






rebates through our Loyalty Reward Plan* Dividends paid out when you retire throughour Retirement Reward Plan^ Access medico-legal experts, 24/7 inemergencies
Local support, from Avant Law’s 80+ medico-legal solicitors nationwide
advice to reduce
















rebates through our Loyalty Reward Plan* Dividends paid out when you retire throughour Retirement Reward Plan^ Access medico-legal experts, 24/7 inemergencies
Local support, from Avant Law’s 80+ medico-legal solicitors nationwide
advice to reduce








Even kids are sleeping less, prompting a surge in medical appointments for young children with sleeping disorders and some parents resorting to buying melatonin supplements online for them.
Anyone who has trouble sleeping may well know the challenge of trying not to become anxious as night falls, because that just seems to make sleep more elusive.
As a chronic insomniac, I can only watch enviously as my partner falls asleep almost before his head hits the pillow.
Sleep health has become big business – fuelling a whole industry of research and treatments with, to be honest, only very modest success to date.
Entrepreneurial types are cashing in on the quest for a better, deeper, longer sleep. Apart from the obvious sleep tracking and white noise devices, there is even a new robot versed in thousands of years of Buddhist breathing techniques that promises to soothe you to sleep.
Even kids are sleeping less, prompting a surge in medical appointments for young children with sleeping disorders and some parents resorting to buying melatonin supplements online for them.
While digital technology cops a fair bit of the blame for sleeping problems, factors such as reduced physical activity and higher rates of anxiety and other mental health issues seem to be implicated too.
Our feature on the big business of sleeping segues nicely with our edition theme of cardiovascular health, with high blood pressure and heart disease prominent on the list of ailments linked to poor sleep.
This month we also look at peripheral artery disease, and some heartening progress in combating deadly mesothelioma.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.



12 Hope for a slowdown of mesothelioma
16 A cure for peripheral artery disease?
20 Close-up: Dr Brittney Wicksteed
24

1 Editorial: Awake to sleep disorders
– Cathy O’Leary
4 News & views
8 In brief
33 Where have all the questions gone?
– Dr Joe Kosterich
34 Earlier call on pathology tests
38 WA Centre for trauma treatment
49 WA's first dementia doulas

A few dozen readers of Medical Forum have been off to the flicks in recent weeks, as winners of our big March movie giveaway.
This month we have our next doctors dozen to win, featuring a fine selection of wine from Frankland Estate. Go to page 53 to read the review by Dr Louis Papaelias, and for a chance to win use the QR code on this page or go to mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director
Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor
Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist
Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au















Two new booklets have been released in WA to help people navigate the challenges of a life-limiting illness.
Palliative Care WA, in association with an expert panel of health professionals, has launched a revision to the popular Palliative Caring booklet and a new companion booklet called My Palliative Care
The WA-specific resources have been developed through sector consultation and in recognition of the need for two tailored, consumer-centric booklets. They provide information to support families and carers as they negotiate the often-uncharted waters of caring for a loved one with a life-limiting illness, and for individuals on the palliative care journey themselves.
Palliative Care WA CEO Lenka Psar-McCabe said the booklets were free, funded via the Greater Choices for at Home Palliative Care, an Australian Government initiative implemented by WA Primary Health Alliance in WA.
“Palliative Care WA first produced Palliative Caring, a comprehensive and cross-sector publication, in 2018. The project created a catalyst to work more closely with service providers, clinicians and community.
“Over the years the booklet has undergone multiple revisions, always with the goal of improving the resource for those caring for loved ones receiving palliative care.”
The Palliative Caring booklet covers a variety of topics to support and guide families and carers through the
Curtin researchers have secured a State Government grant to create a new digital tool identifying people at high risk of dementia.
Led by Professor Blossom Stephan from the Dementia Centre of Excellence at Curtin’s EnAble Institute, the project, in collaboration with Dementia Australia, the University of WA and Edith Cowan University, will try to build a predictive algorithm for dementia using both global and Australian data.
Dementia is a leading cause of disability and death affecting more than 55 million people worldwide, including an estimated 46,000 people in WA.
Professor Stephan said that without a cure, preventative measures were paramount.
“While numerous dementia prediction models exist, none has been developed and tested using Western Australian data and
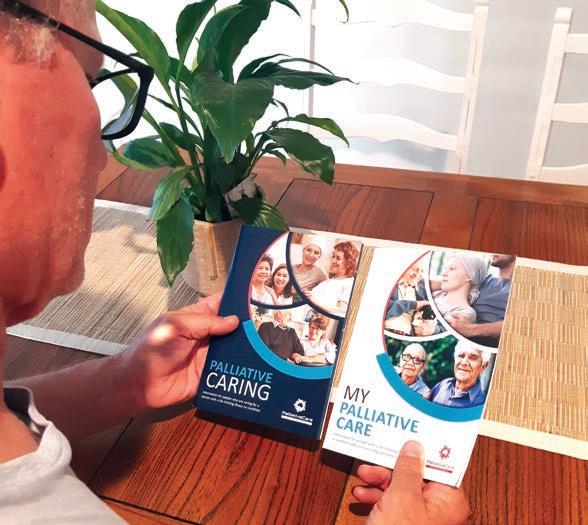
palliative caring journey. These include ‘hoping for the best and planning for the rest’, the role of a carer, what is palliative care, planning and decision-making, caring at home, rural and remote considerations, last days of life and death and bereavement.
My Palliative Care includes similar topics but with an emphasis on helping people make informed decisions that reflect their personal needs and circumstances as they approach this part of their lives.
Copies can be obtained by emailing info@palliativecarewa.asn.au or phoning
1300 551 704. To download a copy visit https://palliativecarewa.asn.au/about-us/news/
targeted intervention is lacking,” she said. “This project has the potential to create a greater public awareness of dementia and its risk factors and make a tangible difference in the lives of individuals affected by the condition.”
The project ‘Dementia Risk Prediction and Risk Reduction in Western Australia: DEMRISK-WA’ is one of four successful recipients to share in $3 million in funding through the WA Cohort Studies Research Support Program.
A surge in cases of syphilis in WA and elsewhere in the country has prompted calls for repeat testing in pregnancy to combat the rise of cases in babies.
The Royal College of Pathologists of Australasia’s Professor Robert Norton has urged healthcare providers to prioritise syphilis testing, particularly in high-risk groups, and emphasised the
need for repeated testing during pregnancy to prevent illness and death in newborns.
Professor Norton said that because syphilis was largely preventable and curable, early detection and intervention was crucial.
“In the past 12 months there have been 6000 new cases of syphilis in Australia, with around 60% of those occurring in males in inner cities, posing a risk of transmission to their female partners,” he said.
“Left untreated, syphilis can cause damage to the heart, brain, eyes and other organs. In pregnant women, syphilis can lead to congenital syphilis (CS) in newborns, resulting in stillbirth, premature birth and long-term developmental issues in infants.
“In Australia, nearly three-quarters of people who have a baby with CS are diagnosed late in pregnancy, leading to missed opportunities
continued on Page 8
Cardiac amyloid, particularly the Transthyretinassociated type (ATTR-CM) is much more common than you think.
Transthyretin is a transport tetramer protein that can misfold when metabolised and ultimately become amyloidogenic. Genetic variants of transthyretin can present with amyloid earlier in life with prominent neurological symptoms, the more common ‘wild type’ has a male preponderance presenting in the seventh and later decades.
Anyone who sees many patients in their 70s and older will come across this condition, often unknowingly. It can be a great mimic of other diseases.
Just a few years ago this was a pretty depressing diagnosis to make, with no particularly effective treatments and relentless progression to severe disability and death. Fortunately, those days are gone, ATTR-CM has effective treatment options now (Stabilisers) for many patients and is a very active area of research for future treatment options within five years (Silencers and Depleters).
ATTR-CM is an infiltrative cardiomyopathy, most commonly presenting with traditional heart failure symptoms (dyspnoea, reduction in exercise tolerance, fluid retention etc) but initially with a normal ejection fraction. Increased myocardial wall thickness is always present, ventricular septum should be >12mm.
Most traditional treatments for heart failure do not work in ATTR-CM, can aggravate symptoms and reduce quality of life.
Clinical signs and symptoms are easily overlooked in elderly patients, many with co-morbidities leading to a missed or very delayed diagnosis. Clinical clues exist to improve detection including unexplained elevated troponin, in contrast to the echocardiogram ECG without voltage criteria for hypertrophy, a history of neurological problems including carpal tunnel syndrome or neuropathy. NT-proBNP elevation is very common. Although this test does not have a Medicare rebate, it is a relatively inexpensive test.
An echocardiogram is a key part of diagnosis. In addition to increased wall thickness, other abnormalities are common – abnormal diastolic function which can be severely abnormal, dilated atria, small pericardial effusions and a peculiar apical sparing pattern on global longitudinal strain (GLS) assessment. GLS is, unfortunately, not a routine assessment for all echo
By Dr Peter Purnell Cardiologist and Clinical Research Director of Advara Heartcare Australiaproviders, it may be worth checking if your provider does do it routinely.
When considering a diagnosis of ATTR-CM it is important to exclude AL cardiac amyloid, a monoclonal light chain disease. This can be done by Serum Free Light Chains, QEPP and Immunofixation and Electrophoresis and Urine Electrophoresis. A haematological opinion should always be sought if these tests are abnormal but, frustratingly, low level monoclonal light chains (MGUS) are not uncommon in elderly patients and unrelated to their ATTR-CM
Confirmation of ATTR-CM no longer requires a myocardial biopsy in the vast majority of patients. It was incidentally discovered that nuclear bone scan scintigraphy would show myocardial uptake in ATTRCM with the amyloid fibrils binding the diphosphonate tracer and diffuse myocardial enhancement is seen.
The intensity of the uptake correlates to the severity of the disease. As long as AL has been excluded, in combination with supportive echo or MRI and clinical features, scintigraphy is the confirming step for diagnosis.
Tafamadis is a ‘Stabiliser’ of Transthyretin, making it less likely to misfold and become amyloidogenic. It has favourable mortality, morbidity and quality of life outcomes. Tafamadis has been available since 2019 but prohibitively expensive. It is now available for class NYHA I or II patients through a free access program in anticipation of PBS listing later this year.
Current research includes ‘Silencers’ which modify DNA or RNA to stop production of Transthyretin (no transthyretin means no new amyloid forms) and ‘Depleters’ Monoclonal Antibody therapies that target ATTR-CM amyloid and may allow immunological mediated regression of disease.
I am currently principal investigator for ongoing studies of Silencers and Depleters of ATTR-CM.

Conventional high end CT
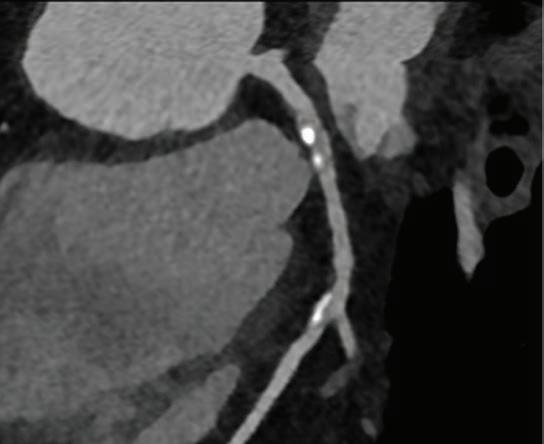
Diagnosis = > 50% stenosis
Photon Counting CT

Diagnosis = minor irregularity only
Photon Counting CT eliminates calcium blooming artefact therefore lessens unnecessary referrals for invasive angiography by up to 50% (e.g. Simon J, J Cardiovasc Comput Tomogr. Jan-Feb 2024 and Zsarnoczay, E. Eur Journal Radiol April 2023)
Conventional high end CT

Dose equivalent = 6 Chest X-ray exams
Photon Counting CT

Dose equivalent = 1 Chest X-ray exam
Photon Counting CT has a revolutionary new detector exquisitely sensitive to X-rays and impervious to electronic noise, making CT at a CXR dose finally a reality (e.g. Dettmer, S. Respiration 2024 and Wassipaul, C. The Lancet Oct 2023)



Professor André Schultz has been appointed as head of Perth’s Walyan Respiratory Research Centre, succeeding Professor Stephen Stick.
Ramsay Health Care has signed a contract with the State Government to continue operating the Joondalup Health Campus for another 15 years, paving the way for a $190 million expansion of its private hospital.

The Channel 7 Telethon Trust has awarded a grant to a team led by Perron Institute and UWA researcher Dr Andrew Tai to develop a novel drug that targets chromosome 15 imprinting disorders, including the rare genetic disease Angelman syndrome.
Telethon Kids Institute’s Chris Brennan-Jones, Rishi Kotecha and Katherine Landweh have been awarded almost $2 million collectively in the WA Near Miss Awards Emerging Leaders 2023 program for work in ear health, cancer treatments and childhood lung disease.

Curtin University has appointed Professor Carlo Marra as Pro Vice-Chancellor in its Faculty of Health Sciences. He has worked in New Zealand as Professor and Dean of the School of Pharmacy at the University of Otago.
WA has become the first Australian State to offer free vaccination to protect babies from respiratory syncytial virus (RSV).
continued from Page 4
for treatment and prevention. The current standard of care is that women are tested for syphilis in their first trimester but may not be tested again during their pregnancy, even though they risk re-infection from their partner.”
Pregnant women should receive syphilis testing in the first trimester, followed by repeat testing towards the end of the second or third trimester, even if the initial test was negative.
Bowel prep explained
A new resource has been developed to help patients ‘bowel
prep’ for a colonoscopy, after concerns that inadequate prepping is hampering clear results.
Bowel Cancer Australia said inadequate bowel preparation occurred in about 7% of colonoscopies, which could lead to repeat procedures impacting waitlists. A good bowel prep was essential to a good colonoscopy and critical to detecting bowel cancer or preventing it through the detection and removal of polyps.
Bowel prep involves emptying and cleaning out the large bowel in preparation for colonoscopy via the intake of oral solution containing strong laxatives.
In the resource, patients are given instructions on how to complete

In 2021, Anne Preston Carter’s grandson Kade was diagnosed with anaplastic large cell lymphoma in the central nervous system – one of only a handful of children in the world with the diagnosis.
Watching helplessly as his parents and siblings struggled while Kade underwent chemotherapy, she decided there must be research to find a cure or better treatment.
While Kade has just turned nine and continues to battle the disease, his family’s efforts have resulted in a special fundraising and awareness event being held in Yallingup on June 8.
Known as Rhapsody for Cancer, the gala black-tie event is in its third year, having previously raised more than $200,000 to advance childhood brain cancer research and support families affected by the disease.
This year’s proceeds will go to two charities – the Pirate Ship Foundation, to fund vital research at the Brain Tumour Research Centre, and the Kids Cancer Support Group to improve the lives of children with cancer and blood disorders being treated at Ward 1A at Perth Children’s Hospital.
The $500-a-head event at Tiller Farm will donate almost 90% of proceeds to the charities.
For more details contact Anne on 0427 042 767 or anne@rhapsodyforcancer.au or buy tickets at https://events.humanitix.com/ rhapsody-for-cancer.
the prep, as well as a list of what they can and cannot eat or drink.
Bowel Cancer Australia said that with more than 900,000 colonoscopies performed annually in the country, poor bowel prep could equate to as many as 63,000 inadequate preparations, leading to poor or cancelled colonoscopies.
If the colonoscopy did proceed, it could be less effective, as polyps and bowel cancer were more likely to be missed due to poor visibility.
The new resource (bowelprep.au) provides a list of easy steps for patients to follow, reminders at each step, and videos to help explain the bowel prep and white/lowresidue diet. Patients can amend the timing of steps as advised by their colonoscopist, if needed.
The resource is configured for every bowel prep solution currently available in Australia.
New Curtin University research has shown Australian young people have major concerns about climate change, which is having a significant impact on their lives and could have broader consequences decades into the future.
Published in Sustainable Earth Reviews, the study surveyed university students belonging to Generation Z – people born between 1995 and 2010 – and found climate change was their number one environmental concern.
More than 80% reported being ‘concerned’ or ‘very concerned’ about climate change, with many revealing they felt anxious over the issue.
Curtin Professor of Sustainability
Dora Marinova said climate anxiety was a contributing factor to Gen Z’s overall sense of unease towards the future, which could have major future ramifications.
“These young people are very concerned and, in a way, intimidated by the lack of concrete action being taken to battle climate change,” Professor Marinova said.
“Gen Z has serious concerns which will not only impact their mental health, which will be something society and the public health system will have to deal with, but also the choices young people

Hollywood Private Hospital is celebrating its 30th anniversary this year as Australia’s largest private hospital.
Originally acquired by the late Paul Ramsay in 1994, Hollywood played a pivotal role in shaping Ramsay Health Care as the largest private hospital operator in the country.
When the hospital was purchased from the Commonwealth Government, Ramsay gained not just a 300-bed facility – it was a valuable piece of WA history dating back to World War II.
Hollywood’s Chief Executive Officer Andrew Tome said that in the past 30 years the hospital had more than tripled its bed numbers.
“In February 1994, the hospital had 207 accredited visiting medical specialists, and now we have more than 800 specialists working over a wide range of disciplines, and we employ close to 2550 people in diverse roles,” he said.
“We have expanded our mental health clinic to make it the largest standalone private mental health hospital in WA, and we opened the first private emergency department north of the river.
Today Hollywood admits about 85,000 inpatients a year and carries out more than 55,000 surgeries and treats about 15,000 emergency patients.
make – how they spend their money, whether they have families, their choice of career and more.”
Public health experts are calling for the Federal Government to urgently implement and properly resource the proposed Australian Centre for Disease Control to ensure COVID advice is consistent across the country.
The call from the Public Health Association of Australia comes as public health experts await further details of the ACDC promised by the Albanese Government during the 2022 federal election.
The ACDC was set up as a $90 million interim body in January this year but is yet to be formally
established or receive ongoing funds.
Professor Simone Pettigrew, health communication expert from the George Institute for Global Health, said the current situation could be negatively impacting public health outcomes, as COVID continued to develop across the country.
“The current COVID-19 messaging differs in complexity, priority and content between the States and territories,” she said. “That makes it harder for Australians to interpret health advice.
“Residents of some States may be receiving more, or less, effective guidance compared with others. A single, clear and consistent source of truth would undoubtedly improve public health outcomes.”

