


























Welcome to our first edition for 2023, as we keep fingers crossed that a new year will take us one step closer to a post-COVID reality.
Of course, the coronavirus has not gone anywhere, particularly in light of China reportedly facing an eye-watering 900 million cases – or 64% of its population – in recent weeks.
But elsewhere COVID continues to evolve from an acute phase to a chronic one.
There are some things we will never get back from the period in which our State was bunkered down with COVID – the delayed elective surgeries that were never rescheduled and the routine health checks that were missed.
But this month Medical Forum looks ahead at some of the new approaches in medicine, including how we test and treat illness – progress that was made despite the pandemic.
We also look at changes in how doctors practise their craft, including the use of telehealth, which benefited from COVID by becoming routine rather a rarity in health care as necessity became the mother of invention.
But we reveal that health authorities and medical indemnity insurers are now casting a more critical eye over the use of online consultations where there has been no previous in-person interaction between doctor and patient.

I’m reliably told that many doctors believe the cracking down on online-only consults has come not a moment too soon.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
There are some things we will never get back from the period in which our State was bunkered down with COVID – the delayed elective surgeries that were never rescheduled and the routine health checks that were missed.

The lucky winner of the doctors dozen from Arlewood Wines featured in our November edition was Dr Angus Jeffrey, who has taken receipt of his prize.


Enjoying tickets to the movie Emily in the New Year were Drs Jenny Smith, Glen Koski, Peter Brockhoff, Maria O’Shea and Craig Schwab


PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au




Journalist Eric Martin 08 9203 5222 eric@mforum.com.au

Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au








Marketing Quinn Hampton quinn@mforum.com.au

Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM


Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
An ambulatory emergency care unit has opened at St John of God Midland Public Hospital to provide urgent assessment and treatment for patients initially presenting to its emergency department.

Hospital CEO Paul Dyer said the unit had been designed to reduce waiting times, improve patient flow, avoid unnecessary overnight admissions and enhance the patient experience.

“With less patients requiring an overnight stay, it will reduce waiting times in the emergency department and enable more beds to be available in the hospital,” he said.
“Suitable patients will be identified in our ED and prioritised for transfer to the ambulatory emergency care unit for same-day assessment and management.”
The unit allows patients to have diagnostic tests and treatments and, if needed, they can return to the unit the following day for an outpatient appointment for further investigations or to ensure they have not deteriorated.
HBF has struck a deal with Ramsay Health Care that will remove some costs associated with roboticassisted procedures.
Robotic technology is increasingly being used in cancer surgery such as radical prostatectomy and the treatment of kidney and bladder cancer but can mean significant out-of-pocket costs for patients.
The new arrangement for eligible HBF members sees the removal of the co-payment previously paid by those undergoing robotic-assisted surgery.
The peak body of psychiatrists has welcomed the decision by the WA State Government to ban LGBTQIA+ conversion therapy.
The decision came after a parliamentary inquiry into Esther House – a private residential rehabilitation facility – revealed that conversion therapy was practised there and residents were subjected to exorcism-type treatment instead of receiving evidence-based care and support to those experiencing distress.
Royal Australian and New Zealand College of Psychiatrists WA Branch chair Dr Michael Verheggen said the college staunchly opposed the practice of any sexual orientation change efforts and noted the dangerous impact it had on the mental health of people.
“Psychiatrists across the board warn that sexual orientation change efforts risk causing significant harm and trauma to individuals,” he said.
“Practices such as conversion therapy contribute to the misrepresentation of alternative sexualities as mental disorders, and to the broader prejudice and discrimination faced by people who identify as LGBTQIA+.
“The RANZCP has previously highlighted in its position statement on sexual orientation change efforts that there is absolutely no scientific evidence to suggest that sexual orientation can be changed.”
Previously underresearched aspects of Parkinson’s disease are revealing new clues
on what triggers the degenerative brain disorder and how to slow its progression.
A paper published in the journal Experimental Biology and Medicine suggests that DNA elements largely ignored in most genetic studies could influence disease development.
Professor Sulev Koks, head of Genetic Epidemiology Research at the Perron Institute for Neurological and Translational Science and Murdoch University’s Centre for Molecular Medicine and Innovative Therapeutics, said transposable elements made up more than 70% of the human genome, but until recently were thought to not have any meaningful function.

“Our research showed that these elements, known as the ‘dark genome’, may have a much more significant impact on the pathophysiology of this disease than previously thought,” he said.
“Depending on location within the genome, they may speed up or slow disease progression.
“Our previous studies have indicated that these DNA
continued on Page 6
As of 1 January 2023, the Medical Board of Australia (MBA) requires all Australian GPs to complete the following continuing professional development (CPD) requisites:
• Log 50 hours of CPD every year
• Complete a professional development plan (PDP) every year
• Refresh your skills with one CPR course during the triennium
RACGP CPD
Minimum Requirements for 2023 - 2025 Triennium (50hrs per year)
Education Activities: activities that expand your General Practice knowledge and skills. Examples - Reading educational material (articles, journals), Workshops, Conferences, Lectures/Webinars.
Measuring Outcomes: activities that use your work data to ensure quality results. Examples - Audits, Practice Accreditation, Development of clinical guidelines.

A CPD clinical audit designed to help you easily manage and provide clinical care for your patients living with diabetes.

Reviewing Performance: activities that require reflection on feedback about your work. Examples - Case based discussions, Peer group learning, Patient feedback.
Annual Criteria for CPD Program Qualification
• Patients with diabetes referred for HbA1c analysis (minimum 40 episodes)
• Minimum 4 program views/logins
• Minimum 12 months of registration
• Reflection activity completed
Skin Excision Evaluation Program
A CPD clinical audit that delivers a truly educational experience by analysing your diagnostic skill for identification of high-risk lesions.
Annual Criteria for CPD Program Qualification
• 40 histological samples submitted on the specific audit request forms
• Minimum 12 months since registration
• Reflection activity completed
Earn
1 0 CPD hours per year! Earn
27.5 CPD hours per year!
There are now three different types of activities you’ll need to complete to gain the required 50 CPD hours each year. Earn
37.5 CPD hours per year!
Clinical Labs facilitates educational workshops with our vast specialist network. We are agile and responsive, providing you with the ability to complete all of your CPD hours with us. Enquire with your Customer Relationship Manager today!
For more information or to register online scan the QR code or visit www.clinicallabs.com.au/cpd
continued from Page 4
sequences, which can change their position within a genome, have a significant regulatory role and a major disease-causing capability.”
Research found that some transposable DNA elements predicted faster progression of the disease, with rapid deterioration of motor or cognitive functions, while others were associated with a slowing of neuronal loss and neurodegeneration.
“This study builds on our other research, contributing to future development of novel approaches for improved diagnosis and more targeted therapies,” Professor Koks said.
Hollywood Private Hospital specialist shoulder and elbow surgeon Travis Falconer recently
A diagnosis of motor neurone disease is obviously devastating for the person on the receiving end and their family caregivers. Telling someone that they have the incurable neurodegenerative disorder is also challenging for the neurologist delivering the news.
Now the experiences of patients, family carers and clinicians have been examined in a recently published study involving UK and Australian researchers.
Professor Samar Aoun, Perron Institute Research Chair in Palliative Care at the University of WA, was a contributor, with the UK study replicating the Australian study developed by Professor Aoun and colleagues in 2015.
“A diagnosis of MND and the subsequent progressive loss of independence, uncertain future and changes to everyday life have a profound effect on the person living with MND and their loved ones,” she said.
“How the diagnosis is delivered can have a significant impact on patient outcomes such as understanding
became the first surgeon in WA to use a HoloLens mixed reality headset during surgery.

Digital holograms are an emerging new tool in operating rooms across the globe. Mixed reality is the merger of real and virtual worlds with enhanced immersion and interaction.
By wearing the headset during a shoulder replacement surgery, Dr Falconer was able to see a 3D hologram of the surgical plan over the patient’s anatomy in real time. This allowed him to use the planning software and refer to data analysis during surgery. By using hand gestures and voice commands, Dr Falconer was able to interact with the holographic objects.
The aim of using mixed reality techniques is to enhance precision and simplify complex surgeries. Being able to refer to the surgical plan during surgery also provides another layer of checks and balances for surgeons.
Parkinson’s disease, multiple sclerosis and mild traumatic brain injury are among the research areas supported in the inaugural round of grants from the Bryant Stokes Neurological Research Fund. The fund, made possible by the philanthropic Sarich family, was established in recognition of
continued on Page 8
the condition, contributing to decision-making, psychological adjustment and satisfaction with care.”
Professor Aoun, who is WA’s 2023 Australian of the Year, said the results from the UK study – like those from the Australian study – highlighted the importance of neurologists and neurology services being aware of the needs of people with MND and their caregivers when they are given the diagnosis.
“An appropriate setting and allowing more time when breaking the news is critically important,” she said.
“Also essential is demonstrating more empathy and clear and honest communication, explaining what the patient can expect, and the care pathway and support services available, such as linking them to MND associations.”

Renowned neurological researcher Professor Byron Kakulas –founding director of the Perron Institute – died aged 90 in early January. Many in the medical fraternity remember him as a great teacher, mentor and colleague.

Rita Mejzini, a PhD candidate at Murdoch University and the Perron Institute, where she is working on precision therapies for motor neurone disease, has received a $100,000 grant from MND Research Australia.
Dr Gareth Wahl is the End of Life Care Program’s new clinical lead, replacing Dr Simon Towler who became chief medical officer in September last year. Dr Wahl is an emergency physician at Sir Charles Gairdner Hospital and the medical lead for Voluntary Assisted Dying at North Metropolitan Health Service.
Lung cancer researcher Professor Fraser Brims from Curtin University was one of 13 successful grant applicants in the Federal Government’s recent $5.15 million boost to Cancer Australia’s Collaborative Cancer Research Scheme.
Dr James Leigh is bound for Oxford University after winning an ‘Australia at Large’ Rhodes Scholarship to study the use of digital technology to improve health services in rural and remote areas of Australia. The 23-year-old is a junior doctor at Fiona Stanley Hospital.

continued from Page 6
neurosurgeon Professor Bryant Stokes’s contribution to the Perron Institute and advancement of neurosciences research.
One of two Parkinson’s projects supported concerns the development of a novel RNAbased treatment for early onset forms of the disease. The other is looking to see whether non-invasive brain stimulation can strengthen connectivity in the motor cortex and reduce tremor in people with Parkinson’s.
Understanding why immune cell changes occur in people
developing multiple sclerosis is one of the studies relating to this neurodegenerative disorder. Another is investigating the potential for preventing damage to and restoring the insulating layer of myelin that forms around nerves. Investigating the potential for gene patching therapy to improve cognitive ability in childhood intellectual disorders such as Down syndrome is another project among eight selected for funding.
More than $700,000 was given in the first round of funding.
St John of God Subiaco Hospital recently celebrated 10 years of providing cardiothoracic care and services in WA, marking the milestone with its multi-disciplinary cardiac care team including medical specialists, nurses and allied health professionals.
Cardiothoracic surgeon and Head of Department Associate Professor Jurgen Passage said the establishment of cardiothoracic services at the hospital was a career highlight for him.

Over the past 10 years, the cardiothoracic team had achieved many milestones, including the introduction of the first minimally invasive surgical program, which in 2017 expanded to include the transcatheter aortic valve implantation (TAVI) procedure.
Curtin University clinical pain researcher Professor Helen Slater has won a 2022 Brilliant Women in Digital Health Award. One of 25 recipients across Australia, Professor Slater was noted for her leadership and work in pain care.
TAVI is a minimally invasive procedure that offers eligible patients with aortic stenosis an alternative to traditional open-heart surgery, improving recovery times and ensuring less discomfort.
Since the procedure was first introduced at the hospital, more than 250 TAVI operations have been performed.

From this month, GP training officially moves back into the fold of Australia’s specialist medical colleges – the Royal Australia College of GPs and the Australian College of Rural and Remote Medicine.
They are now responsible for the Australian General Practice Training program, which trains medical registrars to enable them to work as GPs anywhere in Australia. The program is three to four years of full-time training offered in metropolitan, rural, remote and very remote locations nationally.
RACGP and ACRRM will deliver AGPT program training through their respective college-led training models and have set up a company – Joint Colleges Training Services – to oversee the programs.
The move back to college-led training brings general practice into line with other medical specialist training programs across Australia.
Medical Forum asked RACGP president Dr Nicole Higgins what the new training pathway means for general practice.

