It is not by accident that the theme of the August edition is cancer care – it’s not cancer research, or cancer breakthroughs. It’s care – and it is being delivered every single day, by every single doctor and bench boffin travelling the path alongside a person with cancer.
By some mystical hand or simply lucky spins of the Russian roulette wheel, my experience of cancer care has been as an observer when a loved one is told they have some insanely hideous cancer that will kill them.
In my two closest encounters of cancer treatment, the first was hopeless, the second is ongoing. In both, the care was and is exceptional.
Perhaps it’s the diagnosis of cancer itself that flips a switch. I witnessed our GP move from jovial guardian, to a martial sentinel, speedily gathering as much evidence to expedite that appointment with a specialist. The hospital bedside visits, the counselling to near and dear that GPs and oncologists do so well, was Care and it meant the world.
Recently, I have watched the phenomenon that is Charlie’s Cancer Centre as a family member takes on melanoma.
As a journalist, we hear lots of talk of dysfunctional and overstretched health systems that are taking their toll on patient outcomes and those who work within it. Yes, there is truth there, but that doesn’t take into account the thousands of people who are triaged through the emergency system and into treatment and then home again every day.

In our case, it was triaged and fast-tracked to the Cancer Centre where neurosurgeons, meet medical oncologists, meet radiation oncologists – and a patient and their family who are truly cared for. Hells bells – the staff at the Cancer Centre actually communicate, not just with patients, but with each other AND practitioners … in OTHER hospitals. There is not just care on offer but coordinated care.
Now I can’t speak for their ability to keep patients’ GPs in the loop, that might tip into Rainbow Unicorns territory, but even in those insanely busy places that treat such high volumes of people, they have time to talk with patients AND their families, and if necessary, explain to them again the next day if concern or confusion still reigns. Yes, there are drug trials and the cutting-edge technology which allows these practitioners to offer treatments that have greater efficacy, but it is their care and their ability to look into a patient’s eyes and tell them that they will do everything they can that holds the healing magic.
SYNDICATION AND REPRODUCTION
Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
Yes, there are drug trials and the cutting-edge technology which allows these practitioners to offer treatments that have greater efficacy, but it is their care and their ability to look into a patient’s eyes and tell them that they will do everything they can that holds the healing magic.
14 Cover story: Melanoma in the crosshairs


20 Trials a lifeline

26 Close-up: Dr Janice Bell

40 Raine Study – the Next Gen
60 See the art behind the art
62 Wine review: Castelli Estate – Dr Craig Drummond MW

Dr Crystal Durell, far left, from the Garden Family Medical Clinic was the happy recipient of the Cape Grace doctors dozen from our monthly competition. We also caught up with the winner of May’s winner of Singlefile’s excellent dozen, Dr Smitha Pillay from Balcatta Medical. This month on page 63, Dr Craig Drummond revisits Castelli Estate and falls in love with the tastes of the Great Southern.
To win the wine, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.

PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au

Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au








Marketing Rhiannon Arnold rhiannon@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
OUR PRINTER’S ACCREDITATIONS
49
50

Integrating AI and real-time in vivo digital pathology Professor Camile S. Farah



Nerve entrapment syndromes Professor Krishna Boddu

44
What our biotech sector can learn from Boston Dr Liz Dallimore

Perth Children’s Hospital (PCH) has been chosen as the lead Australasian site for the international PROSpect study, the Prone and Oscillation Paediatric Clinical Trial.
PROSpect principal Investigator Professor Martha Curley from the renowned paediatric intensive care unit (PICU) of the University of Pennsylvania’s School of Nursing was in Perth to meet the study team.
The trial will benefit patients who require ventilation due to acute and severe respiratory failure and aims to identify which combination of ventilation (conventional or high frequency oscillation) and positioning (either supine or prone) is the most effective.
Head of Paediatric Critical Care at PCH Dr Simon Erickson said Professor Curley’s visit was a boost for the PCH PROSpect study.
“Professor Curley’s visit provided welcome recognition of our success with this trial and the fact we have become the lead Australasian site,” he said. “This achievement reflects our dedication to this project and our commitment to improving the outcomes of our patients, particularly given the challenges of recruiting participants to trials like this.”
Fifteen-year-old Annabelle Carr has spent a significant amount of time in the PICU having undergone more than 80 surgical procedures over her lifetime. The procedures relate to her oculodentodigital dysplasia, a rare genetic condition that affects many parts of the body particularly her eyes, teeth and fingers.

The Royal Australian College of GPs has had confirmation that the Western Australian Government does not intend to change the way its existing payroll tax provisions apply to general practice.
RACGP WA Chair Dr Ramya Raman received written confirmation from the government after raising member concerns that WA might follow other states in putting an additional payroll tax burden on GP practices.
Practice owners across Australia already pay payroll tax on their employees, including receptionists, registrars, and nurses, but it hasn’t previously applied to GPs. This is because most doctors are not employees – they lease rooms and facilities from a practice owner and operate under independent agreements.
However, recent court judgements in New South Wales have considered GPs at certain medical practices as employees for payroll tax purposes.
Last year Annabelle became acutely unwell with abdominal pain and underwent emergency surgery at PCH to remove part of her large intestine. She later developed sepsis. She then had to have emergency open heart surgery followed by four weeks in ICU. Her mother Marina consented to be part of the PROSpect study during this time despite her daughter being so unwell.
“It was hard to see Annabelle lying on her stomach once she was part of the trial, but we were pleased at how quickly she recovered, and the ventilator was removed. Despite the stress at the time we knew participating in this study would help other patients in the future,” Mrs Carr said.
Annabelle has now fully recovered from this experience and is pursuing her passion for writing with renewed vigour.
The RACGP has been advocating strongly in all states since and has secured amnesty periods for GPs in South Australia and Queensland.
Deputy Premier and Treasurer Rita Saffioti said under WA’s existing payroll tax provisions, most GPs working in medical practices under independent agreements “are considered contractors running an independent business. The $1 million tax free threshold means the majority are not subject to payroll tax. The Western Australian Government does not intend to change these provisions.”
RACGP WA Chair Dr Ramya Raman welcomed the confirmation as a relief for WA’s GPs.
“Practices operate on thin margins, and if they are hit with an additional payroll tax bill, which can be hundreds-of-thousands of dollars, they will be forced to pass the costs on to patients. If patients can’t afford the gap fees, practices will close,” she said.
The Resolute team headed by psychiatrist
Dr Richard Magtengaard is preparing for its first clinical masterclass – “Caring for those who Serve” at the UWA Club on Saturday, September 2.

Resolute has constructed and is executing a comprehensive approach toward integrating high-quality, trauma-informed clinical services for ADF personnel, veterans, first responder communities, and their families. This year it is partnering with Soldiers & Sirens for the masterclass.
Dr Magtengaard said clinicians were welcome to attend alongside those who have served (and their supporters) to learn from experts
continued on Page 8
PBCI offers streamlined and personalized care for individuals diagnosed with early or advanced breast cancer.
Our team includes specialist breast surgeons, medical oncologists, experienced breast physicians, and a genetic counselor.
We also have dedicated nurses, psychologists, an oncology fellow, a research team, and on-site radiology and radiation oncology.
This comprehensive approach allows us to provide tailored and coordinated treatment options for each patient
PBCI provides a Breast Care Nurse and clinical psychologists to support breast cancer patients
Patients can be seen by an experienced Breast Physician Same-day breast imaging and diagnostic biopsy is available Surveillance for patients with familial high risk is also available.

Breast Cancer Research Centre - WA

Hollywood Consulting Centre Suite 404-407 91 Monash Avenue, Nedlands 6009
T | 08 6500 5501
Clinical trials offer patients access to international drug treatments and patientfocused research to better understand the biology of breast cancer



Dr Shane Kelly, former head of St John of God Health Care has been appointed state manager of Ramsay Health Care.
Dr Michael Page has been inducted as the new president of the AMA (WA) taking the reins from retiring president Dr Mark Duncan-Smith
Health professionals figured prominently in the finalist lists of the Premier’s science awards. Among them, haematologist Professor Wendy Erber (UWA), Alzheimer researcher Professor John Mamo (pictured, Curtin University) and autism researcher Professor Andrew Whitehouse (UWA and TKI) are in the running the Scientist of the Year.

Among the finalists of the mid-career award are paediatric anaethetist Professor Britta Regli-von Ungern-Sternberg (UWA, PCH) and mental health researcher Professor Ashleigh Lin (TKI).
The early career awards acknowledged Dr Rebecca Bennett (Ear Science Institute Australia and Curtin University), microbiologist Dr Kieran Mulroney (Perkins Institute) and clinical psychologist Dr David Preece (Curtin).
In the student category, Denby Evans (TKI, Curtin) is acknowledged for her work with preterm infants, Ingrid Stacey (UWA) for her research on data linkage for acute rheumatic fever and rheumatic heart disease, and biochemist Somayra Mamsa (UWA) on neurodegenerative diseases.
The $20 million development at Abbotsford Private Hospital in West Leederville has opened offering 47 new mental health inpatient beds, new group therapy rooms, administration facilities and additional car parking. The total number of mental health beds now at Abbotsford is 77, more than doubling the hospital’s patient capacity.
continued from Page 4
across respective specialties, and gain meaningful insights from those with a lived experience.
The program includes presentations from James Hepworth, principal of the Veteran Employment Program at Roy Hill, Dr Michael Winlow on medicinal cannabinoids and therapeutic application, exercise as medicine by Katie Stewart and Alex Lim on ketamine, neuroplasticity, treatment-resistant depression and PTSD among other topics.
For clinicians, eight hours of CPD points can by claimed.
All proceeds from the day will go to Soldiers & Sirens WA charity.
Tickets from https://www.trybooking.com/CJNDA and information from hello@resolute.support | www.resolute.support
continued on Page 10
A type of bacteria not routinely tested for has been discovered as the second most common cause of bacterial gastroenteritis, in a study of over 300,000 patient samples.
Researchers from UNSW Sydney have identified Aeromonas as the offending bacterial pathogen.
Until now, it has been believed that after Campylobacter, Salmonella was the next most suspected.

“Our results have found that Aeromonas are the second most prevalent enteric bacterial pathogens across all age groups and are, in fact, the most common enteric bacterial pathogens in children under 18 months,” said Assoc. Professor Li Zhang.
The latest findings, published in Microbiology Spectrum, could have an impact on the diagnostic process for gastroenteritis and ultimately lead to more targeted treatment.
“Historically, Aeromonas species have been largely overlooked and understudied, but they are increasingly recognised as emerging enteric pathogens globally,” A/Prof. Zhang said. The team analysed quantitative real-time PCR data from 341,330 patients with gastroenteritis in Australia between 2015 and 2019 and results were grouped by patient age. Researchers identified a unique infection pattern, characterised by three distinct infection peaks associated with age.
“The occurrence of Aeromonas enteric infections was predominately observed in young children and individuals over 50 years old, suggesting a higher susceptibility to these infections during stages where the immune system tends to be weaker,” says A/Prof. Zhang.
“These findings suggest that both human host and microbial factors contribute to the development of Aeromonas enteric infections.”
Australian medicinal cannabis company Little Green Pharma awarded commercial tender to supply up to AU$1.6 million of its CBD50 product to a French medicinal cannabis trial.
“But the high rate of Aeromonas infection discovered in our study, and significantly, how they are impacting different patient age groups, suggest that Aeromonas species should be included on the common enteric bacterial pathogen examination list,” says A/Prof. Zhang.



continued from Page 8
More than $8 million has now been paid to 340 Western Australian general practices following their applications for a Strengthening Medicare General Practice Grant. With more than 600 applications lodged with WA Primary Health Alliance (WAPHA), the grants are set to support these WA practices to expand patient access.
Most practices have opted to invest their grant across three different (or combined) streams – enhancing digital capability, upgrading infection control, and maintaining or achieving practice accreditation.
A statement from WAPHA said that while the GP grant application process involved additional steps compared to other initiatives, “most WA general practices are now set up as a WAPHA supplier. The benefit of this to practices is that applications for future funding opportunities, such as those flagged in the May 2023 Federal Budget, will be streamlined.”
Data from the Australian Institute of Health and Welfare released results
of its cancer screening audit and in the March quarter this year, 846,000 invitations to participate in the bowel cancer screening program were sent to eligible people aged 50-74.
Of these invitations, 52% were sent to women (437,000) and 48% sent to men (409,000), with 363,000 kits returned for analysis. Of these, 54% were returned by women (197,000) and 46% returned by men (166,000).
The number of completed kits returned was higher than in the December quarter (296,000) and the March quarter a year prior (193,000).
The March quarter 2023 experienced a peak in the number of invitations sent and the number of completed kits returned (846,000 invitations and 363,000 kits respectively) compared to the March quarters of the three previous years (496,000 invitations and 193,000 kits in 2022, 693,000 invitations and 243,000 kits in 2021 and 752,000 invitations and 166,000 kits in 2020).
Observable drops in the number of invitations during summer months was potentially due to the NBCSP Hot-Zone policy, where less invitations were sent to locations where average monthly temperatures are greater than 30°C. Blood present in a collected sample may break down and be more difficult to detect when exposed to high temperatures.
Growing knowledge of the importance of a healthy mouth for overall health and well-being makes access to dental services a priority for the charity Kimberley Dental Team, which was founded by Jan and John Owen in May 2009.
Then, Dr John Owen accompanied his wife Jan, a dental nurse and educator, to Halls Creek because Jan was singing with the Madjitil Moorna students choir comprising children of the Halls Creek District High School. The school welcomed their dental expertise as they had been without a dental therapy service for a considerable time.
It got them thinking about the inequality of dental health care in the remote north so they developed a volunteer team of dental health professionals and the Kimberley Dental Team (KDT) was born.


They have been busy during June and July with two incursions with teams visiting Fitzroy Crossing, having to negotiate the new temporary crossing across the Martuwarra (Fitzroy) river. They ran clinics in numerous communities then on to Halls Creek, Kununurra and back to Halls Creek with stops all along the way. Clinics were set up from district hospitals to front verandas and everything in between.
Eighteen months after acquiring Life Ready physiotherapy clinics, HBF is preparing to rebrand five of the 19 West Australian outlets to HBF Physio. Baldivis, Busselton, Butler, Midland and Rockingham locations will get the name change, while a new clinic in Bull Creek will open alongside the existing local HBF Dental centre.
Physiotherapy is HBF’s third mostclaimed ancillary benefit, accessed by 160,000 members who spend $75 million on physiotherapy services annually.
“Our expansion into the delivery of health services through not only the acquisition of Life Ready last year but also the establishment of HBF Dental enhances the value of private health insurance for our members,” said HBF’s Dr Daniel Heredia.
He said Life Ready and HBF Physio clinics were open to anyone, regardless of their health fund membership and clinical decisions would continue to be made independently by practitioners.
HBF Physio will provide exclusive offers, including a no-gap standard initial physiotherapy consultation for eligible HBF members. And the fund would also cover relevant members for the GLA:D osteoarthritis education and exercise program at Life Ready and HBF Physio clinics.
KDT has collegiate sponsorship from dental groups as well as the McCusker Foundation, Rotary and this year received a grant through the Office of the Chief Dental Officer.
Who is eligible for bowel screening?
Aged 50-74 years

Has a bowel
Who is eligible for breast screening?
Aged 40 years or older
Have breasts or chest tissue
Assigned female at birth
Who is eligible for cervical screening?
Aged 25-74 years
Has a cervix
Ever had any sexual contact
Tips for providing a safe and inclusive environment for your LGBTIQ+ patients


Signs and forms
Display inclusive posters and flags
Update forms to be more inclusive ie. use gender neutral language that allows ample choice for documenting title, pronouns, gender and sexual orientation
Language
Ask your patient about their preferred pronouns. Consider introducing your preferred pronouns
Use gender neutral language
When communicating with patients, reflect their use of language and self-identification. If in doubt, ask what terms they prefer
Training
Provide appropriate and ongoing training for staff on LGBTIQ+ diversity, inclusive care use and terminology
For more information or educational opportunities please visit:
Cancer Council WA Recorded webinarshttps://cancerwa.asn.au/health-professionals/general-practice/recordedwebinars/


Health Pathways Transgender Health and Gender Diversityhttps://wa.communityhealthpathways.org/69205.htm

Sexual Health Quarters EmbraceU is here! - https://embraceu.shq.org.au/
For more information scan the QR code
The article in the July issue of Medical Forum on the difficulty faced by plastic surgeons accessing theatre lists in private hospitals, provided a good overview of a problem that has been developing for a few years.