Of course, it was never supposed to happen.
We had just enjoyed an amazing family holiday in Europe, with mountain biking in Switzerland and then a wedding in Edinburgh. Having caught up with numerous family and friends, we had a rapid turn-around on returning to Perth, then headed to far North Queensland.
My wife, Cathy, and I have done a lot of 4WD camping and were really looking forward to “our time,” heading towards the Great Central Road, and on to Alice Springs.
We then headed north towards Mataranka Springs and drove down the Savannah Way. Lots of remote desert, amazing scenery, great people and the ever-present dirt road corrugations.
We were in Cooktown preparing to go towards the top of Queensland, but fate had other ideas.
Early morning on September 10, we had decided to get ready to leave the campsite. I let Cathy know that I was going to take the awning down and start to pack things up.
The next two days then vanished for me. No searing pain, no tunnel of light. Nothing.
I woke up in Cairns Base Hospital in ICU. I have no memory of that period, although my 30 years of general practice experience meant that I could fill in many of the gaps – the unpleasant details.
Cathy on the other hand remembers everything. It is not so
Dr Mike Civil and his GP wife Catherine weren’t planning a coronary emergency and a two-week immersive at the Cairns Base Hospital. Here Mike pieces together how it all happened.

distressing for her now, as we are now six months down the track and life has nearly returned to normal.
I had had a cardiac arrest. Cathy had heard a thumping sound and had thought that I had fallen off the ladder and was worried that I might have injured myself. She found me collapsed and not breathing.
All those years of training took over. She yelled for help and started CPR. Other members of the campsite came to her aid, the emergency services were called and, fortunately, the camp site had a defibrillator. I was transferred to the local emergency department in Cooktown. Officially, I had had 20 minutes of down time, continuous CPR and four shocks, before the return of spontaneous circulation.
I was intubated and transferred by helicopter to Cairns Base Hospital. A day or so later I was extubated and transferred from ICU to coronary care. I have some vague memories of being on ICU, before waking up properly a couple of days later. I have no memories of this period.
Once I had rejoined the world, I had every cardiac test known to man and cardiologist. These included coronary angiogram, cardiac MRI, echo, etc. Fortunately, a relatively healthy lifestyle, no smoking and good genetics meant that there was very little of note on the tests.
The coronary arteries really had minimal plaque formation. What was found was a small lesion – an area of scarring from old
myocarditis – in the ventricular wall, and that was the likely cause of the electrical disruption, leading to ventricular fibrillation. Possibly a viral infection at some stage in the past. Yes, I had had COVID a year previously, but it could have been from any viral infection.
Arrangements were made for me to have an implantable cardioverter defibrillator (ICD), and a PET scan was performed to ensure that the lesion was not from sarcoid or other active inflammation.
All clear. Exercise stress test –not particularly pleasant, trying to run with four broken ribs (consequences of good CPR!). I did okay on the treadmill and so the ICD now sits just below my left clavicle.
My cardiologist encouraged me with good prognostic indicators, a gradual return to full fitness and no limitations into the future –well, apart from no visiting power stations, or outer space, no scuba diving, etc. ICDs and magnets are not great together.
I recuperated in Queensland for two weeks then flew back to Perth. Since then, it’s been seeing

a cardiologist, cardio-rehab, psychologist, regular trips to my GP, riding my e-bike and generally just readjusting. Meditation daily. No driving for six months meant an e-bike appeared early and that has been great; some independence! One of my dream motorsport projects has kept me distracted and positive. I even enjoyed returning to work, although no intention of going back to full time – yet.
Surprises!
Six months later, I have only very, very, slowly regained some of my
old confidence levels. Generally, I am still anxious and apprehensive in certain ‘busy’ environments. Your mental health takes a hammering. It is not just physical. Sleeping is still pretty ordinary, but all of these things are improving. The few medications that I take are no big deal, some postural symptoms, but only when getting up suddenly.
I am happy to share my story, as even one extra person doing a CPR course could make the same difference to someone experiencing the same story.
Ramsay Clinic Hollywood provides specialised inpatient and day patient services for patients struggling with eating disorders. Treatment comprises a mix of psychiatric interventions, psychological care, nutritional support and peer worker involvement.
• GP-referred (patient does not need own psychiatrist prior to admission)
• Patients are assessed prior to admission for the Day Program and admitted under the Consultant Psychiatrist, Dr Richard Clarke
• Inpatient Program Consultant Psychiatrist – Dr Leighton Chadwick
• Patients can enter the Day Program at any time
• An onsite support group is also available

Further information is available on the Ramsay Clinic Hollywood web site (see ‘For Doctors’ pages) or by contacting Wendy Henson
E: hensonw@ramsayhealth.com.au
M: 0417 404 776
Referral:

• A Best Practice template or writable pdf referral is available
• Email to: rchbookings.hph@ramsayhealth.com.au
• Phone 9346 6850 to discuss pre-admission tests that may be required
Note: Private health insurance, DVA cover or self-funding required

As a disease that is incurable and deadly, mesothelioma is rarely a good news story, but two initiatives originating out of Perth offer some optimism.By Cathy O’Leary
For 60 years, every case of mesothelioma – the rare and aggressive cancer caused by exposure to asbestos – has been dutifully recorded in a WA database, dating back to the start of the epidemic in the 1960s.
Initially, the high-risk group was the workers who mined asbestos in the Wittenoom Gorge, but they were soon followed by a second wave of cases in people such as carpenters who had used asbestos as part of their trade.
And while the painful legacy of the first two waves has largely shown its hand, it has been the next wave – in budding do-it-yourself home renovators – that has worried respiratory specialists in recent years.
While asbestos was banned in Australia in 2003, there have been concerns about the sheer numbers of people doing DIY projects around their home who might come into contact with asbestos – already or in the future.
But there are optimistic signs that the third wave has also turned the corner, with figures from WA’s Mesothelioma Registry suggesting cases have reached a plateau – potentially putting a dent in the feared explosion of cases linked to home renovations.
And the promising sign has coincided with the launch of a new industry-backed resource and support network in WA to better help people living with the terminal disease.
Mesothelioma invariably has a poor prognosis. It is an incurable, universally fatal disease, predominantly of the pleural and peritoneal mesothelium, and primarily caused by exposure to asbestos fibres.
Global asbestos use peaked in the last century, but despite a ban on asbestos import and use in more than 60 countries, it is estimated that more than a million tonnes of asbestos was exported to predominantly developing countries in 2019.
In the early days of its use in Australia, asbestos itself was considered innocuous, with young children even playing in its dusty tailings.
Across developed countries, the first wave of the mesothelioma was caused by exposure to raw fibres from the mining, milling and handling of asbestos. Australia imported and mined asbestos, including chrysotile in New South Wales and crocidolite in WA.
Between 1937 and 1966, about 150,000 tonnes of crocidolite was mined from the Wittenoom region, the town of which was established for miners and their families and was only completely closed in 2022.
The second wave of mesothelioma was caused by workers who used asbestos-containing products in industry, typically construction, boiler workers, carpenters, railways and dockyard workers. After a partial ban on asbestos-containing products in Australia in 1984, there were significant concerns about people being diagnosed with mesothelioma after short-term or low-level exposure to residual asbestos in the built environment at home or at work.
In Australia, 700 to 800 people are now diagnosed with mesothelioma each year, and the WA registry tracks all cases in this State – both work-related and non-occupational.
The latest review of cases, recently published in the journal Respirology, was done by researchers Fraser Brims, Chellan Kumarasamy, Lalitha

Menon, Nola Olsen, Nick de Klerk and Peter Franklin.
Writing in the journal, they said that while Australia introduced a partial ban on asbestos use in the 1980s, there had been continuing concern about exposure to asbestos in the built environment and nonoccupational exposures.
The aim of their study was to look at epidemiological trends in the 60 years since the first case was recorded, and they believed it to be the longest-running mesothelioma cohort study in literature.
Overall, it identified 2796 cases, with males making up 85% of cases, with a median age at diagnosis of 70, a latency of 47 years on average and a median survival of 298 days.
There were strong gender differences related to the source of the exposure.
As expected for a predominantly occupational disease, about 85% of cases were in males, but the proportion of females with a non-occupational source of exposure was much higher, with one in five females having DIY exposure, compared to one in 20 males.
This was likely to reflect historical, social and work-related factors, and highlighted that other household members could be affected by DIY exposure.
A previous report using data from the WA registry had warned of a rising number of mesothelioma cases attributed to home renovation and DIY projects. But the new study found that the annual number of cases of mesothelioma may have hit a plateau at around 100.
“While the absolute numbers of Wittenoom workers developing mesothelioma has not changed much since the 1980s, there has been a steady fall as a proportion of all cases since this time,” the study found.
“There has been significant concern about the third wave of exposure from DIY home renovation and the data in the present study demonstrate that both the proportion of DIY cases has not risen in the last decade and, the incident rate ratio for DIY cases has fallen.
“This provides some of the first evidence that the asbestos ban in Australian enacted in 1984 may have been successful in reducing exposure to the wider community.”
One of the researchers, Professor Fraser Brims from Curtin Medical School, told Medical Forum that when his group looked at this issue back in about 2010, it showed a potentially
continued from Page 13
worrying increase in the number of people exposed as part of the DIY renovations.
“The wider Australian data suggests we might be reaching a plateau in terms of the number of cases, so we wanted to look at that from a WA point of view as well,” he said. “And our study has shown that, yes, in WA we probably are reaching a plateau, and certainly the number of cases in the past five years has been hovering around 100.”
Professor Brims said that, importantly, one of the key headline messages was that the number of people exposed because of DIY renovations seemed to have dropped off.
“We’ve only found three cases that have been exposed after 1984, which is when the initial partial ban came in,” he said.
“It is evidence that the number of cases is slowing, but I think at the same time we’re going to have a very long tail, because more than 40% of all the asbestos we used in Australia is still in our built environment.
“So, the legacy lives on, and the risk and the need for people doing DIY, even if it’s in their own house and they’re just knocking down a wall or the odd chicken coop, means they need to think first about what they’re about to knock down or drill through.”
Professor Brims cautioned that DIY exposure remained an ongoing concern, but there needed to be a nuanced conversation about the actual risk.
“When you look at how busy hardware shops are on a weekend, all those people, and with twothirds of houses built between 1950 and 1980 having asbestos and all those renovations going on, it’s a huge population out there,” he said.
“But in fairness, some of them will have very minor exposure, and that’s the key thing, which is relevant will all the issues going on with contaminated garden mulch over east. The likelihood
of developing mesothelioma and indeed any other asbestos-related disease is entirely related to how much you’re exposed to.
“We hear in the media about the really awful (mesothelioma) cases, which are very rare, but it does highlight the very important public health message that any exposure is potentially dangerous, but your risk from one exposure is very unlikely to cause you disease.”
Professor Brims said that if the current trend continued, he would expect to see the cases to continue to level off.
Barry KnowlesReflections is a not-for-profit organisation that was inspired by the journey of Perth man Barry Knowles and others who fought long battles before losing their lives to the insidious disease.

One of the main driving forces behind the new resource is Barry’s daughter, Jo Morris , who was surprised by the dearth of support and information for those affected by mesothelioma when her dad was ill.
“But in years to come, all the tradies and people who worked with asbestos exposed in the 1960s, ’70s and ’80s are going to die off, and not necessarily from mesothelioma, so as a proportion of cases, those exposed through DIY are probably going to increase because that’s still going on now.”
New WA resource
Professor Brims welcomed the recent efforts of the WA organisation Reflections, of which he is an ambassador. In February this year, it launched a groundbreaking support resource, The Hope Companion, aimed at people with mesothelioma, their carers and health professionals.
“Mesothelioma is a lonely cancer, and Mum and Dad struggled to find the care and support they needed, and access to relevant, accurate information was hard,” she said at the time of the launch.
The resource combines lived experience with medical information, offering support for patients and caregivers. With practical tips, checklists, and space for reflection, it is designed to bring hope after a life-changing diagnosis.
It includes insights from medical, legal and nursing professionals, and covers how the disease is diagnosed and progresses, guidance on living well with mesothelioma, a healthcare management booklet, help for caregivers, end-of-life planning
advice and support for moving forward after loss.
A general guide is backed up by a hard-copy medical booklet which patients can use to track their appointments and medications and log their pain and symptoms.
Professor Anna Nowak, a mesothelioma researcher and Deputy Vice-Chancellor in Research at the University of WA, said it was an invaluable resource for people impacted by a devastating disease.
“Every page combines empathy, common-sense and lived experience with trustworthy medical information,” she said.
Thoracic oncology nurse coordinator Kirsten Stewart said it offered practical and emotional support to both patients and partners through regular contact via phone or support group.
“I know patients find the support invaluable as they’re able to discuss thoughts and feelings with others who are walking the same journey as themselves,” she said.
Doctors, including medical oncologist Dr Melvin Chin and

lung specialist Professor Bruce Robinson, have also welcomed the resource to help patients navigate their mesothelioma care.
Professor Brims said Australia still had one of the highest rates of mesothelioma in the world and relentless asbestos use continued in many countries, so asbestos disease was not going away anytime soon.
“We still have a responsibility to our region to address the catastrophic impact of asbestos use,” he said.
The Hope Companion can be accessed by contacting Reflections on 1800 031 731, email support@reflections.org.au or the website www.reflections.org.au


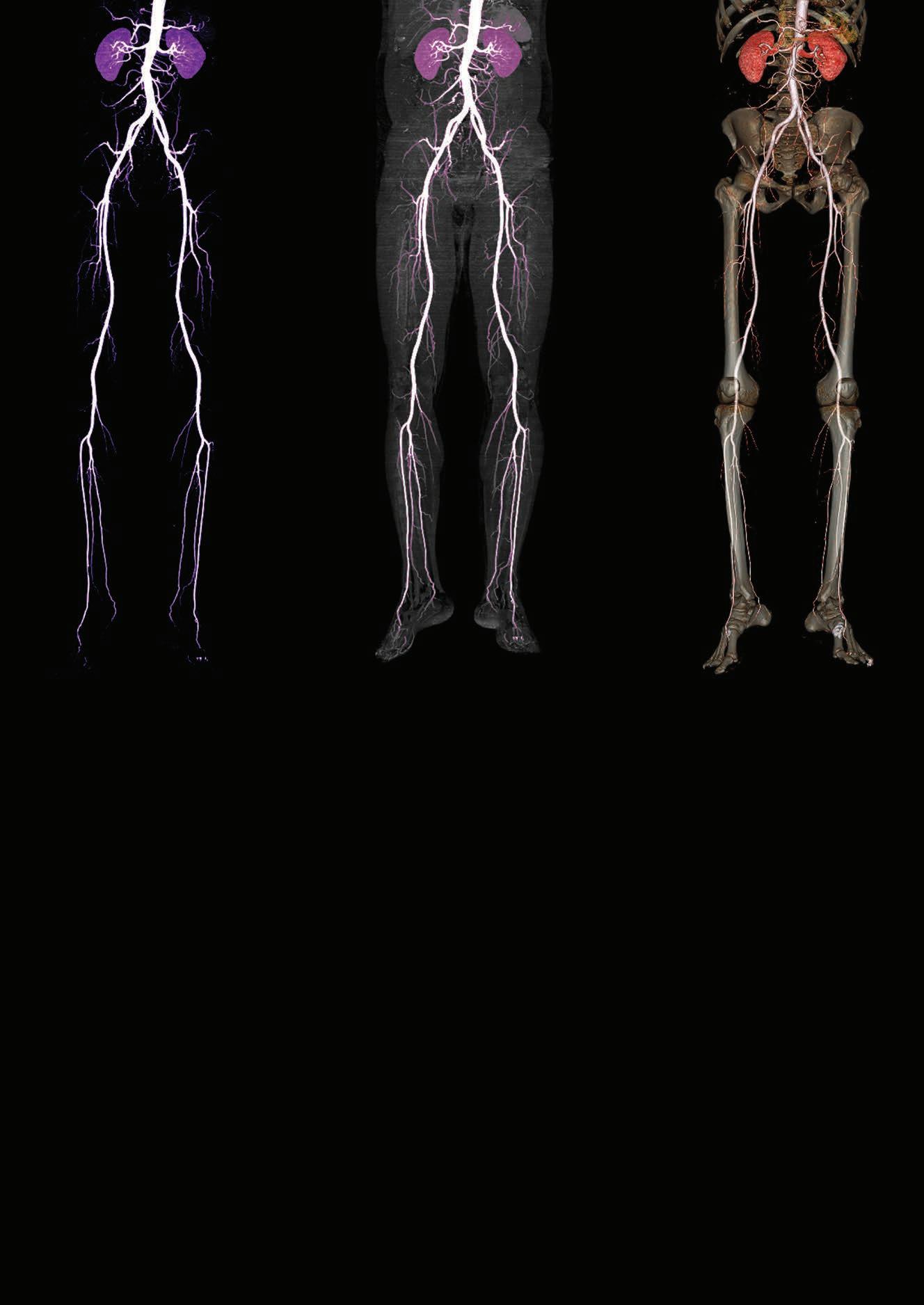
Excitement is palpable among Harry Perkins Institute researchers as they progress the approval stages of a drug that may have the damaging peripheral artery disease on the run.
By Eric MartinEvery few decades a revolutionary discovery is made that changes the outcome of a chronic disease for millions of sufferers. Now, based on the results emerging from researchers at Perth’s Harry Perkins Institute, one such revolutionary breakthrough in the treatment of peripheral artery disease is about to be realised in WA.
Medical Forum spoke with the Perkins Institute’s Associate Professor Juliana Hamzah and vascular surgeon and Head of Department of Vascular and Endovascular Surgery at Sir Charles Gairdner Hospital Professor Shirley Jansen, about what could be the biggest advance in the treatment of atherosclerosis since the invention of statins at the end of the 1970s – and one that potentially dwarfs them –the very real chance of a cure.
PAD, manifested as CLTI, the rate of MACEs and MALEs was 22.6% and 57.2% over 2.5 years, respectively.
“Roughly a fifth will have a cardiac event such as a heart attack in their lifetime and roughly two thirds of them will have an adverse lower limb event, which may mean amputation. In Australia, the cost is $1 billion a year – that’s 20,000 endovascular procedures a year, 5000 open operations for bypass surgery and 1800 legs amputated,” Dr Jansen said.