MF: From 2023, the AGPT program in WA will be run by RACGP and ACRRM. What is the significance of training returning to the colleges?
NH: The return of GP training to the RACGP and ACRRM is an important opportunity for the profession to build on what works and deliver world class training, so future GPs are equipped to meet the challenges of 21st century patient care. Bringing the delivery of the training program back to the colleges brings general practice into line with every other medical discipline nationally.
MF: What will be the impact, if any, on the training for future generations of GPs?
NH: Our priority is ensuring a smooth transition for GPs in training, and their supervisors.
We have designed our delivery operating model, building on and respectful of existing approaches that will minimise disruption throughout the transition. The colleges will continue to build on the successes of the previous custodians of the Australian General Practice Training Program.
The local names and faces in our delivery teams are largely recruited from regional training organisations. They know the geography, the local culture and importantly the registrars, supervisors and training practice staff. They will be central to the program’s success.
State and territory regional leadership and support teams will support these local teams.
Our national leadership teams and support services will provide
national consistency to support systems that enable local delivery. Each regional and local team will have the opportunity to implement regional responses to training delivery that best meets the needs of their communities.
MF: Can you explain the role of the newly formed company, Joint Colleges Training Services?
NH: Our joint venture with the Australian College of Rural and Remote Medicine, Joint Colleges Training Services Pty Ltd (the Company), will oversee joint AGPT training program services.
The company will initially support AGPT activities, including:
• the development and delivery of Aboriginal and Torres Strait Islander health strategic plans, including cultural education and cultural mentorship;
• the provision of registrar housing in remote Northern Territory;
• other potential areas of collaboration to be agreed between ACRRM and the RACGP.
The company will initially adopt the current strategic plans developed by each RTO and then look to develop an integrated, nationally consistent but locally-produced and delivered strategic plan in 2023.
MF: Does GP training need to be more flexible and adaptive to reflect the changing world and the work-life balance?
NH: GP training is an extension of general practice as a profession. General practice has proven just how flexible it can be. It adapted to not just meet, but lead the needs of new world problems like the COVID-19 pandemic responses in Australia over the past two years.
The Australian Government of course play a significant role in enabling the profession’s agility. Telehealth for example would not have been possible without Government support to enable this change to MBS item numbers, which in turn allowed GPs to deliver and bill for consultations online.
We look forward to seeing Australian Government support to continue to enable general practice evolve to meet the needs of our communities as they change.
MF: General practice is facing some major challenges in terms of morale and the Medicare funding model. How is the RACGP approaching the direct responsibility of training the new generation of GPs in the current climate?
NH: As Australia’s largest representative body for GPs, and the next custodians of GP training, our role is also to be strong advocates for GPs, including those in training.
We understand the challenges facing GPs today due to successive governments taking funding from general practice, while at the same time community demand for GP care has increased exponentially due to the impacts of the COVID-19 pandemic, as well as rising rates of chronic conditions, mental health issues, and our ageing population. Our commitment to our members is that we will continue to advocate
for the changes they want and need, to safeguard general practice for the future, and ensure everyone across Australia can access highquality care regardless of their postcode. We know from our latest Health of the Nation report, that funding, work-life balance and wellbeing are of primary concern, particularly due to the growing administrative burden and opaque Medicare rules.
While there are significant challenges, the launch of Australia’s first Parliamentary Friends of General Practice is a significant step towards the voice of general practice being heard loud and clear in parliament.
MF: What changes or improvements will be made to this training journey, particularly for rural generalists’ training?
NH: It’s important to acknowledge that GP training isn’t broken. The Australian GP Training program delivers and maintains world-class primary care.
The transition represents significant change in and of itself. We will ensure continuity in delivery of the program first, taking particular care to ensure our registrars, supervisors and practices are disrupted as little as possible and then look to further opportunities in 2024 and beyond.
MF: What do you see as the role of the WA Primary Health Alliance (WAPHA) in GP training?
NH: WAPHA is one of many Workforce Prioritisation and Planning Organisations charged with mapping supply of the registrar and GP workforce and the corresponding patient demand which will help inform GP training priority areas in 2024 and beyond. WAPHA as a key stakeholder is one of many organisations that will have a voice to inform the college’s approach to GP training via regional advisory councils.
MF: What do governments in general need to do better to support general practice in Australia?
NH: We are continuing to call for more support and funding for patients to access high-quality care through general practice.
The current model of health-care funding in our country is extremely lopsided – more Australians visit a GP every year than any other
service in our entire health system, but funding for general practice patients is less than 8% of total government health spending. We are seeing more and more GPs moving away from bulk billing as Medicare rebates are set nowhere near the level needed to cover rising practice costs. Concerningly, the number of medical students choosing general practice as their preferred specialty is also at an alltime low of 13.8%.
The evidence shows that if we invest more in preventative care for Australians, and measures to keep people well in the community supported by their GP, we will have a healthier population, higher productivity, and lower spending on expensive hospital care. And the RACGP will continue to advocate strongly for this to happen via reforms aligning with our vision for general practice and a sustainable health-care system.
The RACGP has been calling for the Federal Government to implement reforms in the short term to improve patient health outcomes, including:
• enhanced primary care services for people over the age of 65, people with mental health conditions and people with disability
• longer general practice consultations to support patients with complex needs
• improved access to telehealth
• support for patients to see their GP within seven days of an unplanned hospital admission
• improved access to care in rural communities, by encouraging and supporting rural doctors to upskill.
Read this story on mforum.com.au



continued from Page 8
The WA Health Department is supporting a national study into tooth decay in children, with concerns poor oral health can have wideranging effects on their physical and mental health.

Researchers from the University of Adelaide are leading the study which will see more than 30,000 children aged 5-14 from across the country examined as part of a National Child Oral Health Study that will compare findings from the last study in 2012-14.
The four-year study will also followup with about 15,000 teenagers and adults now aged 16-25 years
who took part in the previous study.
The project is supported by various State health departments and the Australian Dental Association.
It is being led by Professor Lisa Jamieson, Director of the Australian Research Centre for Population Oral Health, which is part of the Adelaide Dental School.
“With the use of oral examinations and questionnaire data, we will be able to put the results side by side against what was found in the most recent study in 2012-14,” Professor Jamieson said.
“We will be able to test, model,
West Australian diabetes researchers are investigating if a new medication helping people with type 2 diabetes could also reduce health complications linked to type 1 diabetes.
Dr Lakshini Herat, pictured, has won a $60,000 grant from Perth-based charity Diabetes Research WA to study the effects of sotagliflozin in type 1 diabetes.

Dr Herat, from UWA’s School of Biomedical Sciences and the Dobney Hypertension Centre, said sotagliflozin was already being used in clinical trials to successfully lower blood glucose levels in people with type 2 diabetes.
“This medication is one of a relatively new class of socalled ‘wonder drugs’ known as SGLT1/2 inhibitors which are helping to protect the heart and kidneys in type 2 diabetes by suppressing the proteins in the body known as SGLT1 and SGLT2,” she said.
“Our team has recently discovered, however, that when SGLT2 is blocked, it leads to an increase of the SGLT1 protein in the kidney, possibly limiting the effectiveness of the SGLT2-only inhibiting drugs.”
Dr Herat said that because sotagliflozin was known to reduce the expression of both SGLT1 and SGLT2, it could be a powerful new way to help people with type 1 diabetes, as well as those with type 2.
“SGLT2 inhibitors are so far not being used in type 1 diabetes due to concerns over the risk of diabetic ketoacidosis, so more needs to be known about how sotagliflozin works in the body before it can be prescribed,” she said.
evaluate and disseminate evidence that will enable important questions around child oral health, social and emotional wellbeing, school performance and economic productivity to be answered.”
Tooth decay, otherwise known as dental caries, is the most common childhood infection in Australia.
“Dental caries imposes a large cost on the Australian economy, estimated to be up to $1 billion per year,” Professor Jamieson said.
“It also has a direct coloration to poor school performance, inadequate nutrition, problems with sleeping and adverse social wellbeing.”
Medicare data shows there was a huge uptake of telehealth during COVID-19, with one-third of GP consultations in Australia during September 2020 alone conducted via the technology.
But the marked shift from in-person medical care – born of necessity – has not been without its concerns, particularly in the case of online consultations where the doctor has never previously seen the patient.
Now that the pandemic dust has settled a little, the medico-legal pitfalls are garnering fresh attention, with the release of draft telehealth guidelines from the Medical Board of Australia, as well as changes to the indemnity policy of one of the country’s biggest insurers.
From January 1 this year, Avant’s Practitioner Indemnity Policy cover for telehealth activities changed to exclude telehealth consultations based on online questionnaires and/or text-based chat.
In a statement issued at the end of last year, Avant said the change was due to concerns about the quality of services where there was no real-time faceto-face, video or telephone consultation, and where the practitioner lacked
At the height of the pandemic, telehealth consultations came into their own, but now online-only consults are coming under closer scrutiny, as Cathy O’Leary reports.
access to the patient’s medical records from a previous in-person medical consultation.
Avant said the changes were not intended to apply to pathologists or radiologists.
Around the same time, the Medical Board released its revised telehealth guidelines, which are open for public comment until February 17, and cracked down on the use of online-only consultations. They warn GPs not to rely on text or email consultations for first-time patients.
The draft has a new section on prescriptions that states: “Prescribing or providing healthcare for a patient with whom you have never consulted — whether face to face, via video or telephone — is not good practice and is not supported by the board.
“This includes requests for medication communicated by text, email or online that do not take place in real time and are based on the patient completing a health questionnaire, but where the practitioner has never spoken with the patient.
“Any practitioner who prescribes for patients in these circumstances must be able to explain how the prescribing and management of the patient was appropriate and necessary for these circumstances.”
But the draft guidelines acknowledged that in an emergency, “it may not be possible or appropriate to practise according to these guidelines”, and if no alternative is available, the “telehealth consultation should be as thorough as possible and be followed up with more suitable arrangements.”
“Practitioners should be continuously assessing the appropriateness of the telehealth consultation and whether a direct physical examination of the patient is necessary,” the draft stated.
Many medical groups, including the Royal Australian College of GPs, have already thrown their support behind the proposed guidelines, which they argue are common sense and help address concerns about patient safety and quality of care.
Dr Daniel Heredia , who is the National Medical Board’s practitioner member from WA, said the guidelines had not been revised since 2013, long before the COVID pandemic hit and made telehealth much more commonplace.
He said it had become a big topic of discussion among doctors, given the rise of online services offering prescriptions and referrals without a consultation.

“The peak of COVID is gone, and a lot of things were implemented quickly to accommodate COVID, and now that we’re in a newnormal these guidelines are trying to balance the fact that we have access to these fantastic technologies, but we need to look at how can they be used safely and sustainably,” he said.
“There is some disquiet in the profession around what is called asynchronous medicine, where you can literally send an SMS or fill in a form, and without even seeing a doctor at all, you can be issued with a request form or prescription.”
Dr Heredia said that if the draft guidelines were implemented, it would reinforce the position that, with the exception of some circumstances, a doctor who does not have a prior relationship with a patient should not be issuing a prescription or request form based on an online form.
“You need to actually consult with that patient, and ideally it should be face-to-face and if it can’t be then you have to be able to defend why that wasn’t the case and prove that it was comparable to a face-toface,” he said.
“Having a 10-second conversation
saying, ‘yep just checking that’s you’ and writing a script for medicinal cannabis that is sent to them by SMS – you would have to be able to defend that.”
Dr Heredia said the guidelines were not anti-telehealth in general practice, and he likened it to hybrid working arrangements which had accelerated in popularity because of COVID.
“The world has changed and we’re now in an environment where there is more flexibility, but it has to be balanced, and these guidelines are trying to strike a balance.
“Telehealth is a great modality where used appropriately, as part of a more comprehensive relationship with a primary care practitioner,” he said.

“For following up results, for example, if there is nothing terribly sinister and it’s your usual GP, then why not, rather than driving for half an hour and sitting in a waiting room just to be told everything is pretty much OK other than one result which is off a bit.
“That could be delivered by telehealth and it might be more practical to do so in some cases.”
Dr Heredia said that many doctors wanted some clarity in the postCOVID period about the right mix and what was acceptable in the use of telehealth.
It would also help them deal with pressure from patients, who sometimes wanted to jump online quickly and get what they want.
“Doctors could find it protective because the guidelines give them something to use to defend themselves if patients are pushing to be very transactional without necessarily understanding the risks,” he said.
Feedback on the proposed guidelines can be made by emailing written submissions marked ‘Consultation: revised telehealth guidelines’ to medboardconsultation@ahpra.gov.au by February 17.
A ground-breaking WA project to track the health of young children has notched up a significant milestone and is now playing a key role in global research.
Eric Martin reportsAfter setting out in 2017 to follow 10,000 children and their families for a decade, The ORIGINS Project has started celebrating their first five-year-olds coming through the program from July last year. And while the project hopes to continue following these children and their families into adolescence, Medical Forum caught up with ORIGINS co-director, paediatrician and director of research at Joondalup Health Campus, Professor Desiree Silva , to discuss the outcomes that have already been achieved.
“It is an absolute pot of gold for WA, which we have developed in a fairly short space of time,” Professor Silva said. “It really is a fabulous concept – the dream of helping every child reach their potential – and through ORIGINS we are actually giving children the opportunity to reach it.
“We are collaborating with different researchers, both here and internationally, but I think we are taking the lead on this intervention-style of birth cohorts, certainly, from a national viewpoint. We already have over 16,000 individuals in our group, including the children, their mothers and some fathers or non-birthing partners.”
Professor Silva explained that while intervention birth cohorts have gained in popularity over the past few years, ORIGINS was one of the first to use the approach – a unique way of improving children’s health as they participate in longitudinal research.

“Normally you would observe a birth cohort and describe your findings, without necessarily following that group up until many years later, but with ORIGINS, we are actually creating a platform that enables us to perform intervention as well as observational studies,” she said.
“This means that we are actively trying to improve the lives of those children at different time points – to change their trajectory. If we find something that is not right or can be done better, then that is exactly what we will try to do for our participants.”
Real-time feedback is given to families if an issue is identified and, so far, the team has identified a broad range of concerns in some children, such as developmental delay, sleep problems, growth issues, allergies, iron deficiency and behavioural challenges.
“The main aim is that we want to look at ways to reduce the epidemic of

non-communicable diseases,” Professor Silva said.
“It is not just the COVID tsunami that we are dealing with, we have a pandemic of chronic disease beginning with young children, right up to the elderly, and a significant proportion of these noncommunicable diseases are preprogrammed early in life.
“By providing a healthy start to life and improving our understanding of early pre-programming, we hope to help prevent some of this huge burden of chronic disease.”
Professor Silva said ORIGINS had a particular focus on epigenetics, the process by which an individual’s genes are activated by the environment, switching that gene on or off.
“What we are trying to understand is, what is causing these genes to switch on? What is it in our environment that has changed? What are we eating, what are we breathing that is different? We start looking at the environmental exposure of the mother during pregnancy and continue right through childhood because we know that early exposure probably does impact epigenetics.”
A recent focus has been on the impact of microplastics building up in the placenta during pregnancy,
a topic that has featured in several small studies but has been challenging to validate due to methodological difficulties.
“These studies have attracted huge criticism because not only do we live in a plastic environment, but the samples were also collected using plastic gloves and placed into plastic tubes – maximising the potential for exposure,” Professor Silva said.
“So, we are now collaborating with the Minderoo Foundation, University of Queensland and University of WA looking into this, trying to ensure we collect our samples in a pristine way before they are transferred to the lab in Queensland – a predominantly plastic free environment, set up by the Minderoo Foundation.”
Similarly, the team has been collecting amniotic fluid using plastic-free materials to determine if it has also been contaminated by microplastics.
“You can see I get excited about all this! However, the main aspect is that we have created this incredible research platform that enables lots of projects to be established using our birth cohort,” Professor Silva said.
“For example, we have studies in allergies prevention, obesity reduction, how to improve children’s mental health, how to improve fathers’ health.
“We expected about 25% of children to develop eczema by the time they turn one, but we are actually finding in our cohort that about 40% of them have got some level of eczema. But why is that the case? And why does that seem to be going up every year?”
ORIGINS research has already suggested that there really could be something to the old adage that playing in the dirt will help to develop a strong immune system.

“We're finding that nature is vital for our microbiome,” Professor Silva said. “The bacteria that we engage with outside is really important and we have a great intervention study collaborating with Nature Play WA, working with children about three years of age and bringing them out into nature, so that they can develop their resilience through various activities.
“Yet at the same time, electronic use has distracted people from being outside and we collect a lot of information on the impact that can have in both a positive and negative way, which provides balance to the research.
“We are also asking parents about their children’s sleep, their attention span, and about their behaviour.”
continued on Page 18
continued from Page 17
As the ORIGINS study matures, it is demonstrating a growing ability to investigate transgenerational effects. It will look to enrol grandparents to explore behaviour and environment during a woman’s pregnancy and how that might affect their children’s fertility and egg quality.
“The Raine Study is already doing that. It is about recognising the if you really want to know about why someone has developed something, you have got to go back a few generations as well,” she said.
An unlikely meeting with the former Mayor of the City of Wanneroo, Tracey Roberts – now the federal Member for Pearce, on a flight back from the UK, helped bring ORIGINS to life.
“We spent the entire flight plotting and planning,” Professor Silva said.
“In the Wanneroo area at the time, there was some information published on school readiness, which showed that this was a very high-risk area for schools, with pockets of poor performance compared to the national average.”
There were also high rates of developmental disorder,
mental ill health, obesity and chronic disease.
“It really was an ideal cohort of people because we wanted to capture the whole population of an area, identify problems as they arose, and direct individuals to the services they required, or try and prevent them from developing those issues in the first place,” she said.
“At the same time, my co-director, paediatrician Professor Susan Prescott, had authored a book called ORIGINS – on the origins of disease – and it was a great fit to run this cohort at the Joondalup Health Campus in collaboration with the Telethon Kids Institute (TKI).
“Joondalup Health Campus is almost at a tertiary level with all the exciting research and teaching that is happening here. I have recently been appointed the inaugural Director of Research, where previously I was the Head of Paediatrics for over a decade.”
Professor Silva explained that through their collaboration with TKI, ORIGINS was assisting autism spectrum disorder expert Professor Andrew Whitehouse in developing new video technologies that could help parents better communicate with their infants.
“Andrew's group is specifically looking at is this video technology which is helping to reduce the severity of some of the features of autism in an at-risk population, something that again, is quite unique,” she said.
“The work that will come out of this is really important because if you can actually prevent those features from developing, or reduce the symptoms of autism, that will have a huge impact for so many families.”
Professor Silva also highlighted the outcomes of another critical study run through Curtin University called Early Moves, which is using home videos to investigate certain movements in babies, as early as two weeks of age, to determine their risk of experiencing developmental difficulties.
“We know that at four months of age, an absence of certain movements in babies is almost 95% predictive of cerebral palsy,” Professor Silva said.
“Those babies’ movements are like a video into their early brain development. If they do not have a particular movement then their risk of cerebral palsy is extremely high, and as a result they would be investigated very early on, rather than waiting to find out later in life that they have problems with their motor skills.

“Knowing that you have over a million neuron connections occurring every second, you can really shape things differently if you intervene early. I never would have dreamt that you could find a way to increase the IQ of a population yet potentially, through Early Moves, we do.
“The benefits of these nested studies is that the researchers for Early Moves, for example, are doing quite detailed developmental checks at two years of age, before looking for more funding to do progress to early school years and we also get those results, which can then be compared with other studies.
“For example, once we know how to analyse microplastics in a manner where we are confident that the methodology is acceptable, we could combine that data with the analysis of children’s
movements to further investigate microplastic’s impact on their development or allergy outcomes.”
Significantly, ORIGINS is one of the only studies globally to have collected such a huge dataset both before, during and potentially after the pandemic, particularly in relation to Omicron.
This could have significant value for researchers looking at long-COVID in children because of the way that ORIGINS is structured, collecting data twice during pregnancy, with samples and measurements taken at the birth, followed up by questionnaires and more samples taken at one, three and five years of age.

“Some participants would have had COVID while some wouldn't, but opportunistically, we have also been collecting samples that can be looked at to evaluate whether there are changes in an individual’s metabolomics in relation to COVID exposure,” she said.
“A body of work was also undertaken to look at the health and wellbeing of our ORIGINS families at the height of the pandemic, including the impact of forced lockdowns and financial pressures, but our platform is collecting data, so we will have to find other funding to help with the analysis of that.
“We have this gem, this absolute pot of gold, and we need to find funding to analyse all of these
samples – it is going to create a huge amount of discovery just from analysis.
“These samples are just sitting in freezers, and we need to look at them; we have dust samples collected during pregnancy that fill up rooms and rooms; we have over 300,000 samples in the biobank and that will grow to almost a million by the time we finish this project.
“We want to source funding to scale and be able to analyse a lot more samples in multiple ways: what we'd like to do is to say, ‘OK, yes, you can analyse it, but then go on to investigate all these other aspects as well – don't just do one thing’.”
Professor Silva said there had been a great deal of interest in ORIGINS from the international scientific community now that the data set has grown so substantially, and the project enjoys strong collaboration with Born in Bradford, another intervention birth cohort from a disadvantaged area of the UK.
“We have done some comparative work with COVID and published a paper looking at the mental health effects of COVID in these two very different populations, which interestingly showed that even though we escaped in some ways, the mental health impacts were still comparable,” she said.
“The impact of the virus within families was still very, very high.”
As a paediatrician who works in the mental health space, Professor
Silva pointed out that even before the pandemic, mental health was a significant issue.
“Pre-COVID I would see some children as young as seven, and it was not uncommon that they would present with suicidal ideation,” she said. “We are collecting measures very early and we have certainly seen several children at three and five who were extremely vulnerable.
“All the paediatricians in this area would concur with me that it is quite a frightening situation to be in, to see children that young and that vulnerable. And if they are also impulsive, they will do it if they can, without thinking it through, which is terrifying for families, especially when services are so difficult to access.
“But over the pandemic, things have got significantly worse, and now, the issue is that a lot of these children are on wait lists, which is a real concern for parents as they do not know what to do.
“Yet by being able to direct them to appropriate services at a very young age and support their parents, I think that is where many families have been very grateful for being involved with ORIGINS.”
Recruitment for ORIGINS
(mothers between 20-38 weeks pregnant) ended last December, and Professor Silva explained that due to the current shortage of paediatricians, ORIGINS asks parents to fill out a range of important questionnaires for review, to ensure that they capture any immediate concerns and provide this information back to families.
“We are certainly working on detecting issues in children at one year to 18 months old and directing them appropriately,” she said.
“But we are also using the information that we have gathered to develop technology that can help parents to identify an issue and then direct them to services.
“We must find novel ways to achieve this, using the technology that we have now to create new models of care – there are just not enough specialists around to be able to see people in the way that we used to.”
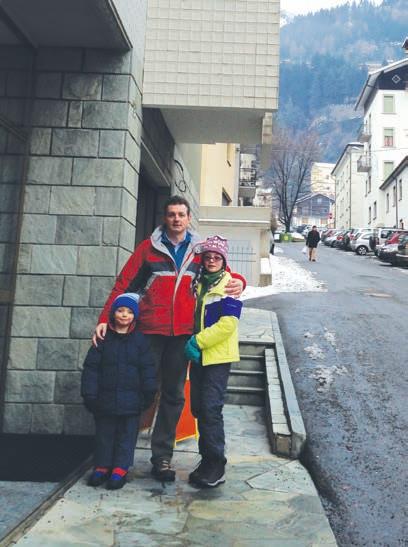
Nick Gottardo only ever wanted to be a doctor and one childhood story has always stuck with him and probably had something to do with it.

Born in the UK, at three months Nick’s father moved his family back to his homeland of Italy. The Gottardos lived in the northern Italian town of Sondalo, home to the E. Morelli Hospital, a 2500-bed tuberculosis sanitorium. By the end of World War II, Villaggio Morelli was the biggest of its kind in Europe and featured deckchairs on the sheltered terraces for aero therapy, which came complete with stunning mountain views.
Sondalo is a mountain village and Nick’s dad Renato, a chef, ran a local hotel. He was also a regular blood donor.
A girl at Nick’s school, named Nadia, had leukemia. In a very clear memory, Nick remembers Renato leaving the house late one night to donate blood because a child was critically ill. He returned some hours later looking visibly shaken. The child, who turned out to be Nadia, had died.

Often it isn’t until years later that we realise how a childhood experience might have shaped us. For Dr Nick Gottardo, there’s a likely link between his choice to research and treat children’s brain cancers and his early years in a small Italian town.
Renato is now 75 and still carries a photo of Nadia in his wallet. He has visited her mother over the years when returning to Italy.
“Nadia was going through leukemia treatment in the late 1970s,” says Nick, a children’s brain cancer specialist. “Had she been born later she might have lived. It hit my dad hard that he couldn’t help save her. I didn’t know what leukemia was at the time. I did know it was traumatic because my father was traumatised by this child’s death.”
Nick grew up speaking only Italian, so when his parents returned to the UK as an eight-year-old, he became a migrant in his own country, in a special class with other kids who couldn’t speak English and had come from all corners of globe.
From his earliest memories, a couple of things stuck in his head about medicine. Two sets of family friends had doctors in them who worked at the sanitorium, plus the spectre of the place literally hung above his Italian home.

By his teens, Nick remained resolute about becoming a doctor but as he was much better at history, French and the arts over sciences, people tried to steer him into law. He was adamant that chemistry, biology and physics were his path and he worked hard to get good grades. Better at biology and chemistry than maths, he also chose Latin because his dad told him drug names were derived from the language.
He was offered a place early and did a Bachelor of Medicine and Bachelor of Surgery from Leeds University. Paediatrics and GP work were the two things which had interested him the most as he moved around his rotations and into residencies.
He worked at the family’s Italian restaurant to put himself through his studies, which apparently did wonders for his bedside manner. Even after he became a qualified doctor, he still put on an apron or hopped behind the bar because he enjoyed it.
Working at Leeds General Infirmary solidified Nick’s decision to become a paediatrician. “I loved working with children and had phenomenal seniors who supervised me.”
By then, he had become known for wearing cartoon and Disney ties. So much so that when he turned up to a job interview wearing a
more conservative tie, the panel questioned his choice.
On seeing an advert for a job in Australia in 1996, Nick headed to the Blue Mountains and worked there for six months. He was eventually lured west by English friends in hospitality who had settled in Perth and he worked as a locum around the State. On the odd Saturday night, he’d wait tables in Perth when his chef friends needed a hand.
While he enjoyed the locum work, Nick’s heart really was with kids. A cold call to PMH got him a job
and he later began a PhD at the Telethon Kids Institute.
“I really fell in love with the specialty. I had looked after this boy who passed away from leukemia and I thought ‘I really want to make a difference and stop him from dying’. He fought so hard and still passed away.”
Becoming part of Kyle’s Camp (through the Kyle Andrews Foundation), a Broome getaway for sick children named after a local boy who had died, further confirmed he had made the right choice. It was Kyle who inspired Nick to do his PhD on T-cell acute lymphoblastic leukemia, a rare and aggressively malignant cancer.
Wanting to learn more, he later spent three years at St Jude Children’s Research Hospital in Memphis, Tennessee, one of the world’s premier childhood cancer institutes. Working as a postdoctoral brain tumour fellow, he gained extensive experience in the lab in brain tumour model generation, preclinical testing and brain cancer cell biology, as well as expertise in the management of children with brain tumours.
“The team was seeing 150 children a year with brain cancer compared to the smaller numbers we were seeing in Perth. They were doing cutting-edge work and writing the book on it, while I was learning how to look after children with brain cancer.
continued on Page 23
Sexual Health North, in Joondalup, we offer a wide range of services for our patients from the diagnosis and management of STIs, HIV, PrEP, Hepatitis B & C, trans and gender diverse health care for those over 18 years old, genital skin conditions and vulvovaginal medicine. Newer services include the provision of long acting reversible contraception (LARC) including intrauterine deviceshormonal and non hormonal.
As our service grows, we will expand and offer further services. Our clinic strives to create a friendly and knowledgeable service in an open-minded atmosphere. We aim to work with our colleagues in primary care and specialist settings for the total wellbeing of our mutual patients. We would also be happy to take calls about your patients.
MBChB (U. of Auckland), FAChSHM
Dr Christine Dykstra trained and completed her fellowship at Royal Perth Hospital, where she has been a specialist sexual health physician for over a decade. With a keen interest in improving sexual health care in Perth, Christine has provided sexual health medical education at various universities and postgraduate programs in Perth.
Her most recent role in research was as the principal investigator for the Royal Perth Hospital site of the WA PrEPIT trial for the provision of HIV pre-exposure prophylaxis in Western Australia. Having lived in Perth’s northern suburbs for many years, Christine is happy to finally bring specialist sexual health care to the Joondalup and Wanneroo regions.


