We live in a world where medical imaging technology and pathology tests can increasingly unravel the mysteries of disease and injury. They are the tools that help doctors diagnose and treat, and they are based on reliable science.
But what if the diagnosis remains elusive? Is it OK to accept we don’t always understand what just happened or why, particularly once the emergency or symptoms have passed?
Recently I have been faced with that dilemma, after weeks of undergoing an assortment of diagnostics – a CT scan, MRI, ultrasound, barium swallow and twice-weekly bloods – all because of some very high enzymes found (by chance) in a blood test. After much discussion with multiple doctors once the imaging gave the all-clear and the enzymes started to head south, the consensus was that no one really knew what happened or why.
We could have done more tests. But I felt 100% fine, and most of the opinion was that this probably mattered more than the high enzyme results.
It is true what one doctor told me – it’s not very satisfying to not find the answer, but we agreed that was far more preferable than finding an answer that was not good news.
If you will indulge me one more observation from my recent medical fora, I was reminded how lucky we are to have a (mostly) excellent public hospital system.
At Fiona Stanley Hospital I watched the care and respect that doctors, nurses, patient assistants and volunteers gave people who were very unwell, disorientated, cranky, emotional, or all of the above.

We are right to be alarmed by stories we hear of people who slip through the cracks, but many more get the care they need – and they don’t make the headlines.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
It is true what one doctor told me – it’s not very satisfying to not find the answer, but we agreed that was far more preferable than finding an answer that was not good news.
12 Cover story: A helping hand for Ukraine

16 Close-up: Dr Anh Nguyen

26 Gene therapy changes the conversation 30 Blood works


LIFESTYLE
52 Car review: The Audi eTron S – Dr Mike Civil 54 Comedy: Georgie Carroll – Nursing a funny bone
1
This month our doctors dozen is from Sandalford, a winery with one of the longest and richest histories in Western Australia. Read Dr Louis Papaelias’ review on page 56, and note his tip to make room in your cellar for the 2018 Reserve Estate Cabernet Sauvignon. We also have a double pass to a show by nurse-turned-comedian Georgie Carroll at next month’s Perth Comedy Festival.
To enter go to the competitions link at www.mforum.com.au or use the QR code on this page.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au





Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au








Marketing Quinn Hampton quinn@mforum.com.au

Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory

Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM

Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au
Dr Alison Salt, an international expert in childhood vision, says recognising the health and developmental issues that can occur with childhood vision impairment is crucial.
The consultant paediatrician in Kids Rehab WA at Perth Children’s Hospital and Clinical Associate Professor at UWA has co-authored a book based on her experience with the Developmental Vision Service at the Great Ormond Street Hospital for Children in the UK.

Children with Vision Impairment incorporates more than four decades of experience from clinician researchers at the UK service in collaboration with leading experts around the world. It aims to support health professionals working with visually impaired children and parents, some of whom contributed to the book.
Dr Salt said one of the key messages was the importance of supporting parents as early as possible to help their babies who have a visual impairment reach their full potential.
“Every aspect of a child’s development including their movement, sound location, language and social development is driven by vision,” she said.
Women are expected to make up a significantly larger proportion of Australia’s GP workforce in the future, with the number of female GPs continuing to grow more quickly.
The number of women GPs in training has surpassed men, at 58% women compared to 39% men, according to the latest RACGP Health of the Nation report.
There were 18,472 women GPs in the workforce in 2020-21, compared to 19,916 men.
RACGP President Dr Nicole Higgins said Australia’s women GPs need to be celebrated and supported.
“More women are becoming GPs than ever, and we should celebrate this as it highlights where progress has been made towards gender equality,” she said. “The days when being a doctor was solely a profession for men are far behind us. However, we still have a way to go to achieve equality.
“One of the key issues is that
“It’s therefore important to view vision impairment in a broad developmental context and consider how to address potential vulnerabilities.
“Despite the challenges these children face, they can develop alongside their peers and achieve remarkable things.”
women GPs tend to spend longer with their patients because they see more people with complex needs. Female GPs spend 19 minutes on average with patients compared to 16 minutes for male GPs.
“But Medicare pays less per minute for longer consultations, meaning women GPs and their patients are being unfairly penalised.”
Dr Higgins said more funding for longer consultations would make a real difference for people with complex needs across Australia.
This included women with sensitive issues, including sexual health and reproductive concerns, mental health issues and those experiencing abuse and violence.
WA’s Great Southern region will soon have access to radiation oncology services close to home, through the State Governmentfunded $13.1 million GenesisCare Albany radiation oncology facility.
Patient care will be managed by a multidisciplinary team of specialised cancer experts, and patients will have rapid access to personalised care for specialist consultation and treatment across many tumour types.
The fit-for-purpose centre allows integration with the Albany Health Campus and Albany public and private hospitals, ensuring patients are supported at all stages of their journey.
Accommodation and transport packages will be offered, as well as bulk billing for Medicare-eligible patients
Black Dog Institute has launched a new health professional resource and education hub to provide easy access to online programs, resources and primary care information on mental health.
continued on Page 8
A Perth paediatrician wants to make other health professionals aware of the impact of vision impairment on a child’s development.
Ms H was a 43 year old woman, mother of two young children, and a successful business executive and she was invited by her employer to undergo a ‘cardiac health assessment’ in March 2019.
The ‘cardiac health assessment’ consisted of a coronary artery calcium score and CT coronary angiogram.
Ms H had no history of cardiac problems but was encouraged by her workplace to undergo the assessment. Dr T was the radiologist in attendance on the day Ms H attended for the procedures, and was the only doctor on site. Unfortunately, Ms H suffered a severe allergic reaction when the Omnipaque dye was administered intravenously. Resuscitation was commenced at the radiology practice, an ambulance called and Ms H was taken to hospital, but she died about a week later without regaining consciousness.
Cause of death was multisystem organ failure and hypoxic/ ischaemic encephalopathy due to anaphylactic reaction to CT contrast medium.
The scan report showed that Ms H had a calcium score of 0 and normal coronary angiogram.
Ms H’s death was the subject of a coronial inquest 1. Ms H’s family requested an Inquest, noting that a number of factual issues required investigation and that there were important public health implications, ‘including the process of company employees being tested, the failure to be seen by a doctor prior to an invasive test and the management of her anaphylactic reaction’.
The inquest lasted over two weeks, involving sixteen witnesses, and six expert witnesses.
The coroner found that the impetus for the ‘cardiac health assessment’ program had arisen from the best of intentions after a worker for Ms H’s employer had suffered but survived a cardiac arrest. Following this, the managing director wanted to give his staff the opportunity to have ‘the best private medical assessment program for heart health’ at the company’s cost, and he asked one of his managers to develop a suitable program.
The coroner investigated the complex arrangements of business entities and individuals involved in the development and implementation of the ‘cardiac health assessment’ program.
The coroner determined that Ms H died as a result of substandard clinical judgement from doctors at the beginning and end of this programme, combined with a misalignment of incentives amongst the various business entities that facilitated the process. The inquest heard evidence about an industry putting profits over patients.
The ‘cardiac health assessment’ program had been developed without obtaining formal and considered medical advice on the risks of the tests, or whether these two tests were the most suitable or whether there should have been a preliminary assessment by a medical practitioner. The radiology request forms were affixed with Dr S’s electronic signature, although he had never seen or spoken to the people undergoing the tests, and he considered his role was to receive the results and have a discussion with the participants about their results.
The coroner considered that Ms H had not fully given her consent as she did not know the true nature of the procedure, and possible alternate pathways, and had not discussed the procedures with either the referring doctor, or the radiologist.
The referring doctor, Dr S, was referred to Ahpra. The coroner was critical that Dr S had allowed his signature to be used for referrals for patients he had not reviewed, and that Dr S failed to apply ethical standards as he considered himself to hold a lesser obligation to persons who he considered to be ‘clients’ or ‘candidates’ rather than ‘patients’.
The radiologist, Dr T, was referred to Ahpra, with the coroner finding that the CT scan was performed on the basis of a referral with insufficient clinical detail, and that Dr T failed to recognise and manage Ms H’s anaphylaxis appropriately.
Extensive recommendations were made by the coroner with many relating to improving the recognition and management of severe contrast reactions and anaphylaxis. Other recommendations include that:
RANZCR prepare a joint position statement with the Cardiac Society of Australia and New Zealand regarding when ‘screening’ is an acceptable indicator for a CT angiogram or other invasive cardiac tests.
RANZCR update its standards and guidelines regarding both clinical requests and consent procedures to address the increasing prevalence of ‘screening’ requests, and to ensure that imaging procedures are not performed for ‘screening’ when lower-risk alternatives might achieve the same end.
the RACGP and the AFOEM prepare a joint position statement on the appropriateness of a practitioner authorising, or otherwise allowing, their signature to be used in referring individuals (whether ‘patients’, ‘clients’ or ‘candidates’) for tests when neither the patient, nor any information specific to the patient, has been reviewed.



Perth urologist Prof Dickon Hayne has accepted the British Journal of Urology ’s Global Prize for 2023, on behalf of the Australian and New Zealand Urogenital and Prostate Cancer Trials Group, for research on local anaesthesia to reduce the discomfort of prostate biopsy.

Dr Charmaine Green, a woman of the Yamaji Nation and a research fellow with the WA Centre for Rural Health in Geraldton, has become the first to be awarded a PhD through Kurongkurl Katitjin, Edith Cowan University’s Centre for Indigenous Australian Education and Research.
WA’s Perron Institute has appointed Emeritus Professor John Finlay-Jones as a board director. With a background in clinical microbiology and immunology, he also takes over as chair of the institute’s research advisory committee.
In other moves, Telethon Kids Institute and the University of Western Australia have appointed Professor Melissa Penny, a leading researcher in malaria and infectious diseases, as the inaugural Fiona Stanley Chair of Child Health Research.

Sherl Westlund, the long-serving executive of Diabetes Research
WA, has stepped down from the role she has held since 2007, after first joining the organisation in 1997.
continued from Page 4
The custom-built platform will provide health professionals with access to evidence-based online resources, including accredited training modules, webinars, podcasts and other e-Mental Health in Practice content.
These are designed to introduce health professionals to online programs and tools, and to demonstrate how e-mental health technologies can be integrated into primary care.
Jan Orman, Black Dog’s GP Services Consultant, said Australia used a stepped care model of mental health care where the
treatment a patient received was matched to the severity of their symptoms.
She said e-mental health treatments were good options for many people with mild to moderate conditions and, in some cases, might be the only treatment needed at that time.
Users will also be able to connect with other health professionals through the Mental Health Community of Practice, where they can exchange ideas, thoughts and experiences with peers via forums moderated by Black Dog Institute’s team of experts.
Bethesda Health Care’s new mental health service and hospital in Cockburn is now accepting referrals.
Bethesda Clinic, which opened in March, is the first private mental health service south of the river, built at a cost of more than $60 million. It aims to offer care closer to home and meet the demand for mental health care in Perth’s southern suburbs as well as the southern regions of WA.


The 75-bed facility provides adult inpatient services and outpatient day programs through the Wellness and Recovery Centre.
The clinic has a dedicated military, veteran and first responder trauma ward, and in a State-first – a women’s-only ward offering patients treatment in a gender-safe environment.
Bethesda CEO Dr Neale Fong said that in a move away from traditional private hospital mental health care, a national-first partnership with Microsoft Cloud for Healthcare would support patients post-discharge to remain mentally well in their home and community.
Science on the Swan – now in its eighth year – runs from May 8-10 at the Perth Convention and Exhibition Centre with the theme Partnering for Success. See register.scienceontheswan@ arinex.com.au
“The digital element of the clinic is what we are really excited about, and our model of care works towards minimising repeat admissions,” he said. “We want to see people supported and well outside of a hospital environment.”
Bethesda Clinic is accepting referrals for general psychiatry, alcohol and other drug addiction, mood and anxiety and trauma.
Stage two will open in the middle of the year, rounding out the 75 beds, and will include a neurostimulation suite with electroconvulsive therapy and repetitive transcranial magnetic stimulation.
Introduction
Cardiovascular disease is common in systemic autoimmune disorders and confers the greatest effect on mortality. In Rheumatoid Arthritis (RA) the increased risk of mortality is up to 50%. Long-term corticosteroids may add to the cardiovascular burden. In addition, some disease-modifying anti-rheumatic drugs (DMARDS) are potentially cardiotoxic.
Atherosclerosis
Atherosclerosis pathogenesis involves an imbalance in pro- and anti-inflammatory cytokine activity. An increased risk of atherosclerosis is present in all the inflammatory joint diseases and, in RA, is commensurate with the risk associated with Diabetes Mellitus.
There is a modifiable increased risk associated with chronic inflammation, while co-existing traditional risk factors may be increased in RA. Disease severity, persistence of disease activity and duration and Rheumatoid Factor concentration are associated with cardiovascular risk.
In Systemic Lupus Erythematosus (SLE), significant increases in coronary artery calcification and carotid intima-media thickness/carotid plaques are reported. Antibody-mediated prothrombotic endothelial damage increases risk to the highest among the SARDS. Manzi et al. showed that for females 4450 years old, those with SLE have a 50-fold increased risk of myocardial infarction. There is a disease specific effect on lipid metabolism which should promote assiduous management of dyslipidaemia.
Several autoimmune diseases are associated with the heart wall and consequent ventricular dysfunction. RA is significantly associated with biventricular diastolic and left ventricular systolic dysfunction which may be asymptomatic. Most studies show that myocardial disease occurs relatively early although it may be asymptomatic for some time. Treatment with methotrexate and biologic response modifiers decrease the risk for heart failure.
In SLE, silent myocardial damage with diastolic dysfunction occurs in >45% of patients. Increased LV wall thickness and mass with decreased LV ejection fraction
By Associate Professor Louise
may be due to vasculitis, myocarditis or vascular stiffening.
Both myocardial fibrosis and myositis are reported in Systemic Sclerosis. Fibrosis is associated with vasospastic events (cardiac Raynaud phenomenon) and is increased in patients who also have skeletal myopathy and results in chronic heart failure.
Idiopathic inflammatory myopathy (IIM) may involve cardiac muscle with consequent heart failure and high mortality. Anti-SRP antibody is associated with cardiac involvement.
About 30% of patients with RA have valvular disease, most commonly fibrotic thickening of the base of the valve with, or without, calcification which may be subclinical. The mitral valve is most commonly involved, followed by the aortic, tricuspid and pulmonary valves. Granulomatous inflammation of the valves can lead to incompetence.
SLE is associated with valvular abnormalities (up to 60%) including thickening and vegetations. The clinical outcomes may include both stenosis and regurgitiation (2-5%). LibmanSacks vegetations involve the mitral valve most frequently, followed by the aortic valve, and are strongly associated with the anti-phospholipid syndrome in which there is a three-fold increase in any valvular lesion. Libman-Sacks vegetations are associated with valvular insufficiency. Severe mitral insufficiency in SLE is associated with anti-SSA antibodies. The tricuspid and pulmonary valves can be affected.
Pericarditis is present in up to 20% of patients with RA.
Serositis is a feature of Systemic Lupus Erythematosus and pericarditis occurs in up to 50%. Tamponade may occur.
Systemic sclerosis is complicated by
pericardial disease in 24% of cases of limited skin disease (lcSS) and 46% of diffuse cutaneous disease (dcSS) and may be accompanied by right HF. The pericardium is fibrotic and there is risk of tamponade.
Various conduction abnormalities are present in the SARDs. Sudden cardiac death occurs twice as frequently in RA as in the general population. Up to a third of patients with AS have 1st degree AV block. The presence of anti-SSA is associated with potentially fatal fetal heart block.
Antiphospholipid Syndrome (APS)
This rare syndrome has an incidence of 1-2 per 100 000 a year. Its importance lies in its effective management. It occurs as a primary disorder or in the presence of other autoimmune disorders, notably lupus. Diagnosis is predicated upon the combination of a single clinical criterion (thrombosis and/or pregnancy morbidity) with persistent antiphospholipid antibody (repeat positive at >/= 12 weeks) at moderatehigh concentration.
The most frequent cardiac manifestations of APS are vegetations, valve thickening or valve dysfunction. APS may also cause occlusive arterial disease in the heart since the site of pathology is endothelium, this includes accelerated atherosclerosis. Other abnormalities include ventricular hypertrophy and dysfunction, intracardiac thrombus and pulmonary hypertension.
Conclusion
Autoimmune disorders convey an increased risk of cardiovascular disease demanding careful assessment and astute clinical management.
References on request
Two trail-blazing women working in the health sector – one a plastic surgeon and the other an Aboriginal health worker – have been inducted into the Western Australian Women’s Hall of Fame.