Compared to coronary artery disease (CAD) and cerebrovascular disease (CeVD), PAD is underappreciated, even though it affects over 230 million people worldwide and is associated with the highest morbidity and mortality rates globally.
Patients with symptomatic lowerextremity PAD generally have more extensive atherosclerosis than those with CAD or CeVD and, despite improved treatment options, the mortality rate in patients with PAD is substantially greater than in the general population – twice the rate in those with intermittent claudication [IC].
“Over time, it can progress to what we call chronic limb threatening ischemia, or CLTI, which is the most severe end of the spectrum where the limb is threatened. In that group of CLTI patients, their mortality is worse than many cancers and fivefold the general population rate,” Professor Jansen said.
Compared to CAD, patients with PAD also have a 1.5 to twofold greater risk for major adverse cardiovascular or limb events (MACEs or MALEs) and those risks increase alongside disease severity: in a contemporary series of Australian patients with greater-risk
“Similarly, revascularisation of CLTI limbs forms a large part of our work in vascular surgery now and what we spend the most time treating at Sir Charles Gairdner Hospital.”
PAD is increasing worldwide with a prevalence that grew >20% over the past decade, with even steeper increases expected for the next decade because of the ageing population and the increasing prevalences of diabetes and obesity – not to mention the rise of smoking in developing countries.
“The rapid increase in diabetes as an accelerant of PAD is bringing it into focus more and more,” Dr Jansen explained.
“There's a significant overlap between PAD and diabetes but diabetes is slightly different because it also has a predilection for smaller vessels and the microcirculation which is why we see retinopathy and nephropathy for example, but also diabetic foot with ulceration and the need for minor and major amputation.”
“The amazing development we would like to share is that we think we might have a drug that can fix this problem,” Professor Hamzah said. “We actually designed this drug initially for treating cancer. We know that it can work in cancer by improving blood vessel circulation to increase drug uptake by tumours.
“We stumbled upon this while investigating a drug for older cancer patients with cardiovascular
comorbidities as cancer drugs nearly always cause cardiovascular issues. It was intended that we could give this drug in combination with cancer therapy to high-risk patients to improve safety and efficacy.
“And that's where Shirley and I have teamed up for the past 10 years. Our goal was to reduce the risk of vascular events, prevent amputation and reduce hospitalisation.
“Amputation is a major problem –some people would rather die than lose a leg. Australia has the second highest amputation rate in the developed world after the US.”
The past few years have seen the widening of the armamentarium of interventionalists from simple angioplasty, stenting, thrombolysis and open bypass grafting to endovascular devices such as atherectomy, laser, cryotherapy, ultrasonic ‘shockwave,’ drugcoated balloons and stents, and absorbable scaffolds.
However, although existing antithrombotic therapies can lower cardiovascular risk, their net effectiveness can be limited by bleeding complications, and while lipid-lowering medications such as statins are strongly recommended in global guidelines, they do not actually remove the build-up of plaque from the arteries.
“All have their advantages and limitations from not only the technology itself and its applicability but also the heterogenous nature of PAD lesion location, length, and calcium load,” Professor Jansen said.
“Similarly, all these invasive treatments are not curative but merely aim to treat crucial limbthreatening events, prevent new ones, or temporise symptoms in a population in whom the risk for needed repeat interventions is high.
“Even if you stop smoking, exercise regularly, are not overweight, manage your diabetes, take antihypertensives and aspirin and statins, or other drugs for your dyslipidaemia, there is still a significant residual risk, because none is curative. And we all know how difficult it can be for many patients to be compliant when taking multiple preventative drugs every day.”
continued on Page 19

continued from Page 17
About half of patients with symptomatic PAD require lower extremity revascularisation (such as bypass surgery, angioplasty with stent insertion, or atherectomy or thrombectomy) during their lifetimes, either electively to treat symptoms of severe claudication, or to save limbs in patients presenting with acute limb ischemia or CLTI.
“But counterintuitively perhaps, revascularisation does not improve overall vascular prognosis, as it does not address the underlying vascular risk. Indeed, there is an even greater risk for MACEs or MALEs in patients who have undergone revascularisation,” Dr Jansen said.
“Lipid metabolism is complex, and the lipid content of plaque is not only cholesterol,” Professor Hamzah elaborated.
“Once you have advanced disease, it’s already too late because lipids have accumulated in the arterial wall, and they are now complex lipids converted into esters from circulating lipids. They mix with glycogen, glycerol, and other compounds before being converted into solid crystals, for example.
“What is clear is that there is currently no drug that breaks down lipids once they are taken up by the cells, and there is no agent that can target lipids in the vessel wall specifically.”
Even though researchers have tried to target plaque previously, none have succeeded, she said, a factor that might be, in part, due to their lack of specificity to the foam cells in the plaque.
“We have patented a drug, developed here at the Harry Perkins Institute that is a reconstructed fusion protein, two proteins joined together, consisting of a biologic agent and ligand that has specific recognition to a receptor that is aberrantly expressed in lipidenriched cells (foam cells) in the arterial wall.
“Hence, this agent, once it enters the blood circulation, targets and accumulates in the arterial wall where lipid deposits and plaques are located.

“That chemical sensor is the key to targeting this drug effectively. It accumulates very well with an excellent biodistribution profile in plaque relative to normal healthy tissue. It congregates on those areas where it is needs to be, and that is exactly what we engineered it to do.
“We know by looking at Professor Jansen’s patient samples from surgery where patients have had plaques removed from their carotid arteries to prevent stroke, all of them seem to show recognition of this drug in lipid-rich regions.
“The original protein is actually naturally produced in our body. When we have a disease, this protein is produced in a high amount and acts on multiple cell types. We reprogram it differently to produce an exclusive effect on lipid-loaded cells, without toxicity. “Its action is highly reproducible throughout the entire arterial system, including the small vessels, and we now know how our drug triggers the cell to metabolise the lipids.”
Professor Hamzah explained that because this novel treatment works by breaking down the chemistry of the lipid itself, using its own processes to do so, the drug effect is specific to plaques.
“We have measured biomarkers for systemic toxicity, we've looked at changes in the arterial wall, blood pressure, etc. When we looked at the baseline clinical markers that we measure in patients who have problems with toxicity and also in a cardiovascular event (such as
creatinine kinase, Mvc2, and uric acid), we could see that the levels were the same as those for the healthy control group.”
The drug is currently undergoing regulatory requirements for approval and commercialisation, but once it is ready for release, both women believe that it could revolutionise treatment for PAD globally.
“Of course, the ideal scenario would be for humans not to get PAD in the first place. However, for those patients who progress despite risk factor management and healthy living, this drug could be an option,” Professor Jansen said.
“There's no reason to think that this could not be a GP prescribed drug, though it will definitely be in the domain of specialists to begin with.”
“The challenging part of bringing a new drug to market is convincing funding bodies that you have a strong contender,” Professor Hamzah explained.
“Even though this is a potential blockbuster, it was tough to convince ourselves and then other people that it was possible to safely and effectively dissolve atherosclerotic plaques. It took us 10 years to replicate the pre-clinical studies that work each time. Only now, I feel more convinced that it's not a fluke or chance.
“It's not completely 100% guaranteed, but it's a ‘first in class’ situation, there is nothing else to compare it with.
“We still have challenges ahead with the human protein – such as, how conserved is the effect of the drug in a human? So that’s our focus now.”
“All the medical management and procedures we have for PAD and CLTI are good, but they are not curative,” Prof. Jansen concluded. “We're thinking about applying the word cure to a pathology that has never had the concept applied to it. And, if it continues to prove itself, that will mean a dramatic difference to millions of people.”
Dr
is part of a new generation of doctors who love their career but are ferocious about making sure there’s also a life to go with it.By Ara Jansen


Armed with a sense of adventure and a passion for the buzz of an emergency department, Dr Brittney Wicksteed is forging a path in medicine which satisfies both her professional and personal goals. While probably a good example of her generation, Brit has taken the proverbial medical bull by the horns and is making it all her own. Recently turned 30, expecting her first child in May with husband Angus and named 2023 AMA Junior Doctor of the Year in WA, Brit firmly believes that work should fit into your life, not the other way around.
“I think it’s because we have seen our grandparents and our parents work so hard and deny themselves
so much,” Brit suggests. “There are all these things they wished they had done. I think if you can, make your work work for you.
“If you can work in a place that’s interesting and that facilitates your lifestyle, then you should do that. Healthcare workers are a valuable resource and it’s a good opportunity to craft your career or work into what you want to do.”
Born in Kalgoorlie, Brit lived in the Wheatbelt town of Quindanning (between Boddington and Williams) and then returned to the Goldfields, before going to boarding school in Perth. Growing up, Brit always thought she would be a vet. By high school, law and
medicine were on her mind. During mock trials she realised law just wouldn’t be right for her.
She took a gap year in Italy as an exchange student before starting an undergraduate degree in science majoring in biomedical science at UWA. It was her first time overseas.
“I had a desire to go and see things and to have some adventures, and going to Italy seemed like the easiest way to do it.”
When Brit started her medical studies, she never thought much about going to the country, despite growing up there, but had always thought she’d work in a city. She soon discovered that working and living in the regions was a perfect opportunity to explore WA’s amazing landscapes.
While doing medicine, her uncle (who is a nurse and paramedic), put her in touch with someone who worked in regional EDs around WA. She went to work with him in Augusta through the Rural Australia Medical Undergraduate Scholarship Scheme. That got her thinking –seeing more of regional WA might tick a number of boxes.
She spent six weeks in Kununurra on a placement program during her studies. In her third year she moved to the Kimberley and continued her studies through the Rural Clinical School of WA.
After graduating in 2018, Brit headed south for a two-year post graduate period at Albany Hospital, returned to the Kimberley for 2021, and in 2022 did a stint in Kalgoorlie. Back in Perth, she’s spent time at working Fiona Stanley and Royal Perth hospitals.
“Emergency medicine has always attracted me. People have different ideas of what it means to be a doctor and what their future would look like. For me it would be something where I can help in a situation and be capable of helping in any way.
“I like working in a team and having a challenging environment to do it in. I try and keep open to what options and experience differ lifestyles that come with different opportunities.

“I like being on my feet and moving around all day. I like teamwork and being able to share my decisionmaking and thought processes with those around me. I like the dynamic nature of how quickly things can change in medicine. I like being able to help make a difference in those first hours of care. You can make all the difference to people’s day, whether it’s a band aid or right up to life-saving care. It’s fun, I like fast work. It’s challenging having to come up with solutions on the fly.
“Sometimes it’s really hard, hard to know exactly what to do. Being a doctor is immediately gratifying

in many ways. You get to see the results right there in real time. There are so many skills you learn and so many ways to use them.
“Sitting in a desk in a clinic is not for me. I get too antsy. I would struggle to sit in a room on my own seeing patients. You get to see the same patients in a rural ED, and you have the ability to close that feedback loop more often. That’s the rewarding part of working in an ED in the country.”
Brit has been influenced in one way or another by all the rural doctors she has worked with, both as a student and as a doctor. What struck her during placements in the country hospitals was the level of happiness and vibrance of the environments. People were willing to have a laugh and knew their coworkers and patients on a personal level.
“Coming to Perth, I felt that people were not as obviously happy, and you didn’t know what their hobbies were. Hospital culture in the country is more social. You know what people like to get up to. There’s a real focus on work-life balance and making choices that are not career oriented but more personal.”
She says she doesn’t buy into the myth that working all the time makes you great at your chosen career. There has to be ample time for doing non-work, human things.
“I have come to understand that doing those things is as essential to being good at your job, being

continued from Page 21
happy, giving good care to your patients and yourself.”
She’s currently working as a registrar doing a five-year ED training program and is just shy of her first 12 months. As she can do it anywhere in Australia and New Zealand, Brit isn’t locked into one hospital. She plans on breaking up the time across a number of different hospitals, and hopefully locations, to gain a breadth of experience so she “can enrich my future workplaces with new and innovative ideas”.
“I’m not rushing. I was having too much fun doing resident jobs and learning different skills before I stepped up to registrar last February. It’s a slow entry compared to a lot of my colleagues. In a career of 30 to 40 years, what’s five?
“Things are slowly changing and there’s now a bit more importance placed on life experience, not just work experience. The importance of being able to structure your work around your life and take time off is why part-time work appeals to me. I see it as map-your-ownadventure.”
Brit is a fan of small gaps and trips, and often. Amongst her friends, she says she’s not alone in this thinking. She and Angus took six months off at the start of 2022, which comprised five weeks in Tasmania and the rest of the time in Europe, working their way through Spain, Croatia, Montenegro, Italy and the UK. She’s made the most of her time in the regions to explore as well, and professionally had the opportunity to visit a couple of Aboriginal communities.
“I met some special people on those communities and got an insight into a life not many people have the privilege of seeing. It’s really important not just for the experience of seeing it, but it gives me some common ground with patients I might see in the future and some appreciation of the challenges they have coming to the city.”
The crazy hours of medicine can be a barrier to finding a partner or

having a family and Brit has seen it among her friends as well. But they share her philosophy that the job as the be all and end all is not how they are choosing to live their lives. They are not resigned to being a doctor on an endless treadmill of work and burnout in an underfunded system.
Determined to do something about it, while working in Albany, she set up and ran a junior doctors society and later one in Broome as well. It’s a forum to raise issues in workplaces – such as improving rosters – in a collegiate space and allows them to be heard.
This has succeeded in bringing junior colleagues together, helps make the workplace more cohesive and creates a sense of camaraderie in a group which is often transitory. She also says it’s the perfect forum to share career choices and how other young doctors are coping with that work-life balance.
In 2020, Brit married Angus, a primary school teacher. Two of the women she met through RCSWA were bridesmaids, testament to the strength of the bonds Brit has made while working regionally.
The pair met at university when Brit decided to take up a new sport and one which had never really been available to her growing up inland –rowing. They connected in the first couple of weeks and the pair has been inseparable since.
Brit calls her husband a city boy who loves spending time in the country. They have a similar sense of adventure, and he doesn’t mind being uprooted and learning new skills for new living locations.
Eventually she’d like to find her way back to Albany – the climate, lifestyle and proximity to Perth tick all the boxes. They keep an eye on real estate, looking to find their dream home.
Together they like to camp, do gentle hikes and explore wherever they are. Good food and wine are usually involved, especially in the Great Southern. In Perth they live close to the beach, have been surf club members for nine years and row surf boats. When not swimming together, they run, and Angus has competed in a number of half Iron Man triathlons.
“I love to have a community of people who love to be outdoors and get involved in activity. Angus’ sisters are part of the same club, so there’s a bit of family rivalry going on.
“Not everyone you need to know in life is from the four walls of a metropolitan hospital. There’s more to be learnt outside the city than people give it credit for. Also, growth happens outside your comfort zone. If you’re always comfortable, you’re not challenging yourself or getting the most out of what life offers.”

As the science of sleep develops, so, too, do the business opportunities and the confusions and pitfalls of what works.
It occupies about one-third of our lives and is considered a natural bodily function like breathing. But for something that should happen with minimal effort, sleeping (or the lack of it) has become big business, with a recent explosion in self-help books, tracking apps and TV documentaries.
Increasingly we are warned about the risks of being sleep-deprived –with the acute effects likened to the impaired function and reaction time of a drunk driver, and that is before we get to the long-term effects on blood pressure and cardiovascular disease.
But people who struggle to sleep at night might argue this message only adds an extra layer of stress, as they become more anxious
By Cathy O’Learyabout not getting enough shut eye, perpetuating the insomnia cycle. Still, a good night’s sleep is considered a restorative process for our body, particularly for the brain by helping our memory, learning and mood.
Sleeping less than six hours on average a night is associated with increased mortality risk and health conditions including hypertension, obesity and heart disease. Less than seven hours has been linked to digestive and neuro-behavioural problems.
Sleep disorders are varied, even within the umbrella of insomnia. For some people, it means difficulty falling asleep, while for others, dozing off is easy enough but they face the dreaded wake-up at 2am, leaving them unable to go back to sleep.
The result can be feeling fatigued and exhausted during the day, and this can go on for months or years, with about 15% of Australian adults stuck with chronic insomnia.
That sleep-deprived pain has fuelled a lucrative sleep health economy, with the sleep aid market reportedly worth about $65 billion a year in the US alone.
And in the digital age, tiredness has become the new norm, with companies selling aids from spooning robots and sleep trackers to calming blankets and hi-tech pyjamas with bioceramic material that is said to absorb the excess body heat that can be an enemy of sleep.
There is also a high-speed sleep research industry, as doctors and
others try to find ways to help people get enough nods.
And the multi-million-dollar question is always – what actually works?
Advice for insomniacs can include anything from avoiding late-in-theday caffeine to using breathing exercises, calming music or white noise, going to bed in a dark and quiet bedroom, and eating different foods in the evening.
Experts believe that if symptoms have lasted more than one or two months, it is likely the insomnia requires targeted treatments that focus on sleep patterns and behaviours.
Non-drug therapy such as cognitive behavioural therapy for insomnia (CBTi) has been shown to be more effective than sleeping pills. It involves education about sleep and offers psychological and behavioural treatments that address the underlying causes of long-term insomnia.
It can be done one-on-one or in small groups and is also offered online.
Some GPs are trained to offer CBTi, but it is more usual for specialist sleep psychologists to offer it. About 70-80% of people with insomnia are reported to sleep better after treatment, with improvements lasting at least a year.
Perth sleep researcher
Dr Jen Walsh PhD, director of the Centre for Sleep Science at the University of WA, said insomnia was the most prevalent sleep disorder seen in people going to visit their doctor.
• try to maintain a sleep schedule that is enough to feel adequately rested, by keeping a fixed wake-up time, even on weekends, and going to bed when you feel sleepy.
• for those who have unavoidable changes in sleep routine such as shift work, catch-up sleep is recommended.
• people who feel like they might not be sleeping enough, especially those sleeping less than seven hours, could test whether allowing a longer sleep schedule or naps helps them sleep longer and results in them feeling more rested.
• for those without a sleep disorder, following good sleep hygiene can still have benefits, such as avoiding caffeine and alcohol in the afternoon and avoiding a heavy meal close to bedtime.
• people should be encouraged to talk to their GP in the first instance if they are concerned about their sleep. Treatment options are available through referrals to sleep specialists for a variety of sleep disorders such as sleep apnoea and insomnia.
• spending more time in bed often results in more time spent awake in bed, which can make insomnia patterns worse.
• drinking coffee and taking naps might help get you through the day but can make it more difficult to fall asleep in the evening.
• drinking alcohol might help people fall asleep quicker, but can cause more frequent awakenings, change how long they sleep and reduce the overall quality of sleep.
are positive, but some outcome measures were positive, and that somewhat aligns with other studies that have included THC,” she said.

