By W. Allen Fink, DO, MHA, CPE, FACEP,
PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER
Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry Lair gerrylair@yahoo.com For
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE: Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006
www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 SmithPrint, Inc. PRINTED IN THE USA

Ezequiel “Zeke” Silva, III, MD, President
Lyssa Ochoa, MD, Vice President
John Shepherd, MD, President-elect
Jennifer R. Rushton, MD, Treasurer
Lubna Naeem, MD, Secretary
John Joseph Nava, MD, Immediate Past President
Woodson “Scott” Jones, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Ana Rodriguez, MD, Member
Raul Santoscoy, DO, Member
Lauren Tarbox, MD, Member
Nancy Vacca, MD, Member
Col. Elisa D. O’Hern, MD, MC, FS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School
Representative
Cynthia Cantu, DO, Medical School Representative
Lori Kels, MD, Medical School Representative
Ronald Rodriguez, MD, Medical School Representative
Victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Director of Membership & Corporate Partnerships
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Monica Jacqueline Salas, MD, Co-chair
Jennifer C. Seger, MD, Co-chair
Lokesh Bathla, MD, Member
Elizabeth Clanton, MD, Member
Erika Gabriela Gonzalez-Reyes, MD, Member
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. K. Jyothula, MD, Member
Kristy Yvonne Kosub, MD, Member
Jaime Pankowsky, MD, Member
George-Thomas Martin Pugh, MD, Member
Rajam S. Ramamurthy, MD, Member
Adam V. Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Boulos Toursarkissian, MD, Member
Francis Vu Tran, MD, Member
Faraz Yousefian, DO, Member
Louis Doucette, Consultant
Brissa Vela, Consultant
Monica Jones, Staff Liaison
Trisha Doucette, Editor
Deepthi S. Akella, Student
Moses Alfaro, Student
Victoria Ayodele, Student
Tue Felix Nguyen, Student
Andrew Ta, Student
Alixandria Fiore Pfeiffer, DO, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, PhD, Volunteer
Rita Espinoza, DrPH, Volunteer
Natalie Reyna Nyren, PA-C, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer
By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)
One of my priorities is to enhance the contributions of BCMS to the Texas Medical Association. A key aspect of this objective is ensuring a robust BCMS presence at TexMed, the TMA’s annual meeting, which took place in early May. I am pleased to report our significant achievements.
TexMed serves as the annual meeting for the TMA House of Delegates (HOD), the policymaking body of the TMA. It also hosts TMA Councils, Committees, Caucuses and Sections and welcomes new leaders and members. Crucially, the HOD conducts its election of new officers, including the President-Elect and members of the TMA Board of Trustees.
Dr. Jayesh “Jay” Shah was elected as the 2024 President-Elect, with his presidency set to begin at TexMed 2025. Jay will be the 14th TMA President from Bexar County and the first Indian-American to serve in this role. He is the first BCMS member to serve as President since William Hinchey, MD in 2007-2008. A former BCMS President, Jay has contributed immensely to the medical community in Bexar and surrounding counties. Jay’s acceptance speech was remarkable.
Jenny Shepherd, the spouse of our BCMS President-Elect, John Shepherd, MD, was inaugurated as the new TMA Alliance President. Jenny’s role extends to the AMA Council on Legislation, where she will help shape AMA legislative policies. Like Jay, Jenny gave a memorable acceptance speech to the TMA HOD.
Beyond our new President-Elect, several BCMS members have assumed TMA leadership roles. For instance, I have been appointed Chair of the TMA Council on Legislation. Over 50 BCMS members serve on various TMA Councils, Caucuses and Sections.
A list of our members and their roles can be found here: www.bcms.org/bcmsdelegates.php

TMA policy is shaped by the HOD through resolutions. Each resolution is assigned to various reference committees by the TMA Speaker and Vice-Speaker, who recommend actions based on the testimony and existing TMA policies. BCMS was well-represented in the reference committees:
• Science and Public Health: David Trueson Lam, MD, Chair
• Financial and Organizational Affairs: Jim Humphreys, MD
• Medical Education and Health Care Quality: Soma S. K. Jyothula, MD
• Socioeconomics: Lyssa N. Ochoa, MD
BCMS sponsored a number of resolutions with the following outcomes:
• Resolution 105 – Developing National Guidelines for Physician Supervision of Midlevel Practitioners: Adopted as Amended
• Resolution 203 – Supporting Diversity-Focused Student Affinity Groups in Medical Education: Adopted
• Resolution 317 – Ensuring Safety with Devices Producing Carbon Monoxide: Adopted
• Resolution 414 – Regulating Non-Compete Clauses for Doctors in Texas: Adopted
• Council on Science and Public Health Report 2 – Bexar Resolution 301 from 2023 – Labeling of Sugar-Sweetened Beverages: Adopted
A full description of these resolutions as well as others from TexMed can be found here: www.texmed.org/uploadedFiles/Current/2016_About_TMA/TMA_Leadership/House_of_Delegates/ Summary%20of%20Actions%202024.pdf
BCMS made a strong impression at TexMed 2024, and we continue to grow in representation and influence. As the voice of physicians in Bexar and surroundiwng counties, the opportunities and responsibilities are substantial. We depend on our dedicated volunteers. If you can spare the time and energy, we invite you to join our TMA delegation.

BCMS has a specific number of delegates based on our total membership. Our delegation also includes several ex-officio delegates, such as members of TMA Councils and Committees and past presidents. Although we had a substantial number of delegates, we did not reach our full allotment, presenting an opportunity for more delegates to participate in future meetings, such as the 2025 TexMed, which will take place in San Antonio.
Learn more about opportunities with BCMS at TMA here: www.bcms.org/committees.php www.texmed.org/hod/
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He is Chair of the TMA Council on Legislation and is a TMA Delegate to the AMA. He serves on the AMA Council on Medical Service, and chairs the AMA RVS Update Committee (RUC).
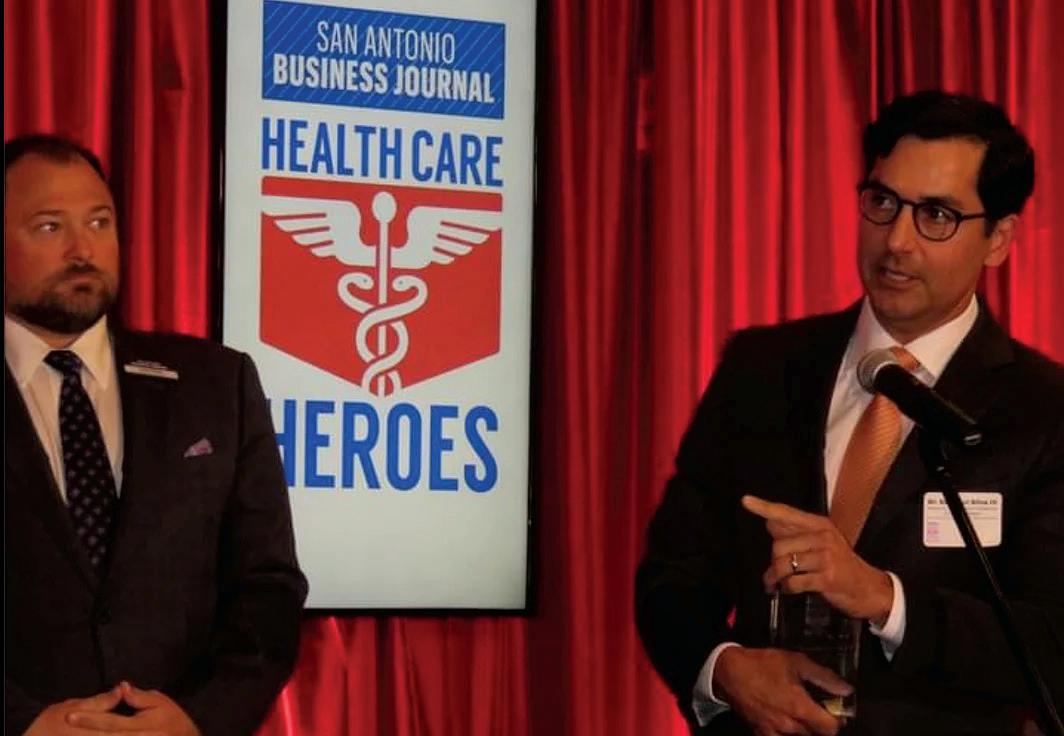
By Gabriella Bradberry
The Bexar County Medical Society’s very own, 2024 BCMS President, Ezequiel “Zeke” Silva, III, MD, was elected to serve on the American Medical Association’s Council on Medical Service. On June 11, 2024, AMA held their Annual Meeting of the House of Delegates where Dr. Silva was voted as one of the council members for the 20242028 term.
The AMA’s Council on Medical Service functions to study and evaluate the social and economic aspect of healthcare. As a council member, Dr. Silva’s roles will include investigating social and economic factors influencing the practice of medicine and to confer with and assist state associations, component societies and national medical specialty societies regarding changing conditions and anticipated proposals that would affect medical care.
Factors that contributed to Dr. Silva’s election included his expertise in payment policy, history of sharing expertise with lawmakers, advocacy on physicians’ practices and patient care and more. Dr. Silva has proven himself to be a voice for medicine.
Congratulations to Dr. Silva on his election as a member of the AMA Council on Medical Service. He has proven to be a voice for not only medicine in Bexar County but across the nation.

Gabriella Bradberry is the Admin/Communications Specialist for the Bexar County Medical Society.






By Victoria Kohler-Webb, BBA, MS
It truly was a Royal Garden Party! Our Alliance gathered for our most beautiful and enduring Alliance tradition — our Past President’s Luncheon. I was so proud to welcome our members to this amazing chance to celebrate our special bond of friendship and highlight the value of our connections. I found the Alliance through dear friends and Past Presidents Cindy Comfort (who delivered our Invocation) and Jenny Shepherd — what a blessing it has been! I always feel welcome with this group, which is why I keep coming back.
Why the Alliance? What do we do? We define our Alliance role in three ways: Community Outreach, Legislative Advocacy and Strengthening the Medical Community. First, speakers Julia Halvorsen, VP Philanthropy, and Brittany Garcia, President-Elect, detailed BCMSA Community Outreach initiatives such as our Period Poverty Project, TMAA BookShare and TMAA Hard Hats for Little Heads.
Who better than our lovely Jenny Shepherd, 2024 TMAA President and two-time June Bratcher Award for Advocacy winner, to bring us up to speed on Legislative Advocacy efforts? Jenny and her team continue finding effective channels for ensuring the voices of doctors and their families are heard in Austin.
Our specialty and core competency since 1917 remains Strengthening the Medical Community. So far in 2024, our Alliance has executed the Period Poverty Project, Hard Hats for Little Heads, Health Fairs, AllMed, Doctor’s Day, Bowl & Barrel New Member Meet-up and pop-up member socials! Stay tuned to our Facebook page, Bexar County Medical Society Alliance, for more!
Past President Danielle Henkes welcomed our Past Presidents (see picture), celebrated their leadership, and led a very moving tribute to our Centennial Past President Lori Boies, who we will all miss so much as she and her family leave us for wonderful new opportunities. Finally, our BCMSA Board, in keeping with our Royal Garden Party theme and reputation for fun, crowned Jenny Shepherd as BCMSA Queen in a special coronation commemorating her 2024 TMAA Presidency.
Thank you to all of you reading who have served this amazing organization as President — your tradition of strong leadership and community service has kept us strong!
At BCMSA, we have FUN and we are DIFFERENCE MAKERS!!! Join us!!

Victoria Kohler-Webb, BBA, MS Marketing Statistics, is the 2024 Alliance President. She and Ben, an ENT/Head & Neck Surgeon, are proud Aggies and parents to Luke, 14, and four rescue dogs.





