THE TECH EFFECT
Medical Imaging Advancements Facilitate Higher Standards of Care


CHANGING THE NARRATIVE
CHANGE
Through innovation we want to change the perspective in the imaging space.
CONTROL
We want to put the control back in the hands of the decision makers.
COST SAVINGS
We understand our customers goals and we are developing a clear pathway to measurable savings.



has been with Tri-Imaging for 11 years!


Reduce risk of wire contamination, free up hands, and organize wires in the sterile field
Invented by an interventional radiologist, CaraClip™
• is a sterile, self-adhesive device that can remain in place for at least 8 hours on dry surfaces, can be repositioned, and withstands fluids such as blood, saline, iodine, contrast, and sterile water
• allows technologists to easily curve, redirect, and advance guidewires without fear of falling outside the sterile field
• instills confidence that devices will be contained in the wire protector, freeing up hands to focus on other important tasks



learn more and see CaraClip in action or visit
Call 1.800.233.5539 or email info@beekley.com to request a sample of CaraClip wire protector today Visit beekley.com/caraclip for Product Safety Information







FEATURES

DIRECTOR’S CUT
Fostering a thriving safety culture goes far beyond fulfilling compliance requirements.
COVER STORY
POCUS, photoncounting CT and theranostics are among the latest high-tech advances in diagnostic imaging professionals have an eye on in 2024 and beyond.


RISING STAR
Career pathway program and hard work pay off for Caitlin LaVoie.


SEPTEMBER 2024



IMAGING NEWS
Catch up on the latest news from around the diagnostic imaging world.

PRODUCT FOCUS
A look at different training options offered in the imaging realm.
EMOTIONAL INTELLIGENCE
People trying to assert themselves can easily create problems if they become aggressive.
President
Vice
Kristin Leavoy kristin@mdpublishing.com
Vice
Jayme
Group
Megan
Editorial John
Editorial
Jason
Melody
Verlon
Rachel
Traci
Art
Karlee
Kristin
Webinars Linda
Digital
Cindy
Haley
Accounting
• On-Site Repair
• Depot Repair
• Parts Sales and Parts Identification
• Loaner Availability
• Technical Support
• Training
• Injector System Sales
• Preventative Maintenance Tools









STEPHANIE BENAVIDEZ
FOCUS IN

BY JOHN WALLACE
Oswego Health makes it a priority to recognize staff for their hard work and commitment to the organization and its patients. One key staff member who continues to shine is Stephanie Benavidez, an article on the health system’s website states.
Benavidez was recently promoted to radiology manager at Oswego Health. Benavidez started her career in the imaging department at Oswego Hospital in 2016, before transitioning in 2019 to serve as a radiologic technologist at the Center for Orthopedic Care.
Born and raised in Phoenix, New York, she earned her Certificate of Radiography from St. Mary’s Hospital in West Palm Beach, Florida, in 1993 and has been licensed in New York since 1994. Benavidez graduated with a Master of Science in Health Services Administration in 2007 and a Master of Business Administration from University of St. Francis in 2010.
The Oswego Health medical imaging department features the most advanced technology and provides a range of services, from general X-rays to computed tomography (CT) and magnetic resonance imaging (MRI). There are five imaging locations throughout Oswego County, including inpatient services at Oswego Hospital and four outpatient locations. As the radiology manager, Benavidez manages the outpatient centers at Oswego Health Services Center, Pulaski Health Center, Fulton Medical Center, and Central Square Medical Center.
Benavidez shares, “I originally started my career at a large hospital in CNY and it just didn’t feel like a family or team. To have this new leadership opportunity in a place that I call home is just amazing. I’m excited to get more involved within the community to provide the best care possible locally.”
As her career advances, Benavidez wants to make it easy for her coworkers to follow her lead.
“I want to be the kind of leader that is respected and trusted. I have learned to allow my staff to do their jobs and not micromanage while being accessible. I appreciate that everyone has different learning capabilities and may have multiple ways of achieving the same goals,” she says.
Her leadership style was no doubt shaped by her mentors.
“I have had multiple mentors and I still have several that I look to for advice and guidance. One of the most important things I have been taught is to be a better listener and not be too quick to judge. I would love to think I am a mentor for another imaging professional,” Benavidez says.
How did she decide on a career in imaging? It all goes back to being a curious child.
STEPHANIE BENAVIDEZ
Radiology Manager at Oswego Health
1. What book are you reading currently? “Atomic Habits” by James Clear.
2. Favorite movie? “Pitch Perfect”
“My stepmother worked in a cardiology office, and I was interested in their ultrasound. I was told that if I wanted to do ultrasound, I would need to go to X-ray school first. I found a wonderful program at St. Mary’s Hospital in West Palm Beach, Florida, with a two-year degree in radiologic technology,” she says.
“Medical imaging has been one of my best life choices. There has never been a worry about needing to find employment and it has been extremely fulfilling with all the different aspects and opportunities available,” she adds.
Another great life choice was saying, “I do.”
“My husband and I are fortunate to have two grown sons, one of which has given us the gift of being grandparents. We have a two-year-old granddaughter and a 6-month-old grandson. Our third child is the furry kind, a 110-pound Siberian Husky named Frankie Blue Eyes,” she says.
Looking ahead, Benavidez predicts big things in imaging.
“I believe AI will become a large part of imaging and, if I had to guess, because of the shortage of radiologists, AI will be a way of getting quicker results,” she says. •
3. What is something most of your coworkers don’t know about you? I always wanted to be a school teacher.
4. Who is your mentor? Arlene Young and Megan McManus. I crave their knowledge and abilities.
5. What is one thing you do every morning to start your day? Visit with my dog, Frankie.
6. Best advice you ever received? Don’t be so consumed by work that you miss out on family and friend time.
7. Who has had the biggest influence on your life? My children. They have kept me grounded and given me the most happiness.
8. What would your superpower be? A mind reader.
9. What are your hobbies? Decorating cakes, cupcakes, cookies, crocheting and reading.
10. What is your perfect meal? Any meal that is sitting down with the people I love most.
STAR RISING
CAITLIN LAVOIE

Career pathway program and hardwork benefit Caitlin Lavoie.
Caitlin LaVoie holds a Bachelor’s of Science in Medical Imaging and a Bachelor’s of Technology in Healthcare Management with certifications in mammography and diagnostic radiology. Her current job title is mammographer with Oswego Health. LaVoie benefitted from a career pathway program at Oswego Health. Her hard work helped her advance from being an employee in patient access to become an X-ray technologist.
“Caitlin’s story is pretty cool and something we’re very proud of,” wrote Jamie Leszczynski, and senior vice president of communications & chief brand officer. ICE Magazine recently found out more about LaVoie and her imaging career.
Q: WHERE ARE YOU FROM?
A:
Fulton, New York
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION? WHAT DEGREES/CERTIFICATIONS DO YOU HAVE?
A: SUNY Upstate Medical University; Bachelor’s Degree in Medical Imaging; Training in Diagnostic Radiology and Mammography.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: When I worked in patient access at Oswego Health’s Fulton Medical Center in 2018, I spent a lot of time with the radiology staff. After learning more about the profession, I knew it was something I was interested in. I also love the challenge. Every exam I do I am always trying to do better than before to improve my skills and ultimately provide optimal images for the patient/doctor.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: The most rewarding aspect of my job is helping people by providing diagnostic images or screening exams to assist the doctor in their findings.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I love working directly with patients, and helping them learn more about why they are coming into the department and what we do.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: The science of how X-rays are made and history behind how radiology started to where it is today and the progress it continues to make.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: Passing my boards!
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: In the next 5 years, I would like to continue learning more. I want to be as versatile and helpful to the department and to patients as I can! •
FUN FACTS
FAVORITE HOBBY: Reading
FAVORITE SHOW: “That ‘70s Show”
FAVORITE FOOD: Chicken Parmesan
FAVORITE VACATION SPOT: Myrtle Beach
1 THING ON YOUR BUCKET LIST: Visit another country
SOMETHING YOUR CO-WORKERS
DON’T KNOW ABOUT YOU: I have a twin brother.
Rad idea
CEM OFFERS FAST MRI

BY JAIMEE HERCHLER & JILL GULLETT
University Hospitals of Cleveland is proud to be one of the only hospitals in North East Ohio to offer patients Contrast Enhanced Mammography (CEM).
Contrast Enhanced Mammography (CEM) is a supplemental imaging exam that combines radiation and contrast dye, similar to that used in a CT scan, to capture images of the breast. This new technology is used to improve the detection of breast cancers. This has been shown to be beneficial for those with a newly diagnosed breast cancer, those with dense breast tissue, and patients who are unable to have a breast MRI.
HOW IT WORKS
An intravenous (IV) line is placed in the arm and the contrast is given through the IV line. After the contrast has been administered, the procedure is similar to a regular mammogram. Two pictures of each breast are obtained, although more pictures may sometimes be needed. The process takes approximately 10 minutes from start to finish.
Following the exam, a radiologist will interpret the images and determine whether additional imaging tests are necessary or if a breast biopsy should be performed. The radiologist can help answer any questions a patient may have.
The contrast dye is naturally absorbed and excreted by the body.
BENEFITS AND RISKS
There are several benefits of CEM. It is safe and faster than a breast MRI. It is effective at detecting cancers, particularly highlighting cancers that may be masked on a regular mammogram or breast ultrasound. It is especially useful for individuals with extremely dense
breast tissue, where cancers can be hidden
With benefits come risks. CEM utilizes radiation for imaging which is slightly more than a standard four-picture mammogram but still within safe limits. Patients with kidney disease may not be able to have the test. While allergic reactions to the dye are rare, the most common reactions are mild, such as hives. CEM is not recommended for individuals with known allergies to contrast dye, those who are pregnant or breastfeeding, or individuals with kidney problems.
PREPARING A FACILITY FOR CEM
CEM requires additional software and hardware (addition of a copper filter) upgrade to the mammogram machine as well as a power injector for the contrast injection. A crash cart and contrast reaction kit should also be easily accessible by all staff.
Staffing requirements included pre- and post- procedural education to include IV placement, standardizing response to contrast reactions, familiarizing technologists with machine settings and use of the power injector. A radiologist or other licensed physician must also be present in the facility to evaluate and treat any contrast associated reaction.
Establishing protocols and a workflow along with proper education and training is essential to a successful program.
With an engaged leadership team and appropriate planning, the implementation of CEM has been worth the effort for University Hospital and one that patients and providers have appreciated. •
Jaimee Herchler is a Radiology Supervisor at University Hospitals St. John Medical Center. Jill Gullet t is a Breast Center Supervisor at University Hospitals Cleveland Medical Center.
Share your RAD IDEA via an email to editor@mdpublishing.com.



Kenneth Saltrick, President of Engineering Services in Twinsburg, Ohio, knows from his long experience that C-arm machines themselves are absolute workhorses.
For customers looking to blend the gap between expensive OEM and unreliable used assemblies, WE have your solution.
Our complete repair contains a new cable assembly, utilizing all OEM cable and components with a harvested plate and connector housing as they are proprietary items. These completely repaired products will have a significant cost savings with build quality above new OEM products and carry a warranty of 180 days, which is untouchable in the market.