As well, a veteran health journalist has been recognised, particularly for her work in the 1970s to raise awareness about the risks from blue asbestos exposure in Wittenoom.
Established in 2011 in recognition of the Centenary of International Women’s Day, the Hall of Fame acknowledges the contributions and achievements women have made to WA’s community, society, history and culture.
Last month, 16 women were inducted, and a further four added to its Roll of Honour for their contribution across areas such as arts, business, community, culture, education, health, sport and STEM.
Those recognised in the health category, sponsored by St John of God Health Care, were Nola Naylor, Director of Aboriginal Health Strategy at the South Metropolitan Health Service, and Perth plastic surgeon Dr Anh Nguyen
Ms Naylor, a proud Banjima woman from the Central Pilbara, helped develop the Aboriginal Health Champions Network Program which identifies staff who undergo a cultural learning opportunity to explore additional understanding and experiences to improve health and wellbeing for Aboriginal people.
Ms Naylor has also partnered
with Aboriginal Health Strategy Directors state-wide and staff from the Training Centre in Subacute Care (TRACS WA) to prepare an introductory module for health clinicians in Aboriginal personcentred care that is culturally appropriate.
She has helped build alliances with health clinicians, support workers, policy makers from WA secondary and tertiary hospitals, and nongovernment and not-for-profit organisations.
These programs all reduce the financial burden on the health system by reducing the incidence of discharge against medical advice.
The Hall of Fame noted Ms Naylor was an outstanding leader and mentor who embodied cultural respect and modelled these behaviours in her daily work.
“Her in-depth knowledge of the spiritual, cultural and health needs of Aboriginal peoples mean Nola plays an integral role in creating a positive hospital experience,” her citation said.
Vietnamese-born Dr Nguyen was recognised for her contribution in a medical specialty which was once male-dominated but has evolved over time.
A Fellow of the Royal Australasian College of Surgeons, Dr Ahn has more than 20 years’ experience in emergency trauma surgery, reconstructive and aesthetic plastic surgery, and is an on-call plastic surgeon and consultant to numerous Perth hospitals including
Posthumously recognised in the Hall of Fame’s Roll of Honour was Catherine Martin , the awardwinning West Australian journalist who was born in 1918 and helped expose Wittenoom’s toxic legacy.
During Martin’s expansive 28-year career in newspapers, she covered subjects including Aboriginal health, remote health care, cancer treatment and the dangers of smoking and drinking alcohol. Her reports triggered overhauls in government procedures and people’s habits.
But it was Martin’s work for The West Australian exposing the deadly toll of the blue asbestos Wittenoom mine in the Pilbara that has left the longest-lasting impression.
In 1978, she began investigating the high incidence of death and disease among workers at the mine — writing the first of many articles which gave a voice to frightened Wittenoom families and concerned medical experts.
The reports contributed to the establishment of a compensation foundation by the mine’s operator, Colonial Sugar Refinery, and earned her the Gold Walkley in 1978.
Last month – 14 years after Martin died in 2009 at the age of 90 — she was posthumously recognised for her trailblazing reporting.


As he watched the Ukrainian crisis unfold last year, information technology-trained Robert Hicken watched in horror as millions of displaced people suddenly faced a health care crisis.
Some Ukrainians were living in occupied territories in their homeland – where hospitals and medical clinics had been decimated – while others were fleeing to countries across Europe and beyond.

For the founder and chief executive officer of Perth-based company Practice Innovators International, which owns and operates the telehealth platform GPNow, the challenge was clear but the logistics were daunting.

After Russia invaded Ukraine in February last year, it was estimated that more than seven million people fled the war-torn nation, while another 44 million remained, often living in volatile and uncertain conditions. With more than 100 hospitals and clinics damaged or destroyed across the country, it was difficult for those still living there to access medical care, while many refugees who relocated were finding it hard to communicate with local doctors because of language barriers.
Mr Hicken hatched an ambitious plan to tweak existing technology and systems used in Australia to link Ukrainian patients to doctors.
The proof of concept was already there, as the company’s telehealth platform had already been used by aged care facilities, remote Aboriginal groups, bushfire-affected communities and Spinal Cord Injuries Australia to provide access to APHRA-certified medical professionals.
A small Perth-based telehealth company has been playing an unlikely role in humanitarian efforts to link displaced Ukrainians with doctors around the world, as Cathy O’Leary explains.
The Yaburara and Coastal Mardudhunera Aboriginal Corporation had partnered with GPNow to provide clinical assessment and consultations for 1000 families across regional WA, while SCIA used the technology to offer online services Australia-wide.
Born in London, Mr Hicken had migrated to Perth in 1989 with a young family, and was inspired to raise funds for spinal care research and treatment after close friend David Prast became a quadriplegic after a surfing accident at Cottesloe Beach in 1995.
Pre-COVID, Mr Hicken had seen the retail evolution of internet sales and decided that telehealth was the next big revolution, but it was still a very doctor-centric model and there were many logistical issues to overcome. His company raised $1 million to build a system that was high definition and low bandwidth, building a video engine from the ground up before testing it with a medical centre group in Melbourne.
“We had started a pilot with Spinal Cord Injury Australia to use telehealth but it wasn’t really working financially, and then bang, COVID hit, and then there was suddenly funding through the NDIS because spinal cord injury patients were cancelling all their medical appointments,” Mr Hicken said.
“Throughout the COVID period we did 15,000 one-hour sessions. It was kind of surreal, and then Paraquad NSW contacted us and wanted to use telehealth too. At the time it helped a lot of patients stay connected.”
In March last year, the GPNow team decided to build a dedicated virtual clinic of Ukrainian medical professionals to help those in need with free medical advice and care. With the project needing significant financial and technical support, Mr Hicken reached out to Amazon Web Services, which had just announced it was keen to support humanitarian projects in Ukraine. Within weeks the Ukrainian CrisisCare Telehealth Service was launched, run in partnership with the World Organisation of Family Doctors (Vasco da Gama Movement), and it started connecting Ukrainian patients to doctors.
It received support in the form of 15,000 cloud service ‘credits’ as well as US$100,000 in cash contributions and technical assistance to keep it running smoothly and protect it from potential cyber threats.
Since then it has been operating on a shoe-string budget to provide primary health care to the most vulnerable and relieve pressure on a health system suffering the effects of war. The medical practitioners are mostly Ukrainian refugees who cannot practice overseas.

To forge connections in the local medical community and find doctors who could provide care, GPNow appointed Dr Vadim Ilyashenko, a highly respected Ukrainian neurosurgeon, as its chief medical officer.
The 24/7 multi-lingual telehealth service has now helped more than 6700 Ukrainian families, with close to 6000 consultations provided by more than 100 medical professionals, including family doctors, paediatricians, neurologists, obstetricians, oncologists, psychologists and psychiatrists.
“There is no medical information on the platform and all of the doctors are anchored to the country where they’re licensed to practise, so the Aussie doctors must be APHRA-certified and provide all their identification and medical indemnity details,” Mr Hicken said.
“We can be beaming in doctors anywhere in the world really quickly to help those in need with free medical advice. People can use their own language and they can choose doctors anywhere in the world. They can view the doctor’s profile and it shows if they’re available online.”
About 90% of the doctors with the service are refugees themselves –many of them women, some with children who left their husbands behind in Ukraine.
“Doctors are paid ¤10 a day to be online, and ¤10 for every consultation, capped at ¤1000 a month. If they do more sessions than that – and many do – they don’t get paid for it,” Mr Hicken said. “They’re an amazing group of dedicated people.”
Despite many being highly qualified medical professionals, they could not otherwise find paid work.
“We had one woman who was an expert oncologist with 20 years’ experience and living in France, who was working at McDonald’s because her qualifications weren’t recognised,” Mr Hicken said.
“These doctors are loving this because they can care for their fellow citizens online. So, it’s a winwin for patients and doctors.”
Mr Hicken said most projects were about increasing revenue but the main KPI with the not-for-profit Ukraine project was about saving lives, with many people willingly volunteering many hours of their time.
Among those helped through the service has been a young woman from Kyiv, Anastassia, who had been living alone in a Polish hostel, separated from her partner who was a Ukrainian soldier.
After seeking help, the 18-year-old was found to have multiple tumours in her neck and spine, and teams
continued on Page 15

continued from Page 13
of doctors worked globally to have her relocated to Amsterdam for life-saving surgery.

“Everyone in our team, all our doctors, have deeply moving stories, as well as horror stories, so we have used the story of Ana to try to make the numbers human,” Mr Hicken said.
Of course, the Perth-born telehealth project is only a small part of a suite of humanitarian efforts by doctors and other volunteers around world.

Soon after the escalation in war last February, Médecins Sans Frontières (Doctors Without Borders) started helping people evacuate from the east to the west of the country by medical train as the front lines inched closer.
One year later, MSF continues to respond to the humanitarian needs of the people affected by the conflict. Across Ukraine and in surrounding countries, hundreds of its staff are working in partnership with local organisations to provide lifesaving medical and mental health care to those who need it most.
That includes providing patient care on board two medical trains, developed with Ukrainian Railways. The medically equipped carriages help to evacuate patients out of hospitals close to active war zones and refers them to hospitals away from the frontlines. One train provides basic medical care and can carry up to 50 patients. The other train is able to carry around 26 patients and is equipped to provide intensive care for patients in serious condition.
Between March and December last year, the two trains evacuated more than 2600 patients and 78 orphans. Other key medical needs include insulin for diabetes patients, as well as medicines for people with other chronic diseases.
A recent report by several human rights and humanitarian groups, including Physicians for Human Rights, estimated that between February 24 and December 31 last
year there were 707 attacks on Ukraine’s health care system.
As a result, 218 hospitals and clinics were damaged or destroyed, 65 ambulances were attacked, and there were 181 documented attacks on other health infrastructure such as pharmacies, blood centres and dental clinics.
At least 62 health workers had been killed and another 52 injured, while many more were threatened, imprisoned, taken hostage or forced to work under Russian occupation.
Back in Australia, Mr Hicken is worried about the future of the Ukraine telehealth service, because the funding from AWS is running out.
While the project has achieved his goal – to use technology to provide medical care to those affected by the war in Ukraine – he is frustrated that, with no end in sight for the war, thousands more people need help.
“What’s killing me is that we know we can help 500,000 families a month – so there are thousands of families who are missing out on the basic primary care they should be getting,” he said.
He recently addressed a meeting hosted by the Rotary Club of Subiaco to implore corporate and private sponsors to dig deep so that the platform can continue in
2023 to employ displaced Ukrainian doctors to plug the gaps in the damaged health infrastructure.
The project is seeking ¤100,000 to continue its work in the first part of this year, with about ¤17,000 raised so far, and is appealing directly to some of WA’s big business leaders and entrepreneurs.
“We want to keep this service going and reach many more Ukrainians in need of care and in ways that traditional aid programs cannot provide,” Mr Hicken said.
“We’ve worked so hard to get here, but we really need help, because we’ve run of money and AWS can’t give us anymore, so we’re seeking private or corporate sponsorships –really anyone who can help.
“The people in Ukraine needing help are still there, they haven’t gone away.
“Many of their doctors are going through great hardship as they are unable to practise outside of Ukraine. We have been helping them to carry on practising medicine to support their families, and our payments have been putting food on their tables.”
Mr Hicken said when the project was first getting off the ground many people thought it was a “crazy crackpot idea” and when he started asking for money some people thought it was a scam.
Others wanted to know why an Australian company was involved.
“I’ve even had Ukrainians look me in the eye and ask “why are you helping us?”
“I probably only gave us a 10% chance but now we’re really doing it.”
“We don’t even call it a war – we don’t take sides. It’s all about helping Ukraine.”
ED: for more information on the Ukraine projects go to:
https://gpnow.net/ukrainian-crisiscare/ and https://msf.org.au/
Working in both emergency and aesthetic plastic surgery has given Dr Anh Nguyen balance and insight into the prejudices against the latter type of work.
 By Ara Jansen
By Ara Jansen
A self-described ugly duckling with straight As, Dr Anh Nguyen arrived in Australia by boat in 1979, the eldest daughter of Vietnamese migrants.
Decades later, Anh straddles two sides of plastic surgery with equal amounts of grace. She has 20 years of experience in emergency trauma plastic surgery, reconstructive surgery as well as aesthetic plastic surgery and non-surgical treatments. Anh is also in rare company as only 15% of plastic surgeons are women.

As a child in Melbourne, Anh struggled and fought against cultural stereotypes that wanted her to participate in beauty pageants and simply find a husband. She was a tomboy and a nerd who studied, ending up on a transformational journey, navigating cross-cultural and societal pressures around academic achievement, beauty and the role of women and her own pre-conceived ideas about plastic surgery.
These issues have turned into the passions which have helped drive her personal and professional life.
“I was never interested in aesthetics, I always said I would never do it,” says Anh about her eventual career path. “I thought it was just vain and something beautiful people did to become more beautiful, glamorous people wanting to be more. There must be more important things to do – I truly believed that.
“In Vietnamese culture, women’s appearances were so important, but I didn’t fit into that. I didn’t like that stereotype where girls had to be beautiful and marry well; that
beauty was more important than brains. My mum was always going on about appearances, so I grew up despising the idea of making myself look beautiful because I had more important things to do.”
Anh went to an all-girls public high school in Melbourne, where “everyone knew they wanted to be an astrophysicist”. She didn’t really know what she wanted to do, but was smart enough that medicine was an option, which she eventually chose.
She studied medicine and surgery at the University of Melbourne and surgical training at St Vincent’s Hospital and The Alfred Hospital. It was while doing a residency at the Royal Children’s Hospital and seeing children with cleft palates and other physical issues, she wondered how on earth they were going to be fixed.
“I always thought that plastics was only about aesthetics, but once I realised what went into helping someone like that, that’s when I got on that pathway. I started out training in general surgery, taking out gall bladders and I really loved that too.”
It was her dad who suggested she apply to specialise in plastic surgery. She ended up being the youngest Perth trainee in the discipline at Royal Perth Hospital. Anh moved to Perth in 2006 and the next year did a burns fellowship with Professor Fiona Wood at RPH while on maternity leave. She completed her plastic surgery training in 2010 having worked at Sir Charles Gairdner Hospital, RPH and PMH.

“By then I had done lots of plastic surgery and lots of trauma work and knew this was what I wanted to do. Then a mentor of mine invited me to a fellowship in Melbourne, an aesthetic one. After the first one I was sold. The surgery was technically beautiful and it was also creative, plus the patients were so grateful.
“I’ve come to realise that if you break your hand, it’s expected that a doctor is going to fix it. You don’t go to someone expecting they will give you a new lease on life and leave you feeling full of confidence and more worthy. How wonderful is that?”
That nexus of art, beauty, medicine and science is why Anh changed her own ideas about aesthetic plastic surgery and cosmetic surgery, a field she has successfully worked in alongside her trauma, emergency and reconstructive work. An experience where she played model during an injectables workshop also helped shift her perspective.
“It’s not vanity at all. People who think they are old and ugly, not good enough or something has changed in how they see themselves can do something.”
Alongside her hospital work, Anh owns two ‘medi-spas’ which offer a selection of treatments as well as cosmetic surgery consultations and products.
Active on social media, the contradiction of how Anh felt earlier in her career about aesthetic surgery is not lost on her.
She’s also committed to sharing her experiences as a mentor for the next generation of plastic and cosmetic surgeons, passing along her skills as an educator, researcher,
continued on Page 18

continued from Page 17
entrepreneur and contemporary physician.
She speaks at medical and beauty and aesthetics-focused conferences, including a recent trip to Melbourne where she spoke at a face-lift conference and then in Hawaii where she shared her professional and personal story with business owners and managers.
“I tell young doctors they can be anything they want to be. They will have the freedom and the choices if they do the hard work now and keep going. I love the ability to share that, being on the other side now.”
Anh has been a supervisor of plastic surgery fellows at Fiona Stanley Hospital since 2015 and is a consultant there as well as at Joondalup Health Campus. Being an on-call plastic surgeon and consultant to numerous Perth hospitals means she can be
regularly found doing operations like reattaching severed fingers. This work keeps her earthed and keeps her microsurgery skills sharp.
“I work mostly in a glamorous environment. It grounds me to work on a major emergency, like someone cutting all the tendons in their arm. It fills my cup to be able to help someone with that. But I also like the balance of emergency and trauma work with the other work I do.”
Last month, Anh was an inductee into the 2023 WA Women’s Hall of Fame alongside 20 other inspiring local women, including journalist Victoria Laurie, Senator Dorinda Cox and WACA CEO Christina Matthews. Humble about the honour and suggesting it’s for crusaders and warriors, she’s forgetting her own journey in a male-dominated specialty.
“I am a warrior in terms of trying to change the narrative and the importance of people feeling good about themselves. If you injure your
knee, it’s automatic that you’ll get it fixed. If you’ve injured your body by gaining 100kg, why is it any less worthy to fix?
“It’s just a different way of thinking about this. It’s about teaching and educating women that aesthetic fixes are not a dirty thing to want to do for themselves. Heaven knows we do enough for everyone else.”

She’s not an advocate for everyone having work done but wants to remove the negative stigma for people who do. Most of her patients are women and around 10% are men, who in the main get facelifts. The most common requests for cosmetic procedures are not from beautiful people who feel it will make them more beautiful but from everyday people who have an issue with a part of their body and feel a fix will really help them live a happier life.
Anh has three children and all the pregnancies happened at pivotal
moments in her career. She fell pregnant with her daughter during her initial plastics training. A specialist told her he didn’t think she was taking her training very seriously. She was thrilled to prove him wrong at more than one turn.

“Sure, I could have made my life easier if I hadn’t gotten pregnant at those moments, but life throws you all sorts of curve balls.” She fell pregnant a second time while she was a consultant and the third when she opened her first clinic.
“Between us, we’re all busy,” she says of her family. “I’m very socially active and coordinating time for all of us around the kids’ activities takes work. Weekends are pretty much always family time. I have lots of interests but rarely enough time to indulge them. I like cooking and baking. I know how to sew and I like designing and making clothes.
“What’s important for me at the moment is mindfulness. I meditate and have counselling and work with a psychologist and life coach.
That helps keep me grounded and working on my own wellness. I was overworked and stressed out for a long time, and this has helped give me some balance.”
She agrees with the flight adage of putting your mask on first so you can be fit and healthy enough to help others. During COVID, she and her staff used to have planking competitions to keep their fitness and spirits up.
“My daughter is considering doing surgery, though I would encourage her on any path which makes her happy. There are not many jobs where you can say you are of service, get paid well and it’s interesting and always challenging. There’s also a side of me that says it was so hard, but you have to keep going for the rewards.
“In surgery the statistics say 30% of those who start training are women but only 15% finish. It’s not because women are not good enough. I think it’s because they decide there’s more to life. Getting this far requires sacrifice. No matter what she chooses, I don’t want my daughter to dim her light.”
Our cardiology centres have recently changed their name from GenesisCare Cardiology to Advara HeartCare, following a change of ownership in late 2022. While things may start to look and sound a little different, our number one priority is continuity of care for your patients.
Our cardiologists, teams and locations remain the same, and this will have no impact on patient care.
For more information: advaraheartcare.com/newname-hcp

As Perth prepares to host the World Transplant Games, WA continues to punch above its weight in the use of donor organs.
Cathy O’Leary reportsIn Australia, there are about 1800 people waitlisted for a life-saving transplant. Another 12,000 people are on dialysis who could benefit from a kidney transplant.
They are some of the key statistics that are expected to get some airtime when Perth hosts the 24th World Transplant Games this month, from April 15-21.
It is the world's largest organ donation awareness event, with athletes from 50 countries flocking to WA to compete for gold, silver and bronze –involving people who have received organs such as heart, liver, lung, kidney, pancreas and bone marrow.
First held 1978 in Portsmouth, UK, the games have grown to become a beacon for transplant recipients, their families and supporters, donor families and living donors.
The games have been held on the continents of North America, South America, Africa, Asia and Europe. This will be the third time the event has been held in Australia, after being previously hosted by Sydney in 1997 and the Gold Coast in 2009.
The seven-day program of high-exertion and low-impact sports, along with many social and cultural events, caters to both elite and social athletes and attracts 2500 participants from over 60 nations.
According to Transplant Australia CEO and World Transplant Games Federation president Chris Thomas , the event serves three purposes – firstly to encourage transplant recipients to be as fit as possible, while accommodating their new life with their transplanted organs.

It also enables organisers to promote organ donation and encourage more people across the world to consider organ donation because they get to see the benefits of donation through the lives of the competing recipients.
And thirdly, it is a way to acknowledge the people who made it possible –the doctors, nurses and the all-important donors.
In 2017, Perth woman Wendy Hawks was given only hours to live. This month, five years after her heart transplant, she will compete in the World Transplant Games.
Wendy, now aged 66, suffered heart failure most of her life due to a viral infection. In 2017, her condition became acute, requiring a left ventricular assist device to keep her heart pumping. After six months on the waiting list, her life was saved when she received a heart transplant in 2018.
Wendy will compete in five events – the 3km walk, shotput, long jump, 200m sprint, and badminton. To prepare for the games, she has been training and competing with Masters Athletics WA.
For her, it is an opportunity to celebrate how far she has come and to inspire others on their own transplant journey. She hopes her participation in the games will raise awareness about the importance of organ and tissue donation and inspire others to consider becoming a donor.
Mr Thomas said with more than 1800 Australians now waiting for a transplant, it was crucial to promote the positive message of the lives saved through the gift of life.
“Every Australian can make a difference by registering as a donor. It takes just one minute but has the potential to give someone years of extra life,” he said.
“These games demonstrate what transplant recipients can achieve on the sporting field. Transplant Australia is committed to improving the lives of those waiting and those who have received a transplant.”

The Australian Government through the Commonwealth Department of Health and the Organ and Tissue Authority and the WA State Government are major partners of the games.

Locally, the event is supported by Tourism WA, the Health Department, VenuesWest and the Department of Local Government, Sport and Cultural Industries.
The games will feature 16 different sports including swimming, athletics, tenpin bowling, table tennis and cycling.
Athletes will compete at numerous sporting venues, including HBF Stadium, WA Athletics Stadium, Bendat Basketball Centre, Gold
Netball Centre and Champion Lakes Regatta Centre, with the opening ceremony to take place at Optus Stadium.
A series of related events including cultural activities, donor recognition opportunities and a gala dinner will also showcase Perth's world-class hospitality and tourism offerings on a global stage.
Health Minister Amber-Jade Sanderson said many people who received organ transplants or tissue donations had a congenital or genetic condition, illness or sudden organ failure.
"Fortunately, Australia has one of the best transplant success rates in the world, with research showing the majority of Australians support organ and tissue donation,” she said.
“The World Transplant Games shows the importance of organ and tissue donation and how it can save and transform lives."
ED: For more information visit www.worldtransplantgames.org
To register as donor, visit www.donatelife.gov.au/ register-donor-today

Australia is sleepwalking into a sicker future that will condemn millions of people to live with avoidable disease and disability, according to recent Grattan Institute report.
But it contends that the Albanese government’s promised Australian Centre for Disease Control, or ACDC, could provide a badly-needed wakeup – but only if preventing chronic disease is a core part of its mission.
The Australian Centre for Disease Control (ACDC): Highway to Health report shows that chronic conditions are the biggest killer in Australia, contributing to nine in 10 deaths.
Not surprisingly, the burden is heaviest on the most disadvantaged Australians, who are twice as likely to have two or more chronic conditions.
And the toll will keep growing because many of the causes of chronic disease, such as obesity, are rising dramatically.
What role will WA play on the Highway to Health asks public health expert Adjunct Professor Terry Slevin
So, it looks like 2023 will be a key year in the creation of the Australian Centre for Disease Control. Like the start of any life, evidence tells us that the first year or two are enormously influential on how that life will unfold for future decades. So will be with the ACDC.
The two milestones for the ACDC this year are the Federal Budget, due on May 9, and the legislation to bring the centre into effect. This will need to be completed this year to allow for the Albanese government’s promised start of the agency in “early 2024.”
The budget for the ACDC needs to be in the hundreds, not tens of millions of dollars, and the legislation that creates it needs to ensure it can function effectively long into the future, including through periods when executive government does not prioritise public health.
Everyone agrees that the ACDC cannot be successful if it does not establish strong and effective relationships with the “boots on the ground” level of government, the States. The pandemic showed some important co-operation across governments, but we all know it could have been better.
Better systems to gather, analyse, report and share data; consistent definitions of terms, rapid evidence analyses as new challenges arise and new evidence emerges; and effective and efficient systems like contact tracing, check-in apps could have all been valuable.
WA has long been proud of its record in areas such as tobacco control, and it was the first State to put in place programs such as Live Lighter. The WA government has reconfirmed its commitment to the Sustainable Health Review recommendation to achieve 5% of health spending going to public and preventive health.
Now is an ideal time for the government to articulate how it plans to reach that target, so as to align with, and potentially help lead efforts to establish the Australian Centre for Disease Control in a co-operative and forward-thinking manner.

The October 2022 Budget, the Albanese government’s first, contained a modest line for the ACDC. They committed $3.2 million, largely to facilitate the consultation and planning process. The May Budget allocation will strongly indicate their level of commitment to the new agency. Recognising that the agency will only commence halfway through the 2023/24 financial year, that initial year’s allocation is perhaps less crucial. But the Budget will also allocate estimates for 2024/25 and 2025/26.
There will also be some internal reallocation. Funds otherwise committed in the Department of Health and Aged Care budget will be reallocated to the ACDC as some existing departmental functions are transferred.
It has already been foreshadowed that the National Medical Stockpile will be transferred into the ACDC. This is a reasonable responsibility for the ACDC to hold. Its budget allocation is, I’m told, a security issue and so not publicly available. However, it’s believed to be $50m+ per year.
Naturally, the budget allocation will need to be aligned with the agency’s scope and as that’s not yet publicly announced, there are challenges to estimate how much it will need. Nonetheless, the ACDC is likely to incorporate the roles of the Communicable Diseases Network Australia and Public Health Laboratory Network to plan for and, where necessary, lead responses to infectious disease outbreaks. Along with addressing
the tsunami of chronic disease, the agency’s budget must be substantial.
In addition, working constructively with States and Territories, where substantive public health powers lie, will also require resourcing.
Co-operation with the jurisdictions is far more likely to be effective if funds are available to boost local capacity, while also maximising consistency.
Similarly, if the ACDC is to lead the enactment of the National Preventive Health Strategy to tackle issues such as alcohol, tobacco and obesity, then proper resource allocation is essential. By way of reference, looking at the modest budget of the Australian National Preventive Health Agency when it was last funded by the Rudd/Gillard government and indexing to 2023 –would be an entry point for funding this aspect of the ACDC work.
We have also suggested that the $25 million remnant funds allocated to the Australian National Preventive Health Agency, revealed in the recent October Budget statement, should be reinvested in non-communicable disease prevention by transferring these funds to the new ACDC.
By way of reference point, for previous investment in preventive health we can look at the National Partnership Agreement on Preventive Health signed by the Rudd government with all States and Territories in 2008. A total of $564.7m was allocated from 2009/10 through to 2014/15. The agreement was amended around 2009 and the funding of the agency was reported in 2012 to total $932.7m in an Australian National Audit Office report dated 2012. It was cut short in 2013 by the Abbott government. At its peak there were $218.3m allocated under the agreement in 2012/13.
Like all areas of the economy, we can’t provide high quality public health programs and advice without recruiting, training and developing the next generation of experts and leaders. We have recommended the creation of a National Public Health Officer Training Program built on the NSW
continued on Page 25
Rural Health West and WA Country Health Service would like to take this opportunity to congratulate the winners of the 2023 WA Rural Health Excellence Awards.
Building Healthy Country Communities
Pilbara Palliative Care Service
Delivered by WA Country Health Service in partnership with Bethesda Health Care
Proudly sponsored by Royal Flying Doctor Service –Western Australia
Clinical Leadership
Dr Jonathan Blundell
Proudly sponsored by Australasian College of Health Service Management
GP of the Year
Dr Michael Dewing
Proudly sponsored by Royal Australian College of General Practitioners
Metropolitan-based Bush Champion
Dr Justin Yeung
Proudly sponsored by Australian Medical Association
People’s Choice
Laura Black
Proudly sponsored by Rural Health West Outreach Services
Rising Star
Kyra King
Proudly sponsored by Curtin University
Rural Allied Health Professional of the Year
Sarah Tomlinson
Proudly sponsored by The University of Notre Dame Australia
Rural Nurse/Midwife of the Year
Chantelle Pears
Proudly sponsored by Edith Cowan University –South West
Rural Researcher or Educator
Professor Bronwyn Peirce and Kathryn Fitzgerald
Joint winners
Proudly sponsored by The Rural Clinical School of Western Australia
Specialist of the Year (Non-GP)
Dr Jared Watts
Proudly sponsored by St John of God Bunbury Hospital
WA Country Health Service Intern of the Year 2022
Dr Lucy Irvine
Proudly sponsored by WA Country Health Service
WA Country Health Service
Resident Medical Officer of the Year 2022
Dr Renita Whittle
Proudly sponsored by WA Country Health Service
Chairmans’ Award
Pilbara Palliative Care Service
continued from Page 23
Health model, which we believe can make an enormous contribution at a cost of around $50m a year.
The other key issue of 2023 is the legislation that establishes the ACDC. The centre needs to be able and confident to provide independent, trusted, authoritative, evidence-based advice. It must also be both acknowledged and sustainable, irrespective of any government’s reluctance to hear such advice.
The ACDC must be able to weather the storm of any future government that might be indifferent – or even hostile – to the value of public health advice and expertise.
This suggests that the ACDC should be established as a new statutory body, similar in governance arrangements as entities such as the Australian Commission on Quality and Safety in Healthcare. That commission has an independent, expert governance board rather than an advisory board, with clear independence mechanisms.
The board membership should come from a diversity of disciplines and segments of Australian society and have unassailable public health credentials and expertise. This would create the balance between the need for independence from government, while achieving accountability and jurisdictional buy-in across our federated system.
The new institution’s structure should reflect a hub-and-spoke model, with a properly resourced administrative centre, to coordinate its activities and functions, and enable international collaborations. These should include jurisdictional offices for regional coordination and engagement, in much the same way as the Public Health Agency
of Canada is structured, staffed with funded positions to capacitate national functions.
We’ve been thinking, talking and writing about the ACDC for decades, and a recent push came around the time we published an editorial in Australian and New Zealand Journal of Public Health in September 2021.
Since then, the Albanese government was elected on a platform of introducing an ACDC. The government has designed and run a consultation process and released a consultation paper to which many organisations, including Public Health Association of Australia, have contributed submission – I understand about 140 were made.
According to the AIHW, in the three years leading into the global pandemic, public health spending has ranged between 1.55% and
1.77% of total health spending. No wonder spending on disease management is getting out of control!
In the first year of the global pandemic, with all the PCR testing and contact tracing, and the early purchases of vaccines, that figure moved to 3.7%. Even with a public health crisis that dominated the world, we still do not reach the recommended target of 5% as suggested by the National Preventive Health Strategy. There is still a long way to go.
This year will be pivotal, with ramifications for public health infrastructure for decades to come. Just focusing on services to help the sick of today is important, but not enough. We must focus on fewer people getting sick in the future.
This is genuinely a once-in-alifetime chance to get this right. So, will it be a Highway to Health for Australians or will it be a “Long way to the shop if you want (proper) disease control”?
ED: Adjunct Professor Terry Slevin is CEO of the Public Health Association of Australia.

The ACDC must be able to weather the storm of any future government that might be indifferent – or even hostile.

The advent of gene therapy to treat spinal muscular atrophy is a major milestone with the potential to revolutionise treatment for some rare neurological conditions.
By Eric MartinThe first few weeks of a child’s life are expected to be full of wonder and joy as the family bonds with their newest member, yet, for some parents, the growing realisation that something is not right with their child is the start of a profoundly different journey.
Spinal muscular atrophy (SMA), as the name suggests, is a condition which impacts the development, function, and degeneration of spinal motor neurons. Although it can present in adults, SMA is the most common genetic cause of death in children under the age of two in Australia.
Dr Maina Kava , a paediatric neurologist, clinical lead for neuromuscular program at Perth Children's Hospital and the state clinical lead for mitochondrial research at the Australian Genomics Health Alliance, has been working with children affected by SMA, which has brought newfound hope to the WA families coming to terms with the diagnosis.
“At PCH, we have an excellent setup and an extensive service that provides a multidisciplinary team approach for children affected by any neuromuscular disorder,” she said.
“The landscape of SMA is rapidly changing, with opportunities for ground-breaking treatments evolving rapidly.”
Dr Kava trained at leading institutions around the world, including India, Australia, and Canada, where she completed her neuromuscular and neurometabolic research before returning to Princess Margaret Hospital, making the transition with the rest of the team to PCH in June 2018.

“For me it has been a steep learning curve, seeing my first patient with SMA, extremely floppy and weak, back home in India during my paediatric rotation as an intern, but with no available treatment at that time,” she said.
“Now, years down the track, with every new patient with SMA I see, I can say something more positive, that there is hope for a potential cure, which is so much
more favourable than even just five years ago when there were only the basic comfort measures, along with supportive care and a referral to palliative care.”
People with spinal muscular atrophy have insufficient levels of the survival motor neuron protein essential for the existence and functioning of motor neurons. This protein is encoded by two genes, SMN1 and SMN2, and in children with SMA, the first gene is missing. With only the SMN2 gene present, children with SMA produce a truncated form of the protein, and having fewer copies of the SMN2 gene is associated with earlier onset of disease and more severe symptoms.
“SMA is a remarkably interesting genetic condition, where all children with the disease do not have the same phenotype,” Dr Kava said.
“This means there are significant differences in the way they present. Some children could have completely normal motor functions, and they may not start exhibiting symptoms until late adulthood, or they may be children who are born with a significant neuro-motor deficit and are not able to move their muscles.
“These children require ventilation or respiratory support to help them with their breathing as soon as they are born and, clinically, we used to classify them as a type zero, which meant children who were presenting with symptoms right at birth.”
SMA is classified into four types depending on the age of onset and its impact on motor function:
• Type 1 – onset 0-6 months, life expectancy is less than two years
• Type 2 – onset 6-18 months, life expectancy is 10-40 years
• Type 3 – onset after 18 months, life expectancy into adulthood
• Type 4 – onset after five years, life expectancy into adulthood.
About half of patients who present are babies with type 1 disease, and by the time a child presents with symptoms, they have already lost 90% of their neurons.
“Children with type 1 SMA can present any time between six weeks to six months. They have significant motor dysfunction, and in most cases, they are not able to sit. 80% of these children die before the age of two years,” Dr Kava said.
“Of all the types of SMA we see in our clinic, Type 2 is the most common phenotype. These children present between 6-18 months of age. They may have initially attained some milestones, such as head control, or the ability to sit upright, but they cannot stand or walk.”
“There is an increased risk of early mortality because there is a significant association with spinal deformity and weak bulbar and respiratory function, which eventually leads to death of these beautiful children.”
“Seemingly simple things like swallowing, breathing, and feeding is affected, and eventually leads to poor nutrition and associated
continued on Page 28
About half of patients who present are babies with type 1 disease, and by the time a child presents with symptoms, they have already lost 90% of their neurons.
continued from Page 27
micro-aspiration of food into the lungs, causing chemical pneumonitis and pneumonia, and all kinds of respiratory dysfunction.”
Dr Kava explained that parents are carriers, and in Australia, there is an incidence of about one in 10,000 live births.
“Usually, we expect about three to four small children with SMA each year, but it varies, as some years we have had none and some years we have had many.”
PCH started its Nusinersen drug program in November 2017 and Dr Kava and her team now have five years' experience of treating children with the synthetic antisense oligonucleotide, otherwise known as Spinraza.
Nusinersen enables the SMN2 gene to produce a full length SMN protein and has been shown to improve motor function in several trials with participants aged from 30 days to 15 years. However, as the drug’s terminal half-life in cerebrospinal fluid is just 19-25 weeks, the 12mg dose, which is delivered by lumbar puncture, needs to be regularly readministered.
“Nusinersen is the first treatment approved for all types of SMA and helps in the production of the survival motor neuron protein. Although it needs to be administered intrathecally, it has been proven to be safe,” Dr Kava said.
“In all the clinical trials, and from our own experience, having done more than 200 injections now – we found that children tolerate the procedure very well.”
The next breakthrough to occur, she said, was the advent of an oral medication, Risdiplam, a modifier of pre-mRNA splicing which also enables the production of fulllength SMN proteins, but one which can only be used in SMA patients who have at least two copies of the SMN2 gene.
Risdiplam can cross the bloodbrain barrier and is metabolised by several enzymes including cytochrome P450 (CYP) 3A4, and
the dose is determined by the age and weight of the child. However, even though Risdiplam is easier to administer than Nusinersen, the drug’s effect on pre-mRNA splicing is not confined to the gene coding for SMN, and though no causal link was shown, three infants died from respiratory complications during the FIREFISH trial.
The drug also needs to be administered every day for the rest of the patient’s life.
A year ago, the PBS listed what is currently the most expensive drug on PBS, Onasemnogene Abeparvovec, which is a SMN1 gene therapy given as an intravenous injection along with a viral vector to enable the gene to reach the spinal motor neurons.
“Genetically, it is an extraordinarily complex technique, and currently, the drug is imported from the US. Up until now we needed to send babies interstate to Sydney or Melbourne to access gene therapy, but as of August 2022, we are able to offer gene therapy at PCH.
“Thanks to the support of PCH executives, we are the third site for gene therapy in the country, and we now have a supply agreement in place with the drug company, Novartis.”
The genetically engineered version of the SMN1 gene is now on the PBS and available for children with

SMA under the age of nine months, yet much like Risdiplam, the weight dependent dosage can result in complications.
“We must be mindful that gene therapy, even though it is genetically based, is still a therapy and not a cure. It helps maintain motor function, but it does not take the disease away. The child still has SMA and will continue to need physiotherapy and regular monitoring in the neuromuscular clinic.”
But Dr Kava stressed the importance of now having a positive message that clinicians can give along with a diagnosis.
“Until a few years ago, when we had a child with a diagnosis of SMA, we were giving them a prognosis (depending on the type of SMA they had) that often included saying things like, ‘your child is never going to walk, they are going to be in a wheelchair for the rest of their life, and that their life span will not be great’,” she said.
“These are things which are heartbreaking to share, and it is a devastating, progressive disease. But having a treatment which can just maintain the disease progress is an important thing, such as having a child who has started to walk will hopefully continue to walk once treatment is initiated.
“We want to help them to become as functional as possible because
the most important thing about SMA is that these children have no intellectual problems. They are in the company of adults and therapists and their IQ is often much higher than those of other children.
“They have so many cognitive skills, but unfortunately, the muscle weakness prevents them from doing things. The children are completely aware of everything, they have normal intellectual function, and then they deteriorate right in front of your eyes.
“Just preserving what they have (in terms of movement) makes a substantial difference for them because that enables them to function to their full capacity, to be their best, and that is so satisfying for everyone involved.
“And that is why we advocate for initiating treatment early, which is what led to the newborn screening program.”
Newborn screening for SMA from dried blood spot started in January this year, and it is currently the only condition on the NBS panel which is picked up by genetic testing.
WA is the second state to have implemented the newborn screening, and while the program has already detected SMA in two infants, Dr Kava stressed that GPs were the backbone of the medical system in Australia and had a significant role to play in the detection and management of SMA.
“Even though we have newborn screening, there are still children out in the community who may have type two, type three, or type four SMA, and these children are going to present with symptoms at some stage,” she said.
“We must also be mindful that we have children at the clinic who do not have Medicare support and are managed by their GPs, who play an important role in terms of following up the children for immediate care after starting medications and making sure the family as a unit is well looked after.”

One of the most important tools for GPs was a neuromuscular hotline.
“My aim is to have a zero-wait time for any child suspected of SMA and
if a GP anywhere in WA suspects a child who has hypotonia or absent reflexes could potentially have SMA, they should ring our hotline and contact us,” Dr Kava said.
“We will help assess the child and decide the best course of action. We do involve the GPs in the management, and we endeavour to help guide and support them.”
Dr Kava said that gene therapy had revolutionised the area for many neurodegenerative conditions.
“So much is changing in neuromuscular genetics, and it is a field to watch,” she said.
“It has been such an amazing journey to be able to come from seeing a child with SMA and giving them a diagnosis for this devastating disease, to now, being able to identify this condition even before it starts presenting with symptoms and then prevent them from occurring.
Our sleep & respiratory centres have recently changed their name from GenesisCare Sleep to Advara Sleep & Respiratory Care, following a change of ownership in late 2022.
Our sleep & respiratory physicians, teams and locations remain the same, and this will have no impact on patient care.