The explosion in reported insomnia has fuelled hundreds of studies looking at the use of possible sleep aids such as cannabinoids and melatonin, but the results so far have been a mixed bag.
Anecdotal reports of benefits from cannabidiols and THC did not necessarily align with some clinical trials which had not shown them to be effective.
“I’ve been involved in studies with THC, and not all findings
“One of the factors here could be the dose, because all the studies are looking at a dose of 150mg per day, which is what is approved by the TGA to be available over the counter as Schedule 3 (no prescription), and the companies want to capitalise on that opportunity so that’s what they’ve been using.
“And maybe that dosage is inadequate, although anecdotally prescribers will say patients report improvements in sleep with lower doses.”
Dr Walsh said another confounding factor could patient selection, with people not necessarily using CBD to treat a sleep problem or insomnia.
“It might be for pain or something else, but then they’re reporting an improvement in sleep. That might be why we’re not seeing
improvements in people just with insomnia – maybe it works with comorbidities such as pain,” she said.
She said there was also a question mark over the use of melatonin, a natural hormone released by the brain each night in response to darkness. While it is available on prescription in Australia, people aged over 55 can buy packs of 30 tablets over the counter from pharmacies.
A growing number of people are bypassing the need for a script by buying the supplement online from overseas. Some parents give it to their children, despite any evidence, as its benefits appear limited to older people who can end up with depleted levels of melatonin as they age.
“There have been quite a few studies looking at the effects of melatonin on sleep in people with insomnia or other sleep disorders, even jetlag, so lots of studies in specific populations,” Dr Walsh said.
“Therefore, there’s been metaanalyses which are interesting continued on Page 26
continued from Page 25
because they’re variable, so that’s really challenging.”
Dr Walsh said the value of melatonin might depend on the population it was being used in, and the formulation.
“In Australia, what you can buy at the chemist is modified, or slowrelease, so it takes a few hours to reach its maximum concentration. So if someone is having trouble falling asleep, then that’s not going to be that useful for them. It’s going to help people who have some sleep maintenance issue,” she said.
“And if you get the tablet form and crush it and destroy the shell and coating, that will modify it, and its bioavailability increases in the short term.
“The research that’s been done is a mixture of looking at quick-release and prolonged-release products, or unspecified release, so if you’re looking at outcome measures such as time to fall asleep versus total sleep duration or the amount of time awake during the night, it’s going to be influenced by the product used.”
The added complication was people buying melatonin from overseas and self-medicating, without necessarily telling their GP.
“If it actually has sleep benefits, then it would have sedative or hypnotic properties, and of the available hypnotics traditionally used or prescribed, it would be one of the safer ones,” she said.
“But the problem is that people are self-treating and very likely it’s not the best treatment option for them. For someone with chronic insomnia, cognitive behavioural therapy is the best treatment, so that is one of the concerns with melatonin being more readily available.”
Dr Walsh said melatonin could also interact with other medications such as anticoagulants, potentially impacting their effects.
An analysis of 31 different supplements available online showed that the amount of

melatonin ranged from minus 83% up to 478% of what was written on the packs, which stated doses of 1mg to 10mg, with the higher discrepancies in the lower doses.
“The rate of melatonin use in children has really spiked too, and that in itself sets kids up to think it’s not harmful and also gives them a belief that you need to take a pill to sleep,” she said.
What the evidence did show clearly was that CBTi worked for insomnia.
“Hopefully, we’re getting that message out there, but the problem is that it is typically done with a specialist sleep psychologist, and there’s just not enough, there are only about 35 in Australia.
“There is online CBTi, and for bread-and-butter insomnia that’s probably OK, but if you have any other co-morbidities, perhaps a mental health disorder or some PTSD, or someone does shift work, then it’s just not appropriate.
“But there are a lot of people working in this area, trying to progress and improve access.”
Despite negative publicity about sleeping tablets, Dr Walsh said there was a place for them, when used selectively rather than as a regular go-to.
“If someone goes in and presents after poor sleep for at least three months, CBT is the best line of
treatment. But if someone is in an acute situation, a death in the family or a relationship break-up, then that’s when you go with the medication, because they might have trouble sleeping, it might be for a week or two weeks. It is enough for their body to get used to them not sleeping, being awake in bed, and then they start worrying about the fact that they’re not sleeping.
“But if you can circumvent that with medication, and intervene, that’s where the medications have value.”
For some people, such as those with asthma, being sleep-deprived can be even more risky. Last month, the National Asthma Council Australia released a new health professional resource outlining steps to treat patients who present with poor asthma control and sleep disturbance.
Respiratory medicine and sleep disorders physician Associate Professor Greg Katsoulotos said it would help when patients with asthma reported persistent nighttime cough.
“Asthma symptoms during sleep or on waking indicate suboptimal asthma control and frequent nocturnal symptoms indicate increased risk of acute asthma exacerbations and should not be accepted as normal,” he said.
“The resource recommends that health professionals should
consider stepping up asthma treatment with anti-inflammatory therapy in a patient with sleep disturbance due to asthma symptoms.”
Nighttime cough could occur with or without wheeze and be a sign of poor asthma control that needed to be addressed, with the patient who might think their cough is due to an infection.
Research continues
Meanwhile, numerous studies are still underway to find the Holy Grail of sleep remedies.
Last month, in a world-first, Australian sleep experts were given just eight weeks to develop and run a sleep treatment program that diagnosed and treated more than 30 volunteers and achieved a success rate of more than 80%.
Lead researcher Professor Danny Eckert and a team from Flinders University used cutting edge technology and
personalised clinical methods to conduct a rigorous clinical trial and treat sleep disorders through the science of sleep.
The findings are featured in the SBS documentary series Australia’s Sleep Revolution with Dr Michael Mosley, in which the medical journalist and chronic insomnia sufferer – along with politicians Barnaby Joyce and Jacqui Lambie –took part in the trial which focused on the most common sleep disorders – insomnia and sleep apnea.
Professor Eckert said people should be aware of the short- and longterm health effects of bad sleep, ranging from high blood pressure to increased risk of cardiovascular disease, stroke, diabetes, depression and chronic disease.

After participants had their sleep tracked, weekly multidisciplinary team meetings with sleep scientists, doctors and psychologists were held to tailor treatments for each person. The scientific findings will soon be published in detail in an international peer reviewed journal.
Earlier research by Flinders University found that getting the recommended 7-9 hours of sleep a night was out of reach for almost one-third of the population.
Resources
Primary care practitioners wanting evidence-based information about diagnosing and managing people with obstructive sleep apnoea and insomnia – the two most common sleep disorders – can go to www. sleepprimarycareresources.org.au
The Sleep Health Foundation has fact sheets aimed at the public but could be useful for physicians wanting to refer their patients
www.sleephealthfoundation.org.au
For more advice about dealing with sleep disorders in people with asthma, go to www.nationalasthma.org.au
Living Diabetes & Endocrinology is WA’s first integrated, comprehensive care centre for people living with diabetes and other endocrine and metabolic conditions delivered by a team of experienced endocrinologists and skilled allied health professionals including:
Endocrinologists
Exercise physiologists Podiatrists
Diabetes educators Psychologists and other allied health professionals
Dieticians
Centrally located in Osborne Park with free parking, Living Diabetes is the vision of one of Perth’s most experienced diabetes specialists, Dr Joey Kaye, providing care for adult patients with all forms of diabetes including GDM, pre-diabetes and cardiometabolic dysfunction. We are also accepting referrals for all forms of general endocrine conditions.

Rapid access for new patients from March 2024 and on-going urgent referral slots
Email: admin@livingdiabetes.com.au Phone: 08 6374 6438
Learn more at www.livingdiabetes.com.au and find out more about our GP education program
Please book a place for the conference at gpurologymasterclass.com.au
Limited

With
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
Healthcare fraud is on the rise so it has become a numbers game, according to Australian experts
Jayesh Kapitan and Roger Darvall-Stevens
Healthcare fraud is increasingly draining resources and compromising patient safety, with identity theft and cyber fraud the biggest issues.
The lucrative nature of health data makes the sector an appealing hunting ground for fraudsters, with the potential to compromise patient data, disrupt critical services and impose substantial financial burdens.
In RSM Australia’s recently-released white paper Healthcare in Australia – A Growing Fraud Trend, we explored the impact of fraud and the standards required to prevent, detect and respond to risks of fraud, theft and corruption.
Australia’s healthcare system is a complex mix of public and private funding sources which creates fraud opportunities, as billing and reimbursement processes can be challenging to navigate and to monitor effectively.
Healthcare fraud can take various forms, including billing for services that were never provided, falsifying patient records, kickbacks and pharmaceutical fraud. However, the sector’s two biggest fraud issues are identity theft perpetrated via cyber-attacks, along with cyber fraud via false invoice, where criminals prey on unsuspecting, and often very busy, staff.
It’s a numbers game. Fraudsters might send thousands of false invoices and only need a few to be paid to make it worthwhile for them, but this one lapse in vigilance can damage a healthcare organisation’s reputation and trust.
About 11% of Australian cybercrime reports originated from Western Australia in 2022-23, according to the Australian Signals Directorate’s Cyber Threat Report 2022-23, while, according to the Office
of the Australian Information Commissioner’s Notifiable Data Breaches Report: January to June 2023, healthcare was the most targeted sector for data breaches in that period, with 15% of all reported breaches occurring in the sector.
It's therefore crucial for healthcare organisations and practitioners to put in place robust processes and, even then, the most robust systems can be bypassed by human error.
Staff training and awareness programs go hand in hand with robust processes and ongoing proactive measures to mitigate fraud risks.
When it comes to fictitious invoices, some look authentic and that's where controls are needed. If you get an invoice without a purchase order or supporting documentation included, then that invoice should be investigated before being processed.
As reliance on electronic health records increase and sensitive patient information is shared amongst providers, cybercriminals target these records through tactics like ransomware attacks, data breaches and phishing schemes. Scamwatch reported ‘phishing’ as the leading scam category in 2023.
A breach of electronic health records not only jeopardises patient privacy but also has the potential to lead to identity theft, fraudulent medical billing and unauthorised access to prescription medications or government benefits, causing serious harm to individuals.
Concerningly, the growth of telehealth appointments, has opened new avenues for fraudsters to impersonate healthcare providers or infiltrate video consultations.


Our healthcare sector must remain vigilant in bolstering its cybersecurity measures, training staff to recognise cyber threats, and adopting robust encryption and access controls to mitigate these cyber-fraud risks and ensure the integrity of healthcare services and patient data.
There is even risk involved in the use of IoT sensors embedded in medical devices. If not secured, these devices can be easily hacked and tampered with, so ensure to focus on basic cyber security controls such as:
Inventory – know what connected medical equipment you have in use so you can secure them.
Password security – change all default usernames and passwords. Use secure passwords and if possible, enable two factor authentication. Unless needed, disable internet and remote access to these devices or allow them only on an as-needed basis.
Updates – keep the device firmware and other software updated to protect them from cyber vulnerabilities.
Backup – backup all configuration data regularly or whenever changes are made to have a ‘Plan B’ in case of a malware infection.
The Australian Standard AS 8001:2021 Fraud and Corruption Control has been the national pre-eminent guide for government and corporates on how to prevent, detect and respond to to risks of fraud and corruption. The key is implementing a robust antifraud program, creating and regularly updating policies and procedures that clearly outline the organisation’s approach to fraud prevention and detection.
ED: Jayesh Kapitan and Roger DarvallStevens work for RSM AustraliaE/Prof Odwyn Jones looks at the evidence of a link between poor air quality and cognitive decline, with our children being most at risk.
Those of us who have had the misfortune of seeing one of their loved ones suffer from Alzheimer’s dementia, know of its destructive effect on their stored knowledge, including their language and thinking skills.
However, how many of us know that more than 2000 children are affected by this terrible disease?
The Childhood Dementia Initiative recently released its world-first report on the State of Childhood Dementia 2022. In it, the organisation’s CEO, Megan Donnell, stated that the report showed that action to date in this area had been grossly inadequate, and was especially evident when assessing the action being taken with other comparable diseases.
As the report states, there are no effective treatments or cures for most childhood dementia disorders, which affect some 700,000 children globally and 2273 in Australia, with an incident rate of one on 2800 births. It highlighted that the number of clinical trials focusing on childhood dementia was considerably less than those dealing with cystic fibrosis (18 times less) and childhood cancer (12 times less).
As Ms Donnell states, when you consider the severity of childhood dementia, the number of children affected, their short life expectancy and the trauma of their families having to watch their children fade away, the inequity and neglect of this patient group is self-evident.
The report also highlights that childhood dementia does not feature in any major action plans and policies, including the WHO Global Action Plan on the public health response to dementia, 2017-2025, nor on the national dementia plans developed by WHO member states.
The report, however, recommends making childhood dementia a health priority, incorporating it into
local, national and global dementia protocols, policies and strategies.
As quoted at the Alzheimer’s Association International Conference (AAIC 2021): “Previous reports have linked long-term air pollution with accumulation of Alzheimer’s disease-related brain plaques, but this is the first accumulated evidence that reducing pollution, especially fine particulates in the air, and pollutants from the burning of fossil fuel, is associated with lower risk of all-cause dementia and Alzheimer’s disease”.
Further, the same media release states that: “While research has linked air quality and cognition previously, these new data at AAIC 2021 explore how air pollutants might impact dementia and what reducing them might mean for long-term brain health.
Among the key findings was evidence that long-term exposure to air pollutants was associated with higher beta amyloid levels in the blood in a large U.S, cohort, indicating a possible biological connection between air quality and physical brain changes that define Alzheimer’s disease.
In 2017, the Guardian Weekly newspaper highlighted that “tens of thousands of children at more than 800 schools, nurseries and colleges in London were exposed to illegal levels of air pollution that could cause lifelong health problems.” London’s mayor, who initiated this study, said that its outcomes were devastating with the city’s poorest inevitably bearing the brunt of this challenge.
A month or so later, the same newspaper referred to the UK government’s modelling, based on data obtained in 2015, which emphasised “that pollution from diesel traffic is not limited to large metropolitan centres, but threatens the health of children and young people in towns and cities

nationwide.” This study’s purpose was to identify schools and nurseries within 150m of a road where the emissions of nitrogen dioxide (NO2) exceeded the EU legal limit of 40mcg per cubic meter of air.
This study’s findings were horrendous, with more than 2000 schools, nurseries, further education centres and after-school clubs throughout England and Wales identified as being within 150m of roads with illegal NO2 levels.
Based on these findings Professor Chris Griffiths of Barts Hospital and London School of Medicine said: “Research on exposure to traffic fumes and children’s lung growth shows that such exposure reduces lung growth, produces long-term ill-health and can cause premature death. We should be outraged that we are exposing our developing children to these obvious problems.”
In another scientific paper (Calderon-Garciduenas et al, 2014) the authors stated that “millions of children in polluted cities are showing brain detrimental effects” and that “protecting children and teens from neural effects of air pollution should be of pressing importance for public health”.
Such detrimental effects include “decreased cognitive function across assessments of verbal and non-verbal intelligence and memory in nine-year-olds.”
According to numerous scientific authors “an intriguing association has also been identified between autism spectrum disorders including, attention deficit hyperactive disorders (ADHD), and particle air pollution.
At about the same time, the Air Quality Group’s Report of the UK’s Department of Environment, Food and Rural Affairs concluded that there is “strong evidence” that diesel powered vehicular emissions affect the cognitive function of children.
Furthermore, earlier research
studies carried out by the University of Southern California, published in the Journal of American Medical Association (2013) concluded that children exposed to high levels of such pollution were three times as likely to have autism, compared with those living in pollution-free environments.
Following the London study of air pollution at nurseries, schools and colleges, the Mayor concluded by stating: “this is an environmental challenge, a public heath challenge, but also – and no one talks about this – it is fundamentally an issue of social justice, because if you are a poor Londoner you are more likely to suffer from illegal air.”
The CO2 factor
Increasing levels of carbon dioxide in the air we breathe not only affects our climate, it also clouds our thinking. Indeed, it is claimed that at levels of 1000 ppm of CO2 , human cognitive ability is reduced by 21%, and as the researcher, P.N. Bierwirth, of the Australian National University states:
“There is general agreement

that levels of CO2 in 29-50% of classrooms commonly exceed 1000ppm and are often very much higher, sometimes reaching levels as high as 6000ppm for extended periods.”
Kindergartens, offices, high schools and universities are also known to have levels of CO2 similar to those in classrooms, depending on the number of persons present and the ventilation system in use.
According to another article (Bierwirth P.N., 2018) “as atmospheric levels of CO2 continue to escalate and drive climate change, the potential impact of CO2 on human cognition, whilst not currently perceived as a global risk, increases outdoor levels of CO2, which add to indoor concentrations (by ventilation), rising to levels higher than those which produce impaired thinking and reduced intelligence.”
It is vitally important for those responsible for the health and wellbeing of the general public, particularly young children and youths, realise the health risks of
inhaling diesel-powered engine exhaust fumes over long periods.
Whereas most Australian cities are not in the same league as the numerous megacities overseas, the fairly recent modelling of the situation in the UK indicates that many smaller cities and towns suffer illegal levels of vehicular traffic pollution.
It therefore behoves us as a civilised nation to do what we can to ensure the health and future wellbeing of all citizens, be they near freeways or in occupations where they may be exposed, in particular to diesel engine exhaust fumes, regularly for long periods.
This applies especially to our children and youths, whose home and learning environments should, ideally, be located where the breathable air is guaranteed to be of satisfactory quality.
As Dr Maria Neira, WHO Director of Public Health states, “the scourge of air pollution in increasingly affecting all of us, but children are the most vulnerable, and this should be very worrying to us all”.

Our state-of-the-art laboratory is equipped with cutting-edge technology to improve your chances of achieving a successful pregnancy.

We offer a comprehensive range of fertility services, such as Ovulation induction (OI), Intrauterine insemination (IUI), In-Vitro Fertilisation (IVF), Intracytoplasmic sperm injection (ICSI), frozen embryo transfer (FET), egg freezing and sperm freezing.
Our fertility specialists also perform a wide range of fertility related surgeries to address issues like endometriosis, fibroids, uterine septum, tubal disease and caesarean scar defect.
We offer bulk billing for all Medicare eligible items. For additional services we provide transparent pricing with no hidden fees or surprise costs.
Holistic approach
We understand that the journey to parenthood can be emotionally challenging, which is why we offer ongoing emotional support and counselling services throughout the treatment process. Our compassionate team of health professionals are available to provide support with the emotional aspects of infertility and IVF, ensuring that you feel cared for every step of the way.
Video consultation
Our video consultation service is available at no extra cost for those who are unable to attend consultations physically.
Convenient locations
Oasis fertility centre has created two state of the art beautifully designed practices to best facilitate the fertility journey at South Perth and Warwick.
South Perth
Phone: 1300 241 654
Email: admin@oasisfertilitycentre.com.au

Dr

Dr

Dr

Dr
oasisfertilitycentre.com.au


In medicine we are supposed to be scientific and questioning. Yet in reality there is often remarkably little questioning of any treatment or approach which becomes ‘orthodoxy’
The medical profession is not immune to societal trends, one of which is living in echo chambers where the only people you interact with are those who you agree with 100%.
I was thinking about this after listening to Chris Cuomo talk about his discussion with Tucker Carlson. These two people are from very different points on the political spectrum. Cuomo began by saying that the establishment hates it when people from different ‘tribes’ talk to each other. Essentially, he felt that divide and conquer was the approach and that many preferred to silence opponents than have debate.
In medicine we are supposed to be scientific and questioning. Yet in reality there is often remarkably little questioning of any treatment or approach which becomes ‘orthodoxy’. Without expressing a view one way or the other, transgender care is a good example. Those who do not fully support affirming care as the only treatment for gender dysphoria are often silenced or sacked.
In March the UK NHS, which was early into this field, announced, “we have concluded that there is not enough evidence to support the safety or clinical effectiveness of [puberty blockers] to make the treatment routinely available at this time”. Going forward they will only be prescribed in clinical trials. This followed recommendations by paediatrician Hillary Cass, who conducted a review of the Tavistock clinic. Scandinavian countries have also significantly changed their approach.
A week earlier, leaked documents cast questions over the operations of World Professional Association for Transgender Care (WPATH). I encourage readers to examine the WPATH files online.
The response to the UK announcement here was essentially silence or “we are doing a great job”. Maybe we are. If so, it should welcome scrutiny.
To quote Charles Kettering: “The world hates change, yet it is the only thing that has brought progress”.
Without being questioning, we would still use leeches and not wash hands before delivering babies. Yet as Semmelweis was castigated for questioning beliefs of the time, we find that it remains not that popular today and certainly wasn’t during the response to the COVID 19 virus. Ask Professor Martin Kulldorff, sacked from Harvard Medical School for questioning lockdowns.
Why is that? Why can’t we debate anymore? Why do we demonise those with differing opinions and label them as purveyors of ‘misinformation’ or ‘hate’. Something for us to ponder.


Many trials are published each year, and it can be hard to keep up with their results and separate the proverbial wheat from the chaff. These are my takes on some major trials from last year.
Semaglutide 2.4mg in a large 17,604 RCT with established CAD, without diabetes and a BMI greater than 27 showed a 20% reduction in CV death, non-fatal MI or non-fatal stroke at a mean follow-up of 40 months. Oral Semaglutide is now available in other countries with similar HbA1c reductions compared to liraglutide with greater reductions in HbA1c compared to SGLT2 antagonists.
Greater weight loss was achieved with Semaglutide compared to liraglutide. Downsides include GI intolerance and cost. The recently published results of the SURMONT-4 withdrawal trial underscores the challenge of weight regain when the drug is stopped.
Two meta-analyses have shown that Tirzepatide (dual GLP-1 and GIP receptor agonist) to be more effective in weight loss. We eagerly await trials on Tirzepatide demonstrating CV protection.
These two trials have challenged the idea of anticoagulation in patients with subclinical AF


detected on implantable cardiac devices.
NOAF-AFNET randomly assigned
2500 patients over the age of 65 lasting for at least six minutes detected by cardiac implanted devices who had at least one additional risk factor for stroke. The mean duration of AF was 2.8 hours. The trial was stopped early at 21 months because of perceived excess bleeding in the Edoxaban arm (31% increased risk, or 5.9% per patient-year vs 4.5% per patient-year). There was a small 19% reduction (4% vs 3.2% per patientyear) in the primary endpoint of
Pathologists have reported a significant increase in reproductive carrier screening in Australia but are urging doctors and patients to consider testing sooner.
The Royal College of Pathologists of Australasia said there had been a significant increase in the uptake of reproductive carrier screening
for cystic fibrosis, spinal muscular atrophy and Fragile X syndrome since the service was added to the Medicare Benefit Schedule last November.
Between November and December 2023, the number of tests requested under item number 73451, for people who are pregnant
stroke, systemic embolism and CV death.
ARTESIA randomly assigned 4000 older patients with a short-lived device detecting AF to apixaban vs aspirin (median duration, 1.5hours). After 3.5 years, Apixaban reduced the primary endpoint of stroke and systemic embolism by 37% (0.78% per patient-year vs 1.24% per patient-year) but increased major bleeding by 80% (1.71% per patientyear vs 0.94% per patient-year).
Both trials demonstrated a reduction in thrombotic events but an increase in bleeding rates. The biggest discovery was the
or planning pregnancy, jumped from 1726 to 6980.
But despite the promising uptick in testing, the college has raised concerns that most people are opting for the test after they are already pregnant, limiting their reproductive options.
Obesity poses a significant challenge, and it is crucial to underscore the numerous benefits offered by GLP-1 agonists
Not all AF is the same and those subclinical episodes detected on devices seem to confer a low stroke rate. Analysis correlating duration and net clinical benefit of anticoagulation is needed PCI can be offered for stable coronary artery disease for symptom relief particularly those who fail medical therapy or are intolerant of medications.
low stroke rates in both trials. What we need now is an analysis correlating duration of AF and net clinical benefit. Some experts have suggested using 24 hours as a cutoff.
This trial randomised 300 patients with stable coronary artery disease without antianginal therapy to Percutaneous Coronary Intervention (PCI) or placebo-PCI (sham control arm).
Not surprisingly, the mean anginal symptom score was significantly lower in the PCI group.
Longer term data on TAVR (Transcatheter aortic valve replacement) in low-risk surgical patients were published. In the PARTNER 3 trial of balloon expandable TAVR, the shortterm benefit of TAVR neutralised over time. Death, stroke and rehospitalisation were all similar and valve haemodynamics matched those of surgical implanted valves. There was more aortic regurgitation in the TAVR arm.
The Evolut low risk four-year results for self-expandable TAVR still demonstrated a benefit for death and stroke compared to SAVR (Surgical aortic valve replacement). Valve haemodynamics were also better in the TAVR arm. New permanent pacemaker rates remained higher in the TAVR arm. Both trials will continue to follow patients.
It is hard not to be impressed with
the technological advancements in the transcatheter aortic valve space and it will be interesting to see the results of the seven and ten-year follow-up.
This trial randomised 14,000 patients at increased CV risk, who were intolerant or unwilling to take statins to Bempedoic acid vs placebo. At a median duration of 40.6 months, there was a 0.75mmol/L reduction in LDL. There was a 13% relative reduction in death, MI stroke and revascularisation – 1.6% absolute risk reduction. This gives us another alternative to those who are unable to take statins. Other options now include Inclisiran (awaiting large ORION-4 trial) and oral PCSK9 inhibitors (showed good reductions in LDL in phase 2 trial).
Author competing interests
Osteoarthritis (OA) is a major cause of chronic knee pain and disability with a reported prevalence of 25-30% of the population over 60 years of age. While traditionally thought of as a purely degenerative disease related to “wear and tear”, the pathophysiology of OA involves a complex interplay of mechanical, biological, and molecular factors leading to inflammation, pain, and structural degeneration.
Current treatments focus on symptom management (pharmacotherapy, physical therapy, surgical interventions). Geniculate artery embolisation (GAE) has emerged as a novel, minimally invasive endovascular procedure aimed at reducing articular inflammatory symptoms associated with OA.
Evidence is increasing that GAE can significantly reduce symptoms, postponing or delaying the need for total knee replacement (TKR). There is also an increasing role evident for GAE in suboptimal functional outcomes following a TKR where a similar inflammatory paradigm is thought to exist. This occurs on the background of a longstanding role of GAE in post TKR haemarthrosis.
Inflammatory mediator cascades induced by OA drive inflammatory pathways including abnormal articular and synovial neorevascularisation (NSR). This angiogenesis has been linked to inflammatory changes to the articular surfaces and synovium, osteophytes, cartilage degeneration, and neuro-sensitisation.
Apart from driving ongoing OA degeneration, the synovial and articular angiogenesis and associated inflammation is thought to be a functional source of pain, swelling,
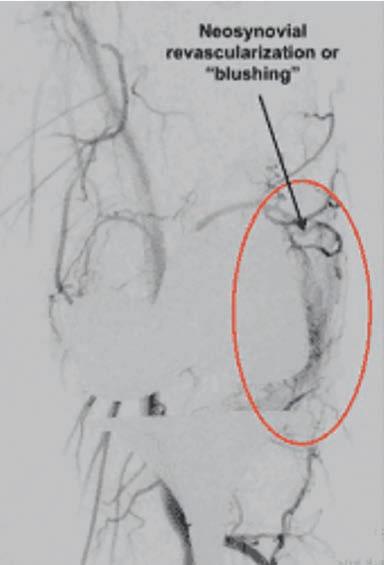
haemarthroses and stiffness.
GAE is thought to mitigate this abnormal angiogenesis, slowing the inflammatory OA drive, thus slowing the progression of degenerative OA changes and reducing symptoms.
GAE is not an isolated treatment option and needs to be considered as part of a tailored comprehensive approach, in close liaison and coordination with orthopaedic surgeons and other musculoskeletal physicians. It appears to have a greater role in mild to moderate OA compared to severe/end-stage as an adjunct management option between conservative management (e.g. physiotherapy, articular injections, pain management) and surgical intervention. This is of benefit in patients wishing to delay a TKR or patients deemed young or of “high risk” for TKR.
Over 60,000 knee replacements are conducted in Australia annually, with variable reports of suboptimal



functional outcomes of 5-18%. While the cause of suboptimal TKR is complex, including mechanical, prosthetic or infective issues, a similar inflammatory paradigm of synovial inflammatory revascularisation and angiogenesis has been theorised.
GAE has developed an increasing role in treating pain, stiffness, haemarthrosis and swelling in patients with no clear mechanical cause who otherwise are looking at a revision TKR or conservative management.
GAE is a low-risk, minimally invasive, percutaneous endovascular procedure conducted under local anaesthetic and sedation. Under angiographic guidance, the geniculate arteries (vessels perfusing the knee arising from the femoral artery) are assessed for typical hypervascular inflammatory synovial blush consistent with inflammatory NSR.
Aside from degeneration, OA has an inflammatory component
Geniculate artery embolisation may be an intermediate option between conservative and surgical management
While still regarded as novel, evidence is mounting to support a role for GAE.
While in some cases inflammatory synovitis can be seen on preprocedure MRI/MRA or SPECT imaging in native knees, it is not always consistent with NSR and is of limited diagnostic benefit. These modalities have limited merit in the setting of an existing TKR. If NSR is identified on the global or selective geniculate angiogram, the NSR is accessed via microcatheterisation via the feeding geniculate artery and embolised using microspheres or liquid embolic agents such as Medtronic Onyx. Coil embolisation is ineffective.
This aim is to treat NSR directly while minimising embolisation of
geniculate vessels themselves. Multiple geniculate arteries are often needed to be catheterised as the NSR is often multifocal and multisourced. Procedure times are approximately 45-60 minutes as a day case or overnight stay with an average return to work within 4-7 days. Maximum benefit is seen after three months.
Technical success has been documented as 99.7%.
Complications include groin access complications, non-target embolisation resulting in transient skin ischaemia (5-10% cases), which in almost all cases is selflimiting, temporary worsening of patient’s knee pain (10% cases) over 2-3 weeks and extremely rare complications such as osteonecrosis and distal embolisation.
The outcome of GAE in native knees in trials and meta-analysis (over 174 papers some with sham arms) showed robust results. Studies demonstrated statistically significant outcome measures and clinically important benefits at all follow-up intervals to 24 months. At two years, only 8.3% of cases required re-intervention with GAE,
and 5.2 % underwent a TKR.
In post knee replacement GAE, local data suggests 82% of patients had statistically significant improvement at three months with the significant benefit maintained in 68% patients at 12 months. Post-24 month outcomes are pending.
Geniculate artery embolisation is a novel, minimally invasive procedure that may reduce pain and improve function in knee osteoarthritis.
Targeting pathological neovascularisation associated with the disease, GAE addresses a key aspect of OA pathophysiology.
Early clinical outcomes are promising, suggesting that GAE may become an important tool in the multidisciplinary management of OA in close coordination with orthopaedic surgeons. With growing evidence, GAE could significantly impact OA treatment, providing relief for patients, reducing reliance on more invasive surgical procedures and long-term medication use.
Author competing interests – the authors were involved in collecting “local data” for the post TKR trial


Paul is a locally trained surgeon who brings with him experience gained from several years of interstate and overseas fellowships, and specialises in:
Hip & Knee replacement
Robotic-assisted joint replacement
Sports knee
Foot & Ankle
Upper & Lower limb trauma
Perth Hip and Knee are a specialist practice focused on the treatment of all aspects of hip and knee pathology. From arthroscopy to complex joint replacement and revision surgery, we deliver excellence in care utilising state-of-art surgical techniques and cutting-edge technologies to achieve optimal outcomes for our patients.
We are delighted to have Paul join Perth Hip & Knee and he is a valued addition to our group of experienced hip & knee surgeons. You can contact his rooms direct at rebgetz@hipnknee.com.au or on 08 6489 1766
Perth Hip & Knee
Suite 1/1 Wexford Street Subiaco WA 6008
PHONE: 6489 1700
EMAL: admin@hipnknee.com.au
www.hipnknee.com.au
With increasing knowledge of the devastating effects of trauma on the first responders to crises, ranging from war, accidents, natural disasters and violence in its myriad forms, the development of effective treatments has given hope for the many service men and women (and their loved ones) who have previously suffered in silence.
WA psychiatrist Dr Mathew Samuel has had a longstanding commitment to serving those who suffer while serving their community. For more than 20 years, he has run and developed Department of Veteran Affairs (DVA) accredited trauma recovery and growth programs in a hospital setting.
In 2021, he and a skilled multidisciplinary team established the community-based WA Centre for Trauma Treatment and Research in Nedlands where they run a series of programs for a growing cohort of first responders along with serving members and veterans.
“Our insight and expertise into understanding the changing needs of those who serve our communities led to the development of an intensive four-week Trauma Recovery and Growth Program for first responders and other uniformed personnel,” Dr Samuel said.
“This program has delivered outstanding results with significant improvements on all measures currently used to assess the DVA TRP programs. In April 2021, we commenced running this program for the WA Police (WAPF), Department of Fire and Emergency Services (DFES), prison officers, Department of Community Protection (DCP) workers, teachers, DVA veterans, and Insurance Commission of WA (ICWA) approved claims.
“Following our success with the First Responders and Veteran Programs we began addressing the current shortfalls in treatment options in WA for workers compensation/ thirdparty insurance, mining industry, and government workers, who have failed most conventional treatments, medication, in-patient admission, and individual psychological interventions.”

Dr Samuel said the intensive fourweek group therapy course offered 100 hours of therapy that not only addressed a person’s trauma but through guided sessions could encourage personal growth.
This holistic approach means that participants are not only psychiatrically and psychologically assessed and helped, they are also given activity and dietary advice from an exercise physiologist and a nutritionist over the course of the program.
“I undertake the baseline psychiatric assessments before a participant begins a program to discover any comorbidities, and there is often a lot going on such as alcohol and other substance use. Significant sleep disturbance is also very common,” Dr Samuel said.
“We ensure that adequate and appropriate medications are prescribed before participants start therapy to give them the best chance of getting the most out of the program.”
The program consists of:
• 20 days group work between 9.30am and 3pm, Monday to Friday, with oversight of consulting psychiatrist.
• 1 x 5-hour-day for relapse prevention, four weeks after the program completion.
• 2 x follow-up assessments at 1-month and 3-months post program completion.
• 2 x 3-hour partners and significant others support.
• Thorough intake assessments and discharge reports by both Clinical Lead, Dr Mathew Samuel, and senior mental health social worker Holly Pearce.
• All catering, stationery, workbooks and manuals supplied.
The WA Centre for Trauma has run 24 program cycles with 5 to 10 participants in each and the feedback has been very positive from the participants and the organisations who have referred them.
The program is run by: Dylan Meldrum (Registered Psychologist), Nina Formentin (Registered Psychologist), Holly Pearce (Mental Health Social Worker), Jess Wilson (Nutritionist), and Pivot Health Group (Exercise Physiologist).
The centre has presented a Poster at the Annual RANZCP Conference in Perth May 2023 and is on track to deliver the next Poster at the Annual APA Meeting in New York May 2024.
Dr Samuel said GP referrals were always fast-tracked.
“We want GPs to know that, despite the growing waiting lists in the private sector, there is help and treatment available for patients who satisfy the diagnosis,” he said.
The aortic valve normally has three cusps, but an abnormal aortic valve from birth can be bicuspid (two cusps), unicuspid (one cusp) or quadricuspid (four cusps).
Less than three cusps (bicuspid and unicuspid) tend to create valve stenosis over time, but overwhelmingly the most common cause for severe aortic stenosis (AS) is calcific disease in older adults. There are a number of associations between severe calcific AS and cardiovascular risk factors, but other than traditional risk factor modification (including blood pressure control), no single treatment has been shown to modify progression of AS once it develops.
Our research group has shown that mild, moderate and severe AS are all common and associated with a significant risk for premature mortality. Severe AS is underdiagnosed and under-treated worldwide, and in Australia we estimate approximately 100,000 Australians have severe AS and approximately 56,000 of them will be expected to die before receiving valve intervention.
Detection of severe AS is a critically important step since symptoms may not be a good guide to AS severity. We recommend regular (at least yearly) auscultation for all patients over the age of 50 years since new onset AS may progress rapidly in some patients. If any degree of AS is suspected, we recommend transthoracic echocardiography as the first test (not stress echo) to determine AS severity.
Patients with mild AS should be followed with repeat echocardiography at two years (unless indicated earlier) and careful control of cardiovascular risk factors. Moderate AS should be referred to a cardiologist with expertise in valvular heart disease for careful review and close monitoring of AS severity. Some patients with moderate AS behave more like severe AS (with

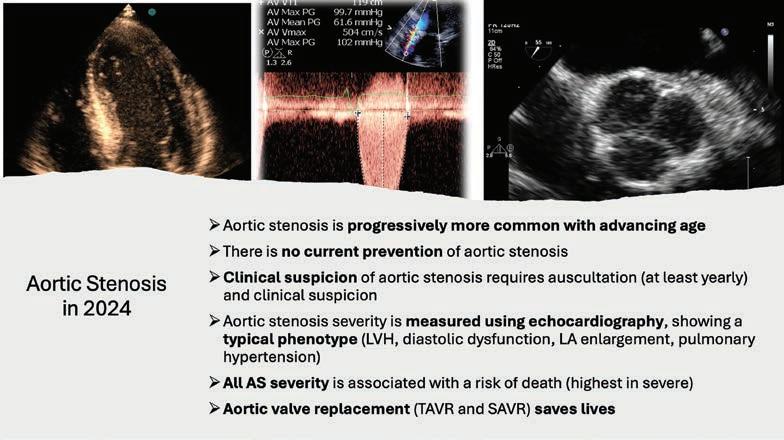
Aortic stenosis is common in older people
High level clinical suspicion is needed for diagnosis
Valve intervention is first-line management in severe AS.
associated symptoms) and may be considered for valve intervention.
All patients with severe AS should be seen by a cardiologist with specific expertise in valvular heart disease with a view to valve intervention at the appropriate time, except in circumstances where valve intervention is inappropriate or contraindicated (such as short prognosis terminal disease or advanced dementia).
Identification and monitoring of patients with AS is imperfect using current methods, and we are investigating new AI methods to help streamline diagnosis and management decisions.
The first-line treatment of severe AS is valve intervention, either by surgical aortic valve replacement (SAVR) or transcatheter valve intervention (TAVI), depending on patient age and comorbidities. Due to the lower risk of valve intervention in recent years, more patients are now being considered.
Recent trials have shown major benefits of valve intervention across the spectrum of surgical risk.
In summary then, aortic stenosis (AS) is common in older Australians and may not be identified without a high clinical suspicion and regular auscultation. Any murmur in older individuals should prompt an echo at least once, to identify the cause of the murmur.
If aortic stenosis, it should be carefully followed, and moderate or greater AS should be referred to a cardiologist with specific expertise in valvular heart disease. Severe AS with symptoms is a Class I indication for aortic valve intervention.
– References available on request
Author competing interests
1989

Opened first BreastScreen WA clinic in Cannington.
1990

BreastScreen WA is mobile! By 1995 there are 4 mobile units travelling around WA.
1993
BreastScreen WA extends North by welcoming a Mirrabooka clinic.
Service continues to expand with a Midland clinic.
Perth City clinic opens and BreastScreen WA becomes first state service to go statewide.
1999
Assessment comes under the BreastScreen WA umbrella - Sir Charles Gairdner and Royal Perth Hospitals. GP Advisory committee is convened.
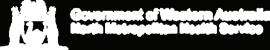
BreastScreen WA achieves full accreditation with BreastScreen Australia.

Launch of website.
BreastScreen WA Consumer Reference Group is formed.
2006
Cannington clinic relocates.
2007
One million screens!
2008
Padbury clinic opens.
2010-11
2014
Online bookings, new website and social media is launched. Cockburn clinic opens.
2015
Wanneroo clinic opens. New breast assessment centre at Fiona Stanley Hospital.
2016

Mandurah clinic opens. Introduction of electronic GP notifications.
2017

performs its 2 millionth screen!

The digital revolution begins.
2012
New mobile screening units are launched. David Jones Rose Clinic opens in Perth City store. Health Promotion team can make opportunistic bookings at events.
2019
A secure client result portal is launched.
2020
COVID-19 Pandemic causes 2 month suspension of services. Clients can now receive

East Perth- Mardalup Clinic opens, first to be Aboriginal co-named.

screening units are launched.

New screening and assessment centre opened in Joondalup.
clinic reopens after a

“Screening Saves Lives” partnership with National Cervical and Bowel Screening Programs to promote screening in the LGBTQIA+ community.

Primary prevention of arteriosclerotic cardiovascular disease (ASCVD) is a desirable but challenging goal to attain. Several strategies to delay the onset of clinically meaningful ASCVD have been proposed, however, clinical application of these strategies is patchy at best.
What clinical counselling and advice could a clinician offer a young asymptomatic patient with a modest family history but no known cardiovascular disease? What evidence-based tests, if any, could inform their predicted risk of ASCVD? Furthermore, are there any actionable interventions to put in place as part of their management plan, to reduce their lifetime risk of clinically relevant ASCVD?
General interventions towards reducing the lifetime risk of cardiovascular events involve a combination of lifestyle modifications such as taking up a healthier diet, avoidance or quitting tobacco smoking and limiting the use of alcohol, and regular health check-ups to monitor markers of metabolic health such as blood pressure, glycaemic control, and cholesterol checks. Intimate knowledge of family history of cardiac disease is also an important motivation, to stay on the preventative front foot.
The concept of low-density lipoprotein cholesterol-years, akin to pack years of smoking, is worth a highlight. Even with optimised lifestyle interventions, serum circulating low-density lipoprotein cholesterol (LDL-C) concentrations often exceed optimum levels, contributing to high cholesterolyears, which is associated with extravascular lipid deposition in tissues.
What’s more, some patients with normal cholesterol levels still harbour a high risk of cardiovascular-related events. To that end, there is merit in considering the atherogenicity of
Atherogenic cholesterol contributes to developing early aggressive atherosclerosis
Moderate intensity aerobic exercise reduces risk
Waist circumference is a worthwhile tool and easily measured.
the LDL-C, which is an important risk factor for atherosclerosis. Routine assay of Lipoprotein A and Apolipoprotein B levels, to identity those with more atherogenic circulating LDL-C, could lead to early intervention in this cohort, possibly delaying the onset of clinically relevant ASCVD.
Clinicians should extol the evidence-based cardiovascular benefits of moderate intensity aerobic exercise, along with muscle strengthening activities. Exercise exerts favourable effects on cardiovascular function such as improving endothelial function and insulin sensitivity, lowering blood pressure and improving lipid indices, as well as reducing systemic inflammation.
Higher maximal oxygen uptake (VO2 max), a strong predictor of cardiorespiratory fitness, is associated with a reduced risk of coronary events. In clinical practice,

routine testing of VO2 max is not routinely available to the well patient.
However, in the modern era, there are various commercially available smart gadgets which purport to measure VO2 max, the maximum amount of oxygen the body can utilise during intense exercise. There may be merit in educating the public about the utility of having a knowledge of one’s VO2 max, not least to act as motivation to undertake routine exercise to improve the VO2 max.
There is a strong association between waist circumference, visceral fat and cardiovascular risk. Visceral fat is stored deep within the abdominal cavity and coats the internal organs. Metabolically active visceral fat promotes endothelial dysfunction and secretes proinflammatory cytokines and adipokines.
Consequently, patients with excess visceral fat are at risk of insulin resistance, dyslipidaemia, systemic hypertension and chronic systemic inflammation. Waist circumference is a simple measurement which is reproducible and can be individualised to a patient’s ideal body weight. It is a powerful tool to use for goal setting to contribute to future cardiovascular health.
The clinical thought process about the dynamics of insulin metabolism is often directed towards patients with abnormal glycaemic control. However, chronic dysregulation of insulin kinetics and hyperinsulinaemic states may be more common in the non-diabetic population, ultimately increasing the risk of ASCVD. To that end, clinical counselling about insulin sensitivity and glycaemic control could contribute to a steadier state metabolic profile, benefiting the well patient in the long run.
– References available on request
Author competing interests- nil

We are pleased to announce our
Dermatologist supervised total body photography and sequential digital dermoscopic imaging for high risk patients with multiple naevi and melanoma.
Urgent Lesion Clinic for suspected melanoma diagnoses or any urgent lesion (private health insurance rebates apply in our day procedure centre).
Personalised melanoma risk assessment to determine surveillance intervals and educate patients on risk factors.
Confocal microscopy for diagnosis and pre-surgical mapping of lentigo maligna (in situ melanoma) at complex and cosmetically sensitive sites (Dr Collgros).
Management of cutaneous toxicities related to medical oncology treatments.


Abdominal aortic aneurysms (AAA) are still known as a ‘silent killer’ as they remain largely asymptomatic until they present with a leak or rupture. Ruptured AAA still have a high prehospital and in-patient mortality despite the advances in technology.
Focus has shifted to the early detection of AAA, management of risk factors that contribute to a faster rate of growth, higher rupture risk and the appropriate mode of intervention when an aneurysm reaches intervention threshold. These factors have been addressed in the recent 2024 European Society of Vascular Surgery guidelines.
An AAA is defined as an aortic diameter of 3cm or more. The prevalence of AAA has significantly decreased over the past two decades mainly due to the decline of smoking, better management of blood pressure and a rise in the use of antiplatelets and statins, all of which have been shown to decrease aneurysm degeneration and rate of growth.
Non-modifiable risk factors in developing an aneurysm include being a male, age and family history. Large population studies had demonstrated the effectiveness of screening for AAA in particular in men at the age of 65 years. Sweden and the United Kingdom screen 65-year-old men while the US taskforce recommends screening for men aged 65 to 75 years who are current or ex-smokers.

However, the Western Australian screening trial failed to demonstrate any benefit in the population due to the high rates of imaging or detection of AAA during routine clinical care.
The heritability of AAA is thought to be up to 70%, with a family history of AAA increasing the prevalence of AAA up to threefold. Therefore, screening is recommended in all men and


Key messages
Abdominal aortic aneurysms remain a silent killer. The heritability is up to 70%
Screening approaches vary around the world. In WA no benefit was found.
Risk factor management is critical where AAA is detected.
women aged 50 or older with a first degree relative with AAA.
Patients with known popliteal and femoral aneurysms should have routine screening at any age, as prevalence of AAA is up to 40% in this subgroup.
Ultrasound remains the mainstay in aneurysm detection, screening and surveillance of AAA. Aneurysms grow at a mean rate of 2.2 mm/ year and this rate is increased in smokers and with increasing AAA size. Ultrasound surveillance of AAA differs in males and females as aneurysms in women tend to rupture earlier than men (see table).
Patients with AAA have a high incidence of cardiovascular disease and management of the underlying risk factors has demonstrated to decrease the risk of cardiovascular morbidity and mortality. Therefore, all patients with AAA should undergo smoking cessation, antiplatelet therapy, statin therapy, BP control and lifestyle advice (exercise and diet)
It is not necessary to restrict exercise or sexual activity in patients with small AAAs, however, restricting vigorous activity in patients with large AAA may be advisable.
Treatment of AAA is offered when risk of intervention is significantly less than the risk of rupture. In men, elective repair should be considered at 55mm whereas in women the threshold is 50mm. The rate of increase of the diameter is another factor for rupture,
The old adage that prevention is better than cure holds strong for cardiovascular disease (CVD). Accounting for 25% of all Australian deaths, CVD costs the Australian health system $12.7 billion annually, placing an enormous burden on individuals, their family and the economy.
Traditional risk factors include modifiable causes (e.g. dyslipidaemia, hypertension, smoking, diabetes and lifestyle). Non-modifiable causes include genetics and gender.
Genetics has potential to be modifiable utilising techniques such as CRISPR. Female gender is not “protective” as such with CVD remaining a major cause of death for Australian females, and gender at best delaying onset. Females have lower rates of goaldirected medical therapy, lower rates of coronary intervention and are underrepresented in clinical trials, potentially worsening CVD outcomes.
It is established that while elevated LDL levels increase the risk of plaque build-up, atherosclerosis is an inflammatory process as demonstrated by the LoDoCo2 trial. There are patients with high LDL levels at lower risk of CVD and half of patients with MI will have ‘normal’ cholesterol levels. More nuance is needed to determine actual risk.

LDL is the major target for lipid lowering with evidencebased therapies to reduce major cardiovascular events (MACE). Increasing HDL with pharmacotherapies has not shown benefit and trials are unlikely to demonstrate this. TG (definite causative factor) has limited evidence-based pharmacotherapies.
Lipoprotein(a) (Lp(a)) is a genetically determined lipid particle related to LDL. It is highly atherogenic with levels determined by SNPs effecting K-IV region. About 20% of the population is considered to have elevated Lp(a), with levels higher in black people and in females, increasing in the post-menopausal period. No therapies exist to reduce Lp(a) with clinical trials continuing.
Dietary modification and lifestyle change are recommended for all patients.
continued from Page 43
therefore, patients with aneurysms which grow >10mm/year should also be considered for repair.
Although endovascular aortic repair (EVAR) remains the primary
treatment option in most patients, open repair is an effective option, particularly in young patients with a long-life expectancy.
Due to risk of late complications with EVAR, long-term yearly surveillance with ultrasound is recommended (usually by the

Statins remain the mainstay for therapy with robust evidence of their efficacy. LDL reduction with high potency agents at mod-high dose is >50%. Perceived and real side effects are common. Despite maximal tolerated statin therapy, many patients will not get to LDL target. Eztimibe is added to statins and confers an additional 20% LDL reduction and a modest relative reduction of MACE of 7% in secondary prevention patients.
For patients meeting PBS criteria, PCSK9-I (twice weekly selfadministered injection) confers a further 50-60% reduction of LDL (on top of statin and ezetimibe) and a 15% reduction in MACE.
Inclisiran, an mRNA therapy targeting PCSK9-I (initially 3/12 then 6/12ly nurse administered injection) is available via a patient familiarisation program and 50% LDL reduction is achieved. The major CV outcome trial result is still pending.
Bempedoic acid (not available in Australia), a statin alternative, lowers LDL by 20% and MACE by 13% in statin intolerant patients.
Lp(a) therapies will potentially confer enormous benefit to patients with elevated levels. Lp(a) is considered to contribute to the residual risk of a future CVD event and therefore treatment is anticipated to reduce risk significantly particularly in the highest 20% of Lp(a) levels.
vascular surgeon). Patients who have undergone open AAA repair usually require a CT scan at 5 years to assess for synchronous aneurysms.
– References on request
Author competing interests – nil
CVD remains the number one killer in Australia
Risk factor management is often suboptimal
Lipid clinics can optimise treatment.
Phase 3 clinical trials are under way with RNA therapies lowering Lp(a) by 95% in patients with high Lp(a) and a history of CVD. Results of these trials will be available over the next few years.
APOCIII is a TG and ANGPTL3 a TG/LDL lipid target therapy with multiple trials utilising RNA therapies planned or ongoing.
The case for lipid clinics
Managing dyslipidaemia can be difficult. Debunking social media conspiracy theories, managing patient side effects, choosing optimal lipid lowering agents, and negotiating the PBS and when to commence newer therapies such as the injectables (mAb PCSK9-I and siRNA Inclisiran) as well as future agents (e.g. Bempedoic acid, Lp(a)
therapies) can be daunting.
Lipid clinics are well established, providing up titration of evidencebased goal directed therapies, genetic assessment, and patient access to research programs (e.g. for currently untreatable conditions such as elevated Lp(a)). They integrate dietary, exercise physiology, pharmacology and rehabilitation services.
Up to 50% of patients are not on statin therapy 12 months after admission for an MI, despite evidence they should be. The ‘why’ is not fully understood and requires more research. Lipid clinics can ensure patients continue therapies clearly demonstrated to reduce risk. This requires education, engagement, support and understanding patient circumstances.
Clinical trials are very important to get new therapies approved, with access facilitated through research units. Public hospital-based and private research groups have links with lipid clinics providing patient access. Clinitrials is currently recruiting to the Acclaim Lp(a) trial and has many patients in follow-up in the Ocean A study
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy
Surgery can be open or endoscopic.

The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
and participated in the now completed Clear Outcomes study of Bempedoic acid.
It is also correct that not all patients will benefit from lipid-lowering therapies and the use of imaging such as CTCA and Ca scores is providing more nuance in our assessment of risk. The AusCVD risk calculator now incorporates Ca score as a reclassification factor.
Lipid clinics can support patients and GPs to optimise lipid management, assessing risk to determine optimal pharmacotherapies, providing patients with reassurance that their condition is treatable, that genetic risk can be screened for and managed appropriately. They can ensure patients get the best management available in an increasingly subspecialised area.
Author competing interests – the author is principal investigator on lipid and heart failure studies, and medical director of cardiology studies at Clinitrial
By Mr Peter Ammon Foot Ankle & Knee Surgery
Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare. St
www.murdochorthopaedic.com.au


(08) 6332
“One in five Australian adults are estimated to live with chronic pain.”
(Commonwealth of Australia, Department of health, 2021)
Chronic pain can be debilitating and have adverse effects on work, sleep and relationships often leading to comorbidities such as, depression, sleep disturbances and fatigue resulting in worsened health and negative societal and financial impact.
An increased reliance on pain medications and the concurrent disorders associated with chronic pain may place individuals at a higher risk of developing a substance use disorder.
Risk factors for Substance use Disorders:
Recurrent and easy access to substances
Stress and financial difficulties
Any mental illness or impairment
PTSD and trauma.
Signs & symptoms of a substance use disorder:
Frequent requests for early prescription refills
Social withdrawal or neglecting responsibilities
Physical changes; weight, poor hygiene or skin problems
Taking higher doses or more frequently than prescribed
Patient requesting prescriptions on first visit, “doctor shopping”
Changes in mood or behaviour; agitation, irritability and mood swings

Defensive or evasive when questioned about medications.
We can help...
If you suspect that a patient may have a substance use disorder, please refer them to Fresh Start, or a suitable specialist.
Referral forms can be found on our website www.freshstart.org.au or call our clinic on 08 9381 1333
Obesity is a major public health problem that is associated with serious comorbidities, including diabetes, dyslipidaemia, cancer and cardiovascular disease (CVD), with premature mortality. Its prevalence has been increasing over the past few decades and is a modern-day pandemic since 2012.
Per the American Society for Metabolic and Bariatric Surgery 2023 guidelines, overweight is a body mass index (BMI) of 25 to <30 kg/m2 and obesity as a BMI of 30 kg/m2.
Over the past decade, the proportion of Australian adults who were overweight or obese had increased from 62.8% in 2011–12 to 65.8% in 2022. This was due to the increase in the proportion of Australian adults categorised as obese, which increased from 27.5% to 31.7% over the same period. Bariatric surgery is increasingly used as a therapeutic option for obesity.
Obesity is a major contributor to cardiovascular risk factors including hypertension, hyperlipidaemia, coronary artery disease (CAD), heart failure (HF), stroke, sleep apnoea and arrhythmias. Its pathogenesis is linked to proinflammatory factors and vessel wall remodelling, among others. Obesity accelerates atherosclerosis by promoting lipid deposition and atherothrombosis formation. It further activates the cytokines and interleukins causing endothelial dysfunction and vascular remodelling.
This translates into cardiovascular disease events including CAD, myocardial infarction and stroke. Excess visceral adiposity leads to the activation of reninangiotensin-aldosterone system, cytokine gene expression, and increased systemic circulation of proatherogenic factors. This in turn leads to myocardial fat accumulation, increased stroke volume, cardiac wall remodelling, and fibrosis manifesting as heart failure. Similar mechanisms lead to

Key messages
Management of obesity is multimodal
Bariatric surgery shows statistically significant risk reduction with CAD, MI, HF, CVA Early referral from GP/ Cardiologists improves cardiovascular outcomes.
left atrial enlargement and fibrosis contributing to arrhythmogenesis.
Lifestyle modifications and increased physical activity are the initial modalities recommended in the management of obesity. Patients with a BMI of at least 35 or >30 kg/m2 with serious obesityrelated comorbidities are eligible for bariatric surgery. The commonly performed bariatric surgeries include sleeve gastrectomy, Rouxen-Y gastric bypass and modified duodenal switches. The benefits of bariatric surgery include greater long-term weight loss, reduction of major adverse cardiovascular events (MACE), and cardiovascular mortality.
Obesity poses a high risk for atheroma formation. Bariatric surgery provides a beneficial effect by altering molecular mechanisms involving inflammation and it can decrease the levels of

oxidative stress and inflammatory markers. It reduces circulating levels of adhesion molecules and improves endothelium-dependent vasodilatory response.
Objectively, several studies have shown that surgery reduces carotid intimal wall thickness in concordance with weight loss. These processes in turn contribute to the risk reduction of atherosclerotic diseases such as CAD, MI and CVA. Although CAD and MI are atherosclerotic processes, they differ in their pathophysiology and clinical manifestations.
CAD is defined as the presence of atherosclerotic plaque within the epicardial coronary arteries. Over time, risk factors potentiate plaque growth. During periods of myocardial oxygen demand, there is endothelial dysfunction causing plaque rupture. This in turn leads to atherothrombosis, vessel occlusion and myocardial infarction.
Bariatric surgery can reduce heart failure risk factors including hypertension, hyperlipidaemia, and diabetes. It also directly acts on the myocardium causing changes in the left ventricle (LV) wall and ejection fraction (EF) percentage.
Bariatric surgery can improve left ventricular systolic dysfunction that results in a statistically significant improvement in left ventricle ejection fraction (LVEF).
Another study showed a 43% reduction in left ventricular mass with subsequent reduction in left atrial and right ventricular wall diameter and epicardial fat. A meta-analysis done by Cuspidi et al. showed significant changes in LV thickness, improvement in LV diastolic function, and a decrease in left atrial diameter.
Given the significant cardiovascular benefits offered by bariatric surgery, the referral from general practitioners and primary care physicians has been lower. This
continued on Page 48

 By A/Prof. Joshua Lewis & Cassandra Smith, Edith Cowan University
By A/Prof. Joshua Lewis & Cassandra Smith, Edith Cowan University
Rapid weight loss in older people is defined as the involuntary decline in total body weight by >5% over a six to 12-month period. This magnitude of weight loss has been suggested by some to be an indicator of health status, and unintentional weight loss occurs in up to one in four communitydwelling frail older adults.
The pathophysiology of rapid weight loss remains poorly understood, However, when it occurs it can be detrimental and shown to be associated with poorer health outcomes including an increased risk of falls, fractures, mortality, institutionalisation, cognitive decline, Alzheimer’s disease, and declines in physical function and quality of life. Traditional management of maintaining weight of the older adult usually incorporates a lifestyle approach (e.g. exercise and healthy diet including adequate protein intake).
Vascular health is essential for the absorption of nutrients at the gut and a nexus between compromised vascular blood supply and suboptimal nutrient absorption may exist.
Abdominal aortic calcification (AAC) is a process involving mineral deposition in the arterial

wall, which represents an early site of vascular calcification, and is a strong predictor of cardiovascular disease (CVD) risk.
AAC is related to musculoskeletal health that is a risk factor of rapid weight loss. For instance older women who had extensive AAC presented with a greater decline in hand grip strength, and older men had higher risk of AAC progression if they had low muscle mass and poorer physical function. AAC in older women is also shown to be related to late-life dementia, as well as increased falls and fractures risk.
continued from Page 47
could be attributed to knowledge gaps, hesitancy, or concerns regarding postoperative care.
A recent Canadian survey showed that more than 50% of physician respondents did not feel equipped to counsel the patients on surgical options and only 11.6% of the obese patients were counselled.
In a Swedish survey, interestingly, 84% of respondents stated that the patients themselves initiated bariatric surgery referral. Physician’s knowledge showed a positive correlation toward referral and management of postoperative issues. This brings into perspective that education and awareness would lead to better patient sampling, thereby cumulatively improving cardiovascular outcomes.
AAC is a marker of multi-site atherosclerosis, related to atherosclerosis and stenosis of other vascular beds (e.g. superior mesenteric arteries), and is related to all-cause mortality. Extent of AAC is also related to the health of other organs such as common bile duct diameter (important for nutrient absorption), suggesting generalised atherosclerosis may affect intra-abdominal organs.
Given that the risk of atherosclerosis of the gastrointestinal tract (coeliac, superior mesenteric and inferior
In conclusion, bariatric surgery shows a statistically significant risk reduction with CAD, MI, HF, CVA, and cardiovascular disease-specific mortality and a non-significant risk reduction of atrial fibrillation.
– References available on request
Author competing interests – the author is a clinical consultant to Lexington Australia and Medtronic Australia.
Results from this study suggests that vascular disease may increase the risk of rapid weight loss in older women
A causal mechanism has not been determined
Better understanding of this link may open the door to new treatments targeting vascular disease.
mesenteric arteries) increases with increasing age and can result in post-prandial abdominal pain and weight loss, we hypothesised in our study that AAC, a potential marker of generalised ischemic gastrointestinal artery disease, is related to rapid weight loss in 929 community dwelling older women (mean ± SD age 75.0 ± 2.6 years).
Key findings of the published work
During five-years of observation, two in five women had rapid weight loss, which was associated with a
49% increase in all-cause mortality in the next 9.5 years. This risk increased to 87% higher in women who experienced rapid weight loss of more than 10% in a 12-month interval. In the one in two women with moderate to extensive AAC, they had 36% and 58% higher odds of having rapid weight loss over the next five years.
These results remained similar after adjusting for dietary factors and cardiovascular risk factors such as blood pressure and cholesterol. Importantly, this link was still seen in women meeting protein and energy and physical activity recommendations. This suggests new interventions to attenuate unexplained weight loss in older people may be required for those with vascular disease.
A limitation of the work is that the mechanisms underlying the relationship between AAC and rapid weight loss remain unclear. One hypothesis is that AAC could be limiting blood flow to the gut, which in turn could be affecting the
While more than 50 million people globally live with dementia, that figure is predicted to triple by 2050, highlighting the need for more support for those affected and their carers.
Community Vision has unveiled a new partnership with Dementia Doulas International, offering a new service to West Australians facing the difficult path of dealing with a loved one who has dementia.
Viewing dementia care from a new perspective, trained Community Vison staff provide support, information, education, liaison and advocacy from post-diagnosis through to the bereavement stage.
Dementia Doulas International conducted a four-day training course with five Community Vision staff, who are all now qualified dementia doulas offering individualised care, with a focus on ensuring that end-of-life plans are in place.
These doulas can initiate early future planning conversations,

incorporate creative ways to care and become an ongoing support for families.
Dementia Doulas International began in 2019 to better meet the needs of those impacted by advancing dementia. While many aged care, disability, mental health, and end of life services were available, there was no other standalone service offering a dementia specific program such as this, tailored to the individual and family needs, based on what stage of the illness they were at.
South Australia was the first state to offer the service, now in WA.
absorption of nutrients. This has the potential to change how we treat those older individuals who present with rapid weight loss. The traditional approach would be to increase protein and energy intake, but data suggests that vascular disease may be driving or a contributor to weight loss, in which case using the traditional approaches may not help with body composition.
Given the poor outcomes commonly associated with rapid weight loss in older adults, AAC may be a tool to identify those older women with highest risk.
– References available on request
Author competing interests – ECU has lodged a patent for automated assessment of abdominal aortic calcification. Associate Professor Joshua Lewis is a named inventor on this patent. The salary of Associate Professor Joshua Lewis and accredited exercise physiologist Dr Cassandra Smith is supported by Heart Foundation Fellowships.
The aim of Dementia Doulas is to keep clients who are living with dementia in their homes and connected with their families and community, for as long as possible.
Registered nurse and general manager of care and service delivery at Community Vision, Tamara Williamson, will lead the WA service.
Dementia Doulas International managing director Wendy Hall said the training of staff already known to their clients and families living with cognitive changes meant community dementia care was taken to a new level.
In 2018, the organisation launched A Roast to Remember, a fundraising initiative which resulted in a community dementia bus which focuses on people in the wider community who do not have immediate access to local dementia services.

Professor Anne Buist and husband Dr Graeme Simsion have written a new book together and are taking it on the road, which includes to the Margaret River Readers & Writers Festival next month.
It’s probably safe to say, when a dusty Professor Anne Buist and Dr Graeme Simsion arrive at the annual Margeret River Readers & Writers Festival next month, they will have driven the furthest of anyone to be there.
The married Melbourne-based team are driving across the country in service of their new book collaboration, The Glass House, to raise awareness of mental health. Over the next six months they’ll be visiting more than 400 bookshops across Australia on The Great Australian Bookshop Tour, holding talks about mental health and donating event proceeds to local charities.
In Margaret River they will join the likes of Wendy Harmer, William McInnes, A.C. Grayling , Andrew O’Hagan and Holly Ringland
By Ara JansenThey’ll be talking about The Glass House, a story of young psychiatry registrar Dr Hannah Wright who starts on the ward at Menzies Hospital. She’s learning on the job in a strained medical system and trying to figure herself out as she and the other trainees deal

with the common and the bizarre, the hilarious and the tragic, the treatable and the confronting.
Characters who end up at Menzies include a woman with a lifethreatening eating disorder and another suffering postpartum

psychosis, fighting to keep her baby.
Combining intelligence, frankness and humour, eminent psychiatrist
Anne tells it like it is, while co-writer Graeme brings the light touch that made his book, The Rosie Project, an international bestseller and respected contribution to the autism conversation.
Anne is Chair of Women’s Mental Health at the University of Melbourne with 30 years of clinical and research experience in perinatal psychiatry. With a multimillion-dollar grant from Beyond Blue, she established an Australiawide screening program for perinatal depression.
She began writing at eight and was going to be an author, but medicine intervened until 2012, which is when she started writing again and she hasn’t stopped. She has written an erotic fiction series under a pseudonym, four crime novels and a standalone thriller.
Anne and Graeme are intimately involved in each other’s writing lives, even with the books they are writing solo. Long walks are pivotal to nutting out everything from storylines and plots to business decisions. They had so much fun, they’ve written the second book
and are starting to think about a third.
“I wrote for almost 10 hours a day for a few weeks to get The Glass House into a first draft, using plenty of lived experience.,” says Anne “Graeme helped with the planning of the chapters and he’s really good

at story structure and I’m good at big picture stuff. He’s good at adding the drama and the light.”
Of course, she can’t use exact patient stories that can be identified but has created potentially real situations and wanted to make sure it mirrored life for hospital staff and patients as much as possible.
“Some of the book has dark humour, but I think that’s something that happens in health. It tends to be a way you cope. I’ve worked in psychiatry for 30 years, so I have a lot to tap into. With very few exceptions, I really like my patients and I feel for them. The ones who have made an impact on me, I will never forget. That’s something that has inspired me and found its way into the book.”
Margaret River Readers & Writers Festival runs from May 17 to May 19.
Tickets and full list of events from www.mrrwfestival.com and details of Anne and Graeme’s tour at www.greataustralianbookshoptour.com.au

Two trailblazing health professionals have featured among the 2024 inductees into the WA Women’s Hall of Fame, recognised in the health category sponsored by St John of God Health Care.
Hungarian-born molecular biologist Emeritus Professor Elizabeth Rakoczy is an internationally recognised scientist working in several fields, including gene therapy and animal model development.
She arrived in Australia with her two small children, when her husband was sponsored by a Perth-based company in 1985. Although she was already a published researcher with a PhD, she was denied working rights as part of their visa condition.
Professor Rakoczy refused to accept her predicament and decided to fight the system, calling all the WA universities, and finally secured an interview with the late Professor Geoff Shellam, at UWA’s department of microbiology. Within months, the university applied to change her visa status, citing her unique expertise.
In 1986, she started working as a research associate and in 1987, was awarded her first three-year grant and became a research officer by the National Health and Medical Research Council.
Continuing her work, she founded the Department of Molecular Ophthalmology at the Lions Eye Institute and was the first in Australia to apply molecular techniques to investigate eye diseases. Her
group developed the gene therapy treatment for wet age-related macular degeneration, replacing painful monthly injections into the eye. She was awarded the prestigious CSL Florey Medal in 2017 for her achievements.
Respiratory medicine nurse practitioner Sue Morey was also inducted, with a career marked by many firsts, including being the youngest charge nurse at her time of her appointment and the first nurse practitioner in respiratory medicine in Australia.
She holds a Bachelor of Health Sciences and a Graduate Diploma in Clinical Specialisation (Nurse Practitioner) and has been actively involved in research in her field of respiratory medicine.
With more than 40 years’ experience, Ms Morey has professional affiliations with the Australian College of Nurse Practitioners, European Cystic Fibrosis Society, International Society for Heart and Lung Transplantation, Transplant Nurses Association, Thoracic Society of Australia and New Zealand, Australian College of Nursing and the Australian Lung Foundation.
In 2004, she was awarded the Order of Australia Medal for her services to respiratory medicine nursing. In
2022, she was appointed patron of the Institute of Respiratory Medicine in WA.
Her eminence in respiratory medicine and her experience in the highly specialised field of lung transplantation has significantly contributed to the community.
Esme Bowen, an inductee in the business category, also has a health background, working in the nursing and disability sectors for more than 35 years.
Her contribution to health advocacy was fostered by her nursing training at Princess Margaret Hospital which started in 1977. She went on to work in post-basic orthopaedic spinal care and did a study tour of Europe visiting the world’s leading spinal injury hospitals.
Within three weeks of returning from Europe, she broke her back in a car crash and was in the spinal unit for six weeks. Her rehabilitation was 18 months in a body brace, and she used the time to study at ECU for her BSc (Nursing). Her experience spurred further focus on spinal injury advocacy.
An isolated vineyard in an isolated corner of WA, 330km south of Perth, Frankland Estate was born in 1988. Sheep farmers Barrie Smith and Judi Cullam planted vines in the “coffee rock” soil – ironstone gravel over a clay subsoil. And the vineyard’s name? Isolation Ridge, naturally.
Natural also because in 2009 Frankland Estate achieved organic certification. The result is healthy resilient vines, giving pristine fruit-making wines of greater balance, broader sensory spectrum and depth of flavour.
The estate is now run by brother and sister Hunter and Elizabeth Smith, with Elizabeth’s husband Brian Kent the winemaker since 2010. As is often the case, children standing on the shoulders of their parents are able to tweak and fine tune the vineyard and wines to a new level of sophistication. Such is the case at Frankland Estate, which has become famous for its rieslings, shiraz (syrah) and cabernet franc. Vinification is gentle and respectful with the aim of highlighting the fruit flavours of the vineyard. Favourite? I’m putting each of the Isolation Ridge wines down in my cellar, while the syrah is my top choice by a whisker.

2023 Frankland Estate Riesling
From an excellent vintage. Tank fermented. A full fruity generously flavoured Riesling, with characteristic floral and citrus lime in abundance. Hints of white peach and a pleasing crisp finish. Will do nicely as aperitif but also enhance grilled fish. (13% alcohol, $35)
2023 Isolation Ridge Riesling
From the original 1988 plantings grown at 256m above sea level. This is similar to the estate Riesling, but with more added aromatics – intense floral and citrus of great complexity. The practice of allowing this wine to rest on its lees for nine months makes for beautiful integration of acidity and phenolics, giving the wine its ‘yumminess’, impressive minerality and length of flavour. A world class wine. Delicious now but will mature and develop for 10 years plus. (13%, $55)
2021 Frankland Estate Shiraz
A fraction of Viognier, Marsanne and Touriga make for a nuanced shiraz style. The bouquet of spice and pepper so typical of cooler climate shiraz fleshed out with red berry and earthy tannins. A wine of balance that the Great Southern does so well. (14.5%, $35)
Review by Dr Louis Papaelias2022 Isolation Ridge Syrah
Syrah is used to denote a style of shiraz that pays homage to the elegant examples from the Rhone Valley. It is fully justified here. Viognier 1.5% and mourvedre 3.5% add aromatics and complexity to a bouquet of spice, licorice, cherries, violets and plum. Again like the riesling, a world class wine and worth every penny. Coincidentally, I recently shared a bottle of the 2018 version with friends and it was just as delicious and youthful. (14%, $55)
Named in honour of Harold Olmo, the US-born viticulturalist who in 1955 declared that Frankland was at least the equal of any place in Australia or California when it came to the potential for Bordeaux-beating cabernet blends. The blend here is surprisingly cabernet franc dominant –90%, cabernet sauvignon 8%, malbec 2%. A blend commonly seen on the right bank of Bordeaux around St Emilion. A nose of complexity. Cedar, subdued fruits, violets. A lovely gentle fruity and savoury palate which caresses and fills the mouth and lingers in its aftertaste. Not a trace of harshness. A worthwhile alternative to the cabernet sauvignon wines that we are usually exposed to. (14.5%, $90)


Well-known jazz composer and conductor Mace Francis releases a tenth album with his orchestra and confesses it’s his most musically revealing.
When you spend a lot of time working with other people’s songs and directing bands, it’s really nice to spend some time on your own creative projects.
For Perth-based jazz notable Mace Francis, his tenth album with the Mace Francis Orchestra was the opportunity to let his imagination run wild.
No stranger to Australia’s jazz community, you might recognise him as artistic director of the Perth International Jazz Festival and the WA Youth Jazz Orchestra, or current Churchill Fellow and composer and band leader of projects including Mace Francis Plus 11 and his New York Nonet.
But if you fancy getting a bit more up close and personal, the Mace Francis Orchestra’s new album is titled No Postcode. Released on April 12, it features six jazz and big band instrumental tracks which have been written and taken different forms over the past six years. What they share is a chance for Mace to express different sides, musical influences, harmonies and orchestral colours.
“I’m particularly excited with this one because I took my time and I wasn’t in any rush,” says Mace.
The album’s title track was a commission for his funeral from
By Ara Jansenfriend Victor O’Connor. Performed live at Victor’s wake, it explores isolation, loss and loneliness but isn’t a sombre listen, especially being influenced by Frank Zappa and Turkish folk.
“I was able to play him a recording from a rehearsal before he died. He loved it and it got the thumbs up. We played a set at the funeral, and it was a real celebration of his life.”
Mace doesn’t play an instrument in the MFO. He directs from the front as conductor and writes and arranges all the original music they perform.
“I lead the orchestra to make sure the music lands the way I want it to, the way I imagine it to sound. The great musicians I work with make it come to life. My job as a conductor during a performance is to make sure everyone comes in when they are supposed to. They all know where they are in the music, but if they look up and need help, then I’m there to guide them through.”
Mace still gets nervous presenting a new tune to the musicians, even though the orchestra has been going for nigh on two decades. While the line-up does change from album to album, musicians Ricki Malet, Ben Collins, Mark Sprogowski, Catherine Noblet and Greg Brenton have remained stalwarts and do numerous solos on the tracks.
The album’s front cover is an original black and white photograph of a caravan, isolated under a tree and cloudy sky, which gives off a feeling of isolation and loneliness.
“This album is more sombre than the others. It’s also the most personal. It’s my main creative outlet. All the other things I do in my life, all the other musicians and music I work with, influence the MFO. Watching younger musicians grow is inspiring. Meeting people from around the world and watching them play inspires me. Composing music is a lonely business, so all the things I do give me the best of both worlds.
“Musically, however, I think I’m much better at celebrating the darker things in my life than the good things, though I am not a depressed person. I like music that is a bit darker and with more tension, I gravitate towards that.
“With No Postcode I got to be more self-indulgent with my darkness. I see a beauty in the darkness as well. The textures and tensions are gorgeous. I see a lightness, beauty, hope and potential in that.”
No Postcode will be released digitally and on CD and vinyl and the album launch happens on April 13 in the early slot at the Ellington Jazz Club.
Tickets from www.ellingtonjazz.com.au
DUNCRAIG
Highly Sought Rare Medical Suite
+Unique opportunity as long term tenant retiring
+98sqm medical consulting suite
+Ample parking
+3 consulting rooms
+Opposite Glengarry Hospital
Asking Rent
$34,300 pa + GST & Outgoings
For further details please contact Rob Selid 0412 198 294
Hollywood Medical Centre
Suite 36, First Floor, 85 Monash Avenue, Nedlands 87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339

Treendale Medical Group
– GP Positions
•DPA Area’s and MMM5 Available
•FSP GP’s are welcome to apply
•Busy & well established Medical Group with 4 Location in the South West of WA
•Full time & Part Time GP Positions in Treendale & Harvey
•Fully computerized and accredited modern practice with nursing and admin support
•Well supported with large team of experienced GP’s
•Situated in the beautiful South West Region surrounded by coast and forest and close to tourist areas in the south of WA
•Only 1 ½ hrs from Perth
•Family friendly working hours and no on call or hospital cover required
•65 – 70% of billings depending on experience
Please forward CV and enquiries to Kylie Wilson kyliew@harveymed.com.au

DUNCRAIG
Duncraig Medical Centre GP required
Full time patient load available. Flexible hours seven days
Excellent remuneration –$200 to $300 per hour.
Predominantly private billing practice
Modern fully computerised practice (Best Practice)
Please contact Michael on 0403 927 934 or michael@duncraigmedicalcentre.com.au

ATWELL
Require VR GP’s Unrestricted for Part-time Positions:
As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights What’s in it for you:
•Supportive and Experienced Admin team
•Doctor owned practice
•Nurse Support
•Onsite Pathology
•Flexible arrangements
•AGPAL Accredited Practice
•Located near FSH and SJOG Murdoch
•Mixed Billing (mainly Private)
If you are interested please contact our Practice Manager for further information on 9332 5556 or email: adminmetrogp@metrogp.com.au

GREENWOOD
Kingsley Family Practice
We are seeking a part time or full time GP to join our well established, busy practice.
You will work in a highly equipped AGPAL accredited practice, alongside GPs with extensive specialised skills, including skin cancer surgery (including flaps and grafts), cosmetic medicine, ultrasoundguided musculoskeletal PRP injections, IUD insertion, ENT operating microscope use, and much more.

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice. We offer a supportive team based culture, experienced administrative staff and quality full time nursing support. Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

We are looking for experience GPs with a passion to make a difference for people seeking help for substance use disorders to join our team at Fresh Start Clinic in Subiaco.
Fresh Start Clinic is the entry point for all clients and patients at Fresh Start. Our doctor’s perform general health checks, and create informed care plans for patient’s recovery.
•Fully bulk billed clinic
•Onsite Pathology
•Best Practice Software
•Nursing support
•Encourage special interest of addiction
•Immediate start
•Free parking Business hours 9am – 5pm
Monday to Friday
For a confidential discussion please email Jeff Claughton ceo@freshstart.org.au

The Best GP Job in Perth – Hands Down! Here’s a job where you finally get Treated (and Paid!) like a Specialist. We are looking for a motivated GP in Skin Cancer Medicine. Join a clinic that puts you first and helps you excel in your career :
•100% Private Billed Skin Checks. No exceptions.
•Procedures privately billed with high gaps
BULL CREEK
Bull Creek Medical – VR GP opportunity
We are seeking full time or part time VR GP to join our friendly team.
It is a mixed billing well established practice providing quality health care for many years.
It is located closer to world class public and private hospitals and near by top public and private schools.
Flexible working hours and terms and conditions are negotiable.
If you are interested in this exciting opportunity, contact practice manager via email:
admin_pm@bullcreekmedical.com or call on 08 9332 0488

NEDLANDS
Niche, Boutique Medical Centre looking for PART-TIME OR FULL-TIME VR GP
Our practice is situated in the Golden Triangle in the Western Suburbs.
Standard consult 23 - $100, 36 - $180 Practice nurse, and an outstanding administration support.
One Saturday per month (AM only) with higher rates.
Please send through your EOI to: manager@nedlandsmedicalcentre.com.au
VR GP POSITION – Full time/Part time
•A busy, well equipped, fully computerized and AGPAL Accredited GP Practice in Perth, WA is looking for a VR Doctor
•Flexible days and hours tailored to your need
•Excellent RN and reception team as well as managerial support and onsite pathology
•Clinical full autonomy guaranteed
•Mixed Billings, using Best Practice Software
•GP private ownership
•Good income potential and emuneration at 72%, negotiable.
•$150 hourly minimum for the first three months.
The practice provides general GP services including skin check and many more.
For enquiries,
Email: highwycombemc@bigpond.com
Phone: 08 9454 6987
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
The practice itself is highly equipped, including on-site ECG, spirometry, ABI machine, ultrasound, digital dermoscopy imaging, ambulatory BP monitoring and a full time chronic disease management nurse.
Mixed billing, offering our GPs 70%.
All appointments privately billed on Saturdays.
For more information please email kingsleypractice@gmail.com or call our Practice Manager Tracy Weare on (08) 9342 0471
•State of the art Mole Scanning Technology
•Fast on boarding, training and mentoring
•Happy staff and expert colleagues
•Expand to Cosmetic medicine or Vein Sclerotherapy
•$200 ph min
•And more…..
What are you waiting for?
moleclinic.link/Best-Job
Please contact Practice Manager on 08 9301 1825
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert

KALAMUNDA/ HIGH WYCOMBE
•Well established and regarded medical practice, about to celebrate 60th year, offers a unique opportunity for a VR General Practitioner
•Long history of being a training practice, both GP Registrars and Medical Students.
•Main surgery in Kalamunda, with a further two surgeries in High Wycombe and second satellite surgery in Kalamunda
•Mixed billing (or private billing if preferred)
•Well organized for Chronic Disease Management and Care of the Elderly, with Primary Care (CDM) Nursing Staff at all four surgeries
•Very nurturing practice, empathic to patients and staff. Supportive of clinical team members with individual special interests (such as cosmetic and skin lesion skills, mental health, LGBTIQA+…)
•Excellent schools in the fantastic Perth Hills area, very welcoming community
•Work life balance a major priority that is respected by the team at Stirk
•Have the best of both worlds; country living with the city only 30 minutes away
Please forward a CV and any enquiries to either Karin Tatnell (0438 211 240) or Dr Mike Civil (0419 965 377 ) or email : manager@stirkmedicalgroup.com

MOUNT LAWLEY
VR GP - Mount Lawley WA - Privately billed After Hours practice
GP After Hours Mount Lawley is a well-established, community-based after-hours practice. We privately bill and are GP owned and run.
We are looking for an experienced VR GP to join our team of clinicians in providing quality after hours care to our patients.
Our practice offers:
•Modern facilities with a fully equipped treatment room
•Fully computerised practice using Best Practice software
•Percentage of the billings with a minimum hourly rate guarantee
•All sessions are 4 hours in duration
•Opportunity for weekend / public holiday sessions
For all enquiries, please email Gina at gpahmtlawley@3rdave.com.au or call 0412760871
75% OF BILLINGS!!
GP positions available in accredited mixed-billing clinics in Burswood and Claremont.
Looking for VR GPs and non-VR GP’s on a full time/part-time basis for weekday and Saturday afternoon sessions. Fully computerised with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

Hillarys Medical Centre is a very busy practice located 15mins from the Per th CBD along the coast. We have a strong focus on family & preventive health medicine
We are a team of 10 doctors with excellent administrative and nursing support staff. We have been in Hillarys for 20 years with dedicated GP owners. We pride ourselves with providing exceptional health care to our community of Hillarys.
We have a modern purpose built well equipped 3 bed treatment room and 10 consulting rooms with quality equipment as well as a spacious staff & meeting room. We are also able to offer secure remote access and secure onsite parking. Pathology & Pharmacy are within our complex.
There is a high-income potential as we are mainly a private billing practice. We would also encourage doctors to develop their own special interests
Our patient base is varied as well as a strong family base practice including women’s & mens health, skin cancer medicine, iron infusions, aviation medicine and more. Our nurses are committed to support for care plans & health assessments.
We are a 7 day a week (Mon to Thur 8am to 7pm, Fri 8am to 6pm, weekends 8.30 to 12.30pm) we have a variety of sessions available and the opportunity to share a Saturday roster with your fellow GP colleagues, with nursing support.
We would require:
Current unrestricted registration with AHPRA as a general practitioner
Current medical indemnity insurance
Full Australian working rights and No DPA restrictions
For confidential discussion please phone
Dr Rod Parker 0447 117 013 or Dr William Thong 0403 171 061 or by emailing admin@hillarysmc.com
COMO
Opening for VR GP - F/time or P/time
Full Private List available now from retiring GPs FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs. Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au

BENTLEY
Burton Street Family Practice
Unrestricted VR GP required for well-established privately-owned mixed-billing practice
With an interest in all areas of general practice, you are expected to share our mission to provide high-quality care for the whole family in a coordinated fashion. Serving a diverse patient demographic, we aim to manage chronic illness to avoid complications and acute issues and reduce the need for hospital presentation and admission.
You are provided clinical autonomy and supported by a strong team of Australian trained GPs, nursing and administrative staff. AGPAL and WAGPET accredited, we offer the opportunity to be involved in teaching medical students and GP registrars.
FREMANTLE
P/T GP required for our friendly practice in the heart of Fremantle. Young demographic with lots of student health, sexual health, women’s health and mental health. Fully equipped, accredited practice with full time practice nurse and onsite pathology, 2-3 days/week, days negotiable.
Contact Stephen on 0411 223 120 or at stephen@westendmed.com.au
Please apply to burtonst@burtonst.com.au or call 08 9458 4558
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert

Gosnells Healthcare Centre has a great opportunity for General Practitioner to join a very well-established practice.
The role would suit a new Fellow or GP who wants to curate their own patient base with a guaranteed minimum offered for 6 months.
Wonderful, friendly practice
Experienced Doctors
Very Large existing and loyal patient base
Mixed billing practice
Enjoy an innovative, modern practice with the latest equipment and software (Best Practice)
70% of billings- plus attractive relocation package
Choose your hours, Our Clinic is open from 8am-5pm Monday-Friday.
On-site services include Pathology, Physiotherapy, Podiatry, Dietician
Fully Accredited practice
DPA Replacement Provider Number available
Safety Net of $150 per hour for 6 months
If you are interested in the exciting opportunity please contact Phil at ceo@spectrumhealth.net.au
Gosnells HealthCare Centre
2227A Albany Highway, Gosnells WA 6110
Join our team at Bullsbrook Medical Centre where you will enjoy every aspect of general practice. We are a well-established clinic with a strong and loyal patient base.
• Value driven, innovative, non-corporate GP owned medical centre with a highly competent administrative and nursing team, supporting the practice and allowing you to focus on servicing the patient demand.
• Large patient base with broad demographics.
• Team of GPs providing high quality care with a strong focus on comprehensive chronic disease management
• Fantastic opportunity for GP’s with special interests
• Friendly working environment of mutual support
• On-site Practice Manager, pathology and allied health.
• Fully computerised (Best Practice).
• AGPAL accredited.
• Training Practice for GP Registrars.
• Independent Contractor Agreement with high income potential
• Incentivised opportunity for FRACGPs interested in providing supervision to training GP’s.
Requirements:
Unrestricted AHPRA registration, VR/FRACGP
For a confidential discussion please contact Dr Raf Francikiewicz on 0424436663 or email raf@bullsbrookmedicalcentre.com.au



Mosman Park Medical Centre is a GP owned practice. We are looking for another GP to join us.
We have six consulting rooms and it is a lovely calm, caring environment with a great patient base. We are close to all amenities including shopping, cafes, beaches and river.
This can be a full-time or part-time position with scope for all GP areas of interest.
Our team of friendly receptionists is complemented by two experienced practice nurses at all times.

For more information please contact admin@mosmanparkmedicalcentre.com.au
Are you seeking a workplace focused on best practice and excellence in clinical care?
At Perth Cardiovascular Institute we believe in providing more than just a diagnostic imaging service. Our team are committed to delivering an excellent patient experience along with clinically robust findings in a timely manner.
Senior staff perform as leaders and assist with training, mentoring and development of less experienced team members. Much of our time is dedicated to ensure our trainees develop superior skillsets to tackle even the most difficult of cases. We foster an environment that promotes asking questions, seeking feedback and sharing of knowledge.
We have world class, internationally renowned cardiologists within our group that support and develop individuals. Our cardiologists are approachable to discuss patient findings and encourage and enable team members to manage patients. In completing our daily duties we go above and beyond expectation with clients repeatedly providing outstanding feedback from their contact with us.
If you wish to know more about the role, feel aligned to the way we do things and are excited by the unique opportunity Perth Cardio offers then we would be thrilled to hear from you.
Please contact Adam Lunghi on Phone (08) 6314 6881 or info@perthcardio.com.au

Ourbeachsidepracticein Albanyis lookingfornewGPs

FRACGPpreferred,flexiblearrangements
Relocationassistanceoffered
Largeanddiversepatientbase,mixedbilling
Yourownspaciousroom
FullycomputerisedandDoctorowned
Nooncallorafterhours



Foraconfidentialdiscussionabout yournextcareermove,call
Jeanat 0400605529 oremail jean.paradise@breckenhealth.com.au

Northbridge Medical Centre is looking for a VR General Practitioner to join our well-established private billing medical practice located between Perth CBD and Mt Lawley
Owned and operated by doctors
High patient load
Taking over existing patient base from relocating GPs
Full Time or Part Time Position available now
65% billings with minimum of $150/ hour for the first 6 months
Joining a team of 6 Doctors with supportive
Nursing, Management and Marketing team
AGPAL accredited, well equipped and fully computerized with Best Practice software
Doctor’s parking available
Requirement: MBBS or equivalent, Vocational Registration / Fellowship, current AHPRA registration
If you are looking to practice quality medicine in a supportive environment, please contact Dr Alex Koh on 0408 037 290 for a confidential conversation or email at Alex@northbridgemedical.com.au
Position will be located on Christmas Island (Indian Ocean Territories) Full time Ongoing Vacancy | Generous remuneration package - negotiable
The Indian Ocean Territories Administration (IOTA) is currently seeking a motivated, professional and suitably qualified person to join our team as the Director of Public Health & Medicine (DPHM) within the Indian Ocean Territories Health Ser vice (IOTHS) based on Christmas Island. This position is a similar level to a Western Australian Country Health Ser vice Senior Medical Officer position.
Package valued in excess of $440,000 including:
Base salary
Employer contribution to superannuation
Commuted allowance calculated at 30% of the annual base salary
District Allowance payable in addition to base salary
Professional development expenses allowance
Generous leave entitlements
Annual return airfares assistance to Perth
Remote support package (including access to subsidised housing and vehicle) for eligible candidates
The IOTHS delivers a primary and acute health care service in two of Australia’s most remote and most spectacular settings - Christmas Island (CI) and the Cocos (Keeling) Islands (CKI). IOTHS includes a 24 hour eight bed hospital and primary care facility on CI and clinics on Home and West Islands in the CKI. The IOTHS is committed to “Working with our communities to keep us healthy for the whole of our lives”.
The DPHM is primarily responsible for the delivery of quality medical and emergency services to the communities of CI and the CKI. The DPHM will: Supervise and support the District Medical Officers on both CI and CKI; the Medical Scientist and Community Social Worker on CI, using performance agreements and structured performance appraisals; Undertake clinical duties by providing direct patient care to the community in primary, secondary, emergency and community health care settings; Provide advice on the appropriate visiting specialist’s arrangements (medical and allied health) and for reviewing services provided;
Provide leadership to direct reports and ensure responsible, efficient and effective management of the human, physical, financial and systems resources for medical services;
In addition, the DPHM further plays a key role within the Executive Management Team of the IOTHS.
Our ideal candidate will have a demonstrated ability to lead and manage a clinical portfolio, have recent (within the last 12 months) and substantial experience working effectively in a rural or remote cross cultural environment within an Emergency Department, as well as experience in in-patient management, public health, women’s health, child health and chronic disease management. Further the successful candidate will also possess emergency life support skills and be committed to ongoing medical self education and the education of other staff.
The successful candidate will be registered as, or be eligible for, a medical practitioner with the Australian Health Practitioner Regulation Agency (APHRA), and hold a post graduate qualification and/or have recognised current clinical experience in General Practice. Further, the successful applicant will also hold a current Western Australian Working with Children Check, hold a ‘C’ class manual Driver’s Licence transferable to the Indian Ocean Territories and be subject to a health assessment and preemployment screening.
For an application pack outlining how you can apply for this oppor tunit y, please contact the IOTA Human Resources Team at IOTHRTeam@infrastructure.gov.au and quote position number 109097






1.
2.
3.
Spectrum Health has a team of professional and skilled managers with many years of industry experience who ensure the seamless and successful operation of medical practices.
Dr Vishnu Gopalan, the Chairman of Spectrum Health helms an expansive network of medical centres with a
6.
strong
The Spectrum Health team welcomes the opportunity to partner with you in general practice.