Clock Off THE ANTHONY ANDERSON, RT(R)
BY MATT SKOUFALOS
After more than two decades in the medical imaging field as a radiologic technologist, and nearly 30 in active and reserve duty with the U.S. Army, Anthony Anderson has spent the past 12 years of his life working in sales for CMS Imaging of North Charleston, South Carolina, as its medical account manager presenting Fuji and Shimadzu equipment in Tennessee.
The retired drill sergeant began life in a small town in southern Georgia, earning a football scholarship that led him to college in California, and then to the University of Washington, where he “got to play a little bit” under College Football Hall of Fame Coach Don James. Upon graduating with a degree in physical education, Anderson then returned to school to become a radiologic technologist.
By 1990, he had joined the OR staff at Swedish Medical Center in downtown Seattle, where he worked alongside members of Orthopedic Physician Associates, a practice that cared for athletes from many of the city’s professional
sports franchises, including the Seahawks, Mariners, and Supersonics. One of them, Dr. Richard Zorn, was impressed by Anderson’s unflappable demeanor in the operating room, and asked whether he’d be interested in joining the group.
“You’ve got to know somebody, be in the right place at the right time, and work with the team doctors,” Anderson said. “Once they saw how I was and how I carried myself, that’s how I got my initial start in. We’re not intimidated by stars, and they want that professionalism. Once guys have proven they’re professionals, they like it.”
From that moment on, Anderson went to work as a team RT for the Seattle Seahawks. On Sundays, he was on the sidelines of every one of their home games, ready to help acquire the images that would allow team physicians to determine whether an injured player was too seriously hurt to return to the game.
“It’s totally different, and that’s why everybody that works in a hospital environment can’t work in a sports medicine environment,” Anderson said. “The patients aren’t going to be walking and talking through, and we have to be as fast as we can because the game is still going on. These guys have pads and pants on; with any type of head injury,
you have to shoot through the helmets.
“We’re not being critiqued by a doctor or radiologist,” he said. “The ortho guy has to make that determination on the spot, broken or not broken, ready to go back in. Usually any player is going to have a trainer and a doctor come with them, and they’re going to evaluate them.”
Just like the players on the field, working on an NFL sideline is fast-paced, high-stakes, and demands immediate results. Although they’re employed by the home team, medical professionals on NFL sidelines are responsible for treating players from the visiting side as well, and Anderson said he’s never worked a game without taking X-rays of multiple people during its duration.
Throughout the length of a season, injuries mount, and team physicians are tracking the health of every player as it’s tested by repeated stressors in practice, training and the game. Periodic imaging allows those same physicians to determine whether those players’ injuries are on the mend or continuing to mount. Anderson has stories of being on hand while physicians managed player injuries with contrast imaging and pain medication.
“We can do everything from minor
finger injuries all the way up to lumbar spines if we have to,” Anderson said, adding “it’s pretty rare if we do that.”
“We don’t do trauma,” he said. “If they get put on the backboard, anything major or cervical, they have to go to the hospital. If they can walk or ride on the cart, we will do that: extremities, shoulders, hands, wrists, ankles, shoulders, feet.”
X-ray is the most commonly utilized modality during an NFL game; many teams keep computed tomography (CT) scanners at their practice facilities, and only those franchises that locate their stadia nearby have access to them within enough time to image a player during the course of a game. MRI would take too long to acquire an image within the duration of a game.
Anderson was part of the Seahawks from the late 1990s until about 2011, when he moved to South Carolina with the Steadman Clinic. Around that time, Dr. Spero Karas became the head team physician for the Atlanta Falcons, and invited Anderson to come with him. The Seahawks had been flying Anderson out from South Carolina to Seattle for every home game – as the Army had been to retain him as a drill sergeant – and the commute was significant.
By the time he made Atlanta, Anderson had been with the Seahawks for two Super Bowl appearances, but he didn’t get to work the contest himself until he landed with the Falcons when the team hosted Super Bowl 53 between the L.A. Rams and New England Patriots. In Georgia, Anderson has also worked the SEC Championship Game, Chick-fil-A Bowl, Heritage Bowl, Peach Bowl, and any other event that needs X-ray support. He still laments the near-miss of working the 2020 NCAA Final Four at Mercedes Benz Stadium, which was unfortunately cancelled by the novel coronavirus (COVID-19) pandemic.
These days, working with the Falcons is almost a moonlighting gig for Anderson, who can foresee the end of his time on the sidelines. Since there are two RTs at every contest, he will handle about five Falcons games himself, and hand off the others to his
colleagues Mark Seavey and Rodney Smith of Children’s Hospital of Atlanta.
“I’ve been in it so long, I’ve seen every team,” he said. “They’re more excited about it.”
That having been said, Anderson definitely has his share of treasured memories from his experiences in the league. Working with the Seahawks during the Marshawn Lynch era is among them; meeting stars like John Randle and Jerry Rice is another.
“I’ve seen Beast Mode” – Lynch’s nickname – “full up and in person from the beginning to the end,” Anderson said. “I was there when Terrell Owens did the Sharpie celebration in the end zone.”
Anderson is also aware that the por-

tability of his imaging career has allowed him to enjoy moments like those he’s seen first-hand from angles that fans and spectators could only catch on video.
“Every time I would stand on the sideline, I’d think about people spending four or five hundred dollars to sit above me, and I’m on the sideline,” he said. “We get paid, but we don’t care, we got the best seats in the house.”
“You think about all the RTs in the country, and there’s less than 100 that get to do this,” Anderson said. “That’s a really small funnel. I’ve gotten to do things that people would think and dream about.” •


ICE A COOL SERIES FOR HOT TOPICS
ICE Webinars: The Series Everyone is Talking About!
ICE Magazine connects with industry leaders to provide top-quality educational opportunities through its monthly webinar series. Reach key decision makers and imaging leaders with your company's message, while collecting important data for sales.




“I love that ICE webinars help me gain my CEUs, it also helps that they have some of the best presenters/lecturers!”
I love that ICE webinars help me gain my CEUs, it also helps that they have some of the best presenters/lecturers!
- J. Sturm, Nuclear Medicine Technologist, Novant Health Brunswick Medical Center.
- J.Sturm, Nuclear Medicine Technologist, Novant Health Brunswick Medical Center.


“The content is always relevant and timely, very professional presentations.”
The content is always relevant and timely, very professional presentations.
– N. Godby, Director of Radiology, Cabell Huntington Hospital Inc.
– N. Godby, Director of Radiology, Cabell Huntington Hospital Inc.
“Learn about best practices and newer technology.”
Learn about best practices and newer technology.
– K. Stich, Radiology Director,East Market, University Hospitals.
– K.Stich, Radiology Director,East Market, University Hospitals.
ICE debut
PartsSource Vice President and General Manager of Imaging Francis Vonder Haar recently shared more information about the company and what it offers imaging professionals.
PartsSource is the leading technology and enterprise software platform for managing mission-critical health care equipment. With the mission of ensuring health care is always on, PartsSource empowers owners and operators of mission-critical equipment to maximize clinical availability and patient throughput, while achieving sustainable savings and efficiencies.
“We connect more than 5,000 hospitals and 15,000 clinical sites with more than 10,000 suppliers, enabling access to parts, services and training,” Haar said.
“What I am most excited about is the work we are advancing to elevate the service experience for imaging professionals,” Haar added. “We have conducted extensive market research and are investing in building a new customer service approach that centers around something new to the company – inventory with over 60,000 imaging SKUs available for instant quoting and same-day shipping. We are committed to being the preferred choice of every imaging professional and this new approach is delivering the reliability and responsiveness our imaging customers require.
Q: HOW DOES YOUR COMPANY STAND OUT IN THE IMAGING SPACE?
HAAR: PartsSource has joined forces with RSTI (Radiological Service Training Institute) to improve equipment uptime and cost savings for imaging customers through comprehensive solutions across parts, services and training. We are working together to expand the selection of training courses available and investing in the latest technology for students to gain hands-on experience. The PartsSource enterprise software platform (PartsSource PRO) is the first and only platform designed specifically to manage the workflows of HTM (healthcare technology management) professionals. 1,600 leading hospitals across the country have implemented this technology to solve a shared set of challenges, maximize asset uptime, reduce costs, and increase procurement efficiency related to equipment maintenance. We currently offer exclusive training discounts to all members of the PartsSource PRO community.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY? DO YOU HAVE ANY GOALS YOU WOULD LIKE TO ACHIEVE IN THE NEAR FUTURE?
HAAR: We are partnering with RSTI and CBET (College of Biomedical Equipment Technology) to address the growing gap between the supply and demand for skilled technical resources. Together we are designing PRO Talent, a comprehen-
sive solution to power the development of HTM teams, including four digital-first modules which will be integrated into the PartsSource PRO platform, including Evaluation, Onboarding, Training and Recruitment. Additionally, I am excited to announce that after a year-long process, RSTI is now an approved SkillBridge program to connect returning Service Members to career job training in diagnostic imaging service. We are well on our way to graduating 25 veterans through this program in 2025.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE ICE MAGAZINE READERS TO KNOW?
HAAR: PartsSource is continuously innovating and designing a diverse array of imaging solutions to help ensure health care is always on. Through advanced sourcing, after-hours support, unmatched data-driven inventory insights, and best-in-market training with RSTI, we are offering comprehensive capabilities and support to give imaging professionals a pathway to success. It is truly an exciting time at PartsSource, and we invite the ICE readers to contact us and learn more.
To learn more about PartsSource imaging parts, visit www.partssource. com/shop/medical-imaging-and-glassware or call 877-497-6412
To learn more about RSTI training, visit www.partssource.com/ shop/services-and-repairs-professional-services-training-education •
Imaging News
A LOOK AT WHAT’S CHANGING IN THE IMAGING INDUSTRY
LG LAUNCHES 5MP DIAGNOSTIC MONITOR FOR BREAST IMAGING
LG Electronics (LG) is accelerating its B2B medical device business, expanding its lineup of diagnostic monitors with the new 21HQ613D-B, which was recently cleared by the U.S. Food and Drug Administration for sale in the U.S.
Intended for digital mammography and digital breast tomosynthesis, the 21HQ613D-B is a 21.3-inch 5-megapixel (MP) IPS diagnostic monitor designed to deliver high-definition radiological images and maintains consistent image quality through its internal front calibration sensor and calibration software.
The 21HQ613D-B offers exceptional definition and brightness. Its LG IPS display provides a resolution of 2,048 x 2,560, a luminance of 1100cd/m² and a contrast ratio of 1800:1. Suitable for reviewing various types of medical images, including breast MRIs, CT scans and ultrasound, the diagnostic monitor features an internal front sensor that removes the need for an external calibration device. With LG Calibration Studio medical software, users can conveniently conduct DICOM calibration and quality assurance tests that comply with international quality control standards for medical monitors.
The 21HQ613D-B also incorporates helpful features to assist users in the close examination of medical images, such as Focus View Mode. Controllable with either a mouse or keyboard, Focus View Mode lets users focus in on a specific part of an image, dimming the rest of the screen in order to highlight the selected area. Additionally, Multi-Resolution Mode (5, 3 and 2MP) makes it possible to quickly adjust screen resolution to suit the type of image being viewed.

APERTO LUCENT 0.4T OPEN MRI SYSTEM UNVEILED
FUJIFILM Healthcare Americas Corporation has announced the U.S. launch of APERTO Lucent, a powerful open 0.4T MRI system. Relying on renowned Fujifilm permanent magnet technology, the new MRI system boasts a unique single-pillar design. The wide, laterally moving table complements the system’s open architecture to offer a comfortable patient experience.
Beyond its patient comfort advantages, the new MRI system addresses today’s capability and quality needs. RADAR motion compensating pulse sequence technology enables reduced need for rescans and minimizing artifact impact on workflow. RADAR sequences can be applied, from head to extremities, including shoulder and cervical spine, where patient motion can particularly challenge the MRI exam.
CHESS type RF Fat saturation complements STIR and Dixon type FatSep sequences, offering a comprehensive fat suppression capability. APERTO Lucent features eight channels of active patient shimming, designed to provide the highest possible field uniformity in support of fat suppression and enhanced image quality.
Spatial resolution and high signal-to-noise ratio (SNR) are promoted by sensitive solenoid technology RF receiver coils and IP-Recon, Fujifilm’s iterative reconstruction algorithm. IPRecon mitigates image noise using a wavelet transform approach, which helps to provide high quality images under demanding resolution requirements.
“APERTO Lucent is a perfect solution for providers looking for a space-saving, cost-effective system that enhances the MRI patient experience,” said Shawn Etheridge, executive director, modality solutions marketing, FUJIFILM Healthcare Americas Corporation. “With permanent magnet open MRI technology, there is little need for additional equipment and infrastructure to maintain the magnetic field, keeping installation and operating costs low for our customers and providing a stronger return on investment.”