Our name has changed, but our high-quality patient-focused care remains the same.
One in three Australians will rely on blood donation at some point in their lifetime. With a shortfall of donors to meet the high demand, it is hoped recent eligibility changes will turn that around.
Despite efforts to minimise the use of blood transfusions in surgery, donor blood is always needed by more than a million patients each year.
Over 33,000 blood donations are needed every week in Australia to meet the clinical demand for blood – that is a requirement of more than 1.7 million donations. In WA, it means more than 3500 blood donations a week.
Dr James Daly, Medical Director of Pathology Services at the Australian Red Cross Blood Service, told Medical Forum there is a critical need for more people to donate blood – and now with recent eligibility changes, more can.

One blood donation can save up to three lives – helping patients with cancer, anaemia, trauma-related injuries, kidney disease, those undergoing surgery, pregnant women and new mothers, and patients with chronic conditions requiring blood transfusions.
“We all know somebody who has needed a transfusion or bloodderived treatment at some point,” he said. “At the moment only one in 30 Australians donate blood, while that’s still half a million active donors, there are many more Australians who would be eligible to donate.”
Donor eligibility rules are based on medical and scientific evidence and are continuously revised.
 By Kathy Skantzos
By Kathy Skantzos
Restrictions for blood donation have changed for people with tattoos and people at risk of being exposed to sexually transmitted diseases such as HIV, for example.
“We’ve recently had some big changes to some of our longstanding deferrals, and finetuning some of the deferrals for COVID,” Dr Daly said.
Bans lifted Notably, the two-decade blood donation ban for anyone who lived in the UK between 1980 and 1996 for six months or more during the mad cow disease outbreak was lifted in July 2022. The ban was a precautionary measure put in place in December 2000 in response to concerns about the risk of human variant Creutzfeldt-Jakob Disease (vCJD).
When the Therapeutic Goods Administration lifted the ban, after Lifeblood’s medical experts worked with the University of New South Wales’ Kirby Institute to research the risk of vCJD in Australia’s blood donor population, the Red Cross has since welcomed an extra 60,000 donations from this group.
The change has been especially well received in WA.
“Up to 17% of our donor attendances have been from that group of previously deferred donors. It’s been more than we anticipated in terms of the uptake of donations from that group,” Dr Daly said.
Restrictions for blood donors with tattoos has also changed, with recent large-scale clinical research showing there have been no infections from their plasma donations.
“Looking at the data from the past two years of plasma donation (when the ban was lifted for those who had a tattoo from a licensed parlour in Australia), there have been no tattoo-related infections identified in 20,000 donors who’ve donated plasma upfront,” Dr Daly said.
Blood components prepared by Lifeblood include red cells, platelets, fresh frozen plasma, cryodepleted plasma and cryoprecipitate. There are a growing number of patients relying on plasma donations for the treatment of cancer, immune disorders, haemophilia, trauma and kidney disease – making plasma donations just as important as other forms of blood donation.
People with new tattoos can donate plasma immediately after getting a new tattoo, however they still needed to wait four months to give blood, red cells or platelets, but Dr Daly said this could also change.
“We do think we could remove that deferral for the fresh components as well, and we’ll be submitting to TGA shortly about that,” he said.
The Red Cross experienced a huge drop in the number of blood donations due to COVID-19, partly due to the time donors had to wait after recovering from the virus. Up until early 2022, blood donors were
required to wait 28 days after being exposed to the virus before being eligible to donate.
Now, with more scientific knowledge about the virus and most of the population having had exposure to it and having been vaccinated, the restriction for donating blood after a COVID case has now been lifted to seven days after recovery.
Dr Daly said that donors are asked to wait three days after a COVID vaccination before donating blood, plasma or platelets.
One of the most contentious deferrals is for sexual activity, including people at a higher risk of exposure to HIV. Sexually active people in groups with a statistically higher risk of HIV infection cannot donate – unless they allow a window where there is no sexual activity.
“Our present policy is that anyone who’s at higher risk of exposure to a new HIV infection must wait three months since their last highrisk sexual activity before they can donate blood,” Dr Daly said.
Australia currently has one of the lowest risks in the world of being infected with HIV through a blood transfusion.
“There was a change in 2021 when we reduced that deferral from 12 months to three months since their last sexual contact. We’re actively considering if we can completely remove that rule for plasma donation, similar to the tattoo deferral,” Dr Daly said.

If this change is approved, Australia will be the first country in the world to implement this plasma pathway.
The National Blood Authority is active in promoting patient blood management, with a series of guidelines reflecting a systematic review of the scientific literature and clinical expert consensus. These cover six different settings –clinical bleeding, perioperative, medical, critical care, obstetrics and maternity, neonatal and paediatrics.
continued on Page 33

Eligible HBF members* can now access this support program which reflects the latest evidence in osteoarthritis research, delivered and supported by trained physiotherapists.
Fully covered for eligible HBF members*
Eligible members can access the program at no additional cost when delivered by a participating Life Ready clinic.
Proven 33% reduction in pain intensity on completion of the program1
3 months after the program, participants experienced an average pain reduction of 33%. There was also an average improvement in joint-related quality of life of 31% for knee participants, with 47% of these participants also reporting a reduction in use of pain relief medication.
Applied to everyday activities – enhancing success
Participants are provided education sessions and given exercises that are suitable and practical for everyday application.
Group sessions delivered by physiotherapists
6 weeks of exercise sessions, education classes and follow up to help patients manage symptoms and develop long term habits.
Aligned to national and international clinical guidelines for osteoarthritis treatment
For more ways HBF can support your patients with a range of health programs visit hbf.com.au/health programs
continued from Page 31
There has been a shift towards defining the most appropriate use of blood products to ensure they are used only in situations where clinicians know patients are going to benefit from them, which includes the correct use of blood transfusions.
“It is important for us to recognise that blood is a precious and limited therapeutic product, donated by the goodwill of blood donors and we should respect that, use it appropriately and make sure we don’t waste it and use it for patients who need it,” Dr Daly said.
“Taking that principal along with the emerging evidence that transfusion isn’t always in the best interest of patients, this movement of patient blood management has emerged.”
The landmark TRICC study in 1999 is one of the earliest examples that supports the use of a restrictive transfusion strategy for ICU patients, targeting haemoglobin of 70 g/L.
“We’ve had some good clinical trials that show transfusion may not improve patient outcomes and may in fact be detrimental,” Dr Daly said.
“Rather than transfusing patients when haemoglobin dropped to 90 g/L, they compared that with waiting a bit longer until haemoglobin dropped to 70 g/L and there was no difference in outcomes. There were no benefits from transfusing patients more liberally – in fact restrictive transfusion of patients was probably more beneficial.”
Since then, many other studies have looked at restrictive transfusion practices with red cells and with platelets to define when it is appropriate to give blood.

“The aim is to improve patient outcomes by optimising and conserving their own blood –minimising blood loss, avoiding unnecessary transfusions by using blood products and nonblood alternatives to treatments appropriately and based on evidence that patients are going to benefit from it,” Dr Daly said.
Dr Daly said GPs played a critical role in identifying anaemia or iron deficiency in patients. This was particularly important for avoiding adverse outcomes for patients undergoing elective surgery where there was a potential risk of blood loss and an increased chance of blood transfusion, as outlined in the National Blood Authority’s perioperative patient blood management guide.
“GPs preparing their patients for elective surgery also need to flag with the surgical team if their patients are on medications that might increase their risk of bleeding, such as anticoagulants or anti-platelet medications, and more broadly if patients have antibodies to particular blood groups or if they have a rare blood type or special transfusion requirements,” Dr Daly said.
The state-wide antibody register, which is unique to WA, enables any patient who has had a red-cell antibody identified in any labs to have this information listed on the register, with their consent.
There are some medical conditions and other exclusions that restrict patients’ eligibility for blood donation – but common medical conditions and medications such as antihypertensive medications are not necessarily exclusions.
People with type 1 diabetes, for example, require the approval of their treating doctor or a medical officer to give blood, on the proviso
that their blood sugar levels are well controlled and they have no active complications such as eye, heart, blood vessel or kidney problems.
“We have many donor eligibility rules, which are designed to help donors’ wellbeing as well as that of the recipient,” Dr Daly explained. People carrying in-demand blood, such as cases of genetic haemochromatosis, or iron overload, should be encouraged to become blood donors if they are eligible. Giving blood helps these donors offload some of their iron, while their iron-rich blood is useful for patients with anaemia.
Lifeblood is eager to identify donors who have developed an antibody to the RhD blood group, known as anti-D.
“We need those donors to make a very special product called RhD immunoglobulin – used for pregnant women who are D-negative to prevent their babies being affected by haemolytic disease of the newborn, or erythroblastosis fetalis” Dr Daly said.
“We are very keen for donors who have anti-D to contact Lifeblood,” Dr Daly said.
With a strong demand for blood donation, Dr Daly encourages doctors to refer patients between 18 and 75 to Lifeblood to find out if they’re eligible to donate blood.
“The demand is always there,” he says.


Cancer outcomes in Australia are among the best in the world, but these outcomes are not experienced equally by all Australians. The issue of navigation in cancer care has been topical among patient communities and clinicians for some time.
It’s time to initiate a canceragnostic model to test the potential of a unified approach to cancer care navigation.
All.Can Australia is part of global organisation, All.Can International, which was established to improve patient outcomes throughout the entire cancer continuum, by driving better patient care through improved efficiencies based on the principles of value-based health care.
Its approach is to mobilise people with cancer, healthcare professionals, industry partners and other key stakeholders across health system to enable the collaboration that is required to implement solutions that will lead to meaningful change.
Across Australia, this is being done by representatives from cancer organisations, the biopharmaceutical industry, university faculties, consumer advocates and pharmacists.
All.Can Australia has been advocating for a cancer-agnostic approach to cancer navigation since 2021, when the organisation released Australia’s first pancancer care navigation model. The proposal is to use one carefully designed model to transform cancer care delivery for all patients, regardless of cancer type, cancer stage, patient demographic or location.
As clinicians who understand the impact of fragmented cancer care, we believe a deliberate, integrated
approach to navigation would make our complex health system easier for patients to navigate and remove some of the biggest pain points they experience in improving or maintaining their quality of life.
Recent insights arising from a recent webinar organised by All. Cam Australia confirmed that we need to work together to overcome the currently siloed nature of cancer care. It is not just about developing new approaches and resources. It is about a collective approach to the delivery of cancer care support, better connecting existing services to improve the disparities in how patients access the resources already available, including dedicated cancer-specific nurses such as breast care nurses.
The current reality is that clinicians are the ones assisting with care navigation and they are not necessarily best resourced and often too time-poor to assist. This leaves patients to their own resources often based on the internet.
Guiding patients through the health system when they are at their most vulnerable can be done better, more efficiently and effectively by trained people and technology.
To make pan-cancer navigation a reality, there will need to be adequate human resourcing, education, leadership and mentoring of appropriately trained healthcare professionals, as well as suitable evaluation processes in order to make informed decisions.
The benefits of a comprehensive cancer care navigation program are likely to be substantial, including improved outcomes for healthcare consumers as well as a more efficient healthcare system.
Positive impacts include reducing emergency department visits, more efficient inpatient services,
reduction in duplication of services and, overall, decreased time traversing the cancer treatment pathway. Cancer navigation will improve the healthcare consumer experience by reducing stress and anxiety, reducing barriers to investigations, diagnosis and treatment, and improving continuity of care.
Fortunately, the necessary modelling and cost benefits analyses have already been considered. We estimate that a pan-cancer navigation model in Tasmania run through the Primary Health Network, would generate $2.2 million in net savings per annum, or $724 per patient, delivering a 39% return on required investment (based on the budgeted service cost to fund the pilot for five years). At a peak level of operation, the pilot could provide support to 4913 cancer patients annually.
Increased efficiency in cancer care is about breaking down organisational barriers and silos. It is about optimising the use of existing services already in place at a national, regional or local level, and how these services can be better coordinated and connected. A unified approach to cancer navigation can help us become a country with not just the best cancer outcomes but the most efficient cancer care system in the world.
ED: Prof Zalcberg is board director of All. Can Australia and a consultant medical oncologist at Alfred Health and Head of the Cancer Research Program at Monash University’s School of Public and Clin. A/ Prof Nott is a medical oncologist at Icon Cancer Centre.


Dermatologist-led cosmetic medicine service
Doctor-delivered treatments, for GP-referred patients

Laser modalities for
Rosacea
Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
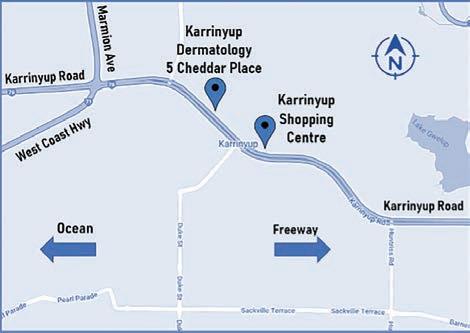
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.
Hair loss, nausea, vomiting, fatigue and headaches – these are just some of the side effects cancer patients fear when faced with the prospect of chemotherapy. But what if there were another way?
With recent funding granted by the Ovarian Cancer Research Foundation, our team is testing a new treatment for ovarian cancer that promises fewer side effects. It does this by relying on the body’s own immune system to fight the tumour, instead of having to endure the wrecking ball effects that traditional chemotherapy has on the rest of the body.
Although current immune therapies have had great success in the treatment of cancers such as melanoma, it is much less effective in treating ovarian cancer.
My team at Mater Research and the University of Queensland will test whether combining a low, sub-clinical dose of two drugs –not previously used together – can help the patient’s immune system recognise and kill the cancer cells with minimal side effects.

We are using an existing chemotherapy drug, hydroxyurea, combined with newer inhibitors of checkpoint kinase 1, which plays an important role in regulating the body’s response to DNA damage.
I liken the effects of this combination to a phenomenon you might see in any Australian shed when using the epoxy resin glue Araldite. The individual components are ineffective, but the combination comes together in just the right way – becoming a great adhesive.
Our combination already shows promising results in animal studies for ovarian cancer with it not only blocking tumour growth, but the immune system appears to be responding to the tumour. Our idea is to use this combination to kill the
tumour, treating the acute effects of the disease, and at the same time enhance the immune response to the tumour, essentially vaccinating the patient against their own cancer and improving effectiveness to achieve remission and reducing the chance of relapse.
The OCRF grant of $500,486 will be dedicated to validating and extending our findings. It is focused on getting a more detailed understanding of the immune responses triggered by the treatment with the aim of identifying specific immune targets to enhance and extend this antitumour response.
If successful, we will see whether this combination, plus the specific form of immunotherapy identified in our studies promotes a strong immune response in patients with high-grade, serious ovarian cancer, and determine whether such a response could improve long-term survival.
New treatments are vital to reduce ovarian cancer deaths. While most patients with high-grade, serous ovarian cancer respond to standard chemotherapy, most of them will fail within a couple of years due to the cancer becoming resistant to available treatments when they experience recurrence.
Some patients will benefit from PARP inhibitors, but even those
benefits can be short-lived. This means that there’s a lot of ovarian cancer patients who don’t have a viable alternative. Unlike chemotherapy, this immunemodulating therapy would leave patients with their immune system intact and also reduce the side effects that are a consequence of normal tissue toxicities.
My own wife underwent chemotherapy, which gave me a front row seat to its toxic side effects. This experience tells me we have do better. If nothing else, if it’s possible to simply remove the distress someone has to endure in order to just be treated — that would be a win.
I’ve seen women cut down in the prime of their lives after their ovarian cancer was sadly caught too late. So, working with groups like OCRF really does help researchers in the sector, particularly by meeting the people who are supporting us. It is a good reminder of why we do what we do.
It’s not an academic pursuit. It’s about changing outcomes for people.




There is a reasonable body of research showing that having time in nature, be it a park, bushland or even the beach, is good for our physical and mental health. On a small scale, being in the garden can also be soothing.
While not being the world’s most accomplished gardener, I do find that it is both relaxing and satisfying to potter around the garden planting seeds and watching them grow, and flowers bloom.
We don’t necessarily want all seeds to grow fully, as gardens can be overrun by weeds if these are not, to use the pun, “weeded out”. There is a process to support what we want while being aware of what we don’t. Ignoring the latter won’t make it go away.
Where am I going with this?
A study published last month shows that the seeds for an increase in cardiovascular disease was planted in 2020. “Estimated consumption in the first half of 2020 was significantly higher (~30%) than the previous period. Sales of NRT products…in the first half of the year (2020) were consistently lower than in the second half.”
The authors conclude that increased smoking rates may have been due to people managing higher stress from loneliness due to lockdowns and also that working from home allowed greater capacity to smoke.
The effects of this unwanted seeding will not be seen straight away and could play out over the next few decades. Thus, we will not have a daily update from politicians.
On the plus side, deaths from cardiovascular disease have fallen considerably since the start of the century. AIHW data shows the rates of death per hundred thousand population has fallen by nearly two thirds in those older than 55. This is a pretty good achievement and one that is worth celebrating while simultaneously encouraging us to continue to seek to further reduce the prevalence.
Let us also hope that even though the downward trend may slow that the long-term effects of the last few years, it does not reverse it.
To return to where we started, American researchers have found that people who garden experience many health benefits, including easing of stress and anxiety and a lowering of the risk for various illnesses. “Those who garden tend to be a healthier weight, exercise more, and eat more fibrous fruits and vegetables, which reduces risk for cancer and improves heart health”.
Sometimes looking after our health is simpler than we think.
Increased smoking rates may have been due to people managing higher stress from loneliness due to lockdowns and also that working from home allowed greater capacity to smoke.

Patients can have many questions about CT scans and may turn to Google for answers. While individual circumstances differ, general information can be very useful. The first question is often: How much radiation does a CT scan give?

CT scans deliver a small dose of radiation. While this dose is often more than a simple X-ray it is in fact similar to one year’s worth of radiation you receive passively from nature such as from the cosmos, the earth and foodstuffs.
Can CT scan radiation cause cancer?
= people who get cancer because of the CT scan
= people who do get cancer but not from the CT scan
(anonymised) patient radiation dose records to a government agency (ARPANSA) to make sure

they are appropriate. Technicians who conduct the scan) are also educated in these matters.
“Low Dose CT” usually refers to a type of scan that is appropriate for specific purposes only. Radiologists and radiographers are well versed in the appropriate use of low dose CT.
How many CT scans can I have before I am at risk?
Doctors are mindful of how many CT scans you have had in your life and once that gets up to 10 or so they may be more cautious. If you have an illness that is likely to be significantly life-shortening (such as is the case for some cancers) or immediately life-threatening (such as major trauma, blood clots, heart attack or serious infection) the number of CT scans is usually of lesser concern.
Not that we know of. No hereditary effects have been found in studies of the children or grandchildren of the atomic bomb survivors.
Can I have a scan while I’m pregnant or breast feeding?
It is safe to breast feed after having a CT scan as the radiation does not enter or affect breast milk. If
A CT scan is equivalent to about one year’s worth of background radiation.
Dosage of radiation is minimised and individualised.

Any investigation carries risks and benefits which must be weighed up.
the patient is pregnant, there is a theoretical small risk to the fetus and this will be taken into account by the referring doctor and the radiologist and also discussed with you before the scan.
Can CT radiation come out of my body and endanger others?
No. You will not become radioactive or pose any risk to others. This is apart from when a CT scan is combined with a PET (nuclear) scan – in such case you will emit radiation for a short period of time and will be informed how to manage this at the scan appointment.
Is there a different scan I can have instead?
Each imaging test, whether MRI, ultrasound, nuclear medicine, or plain X-rays, has strengths and weaknesses for each medical condition. The radiologist has accepted the referral from a doctor on the basis that CT is the best test for you. In cases where it is a ‘close call’ between tests, the radiologist will discuss which way to go with your doctor beforehand. You can ask the radiographer or radiologist about the choice of scan when you arrive at the imaging clinic.
Author competing interests – nil
Researchers at Edith Cowan University are running a survey to gauge awareness of national exercise in cancer care guidelines and how they are used in clinical practice.
It also aims to identify barriers that discourage exercise guidelines being translated into standard care for cancer survivors.
The research is open to any health professional (other than a physiotherapist or exercise physiologist) involved in the care of people with cancer in Australia.
Over the past two decades, strong evidence has emerged to support the role of exercise as an important co-therapy for people with cancer.
Clincical Oncology Society of Australia guidelines ask health professionals involved in the care of people with cancer to discuss the role of exercise in their recovery; advise patients to follow exercise guidelines; and to refer patients to a specialist allied health professional such as an accredited exercise physiologist or physiotherapist with experience in cancer care.
For more information about the project email chief investigator Dr Jack Dalla Via at j.dallavia@ecu.edu.au

To complete the survey go to https://eaecu.au1.qualtrics.com/jfe/form/SV_3qsHJMsYb3hpM7s
By Mr Peter Ammon Foot Ankle & Knee Surgery

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Major advances in diabetes care have dramatically improved health outcomes for people living with Type 1 diabetes (T1D). However, cardiovascular disease (CVD) remains the leading cause of death in people living with T1D.
CVD mortality and hospitalised CVD events are 20-30-fold and eightfold higher (respectively) compared to age-matched populations. Physical activity (PA) is a mainstay management strategy for people living with T1D owing to its benefits to dyslipidaemia, endothelial function and insulin resistance, all contributing factors to cardiovascular risk in this population.
Although meeting PA recommendations can be challenging for everyone, people living with T1D appear to experience even greater difficulties, as evidenced by higher rates of insufficient activity. Studies have shown 65% to 82% of T1D study participants did not meet PA recommendations, compared with 48% to 61% in the general population.
A recent systematic scoping review examined barriers to and facilitators of PA in adults living with T1D and identified hypoglycaemia and fear of hypoglycaemia as the most reported barriers.
Successful, safe participation in PA requires advanced knowledge, self-management skills and selfefficacy from the person living with the condition. Without careful and complex adjustment of insulin and or carbohydrate in response to activity type, intensity, and duration, dramatic fluctuations in blood glucose can occur.
Most people living with T1D will agree, hypoglycaemia is at best unpleasant and can be embarrassing. Recurrent and severe episodes of hypoglycaemia can also precipitate cardiovascular events in those who are high cardiovascular risk. To avoid these unpleasant consequences, people with T1D may choose to avoid factors which precipitate it, including PA.
Physical activity (PA) is inversely associated with incident CVD in those living with T1D. Specific barriers to PA in the T1D population include hypoglycaemia and fear of hypoglycaemia
A structured, theory-driven approach to diabetes selfmanagement is required to adequately address unique diabetes-specific barriers.
Existing health promotion initiatives and general discussions about increasing PA, may not be suitable for this population who experience unique barriers to activity. Even if doing some PA, many living with T1D feel restricted in what they can do and may not pursue their PA goals, often because changing their routine precipitates variation in their once predictable glucose levels.
Unfortunately, research has shown that people living with T1D do not always feel supported by their diabetes health professionals to navigate this complex area of diabetes self-management. Some studies even suggest that activity is discouraged by some health professionals.
We know that health professionals generally experience low confidence, knowledge, and clinical skills in this area and often do not have time during a consult to broach such a complex topic of management.
Despite these challenges, a consistent and supportive approach towards PA and diabetes self-management is paramount for this population who are already at significantly increased cardiovascular risk.
In 2017, Michael Riddell and colleagues published a consensus statement on exercise management for T1D in an effort to improve and standardise advice given by diabetes health professionals. Although this guidance is critical in setting foundations for consistent,
evidence-informed education in this area, a gap remains in facilitating the application of these evidencebased recommendations to reduce barriers to PA for this population.
In partnership with local researchers, Diabetes WA piloted a theory-driven structured selfmanagement program designed to address diabetes-specific barriers to PA. Results from this pilot randomised controlled trial suggest and reaffirm that providing education on blood glucose management for PA to adults living with T1D is challenging owing to complex diabetes-specific barriers to PA. Health professionals need to consider these diabetes-specific barriers before using theorydriven approaches to PA behaviour change.
Such interactions should focus on improving self-efficacy through mastery experience, i.e. learning from one’s own experiences and guided trial and error. Credentialled diabetes educators, particularly of dietetic or exercise physiology backgrounds, are uniquely placed and skilled in this area to provide education grounded in behaviour change theory that encourage psychosocial concepts such as self-efficacy and self-determined motivation.
The use of a skilled multidisciplinary team will provide the continuity and specialised support required to address the unique barriers to PA faced by our type 1 community.
Although the findings are specific to those living with T1D, we postulate some of the issues discussed are also experienced by those living with type 2 diabetes who are insulin requiring. We continue to endeavor to understand the challenging barriers to PA faced by all those living with diabetes and provide evidence-informed structured education to support our community.
Author competing interests – the author was involved in research described

An accurate assessment of respiratory muscle strength is essential when diagnosing respiratory diseases and studying respiratory function in individuals with chronic conditions. Assessment of respiratory muscle strength involves examination of maximum inspiratory and expiratory pressure using a pressure manometer. This measuring method is non-invasive, simple, and well tolerated.
Despite widespread utilisation of this technique, there is little evidence to guide clinicians and respiratory scientists on the best methods to obtain accurate and reliable respiratory muscle strength values. This gap in the literature was in focus for us and colleagues who reviewed the reproducibility of respiratory muscle strength examination procedures.
Studies have identified several factors affecting the reproducibility in the assessment of maximum inspiratory and expiratory pressure. For example, test results vary depending on the tested individual’s ability to coordinate respiratory manoeuvres and learning effects. Therefore, it is possible to obtain higher pressure values after repeated efforts and testing sessions.
Improvements in muscle strength can also be attributed to enhanced neural drive to respiratory muscles after repeated muscle contractions. Studies have also detected differences in the reproducibility of the manoeuvres whether the inspiratory effort is performed from residual volume or functional residual capacity, using a flanged or rounded (not flanged) mouthpiece, or whether the inspiratory effort is performed in the mouth or nose.
Clinicians should consider other physiological factors affecting the reproducibility of the maximum inspiratory pressure manoeuvre. For example, in individuals with obstructive lung diseases, repeated inspiratory efforts may induce
Little evidence exists to guide clinicians and respiratory scientists on the best methods to obtain accurate and reliable respiratory muscle strength values

Most studies reviewed repeat testing sessions two and up to four times in different days to enhance the reliability of these values Inspiratory muscles warm-up protocols are more effective than performing a single or repeated testing sessions of maximum respiratory pressure.
dynamic hyperinflation of the lungs. At higher lung volumes, inspiratory muscles are less efficient to produce negative pressure reducing the repeatability of the inspiratory manoeuvre.
Similarly, during repeated testing, individuals may fail in identifying the initial lung volume to start the effort. Higher efforts may be explained by individuals initiating the effort from subsequent lower lung volumes and the increased elastic recoil of the chest will contribute to generate more pressure. Therefore, clinicians should consider the lung volumes
at which the respiratory effort is initiated.
Another relevant factor is that most studies reporting reliability of maximum respiratory pressure use a pressure threshold device that induces a quasi-static contraction of respiratory muscles.
On the contrary, a small number of studies have used flow resistance loading devices that induce a dynamic contraction. This different muscle contraction pattern may have an additional effect in the coordination and learning effect of the inspiratory effort. A standardised testing protocol for measuring maximum respiratory pressure is lacking
Furthermore, non-accurate baseline values before the commencement of a respiratory muscle training program have implications in the validity of the intervention. For example, if the results of a single testing session or submaximal efforts are used to design a respiratory muscle training program, it is possible that the improvements in respiratory muscle strength are overestimated. Part of the changes after training can be attributed to higher efforts, motivation, and improved coordination and neural drive.
The recently conducted examination of the literature revealed three methodologies to enhance the reliability of respiratory muscle strength values:
1) In a small number of studies participants were asked to
perform up to 20 inspiratory efforts in one testing session.
2) Another small number of studies have included a warm-up protocol of inspiratory muscles before testing.
3) Most of the studies have


Cardiovascular disease (CVD) is the leading cause of death in Australia, with one person dying of CVD every 13 minutes. Those surviving a heart attack or stroke usually face long-term disabilities.
CVD risk factors are wellestablished and include an unhealthy diet, sedentary lifestyle, obesity, smoking and excessive alcohol consumption. A diet lacking in vegetables, fruits, whole grains and legumes while high in saturated fats, added sugars, and salt, can increase the risk of CVD.
Emerging evidence also shows that prolonged exposure to physiological stress increases the risk of CVD. Additionally, CVD itself, is a risk factor for mental health
Cardiovascular disease (CVD) is the number one cause of death
Poor diet is one of the leading risk factors for CVD
Vegetables are key to a hearthealthy diet.
repeated the testing session two and up to four times in different days.
Analysis of these methodologies showed that inspiratory muscle warm-up protocols produce greater increases in maximum inspiratory pressure values compared with performing single or repeated measures of respiratory pressure in different testing sessions.