However, comments made by HBF’s Executive General Manager Insurance and Health Services, Dr Heredia, require clarification.
In the article he is quoted as saying: “It also had to be recognised that because a lot of the procedures in question were cosmetic, when there were scarce resources and
limited theatre time, hospitals had to make decisions on urgent vs cosmetic surgery.” He predicted some of the cosmetic work would “increasingly move into day surgery or doctor-run type facilities.”
The current access issues are not with cosmetic surgical procedures.
Private health insurance does not cover cosmetic surgery. Hospitals charge patients directly for their theatre and admission costs, usually based on length of theatre
AMA WA this year is celebrating its 125th anniversary and the occasion was marked at the association’s Medcon ball last month with more than 500 in attendance to see some of its luminaries recognised for service in the annual awards.
GP Dr Barry Fatovich has long been a health champion and was acknowledged as such with the Jonathan Morling Health Champion of the Year award, sponsored by the Doctors Health Advisory Service WA. Dr Fatovich joined the Lockridge General Practice in 1979, doing the full range of general practice, including care of nursing home residents and GP obstetrics. He was involved in the RACGP as Chair of the National Research Committee and was the State Director of the RACGP training program for 10 years. He has been involved in a variety of community activities and has been a DHAS WA member since 1998.
Former state and national AMA President Dr Michael Gannon won the Hippocrates Award. He is currently president of MDA National. His chairmanships include the perinatal and infant mortality committee for WA
times that are profitable for the hospital.
The Medical Benefits Schedule, and therefore private health insurance, does cover surgical procedures for reconstructive or functional reasons.
For these procedures, the hospital accepts payment according to their contract with the health fund. As the article outlines, this varies but may be based on procedure banding or the DRG system.
The procedures which are currently of greatest concern are autologous
Health and medical advisory committee at St John of God Subiaco Hospital.
The President’s Award went to former Chief Scientist Professor Lyn Beazley who has been a tireless advocate for research into the health sciences through her numerous representations on administrative, research and funding boards.
Dr Brittney Wicksteed is the 2023 Junior Doctor of the Year (the Dr Camille Michener Legacy Award). She is an Emergency Medicine trainee. Dr Wicksteed is the Vice President of the Rural Doctors Association of WA.

The antecedent of AMA (WA) began on August 5, 1898, when a sub-committee was created to progress affiliation with the British Medical Association. Dr Alfred Waylen was unanimously elected president. In 1962, four years after the first medical school was opened at the University of WA, it became the Australian Medical Association (AMA).
In 1975, the first industrial agreement applying to all doctors in teaching hospitals was developed. Nine years later, the AMA (WA) secured formal recognition to represent industrially medical practitioners employed in public hospitals.
breast reconstruction and belt lipectomy following massive weight loss. These procedures are often long and complex, with relatively long inpatient stays.
They utilise a large amount of theatre time which is not adequately compensated for by the amount paid by insurers, and hence leads private hospitals to see them as “loss makers” and actively avoid doing these cases.
This is leading to the current issue where patients holding private insurance, which theoretically covers these procedures, but in practice they have difficulty accessing them in the private sector.
The most common autologous breast reconstruction is a free DIEP flap. This is a complex microsurgical procedure which takes approximately six hours for a unilateral procedure, and often up to 10 hours for a bilateral procedure, when performed at the time of mastectomy.
These patients require high dependency care post-operatively.
Given the complexity of the surgery and aftercare these procedures can only be safely done in large private or public hospitals with appropriate resources. They are not suitable for the smaller day surgery or overnight facilities where many plastic surgery lists are done.
DIEP flaps provide an excellent choice for breast reconstruction for many women, particularly for those patients who for various reasons wish to avoid implant reconstruction or who require radiotherapy as part of their breast cancer treatment.
While they are resource intensive at the initial procedure, there is evidence that in addition to being a good clinical option, they are cost effective over the lifetime of the patient as there is a much lower rate of revisional surgery, often required for implant-based procedures.
Patients requiring belt lipectomy after massive weight loss are also affected by the current situation. These patients have often had bariatric surgery and present having lost 50-60kg or more of weight, resulting in dramatic amounts of excess skin.
Contrary to some perceptions these are not primarily cosmetic procedures. These patients have significant functional problems including dragging pain, difficulties with clothing and skin integrity issues as well as significant psychological distress.
Belt lipectomy is, again, a relatively long procedure, with significant risks and aftercare requirements and combined with the frequent co-morbidities found in this group,
means it often needs to be done in a larger facility to ensure the safety of the patient.
The current situation has developed over time due to a complex, often opaque system that means some procedures and specialties are looked on much more favourably than others by private hospitals.
Fundamentally this results in a situation where patients who very legitimately require surgery for medical reasons, are not able to access the care they require.
Ultimately this is about equity of access for patients who have taken out private insurance, with the reasonable assumption that they have comprehensive cover for their health requirements.
The issue requires urgent attention.
ED: Brigid Corrigan is a plastic surgeon and council member of the Australian Society of Plastic Surgeons.


In reply, Dr Daniel Heredia writes: Feedback from plastic surgeons is that access issues are faced for both cosmetic and medically necessary procedures. However, I agree with Dr Corrigan that of greatest concern is the access issues currently faced by patients who require plastic surgery for reconstructive or functional reasons.
“While the AMA (WA) has grown and evolved over the years, our core business and foundations remain the same. Our primary work is to advocate for doctors and student doctors, to continually improve the working conditions of doctors, and engage doctors in policy making for a world-class health system,” the association said.
2 Health Minister Amber Jade Sanderson, Dr Brittany Wicksteed and AMA (WA) President Dr Michael Page


Exciting results from mRNA drug trials on melanoma here in WA are giving heart to patients and clinicians across the globe.
 By Eric Martin
By Eric Martin
There is tantalising new hope for melanoma sufferers with West Australian researchers playing a significant role in the trial of a personalised, cancer vaccine therapy – the first of its kind in the world.
The drug trial is testing mRNA4157, which uses the DNA from a patient’s tumour to help develop a unique treatment for that individual. It is currently being trialled at various hospitals around the world, and lead researcher, Clinical Professor Adnan Khattak , who is a consultant at Fiona Stanley Hospital as well as a private practice at Hollywood Private Hospital, said the trial was taking a personalised approach to melanoma treatment in the hope of improving survival rates over and above that offered by standard immunotherapy.
“Dealing with melanoma in WA is very challenging. Perth obviously has a lot of sunshine, our incidence of skin cancer is considerably higher, and the prognosis depends upon how targeted the melanoma is at the time of diagnosis –because it might be too late,” Professor Khattak explained.

“Men can seek medical help quite late because they either ignore their symptoms or do not do their regular skin checks, and their melanomas can become much more advanced before they are detected. Not to mention the fact that melanomas in men are often more aggressive.
“In contrast, women are usually more careful of their skin and makeup provides some level of protection from direct exposure to the sun, but no matter what happens, I think we need to raise awareness that while these drugs are good, nothing is better than not developing melanoma in the first place.”
The vaccine trial was a phase two study involving 157 patients and, while it was an international study, Australia contributed a significant number of participants, with Perth the leading site worldwide.
“The intention was to take high-risk melanoma patients who had undergone surgery and immunotherapy and were at a
significant risk of relapse. For example, most patients had stage three melanoma, which would carry a relapse risk over 70% within the next five years even after curative surgery,” he said.
“This means surgery is not curing almost two thirds of our patients, and standard immunotherapy is reducing this relative risk to about 30-35%, but that is still a significant risk. Despite surgery and immunotherapy for 12 months, you still stand a one in three chance of the melanoma coming back.
“It is quite an aggressive disease and we wanted to see if we could further shrink this relapse risk and increase the cure rate.
“Secondly, standard immunotherapy is a very generic treatment, where you give the same drug to the same group of patients. It’s not rocket science that it may work for some, but not for others.
“It's a one-size-fits all approach, whereas what we did in the personalised cancer vaccine study was that patients would go through the same pathway, then start their treatment as per the standard protocol, but in addition to that, we also analyse the tumour tissue.”
The tumour removed during surgery was sent to Professor Khattak’s team along with a blood sample for genetic sequencing to identify the specific proteins, or neoantigens, of the cancer cells.
“Using a complex computing algorithm at Moderna, they identified up to 34 such neoantigens and using that data to design a custom-built mRNA vaccine for that individual patient's tumour, which was different than any other vaccine for any other patient on that trial. If we get 10 patients, the tumours will be seen and there'll be 10 different vaccines,” Professor Khattak said.
“In some cases, we identified 31 neoantigens, in some we had identified 32, and in others 34. However, in most instances, we identified certain mutations, then came up with a vaccine specifically designed for that patient's tumour type, which was sent back to the treating institution.”
Moderna has been using AI based algorithms in conjunction with their bioinformatic system, allowing them to generate data for each group of patients that they treat –and with each new patient, more information is collected.
“The whole turnaround time was about six to eight weeks and in the interim, the patient had started the standard immunotherapy treatment so there was no disadvantage to them. When the vaccine arrived, we usually started it with the third dose of immunotherapy, for a total of nine doses,” he said.
“And when we followed them up, compared to what the standard immunotherapy offered, there was further improvement in terms of reducing the risk of distant relapse.
“Obviously, we didn’t know COVID was going to hit a year after starting this trial, but we used the same technology that Moderna then used for COVID vaccination where they studied the COVID genome, identified the spike protein and then produced an mRNA vaccine specifically for it.
“Moderna were too busy making COVID vaccines which meant the computerised random allocation was put on hold for three months, with patients manually allocated for treatment with only one drug.
“When the study reopened, most of my patients ended up receiving the two drugs and I am yet to see a single patient who has experienced disease relapse.”
Professor Khattak said that the single stranded mRNA were sequences of proteins encoded with a simple terminal and encased in a lipid formulation acting as a preservative. There was no toxicity as such and so far, researchers have not seen any long-term complications.
“In fact, standard immunotherapy can lead to many long-term side effects that we see daily, but those on the vaccine trial no one has had a long-term consequence of any sort. Only, short-term immune phenomena have been noted, and many of my patients are now to two to three years on,” he said.
“My personal experience, in terms of treating all these patients, data continued on Page 17
Bethesda Clinic is a voluntary, adult only, 75 bed clinic that provides multidisciplinary clinical services to aid recovery from mental health issues through inpatient and day patient programs.
Services Bethesda Clinic provides:
Inpatient care and therapy programs managed by a multidisciplinary team. Day patient therapy programs in the Wellness and Recovery Centre. Psychiatric and psychological services for those experiencing mental health issues.
Specialties:
DVA-accredited Trauma Recovery for veterans, military and first responder communities. The first designated women’s-only ward in Western Australia, providing a safe recovery environment.

Alcohol and other drug use.
General mental health.
How to refer to Bethesda Clinic:
Download the referral direct from our website bethesdaclinic.org.au/referrals
Find us on HealthLink: Bethesda Clinic
Contact Bethesda’s Triage Officer on (08) 6378 4999 or BC.Triage@bethesda.org.au
Bethesda Clinic
1 Honour Way, Cockburn Central WA 6164
Phone (08) 6378 4900
bethesdaclinic.org.au

continued from Page 15
has shown that in high-risk patients, where 80% of the relapses would have happened by now, we have not seen a single one.
“Much like we saw with COVID vaccination, patients usually get a sore arm, local redness at the site of injection, maybe a bit of a fever or body aches for 24 to 48 hours, and then it settles on its own.
“We also saw that by the time we had administered the third or the fourth vaccine, that was when the immune response really kicked in and then there were very encouraging results, but not practice-changing yet.”
At this stage, a person must have stage two or stage three melanomas with potentially resectable disease.
“The surgeons have already operated on these patients, and then we use those tumour samples to identify whatever microscopic elements of the disease were left behind – that's what we want to mop up,” Professor Khattak explained.
“These are the groups of patients that we really need to focus on, using a more precautionary treatment, because once they develop stage four metastatic disease, the number of patients that get potentially cured is small.
“It is a preventative vaccine in a sense that it is stopping the cancer from relapsing, but it is not a primary prevention vaccine that you could give to somebody to prevent them from developing melanoma –sadly, we are not there yet.”
Professor Khattak said that while the exact cost of the drug treatment was unknown at this stage, as it was administered in the context of a clinical trial, he predicted that it would be an expensive technology to rollout due to the length of the process involved.
“Standard immunotherapy, which is a very generic approach, costs somewhere between $100,000 and $150,000 a year,” he said.
“And if you are talking about personalised cancer vaccine
therapy, there is a lot of logistical steps involved in terms of getting the tumour, sending it off for genetic testing, analysing the blood sample, differentiating normal from abnormal, and then feeding that data into cloud-based computing algorithms to identify the salient features in order to design a vaccine.
“The whole process takes so much time.”
Professor Khattak highlighted that his research group were now working in collaboration with Edith Cowan University to identify certain molecular markers, proteins and antibodies which can be isolated from blood samples taken from a melanoma patient.
“Once you can identify certain molecules, you can target those with specific vaccines and we want to see if we can predict if somebody's going to develop melanoma using blood tests to identify high-risk groups. But I think we’re still a good decade away from that,” he said.
“We are about to start rolling out a bigger clinical research study at Hollywood Private Hospital soon and while we hope that will be the first site in the world to open – and it would be fantastic to get the first Western Australian patient on that study – most importantly, we need to follow the textbook and reproduce these results in the
context of a much bigger study involving at least 1000 patients.
“Our upcoming study is likely to recruit fast, given how positive the feedback has been to the previous study globally. I think patients will seek out these studies as soon as possible, and while an average study takes two to three years to complete this sort of recruitment, I think our study will be able to recruit all the participants within a year.
“I am the primary investigator, and we have got contact details on the Hollywood hospital website, under clinical research, so they can contact us or speak to their treating plastic surgeon who is reviewing the melanoma – most of them are aware of it.
“They can also speak to their GPs who are more than welcome to contact me, and we are very happy to advise if their patient is eligible or not. But the study is not for all the melanoma patients. We are targeting stage two B or higher melanoma because the risk of relapse is high.
Professor Khattak pointed out that this new technology had the potential to revolutionise cancer treatment as we know it.
continued on Page 19
Dermatologist-led cosmetic medicine service

Doctor-delivered treatments, for GP-referred patients
Laser modalities for
Rosacea
Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
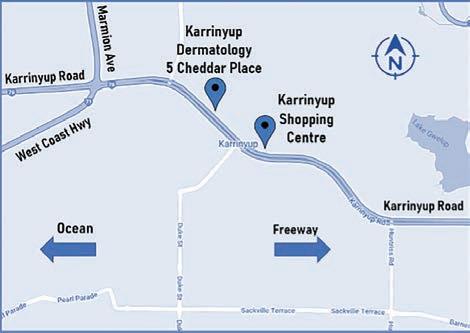
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.


continued from Page 17
“Treating advanced melanoma is just the tip of the iceberg. For example, there was a good pancreatic cancer study published in Nature recently, and even though it was a small group of patients, it showed encouraging results.
“I am also in discussion with Merck and Moderna, trying to get some other studies based in WA as well, and we are proud to be able to offer those studies to our patients. “Our study will also be rolled out to lung, kidney and bowel cancer, which is what has caused so much excitement in the world of cancer management. If you can identify your enemy, you can prepare to meet it better.”
Medical Forum asked Professor Khattak, why, if patients are regularly subjected to blood tests and blood pressure readings when they visit the GP, are skin checks – particularly important for


West Australians – carried out so infrequently?

“I was just talking to a 41-year-old gentleman who is a landscape designer, and obviously, he must work outside,” he said. We see a lot of farmers as well, this is their lifestyle, and they cannot avoid it, but we can at least identify the highest-risk professions and try to raise awareness about greater skin protection as well as insisting on regular skin checks,” he said.
“I'd also highly recommend that all the clinicians discuss participation in clinical trials with their patients because this is how we learn, this is how we find out what works and what doesn't.”
The patients who took part in the Moderna study accessed it in 2019 and 2020 – when the drug was a novel therapy and still not available to public – even though the trial had positive results.
“By the time we recruit phase three,
and the results are still positive, we are really looking at 2026 or 2027 before the drug becomes available to the public,” Dr Khattak said.
“We strongly negotiated and lobbied that public patients should be given the opportunity to take part in these clinical trials. If somebody does not have the resources or private insurance, that does not mean that they are less important or their cancer is less severe, and I think they should be given the opportunity.
“I'm proud that nearly two thirds of our patients are public patients despite this being done in a private hospital.”
Read this story on mforum.com.au
Whether it's for knees, hips, hands, arms, legs or shoulders, St John of God Mt Lawley Hospital orthopaedic services provide care from pre-surgery through to rehabilitation to get your patients moving.
Mr Brett Bairstow
Lower limb (hip and knee) surgery, joint replacement, and sports injuries

Dr Murray Blythe
Lower limb (hip, knee, foot and ankle) surgery and joint replacements
Dr Wael Chiri

Upper limb (shoulder, elbow, wrist and hand) surgery and trauma
Dr Humza Khan
Wrist and hand trauma and surgery
Dr Doug Kingwell




Hip, knee, shoulder and elbow arthroscopy, shoulder arthroplasty and sports injuries
Dr Michael Ledger
Lower
To learn more about our specialists’ expertise and specialties, scan the QR code. Email GP.MtLawley@sjog.org.au • visit sjog.org.au/mtlawley and search ‘orthopaedic surgery’.
Mr Jon Spencer
Upper and lower limb surgery, joint replacement and trauma
Mr Emerik Trinajstic
Lower limb surgery, joint replacement and trauma
Blood cancer was in the spotlight this month with a new report highlighting national inconsistencies in treatment access. Professor Chan Cheah at Blood Cancer Research WA is addressing that here.
 Jan Hallam reports
Jan Hallam reports
The Leukaemia Foundation’s latest State of the Nation report highlighted the difficulty and the inequity of treating blood cancer in Australia, which often started right at the beginning of a patient’s journey.
“Getting an accurate blood cancer diagnosis and the best treatment can be challenging. Difficulties can arise depending on where a person lives and, in some cases, whether they can afford to pay for tests and treatments. It’s unfair that someone's postcode or other personal circumstances could affect the quality of treatment they receive,” foundation CEO Chris Tanti said.
“The inconsistencies in Australia’s healthcare system directly impacts people with blood cancer and this is costing lives. We need continued focus on preparing and implementing national clinical standards to ensure Australians across the country are accurately diagnosed and have equitable access to skilled healthcare professionals who deliver best practice care.”
The report surveyed 4600 people with blood cancer, the results of which formed the cornerstone of its recommendations.
It found that, among some of the inconsistencies in accessing treatment, around 13% of people with blood cancer waited more than two months from their first appointment to obtain a referral to a specialist. A quarter of people with blood cancer were referred to one or more other specialists before being referred to the haematologist they needed. More than a third waited more than a month to see a haematologist.
When investigated, the report found that many life-saving blood cancer treatments and therapies used overseas weren’t routinely used or available in Australia yet.
And that’s what haematologist Professor Chan Cheah has worked assiduously here in WA since 2018 to address.
Professor Cheah is a model research clinician. He graduated in medicine from UWA in 2003, trained at Fremantle Hospital before heading to the Peter MacCallum Cancer Centre in Melbourne and the MD Anderson Cancer Center in Houston.

On his return to WA in 2015, he knew what treatments were being trialled over east and around the world, and what our blood cancer patients were missing out on.
Through his work at Sir Charles Gairdner Hospital, Hollywood Private Hospital and Linear Clinical Research, he was perfectly positioned to address the imbalance. In 2016, he started the charity, Blood Cancer Research WA, which increased exponentially WA blood cancer patients’ access to various clinical trials.
“There was a shortfall in clinical trial offering for haematology patients in WA. Compared with Melbourne and Houston, patients in WA were significantly disadvantaged and a lot of patients were at the point where they had run out of standard options,” he said.
“They were having to make a big decision – either relocate to the Eastern States for a clinical trial or receive palliative care. So, it was clear that we needed to bridge that gap by opening more trials to offer access to novel agents.
“We've been fortunate in the past 5-7 years, in particular, to have seen an explosion in highly effective treatments for patients with blood cancers, and the field is
moving very quickly. However, the shortest possible time between a drug entering phase one trials and marketing (which almost always happens in the US first) is about 4-5 years. And in Australia, the delay until commercial availability is even longer.
“So, I identified pretty rapidly that the major barrier towards opening more studies and having more access to new drugs available for people was resourcing.”
However, there is some truth to the old adage, build it and they will come.
Patient demand wasn’t ever going to be an issue, but Professor Cheah did identify that having clinicians willing to step into the meticulous and time-consuming research realm was.
“There was a bottleneck for specialist time, especially in early phase trials where there's a lot of safety protocols and assessments built in. It's a huge amount of extra work for specialists to treat patients on study, and most people are already at maximum capacity just with their standard job,” he said.
“Not everyone has the desire to be a clinical trial investigator on top of everything else that they do. So, we established at Blood Cancer Research WA a paid pathway for fellows who are early in their career and have an interest in doing extra training as clinical researchers, and that has taken a lot of administrative burden away from specialists.
“Our charity supports the employment of five fellows and two nurse practitioners, through a combination of philanthropic money and partner institutions. The fellow's role is to look after the patients, and they have had an enormous multiplier effect in terms of the ability to get people on study.
“It has allowed us to open complicated, labour-intensive studies and give doctors whose patients may have relapsed with whatever kind of lymphoma, an easy pathway to refer them for new treatment.”
This recruitment model has seen Blood Cancer Research WA increase its trial offerings over the past five years.
“Where four years ago, we had about seven or eight trials going and enrolling 30 to 40 patients a year, those figures have grown to about a rolling average of 30 to 35 studies a year enrolling more than 120 patients,” Professor Cheah said.
“A lot of those patients are still on study even two, three, four years later. The cumulative figure of close to 1000 patients that have been treated on study is because many of the drugs are so effective, the patients remain on study in remission. They are usually well and getting on with their lives. And that’s a great thing to see.”
In the few short years of its life, Blood Cancer Research WA has fulfilled a much-needed gap in offering patients not only treatment but hope, when hope was fading.
“I’ve received amazing support along the way. Philanthropists here have been incredibly generous and my colleagues around the State have been hugely collaborative by referring patients,” he said.
“Many of the successes we've had have largely been driven by referrals from people outside our own catchment. I think this speaks to the fact that my colleagues around the state know that we provide their patients a good service.
“Research organisations like ours depend on that collaboration –without that, we wouldn't have been as successful because, like anything in life, the benefits come from scaling.”
Two families spoke to Health Consumer Council’s Rachel Seeley about childhood cancer survivorship and the fragmented transition to adult services.

Around 750 children aged 0-14 years are diagnosed with cancer every year in Australia, according to Cancer Council. Each devastating diagnosis is met with hope, as advancements in treatment turn the focus to survivorship and the ongoing physical and emotional impacts of childhood cancer.
According to paediatric and adolescent oncologist Dr Thomas Walwyn, many large international studies show survivors of childhood cancer have an increased risk of chronic health conditions that can impact them years later.
“There are well-established guidelines for ongoing, life-long care for these children,” Dr Walwyn said. “These guidelines are changing with the increasing evidence and will continue to do so.
“As such it is vital that adult survivors of childhood cancer therapy are informed and have their care shared with and coordinated by a clinical service staffed with experts in this evolving field.”
Currently, there is no such service in WA. As a result, those who make the transition from paediatric to adult services have little support to navigate a fragmented system that has little big-picture planning for their ongoing wellbeing.
“This service is needed to support the wellness and optimal life participation of the adult survivors of childhood cancer therapy,” Dr Walwyn said.
It’s a sentiment echoed by many families in WA, including two parents who shared their stories with Health Consumers’ Council.
Lee’s son, Hugh, was 15 when he was diagnosed with sarcoma. Having previously had breast cancer herself, Lee had a good understanding of what he was in for and why keeping him connected to friends and community would be so important.
“It made me understand straight away how lonely a cancer diagnosis is and how important it was to keep Hugh as connected as possible. Hugh’s a social kid, it was very important that he didn’t get isolated.
“At times you feel like you're the only person who's going through this. And then when we worked out it was sarcoma, and that’s a rare cancer, that’s even more lonely, because you really do feel sometimes that you are the only person in the world who’s got this thing.”
Lee spoke about how the connection to other kids going through treatment, and their parents, was so important during their time at the children’s hospital (Hugh was treated at Princess Margaret Hospital).
“When we first got there, other parents who were a bit more advanced through the process than us, took us in and stepped us through what was going on and helped us navigate the system in the hospital.”
Communal areas and shared rooms played an important role in maintaining connection, with Lee sharing how small moments like Sunday morning pancake parties and picnics with visitors were vital to the whole family’s wellbeing.
“It made us feel like we were still in the real world, and that’s really important. From what we’ve seen, that support doesn’t seem to be there anymore and that’s sad.”
Through their peer support work, Lee and Hugh have seen the impact of that lack of connection, particularly in older kids who are being treated in the adult system. With less focus on education and none of the camaraderie of other families, the lack of support in the adult system can be brutal.
“They feel very, very alone, and so do their parents,” Lee said.
Hugh was 17 ½ when he transitioned from childhood services, and the
lack of connection and support was something that really struck Lee.
“When he was coming up to the end of his treatment, after he’d had surgery and eight rounds of chemo, that last couple of weeks knowing that we were going to be released from that regular care was scary. And when it happened, we both felt cut adrift.
“We’d had lots of hands holding onto us and stepping us through everything in the child services, and all of a sudden that was going to be taken away from us. Hugh said he felt like there was very little information given to him about what to expect in adult services. He felt dismissed, and I felt the safety net had been removed.”
Being treated in adult hospitals for ongoing care as a childhood cancer survivor is complex and fragmented, as Lee and Hugh soon discovered.
“Hugh said when he was in the adult system and waiting to see the orthopedic surgeon, often he was the only person under 60 in the waiting room, and it made him feel like a freak, it was very difficult.
“The best thing for Hugh would have been the survivorship clinic. That’s the biggest thing I feel that he’s really missed out on,” Lee said. While no two cancer journeys are the same, the struggle to transition to adult care is a common theme.
“It is an area that is seriously underfunded and under-resourced,” said Sherrie, another consumer who shared her story.
Sherrie’s daughter Teneille was diagnosed with leukemia when she was a year old. Her treatment was gruelling, and Sherrie’s family quickly learned that life rarely returns to ‘normal’ after childhood cancer.
“The end of treatment came when Teneille was nearly four. We thought it would all be over, and life could be normal, but we know now that’s rarely the case with childhood cancer,” she said.
New normal
“For the first five years following the cancer treatment, there are still a lot of hospital visits, blood tests and various other tests to monitor for relapses and side effects. It’s a stressful way to live, waiting for the results each time and wondering if you’re going to be delivered bad news again.”
Currently, the Oncology Survivorship Service at Perth Children’s Hospital runs from three to five years after therapy, until the transition to the adult sector.
“Unfortunately, once children age out of the survivorship clinic at the children’s hospital, there is no childhood cancer survivorship clinic in the adult hospitals. It is a huge oversight and a massive concern to families,” she said.
Reflecting on the unique, ongoing health needs of adult survivors of childhood cancer, Sherrie said her daughter, like many, needed specific monitoring as she aged.

“The onus has been placed on the survivors themselves to be informed and educate their doctors, which is fraught with problems. This is an area of great concern and big changes need to be made to ensure survivors are given the adequate care they need (and deserve) in a purpose-built childhood cancer survivorship clinic,” Sherrie said.
“We really need to do so much better.”
Teneille is now 16 and facing many long-term late effects of cancer and its treatment. Chronic pain, chronic fatigue, neurocognitive issues and mental health issues all have had a significant impact on her life, from school to work, sport, and social wellbeing.
continued on Page 25
Dr Andrew Tan
Dr Jeff Thavaseelan

Dr Trent Barrett
Dr Matt Brown
Dr Akhil Hamid
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
continued from Page 23
She regularly meets with a team of specialists in the fields of complex pain, psychology, gynaecology, ophthalmology, podiatry, physiotherapy, cardiology, and adolescent medicine, attending hospital often as an outpatient. These frequent appointments, tests and follow-ups have highlighted the need for a cohesive service with a multidisciplinary team dedicated to helping childhood cancer survivors thrive.
“Childhood cancer treatment is not the same as adult cancer treatment,” Sherrie said.
Childhood cancers are often treated more aggressively than adults, and treatment is administered while brains and bodies are still developing, making survivors more susceptible to
long-term side effects months or years later.”
“It's easy to assume that life goes back to normal once treatment is over, but it rarely ever does.”
Lee shared a similar outlook about the need for coordinated care for childhood cancer survivors, sharing how much she had to push to ensure all areas of Hugh’s health were monitored.
Their experiences highlight the need for holistic care from the beginning of the cancer journey, not just for the child but also their family.
“Cancer treatment is traumatic for children and support early on might possibly minimise the impact it has on the survivor in the future,” Sherrie said.
The need for increased support
A project using fun, dialoguefree animations created by and made inclusive for people with neurodiversity and disabilities has won an $18,000 National Science Week grant to help people with autism engage with science, technology and art.
MicroToons is a collaboration between Edith Cowan University academic Dr Rina Fu (or ‘Dr Rina’, as she’s known by many), animation studio Red Bird Creative and disability services provider 4lifeskills, and uses dialogue-free animated short stories to explain various aspects of biology, featuring characters such as blood cells and microbes.
Autistic and neurodiverse artists are involved throughout the creative process, from storyboarding, to the evolution of characters from pencil sketches to computer graphics and moving animations.
Dr Fu, from ECU’s School of Medical and Health Sciences, has a brother with autism, who has inspired her work.
“People with autism can struggle
to engage with science, technology and art, but when they manage to, it can empower them,” Dr Fu said.
“For a lot of neurodiverse people, the stimulus which makes something enjoyable for the wider population can actually be stressful, overstimulating and a trigger point for anxiety and behavioural changes.
“So, for MicroToons, we were careful with our colour scheme, so it’s not fluoro, bright yellow on the screen, which research has shown can prove challenging for people with autism. There’s also no dialogue so it there is no language barrier and therefore easily translatable to other languages.
“Using cinematic sound effects and simple labels makes the complexity easily understandable for a wide audience. So, whatever your background, you’ll take something away from the MicroToons story.

“As a sister and carer of a brother with nonverbal autism, growing up he’s never done science in his schools because it’s understandably never a priority – the focus is usually on social skills and self-care skills.”
for childhood cancer survivorship in WA has been recognised for many years. A clinician and consumer effort in 2013-14 resulted in a proposed model of care but attempts to find support to implement it foundered.
“The WA Cancer Plan 20202025 identifies establishment of a statewide survivorship clinic for adult survivors of childhood cancer and development of a cancer transition health pathway that links general practitioners to the adult service as priorities,” Dr Walwyn said.
“These now need to be implemented more than ever as the adult survivors of childhood cancer therapy at PMH and now PCH fall through the gaps.”
ED: Rachel Seeley is part of the engagement team at Health Consumers’ Council of WA
Dr Fu regularly visits schools which has emphasised to her the impact inclusive messaging can have.
“As an invited speaker for TechTrails, I shared about my journey from a girl to a scientist and showcased MicroToons in a mainstream school,” she said. “I mentioned how the drawings were done by a girl with autism and a girl in Year 9, she came up and said, ‘I have autism and I’ve never thought that I could do STEM’.
“So, the dream is to create a MicroToons TV series because the experiences I’ve had when showing it to people proves it can be really meaningful and empower young students to be artists and scientists.”
Adjunct Professor Janice Bell brings a deep and wide knowledge base to her work as a GP and as CEO of WAGPET.
 By Ara Jansen
By Ara Jansen
While she may be a general practitioner, Adjunct Professor Janice Bell considers herself a generalist in life.
Janice has been the CEO of Western Australian General Practice Education and Training, best known as WAGPET for almost 20 years. WAGPET is now winding up, as GP training will now be delivered by the Australia College of Rural and Remote Medicine (ACRRM), the Royal Australian College of General Practitioners (RACGP), the WA Primary Health Network (WAPHA), a to-be-formed First Nations GP Training Committee (FNGPTC) and Services Australia.
Born and raised in Perth, Janice is also deeply connected with New York. Her husband, Kim Lyons, worked in the Big Apple as a young lawyer. When the pair visited in 2006, they fell in love with the city and bought property there, which also allowed them to further explore the northern hemisphere without the constant long-haul flights.
On leaving school, Janice declared she wanted to do medicine. Perhaps this was influenced by having survived peritonitis at 13 from a missed appendicitis, one of the many that didn’t behave according to the textbooks. She was lucky enough that the general surgeon who operated, not knowing what he would find, saved her life, although it was touch and go for several days and took months to fully recover.
The idea of another health professional in the family didn’t impress her mother, who, herself, had been involved. She forbade that path. Instead, Janice got a scholarship to go to university to do arts and education, with a view to becoming a secondary school teacher.
Janice then worked with various helping professions, including community development, mental health, community services (community welfare, child protection and juvenile justice), public health and second chance education. She also set up her own management consultancy, which focused on organisational development and performance management.
Despite a non-religious upbringing, Janice spent three years studying theology as a trainee minister. Realising she loved theology –learning about how people have understood or found meaning in their lives over millennia – but wasn’t cut out for religious life, Janice was at a career crossroads. A midlife crisis. A counsellor she saw asked her – almost out of the blue – how long had she wanted to be a doctor?
Having avoided or confused the call to study medicine up until then, Janice gave up her secure, wellregarded public service career and went to study medicine at UWA. She was nearly the eldest in her year and received few exemptions for her previous work or degrees.

In the end, she chose to be a GP because while she enjoyed all her rotations in hospital, she recognised
she didn’t want to work in such an anonymous, fractured system.
“Mostly I wanted to prevent patients from ending up in hospital when so often that could have been avoided,” she says. “I became a GP in the days when even in the city we did minor surgery, had inpatients in the local hospital and did all our own home and residential care visits. Sometimes, a non-GP specialist would come to my practice and we would see the patient together, decide a plan together. The tertiary hospital emergency department would ring day or night if they were treating a patient of mine and a diagnosis or management decision needed my input.
“I fear that time was eroded by workforce shortages in general practice, the opportunistic growth in scope of many non-GP specialists into GP work and the at-first informal and then formal credentialing that diminished the involvement of primary health care in the joined-up patient journey.”
While a GP she was approached to work with the RACGP training program, then to become a national manager of GPEA, the innovative subsidiary arm of the RACGP, with responsibility for AMC preparation courses, special projects such as the Medicare Plus option for nonGP specialist to work in general practice under supervision and vocational training for WA and SA.
In 2003, she was asked to nominate for the WAGPET board, became vice-chair and was then appointed CEO in 2004. That was 19 years ago and, for most of that time, Janice has continued to practise as a GP.

“What I thought would be a shortterm role at WAGPET turned out
continued on Page 29

continued from Page 27
to be an amazing opportunity and probably the most personally and professionally confronting task I have ever undertaken. I am eternally grateful for that. I can honestly say nothing, and no one, scares me nowadays!
“There was nothing to hate about my job. Ever. Everything frustrating or exasperating was an opportunity to learn and adapt and try something new. It was never boring, and I never felt I mastered it. There was always more.”
In 2011, Janice was awarded the RACGP Rose Hunt medal for services to general practice. She was appointed the inaugural Chair of the Curtin Medical School External Advisory Board in 2016 and an adjunct professor. In 2022 she was awarded an Honorary Doctorate in Medicine for services to medical education, health workforce and general practice.
Janice applies what she has learned from her patients to every aspect of her life and work – to listen and to listen deeply and fully, always 100% in the moment. The human capacity to heal and to harm astonishes her, even a quarter century later.

“There is so much we do not know for all that we do know about health and disease, wellbeing and illness.”
While she admits it may sound quaint, Janice is convinced medicine for most is a calling.
“I don’t think we understand this well enough or explore it fully enough when we select medical students these days. Some tremendous would-be doctors are lost this way, while others who find their way to my door have been quite bewildered to have ended up somewhere they never intended, for better or worse.”
If medicine is not a calling, she says, but merely a respectable, wellpaying job, it can be brutal on the ego and sense of well-being.
“We can argue it is the system, which it is to a degree, or the very nature of the task at hand, which it is unquestionably. Especially general practice can be lonely
when you’re dealing with the front end of an obscure serious illness or nothing but a passing shadow – time with watchful waiting sometimes being the only difference influencing the outcome.
“We can wait for the system or the wisdom of medicine to change – and it is changing all the time –but if you are going to be a good doctor, you will be rubbing up against life in this way, every day. It is a tremendous gift, no doubt, but not always a comfortable ride.”
When she’s not being fascinated by work, Janice is interested in many things. She has studied Chinese and integrative medicine – two other languages with which to understand the patient experience. An early riser, a couple of hours a day are spent on the Chinese martials arts of qi gong and pa tuan chin. She likes reading, thinking, creating, exploring and simply enjoying life.
“Trying to be in balance with everything and going with the flow is what I aspire to – and being more Taoist, a never-ending intention into action for me. Medicine has been great in keeping it real and staying in touch with what’s happening on the ground. Medicine keeps me humble. Being a GP has never allowed me to think I have arrived – and that’s a gift of medicine –because there is much I don’t know and the more I don’t know, the more the search goes on.”
Janice quotes cyberpunk author William Gibson when she says “the future is here now, but it is distributed unevenly” in answering
what motivates her to remain a doctor. Her drive has been and continues to be for safe, quality, accessible and affordable health care for those who need it most.
“It is not only being better clinicians but about being better humans that will make this provision more equitable. There are so many practical and addressable ways I know to resolve this inequity in primary health care. I have worked tirelessly on many fronts towards this more evenly distributed future, even before I became a doctor.
“I admire those around me who are equal to this task and are making a difference on the ground, even as ignorant forces too often dismantle their efforts, sometimes unintentionally. As WAGPET CEO my contribution was through supporting and training doctors to work where they are needed most. We sought to train and support not just any doctors, but compassionate, kind, culturally safe and clinically competent doctors.
“Some of my best days were signing completion of training forms for an ever-increasing number of new fellows each year and watching the majority work in that place that embraced them, both their community and WAGPET. Seeing so many come back to be teachers, supervisors, assessors, educators, and staff is truly gratifying and fulfilling.
“WAGPET may be winding down, but the spirit of collegiality and community-centric medicine lives on. And wherever I can help breathe even more life into that spirit, that’s where I am headed next.”

Research is ringing an alarm bell and showing that carers live with significantly higher levels of psychological distress and lower levels of wellbeing than the average Australian. Not only that, but recent research indicates that 57% of WA carers receiving government payments are living below the poverty line and are often drawing on their own savings to help support their loved ones and keep the family unit together. So, let’s talk about carers. After all, almost everyone one of us, at some point, has been or will be a carer.
A carer is someone who provides unpaid care and support to family members and friends who are living with disability, mental ill health, a long-term health condition (including a chronic condition or terminal illness), an alcohol or other drug dependency, or who is frail aged.
There are over 2.65 million carers across Australia (nearly 11% of the population), and over 320,000 in WA. In 2020, the estimated hourly cost of formal care in place of unpaid care was $36.12 per hour. When the work carers undertake is extrapolated, this equates to a total replacement cost of $77.9 billion nationally.
To put that into perspective, according to the Australian Institute of Health and Welfare, there are only 642,000 registered health professionals in Australia. That’s four unpaid carers to every one paid health professional.
Due to the impact and tasks undertaken, those in an unpaid caring role will often be unable to be engage in paid employment. This reduces their earning capacity in the short-to-medium term but also impacts their long-term financial security and ability to accrue superannuation.
On average, carers forego more than $390,000 in lost wages to age 67 and a further $175,000 in superannuation. This, in combination with other systemic faults in social housing, health and community supports and carer concession processes, result in a recipe ripe for homelessness and lower socio-economic outcomes.
Despite the substantial impact of the caring role, state, territory and federal legislation is insufficient in attempting to achieve its intent of building awareness and recognition and carer recognition Acts around Australia are not enforceable.
Recognition is the key element underlining the broad and significant challenges that people in an unpaid caring role face, whether this be recognition of self as a carer, or recognition by outside parties of their role as a carer. This could be by family, friends, community, hospitals, GPs or by the services carers navigate themselves for, and on behalf of, the person for whom they care.
In June 2023, the Australian House of Representatives’ Standing Committee on Social Policy and Legal Affairs instigated an inquiry into the recognition of unpaid carers. Overall, the inquiry will examine the provisions and operation of the federal Carers Recognition Act 2010 (the Act) and consider what the role of a reformed Act
Carers WA, as the peak body representing and advocating for the needs and interests of unpaid carers in Western Australia received an invitation from the committee to provide a submission to the inquiry and will be doing so within the confines of the Terms of Reference. Unfortunately, the inquiry does not include the ‘adequacy’ of carers’ payments.
While Carers WA welcomes the inquiry into the recognition of unpaid carers, the exclusion of carer payments from its scope, eliminates consideration of an element of the full picture of carer recognition, and does not go towards securing a positive economic future for carers.
However, the scope of the inquiry does include the effectiveness of carer legislation in recognising and raising awareness of the role of unpaid carers, at a state, territory and federal level. It will also look at options for better identification of unpaid carers in Australia.
Cementing the necessity for such an inquiry as this, is the need for the term ‘carer’ to be clearly defined in every medium in which they are referred to, whether this be an article, policy submission or other means.
We are all part of the change and identifying and recognising carers is the first step to reform. We should all be appalled that 57% of WA carers live below the poverty line and are being expected to contribute financially to the wellbeing of others; all without thanks, recognition or hope of a secure financial future.
Carers WA invites you to work with us to achieve an improved quality of life for family carers in our state.
– References on request
ED: Richard Newman is CEO of Carers WA. www.carerswa.asn.au

may be.
While those living with life-limiting and chronic illnesses face great challenges, so, too, do the family and friends who care for them, and they are often overlooked, writes Richard Newman

The death of a baby, while in utero, is devastating for parents. A late stillbirth (28 weeks or more) can have a profound and long-lasting effect. For many parents, the baby has been named, nursery painted, car seat installed, and grandparents are excited.

In 2016, Australia’s late gestation stillbirth rate was estimated to be 35% higher than countries with the lowest rates. In 2015-16, almost 20% of all stillbirths and 5% of term stillbirths were classified as unexplained. Currently, six stillbirths occur each day in Australia.
These numbers are devastating, as is the pain for parents – yet some of these stillbirths can potentially be prevented.
Following a Senate enquiry in 2018, stillbirth was recognised as a public health issue in Australia. This led to the Federal Government establishing the National Stillbirth Action and Implementation Plan in 2020 with 16 action plans, including stillbirth prevention, education, holistic bereavement care and stillbirth research.
Furthermore, thorough stillbirth investigation offers an opportunity to detect previously undiagnosed maternal disorders, plan future pregnancy pathways, and aid the grieving process.
Stillbirth investigation is best thought of as a comprehensive care package. Having a post-mortem report available is of little use if the parents don’t have the opportunity for the findings to be explained.
Knowledge about a newly diagnosed genetic disorder or recurrent placenta abnormality – with potential implications for future pregnancies – without an appropriate referral pathway in place, is potentially negligent. Leaving a parent to process the trauma of the loss of a loved one in an age of increased understanding of mental health seems unkind, when access to pastoral care and counselling is readily available.
Care of a patient, in the context of a stillbirth, aims to address all the above.
This care is best provided through a perinatal loss service – the components of which include a coordinator, clinicians trained in stillbirth investigation, a postmortem service, bereavement care, and clinical follow-up.
The Paediatric and Perinatal Department at PathWest, Perth Children’s Hospital (PCH), is integral to the service, with a particular focus on post-mortem examination, bereavement care and close liaison with clinicians.
There are five perinatal pathologists who also provide
Grieving the loss of a child is a process, it begins the day your child passes and ends the day the parent joins them.
– BJ Karrer
a diagnostic paediatric service. The post-mortem team consists of five perinatal pathologists, an experienced post-mortem coordinator, and mortuary assistants.
Over many years, the team has developed a dedicated, integrated and comprehensive service. The team can assist with everything from transport of a baby to advice on funeral arrangements. The service is offered state-wide with no cost to the parents.
From a practical aspect, there are three types of post-mortem examination which may involve cutting of the body, but not always. The range of examination offered include full, limited and external. Once a body is received at the King Edward Memorial Hospital (KEMH) mortuary, the actual postmortem takes place at PCH where pathologists are located.
The baby is prepared for postmortem examination by a mortuary technician. This includes a standardised set of clinical photos and measurements. Social photos may also be taken together with hand and footprints, as per consent. A babygram (a form of x-ray) is performed on every baby, mainly to assess the skeletal structure and development. The body is then transported to PCH for the examination, always accompanied by a mortuary technician, and handled with great care and respect.
1. Full post-mortem: the external aspect of the baby is carefully examined. A skin excision is then made from the sternal notch
down to the lower abdomen. The chest plate is removed. All organs are examined, weighed and sampled. Clinical photographs are taken as required. Tissue is further sampled for ancillary studies (microbiology, virology, genetics) as required. It is usual practice to snap-freeze a peasized piece of tissue (usually muscle) for later genetic analysis if needed. The sampled organ tissue is processed into paraffin wax blocks, from which histological slides are prepared for microscopic investigation. The placenta is always examined as routine, regardless of postmortem type, and examination includes sampling of tissue for histological examination and ancillary tests (as required).
2. Limited post-mortem: the body is prepared as described above. The extent of examination is limited to the parent’s wishes. For example, only the brain or heart are examined, depending on the clinical scenario. A limited post-mortem may be appropriate when tissue needs to be taken for genetic investigation. In such a case, a small one-centimetre incision is made in the thigh and muscle sampled. The placenta is always examined.
3. External examination: the body is again prepared as described above. The external aspect is carefully examined, but no incisions are made. The placenta is examined as per routine. A small portion of umbilical cord or placenta parenchyma is snap-frozen for future testing if required.
Following post-mortem examination, all organs are returned
to the body, which is carefully reconstructed. Once dressed, there is little evidence of incision and the baby can be viewed by parents, if desired.
The post-mortem report takes six to eight weeks to complete, depending on complexity, and is sent directly to the requesting clinician (not the parents). The integrated report lists all the important findings, and a comment is provided as to the likely cause of death (where possible).
A plain language report, which describes the salient findings in an easy-to-understand manner, can also be requested. This is sent to the requesting clinician who can pass it on to the parents. Ideally, the parents are briefed on the findings. In the setting of KEMH, parents can attend a perinatal loss clinic six to eight weeks after the death of their baby. This allows an opportunity for the findings of the post-mortem report to be explained and further follow-up or referral arranged.
Parents requiring bereavement support are guided along appropriate care pathways.
Finally, all deaths are reviewed at a mortality review meeting. The postmortem report provides important information for death clarification and inform health statistics.
These steps form part of the care pathway for parents at a very difficult time. Understanding the cause of death can help bring closure, remove blame, and help with future pregnancy planning. Although a young life can’t be replaced, compassionate care can be a much-needed support.
A WA led team developing a new neuroprotective therapy and diagnostic to reduce disability in babies suffering brain injury has been awarded significant funding from the Stan Perron Charitable Foundation as well as UWA and local biotech company, Argenica Therapeutics bringing the total value of the program to $5.6 million.
“Neonatal encephalopathy is characterised by abnormal brain function affecting preterm and term infants,” said program leader Dr Adam Edwards. “Resulting most commonly from lack of oxygen during pregnancy or birth, this ‘umbrella’ syndrome can cause severe and permanent disabilities such as cerebral palsy and epilepsy.
“Despite significant improvements in neonatal critical care, there are no drug therapies to protect babies from this type of brain injury.”
The funding will help advance the preclinical development of a neuroprotective drug as a therapeutic, as well as a magnetic resonance imaging diagnostic for preterm and term neonatal encephalopathy.
The neuroprotective drug, ARG-007, which has demonstrated safety after a Phase I clinical trial in healthy humans, has also demonstrated the ability to significantly reduce brain cell death in preclinical models of preterm and term infant brain injury.
Perth Radiological Clinic offers PET/CT, nuclear medicine, MRI, CT and interventional radiology expertise for oncology patients.


Our expert oncology team are involved in private and public multidisciplinary meetings across all facets of oncology imaging.
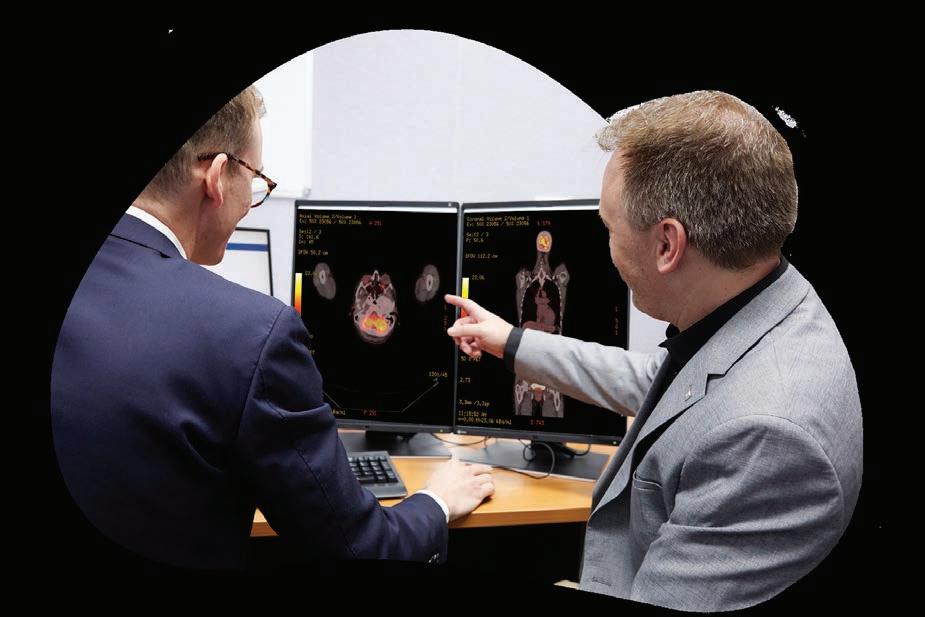
PET/CT now available at three convenient locations, with a new clinic opening soon at Murdoch Square.
Please contact our customer relations team for more information or email assist@perthradclinic.com.au

Most clinicians will relate to the emotional and professional responsibility that comes with caring for people – medicine is a science but one that is deeply rooted in our humanness.
For those who work exclusively in paediatrics, there are the added dimensions of innocence and vulnerability that comes with children and young people.
In the end, the pressures that all clinicians feel come from a place of wanting the best for the people in their care by offering hope and treatment.
The motivation behind the recently finalised Paediatric Palliative Care National Action Plan springs from these values.
Despite community preconceptions, hope and treatment are equally important to the practice of palliative care, especially in the context of paediatrics.
The idea of there being a paediatric specialty within palliative care challenges the picture many have in their mind, a picture where end of life has an elderly face.
Our society isn’t comfortable with the idea of children and young people dying – that will never change, but what does need to change is the understanding of and access to palliative care for them.
Recent data shows there are currently about 30,000 children and young people aged between 0 and 21 years, living with a lifelimiting illness in Australia who would benefit from palliative care. When you add family and friends to the picture, the ripple effect of paediatric palliative care extends to many more thousands of people.
Palliative Care Australia adopts the World Health Organization definition of palliative care for children and their families:
• Palliative care for children is the active total care of the child’s body, mind and spirit and also involves giving support to the family.
• It begins when illness is
diagnosed and continues regardless of whether or not a child receives treatment directed at the disease.
• Health providers must evaluate and alleviate a child’s physical, psychological and social distress.
• Effective palliative care requires a broad multidisciplinary approach that includes the family and makes use of available community resources. It can be successfully implemented even if resources are limited.
• It can be provided in tertiary care facilities, in community health centres and even in children’s homes.
The action plan wraps itself around all aspects of this definition.
The physiological and psychological developments that are naturally a part of childhood and adolescence hugely influence the delivery of palliative care.

This expands the breadth of expertise required in the care team and is what the action plan informs.
Developed over three years as a partnership between Palliative Care Australia and Paediatric Palliative Care Australia and New Zealand, the action plan draws on extensive consumer co-design.
The families who took part did so as part of their children’s legacy, “so that our child’s death meant
something.” In sharing their experiences, these families and carers see the need for us to do better and be better.
This groundbreaking document is a roadmap that guides the way children and young people with lifelimiting conditions and their loved ones are supported.
Throughout a child or young person’s illness, their care needs will vary. They will potently dip in and out of palliative care and in equal measures engage with curative treatments.
The action plan strongly makes the case for a collaborative approach to that care, a practice that connects doctors, nurses, allied health, volunteers and specialist palliative care services.
The action plan has 18 recommendations including measures that deal with quality, access, information sharing, collaboration, data and research. Investment from governments and the sector is needed. However, much of what is outlined can be achieved by health professionals as part of their own clinical development.
Indeed, the bigger paediatric palliative care project that the action plan is a part of, has developed a range of tools to support care in acute, hospice and community settings – wherever the child, young person, and their loved ones choose.
The next phase of the project builds on enhancing paediatric palliative care for all who need it, wherever they are.
The action plan can be downloaded from https://paediatricpalliativecare.org.au/ resource/the-paediatric-palliative-carenational-action-plan/ It was developed with funding from the Australian Government.
National changes to the way opioid replacement treatments are dispensed may only be minor for WA, but it has gone some way to break the stigma.
Eric Martin reportsAustralia now ranks third, behind the US and Canada, for the highest rate of lethal opioid overdoses, a figure that has climbed steadily by 3.5% each year over the past two decades, reaching 5.38 deaths for every 100,000 in 2019.
According to the Illicit Drug Reporting System (IDRS), half the nation’s 2020 opioid-related deaths involved heroin, followed by natural and semisynthetic opioids such as codeine or morphine at 32%, with more than three quarters of these overdoses occurring at home.
For many years, the taboo nature of the topic, not to mention the public outcry at the suggestion of locating treatment services locally, meant that commitments to upgrade the funding model for opioid dependency treatment (ODT) medicines have been neglected.
However, from 1 July this year, changes to how ODT medicines were listed under the Community Access Program meant that patients for the first time have gained a PBS co-payment for up to 28 days’ supply, with the amount paid contributing towards their Safety Net threshold.

Dr John Edwards has been one of the State’s leading frontline experts in treating addiction, particularly opioid dependency. Medical Forum discussed with him the pros and cons of the changes, especially given the unique situation in WA, which already dispenses ODTs from pharmacy depots.
“This is the biggest thing that's happened in the past 30 years for opiate replacement treatment, and it's got a lot of positive implications and it's got some negative ones. But I think across the board, it's a positive thing, going against the stigma and normalising the way that opiate addiction is handled,” he said.
“This is turning buprenorphine, the Subutex, Suboxone and methadone into a normal medication that is on the PBS and is managed just like everything else.
“There's been efforts from those working in opiate maintenance programs to try to change the process because it has been very unfair that it is the only medical condition where the end user bares the cost of the of the treatment daily.
“The political drive has been very strong for this to go ahead, and it is needed to be. Whoever is behind it is very courageous and I want to thank them.”
Dr Edwards said that generally, most of his patients were on health care cards, but for some who were on methadone, which was common, their outgoing expenses could be as much as $500 a month.
“It was the dispensing which attracted charge and the pharmacy was charging it every day, and while it's been seen as an unfair condition for years, no one's been willing to change it,” Dr Edwards said.
All the research that has been done in the past 30 years on methadone programs has shown that the main reason that people drop out is the cost, both financially and in terms of the effort required to maintain that dose every day.
“This treatment is recognised as one that saves the community money,” Dr Edwards said. “It has
been researched over and over, at multiple sites and in multiple projects, that show a dollar spent on this type of program saves the community between $7 and $10 in terms of general costs.
“This schedule has been shown to be the gold standard, the best management for a person with opiate dependence, particularly long-term opiate dependence where detox doesn't work, and they have a history of dangerous, longterm use.”
Patients can continue to be prescribed their ODT medicines from their current medical or nurse practitioner and access ODTs from their current dosing site, but in an equally momentous change, from July 1, additional private dispensing or dosing fees can no longer be charged by community or hospital pharmacies.
The PBS issued a statement that patients would not have to pay “additional out-of-pocket costs for activities associated with the preparation of in-pharmacy or take-away doses of methadone liquid, buprenorphine sublingual tablet and buprenorphine and naloxone sublingual films.”
It said a community pharmacy program for ODT medicines would be established, including on-site pharmacist administration of injectable buprenorphine, and that it would introduce a nationally consistent payment for ODT services provided by community pharmacists.
Historically, the dispensing charge was the financial basis for the treatment clinic model popular across the Eastern States, as well as a financial incentive for WA pharmacies to participate in the program.
“There were big differences between States how things were done with the biggest contrast being between NSW and WA,” Dr Edwards explained.
“In WA, virtually everybody who is on a program was dosed in a community pharmacy, but in NSW there are a lot of public and private clinics where a person would see their doctor, but it is also where

they got their dose, provided free by the NSW government.
“There will be major upheavals in NSW. I think they have got valid concerns about how they will manage in the long term, and the changes have caused an outcry because public clinics relied on those dispensing fees to stay viable.
“If they shut down, it would recreate so many issues that we thought were already dealt with – it would be a disaster to do that with nothing in place and they may have to change their model to something more like WA.
“The issue would be that because it hasn't run that way in NSW, community pharmacies won’t have the expertise, the network, or the ability to provide this service straight away, let alone having the will to do it.”
Dr Edwards said that under the old system, WA pharmacies were provided with methadone or buprenorphine, Subutex and Suboxone, and the GP would write a non-S-100 script that allowed for a certain length of treatment.
“You might write that script for one month, two months, three months, or even two days, and the script would have state authorisation. The pharmacy would receive the methadone or buprenorphine at zero cost under the S-100, and they would dispense it and charge the person their $5 to $7,” he said.
“The methadone was distributed in a liquid, diluted in water and the patients drank it in the pharmacy, supervised by the pharmacist. There were some provisions for takeaway doses, while the buprenorphine was either a tablet or a strip, both of which were dissolved in the mouth – there was no injecting.”
The new depot preparations, which are monthly injections, will be administered by the pharmacist or an approved person in the same way that Australians can get a COVID or flu vaccination.
“A person on a health care card will pay the $7 for a standard prescription, but somebody who's not, will have a single payment of $30 once every 28 days,” Dr Edwards said.
continued on Page 39
You are what you eat. And healthier cooking leads to a healthier lifestyle. Saladmaster cookware sets are a new way to cook that will transform the way you feel.

Faster Cooking: Our Vapo-Valve™ technology and semi-vacuum cooking method makes cooking more efficient, precise and quick. When the temperature exceeds the optimal cooking temperature, the built-in Vapo-Valve clicks, letting you know it’s time to reduce the heat to avoid overcooking.
Fat-free cooking: Cooking with Saladmaster enables you to skip adding oil, butter or excess fat. The Vapo-Valve creates a semi-vacuum that maintains your food’s natural flavour by locking in moisture. Our oil-free cookware consistently delivers healthy and delicious meals for every occasion.
Better Nutrition: By locking in the food’s moisture, you don’t need to add water when cooking, which preserves vitamins and nutrients in your food while also protecting the natural flavour of ingredients.

continued from Page 37
“Much of the process will happen the same way and the level of state authorisation will not change – the only difference is it moves from S-100 to the standard PBS and people will now also be eligible for safety net payments.
“I think it is going to be a bit harder because the scripts will have to be written with exact quantities, stating just how many tablets or how much liquid is to be given within the 28 days, but in the past, we have often written scripts that allowed some variability.

“The other potential issue is that patients will only be allowed to collect their medication from the depots once every four weeks on the PBS system, yet some of them don't last four weeks and they're expensive – more than $300 each round. Potentially, there's going to be associated holding costs for pharmacies if they're looking after their customers.
“However, we have used the depots for about three or four years now in WA, or at least my practice has, and it's turned out to be a real game changer in terms of the quality of treatment that people receive, their safety, and the freedom that they have – such as a much better ability to travel to work.”
Dr Edwards believed that there was a great deal of public misconception about the opiate replacement treatment program.
“Although some patients are chaotic people who are struggling and might match the ‘stereotype,’ most are not, and you wouldn't pick them in a crowd,” he said.
“People on methadone or other opiate replacement therapies are often working, raising families. They might be teachers or police officers and you would never know because they have moved on from their illicit use and got their life together.
“And that is the whole point of it. That is why it is so useful – they can move on with their life without having to cope without the opiate replacement.
“The most common reason that
people become dependent on opiates is because of trauma. Early life trauma impacts 80% or 90% of the people that I would see and, oftentimes, it has such an affect that they cannot manage without the opiate.”
Dr Edwards believed that GPs have a crucial role to play in helping to combat Australia’s opioid dependence.
“In the same way that a GP might have a handful of people on a depot antipsychotic, where they would see the pharmacist once a month for an injection – managing someone on a depot-based opiate is no harder than that,” he said.
“There is a bit of training and red tape, but it's not that difficult to manage those steps and depots have proven themselves – they've been around long enough that we understand how to use them and how easy they make it for a GP to manage a patient needing opiate replacement.
“GPs do much more difficult things and, personally, I have found that it has been one of the most gratifying things I have done in medicine. The people that we deal with really do get better, you can see those changes over time, and they are a group who are incredibly grateful just to get care. They have often been chased off from other providers’ places.”
“My practice looks after about 800 people on this program, which represents a quarter of the total
number of participants. Although I am a specialist in the area, we just cannot take more people, even though we would if we could, and there is a huge demand that is currently unmet.”
However, Dr Edwards also believed that having an awareness that dependence could be a problem with opioids, it was just as important not to be afraid of prescribing them.
“One of the worst things to happen is that a lot of GPs won't prescribe opiates at all anymore – they’re scared off it, no matter the level of need,” he said.
“We now know that long-term chronic pain, like mechanical pain, is not well served by prescribing opiates but, sometimes, for a person who is dealing with overwhelming or unbearable emotional distress, opiates are the only thing that keeps them going.
“Giving an opiate replacement provides a safer situation where they can get their life in order and not have to live in the illicit world, not have to spend all their money, and not have to take risks.
“They no longer need to associate with drug dealers and can normalise their lives, starting to better manage their trauma once they have developed that resilience and improved their emotional strength. Then they are in a position where they can deal with the physical addiction – and sometimes that takes years.”
One of Charlotte Diaz’s earliest memories were special outings to meet a woman named Sue, based in the Raine Study’s then centre in Subiaco. There, Charlotte would be involved in fun activities, an experience the now 32-year-old professional and mother says were something she looked forward to.
“Sue made it fun, and I felt excited to be a part of it,” says Charlotte, who now works as a community relations practitioner for a mining company.
“My parents are very altruistic by nature and because of that, they provided me with what it was to be a part of something bigger. By playing a small role, I was contributing something about me that could unlock some major breakthrough in research.”
Charlotte, for example, had asthma as a child, and realised that if being a Raine Study volunteer could result in a better way of managing the condition, then “it was a privilege”.
From a very early age, Charlotte – like many others in Western Australiawas a research subject in a this truly unique multi-generational study, one that has tracked almost 3000 young adults over 33 years since they were 18 weeks in-utero.
“I remember the physical tests, like seeing how many sit-ups we could do in a minute, but I mostly remember going to the Lion’s Eye Institute, which was fascinating, as that was like an optometrist on steroids. It was a great way to learn about my own health while knowing it’s being used in research data.”
For 33 years, 2900 Perth women and the 2868 children they gave birth to between 1989 and 1992 have taken part in different research studies tracking their physical and mental health.

As the WA Raine Study – the world’s longest-running prebirth cohort study – launches its biggest follow-up, Suzanne Harrison explores both sides of the equation.
Starting with a study of the impact of ultrasound during pregnancy when it first started, the Raine Study has collected millions of bits of biological, lifestyle, and environmental information from these babies and their parents at multiple checkpoints through infancy, childhood, adolescence and adulthood.
Those parents (Generation one) and their babies (Generation two) have since taken part in 17 different followup studies, contributing to groundbreaking research on physical health, mental health, lifestyle, and genetics. The babies are now 33 years old and are having their own children (Generation three).

The Raine Study was a world first when it came to investigating the origins of a child’s future health from before birth, and it continues to use this information to demonstrate the prebirth origins of disease and ill-health not only in childhood but through adolescence and into adulthood.
In collaboration with its participants, the Raine Study has collected extensive data on health, mental health, behaviour,
environment as well as social, educational and work outcomes.
It holds more than 30,000 phenotypic data points, 30 million genetic data points, and more than 170,000 biosamples (blood, saliva, faeces, cord blood, baby teeth) and has been able to link this (anonymised) data to WA government sources including school and hospital records.
Thanks to the Raine Study, researchers have established the direct link between a pregnant woman’s health choices and her child’s health outcomes, which have gone on to inform global health policy, from setting fetal growth standards to confirming that children conceived via IVF have the same long-term health outlook by adulthood as their naturally conceived counterparts.
Furthermore, the Raine Study recently announced that a grant from the Telethon Trust will enable it to start recruiting all current and future children born to the original Raine Study babies. That is, babies such as Charlotte’s now two-yearold, Chloe, who Charlotte says will definitely be involved in the research.
This will make it the first threegeneration pregnancy cohort study in the world, with the potential to improve understanding of the intergenerational determinants of health and wellbeing across three generations.
continued on Page 42

continued from Page 41
This latest study has been called the Generations Follow-Up and to be successful, it needs to complete assessments with as many of the original parents and their now 33-year-old offspring as it can over the next three years.
Associate Professor Rebecca Glauert , the University of Western Australia’s Scientific Director, says the Raine Study has been exceptional at maintaining contact with the families involved.

“Now, they are excited and enthusiastic to bring their children in. It’s something that they’re giving back to society, and their generosity of spirit to medical science is so significant,” she said. For participants, it’s also informative for their own health and wellbeing.
The study keeps their baby teeth, faecal collections, sperm, data on what they eat, how they sleep – to name a few. Participants can access all this information and meet other participants, attend symposiums and keep up with those involved, if they so wish.
Researchers from all Australia and the world can also access the study’s data.
Since 2014, research is undertaken at Raine Study house at UWA. For the original generation two children seen first at the age of two or three, right up to the late 20s, they were studied in Subiaco within the old Princess Margaret Hospital.
As Dr Glauert explains, there are other birth cohort studies in the world, but the Raine is the first and longest running pregnancy cohort study globally and its expansion will have exponential benefits.
“It’s not just the collection of new data. The addition of this third generation of participants will mean that existing data can be applied in new ways to enable intergenerational research that simply hasn’t been possible before now.”
Current health data shows that around 40% of children in Australia will develop a long-term health
condition. Researchers will now be able to trace the causes of these conditions across multiple generations and potentially intervene to reduce the likelihood of them developing.
“The first study (with Generation one) focused on ultra-sounds during pregnancy, and the findings of that had significant impact on the lives of babies. The IVF study was equally as interesting and there has been a lot of work done of phthalates from plastics. There are 700 publications that have come out since the original cohort was recorded,” she said.
Telethon Kids Institute’s Professor Graham Hall said he had been involved with the Raine Study for many years, leading lung function follow-up tests when the participants were 22 years of age. The measures taken then built upon previous lung function testing done at age five and 14.
“We’ve been really interested in looking at what factors are associated with kids whose asthma persists into adulthood,” Professor Hall said. “Because the Raine Study has collected so much information over the years, we can start to
tease out what those factors might be and look at why some kids will grow out of their childhood asthma, but also why others don’t.”
There are currently more than 150 researchers utilising the Raine Study. The investigators bring expertise from 25 broad areas of research including asthma and atopy, cardiovascular and metabolic heath, childhood developmental growth, dental health, diabetes, genetic epidemiology, gastroenterology, infection and immunity, mental health, musculoskeletal development, nutrition, physical activity, ophthalmology, pregnancy and birth, reproductive health, sleep and risk-taking behaviour. The study also focuses on socio-economic factors and is representative of the WA population as a whole.
For those new to the Raine Study, the question begs – how did they find the original cohort and why is it called the Raine Study?
Mary Bertha Raine was born in London in 1877, the eldest of 13 children. She arrived in Perth in 1904 aged 23 and, despite humble beginnings, she was a strong and astute woman who worked hard and soon invested and built multiple property assets, notably the Wentworth Hotel in what is now Raine Square.
Mary’s second husband and business partner, Arnold ‘Joe’ Yeldham, died in 1957, and the devastated Mary donated her financial legacy to UWA. The Joe and Mary Yeldham Foundation was born, initially to research the causes of arteriosclerosis, the cause of Joe’s death. Upon her death in 1960, Mary bequeathed nearly $1 million to the Raine Foundation (now the Raine Medical Research Foundation).
Nearly 30 years later, a young obstetrician named John Newnham had a chance meeting with the foundation’s accountant. The accountant told him they were looking for a grant to begin a largescale visionary project. The application was speedily submitted, and the award was made. The Raine Study team got
underway immediately. The women recruited were randomly assigned either routine obstetric ultrasound or multiple scans.
Extensive data was collected during pregnancy and the children were assessed at birth. All the women were volunteers who were approached at King Edward Memorial Hospital (KEMH), a story that Charlotte’s mother told her when she was so young, she has never not known about it.
Dr Glauert says the Generation one women were recruited between 1989 and 1992, but what makes it so special is now that “their babies are having babies”.
An additional group is Generation zero, the grandparents of Generation two.
Between 2019 and 2019, grandparents were invited into the Raine Study for the first time. The initial focus was on breast density following breast scans of generation two female participants and their mothers (Generation one).
Now, with the advent of Generation three, Dr Glauert is calling on anyone who was once part of the Raine Study to get back in contact, via the website, email, social media, or telephone.
She wants past participants to know that it’s never too late to reengage with the Raine Study. Never too late
“It doesn’t matter how long it’s been since you last saw us, or where you might be in Australia or around the world – you’ll always be part of the Raine Study. Your involvement in the Generations Follow-Up will make the Raine Study incrementally, exponentially better.”
For someone like Charlotte, it’s been a part of her life – and she is more than happy it has been.
“My colleagues and I were doing an ice breaker and we were asked to tell everyone something about us and mine was that I am part of the world’s longest pregnancy
cohort,” Charlotte says. Someone else said, ‘so am I’ and straight away we had this bond. You know what it involves and how that has contributed.”
The Raine Study is a joint venture between UWA, Curtin University, Telethon Kids Institute, Women and Infants Research Foundation, Edith Cowan University, Murdoch University and University of Notre Dame Australia. Flinders University in South Australia and Newcastle University in New South Wales are institutional partners. The study receives additional funding support from the Raine Medical Research Foundation and National Health and Medical Research Council.

Former Raine Study participants can update their contact information at:
https://rainestudy.org.au or email rainestudy@uwa.edu.au
Evidence-based research is integral to academia, driving innovation and improving understanding while informing global policy. One area lauded by some and discouraged by others is cross-disciplinary research, specifically between the social and medical sciences.
These domains are viewed as separate entities within the medical community. One may therefore wonder what good can come from blending them.
Nevertheless, cross-disciplinary research has been a cornerstone of certain scholarly communities for decades. For instance, East China Normal University recently celebrated its 70th anniversary and has been a leader in crossdisciplinary research mixing branches of the social and medical sciences, including basic and applied sciences, engineering, physics, and economics.
This merging of scientific fields has spawned research on green material manufacturing, gene-editing technologies, and mathematics students’ educational competency.
Facilities such as these that emphasise cross-disciplinary research show the immense potential such work holds for knowledge and discovery. However, barriers continue to limit its implementation.
A recent article in Perspectives on Medical Education examined crossdisciplinary knowledge flow within medical education research and higher education. The authors found that medical education researchers use a narrower range of knowledge communities than those in higher education: 80% of the former group’s citations come from health and medical education journals, whereas the latter group cites only 36% of work from within their own domain, the remainder come from across the social sciences.
These results suggest that experts in higher education converse with
other academics from a range of communities, increasing the number of perspectives they encounter, and the insight brought into their field.
The most significant benefit of cross-disciplinary research – and the reason why many worldwide research powerhouses stress it – is that it enables knowledge exchange while sparking innovative responses to complex health challenges. The common phrase “thinking outside the box” happens as academics step outside the bounds of their respective disciplines to pull information from other scientific realms.
Yet obstacles persist. One major difficulty is the lack of evidence to guide the design and implementation of such research, which hampers collective action. Advances have been made to lessen these limitations: a 2020 review showed that crossdisciplinary research is best fostered by leadership and teamwork at the research team and institutional levels. The review also indicated that personal qualities, such as receptiveness to new ideas and the funder’s power and influence, further affect scholars’ abilities to perform this type of work. Moreover, challenges arise in affording academic researchers the opportunity to choose topics and directions while meeting the needs of those overseeing and funding their efforts.
Knowledge is power. It makes research an asset and a potentially costly area, especially as research technologies expand. As in most situations involving money, there is usually substantial oversight concerning what has been completed to ensure that funding bodies’ needs are fulfilled and that the research is relevant to society and the economy. Yet these constraints can stunt academic freedom and even obstruct innovative discoveries.
Another barrier to academic
freedom is universities’ and faculty members’ desire for research staff to publish within their own areas to enhance departmental recognition. This laser focus can dramatically limit scholars’ chances to study cross-disciplinary topics. Researchers may be similarly prevented from assuming novel stances. As such, facilities may generate more output on a specific topic, but it is unlikely to be as groundbreaking as cross-disciplinary research can potentially be.
Cross-disciplinary research encourages creative solutions to age-old problems. However, urging professionals to stay within the confines of their discipline can restrict the answers available to them, reducing the probability of breakthroughs.
As Stefan Hell explained in 2019, when scholars are not granted the freedom to choose their research subjects, they go into their research with already limited potential to make important discoveries—and if their methodological options are few, then their chances decrease further.
Academics who perform crossdisciplinary research can enlarge the evidence base through multiple modalities, even for unusual pairings such as tourism and medicine.
Innovative papers integrating these seemingly distinct areas have offered valuable insight into the roles of tourism in individuals’ health and quality of life.
Academic freedom does call for a certain degree of management, namely in ensuring specific rules are followed. But there is immense promise in giving researchers the freedom to test new means of solving problems, especially by working with other disciplines.
ED: Dr Jun Wen is a lecturer in Tourism and Service Marketing at the School of Business and Law, Edith Cowan University.

Thinking outside the box to solve stubborn problems takes courage and imagination, says ECU’s Dr Jun Wen
 neuroscientist Dr Liz Dallimore
neuroscientist Dr Liz Dallimore

I recently attended the largest and most influential global event for the biotechnology industry in Boston, the Biotechnology Innovation Organisation International Conference 2023 (BIO), as part of an Australian delegation promoting Western Australia’s biotechnology benefits. Boston is one of the world’s leading biotech hubs, centred largely around Kendall Square in Cambridge, with more than 1000 biotech companies, representation from all the major pharmaceutical companies, and a continued funnel of research from teaching hospitals, Massachusetts Institute of Technology and Harvard.
In 2008, $1 billion was pumped into the sector to create a collaborative, centralised environment, promoting knowledge-sharing and innovation.
As it stands, Western Australia boasts world-class research institutions, universities and medical facilities renowned for their expertise, with some of the brightest minds in the world. However, in order to truly capitalise on this, WA must now take the next step to developing a centralised, collaborative hub – similar to that in Boston – to solidify our position as a global leader in research, development and commercialisation.
We have strong foundations in that WA has a thriving earlystage clinical trial ecosystem, with an exceptional reputation for delivering first in-human trial results, and we are also starting to develop deep capabilities in service areas through clinical research organisations.
Next steps should include building capabilities to service global areas where data is the output – that is, we don’t need to be physically located in the country of the customer. This idea came through
a visit to Ginko Bioworks in Boston, a US$3.7 billion biology service company – their only output is data, while harnessing automation to scale.
Western Australia has an enviable time zone in which to service countries throughout Asia, utilising our highly skilled expertise in both medical research and process automation.
However, to foster and sustainably grow the sector, work is also required to develop a more sophisticated venture capital landscape and educate West Australian investors to back these innovative companies to help diversify our economy.
Committed funding can be used to assist in bolstering research infrastructure, attracting and retaining leading researchers from around the globe, and supporting clinical trials to ensure groundbreaking discoveries make their way from the lab to the patient’s bedside.
Investment should also provide crucial support for startups and small-to-medium enterprises (SMEs) by offering grants, funding schemes, and business incubators, through the development of an environment that encourages risk.
Western Australia is also uniquely positioned with a wealth of natural resources that are currently untapped for discovering novel therapeutic agents, but by empowering researchers and scientists to collaborate and explore these, there is the potential for accelerated drug discovery and personalised medicine approaches.
We are on the cusp of transformative change, which could take WA’s life sciences sector to new levels.
This would also deliver benefits to the State’s economic diversification and growth agenda, and the overall health of the population.
A thriving life sciences sector here is achievable, but it requires a robust ecosystem nurturing entrepreneurship and the commercialisation of scientific breakthroughs, which will in turn create high-skilled job opportunities, reduce brain drain, and lead to increased productivity and prosperity for the region.
ED: Dr Dallimore is a neuroscientist, CEO and Managing Director of drug development company Argenica Therapeutics, and co-founder and Executive Chairman of medical device company Inspiring Holdings.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Data shows that, not surprisingly, cancer screening took a hit during COVID. This even applied to bowel cancer screening which, compared to breast or cervical cancer screening does not require one to attend a facility outside the house –unless one counts a post box as a facility. The question that is unanswered and may never be is what impact this will have on morbidity and mortality over the next decade or two.
Conventional thinking would tell us that the lost opportunity to find a cancer early, once lost can never be regained. In fact, by definition, a cancer found later is not found early. However, there is a school of thought that in some instances we are over diagnosing indolent lesions, which would not impact the person during their lifetime if not found.
Screening for cervical cancer was changed to five yearly and started later due to the view that too many women were undergoing colposcopes and other procedures that they ultimately did not need. Critics have pointed to the number of men who die with, not of, prostate cancer detected on routine PSA testing.
History tells us that when we believe today has a fair chance of being shown to be wrong at a future point in time. The term ‘ontological shock’ is defined as the state of being forced to question one’s world view. This is something we tend to resist in medicine. A recent study suggested that opiates may be no more effective than placebo in treating neck and back pain. Most of the commentary was critical of the study. There may be valid grounds for criticism. It was a small study and seems counterintuitive. Yet the latter is why we should be very curious as it creates ontological shock. What if our world view on use of opiates is wrong?
Dr Vinay Prasad writing in Sensible Medicine describes the case of a 74-year-old man who enjoyed smoking cigarettes (I know!) and tinkering on cars. Routine screening had found a lung cancer. “I have never felt bad in my life except for what you doctors did to me,” the patient said.
Prasad notes: “The only thing we know for sure is we gave a man side effects and kept him from doing what he loves. What we have no idea is whether he is better off.”
A genuine ontological shock will come if we find cancer morbidity and mortality does not rise as we expect with reduced screening. Time will tell.
The term ‘ontological shock’ is defined as the state of being forced to question one’s world view.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments


There is no systematic (population or targeted) screening for melanoma in Australia, however, there is evidence of significant ad-hoc (opportunistic) screening as well as early detection. There is currently insufficient evidence to support a change from ad-hoc to systematic screening.
Patients at high risk of developing melanoma may be considered as those with a previous history of melanoma, or with family history of melanoma and other risk factors, including use of sunbeds, multiple sun burns, fair skin and dysplastic naevus syndrome.
The risk of primary melanoma or subsequent melanoma can be estimated using the Melanoma Institute of Australia’s online risk prediction tool. Dermatologist surveillance using total body photography (TBP) and sequential digital dermoscopic imaging (SDDI), has shown earlier detection of melanoma and lower excision rates in high-risk patients.
A randomised control trial is currently underway in Australia to assess the value of TBP and SDDI in the targeted high and ultra-high risk melanoma patient setting.
As technology and artificial intelligence (AI) continue to demonstrate promise in dermatology, we provide an update and discuss the role of reflectance confocal microscopy (RCM), TBP, SDDI and AI in the high-risk melanoma surveillance setting.
RCM is a non-invasive ‘optical biopsy’ that enhances diagnostic accuracy when evaluating lesions with equivocal dermoscopy. As a second step evaluation after dermoscopy, it improves sensitivity and specificity, reducing the number needed to treat.
RCM prevents unnecessary surgical procedures, especially in cosmetically sensitive areas. It is particularly useful for large pigmented facial lesions where
RCM is a helpful imaging modality that can be used as an adjunctive, second-level assessment for equivocal lesions. Correlation with clinical/dermoscopic/pathological findings is essential. There is a demand for noninvasive imaging modalities to detect melanoma early and to avoid unnecessary excisions. Appropriately selected high-risk melanoma patients may benefit from the use of TBP, SDDI and RCM.
Although promising, more studies are required to further support the use of AI for diagnosis of pigmented lesions and to detect changes in TBP.
dermoscopy can be unreliable and obtaining a representative biopsy can be challenging.
RCM is also used to accurately define the margins of lentigo maligna prior to surgery, monitor melanoma recurrence in cases of unresectable disease or narrow margins and to assess the response after non-surgical treatments. Other indications include lesions with dermoscopy features of regression (grey colour), amelanotic lesions and mucosal lesions.
A two-step enhanced surveillance approach using interval TBP and
SDDI may be used for high-risk melanoma patient surveillance.
TBP can facilitate the detection of de novo (new) lesions and clinical changes in existing lesions and SDDI is used to identify dermoscopic changes in existing lesions.
The ABCDE criteria of melanoma includes the ‘E’ for evolving (changes in size, shape or structures) – this dynamic evaluation is not possible with standard surveillance using naked eye examination and dermoscopy alone or relies upon patient reported changes only. Our understanding of these dynamic changes is evolving and the interpretation of malignant versus benign dynamic changes relies upon the expertise of the user, with recent studies improving our understanding. Given the potential for undesirable outcomes with TBP (overtreatment and overdiagnosis), it is currently not recommended for use in low-risk populations.
AI has performed well in silico and will play a future role in melanoma detection and surveillance. However, real world data and regulation is currently lacking to support its safe, effective and ethical use. Hence, commercially available AI systems are currently not recommended for use in clinical practice. Some studies have shown that AI has a role in automatic detection of changes in TBP comparison, however, human supervision is still required.
RCM, TBP and SDDI are valuable tools in enhancing the diagnostic accuracy of melanoma. These tools require experienced human users, appropriate patient selection and dependable follow up processes to ensure quality and safety. Excisional biopsy remains the standard for melanoma diagnosis.
– References available on request. Author competing interests – nil.

Positive prostate cancer diagnosis in Australia affects more than 24,000 men each year. Men have a one in six risk of developing the disease by the age of 85, and with our ageing population, this has substantial implications for individuals, families, and our health-care system.
While the saying ‘you die with and not from prostate cancer' may have held more truth in the past, we must consider the significant increase in median life expectancy of Australian men over the past three decades – from 74.4 years in 1991 to 81.3 years in 2021. Prostate cancer is the second most common cause of cancer-related deaths among men (approx 3,500 annually).
Fortunately, early detection of prostate cancer offers high treatment success rates. Recent advancements have revolutionised how we diagnose and treat patients, resulting in a significant reduction in morbidity.
These transformative changes include:
i. the use of MRI scans to minimise unnecessary biopsies,
ii. recommending active surveillance for low-grade prostate cancer to reduce overtreatment,
iii. transition from transrectal to transperineal biopsy to minimise sepsis risk and improve biopsy accuracy,
iv. improvement in treatment precision through robotic surgery and advanced radiotherapy delivery techniques.
Yet one fear remains entrenched in our patients – the association of prostate cancer with incontinence.
As surgeons, our aim when treating prostate cancer is to achieve a trifecta of outcomes: clear margins, continence and potency. While oncological outcomes take precedence, the functional aspects, especially continence, have historically been portrayed negatively and can act as a deterrent to radical prostatectomy.
Over time, countless technical refinements have been made to address this with varying degrees of benefit and even the transition from open/laparoscopic to roboticassisted radical prostatectomy (RARP) has not shown widespread improvements in functional outcomes.
This is somewhat understandable as in majority of cases today, a RARP still follows a similar dissection to open prostatectomy – an anterior approach with access to the prostate achieved by developing the retropubic space and mobilising the bladder. In this way, bladder angulation, endopelvic fascia, neurovascular bundles, puboprostatic ligaments, accessory pudendal vessels and the Santorini plexus, all which can contribute towards potency and continence outcomes, are at risk of damage.
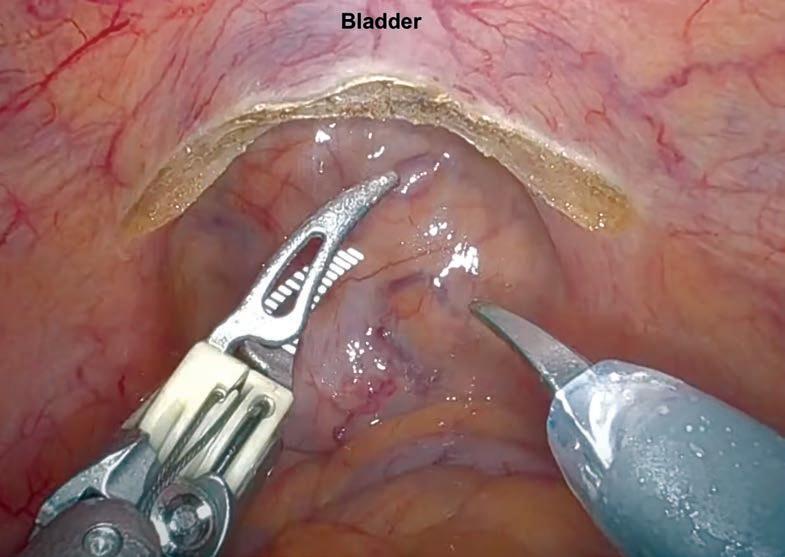
A significant advancement in RARP is the pioneering work of Professor Bocciardi, who introduced the Retzius-sparing robot-assisted radical prostatectomy (rsRARP) in 2010. This innovative approach diverges from traditional methods by avoiding anterior structures and minimising dissection other than that of the prostate itself.
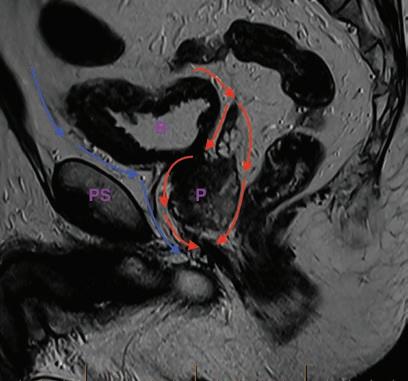
Utilising the capabilities of robotic surgery, rsRARP involves making an incision in the parietal peritoneum at the anterior surface of the pouch of Douglas, allowing direct access

Prostate cancer is the most common cancer in Australia with one in six men diagnosed by the age 85
Retzius-sparing prostatectomy has superior continence outcomes with a high proportion of men achieving full continence from trial of void
Patient selection is important to achieve the prostatectomy trifecta – clear margins, continence and potency.
to the base of the prostate without the need for bladder mobilisation. The seminal vesicles and vasa are first dissected, followed by an incision in Denonvillier's fascia.
In low-risk patients, an intrafascial plane can be developed posteriorly, extended to the apex, and then continued laterally to enable the full preservation of the neurovascular bundle. The bladder neck is then isolated, and anterior dissection is completed beneath the Santorini plexus and puboprostatic ligaments. Finally, the apex is
dissected with maximal urethral length preservation and then reconstruction is completed with a urethrovesical anastomosis.
Bocciardi's team published the outcomes of their first 200 cases, demonstrating an immediate continence rate of over 90% (from catheter removal at day seven post-op) and a less than 5% risk of incontinence beyond 12 months. Similar impressive continence outcomes have been reported by the few surgeons who have transitioned to this technique.
Two systematic reviews and metaanalyses of the published literature confirms the superiority of this technique with regards to both early and long-term continence outcomes. However, while Bocciardi’s group also reported outstanding potency outcomes (80% recovery at 12 months in men with normal preoperative function undergoing a bilateral nerve spare), the systematic review failed to show a statistically significant benefit in potency results when comparing rsRARP with RARP.
One of the primary criticisms of rsRARP is an increased risk of

positive surgical margins (PSMs). The highest risk is in those with anterior tumours, but the reported increased rate could also in part be due to the learning curve as most studies published thus far have compared surgeons' initial experiences with rsRARP to their well-established techniques for RARP.
Bocciardi’s group themselves reported a drop in PSM rate from 22.4% to 10.1% for their first 100 and subsequent 100 rsRARPs. Considering that most prostate cancer occurs in the peripheral zone, diligent patient selection could still allow the majority of men to undergo a rsRARP with superior functional outcomes without compromising oncological results.
In pursuing the ‘perfect prostatectomy’ – an operation to cure cancer with no functional detriment – rsRARP is a remarkable breakthrough. Its refinement and more widespread adoption with appropriate patient selection could help change the notion of post prostatectomy incontinence, enhancing patient experiences and overall satisfaction.
Author competing interests – nil
Mammography is a technically exacting procedure and occasionally it is not possible. In order to perform a technically adequate mammogram there are some client requirements that must be met, including:

sufficient muscle control to hold the upper body and arms in the position required, and remain motionless for 30 seconds being able to comprehend and cooperate with instructions such as “hold your breath” ability to consent to the procedure and potentially uncomfortable examination, such as clients not pulling away from the machine or staff coping emotionally with the unfamiliar situation and clinical environment as a mammography can be distressing for some clients.
On the occasions that a mammogram cannot be done for technical reasons, a BSWA team member will recommend that clients book an appointment with their GP to discuss other screening options.
For further information on alternative screening options, please email the Liaison GP at breastscreenwa@health.wa.gov.au.
Women may book online at www.breastscreen.health.wa.gov.au or phone 13 20 50
Unfortunately, mammography is not always possible



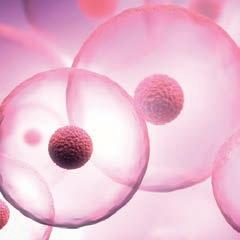

Adora Fertility provides affordable IVF without compromising on quality. By referring your patient to one of our highly qualified specialists, they will receive a tailored approach to their fertility treatment plans with medications sensitive to their needs. Out-of-pocket costs are typically less than $2,000 for a fully stimulated IVF cycle. Give your patients the best chance of conception without the financial sacrifice.
Our range of fertility treatment options has expanded to include our newly launched, Known Donor Program. As part of this program, patients can access affordable fertility treatment with donated sperm, eggs or embryos from a donor known to the patient. By facilitating sperm, egg and embryo donation in this way, we know that we can help more people grow their families in more ways.
 By Dr Michelle Cronje, Medical Oncologist, Subiaco
By Dr Michelle Cronje, Medical Oncologist, Subiaco
Breast cancer diagnosis in Australia affects over 20,000 women each year. As early detection rates improve and treatment paradigms evolve, breast cancer mortality is decreasing. Consequently, there is a growing population of breast cancer survivors with unique health concerns and service needs.
The vast majority (over 70%) of breast cancers are estrogen receptor positive. For these women, the addition of adjuvant endocrine therapy for at least five years is highly effective at reducing the risk of breast cancer recurrence.
Options include tamoxifen, aromatase inhibitor +/ovarian suppression with zoladex or surgical bilateral oophorectomy +/- hysterectomy.
It must be acknowledged that this comes at a cost for many of these women in terms of quality of life. Side effects including hot flushes, sexual dysfunction, weight gain, musculoskeletal symptoms and fatigue can be significant.
As patients transition to six- or 12-monthly follow-up with their cancer specialist, GPs are left to manage these side effects or patients seek alternative treatments or manage alone. Outside of a clinical trial, discontinuation rates range from 31-75% after five years of treatment.
Breast cancer affects over 20,000 women each year in Australia.
Hormonal treatments prescribed for breast cancer can cause distressing symptoms
Breast cancer survivors, want more support to manage symptoms.
Hormonal treatments prescribed for breast cancer can cause vaginal atrophy – thinning, drying and inflammation of the vaginal wall that results in discomfort, painful sexual intercourse and distressing urinary symptoms. Moderate-severe vaginal atrophy affects up to 75% of breast cancer survivors, and data from the Breast Cancer Network Australia (BCNA) demonstrates survivors want more support to manage symptoms.
A study by Peate et. al. (an online cross-sectional survey distributed through BCNA was highly informative with 524 of the 2286 women responding. The most common symptoms were hot flushes/night sweats and sleep disturbance (both 89%), vaginal dryness (75%), mood swings (62%) and sexual problems (60%). Symptoms were mild (21-33%) or moderate (21-38%) in about a third, and severe in up to one quarter (8-26%) of the cohort. Only 32% of these women were offered treatment – 49% found this “somewhat effective” and 34% found it ineffective. The majority wanted more support to manage their symptoms.

There is an excellent review by Franzoi et. al. published in The Lancet 2021 that summarises evidence-based approaches for the management of side-effects of adjuvant endocrine therapy in patients with breast cancer. This is a helpful resource for GPs who care for breast cancer survivors frequently (or even infrequently).
Interestingly, cognitive behavioural therapy can effectively help breast cancer survivors manage vasomotor symptoms by affecting their perception and cognitive appraisal of hot flushes. A commonly asked question is if HRT, topical estrogens are safe. There is no evidence that the risk of breast cancer recurrence increases with local vaginal estrogen, but several studies have shown that, theoretically, topical vaginal estrogens may increase serum estroedial in pre-menopausal patients on aromatase inhibitor with ovarian suppression and risk depends on individual patient. Opinions vary – the key is to ask the treating oncologist. Generally, one would try non-hormonal options first.
– References available on request
Author competing interests- nil




In recent years, the field of medicine has witnessed a significant paradigm shift with the integration of artificial intelligence (AI) in various specialties. One such groundbreaking application is in surgical oncology.
The convergence of AI with realtime in vivo digital pathology has emerged as a powerful combination, empowering surgeons with accurate, real-time information during the surgical procedure.
Traditional cancer surgeries have relied on histopathological examination of preoperative biopsy specimens to determine the extent and type of malignancy, and postoperative assessment of the resected tissue to determine margin clearance. These processes typically require several days, leaving

surgeons with limited information during the operation itself.
A significant advancement in surgical oncology is the integration of real-time in-vivo digital pathology with AI algorithms. This cutting-edge technology enables pathologists to examine tissue samples intraoperatively, providing immediate feedback to surgeons during the procedure. Rather than relying on frozen section analysis, real-time in vivo digital pathology allows for instant assessment without disrupting the surgical workflow.

This advancement offers several critical benefits to surgeons and pathologists alike. These include:
1. Improved accuracy: AI algorithms can quickly and accurately identify cancerous


cells, distinguish between different tumour types, and assess tumour margins. This level of precision significantly reduces the chances of leaving cancerous cells behind, improving the effectiveness of surgical resection.
2. Speed and efficiency: Realtime in vivo digital pathology with AI enables rapid analysis of tissue samples, providing immediate results to the surgical team. This accelerated workflow reduces operating time, mitigates potential complications, and shortens the patient's time under anaesthesia.
3. Enhanced decision support: AI-driven real-time pathology systems act as valuable decision support tools for surgeons. They can provide insights into the
The integration of artificial intelligence with real-time in vivo digital pathology has ushered in a new era of precision and efficiency in surgical oncology.
AI-driven systems offer improved accuracy, speed, and decision support, enabling surgeons to provide more targeted and personalised care to cancer patients.
The ongoing development and integration of AI in surgical oncology hold tremendous potential for transforming patient outcomes and shaping the future of cancer surgery.
tumour’s molecular profile and potential response to specific therapies, aiding in personalised treatment planning.
4. Integration with imaging modalities: AI algorithms can also be integrated with various imaging modalities, such as MRI, CT and PET scans. This fusion of
continued on Page 56
GenesisCare at Hollywood offers access to radiation oncology consultations, treatment, and access to allied health support services. We offer modern evidence-based techniques and technology combined with compassionate care – aiming to deliver the best possible patient experience and outcomes.
We offer patients:
• Personalised treatment plans, striving for minimal wait times
• Tattoo-free technology
• Access to a wide range of allied health services (including exercise physiology), accommodation, and transportation packages
• For patients who are eligible for Medicare, approximately 80 to 90% of radiation therapy treatment costs are often covered by Medicare rebates

• Private health insurance is not required for radiation therapy
• A multidisciplinary team of supportive clinical professionals
*For radiation treatment patients. Based on patient survey results Oct 2021–2022. CSAT score 100%

genesiscare.com
An original captured image (A) is enhanced and denoised in real-time (B) using image pre-processing, filtering, and masking which allow more detailed inputs for Deep Neural Networks. Nuclei are extracted (C), followed by cell boundary segmentation (D), and mapping of optical vector intensity (E) to further enhance segmentation. In this way, algorithms can measure features such as cell and nuclear size, cell and nuclear pleomorphism, altered nuclear:cytoplasmic ratio, cell crowding, presence of inflammatory cells and other features (F), all of which are used to make quantitative assessments of tumour compared to normal tissue intraoperatively.


continued from Page 55
information enhances the surgeon's understanding of the tumour’s precise location, size, and extent, resulting in more precise and targeted surgical interventions.
5. Training and skill development: AI can be leveraged for training surgeons and pathologists. By analysing vast datasets, AI algorithms can simulate different scenarios and provide trainees with invaluable learning opportunities in a safe, controlled environment.
The integration of AI in real-time in vivo digital pathology holds great promise for improving patient outcomes in surgical oncology. Benefits can be summarised as:
1. Reduced recurrence rates: With the assistance of AI, surgeons can achieve more precise tumour removal, leading to reduced recurrence rates and potentially improving long-term survival for cancer patients.
2. Minimised complications: Faster and more accurate tissue analysis during surgery reduces the likelihood of complications associated with incomplete tumour removal, preserving critical healthy tissue and minimising post-operative side effects.

3. Personalised treatment: AI-powered real-time pathology can provide valuable insights into the tumour’s molecular profile, helping to tailor treatment plans to each patient's specific needs. This personalised approach enhances treatment efficacy and reduces the risk of unnecessary therapies.
4. Increased accessibility: AI's ability to analyse pathology and imaging data rapidly can help bridge the gap between high-resource and lowresource settings, making advanced diagnostic and surgical capabilities more accessible to underserved populations.
While the integration of AI in real-time in vivo digital pathology presents promising prospects, several issues need to be addressed for its widespread adoption such as data privacy and security, regulatory approval, interoperability and ethical considerations. Nonetheless, by augmenting surgeons' capabilities and fostering personalised patient care, AI is paving the way for a future where oncologic surgeries are safer, more efficient, and yield better outcomes.
Author competing interests – the author is CEO & Managing Director of Optiscan Imaging Limited, an ASX-listed which has developed, manufactured handheld confocal laser endomicroscopes for real-time intraoperative digital pathology.


Cervical cancer is driven almost exclusively by infection of the cervix with the ubiquitous, sexually transmitted Human Papilloma Virus (HPV). It is one of the most preventable cancers and this year is predicted to cause around 200 Australian deaths, almost all of these occurring in those who are under-screened or have never been screened.
The HPV virus causes cancer by infecting cervical cells, causing alterations in internal cell signalling pathways, leading to pre-malignant and malignant change. When caught early through screening, the affected cells can be monitored for resolution or treated with surgery to prevent the progression to lifethreatening disease.

In 2017, 10 years after the HPV vaccine was introduced onto the Australian National Vaccination Program, the National Cervical Screening Program (NCSP) was overhauled in Australia to a fiveyearly HPV-testing cycle for women and people with a cervix aged 25-74 years who have had sexual contact.
For most people, the mandated screening test was a cliniciancollected sample of the directly visualised cervix using a speculum. A small number of under-screened and high-risk groups had the option of a vaginal self-collect sample at the time.
On July 1, 2022, an update to the NCSP expanded eligibility for selfcollect of vaginal samples and is now available as a primary screening option for most women.
The new vaginal self-collect pathway follows research demonstrating equal accuracy in HPV detection between self-collect samples and clinician collected samples. Qualitative research also demonstrates the self-collect pathway will increase participation in the NCSP, particularly of First Nations people, those of culturally and linguistically diverse backgrounds (CALD), those with past trauma or previous negative
Key messages
Cervical cancer deaths are largely preventable
Most deaths occur in underscreened populations
Self-collection can improve screening rates and reduce mortality.
experiences of a speculum examination.
Self-collection is not recommended for people with gynaecological symptoms, undergoing ‘Test of Cure’ surveillance, with previous total hysterectomy for high-grade squamous or glandular lesions, exposed to Diethylstilbestrol (DES) in utero and/or who have had adenocarcinoma in situ (ACIS).
If a self-collect swab is positive for High-Risk HPV (specifically subtypes 16 or 18), the patient will be recommended for colposcopy. A physician collected liquid based sample for cytological assessment (LBC) should be considered prior to colposcopy to help guide the
colposcopist at the time of procedure. If intermediate Risk HPV is detected, an LBC sample is recommended. If negative, the recommendation is routine HPV rescreen at the standard five-year interval.
Maximising participation through all means, including self-collect vaginal swabs, contribute to the renewed NCSP achieving its predicted benefit on cervical cancer outcomes.
In unvaccinated cohorts, the renewed NCSP is predicted to result in a 31% reduction in cervical cancer incidence and a 36% reduction in cervical cancer mortality compared to the previous program (265 fewer cancer cases and 82 fewer cancer deaths annually) and a 24% reduction in incidence and a 29% reduction in mortality (85 fewer cancer cases and 28 fewer deaths each year) in HPV vaccinated cohorts.
Author competing interests – nil

When faced with chronic pain syndromes, health-care providers should consider nerve entrapment syndromes (NES) originating from the peripheral nervous system and musculoskeletal system in the diagnostic process.
Despite extensive investigations, patients with NES often receive normal results, leading to frustration and inappropriate treatments. Recognising NES as a potential cause of pain is crucial to address the underlying issue effectively.
In cases of chronic pain where the cause is elusive, some may prematurely label the pain as psychosomatic. Misdiagnosing pain as psychosomatic without ruling out NES or other subtle conditions causes significant distress for patients, prolongs suffering and unsuccessful interventions, limiting patients' options and diminishing their quality of life.
A paradigm shift is necessary to prevent patients from resorting to desperate measures due to the unbearable pain caused by difficult-
Key messages
Misdiagnosing pain as psychosomatic without ruling out Nerve Entrapment. Syndrome (NES) or other subtle conditions can have longstanding consequences, including suicidal attempts and requests for euthanasia.
Incorporating Carnett's sign in all abdominal pain assessments is encouraged.
An in-depth understanding of opioid prescriptions for chronic pain, taking into account their paradoxical effects remains essential.
NES can manifest anywhere in the body.
to-identify conditions like nerve entrapment.
NES treatment pathway
I have developed a six-step diagnostic and treatment pathway to accurately diagnose and manage
NES. This pathway provides a systematic approach to identifying and addressing nerve entrapment and other subtle causes of pain, ensuring appropriate care for patients.
First and foremost, medical, surgical, malignant, and other potential causes of pain should be carefully evaluated and excluded.
Preparation: Evaluate the patient's pain and factors influencing it, considering the systematic weaning from opioids if possible.
Examination: Conduct a focused physical examination and functional assessment to understand the impact of pain on the patient's daily life. NES can manifest anywhere in the body and a high index of suspension is required to include in the differential diagnosis of chronic pain.
Specific indicators like the Carnett sign with normal biochemical markers, and negative investigations strongly suggest anterior cutaneous nerve entrapment syndrome (ACNES).
Pain mapping: Use digital palpation to identify areas of pain and mark pain epicentres within the painful area. Measure their position in relation to reference points. The shape of the painful area such as a specific focal point, shape of a muscle, nerve distribution, or a combination helps identify where the pain is originating.
Ultrasound imaging (sonomapping): Perform ultrasound imaging of pain epicentres to identify abnormalities in various tissue layers. The technique of conducting sono examination is important to detect subtle pathologies like angiolipomas and scars with possible NES that are often missed in routine scanning.

Diagnostic and therapeutic injections: Administer local anesthetic injections guided by ultrasound into the identified pathological areas. These injections can relieve pain instantaneously and confirm the peripheral origin of the pain. Hydro dissection, using dilute local anesthetic with
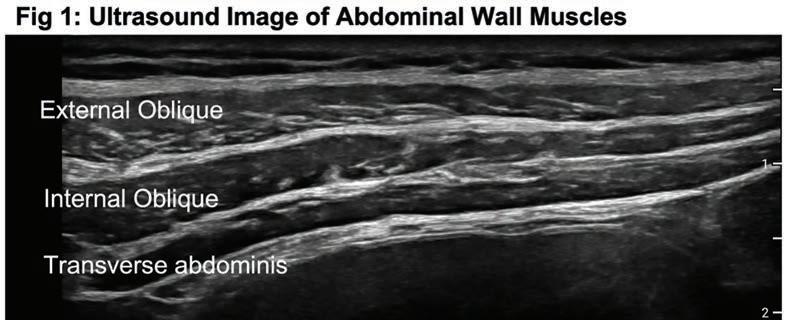
or without adjuvants, can release nerve entrapments and further assist in managing other conditions.
Rehabilitation and follow-up: Emphasise active movements of the treated area during the soft tissue healing phase, which is usually six weeks to prevent re-entrapment of nerves. Patient education and involvement are crucial in maximising treatment outcomes.
Several factors can contribute to the inability to alleviate nerve entrapment pain:
Patient-related factors: Inaccurate expression of pain location or continued opioid use may hinder successful treatment.
Proceduralist-related factors:
Challenges in accurately identifying the location of nerve entrapment or detecting other pathologies can impede effective treatment.
Persistence of entrapment: Inadequate release of the trapped nerve despite hydro dissection may require additional procedures.
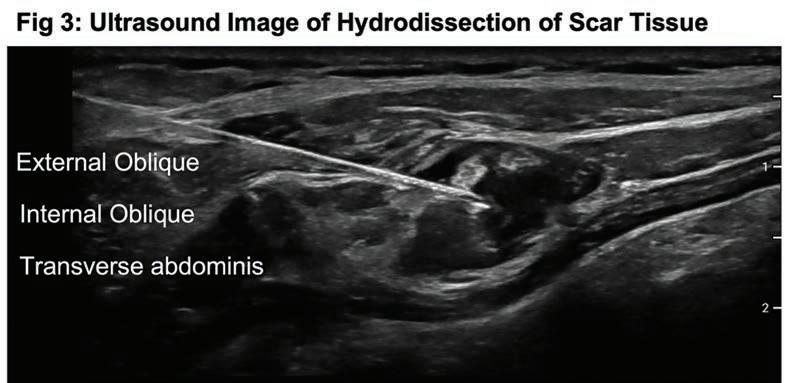
Lack of proactive measures: Failure
to engage in vigorous movements of the affected area can lead to re-entrapment of nerves following initial good relief of pain.
This involves appropriate prescribing, weaning plans, disposal, prevention of diversion and management of opioid use disorder. At the time of initiation of opioid therapy, it is important to discuss weaning plans with patients and if appropriate empower them by letting them know that they don't require a doctor's permission to reduce or stop taking pain medications.
In summary, nerve entrapment syndromes present a diagnostic challenge and can result in ineffective treatments if overlooked. Trusting the patient's account and ruling out other subtle causes of pain, including NES, before initiating opioid therapy or considering psychosomatic causes is crucial. By adopting the NES treatment pathway and increasing awareness of NES, health-care providers can improve patient outcomes and alleviate suffering.

The Margaret River Regional Open Studios event celebrates 10 years this year and is now one of the biggest in the country. Meet one of this year’s artists, ceramicist Georgia Zoric.
 By Ara Jansen
By Ara Jansen
When Georgia Zoric agreed to put her art on display for the first time at the Margaret River Regional Open Studios last year, she didn’t expect such a warm reception. She also didn’t expect to hear so many stories and floods of tears.
“Being part of the open studios was incredible,” enthuses Zoric. “Every day I would have someone come in and spontaneously burst into tears. My work seems to have a very ancestral feel to it and reminds people of something, even if they can’t quite put their finger on it.
“There was plenty of laughter too! Both things seemed to illicit a healing response. Hearing these stories became an unexpected privilege of being part of this event.”
Running from September 9-24, this year’s 10th anniversary event features 166 artists and 44 new studios to visit. It’s an opportunity for the public to visit artists in their studios, see their work and talk to them about it. The works are also for sale and 100% of proceeds go to the artists. This free annual showcase has become the biggest of its kind in Australia.
“I love that so many artists are generous with their time and willing to share their process with their studio visitors, especially with other artists,” Zoric says.
Last year was the first time Zoric had publicly displayed her works. She describes it as one of the most positive experiences of her life. Because she has a studio in the middle of her house, she recreated her studio at The Bond Store at ArtGeo, right down to the furniture and plants she normally surrounds herself with.
A life-long artist, Zoric came late to finding the art of her heart. She hails from a family of makers, including her mother, a well-known knitwear designer, while one of her two sisters is a fashion designer.
“I grew up in a house where making a living from art was encouraged, if not essential and completely normal. We were always making something.”
Over the years, while raising her children in the South West, she has quietly and determinedly taught herself different arts from painting to carving. It has only been in the last few years that she has settled on ceramics. You’ll find one of her first big works, The Postmaster, submerged amongst more than a

Her work has an ocean or seafaring theme – characters in jumpers, which mimic the textures of the wool of her childhood and textured ceramic bottles, reminding her of the glass bottles which her family collected and were all over the

house. She prefers matte to gloss and her tones are muted, almost like you might be viewing the pieces underwater. All these things make you want to reach out and touch the work, which has a heavy and reliable footprint, over being dainty.
“This event made me realise that the work I was creating for myself was also something other people liked. At 51, I’ve really found my niche as a ceramicist. I hope the event inspires everyone who visits a studio and I think it’s fair to say, be prepared for interesting conversations.”
For information about the Margaret River Regional Open Studios, go to https://mrropenstudios.com.au/ The site features the new Artist TrailMaker which will help plan your arty adventure by mapping all the artists you want to visit in Google Maps.

It was in 2004 that the Castelli family purchased their property on Mount Shadforth in picturesque Denmark. Originally intended as their holiday property, Sam Castelli’s Italian wine-making heritage took over, and so he completed the partially built winery that was on the property. Today Castelli Estate produces a range of wines not only from the home vineyard, but also taking advantage of the terroirs and microclimates across the Great Southern and selecting parcels of fruit which express the attributes of this great region. This all works well in the hands of winemaker Andrew Vessey, who brings with him extensive experience having worked in wineries across Europe, Australia and New Zealand. The resultant wines come highly recommended.


A true expression of Riesling from the Great Southern. Intense, pristine, focused fruit with a linear profile. Floral kaffir lime aromatics, with Meyer lemon flavours, a talcum powder mouthfeel. High acidity gives a crisp clean finish. Can drink now or allow more complex flavours to evolve over the years ahead.
A nice Pinot. It’s a result of a good vintage for Pinot, with cold temperatures, late ripening and harvesting giving the acidity required to get this difficult variety correct. Fruit was from the home vineyard and underwent detailed vinification with different clones handled differently in the winery. Having spent years studying the differing nuances of the subregions of Burgundy, I cannot help drawing comparisons with this wine very much in the style of Morey-StDenis, being an attractive delicate brighter style. It has vibrant red cherry aromas, fresh raspberry and cranberry flavours, and some spiciness from background oak.
A youthful, big, ripe wine from a warm vintage. The predominant Shiraz gives the blueberry, white pepper characters. Herbal, earthy, savoury elements from the Malbec also give this wine a real tannic hit. Enjoy it over the next few years.
$ 37)
A good Cab Sav from that nearperfect 2018 vintage. Still shows a youthful meniscus in the glass – obviously in for the long haul. Complex aromas of black fruits, clove, a touch of allspice. Fullbodied palate with big flavours of blackberry, black olive and coffee. Fine tannins across the palate. Great length. Good value for money in a wine that will reward for a further 10 or 12 years.
An outstanding Chardonnay from the Denmark home property marketed under Castelli’s special premium label. Pristine in the glass. Beguiling nose is a marriage of ripe primary fruit and quality oak. Lemon citrus, stonefruits, some brioche. The palate is vibrant, clean, focused and long. Flavours of grapefruit, citrus and pineapple with mineral elements. A creamy touch from partial malolactic ferment. Beautifully integrated oak. A 6-8 year wine. The Denmark subregion is certainly coming of ‘Chardonnay age’ with wines like this.

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat.