Exercise training overloads, stretches, and weakens the pelvic floor
The latter hypothesis is the most widely accepted. If the pelvic floor complex is functioning adequately, it counteracts the increases in intraabdominal pressure and ground force reactions generated during exercise and maintains continence and support. If the pelvic floor complex is not able to counteract these forces, then PFD may occur6. The physiopathology of PFD in female athletes is multi-layered and complex and likely to involve interrelated neuromuscular, biomechanical, morphological, anatomical, and metabolic factors22
There are many actionable steps that can be undertaken by those working with female footballers to prevent, manage and treat PFD:
1. Education - Knowledge can empower the footballer to understand her pelvic health, recognise that symptoms of pelvic floor dysfunction are ‘common but not normal’ and that they can be prevented / treated.
2. Screening - To bridge the gap whereby PFD is under recognised and under treated, screening for PFD key. The PFD-Sentinel23 is a tool recently developed to aid sports medicine clinicians (eg, musculoskeletal/ sports physiotherapists, sports medicine physicians) in referring female athletes to a PFD specialist such as a urogynaecologist or pelvic health physiotherapist. This step could be a starting point towards early PFD specialist management and should be administered on a regular basis.
3. Pelvic floor muscle training (PFMT) PFMT has been shown to improve the signs and symptoms of PFD24. PFMT as part of all female footballers’ training programs is recommended using the strength and conditioning principles of individualisation, specificity, overload and progression11, especially if they are symptomatic of PFD but even if they are asymptomatic given the forces generated through the pelvic floor complex during strenuous sports.
When teaching footballers how to train the pelvic floor, useful cues like ‘squeeze the anus’ or ‘stop the flow of urine’ (25) have been shown to be effective verbal instructions for correctly contracting the pelvic floor muscles. PFMT should target both fibre types of the PFM. Fast twitch fibres will be targeted by rapid maximum voluntary contractions and slow twitch fibres targeted by slower endurance holds11. Encourage the athlete to engage in focussed PFMT of 3 sets of 8 to 12 sustained close to maximum PFM contractions and one to two repetitions of ballistic PFM recruitments repeated three to four times a week6. PFMT should be carried out in as functional position as possible. Signs of breath holding, firmly squeezing glutes or bracing the abdominal wall may be signs that the training is being carried out incorrectly and onward referral to a pelvic health physiotherapist may be indicated.
FEMTECH is now also being used to guide and provide biofeedback which the athletic population may find useful and motivational when introducing PFMT into their programs.
feature 28 info@fmpa.co.uk
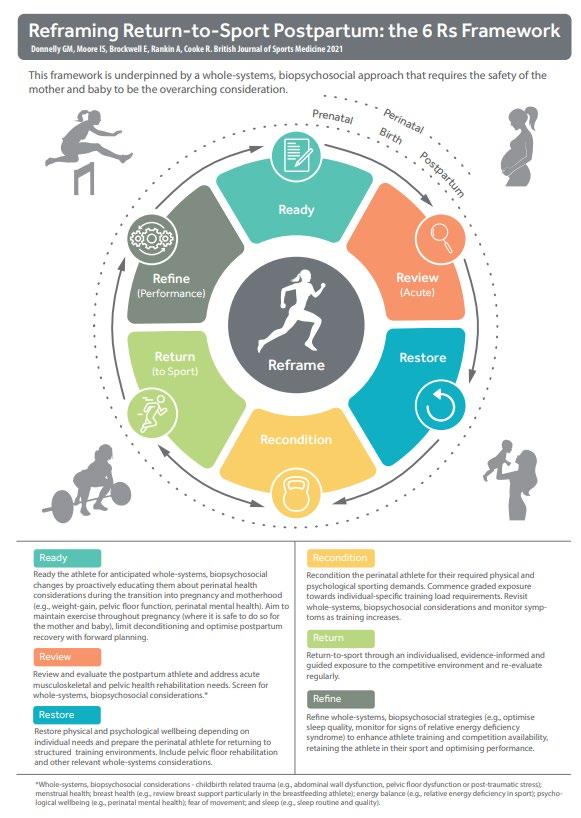
29 medicine & performance football www.fmpa.co.uk
Figure 1: Donnelly GM, Moore IS, Brockwell E, Rankin A, Cooke, R. Reframing return-to-sport postpartum: the 6 Rs framework British Journal of Sports Medicine 2022;56:244-245.
4. Signposting to and collaborating with pelvic health specialists (eg pelvic health physiotherapists / urogynaecologists)
Individualised assessment and PFMT with a pelvic health physiotherapist is recommended as first line management for some PFD presentations such as UI26. Research illustrates that educational programs and verbal cues alone may not be sufficient to improve voluntary contractions of the pelvic floor muscles27. Therefore, including a pelvic health physiotherapist as part of the sports medicine multidisciplinary team who can assess and treat the pelvic floor complex is important.
Surgery is rarely indicated for this population but signposting to a urogynaecologist may occasionally be of benefit if symptoms are not improving with pelvic health physiotherapy alone.
Pelvic Health, Pregnancy and The Mother
Athlete
“Far too often we see women having to make a choice between motherhood and their career. It would be very sad to lose out on the talent we have because they feel like they can’t do both.”
Sydney Leroux Dwyer United States Orlando Pride (Twitter Feb 2020)
Pregnancy and motherhood were once seen to mark the end of a female footballer’s career but in recent years footballers like Alex Morgan, Sara Bjork Gunnarsdottir and Melanie Leupolz have demonstrated that motherhood and a career in football can co-exist particularly if the right support is provided.
Guidance28 supports the safety and benefits of prenatal exercise but this is primarily limited to the general obstetric population. As discussed previously athletes have a higher risk of PFD than non-athletes and there is also an increased prevalence in postpartum women compared to nulliparous women. An online questionnaire of 881 highlighted that when running, 29% of postpartum runners reported symptoms of urinary incontinence. Interestingly, it also showed
that up to 84% reported musculoskeletal pain. Vaginal heaviness and fear of movement were two symptoms that were a barrier to returning to postpartum running29. Postpartum women have also been found to have reduced abdominal wall strength postpartum regardless of delivery which may contribute to poor trunk control, and suboptimal return to sport30. Addressing these concerns as well as considering breast health, physical deconditioning, hormonal changes, psychological well-being, and sleep is essential when returning any postpartum player back to football.
The narrative around perinatal care is changing. Pregnancy and childbirth can be seen as an opportunity to prepare and ready the athlete for impending physical and psychological changes; a proactive rather than reactive approach to athlete care31. Every woman’s recovery timeline can vary and is unique and her postpartum return to sport must be given time and rehabilitation considerations just like any other significant musculoskeletal injury. The 6Rs framework31 (see figure 1) has been proposed to guide multidisciplinary teams in preparing, returning and optimizing perinatal athletes for their sport. It suggests an individualized, wholesystems, biopsychosocial model of care32 and encourages the MDT working with the athlete to include a specialist pelvic health physiotherapist, midwife, obstetric and gynaecological consultants so that all perinatal considerations including pelvic health are catered for. By taking an approach like that suggested within the 6Rs framework, it is likely that we will continue to see women return to their football optimally, successfully, and indeed better and stronger than ever before.
Future-Proofing the female footballer’s pelvic health - The perimenopause and beyond Menopause; defined as the permanent cessation of menses33, typically occurs between the ages of 42 and 58 years. During the early transition
to the menopause, the perimenopause, females experience physiological and hormonal changes that impact on multi body systems including the urogenital system. A decline in estrogen affects the endopelvic fasica, levator ani, and uterosacral ligaments by altering structure and or function34 These changes can cause or exacerbate PFD. Armed with this knowledge, it is important that those working with female footballers educate about these inevitable changes. These changes are unlikely to occur before the footballer’s retirement (although Premature menopause affects 1% of women under the age of 40 years) but encouraging players to adopt a proactive, preventative approach to their pelvic health whilst young, screening them regularly for signs and symptoms of pelvic floor dysfunction and incorporating PFMT into their training programs is essential to futureproof their pelvic, physical and mental health.
Conclusion
Pelvic floor dysfunction is prevalent amongst female footballers. PFD can impact a player’s physical and mental health, affect their performance and potentially be a barrier to play. Knowledge gaps still remain around this health area but it is highly recommended that those working with female footballers screen for signs and symptoms of pelvic floor dysfunction and educate in order to destigmatize and demystify these common but not normal conditions. Expanding the multidisciplinary team to include specialists like pelvic health physiotherapists/ urogynaecologists will enrich and allow for effective measures to prevent and manage symptoms of PFD. By adopting this approach we are one step closer to ensuring that the full potential of all players is reached.

The perinatal period is a time of huge change for female footballers but shouldn’t be a time where female footballers consider leaving the sport because of these changes and uncertainty around how to return to sport optimally (unless they choose to do so). Considering the perinatal period within a Return to sports framework, like the 6Rs allows for a proactive approach that will return the player back to her sport, in hope stronger than ever before.
Beyond the player, pelvic floor issues are of huge concern to all women working within football, including coaches and referees and a similar approach to their pelvic health should be adopted. Beyond football, pelvic floor dysfunction is a public health concern. Most women ignore or even put up with pelvic floor dysfunction. Many consider it too embarrassing to discuss, many do not realize that there is so much that can be done to prevent and manage symptoms and the fallout from this is huge! If football takes the lead in pelvic health management and opens the conversation around pelvic health the impact on female health worldwide could be remarkably positive and a likely game changer for 51% of the world’s population!
feature 30 info@fmpa.co.uk
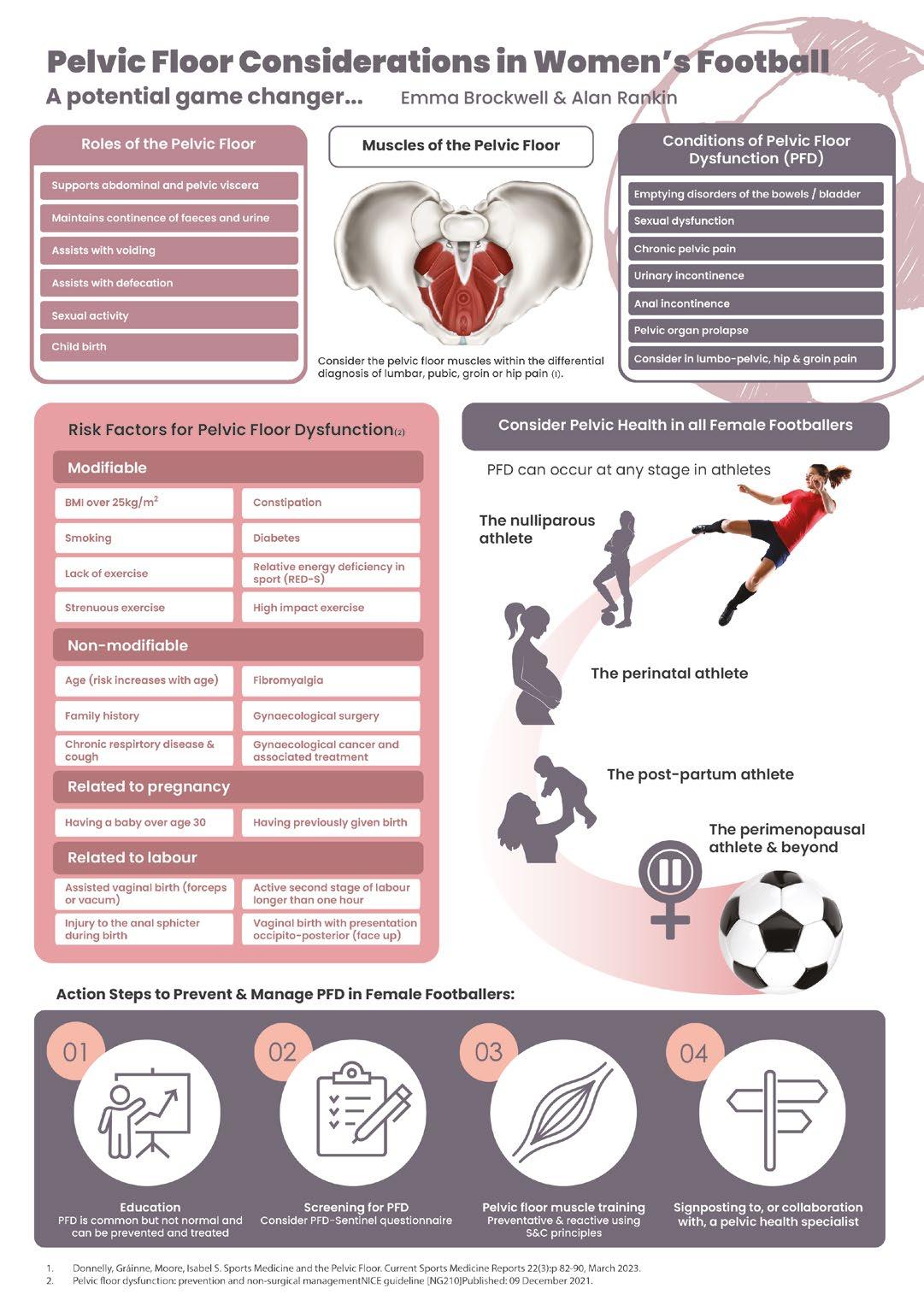
31 medicine & performance football www.fmpa.co.uk
References
1. FIFA’s ‘Raising our game 2020 women’s football Report’ https://fifpro.org/media/1n4mp3ht/fifpro-womens-report_eng-lowres.pdf
2. Macall A, Mountjoy M, Witte M, Serner A & Massey A (2022) Driving the future of health and performance in Women’s football, Science and Medicine in Football, 6:5, 545-546, DOI: 10.1080/24733938.2022.2152543
3. J. J. Forsyth, L. Sams, A. D. Blackett, N. Ellis & M.-S. Abouna (2022): Menstrual cycle, hormonal contraception and pregnancy in women’s football: perceptions of players, coaches and managers, Sport in Society, DOI: 10.1080/17430437.2022.2125385
4. Bruinvels G, Burden RJ, McGregor AJ, et alSport, exercise and the menstrual cycle: where is the research?British Journal of Sports Medicine 2017;51:487-488
5. Cowley, E. S., Olenick, A. A., McNulty, K. L., & Ross, E. Z. (2021). “Invisible Sportswomen”: The Sex Data Gap in Sport and Exercise Science Research, Women in Sport and Physical Activity Journal, 29(2), 146-151. Retrieved Mar 28, 2023, from https://doi.org/10.1123/wspaj.2021-0028
6. Bø K, Nygaard IE. Is Physical Activity Good or Bad for the Female Pelvic Floor? A Narrative Review. Sports Med. 2020 Mar;50(3):471-484. doi: 10.1007/s40279-01901243-1. PMID: 31820378; PMCID: PMC7018791
7. Joy EA, Van Hala S, Cooper L. Health-related concerns of the female athlete: a lifespan approach. Am Fam Physician. 2009 Mar 15;79(6):489-95. PMID: 19323362
8. Female Athlete Issues for the Team Physician: A Consensus Statement-2017 Update. Curr Sports Med Rep. 2018 May;17(5):163-171. doi: 10.1249/ JSR.0000000000000482. PMID: 29738322
9. Frawley H, Shelly B, Morin M, et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourology and Urodynamics. 2021;40:1217‐1260. https://doi.org/10.1002/nau.24658
10. Gilpin, S A, Gosling, J A, Smith, A R B et al (1989). ‘The pathogenesis of genito-urinary prolapse and stress incontinence of urine: A histological and histochemical study’, British Journal of Obstetrics and Gynaecology, 96, 31-38
11. Donnelly GM, Moore IS. Sports Medicine and the Pelvic Floor. Curr Sports Med Rep. 2023 Mar 1;22(3):82-90. doi: 10.1249/JSR.0000000000001045. PMID: 36866951
12. Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ; Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008 Sep 17;300(11):1311-6. doi: 10.1001/jama.300.11.1311. PMID: 18799443; PMCID: PMC2918416.
13. Teixeira RV, Colla C, Sbruzzi G, Mallmann A, Paiva LL. Prevalence of urinary incontinence in female athletes: a systematic review with meta‐analysis. Int Urogynecol J. 2018;29:1717‐1725. 10.1007/s00192-018-3651-1.
14. Fernandes A, Fitz F, Silva A, Filoni E, Filho JM. 0016 Evaluation of the prevalence of urinary incontinence symptoms in adolescent female soccer players and their impact on quality of life. Occup Environ Med. 2014;71(Suppl 1):A59–A60.
15. Skaug KL, Engh ME, Frawley H, Bø K. Prevalence of Pelvic Floor Dysfunction, Bother, and Risk Factors and Knowledge of the Pelvic Floor Muscles in Norwegian Male and Female Powerlifters and Olympic Weightlifters. J Strength Cond Res. 2022 Oct 1;36(10):2800-2807. doi: 10.1519/JSC.0000000000003919. Epub 2020 Dec 3. PMID: 33278274.
16. Yi J, Tenfelde S, Tell D, Brincat C, Fitzgerald C. Triathlete Risk of Pelvic Floor Disorders, Pelvic Girdle Pain, and Female Athlete Triad. Female Pelvic Med Reconstr Surg. 2016 Sep-Oct;22(5):373-6. doi: 10.1097/SPV.0000000000000296. PMID: 27403753.
17. Pelvic floor dysfunction: prevention and non-surgical management NICE guideline [NG210]Published: 09 December 2021
18. Culleton-Quinn E, Bø K, Fleming N, Mockler D, Cusack C, Daly D. Elite female athletes’ experiences of symptoms of pelvic floor dysfunction: A systematic review. Int Urogynecol J. 2022 Oct;33(10):2681-2711. doi: 10.1007/s00192-022-05302-6. Epub 2022 Aug 30. PMID: 36040507; PMCID: PMC9477953.
19. Wikander L, Kirshbaum MN, Waheed N, Gahreman DE. Urinary Incontinence in Competitive Women Weightlifters. J Strength Cond Res. 2022 Nov 1;36(11):3130-3135. doi: 10.1519/JSC.0000000000004052. Epub 2021 Jun 3. PMID: 34100787; PMCID: PMC9592169.
20. Dakic JG, Cook J, Hay-Smith J et al. Pelvic floor disorders stop women exercising: a survey of 4556 symptomatic women. J Sci Med Sport 2021;24(12):1211-1217. doi:10.1016/j.jsams.2021.06.003.
21. Dakic JG, J. Hay-Smith, J. Cook, et al., Screening for pelvic floor symptoms in exercising women: a survey of 636 health and exercise profess..., Journal of Science and Medicine in Sport, https://doi.org/10.1016/j.jsams.2023.01.008
22. Rebuildo 2018 Rebullido TR, Chulvi-Medrano I, Avery D. Pelvic floor dysfunction in female athelte. Strength and Conditioning Journal 2018
23. Giagio S, Salvioli S, Innocenti T, et al PFD-SENTINEL: Development of a screening tool for pelvic floor dysfunction in female athletes through an international Delphi consensus British Journal of Sports Medicine Published Online First: 14 December 2022. doi: 10.1136/bjsports-2022-105985
24. 86. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018; 10:Cd005654
25. Dar G, Ami N. What us the most effective verbal instruction for correctly contracting the pelvic floor muscles? Neurology and urodynamics 37(8) 2018
26. Abrams P, Andersson KE, Apostolidis A, Birder L, Bliss D, Brubaker L, Cardozo L, Castro-Diaz D, O’Connell PR, Cottenden A, Cotterill N, de Ridder D, Dmochowski R, Dumoulin C, Fader M, Fry C, Goldman H, Hanno P, Homma Y, Khullar V, Maher C, Milsom I, Newman D, Nijman RJM, Rademakers K, Robinson D, Rosier P, Rovner E, Salvatore S, Takeda M, Wagg A, Wagner T, Wein A; members of the committees. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: EVALUATION AND TREATMENT OF URINARY INCONTINENCE, PELVIC ORGAN PROLAPSE AND FAECAL INCONTINENCE. Neurourol Urodyn. 2018 Sep;37(7):2271-2272. doi: 10.1002/nau.23551. Epub 2018 Aug 14. PMID: 30106223.
27. de Andrade RL, Bø K, Antonio FI, Driusso P, Mateus-Vasconcelos ECL, Ramos S, Julio MP, Ferreira CHJ. An education program about pelvic floor muscles improved women’s knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: a randomised trial. J Physiother. 2018 Apr;64(2):91-96. doi: 10.1016/j. jphys.2018.02.010. Epub 2018 Mar 21. PMID: 29574170.
28. Mottola MF, Davenport MH, Ruchat S, et al 2019 Canadian guideline for physical activity throughout pregnancy British Journal of Sports Medicine 2018;52:1339-1346
29. Moore IS, James ML, Brockwell E, Perkins J, Jones AL, Donnelly GM. Multidisciplinary, biopsychosocial factors contributing to return to running and running related stress urinary incontinence in postpartum women. Br J Sports Med. 2021;55(22):1286-1292. do i:10.1136/bjsports-2021-104168
30. Deering RE, Cruz M, Senefeld JW, Pashibin T, Eickmeyer S, Hunter SK. Impaired trunk flexor strength, fatigability, and steadiness in postpartum women. Med Sci Sports Exerc. 2018;50(8):1558-1569.doi:10.1249/mss.0000000000001609
31. Donnelly GM, Moore IS, Brockwell E, Rankin A, Cooke R. Reframing return-to-sport postpartum: the 6Rs framework. Br J Sports Med. 2022;56(5):244-245. doi:10.1136/ bjsports-2021-104877
32. Donnelly GM, Brockwell E, Rankin A. Beyond the musculoskeletal system: considering whole-systems readiness for running postpartum. J Women’s Health Phys Ther 2021;46
33. Santoro N, Roeca C, Peters BA, Neal-Perry G. The Menopause transition: signs, symptoms, and management options. J Clin Endocrinol Metab. 2021;106(1):1–15. doi:10.1210/clinem/dgaa764.
34. Rothschild, Carey E. PT, DPT1; Collingwood, Tara Gidus MS, RDN, CSSD, LDN, ASCM-CPT2. Maximizing Running Participation and Performance Through Menopause. Journal of Women’s & Pelvic Health Physical Therapy 47(2):p 133-143, April/June 2023. | DOI: 10.1097/JWH.0000000000000276
32 info@fmpa.co.uk medicine & performance football feature


PREGNANCY IN FOOTBALL, A BLANKET BAN?
FEATURE / EVA FERRER MD
Introduction
Given that some national guidelines advise pregnant women to avoid football while pregnant1,5 it may be easy to ignore this topic and avoid any discussion, giving it a blanket ban. However, as with most things in life, it is not always clear cut and as something we will feasibly encounter working in women’s football, we should seek to understand the landscape better.
State of the Art


Professionalism of the women’s game is growing rapidly and research into specific health and performance issues for the players is accelerating. We need to be up to date with the latest literature and open to changing developments in all areas, including
pregnancy and the postpartum period.
The main question I will address in this article is; ‘how can pregnancy and postpartum period, be managed for a football player?’
Despite a growing amount of research literature in women’s football, not many studies on pregnancy in postpartum in sport have been published 2,7 and even less, on football players. Given such a lack, it is no surprise that there are no globally accepted, scientifically validated recommendations or approach to managing a pregnant/postpartum athlete, regardless if in football or other sports. Research is therefore clearly urgently needed looking into health issues related to pregnancy and football,
and how to manage each individual situation. Nevertheless, while there is limited research, this is something that we as practitioners can and likely will come across and must deal with.
What Should We Consider For The Pregnant Footballer?
Contraindications and health benefits
We need to remember that in the absence of contraindications (Figure 1 and 2) being an active mum is associated with multiple health positive effects 1,2,3 that can range from physical benefits such as decrease risk of pre-eclampsia 18,19 or urinary incontinence to mental health benefits such improving depressionrelated symptoms.
Barça Innovation Hub of Football Club Barcelona. Barcelona (Spain) Sports Medicine Unit, Hospital Clínic-Sant Joan de Déu. Barcelona (Spain)
Figure 1: Absolute contraindications *Adapted from Canadian guideline for physical activity throughout pregnancy
Incompetent cervix Uncontrolled DM I, thyroid disease or hypertension Placenta previa after 28 weeks Intrauterine Growth Restriction High-order multiple pregnancy Other serious CV, respiratory or systemic disorders Unexplained persistent vaginal bleeding Rupture membranes, premature labour Rupture membranes, premature labour Malnutrition Recurrent pregnancy loss Gestational hypertension Mild/modarate CV or respiratory disease Symptomatic anaemia History of spontaneous pre-term birth Other significant medical conditions Twin pregnancy after the 28th week Eating disorder 35 feature www.fmpa.co.uk medicine & performance football
Figure 2: Relative contraindications. *Adapted from Canadian guideline for physical activity throughout pregnancy
*Reproduced by permission of
Anatomic, metabolic and physiological changes and adaptations
For the athlete healthcare professional, our interest should be specially focused on the physiological and anatomical changes that occur during pregnancy6. These must be considered when designing the physical activity program10. Each woman and each pregnancy can and most likely will be different.
Maternal physiological adaptations to pregnancy have to be considered by modifying exercise routines and/or activity patterns. Changes in normal metabolic processes exist to accommodate the needs of the developing foetus (Figure

3). Pregnancy entails great changes in maternal hemodynamics, such as increase in blood volume, heart rate, and stroke volume, and a decrease in systemic vascular resistance4. The respiratory system can undergo changes due to anatomical and functional alterations2 Regarding hormones during pregnancy progesterone, relaxin and oestradiol are responsible for softening pelvic ligaments for childbirth9,21. Oestradiol affects the structure of bone, muscle, tendon and ligaments. Bone and muscle receive positive feedback improving its function while in tendons and ligaments oestrogens decreases stiffness that affects directly the risk of injury and the level of performance20
The anatomical changes that occur during the pregnancy period have an impact on how women’s ability to perform physical activity, exercise or sport. Changes in trunk mobility and motion control due to increased mass and dimensions, may reduce the functional range of motion of the trunk segments14 Due to the need to accommodate the growing foetus, the uterus expands and lumbar lordosis progresses displacing the centre of gravidity. This fact will change all the possibility of maintaining previous balance, which will be now poorer, and will need adaptations to compensate it. Wider stance and changing the step length will be a mechanical adaptation to occur in a progressive way14 The hip, related to the expansion of the uterus and the widening of
Figure 3: Main physiological adaptations of the mother’s body during pregnancy (HR, heart rate; VO2, oxygen consumption)
the author
feature 36 info@fmpa.co.uk
the pubic symphysis will increase its flexion angle. However, not only does the pelvic area go through changes, the joints do too. Ligamentous laxity can affect stability of all weight-bearing joints from the pelvis to the feet15. The knees will increase their flexion but will reduce the extension, which will be responsible for biomechanical changes when walking or running. The decrease of ankle dorsiflexion and plantar flexion can also be an issue for a correct ability to move. As pregnancy progresses the body adapts to the changes previously mentioned and in each trimester several outcomes have a higher probability of existing. Some of the highlights are as follows:
First trimester
While exercising, average core body temperature increases by 1.5ºC after 30 min. At what level of exercise and what environmental temperature and humidity the upper limit for maternal core temperature is exceeded is still being studied. There is given evidence that during organogenesis, maternal hyperthermia above 39ºC may be teratogenic11. Caution should be taken to keep core temperature < 39ºC12, the hypothesised teratogenic threshold during pregnancy, while exercising.
Second and third trimester
Studies regarding this period are somehow controversial. Foetal growth restriction (FGR) and insufficient gestational-weightgain are possible negative outcomes that can overcome during this pregnancy period when exercising at levels significantly above recommendations7,17
Some authors suggest that practicing exercise at high-intensity may cause alterations in foetal heart rate (FHR)17 but other publications indicate that vigorous intensity exercise completed into the third trimester appears to be safe for most healthy pregnancies. Due to these dual results, professionals recommend avoiding exercising at a perceived exertion relative to ≥90% maximum heart rate13
Athletes can also experience major symptoms that can limit the possibility to practice. Nausea and vomiting has prevalence rates of between 50% and 80% in early pregnancy3 Fatigue can also be an issue22 as it decreases capacity for physical work.
In general population the prevalence rate of pregnancy-related low back pain (LBP) is estimated to be about 50% during pregnancy while elite athletes experienced a lower prevalence of pregnancy induced LBP compared with non-elite athletes23 probably associated with stronger abdominal musculature. Urinary incontinence is caused by the increase of pressure, pelvic floor distensibility and the bladder volume4
Sport can aggravate the symptoms of incontinence, which can have an average incidence around 26%.
Screening, Exercising & Monitoring
Once the player knows she is pregnant, she is surrounded by doubts around what she can/cannot, should/should not do. The first step to take, should be to collect all the information regarding this pregnancy and previous one(s) (if applicable). To facilitate the process of medical screening1, a useful and accessible tool is the Get
Active Questionnaire for Pregnancy (GAQ-P) (https://csep.ca/2021/05/27/getactive-questionnaire-for-pregnancy/)24 that provides a checklist format of contraindications (both absolute and relative) to maternal exercise. Other specific issues that could be asked for are related to history of eating disorders, previous menstrual function and pelvic floor health. Once cleared and if needed double-checked with the health care professional in charge of the players pregnancy, an individualized program should be established.
Recommendations based on the current medical guidance, are that pregnant players should not continue playing football beyond the first trimester. In the second trimester foetus moves higher and is unprotected by the pelvis, increasing the risk of damage26

Monitoring the player’s activity is a measure that will give the health practitioner information, on any change that could compromise the athlete and the foetus health. At the same time by tracking the different variables it will be easier to individualize and progress the fitness program.
Studies show that transient foetal bradycardia can exist when pregnant elite athletes exercise above 90% of the maximal maternal heart rate; therefore, the pregnant women should avoid exercising over ≥90% MHR27. Borg scale can also be used as a monitoring method but it does not correlate strongly with heart rate, if used it should stay between 12-14 if moderate exercise
37 medicine & performance football www.fmpa.co.uk
is targeted28. During exercise in normal pregnant subjects, there are diminished responses for every respiratory function, reflecting a decrease in pulmonary reserve and inability to exercise anaerobically.16
Considering the aforementioned physiological and anatomical changes of pregnancy, the recommendations for a healthy pregnancy program should follow, from week 1 to week 34 focus in physical condition and strength while from week 35 to delivery mobility, meditation, physical conditioning and strength are the main areas to focus on. Bear in mind, that during the 2nd and 3rd trimester when a pregnant woman is in a supine position the gravid uterus compresses the inferior vena cava, leading to decreased venous central ruturn and can cause a hypotension supine syndrome that usually occurs within 3–10 minutes after lying down.1
Due to the high incidence of urinary incontinence and pelvic floor dysfunction in late pregnancy and the postpartum period24, it is important to include pelvic floor exercise. These should be performed with “Exhale on exertion” to avoid increasing the intraabdominal pressure, when working.
Monitoring should not be limited to the player’s physical condition, mental health and nutritional needs should be followed up too. As mentioned previously, pregnant woman can experience physiological distress, to manage this situation, mental health must be followed as some athletes may feel anxiety regarding returning to a competitive level following childbirth7 On the other hand, ensuring maintenance of hydration and fuelling is also particularly important when practicing physical activity during pregnancy. A good balance between exercise and energy intake is basic for the foetus and the mother’s good health. Gestational Weight Gain (GWG) is an indicator for sufficient energy intake for foetal growth and development24
Postpartum Period And Return To Play (RTP)
After delivery return to play should not be rushed, the possible program to follow should be adapted to the different phases, depending on the individual rehabilitation needs. If pregnancy, labour, and birth has been uncomplicated and the new-mother feels capable while staying in the hospital, she can start rehabilitation focusing in pelvic floor exercises.
Once at home and during the initial postpartum period the clinical guidelines recommend women to gradually return to low-impact exercise, as 12 weeks are required
Figure 4: A proactive and individualised management will help to achieve a secure elite return to play. Although there is little evidence amongst elite athletes, it has even been postulated that some pregnancy-induced physiological changes may enhance exercise potential (30).
for the musculoskeletal soft tissues to heal24
Different authors divide the athlete RTP period in several phases. Donelly and colleagues29 propose the 6 Rs framework, ensuring that all aspects of perinatal athlete performance are considered, these 6 “R” are Ready (1-6 weeks), Review (8-12 weeks), Restore (12-16 weeks), Recondition (+16 weeks), Return and Refine. While Jackson et al24 gives a novel integrative concept to return elite female athletes dividing the post-partum period in “active recovery” focusing in low impact exercises and improving pelvic floor, “training” with increase in load and progressive exposure to impact and finally “performance” with sport specific exercises.
Healthcare professionals need to supervise closely the player’s physical and mental progress and follow some of the issues that are known to be important concerns that can impact on performance7,24,29, summarized in figure 4.
- Lack of sleep
- Pelvic floor disfunction
- Breast feeding
- Mental health
- Altered energy balance
- Increased joint laxity
Conclusions
A multidisciplinary physiological, physical and mental approach is needed to provide the player security and stability during the entire pregnancy and postpartum period. Even though more and more researchers are focusing on this female vital stage, more research is required to advance knowledge and understanding of pregnant and postpartum elite athletes, especially in football.
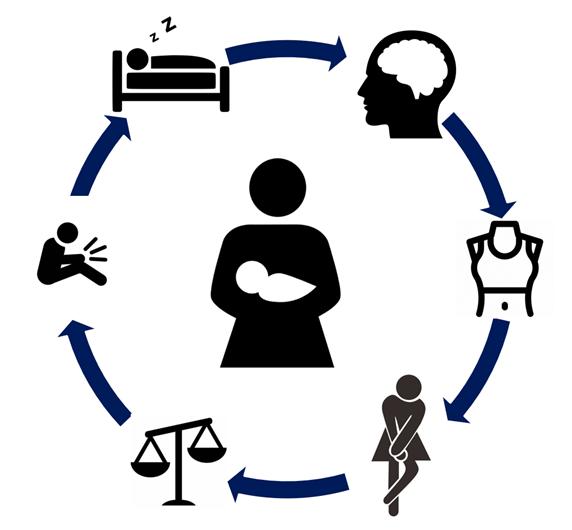
Take-home messages:
- The player needs to continue being active to achieve a healthy pregnancy, for her and her baby.
- Football is a contact sport and that’s an important fact that limits the player to continue playing.
- It is essential to be aware of the changes the players body will suffer.
- Throughout pregnancy individual adaptation will be needed, be cautious but not scared.
- Keep in mind that pregnancy does not finish after 9 months, a post-delivery period exists and that includes return to play.
- A multidisciplinary physiological, physical and mental approach is needed.
feature 38 info@fmpa.co.uk
References
1. Mottola MF, Davenport MH, Ruchat S-M, et al. 2019 Canadian guideline for physical activity throughout pregnancy Br J Sports Med 2018;52:1339–1346.
2. Wieloch N, Klostermann A, Kimmich N, et al. Sport and exercise recommendations for pregnant athletes: a systematic scoping review. BMJ Open Sport & Exercise Medicine 2022
3. Bø K, Artal R, Barakat R, et al. Br J Sports Med 2016;50:1297–1305.
4. Barakat R, Perales M, Garatachea N, et al. Exercise during pregnancy. A narrative review asking: what do we know? British Journal of Sports Medicine 2015;49:1377-1381.
5. Artal R, O’Toole M.Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period BJSM 2003;37:6-12.
6. Solli GS, Sandbakk Øyvind. Training characteristics during pregnancy and postpartum in the world’s most successful cross country skier. Front Physiol 2018 ;9:595.
7. L’Heveder, A.; Chan, M.; Mitra, A.; Kasaven, L.; Saso, S.; Prior, T.; Pollock, N.; Dooley, M.; Joash, K.; Jones, B.P. Sports Obstetrics: Implications of Pregnancy in Elite Sportswomen, a Narrative Review. J. Clin. Med. 2022, 11, 497
8. Soma-Pillay, P.; Nelson-Piercy, C.; Tolppanen, H.; Mebazaa, A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 2016, 27, 89–94
9. Chidi-Ogbolu, N.; Baar, K. Effect of Estrogen on Musculoskeletal Performance and Injury Risk. Front. Physiol. 2019, 9, 1834.
10. A Bump in the Road? The BASES Expert Statement on Pregnant and Postnatal Athletes. The Sport and Exercise Scientist, Issue 74, Winter 2022.
11. Davenport, M.H.; Yoo, C.; Mottola, M.F.; Poitras, V.J.; Garcia, A.J.; Gray, C.; Barrowman, N.; Davies, G.A.; Kathol, A.; Skow, R.J.; et al. Effects of prenatal exercise on incidence of congenital anomalies and hyperthermia: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 116–123.
12. Ravanelli, N.; Casasola, W.; English, T.; Edwards, K.; Jay, O. Heat stress and fetal risk. Environmental limits for exercise and passive heat stress during pregnancy: A systematic review with best evidence synthesis. Br. J. Sports Med. 2019, 53, 799–805.
13. Beetham, K.S.; Giles, C.; Noetel, M.; Clifton, V.; Jones, J.C.; Naughton, G. The effects of vigorous intensity exercise in the third trimester of pregnancy: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019, 19, 281.
14. Gilleard W, Crosbie J, Smith R. Effect of pregnancy on trunk range of motion when sitting and standing. Acta Obstet Gynecol Scand. 2002 Nov;81(11):1011-20
15. Ritchie, J Orthopedic Considerations During Pregnancy. Clinical Obstetrics and Gynecology 46(2):p 456-466, June 2003.
16. Artal,R , Wiswell, R, Romem, Y,Dorey F. Pulmonary responses to exercise in pregnancy, American Journal of Obstetrics and Gynecology,154 (2),1986, 378-383,
17. Salvesen KÅ, Hem E, Sundgot-Borgen J. Fetal wellbeing may be compromised during strenuous exercise among pregnant elite athletes. Br J Sports Med. 2012 Mar;46(4):279-83.
18. Brown, W.J.; Hayman, M.; Haakstad, L.A.H.; Lamerton, T.; Mena, G.P.; Green, A.; Keating, S.E.; Gomes, G.A.O.; Coombes, J.S.; Mielke, G.I. Australian guidelines for physical activity in pregnancy and postpartum. J. Sci. Med. Sport 2022, 25, 511–519.
19. Genest,D, Falcao,S , Gutkowska J, Lavoie J. Impact of exercise training on preeclampsia: potential preventive mechanisms. Hypertension. 2012 Nov;60(5):1104-9
20. Kumar P, Magon N. Hormones in pregnancy. Niger Med J. 2012 Oct;53(4):179-83.
21. Waugh, C, Scott, A. Case Studies in Physiology: Adaptation of load-bearing tendons during pregnancy May2022 Journal of Applied Physiology 2022 132:5, 1280-1289
22. Pugh LC. Childbirth and the measurement of fatigue. J Nurs Meas 1993;1:57–66.
23. Wowdzia JB, McHugh TL, Thornton J, Sivak A, Mottola MF, Davenport MH. Elite Athletes and Pregnancy Outcomes: A Systematic Review and Meta-analysis. Med Sci Sports Exerc. 2021 Mar 1;53(3):534-542
24. Jackson, T; Bostock, E; Hassan, A; Greeves, J; Sale,C Elliott-Sale, K1. The Legacy of Pregnancy: Elite Athletes and Women in Arduous Occupations. Exercise and Sport Sciences Reviews 50(1):p 14-24, January 2022.
25. James, M; Moore, I; Donnelly, Gráinne M., Brockwell, E Perkins, J; Coltman, C. Running During Pregnancy and Postpartum, Part A: Why Do Women Stop Running During Pregnancy and Not Return to Running in the Postpartum Period?. Journal of Women’s Health Physical Therapy 46(3):p 111-123, July/September 2022.
26. Torede, M. Guidelines for safe participation con contact and collision sports. Participation of the pregnant athlete in contact and collision sports
27. Beetham, K.S., Giles, C., Noetel, M. et al. The effects of vigorous intensity exercise in the third trimester of pregnancy: a systematic review and meta-analysis. BMC Pregnancy Childbirth 19, 281 (2019)
28. DA Silva DF, Mohammad S, Hutchinson KA, Adamo KB. Cross-Validation of Ratings of Perceived Exertion Derived from Heart Rate Target Ranges Recommended for Pregnant Women. Int J Exerc Sci. 2020 Sep 1;13(3):1340-1351.
29. Donnelly GM, Moore IS, Brockwell E, et al. Reframing return-to-sport postpartum: the 6 Rs framework British Journal of Sports Medicine 2022;56:244-245.
30. Kimber ML, Meyer S, McHugh TL, Thornton J, Khurana R, Sivak A, Davenport MH. Health Outcomes after Pregnancy in Elite Athletes: A Systematic Review and Meta-analysis. Med Sci Sports Exerc. 2021 Aug 1;53(8):1739-1747
39 medicine & performance football www.fmpa.co.uk
MENSTRUAL CYCLE: PRACTICAL CONSIDERATIONS FOR THE TEAM PHYSICIAN
Introduction
The female athlete faces a changing hormonal milieu thorough the menstrual cycle. The reproductive hormones have an impact on several physiological systems and may influence training adaptions, performance, recovery, and injury risk.
It is still unclear the direction and magnitude of these effects in the different phases of the menstrual cycle. Research about this topic is limited and the menstrual cycle is frequently considered a barrier to include female athletes in sports performance studies1-4. In the scarce literature available, the methodological quality is generally low, and the results are often conflicting5-6
Due to the large variation of the hormonal profile during the menstrual cycle between athletes, and within the same athlete on different cycles, monitoring cycle phases and symptoms is paramount to develop a tailored strategy.
The focus of this article is the eumenorrheic athlete, with a menstrual cycle length between 21 and 35 days, with 9 or more consecutive periods per year7. The use of
Menstrual Cycle
hormonal contraception and its relation to performance and injury risk will not be reviewed8
The menstrual cycle
The menstrual cycle is a biological rhythm that prepares the female reproductive tract for pregnancy and is the result of an interaction between hypothalamic, hypophyseal and ovarian hormones9. There are estrogen and progesterone fluctuations along each cycle, that normally last for 28 days on average (range 21 to 35 days)2, 10, 11
There are two main phases, the follicular phase, and the luteal phase. These phases are separated by ovulation when an egg is released from the ovary. The cycle can be further divided 3, 5, 6 or 7 phases. In the 6-phase cycle one can consider: early follicular (menstrual phase), late follicular, ovulation, early luteal, mid-luteal and late luteal (premenstrual phase) phases. In Figure
1 a 28-day eumenorrheic cycle is represented. The follicular phase begins with the first day of menses (day 1-5) and both estrogen and progesterone are low. Estrogen increases steadily and peaks just before ovulation (12 to 14 days after menstruation onset) and
then it starts to decline. In late follicular phase, estrogen levels are high and progesterone levels are low. After ovulation, the luteal phase begins and there is a gradual increase in progesterone levels. In the mid-luteal phase estrogen levels also increase, resulting in high levels of both hormones in this phase. Both hormones’ levels start to decrease in the late luteal phase, resulting on low levels of estrogen and progesterone in the premenstrual phase10
The female steroids have numerous effects on body systems12,9. Estrogen has anabolic and neuroexcitatory effect and decreases connective tissue stiffness. Progesterone has antiestrogen effect, with a catabolic and neuroinhibitory effect. In addition, progesterone also has thermogenic and hyperventilation effects2,9-12. The interplay of these hormones can be synergistic, antagonistic, or interactive on sports performance9
In terms of hormone levels, the cycle has 3 distinct patterns: low estrogen and progesterone (early follicular phase), high estrogen and low progesterone (ovulation) and high estrogen and progesterone (mid luteal phase)3
FEATURE / RITA TOMÁS, MD, MS
Team Physician, Portugal Women’s National Team Health and Performance Unit, Portuguese Football Federation Portuguese Football School, Portuguese Football Federation
Oestrogen Progesterone Low oestrogen Low progesterone High oestrogen Low progesterone High oestrogen High progesterone Indicative hormone levels Early follicular Late follicular Ovulation Early luteal Mid-luteal Late luteal 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 days
feature 40 info@fmpa.co.uk
Figure 1: Adapted from McNulty et al. Sports Med (2020)
How to determine menstrual cycle phase
The calendar-based counting method is useful to predict menstruation, but bleeding does not confirm that an ovulation has occurred, nor it excludes luteal phase deficiency. These abnormalities are more common in heavy exercisers, so this can occur more often in asymptomatic elite sports women than in general population.
Basal body temperature measurement relies on the fact that after ovulation there is an increase in basal body temperature of 0.30.6o Celsius3,13 due to the rise of progesterone and its thermogenic effect. This temperature peak can be a surrogate that ovulation has occurred, although it does not inform of the actual progesterone level. Several factors can influence basal body temperature readings such as stress, sleep disturbances, illness, and other environmental factors, so this method is not recommended3. Urinary LH measurements allows us to determine the peak of this hormone and it’s known that ovulation usually occurs within 14-26 hours of the LH peak.
Unquestionably, serum hormone analysis is the gold standard to establish the actual levels of each hormone at a certain time. Assessment of progesterone level at mid-luteal phase allows us to confirm an anovulatory or a luteal phase deficiency cycle, if the level falls below a cutoff value. In the research setting, including these athletes in the analysis will lead to confounding results, therefore this should be used an exclusion criterion for such studies3
Salivary hormone measurements may need several samples collected during the day to achieve reliable results due the pulsatile pattern of salivary estrogen3
Menstrual Cycle symptoms
Abdominal pain/distension
Headache
Back pain
Fatigue
Nausea/vomiting
Hot flashes
Breast tenderness
Muscle aches
Dizziness
Swelling
Table 1: Adapted from the Menstrual Distress Questionnaire 15
To improve the methodological quality of research, a more robust phase verification is needed so combination of methods should be used. A 3-step method is recommended 14: a calendarbased counting, plus urinary LH surge detection kit, plus progesterone measurement at the luteal phase. This will allow us to confirm that the woman is at the luteal phase. Other phases can be established from this assumption and further confirmed with serum estrogen measurements 3,7,14
Sleep disturbances
Difficulty concentrating
Forgetfulness
Anxiety
Irritability
Mood swings
Restlessness
Crying
Restlessness
Food craving
Cycle and symptoms tracking A menstrual status, menstrual loss flow, and symptoms diary should be encouraged. Severity of symptoms and measures of wellness/readiness to train should also be recorded. A nonexhaustive list of symptoms is presented in Table 115. Symptom intensity can be assessed with a Likert scale (e.g., 1 - “no experience of symptoms” to 6 -” disabling symptom”).
Athletes should be aware of their menstrual cycle phases and how they feel across the cycle, especially in the more symptomatic phases such as the premenstrual and menstrual phases (late luteal and early follicular, respectively). This will allow practitioners to develop an individualized management strategy, namely, adjusting training, rest, nutrition, and pharmacological interventions when needed, to promote physical and mental wellbeing and readiness to train1
Female athletes should feel at ease to discuss any menstrual cycle related topic with their medical team. Talking about menstruation, premenstrual syndrome, period cramps should be normalized, like any other health issue1
The coaching staff should have a basic knowledge about the topic as this is a variable than can impact the player’s wellbeing and performance.

41 medicine & performance football www.fmpa.co.uk
The menstrual cycle and performance
In a metanalysis performance was trivially reduced during early follicular phase compared to other phases5. The low estrogen and progesterone levels in menstrual phase could eventually hinder performance but this has not been confirmed by other recent reviews11, 13, 16
In terms of strength performance, a metanalysis only found non-significant trivial to small differences among phases in the studies outcomes10
Menstrual Cycle and Performance
Due the poor quality of the studies, large variation among studies and the trivial effect size, no guidelines could be formulated at this time.
The most frequent comparison is between the early follicular phase (both hormones are low) with the mid-luteal phase (both hormones are high). However, comparing early follicular with late follicular is also important as it could test the unopposed effect of
Menstrual Cycle and Injuries Incidence




Wojtys 1998 Wojtys 2002 Beynnon 2006 Adachi 2008 Ruedel 2009 Martin 2021
estrogen on performance (pre-ovulation).
Negative symptoms such as pain and fatigue are more common around the pre-menstrual and menstrual phases (late luteal and early follicular) and are perceived by the athletes to be detrimental to their performance [11]. Athletes perceived that their performance is at its best around ovulation and at its worst at early follicular and late luteal but these finding do not align with the objectively measured performance outcomes11,17
Oestrogen Progesterone Indicative hormone levels Early follicular Late follicular Ovulation Early luteal Mid-luteal Late luteal 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 days
Figure 3: McNulty et al. Sports Med (2020). Somerson et al JBJS Reviews (2019). Martin et al. Front Sports Act Living (2021). Randell et al. Sports Med (2021). Legerlotz & Nobis. Front Physiol (2022)
Myklebust 1998 Slauterbeckl 2002
Myklebust
Higher
Oestrogen Progesterone Indicative hormone levels Early follicular Late follicular Ovulation Early luteal Mid-luteal Late luteal 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 days
1998
injury incidence
Figure 2: McNulty et al. Sports Med (2020). Carmichael et al . Int J Environ Res Public Health (2021). Blagrove et al. J Sci Sports Med (2020). Meignié et al. Front Physiol (2021) . Ekenros et al. Frontiers Physiol (2022)
✅ Best perceived performance ❎ Worst perceived performance
feature 42 info@fmpa.co.uk
The menstrual cycle and injuries
Limited evidence shows two peaks of injury incidence (namely ACL tears), around ovulation and late luteal/early follicular, but it does not suffice to recommend changing risk mitigation practices along the menstrual cycle 6
Around ovulation, estrogen levels are higher and unopposed by progesterone (that is low). Estrogen decreases stiffness of tendons and ligaments and that could make female athlete more prone to injuries during this phase 18. Nonetheless, this has not been confirmed by the latest reviews that had a special focus on ACL injuries 19,20. A recent study with elite footballers found that muscle and tendon injuries occurred twice more frequently in late follicular in comparison to early follicular and luteal phase 21. However, this study relied on self-reported cycle length (calendarbased method) to determine the menstrual cycles phases, so the findings must be interpreted with caution. More studies are needed to make guidelines regarding injury risk management across the menstrual cycle 22. Sports injuries are a complex phenomenon and result of the
interaction of several risk factors and possibly female steroids hormone levels could be one of them 23. Other factors related to the female sex and gender, unrelated to hormone profile, such as environmental aspects, could play a key role 24
The menstrual cycle and training
Phased-based resistance training to maximize adaption (e.g., taking advantage of the anabolic effect of estrogen) is potentially promising, but evidence is poor and inconsistent 25
Two recent reviews analysed longterm adaptation to resistance training across the menstrual cycle, but the methodological flaws of the studies included limit the conclusions 25,26. One review concluded that the symptoms of DOMS and strength loss were lower in the mid-luteal phase in comparison with early follicular phase, so higher training load could be recommended at that phase 25. In the other review, some studies found follicular phase training to be superior to luteal and regular training (training on both phases) 26. Unfortunately, the low quality
of the studies limits the application of the findings. The current evidence is insufficient to warrant a general recommendation on resistance training according to the menstrual cycle phase.
Conclusions
Periodising training and injury prevention programs based on the menstrual cycle phase had limited evidence. Further high-quality research is needed, namely in comprehensive menstrual cycle phase detection methods. Nonetheless, menstrual cycle monitoring and symptoms tracking is recommended to adjust training and other strategies to promote to wellbeing and readiness to perform in the most symptomatic phases.
Players should be encouraged to improve their knowledge and awareness about their menstrual cycle phase and its relation to sports performance and wellness.
Due to the large variability of the menstrual cycle between players and within player, an individualised approach is currently recommended.

43 medicine & performance football www.fmpa.co.uk
References
1. Bruinvels G. ,Hackney A.C. & Pedlar C.R. (2022). Menstrual Cycle: The Importance of Both the Phases and the Transitions Between Phases on Training and Performance. Sports Med, Jul;52(7):1457-1460.
2. Sims S.T. & Heather A.K. (2018). Myths and Methodologies: Reducing scientific design ambiguity in studies comparing sexes and/or menstrual cycle phases. Exp Physiol, Oct;103(10):1309-1317.
3. Jonge X. A. C. J., Thompson B. & Han A. (2019). Methodological Recommendations for Menstrual Cycle Research in Sports and Exercise. Med Sci Sports Exerc, Dec;51(12):2610-2617.
4. Meignié A., Toussaint J.F. & Antero J. (2022). Dealing with menstrual cycle in sport: stop finding excuses to exclude women from research. Eur J Appl Physiol, Nov; 122(11):2489-2490.
5. McNulty K.L., Elliott-Sale K.J., Dolan E., Swinton P.A., Ansdell P., Goodall S., Thomas K. & Hicks K.M. (2020). The Effects of Menstrual Cycle Phase on Exercise Performance in Eumenorrheic Women: A Systematic Review and Meta-Analysis. Sports Med, 50(10):1813-1827.
6. Randell R.K., Clifford T., Drust B., Moss S.L., Unnithan V.B., De Ste Croix M.B.A., Datson N., Martin D., Mayho H., Carter J.M. & Rollo I. (2021). Physiological Characteristics of Female Soccer Players and Health and Performance Considerations: A Narrative Review. Sports Med, Jul;51(7):1377-1399.
7. Elliott-Sale K.J., Minahan C.L., de Jonge X.A.K.J., Ackerman K.E., Sipilä S., Constantini N.W., Lebrun C.M. & Hackney A.C. (2021). Methodological Considerations for Studies in Sport and Exercise Science with Women as Participants: A Working Guide for Standards of Practice for Research on Women. Sports Med. 2021 May;51(5):843-861.
8. Elliott-Sale K.J., McNulty K.L., Ansdell P., Goodall S., Hicks K.M., Thomas K., Swinton P.A. & Dolan E. (2020) The Effects of Oral Contraceptives on Exercise Performance in Women: A Systematic Review and Meta-analysis. .Sports Med, Oct;50(10):1785-1812
9. Constantini N.W., Dubnov G. & Lebrun C.M. (2005) The menstrual cycle and sport performance. Clin Sports Med, Apr;24(2): e51-82, xiii-xiv.
10. Blagrove R.C., Bruinvels G. & Pedlar CR. (2020) Variations in strength-related measures during the menstrual cycle in eumenorrheic women: A systematic review and meta-analysis. J Sci Med Sport, Dec;23(12):1220-1227.
11. Carmichael M.A., Thomson R.L., Moran L.J. & Wycherley T.P. (2021). The Impact of Menstrual Cycle Phase on Athletes’ Performance: A Narrative Review. Int J Environ Res Public Health, Feb 9;18(4):1667.
12. Jonge X. A. C. J. (2003). Effects of the menstrual cycle on exercise performance. Sports Med, ;33(11):833-51.
13. Colenso-Semple L.M., D’Souza A.C., Elliott-Sale K.J. & Phillips S.M. (2023). Current evidence shows no influence of women’s menstrual cycle phase on acute strength performance or adaptations to resistance exercise training. Front Sports Act Living, Mar 23;5:1054542.
14. Schaumberg M.A., Jenkins D.G., Jonge X.A.C.J, Emmerton L.M. & Skinner T.L. (2017). Three-step method for menstrual and oral contraceptive cycle verification. J Sci Med Sport. 2017 Nov;20(11):965-969.
15. Moos R.H. (1968). The development of a menstrual distress questionnaire. Psychosom Med, Nov-Dec;30(6):853-67.
16. Meignié A., Duclos M., Carling C., Orhant E., Provost P., Toussaint J.F. & Antero J. (2021). The Effects of Menstrual Cycle Phase on Elite Athlete Performance: A Critical and Systematic Review. Front Physiol. 2021 May 19;12:654585.
17. Ekenros L., von Rosen P., Solli G.S., Sandbakk Ø., Holmberg H.C., Hirschberg A.L. & Fridén C. (2022). Perceived impact of the menstrual cycle and hormonal contraceptives on physical exercise and performance in 1,086 athletes from 57 sports.Front Physiol, Aug 30;13:954760.
18. Chidi-Ogbolu N. & Baar K. (2019). Effect of Estrogen on Musculoskeletal Performance and Injury Risk. Front Physiol, Jan 15;9:1834.
19. Dos’Santos T., Stebbings G.K., Morse C., Shashidharan M., Daniels K.A.J., & Sanderson A. (2023) Effects of the menstrual cycle phase on anterior cruciate ligament neuromuscular and biomechanical injury risk surrogates in eumenorrheic and naturally menstruating women: A systematic review.. PLoS One, Jan 26;18(1): e0280800
20. Somerson J.S., Isby I.J., Hagen M.S., Kweon C.Y. & Gee A.O. (2019). The Menstrual Cycle May Affect Anterior Knee Laxity and the Rate of Anterior Cruciate Ligament Rupture: A Systematic Review and Meta-Analysis.JBJS Rev., Sep;7(9): e2.
21. Martin D., Timmins K., Cowie C., Alty J., Mehta R., Tang A. & Varley I. (2021). Injury Incidence Across the Menstrual Cycle in International Footballers. Front Sports Act Living, Mar 1;3:616999. doi: 10.3389/fspor.2021.616999
22. Legerlotz K. & Nobis T (2022) . Insights in the Effect of Fluctuating Female Hormones on Injury Risk-Challenge and Chance. Front Physiol, Feb 17;13:827726.
23. Bittencourt N. F. N., Meeuwisse W.H., Mendonça L.D., Nettel-Aguirre A., Ocarino J.M. & Fonseca S.T. (2016). Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition-narrative review and new concept. Br J Sports Med, Nov;50(21):1309-1314
24. Parsons J.L., Coen S.E. & Bekker S (2021). Anterior cruciate ligament injury: towards a gendered environmental approach. Br J Sports Med. 2021 Sep;55(17):984-990
25. Romero-Parra N., Cupeiro R., Alfaro-Magallanes V.M., Rael B, Rubio-Arias J.Á., Peinado A.B. & Benito P.J. IronFEMME Study Group. (2021). Exercise-Induced Muscle Damage During the Menstrual Cycle: A Systematic Review and Meta-Analysis. J Strength Cond Res, Feb 1;35(2):549-561
26. Thompson B., Almarjawi A., Sculley D. & Jonge X. A. C. J., (2020). the Effect of the Menstrual Cycle and Oral Contraceptives on Acute Responses and Chronic Adaptations to Resistance Training: A Systematic Review of the Literature. Sports Med, Jan;50(1):171-185.
44 info@fmpa.co.uk medicine & performance football feature































THANK YOU TO OUR FMPA 2023 CONFERENCE EXHIBITORS 2023 THURSDAY 1 ST JUNE Sponsored by The Rehab T E A M Together Everyone Achieves More #fmpa2023 LEICESTER CITY FOOTBALL CLUB KING POWER STADIUM LE2 7FL
THE EFFECTS OF THE MENSTRUAL CYCLE ON BOTH TRAINING & MATCH DAY PHYSICAL PERFORMANCE USING SUBJECTIVE & OBJECTIVE MEASURES
Introduction
The interest in female football over the last 10 years has increased (Tremback-Ball et al, 2021) this has led to an increase in the amount of research into the female game. Tremback-Ball et al, (2021) suggests that injuries that are related to training and games have increased holistically as the number of women that participate in sport increases, in turn women are more likely to suffer from ligament injuries compared to a male athlete in the same sport (Zuckerman et al, 2018; Baugh et al, 2018 and Stijak et al, 2015).

An emerging topic in contemporary research is the effect of the menstrual cycle on physical performance in women (Meignie et al, 2021). Oestrogen has been found to have an anabolic effect on the skeletal muscle and is responsible for the changes in glycogen stores and the utilisation of
fats (Julian et al, 2017). Progesterone has thought to be an anti-oestrogen effect suggesting that the changes in these hormones during the different phases would influence player performance with performance being defined as short duration activities such as speed and power (Carmichael et al, 2021). McNulty et al, (2020) states that using performance markers such as the work done, time to complete, peak output and ratios and the amount of force generated, concluded with the fluctuation in these hormones lead to a decrease in muscular performance, submaximal and maximal intense exercise in the early follicular phase of the cycle. They found that performance was consistent through the other phases.
The relaxin, hormone known to increase joint laxity to accommodate the body to prepare for childbirth (Bond et al, 2004 and
Reed and Carr, 2018), regulates the activity of the muscles in the uterus to prevent them contracting during the menstrual cycle. The levels of this hormone are at their highest during the mid-luteal phase and reduce as menstruation begins (Reed and Carr, 2018). Research suggests that at certain points in a female’s menstrual cycle that they may be at a higher risk of injury, thought to be because of the effects the hormone has on connective tissue (Stijak et al, 2015 and Zuckerman et al, 2018), in reducing joint stability.
Further, Sawai et al, (2018) suggests that the physiological symptoms of the menstrual phases can affect performance in some athletes in both training and competition. Lack of sleep quality and quantity can be a factor which can result in a decrease in cognitive performance that in turn may affect the athlete’s
FEATURE / LISA EDWARDS MSC SST
47 feature www.fmpa.co.uk medicine & performance football
ability to perform. Fullagar et al, (2015) and Ihalainen, (2019) states that 75% of the participants reported to experience negative performance side effects at certain times of the cycle including loss of strength, inflammation, metabolism, fluid balance and body temperature. Bruivels et al, (2020) looked at the menstrual cycle and the effects that it has on performance and found that there was a link. This study was completed via a wellness app that included questions based on mood, tiredness, fatigue and stomach cramps. The results showed that symptoms had an effect on the player missing training or training being adapted (P<0.05), missing a competitive event/fixture (P<0.05), taking time off work (P<0.05) and taking medication to help supress the symptoms (P<0.05). Further, 90.6% of the participants reported mood changes and anxiety during the menses active phase. These findings could pose both negative and positive response impeding performance, such as increase in levels of impulsivity with potential increases in injury risk. A result in a positive performance on the pitch could be due to the player not thinking about their symptoms as they are focussed on the game or training session (Hickmann, 2004). McNulty, (2020) supports this suggestion that hormone levels fluctuate through the different phases of the cycle.
The effect of the menstrual cycle on a female’s physical performance has been identified as a key consideration for women’s sport and the need for further research in this area has been identified. There is a limited amount of research to provide clarity on whether performance
is affected during menstruation in a female football population, and available literature offers conflicting results. Further research and consideration of different performance measures may therefore be required. The aim of this study therefore is to investigate the effects of the menstrual cycle on multi measures of subjective and objective performance measures within mid-competitive season across training and matches in a population of female footballers.

Methods
Fifteen female football players agreed to take part in the study. All players were participating regularly in training and playing in competitive matches at academy level playing against both boys and girls. Before every training session and match, participants were required to complete a wellness form the morning of training and on match day which reported their date and length of menses, energy levels, stress, mood state and sleep quality. Catapult One GPS devices were assigned to a participant and worn at each training and match fixture. The measures included distance covered and minutes, sprint distance, player load and top speed. RPE scores were taken after each training and match to determine how the participants rated the session (to provide a score of session intensity).
Results
On initial analysis post hoc it appears there is no significant main effect of the menstrual on performance metrics when ran through on SPSS on training data. However, significant main effects were reported for match day subjective data.
When collapsing the data, a significant difference in RPE scores (P=0.044) and energy levels (P=0.054) were noted. Further, when condensing the data and only considering averages of players where there are significant instances of Menses Active (n=3 or more in Training Data, n=2 or more in Game Data) in the players recording, comparisons of individual athlete’s average between active and inactive menses stages can be drawn across 4 players in both Training (Table 3) and Game (Table 4) data. In the Training Data (Table 3), the performance data on average across the 4 players shows a significant decrease in Sprints Distances, Power Plays and Impacts of 30% and more. Player 9 was an anomaly to this data and showed signs of increased performance, on average this still showed significant differences as a whole. All other performance data also shows decreases in output on average with players training loads dropping on average of 13.24% and players covering 11.11% less in total at training (KM).
On Wellness scoring players also were 10.38% higher on average in their Mood States and 12.41% lower in Stress Levels on average when combining these scores. In analysis of this, athletes appear happier and less stressed during training when Menses is active.
On reflection of game data (Table 4) this shows a different set of metrics and performance outcomes when considering the large drops in performance data at training in comparing players Menses Active vs Inactive stages. Whilst Sprint Distance (m) is lower at 15.66% it is not as significant a change as the 31.34% that is seen in the training data (Table 3). Total distance covered (KM) is marginally higher by 7.81% on average and player load is also on average slightly higher by 8.98% on average. Most significantly the number of recorded impacts (which according to Catapult GPS data is “Accelerometer data measured at 400 times per second in each of three axis is used to detect impacts that rate above 5g (49 m/s2). As such, impacts are considered significant events that exclude footsteps during walking and running”.) in game actions this would be considered high impact tackles, body collisions and players coming together in aggressive moments is 150% higher when Menses Active.
On Wellness scoring for Game Data (Table 4) RPE scores are on average 11.47% higher across the 4 players, with energy levels 9.85% lower and players report on average being 10.37% less stressed.
feature 48 info@fmpa.co.uk
Training Data
Match Day Data
Player Distance (km) Sprint Distance (m) Power Plays Energy (kcal) Impacts Player Load Top Speed (m/s) Distance (m/min) R P E Menses active Mood state Energy levels Stress Motivation 1 7 145 19 814 1 386 6 55 6 1 4 4 5 5 2 7 171 20 819 2 405 6 54 6 1 4 4 3 4 3 6 101 13 692 1 355 6 48 6 1 4 4 4 4 4 6 89 10 731 5 409 6 50 7 1 6 6 5 6 5 6 106 15 716 1 326 6 54 6 1 5 5 5 5 6 6 117 16 710 3 373 6 51 6 1 5 5 5 5 7 7 170 22 796 2 372 7 59 6 1 5 5 5 5 8 7 198 25 753 2 374 7 55 7 1 5 5 5 5 9 7 149 22 849 1 402 6 57 7 1 5 4 4 5 10 6 127 15 681 6 333 6 45 6 1 5 5 4 5 11 6 70 10 731 1 353 6 50 6 1 4 4 5 4 12 6 158 17 697 3 325 7 48 6 1 5 5 5 5 13 7 289 29 814 1 384 7 53 5 1 7 7 6 7 14 7 159 20 792 1 366 7 56 5 1 5 5 5 6 15 6 152 20 698 3 370 6 48 5 1 4 4 5 4 Average 6 147 18 753 2 369 6 52 6 1 5 5 5 5 Standard Deviation 0.4 49.1 4.9 52.3 1.4 25.0 0.2 3.7 0.5 0.1 0.7 0.8 0.6 0.8 Table 1: Averages and standard deviation of players from 1-15
Player Number of Games Distance (km) Sprint Distance (m) Power Plays Energy (kcal) Impacts Player Load Top Speed (m/s) Distance (m/min) R P E Menses active Mood state Energy levels Stress Motivation 1 6 10 387 39 1173 1 462 7 71 8 1 5 5 5 6 2 10 10 447 46 1168 4 510 7 69 8 1 5 5 4 5 3 9 8 274 26 932 2 447 7 56 8 1 6 6 5 6 4 8 7 150 18 768 6 385 6 51 9 1 6 7 5 7 5 10 8 302 32 986 2 401 7 66 8 1 6 6 5 6 6 9 7 276 30 834 3 394 7 55 8 1 5 6 5 6 7 10 9 358 32 1073 3 469 7 65 8 1 5 5 4 5 8 9 10 560 48 1142 2 477 7 73 8 1 5 5 5 5 9 8 8 215 28 930 1 403 7 71 8 1 6 6 5 6 10 8 9 344 34 1034 5 462 7 56 8 1 5 6 4 6 11 3 12 329 42 1346 4 567 7 63 8 1 6 7 5 6 12 9 9 381 38 1023 2 404 7 62 8 1 5 5 5 5 13 9 9 555 44 1100 2 465 7 66 7 1 5 6 5 6 14 5 8 585 42 963 1 410 7 63 7 1 5 5 6 6 15 7 9 484 43 1121 2 498 7 67 8 1 4 4 5 5 Average 8 8.9 376.5 36 1039.5 2.7 450.2 7 64 8 1 5 5 5 6 Standard Deviation 1.9 1.2 124.7 8.3 141.1 1.4 49.5 0.3 6.5 0.4 0.1 0.5 0.7 0.4 0.6 Table 2: Averages and standard deviation of players 1-15 49 medicine & performance football www.fmpa.co.uk
Player Name Distance (km) Sprint Distance (m) Power Plays Energy (kcal) Impacts Player Load Top Speed (m/s) Distance Per Min (m/min) R P E Menses active Mood state Energy levels Stress Motivation Player 1 Menses Inactive 7 157 20 820 1 391 7 55 6 1 4 4 5 5 Player 1 Menses Active 7 139 18 763 1 359 6 54 6 2 4 4 4 5 Difference 0 19 2 58 0 32 0 1 0 -1 0 0 1 0 Difference % 5.61% 12% 9% 7% -2% 8% 5% 2% 7% -100% 4% 4% 20% 6% Player 3 Menses Inactive 6 130 17 754 1 388 6 51 6 1 4 4 4 4 Player 3 Menses Active 4 12 3 505 0 256 5 41 7 2 5 4 4 4 Difference 2 119 14 249 1 132 1 10 -1 -1 0 0 0 0 Difference % 32.33% 91% 84% 33% 100% 34% 23% 20% -11% -100% -11% -3% -11% 0% Player 9 Menses Inactive 7 146 22 838 1 401 6 57 7 1 5 4 4 5 Player 9 Menses Active 7 161 20 887 1 406 6 59 7 2 6 5 3 6 Difference 0 -14 2 -49 1 -5 0 -3 0 -1 -1 -1 2 -1 Difference % -6.56% -10% 11% -6% 54% -1% 5% -5% -7% -100% -25% -14% 36% -32% Player 13 Menses Inactive 7 317 32 843 1 398 7 52 5 1 7 7 6 7 Player 13 Menses Active 6 214 22 736 1 349 7 56 5 2 7 7 5 7 Difference 1 103 10 107 0 48 0 -3 0 -1 -1 0 0 0 Difference % 13.05% 32% 31% 13% -7% 12% 5% -6% -5% -100% -11% -3% 5% -3% Average All % Difference 11.11% 31.34% 33.74% 11.74% 36.31% 13.24% 9.62% 2.64% -4.11% -100% -10.38% -3.81% 12.41% -7.28%
feature 50 info@fmpa.co.uk
Table 3: Comparison of Training Data for select players with Menses Inactive vs Active comparison
Player Name Distance (km) Sprint Distance (m) Power Plays Energy (kcal) Impacts Player Load Top Speed (m/s) Distance Per Min (m/min) R P E Menses active Mood state Energy levels Stress Motivation Player 5 Menses Inactive 8 309 31 917 1 377 7 59 7 1 6 6 5 6 Player 5 Menses Active 10 284 36 1147 4 458 7 81 9 2 5 5 5 5 Difference -2 25 -6 -229 -3 -82 0 -22 -2 -1 0 1 0 1 Difference % 0 8% -19% -25% -279% -22% 1% -37% -21% -100% 7% 20% 9% 19% Player 6 Menses Inactive 8 321 31 864 3 393 7 57 8 1 5 5 5 6 Player 6 Menses Active 6 179 25 737 5 378 6 46 8 2 7 7 5 7 Difference 1 141 6 127 -2 15 0 11 0 -1 -2 -1 1 -1 Difference % 0 44% 18% 15% -69% 4% 4% 20% 0% -100% -30% -22% 10% -15% Player 8 Menses Inactive 10 576 49 1169 2 476 7 71 8 1 5 5 5 5 Player 8 Menses Active 10 507 44 1046 1 482 7 81 9 2 5 4 5 5 Difference 0 69 5 123 1 -6 0 -10 -1 -1 0 1 0 1 Difference % 0 12% 11% 11% 56% -1% 1% -13% -10% -100% -3% 18% 0% 10% Player 9 Menses Inactive 9 252 33 1087 1 475 7 67 8 1 6 6 5 6 Player 9 Menses Active 11 255 31 1288 4 554 7 58 9 2 4 5 4 5 Difference -2 -4 2 -201 -3 -79 0 10 -1 -1 2 1 1 1 Difference % 0 -1% 6% -18% -308% -17% 2% 14% -15% -100% 30% 23% 22% 10% Average All % Difference -7.81% 15.66% 4.06% -4.54% -150% -8.98% 1.93% -3.99% -11.47% -100% 0.93% 9.85% 10.37% 6.04%
51 medicine & performance football www.fmpa.co.uk
Table 4: Comparison of Game Data for select players with Menses Inactive vs Active comparison
Conclusion
The results of the study are in support of the menstrual cycle effecting an individual players performance on both subjective and objective measures. There is a significant drop of performance in training rather than game data. One potential factor for this could be due to the difference in environment with training being a more learning focused environment versus match day which is a more focused, competitive environment. Another finding was there appeared to be an increase in impacts during a game which could explain the reason there are more ligament injuries in female football with making tackles without thinking of the consequences.

This increase in impulsivity can also be a positive factor with more sanctioned aggression leading to positive impacts of the outcome of the game.
Training Performance was impacted significantly with players training levels dropping by around 30% in some cases, player Mood and Stress levels were also affected. The implications of this are players training levels will dip during this phase of the menstrual cycle, without taking this into consideration, GPS Performance data could be misconstrued and players performance could be negatively looked upon in this stage of the menstrual cycle outside of context.
References
Baugh, C; Weintraub, G; Gregory, A; Djoko, A; Dompier, T; Kerr, Z. (2018). Descriptive epidemiology of injuries sustained in Na tional Collegiate Athletic association Men’s and Women’s volleyball. Sports Health; 2018;10(1):60-69. Doi: 10.1177/1941738117733685
Bond, C; Parry, L and Samuel C. (2004) Increased expression of the relaxin receptor (LGR7) in human endometrium during the secretory phase of the menstrual cycle. Journal of clinical endocrinol metabolism. 2004;89(7):3477-3485
Bruinvels, G; Goldsmith, E; Blagrove, R; Simpkin, A; Lewis, N; Morton, K; Suppiah, A and Rogers, J. (2020) Prevalence and frequ ency of menstrual cycle symptoms are associated with availability to train and compete. British Journal of Sports Medicine. 2020. Do i: 10.1136/bjsports-2020-102792.
Carmichael, M; Thompson, R; Moran, L and Wycherley, T. (2021) The impact of menstrual cycle phase on athletes’ performance: A narrative review. International Journal of Environmental Research and Public Health. 2021,18(4):1667. Doi: 10.3390/ijerph180416 67
Fullagar, H; Skorski, S; Duffield, R; Hammes, D; Coutts, A and Meyer, T. (2015) Sleep and athletic performance: the effects of sleep loss on exercise performance and physiological and cognitive responses to exercise. Sports Medicine. 2015;45(2):161-186. Doi:10 .1007/ s40279-014-0260-0
Hickman, S. (2004) Impulsivity as a predictor of athlete success and negative consequences in NFL Football Players. University of Massachusetts Amherst. https://scholarworks.umass.edu/dissertations_1/3306?utm_source=scholarworks.umass.edu%2Fdiss ertations_1%2F3306&utm_medium=PDF&utm_campaign=PDFCoverPages
Julian, R; Hecksteden, A; Fullagar, H and Meyer, T. (2017) The effects of menstrual cycle phase on physical performance in fema le soccer players. PLOS ONE. 2017. Doi: 10.1371/journal.pone.0173951
McNulty, K; Elliott-Sale, K;Dolan, E; Swinton, P; Ansdell, PGoodall, S; Thomas, K and Hicks, K. (2020) The effects of menstrual cycle phase on exercise performance in eumenorrheic women: A systematic review and meta-analysis. Sports Medicine, 50, 1813-1827. Doi : 10.1007/s40279-020-01319-3
Meignie, A; Duclos, M; Carling, C; Orhant, E; Provost, P; Toussaint, J and Antero, J (2021) The effects of menstrual cycle phas e on elite athlete performance: A critical and systemic review. Frontiers in Physiology.2021.12;1-10. Doi:10.3389/fphys.2021.654585
Reed, B and Carr, B. (2018) The normal menstrual cycle and the control of ovulation. National library of medicine.
Sawai, A; Tochigi, Y and Kavaliova, N (2018) MRI reveals menstrually-related muscle edema that negatively affects athlete agili ty in young women. PLOS ONE. 2018;13(1):e0191022. Doi: 10.1371/journal.pone.0191022
Stijak, L; Kadija, M and Djulejic, V (2015) The influence of sex hormones on anterior cruciate ligament rupture;female study. K nee Surg Sports Traumatol Arthrosc.2015;23:2742-2749. Doi:10.1007/s00167-014-3077-3
Tremback-Ball, A; Fulton, K; Giamietro, N; Gibbons, M; Kneller, A and Zelinka, H. (2021) Effect of the menstrual cycle on athle tic performance in NCAA Division III collegiate athletes. Journal of Women’s Health Physical therapy. 2021;45(1):20-26. Doi: 10.109 7/ JWH.00000000000188
Zuckerman, S; Wegner, A and Roos, K. (2018) Injuries sustained in National Collegiate Athletic Association Men’s and Women’s basketball. British Journal of Sports Medicine. 2018;52:261-268. Doi: 10.1136/bjsportd-2016-096005
52 info@fmpa.co.uk medicine & performance football feature
LEGAL Compromise agreement
“...I took your advice and have been working with the FMPA lawyer on the conclusion of my contract. Martin from his swift response on day one has been a real rock on my side and he has stayed in contact with me at regular intervals. His professionalism and knowledge of the football contract has helped me to be both realistic and hopeful regarding my case. We are now at the final stages of discussions with the club and the financial and emotional support I have has come through my contact with Martin. I am also immensely grateful to the FMPA for your help and support at this difficult time. At a low point in my life both the FMPA and Martin have helped me get the contractual situation sorted with as little fuss as possible and that’s been important to me and my family.”
Head of Medicine, League 2
Contract review
“...I just wanted to drop you an email to let you know how helpful Martin has been this last week. Although away, and with poor signal, he consistently made the effort to respond quickly to my questions when the club came back with updated terms. I believe his guidance has been fundamental to my negotiations.”
Head Physiotherapist, Premier League
“...Thank you so much. Really appreciate your help with this, it’s brilliant that the FMPA offer this service to its members. This stuff can be a minefield.”
Lead Sports Scientist, Premier League
JOIN TODAY www.fmpa.co.uk/legal Tel: 0333 4567897

FMPA Business Directory FMPA Business Directory is now available on the FMPA site to give members quick access to products/services. VIEW THE DIRECTORY www.fmpa.co.uk/fmpa-directory







 Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine






























 FEATURE / DR JOANNE L PARSONS, DR SHEREE BEKKER, DR STEPHANIE E COEN
FEATURE / DR JOANNE L PARSONS, DR SHEREE BEKKER, DR STEPHANIE E COEN