MBChB (U. of Liverpool, UK), FAChSHM, MRCP (UK), DIP G-U-MED, DFSRH
Dr Michelle Yong initially gained her experience in sexual health and HIV management at Royal Liverpool University Hospital, UK. Moving to Perth in 2012, she continues to develop her clinical skills at Royal Perth Hospital including transgender medicine.
Sexual health issues can feel embarrassing for many patients. Michelle excels at putting patients at ease with her non-judgmental and empathetic manner along with a healthy dose of humour. She would like to put her expertise to good use by setting up specialist sexual health service to serve the communities of the Northern suburbs.
In order to help reduce the rates of STIs in our community, we offer our patients the opportunity for on-site consultation, pathology / investigations , and medication dispensing with many acute STI treatments. For acute STIs, we try to keep fees to a minimum. You can contact our friendly team to discuss your patient’s needs.
continued from Page 21
“All that work gave me the grounding to be an independent doctor and researcher. I remain passionate about this and have seen major changes over the years. We’ve done all this research and there’s still so much to understand about brain cancers – there are more than 100 types.
“We do, however, understand them much better than when I first started. I’m a piece of a very large puzzle with people around the world. Together we have a much better understanding of the diseases and we’re trying to find more effective and less toxic treatments. The battle is ongoing.
“I still think about Nadia. Especially given we now cure 80-85% of children with childhood cancer.”
Today Nick is co-head of the Telethon Kids Institute's Brain Tumour Research Team and a Consultant Paediatric Oncologist/ Neuro-Oncologist and Head of Department of Paediatric Oncology and Haematology at Perth Children’s Hospital. He’s also an Adjunct Associate Clinical Professor at the University of Western Australia.
Married for 24 years to WA local Carolyn, the couple have two children – Alyssa who is studying pharmacy and 13-yearold Bryce. Dad and son mountain bike together and Nick plays cameraman for Bryce’s YouTube channel about remote control rock crawler cars.


The Gottardos have also travelled extensively together. That’s when Nick has time to put his “decent knife skills” to use, cooking fancy meals for friends and family.
A recent black belt in tae kwondo, Nick wanted to continue with martial arts while living in Memphis. Unable to find a dojo, he discovered a local karate school and at 35 went back to being a white belt. Turns out, it wasn’t just any karate school but the Tennessee Karate Institute — the martial arts school that Elvis co-founded.
Nick’s chief instructor was former Tennessee Supreme Court Chief Justice Janice Holder, a fifth degree
black belt alongside Elvis’ friend and partner, Grandmaster Patrick “The Viper” Wrenn.
“Elvis was into martial arts and he credited it for his mental health. It was a very interesting experience to meet these people and be exposed to a different kind of martial arts,” Nick says.
“A couple of years ago my son was watching the show Cobra Kai (a spin-off of The Karate Kid on Netflix) and suggested I get back into tae kwon-do. I started from the beginning with Bryce. I’ve currently got a yellow belt with a green tip and at 52, am one of the oldest in the class.
“For me it’s a time to switch off
from work and spend time with my son. I really have to connect with the movements and don’t have time to think about something I have to write or check on or review.”
Nick’s philosophy is that while he might not be able to stop all the children he treats from dying, he can make their lives the best they can be for the time they have left.
“I always try my best to find the best treatment and go with the attitude of doing the most to defeat the tumour. There are some that are incurable, but you think about extending a child’s life with quality by using all the science, training, knowledge and connections you have. If you work with that principle and do the best you can and buy them some quality time, that’s how I reconcile it. I recognise I can’t save them all.”
It’s the support of his wife and kids which get him through the times which are overwhelming. “Kids with cancer are resilient and I am constantly inspired by them. It’s amazing what they go through. They pick themselves up, dust themselves off and get on with it.”
 Martin reports
Martin reports
With up to 57 West Australians hospitalised every day due to alcohol-linked conditions, last year’s opening of a private 30-bed specialised addictions inpatient service in Nedlands met a need from day one.

Patients to the Ramsay Clinic Hollywood can be admitted for a period of detoxification while engaging in therapy focusing on addictions recovery and harm minimisation.
Psychiatrist and Medical Director of Addictions, Dr Kavita Seth, who also works at Fiona Stanley Hospital, said the main drive to open this ward at Hollywood was because of the scarce number of services providing inpatient detox.
“I work with Dr Cathryn D’Cruz, who is a GP with extensive experience in addictions medicine, and we work as a team catering for both the physical and mental health needs of patients,” Dr Seth said. “Cathryn oversees the addiction and physical side of things in both the detox space and for those with long-term addiction management needs.
“And then I explore, with the patients, why they self-medicate –and most of the time it is untreated mental health issues or past trauma – before talking to them about the suitability of medications or a combination of medication and psychology.”
Dr D’Cruz said that from a GP’s perspective, it was important that people address their addiction issues, but a GP could only do so much.
“Occasionally, patients need to come into an inpatient setting to be detoxed because for some people it is just not appropriate to detox at home,” she said.
“What I particularly like about this service is that not only do people get a safe detox, supervised by medical personnel and experienced addiction nurses, they get the benefit of a psychiatrist who is also an addiction specialist. And that is rare.
“Addiction is so tied up with mental health and that issue must be addressed as well.”
Having the detox unit located in a
hospital had the added benefit that an emergency team is on hand.
“You have the backup of an ED, a functioning pharmacy, fully-trained mental health nurses and allied health as well as access to inpatient referrals for the co-morbidities that people with addiction issues often have,” Dr D’Cruz said.
Pain specialists, liver specialists or a cardiologist are a call away, Dr Seth said.
“The key thing is that the staff feel well supported and the patient feels like they are getting much more holistic treatment. They are not just coming in and getting an addiction dealt with, while the underlying issue remains unresolved.”
Dr Seth also pointed out the value of the follow-up outpatient service, with all Nickoll Ward patients discharged into one of the substance recovery programs on offer.
“Patients are encouraged to participate in support groups such as Alcoholics Anonymous, and AA
continued on Page 27

Eligible HBF members* can now access this support program which reflects the latest evidence in osteoarthritis research, delivered and supported by trained physiotherapists.
Fully covered for eligible HBF members*
Eligible members can access the program at no additional cost when delivered by a participating Life Ready clinic.
Proven 33% reduction in pain intensity on completion of the program1
3 months after the program, participants experienced an average pain reduction of 33%. There was also an average improvement in joint-related quality of life of 31% for knee participants, with 47% of these participants also reporting a reduction in use of pain relief medication.
Applied to everyday activities – enhancing success
Participants are provided education sessions and given exercises that are suitable and practical for everyday application.
Group sessions delivered by physiotherapists
6 weeks of exercise sessions, education classes and follow up to help patients manage symptoms and develop long term habits.
Aligned to national and international clinical guidelines for osteoarthritis treatment
For more ways HBF can support your patients with a range of health programs visit hbf.com.au/health programs
continued from Page 25
is invited to come into the ward and introduce themselves, because sometimes patients are quite hesitant about attending these sort of support groups once they have left our care.
“These patients often carry stigmas about the possible exposure of their treatment and being introduced to these services in the hospital actually alleviates many of their fears and gives them access to more support on the outside.
“We even have carers’ nights where carers are welcome to ask any questions they might have, and seek advice on how to look after their loved ones after they leave hospital – to help them identify what to look out for, early warning signs and what they should avoid”
Dr Seth said that while there used to be more typical indicators associated with addiction in the past, such as a lack of social support or long-term unemployment, when COVID emerged, the prevalence of substance-use disorders went up exponentially.
The negative impact of these behaviours on people’s lives had been profound. For example, in 2020, 78% of West Australians reported being concerned about the impact of alcohol on mental health, and in 2021, WA Police attended more than 25 alcoholrelated family assaults each day.
“The biggest referral we get is for alcohol dependence and one possibility as to the reason why is its ready availability,” Dr Seth said.

“We have a lot of professional people coming through – in fact, we have nearly all the professions represented in our demographic – and they feel safe and comfortable here as we maintain strict confidentiality.
“For many professionals, there can be a lot of concern about the potential to lose their registration, in addition to the sense of shame. We support them and then they go back to work functioning, it's really rewarding.”
Dr D’Cruz said the early detection of problems was important.
“If people come in early, who are encouraged by their partner or their workplace to attend, they are still employed and have not burned any bridges yet. These are the people we love to see so that we can get them functioning back in society, in their personal lives and their occupations,” she said.
“But in the end, the most striking thing is that they want help and know that it is the right time for treatment – they have had that light bulb moment.”
Dr Seth said the usual drivers of action were partners – saying things such as, ‘if you don't get into a hospital and address your addiction issues now, this will be the end of our marriage’, or employers saying, ‘you have to improve your performance, take the time you need just to get yourself sorted out and come back’.
However, workplaces have stepped up to improve employees’ mental health.
“Employers and managers are becoming more accommodating and accepting of mental health aspects with often underlying addiction issues and are providing that support,” she said.
“As it becomes more prevalent, it is also becoming more common in the workplace to find either someone with lived experience or someone living with a person with mental health issues, which is having a big impact destigmatising mental health and addiction issues.
“It's not like back in the old days, when taking the time to get yourself sorted out could get you fired. Now, people are supported by being able to sit and talk with someone who has a mental health background and then a plan is made for a transition back to work.”
Dr D’Cruz said there was good capacity within the new service, so if a GP identified someone who needed help, it was available.
“It can really help GPs get effective treatment for some of those patients who can be hard to manage at times. If they do refer, the patient will be reviewed by a psychiatrist and other specialists if needed and we will always write back to the GP – the communication is there.”

Allowing multiple prescribers will have a detrimental effect on antibiotic resistance, says Dr Ramya Raman

A 15-month-old baby who attends day care is brought in by her mother to see me. She is worried that her baby has had a cough for four days, has a runny nose, is feeling warm to touch, has had reduced intake of solids and is generally grumpy. In the era of the pandemic, COVID-19 certainly crosses our minds.
So, we triage this baby over a phone consult and then wear a mask and review in person in our rooms. On examination, the child is alert, and examination is mostly unremarkable except noting some erythema in the throat.
The mum asks: ‘Does my baby need antibiotics? She has not been sleeping and it’s the fourth time she has been unwell in six months. She has been so grizzly, and her nose just keeps running and she is not sleeping well. Can you please just give us some medication? My friend’s daughter had an issue like this and she had antibiotics which just cured everything.’
This is not an uncommon encounter in general practice. Patients ‘demanding’ or ‘requesting’ antibiotics can lead to overprescribing. Responding to the pressure to prescribe can be managed by foreshadowing a non-antibiotic outcome and using persuasion when confronted with resistance. This is about how medical practitioners communicate and when they communicate.
Safe prescribing relies on accurate diagnosis. In medicine, research has shown that clinical reasoning is not a separate skill acquired independently of medical knowledge and other diagnostics skills. Instead, it is a stage theory of the development of medical expertise, in which knowledge acquisition and clinical reasoning go hand in hand.
This is a complex process where, initially, medical students take in large volumes of knowledge about
basic sciences, there is knowledge accretion and validation, then integration from various domains including clinical sciences, biochemistry, pathophysiology to name a few. The next stage of learning evolves where there is encapsulation of biomedical knowledge into clinical knowledge, which arises from a range of clinical encounters.
The process relies on extensive medical experience and training which helps to ensure medical governance for prescribing in a clinical encounter. It is commonly referred to as ‘illness scripts.’ Therefore, people whose knowledge is organised in illness scripts have an advantage over those who only have semantic networks at their disposal.
While problem solving, a medical practitioner activates one or a few of these illness scripts. Subsequently, the illness scripts are matched to the information provided by the patient. The illness scripts not only incorporate matching information given by the patient, they also generate expectations about other signs and symptoms the patient may have. This leads us, as clinicians, to seek a history and perform a physical examination.
In this process, expected values are substituted by real findings, whilst scripts that fail are deactivated, which leads to a list of differential diagnoses. During this process, illness scripts are adjusted based on specific features of the patient. It is evident that medical training and expertise is obtained through years of experience, is a dynamic process and reliant on reflective reasoning, yet non-medical prescribing is becoming vastly incorporated into many jurisdictions in Australia.
Allowing more non-medical prescribers in Australia will increase antimicrobial resistance (AMR) –making infections harder to treat and raising the risk of disease spreading and severe illness. The World Health Organization has declared AMR one of the top 10 global public health threats facing humanity, with an estimated 1.27 million deaths due to resistant bacteria in 2019 alone.
Misuse and overuse of antibiotics are the main drivers of AMR. The Queensland Urinary Tract Infection Pharmacy Pilot (UTIPP-Q) is one such example that has raised significant concerns about injudicious use of antibiotic
continued on Page 30

A program developed by Danish researchers is now a non-surgical option for Australians with osteoarthritis, explains HBF’s Dr Daniel Heredia