Help your patient and their family make the best-informed decisions.
Earn free online Continuing Medical Education (CME) credits developed by the Texas Department of State Health Services and physician experts on Alzheimer’s disease and related dementias. These courses will keep you up to date on the latest validated assessment and screening tools, help you direct patients to community resources, and reinforce your role in helping patients and their families manage symptoms throughout the disease process.
Courses coming soon at dshs.texas.gov/alzheimers-disease/provider
By Michelle Fricke, MD
In the hustle and bustle of urban life, where skyscrapers tower and vehicles fill the streets, air pollution has become an unavoidable reality. While we often hear about its detrimental effects on respiratory health, air pollution can impact skin health by accelerating aging, triggering inflammation, and exacerbating existing skin conditions.
A major issue associated with pollution is its capacity to produce free radicals within the skin. Free radicals are unstable molecules that induce oxidative stress, resulting in cellular harm and accelerated skin aging. This oxidative stress can trigger the degradation of collagen and elastin, reducing the skin’s elasticity and firmness, consequently contributing to premature development of wrinkles and fine lines. It can also affect the natural skin barrier function, allowing harmful substances to penetrate more easily. This can result in skin sensitivity, irritation, inflammation, redness and the exacerbation of existing skin conditions
However, amidst this urban backdrop, there are steps we can take to fortify our skin’s defenses and mitigate the damage caused by environmental pollutants.
Counteracting airborne pollutants can be as straightforward as cleansing your face with an appropriate cleanser. Throughout the day, particulate matter attaches to the skin. Establishing a thorough cleansing routine is the cornerstone of protecting your skin from pollution. Opt for gentle cleansers that effectively remove dirt, grime and pollutants without stripping away the skin’s natural oils.
Antioxidants are your skin’s best allies in the battle against pollution-induced oxidative stress. Antioxidants can help your skin fight air pollution, cigarette smoke and UV radiation. Incorporate skincare products rich in antioxidants such as vitamin C, vitamin E and niacinamide into your daily regimen. These potent ingredients neutralize free radicals, repair cellular damage, and fortify the skin’s natural defense mechanisms.
Strengthening the skin barrier is crucial for minimizing the penetration of harmful pollutants. Look for moisturizers containing ceramides, fatty acids and cholesterol, which replenish lipid levels and reinforce the skin’s protective barrier. Additionally, occlusive agents like petroleum jelly or dimethicone form a protective seal, preventing pollutants from adhering to the skin’s surface.
Sunscreen isn’t just for sunny days; it’s a year-round essential, espe-

cially in urban environments where pollution exacerbates UV damage. Choose a broad-spectrum sunscreen with a high SPF and PA rating to shield against UV radiation. Reapply sunscreen at least every two hours, particularly if you spend extended periods outdoors.
This can cause you to transfer dust and pollutants.
Proper hydration is essential for maintaining skin health and resilience against environmental stressors. Hyaluronic acid-infused serums and moisturizers replenish moisture levels, plump up the skin, and create a protective barrier against pollutants. Additionally, facial mists containing humectants like glycerin or panthenol provide on-the-go hydration, refreshing the skin and enhancing its natural defenses.
Nourish your skin from within by adopting a diet rich in antioxidant-rich fruits and vegetables, omega-3 fatty acids and hydration-promoting foods. Foods like berries, leafy greens, fatty fish and nuts bolster the skin’s natural defenses, enhancing its resilience against environmental aggressors.
Prioritize adequate sleep and stress management techniques as integral components of your skincare routine. Quality sleep allows the skin to regenerate and repair overnight, while stress reduction techniques such as meditation, yoga or deep breathing exercises mitigate the inflammatory response triggered by pollution exposure, preserving skin health. In conclusion, safeguarding your skin from the harmful effects of air pollution requires a multifaceted approach that combines diligent skincare habits, lifestyle adjustments and environmental awareness. By adopting these protective measures, you can strengthen your skin’s natural defenses, mitigate the damaging effects of pollution, and preserve its youthful vitality in the face of urban environmental challenges

Dr. Michelle Fricke is board certified by the American Board of Dermatology with Alamo Heights Dermatology. She is a member of the Bexar County Medical Society.



By Patricio de Hoyos Zambrano, MD
Understanding that breathing polluted air will affect our lung health is not a mystery. Nevertheless, when pollution comes with economic prosperity, our recurring mistake is to be blinded by the “prosperity” and take in the smoke as part of our lives.
Not many know what happened in Donora, Pennsylvania in 1948. A town that was proud of its industry with large steel and zinc mills that provided its residents with work and stability. Heavy smoke was the norm, however, on the night of October 29, 1948, a thick smog covered the town for several days impairing visibility and affecting everyone’s lungs. At least 20 people lost their lives that night. After that event, almost half of the population was not able to breathe like they used to.
The World Health Organization (WHO) estimates that every year, 3.2 million people die prematurely due to household air pollution that is caused by using solid fuels and kerosene used for cooking. Particulate matter (PM) and other pollutants in household air can cause continued inflammation of the airways and contribute to significant impairment of the immune system. Household air pollution has a wide range of impact on health that includes ischemic heart disease as well as increased risk of lower respiratory infections, chronic obstructive pulmonary disease, asthma and lung cancer.
There are different variables to consider when contemplating how exposure to air pollution occurs. People in low to middle income countries, close to 3 billion people in the world, rely on biomass fuels for daily activities including household heating and cooking. This includes using solid fuels such as wood, dung, crop waste and coal that are often burned inefficiently. Combustion of solid fuels produces gases such as nitrogen dioxide (NO2), carbon monoxide (CO) and particulate matter (PM). Households in high income countries have observed lower pollutant concentrations. However, even in the United States, about 6.5 million people continue to use solid fuels for heating, especially in rural areas. Urbanization predisposes individuals in high-income settings to other pollutants indoors, that include particulate matter, environmental tobacco smoke, toxic cleaning chemicals and gases such as nitrogen dioxide (NO2) from cooking and heating. The presence of these noxious gases in combination with a poorly ventilated household increases the risk of impaired lung development in children, higher risk of pneumonia, risk of asthma, COPD, lung cancer and increased exacerbation of respiratory diseases.
PM is especially concerning for public health given its widespread human exposure as a pollutant derived from combustion sources. It consists on inhalable particles with an aerodynamic diameter of 10 μm or less (PM10) and fine particles with an aerodynamic diameter of 2.5 μm or less (PM2.5). The WHO has established air quality guidelines recommending upper limit of 24 hour mean concentrations for PM10 of 50 μg/m3 and PM2.5 of 25 μg/m3. Liu et al. published a study demonstrating ambient particulate air pollution and daily mortality in 652 cities. Using uniform statistical methods, the annual mean daily concentrations found during the entire study sample showed PM10 of 56.0 μg/m3 and PM2.5 of 35.6 μg/m3. Results showed that an increase of 10 μg/m3 increase in a 2-day period increased the total cardiovascular and respiratory mortality. For an increase of 10 μg/m3 for PM10, the increase in all-cause mortality was of 0.44 percent. An observed increased risk of all-cause mortality of 0.68 percent was reported for an
increase of 10 μg/m3 of PM25. This study confirmed a positive association of total cardiovascular and respiratory mortality with short-term exposure to PM10 and PM2.5 increase.
A strong association has been demonstrated between household air pollution and the risk of acute lower respiratory infections around the world. In a meta-analysis of 24 studies, Dherani et al demonstrated that exposure to solid fuel use during childhood increased risk of respiratory infections by 78 percent. Indoor gas stove use for cooking has been associated with an increased risk of asthma among children. Gruenwald et al concluded that 12.7 percent of current childhood asthma in the United States is attributable to gas stove use. This is a preventable exposure and comparable to the burden from secondhand smoke exposure.
There is a large amount of evidence showing more ways in which air pollution affects our respiratory health. Efforts made by our governments on reducing emissions and actions, such as banning gas stoves or supporting clean energy and transportation, spark controversy these days. Many choose to have an illusion of prosperity and sacrifice the quality of the air we breathe, the comfort of choosing to ignore the damage pollution causes our lungs in exchange for money and economic growth. We have a choice on the air we breathe; let’s choose to breath air that won’t make us sick.
References:
1. Raju S, Siddharthan T, McCormack MC. Indoor Air Pollution and Respiratory Health. Clin Chest Med. 2020;41(4):825-843. doi:10.1016/j.ccm.2020.08.014
2. Jacobs ET, Burgess JL, Abbott MB. The Donora Smog Revisited: 70 Years After the Event That Inspired the Clean Air Act. Am J Public Health. 2018;108(S2):S85-S88. doi:10.2105/ AJPH.2017.304219
3. Liu, C, Chen, R, Sera, F, Vicedo-Cabrera, AM, Guo, Y, Tong, S, Coelho, M, Saldiva, PHN, Lavigne, E, Matus, P, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019, 381, 705–715
4. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ. 2008;86(5):390–398C. 10.2471/blt.07.044529
5. Gruenwald T, Seals BA, Knibbs LD, Hosgood HD III. Population Attributable Fraction of Gas Stoves and Childhood Asthma in the United States. International Journal of Environmental Research and Public Health. 2023; 20(1):75. https://doi. org/10.3390/ijerph20010075

Patricio de Hoyos Zambrano, MD, is board certified in Internal Medicine and Pulmonary Medicine. He is the Medical Director, Advanced Emphysema Service Line, at Texas IPS, and a member of the Bexar County Medical Society.

By Soma Jyothula, MD, FCCP
Shopping with a teenage daughter means meandering into personal beauty product stores without a clue about most of the products being sold and finding the closest bench to wait out the time. On one of those days, browsing through my favorite news website, I came across a news item describing a ban on use of microbeads in personal beauty products in the UK. This was followed by another article on how microplastics were found in the clouds above Mount Fuji.1 After parsing through the actual article and seeing the robust manner the investigators collected the samples to minimize any contamination from terrestrial sources made me realize, we have plastic floating in the air and within clouds at 12,000 feet above sea level (height of Mt Fuji is 12,388 feet). Beyond the incredulity of the fact, the word which stuck me was microplastics.
Plastics are defined in pure chemical terms as organic polymers (chains of organic molecules). Unlike natural polymers like hair, nails,
animal horns or natural rubber, plastics are partially or completely synthetic. Plastics are an integral component of modern human life. Its discovery and widespread use have led to the modern civilization and lifestyle. Presence of plastic in soil sediments is considered one of the markers of the Anthropocene (human era) on the geological time scale. Plastics are ubiquitous in our life — they pervade our home, immediate environment, beaches, deepest depths of the oceans, the highest peaks on planet earth and are an inviolable sign of human pollution. Beyond being an eyesore, the same property which has made modern human life possible is also slowly choking it (inert and indestructible nature). The timescale for a plastic grocery bag to degrade is in hundreds of years.
Microplastics are a different beast. Unlike the visible plastics products we see with the naked eye, they are microscopic. Their size varies from 5mm to 0.005mm. For perspective, human hair breath is around
0.1mm. Emerging research has shown microplastics have pervaded the human environment and various ecosystems. As the above-mentioned paper showed presence in clouds, microplastics have been identified in house dust, indoor air, clothes we wear, water we drink and the food we eat. Yes, microplastics have been seen inside chicken and fish meat. Increasingly, microplastics are being discovered in various human tissues (blood, liver, lung, kidney) and in breast milk.2 A recent NEJM paper created a stir by discovering microplastics in carotid plaque samples obtained during carotid endarterectomy.3 Carotid plaques are in no direct connection to the environment and the microplastics discovered in a plaque had to breach various physical barriers to enter the human body and circulate in the bloodstream for a significant duration of time, be ingested by macrophages and subsequently get incorporated into a plaque (time scale is probably in years).
Microplastics come from two predominant sources. Primary sources will be various products that incorporate microplastics like various beauty products such as cleansers and toothpaste. Secondary sources are where degradation and breakdown of plastics produce microplastics (plastic containers and food wraps/pouches are an example). How are microplastics able to invade human tissues? Ingestion is one of the primary sources. Microplastics have permeated the ecosystem into the food chain to be part of animal products like fish, shrimp and mussels. Presence in soil leads to presence in agricultural products like apples and carrots. Water sources include tap water and bottled water, with higher concentrations in bottled water. Plastic used for food packaging leads to leaching into edible food. A single coffee bag can release 10,000 microparticles. Inhalation is another mode. Urban areas have significant concentrations; indoor environments act as traps and show higher amounts. Skin is another conduit and personal care products are manufactured with microplastics. The small size of the microplastics and presence of any breakdown in skin will increase absorption into the human body. Once the particles enter the human body, depending on size and nature, they can translocate into various tissues as revealed by their identification in various parts of the human viscera.
Any discerning scientific mind will ask the next question. What effect will these microplastics have on the human body? Humans evolved roughly around 200 to 300 thousand years ago, and the current generation is roughly 7,500 to 15,000 generations away from the founder population. As a species on a biological level, our bodies have only encountered microplastics for the past couple of generations. The time span to develop adaptations is extremely short. Current literature in animals shows various deleterious effects on animal biology. The NEJM paper showed that half the patients who had microplastics in their plaques had a higher risk of death from cardiovascular events. Microparticles increase inflammation in human tissues, contributing to chronic inflammation and diminishing the ability to fight pathogens. Toxicity in lungs is dose, size and ligand dependent. The presence of microplastics in breast milk is particularly frightening as exposure starts right with our first meal. Much research is to be done, but the signs from available evidence show that we will see a causative role in human disease with much more clarity in the future.
Without sounding as an alarmist, we need to start taking steps to decrease our exposure to microplastics. At a policy level, the UK has already banned microbeads in personal beauty products. We ingest about a credit card-sized amount of microplastics in a week. The con-
sumer report has put forward a few simple measures to decrease the amount of ingested microplastics.4
1. Drink tap water and avoid bottled water.
2. Heat food in or on a stove and microwave in glass containers. Avoid microwaving in plastic containers.
3. Buy and store food in glass, silicone or foil and avoid plastic containers.
4. Eat fresh food and avoid processed food wrapped in plastic covers.
5. Vacuum household surfaces regularly along with dusting.
Beyond these personal changes in habits, be a good global citizen. The pervasiveness of plastic pollution is way beyond our immediate environment. Participate in public dialogue to decrease plastic usage and waste. Be part of the change to lead to a safer plastic-free life. The plastic we have generated will last a long way after our lifetime; we need to provide a better environment for our future generations. The call for action STARTS NOW.
References:
1. Wang Y et al. Airborne hydrophilic microplastics in cloud water at high altitudes and their role in cloud formation. Environ Chem Lett 21, 3055–3062 (2023). https://doi.org/10.1007/ s10311-023-01626-x
2. Li Y et al. Microplastics in the human body: A comprehensive review of exposure, distribution, migration mechanisms, and toxicity. Sci Total Environ. 2024 Jun 22;946:174215. doi: 10.1016/j. scitotenv.2024.174215. Epub ahead of print. PMID: 38914339
3. Marfella R et al. Microplastics and Nanoplastics in Atheromas and Cardiovascular Events. N Engl J Med. 2024 Mar 7;390(10):900-910. doi: 10.1056/NEJMoa2309822. PMID: 38446676; PMCID: PMC11009876
4. https://www.consumerreports.org/health/health-wellness/howto-eat-less-plastic-microplastics-in-food-water-a8899165110/

Soma Jyothula, MD, FCCP, is a practicing pulmonary and critical care physician, and is the Chief of Pulmonary Medicine and Lung Transplantation at Methodist Hospital. Dr. Jyothula is a member of the Bexar County Medical Society and serves on the Publications Committee.


By Ami Chatrath, MD
Eating disorders are a group of conditions that involve distorted views of one’s body paired with behaviors that impact eating or lead to weight loss. A few of these conditions include anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED).
Eating disorders often lead to numerous medical and psychiatric complications. Relative to other psychiatric conditions, eating disorders have a greater risk of suicide attempts and have the second highest mortality rate, after opioid use disorders. Symptoms that require medical management include bradycardia, syncope, seizures, dehydration, growth concerns, failure to thrive, gastroparesis, osteoporosis and/or amenorrhea.
Unfortunately, symptoms occur for many years before treatment is either sought or implemented. Identifying risk factors, specifically biological, psychologic and social influences, can lead to earlier diagnosis and treatment.
Clinicians currently utilize the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), published in 2022, to assess and diagnose various mental health-related conditions.
AN involves restriction of energy intake relative to requirements, leading to a significantly low body weight. There is intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain. Furthermore, there is a disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight.
The restricting type describes weight loss obtained through methods such as dieting, fasting or excessive exercise. Binge eating/purging type involves binge eating with resultant purging by methods that include self-induced vomiting or misuse of laxatives, diuretics or ene-
mas. Atypical anorexia nervosa involves meeting all criteria for AN, except that the individual’s weight remains around or above the normal range, as measured by BMI.
BN involves recurrent episodes of binge eating, which is described as eating an amount of food that is definitely larger than what most individuals would eat and a sense of lack of control over eating during the episode. Additionally, there are recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting or misuse of laxatives, diuretics or enemas.
BED is centered on recurrent episodes of binge eating without inappropriate compensatory behaviors. These episodes are associated with eating much more rapidly than normal, eating until feeling uncomfortably full, eating large amounts of food when not feeling physically hungry, eating alone because of feeling embarrassed by how much one is eating, and/or feeling disgusted with oneself, depressed or very guilty afterward.
Genetics, as in most medical and psychiatric conditions, increases the overall risk of developing an eating disorder. Although there is a higher degree of heritability for AN, BN and BED have elevated heritability rates themselves. As suspected, females are more likely to develop an eating disorder compared to males. Disturbances in leptin, melanocortin and neurotrophin molecules and variations in dopamine, serotonin and cannabinoid levels have also been implicated. The presence of an autoimmune disease is linked to a higher risk of developing BN.
Certain early childhood experiences, including elevated maternal expectations, lower parental emotional connectedness and negative parental comments related to weight increases the risk of developing eating disorders. Furthermore, victims of physical or sexual abuse are associated with a higher prevalence of BN and related eating disorders that particularly involve binging and purging.
Certain sociocultural and ethnic factors play a part as well. Evidence suggests that BN is more prevalent in minority ethnicities. Relative to other ethnic groups, Black Americans possess higher rates of BED. LGBTQIA+ identifying individuals have an elevated risk of developing an eating disorder. Restrictive behaviors are associated with higher education levels and binging is associated with historical or current food insecurity.
As it pertains to personality traits, perfectionism is most commonly found in individuals with AN and BN whereas obsessiveness is associated with AN. Emotional dysregulation and impulsivity are associated with BN and related eating disorders that involve binging and purging.
From an environmental perspective, eating disorders are more prevalent in models and athletes that participate in certain activities, including wrestling, dance and gymnastics. The increased rates of disordered eating in these specific activities can be attributed to strict dieting expectations and pressure to maintain low body fat levels.
Social influences have the ability to negatively impact an individual’s perception of their body image. Historical traditional media has typically valued a thin body habitus as the ideal body shape and current social media trends continue to perpetuate this ideal. Platforms that rely on images, such as Snapchat and Instagram, have been asso -
ciated with body image concerns and eating disorders. Trends such as fitspiration, which may cause an overreliance on “clean eating” or excessive exercise, or thinspiration, which may encourage starvation with a goal of a thin body habitus, may reinforce disordered views of one’s body.
From a psychiatric perspective, certain mental health conditions and personality traits elevate the likelihood of developing an eating disorder. Major depressive disorder is found in 75 percent of those with eating disorders that involve binging and purging. Furthermore, social anxiety disorder impacts about 42 percent of individuals suffering with an eating disorder.
The signs and symptoms of eating disorders impact multiple organ systems and the development of eating disorders is dependent on a variety of risk factors. This highlights the importance that all physicians, regardless of specialty, screen for eating disorders and refer to an eating disorder specialist for collaborative treatment. This is particularly important when patients possess non-modifiable risk factors. Additionally, community awareness strategies and education to alter modifiable risk factors can mitigate the likelihood of individuals developing an eating disorder.
1. American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi. org/10.1176/appi.books.9780890425787
2. Barakat, S, McLean, SA, Bryant, E. et al. Risk factors for eating disorders: findings from a rapid review. J Eat Disord 11, 8 (2023). https://doi.org/10.1186/s40337-022-00717-4
3. Dane, A, & Bhatia, K. (2023). The social media diet: A scoping review to investigate the association between social media, body image and eating disorders amongst young people. PLOS global public health, 3(3), e0001091. https://doi.org/10.1371/journal. pgph.0001091
4. Eating Disorders: A Guide to Medical Care (Fourth edition). (2021). (Ser. AED Report). Academy for Eating Disorders
5. Mitchison, D, & Hay, PJ. (2014). The epidemiology of eating disorders: genetic, environmental, and societal factors. Clinical epidemiology, 6, 89–97. https://doi.org/10.2147/CLEP.S40841

Ami Chatrath, MD, is a board-certified psychiatrist that is the co-founder of wiseMIND based in San Antonio, Texas and one of the staff psychiatrists for Esperanza Eating Disorder Center. He completed his residency at UT Health Science Center - San Antonio and served as chief resident of psychiatry for University Hospital in his final year of training. Dr. Chatrath chose to pursue psychiatry as a profession due to the valuable relationships he formed working with patients and helping them live rewarding and satisfying lives. He is a member of the Bexar County Medical Society.

By Heidi L. Benavides, MSN, RN, CMSRN, DNPc, Christiane Meireles, PhD, RDN, LD, and Paula Christianson-Silva, DNP, FNP-BC, ANP-BC
AWhole Food, Plant-Based (WFPB) eating pattern is an evidence-based modality to prevent, treat and, in some cases, reverse chronic disease.4, 6, 8, 10 In 2017, there were over 11 million worldwide deaths due to dietary risk factors that contributed to cardiovascular disease, type 2 diabetes, cancer and other causes.1 More than 50 percent of the dietary-related deaths were due to high sodium intake (3 million deaths) and a low intake of whole grain (3 million deaths), fruits (2 million), vegetables and nuts/seeds. The leading cause of dietary deaths in young adults ages 25-50 was from low fiber, while older adults aged 70 years and over was due to high sodium diets.
What is a Whole Food, Plant-Based Diet?
A WFPB diet includes nutrient dense foods with an abundance of antioxidants and fiber, which are minimally processed.2 WFPB foods include whole grains, nuts, seeds, legumes, vegetables and fruits. Animal products (dairy, animal meat or fish) and processed foods are excluded. There are many myths about WFPB diets, but the evidence supports a WFPB approach (or eating pattern) for children, adolescents, adults and pregnant individuals.7, 9 There are many types of versatile plant-based protein sources (soy, beans, lentils, peanuts, whole grains, and nuts and seeds).7 Plants are good sources of calcium, including kale, broccoli, tofu, spinach and bok choy.
Patients should be taught about the marketing trap of processed plantbased foods, which can be high in sodium and fat. The packaging can make the product look healthy and often is misunderstood by the patient.
Individuals engage in a WFPB eating pattern for many reasons. Some may have health issues and want to try a dietary modality to treat or potentially cure their disease, while others may want to prevent disease. WFPB diets are known to help with climate change. Additionally, others may want to protect animals from a difficult life and a painful death.
Transitioning to a WFPB diet can be simple with the right tools and depends on the patient’s stage of change. Patients may be in the precontemplation stage, while others are already in the maintenance stage. Understanding and reinforcing the patient’s motivation for change may help support the patient’s dietary transition. Patients may want to gradually transition to a WFPB diet by starting with a “Meatless Monday” or trying one WFPB meal per week, while others may want to transition immediately to a 100 percent plant-based eating pattern. Some patients may never want to stop eating meat and, in this case, clinicians will want to encourage an increase in whole, plantbased foods and water consumption while also decreasing animal products and processed foods.
Clinicians may find challenges in obtaining patient buy-in for any lifestyle modifications because behavior change can be difficult. Clinicians can use motivational interviewing techniques, perhaps leading the conversation by asking the patient if they would like more information about treating their disease with lifestyle changes, which may reduce their overall costs and medication dosing (or possibly stopping medication[s] completely). Many patients will be open to learning more.
Clinician Education
Clinicians may not feel competent in WFPB education. The American College of Lifestyle Medicine (ACLM) is a professional organization dedicated to the six pillars of wellness (including WFPB diets). Several education modalities exist to include webinars, conferences, interest groups and diplomate certification.
Patient Education
The ACLM has a 43-page Food as Medicine Jumpstart Guide, which educates about WFPB diet meal planning.3 Additionally, there
are many other ACLM member handouts that provide evidence-based lifestyle measures.
Forks-Over-Knives is a website to support healthy dietary changes. There are also several Netflix documentaries we recommend to patients: Forks-Over-Knives, Blue Zones, You Are What You Eat and The Game Changers.
The University of Texas Health San Antonio School of Nursing has an innovative, data-driven program to help transition patients to a WFPB diet.11 The Green Wellness Program: Plants-2-Plate is a sixmonth, interprofessional lifestyle modification program using shared medical appointments (SMAs) with a registered nurse, family nurse practitioner and registered dietitian. Patients can self-refer or clinicians can refer patients through the same website intake form. Patients complete an institutionally approved SMA confidentiality agreement. A comprehensive provider medical appointment is completed with fasting labs at zero, three and six months. Patients meet individually with the registered dietitian twice. Education during the 14 SMAs (one hour each) is focused on the ACLM six pillars of wellness (whole foods/plant-based diet, physical activity, restorative sleep, social connections, stress reduction and avoidance of risky substances), chronic illnesses and a cooking class by a registered dietitian/chef. Education, social support and goal setting are essential aspects of the program. Our results have shown improved health outcomes including weight reduction, decreased inflammatory markers, improved FibroScans and liver function tests, reduced hemoglobin A1Cs, improved energy and decreased blood pressure. Self-reported pre- and post-program health and nutrition surveys are completed.
WFPB education should be part of every medical visit. The use of SMAs can improve delivery of care, increase clinician and patient satisfaction, and increase productivity and revenue.5 Clinicians can obtain continuing education hours to improve knowledge of a WFPB eating pattern. Patients can be referred to other healthcare disciplines who specialize in a WFBP eating pattern and other lifestyle measures to improve health outcomes. Health professions education should emphasize evidence-based, WFPB concepts within undergraduate and graduate programs.
A Whole Food, Plant-Based dietary eating pattern is an evidence-based modality that should be at the forefront of a patient’s treatment plan. Eating a variety of plant-based, whole foods have been shown to be safe for most individuals. Clinicians can improve their patient health outcomes through innovative WFPB education approaches and play an important role in WFPB disease prevention, management and possibly disease remission.
References:
1. Ashfin, A, Sur, PJ, Kairsten, FA, et al. (2019). Health effects of dietary risks in 195 countries, 1990-2017: A systematic analysis for the Global Burden of Disease study 2017. Lancet,393. 19581972. https://doi.org/10.1016/S0140-6736(19)30004-8
2. American College of Lifestyle Medicine (n.d.a.). Home page. https://lifestylemedicine.org/
3. American College of Lifestyle Medicine (n.d.b.). Food as medicine jumpstart. https://lifestylemedicine.org/wp-content/ uploads/2024/01/ACLM-Food-As-Medicine-Jumpstart-8.5x11.pdf
4. Bansal, S, Connolly, M, & Harder, T. (2022). Impact of a wholefoods, plant-based nutrition intervention on patients living with chronic disease in an underserved community. American Journal of Lifestyle Medicine, 16(3), 382-389. https://doi. org/10.1177/15598276211018159
5. Christianson-Silva, P, Benavides, H & Meireles, C. (2023). Using shared medical appointments in your practice, The Journal for Nurse Practitioners, 19 (8), 1-3. https://doi.org/10.1016/j.nurpra.2023.104709
6. Esselstyn, CB. (2001). Resolving the coronary artery disease epidemic through plant-based nutrition. Preventative Cardiology, 4(4). 171-177. https://doi.org/10.1111/j.1520037x.2001.00538.x
7. Lu, I. (2021). Busting nutrition myths: How plant-based diets are healthy for children & families. https://nutritionstudies.org/ busting-nutrition-myths-how-plant-based-diets-are-healthy-forchildren-families/
8. Ornish D, Scherwitz, LW, Billings, JH, et al. (1998) Intensive lifestyle changes for reversal of coronary heart disease. JAMA,280(23). 2001-2007. https://doi.org/10.1001/ jama.280.23.2001
9. Shah, R, Davis, B, & Katz, DL. (2020). Nourish: The definitive plant-based nutrition guide for families—with tips & recipes for bringing health, joy & connection to your dinner table.
10. Tuso, PJ, Ismail, MH, Ha, BP, & Bartolotto C. (2013). Nutritional update for physicians: plant-based diets. Permanente Journal,17(2), 61-66. https://doi.org/10.7812/TPP12-085
11. Wellness 360 Clinic (n.d.). Green Wellness Program: Plants-2Plate. https://wellness360.uthealthsa.org/green-wellness-program-plants-2-plate/

Heidi Benavides is a registered nurse and currently an Associate Professor/Clinical at UT Health San Antonio. She is passionate about plant-based nutrition and lifestyle medicine as a means to prevent, manage and reverse chronic illness. Heidi spearheaded and co-founded the Green Wellness Program: Plants-2-Plate utilizing shared medical appointments with an interdisciplinary methodology and serves as program director.

Christiane Meireles, PhD, RD, LD, is a registered dietitian and clinical associate professor at the School of Nursing at UT Health San Antonio with over 35 years of experience in clinical, community and research settings. As a clinical dietitian, her work is predominantly on primary care focusing on chronic diseases, mainly diabetes, chronic kidney disease and obesity. As a researcher, nutrition in kidney disease, women’s health and, more recently, plant-based diets are the center of her studies. Christiane Meireles is co-founder of the Green Wellness Program: Plants-2-Plate.

Paula Christianson-Silva, DNP, FNP-BC, ANP-BC, DipACLM, is a clinical professor and family nurse practitioner at UT Health San Antonio with expertise in interprofessional care models, lifestyle medicine and NP education. She has been a primary care NP and educator since 1989. At UT Health, Dr. Christianson-Silva has been active in DNP Program curriculum development and is co-founder of the Green Wellness Program: Plants-2-Plate.

By Adelita G. Cantu, PhD, RN, FAAN
Founded in 2003 by concerned Central Texas physicians, Texas Physicians for Social Responsibility (TxPSR) serves as the state chapter of the National PSR. Dedicated to addressing environmental threats to public health, TxPSR focuses on mitigating risks associated with climate change, fossil fuel production and environmental toxins through policy advocacy, medical education and programs tailored for vulnerable populations.
TxPSR stands at the forefront of the healthcare landscape, advocating not only for individual well-being but also for the broader health of communities and the planet. Founded on the principles of social responsibility, this organization brings together physicians with other health professionals and health professional students dedicated to addressing pressing social and environmental issues affecting Texans and beyond.
As a vital link between the healthcare community and policymakers, TxPSR endeavors to raise awareness and educate decision-makers about the public health hazards linked to climate change, fossil fuels and environmental contaminants. To influence policy and safeguard environmental health, TxPSR members advocate for including these public health hazards in curriculum through electives, lectures and training sessions for healthcare professionals and students, offer testimonies at legislative hearings, publish articles and letters, engage in
discussions with elected officials on key policy matters, and collaborate with environmental organizations to amplify health perspectives. Recent notable achievements include:
• Conducting the fourth course in environmental health at UT Dell Medical School, receiving positive and constructive evaluations from students and faculty.
• Assisting in the development and implementation of the first environmental health course at Baylor College of Medicine, and the first course on climate change and health at UT Southwestern School of Medicine.
• Assisting in the development and implementation of the first interprofessional environmental health and climate change elective course at UT Health San Antonio.
• Contributing to the drafting and revision of organ system slides to be incorporated into the core curriculum at UT Southwestern Medical School.
• Developing and launching Texas’ first continuing education program for healthcare professionals focused on climate change’s impacts on health. This program includes webinars on topics such as excessive heat exposure, infectious disease risks in floodwaters, climate change’s impacts on cancer, reducing the carbon footprint of medical practices, the health and carbon emission impacts of
diet, climate change’s effects on children’s health, disaster preparedness for healthcare professionals, air pollution’s impact on human health, and strategies to address climate change’s effects on mental health.
• Increasing medical student participation on TxPSR’s board to include four medical students from Baylor College of Medicine, UT Dell, UT Southwestern and UTMB medical schools.
Texas, with its vast industrial and energy sectors, faces significant environmental challenges, from air and water pollution to the impacts of climate change such as extreme heat events. TxPSR works tirelessly to raise awareness about these issues and advocates for policies that promote clean energy, reduce pollution, and protect public health.
Moreover, TxPSR is committed to promoting peace and preventing nuclear threats. In a world where the specter of nuclear conflict looms large, this organization understands the catastrophic consequences such events would have on public health and global security. Through education and advocacy, TxPSR strives to reduce the risk of nuclear proliferation and advocates for disarmament measures that prioritize human well-being.
Additionally, TxPSR plays a crucial role in advocating for equitable access to healthcare. In a state where healthcare disparities persist, par-
ticularly among marginalized communities, TxPSR works to address systemic inequities and promote policies that ensure all Texans have access to quality healthcare services.
TxPSR’s impact extends far beyond the borders of Texas. As part of the larger Physicians for Social Responsibility network, which spans across the United States and globally, TxPSR collaborates with like-minded organizations to address shared challenges and advocate for policies that prioritize health, equity and sustainability.
In a time marked by unprecedented health and environmental crises, the work of Texas Physicians for Social Responsibility is more vital than ever. By championing the health of communities and the planet, advocating for social justice, and promoting peace, TxPSR exemplifies the power of health professionals to effect positive change beyond the confines of the clinic. As Texans and global citizens, we all have a stake in the vision of a healthier, more just and secure world that TxPSR tirelessly pursues.
www.texaspsr.org

Adelita G. Cantu, PhD, RN, FAAN, Board Chair, Texas Physicians for Social Responsibility. She serves on the BCMS Publications Committee.


Interview with Leni Kirkman, Executive Vice President, Chief Marketing Communications & Corporate Affairs Officer at University Health; conducted by Elizabeth Allen, Director of External Communications at University Health, and Trisha Doucette, Editor, San Antonio Medicine magazine.
Photography by Mark Greenberg for University Health
The built environment impacts how people physically maneuver and function in a space, but it also contributes to a sense of safety and overall well-being — or not. As a result, people are constantly trying to reshape the physical component of a space to positively impact the emotional response it evokes. This action is ever-present in hospital design.
In fact, each historical era created its own unique hospital design that responded to the practice of healthcare in that period. Beginning in the 10th century, basilicas evolved from religious buildings where people sought refuge, to hospitals. By the Renaissance Period, crossward hospitals emerged and were eventually modified into four angled wards with an altar in the center so that all patients could participate in mass. Gender-segregated wards were established in the 17th century, and by the 19th century, wards radiating from a central station allowed direct sight lines to patients’ beds and more windows were added for natural ventilation. The early 20th century brought social class to the mix with the introduction of private rooms and also reserved space for medical specializations. Then between the 1960s-80s, the Mega-Hospital was designed in response to population demands and the space required for healthcare technologies.1
Today, good hospital design focusses on improving the overall healthcare experience for patients as well as providers while accommodating the constant evolvement of technological advancements and patient demographics.2 Architecturally, adaptability and sustainability are imperative but both patients and staff benefit from a well-designed, aesthetically pleasing space. In clinical care areas where patients are conscious, natural light with window views, art, sound, and material and color palettes all create a calming and healing environment. Beyond clinical care areas, addressing patients’ comfort begins upon



their arrival to the facility and continues inside where concierge services are common in a visually appealing public space and curated art installations reference elements of hospitality design.3
At University Health in San Antonio, Texas, administrators intentionally made the decision to create uplifting environments and utilize color. “Architecture and Design is your first step in understanding the patient experience. I would argue that design is as important as any other form of healthcare,” said Leni Kirkman, Executive Vice President, Chief Marketing Communications & Corporate Affairs Officer at University Health.
While some architects may have specialized experience in building hospitals and ambulatory care clinics, the healthcare landscape is constantly growing and changing. At University Health, the architectural team meets with hospital user groups to understand the flow of how they do their work, the types of spaces they need for productivity and efficiency, how they care for patients and how they work as an academic medical center.
In 2008, during the planning phase of the Sky Tower at University Health, a Master Facilities Planning Committee considered spatial principles and how the service of a space is designed. Right-sizing spaces for specific procedures and patients in wheelchairs or walkers, chairs to suit different purposes throughout the hospital and special considerations for visiting family members were addressed. They came up with the concept of designing patient rooms with three zones: a family zone with comfortable chairs and a couch that expands to a bed, the patient area with personal space and the care team area where equipment can be moved about. This zone model has continued through the construction of the Women’s & Children’s Hospital and other community hospitals.
Accommodating family members was especially important, as family support is essential in creating a healing environment. “We want to be able to understand the needs of our community, and we want to make it as comfortable for patients as possible. Going to the hospital is stressful.
When you think about design, there are a lot of decisions we can make to reduce that stress by allowing families to be there for support.”
Another concept that came to fruition from the 2008 planning phase was the SaludeArte: Art of Healing program, which encompasses art exhibits, performance art and workshops for patients and staff. Gardens were incorporated into design to offer respite for visitors and provide soothing views from inside spaces, and color psychology was used to determine palettes for specific needs and areas. Kirkman explained, “Intentional elements such as nature, art and design enhancements are extremely important in creating spaces that reduce anxieties and make hospitals feel warmer and more welcoming. We saw on day one of the Sky Tower opening the importance of these visual elements through patient and family testimonials.”
In a world where consumers are demanding experiences in everyday social interactions, hospitals are evolving to include more positive sensory stimulation that promotes a kinder, calming healing environment.
References:
1. Perales, A. Design & Healing Hospital Typologies. Typologies: A Taxonomy of Type is from The Architecture of Health: Hospital Design and the Constriction of Dignity by Michael P. Murphy Jr. with Jeffrey Mansfield and MASS Desgn Group (2021, Cooper Hewitt). https://artsandculture.google.com/story/ design-amp-healing-hospital-typologies-cooper-hewitt-national-design-museum/XAWRwVgcQpJ39g?hl=en
2. Evolution of Modern Hospital Architecture: Innovations, Trends, and Impact. Healthcare 360 Magazine. https://heathcare360magazine.com/evolution-modern-hospital-architecture/
3. Staczek, D. 10 Elements of the Perfect Hospital Design. Architizer. https://architizer.com/blog/practice/details/perfect-hospital-design/

By Allison Hays Lane
There was a time when drabness was the dominant aesthetic theme in medical spaces, but hospitals and clinics have begun turning to a design principal that incorporates the use of natural light, exposure to nature and uplifting colors.
University Health embraced this philosophy of beauty as a healing element. We launched an early and groundbreaking art program, and with our growth and expansion have incorporated art into the built environment and woven it into our wellness resources for both patients and staff.
Studies show that art can promote patient relaxation by reducing stress, anxiety and pain levels. One study published in the American Journal Public Health focused on the positive outcomes of four primary areas of art, including music, visual arts, move-based creative expression and expressive writing. The study noted, “In all four areas of creative artistic expression reviewed here, there are clear indications that artistic engagement has significantly positive effects on health.”
The Mayo Clinic Press said, “Creative arts therapy is used in treatment for a variety of conditions spanning mental health, cancer, stroke and




board.
more. The idea behind creative arts therapy is that artistic expression can help people to feel better and motivated to recover and address clinical needs such as reducing anxiety and blood pressure.”
Experts continue to research the benefits of art in healing. National Endowment for the Arts Research Director Sunil Iyengar has led efforts during the last decade to explore the importance, value and multiple benefits of exposure to all arts on mental health, economic development, education, scientific research and overall well being in communities all over the world.
Through our SaludArte: Art of Healing program, we have incorporated evidenced-based and trauma-informed care design standards to create a hopeful, compassionate, colorful and uplifting environment.
Art creates a more soothing and healing environment every day — from the child who is less afraid as they gaze at the colorful image of an animal friend on their hospital room wall to the laboring mother who experiences less pain as she focuses on soothing music. We hear from our staff who are better able to care for patients when they have an opportunity to stop and recharge in a quiet space, or engage in journaling to express their emotions. All forms of art are important in a healing environment and we regularly see the effects in our staff and the patients we serve.
“Art is important in creating spaces that reduce anxiety and promote healing,” said Leni Kirkman, executive vice president and chief marketing, commu nications & corporate affairs officer for University Health.


As part of the SaludArte: Art of Healing program’s larger vision, our work reflects the community, improves the experience of our patients and visitors, and communicates our mission through art and design enhancements.
Since 2010, our nationally recognized, award-winning program has grown to offer more than 65+ art-related activities annually for our patients and staff, including:
• Art writing workshops
• Meditation, yoga and wellness workshops
• Poetry readings
• Artist demonstrations in all mediums
• Art in the Garden and lobby with dance music performances
• Staff art kit giveaways and tours
• A-I-R our new University Health Artist in Residence starting this fall
• Supporting system-wide wellness week activities
• SaludArte Staff art educators who can lead retreats, workshops and events
• Art Therapy for Child Life and OBYGN
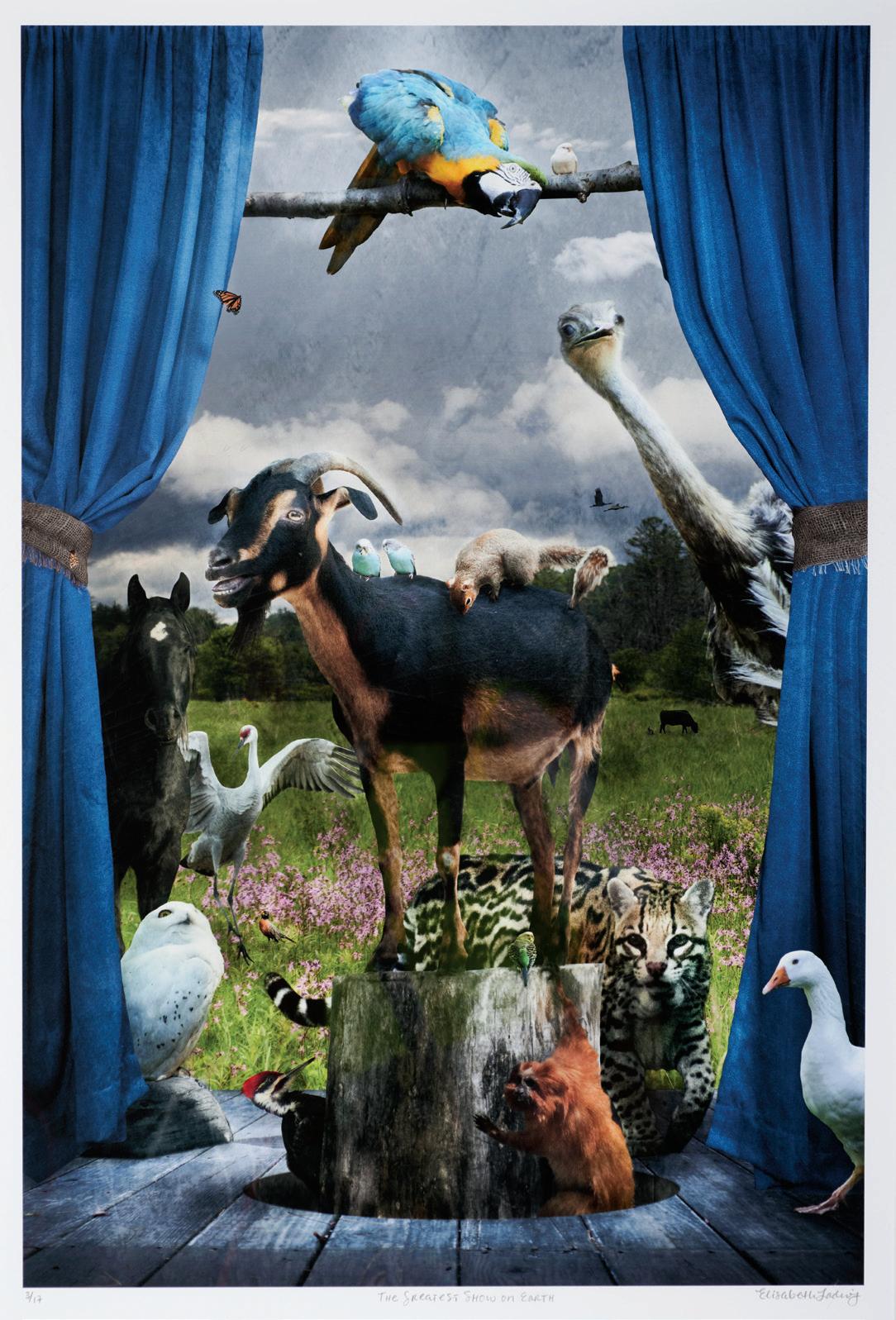
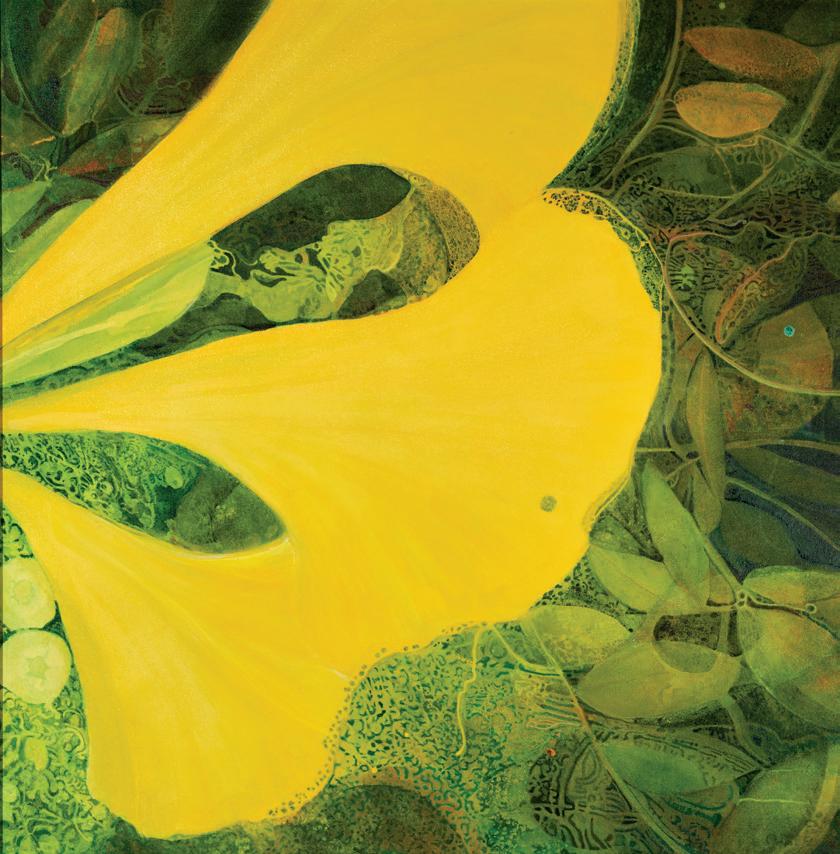
In December 2023, we opened our new Women’s and Children’s Hospital. This facility proudly joins our SaludArte program with more than 1,500 artworks, bringing our total to more than 5,500 objects. The new hospital provides the perfect “blank canvas” to bring national and local artists together to improve mood, stress and comfort. Our building’s design theme was Texas Flowers and Fauna, a visual vocabulary we will be continuing in our four new community capital improvements projects that broke ground this year.
The response to the light, beauty and color in the new hospital has been one of keen interest and appreciation by staff, patients and visitors.
“People stop and look at the art,” Kirkman said. “They read the labels. You just don’t see that in a hospital that has not intentionally made the decision to incorporate these elements.”

Allison Hays Lane has worked in the arts for over 30 years. She is the executive curator of planning, design and construction at University Health and leads the award winning SaludArte: Art of Healing program. Hays Lane earned a bachelor’s degree in art history from Sarah Lawrence College and a master’s degree in museum education from Bank Street College.


By Gregory Michael Tomlinson, Arunabh Bhattacharya, PhD, and Ramaswamy Sharma, MS, PhD
Inflammation is a term we frequently hear associated with certain foods, aging, exercise, infection and in many other contexts. What exactly is inflammation? Is it good or bad? Is it possible to reduce your body’s inflammation? Read on to find answers to these questions based on current knowledge.
Inflammation can be generally defined as the body’s natural response to protect itself from harm. Inflammation occurs when our body senses foreign bodies such as bacteria and viruses (called pathogens), noxious chemicals and physical objects such as nails that puncture our skin. Our bodies immediately launch an “immune” response, channeling cells that act as sentries to capture any invading pathogen that traverses the broken barrier. The inflammatory process begins when these cells come across entities that are either new to them or if they associate them with pathogens they have previously encountered. If the immune cells are short in numbers, they send out signals to recruit other immune cells traveling in the blood. They work in tandem with these newly recruited immune cells to help neutralize the threat by either engulfing these invaders and killing them, or by secreting proteins and other highly reactive molecules that can destroy them.10 Unfortunately, collateral damage is inevitable and innocent cells that neighbor pathogen-infected cells may also die and release their contents, further amplifying the inflammatory response. As inflammation peaks (called acute inflammation), we may observe an increase in heat (calor), pain (dolor), redness (rubor), swelling (tumor) and loss of function (functio laesa) in the breached area. However, once the immune cells complete their duties, they release anti-inflammatory substances that help shut
down the reaction, restoring normalcy. Thus, inflammation can be helpful and protective if it is tightly regulated.
In some cases, however, our immune cells are either unable to fully contain the entities or begin attacking our own cells, setting off a repetitive cascade of events, resulting in long-term or chronic inflammation. Such chronic inflammation has been associated with many diseases, including asthma, rheumatoid arthritis, multiple sclerosis and irritable bowel syndrome, each having their unique triggers and manifestations. Inflammation is also associated with the development and progression of atherosclerosis that can result in heart attacks. Chronic inflammation has been associated with acceleration of our natural aging process, so much so that scientists have coined a term for it, “inflammaging.” It is thought that reducing chronic inflammation, while preserving the beneficial effects of short-term inflammation, can profoundly benefit the quality of life while slowing down the aging process.
Stress is also associated with inflammation. With continuous stress, our body can release hormones such as adrenaline that can trigger inflammation.7 Chronic stress is also associated with structural changes within the brain, and is thought to exacerbate cardiovascular disease, and worsen depression.9 Clearly, the inflammatory process can go awry and become unhelpful, even harmful, in these cases.
Exercise has an interesting relationship with inflammation. Intense exercise for 60 minutes or longer can trigger acute inflammation.3 Simply put, exercise is intense when you are unable to say more than a few words without gasping for breath as you exercise. However, moderate physical exercise with appropriate resting periods has strong anti-in-
flammatory effects.3 Moderate exercise is when you can comfortably talk, but not sing during exercise. Anti-inflammatory effects are associated with 20-40 minutes of moderate exercise, five times per week. One mechanism by which exercise may reduce inflammation is through the promotion of fat loss. Adipose (fat) tissue releases molecules called adipokines. Adipokines lead to a chronic low-grade state of inflammation by triggering the release of chemicals that activate immune cells and damage nearby tissue.8 Adipokines have been associated with diseases such as type 2 diabetes mellitus.4 Exercise also stimulates the release of chemicals called endorphins in our brain, which reduce stress,6 and consequently, inflammation.
Complementing sufficient aerobic exercise is a well-rounded diet. Consider replacing fried foods, refined carbohydrates and processed meats that are known to elevate inflammation with anti-inflammatory foods. A good mnemonic to remember for those who love fish is “SMASH,” abbreviated for Salmon, Mackerel, Anchovies, Sardines and Herring; these fish contain high amounts of omega-3, a fatty acid our body does not produce, but has important effects in reducing
the production of pro-inflammatory molecules.2 Other foods with anti-inflammatory benefits include those rich in antioxidants such as berries and cruciferous vegetables. “Good” fats such as avocados and olive oil, as well as foods such as nuts, turmeric and dark chocolate can also reduce the amounts of pro-inflammatory chemicals in our bodies. One study found that consuming one gram of omega-3 a day can reduce the risk of a heart attack by five percent.12
Reducing stress is a personalized journey that differs for everyone. Though there is no universal solution, an effective first step is identifying our stressors. This allows us to work on managing or resolving them by spending time with loved ones, attending therapy, mindfulness-based stress reduction (MBSR) and exercise. There are a variety of supplements advertised as effective at reducing stress, and further research is needed to confirm this. Some supplements that have shown promise to lower stress is melatonin (to regulate sleep cycles11; magnesium1; and Rhodiola rosea.5 Through embracing anti-inflammatory lifestyle changes such as stress reduction, diet modification and exercise, we possess the ability to live a healthy and happier tomorrow.
References:
1. Boyle, NB, Lawton, C, & Dye, L. (2017, Apr 26). The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review. Nutrients, 9(5). https://doi.org/10.3390/ nu9050429
2. Calder, PC. (2017, Oct 15). Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans, 45(5), 1105-1115. https://doi.org/10.1042/BST20160474
3. Cerqueira, E, Marinho, DA, Neiva, HP, & Lourenco, O. (2019). Inflammatory Effects of High and Moderate Intensity Exercise-A Systematic Review. Front Physiol, 10, 1550. https://doi. org/10.3389/fphys.2019.01550
4. Chait, A, & den Hartigh, LJ. (2020). Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front Cardiovasc Med, 7, 22. https://doi.org/10.3389/fcvm.2020.00022
5. Edwards, D, Heufelder, A, & Zimmermann, A. (2012, Aug). Therapeutic effects and safety of Rhodiola rosea extract WS(R) 1375 in subjects with life-stress symptoms--results of an open-label study. Phytother Res, 26(8), 1220-1225. https://doi. org/10.1002/ptr.3712
6. Jackson, EM. (2013). STRESS RELIEF: The Role of Exercise in Stress Management. ACSM’s Health & Fitness Journal, 17, 14–19.
7. Liu, YZ, Wang, YX, & Jiang, CL. (2017). Inflammation: The Common Pathway of Stress-Related Diseases. Front Hum Neurosci, 11, 316. https://doi.org/10.3389/fnhum.2017.00316
8. Mancuso, P. (2016). The role of adipokines in chronic inflammation. Immunotargets Ther, 5, 47-56. https://doi.org/10.2147/ ITT.S73223
9. Mariotti, A. (2015). The effects of chronic stress on health: new insights into the molecular mechanisms of brain–body communication. Future Science OA, 1(3), null. https://doi.org/10.4155/fso.15.21
10. Medzhitov, R. (2010, Mar 19). Inflammation 2010: new adventures of an old flame. Cell, 140(6), 771-776. https://doi. org/10.1016/j.cell.2010.03.006
11. Satyanarayanan, SK, Su, H, Lin, YW, & Su, K. P. (2018). Circadian Rhythm and Melatonin in the Treatment of Depression. Curr Pharm Des, 24(22), 2549-2555. https://doi.org/10.2174/13816 12824666180803112304
12. Shen, S, Gong, C, Jin, K, Zhou, L, Xiao, Y, & Ma, L. (2022). Omega3 Fatty Acid Supplementation and Coronary Heart Disease Risks: A Meta-Analysis of Randomized Controlled Clinical Trials. Front Nutr, 9, 809311. https://doi.org/10.3389/fnut.2022.809311

Gregory Michael Tomlinson is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. He is passionate about preventative and lifestyle medicine, and interested in pursuing psychiatry or neurology.

Arunabh Bhattacharya, PhD, is an Associate Professor at the University of the Incarnate Word School of Osteopathic Medicine. He is passionate about researching factors that influence healthy aging.

Ramaswamy Sharma, MS, PhD, is a Professor at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.
By W. Allen Fink, DO, MHA, CPE, FACEP, FACHE
UT Health Outpatient and Surgery Center at Kyle Seale Parkway opened its doors and began welcoming patients this spring.
At a recent ribbon-cutting ceremony to celebrate the opening, Acting President Robert Hromas, MD, FACP, said: “We are on a mission here at UT Health San Antonio to make lives better. It’s a mission we live out every day by increasing access and advancing medicine.”
I couldn’t agree more. We dedicate ourselves to meeting the healthcare challenges our community faces today and will face in the future.
The new five-story, 108,000-square-foot outpatient and surgery center offers primary care and specialty care at one state-of-the-art location.
This is why UT Health San Antonio is remarkable. This facility allows us to offer critically needed specialties including obstetrics and gynecology, orthopaedics, ophthalmology, radiology and urology, all connected in one place, to create multidisciplinary yet individualized care for the people of the Northwest Side of San Antonio.
Its location — off Loop 1604 — is no coincidence.
Strategically built near The Rock at La Cantera and The University of Texas at San Antonio, the location also serves as the central hub for UT Health San Antonio’s growing sports medicine program. Its mission? To keep athletes and all South Texans moving and to enhance human performance.
As the Official Sports Medicine Partner of the San Antonio Spurs and the Official Health Care Partner of UTSA Athletics, UT Health San Antonio brings advanced sports medicine services to professional and collegiate athletes, and patients of all ages.
The sports medicine program at UT Health San Antonio has a rich history — pioneering expert musculoskeletal care across South Texas for more than 50 years.
From diagnosis to treatment and rehabilitation, our integrated team of highly specialized orthopaedic providers, psychiatrists and primary care physicians collaborate seamlessly to provide a multidisciplinary approach to athletic health.
That means at UT Health San Antonio, the community can get expert multispecialty treatments for sprained ankles, concussions, arthritis, tennis elbow or torn ACLs with board-certified professional and collegiate team doctors.
Guy Nicolette, MD, is among them. He serves as the lead sports medicine physician for the San Antonio Spurs and is an associate clinical professor at the Long School of Medicine at The University of Texas Health Science Center at San Antonio. He also treats patients at UT Health at Kyle Seale Parkway and brings over 20 years of experience to the team.
Both the Spurs and UT Health San Antonio are committed, in word and deed, to translating all that we learn from taking care of elite athletes into better health for the greater San Antonio community.
Nicolette and the entire sports medicine team are dedicated to treating every patient like professional players.
From modern treatments for joints, bones and muscles to concussion management and sports psychology, UT Health at Kyle Seale Parkway offers patients advanced ultrasound imaging for both bedside diagnostic and therapeutic use, such as orthobiologic injections.
Our approach is grounded in modern techniques. Proven interventions including shockwave therapy and platelet-rich plasma injections can be tailored to address a spectrum of conditions that may impede an active lifestyle.”
When surgery is needed, patients can receive surgical care at the UT Health Outpatient and Surgery Center at Kyle Seale Parkway.
The surgery center is staffed by board-certified surgeons, anesthesiologists, registered nurses and medical technicians specially trained in surgical and recovery care. It provides safe, contemporary suites for surgical procedures that don’t require an overnight stay.
UT Health at Kyle Seale Parkway was built to create more access to the top-tier academic medicine our community needs and deserves. Its opening is momentous for our institution and for the patients we are privileged to serve.

W. Allen Fink, DO, MHA, CPE, FACEP, FACHE. is the Chief Medical Officer at UT Health San Antonio. He oversees a comprehensive medical group, an Ambulatory Surgery Center and the soon to open Multispecialty and Research Hospital. Dr. Fink is board-certified in Emergency Medicine, a Certified Physician Executive, and a Fellow of both the American College of Healthcare Executives and the American College of Emergency Physicians. He is an Associate Professor/Clinical at the UT Health San Antonio Joe R. and Teresa Lozano Long School of Medicine and holds a cross appointment at the University of Texas School of Public Health, San Antonio.





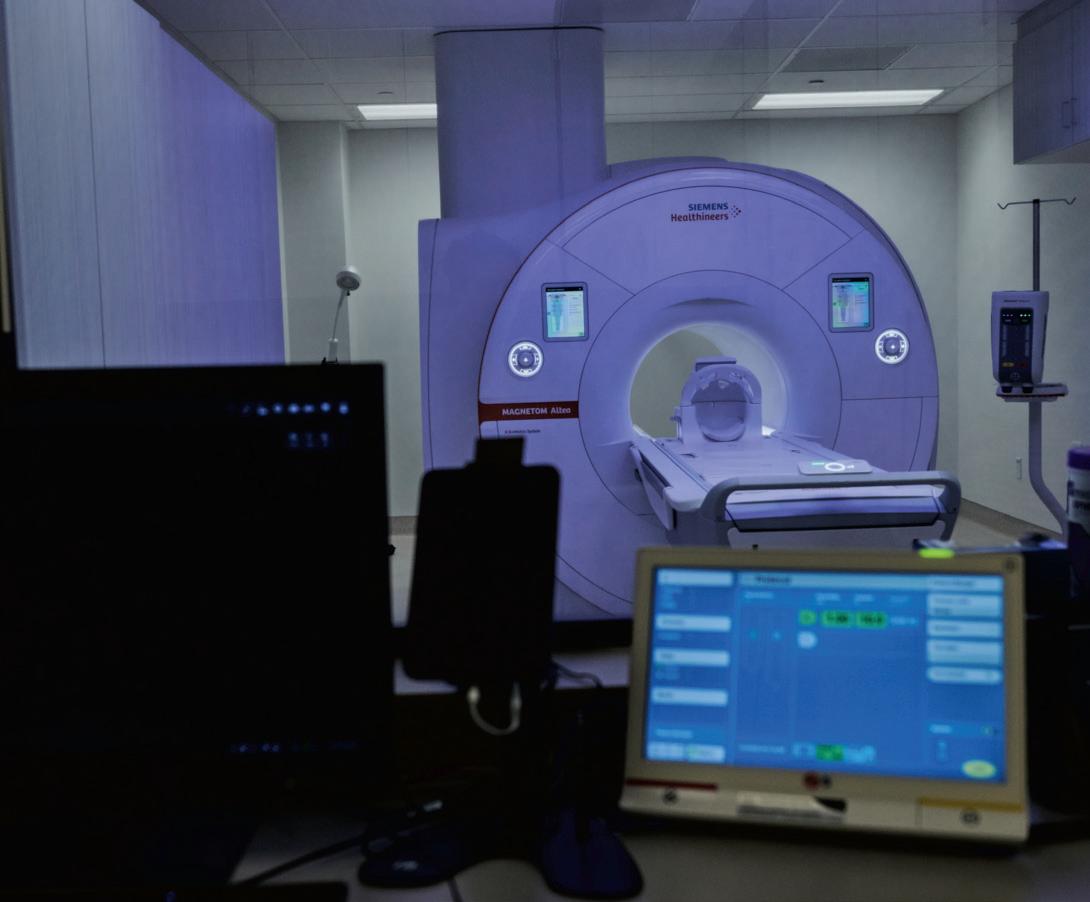
By Michael L. Kreager, JD, LLM

This year adds two more compliance deadlines for physicians and their medical practices.
September 4, 2024
New FTC Rule. The Federal Trade Commission adopted a rule in April that bans most covenants not to compete.
Action Required. By September 4, 2024, employers must inform their workers that any post-employment restrictions on competition are no longer enforceable. The rule applies to virtually all workers, including physicians.
Content of the Notice. The notice must identify the employer and must be sent to its workers who are subject to a noncompete. Workers include employees and independent contractors who are subject to a noncompete, including former workers. The notice must state that the noncompete will not be, and cannot legally be, enforced against the workers. The notice can be hand delivered, mailed, sent by email or sent by text.
Why. The FTC’s rule is effective September 4, however, employers must send the notice to workers by that date. The rule effectively bans existing and future noncompete agreements that apply after the end of employment. Only the portion of the agreement that is a noncompete will no longer be enforceable. The remainder of the agreement will still operate. Amendments to the agreement are not necessary.
Court Challenges. There are several court cases pending that seek to challenge the rule. If a court does not delay the rule before this date, employers will still need to send the notice to their workers and refrain from entering into new noncompetes.
Who Is Affected. The rule applies to all employers who are not otherwise outside of the FTC’s jurisdiction, e.g., state institutions. Nonprofit corporations are usually outside the FTC’s jurisdiction, but nevertheless, under certain circumstances, the rule may apply to some nonprofits.
Important Exceptions. The rule does not outlaw a noncompete while the worker is engaged; it applies only after the end of engagement. The rule grandfathers existing noncompete agreements with senior executives making $151,164 or more annually and having final policy-making authority. But the rule outlaws new noncompetes with senior executives after September 4. Employers may still enforce violations of their noncompetes that occur before September 4. Lastly, a buyer of a medical practice may still require noncompetes from the sellers. Similarly, a noncompete may be required in connection with the purchase and sale of an ownership interest in a practice.
More Information. This summary is not exhaustive and does not cover all the specifics of the FTC’s rule. You can obtain more information about the rule at https://www.ftc.gov/legal-library/browse/rules/ noncompete-rule, and be sure to get legal advice from your attorney.
BOI Reports. The Corporate Transparency Act became effective January 1, 2024. The new law requires small businesses to report to the Financial Crimes Enforcement Network (FinCEN), a bureau of the Department of Treasury, identifying information about its owners and senior officers. These reports are called Beneficial Ownership Information, or BOI, reports.
Deadline for Reporting. All entities formed before January 1, 2024, must file their BOI reports with FinCEN before December 31, 2024. Entities formed during 2024 must file their BOI reports within 90 days of formation. Entities formed after 2024 must file their BOI report within 30 days of formation.
Responsible Reporting Person. The small business is responsible for filing the BOI report. Virtually all small businesses are subject to the reporting rule, which includes professional associations (PA) and professional limited liability companies (PLLC). In addition, all other physician-owned entities, such as family limited partnerships, corporations and limited liability companies must file a BOI report with FinCEN.
Information Reported. Each person owning 25 percent or more of the business entity and each officer must provide a photo ID, such as a current driver’s license, which will be uploaded to FinCEN as part of the BOI report. It is important to remember that the business entity must report changes in its BOI information within 30 days, such as a change in an owner’s current residential address.
Failure to Report. There are civil and criminal penalties for willfully failing to comply with the law.
More Information. More information can be found at FinCEN’s website at www.fincen.gov/boi. The law and its implementing regulations are complex. Talk to your CPA or attorney for advice about compliance.
BCMS thanks attorney Mike Kreager with the Kreager Mitchell PLLC law firm for highlighting these deadlines.

Michael L. Kreager, JD, LLM, is the founder of Kreager Mitchell PLLC, a San Antonio law firm serving the needs of physicians. He has authored several books on physician employment contracts for the Texas Medical Association. In addition, he authored the popular guide, “The Physician Employment Contract,” which is in its fourth edition. It is a free publication.
By Gabriella Bradberry
More and more women than ever are becoming doctors, with female medical students beginning to outnumber their male peers in recent years.1 This shift in medical school attendance is an exciting development for both the world of medicine and women alike. With this ever-increasing percentage, it is difficult to believe that not so long ago, the number of licensed female physicians was an absolute zero. During the early years of American history, a few women worked as apprentices and practiced as unlicensed physicians, but none were permitted to attend medical school.2 It was not until 1849 that Dr. Elizabeth Blackwell cemented her place into history as the first woman to receive a medical degree in America, thus helping pave the way for the female physicians of today.
Initially, Blackwell did not plan to pursue medicine and instead worked as a schoolteacher in Cincinnati alongside her mother and sister. It was not until her close family friend, Mary Donaldson, fell deeply ill that her perspective and goals shifted.3 While on her deathbed, Donaldson, who was likely dying due to uterine cancer, confided to Blackwell that she would have been more comfortable seeking treatment earlier had she been able to explain her symptoms to a female physician. This devastating confession ignited Blackwell with the goal to earn her medical degree and become the physician that her friend had so desperately needed.
The road to achieving a medical degree would be filled with many obstacles. Blackwell was not the first woman in America to pursue entrance into medical school. During the 1800s, few medical schools existed and none accepted women, leaving women to pursue alternative routes of education. Rather than be discouraged by the odds in front of her, Blackwell studied rigorously, attended medical lectures, worked as an apprentice, and applied to any and every medical school she could find.
Finally, Elizabeth Blackwell’s application arrived at the desk of the dean of Geneva Medical College in upstate New York. The dean was eager to reject Blackwell’s application, but along with it came an astute letter of recommendation from a well-respected physician she studied with. Rather than risk displeasing a colleague, the dean opted to have the student body vote on the matter, and much to his surprise, the students decided to admit Blackwell as part of a practical joke.4 Regardless, Blackwell remained serious in her pursuit of a medical degree and instantly accepted the invitation with immense gratitude.
While Blackwell was technically accepted into medical school, she was not met with welcoming arms. Silence overcame the other students the moment she first walked into class. Eventually, her peers would soon overcome their shyness in favor of throwing paper darts at Blackwell. She ignored these attempts of provocation, but when the professors attempted to bar Blackwell from attending classroom dissections, she protested for the right to attend.4
Despite the continuous pushback Blackwell faced from the community surrounding her, she continued to diligently work toward earning her
diploma, gaining the respect of the students and faculty along the way. On the morning of January 29, 1849, Blackwell’s efforts proved worthy when she graduated top of her class and became the first woman in America to earn a medical degree.5
While Blackwell’s career did not magically develop into one without discrimination and challenge, she felt solace in seeing the affects her accomplishment had on other women. In fact, Dr. Elizabeth Blackwell even inspired her very own sister, Emily, to pursue a medical degree of her own and become a surgeon. Together, the Blackwell sisters established the New York Infirmary for Women and Children in 1857, where they pursued the mission of providing care for women and positions for female physicians.2
Blackwell would later go on to open a medical college in New York City and eventually move permanently to London where she taught as a professor of gynecology. Throughout her career, she would emphasize preventative care and personal hygiene and eventually assist in the founding of the National Health Society and U.S. Sanitary Commission.2
Dr. Elizabeth Blackwell passed away in 1910, but the impact she had on women’s rights and the medical world are eternal. During her life, she tirelessly strived to create opportunities for fellow female physicians, and her legacy serves as a continuous inspiration to persevere even in the face of discrimination. In the words of Dr. Elizabeth Blackwell herself, “It is not easy to be a pioneer — but oh is it fascinating! I would not trade one moment, even the worst moment, for all the riches of the world.”5
References:
1. O’Connell-Domenech, A. (2024, Feb 22). More women than ever are becoming doctors; here’s why there are still so few. The Hill. https://thehill.com/changing-america/respect/equality/4479304-more-women-than-ever-are-becoming-doctorsheres-why-there-are-still-so-few/
2. Michals, E. (2015). Elizabeth Blackwell. National Women’s History Museum. https://www.womenshistory.org/education-resources/biographies/elizabeth-blackwell
3. NUHW Editors. (2022, March 17). Elizabeth Blackwell. National Union of Healthcare Workers. https://nuhw.org/elizabeth-blackwell/
4. Fuller, M. (2003, May & June). Woman attends medical school. Hobart and William Smith. https://www.hws.edu/about/history/elizabeth-blackwell/woman-attends-medical-school.aspx
5. Biography.com Editors. (2021, March 31). Elizabeth Blackwell Biography. Biography.com, https://www.biography.com/scientist/elizabeth-blackwell

Gabriella Bradberry is the Admin/Communications Specialist for the Bexar County Medical Society.

Artist’s Note: This painting is based on a picture I took on my trip to India. It depicts a young girl in a village in Rajasthan who was carrying large pieces of wood to help her mother cook in a traditional-wood burning stove. In these regions, cooking is still carried out this way because they do not have access to cooking-gas stoves. Families like hers represent vulnerable populations who live in remote areas with limited access to medical care. This particular village is situated in a desert region which is subject to high temperature, and inhabitants can suffer from conditions like dehydration, heatstroke, depletion of nutrition, which are only worsened by global warming and the resulting higher temperatures. It is necessary as healthcare providers to advocate for more healthcare facilities for people living in rural areas to ensure equal access to care. We also need to become stewards of the environment in these times of changing climates to reduce the negative effects of global warming on people living in vulnerable areas.
Class of 2026
Long School of Medicine UT Health-San Antonio

Artist’s Note: I sought to explore the role of familial bonds in planetary health through acrylic painting. I wanted to highlight the joy and wonder that can exist in simple acts of living, generational guidance, and the evolving responsibilities of children. The color palette was pulled from hues observed in photographs of Earth from space, creating a visual connection between the microcosm of a shared meal between individuals, and the macrocosm of our planet. I drew inspiration from my journey as first a daughter reliant on family guidance and the wonder that comes with it, to assuming responsibility to shed light on community and planetary questions as a future healthcare worker, and the eventual obligations to family as their caretaker and living memory. Through a shared bowl of rice, I want to invite contemplation on our collective responsibility to nurture and protect both our personal history and the planet for current and future generations.
Long
UT Health-San Antonio
By Lori Boies, PhD, MPH
Our Bexar County Medical Society Alliance is one of the oldest in the state of Texas (third oldest to be exact). The Alliance — named the Auxiliary at the time — first met on October 29, 1917 at the Menger Hotel to make surgical dressings for the local Red Cross during World War I. In May of 1918, during the TMA annual session in San Antonio, 350 doctors’ wives organized the Alliance to the State Association, and Mrs. E. H. Cary was elected the first president.
Early on, emphasis was placed on serving the community with health education programs, promoting friendship among doctors’ families, and taking an active interest in legislative matters affecting medicine on both state and federal levels. Women’s suffrage was still in Congress in 1919, but the early Alliance showed insight that women’s roles were changing forever.
In the 1930s, the Alliance assisted with a city-wide survey of preschool children in cooperation with a national program for child health and protection — a delegate was invited to attend meetings of a national movement at the White House conference in February 1931. Over the following years, the Alliance strengthened and expanded its focus on bringing needed healthcare programs on nutrition, safety, science fairs and health careers to the San Antonio community, while continuing to be active in legislative issues.
In the 1990s, the Alliance joined the state auxiliaries to focus on our youth with “Healthier Youth 2000,” and partnered with schools on a “Drug- Free Graduation.” We addressed the AIDS crisis in San Antonio, providing supplies for children in crisis, and we reached across our southern border to aid impoverished pueblos outside of Mexico City with donated medical supplies and medical care. We continued to support the education of nurses with scholarships, raised funds for medical research and student loans, and participated in legislation at the local, state and federal levels. Organ donation and breast cancer awareness were key efforts, with our Breast Cancer Bingo touted an award-winning program.
Through years of dedicated service, we have forged friendships through the Book Club, Playgroup, cooking classes, investment seminars and other supporting social events. Today, Alliance membership has grown to better reflect the changing physician family, with male spouses joining the traditionally female Alliance, physicians themselves joining to support the Alliance, and 2013 saw the election of our first male Alliance president.
From its inception, the Alliance was organized “to create fellowship among families of physicians and to foster activities in benevolent, philanthropic, charitable and patriotic endeavors.” As the Alliance prepares to celebrate its 107th anniversary, I feel that this statement still fully embodies what we represent.
How do we continue to “create fellowship among families of physicians,” when the definition of the physician family has changed since the founding of the Alliance during World War I? We recognize that

half of graduating medical students are female; many households now have two working spouses (possibly two physicians), and the role of the traditional “housewife” has evolved. While being the spouse of a physician grants us many benefits, there are inherent sacrifices. I joined the Alliance in 2010 when my husband, Brian, and I moved to San Antonio for his residency. The Alliance proved to be a cornerstone in making San Antonio feel like home in those early, demanding years. The friendships I have gained have always been refreshing to me, a silver-lining, as physician families alone understand the rigors of a life in medicine. This was exemplified in the ways we came together during the stressful COVID years. We all rallied around each other as we dealt with the fear, uncertainty and sometimes even more demands on our spouse’s time. When we lost one of our beloved past-presidents, Rebecca Christopherson (2015), to COVID, we came together to honor her through planting a tree in her neighborhood so that all could remember her bright spirit. Ultimately, we are the family of medicine.
How do we stay true to the pledge to “foster activities in benevolent, philanthropic, charitable and patriotic endeavors” a century after our inception? We have many volunteer opportunities organized by our VP of Civic and Philanthropic activities for our members who are interested in serving our community. Historically, we have given away thousands of bicycle helmets to children through the TMA Foundation’s “Hard Hats for Little Heads” program to prevent head injuries. We have also participated in immunization drives, addressed issues around alcoholism and period poverty, volunteered at men’s and women’s shelters, provided books to children with cleft lips and palates to help bolster self-esteem, partnered with the TMA Foundation to enhance literacy by providing books to pediatrician’s offices, and countless other initiatives in our 107 years of giving back to our county through the lens of creating a healthier community. Additionally, we raise thousands of dollars in scholarships for university students in Bexar County studying Pre-Health Professions, and provide scholarships to medical students at both UT Health San Antonio Long School of Medicine and the University of the Incarnate Word School of Osteopathic Medicine. Since 1917, the BCMSA has served as a beacon in the medical community to answer the call with creative solutions when needs arise in our county.
I was honored to serve as the 2017 BCMSA President during our Centennial Celebration. The presidents who both served immediately before and after me are legends in their own right, as they have gone on to serve as President of the Texas Medical Association Alliance — Jennifer Lewis (2016) and Jenny Shepherd (2018). Jenny is our current TMAA president and has shined through her work in advocacy, being the only two-time winner of the TEXPAC June Bratcher Award for Political Action, as well as being recognized nationally by the AMA Alliance. We are lucky to be surrounded by such trailblazers in our own county who are generous with their time.
It is bittersweet for me to reminisce on my time with the Alliance as the Boies family is relocating to Greensboro, NC where Brian serves as the Chief Academic Officer and Senior Vice President of Cone Health. For both of us, the Alliance and Bexar County Medical Society helped us grow into the individuals we are today through the opportunities afforded to us. I feel that I grew up with the Alliance, as these friends saw me defend my PhD dissertation, get my first real job, and celebrated the birth of our daughters, Helen and Julie, by graciously throwing the most beautiful showers for me and offering help whenever I needed it. I would not be the person I am

Among the other new officers of the Woman's
the
County Medical Society are, from left to right above, Mesdames M. A. Childers, Jr., publicity secretary; Russell T. Snip, treasurer; Cornelius H. Nau, corresponding secretary, and Royall N. Calder, fourth vice-president.


today without the Alliance. I am extremely indebted to the Alliance and the beautiful friendships I have made in the past 14 years. If you aren’t a member of the Bexar County Medical Society Alliance yet, I hope you decide to join the family of medicine.

Lori Boies, PhD, MPH, is the 2023 – 2024 TMAA VP of Fiscal Affairs, and the 2017 BCMSA President. She is an Assistant Professor of Biological Sciences and Bioinformatics at St. Mary’s University

the Women’s Auxiliary to the Bexar County Medical Society assisting with the entertainment of visitors.



We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark
President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank
(HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank www.broadwaybank.com
“We’re here for good.”

The Bank of San Antonio (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the
few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier 210-807-5581
Brandi.Vitier@thebankofsa.com www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner
210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (★★★ Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com www.americanhealthimaging.com (main site) www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)


Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor
210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
www.hancockwhitney.com
John Riquelme San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com

Conviva Care Center (HHH Gold Sponsor)
Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better
outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter 812-272-9838
KGary4@humana.com www.convivacareers.com
“Fuel Your Passion & Find Your Purpose”

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
https://uthscsa.edu/ Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
Healthcare Administration Consultants (HH Silver Sponsor)
Our mission is to help healthcare organizations small or large to achieve sustainable growth and success by providing them with expert healthcare administration consulting services. We focus on key factors such as: revenue, supply chain visibility, and aligning operations to save time so that your team can focus on improving the patient’s health and well-being. We transform patient care outcomes and employee working experiences while driving brand and revenue growth.
Dr. Reshma Beherry, DHA
Doctor of Healthcare Administration
210-602-6905
RB@administrative-consultants.com
https://administrative-consultants.com/
SERVICES

Equality Health
(HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner 844-554-3473 Rachel@dialops.net
Insperity
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone
Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits 512-370-1776
Wendell.England@tmait.org 800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvis Medical Suites
(HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer
210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol Field Sales Consultant 210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct)
KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor) SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® QKA Senior Private Wealth Advisor 512-649-8113
Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We’re Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Mike DeQuattro
Director of Operations - Texas & New Mexico 210-918-8737
Mike.DeQuattro@favoritestaffing.com “Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Pedro Caretto VP of Business Development 786-437-4009
PCaretto@eleosvhs.com www.eleosvhs.com

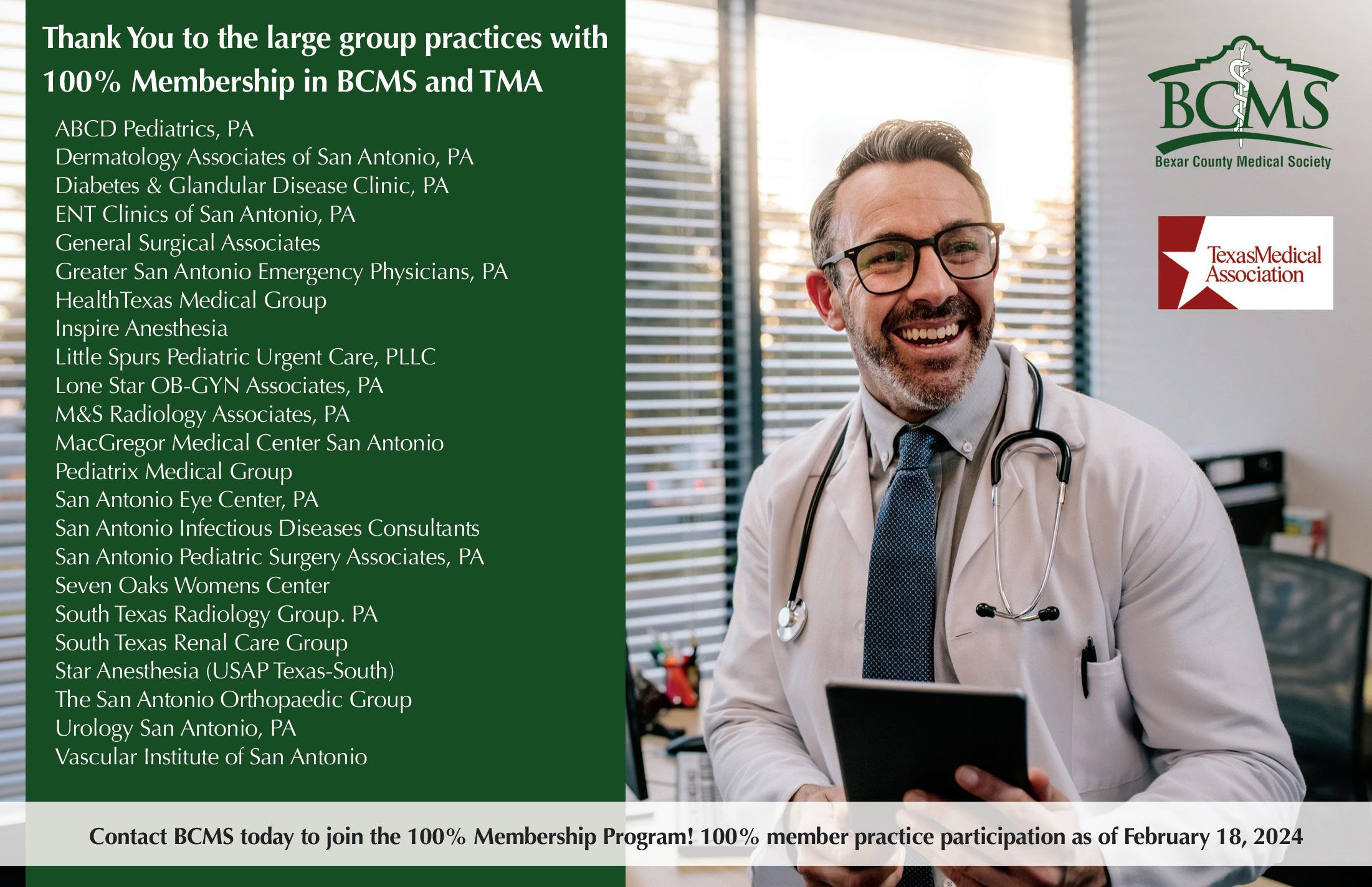

By Stephen Schutz, MD




Audi is now a leader in the luxury battery electric vehicle (BEV) space, and they’ve achieved that status by building vehicles that provide the “Audi-ness” customers crave along with all-electric propulsion.
The 2024 Q8 e-tron® Sportback SUV is their latest effort, and it’s a good one. Just remember my usual words of caution to anyone considering a new BEV (more on this below).
For starters, the Q8 e-tron Sportback is yet another example of a luxury SUV that’s been coupe-ified — think Porsche Cayenne Coupe or BMW X6 — which is either a good or bad thing depending on your point of view. If you want maximum utility, you won’t appreciate the loss of interior space in the Sportback, and in that case I’d refer you to the standard (and boxier) Q8 e-tron. On the other hand, if you want more sportiness combined with a sleeker exterior design, then the Q8 e-tron Sportback is for you.
Speaking of exterior design, the Q8 e-tron Sportback is attractive with a flowing profile augmented by — and this is typical Audi — space age and very attractive head- and taillights.
One of the pillars of Audi luxury leadership since the 1990s has been exterior lighting, and Audi’s newest models move that area of excellence forward. Every light that you can see is LED (obvs), but the way the lights are shaped and move is pleasurable to behold. Naturally they do their job very well and don’t just look cool. Just when I think another brand is approaching Audi’s lighting abilities, Volkswagen’s venerable luxury brand takes another step forward.
The same is true for the Q8 e-tron Sportback’s interior, which is attractive and technologically advanced. While everything has been digitalized, including the gauge cluster behind the steering wheel, the familiar Audi touchstones of black background/white numbers/ red needles remain, as do the expensive looking and feeling materials that remind you every time you get behind the wheel that all those hours of hard work you’ve spent in the hospital or your office have been rewarded.
There is less of that feeling when you sit in the back seat though, because the sloping roofline that adds to the Q8 e-tron Sportback’s good looks subtracts from rear seat headroom. I’m 6’2” and felt claustrophobic back there, and luggage space under the rear hatch is also limited.
Driving the Q8 e-tron Sportback is similar to what you’d experience behind the wheel of a regular internal combustion Q8, only quieter. The suspension, clearly tuned to “comfort,” handles bumps and potholes with ease, and the Q8 e-tron Sportback’s highway manners are excellent. Athletic maneuvers, however, are umm, not encouraged, and agility is limited by the big Audi’s 5,962lbs curb weight.
The Q8 e-tron Sportback is quick, though. Car and Driver reported a 5.2 second 0-60MPH time, which is impressive. Less impressive is the 296-mile range on a full charge, a number that we all know reflects optimal temperatures and conditions.

Pricing for the Audi Q8 e-tron Sportback BEV starts at around $79,000 for the Premium and maxes out at $90,000 for loaded Prestige models. Not cheap.
And that brings me to my usual words of caution about BEVs: Before buying an Audi Q8 e-tron Sportback or any other BEV, think about how you’ll use it. If you have a home charger, commuting and running errands in a BEV are a cinch, but long trips may be challenging. Automotive News and The Wall Street Journal have recently reported that the charging infrastructure isn’t what it should be to support long trips in a BEV, and outages at existing charging stations are a continuing challenge.
In addition, resale values for BEVs generally lag behind their equivalent internal combustion competitors, so consider leasing. Of course, BEVs come with government incentives unavailable to buyers of vehicles that burn gasoline, so there are a number of factors you need to consider. (For the record, government BEV incentives are usually offered to customers who lease BEVs, not just those who purchase them.)
The Audi Q8 e-tron Sportback is a luxury BEV that brings the “electric” while also bringing the “Audi.” If you want an all-electric car that gives you both of those things, give BCMS’ Phil Hornbeak a call at 210-301-4367.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson
877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Auto Group
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000