A warm-up protocol consists of performing two sets of 30 inspiratory efforts between 30% and 80% of the maximum inspiratory pressure measured. Studies in healthy individuals using a load of 40% of the baseline inspiratory pressure have shown the largest effect in increasing maximum inspiratory pressure. However, warm-up protocols have not been tested in expiratory muscles and in clinical populations. Similar results are reasonable to expect but further research is needed to verify these hypotheses.
Author competing interests – nil
conditions, such as depression and anxiety, and vice-versa. Much more needs to be done to improve these lifestyle risk factors to reduce CVD burden.
Healthy eating
Lifestyle factors are modifiable. Improving diet can prevent progression and reduce CVD risk.
The National Heart Foundation of Australia recommends plant foods to make up the most of an individual’s diet including lots of vegetables, fruit, wholegrains, and legumes (chickpeas, beans, and lentils). Fish and seafood can be included with smaller servings of other animal-based products, such as milk, cheese, yoghurt, eggs, poultry, and lean meat.
This heart-healthy dietary pattern is high in fibre, vitamins, minerals and other protective plant chemicals, and low in saturated fat, added sugars and salt. These are all recommendations that will improve several CVD risk factors including
continued on Page 46

Vascular leg pain can occur at rest, following exertion or both.
Vascular claudicant pain is described as fatigue, discomfort or cramping of the muscles of the lower limbs, consistently induced by exercise and consistently relieved by rest. It does not occur at rest and is not positional.
The pain mostly affects the calf muscles but can affect the thigh, buttock and foot muscles depending on the location of the flow-limiting lesion. Flow limitation is commonly due to atherosclerosis, but rarer causes include popliteal artery entrapment syndrome, popliteal adventitial cystic disease, dissection (often associated with trauma or vessel fragility syndrome), fibromuscular dysplasia and arteritis.
Severity is described by the distance walked before symptom onset and inability to walk further. Lifestyle-limiting claudication is defined by the patient rather than any test. In a relatively young fit patient, a claudication distance of 500m may be very limiting, while an elderly patient with airways
Key messages
Vascular leg pain can be due to ischaemic rest pain or claudication
Initial investigations should be non-invasive; functional and anatomical
Risk factor modification and best medical therapy are critical, together with exercise in claudicants.
disease may not feel limited by a claudication distance of 100m.
Vascular claudication due to atherosclerosis is usually associated with smoking, diabetes, dyslipidaemia, and hypertension. Its incidence increases with age (rare <50yrs) and is often associated with occlusive disease in other territories such as the cardiovascular and cerebrovascular beds. Hence intermittent claudication is often called life rather than limbthreatening, as heart attack and stroke are more common than lower limb amputation.
continued from Page 45
blood pressure, cholesterol, weight, and diabetes risk.
Studies have consistently found that higher intakes of vegetables and fruit can lead to a 20% lower risk of CVD – that is a 5% lower risk for each additional serving consumed.
However, less than half (~45%) of Australian adults meet the recommended two servings of fruit a day (300g) and less than one in 13 consume the recommended 5-6 servings of vegetables every day (375-450g).
Clearly, more work needs to be done to increase vegetable consumption among the population.
Focusing on simple, achievable, and targeted goals such as increasing vegetable intake by as little as 1-2 servings every day of specific vegetables may be the key to getting people to eat more.
Not all vegetables are created equal. Specific types of vegetables, containing differing levels of vitamins, minerals and other plant chemicals, benefit cardiovascular health. For example, higher intakes of cruciferous vegetables (e.g.
Mimics of vascular claudication include musculoskeletal (osteoarthritis, soft tissue inflammation, complicated Baker’s cyst), neurological (spinal stenosis or radiculopathy) or venous (venoocclusive or venous incompetence) causes or compartment syndrome.
Vascular ischaemic rest pain is a serious life and limb threat requiring urgent investigation and management. This burning pain commonly affects the forefoot and toes when the leg is elevated in the bed at night and may be relieved by dependency. Rest pain or tissue loss is considered chronic limb threatening ischaemia (CLTI). Mimics of vascular ischaemic rest pain include diabetic neuropathy and complex regional pain syndrome. On assessment, pulses may be absent and skin changes evident in CLTI but these are often normal in claudicants. Although ankle brachial indices (ABIs) and toe pressures (TPs) at rest are useful for evaluating CLTI, they are not generally useful for evaluating vascular claudication being normal in many cases.
The most useful initial investigation
broccoli, kale, cabbage, Brussels sprouts, cauliflower) have been consistently shown to be associated with a lower risk of CVD in large population studies around the world. Cruciferous vegetables are rich in many vital nutrients, but also other protective plant chemicals that fight against oxidative stress and low-grade inflammation.
These protective plant chemicals are vital for those who are at an increased risk of CVD and have poor blood vessel health (e.g. those with high blood pressure, unhealthy blood cholesterol levels, diabetes, obesity, and/or that smoke).
to evaluate or exclude vascular claudication is a non-invasive Exercise Ankle Brachial Index Treadmill study. If ABIs are not calculable due to calf vessel incompressibility, TPs and toe brachial indices (TBIs) can be used. Even if these are not able to be calculated, documenting a patient’s limitation on a supervised treadmill study, routinely performed in most vascular ultrasound laboratories, allows diagnosis to be confirmed and graded.


Following this a non-invasive duplex study can determine the likely location, type and severity of flow-limiting lesion/s and exclude aneurysmal change and evaluate access should intervention be required. CTA or MRA should be reserved for pre-intervention planning, and angiography reserved for intervention.
Once a diagnosis of lifestyle limiting vascular claudication is made, the
information needs to be processed in the context of the patient’s disability and the impact upon their quality of life, balanced against the natural history of the disease, procedural risks, and durability of any intervention.
The first step, and most critical lifesaving intervention in symptomatic peripheral vascular disease (PVD), is risk factor modification and optimal medical therapy which includes assistance with smoking cessation, control of blood pressure, blood sugar, lipids, advice on diet, weight control, regular exercise and antiplatelet therapy (aspirin or clopidogrel).
CLTI requires immediate referral for treatment. However, in the setting of vascular claudication, we may not immediately treat a symptomatic lesion, focusing initially on vascular risk factor modification, optimal medial therapy to prevent disease progression, and exercise to increase
claudication distance and avoid intervention. This may also prevent heart attack or stroke.
An urgent indication for intervention is the small minority of patients who may progress to CLTI. If after six months, vascular claudication is lifestyle limiting and not improving, intervention may be warranted.
Endovascular treatment is usually preferred as it is minimally invasive. Performed percutaneously under local anaesthetic with sedation as a day case or overnight stay, it provides instant symptom resolution but is less durable (higher risk of restenosis and acute occlusion) compared to open surgery, which requires a suitable venous conduit and comes with increased morbidity and mortality.
If there is clinical suspicion of rest pain or lifestyle limiting vascular claudication, early referral to a vascular surgeon should be considered for clinical assessment, non-invasive investigation and management. Intervention in CLTI is always urgently required to save life and limb.
If, how and when to intervene in claudication is a complex decision made with a well-informed patient, understanding that often after instituting optimal medical therapy, risk factor control and regular exercise, no intervention may be the best choice.
Author competing interests – nil
Higher intakes of leafy green vegetables (e.g. spinach, lettuce, rocket) have also been linked to a lower incidence of CVD. Eating just one cup of raw leafy green vegetables (or 1/2 cup cooked) is associated with a substantial lower risk of CVD. Leafy green vegetables are naturally rich in nitrates, which have cardioprotective effects via the release of nitric oxide.
Increasing cruciferous and leafy green vegetables and adhering to a diet that aligns with the Heart Foundation recommendations will attenuate excess damage to blood vessels and improve overall health and wellbeing.
Communicating
General practitioners and other health professionals play a vital role in reinforcing heart-healthy
dietary recommendations to improve awareness and the substantial burden CVD has on our communities.

Reinforcing the importance of vegetables for heart health, particularly cruciferous and leafy green vegetables, is key to protecting the hearts of our
population. Simple advice such as “target 5 serves of vegetables per day and make sure at least one of those serves is cruciferous and another is leafy green vegetables” will have a large impact.
ED: Dr Blekkenhorst and Dr RadavelliBagatini are post-doctoral researchers at ECU

Syphilis rates are rising in Western Australia. Of particular concern, rates have been rising in women of reproductive age, with an associated re-emergence of congenital syphilis.
In metropolitan Perth, the period 2015-2021 saw an 18-fold increase in diagnoses of infectious syphilis among women of reproductive age. Currently, infections in women of reproductive age make up almost a quarter of all infectious syphilis notifications in Perth, and almost half of infectious syphilis notifications in regional WA.
To address the threat of congenital syphilis, routine syphilis screening for all pregnant women in WA is now recommended at a minimum three times in pregnancy: at the initial visit, with other blood tests at 28 weeks, and at 36 weeks or birth (whichever occurs earlier). Pregnant women living in the Kimberley, Pilbara and Goldfields should be additionally screened at birth and six weeks post-partum. Any woman who has a change in sexual partner or other feature on history or examination that is concerning for syphilis should be additionally tested.
Syphilis is known as the ‘Great Masquerader’ or ‘Great Mimicker’. It can present with a wide range of symptoms or be asymptomatic. Clinicians are therefore encouraged to screen widely for syphilis, and frequently in groups experiencing higher rates of syphilis, which include:
• Aboriginal and Torres Strait Islander people
• People experiencing homelessness or unstable accommodation
• People who use methamphetamine or inject drugs
• Men who have sex with men
• People from a culturally and linguistically diverse background Syphilis testing can be done by serology for syphilis antibodies and swab of an ulcer or skin lesion for
Key messages
Screen widely for syphilis and at least three times during pregnancy
Treatment is with IM benzathine penicillin
Contact tracing is important to reduce spread and risk of re-infection.
syphilis PCR – this can be important to secure the diagnosis in very early infection, as PCR may be positive before seroconversion.
The treatment for syphilis is benzathine benzylpenicillin, given by intramuscular injection. This is a long-acting form of penicillin that is different to more commonly used forms of penicillin. It may be ordered through the Prescriber Bag but is not readily available at community pharmacies, therefore clinicians are encouraged to keep it in stock to avoid delays to treatment.
The dose for infectious syphilis is 2.4 million units, given as a stat dose. Benzathine benzylpenicillin comes in pre-filled syringes of 1.2 million units each, therefore the therapeutic dose of 2.4 million units comprises two pre-filled syringes, ideally given simultaneously into each buttock.
Non-infectious syphilis requires three doses of 2.4 million units, given once weekly over three weeks.
Contact tracing is an important aspect of management. Sexual contacts may be treated empirically without waiting for results.

Other practice points for syphilis management are outlined in Figure 1. Full details on management of syphilis are available in the online Silver Book STI/BBV Management Guidelines. Clinicians may also wish to use the “Decision Making in Syphilis” chart or online interactive tool developed by ASHM.
Resources for Clinicians include;
Silver Book STI/BBV management guidelines, State-wide Maternity Shared Care Guidelines, Decision Making in Syphilis – interactive tool or PDF chart and your local public health unit.
Author competing interests- nil

Anaemia is a common complication of chronic kidney disease (CKD), associated with reduced quality of life and increased morbidity and mortality. Its prevalence and severity increase as the estimated glomerular filtration rate (eGFR) declines, affecting up to 60% of CKD non-dialysis dependent patients.
Complex and interplaying factors contribute to anaemia in CKD (Table 1). The reduction in endogenous erythropoietin (EPO) levels is considered a primary driver. EPO, a hormone essential for erythropoiesis, is produced primarily in the kidney, with deficiency beginning early in CKD and becoming more severe when eGFR drops below 30ml/ min/1.73m2.
Absolute and relative iron deficiency is common in CKD patients. The ‘uraemic’ state and other comorbidities leading to chronic inflammation prevent adequate gastrointestinal iron absorption and release of iron from body stores. Hepcidin, a protein produced in the liver, is the primary regulator of iron absorption. Its upregulation secondary to inflammation, and reduced clearance by the kidneys in CKD, leads to inhibition of ferroportin,
The causes of anaemia in CKD patients are multifactorial and diverse
New anaemia in stable CKD patients may indicate a new pathology and requires investigation
The mainstay of treatment is iron replacement and ESAs; KDIGO recommends targeting TSAT ≤30% & ferritin ≤500ug/L and Hb 100-120g/L.
and hence reduced intestinal iron absorption.
Poor bone marrow response to EPO due to uraemic toxins, reduced red blood cell life span, frequent venesection, vitamin B12 and folic acid deficiencies, hyperparathyroidism and infection may all contribute to the development of anaemia.
The 2012 KDIGO guidelines recommend screening patients for anaemia when first evaluated for CKD with a full blood count, iron studies, B12 and folate. CKD patients with anaemia should have a thorough history and evaluation to assess for the common causes of
Factors contributing to anaemia in CKD (eGFR <60ml/min/1.73m^2)
Decreased erythropoietin production
Iron deficiency (absolute or functional)
Blood loss (platelet dysfunction, venesection, haemodialysis)
High hepcidin level (chronic inflammation, reduced clearance)
Inflammation (infection, co-morbidities)
Shortened red blood cell span
Bone marrow suppression by uraemia

CKD-Mineral Bone Disease (hyperparathyroidism)
Deficiency of Vitamin B12 and folate
Infection
anaemia (e.g. bleeding, malignancy and haemaglobinopathies). In patients with CKD but stable kidney function, anaemia may herald a new pathology, hence should be investigated in a targeted manner. If investigations do not reveal an alternative cause, it may be presumed that the anaemia is primarily due to EPO deficiency and CKD. After initial screening, patients are monitored for anaemia +/- iron deficiency on a three to six monthly basis.
Mainstay treatments include oral or intravenous iron replacement, erythropoiesis-stimulating agents (ESAs) and rarely, red blood cell (RBC) transfusions. Management and targets of anaemia therapy do vary.
Iron is required for an adequate erythropoietic response to EPO, iron deficient anaemic patients should be treated with iron prior to administration of ESAs. KDIGO recommends replacing iron when serum ferritin ≤ 100ng/mL and TSAT ≤ 20%. Administration of oral iron supplements in single doses on alternate days optimises absorption by preventing increased serum hepcidin levels.
However, oral iron may lead to dose-related gastrointestinal side effects adversely affecting nutritional intake, and absorption
continued on Page 51
GUARANTEED ACCESS TO A SURGEON ALL YEAR ROUND







continued from Page 49
may be limited by medications such as proton pump inhibitors. When offering IV iron therapy, KDIGO suggests high-dose lowfrequency (≤2 infusions, each ≥500mg iron) prescriptions. IV iron has been shown to be more efficacious in improving ferritin and haemoglobin levels, while decreasing ESA and transfusion requirements.
Current literature demonstrates patients with heart failure with reduced ejection fraction and iron deficiency have improved outcomes with IV iron supplementation in terms of heart failure symptoms, functional class and quality of life. The interplay between heart failure, iron deficiency and renal disease is well recognised, with each comorbidity reducing the survival in these patients.
Patients should receive a 1-3 month trial of iron therapy, with the route
of administration (oral vs IV) being determined by factors such as the severity of iron deficiency, tolerability and cost. While variability in targets exists, KDIGO suggests targeting TSAT ≤30% & ferritin ≤500ug/L.
Prior to initiating ESA therapy, all correctable causes of anaemia should be optimised. There are a range of EPO analogues which differ in properties such as halflife and EPO receptor affinity. They are generally commenced for patients with Hb ≤100g/L, with consideration of factors such as symptoms attributable to anaemia, the rate of fall of Hb, prior response to iron therapy, and relative risks of ESAs.
The target Hb concentration with ESA therapy remains controversial, although current literature demonstrates benefits in correcting Hb below ≤100g/L, but also increased risks of stroke and cardiovascular complications