One in five Australians over the age of 45 has osteoarthritis. The biggest risk factors are age, inactivity and obesity, and it is more common in people aged over 40 or those who have had a prior joint injury. Family history can also play a part.
For some people, symptoms are relatively mild but for others the symptoms are severe, ongoing and debilitating. The good news is that for most people, osteoarthritis can be effectively managed and the outlook is positive.
RACGP clinical guidelines recommend that joint replacement surgery is only considered once conservative management options (patient education and exercise therapy, combined with weight reduction, if necessary) have been exhausted.
However, the provision of lifestyle management support is relatively infrequent in Australia. Physiotherapy programs can be prohibitively expensive and even when exercise is recommended, patients are sometimes deemed to have failed non-surgical management without having received a sufficient exercise dose.
To support patients and referrers seeking high quality conservative
management for OA, including adequately dosed exercise, HBF offers the internationallyrecognised GLA:D program to eligible members at participating Life Ready clinics in WA.
What is GLA:D?
Good Life with osteoArthritis: Denmark (GLA:D) is an education and exercise program developed in 2012 by Danish clinical researchers to help people with hip or knee OA to manage or reduce their symptoms. Introduced in Australia in 2017, it is overseen by La Trobe University to ensure the program’s delivery is to University of Southern Denmark quality standards and guidelines.
Two group education sessions and 12 supervised small group exercise sessions (over six weeks) are delivered by physiotherapists or exercise physiologists who have been trained and certified by GLA:D Australia.
The program is based on evidence supporting the use of education and exercise therapy to manage hip and knee OA. While surgery can be a highly effective option for many people living with OA, GLA:D provides people with quality education and exercise support that can prevent the need for surgery.
continued from Page 29
prescribing. There is evidence that points to pharmacists overprescribing in comparison to medical practitioners and increased availability of antibiotics will increase the emergence and spread of resistance.
Recently, in clinical practice, we
are seeing a shortage of many medications including amoxycillin, which has been attributed to ‘manufacturing issues.’ This has led to the need to prescribe second or third generation antibiotics for common bacterial conditions, particularly in children. This increases the risk of AMR. In this mix, add more non-medical prescribers and we are setting
All consenting program participants are enrolled into an online data registry – the largest allied health registry in Australia for any chronic health condition, according to Associate Professor Christian Barton, the co-project lead of the GLA:D Australia program. The registry is managed by researchers at La Trobe University and supports long-term evaluation of program efficacy in improving management of OA and surgery avoidance.
By December 2022, more than 2500 physiotherapists and accredited exercise physiologists across the country had completed training through GLA:D Australia.
HBF has funded certified training for 57 Life Ready physiotherapists and is the first private health insurer to offer GLA:D as a fully covered health support program to eligible members.
The program’s efficacy now runs in Denmark, Canada, China, Switzerland, New Zealand, Australia and Germany. Between January 2018 and December 2021, more than 10,400 people had undertaken the program in Australia, of which:
• 82% reported their knee as their primary problem joint
• 80% of the knee participants
ourselves up for a public health challenge.
The Global Antimicrobial Resistance and Use Surveillance System (GLASS) 2022, recently published common bacterial infections with increasing resistance is on the rise. This includes over 60% of Neisseria gonorrhoea isolates and more than 20% of E.coli isolates, which is the
.
and 71% of hip participants were overweight or obese
• 74% of knee and 68% of hip participants had OA symptoms for more than a year when starting GLA:D
• 42% of knee and 25% of hip participants had undergone previous surgery
• 61% of knee and 58% of hip participants had other health conditions such as high blood pressure and high cholesterol.
After three months and 12 months:
• the average knee/hip pain
intensity decreased and was maintained
• medication use decreased and was maintained
• average joint-related quality of life increased, and
• participation in and confidence undertaking physical activity increased.
In addition, a substantial proportion of participants who wanted surgery at baseline had not had surgery and no longer desired it after the program, reflecting a shift in attitudes and suggesting
an opportunity for minimising unwarranted surgery.
The program is safe for older adults and has advantages beyond OA management. Many Australians with OA have at least one other chronic disease – most commonly cardiovascular disease, back pain and mental health conditions, all of which can benefit from increased exercise and physical activity.

most common organism causing urinary tract infections.
We need to consider the impact of expanding scope of practice on promoting higher use of antibiotics leading to AMR. Health policy needs to be designed with a strong commitment to adequate surveillance programs, prompt diagnostic techniques and robust
research initiatives. We also must consider increased funding for general practice, which will drive better health outcomes for patients and, ultimately, reduce patient hospital admissions and re-admissions.
As Newton’s third law states, ‘for every action there is an equal and opposite reaction’. We need
to consider each of our actions particularly considering our health care policies to ensure we maintain social and economic resilience.
“We have had twelve fit-out contract companies at
St John Of God - Wexford Centre site, and without doubt Medifit Design & Construction stands head & shoulders above the rest for professionalism & quality, I have no problem recommending Medifit for any future works”.
Since 2002, Medifit has helped hundreds of healthcare providers create their dream practices. Our award winning design and construction service will deliver a practice that will enhance your working life and we do it with integrity and transparency from our Perth Head Office.
As Australia’s premier healthcare design and construction provider, we know what it takes to create a beautiful, productive working environment.


If you are considering space at Murdoch, contact Medifit today for a no obligation consultation.

The acute stressors of the pandemic may have settled but many health professionals are feeling prolonged stress and high levels of burnout. Dr Melissa Black explains.
Many of the stressors that we hear about at The Essential Network for Health Professionals (TEN) existed long before COVID-19 and will continue to exist afterwards, which is why looking after your own and colleagues’ mental health is so important.

The pandemic highlighted both the acute and ongoing mental health needs of health professionals. This cohort faces unique pressures and the mental health needs are constantly evolving. TEN was created by health professionals for health professionals, to address the need to access convenient, confidential support for mental health during the COVID-19 pandemic and beyond.
To date, more than 75,000 healthcare workers have visited the e-health hub via the Black Dog Institute website and over 16,500 digital mental health assessments have been completed.
The website provides a suite of mental health support resources and services, most of which can be accessed anonymously and at any time. Through this service, health professionals can choose combinations of care that match their individual needs including:
• A navigating burnout resource to help people to manage and minimise the impact of burnout in themselves and their colleagues. The course is divided into nine short sections so you can easily squeeze them into your day. Some sections take as little as 10 minutes to complete.
• Digital mental health checkup to assess your own levels of stress, depression, anxiety, burnout and traumatic responses and access suitable resources.
• Online fact sheets and resources covering a range of mental health, workplace and life stressors.
• Links to the Hand-N-Hand peer
support network , a preclinical service connecting you to an individual or a group of peers for support.
• Access to the TEN clinical service, providing up to five confidential, one-hour sessions with a clinical psychologist or psychiatrist at Black Dog Institute. This is a free, confidential national service delivered via telehealth and health-care workers do not require a referral to access them.
Black Dog Institute clinical psychologists and psychiatrists have worked with over 200 health-care workers over the past few years to provide support and referrals for a range of difficulties. Burnout is the most common presentation, along with depression, anxiety, post-traumatic stress, workplace difficulties, and family/relationship concerns.
Burnout is a form of exhaustion that’s largely caused by persistent stress at work. Symptoms include both emotional and physical exhaustion, low motivation or mood; feelings of isolation and disengagement; procrastination; irritability; and physical responses such as disrupted sleep, headaches and body pains. These symptoms can look like depression and anxiety but are primarily caused by workplace pressures.
Many of these health professionals
have told us that that they were not comfortable accessing support through their workplace or traditional Medicare pathways, due to concerns about confidentiality, mandatory reporting and the stigma associated with seeking help.
As a national telehealth service, TEN provides support for health professionals all over the country –increasing access to mental health support for those who may not wish to speak to colleagues in their own communities and professional networks.
We often provide care for other health professionals, but also need to apply the same care to ourselves. Just like putting on your own oxygen mask first, looking after your own wellbeing allows you to be at your best for yourself, your patients, and your loved ones, and last the distance in our rewarding and taxing care professions.
The beginning of a new year is a great time to check in on how you best look after yourself, and this will look different for every person. It is important to work out what’s important to you in both your life at work and outside of work, and what fits with your schedule to make these practices sustainable in the long term.
Take time to plan some self-care activities including exercise, fun and time with loved ones. Plan time out each week and longer breaks over the course of the year and set boundaries to ensure that your workload does not become overwhelming.
To learn more about TEN visit https://www.blackdoginstitute.org. au/the-essential-network/
ED: Dr Melissa Black is a clinical psychologist and clinical research fellow at the Black Dog Institute.


These programs allow patients to address mental health issues with minimal wait time or disruption to their everyday lives.
Structured, therapeutic group sessions tailored to the specific needs of patients experiencing:
• Depression
• Anxiety
• Bi-polar disorder
• Personality disorder
• Trauma
• Eating disorders
• Substance dependency
For more information visit ramsaymentalhealth.com.au/hollywood
• Refer directly to Ramsay Clinic Hollywood, no psychiatrist referral necessary
• Cost covered under private health insurance (top cover in psychiatric)
For a GP information pack, please contact Wendy Henson HensonW@ramsayhealth.com.au
People
ramsaymentalhealth.com.au
caring for people

The new year is a time when we wade through articles in the popular media about “shedding holiday kilos” and “getting beach ready.”
They may seem harmless, but in fact diet culture and body shaming cause real health harm. That’s why it’s great that we’re seeing signs of a revolution whereby people with lived experience are involved in discussions about weight issues and obesity.
I have often observed that having a consumer and lived experience perspective in the room when health service plans are being developed, or health topics are being discussed at conferences, changes the nature of the discussion.
We need to move away from the idea that it’s OK to have just a handful of people with consumer, carer or lived experience perspectives in a room when there are hundreds of other people with professional or learned experience perspectives.
I’m convinced that consumer perspectives should be at every table where decisions that impact us are being made – this includes at the highest levels of government, for example, when health service funding models are being conceived and developed.
This means organisations need to step up their level of investment in capacity building for people with consumer, carer or lived experience perspectives to become “learned experience” experts – particularly in technical areas – while retaining a consumer, carer or lived experience lens.
In the discussions I have had the privilege of being a part of through my job, I feel a responsibility to speak consumer and lived experience perspectives into the room.
There is currently no democratic forum in Australia where consumers, carers, and community members can hold our elected representatives to account for the state of our health and social care system.


We are required to talk to our State representatives on Statefunded issues and our Federal representatives on Commonwealthfunded issues. This is a massive contributor to the ongoing tolerance of a highly fragmented health and social care system.
It is essential that consumer and lived experience perspectives are present at every discussion that impacts our health and social wellbeing – so that people can move away from “meh, what are you going to do?” to “right, what are we going to do!”.
With discussions ongoing in multiple forums in both WA and federally to address issues of great importance to the community – such as the Strengthening Medicare Taskforce and the WA Emergency Department Reform Ministerial Taskforce, perhaps it’s time for a forum where WA consumers and health professionals can sit together with elected representatives and officials from both levels of government to nut out the best solutions for WA –together.
It is hard to believe that 2023 is well underway. With the pandemic over in all but name, attention this year will need to switch to all the health issues which never went away and, in many instances, got worse over the past three years.
There is an old adage about putting the horse before the cart. Delivery of medical services occurs within a system. It is fair to say that many of the issues of access to services are a function of the system. This includes the shortage of people, the remuneration offered, time largely wasted on bureaucratic requirements and the inability of practitioners to do what they are trained to do.
Overarching all of this is the Medicare system, which has served Australia well since its introduction in 1984. However, a 40-year-old car, which has never had adequate maintenance, will ultimately break down. Yet, any discussion of reform, let alone actual reform, was effectively destroyed by the ill-fated “Mediscare” campaign of 2016 meaning that the current review will lead to minor tinkering.
Doctors are voting with their feet. It is estimated the GP workforce contracted by 3% in the two years to June 2022. The ability to see a private paediatrician in Perth is negligible. Wait times in other specialties are growing. And to paraphrase Basil Fawlty, don’t mention the public waiting list times.

Still, it could be worse. In the UK, ads are being run encouraging people to think twice before seeking services in the NHS. In some respects, this is not unreasonable. We are all familiar with people presenting with an issue which could easily have been managed at home. However, it says much about the view from above about the capacity of the NHS.
Someone made the astute observation that it is no use having a service which is free at point of delivery if you cannot get to the point of delivery. Australia is not at this point, but we are moving in that direction. And yes, the US system is not the answer as it achieves the same result via a different pathway. There is a middle way if we want to find it.
Albert Einstein is claimed to have defined insanity as doing the same thing repeatedly and expecting a different outcome. A system that cannot be touched will ultimately collapse. Our start point must be that we need a system geared to the 21st versus 20th century. We need new ideas!
Doctors are voting with their feet. It is estimated the GP workforce contracted by 3% in the two years to June 2022. The ability to see a private paediatrician in Perth is negligible.


Muscle fibres are the motors that power our movements, allowing us to walk, run, eat or hug a loved one. But the extracellular matrix (ECM), a dynamic and complex network of proteins and molecules within which our fibres are housed, is now known to play an essential role in muscle function, growth, injury recovery and ageing.
Measuring cellular activities within the ECM may potentially inform targeted physical activity treatments aiming to improve ECM status and enhance disease treatment. Yet these potentially important biomarkers are still underused in both research and clinical environments.
The ECM may be the next place to search for clues on how to improve muscle function and delay or overcome the effects of ageing and disease.
Muscle disuse in response to inactivity, injury or ageing can trigger non-optimal changes in the ECM including muscle connective tissue proliferation leading to
Muscle extracellular matrix (ECM) may be key for physical activity treatments and enhancing disease treatment
Even a single exercise session can evoke powerful changes resulting in improvements in muscle ECM biomechanical and physiological properties
Several ECM biomarkers can assess different aspects of ECM status and changes in response to exercise, disuse, and disease. Beware intricacies of interpretation before using them.
stiffness and immobility. However, maintaining the muscle at a longer length during immobilisation can attenuate negative outcomes, and these are clearly visible through ECM biomarker assessments. Even a single exercise session can evoke powerful changes resulting in improvements in muscle ECM biomechanical and physiological
properties These benefits are amplified when exercise is repeated over time.
Due to a lack of research, many questions remain regarding muscle ECM biology and its implications for human health and physical function. It remains unclear which exercises are best for stimulating ECM remodelling or collagen synthesis, which biomarkers can accurately assess ECM status or how alterations in the ECM affect responses to acute or long-term exercise regimes, disuse, or ageing. We also lack an understanding as to how these adaptations affect muscle function in terms of injury recovery, health maintenance, and physical performance enhancement.
With numerous biomarkers readily available, practitioners should be well informed about interpreting the data correctly. For example, a change in the abundance of a biomarker examined in blood may provide different information to that same biomarker being examined in muscle tissue, e.g. an increase in blood hydroxyproline concentration (a molecule present in all types of collagen) may indicate increased collagen breakdown, while increased muscle hydroxyproline indicates increased muscle collagen content. Awareness of these intricacies is critical before interpreting changes in biomarker levels.

Promising blood, urine and even sweat biomarkers for ECM remodelling, ECM status, and exercise, disuse and ageing effects are shown in figure 1. In humans, collagen fractional synthesis rate appears to be the most consistent biomarker for assessing acute collagen synthesis, whereas collagen IV and hydroxyproline appear to be reliable for assessing acute collagen breakdown.
This may be relevant in diseases where collagen turnover assessment is important, such as muscular dystrophy, rheumatoid arthritis, or Ehlers–Danlos syndromes.
Additionally, integrin- α7, tenascin-C, and collagen IV in tissue samples can be used to reliably assess acute changes in the basal membrane, ECM-to-cell adhesion, and the collagen scaffold itself, respectively. Hydroxyproline and prolyl 4-hydroxylase also appear reliable for assessing long-
term collagen synthesis, whereas integrin- β 1 increases consistently with long-term exercise and indicates changes in cell-to-ECM anchorage.
Such changes can translate to novel treatments for diseases; (e.g. increased integrin content in mice with muscular dystrophy can dramatically reduce the severity of dystrophy symptoms).
Currently, no reliable human biofluid markers exist for the assessment of long-term ECM adaptations,

so more research is needed. Promising candidate biofluid markers include P3NP and TGF- β for assessing collagen synthesis and hydroxylysylpyridinoline for assessing changes in collagen’s structural profile (i.e. optimally linked collagen vs collagen that linked via glycation, which is stiffer and prone to injury and disease).

ECM markers for disuse and ageing are also yet to be established, but data from animal studies suggest that prolyl 4-hydroxylase and galactosylhydroxylysyl glucosyltransferase might be promising indicators of collagen synthesis changes. Nevertheless, muscle ICTP, PINP, and MMP2 for disuse and galactosylhydroxylysyl glucosyltransferase for ageing are promising human biomarkers of collagen synthesis that remain to be explored.
Hopefully, in the next few decades, researchers and practitioners will better understand the immense potential of muscle ECM on responses and adaptations to disease, exercise, injury, and ageing. So far, we have largely ignored much of what happens inside the muscle fibre within the ECM. Further research may inform us how to better target and stimulate this muscle domain, leading to new ways to train rehabilitate muscles, and even treat diseases.
This new era of understanding could potentially revolutionise how we approach health care by providing personalised strategies based on each individual’s unique biochemical fingerprint from their ECM response profile.
ED: Dr Mavropalias is a researcher at ECU and Murdoch University and Prof Blazevich is from ECU.
Author competing interests – nil
Read this story on mforum.com.au
CT is one of the most transformative advances in medicine in the past 100 years. It is estimated to have a substantial impact on the speed of diagnosis in 50% of cases and, in a high proportion, the result is decisive in outcome. Approximately 15 per 1000 people undergo a CT scan annually in Australia.


Radiation is possibly the longeststudied carcinogen, with reports dating back to the early 1900s. Radiation risks are divided into so-called deterministic (acutely after large doses of radiation e.g. radiotherapy) or stochastic (arising in the longer term, usually decades after a significant exposure). The stochastic effects are applicable to CT, chief among them is cancer. There are expressed concerns about the safety of CT scans though these are often not consistent with data from higher quality studies nor the consensus opinions of authoritative bodies.
Scanner software provides an accurate dose estimate on a per patient basis, expressed in mili Gray per centimetre – this appears in the dose card image on the image viewer (PACS) as the Dose Length Product (DLP). In the radiologist’s report, this may have been converted to mili Sieverts (mSv), a measure weighted to the particular radiation sensitivity of the region scanned. For example, a DLP of 200 mGy.cm for the head yields an effective dose of 1 mSv, though for the chest this same DLP translates to 3 mSv, reflecting the differences in tissue sensitivity of these two regions.
The choice of the dose is the attending radiologist’s, in consultation with the radiographer, when needed. Firstly, it is incumbent on radiologists to ensure the scan is warranted and that CT is the best imaging modality to answer the clinical question.
To enhance outcomes, radiologists

are periodically required to submit their radiation dose records to the Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) and are provided with updated diagnostic reference levels to ensure they are within reasonable range of their peers.
While there is no broadly accepted definition of what constitutes a lowdose CT, it is commonly reserved for scans less than 1mSv. Thresholds will undoubtedly change, or terminology shift (e.g. the recent use of ‘ultra’ or ‘hyper’ low dose) as technology continues to improve.
Importantly, a low-dose CT is often inappropriate (e.g. characterising a renal mass may require a standard dose of 10 mSv though excluding a renal stone just 1 mSv). Other indications for low-dose CT include lung cancer screening, paranasal
sinus imaging, virtual colonoscopy and coronary calcium scoring. Doses do vary and will usually reflect the particular requirements for the clinical question or result from patient-specific factors. For example, the dose used will often be higher for an obese patient (though curiously not necessarily the biological effect because of the radioprotective effect of subcutaneous fat).
Each imaging modality (e.g. MRI, ultrasound) has strengths and weaknesses with regards cost, availability, comfort and fitness for purpose. For broad recommendations, we refer to the published diagnostic imaging pathways and, if there is persisting uncertainty, a radiologist should be consulted. A user-friendly pathway (developed in WA and

Radiation doses from CT scans are low (and getting lower) and the risk is small to none.
Radiologists are bound to strict radiation hygiene with doses tailored to purpose and no more.
A radiologist considers the appropriateness of every scan prescribing dose in accordance with patients’ best interests.



now adopted by the UK National Institute for Care and Health Excellence) can be found at: https://radiologyacrossborders.org/ diagnostic_imaging_pathways/



CT scans cause acute DNA damage (double strand breaks), however, this process is also occurring naturally and continuously and typically managed by the body’s regulatory system before generating cancer. The highest (and only direct) level of evidence of radiation-induced carcinogenesis is derived from survivors of the atomic bomb blasts in Hiroshima
and Nagasaki. These studies show a linear dose-risk relationship for individuals receiving 100mSv or above.
Some patients will undergo numerous CT scans during their lifetime, though with current and foreseeable applications and technological advancements, this will unlikely exceed an accumulation of 100mSv or more. This excludes some patients with a significantly shortened life expectancy (e.g. those with poorer prognosis cancers).
Some recent indirect evidence suggests CT scans cause cancer. However, this evidence is significantly flawed including high uncertainty about the doses, lack of detail about scan indication or past medical history, and no consideration of doses from other imaging tests. Hence the potential for reversed causality bias is high, as it is in most published radiation risk science.
The preponderance of data, including that from other recent studies, taking such factors into account (though there may be other limitations), has not shown an
excess in cancer risk from CT scans, though these studies have not proven the risk is zero.
The effect (if any) of CT scans is simply too small to be registerable with the data available to date. Several studies with improved designs are underway.
In children, some tissues are more sensitive, some have the same sensitivity and others less sensitive to radiation than adult tissues. Thus far the evidence is too weak to establish an association between CT radiation and cancer in children. Nevertheless (and fortuitously), doses required for diagnostic acceptability in children are typically smaller than those in adults. In addition, there has been extraordinary effort made by radiological colleges in recent years to increase awareness and promote particular attention to minimising doses in children.
Note – radiation refers to ionising radiation









Author competing interests – Dr Murray has a commercial interest in a provider of CT scan services





rTMS


Non-palpable breast lesions are not easy to resect without prior localisation. With the increased uptake of breast screening, there are more impalpable lesions detected that requires surgical excision – indeterminate and biopsy proven malignant lesions. The traditional, and only available approach for many years, has been image-guided hookwire localisation. This is a fine wire with a thickened portion inserted into the breast on the morning of surgery by the radiologist, under ultrasound or mammographic guidance. After it is inserted, a mammogram is performed with the hookwire in situ to provide a visual guide for the surgeon during surgical resection. The patient is told not to move her arm for fear of dislodging the wire. Breast movement is also painful unless she is wearing a bra. The hookwire protrudes out the breast until it is removed at the time of the lesion resection. The patient would have come into hospital early on the morning of surgery to have the hookwire inserted, and then wait for many hours until her operation time. Scheduling for the radiologist is also stressful as multiple hookwires are sometimes required in many women in one day.
The Magseed and Sentimag system
is a new localisation technique, which is now available to women in WA. Essentially, a tiny (5 x 1mm) metal marker is inserted into the breast by the radiologist. A ‘metal detector’ through magnetic technology (Fig. 3) is used by the surgeon in theatre to localise the impalpable lesion. The Magseed is made of surgical grade stainless


steel and has no expiry date.
Radiologists are already familiar with placing markers into breasts at the time of biopsy of indeterminate lesions. The Magseed insertion technique is no different. It can be placed into the breast days in advance and women are not even aware of it. It is also an easy technique to learn for the surgeon. Women can still have MRI breast with Magseed in situ, but there will be a small void artefact in their MRI scan. However, we are currently only using Magseed as a surgical localisation tool and all Magseeds will be removed.


Screening has led to an increase in non-palpable lesions being detected
Magseed and Magtrace represents the biggest shift in breast surgery for many years and will transform the operative day.
The Magseed and Sentimag system has already been widely used internationally and interstate. COVID delayed its introduction to more women in Western Australia.

There are other seed/marker technology available, and we have assessed them and found Magseed to be the most user and patient friendly.
For instance, radio-guided occult lesion localisation using Iodine-125 seeds (ROLLIS), is available as a hookwire alternative. However, it is a radioactive product that will decay and differing regulatory bodies have variable restriction to the number of days it can remain in situ. Radioactive seeds are also
labour intensive to order and track and need to be disposed of safely by medical physics.
It is a major problem if a ROLLIS seed is lost and not retrieved in surgery. Whereas losing a Magseed is not an issue as long as the surgeon has resected the lesion in question.
Magtrace is a suspension of magnetic particles. It is non-toxic, non-radioactive (unlike traditional Tc-99) and is without anaphylaxis risk of Patent Blue dye. Magtrace now has NICE recommendation
and FDA approval for sentinel node localisation, an important part of breast cancer staging.
It allows the surgeon to inject up to seven days before surgery, improving scheduling efficiency, especially for cases booked on Monday mornings. We hope to start offering Magtrace in early 2023.

– References available on request
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Mitral regurgitation (MR) affects 2% of the population and can be grouped into those with primary (degenerative) or secondary (functional) mitral regurgitation. The best way I describe this to patients is that there is either a problem with the door and hinges, or the frame of the door.
In degenerative MR the issue is with the door itself (i.e. myxomatous and valve prolapse) or the hinges (subvalvular apparatus e.g. ruptured chordae and flail) that prevents coaptation of the anterior and posterior leaflets. In functional MR the issue is with an enlarged door frame and caused by the patient’s underlying cardiomyopathy (e.g. ischaemia). The doors are often normal, but the leaflets are pulled apart due to left ventricular dilatation. In certain cases, there is mixed disease.
TMVr, or edge-to-edge repair, is based on the surgical technique of putting an Alfieri stitch to approximate the anterior and posterior leaflet creating a double orifice and reducing mitral regurgitation. It reduces symptoms of heart failure, hospitalisation and improves quality of life.
TMRv is approved in patients who are at unacceptably high risk for surgical mitral valve replacement and are on optimal medical therapy with 3+ to 4+ mitral regurgitation on echo, with ongoing NYHA class II-IV heart failure symptoms and ejection fraction above 20%.
Imaging with transthoracic (TTE) and transoesophageal echocardiography (TOE) to assess the cause of MR and procedural planning is key. Exclusion of coronary disease and haemodynamic assessment with right heart catheterisation allows clinicians to tailor optimal medical therapy and consider revascularisation.
Mitral regurgitation is dynamic and measures to achieve
Mitral regurgitation is common and should be managed aggressively and referred for specialist follow-up
TMVr reduces symptoms of heart failure, reduces hospitalisation and improves quality of life
Following measurements of valve area, leaflet length and mechanism of mitral regurgitation the appropriate device size is selected. The device is positioned perpendicular to the line of coaptation to target the regurgitant jet and the leaflets are either simultaneous or independent grasped to achieve optimal leaflet coaptation.
euvolaemia, reduce blood pressure, regulate heart rate, treat rhythm disturbance (e.g., AF) and improve cardiac synchrony (e.g., cardiac resynchronisation therapy) will improve MR and improve the clinical outcomes post TMVr.
Timing for intervention is when symptomatic patients on optimal medical therapy show signs of haemodynamic decompensation. For example, pulmonary hypertension at rest or on exercise without a significant precapillary component, dilatation of the left ventricle, reduction in ejection fraction, hospitalisation for heart failure or development of atrial fibrillation (often poorly tolerated).
Patient cases are reviewed by a multidisciplinary heart team consisting of a clinical nurse coordinator, structural and imaging cardiologists, anaesthetists, and cardiothoracic surgeon. We assess patients for frailty and quality of life, review their echoes for suitability for edge-to-edge repair and strategy for device implantation.
The procedure is performed under general anaesthetic and takes under three hours. Access is via the right femoral vein followed by transeptal puncture into the left atrium under TOE guidance. A steerable guide is then advanced and positioned in the left atrium, the patient is fully heparinised and left atrial pressures are taken.
TMVr is a safe procedure, and most patients are discharged the following day without the need for lifelong anticoagulation unless there was a prior indication. Read this story on
The residual regurgitation is then assessed by TOE, valve area calculated to assess for mitral stenosis and device stability prior to the device being deployed. In valves that have large regurgitant orifices more than one clip is used to approximate the leaflets or provide stabilisation and an annuloplasty effect.
Post-implant left atrial pressure is measured to evaluate the haemodynamic effects and the guide sheath is removed. The septum is assessed by TOE for bidirectional shunt and closed using an ASD closure device if required. The femoral vein is closed using a stitch in a pre-close fashion or a Z stitch to provide external compression.
Post-procedurally the patients are monitored in a cardiac ward overnight and a TTE is performed prior to discharge to assess for residual MR, device stability and exclude any complications from the procedure. The majority of the patients are discharged the next day. Patients are put on aspirin and clopidogrel for six months only and do not need to be anticoagulated unless they have a prior indication (e.g. AF).
Author competing interests – No relevant disclosures



































 By Dr Liezhou Zhong & Amanda Orchard, ECU
By Dr Liezhou Zhong & Amanda Orchard, ECU

Poor nutrition contributes to more deaths globally than any other factor including smoking and inadequate physical activity. It is estimated to be responsible for 7% of Australia’s disease burden. Despite the perception that it is “an issue of the past” in Australia, malnutrition is disproportionately common in various vulnerable groups such as people who have difficulties chewing (e.g., tooth loss, dry mouth, gum disease) and swallowing (dysphagia), who require texture modified foods.
Texture modified foods are generally minced, pureed or thickened to reduce the risk of aspiration and choking. It is estimated that 8% of the population worldwide has difficulty swallowing. Speech Pathology Australia suggest that over one million Australians are affected by swallowing disorders, including people with motor neurone disease, multiple sclerosis, Parkinson’s disease or Alzheimer’s disease, cancer/stroke survivors, the geriatric population and children with cerebral palsy.
These foods often lack visual and/ or taste appeal and are regularly served in “blobs” and “ice cream
Poor nutrition contributes to more deaths globally than smoking
Texture-modified foods often have lacked nutritional value and aesthetic appeal
3D printing of foods offers a solution.

scoops”, making people feel “left out”. Poor food visual quality impacts food intake, physical health, mood and mental wellbeing. Furthermore, in order to achieve the required texture, the foods are commonly overcooked, destroying nutrients and diluting flavour. People on texture modified foods report lower appetite, vitamin A & E intake, protein and fluid intake, and higher weight loss than those on a standard diet.
Eating for pleasure and health in communities on texture modified diets is often sacrificed in favour of safe eating. Three-dimensional (3D) food printing technology is an innovative solution to improve food enjoyment in these vulnerable groups by rebuilding the foods
into aesthetically pleasing dishes. 3D food printing can fabricate food objects layer by layer, from the bottom to the top, to achieve designed shapes.
3D food printing is a new frontier in the food industry and has been rendered as a “magic bullet” to enable rapid prototyping, customised food design, and personalised nutrition (based on food preferences, health conditions, specific dietary requirements, and social context).
Extrusion-based 3D food printers are the most common as their relatively simple operation and easy material handling are compatible with a wide range of food materials. Typically, these materials should flow through a nozzle and then be self-supporting after being served. This includes chocolate, fats, dough, pureed or mashed fruits and vegetables, edible gels (gums, starch and protein), hummus, creamy cheese, icing, spread, surimi and meat slurry. Thus, texture modified foods are ideal for extrusion-based 3D food printing.
The most apparent advantage of 3D food printing is its freedom
continued on Page 49




Many Australian children have problems with language development by the time they start school, but the signs are not always obvious.
But if a five-year-old is unable to tell a simple story, it may be a sign they have a disorder affecting their language development, according to Macquarie University linguistics researchers.

Speech and language pathology researcher Dr JaeHyun Kim said that with 10% of children reaching primary school with some level of difficulty with language, the problem was more widespread than most people might imagine.
“Only a small portion of these children have language development problems as a result of medical conditions like hearing loss,” Dr Kim said.
“The rest of them – 7% of all children – have a developmental language disorder without any obvious medical conditions.
“We’re not talking conditions like stuttering – a study of children who stutter found that they can have better-thanaverage language skills. Developmental language disorder is a problem with using and understanding language.”
In a paper published in Communication Disorders Quarterly, Dr Kim and Department of Linguistics colleagues Dr Ben Davies and Dr Nan Xu Rattanasone found 80% of people surveyed had not even heard of developmental language disorder.
“That’s a real problem, because if we’re not aware of something, we can’t start getting help,” Dr Kim said. “We are now concerned that more and more children are reaching school with poor language skills.”
He said there were signs that parents and health professionals could watch for.
Up to the age of five, language disorder could manifest as problems with spoken language, such as only being able to understand simple sentences.
One of the most prominent warning signs at that age was having trouble telling a fictional story in a coherent way.
They said seeking help from a speech pathologist was critical.

Transcranial Magnetic Stimulation (TMS) has finally become a well-established treatment for major depressive illness, which is frequently associated with all other psychiatric conditions, ranging from generalised anxiety to PTSD, OCD, and functional psychotic disorders.
Despite its relative youth, TMS has already relieved a burden of chronically dysphoric effect and profound anhedonia (inability to experience pleasure).
These clinical successes make it timely to review the current understanding of TMS techniques and consider new advances that may transform practice.
TMS uses rapid pulses of a magnetic field to non-invasively induce electrical currents in the brain to modulate the brain's endogenous (internal neuromodulation) activity and function. Repetitive TMS is delivered via a coil held over the
TMS activates multiple brain circuits downstream of the stimulated targets
The effects of TMS can be seen in structures located deep in the brain and in non-neuronal cells
TMS may help treat disorders associated with pathology in deeper brain regions (e.g., Parkinson's disease) or linked to particular cell types (e.g. oligodendrocytes in MS).
scalp. This magnetic stimulation can be targeted to specific brain regions using scalp measurements or MRI-guided neuronavigation. Functional neuronavigation with EEG can be used, though it is not a standard method (yet) to identify stimulation sites.
The traditional view of TMS is that it alters brain plasticity at the stimulation site. The emerging
continued from Page 47
to achieve appealing food presentations. Beyond shapes, food sensory properties, such as colour, taste, smell and mouthfeel, can be precisely manipulated using 3D food printing. The food materials used in 3D food printing can be fortified or even medically tailored for those vulnerable communities who often have a wide range of health conditions.
Of note, by constructing different inner and outside food structures and shapes, we can control the nutrient release of the 3D-printed food products (i.e. releaseretardation food). The digestibility of 3D printed foods can also be modulated, which can further
affect satiety and food intake. This strategy has also been used to deliver probiotics.
In addition to health-related applications, 3D food printing technology can offer a unique opportunity to improve food sustainability. Aesthetically imperfect and underutilised fruits and vegetables that otherwise end in landfill can be freeze-dried to be high-value, nutrient-dense food ingredients by removing water in raw fresh produce at very low temperatures. The ingredients can then be used to fortify texturemodified foods through 3D food printing.
There is an increasing number of free resources (e.g. free recipes: https://texturedfoods.com/
evidence suggests that this is just the tip of the iceberg –TMS activates neurons (at the stimulation site), which in turn, trigger downstream activation of many other brain regions, setting up a chain reaction of activation throughout interconnected circuits.
In psychiatry, the ultimate target of this stimulation is the limbic system, made up of the hippocampus, amygdala, and many other subcortical structures involved in modulating our emotions and neurovegetative responses.
MRI imaging data and other neuroimaging analytical tools reveal that TMS alters the activity of multiple regions throughout the brain along neural pathways. The resulting multiple "chain reactions" modulate the function of the complex brain circuits involved in mood regulation. Importantly, these observations
recipes-3 and cooking instructions: https://www.iddsi.org/TestingMethods) to help people prepare nutritious and safe texture-modified foods. However, preparing them so they are safe for swallowing but also appealing is still a huge daily challenge to chefs and caregivers. To this end, together with freeze dried food ingredients, 3D food printers can be a powerful kitchen appliance helping families prepare safe, nutrient-dense and appealing texture modified foods.
– References are available on request.
ED: The authors are researchers at the Nutrition & Health Innovation Research Institute, ECU
Author competing interest – the authors have been involved in developing the technology described


have provided key insights that biochemical theories of emotional

These findings open a range of new disease targets for TMS because it may be used to rescue connectivity
function in regions located deep in the brain and inaccessible to direct interventions. Furthermore, the therapeutic relevance of targeting brain networks is not restricted
and may be used to target other neurological conditions involving underpinning motor symptoms. Even though the SN is located deep within the brain, there is evidence that TMS can provide benefits by altering the connectivity patterns of other brain regions involved in motor control.
the supplementary motor area improved symptoms of PD by normalising abnormal brain functional connectivity patterns in general and freezing of gait in particular! These changes were directly related to the neurophysiology of motor centres
and not mediated by mood and affective states.
This study further correlated the changes in whole brain connectivity with the reduction in symptoms by developing imaging biomarkers that were used to track response to TMS. The ability to study wholebrain connectivity patterns using novel exploratory multivariate approaches therefore leads to personalised treatments – an area already being explored in depression.
Basic research has highlighted some unexpected targets of TMS indicating that focus should move beyond the electrically sensitive neurons (nerve cells). TMS has recently been shown to affect nonneuronal cells in the brain, including astrocytes and oligodendrocytes. These findings broaden the possible therapeutic applications to inflammatory conditions and demyelinating disorders such as multiple sclerosis and post-stroke rehabilitation.
Author competing interests –Dr Hryniewicki is a director of Modalis, which provides TMS services

Australian researchers recently found they contribute to cancer risk, there was a caveat – quantity consumption of bacon, ham and salami. In 2015, the International Agency for Research on Cancer at the World Health Organization assessed more than 800 studies to understand the link between
It found sufficient evidence that eating processed meats caused
because of their nitrites content, while cooking processed meat, particularly over high heat or an open flame, was also likely to be a problem.
But they stressed that different carcinogens had varying levels of impact on cancer risk. For tobacco smoke, the impact was high – the lifetime risk of lung cancer in a non-smoker was 1% and in a heavy smoker it was 25%. For someone who consumed processed meat frequently rather than moderately, their lifetime risk of colorectal cancer increased from 5% to 6%.
The UNSW Sydney researchers said this meant that while there was strong evidence that eating
processed meats caused colorectal cancer, the actual impact on cancer risk was relatively small.
And while eating salami could contribute to cancer, there were also ways to potentially counteract the effects of processed meats in the gut – at least partially. This included eating foods like fruits, vegetables and whole grains.
After considering the risks, the researchers concluded it was likely to be safe to occasionally have salami or order a BLT. The increased risk of cancer was really only measurable in people who ate processed meat on a regular and daily basis.
GUARANTEED ACCESS TO A SURGEON ALL YEAR ROUND








Primary aldosteronism (PA) is the most common secondary cause of hypertension, with a recent study highlighting this may be present in 14% of patients with newly diagnosed hypertension between the ages of 18-80 years. This study based in primary care in Melbourne studied patients with newly diagnosed hypertension (>140 mmHg systolic or >90 mmHg diastolic) on two occasions and performed screening with the aldosterone to renin ratio (ARR). Twenty five percent of patients had two elevated ARRs, with PA confirmed using the seated saline suppression test in 14% of people with newly diagnosed hypertension.
Diagnosis of PA is very important, as patients with PA have worse cardiovascular outcomes than blood pressure matched patients with essential hypertension. Patients found to have unilateral PA can be cured with adrenalectomy, and those with bilateral excess aldosterone secretion can have many of the cardiovascular risks mitigated by early mineralocorticoid receptor antagonist therapy. ARR should be performed in all patients with newly diagnosed hypertension, and if elevated on two occasions, these patients should be referred for endocrinology review and confirmation testing. Note many antihypertensive therapies impair the interpretation of the ARR.
Genetic testing for familial hypercholesterolaemia (FH), a common inherited disorder of low density lipoprotein cholesterol (LDL-c) catabolism leading to premature atherosclerotic cardiovascular disease (asCVD) is recommended for adults and children with FH in the recently published adult and paediatric FH guidelines. However, the uptake of genetic testing has be lower than predicted over the last two years, with ~90,000 of the likely ~100,000 people with FH in Australia remaining undiagnosed. There is
Primary aldosteronism is the commonest secondary cause of hypertension – recommend performing an aldosterone to renin ratio in all patients with newly diagnosed hypertension to screen for PA
Uptake of genetic testing for familial hypercholesterolaemia has been well below expectations, a raised awareness of FH and genetic testing is required for all clinicians
The PBS has altered the criteria for Evolocumab therapy for patients with symptomatic atherosclerotic cardiovascular reducing the LDL-c threshold to >1.8, and allowing prescription from primary care in consultation with a specialist physician.
strong evidence that early treatment reduces the excess cardiovascular risk associated with this genetic condition. However, the largest challenge in FH management worldwide is to increase awareness of FH. A healthy lifestyle along with lipid lowering therapy are the cornerstones of therapy. Lipid lowering therapy dramatically reduces the risk of asCVD and is currently recommended from age of 10 for children with FH.
Genetic testing is the gold standard for diagnosing patients with FH and
is Medicare rebated for index cases (the first person tested in a kindred) if requested by a specialist physician for a patient who has any of the following: a Dutch Lipid Network Criteria Score of at least 6, OR an LDL-cholesterol or 6.5 mmol/L or more in the absence of secondary causes, OR an LDL-cholesterol of between 5.0 and 6.5 mmol/L with signs of premature or accelerated atherogenesis. Genetic testing for family members (cascade testing) in first (50% risk per person) and second (25% risk per person) degree family members is rebated by Medicare and can be requested by any doctor involved with their care. The private laboratory I work with has an accredited audit established to assist clinicians identifying patients with potential FH. Clinicians enrolling in the audit are presented with a list of their patients at high risk of FH based on lipid profiles over the last 12 months alongside an algorithm to assist them establishing the likelihood of FH and how to progress to FH genetic testing if appropriate.
Medicare have revised the funding criteria for the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor Evolocumab on the 1st of December 2022 for patients with symptomatic atherosclerotic cardiovascular
continued on Page 55

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Osteoporotic fracture is a progressive genetic and agerelated disorder that may need both lifestyle and pharmaceutical prevention. Management needs at least two specific consultations, the first directed to discussion of risk and second a review with additional testing to decide on management.
Previously, treatment decisions have been made on the T-score value of below -2.5 (this is the patient’s bone mineral density (BMD) expressed as a SD score below the young normal mean). In recent years using additional data, especially age and sex, have resulted in computation of 10-year percentage risk of fracture that is understandable to clinicians and patients and is commonly used in determining treatments for other diseases such as CVD.
The best researched is the Fracture Risk Assessment Tool FRAX https://www.sheffield.ac.uk/FRAX/ tool.aspx?country=31
Before requesting a DXA BMD, a risk assessment can be carried out with FRAX, however, published data identifies a substantial improvement in risk calculation if a
Osteoporotic fractures need lifestyle and pharmaceutical management
The Fracture Risk Assessment Tool FRAX is the best researched Risk explanation to the patient based on a suitable scan is key.
femoral neck BMD is incorporated in the calculation. So, at the first consultation to consider bone disease, a fracture risk calculation can be carried out without a BMD. Depending on whether the patient meets the requirement for a partially MBS supported BMD test (see table 1) or whether they will pay the whole cost themselves, the decision can be made to review the data at the next visit together with any biochemical testing that is indicated.
For advising the patient on the interpretation of the fracture risk calculation, it is helpful to explain that the mean 10-year risk of osteoporotic fracture in Australia of 60- to 75-year-old women is approximately 10%. In the UK the indication for pharmaceutical
UWAtherapy has been set around a 20% 10-year risk for a major osteoporotic fracture (hip, spine and leg and arm long bone) or a hip fracture of 3% 10-year risk as calculated by FRAX UK.
Risks below these may suggest attention to diet and exercise.
Risks above these may suggest additional prescription of one of the nine pharmaceuticals approved for fracture reduction in Australia.
The clinical advice is often dependent on a competent DXA bone density and graph, that substantially improves prediction of fracture and is an important part of the explanation of the risks and management plan to the patient. It should not increase consultation time. Notice the important words relating to DXA BMD, competent, graph, explanation, and time.
The problem with getting a world class bone density test in Perth is that many service reports are not reviewed and interpreted by an expert in the technology. The T-score result is based on assessing a very specific area of skeleton, if
continued on Page 57
continued from Page 53
disease, reducing the LDL-c threshold from >2.6 mmol/L to >1.8 mmol/L on maximum tolerated statin therapy and ezetimibe. It has also allowed the initial prescription to be from either a specialist physician or a physician who has consulted a specialist physician. The other criteria for heterozygous FH or non-FH remain in place, please refer to the PBS website for details.
The streamlined repeat prescription process remains for all medical practitioners. It is anticipated that
these criteria will also be applied for Alirocumab, although the time frame is uncertain at this stage. Thus, many patients with symptomatic vascular disease will now have funded access to Evolocumab, therefore raising awareness for this to clinicians and patients alike is important. It was also encouraging to have the FOURIER-OLE open label extension trial published late this year which demonstrated Evolocumab was safe and well tolerated for a median of 5 years and maximum 8.4 years follow up. Importantly, this trial showed a 15.4% reduction in the composite endpoint
of cardiovascular death, myocardial infarction, stroke, unstable angina or coronary revascularisation in those patients on active treatment for the entire trial compared to patients on placebo during the FOURIER trial who switched to Evolocumab at the inception of the extension study.
– References available on request
Author competing interests – I work for Clinipath Pathology, PathWest Laboratory Medicine, Department of Biochemistry and Cardiovascular Genetics, Royal Perth Hospital Cardiometabolic unit, the Medical School UWA and the clinical lead of cardiometabolic medicine at the WA Specialist Centre.



FAR UVC Light at 222nm destroys airborne and surface viruses and bacteria continuously It is safe for humans and animals!


UVC light 222nm is effective against Viruses, including SARS-CoV-2 (COVID) and influenza together with Multi-drug resistant bacteria in the air, on living human tissue and on surfaces.
FAR-UVC lightning is the first safe, effective, autonomous and continuous disinfection system for occupied spaces that is highly cost effective – saving unnecessary expenses.


For more information contact:
Les Schneider +61 423 88 9774
Toll Free 1300 007 888
Unit 33/110 Inspiration Drive, Wangara, Western Australia 6065
W: www.medisupply.net.au
E: info@medisupply.net.au

continued from Page 55
for example the DXA technologist gets the wrong vertebrae or does not correctly internally rotate the femur then the result is not valid. Thus, it is essential to review the image from which the T-score was provided to ensure that there are no technical problems. In addition, the image must include the patient’s data in regard to the normative reference range given that this is the basis of the T-score. This then becomes an important teaching point /explanation for the patient so that they can see their position in regard to the rest of the population. Despite the centrality of the image, some services specifically state that they do not provide access to it. Provision of such images allows you to ensure that each of the important provisions – competence, explanation, and time are fulfilled.
Author competing interests – nil

BreastScreen WA adheres to rigorous data security measures to ensure that the personal information (electronic and hard-copy) provided by clients from screening and assessment clinic visits, are protected from unauthorised use, disclosure or loss.

• BreastScreen WA is part of the WA Health Network and security of the information is monitored and governed by the WA Department of Health.


• BreastScreen WA staff and other authorised people have a legal obligation to keep your patient’s health information confidential.
• BreastScreen WA undergoes regular data audits to ensure the security and integrity of the client data stored.
For further information see https://www.breastscreen.health. wa.gov.au/About-Us/Your-information
phone
20 50
Perth sexual health expert and musician Lucy Peach wants all women, girls and people with cycles to be empowered by their periods. She’s even written songs and a live show to help spread the message.
By Ara Jansen
When Lucy Peach’s young son barged into the bathroom while she was changing a tampon, she realised it was an important moment. When he asked whether he should consider it disgusting, she realised she had a chance to release a stereotype and told him it wasn’t disgusting, but actually quite natural.
The period preacher, author and folksinger – often called the Period Queen – has made it her mission to get everyone talking about periods and to do away with the stigma of being embarrassed and rise above all those unkind words that have ever been hurled at women over their menstrual cycle.

The Perth mother of two boys has spent the past two decades studying women’s health and wellbeing, human biology and menstruality leadership. She has a Bachelor of Science in human biology and biomedicine and a graduate diploma of education in human biology.
“This kind of body positivity is important and it’s part of being human and we have been conned into the story that there’s something wrong with us and we
have to spend our lives fixing ourselves,” says Lucy. “I love to see young women claim themselves and not be apologetic for what makes them who they are. Everyone deserves to have great body literacy.”
Starting her career as a human biology teacher and sexual health educator, Lucy also built a parallel career as a folk-pop singersongwriter. Combining the two, Lucy used her own cycle as a tool to create music that won her WA’s Best Folk Act of 2016.

Lucy’s mission – while often wearing red – is to empower girls, women and those who menstruate throughout their cycles. She says the hormonal phases can be broken into four – dream, do, give and take. Understanding these phases allows you to make the most of your cycle and harnessing “period superpowers”.
It doesn’t need to be a random emotional rollercoaster, but instead across a month having a time to dream, a time to do, a time to give and a time to take helps you make the most of your energy and creativity.
She’s done a TED talk titled The Power of the Period and has written a popular book called Period Queen. Using her musical talents, she created a hugely successful and award-winning live show called My Greatest Period Ever
Returning by popular demand to this year’s Fringe World festival, it’s a hilarious and heartfelt show which combines music and menstrual messages. She’s joined on stage by her husband Richard, who creates live illustrations so you can learn how to hack your period and turn it into the greatest ever.
Lucy started on her own journey of discovering more about the phases within her cycle in her late 20s. She hasn’t stopped talking about them since.
“I’d had periods for 15 years and thought I was a pretty good feminist and felt pretty good about my body,” says Lucy. “Once I realised there was a cyclical part to how I felt and my energy levels, I realised I was kind of awful to myself when I was pre-menstrual. I was critical about myself and doubted myself.”
When she started to figure out things like understanding her tolerance would probably be short with just about anything during certain times, it allowed her to acknowledge that and work with it. Her work doesn’t only target females. She encourages men to be curious about the cycles of the women in their lives. “It benefits everyone when they have a clearer understanding of how having a cycle makes you feel and what happens across a month.”
She has a number of online courses, works in schools and is currently working with businesses to help them empower employees to work with their cycle.
My Greatest Period Ever is at Fringe World until February 12. The Sunday shows are family shows and especially suitable for young kids.
https://fringeworld.com.
au/whats_on/my-greatestperiod-ever-fw2023


Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.


Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.



There’s nothing more human than sitting looking at the stars and wondering what it all means, says artistic director Iain Grandage.
Celebrating the theme of djinda –stars – Perth Festival is looking both to the heavens and into the cosmos of the heart this year.
“It’s certainly a theme which can make us all feel connected – to each other and to the world,” says Iain, as the festival prepares to celebrate its 70th anniversary.
After a few years of restrictions this year’s theme is all the more perfect for reaching back out into the world – and indeed up to the stars – to reconnect with the power of art, with others and ourselves.
Djoondal is the free opening event, an immersive show using cuttingedge technology and ancient storytelling to tell the tale of the spirit woman with the long white hair who created the milky way and lives on in Joondalup.

Highlights of the festival are set to include musician Bjork’s rare performance of her theatrical extravaganza, Cornucopia, the thrilling gothic cine-theatre Strange Case of Dr Jekyll and Mr Hyde by Sydney Theatre Company and the dance-drum sensation Manifesto.
Heading indoors this year, the contemporary music program takes over The Rechabite. It’s packed with a varied menu from Bon Iver, Peaches and riot girrrl pioneers Bikini Kill to psych rockers Mdou Moctar and Flewnt’s Boorloo Block Party.
“The energy in this room is going to be amazing. There’s a great diversity in the program which is powered by the fact that pop and contemporary music have the wonderful ability to be right on the pulse of contemporary society. This is the first time we’ve had international artists for a few years and the world has changed a lot in that time. I’m keen to hear what they have to say.”
The 2023 visual arts program explores not only the stars but the darker spaces between them with exhibitions, a series of short films and a new public artwork you can contribute to called Between Us.
Iain says he continues to be proud of the festival’s ongoing commitment to local Indigenous storytelling in all its forms. This year’s festival includes a meditation on women’s stories called Punkaliyarra, the WA Youth Theatre Company performing the world premieres of Seven Sisters and an inspiring outdoor concert called Songs for Freedom
The much-loved Kronos Quartet celebrate its 50th anniversary by collaborating with Noongar composer Mattakitj for a world premiere, alongside presenting signature pieces from their vast repertoire. Reimagining John Cage’s Sonatas and Interludes, The Cage Project is turned into a threedimensional world at the hands of sound artist Matthias SchackArnott and French pianist Cedric Tiberghien.
There’s also the always-popular Lotterywest Films at the Somerville until April and the Literature & Ideas program at the Fremantle Arts Centre kicking off later this month.
“Looking at the stars is a very healthy way to gain some perspective on what we think we can achieve. For the last few years, we have paid more attention to our own space, and now it’s interesting to welcome visitors from other places and first nations artists from around the world. There’s a great sense of energy about that and a great appetite to connect.”
Perth Festival runs from February 10 to March 5. For program and ticketing details: www.perthfestival.com.au
Perth Festival turns 70 this year and looks to the stars, with an exciting program that invites the world back in and is packed with possibility.
After a busy year playing catch-up on surgery delayed by COVID, WA’s private hospital sector hosted an array of soirees at the end of last year to thank their doctors.



Among those to clink champagne glasses to a better 2023 were Ramsay Health Care, Bethesda Health Care and St John of God Subiaco, Midland and Mt Lawley hospitals.
The St John’s get-togethers were also a chance to farewell retiring SJOG Health Care CEO Dr Shane Kelly.
1 Ellen Almond, Dr Bridget Corrigan, Dr Michael Gannon and Dr Jo Colvin
2 Dr Olivia MacVie, Dr Shane Kelly, SJOG Subiaco CEO Tina Chinery and SJOG Health Care board chair Kerry Sanderson
3 Stephanie Mann, Prof Eli Gubbay, Elizabeth Gubbay and Dr Adam Gubbay






It was orthopaedics pitted against heart and cancer survivors – with the addition of women’s teams for the first time – when hockey players from all walks of life competed in Perth at the end of last year.
The annual Chest Rad Western Hockey Masters Gala Day was held at Perth Hockey Stadium on December 10.


After its success across the past few years and expansion in 2021, the event was bigger and better than ever, with the combination of the
annual Bionic Cup played between knee and hip replacement patients, and the heart versus cancer Survivors Cup, and the OBE Cup for men aged over 80.
There was also an inaugural women’s match – the Nice’n’Kneesy versus Breast Friends Cup –where women with hip and knee replacements came up against cancer and heart survivors.
The results were:
• Chest Rad Inaugural Cup ladies (Nice’n’Kneesy v Breast Friends): 4-2
• Survivors Cup men (Cancer v Heart): 1-2
• Bionic Cup men (Hips v Knees): 3-6
• OBE Cup men (White v Gold): 4-1
Tony Jones was part of the event’s organising team along with Dan Hill, Simon Thompson and Bob Bowyer in 2021, and was back behind the wheel for round two of the successful event.
Having overcome prostate cancer himself, Jones said the event had evolved into a huge success. Its origins began with the ‘Hips
versus Knees’ tournament in 2016, with 15 knee replacement recoverees playing against 15 who had undergone hip replacements.
It was such a success over the years that it turned into a gala day, providing a community for people to come together.
An eagerly-anticipated day for many, survivors are able to join forces for a day of hockey fun, and to celebrate the advancements of modern medicine.
“I think it’s very special,” Mr Jones said.
“Medical science is allowing people to get back into some sport they love and still be competitive and enjoy it. Survivors of key life dramas are able to move on and enjoy sport in their lives, and both genders participated this year.
“Hockey can be played at all ages. We have two teams of over 80-yearolds actively running around and competing in a physical sport.”
Across a wide range of models, take advantage of:





YEEARS / 75 7 ,000 0 KM SC S HEDULE L D SERVICING*
YE Y AR STANDARRD D MANUFACTUR U ER E ’S WA W RRANANTTY^


Plus, receive a 3.98% p.a. comparison rate± over 36 months on new and demonstrator Audi A4, S4, A5 and S5 models~
