MEDICAL CENTER ADDS SOFTVUE BREAST ULTRASOUND TOMOGRAPHY SYSTEM
Delphinus Medical Technologies, a medical imaging company that developed the SoftVue Breast Ultrasound Tomography (UST), has announced the latest installation of its breast imaging technology at McLeod Regional Medical Center in Florence, South Carolina.
“SoftVue UST is the only imaging modality designed specifically to find more cancer in women with dense breasts and is also the only ultrasound-based breast imaging system that is FDA-approved for same-day screening as mammography. Delphinus designed the system as an adjunct to mammography for women with dense breasts to address the fact that breast cancer screening with mammography alone reduces mortality by 41% in women with non-dense breasts but reduces mortality by only 13% in women with dense breasts,” according to a news release.
“Mammogram screening has been plagued for decades by the challenges of breast tissue density,” said W. Shawn Conwell, MD, FACR, medical director, breast and women’s imaging, McLeod Regional Medical Center. “The denser the breast tissue, the harder it is to detect a mass. It’s like looking for a polar bear in a snowstorm.”
When combined with mammography, SoftVue increases sensitivity by 20 percent and specificity by eight percent, offering comprehensive characterization at the point of screening which helps increase cancer detection and reduce short-term follow-ups.
NIH: RISKS, BENEFITS OF INTEGRATING AI INTO DECISION-MAKING
GPT-4V, an AI model, often made mistakes when describing the medical image and explaining its reasoning behind the diagnosis – even in cases where it made the correct final choice.
Researchers at the National Institutes of Health (NIH) found that an artificial intelligence (AI) model solved medical quiz questions – designed to test health professionals’ ability to diagnose patients based on clinical images and a brief text summary – with high accuracy. However, physician-graders found the AI model made mistakes when describing images and explaining how its decision-making led to the correct answer. The findings, which shed light on AI’s potential in the clinical setting, were published in npj Digital Medicine. The study was led by researchers from NIH’s National Library of Medicine (NLM) and Weill Cornell Medicine, New York City.
“Integration of AI into health care holds great promise as a tool to help medical professionals diagnose patients faster, allowing them to start treatment sooner,” said NLM Acting Director Stephen Sherry, Ph.D. “However, as this study shows, AI is not advanced enough yet to replace human experience, which is crucial for accurate diagnosis.”
The AI model and human physicians answered questions from the New England Journal of Medicine (NEJM)’s Image Challenge. The challenge is an online quiz that provides real clinical images and a short text description that includes details about the patient’s symptoms and presentation, then asks users to choose the correct diagnosis from multiple-choice answers.
The researchers tasked the AI model to answer 207 image challenge questions and provide a written rationale to justify each answer. The prompt specified that the rationale should include a description of the image, a summary of relevant medical knowledge, and provide step-by-step reasoning for how the model chose the answer.
Nine physicians from various institutions were recruited, each with a different medical specialty, and answered their assigned questions first in a “closed-book” setting, (without referring to any external materials such as online resources) and then in an “open-book” setting (using external resources). The researchers then provided the physicians with the correct answer, along with the AI model’s answer and corresponding rationale. Finally, the physicians were asked to score the AI model’s ability to describe the image, summarize relevant medical knowledge, and provide its step-by-step reasoning.
The researchers found that the AI model and physicians scored highly in selecting the correct diagnosis. Interestingly, the AI model selected the correct diagnosis more often than physicians in closed-book settings, while physicians with open-book tools performed better than the AI model, especially when answering the questions ranked most difficult.
Importantly, based on physician evaluations, the AI model often made mistakes when describing the medical image and explaining its reasoning behind the diagnosis — even in cases where it made the correct final choice. In one example, the AI model was provided with a photo of a patient’s arm with two lesions. A physician would easily recognize that both lesions were caused by the same condition. However, because the lesions were presented at different angles — causing the illusion of different colors and shapes — the AI model failed to recognize that both lesions could be related to the same diagnosis.
The researchers argue that these findings underpin the importance of evaluating multi-modal AI technology further before introducing it into the clinical setting.

RTI REPORTS 40% GROWTH IN PRODUCT SALES FOR THE FIRST HALF OF 2024
RTI, a leading manufacturer of quality assurance (QA) solutions for diagnostic radiology, has reported a 40% increase in product sales for the first six months of 2024 compared to the same period in 2023.
This significant growth coincides with the launch of Mako, RTI’s new premium solution for X-ray quality assurance. Mako is the most efficient and accurate meter available, offering the broadest application range in the market. It is a pioneering solution that revolutionizes workflow management while providing unparalleled plug-and-play simplicity.
Fredric Eliasson, vice president of sales, states: “We are experiencing significant sales growth across most regions. Our hardware solutions meet and surpass the high standards of an increasingly demanding industry. They are highly accurate and resilient, seamlessly integrating with Ocean Next, our comprehensive software solution for tablets, PCs and the Cloud. The sales team and our partners have done a great job in bringing this message to the market.”
RTI’s Cloud solution, myRTI, features automatic backup of your entire Ocean Next database, synchronization across multiple devices, and more. The new Mako solution, released in December 2023, is now available in all markets worldwide.


RSNA MAKES STRIDES IN NARROWING RADIOLOGY GENDER GAP
The radiology gender gap is decreasing, but there remains work to be done, according to an editorial published in RadioGraphics, a journal of the Radiological Society of North America (RSNA).
In 2022, nearly half of residents and fellows in Accreditation Council for Graduate Medical Education (ACGME)-accredited programs were female. However, less than 27% of active diagnostic radiologists and only 10% of active interventional radiologists are female. Within the 48 largest medical specialty groups, diagnostic radiology ranks 41st and interventional radiology ranks 47th in percentage of female trainees.
To foster a diverse workforce in radiology and to ensure leadership diversity, RSNA established the Committee on Diversity, Equity and Inclusion (CDEI) in 2018. The RSNA CDEI has been instrumental in raising awareness, attracting a broader talent pool and establishing a supportive environment for professional advancement within radiology. The CDEI and RSNA have implemented programs – including dedicated research grants and mentorship initiatives – to provide direct support to underrepresented groups.
“RSNA has made significant strides in the last few years to address the gender and diversity gap in our specialty and within the Society,” said senior author Maureen P. Kohi, M.D., Ernest H. Wood Distinguished Professor and Chair in the Department of Radiology at the University of North Carolina at Chapel Hill. “This manuscript serves as a benchmark to show short-term progress.”
RSNA’s efforts have brought about important changes in gender diversity among the society’s faculty and leadership. In 2023, data reveal a positive trend in RSNA annual meeting faculty gender diversity, with 55% male and 43% female speakers, compared with 67% male and 29% female speak-
ers in 2014. In 2023, the composition of RSNA committee chairs was 58% male and 42% female, compared with 72% male and 28% female in 2014. The composition of the RSNA Research & Education Foundation Board of Trustees was 58% male and 42% female in 2023, compared with 83% male and 17% female in 2014. The composition of the RSNA Board of Directors has varied over the past decade and is currently at 70% male and 30% female.
Although recent advances are promising, the authors emphasize that more work needs to be done. While pathway programs and mentorship/sponsorship are pivotal for DEI advancement, they do not address structural biases in medicine – including discrimination and microaggressions – that contribute to underrepresentation of women and underrepresented in medicine (URiM) groups in radiology and in leadership roles. Unconscious bias affects assessments of peers, trainees and medical students, and can have a significant impact on factors ranging from admissions to leadership appointments.
The authors state that awareness and the use of rational decision-making processes will help reduce the influence of bias, creating a more equitable community. They stress that future initiatives should prioritize inclusivity, collect expanded diversity data, and engage the entire radiology community to create a truly inclusive work environment for all.
“I hope that our collective efforts can create a diverse field matching our patient population,” Kohi said. “I feel RSNA’s DEI initiatives will make this dream a reality, and I am proud of the RSNA Board for supporting such efforts. I hope that we can continue to build leadership and mentorship opportunities for our URiM trainees and junior faculty and develop the next generation of diverse leaders.”
HYPERFINE ANNOUNCES
FDA CLEARANCE OF SOFTWARE
UPDATE
Hyperfine, a medical device company that has redefined brain imaging with the world’s first FDA-cleared portable magnetic resonance brain imaging system – the Swoop system – has announced the clearance of the ninth generation of AI-powered Swoop system software. This advanced software significantly reduces scan times across multiple MR sequences without sacrificing image quality. The U.S. Food and Drug Administration (FDA) clearance of this software further solidifies Hyperfine as a leader in AI-powered health technology.
These scan time reductions may enable Swoop system images to help speed up the diagnostic process in acute care settings, which is crucial for time-sensitive medical conditions such as stroke, where every second counts. Reducing the overall acquisition time for sequences can also decrease the negative impact of patient motion on image quality.

Professor Adnan Siddiqui, MD, Ph.D., from the University of Buffalo, emphasized the impact of rapid imaging capabilities, saying, “Timely MR brain imaging is essential for clinicians making critical treatment decisions, particularly in acute neurological episodes like strokes. We have been an active site in the ACTION PMR study assessing the use of the Swoop system in stroke diagnosis, and this latest software will help the Swoop system more seamlessly integrate into stroke workflows. It is wonderful to see Hyperfine respond quickly to clinical feedback and continue to innovate to improve the Swoop system.”
GE HEALTHCARE TO ACQUIRE CLINICAL AI BUSINESS FROM INTELLIGENT ULTRASOUND
GE HealthCare has announced that it has entered into an agreement to acquire Intelligent Ultrasound Group PLC’s (Intelligent Ultrasound) clinical artificial intelligence (AI) software business for total consideration of approximately $51 million. Intelligent Ultrasound is a leader in integrated AI-driven image analysis tools designed to make ultrasound smarter and more efficient. GE HealthCare plans to incorporate these solutions across the ultrasound portfolio, strengthening its capabilities with technology that helps improve workflows and enhance ease-of-use for the benefit of clinicians and patients.
“We are pleased to bring innovative technology from Intelligent Ultrasound into GE HealthCare’s Ultrasound portfolio, allowing us to fully integrate these solutions into our systems to help clinicians improve workflow, reduce repetitive tasks, and simplify exams,” said Phil Rackliffe, president and CEO of Ultrasound and Image Guided Therapies, GE HealthCare. “This technology and the experts who developed it will help enhance our portfolio of AI-enabled devices and accelerate our pace of development of next-generation AI tools.”
Intelligent Ultrasound has pioneered the ScanNav Assist AI technology, which powers SonoLystlive and SonoLyst
X/IR, available on GE HealthCare’s Voluson Expert and Voluson Signature ultrasound devices. SonoLyst is also currently available on the Voluson SWIFT. By acquiring this business, GE HealthCare also adds an AI innovation pipeline that serves to help advance future development and realize long-term efficiencies.
GE HealthCare plans to welcome the team of research and development experts from Intelligent Ultrasound, who will help drive AI-enabled image recognition and innovation for GE HealthCare Women’s Health ultrasound devices as well as across the broader portfolio. This agreement follows GE HealthCare’s acquisition of Caption Health in 2023, which added new capabilities in AI-enabled image guidance and AI development expertise to aid in early disease detection in other areas.
“I really believe that we are at the start of a wave of AI making a profound difference to medical imaging, and especially ultrasound,” said Nick Sleep, chief operating officer, Intelligent Ultrasound, who will join GE HealthCare. “Becoming part of the GE HealthCare family will help speed the adoption of this technology and make ultrasound even easier for customers to use.” •

PRODUCTS Market Report
Medical Imaging Market Continues to Climb
STAFF REPORT
Training for medical imaging technologists and repair technicians should grow in coming years to mirror the expected growth of the global medical imaging market. Grand View Research is one research firm that excepts the global medical imaging market to continue its recent growth in the coming years.
“The global medical imaging market size was estimated at $39.8 billion in 2023 and is projected to grow at a CAGR of 4.9% from 2024 to 2030. The increasing prevalence of chronic diseases, demand for early disease diagnosis and detection tools, along with growing geriatric population are anticipated to drive this growth. Factors such as the rising investments by key players, product innovations, and technological advancements such as integration of artificial intelligence (AI) in medical imaging and development of point-ofcare medical imaging equipment are expected to further fuel the growth,” according to Grand View Research.
New technology is one area that Grand View Research predicts will fuel growth of the global medical imaging market. New technology also means additional training for imaging professionals.
“Technological advancement is driving the medical imaging market growth, particularly through the development and adoption of portable, wearable, and point-of-care (POC) medical imaging devices,” Grand View Research states.
“These innovations have expanded the capabilities of medical imaging and made it more accessible and convenient. By integrating cutting-edge technologies, the medical imaging sector is now able to offer solutions that can be used outside of traditional hospital settings, enabling continuous monitoring and immediate diagnostics in various environments. This shift towards more mobile and user-friendly devices has the potential to revolutionize patient care, making it easier to diagnose and monitor conditions in real time, thus significantly improving the efficiency and effectiveness
of health care services.”
“For instance, in February 2024, Visage Imaging, a diagnostic imaging and multimedia enterprise, introduced its new product, Visage Ease VP. This innovative imaging platform is designed for use with Apple’s augmented reality headset, the Apple Vision Pro. The company provides cloud-based, AI-driven enterprise imaging solutions such as Visage 7, Visage Ease, and Visage Ease Pro,” Grand View Research continues. “These platforms enable users to review diagnostic images and work together with peers. Visage Imaging states that its technology enhances the efficiency and accuracy of radiologists’ analyses and their overall workflow.”
Global Market Insights is another research firm that predicts market growth.
“Medical imaging market size was worth $40 billion in 2022 and is poised to grow at 5.5% CAGR from 2023 to 2032, driven by the incremental innovations and advancements in medical imaging technology,” Global Market Insights reports.
Mordor Intelligence also predicts market growth.
“The diagnostic imaging market size is estimated at $46.96 billion in 2024, and is expected to reach $57.63 billion by 2029, growing at a CAGR of 4.18% during the forecast period (2024-2029),” Mordor Intelligence reports.
“The main things that are driving the growth of the diagnostic imaging market are the increase in chronic diseases, the rise in the number of older people, and the use of more advanced imaging technologies,” Mordor Intelligence adds.
The firm Market Research Future also predicts growth.
“The diagnostic imaging market is expected to reach $49.66 billion by 2032 at a CAGR 4.7% during the forecast period 2023-2032. Diagnostic imaging is used to detect medical complications and help in illness or condition therapy. The drivers driving market expansion include an aging population, an increase in chronic illnesses, and technological advancements. Furthermore, increased R&D investment and aggressive methods used by leading companies, such as new product releases, are driving market expansion,” according to Market Research Future. •
Product Focus
Training
SIEMENS HEALTHINEERS
FlexForce Tech Program
The FlexForce Tech program from Siemens Healthineers connects health care institutions with temporary or permanent, fully vetted radiologic technologists trained by Siemens Healthineers and supported throughout their clinical engagements. Flexible engagements range from four consecutive weeks for the FlexForce Start-Up Tech to three or more months for standard FlexForce Tech assignments. In addition to providing technologists for onsite scanning, FlexForce Tech connects institutions with technologists to perform WeScan remote magnetic resonance imaging as well as remote 3D image post-processing. These remote assistance services expand clinical imaging capabilities and capacities. Together, these solutions can help institutions bridge workforce gaps, contributing toward a sustainable, future-ready workforce and enabling exceptional patient care.

*Disclaimer: Products are listed in no particular order.
RSTI Training
Meet the instructors behind the brand, RSTI’s team representing over 187+ combined imaging experience for a 23+ year average tenure. Radiological Service Training Institute – training the industry since 1985!
MAULL BIOMEDICAL Training 2



Maull Biomedical Training is an independent training company that specializes in contrast injector training. Founded in 2008, Maull Biomedical teaches the proper operation, maintenance and troubleshooting for a dozen different contrast injector models. With their MIST (Maull Injector Service Tool) software, they are capable of delivering the industry’s best injector training program to you in a live classroom setting as well as providing remote injector training right to your laptop with online quizzes and software. For more information, visit www.maullbiomedical.com or contact Steve Maull at steve@maullbiomedical.com.
*Disclaimer: Products are listed in no particular order.
DIRECTMED Training
DirectMed offers training on the latest technology in Siemens imaging equipment, from basic to expert engineer level. The course phases allow engineers to learn at a pace that is efficient for and effective for them. All courses are AAMI Certified and provide continuing education units. The AAMI certified instructors bring a wealth of knowledge and field experience to guide engineers to excellence. For more information, visit https://directmedparts.com/training/
GE HEALTHCARE Global Training Centers
At GE HealthCare, technical service training embraces a modern, skills-based learning strategy which resonates with our newer workforce, helps to increase the effectiveness of training, occurs in the flow of work (immediately deployable), and is consistently transportable across modalities. The GE HealthCare Institute in Wisconsin, one of four GE HealthCare global training centers, leverages this approach to deliver technical training to more than 8,500 students annually. Onsite courses and staged clinical settings offer real-world clinical environments – including emergency and surgical room settings – to provide students with hands-on opportunities to learn on more than $125 million of imaging, ultrasound and patient care equipment. They also leverage more than 700 virtual experiences –more than 150 virtual machines, 400 virtual hands-on labs and 150 augmented reality experiences to practice these skills. Students include GE HealthCare field engineers, biomedical engineers, in-house engineers and customers from more than 50 countries. Additionally, the leadership training programs provide further opportunities for professional development.


TRI-IMAGING Training Program
The training program at Tri-Imaging transcends traditional education by instilling skills that will resonate throughout one’s professional journey for years to come. Unlike conventional training experiences focused solely on facts and figures, Tri-Imaging prioritizes imparting practical, applicable skills. Tri-Imaging’s commitment extends to fostering a deep understanding of the intricate inner workings of various devices and machines that students will service in their careers. Tri-Imaging believes in nurturing individual growth, and to that end, it provides one-on-one assistance for each student.
• The fastest growing HTM talent network in the country.
MAGAZINE NEWS MAGAZINE NEWS
• 350+ open opportunities throughout the United States.

» A variety of posting options ranging from single-job postings to 12-month unlimited memberships.
“My HR department advertised on various government sites and our web site but we did not get a single applicant in over 120 days. Fairbanks Alaska is hard to recruit for but I took out an ad on HTM Jobs and got two good applicants in less than 30 days. I am hiring them both. Thanks HTM Jobs.”
- D. Anderson,
Featured Employers: Agiliti, Kaiser Permanente, Renovo Solutions, TRIMEDX, Tech Knowledge Associates, Blue Water Thinking, and more!
DIRECTOR’S CIRCLE
In this month’s Director’s Circle, ICE Magazine asked imaging directors and other leaders to share their insights regarding training. Continue reading to find out what to look for when seelking training as well as how training has changed in recent years.
Participants in this month’s Director’s Circle are:
• Beth Allen, Director of Clinical Operation Banner Imaging
• Michelle Dossa, Ph.D., CRA, RT(R), Radiology Director, West Market, University Hospitals
• Bryan Henderson, Ph.D., MBA, RT(R), Radiology Director, Valley Presbyterian Hospital, Los Angeles, California
• Amanda Miller, Imaging Manager, The Ohio State University Wexner Medical Center
• Jacqui Rose, MBA, CRA, RT(R), FAHRA, System Director of Radiology, UC Health
Q: HOW HAS THE TRAINING OF IMAGING PROFESSIONALS CHANGED OVER THE PAST 5 YEARS?
Allen: In the past 5 years, I have seen less enthusiasm to cross train. We have had less interest in cross-training opportunities when we used to have a wait list for a cross-training position.
Dossa: Programs/Clinicals – Imaging programs continue to teach many of the same concepts as I learned 30 years ago. But today, changes in how soon we employ our students has changed. We promote tech extender and GXMO positions more than in the past as a stepping stone into the organization. Cross-training opportunities are more frequent. We do not see as many external candidates applying, so our student and cross training pipelines have grown in strength over the past several years. We actively look for technologists who have the desire to cross train into other modalities and provide them the resources to do this. We worked closely with one of our community colleges to develop a CT didactic course that is covered by our tuition reimbursement program
in order to send our techs for that part of modality training. We ensure all other advanced imaging programs such as MRI are covered by our tuition reimbursement as well. Technologists are doing these advanced imaging programs much earlier in their careers than in the past to help us combat technologist shortages.
Henderson: Technology in imaging changes rapidly and it sometimes feels hard to keep up. As leaders, we should provide our employees with as much help as possible. I send my employees for additional imaging training, educational conferences and even subscribe them to radiology magazines, so that they can stay on top of emerging technological advancements. I also pair up my new hires with my senior employees to work together throughout their orientation. The senior employees show the younger employees oldschool positioning tricks, while the younger employees show the senior employees how to use all the latest computer technology. It’s a win-win for both generations.
Miller: The rapidly growing shortage of technologists has led many facilities to increasingly rely on travel staff to support their departmental needs. This staffing shortfall, coupled with the urgent need to bring in travel support, has significantly impacted the onboarding and training processes. Procedures that typically take three months must now be expedited, leaving many facilities and managers scrambling. This greatly affects the training staff, who feel pressured to cover everything in a day. Consequently, the overall process has been sped up, leading to an increase in online courses and learning for equipment and procedural processing.
Rose: Training has become more difficult and more time consuming recently primarily due to the shortage of quality staff to do this training and the need to stay productive. This causes delays in training and our new teammates are extending
their training to get to a good comfort level. Leadership training has evolved to more online and virtual offerings post-pandemic and shortage of funds to support this. This is tremendously helpful due to that lack of resources but continued desire to help develop our teams. Thinking creatively is critical to get all types of training done.
Q: WHAT SHOULD AN INDIVIDUAL LOOK FOR WHEN CONSIDERING TRAINING OPPORTUNITIES?
Allen: Individuals should understand the role they would be training for. They should also consider their personal goals and what the expectations are surrounding the training.
Dossa: Training opportunities need to be a good fit for both the individual considering them as well as for the organization who invests in the training. For the individual who is considering a training opportunity, do your research. Be sure to understand the requirements, time commitment and long-term benefits. And for the organization, be sure to right match individuals with opportunities. Have stay interviews/discussions with team members to truly understand their career goals in both the short and long term. From there, work together to map out these goals and provide resources to help them achieve these goals.
Henderson: Radiologic technologists should always be looking to increase their technological skills and a great way to do this is by cross training into other imaging modalities. There are numerous e-training programs that can be found online, that will allow radiographers to seek out that additional knowledge.
Miller: I believe a hands-on approach is the most effective since it allows for questions and feedback to be provided by the trainers in real-time. Vendor-provided training is also crucial and essential. Purchasing additional education is always a good decision as it can be used for refresher training and for training incoming staff. This education can include online virtual support and additional training applications to build staff confidence and knowledge. It allows each staff member to approach their training in the way they learn best. Superuser training is another excellent opportunity for staff to become deeply familiar with the equipment and gain the ability to adjust settings and troubleshoot issues. Superusers are valuable resources for training and help expand the overall knowledge and proficiency of the team.
Rose: Flexible schedules, quality content, reasonable expense. Timely availability. All of these things will make all types of training more readily available and utilized.
Q: HOW CAN TRAINING ADVANCE ONE’S CAREER?
Allen: Training can advance one’s career by showing they are open to new things, whether it is learning a new modality, software or management skills. Once trained, that training is yours to keep regardless of what the next step is.
Dossa: We actively look for individuals who have a desire to learn more, take classes and be life-long learners. These individuals demonstrate how training can advance one’s career. Someone with the initiative to cross train and work in other modalities, allows us to promote to multi-modality posi-