These programs allow patients to address mental health issues with minimal wait time or disruption to their everyday lives.
Structured, therapeutic group sessions tailored to the specific needs of patients experiencing:
• Depression
• Anxiety
• Bi-polar disorder
• Personality disorder
• Trauma
• Eating disorders
• Substance dependency
For more information visit: ramsaymentalhealth.com.au/hollywood
• Refer directly to Ramsay Clinic Hollywood, no psychiatrist referral necessary
• Cost covered under private health insurance (top cover in psychiatric)
For a GP information pack: please contact Wendy Henson HensonW@ramsayhealth.com.au
Hence an individualised approach is needed for a target of 100120g/L. Subcutaneous injections in non-dialysis patients are generally administered on a weekly to monthly basis.
ESAs should be used with caution, if at all, in those with a history of, or active malignancy, stroke and vascular access thrombosis. Hyporesponsive patients should be screened for other causes of anaemia, inflammation and hyperparathyroidism. While ESAs have been demonstrated to improve quality of life, there does not appear to be a direct mortality benefit.
In those under consideration for renal transplantation, RBC transfusion should be avoided where possible to minimise the risk of allosensitisation.
– References on request
Author competing interests – nil
I don’t often get to ‘test’ an SUV… and this is not just any SUV. The Audi eTron S is not only right up there in the luxury stakes, it is also electric – fully electric!

I haven’t always warmed to the whole SUV space when it comes to cars that I would rush and spend my hard-earned cash on. I have always had the view that if you want a 4WD, then you shouldn’t hesitate to be able to drive it down the Cape Le Grande beach or at least consider the Gibb River Road or Canning Stock Route.
I mean it should be not too precious, so why have a luxury one? And then to go and make it electric – surely not!
So, I throw down the challenge to Audi…can you convince me otherwise?
The gorgeous Royal Blue eTron S is definitely off to a good start. That blue is just perfect.
This is a large car with oodles of street presence. A very impressive
lightshow when waking up the car, fancy flowing graphic type indicators and rear lights.
As with other EVs, the more usual electric items are just that bit more impressive. As with some of the other main line manufacturers of hydrocarbon-fuelled cars, the fact that it is electric is still understated. Tesla yells EV, whereas Audi says we’re a luxury car which just happens to be an EV.
A combination of no less than three digital displays, but the controls to all are reasonably intuitive, even to the point that I can scroll around while driving in rush-hour traffic and not take my attention too far away from the cars around me. Everything is adjustable and displayed. Google maps is clear and a lot better than my phone-based version.
Of course, the one thing that I would really like to play with is the different driver modes, but will need to wait until I am not driving to a medical symposium for that particular fun.
The tank/battery has a declared range of 350 odd km (according to the display) and is also recorded as full, so I guess that is the range. Still a little low, particularly for my view of an SUV, but workable and usable.
I would have thought that to really get the most out of all the available range, a smaller, lighter design would have been more desirable. The helpful salesman pointed out to me that if you have the camera side mirrors on the doors, then you gain an extra 10km of range, surely slimming down the overall dimensions would achieve a lot more.
This is a big car. I am Mr Average when it comes to height and weight (my wife might dispute the weight), but I almost felt a little lost when getting into the car. It will clearly accommodate five adults with no issues, so taking mobs of kids to school with all the assorted back packs, hockey sticks etc is clearly not going to be an issue.
No issues with “Tarmac Cowboy” challenges then. Big car it is.
But, with 800 + Newton metres of Torque, sluggish it isn’t. The weight of the necessary batteries keeps the car firmly planted on the road and so performance feels great, as does confidence, particularly for such a big car.
The car never felt hard work to drive. I rapidly felt confident that I could judge all the corners and meet the challenges of driving through congested school drop-off zones. Steering was precise and direct. Suspension was moderately firm (we are currently in Comfort mode). Comfort mode certainly lives up to its descriptor. I felt that I could comfortably drive to the limits of the car’s range, arrive and then feel fresh and relaxed when jumping to that next appointment.
The cabin has all the luxuries that you would expect from a market-leader – fully adjustable comfortable seats, excellent climate control and sound system. There are all the driver aids – lane assist, cruise control etc. The central console area between the front seats is a little more ‘out there’ compared with other manufacturers, with more of a ‘cage’ type appearance, but, it still has plenty of space for any cups, wallets, keys, phones, and day-today bits and pieces.
Reversing is easy with multiple different camera views including a simulated 3D image of where the car is, in relation to its surroundings. So, everything is there, but what is it like to drive?
There are numerous different modes: Comfort, Dynamic, Efficiency, Automatic, to name the important ones.

Dynamic raises the car slightly, firms up the suspension and gives more confidence to push the SUV along as if it were the more-sporty GT. Definitely my preferred mode.
I found the Efficiency-mode made the suspension a little too soft and wallowy, not sure why that would be more efficient.
Automatic-mode will also allow more obvious energy recovery with breaking, and it is nice to see the range can actually increase, a little, as the batteries get a boost.
As much as it would be nice to have a drive down that gravel road, I would prefer not to ruin my chances of having a play with other toys from the Audi Toy Store!

Yes, the car is attractive to look at, incredibly well appointed, does not lack for any electronic driver gizmo. It is responsive to drive, but of course there is no working down the gearbox as you set the car up for the next corner.
You will arrive at your destination,
unruffled – comfort driving for the busy exec, perfectly acceptable for the busy Mum taking kids to this that and the other. But would I want one?
I still hanker for enjoying the pleasure of driving, something more mechanical, so (for me) it’s perhaps a “not yet” but it is very tempting. I enjoy taking my Troopie off-road and not having to consider range issues, my little Clubman gives me all the tactile driving pleasures that I still enjoy. I would need to replace both to have the eTron S.
Now the eTron GT… hmm, that might be a different story!
Overseas model with optional equipment shown.

“I love all the bits of my life,” proclaims Georgie Carroll. “I have a really good happy barometer.”
The registered nurse and comedian has plenty to cheer about because she’s getting someone to cover her shifts when she heads west for the Perth Comedy Festival in May.
The English-born Carroll lives in Adelaide and has worked in hospitals for most of her career. She says everyone loves a good hospital story. Like her personality, her style is a joyful bluntness brimming with charm. Carroll’s Three Stages of Nursing routine – dividing nurses into dolphins, penguins and orcas –has been viewed more than seven million times.
Her mum has recently moved to Australia and is living with Carroll, her husband and two teenage boys. “I’ve worked out there’s no point trying to make someone feel bad when you can try and make them laugh. I’ve left my first ever clip online because I was a bit mean in it. I don’t do that anymore and have learnt to be smarter. For example, I know I will never be able to talk about something like addiction with humour,” she says.
But there are plenty of funny things to mine, from the regular shifts she takes at the hospital, and is more likely to rag on the staff than the patients. Allied health staff are
always fair game and can “get hit pretty hard”. Her family are not let off easily either – cue a story about her husband’s scrotum and her poles and holes chat (aka the birds and the bees) with her boys.
“The people you work with are a bit like family and you love them, but you don’t like them all,” she says
When she started appearing on television shows, patients started to recognise her. She has a simple rule on how she engages with them on that level – are their pants on or off? If their pants are off, she’ll often say something like “yeah people say I look like her” to assuage any fears that they might wind up as the butt of her next on-stage routine.
As her comedy has become more popular, she’s done less shifts at the hospital. But Carroll also loves the way she can be touring for a week, arrive home on a Sunday and on Monday be donning her scrubs.

The author and podcaster loves being busy, so juggling family and her two careers feels pretty good. Her husband – the king of a spreadsheet – has been enormously supportive.
“He’s the best model of a human ever. He works 9-to-5 and has found his passion. He has helped me set things up so I can be everything I want to be. I’m trying to dip my toe into England and maybe break there.”
Carroll says it’s no surprise there seems to be a growing number of healthcare professions turning to comedy. When you’ve spent a career caring for other people, comedy is an outlet which is totally yours.
It makes for an ideal solo sport after endless team playing. Generally, she says their outlook tends to be more ballsy than the bleak, which often typecasts medical humour.
“I reckon I can get away with a lot more because of my nursing background, like I’m judging you but I also care very much.
“Laughter is one of the best weapons you have against stress on the job and comedy is a great way to get that out.”
Georgie Carroll performs at the Perth Comedy Festival on May 12 and 13. The festival also features a host of Australian and international comedians such as Akmal, Dave O’Doherty, Nat’s What I Reckon, Josie Long, Rueben Kaye, Jason Leong and Dylan Moran.
Details and ticketing at www.perthcomedyfestival.com
WIN: We have a double pass to Georgie Carroll’s show to give away, at www.mforum.com.au
She’s a registered nurse and a comedian. What could possibly be funny about that? Georgie Carroll will show you, at the Perth Comedy Festival.
Taste Great Southern returns for 11 days of fresh local food, boutique wine and beverages all showing off the natural and cultivated beauty of the Great Southern. From beachfronts and barbecues to restaurants and wineries, events will be held inside and out, showcasing everything from cheese and heirloom vegetables to oysters, beef, wine and bush food.
From May 4-14 there will be more than 40 culinary experiences (paid and some free) featuring more than 20 chefs at unique dinners, degustations, markets, wine sessions, music events and more.
Events will be spread across the Great Southern, including in Albany, Denmark, Mt Barker, Frankland River, Katanning and Kojonup. They include local tastings and dinner with author Karen Herbert in Tambellup, and Eyre Park (Albany) hosts an open-air cellar door for wine, brews, spirits, local food and workshops.
By Ara JansenEvent director Richard Campbell is at the reins of the festival for the eighth year and retains his passion for food and wine events.
“I love this event, not only because it’s good for tourism but the wine from the Great Southern is exceptional and the individual events are always a lot of fun,” he says. “All the produce comes from local farms and you can’t get fresher than that.”
The Djeran Celebration spotlights the culture of the Menang, Koreng and Pibelman people of the region at the traditional meeting place and food source, the 6,000-year-old Fish Traps. Enjoy a foraging tour, canapes, three-course lunch by Paul Iskov and non-alcoholic drinks.
Celebrity chef Gary Mehigan hosts a number of events including a free local event at the Albany Farmers Market where he’ll shop and cook something spontaneous from what he finds on the day.
One of the things Richard loves
about the festival is the imagination local chefs, cooks and wine makers have used in coming up with interesting and entertaining ways to show off their passions and produce. For example, Fire and Feast in Mt Barker is held at an orchard and asks you to come rugged up for lamb on a spit plus fruit wines and traditional South African dessert.
There’s a women of the region lunch, tastings of aged rieslings, a night with a cook who also sings and the Kendenup Cook Off where you can enter and cook your best burger for the judges and the public to rate.

Visitors will probably be happy to know, that apart from a few events, most of them start late morning so there is plenty of time to sleep in and sleep off any effects from the day before.
Tickets and event information: www.wineandfood.com.au/ taste-great-southern
If you love food, wine and flavours of the Great Southern, then May will be a treat.
In 1840 John Septimus Roe, Western Australia’s first Surveyor General was granted by Queen Victoria 4,000 acres of riverbank land at West Swan. He named it Sandalford after a priory in his English home at Berkshire. The property was well managed and became prosperous as an agrarian estate supporting crops, cattle, fruit and vegetables and vines for table grapes, sultanas, raisins, currants and wine grapes. Early varieties planted were Shiraz, Verdelho, Cabernet Sauvignon and Frontignac.
The estate survived the vicissitudes of the Great Depression and two world wars and in 1970 made its second acquisition of prime viticultural land. Influenced by Dr John Gladstones’ treatise on the suitability of the Margaret River region for premium wine production, and winemaker Dorham Mann, the Roe family purchased 300ha at Wilyabrup joining the other pioneers of the Margaret River vineyards.
The next quantum change came in 1990 with the purchase of the estate by the Prendiville family headed by Peter and Debra Prendiville. The Prendivilles, who were experienced operators in tourism and hospitality, poured in the capital to take Sandalford to the next level of quality wine production. Today a comprehensive range of wine is produced – from the budget priced right up to the super premium Prendiville range. Wine making and viticulture is of a very high standard.


Made from old vine Swan Valley Chenin Blanc. Machine-harvested, cold-stabilised with barrel and stainless-steel fermentation. Three months on yeast lees shows as a savoury textural backdrop to the delicious floral and fresh pristine fruit flavours with a note of citrus. A mouth-filling, flavoursome white that can easily accompany seafood, spicy Asian cooking and white meats. Lovely drinking and quite beguiling (12.5% alcohol. $30)
From a cool Swan Valley vintage, this Shiraz shows abundant purple fruits at the peppery end of the shiraz flavour spectrum. Spice is also evident. Oak handling is refined and understated adding to the overall delicious appeal. Refined clean and crisp. If only John Septimus Roe were here to witness what his vineyard could achieve! (14.5% alcohol. $50)

Made from Wilyabrup fruit and partially barrel fermented this Bordeaux blend has an attractive aroma of berries with a touch of cedarwood. Deliciously clean in the mouth, the fruit oak tannins are beautifully balanced. Lovely to drink right now but will keep easily for five years. (14.0% alcohol $25)
2018 was an outstanding vintage year for Margaret River. The 40+ year-old Cabernet vines from this dress circle address in Wilyabrup with a smidgeon (2%) of Malbec have delivered a world class example of Cabernet Sauvignon. This wine spent 13 months in French oak casks which has underpinned the gorgeous, sweet fruit intensity with fine silky tannins and a long persisting finish. Whilst immensely enjoyable now it will easily live for 10-20 years. (14.5% alcohol. $50)

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat.