Charity from the heart



























Well didn’t the guestimate of Medicare rorting by doctors put the cat among the pigeons?
Having worked in mainstream media for many years, I’ve seen sweeping criticisms of ‘sensational reporting’ when people simply do not agree with the story, even when it is factual and fair.
But it is difficult to see how anything in Margaret Faux’s PhD thesis into Medicare billing gave substance to the headline figure of $8 billion that was said to have been wrongly siphoned out of Medicare by doctors.
After originally hedging his bets by neither accepting nor dismissing the media reports, Federal health minister Mark Butler later ruled there was no evidence to back the $8b claim, but has since enlisted a health economist to delve into Medicare anyway.
There seems to be at least some consensus that the system is broken.
One thing that is not broken is the travel bug, which has been reignited after three years of pent-up demand. This month, we look at travel medicine and what it means in COVID times.
A recent survey commissioned by a pharmaceutical company found that only 15% of Australians planning to travel overseas had thought about getting any health travel advice. Fewer than onethird thought it was a good idea to discuss it with their doctor. This is despite ongoing reports of West Australians visiting their favourite overseas destination – which we sometimes forget is in a developing country – and getting the dreaded Bali belly.
And as we digest the full implications of the Medibank data theft, we also examine what is happening with how our health data is collected and used.

While the pandemic broke down some resistance to the use of My Health Record by consumers and practitioners, it is still a bumpy road ahead.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
There seems to be at least some consensus that the system is broken.



Dr Wai Leong is the lucky winner of a great selection of wines from Knee Deep featured in our October doctors dozen competition. This month, we have on offer a dozen bottles from Rosenthal Wines, reviewed by Dr Louis Papaelias, on page 59. We also have five double in-season passes to Emily, the new biographical drama based on the life of English writer Emily Bronte. To win the wine or the movie tickets, go to www.mforum.com.au or use the QR code on this page. Good luck!

Fonda Grapsas – Director







Tony Jones – Director tonyj@mforum.com.au



EDITORIAL TEAM


Editor
Cathy O'Leary 0430 322 066 editor@mforum.com.au

Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au


Marketing Quinn Hampton quinn@mforum.com.au

Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006 Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
National efforts to safely prevent preterm and early term birth – which originated in WA – recently celebrated a landmark event in Sydney.
Teams from more than 50 Australian maternity hospitals met at Sydney Olympic Park for the first critical learning session of Every Week Counts – the national preterm birth prevention collaborative.

Being born too early remains the leading cause of death and disability in children up to five years of age in the developed world. Preventing this major complication of pregnancy and its far-reaching impacts is now considered a high priority in health care.
Every Week Counts is a two-year initiative aiming to safely lower the rate of preterm and early term birth within participating maternity units in Australia and lead to ongoing better practice.
In recent years, the rate of preterm birth has been rising dramatically in many countries, including Australia, with more than 8% of births occurring too early, and almost double that rate in First Nation Australians.
The national program to safely lower the rate of preterm birth began with a state-wide program launched in WA in 2014.
At the recent event in Sydney, hospital teams represented every state and territory, ranging from the largest tertiary services to key services in regional and remote communities providing local care.
Leading obstetricians, midwives, GPs, sonographers and neonatologists, together with consumers and quality improvement experts, met to bridge the gap between what is happening on the ground and what experts know will improve outcomes for women and their babies.
Every Week Counts is a collaboration between the Australian Preterm Birth Prevention Alliance, Women’s Healthcare Australasia, the Institute for Healthcare Improvement, Safer Care Victoria and the Women and Infants Research Foundation, and is being funded by the Commonwealth Government.
Curtin University-led research will provide the first estimates of the number of Aboriginal children with ear infections and hearing loss.
Chief investigator Associate Professor Christopher BrennanJones from Curtin’s School of Allied Health and Telethon Kids Institute said his project would look at the rate of hearing loss caused by otitis media in Aboriginal children.
It will also consider the effectiveness of ear health promotion programs, with the findings to help inform national policy.
“Aboriginal children are known to be at greater risk of otitis media and associated hearing loss than the general population yet we still do not have reliable estimates of its prevalence for Aboriginal children from birth to five years of age,” he said.
“Our research will provide these estimates and demonstrate the feasibility of screening for ear infections and hearing loss from two months of age.”
It will also test the effectiveness of
the ‘Blow, Breathe, Cough’ health promotion intervention to resolve ear infections and prevent hearing loss without the need for surgery.
A separate project will develop an online platform to help adults with hearing loss to make informed decisions about their hearing health care.
Chief Investigator Associate Professor Melanie Ferguson, from the Curtin enAble Institute, Curtin School of Allied Health and the Ear Science Institute Australia, will develop an app called HearChoice, which will outline the pros and cons of available hearing health-care options such as the different types of hearing aids, new technologies called ‘hearables’ and assistive listening devices.
A new dedicated eye facility has opened in Subiaco, aimed at improving the experience and care for St John of God Subiaco Hospital patients undergoing eye procedures and treatments.
Following its opening in October,
all surgery performed by SJOG Subiaco Hospital ophthalmologists will now be undertaken at the dedicated eye unit, located at the former site of SJOG Wembley Day Surgery in Cambridge St.
SJOG Subiaco Hospital CEO Tina Chinery said that the new facility would provide a new level of dedicated services to care for eyes.
“We are excited to open this new facility to improve the experience for patients undergoing eye procedures and treatments by fasttracking their time in hospital and providing specialist support focused on their clinical needs,” she said.
“We have also invested in the latest ophthalmic technologies and equipment, including new ophthalmic patient chairs, which patients will remain in throughout their surgical journey, from the preadmission process to recovery.”
The facility was officially opened by SJOG Health Care board chair Kerry Sanderson at an opening and blessing ceremony.
Metastatic melanoma (MM) refers to the deposition of malignant melanoma cells distant to the primary tumour, usually via lymphatic or haematogenous spread.

Mrs P is a 47-year-old woman who presented to her GP with a threeweek history of left breast pain and a palpable lump. Notably she has a past medical history of a left forearm melanoma which had been completely excised with a negative sentinel node several years ago. Ultrasound of her left breast demonstrated an 8cm x 6cm predominantly cystic, partly solid lesion with some mildly atypical features. This was felt most likely to be a haemorrhagic breast cyst. She underwent ultrasound guided fine needle aspiration (FNA) of the cyst fluid and subsequent core biopsy of the more solid components.
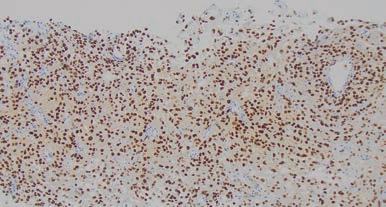
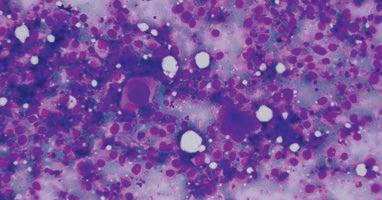
Cytological examination of the FNA showed numerous dispersed large atypical cells as well as background macrophages containing melanin pigment (Figure 1). Histological examination of the breast core biopsy showed sheets of atypical cells, many surrounding small blood vessels with admixed inflammatory cells (Figure 2). Immunohistochemistry confirmed melanocytic differentiation with the tumour cells staining positive for melanocytic markers (SOX10 – Figure 3) and negative for breast cancer markers (Cytokeratin, estrogen/progesterone receptor). A diagnosis of metastatic melanoma was made. Subsequent molecular testing demonstrated a BRAF somatic mutation was present in the malignant cells.
 By Dr Aaron Andreas MBChB(Hons) Genetics BS(Hons) FRCPath
By Dr Aaron Andreas MBChB(Hons) Genetics BS(Hons) FRCPath
Figure 2. Breast core biopsy showing sheets of malignant melanoma cells surrounding a vascular structure. Scattered macrophages with pigment can be seen in the background.
Metastasis accounts for the vast majority of morbidity and mortality related to melanoma. The most common sites are the skin, lymph nodes, lung, bone, brain and intestines. However any site in the body can be effected. Metastasis can occur even with very early primary melanomas which have been completely excised, and often occur many years and even decades following the removal of the primary tumour. MM has a highly variably cytological/ histological appearance and can mimic many other malignancies, often requiring confirmation with melanoma markers using immunohistochemistry. There should be a low threshold for testing with melanoma markers in patients with a known history of melanoma
Figure 3. SOX-10 immunostain showing positive staining of the neoplastic cells, confirming melanocytic differentiation.
to ensure cases are not missed or misdiagnosed. Approximately half of MM carries mutations in the BRAF gene which helps them grow and proliferate. Specific targeted therapies now exist which are highly effective against BRAF mutated MM and so newly diagnosed MM are routinely screened for BRAF mutations.

Clinical Labs offers GPs the opportunity to earn CPD hours by participating in our Skin Excision Evaluation Program. Our unique program offers a truly educational experience, by analysing participants diagnostic skill for identification of high-risk lesions.
To register now for the 2023-2035 triennium, visit clinicallabs.com.au/skinregistration, or scan the QR code, and complete our digital registration form.
MM can occur years or even decades after the primary tumour excision and can effect any part of the body.
MM can mimic many other malignancies both clinically and histologically, therefore it is important to provide a history of melanoma on request form for any patients undergoing a FNA or biopsy regardless of the site involved.
Newly diagnosed MM are routinely screened for BRAF mutations to help detect cases which may respond to targeted BRAF inhibiting therapies.
Wembley Day Surgery closed on September 23, with procedures transferred to the main hospital.
Health treatments evolve at breakneck speed and rely on research to drive the newest therapies and breakthroughs. While good health research depends on community involvement, it can sometimes be hard for people to know where to start.
In response, Edith Cowan University has launched a new register to make it easier for people to be involved in ongoing and future medical research. It allows those who sign up to receive information about research projects that match their areas of interest, such as mental health, maternity care or diabetes.
There are more than 20 health areas to choose from, with participants able to select multiple preferences. Some of the current research
projects seeking participants include studies on the effect of physical activity on mental health, and better communication in aged care facilities.
Project coordinator Danielle Brown said the register would benefit researchers, but also provide a way for people to be involved in research relating to potential treatments relevant to themselves or loved ones.
WA-based health insurer HIF has announced a new partnership with Binar Futures – a not-for-profit sport, education and leadership organisation supporting Indigenous youth in Western Australia.
The three-year partnership will see HIF provide funding for Binar’s sporting teams and homework classes, while HIF employees will be invited to participate volunteering opportunities.
Binar Futures was founded by Midland businessman Adam
The first clinical trial is underway for a novel neuroprotective drug developed in Western Australia to reduce brain tissue death after ischaemic stroke.
The Phase 1 trial is testing the safety, tolerability and pharmacokinetic effects of the drug in healthy human volunteers.
The drug candidate, ARG-007, was developed by Perron Institute and University of Western Australia researchers Professors Bruno Meloni and Neville Knuckey and their team. It has been shown to improve outcomes in preclinical models.

An ischaemic stroke occurs when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. There are currently no neuroprotective treatments that minimise the brain damage that occurs immediately after an ischaemic stroke.
Argenica Therapeutics, the biotechnology company commercialising ARG-007, has announced that the first volunteer to receive a dose showed no serious safety issues 24 hours after being injected.
This has opened the way for dosing the remaining participants in cohort one. All follow-up safety data will be presented to the scientific review committee, which will then confirm the progress of the trial to the next cohort.
The Phase 1 clinical trial, conducted at the Linear Clinical Research facility in Perth, will assess ARG-007 across
Desmond in 2011 when he supported a local basketball team of six Indigenous youths. It has grown to now support more than 1400 young people across Perth in sporting pursuits, education opportunities, leadership training, employment and cultural awareness.
Calls to a new Ahpra cosmetic surgery hotline have already resulted in the launch of 13 new investigations over allegations of unsafe or inappropriate practice.
The hotline has received 60 calls since it opened in September, with Ahpra launching an average of one new investigation a week based on these tip-offs.
Allegations being investigated include continuing to advertise services and allegedly taking appointments while holding nonpractising registration; intimidation of patients; inappropriate claims
four cohorts of healthy adult volunteers, with each group receiving an increasing dose.
The trial is double blind so neither the participants or the investigators know which volunteers are receiving a dose of ARG-007 and which receive a placebo.
“Commencing clinical trials is a significant milestone,” Professor Meloni said. “We have been working toward this goal for almost a decade and I’m incredibly proud of what we have achieved so far.”
Argenica’s CEO and managing director Dr Liz Dallimore said it was a pivotal moment to take the ground-breaking research from the Perron Institute and UWA into the clinic.
“The aim is for the new therapeutic to be administered by first responders to protect brain tissue against damage during a stroke with further potential to enhance recovery once a stroke has occurred,” she said.

Dr Lachlan Henderson takes up the role of CEO of HBF in February. Born and raised in Perth, he has more than 30 years’ experience as a GP and in clinical and managerial roles, most recently at Epworth HeathCare, Victoria’s largest notfor-profit private hospital group.

Top Perth childhood brain cancer researcher Professor Nick Gottardo is Cancer Council WA’s 2022 Cancer Researcher of the Year. The Telethon Kids Institute researcher is head of oncology and haematology at Perth Children’s Hospital.

St John of God Health Care has appointed Professor Steve Webb as its new director of research. He has worked for more than 16 years as an intensive care physician at SJOG Subiaco Hospital.
Child health researcher Professor Donna Cross has joined the Healthway Board for a three-year term.
Multiple sclerosis researcher Dr Marzena Fabis-Pedrini is the 2022 Perron Institute Aspire Award winner for her work looking at the cause of MS and improved treatments.
A winner in the annual Curtinnnovation Awards is HerHelp. Developed by Curtin health sciences student Alexis McDonald, the mobile application helps women access wellness resources and mental health professionals.
Guardian Exercise Rehabilitation and Custodian Work Assist have appointed Robert Pierce as their new CEO.
continued from Page 6
about expertise and unrealistic expectations in advertising; and poor post-operative care and infection control.
Ahpra CEO Martin Fletcher said the allegations related to practitioners and matters which had never previously been reported. He urged anyone who had a bad cosmetic surgery experience to report it on 1300 361 041.
Practitioners can also use the hotline to report their concerns, which can be made confidentially. The Medical Board of Australia has written to 133,000 medical practitioners reminding them of their obligations to report unsafe practice.
The Women and Newborn Health Service has recently published three new booklets to support women make their own choices about pregnancy options.
The new resource includes information booklets for consumers and health professionals, including complications during pregnancy, and support and counselling available for people seeking abortion.
It covers abortion care information and legal obligations for medical practitioners within the current laws in WA, as well as information about support services available at WNHS and in the community for people experiencing an unintended pregnancy.
A record $8.3 million was recently raised for WA cancer research by the nation’s biggest charity bike ride, the MACA Cancer 200 Ride for Research.
The money will go to Perth’s Harry Perkins Institute of Medical Research to support work investigating the hardest-to-treat cancers.
More than 1500 riders set off from Optus Stadium on the 200km ride to Mandurah.

Perkins director Professor Peter Leedman said vital new cancer research would be able to go ahead because of the funds raised by the charity ride.
“We will be able to attract and retain even more of the best scientists from across the globe and support them with sophisticated equipment to enable further discoveries about cancer and help develop new treatment,” he said.
Rider and cancer survivor Kane Blackburn raised more than $75,000 for this year’s event.
“I did my first ride in 2016, six months after getting out of hospital after a receiving a radical procedure, a stem cell transplant to treat my blood cancer,” Kane said.
The survival rate for this type of cancer was 30%.
“Our family has lost several members to cancer, including most recently my father in March this year. I never expected we’d bond over cancer stories,” he said.
“In a way this ride saved our family. It was something for us to rally around. Most don’t even like riding, but it’s been a focal point to funnel our energy.
“It gives us optimism that in the future cancers will be prevented, that cures and treatments will be developed and refined and it gives us comfort that we are doing something for others after losing the people we love – this is why I ride.”
Mining companies MACA, Mineral Resources and WesTrac provided equipment and assistance with logistics to reduce the costs of the event and maximise the funds directed to cancer research.
In the 11 years of the ride, more than $55m has been raised for cancer research at the Perkins institute.
Whether Dr Kushwin Rajamani is talking about medicine, his family or his extensive philanthropy, there’s one word which keeps coming up – heart.
The cardiologist and dad of two seems to apply it to everything he does, including the name of his practice – Omni Corde which is Latin for “all heart”. On top of that, he seems to have tremendous energy to be enthusiastically engaging in these three significant loves of his life.
Given these passions, perhaps it’s no surprise that Kushwin became a cardiologist – dealing with matters of the heart. His dual interest in cardiac anatomy and physiology ignited the pursuit of cardiology with a sub-specialty in heart rhythm disorders. Rotations during medical school cemented his plan. He also considers the research element dynamic and progressive, for which he has received several national awards.
In 2018, Kushwin established a solo practice called Omni Corde so he could dedicate his practice to caring for patients with heart rhythm conditions. He enjoys the autonomy of running a solo practice and is able to focus primarily on patient outcomes. This also allows him to spend time with his family, plus raise funds and awareness for his charity projects.

Born and raised in Sri Lanka,
Kushwin did his medical degree at Ireland’s Royal College of Surgeons and moved to Australia after completing his internship. He completed basic and advanced physician training in cardiology at Royal Prince Alfred Hospital in 2011 and has a PhD from the University of Sydney. He also spent two years at the Cleveland Clinic in Ohio, which has pioneered numerous medical breakthroughs including the first coronary angiogram, maintaining their number one ranking in cardiology for more than 25 years.
As a child, Kushwin was a diligent student and gained entrance to a local international school, which opened doors to study medicine in the UK. He did his last year of high school in London and was accepted into the Royal College of Surgeons before they’d even seen his results.
Kushwin’s father has no formal education and can only write numbers, while his mother only went to primary school. Educating their children was a huge priority for them. Their son wanted to make his parents proud by doing really well.
“Seeing my parents struggle was a huge motivation to be successful,” explains Kushwin. “At their social and economic level, getting us educated was a huge challenge.
“I like people and enjoyed science
so that made medicine a natural path to pursue. I was quite an introvert and probably was a total nerd at school. I enjoyed reading and was comfortable in my own company, but I also connected well with people who had similar interests and generally had a wide awareness.”
Unlike many of his school friends, he didn’t have the same support systems, so he crafted a strong work ethic, and he figured out what would give him an advantage from an early age. He did this by dedicating extra hours to reading, which eventually set him up perfectly for the long hours of medical school.
At college, he was further challenged by suddenly being in the company of students who were also high performing, once again pushing him to discover techniques which created an edge in an extremely competitive environment.
“I ended up with an honours degree but, to be honest, I think it had more to do with the hours I put in. What I had learnt was how to be strategic and how to adapt in order to achieve my goal.”
Initially he was going to work in America after graduating but a friend suggested coming to Australia. When Kushwin compared the lifestyle for a doctor,
There’s heart in everything Associate Professor Kushwin Rajamani does – from the name of his practice to the charity work he does and the time he spends with his family.
By Ara Jansen
my parents struggle was a huge motivation to be successful. At their social and economic level, getting us educated was a huge challenge.”

“Seeing
This year marks the 40th year of Silverchain’s palliative care service that has provided generations of Western Australians with access to quality palliative care in their homes.
Since the program began with the State Government and the Cancer Council in August 1982, our service is now nationally and internationally recognised for our outstanding outcomes. According to the Productivity Commission, approximately 70% of Australians would prefer to die at home but only 15% are able to do so.
Our holistic approach provides a gold standard of care to nearly 3,500 West Australians each year. Almost 60% of clients who died were able to do so in the comfort and safety of their own homes.
As a result Western Australia now has the lowest number of palliative care beds per capita in hospitals nationally.

Our innovative service is defined by a dedicated team who provide complete care with compassion and unwavering commitment to our clients of all ages, including babies and children.
Due to the quality of our care, we were voted the most trusted home care brand in the state for 2022.
For more information or to refer our services, please call: 1300 300 122
silverchain.org.au/refer-to-us/western-australia info@silverchain.org.au
Australia won hands down. He arrived in 2004 and embraced the opportunities, allowing him to live the life he had dreamed of.
When he went to work at the Cleveland Clinic in 2013, it was another big victory because he was pleased to have achieved it on merit and without an introduction.
“It was a huge win for me for many reasons – to look back at my parents to see how far I had come from a small seaside village to the No. 1 cardiac hospital in the United States. My parents could take pride in all the sacrifices they made for me now that their son made it to that level. No one can take that away and money can’t buy that,” he says.
In between work and being with his family – Kushwin is married and has a daughter, five, and a seven-year-old son – he very much enjoys gardening. He spends the other part of his time pursuing his passion for philanthropy which focuses on humanitarian aid and climate change action. Kushwin self-finances projects as well as being an active fundraiser while advocating for numerous causes.
“I want to use my energy in the most constructive way and leverage it for the greater good. My purpose is to make the biggest difference possible for the benefit of the generation to come.”
Highly concerned about the world today’s children will inherit, he has independently built schools across Asia, supported clean water and sanitation projects in Sri Lanka and funded several emergency relief operations in Bangladesh and Africa. He recently raised more than $35,000 for the Foundation of Goodness which feeds the hungry by hosting a Sri Lankan culinary and cultural experience dinner.
Kushwin is actively involved in medical missions and travels to Sri Lanka to implant pacemakers in patients living in remote regions with limited medical facilities. In 2019, Rotary International awarded him the Paul Harris Fellowship in recognition of his contribution towards humanity.
One of his urgent priorities is climate change action and because of this, he has partnered with world renowned orangutan expert Leif Cocks, formerly of Perth Zoo, who founded The Orangutan Project. Kushwin is actively raising money for the not-for-profit which has a target of $1 million to preserve 100,000 hectares of Indonesia’s Leuser ecosystem, the last place on earth where critically endangered orangutans, elephants, rhinos and tigers coexist in the wild.
He has pledged to match every dollar the project raises, up to $500,000.

Raised in a very pious home, Kushwin is now much more interested in spirituality than religion. He partners with people and organisations he feels he can trust on philanthropic and charity projects. Using social media to find and network with them, he often works late into the night. He always strives to partner with groups where funds are most efficiently used.
“Humanitarian work can be time consuming and exhausting but I feel energised by the satisfaction that someone, somewhere has been fed, clothed or educated as a result of these efforts.
“I feel generosity is a fundamental duty. We are in the middle of a global existential crisis and it’s critical we take a world approach rather than living totally in selfinterest.”

A fan of simplicity in all areas of life he’s determined to give as many dollars as possible while walking his walk. In case you’re curious, he drives a 10-year-old Holden, which is worth less than $1000.
“My life philosophy is based on compassion and love. We have one life. There is no bucket list for me. What I want to know is that when my time comes, I want to feel that I have given it my all to make this planet a better place.”
Australians are taking to travel again, with vigour. Do we still need to take precautions and if so, what’s the best advice for concerned travellers? Suzanne Harrison reports.
Regular business traveller Christian has done away with COVID-related caution since his first foray into overseas travel earlier this year.
“On my initial trip to US in February, I took all possible precautions, from masks, sanitisers and vaccine boosters,” says the Perth finance professional, freshly returned from another overseas visit.
“Nowadays, I am far less cautious and, dare I say, am back to a prepandemic mindset and routines.”
Lucky for Christian, he is not in a high-risk category. Still, he is one of hundreds of thousands of Australians flocking to the skies, vaccinations and testing requirements checked off. And mostly not for business or family reasons.
In August this year, the Australian Bureau of Statistics reported that holidays were Australians most popular reason for overseas travel in June, with 169,000 returning from short trips overseas.
Jenny Dobak, ABS director of migration statistics, said this was the first time such figures had been seen since the beginning of the COVID-19 pandemic, overtaking visiting friends or relatives.
For those without pre-existing issues and the young and fully vaccinated, it’s understandable that concern has dissipated – it was more than an 18-month ban on overseas travel without exemptions.
Yet for many others, such as the elderly, or those with chronic conditions, there is the lingering question of whether travel is safe when it comes to COVID, or how to deal with the problem should COVID arise. And family doctors now have the extra challenge of being at the frontline of that advice, one that can change rapidly with an evolving situation.

So, what is the best advice to offer now, and what challenge does that represent to doctors, especially as people have become responsible for themselves and are not under any obligation – in many countries – to abide by COVID-related regulations?
It seems the consensus is by all means, go travelling, but preparation is key and precautions need to be tailored to suit, depending on an individual’s state of health and where they are travelling to, a situation that is hardly new, just slightly more complicated, and/or time consuming.
When it comes to the patient, “people should be mindful that they are personally responsible,” says Jaya Dantas , Professor of International Health at Curtin School of Population Health. “Have the third COVID vaccination dose if you can, always carry a mask, take a small hand sanitiser and try to avoid huge crowds.”

Professor Dantas herself always wears a mask on long-haul flights when sleeping, downloads her international vaccination certificate
with the QR code and takes a printout, too, as some countries may not put as much weight into a digital format.
She ensures other vaccinations are also up to date (flu, yellow fever, tetanus, for example); that she is carrying RATs, over-the-counter pain relief, antihistamines and anti-inflammatories, and a few days before flying checks relevant travel websites for any possible requirements or restrictions to the place of travel.
Mask-wearing is still a hot topic. While many favour it, others are glad it is no longer mandatory on flights.
The “great unmasking” as it was called in the press, was launched on September 9 on all domestic Australian flights and international flights to Australia.
In mid-June this year, major airports declared masks optional, with many keen travellers welcoming the news. Flying now, Professor Dantas says she hardly sees any Australians wearing masks domestically, but on a recent flight to India, everyone was wearing one. As Professor Dantas says, “wear a mask if you want to.”

However, for regular Perthbased business traveller and now, overseas holiday maker Andrew,
mask-wearing in the airport – not the plane – has become his go-to when it comes to avoiding COVID.

“I don’t wear a mask on the plane, as most are well ventilated with HEPA filters,” he says. “But at the gate, or in a heavy queue, it’s usually a crowded, locked-in environment, so I am actually more careful in the airport itself.”
As for the need to visit a GP prior to departure, Professor Nick Zwar, chair of the RACGP Travel Medicine Specific Interest Group and based in Queensland, advises that if you are otherwise healthy and travelling to a location such as New Zealand, Central Europe, the US or Canada, then it’s not necessary.
But for those with long-term medication requirements who are older or have a chronic condition, then it’s a good idea.
“Your medical summary should be printed out. That can be very helpful, as is travel insurance.” Professor Zwar adds.
A classic example of how COVID can upend travel even in our postCOVID-peak world is the outbreak
www.miga.com.au/qantas-tc.


reported in October this year on the ship, Coral Princess, on which a number of people were infected. Luckily, with vaccination and rigorous testing in today’s travel environment, this kind of drama unfolds with much less fanfare, particularly as the ship was in Australian waters.
More importantly, how would the traveller be best prepared if they do become infected on such a ship?
One thing to note is that the Australian Department of Health and Aged Care says the Government’s ability to provide consular services or support on board an international cruise ship is likely to be limited.
“Cruise ships are a significant risk for COVID, the flu, diarrhoea, there are a lot of people in a small space and even if they are taking steps to contain it, we’re still seeing outbreaks,” Professor Zwar says.
“So, people need to think how they’d respond. And if they are going on a ship, buy disinfectant, wash hands regularly and wear a mask.
“If you want to reduce your chances of catching COVID – or anything in a confined space – and therefore have your travel uninterrupted, wear a mask, even interstate travel.”
Professor Zwar says only about 40% of Australians visit their GP before going overseas, and there is a tendency for people to think about pre-travel advice at the last minute. “But in our enthusiasm, we have not thought through how things are different now.”
Professor Zwar suggests people simply think potential situations through and be prepared.
As for a reliable website suggestion, he advises checking the US Centre for Diseases and Control and Prevention and in Australia, Smartraveller (www.smartraveller. gov.au/) because they are well-managed and up-to-date, particularly when it comes to areas that should be avoided.
The Smartraveller website provides travel advisories for 178
destinations, with an advice level for updates to its travel advice, general advice before you go, and while you're away – especially when things go wrong overseas –and information about Australia's consular services.
Of course, there is still the issue of variants, which the world will continue to see.
“One hopes that these become less virulent,” Professor Zwar concludes. “But there is no guarantee.”
Amid that lack of guarantee, the RACGP has outlined in the travel medicine document for the 2022 curriculum and syllabus for Australian general practice, that “lots of people won't make a specific appointment for a travel consultation.”
The document suggests encouraging patients to book a long appointment, where possible, and use systems to help them indicate they’re attending for a travel health consultation.
“However, you might only learn about their travel incidentally,” the report states, “at a consultation for another reason, and they may be leaving too soon to book in again. Be prepared to rapidly prioritise travel health strategies in the available consultation time and give patients resources.”
Always talk about travel insurance and what it does and doesn't cover, the document continues.
“Pregnancy and pre-existing conditions are essential to declare. Travel-related risks exist even in domestic travel, as it’s still important to discuss (risks) to destinations in Australia, particularly for trips of longer duration, those to more remote destinations, or for individuals with pre-existing medical conditions.”
This checklist from Smartraveller also makes it easier for travellers:

• Read the general travel advice before you go to help plan to stay safe and healthy. Find out what you need to do if you're travelling with children
• Get a health check and organise your travel vaccinations. Some vaccinations need to be done well before your trip, particularly those that need several doses
• Plan contingencies if you end up overseas longer than expected
• Check with your travel provider. They can help you understand rules and requirements specific to your planned trip.
For the unvaccinated, Smartraveller strongly discourages international travel due to the health risks posed by COVID-19.
“Understand that the risks might be different for you. Airlines and cruise lines may have a vaccination policy that prevents you from travelling with them. You may face more difficulty finding flights.”
For the vaccinated, it may be that – like Christian – it comes as no surprise several US data companies reported the second most Googled search of 2021 was, ‘where’s my refund?’
“High airfare costs and significant flight delays have been the biggest pain points,” Christian says of recent travel. “Initially, it was pre-departure and pre-arrival vaccination paperwork but that seems to have all but disappeared on the countries I’ve been visiting.”
ED: Professor Jaya Dantas is also Deputy Chair, Academic Board, Dean International, Faculty of Health Sciences at Curtin University. Professor Nicholas Zwar is also the Executive Dean, Faculty of Health Sciences and Medicine, Bond University, Queensland.

Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.
Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.
Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.

Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.
Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.
Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.
Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.
Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.
Visit our website to see our range of solutions, as well as offering you a complimentary, obligation-free on-site assessment where we can explore the possibilities.
Visit our website to see our range of solutions, as well as offering you a complimentary, obligation-free on-site assessment where we can explore the possibilities.
Visit our website to see our range
The Long Island
The Long Island
6 Colin Street, Dalkeith
6 Colin Street, Dalkeith
The Long Island
Rod Dawes 0418 941 415 Sat/Sun 1-5pm & Wed 2-5pm or Private Appointment
Rod Dawes 0418 941 415
Sat/Sun 1-5pm & Wed 2-5pm or Private Appointment
atriumhomes.com.au
atriumhomes.com.au
The Edge
Head Office
Head Office
Head Office
Mt Pleasant Ben McCarthy 0402 349 224
The Edge
Mt Pleasant Ben McCarthy 0402 349 224
Private Appointment Only
The Edge Mt Pleasant Ben McCarthy 0402 349 224 Private Appointment Only
Private Appointment Only
Follow us
Willcock Street, Ardross WA 6153
9 Willcock Street, Ardross WA 6153
Willcock Street, Ardross WA 6153
9 Willcock Street, Ardross WA 6153
enquiries@atriumhomes.com.au Ph: 6310 8888 Fax: 6310 8889 A/H: 0418 941 415

E: enquiries@atriumhomes.com.au

enquiries@atriumhomes.com.au Ph: 6310 8888 Fax: 6310 8889 A/H: 0418 941 415

Ph: 6310 8888 Fax: 6310 8889 A/H: 0418 941 415

E: enquiries@atriumhomes.com.au Ph: 6310 8888 Fax: 6310 8889 A/H: 0418 941 415

Find us on houzz.com
Scan to read
*Conditions apply. BC # 13344
Sedentary lifestyles with improper nutrition, an ageing population, increased obesity and declining mental health – the world’s population is facing a multitude of health risks that are both emotionally and financially costly.
Scientists and policymakers are seeking ways to address these risks, with innovative approaches providing valuable tools to address the health of our society.
The positive effects of travel and tourism have been researched and understood for decades. However, researchers are now becoming more creative in applying these known positive effects to health and wellbeing.
The World Health Organization reported that the global life expectancy has increased by six years since 2000, and the proportion of people aged 65 years and older is projected to double by 2050.
The list of health problems associated with ageing is long –diabetes, cardiovascular disease, cancer, depression, dementia and Alzheimer’s disease, while mental health is considered a global health concern for all ages.
People with mental health conditions die prematurely, suffer discrimination and can have challenging relationships. The WHO estimates that the global cost of anxiety and depression, two common mental health conditions, is equivalent to US $1 trillion annually.
Obesity, which contributes to cardiovascular disease, diabetes and some cancers, has been identified by the World Health Statistics 2022 bulletin as increasingly affecting children, adolescents and adults.
But how can tourism make an actual difference to these complex health conditions?
It is helpful to understand some of the known positive effects of tourism. For one, most tourism experiences require some level of physical activity to access and enjoy a destination. Increased physical activity can improve brain activity and lower risks for diabetes, cardiovascular disease, anxiety, depression and obesity.
On another level, tourism activities elicit positive emotions including joy, gratitude, serenity and love. When positive emotions dominate, negative emotions, including anxiety, sadness, and despair, tend to be quieter.
Social interactions are an inevitable part of tourism experiences, and positive social interactions stimulate the brain and are good for overall mental health. The sights, sounds, smells and tactile experiences of a new location all provide mental stimulation, known to reduce the risk of dementia-related diseases.
The act of “tourism” can be as simple as a museum tour or as elaborate as a week-long beach vacation. Exploring a new park is another way to experience the benefits of tourism.
Our multidisciplinary team of ECU researchers from both
tourism, marketing and medical sciences proposed that tourism could be included as a treatment intervention for dementia patients. Mental stimulation, sensory experiences and increased activity are all known interventions for dementia – why not use tourism to deliver these benefits?
Unfortunately, physical and mental disabilities, along with world health crises such as the COVID-19 pandemic, can be barriers to travel. Tourism researchers have been exploring the use of virtual reality (VR) tourism to bring destinations to travellers. VR tourism could enable nursing home residents with dementia, or those who may have mobility issues, to enjoy some of the benefits of tourism without the need to physically travel.
These virtual tourism experiences would still provide mental stimulation, positive emotions, and allow for social interactions with caregivers following the experience.
It will take a pioneering spirit to provide solutions to the growing list of global health concerns. Multidisciplinary research has great potential to propose creative applications of known theories to benefit the population.
In spite of the concerning state of global health, we are at an exciting time where researchers are coming together in the name of a shared passion for the greater good. Let’s keep an open mind and see where these pioneers might take us.

ED: Dr Jun Wen is a lecturer in tourism and service marketing at the School of Business and Law, Edith Cowan University. He researches global health, tourism marketing and travel medicine.
Dr Danni Zheng, Fudan University, China; Professor Haifeng Hou, Shandong First Medical University, China; Professor Ian Phau, Curtin University; and Professor Wei Wang, Edith Cowan University, contributed to this article.

The pandemic broke down some resistance to the use of My Health Record by consumers and practitioners. The challenge is to keep that momentum going.
Eric Martin reportsAustralian governments and many healthcare providers have prioritised digital health as key to improving service delivery and health outcomes, yet with the surge of online information during the pandemic, much of that development seems to have bypassed the very system it was supposed to serve.
My Health Record was touted as “an unprecedented platform for innovation in the provision of digital apps and tools that will support Australians and their health providers to improve health and wellbeing.” But six years and more than $2 billion later, the system is still struggling to reach its full potential.
As the looming end-of-2022 deadlines for its first objectives approach, Medical Forum spoke with the RACGP’s Dr David Adam, the Australian Digital Health Agency (ADHA), and Professor Jaya Dantas, of Curtin University to explore some of the issues impacting My Health Record.
“There has long been an expectation from patients that all the services across Australia should be digitally connected, and I certainly have patients who expect me to be able to share my record completely with another doctor at another practice,” Dr Adam said.
“But I think the community awareness of what My Health
Record (MHR) allows is still limited – I have not seen a huge increase in the number of patients who report that they have accessed their own information through the system.”
Professor Dantas explained that MHR was a rebranding of the original digital healthcare system launched in 2012, which had only managed to attract about four million people over four years. The ADHA was established in 2016 to lead the development and implementation of MHR.
“Co-ordinated research, including intervention studies and pilot programs, was undertaken by the agency not only to drive innovation and increase uptake, but also identify the challenges,” she said.
The National Digital Health Strategy established that by the end of 2018, every Australian would have a MHR, unless they choose not to, and by 2022, people would be able to access their health information online at any time, with every health-care provider able to communicate with other professionals and their patients via secure digital channels.
“But unfortunately, as you know, and as most of your readers will know, that's a nice idea, but it doesn't really exist,” Dr Adam said. “However, what I will say is that My Health Record is certainly becoming more useful on an almost monthly basis.
“Our practice has been connected to the My Health Record system for a long time, but in the last 12 months
The architect of federal public service reforms, David Thodey, will lead a user audit of the newly relaunched myGov portal in a move that could lead to the government’s multiple services and brands finally being consolidated into one website and app.
The user audit was promised by Government Services and NDIS Minister Bill Shorten ahead of the election campaign and comes after the portal was relaunched recently.
Mr Shorten has appointed former Telstra CEO David Thodey to lead a panel overseeing a user audit of the myGov system, which links Australian residents to
we've seen the biggest degree of improvement, where it has just become so much more useful.
“For example, the integration with the Australian immunisation record was always a bit hit and miss because the Australian Immunisation Register itself was patchy and there was no requirement for anyone to upload records to it - you were never sure that there was a complete picture,” he said.
“But now that all vaccines must be uploaded, particularly COVID and influenza vaccinations, having access to the immunisation register through My Health Record is much easier than using the register directly.”

COVID has been the biggest driver of Australian’s uptake of MHR and, in January 2022, Acting ADHA CEO Paul Creech said more and more Australians were using the system to help manage the impact.
“COVID test results come from pathology providers and the majority of pathology providers in Australia routinely upload test results to My Health Record,” Mr Creech said. “We’ve seen huge demand since last July, with more than one million views a month by consumers across Australia.”
People could see their COVID test results as soon as they were uploaded to MHR often faster than they would have received an SMS. The dashboard was also updated at the beginning of 2022 to include vaccination details and test results,
Medicare, the My Health Record, My Aged Care and the National Disability Insurance Scheme.
Mr Thodey will report back to the government by the end of the year.
“The current two-year program for improving myGov ends in mid-2023 and the audit will help to inform the next steps for the upgraded myGov platform,” said Mr Shorten, who has made it clear he wants myGov to be the portal for all federal and state services.

medical conditions, relevant medicines, and allergy information, as well as links to the vaccine clinic finder and side-effects checker.
The AHDA stated at the time that each month more consumers were viewing their own information, with nearly 13.75 million COVID-related documents viewed in January 2022, and a 580% increase in pathology views by consumers from 2020-21.
“For researchers and population health experts, COVID has highlighted the immense need for tele-health and digital health and the information and benefits this provides. Globally, there is increased use of digital technologies to provide better health care,” Professor Dantas said.
“The past 12 months has indicated an increased use of My Health Record by Australians - there are 23.3 million records as of June 2022 and 22 million have data in the records.
“The current statistics indicate that 99% of pharmacies and GPs are registered and have used health care records, 97% of public hospitals are registered and 95% have used My Health Record.”
However, from the January peak of 13.75 million, the number of Australians accessing MHR has dropped alongside concerns about COVID, with figures from June showing that only 4.99 million people retrieved their data – much closer to the monthly average.
“I'm always careful about drawing too many conclusions from that number,” Dr Adam said.
“My experience is that for almost everyone who has a record, yes, it does contain some information, but almost all of that is pulled from automated systems. It's Medicare data, immunisation data, PBS data and I'm not sure that accurately reflects the number of people who are actually engaged with the system.
“One of the main goals of My Health Record was to have patients more empowered and have more
understanding of their health care information, but I haven't seen that translate into real life yet in any kind of significant way.”
Dr Adam attributed this observation to the fact that the information in MHR, although improving, still suffered from the patchwork nature of its implementation.
“We have certainly seen a lot more of the local labs start uploading information to MHR rather than posting patients copies of their results, but all the private radiology firms have their own patient portals and patient systems, and many of the lab providers do as well,” he said.
“We have two parallel ways of doing the same thing, one of which is duplicated many times.”
However, progress could soon be made in addressing this hurdle with the announcement on August 24 this year that ADHA had signed a deal with Health Level Seven Australia Ltd (HL7) to develop specific digital health standards and specifications to improve connectivity – Fast Healthcare Interoperability Resources (FIHR).
Agency CEO Amanda Cattermole said the ADHA’s partnership with HL7 would have a direct impact on consumers gaining better access to their health information.
“Put simply, FHIR is the how-to guide that enables health information movement from one place to another, a freely available and nationally endorsed

interoperability standard,” she said. “The agency and HL7 recognise that different parts of the health system are at different points in the digital journey. The long established V2 and CDA standards are widely used, and these will continue to be supported during the transition to FHIR.”
“One of our priorities through the partnership is to more clearly communicate requirements for standards for national acceptance across public and private health and social care.”
Professor Dantas said it was well known that one of the main reasons My Health Record had initially struggled to gain traction was concern for the safety of information shared by Australians. However, trust in the system’s privacy standards had increased.
“We know that about 2.5 million Australians had opted out of the My Health System before the cutoff date in 2019 even though the government had assured people of the security and safety their data,” she said.
“Yet out of the 2.5 million, 240,000 have now registered for the record. Patients know that My Health Record is a safe and secure site. However, the next step would be to have simple information in different languages and for population groups who have low literacy.
“We also need targeted public awareness of the need for the My Health Record and how it can assist us to manage our health, with
information provided to our GPs, specialists, pharmacies, and other providers.”
Dr Adam explained that one of the reasons doctors may still be wary of fully embracing the system could stem from the historical approach to protect patient confidentiality.
“Many of us have concerns about information, privacy, and security. I personally have a lot of trust in the My Health Record system from a confidentiality and privacy point of view. But I understand that this is my view, and it is not one that all my colleagues necessarily share,” he said.
“I think some of us are still holding onto the model that our notes are our property: we know we make them, that the patient always has full access to them, except under very limited circumstances; but I think there are still people who would not feel comfortable with everything they write in the notes being seen by other doctors, or by patients themselves.
“I also think there are still a lot of people who have questions and concerns about it, even though the
number of people who originally opted out is relatively small, and unfortunately, many of my patients who would get the most benefit out of something like My Health Record, are also the ones concerned about other people accessing their information.

“I understand, and I respect that decision. But, for example, it is much harder to check what dose of drug was administered at another practice – we have to call their pharmacy like we used to do.”
Both he and Professor Dantas also lamented that there was no mechanism to effectively address the necessity to manually enter and upload data, with Dr Adam pointing out the potential for patient misunderstanding between the 15-minute consultation time and a bill showing 25 minutes.
“I generally try to do most of my administration with the patient in the room because they know what's going on and they know what's happening about them,” he said.

“The fact that adding information to a patient's record is considered Medicare billable time was
something that the RACGP lobbied really hard for, and I think it has definitely helped.
“The problem more generally is that bulk billing for most practices is no longer sustainable, and GPs need to think about ways of streamlining access.”
“The billable time is a real issue and does impact not only uploading data but also patient consults and interaction. It is an acknowledged problem but there seems to be no movement to address this,” Professor Dantas said.
“The business or corporate model of billable time used by the government is another issue.”
Dr Adam said that he does emergency public work as well as general practice and the MHR proved its usefulness.
“When people have a good summary in their My Health Record, that is hugely helpful, and we certainly rely on it – thank you to everyone who has been working to keep the records up to date.”
•
As floods continue to inundate communities across Australia and other regions face drought, the medical profession is increasingly taking up the call to arms on climate change.

Last month, a coalition of peak medical bodies and experts warned of mounting pressure from climate change-related health impacts on strained healthcare systems.
This followed the release of the 2022 report of the MJA-Lancet “Countdown on Health and Climate Change”, from a multi-disciplinary research group that conducts annual check-ups of Australia’s progress in tackling climate change and its health impacts.
The review found the health of Australians was being jeopardised by increasing exposure to extreme fire danger, life-threatening heat and severe drought, and more people were being displaced by weather-related disasters.
Macquarie University’s Associate Professor Paul Beggs, who led this year’s report, said Australia’s health system capacity had also deteriorated over the study period.
“In this year’s study there’s a very concerning combination of findings for Australia – increasing climate-related health threats and indicators of reduced health system capacity,” he said.
“We found numerous mounting risks to Australians’ health from fires, floods, drought, and heat and, worryingly, we also found that, for the first time since we began tracking, Australia’s health emergency management capacity has fallen.”
Professor Beggs welcomed the Federal Government’s recent budget commitment of $3.4 million over four years to develop a national climate and health strategy and set up a National Health Sustainability and Climate Unit, but he said more urgent action was needed.

In response to the MJA-Lancet report, several medical groups, including the Australian Medical Association, the Royal Australasian College of Physicians, the Public Health Association of Australia and the Australian Medical Students’ Association, called for policy measures to help safeguard human health from climate impacts.
Key recommendations include developing health and climate change plans at all levels of government; more consistently aligning government energy policies with the goals of the Paris Agreement; and incorporating environmental sustainability principles in an upcoming update of the Australian Dietary Guidelines.

AMA president Professor Steve Robson said Australia was seeing poorer health outcomes from increasing climate disasters but there was still time to mitigate the worst impacts of climate change for the next generation.

“I ask policy-makers to read this report and to act urgently on its recommendations,” he said.
Meanwhile, Doctors for the Environment Australia argues that climate change knowledge must be included in medical education.
It has helped to launch a new teaching resource – developed in collaboration with medical students and staff – to connect the dots between foundational medical learning and the clinical effects of climate change.
The DEA believes the medical workforce needs to be educated on ways to mitigate the health effects of climate change, and that these lessons need to be integrated at all levels of medical education.
The ‘planetary health organ system map’ is a new teaching tool that integrates the pathophysiological consequences of climate change into the classical organ-systems based medical curriculum.
Developed by members of DEA from the University of Melbourne, it connects planetary health – or the health of human populations and
the natural world upon which this health depends – with patient care in a way that ensures the concepts are clinically relevant and can be translated into day-to-day practice.
The map also emphasises the positive health co-benefits to patients of environmentally sustainable health care.
Chair of the DEA Dr John Van Der Kallen said everyone working in health, especially doctors, needed to be aware of the links between the environment, our changing climate and health.
All medical educators, including those at medical school, prevocational teaching hospital and medical specialty college levels, were being urged to incorporate the resource into their curricula.
Those interested can contact the DEA at admin@dea.org.au.
On behalf of the Doctors and staff at SKG Radiology, we thank you for your continued support throughout the year and wish you and your family a safe and happy festive season.

COVID-19 has highlighted the issues that international merchant seafarers face when receiving health care in Australian waters. Over the course of the pandemic, the International Maritime Organisation estimated 400,000 seafarers globally were stranded on ships that were unable to be repatriated due to border restrictions.
While restrictions have now been lifted, secure border operations in Western Australia imposed barriers to receiving timely care during this period.
For those working in our northern regional hospitals, many of the issues seen pre-dated the pandemic. Doctors in port cities such as Karratha, Hedland and Geraldton frequently attend to the medical needs of these individuals who work one of the most hazardous jobs in the world.
Access to reliable primary care services is limited during months at sea. Between 2005 and 2012 the Australian Transport Safety Bureau recorded 245 incidents resulting in seafarers being seriously injured or dying. Furthermore, language barriers and limited finances make it less likely for these patients to seek appropriate care early.
Information provided regarding previous international ports visited and past medical history is commonly scant, and patients may present with more severe illness than previously communicated. Occasionally, cases such as meningitis, which may provide chemoprophylaxis of crew members, a difficult task if a berthed vessel has departed. Practitioners witness instances of inappropriate self-care or symptom minimisation as patients may feel workplace pressures regarding the implications of accessing health care via their employers. Often these individuals support several family members and without
access to sick leave have little or no financial surety.
West Australians reap great benefit from our minerals and resources sector, which relies heavily on these contractors to carry exports offshore. It might come as a surprise to know they are still not recognised as essential workers by the Australian Maritime Safety Authority.

Crew are isolated and operate in small teams away at sea together for prolonged periods. Seeing the psychological impact that an unexpected death and illness has on colleagues, has led to some charitable organisations providing support for those in crisis.
Despite this, medical care remains fragmented enroute to Australia and there have been instances of delayed presentation of malignancy and serious preventable illnesses. With stopovers commonly lasting less than 24 hours, rural clinicians are troubled with the dilemma of how to provide treatment according to Australian standards of care as the follow-up of investigations is difficult.
Increasing the awareness of the
challenges faced when assessing and treating these vulnerable patients will help us work together to treat these individuals with respect and dignity. They are vital to our economy and greater resources could be provided by corporations alongside structured recommendations for care by health-care regulators.
Some suggestions that could help include:
• Mandatory information collected for patient encounters including ports visited, immunisations, occupational screening, correct contact details and a best possible medication history.
• Digital live video translation services to improve history taking and communication when non-English speaking patients are in our hospitals.
• Nominating a contact within each shipping agency for the communication of medical results and the safe transmission of personal information compliant with privacy legislation.
• A national ‘seafarer safety net’ using private industry funds to assist with the costs of sight, life or limb threatening interventions within the Australian health system.
• Open-access electronic medical record software that can be easily utilised by vessels with limited internet connection interfacing with Australian digital services. This may allow an Individual Healthcare Identifier to create non-resident MyHealthRecord data for patients who frequent various Australian health care facilities.
Read this story on mforum.com.au


Three WA organisations have taken out all the finalist places in the 2022 HESTA Excellence Awards for outstanding community services.
In total, 24 organisations and teams from around Australia were named finalists for their work in the categories of disability, allied health, aged care and community services.
In the category of community services, St Patrick’s Community Support Centre in Fremantle was recognised for its programs and services supporting families and individuals facing complex challenges. Library Connect, the first of its kind in WA, places a support worker within the welcoming environment of the public library, improving access to support for families and individuals and reducing stigma.
During COVID, St Pat’s delivered 35,000 meals as part of the Doorstop Diners program, ensuring people experiencing disadvantage or isolation had access to nutritious daily meals and support services. Their ‘20 Lives 20 Homes’ Fremantle pilot program had a 76% success rate in supporting people to not only secure but maintain permanent housing.
The second finalist in the category was Women’s Health & Family Services in Northbridge, recognised for its commitment in providing connected health care for women. Until 2021, there was no single client information record that could be shared between their primary care providers, counsellors and family and domestic violence advocates.
The team addressed this issue by implementing a cloud-based primary software, so all practitioners could access case notes. Now
clients do not have to retell their story or history as they move between programs within the organisation, which helps provide a more holistic service.
WHFS plan to deploy a client portal, embedded into the organisation’s website, where clients can self-refer and book appointments with the team.
The third finalist, Zonta House Refuge Association, was recognised for its work providing support and opportunities for victims and survivors of family and domestic violence, from prevention to crisis response to recovery, redress and rebuilding.
In the category of team excellence in aged care, Brightwater Care Group’s Falls Improvement Program Team was a finalist, recognised for identifying and
implementing evidence-based strategies to reduce fall rates, better support aged care residents and improve overall knowledge gaps. The program provides professional development and educational sessions for staff to minimise risks and hazards.

The team also introduced weekly exercise sessions for residents to help prevent falls and hosted zoom chair yoga sessions in 2022. The program saw a 28% decline in fall rates within six months.
A WA finalist in the category of team excellence in allied health was the Baby Play Academy Team at Western Kids Health, which was recognised for going above and beyond to empower parents to support baby development.
When COVID hit, Western Kids Health was inundated with messages from anxious parents concerned about their baby’s growth. To address the lack of accessible and affordable support and information for parents, the team developed the Baby Play Academy.
The academy is an online education and support pathway for parents and caregivers, combining digital resources, community forums, telehealth consultations and referrals. The team spent a year creating video and written content covering infant motor, language, social and cognitive skills development.
The academy has since grown to support over 2000 members, improving parent knowledge, skills and confidence. The team also uses Instagram to support parents all over the world, with over 130,000 followers.
Warmest greetings of the season, best wishes of health & happiness for 2023 to all our referring doctors, colleagues & their families. We appreciate your continued support & look forward to working with you all in the New Year to mutually care for the health & wellbeing of our patients.

Best of health
Marek Garbowski & Perth Vascular Clinic Team




Perth Vascular Clinic is WA’s leading vascular solutions centre. We offer state of the art management & treatment of conditions affecting vascular health, with convenient access to rooms based minimally invasive vascular investigations and treatment.


Dr Marek Garbowski is a qualified, highly experienced vascular & endovascular surgeon in all aspects of diagnosis and management of arterial & venous diseases, specialising in:
Comprehensive assessment & patientoriented best medical & surgical management of all vascular problems
Open and Endovascular management of Peripheral Vascular Disease, Aneurysms & Carotid disease
Endovenous management of Pelvic Congestion Syndrome
Thoracic Outlet Syndrome surgery
Varicose Veins – primary & redo surgery and minimally invasive treatments: Radio Frequency Ablation (RFA) & Sclerotherapy Leg ulcers & diabetic foot problems
All aspects of vascular and dialysis access
Hyperhidrosis: Thoracoscopic Sympathectomy & miraDry
In my time working in the disability sector, recruiting carers in Perth has never been more difficult. The tight labour market has meant finding new carers is a real challenge, but also know there are people considering a career change that will give them real personal satisfaction. Caring more than fits that bill.








I would never sugar-coat it – it can be tough at times – but the people who are cut out for it would never think of doing anything else. It’s a job where you can genuinely change someone’s life for the better and deliver a real and tangible benefit to the WA community.
Anyone sick of the sight of their computer screen and longing for a job that gets them up and about should consider caring, which by its nature involves real human interaction
There are also low barriers to entry. While there are certain skills that make someone a good carer, like being observant, diligent, empathetic and organised, the qualifications and certificates required can be achieved relatively quickly.
Many opportunities also present for career progression. Being an effective carer stands you in good stead to take on many other roles,
train other carers, look at systems and processes and move up the salary ladder.
A lot of people see caring as ‘just a job’, with a static salary, but it can be a profession or a career that leads to managerial roles.
There is a gap in the quality of care between what is offered by the NDIS and what anyone living with a disability truly deserves. Our entire mission is based around filling that gap, and supporting our carers is integral to that.
ED: Andrea Cooper is the CEO of disability support service New Chapters, New Beginnings.

Amid acute workforce shortages, more people should be encouraged to consider caring as a career, says disability support service CEO Andrea Cooper
If you had to choose between a neurological disorder or cancer, which would you choose?
Both are increasing prevalent and burdensome, though one is much easier to navigate through the health system than the other. Cancer often comes with a clearcut diagnosis, encouraging research and statistics offering hope for recovery, a well-worn and effective care pathway and well-funded wraparound physical and mental health services.
The neurological journey is typically stagnated, frustrating, lonely and sometimes terrifying. With over 600 – mostly rare – disorders of the brain, spinal cord and nervous system, each affecting sufferers in widely varying ways, neurological conditions are comparatively complex, far less understood and more difficult to diagnose, traverse and treat.

Conditions can be:
• Episodic or recurrent, such as migraine and epilepsy
• Stable with changing needs, such as cerebral palsy, fibromyalgia and Tourette syndrome
• Progressive and incurable, such as dementia, brain or spinal tumour, Parkinson’s and motor neurone disease
• Sudden onset stemming from an isolated neurological incident, such as meningitis, stroke or other brain or spinal cord traumatic injury.
Neurological conditions carry a significant burden. In 2017, 10.9 million Australians were living with a neurological disorder, causing 33,000 deaths and 608,000 Disability Adjusted Life Years per annum, at a cost of $30.5 billion a year. The numbers are staggering, yet neurology continues to be a neglected specialty and poor investment in neurological health is failing to meet the needs of this growing patient group.
New to my role as CEO of the Neurological Council, the service gaps and health care navigation difficulties are clearly visible. Our Neurocare community neurological nurses navigate these challenges, roadblocks and dead ends when supporting patients to find:
• Lack of neurological specialists resulting in long appointment wait times
• Lack of local accessibility requiring most patients to travel to metro hospitals and clinics
• Lack of ‘one stop shop’ hub or online information, education or service directory
• Debilitating neurological symptoms not treated because of ‘unrecognised conditions’ such as functional neurological disorder, Lyme disease and post-COVID
neurological syndrome
• Availability and affordability of basic home care services due to worker shortages, lack of regional providers and inflated NDIS and My Aged Care (MAC) pricing
• Affordability of necessary allied health therapies including neuro-nursing, neuropsychology, exercise physiology, physiotherapy, occupational therapy, speech pathology and social work, with inflated NDIS and MAC pricing and ‘token’ interventions

• NDIS decision makers routinely rejecting neurologist and functional capacity reports
• No NDIS for over 65s, MAC means tested and capped at $56,000, and those in residential
Do neurological conditions have a care pathway or is it a road to nowhere, asks Neurological Council of WA CEO Etta Palumbo.
aged care deemed not “living in the community” or “double dipping” if they need specialised disability care
• WA neurological not-for-profits struggling to deliver sustainable services, supplemented by patchy, disease specific support groups that rely on donations and volunteers, who are themselves often carers or sufferers of a condition.
With limited options, patients and carers shoulder most of the burden, typically spending only a few hours each year in contact with clinicians and trying to self-manage their symptoms or decline the rest of the time, until a health crisis.
With pressure on our hospital system, we must invest in a co-designed, sector-wide approach to effectively manage neurological conditions. Patients need funded or affordable services at varying levels of intensity, which they can access according to their needs and disease progression.
Pathways need to range from self-care, community interventions with specialist input, through to complex and rapid access emergency care.
To improve the neurological patient’s experience and outcomes and liberate scarce health resources, we need a model of care that is:
• Person-centred with a written care plan built around the individual’s needs, priorities and wishes for managing their symptoms or condition
• Cognisant of psychological and cognitive impacts and concurrently supporting mental well-being
• Proactive with educational, preventive, maintenance, and restorative components

• Community-based delivered near to the patient, in the community or at home
• Multi-agency and multi-sector with a unified, integrated, and well-coordinated approach, and timely and effective interagency, GP and patient communication and movement through care pathways
• Utilising and training GPs and community neuronurses to support patient pre-screening, assessment administration, care plan implementation and support, and health monitoring and maintenance between appointments
• Practical and accessible including a clinically trained general neurological helpline, community neurological nursing and allied health non-emergency response team and respite options for all ages
• Embracing new technology to digitise information, support, assessments, and data collection; connect a multidisciplinary care team and use smart devices to monitor and drive timely care according to needs
• Facilitating access to disability funding for people with neurological disabilities, regardless of age with ringfenced packages for rapidly progressing and sudden onset conditions to prevent default premature entry into residential care.
In an ageing society where neurological conditions dramatically increase with age, if not now, when?
By Mr Peter Ammon Foot Ankle & Knee Surgery


St John of God Medical Centre
Suite 10, 100 Murdoch Drive Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au
Murdoch Orthopaedic Clinic Pty Ltd ACN 064 146 774 ABN 23 070 745 210
Pre-COVID, the loss of smell was often dismissed as a trivial medical complaint. But an expatriate Italian-Australian living in the UK is helping to rewrite the textbook on anosmia.
By Cathy O’LearyJournalist Paola Totaro remembers being puzzled at smelling nothing from the fragrant hand moisturiser she used every day in her London home. That feeling turned to panic when even the ammonia-based toilet cleaner yielded zero response at nose-level.
It was March 2020, and she was about to find out she had COVID and would be one of millions of people around the world to suddenly find they had lost their fifth sense, seemingly overnight.
Her experience trying to recover her ability to smell would take many months and include ‘smell training’ to rewire the brain to recognise smells, both pleasant and otherwise.

With her co-author husband – former WA journalist turned author Robert Wainwright –Totaro has put pen to paper to enlighten people – including GPs – on the huge impact of losing the ability to smell in the book On the Scent
“Locked down at home in London, I could smell nothing of my domestic world either, which made life feel alien and flat,” she writes. “In normal times, walking the dog each day is a stop-start affair (much to my husband’s irritation) because I revel in slowing down and inhaling the smell of the outdoors, whether it is freshly mown grass, the heady scent of cherry blossom, new eruptions of daffodils or the first sprigs of climbing rose. Flowers without scent felt like a cruel mockery, their beauty visible but lacking the dimension I love most.”
She felt bad complaining when people were dying of COVID but “the few pleasures left during lockdown – food, booze, the outdoors – had lost their joy.”
“At the dinner table, red wine tasted like salty water, white wine like a mild, odourless vinegar. My favourite aperitif, gin, was barely perceptible in the overwhelming, cloying sweetness of the tonic. “Steak felt like biting into a slab of flabby leather, chicken a horrifying, bony, rubber, while dark chocolate, my favourite, tasted like unscented soap.”
Wainwright takes over the narration, briefly, to describe the devastation he saw when his wife –their household’s chief sniffer – lost her sense of smell.
While initially motivated to investigate anosmia out of self-interest, Totaro was also journalistically intrigued by this ‘Cinderella’ sense, soon learning of the interplay between our senses of taste and smell, with the process of tasting starting when we first chew our food, with the true flavour coming from the chemical mix of odours released.
On the Scent covers in entertaining detail how the olfactory system works, and how devastating it is when it stops.
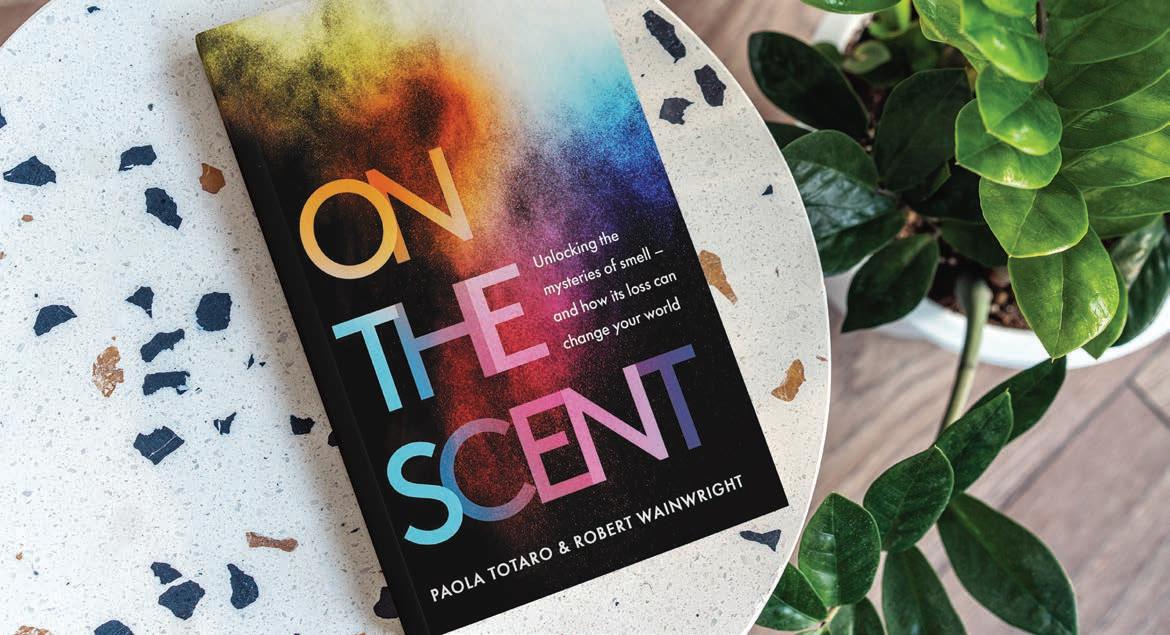
Totaro explains that from the moment we take our first breath, we inhale and exhale around 22,000 times a day, flooding our olfactory system with odours.
“The outside world can tell us immediately if our room smells musty or our clothes need a wash; if the baby’s nappy needs changing or the jasmine outside is in bloom,” she notes.
Totaro has interviewed some of best olfactory specialists in the world such as Aarhus University’s Professor Alexander Fjaldstad, a specialist physician and co-founder of Denmark’s first outpatient clinic for taste and smell disorder, one of many to explain that smelling is as much about the brain as the nose.
He likens the process to a program or app running on a laptop or smartphone. Smells have a direct shortcut into the part of the brain that relates to ‘liking’ and pleasurable appreciation but also, importantly, to ‘bad’ smells.
In the course of her journey to recovery, Totaro explains how she learnt there was no quick fix from anosmia, and it took months of retraining for familiar scents to return. Smell training is like learning a new language.
Totaro discovered that her father, Paolo, had also lost his sense of smell, many years before he was eventually diagnosed with Parkinson’s disease.
She ponders whether her father’s olfactory loss might have been a red flag missed
by the GP at the time, citing solid research suggesting smell loss is often a very early symptom of Parkinson’s.

Totaro argues the case for smell testing to be incorporated into routine health checks as part of a measure of overall physiological and emotional wellbeing, perhaps at the GP surgery, particularly if a patient presents with a smell or taste concern.
She makes a strong case for smell being the poor cousin in medical research labs for too long, only now changing because of the big number of cases of anosmia fuelled by COVID.
“If there is a silver lining to this terrible chapter in modern human history, it is that it has forced a reevaluation of our sense of smell,” she concludes, “not just for its importance to our quality of life but as a powerful sentinel and hitherto unsung surveillance system that when properly read can tell us so much about our physical and mental health.” On




8 billion people on earth and no two are identical, meaning there is never a one-sizefits all approach in medicine – even if the government wants it.
Dr Joe Kosterich | Clinical Editor
Time supposedly speeds up as one gets older. This year has flown by, and this opinion seems to be held across all age groups. Maybe it is the hangover from the pandemic, maybe for doctors (at least) it is the ongoing pressure from all directions and maybe time is actually speeding up.
For most, Christmas is a time of celebration and this year, for the first time since 2019, families will be able to reunite across state borders and the world. New year is a time for setting goals, and many may be seriously reflecting on their priorities and how they want to invest their time. Nobody on their death bed regrets not spending more time at the office.
The holidays are also a time to relax and catch up with reading. Substack has many excellent writers and is worth exploring. Check out Dr Vinay Prasad and Sensible Medicine
Biologist Luana Maroja wrote on common sense (Substack), the loss of academic freedom and ability to do research in certain fields, and notes “the dangers of closing off so many avenues of inquiry is that science itself becomes an extension of ideology and is no longer an endeavour predicated on pursuing knowledge and truth.”
California has legislated against doctors diverting from the government line. Closer to home, Queensland has passed legislation which is not dissimilar. There are 8 billion people on earth and no two are identical, meaning there is never a one-size-fits all approach in medicine – even if the government wants it. Penicillin is first line treatment for bacterial tonsillitis, but to a person allergic to it, the harms outweigh the benefits.
The lessons of allowing incremental reduction of freedom in society and excluding “the other” must never be forgotten. Senior SS officer Reinhard Heydrich said in 1938 “Asocial elements are defined as people who show their hostile attitudes to society, even if they are not criminals, that they do not want to integrate into the community.” Who gets to define ‘asocial’?
Ronald Regan observed that freedom is only ever one generation away from being lost and must be defended. The ability of doctors to do what is best for the patient in front of them and not be a government functionary must be defended for the next generation of doctors and patients. This is our responsibility.
A big thank you to our readers, and those doctors and health professionals who have taken the time out of their busy lives to share their knowledge with us.
Wishing you a very Merry Christmas and a happy New Year.
There are
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Hypertension affects around one third of the adult population in Australia and represents the leading modifiable risk factor for major adverse outcomes such as coronary heart disease and cerebrovascular disease globally.
To put this into an Australian context, elevated blood pressure (BP) alone is responsible for 43% of coronary heart disease, 41% of stroke, 65% of the burden of hypertensive heart disease, 38% of chronic kidney disease, 32% of atrial fibrillation and flutter and 3.6% of dementia.
While these numbers should not deter from the valid concept of overall cardiovascular risk assessment as the basis for clinical management, they do highlight the importance of frequent and accurate BP measurement and the relevance of adequate BP management in line with the latest evidence.
Lowering of blood pressure by any means is one of the most effective health interventions that can be achieved by lifestyle modification, guideline-based pharmacotherapy including early combination therapy, and interventional approaches where required, representing three major pillars of hypertension management.
Indeed, a recent meta-analysis based on individual participantlevel data from 344,716 participants demonstrated that a systolic BP reduction of 5 mmHg is associated with a 10% reduction in major cardiovascular events. This was irrespective of the baseline BP level and evident in both patients with and without previous cardiovascular disease.
Based on these findings it would seem logical that controlling BP is a priority on the national health agenda.
However, we are far from it, with recent data demonstrating that only around 50% of Australians with hypertension are aware of the condition, and only 32% of patients
Hypertension is the leading modifiable risk factor for major adverse health outcomes
Blood pressure control rates in Australia remain unacceptably low
A national concerted effort is required to curb the enormous burden of hypertension.
with treated hypertension achieve adequate BP control.
Economic analyses suggest that adequate treatment and achieving control of BP in patients currently living with hypertension would save 83,000 lives over the working lifetime and save $91.6 billion in Gross Domestic Product. Hypertension remains a neglected priority.
The High Blood Pressure Research Council of Australia (HBPRCA) has been at the forefront of research into the causes, prevention and treatment of high blood pressure since its inception in 1979. Its members are among the national and international leaders in the field of cardiovascular research and have contributed substantially to the national and international literature.
While discovery and clinical research are critical to identify novel treatment options and provide robust trial evidence to inform guidelines and clinical recommendations, research alone is insufficient to curb the burden that hypertension poses on the Australian society.
The HBPRCA Executive Committee in 2020 set out to create a national entity that would focus on all aspects of hypertension with the mission of “advancing health through the prevention, detection and control of high blood pressure and its complications”. It aims to work with leading minds across all relevant medical and health disciplines and consumers to advance research and education
and to engage policy makers to ensure all adult Australians will be screened for elevated BP and receive adequate support to avoid the potentially deadly complications of hypertension. After surveying the membership of the HBPRCA, it was agreed to transition to the new entity named Hypertension Australia, which will be launched officially on December 8 at the HBPRCA Annual Scientific Meeting.
Hypertension Australia aims to deliver its vision of “Australians having the best-managed blood pressure in the world” by striving for excellence in several core areas including:
• Research: knowledge generation through discovery and innovation, and translation into practice
• Education: knowledge translation by turning policy and discovery into practice
• Implementation: Translation of research and education into practice
• Development of guidelines and position papers
• Advocacy: Creating supportive environments through public policy and healthy lifestyles.
This is only possible in close partnership with relevant stakeholders including the National Heart Foundation, Stroke Foundation, Kidney Health Australia, colleges, primary care physicians, nurses, pharmacists, consumer groups and all interested to contribute.
An important first step is the creation of a national taskforce as a close collaboration between Hypertension Australia and the Australian Cardiovascular Alliance (ACvA), which will also be launched in December.
Now is the time to make a difference.
References available on request Author competing interests – nil

The COVID state of emergency ended with health worker vaccine mandates quietly revoked in November. The mandates were imposed to “limit the spread of COVID-19 among vulnerable populations in Western Australia” and to “abate the risk to health care workers and health support workers who are at a higher risk of exposure”, the Chief Health Officer said. It is difficult to find any robust evidence supporting this policy.
There was never convincing evidence the vaccines limit the spread. That they were needed to protect the vulnerable was based more on hope, good intentions and hypothetical modelling than critical appraisal of real-world evidence.
mRNA injections stimulate circulating antibodies that reduce disease severity once the virus reaches the alveoli, but do not confer mucosal immunity. This was corroborated by early studies that showed similar nasal viral loads in the vaccinated and unvaccinated. Even before mandates were introduced, breakthrough infections were commonly observed.
The randomised controlled trial securing emergency authorisation did not consider transmissibility as an outcome (confirmed in the European Parliament by a Pfizer executive).
Since Omicron, new subvariants have spread at a high rate despite 95% of our population double vaccinated and over 80% triple vaccinated. With each successive dose, we’ve seen vaccine effectiveness become weaker, shorter lasting and eventually negative. New South Wales health surveillance data consistently show a direct correlation between number of vaccinations and population rates of hospitalisation.
This makes immunological sense as the injections were designed to produce antibodies to the Wuhan spike protein, but with over 30 mutations there has been inevitable immune escape. The antibody response to the original
antigen led to immune imprinting, a phenomenon that impairs the immune system’s ability to respond to later variant antigens, explaining empirical evidence that vaccinated people remain infective longer than unvaccinated.
The vaccines failed to limit COVID spread. Mass vaccination campaigns and mandates may have prolonged the pandemic. Our World in Data shows much lower COVID case numbers in countries with low vaccination rates, both across the board and in specific regions when we compare high income with upper middle and lower middle-income countries (e.g. Australia vs South Africa, or Israel vs Jordan).
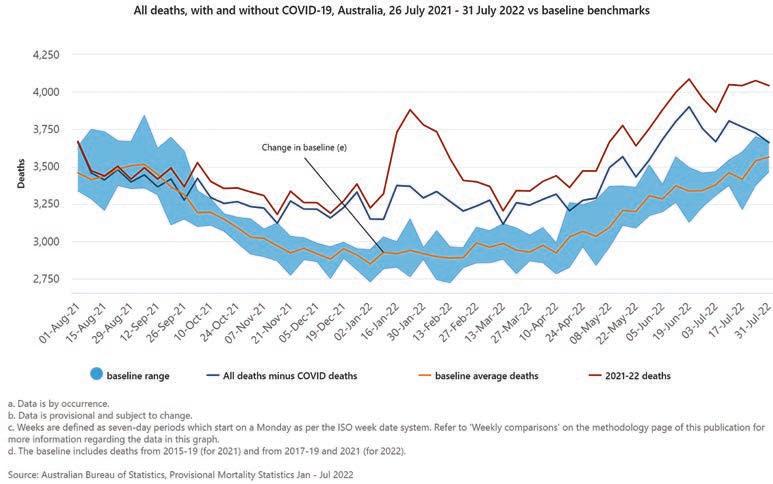
The vaccine’s inability to prevent infection or transmission was acknowledged by the US CDC in August, when it stopped differentiating its public health guidance between the vaccinated and unvaccinated.
“Do it for others” has ultimately proven to be little more than a collectivist myth based on nonexistent or, at best, flimsy data.
As the mRNA injections do not prevent transmission, but may reduce disease severity, they can be considered preventative treatment rather than true vaccines. Thus, people should have the right to
freely choose treatment based on their personal weighing of benefits and risks.
Mandating treatment rejects core ethical principles of informed consent and bodily autonomy. The Australian Immunisation Handbook emphasises that, before vaccination, valid consent must be given voluntarily “in the absence of undue pressure, coercion or manipulation”.
Using novel technology that was rushed to market, these injections remain experimental while effectiveness and safety data are collected and evaluated. Mandating experimental treatment runs counter to the Hippocratic Oath and Nuremberg Code.
In working age people where mandates applied, COVID is overwhelmingly a mild disease. Australian data show a case fatality rate below 0.1% in the 20-70-year age group. It remains unclear why well-researched pandemic preparedness plans updated less than a year before the outbreak were binned, while a risk-stratified approach was ignored as advocated in the Great Barrington Declaration.
This would have seen “focused protection” measures including vaccination targeting the old and vulnerable while allowing others to make their own risk-informed decision.
The vaccines were promoted as “95% effective” based on the relative risk reduction of symptomatic infection, rather than the absolute risk reduction of only 0.84%. At 0.1% case fatality rate, the absolute risk reduction for COVID death is thus 0.00084%, or a 1 in 119,000 chance that the vaccine prevents death in this age group.
To balance this with the potential harms, we need to consider that the mRNA injection instructs our cells to manufacture the toxic spike protein, which damages endothelial cells and is highly inflammatory and thrombogenic.
After vaccination, spike protein is biodistributed widely and persists longer at higher plasma levels than after infection. Whereas natural mRNA breaks down within hours, synthetic mRNA and spike protein are still detected in lymph nodes two months after the second dose. Pharmacovigilance data show an unprecedented number of serious adverse events, mostly in those under 70. Clinical trial data showed a 1 in 800 absolute risk of serious adverse events after vaccination, far exceeding the risk of COVID
hospitalisation (cardiac injury most reported). Two studies detected subclinical myocarditis in 2.8% of young men based on postvaccination troponin levels.
We are currently witnessing excess mortality across the Western world (Australia 17% above the five-year baseline). The excess mortality curve started its rise at the height of the vaccination campaign before our borders opened and infections peaked (see ABS graph). Most of the excess deaths are non-COVID related. Actuarial and life insurance data overseas show the excess mortality occurring mostly in the young and employed population.
The exact cause of excess non-COVID deaths is yet to be characterised but may be collateral damage from our pandemic response. They cannot be automatically linked to the vaccines, yet a causal relationship cannot be ruled out. Almost two years into the roll-out, it is disturbing that no government or health authority promoting the vaccines has seriously looked at analysing these concerning safety signals.
In an age group at minimal risk from
the disease, even if at higher risk of exposure in the health-care setting, it is perplexing why health worker vaccine and booster mandates applied for so long while evidence of net vaccine harm was available.
We need more open, honest and robust debate and an independent inquiry into the government’s COVID vaccine policy and wider pandemic response. We must learn lessons and there must be accountability so that future mistakes can be avoided.
1. Household transmission of the SARS-CoV-2 Omicron variant in Denmark - PMC (nih.gov).
2. Duration of Shedding of Culturable Virus in SARS-CoV-2 Omicron (BA.1) Infection | NEJM
3. Fifty Years Later: The Significance of the Nuremberg Code | NEJM
4. Curing the pandemic of misinformation on COVID-19 mRNA vaccines through real evidencebased medicine - Part 1 | Malhotra | Journal of Insulin Resistance
5. Serious adverse events of special interest following mRNA COVID-19 vaccination in randomized trials in adults - ScienceDirect
6. Cardiovascular Effects of the BNT162b2 mRNA COVID-19 Vaccine in Adolescents[v1] | Preprints
7. Mueller, Christopher. Myocardial Injury after mRNA booster vaccination. Presented at European Society of Cardiology conference 28 August 2022 EUROPEAN-SOCIETY-CARDIOLOGYCONGRESS-AUG22-MUELLER-MYOCARDIALINJURY-AFTER-mRNA-BOOSTER.pdf | DocDroid
– More references on request
ED: As noted this article is the opinion of the author.

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Snoring is very common, affecting about around 10-30% of young children. When habitual (three or more nights per week) or with observed apnoea, this needs further evaluation for OSA.
OSA is common in children of all ages particularly in school-aged children where adenotonsillar hypertrophy peaks. Children who snore and have risks such as obesity, comorbidities such as hypertension or poor asthma control benefit from further assessment. There are distinct differences to adult OSA as outlined in the table.
Nocturnal symptoms include gasping (albeit harder to recognise in children), sleepwalking, enuresis, unrefreshing sleep despite adequate duration or excessive sweating. Daytime symptoms include poor school functioning, ADHD-like behaviour and other disruptive behaviours. Epworth score and non-attended sleep tests used in adults are not generally validated or used.
Whilst the long-term cardiovascular and metabolic morbidities consequent to adult OSA are well depicted, such consequences in children are not really known.
In cases of mild OSA, antiinflammatory therapy such as nasal steroids have proven efficacy and the mainstay. Early reports suggested very high efficacy (>85%) from adenotonsillectomy, however, the contemporary data
OSA is common in children but quite different clinically to adult OSA
Conservative and surgical treatments have a primary role Parasomnias generally resolve and lifestyle measures are first line.
has revealed cure rates are much lower especially with more obese children. CPAP has well proven benefits in children with adherence rates similar to adults. Dental therapies have an emerging role.
Many children will experience one form of parasomnia, often in the non-REM category. These include sleepwalking, confusional arousals and night terrors. They share many similarities often with a familial history and arising in the first half of the evening. They usually arise from partial awakening from deep (usually stage 3) sleep.
Night terrors peak around 5-7 years and are different to terrifying nightmares in that there is very poor recall of the event the next day and the child appears to not be fully awake with limited cognition during events (as with sleepwalking).
A piercing scream marks the beginning of the partial arousal, followed by cries or vocalisation of
Most
Obstructive
First line therapy often CPAP
RDI/AHI >10 on sleep studies suggests severe OSA.
First line therapy is surgical
RDI >30/hr in adults is classified as severe
marked distress. The child appears petrified, with unfocused eyes, intense sweating, heart racing and might jump out of bed and run around with potential injury resulting. These events typically end abruptly, usually within five minutes.
Differentiating with nocturnal seizures or REM, parasomnias may be a challenge. Video documentation at home can be helpful.
Management includes injury minimisation measures, with adjustment in the home environment especially securing windows, stairs and doors. It is imperative to reassure parents that this is not representing a primary psychological problem and tends to diminish and almost always resolve as the child gets older.
Parents are advised to not try and awaken the child because this can result in more frequent events in the evening and sometimes cause an outburst and confusional awakening with distress. They should be encouraged to let the event run its course, gently guide the child back to bed with minimal intervention other than injury prevention.
Avoiding triggers such as sleep deprivation, attention to good sleep routines, reducing bedroom disturbances such as noises and pets is advised. Some medications such as SSRIs can provoke these parasomnias. Addressing any stress and sleep pathology such as sleep apnoea is also relevant.
In severe and frequent cases, a more systematic behavioural approach, programmed awakenings and a referral may be needed. In a small fraction, medications such as clonazepam are useful adjuncts to the above.
Author competing interests – nil

Precision medicine is an emerging approach to disease treatment and prevention that considers individual gene variability, environment and lifestyle. In contrast to a one-size-fits-all approach, improved outcomes can be achieved with individually targeted health-care advice. This is especially powerful in oncology, with treatments based on the individual’s tumour genetics.
Otitis media (OM), rhinosinusitis, sleep disordered breathing (SDB) are common presentations. The sequelae include complaints of difficulty breathing, sleeping, feeding and hearing, subsequently affecting growth, mood, behaviour, learning, communication and development.

Anecdotally, most children presenting to an ENT clinic have a parent who, as a child, also suffered recurrent tonsillitis or OM. Twins studies also show a strong heritable component in OM.
Co-researchers at the Telethon Kids Institute (TKI) have identified one gene and several genetic loci that may host candidate genes indicating risk of OM. Although gene therapy appears a long way off, injecting genes, via a viral vector, into the cochlea to treat hearing loss, is entering clinical trials.
Mannose binding lectin (MBL) is an integral part of the innate immune system. Unpublished data from a paediatric cohort at St John of God Hospital (SJGH) Subiaco, found approximately 35% of patients requiring surgical intervention for SDB were MBL deficient. A further 5-7% of patients had an immunoglobulin deficiency. None of these deficiencies can be directly corrected, apart from immunoglobulin replacement in severe cases.
Our research also shows that day-care attendance is correlated with increased risk for surgical intervention for OM. Armed with such data, for the high-risk patient, advice could be to minimise
day-care attendance, encourage influenza and other vaccination, lower the threshold for antibiotic prescription etc.
TKI co-researchers have also uncovered complex interactions between the immune system, the nasopharyngeal microbiome, nasopharyngeal and middle ear viral pathogens, bacterial pathogens (H. Influenzae) and biofilm formation, resulting in persistent disease.
These studies have led to two novel therapies in clinical trials: 1) Dornase Alpha (usually used to treat viscous secretions in cystic fibrosis) to dissolve the persistent middle ear biofilm and, 2) a nasal vaccine to replace the pathogenic nasopharyngeal microbiome with a healthy one. Our animal model shows markedly reduced rates of OM, indicating that these treatments could dramatically alter management in the future.
We found that in children with SDB, similar persistent infections within the tonsils and adenoid cause chronic inflammation and
hypertrophy, presenting targets for future anti-microbial therapies to treat SDB.
Immune deficiency and atopy contribute to presentations of rhinitis, sinusitis and airway obstruction. Unlike adults, paediatric allergic rhinitis is strongly associated with SDB. Identifying rhinitis, aeroallergens, effective topical therapy, allergen avoidance and desensitisation, play an important primary and adjuvant role in treating SDB and rhinosinusitis in children.
Patients with adenotonsillar hypertrophy often present with dysphagia (especially meat). We found that most children undergoing adenotonsillectomy (SJGH cohort), were iron deficient. It is uncertain if diet alone is responsible. Eosinophilic oesophagitis and coeliac disease are often also identified in this dysphagic population.
Some of these children have persistent lethargy, despite sleep improvement after surgery, and can be counselled to increase iron-rich foods, or other supplements. In children presenting with restless
Consider genetics, microbiome, immune status nutrition and lifestyle not just the organ system
Individualised
sleep without snoring, but resultant periodic limb movement disorder, and/or behavioural and learning issues, iron supplements alone may be recommended.
Using validated questionnaires, our team demonstrated the efficacy of symptom-based targeting of surgery for sleep disordered breathing. Furthermore, we showed that in younger children, iron deficiency may cause persistent daytime lethargy and behavioural problems that may require supplementation.
Although adenotonsillectomy is highly effective to treat SDB
in children (success rates in randomised controlled trials >85%), the risk of post-operative haemorrhage is a concern. The Perth Children’s Hospital (PCH) ENT department pioneered tranexamic acid use in secondary haemorrhage to reduce return to theatre rates (<1%).
Further improvements in technology and technique have resulted in the intra-capsular tonsillectomy for selected patients, reducing recovery times to a few days, and bleeding rates to near zero. In complex, nonobese, CPAP intolerant patients where adenotonsillectomy fails (e.g. trisomy 21), midline posterior glossectomy is effective.

The virtual or in-person meeting of medical, surgical, and allied health teams in the aero-digestive diseases arena was pioneered in Australia at Princess Margaret Hospital in 2006. This enabled the coordinated care of complex patients, in teaching hospitals and private practice. The Complex Airway Team at PCH is a multi-disciplinary group meeting frequently and communicating daily.
For example, a child with
snoring, dysphagia, failure to thrive and chronic respiratory pathology will be discussed by the otolaryngologist, respiratory physician, gastroenterologist, speech pathologist and dietitian. Investigations (sleep studies, blood tests, lung function studies, contrast swallow assessment) and clinical findings are compared and communicated to the primary care team. If surgery is contemplated, a bronchoscopy, oesophagoscopy and adenotonsillectomy can be combined under one general anaesthetic, with concurrent multispecialty opinions and treatment.
Targeted nutrition, feeding, sleep hygiene, day-care attendance, supplemental vaccination and allied health interventions all help to reduce the burden of disease and improve outcomes of medical and surgical interventions, and can be targeted to each child’s unique clinical and social picture.
– References available on request
Author competing interests – the author has been involved in some of the research described




Chronic kidney disease (CKD) has five stages of progression, with the first three stages (eGFR ≥30ml/min/1.73m2) usually being managed in primary care.
Approximately 1.7 million Australian (~1 in10) aged 18 years and older have indicators of CKD, with CKD responsible for 16% of all hospitalisations in Australia and contributing to over 11% of all deaths. The impact of kidney disease on lost productivity in Australia between 2020 and 2029 is predicted to amount to $141.3 billion in GDP.
The number of patients with end stage kidney disease (ESKD) also continues to expand and has become a major challenge for health systems globally, with 2.6 million people receiving renal replacement therapy in 2010 expected to grow to 14.5 million people needing renal replacement therapy by 2030.
Management of early CKD focuses on optimisation of cardiovascular risk factors, such as treating blood pressure to target and achieving tight glycaemic control in diabetics which also improves renal outcomes. Where appropriate, pharmacological therapies that have been demonstrated to slow the progression of CKD, namely renin-angiotensin system blockade, statins, GLP-1 receptor agonists and SGLT2 inhibitors (Dapagliflozin has recently been approved on the PBS for the management of proteinuric CKD: streamline authority 13230) should be instituted.
The Kidney Health Australia Chronic Disease (CKD) Management in Primary Care publication is an excellent resource to use when performing kidney health checks on individuals who have risk factors for CKD.
As the patient’s condition progresses to stage four and five (or for patients with CKD stage 3 that is rapidly progressing – e.g. a
Chronic kidney disease is common with significant morbidity and economic cost
A multidisciplinary approach including coordination with primary care enhances patient outcomes
Encourage home therapies including peritoneal dialysis where possible.
sustained annual loss of eGFR of ≥ 5ml/min/1.73m2/year), patients should ideally be referred to specialised nephrology services for further management.
In addition to continuing therapies to delay disease progression and adjusting medications that may accumulate or become harmful due to reduced clearance, discussions will commence to prepare the patient for transition to a renal replacement therapy, or supportive care.
In our unit this care is led by a multidisciplinary team, incorporating renal physicians, pre-dialysis and CKD educators, vascular access specialists, dietitians and diabetes educators to deliver a “one stop shop” to manage significant co-morbid medical conditions and to focus on efforts to improve quality of life.
Treatment options for ESKD patients include haemodialysis (HD), peritoneal dialysis (PD), transplantation and supportive care. People who choose PD carry this out at home, whereas HD is primarily performed in satellite dialysis units or in hospital in-centre units, although the number of patients doing home HD is growing. There is a major focus nationally and internationally on growing home therapy use (for appropriate patients) due to improved quality of life and significant cost savings for the health system.
A multidisciplinary model of care has become an important addition to the NHMS renal service and is delivered through a coordinated patient-centred clinic. This team helps guide patients from the predialysis stage to renal replacement therapy. Coordination with primary care management plays a critical role and key areas under development to strengthen these relationships include:
• Opportunities to provide outreach into practices to discuss CKD management and shared care models.
• Opportunities for observerships within the renal unit.
• A combined standardised management plan format which enables easier communication between tertiary and primary health
• A focus on how we can manage those patients that have chosen a supportive care pathway.
The Sir Charles Gairdner Osborne Park Health Care Group Nephrology website provides comprehensive resources and information for patients and primary health providers.
Home therapies should be encouraged for those individuals who are able. They provide the patient with greater treatment flexibility, independence, responsibility and better quality of life. Several studies have now demonstrated that PD is at least as good or even better than HD in the first few years for patients who commence dialysis.
– References are available on request
Author competing interests – nil
The Kidney Australia management booklet is available at kidney.org.au/uploads/resources

Glaucoma still is the number one cause of preventable blindness in the Western world and is still a silent condition until it's very late. Thus, it is worth remembering its importance and that of screening.
Glaucoma is the commonest form of optic neuropathy where the optic nerve, which comprises approximately 1.5 million nerve fibres subserving all visual functioning from vision to brightness to movement to colour etc., decays earlier than it should do in life.
This is typically due to increased eye pressure relative to the eye’s tolerance to that pressure. Genetic, vascular, and other unknown and untreatable factors also play a role but, in essence pressure, control is the treatment mainstay.
One of the modalities of monitoring glaucoma is the visual fields progress. Figure 1 shows a very characteristic pattern. The patient is slowly losing (note the time frame) the superior component of the visual field corresponding to a defect forming in the inferior part of the optic nerve. This can be seen with the ophthalmoscope and is represented below in the Heidelberg (HRT) scan showing the inferior notching of the nerve (Figure 2).
When we examine for glaucoma, we tend to examine the triad of intraocular pressure, the appearance of the nerve and the visual fields. No one thing in isolation typically can make the diagnosis.
Fortunately, through extensive epidemiological studies and increased awareness and improved screening by our optometrist colleagues, we are picking it up much earlier and therefore can intervene sooner. The greatest risk of severe glaucoma remains late detection in terms of progression.
Another major risk is genetic susceptibility – accounting for about 20%. Myopia or short sightedness tends to increase
the risk of glaucoma as does migraine and lower blood pressure, presumedly because of impaired optic nerve head perfusion.
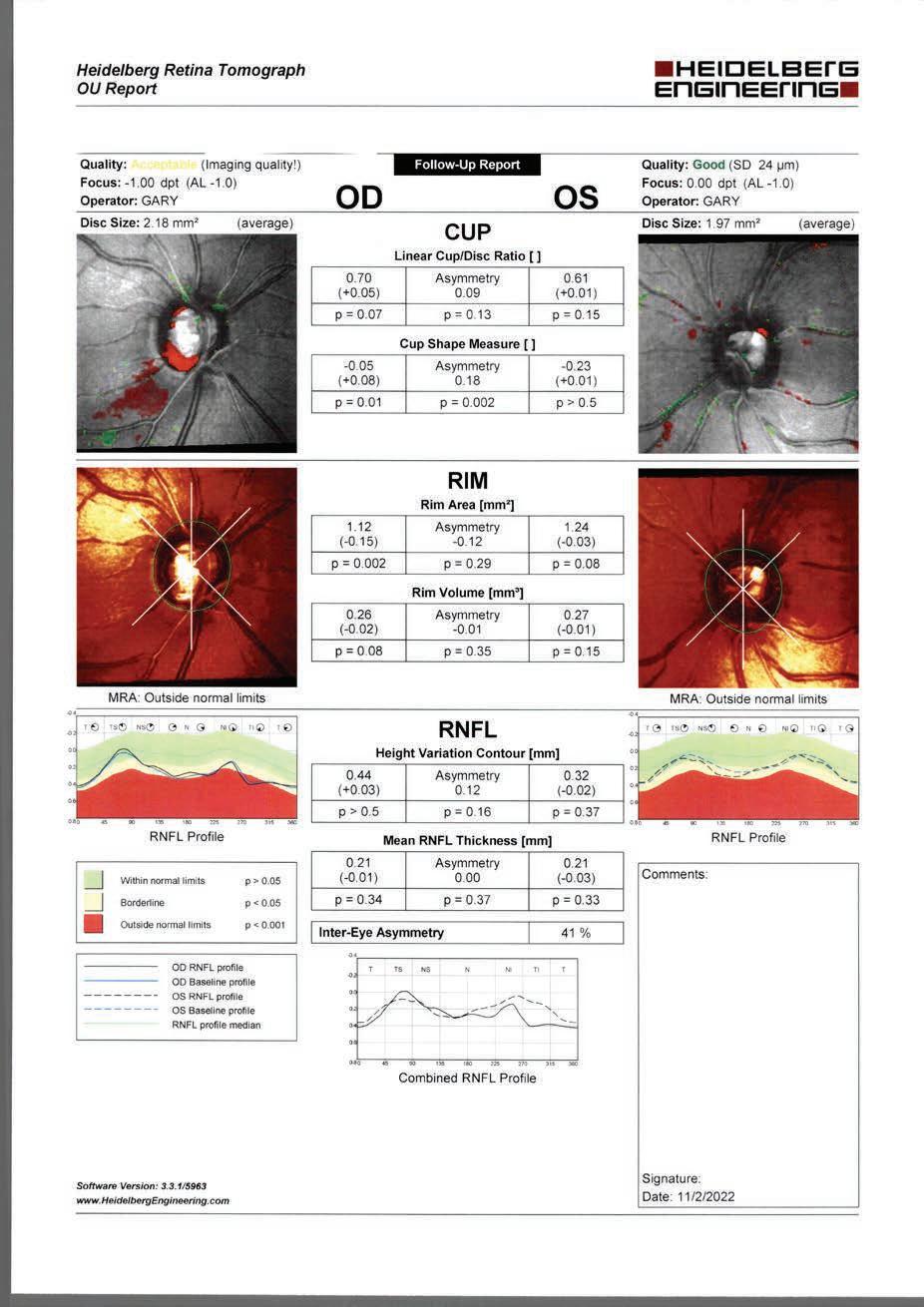
The fundamental treatment for glaucoma is still to get the pressure down and keep it down to an acceptable target pressure. This can be done via a range of modalities – a range drops would cover more than 90% of patient
Glaucoma remains an extremely common, treatable and challenging condition with devasting results if undetected
Early detection and specialist referral is the key
New surgical treatments are emerging but traditional surgery and drops remain mainstay
are used to lower the pressure in a small percentage of people.
Traditional trabeculectomy is still an excellent procedure, which is now challenged by MIGS or minimally invasive glaucoma surgery. While these techniques have shown great promise, they are still presenting their share of problems as with any device in terms or complications and efficacy.
Some MIGS devices beyond the scope of this article for researching include Xen stents, iStents, pressrflo stents and others such as the Hydrus. Having a considerable experience with the above, a traditional trabeculectomy is still a good option having the benefit of decades of data collection, but others are showing promise (and problems). No glaucoma surgery is without these. There is a next level shunt group for more severe and secondary glaucoma, also when other treatments have been exhausted.
Primary or open angle glaucoma is still by far the most significant glaucoma to concentrate on and unfortunately at medical school the feared acute angle glaucoma was pushed so hard as to colour our view about glaucoma, when, in fact, it probably represents 1% per year in the at-risk population, which is incredibly small.
In real numbers, it's probably seen approximately once a year in a glaucoma practice. There is an in between phenomena which is referred to as chronic angle closure but is be treated as open angle glaucoma except one of the fundamentals is either lens removal (cataract), or peripheral iridotomy, which is becoming increasingly rare in my practice, especially with improved and safer lens/cataract surgery.
Just as general screening for other medical conditions is commonplace – prostate, breast, blood pressure etc. – glaucoma screening, which can certainly start at an optometry level, is still a fundamental part of a general health check which shouldn’t be overlooked.
Author competing interests – nilA team of international researchers threw the cat among the pigeons when they suggested that even a small amount of caffeine while pregnant might be linked to a woman’s child being short.
They followed up children of women who had low levels of caffeine and paraxanthine – a metabolite of caffeine – during their pregnancy at ages four to eight years, and said these children were shorter than the children of women who had no caffeine during their pregnancy.
Figure 1:
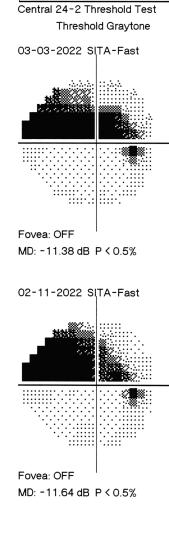

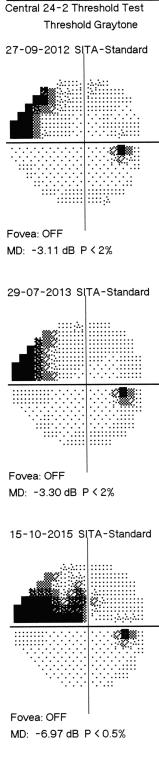
Although the clinical implications were unclear for relatively small observed differences, the team said the findings suggested that small amounts of daily maternal caffeine consumption were associated with shorter stature in their offspring that persisted into childhood.
But Dr Gavin Pereira, a professor of epidemiology and biostatistics at Curtin University, said there was not enough evidence that caffeine during pregnancy hampered the subsequent growth.
The researchers’ conclusion that “increasing levels” of caffeine and paraxanthine, even in low amounts,
was associated with shorter stature in early childhood was incorrect.
“All that can be concluded from this study is that the children born to women who consumed higher levels of caffeine were shorter than the children born to women who consumed relatively lower levels of caffeine,” Dr Pereira said.
“The correlation observed in this study can be explained by the existence of a common cause of both caffeine consumption and growth restriction – poverty, stress and dietary factors.”

Fresh Start provides services across the Fresh Start Clinic, Fresh Start Lodge, Fresh Start Psychology and Fresh Start Northam We are committed to treating people with addiction and supporting them through recovery and are always looking to expand our network of professionals and volunteers If you are looking for a new employment opportunity, volunteer role or to build on your existing knowledge visit our careers page to apply.

Abdominal aortic calcification or AAC is the deposition of calcium within the intimal or medial layers of the aortic wall. The presence of AAC is evidence of aortovascular disease and has been shown to be a marker of generalised atherosclerosis at other vascular beds e.g. coronary and carotid arteries, and/or medial calcifications seen in certain clinical populations and advanced ages.
Unlike coronary artery calcifications (CAC), AAC appears to be driven to a lesser extent by traditional atherosclerotic cardiovascular risk factors such as lipids. Instead, low muscle and bone mass and chronic kidney disease appear to be important drivers of higher prevalence and extent of AAC.
AAC can be assessed by expert readers on lateral thoracolumbar x-rays or vertebral fracture assessment images from bone density machines. The extent of calcification is semi-quantified based on the proportion of the calcification on the posterior and anterior aortic wall, relative to the adjacent lumbar vertebrae (L1 to L4). More recently new, state-ofthe-art machine learning algorithms have been developed to automate this process.
Is AAC normal, and how does it affect the function of the aorta?
A healthy aorta (no calcification) would not be visible on these images. Autopsy and imaging studies have identified that the iliac artery bifurcation and abdominal aorta are often the first sites where vascular calcification is seen.
While AAC is common in older people, it is not normal. AAC has been shown to increase aortic stiffness, raise central blood pressure and widen pulse pressure contributing to damage to highflow, low-resistance organs such as the heart, brain and kidneys.
There is now good evidence that AAC is consistently related to
Abdominal aortic calcification can be assessed on thoracolumbar x-ray or bone density assessment
AAC is related to higher rates of cardiovascular disease
Its finding can assist with reinforcing lifestyle advice to patients.
higher cardiovascular disease (CVD) risk and poorer long-term prognosis in the general population and in people with chronic kidney disease.
AAC is also associated with increased risk of CVD events in middle-aged men and women without CAC. Importantly, AAC also predicts coronary heart disease events in addition to and independent of CAC and is more strongly related to CVD and allcause deaths.
Taken together this emerging research suggests assessing AAC represents an early opportunity to identify people at risk of CVD events, often before the onset of CAC and provides additional prognostic information to CAC.
With regards to other health outcomes, AAC is related to poorer handgrip strength, the decline in handgrip strength over five years and increased long-term falls risk. Additionally higher AAC has been associated with low bone mineral density and increased risk of osteoporotic fractures.
AAC is inversely related to poorer cognitive function and more recently moderate to extensive AAC has been associated with a doubling in the risk of developing late-life dementia in older women. The exact mechanism(s) underlying these relationships remain unclear but are a developing area of research interest.
What can you do if AAC is seen
on images? Currently, there are no guidelines or recommendations for when AAC is observed. If moderate to extensive AAC is seen in patients without known CVD, then consideration of traditional risk factors e.g. lipids, blood pressure and glycaemic control, as well as non-traditional risk factors such as renal function, muscle and bone mass may be warranted.
So, what to tell patients if AAC is seen on these images? Providing feedback of vascular imaging results to individuals, particularly those with moderate to extensive AAC, may be an opportunity to reinforce healthy lifestyle recommendations that improve CVD risk factor control. Exercise and dietary factors (e.g. fruit and vegetables rich in vitamin K1 and flavonoids) may help to reduce the progression of AAC and development of clinical CVD.
Multidisciplinary approaches incorporating dietitians and accredited exercise physiologists may be encouraged to help support patients with making these lifestyle changes.
ED: A/Prof Lewis is a Heart Foundation Future Leader Fellow and board member of the WA Cardiovascular Research Alliance. Dr Smith is an accredited exercise physiologist and postdoctoral research fellow at ECU.


Both authors are members of the Nutrition & Health Innovation Research Institute at ECU.
Author competing interests – ECU has lodged a patent for automated assessment of abdominal aortic calcification. A/Prof Lewis is one of the named inventors on this patent.
At BreastScreen WA (BSWA), women from the age of 40 are eligible for annual screening mammograms if they meet one of the following criteria:
One or more 1st degree relatives (mother, sister, daughter, father, brother, son) with breast cancer before the age of 50;
- One or more 1st degree relatives with cancer in both breasts (diagnosed at any age);

Two or more 1st degree relatives with breast cancer (diagnosed at any age);
Past personal history of breast cancer;
Past personal history of ovarian cancer;
Past personal history of a biopsy proven borderline lesion (Atypical Ductal Hyperplasia, Lobular Neoplasia (LCIS, ALH))
Between 10% to 15% of women are currently rescreened annually at BreastScreen WA.

Only a limited past history and family history can be obtained by the radiographer at the time of the woman’s screening examination. BreastScreen WA may not be aware of important second degree relative family history information that could warrant a woman attending for annual screening.
A breast cancer risk assessment and risk management decision support tool recommended by Cancer Australia is available for GPs called iPrevent https://www.petermac.org/iprevent. If GPs believe that annual screening is indicated for their patient who does not meet the current BSWA criteria, just use iPrevent and provide that information to BSWA when referring a client for annual screening. iPrevent is a RACGP accepted clinical resource that can help women derive the benefits of screening mammography, by helping determine their risk and appropriate screening interval.
Women may book online - www.breastscreen.health.wa.gov.au

Persistent idiopathic dentoalveolar pain (PIDAP) is a persistent unilateral intraoral pain. The pain is localised to the dentoalveolar region such as the teeth or alveolar bone, and rarely involves multiple sites.
Persistent idiopathic facial pain (PIFP) is pain with variable features, in the absence of clinical neurological deficit or preceding causative event. The distribution is often poorly localised to the face and not within a peripheral nerve distribution. It has been reported more often localised to the upper jaw, and may extend to the region of the eyes, nose, cheek and temple.
Other terms for these conditions have included ‘atypical facial pain’, atypical odontalgia; primary persistent dentoalveolar pain disorder (PDAP); and phantom tooth pain, although these terms may encompass other diagnoses.
According to the International Classification of Orofacial Pain-1, these conditions may have variable features but recur daily for more than two hours a day for more than three months, in the absence of any preceding causative event. With time, and central sensitisation, symptoms may spread to a wider area of the craniocervical region and does not have to follow a dermatomal pattern. The pain may have exacerbations and be aggravated by stress.
Sensory abnormalities such as allodynia, hyperalgesia,
hypaesthesia, and/or hypoalgesia are rare in PIDAP, although allodynia in the gingival sulcus of the affected teeth appears to be a more common reported feature.
An association with endodontically treated teeth has also been reported with PIDAP. In PIFP, there may be somatosensory changes such as dysesthesia, a subjective sensation of numbness and/ or swelling, but with no objective sensory deficits or swelling.
The aetiopathogenesis and causes of PIFP and PIDAP remains poorly understood. It is generally accepted to be an idiopathic neuropathic pain with centrally mediated mechanisms.
Some patients with PIFP showed neurophysiological findings that may be indicative of peripheral nerve dysfunction including abnormal nerve responses, increased excitability and deficient habituation. On positron emission tomography (PET) studies, PIFP patients have shown blood flow and dopamine receptor changes in areas of the brain and brain stem.
There is a significant association with psychiatric comorbidities such as anxiety disorders, affective disorders, and psychosis. Some cases are associated with functional somatic syndromes with comorbidities such as chronic widespread pain, fibromyalgia, and irritable bowel syndrome.
Due to differences in nomenclature and previous non-standardised
diagnostic criteria, epidemiological data is difficult to obtain. There are reports of female predominance.
Patients should see their dentist and the clinical and radiographic examinations should be thorough, so any potential orofacial or dental cause is ruled out, including volumetric imaging such as cone beam computed tomography for the dentition where applicable.
It is important to exclude other potential causes of the pain, such as odontogenic pathology or referred pain. The clinical neurological examination is normal.
Differential diagnoses may include odontogenic pain, traumatic trigeminal neuropathies, regional myofascial pain, atypical neurovascular pains, atypical neuropathic pain, some forms of primary headaches, idiopathic trigeminal neuralgia, and referred pain. If the pain onset is within six months of a causative event, consider post-traumatic trigeminal neuropathic pain.
Misdiagnosis may lead to unnecessary dental treatment, and caution should be exercised to avoid this. Management can be challenging, and different agents and strategies have been trialled, all to variable effect.
Pharmacological therapy may include systemic medications such as tricyclic antidepressants, anxiolytics, gabapentinoids, anticonvulsants, and selective noradrenaline reuptake inhibitors. Topical forms of tricyclic antidepressants, gabapentinoids, anticonvulsants and ketamine have been trialled.
Other management trialled with some limited success include acupuncture, hypnosis and biofeedback. While prognosis of this condition is unknown, it is believed to be poor, and some patients remain unresponsive to medication and management. Author competing interests – nil
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options. For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au Healthlink: puclinic Hollywood Clinic | Wexford Clinic

Shane La Bianca Dr Andrew Tan Dr Jeff Thavaseelan Dr Trent Barrett Dr Matt Brown
Dr Akhil Hamid Dr Manmeet Saluja Dr Alarick Picardo Dr Steve McCombie
Urological care centred around all patients.

Chronic kidney disease (CKD) is a major risk factor for cardiovascular disease. One in three Australians have risk factors for CKD e.g. hypertension, diabetes, and obesity. It is therefore vital to investigate early, identify and intervene.
If detected and managed in time, deterioration in kidney function can be reduced by as much as 50%.
As well as medical management, nutrition therapy provided by a renal dietitian is paramount and has been shown to assist by slowing CKD progression and preventing advancing kidney failure.
In early stages of CKD (1-3a), addressing lifestyle and risk factors such as weight, blood pressure and glycemic control are essential. Promoting healthy eating patterns that include reducing salt, red meat, processed foods, and fats, while increasing fruit, vegetables, omega 3 sources and wholegrains is fundamental.
Over-restricting certain foods (e.g. dietary sources of potassium) at this point is unnecessary and often counterproductive unless clinically needed.
Once patients progress to CKD 3b – 5, a renal dietitian can offer more specific nutritional advice and adapt according to common symptoms. Often patients experience nausea, constipation, fatigue, taste changes and anorexia. Providing education to manage them is vital to slow the progression of disease and prevent malnutrition.
Contrary to popular belief, there is no such thing as the one-sizefits all renal diet. Managing dietary intake in CKD is one of the most complicated diets to treat due to a complex balance of maintaining individual optimal nutritional status, protecting the function of the kidney, responding to biochemical imbalances and managing comorbidities.
Protein, potassium and phosphorus
Protein source is now a key
A renal dietitian can help manage nutritional impact symptoms and slow progression of CKD Encourage fruit, vegetables and fibre rich foods
Prevent over restricting e.g. a low-potassium diet for all is inappropriate.
consideration with much research looking at the role of plant-based proteins in CKD. Recent studies have indicated that plant-based proteins when consumed in a varied diet (e.g. Med Diet/DASH) are not only nutritionally adequate but have pleiotropic effects which may favour their use in patients with CKD.
Once CKD is diagnosed, often the first thing a patient is told (or reads) is not to eat bananas, stone fruit, potatoes, avocado, wholegrains, nuts and dairy. They are given lists of foods high in potassium and phosphate (often conflicting) to avoid, regardless of their biochemistry and stage of CKD. I often see patients who have overly restricted their diet based on misinformation given to them and have lost weight, are constipated (lacking fibre) are fed up and no longer have any enjoyment in food.
It is not until a patients eGFR is less than 45mL/min/1.73 m2 that they appear to have impaired potassium tolerance due to reduced kaliuresis. Other factors causing hyperkalaemia should be investigated such as metabolic acidosis and medications (e.g. spironolactone.)
Optimising the carbohydrate content of the meal, especially fibre will impact how potassium is distributed. Dietary fibre not only increases faecal potassium output dramatically, due in part to reduced absorption, but stimulates insulin response and thus potassium uptake into the cells and improves constipation. So, the key
message here is to promote the “2 & 5” serves per day of fruit and vegetables and not restrict.
Dietary phosphorus is found in animal-based products (meat, fish, poultry and dairy), plantbased (beans, peas, legumes, cereals, grains, nuts and seeds) and convenience foods with phosphorus containing additives. It is often unnecessarily restricted due to the role of hyperphosphataemia in bone mineral disorders.
Patients are often told to avoid (essential) wholegrains, dairy and nuts. However, the bioavailability of phosphorus is important to consider. Food additives are 90100% bioavailable whilst animalbased products are 40-60% absorbed and plant-based products 30% (from being bound to phytate).
Studies looking at protein sources of phosphorus showed a vegetarian diet versus meat diet led to lower serum phosphate. A recent Irish study looked at a plant-based diet (pulses, nuts and wholegrains) versus standard diet in dialysis patients. They found both serum phosphate and potassium didn’t change, but variety of foods and fibre both increased significantly.
The benefits of a more plantbased diet are widespread, promoting acid base balance as it generates bicarbonate naturally, reducing severity of hypertension and hyperphosphatemia. It also increases fibre improving glycaemic control and reducing severity of constipation.
Early detection is key, with renal dietetic input and symptom management essential. Instead of limiting wholegrains, fruit, and vegetables, the patient should be encouraged to include a variety of these foods while limiting processed foods. And finally, always keep education simple and consistent.
Author competing interests – nil
Local photographer Brett Leigh Dicks is fascinated by urban landscapes. This time his lens has been focused on the humble lunch bar.
 By Ara Jansen
By Ara Jansen
Lunch bars by definition are not particularly glamorous places. In Perth, they used to be the place you went when you hankered for a chico roll, chips or something else your cardiologist wouldn’t be thrilled about.
They’re also typically tucked away in suburban, industrial and commercial areas and have been sustaining the work force with no-frills fast food since the 1950s. Today they continue to feed a community of mostly bluecollar workers, reasonably untouched by both gastronomical fashions and architectural trends.

Research on another project led Perthbased photographer Brett Leigh Dicks to Welshpool’s Radium Lunch Bar and somehow, after that, he just kept seeing more and more lunch bars on his travels around the city.
“They are quite unique and they have adapted,” says Brett. “They don’t follow a standard type and tend to do their own thing outside trends. I just fell in love with them.”
The result is a photographic book called Lunch Bars: Exploring Western Australia’s Fast-Food Culture

“They have such a dodgy reputation, but they are individual” Brett says. “While plenty serve what you’d expect for hot and hearty fare, others have made it all their own, specialising in a particular cuisine, including one place which serves delicious German bratwurst.”
He’s approached each external shot with a stark austerity, without cars and people bustling through the images. It’s a quiet but powerful statement which sits companionably in a decadesdeep portfolio which includes photography on decommissioned American prisons, abandoned nuclear missile bases and Aboriginal missions in the WA.
“There were two ways to approach this – bustling or stark. I wanted to do an archaeological investigation to be about the lunch bar rather than the menu or the clientele. I wanted it to be the story of the buildings and by doing that I think I
really captured the diversity of the character of the facades.”
He’s also chosen to shoot the frontages and buildings in the bright and harsh full sunlight. Each photo includes a good section of blue sky, which the photographer considers quintessentially West Australian. “Like a lot of the architecture, it’s very WA.”

Brett visited and revisited more than 100 lunch bars while the State was cut off from the rest of the world. Just over half made it into the book. He also got to know some of the owners quite well, and on Saturday mornings often took his 11-year-old son to one for lunch.
An Australian-American, Brett is based in Fremantle but splits his time with California. Since he has only lived in Perth since the pandemic, the book was a great way to get to know the city better.
“In the US, I loved driving around commercial and industrial areas. I think one of the reasons it resonated was because it was after going through isolation. It was dark times and it offered something a bit whimsical.”
Photographs and copies of the book are available from Brett’s website: www.brettleighdicks.net
While she’s been an actor all of her career, Frances O’Connor has finally achieved a dream. She has made her writing and directorial debut with a fresh imagining of the life of Emily Bronte in a film called Emily


While the idea has been in her heart and mind for nigh on a decade, it wasn’t until three years ago that Frances got serious and started working on the project in earnest. She worked with a script editor to get the writing taut after a friend told her in order to direct, she should write the movie herself.
Born in England but raised in Perth, Frances was a WAAPA graduate before her breakout role in the movie Love and Other Catastrophes Among others, she has gone on to appear in Mansfield Park, Bedazzled, The Importance of Being Earnest and Blessed as well as numerous television appearances in works such as Mr Selfridge, Madam Bovary and The Missing
Seeing her name in the opening credits felt incredible and like a scene from the movie where Emily first sees her own name on the spines of her books. As a writer, Frances feels a kinship with Emily who is searching for her voice and identity, on the way to writing the Wuthering Heights
“I wanted to write a story that was saying something about what I had
been thinking about in my life,” says Frances, “which was how to be an authentic voice or person and woman when that’s not being reflected back to you, or those qualities in you are seen as not good.
“As a young actress I was struggling with how to be true to myself in the film industry and be a creative person when I’m just judged on how I look and wanting to be approved of. In life there’s still a lot of pressure for women to be like that.”
Emily stars Emma Mackey (Sex Education and Death on the Nile) in the title role alongside her sister Charlotte (Alexandra Dowling – The Musketeers), Anne Bronte played by Amelia Gething (The Spanish Princess) and Oliver Jackson-Cohen as curate William Weightman. The movie also features the other pivotal people in Emily’s life – her brother Branwell and her father.
The movie explores a young woman’s battle with her darker, wilder side and what drove Emily to write a book which in the movie Charlotte calls “ugly and base, full of selfish people who only care for themselves”.
“It wasn’t the kind of novel a woman should have written at the time,” Frances says. “I was interested in saying that when a woman has
some power and does have something different to say, they can expect some people not to like that. Weightman falling in love with Emily is kind of like the patriarchy falling in love with Emily and then not really liking some aspects of her.
“Emily is a creative being. It’s just pouring out of her; she is connected to nature, to everything. I felt that as a young woman and for women now, we still feel like if we show some of the darker aspects of ourselves, will we still be accepted? And sometimes the answer is no.”
Turning her hand to writing and directing has opened new avenues both as an artist and emotional explorer, which Frances O’Connor is keen to pursue. The award-winning actress is excited that on the other side of 50 there’s a whole different world opening up.
Emily opens in cinemas on January 12.
We have five double tickets to give away. To enter go to www.mforum.com.au and click the competitions tab.
Coby Ladwig and Luke Eckersley, both WA men, are the force behind the Rosenthal brand. They also make wines under the Kings Landing label.
Added to that, Denmark-raised Coby has been the man behind the very impressive range of wines coming from Singlefile Estate in Denmark. The focus at Rosenthal is on the coolest regions of WA with grapes coming from Mt Barker, Frankland and Pemberton, which are processed at the Denmark winery.
The Rosenthal name comes from Dr John Rosenthal, who began in Manjimup in 2001 focusing on Shiraz and Cabernet Sauvignon. The original Rosenthal vineyard was planted by Gerald and Marjorie Richings on the rich loamy soils of their Springfield Park cattle stud.

Coby and Luke took ownership in 2012 and expanded the sourcing of wines to all over the Great Southern. The aim has been to source premium fruit with an intelligent and sensitive approach to its handling in the winery. Production is small and the focus is on quality. The wines have a purity and precision about them that make for thoughtful and enjoyable appreciation.

From a cool vintage, the fruit was gently pressed and fermented in stainless steel. A classic Mt Barker Riesling from the Langton vineyard showing the typical floral bouquet, with citrus overtones. Crisp and clean. This will mature beautifully for 10 years. (12.1% alcohol, $35)
Sourced from 30-year-old vines in the Salitage vineyard in Pemberton. Slowbarrel fermentation with 30% indigenous yeasts and 40% new oak. A very attractive bouquet of restrained floral peach and a touch of citrus. Spice and fruitiness, well integrated, leading to a long seamless mouth-filling finish. Lovely wine now but will keep. (13.3% alcohol, $60) Recommended

The Acacia vineyard in Frankland was the source of grapes for this deep, darkcoloured Shiraz. As with the chardonnay, a proportion of wild yeasts have had an impact. Plums, leather spice and earth all combine to give a rich mouth-filling experience wrapped up in moreish soft savoury tannins. The flavours linger long on the finish. Lovely to drink now with ageing potential (14.5%, alcohol $60).
The Riversdale vineyard in Frankland has a track record of producing some of Australia’s finest wines This cabernet is no exception. Gorgeous cassis, cedar aromas lead onto a veritable flavour explosion of berries seamlessly wrapped in fine lingering tannins. Excellent balance and a long lingering finish. Cellar easily for 10 years (14.5% alcohol, $60) Recommended
You’re invited to explore the ways MRI-guided Transcranial Magnetic Stimulation (TMS) can benefit your patients during a complimentary Coffee ‘n’ Conversation session with a psychiatrist from sentien sentien’s dedicated team is utilising TMS to make headway in the treatment of depression and other psychiatric conditions, including Obsessive-Compulsive Disorder (OCD) and Post-Traumatic Stress Disorder (PTSD). TMS can also improve the burden of physical pain and has even been utilised for medical rehabilitation (e.g. post-stroke recovery), managing fibromyalgia and relieving the symptoms of tinnitus.
This procedure is: Non-invasive Outpatient-based


Listed on the MBS for treatment-resistant depression







If you would like to find out more, one of sentien’s TMS experts would be delighted to attend your practice for an in-person information session. Video conferences can also be arranged, should you prefer. Please email hello@sentientms.au to register your interest.
1800 for TMS hello@sent ientms.au www.sentientms.au