tions. Someone with the initiative to learn new skills/take on new tasks in their current modality, provides an opportunity to be promoted through our career ladder. Starting as a tech I, those that take on more in conjunction with years of experience, can be promoted to tech 2 and tech 3 positions. And, of course, we are looking for those who take the initiative to be involved in advanced degree programs as we develop leadership succession plans for our future.
Henderson: For those technologists who want to be better with their job skills or even move up in the organization, they should look to cross train in as many imaging modalities as possible. Not only does this increase their own net worth by getting pay increases, but it makes them more useful for leaders preparing a department schedule, as this highly trained staff member can be scheduled in multiple imaging departments.
Miller: Training and additional education provide a comprehensive understanding of equipment and procedures, boosting confidence in handling challenging situations. This training can also open doors to mentorship and teaching opportunities, as well as lead to educational or leadership advancements.
Rose: The more skills our team has, the more successful they can be and better prepared to move to the next level when the opportunity presents. As leaders, it’s our goal to have highly effective teams and that will naturally be noticed and lead to opportunities in leadership roles.
Q: HOW DOES AN EMPLOYEE’S TRAINING BENEFIT A FACILITY?
Allen: Training benefits a facility by investing in current team members to expand services and promote from within. This can lead to better retention and the savings that comes with that. By offering advancement opportunities, facilities can be more attractive to potential candidates.
Dossa: Quality training results in quality team members who provide excellent care to our patients and families, who are good stewards of our financial resources, and who support our organization’s mission, vision and values. Quality patient experience, teamwork and resource management result in positive organizational outcomes. These positive outcomes ensure that our organization maintains a healthy operating margin that can be reinvested into our facilities, equipment and teams.
Henderson: When an employee invests in their own well-being; it not only benefits them as a person, but also their employer. Additional employee training provides patients with higher quality imaging studies and better services that improves overall patient satisfaction, as there are less repeats
and errors and this greatly benefits the employer as well.
Miller: There are multiple reasons why a facility should invest in and continue employee training. Providing employees with the correct resources and tools allows them to grow and improve while building their confidence. Setting up the employee for success! Ongoing training demonstrates an investment in employees, improving job satisfaction and staff retention. Patient satisfaction will also improve due to the increased efficiency and comfort level of the staff. This makes patients feel comfortable and safe with the care they are receiving. Trained employees also gain the confidence to train others, enhancing the overall efficiency of the department. Efficient processes decrease turnaround times, allowing for more exams to be completed and providing an opportunity to increase revenue.
Rose: Employee training tremendously benefits all organizations and patients by increasing their knowledge and capabilities. Those teammates are more effective, productive, safe and improve all levels of service. This is a significant win for any organization lucky to have them on board.
Q: WHAT ELSE SHOULD ICE MAGAZINE
READERS KNOW ABOUT TRAINING?
Allen: Training is always an opportunity to learn more, which is yours to keep. A good training program requires great “trainees” that are willing to put forth the effort to learn and engaged “trainers” that are invested in progress. Both need to be given the time needed to make the program successful.
Dossa: Be a life-long learner. Change is the only constant and those who have the mindset to continuously learn and improve day to day with training will be successful. Utilize both internal and external partners in developing training opportunities for your teams. There are great resources all around you.
Henderson: There is a plethora of educational resources and training available to radiographers online. Everything from tutorials to cross-training guidelines are available for employees to review, prior to them scheduling or enrolling in educational classes.
Miller: To be the best at getting better by investing in our people and teams.
Rose: New creative models for training our teammates is imperative in our busy world. Vendor partners have stepped into those environments to improve overall training and thus boost competency. By leveraging these partnerships, hospitals and health systems ultimately benefit. •




Azurion)


THE TECH EFFECT
Medical Imaging Advancements Facilitate Higher Standards
of Care



BY MATT SKOUFALOS
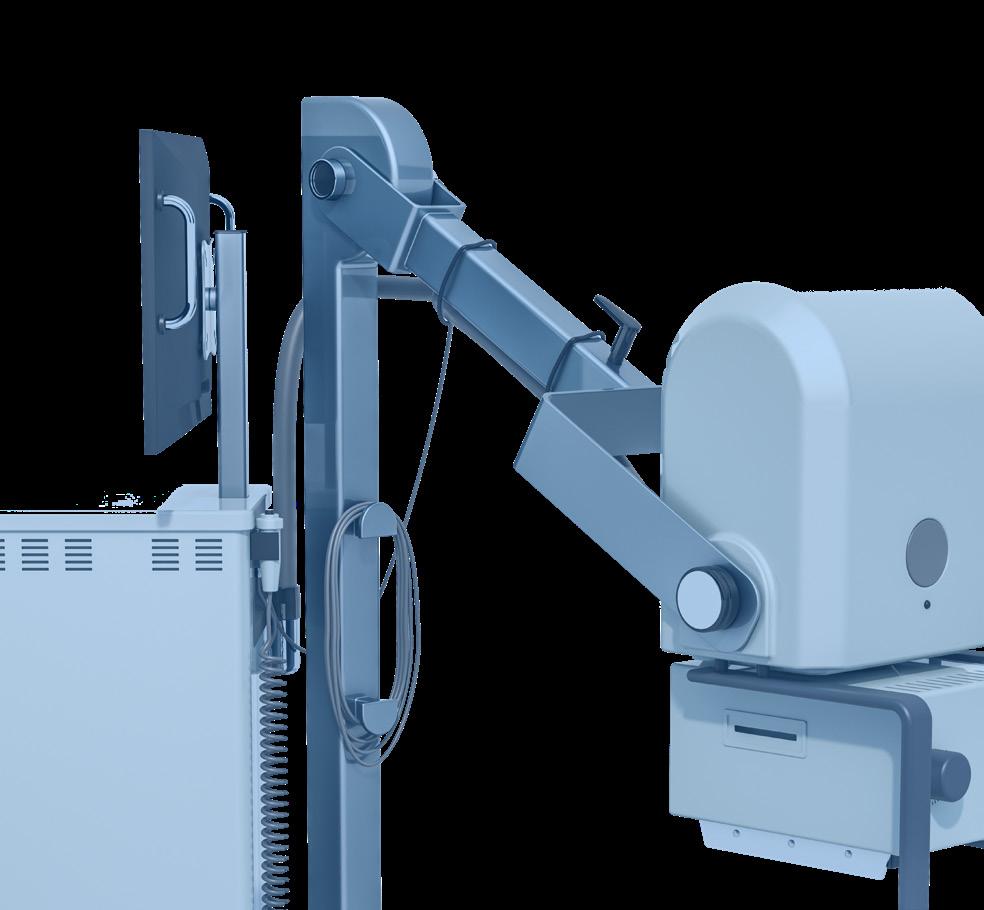
Since the earliest medical applications harnessing the power of X-rays, the diagnostic imaging space has ever expanded with the emergence of new technologies, new applications of existing technologies, and the systems and people that support their interoperability.
POCUS
Although point of care ultrasound (POCUS) has been in use at the patient bedside since the 1980s, technological innovations by Butterfly Network Inc. and others have demonstrated a recent shift away from traditional ultrasound construction methods in favor of a lower-cost, smaller form-factor product. Darius Shahida, chief strategy officer and chief business development officer at Butterfly Network Inc., describes the company’s iQ product, now in its third iteration, as a fundamentally new approach to building ultrasound devices.
“Prior technology was predicated upon piezoelectric crystals, which are prohibitively expensive to manufacture,” Shahida said. “Beyond cost, they’re hand-cut and hard-wired to a specific frequency or imaging application. Our technology, Ultrasound-on-Chip, allows us to image the entire body with a single probe at a really disruptive price point.”
“Any of the large incumbents sell a phased array, a linear, and a curvilinear probe; some are for very shallow vascular applications, others are for deep abdominal applications,” Shahida said. “The beauty of Butterfly is that we can do all of that, achieving a frequency range of 1-12 MHz with one single probe. We’re a digital solution in an analog world.”
In addition to its versatility of function, the Butterfly iQ3 is priced like a high-end, personal electronic device, capable of connecting easily with other handheld peripherals. By creating a product that can be carried like a phone and that interacts with one seamlessly, its design emphasizes both portability and ubiquity for practitioners when they need it. The company expects to further evolve the underlying technology that powers the device “nonlinearly,” Shahida said.
“Our architecture lends itself to other form factors that we are building ourselves – a wearable, patch-based form factor – and other architectures that miniaturize our transducer so that it can fit into and power other form factors,” he said. “We will continue to iterate and improve our performance until we reach a point of equivalency or superiority to cart scanners.”
Butterfly also has worked to make its brand top-of-mind for the same reasons. Medical students at the University of California Irvine and Temple University in Philadelphia, Pennsylvania, were given iQ devices at their white coat ceremonies in 2019 and 2021, respectively, because the deans at those universities believed in the utility of their medical students having POCUS technology integrated into their curriculum as well as their clinicals. Shahida likened the choice to Microsoft giving its Office software suite to college students, the better to prepare them for the white-collar workforce and inspire brand loyalty.
“It was very core to our strategy to align ourselves with the next generation of practicing physicians,” he said. “We want the next generation of practitioners to go out practicing medicine with Butterfly devices in their pockets.”
In addition to the digital-device price point, Butterfly is selling “to every single specialty in virtually every setting globally,” Shahida said; a function of the company investing heavily in its supply chain and an omnichannel e-commerce sales strategy that supports broad dispersal of the iQ+ and iQ3 devices.
“Any licensed health care practitioner can go on our website and purchase a device that we will ship to them in just a few business days,” Shahida said. “In about seven clicks, they can check out and have a device in their hands in a matter of days. That allows us to access the fragmented practitioner market; we also have a very large health systems team that allows us to leverage a direct sales force domestically and in key international markets.”
Butterfly has sold more than 150,000 units, and Shahida said the company has its sights set on even greater gains by working to close the access gap for medical imaging in regions that don’t have it.
“One of the most exciting opportunities that we face is that the following two facts are simultaneously true: twothirds of the world’s population lack access to simple medical imaging, and about 80 percent of diagnostic dilemmas can be addressed using simple medical imaging,” he said. “I do not believe there’s a condition on Earth for which an earlier diagnosis leads to an adverse outcome. The quicker you get that information, the quicker you can make that decision and alter the pathway of care.”
Butterfly also claims to have “the largest cloud-based, de-identified ultrasound image repository on earth,” to their knowledge, with which to train its Artificial Intelligence (AI) software. Last year, the company launched “Butterfly Garden,” its version of the Apple store and “an AI marketplace for imaging applications,” Shahida said. More than 300 companies have applied to use its software development kit to create and deploy AI-powered tools for iQ users, and Butterfly has signed some 15 to 20 partners to date, he said.
Shahida described its platform as enabling users “to access and interact with all sorts of technologies that help with guidance and capturing images.”
“We created a solution that the largest technology creators failed to create, in part because doing so would disrupt their core business,” he said.
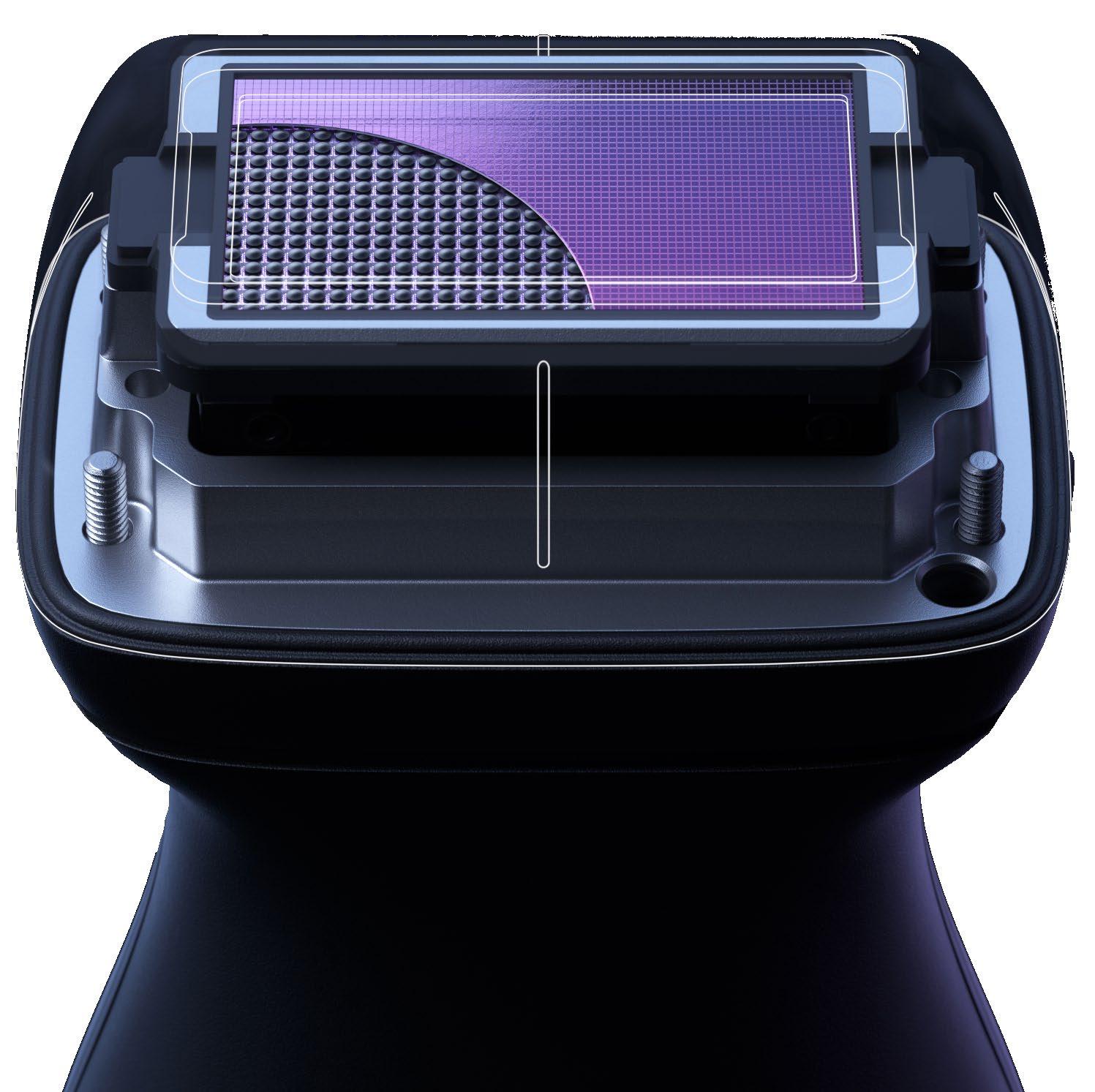
PHOTON-COUNTING CT
Meanwhile, one of the largest players in the medical imaging space, Siemens Healthineers, continues to make inroads in finding additional applications for its photon-counting computed tomography (CT) scanners. Matthew Fuld, Ph.D., director of photon-counting CT at Siemens Healthineers North America, said the technology is having an impact on
COVER STORY
cardiovascular, neurosurgery, oncology and even cerebrospinal fluid (CSF) leak patients.
The last of these, Fuld said, have seen results of such significance in identifying the venous fistulas that cause spontaneous intracranial hypotension (SIH) where other forms of imaging cannot, that patients have begun to approach the manufacturer, asking where they could locate health systems that have deployed its NAEOTOM Alpha CT scanner.
“This is a topic I’ve never experienced personally in my career, where I’ve seen patients seeking out Siemens Healthineers to find out where this technology is available,” Fuld said. “They want it in more locations because it enables them to find out where their disease is located; once you can see where the leak is, you can treat it.”
Photon-counting CT is an idea that’s been around for decades, but has taken years, significant research, and financial investments to develop a functional and effective technology capable of measuring every single photon. The complexity involved in manufacturing the cadmium telluride crystals at the heart of the photon-counting detector is significant and expensive. In nature, creating the crystals takes thousands of years; in controlled laboratory environments, growing one ampule of cadmium telluride crystal is a 90-day process, “and if you mess it up on day 88, you start over,” Fuld said.
To that end, the company has constructed a second, largescale crystal-growing factory in Forchheim, Germany, to complement its first, the better to increase downstream adoption of photon-counting CT.
“We’ve started at the absolute highest end of the technology; now we plan to bring that technology down into our portfolio into facilities that are willing to go down one notch or two,” Fuld said. “Eventually, everywhere in the portfolio is the plan.”
Describing photon-counting CT as “ground-breaking” isn’t just Fuld’s language. In October 2021, when the federal U.S. Food and Drug Administration approved NAEOTOM Alpha scanner for widespread use, the agency itself issued a press release that hailed the device as “the first major new technology for computed tomography imaging in nearly a decade.” It enables the improved spatial and contrast resolution that underpins higher-quality image capture and delivers more effective diagnostic results. Three years later, the manufacturer has seen nearly 450 publications on work enabled by the NAEOTOM Alpha since its launch.
“It’s not just people who want the next new, shiny thing, it’s the topic everyone wants to hear about, and wants to find out more to implement,” Fuld said. “We are expanding and exploring towards what we could do to make it more available to more customers. It’s a technology we see across all our install base in the future, and very positive things – new scanners – in the next short-term.”
NAEOTOM Alpha users have published studies of patient cases demonstrating “dramatic congenital heart patients with tremendous abnormalities” that have become treatable in ways that they weren’t previously because photon-counting CT pro-
vided a pathway for surgical planning.
“Photon-counting CT lets you see all this information at radiation doses that are so low that it would be impractical to attempt that on conventional, energy-integrating CT technology,” Fuld said. “Photon counting is giving people the information to make better diagnostic decisions in many fields. As we have more capability, the cost will come down as we move through.”
THERANOSTICS
For as much as photon-counting CT has made generational advances in CT technology, Siemens Healthineers also foresees increased utilization in theranostics – using one radioactive drug to diagnose disease and a second to deliver targeted therapy –as nuclear medicine and radiation oncology practices begin to customize their own infrastructures from the ground up.
Siemens Healthineers Global Lead of Theranostics Solutions Lady Sawoszczyk said that new technologies can improve workflow and resolve operational issues associated with imaging and radiopharmaceutical manufacturing.
After its 2021 acquisition of Varian Medical Systems, Siemens Healthineers focused on the continued development of the cloud-based Varian ARIA CORE workflow management software, which addresses emerging needs in theranostics. In June 2024, Siemens Healthineers unveiled new theranostics features for the ARIA Systemic Therapy Management (STM) module for ARIA CORE. With drug ordering, pharmacy dispensing, inventory, and administration features, STM is aimed at helping manage cancer patients’ needs and automating tasks to support burnedout staff.
“We see patient volumes going up, and more centers starting to open, but the standard of care for workflow is still being addressed by clinicians and administrative staff,” Sawoszczyk said.
“We found a lot of customers in theranostics are having these challenges, trying to automate a lot of the tasks that cannot be automated. That’s changed quite rapidly, so we’re trying to meet that demand to try to help those institutions.”
ARIA CORE strives to resolve analog, pen-and-paper tasking associated with the regulatory checks related to the process of administering theranostics by automating elements of it. In addition to removing human error from the process, Sawoszczyk hopes that a software-based solution can also close shortfalls in staffing that can also hamper operations.
“As an imaging company providing these scanners to make them more workflow-efficient, we’re also looking at software,” Sawoszczyk said. “I’ve been on that side when I worked in the clinical environment, and we were doing eight infusions a day. If I could find a way to automate what we were doing, I could maybe provide two times more infusion appointment for patients, and maybe do 16 patients a day.”
Another difficulty in the field involves growing the myriad applications for theranostics interventions when the clinical trial process is so arduous and time-consuming. Sawoszczyk spoke about efforts to spur collaboration among researchers, profes-

sional imaging specialty societies, and the FDA itself to deliver these life-saving treatments more quickly to patients who need them.
“We want to make sure that we ensure the safety of these theranostics patients as we move from third-line to first-line treatments,” she said. “Novartis just published a very promising trial for first-line treatment of neuroendocrine tumors, and I am hopeful they will submit for FDA approval sometime in 2025.”
“The supply chain will continue to be a challenge,” Sawoszczyk said. “Imaging companies also have been looking to partner with pharmaceutical companies to try to solve some of these challenges. It’s a global challenge, but there are companies that are building massive infrastructure.”
To her point, the billion-dollar, 70,000-square-feet radiopharmaceutical therapy agent manufacturing facility that Novartis opened in Indianapolis is only one of many that’s needed to develop, produce, and distribute the supply of therapeutic agents at the heart of theranostics. Until radiopharmaceutical companies can supply the field, various vendors, physicians, and professional societies will be relied upon to facilitate its future growth, Sawoszczyk said.
“Every physician believes that they are practicing theranostics in one particular way, and that’s the only way to practice theranostics,” she said. “But if you take a physician practicing in the middle of the United States, and a physician practicing in New York, their resources are very different. There’s more than one way to practice theranostics. As long as you’re able to treat the patient effectively, safely, and efficiently, then patients will be able to benefit from theranostics.”
SOFTWARE
Just as meaningful to the medical imaging space as innovative, cutting-edge, or entirely novel diagnostic and therapeutic technologies is the software that underpins the organization, security, and accessibility of their data. Jordan Bazinsky, CEO of medical imaging management company Intelerad Medical Systems, believes that the next phases of imaging innovation will turn on “fully unlocking the value of generative AI and the cloud.”
“In the context of imaging, there’s so much value there,”
Bazinsky said. “Scalability of viewing power and storage power is incredible, as is the security structure, and the ability to collocate people who are dispersed regionally in this work from wherever environment.”
“Generative AI can support improvements in workflow on the diagnostic side,” he said. “How do we help radiologists or clinicians identify true positives, boot out false positives, and work on ensuring that we’re putting all these cloud value points out for our customers and making a first-class system?”
Bringing medical imaging technology to the point of care also helps improve accessibility by reducing workflow steps, operational costs, and other barriers to the delivery of care. With about half the global population lacking access to medical imaging technologies, distributed computing and storage networks can help close some of that gap.
“Medical imaging is the tip of the spear,” Bazinsky said. “You can’t treat someone if you can’t diagnose them. There is complex imaging that can only happen in certain settings of care.”
“Much farther out, what’s the transformative thing that is going to happen in medical imaging that’s going to really change the role of imaging in society and in the health care system?” he asked. “Personalized medicine, that’s really exciting; being able to capture more at ever-earlier stages, all in an attempt to intercede much more quickly.”
“To think that ultrasound is only 68 years old, CT only 53, MRI only 47, we remain in such early stages of what’s possible,” Bazinsky said. “The types of interactions in the body that are being looked at doesn’t lessen the need for really talented clinicians; it just shifts how they spend their day.”
Software products like InteleShare are Intelerad’s answer to facilitating the freer, more intelligent, more rapid exchange of medical images among referring physicians, specialists, and even patients themselves. Bazinsky spoke about working to anticipate “the many endpoints that no one could solve for” by managing data more intelligently within physician workflows. AI-powered solutions can support better-quality care, fewer adverse events, and “better understanding of the patient chronology,” i.e., electronic medical records.
“All that data in the past lives inside of paper charts,” he said. “In this day and age, we’re much better equipped to hand that information out, but a clinician still has to sort through that information,” he said. “There’s plenty of data out there with which to train models, but for smaller populations, like pediatrics, the event isn’t quite as large, so it can be a lot harder to identify a disease state.”
“There’s a lot out there waiting to get unlocked,” Bazinsky said. “There’s plenty out there to get better at for most companies, but even when that happens, things will evolve more. I expect that there’s this finish line that doesn’t get reached.” •



DIRECTOR’S CUT
BY NICOLE DHANRAJ
BUILDING A THRIVING SAFETY CULTURE IN YOUR RADIOLOGY DEPARTMENT
Recent events serve as a stark reminder of the paramount importance of safety in our imaging department. Fostering a thriving safety culture goes far beyond fulfilling compliance requirements. It is a strategic cornerstone that elevates both patient care and our department’s reputation for excellence. By prioritizing safety, we create an environment where exceptional care and risk mitigation go hand-in-hand.
LEADERSHIP: SETTING THE TONE FOR SAFETY EXCELLENCE
Leaders play a pivotal role in shaping safety culture. By actively championing safety, fostering open communication, and eliminating mixed messages, you set the standard for your team. Your genuine commitment, evident in both words and actions, inspires staff to prioritize patient well-being and proactively identify potential risks. Here are key principles to remember:
• Prioritize safety, never compromising speed, convenience or external pressures.
• Make safety a continuous conversation and effort. Don’t wait for incidents to happen before taking action.
• Safety is everyone’s responsibility. Encourage ownership by all staff, not just the safety team.
• Focus on improvement, not punishment, through disciplinary processes. Use them as learning opportunities.
• Strive for uniform safety practices across all departments. Inconsistencies create confusion.
• Engage leadership in championing safety, not just delegating it.
BUILDING TRUST AND EMPOWERING STAFF
A cornerstone of a thriving safety culture is trust. Encourage open communication and active participation in safety discussions. Empower staff to raise concerns without fear of reprisal. This fosters a collaborative environment where everyone feels invested in upholding safety standards.
MOVING BEYOND CHECKLISTS: MEANINGFUL SAFETY ASSESSMENTS
Effective safety assessments go deeper than compliance checklists. They focus on understanding the “why” behind our safety protocols and procedures. Regular assessments that gauge staff comprehension and solicit feedback ensure your safety initiatives are targeted and impactful. You will be surprised sometimes at the findings from these assessments. Consider incorporating mock scenarios or soliciting staff suggestions for improvement.
Building a thriving safety culture is a never-ending endeavor, but the rewards are immeasurable specifically for our patients. By consistently prioritizing safety, fostering open communication, and empowering your staff, you create an environment where exceptional patient care and risk reduction are deeply intertwined.
This ongoing commitment not only safeguards your patients but also positions your department as a leader in excellence. Remember, a thriving safety culture is a journey, not a destination. Embrace the continuous pursuit of improvement, and you’ll cultivate a department where safety is not just a value, but a way of life. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.

PACS/IT/AI
BY MARK WATTS
TTRANSFORMATIVE POTENTIAL OF AI IN NON-CLINICAL INNOVATIONS
here is a commercial for a national health care provider that does not tout the clinical excellence of its team but highlights the hassle of “filling out forms, disorganized scheduling, and the bills and the non-bills.” This is a well-understood experience of interacting with the U.S. health care system. We know that 20 percent of the cost of health care in the U.S. is related to administration. This is an opportunity area we should focus on when we brainstorm on artificial intelligence’s role in health care.
Artificial intelligence has emerged as a transformative force across various industries, and its potential to revolutionize medical practice is particularly compelling. While much attention has been given to AI’s clinical applications, such as diagnostics and treatment planning, non-clinical innovations driven by AI hold equally significant promise. These innovations can enhance health care operations, improve patient experiences and optimize resource utilization. As an administrator in health care, I am convinced that embracing AI in non-clinical domains is essential for the future of medical practice. This essay explores the various real-world ways AI can drive non-clinical innovations in health care.
1. AUTOMATED DOCUMENTATION AND TRANSCRIPTION:
• Nuance’s Dragon Medical One: This AI-powered speech recognition and natural language processing (NLP) tool transcribes spoken words into text in real-time. It allows clinicians to quickly document patient encounters without manual typing, saving time and reducing administrative burden.
2. SUPPLY CHAIN MANAGEMENT:
• Predictive Analytics for Inventory Management: AI algorithms analyze historical data and external factors to forecast demand for medical supplies. This proactive approach helps prevent shortages and
overstock situations, ensuring health care facilities are well-prepared to meet patient needs.
3. WORKFORCE MANAGEMENT:
• AI-Driven Staff Scheduling: Predictive analytics can analyze patient volume patterns and staff performance data to create efficient schedules. This minimizes burnout and ensures adequate coverage, enhancing staff satisfaction and retention.
4. DATA SECURITY AND PRIVACY:
• Real-Time Threat Detection: Machine learning algorithms can identify unusual patterns and behaviors that may indicate a security breach. This allows for swift intervention and enhances data security and privacy.
5. FINANCIAL MANAGEMENT:
• Fraud Detection in Billing: AI algorithms can analyze billing data to identify patterns indicative of fraud or errors. This enables health care providers to take corrective action and improve financial management.
6. TELEMEDICINE AND REMOTE MONITORING:
• AI-Powered Telemedicine Platforms: These platforms facilitate virtual consultations, allowing patients to receive medical advice and care from the comfort of their homes. AI algorithms can also analyze data from wearable devices to monitor patients’ vital signs and detect early warning signs of health issues.
These examples demonstrate how AI can drive non-clinical innovations in health care, improving efficiency, reducing costs and enhancing patient experience.
7. STREAMLINING ADMINISTRATIVE PROCESSES:
Administrative tasks in health care, such as scheduling, billing, and documentation, are often time-consuming and prone to errors. AI-powered solutions can automate these processes, reducing the administrative burden on
health care professionals and allowing them to focus more on patient care. For instance, AI-driven chatbots can handle appointment scheduling and reminders, while NLP algorithms can assist in transcribing and organizing medical records. By streamlining administrative tasks, AI can improve efficiency and reduce operational costs.
8. ENHANCING PATIENT ENGAGEMENT AND EXPERIENCE:
AI can play a pivotal role in enhancing patient engagement and experience. Personalized AI-driven health assistants can provide patients with tailored health information, reminders for medication adherence, and lifestyle recommendations. These virtual assistants can also answer common medical queries, reducing the need for patients to visit health care facilities for minor concerns. Additionally, AI-powered sentiment analysis can help health care providers gauge patient satisfaction and identify areas for improvement, leading to better patient experiences and outcomes.
9. OPTIMIZING SUPPLY CHAIN MANAGEMENT:
Effective supply chain management is crucial for ensuring the availability of medical supplies and equipment. AI can optimize supply chain operations by predicting demand, managing inventory and identifying potential disruptions. Machine learning algorithms can analyze historical data and external factors, such as seasonal trends and disease outbreaks, to forecast demand accurately. This proactive approach can prevent shortages and overstock situations, ensuring that health care facilities are well-prepared to meet patient needs.
10. IMPROVING WORKFORCE MANAGEMENT:
AI can revolutionize workforce management in health care by optimizing staff scheduling, predicting staffing needs and identifying skill gaps. Predictive analytics can analyze patient volume patterns and staff performance data to create efficient schedules that minimize burnout and ensure adequate coverage. AI can also assist in identifying training needs and recommending personalized development plans for health care professionals. By improving workforce management, AI can enhance staff satisfaction and retention, ultimately leading to better patient care.
11. ENHANCING DATA SECURITY AND PRIVACY:
Data security and privacy are paramount in health care, given the sensitive nature of patient information. AI can bolster data security by detecting and mitigating cyber threats in real-time. Machine learning algorithms can identify unusual patterns and behaviors that may indicate a security breach, allowing for swift intervention. Additionally, AI can assist in ensuring compliance with data protection regulations by automating data anonymization and encryption processes. By enhancing data security and privacy, AI can build trust among patients and health care providers.
12. FACILITATING RESEARCH AND DEVELOPMENT:
AI can accelerate research and development in health care by analyzing vast amounts of data and identifying patterns that may not be apparent to human researchers. AI-driven data mining and machine learning techniques can uncover insights from clinical trials, electronic health records, and scientific literature, leading to the discovery of new treatments and therapies. Furthermore, AI can streamline the drug development process by predicting the efficacy and safety of potential compounds, reducing the time and cost associated with bringing new drugs to market.
13.
SUPPORTING PUBLIC HEALTH INITIATIVES:
AI can support public health initiatives by providing valuable insights into population health trends and disease outbreaks. Predictive analytics can analyze data from various sources, such as social media, environmental sensors, and health records, to identify emerging health threats and inform public health interventions. AI can also assist in monitoring the effectiveness of public health campaigns and optimizing resource allocation. By supporting public health initiatives, AI can contribute to the prevention and control of diseases on a larger scale.
14. ENHANCING TELEMEDICINE AND REMOTE MONITORING:
The COVID-19 pandemic has highlighted the importance of telemedicine and remote monitoring in health care. AI can enhance these services by providing real-time analysis of patient data and enabling remote diagnosis and treatment. For example, AI-powered algorithms can analyze data from wearable devices to monitor patients’ vital signs and detect early warning signs of health issues. Additionally, AI-driven telemedicine platforms can facilitate virtual consultations, allowing patients to receive medical advice and care from the comfort of their homes.
The potential of AI to drive non-clinical innovations in medical practice is vast and transformative. AI can revolutionize health care operations and improve patient outcomes by streamlining administrative processes, enhancing patient engagement, optimizing supply chain management, improving workforce management, bolstering data security, facilitating research and development, supporting public health initiatives, enhancing telemedicine, improving financial management, and promoting ethical AI adoption. Embracing AI in non-clinical domains is essential for the future of medical practice. By harnessing the power of AI, we can create a more efficient, effective and equitable health care system for all. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.

BY NICOLE DHANRAJ
NOT ALL FAILURE IS EQUITABLE
The relentless pursuit of innovation is the lifeblood of radiology. Discoveries and advancements require calculated risks and the willingness to learn from setbacks. While leaders often champion failure as a stepping stone to success, this narrative overlooks a harsh reality: the double standard of failure faced by underrepresented populations within our imaging teams.
THE BURDEN OF FAILURE: NOT ALL SETBACKS ARE CREATED EQUAL
For imaging professionals from marginalized communities, the consequences of failure can be far more severe. Lacking the safety net of social and economic privilege, the pressure to succeed becomes suffocating, and can take quite the mental toll. The fear of mistakes overshadows the freedom to be creative and take risks. This not only limits individual growth but also deprives our departments of their efforts.
BUILDING A CULTURE OF EQUITABLE FAILURE
The path toward a more inclusive and innovative radiology future requires dismantling the double standard of failure. Here are some actionable strategies you, as an imaging leaders can implement:
1. Create an environment where all team members feel comfortable taking risks and openly discussing failures. Celebrate stories of resilience from diverse backgrounds, showcasing the power of learning from setbacks.
2. Establish mentorship programs and be intentional about connecting underrepresented professionals with experienced leaders. Mentors can offer guidance, share their experiences with failure, and provide a supportive network to navigate challenges.
3. Implement regular training on concepts like unconscious bias to delve into its impact on evalua -
tions especially in marginalized groups.
4. Shift the focus from flawless execution to valuing effort, creativity, and the ability to learn from mistakes. Recognize progress.
5. Develop anonymous surveys, focus groups, or other mechanisms for employees to provide and receive constructive feedback without fear of retribution.
6. Champion organizational policies that support equitable opportunities. This includes fair performance evaluations, transparent promotion criteria, and accessible professional development resources.
MEASURING PROGRESS AND MOVING FORWARD
Tracking progress on these initiatives is crucial. Leaders can establish metrics to measure the effectiveness of implemented strategies, demonstrating commitment to accountability and continuous improvement. By promoting a culture that genuinely embraces learning from failure we can empower everyone to take calculated risks, learn from setbacks, and contribute their unique talents to radiology. Ensuring equity in failure increases our drive for progress and inclusion in our profession.
Let’s lead the charge in dismantling the double standard of failure! By implementing these strategies, we can cultivate a thriving radiology field where diversity of thought thrives. In this environment, everyone feels emboldened to learn, innovate and contribute their best talents without the crippling fear of failure holding them back. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.







EMOTIONAL INTELLIGENCE
BY DANIEL BOBINSKI
TTHE DIFFERENCE BETWEEN ASSERTIVE AND AGGRESSIVE
oo often, people think they’re being assertive when they’re really being aggressive. This mistake is usually accidental, but people trying to assert themselves can easily create problems if they’re not sure of the differences between the two styles.
To help us clarify the differences, let’s imagine a graph. The vertical axis represents your ability to stand up for yourself to get your needs met, and the horizontal axis represents your ability to have genuine consideration for others and a concern that they get their needs met.
If we draw two perpendicular lines and create four quadrants on the graph, we can label them aggressive, assertive, passive and passive aggressive. Almost everyone tends to be in one of those quadrants. To better understand the difference between assertive and aggressive, let’s consider the characteristics of each box.
The upper left box on our graph scores high in standing up for oneself but low in consideration of others. This is the aggressive box. People scoring this way are adept at getting their views heard and their needs met, but tend not to consider other people’s point of view. Using common vernacular, such a person has a strong desire to “win” and generally doesn’t have an interest in what others want or need.
In some cases, people become super aggressive. That is, not only will they fight to win, they’ll also fight to ensure the other party loses. Generally speaking, being aggressive is unhealthy for workplace cohesiveness and it doesn’t align with the idea of teamwork.
The lower right quadrant is labelled passive. People scoring here are quick to consider others’ perspectives and will sometimes even help others get their needs met. However, they tend not to stand up for what is rightly theirs. And, because they won’t be firm in getting their own needs met, they may build up a lot of unspoken resentment. As you can imagine, passive behavior in the workplace is also unhealthy.
The lower left quadrant is labelled passive aggressive. Frankly, I feel sorry for people who score here. These folks usually don’t openly state what they want, nor will they strive to truly consider other people’s point of view. As such, they struggle seeing the bigger picture and often view themselves as victims. People in this group may sometimes be malicious and any hostility always carries plausible deniability. If you’ve been around this type of person, you know it’s an unhealthy position to take and not good for workplace progress.
Finally, we have the upper right quadrant, which is labelled assertive. People scoring here want others to score a win but will also stand up for their own needs. Think of it as a win-win mentality. Assertive people are a refreshing breath of fresh air in the workplace. It seems they are always striving to get things done while working to ensure everyone is rowing together in the same general direction.
As mentioned earlier, assertiveness is the healthiest place to be. That said, being in that quadrant usually requires a conscious choice. And being assertive requires a bit of practice balancing out the win-win.
BECOMING ASSERTIVE
Aggressive people must learn empathy and passive people must develop courage. Passive-aggressive people will have the most difficulty in transitioning to assertiveness. Frankly, they often need a lot of personal healing, because it’s not uncommon for their sense of survival to be based on ignoring or distorting reality.
In the Oxford English Dictionary, the verb “assert” means “to state an opinion, claim a right, or establish authority.” Obviously, those attributes are to be encouraged as they are part of assertiveness. However, being assertive goes beyond that. It includes doing what’s in that definition plus the practice of maintaining a high regard for what other people want or need. Remember, the assertiveness quadrant is just as easily called, “win-win thinking.”

Essentially, think of assertiveness as having a mindset that says, “I want to win, but I’m not going to walk over you to do it – I’m going to respect what you want and work to help you get your win, too.”
A CHANGE OF THINKING IS REQUIRED
Many people struggle with differentiating between aggressiveness and assertiveness. The key is thinking win-win. Way too often I hear people giving lip service to achieving win-win outcomes, but their thinking is still win-lose (aggressiveness). When someone’s thinking is not geared toward helping other people get what they want in addition to achieving a win for themselves, then achieving win-win outcomes pretty much falls to random chance.
If you find yourself being either passive or aggressive and want to move into being assertive, allow me to point you Habit 5 from Stephen Covey’s, “7 Habits of Highly Effective People.” It’s “seek first to understand, then be understood.” In this axiom we see the balance: An ability to genuinely consider someone else’s point of view (seek first to understand), and an ability to stand up and get your needs met (then be understood).
THE DANGER OF IMBALANCE
One problem I’ve seen in some passive people who’ve tried to be assertive is that they overshoot the mark.
They finally stand up to voice their desires, but then they jump straight to aggressiveness. In other words, they go from acquiescing to the needs of others (passiveness) to totally ignoring the needs of others (aggressiveness). This is a common mistake, so it’s important that passive people understand the need for a balance.
Personally, I think the order of Covey’s fifth habit is excellent, because by first seeking to understand someone else’s point of view, you’re establishing the groundwork for an attitude and practice of fairness. Then, after you genuinely understand the other person’s point of view, it’s only fair that you be heard and understood as well.
The key to success in this effort is striving for balance. Granted, sometimes one has to cautiously choose one’s battles, but the more balance there is in seeking to understand and seeking to be understood, the healthier your communications – and your workplace – will be. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.




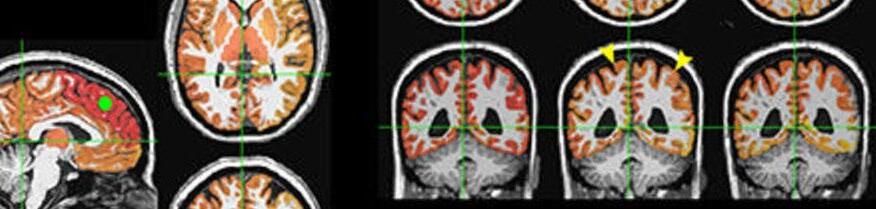
MEDICINE FOR THE SOUL
LIGHT THERAPY INCREASES BRAIN CONNECTIVITY FOLLOWING INJURY
Low-level light therapy appears to affect healing in the brains of people who suffered significant brain injuries, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA).
Lights of different wavelengths have been studied for years for their wound-healing properties. Researchers at Massachusetts General Hospital (MGH) conducted low-level light therapy on 38 patients who had suffered moderate traumatic brain injury, an injury to the head serious enough to alter cognition and/or be visible on a brain scan. Patients received light therapy within 72 hours of their injuries through a helmet that emits near-infrared light.
“The skull is quite transparent to near-infrared light,” said study co-lead author Rajiv Gupta, M.D., Ph.D., from the department of radiology at MGH. “Once you put the helmet on, your whole brain is bathing in this light.”
The researchers used an imaging technique called functional MRI to gauge the effects of the light therapy. They focused on the brain’s resting-state functional connectivity, the communication between brain regions that occurs when a person is at rest and not engaged in a specific task. The researchers compared MRI results during three recovery phases: the acute phase of within one week after injury, the subacute phase of two to three weeks post-injury and the late-subacute phase of three months after injury.
Of the 38 patients in the trial, 21 did not receive light therapy while wearing the helmet. This was done to serve as a control to minimize bias due to patient characteristics and to avoid potential placebo effects.
Patients who received low-level light therapy showed a greater change in resting-state connectivity in seven brain region pairs during the acute-to-subacute recovery phase compared to the control participants.
“There was increased connectivity in those receiving light treatment, primarily within the first two weeks,” said study coauthor Nathaniel Mercaldo, Ph.D., a statistician with MGH. “We were unable to detect differences in connectivity between the two treatment groups long term, so although the treatment appears to increase the brain connectivity initially, its long-term effects are still to be determined.”
The precise mechanism of the light therapy’s effects on the
brain is also still to be determined. Previous research points to the alteration of an enzyme in the cell’s mitochondria (often referred to as the “powerhouse” of a cell), Gupta said. This leads to more production of adenosine triphosphate, a molecule that stores and transfers energy in the cells. Light therapy has also been linked with blood vessel dilation and anti-inflammatory effects.
“There is still a lot of work to be done to understand the exact physiological mechanism behind these effects,” said study coauthor Suk-tak Chan, Ph.D., a biomedical engineer at MGH.
While connectivity increased for the light therapy-treated patients during the acute to subacute phases, there was no evidence of a difference in clinical outcomes between the treated and control participants. Additional studies with larger cohorts of patients and correlative imaging beyond three months may help determine the therapeutic role of light in traumatic brain injury.
The researchers expect the role of light therapy to expand as more study results come in. The 810-nanometer-wavelength light used in the study is already employed in various therapeutic applications. It’s safe, easy to administer and does not require surgery or medications. The helmet’s portability means it can be delivered in settings outside of the hospital. It may have applications in treating many other neurological conditions, according to Gupta.
“There are lots of disorders of connectivity, mostly in psychiatry, where this intervention may have a role,” he said. “PTSD, depression, autism: these are all promising areas for light therapy.” •
REFERENCE
“Effects of Low-Level Light Therapy on Resting-State Connectivity Following Moderate Traumatic Brain Injury: Secondary Analyses of a Double-blinded, Placebo-controlled Study.” Collaborating with Drs. Gupta, Mercaldo and Chan were Maria G. Figueiro Longo, M.D., Jonathan Welt, M.D., Arman Avesta, M.D., Jarone Lee, M.D., Michael H. Lev, M.D., Eva-Maria Ratai, Ph.D., Michael R. Wenke, B.S., Blair A. Parry, B.A., Lynn Drake, M.D., Richard R. Anderson, M.D., Terry Rauch, Ph.D., Ramon Diaz-Arrastia, M.D., Kenneth K. Kwong, Ph.D., Michael Hamblin, Ph.D., and Benjamin Vakoc, Ph.D.
ICE Break






•
•
•
•

•
•









































































































































































































































































































































