Oh, to have a dollar for every health taskforce review.
The sceptic in me had the recent report into Medicare already relegated to the bookcase of Well-meaning but Detail-Lite Health Reports before the ink was even dry at the printers.
The name itself was positive enough – Strengthening Medicare –until I revisited the previous Federal Government’s Primary Health Care 10 Year Plan 2022-2032 – or should that be 12-month plan? –which also talked about “strengthening” primary health care.
That plan – then-Health Minister Greg Hunt’s last hurrah to general practice – spoke about person-centred primary health care, teamwork and integrated care.
Some of that sounds a lot like Version.2023, which talks about multidisciplinary teams, longer consults and blended funding models. Snap!
Labor’s plan also refers to a ‘strengthened’ role for Primary Health Networks – which had some GPs choking on their Weeties at the thought of putting more funding into bureaucracy rather than the coalface.
Another similarity between the 2022 and 2023 reports is that neither directly addresses the elephant in the room – calls for significant increases to Medicare rebates.
Grossly inadequate increases to what the Commonwealth pays GPs – the rebate for a level B consult went up 65 cents last July –has contributed to the haemorrhaging of the bulk billing system designed to protect the most vulnerable patients.

The Strengthening Medicare report lays out reforms to modernise the health system and bolster general practice, and guides how the Federal Government should invest the $750 million it pledged ahead of last year’s election.
The optimist in me hopes that some of that funding will actually find its way to GPs and their patients.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
Labor’s plan also refers to a ‘strengthened’ role for Primary Health Networks – which had some GPs choking on their Weeties at the thought of putting more funding into bureaucracy rather than the coalface.
10 Bulk billing – where to from here?
14 Broadening primary care

18 Adult ADHD

24 Close-up: Dr Lawrence Beilin

58 Two loves make a creative life
60 The stars descend
61 Wine review: Cape Mentelle – Dr Craig Drummond
The winner of our December doctors dozen from Rosenthal Wines was Dr Paul Kwei
This month, another lucky reader can win a superb selection of wine from Cape Mentelle worth more than $800, including a very special 2018 Cabernet Sauvignon. Read Dr Craig Drummond’s review of Cape Mentelle on page 61, and for your chance to win a dozen bottles go to the competitions link at www.mforum.com.au or use the QR code on this page.
As a special offer, everyone who enters the competition will be sent an invitation to join Cape Mentelle’s mailing list, with access to an exclusive pre-release of its 2018 Cabernet Sauvignon.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au


Journalist Eric Martin 08 9203 5222 eric@mforum.com.au

Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au




Marketing Quinn Hampton quinn@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au

CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
This magazine has been printed using solar electricity, and the paper from plantation-based timber has been manufactured and printed with ISO 14001 accreditation, the highest environmental standard.

44
Procedural management of painful diabetic neuropathy

47 Thyroid Nodules – the good, bad and ugly A/Prof Ming Khoon



56
Non-melanoma pigmented skin lesions Clin. A/Prof Jonathan Chan


inaugural Byron Kakulas Medal.
Professor Dao-Yi Yu, from UWA’s medical school and head of the Lions Eye Institute's physiology and pharmacology group, was recognised for the minimally invasive surgical system he developed with his team.
Around 300,000 Australians and more than 70 million people worldwide are affected by glaucoma, which causes irreversible vision loss due to damage to the optic nerve. As the sight loss is usually gradual, early detection and treatment are vitally important.
Professor John Finlay-Jones, chair of the independent selection committee, said the potential of the gamechanging surgical system developed by Professor DaoYi Yu and his team to save sight was enormous.
“More than 100,000 glaucoma patients have retained their eyesight since the system was approved by the US FDA in 2016,” he said. “It was approved by Australia’s Therapeutic Goods Administration in 2018 and is globally recognised as one of the safest and most effective treatments for glaucoma.”
The second of the two Byron Kakulas medals went to the Perioperative Medicine Team – a collaboration between Perth Children’s Hospital Anaesthesia and

Aphra has promised to improve its handling of sexual boundary matters, following media reports about health practitioners still working after being sanctioned for sexual misconduct.
A six-month investigation by the ABC’s Four Corners revealed that almost 500 health practitioners had been sanctioned for sexual misconduct involving patients since 2010, and some continued to work. It claimed four convicted paedophiles and a convicted rapist were still registered as doctors.
Aphra said there were “some things it could do quickly,” while others required legislative change.
CEO Martin Fletcher said sexual exploitation of patients was a gross abuse of trust and could lead to long-lasting and profound damage.
“The community rightly expects that only practitioners who are fit to practise will be registered and that regulators will take prompt action to protect patients from sexual misconduct by health practitioners,” he said.
Pain Medicine Department, UWA’s Laboratory for Drug Delivery and Telethon Kids Institute.
A team led by Professor Britta Regli-von UngernSternberg, foundation chair of Paediatric Anaesthesia at UWA and consultant anaesthetist at PCH, has the most active patient-centred paediatric anaesthesia research program in Australasia.
It developed a chocolate-based delivery system to mask the bitter taste of some medications.
“We have learnt from history and made many changes to better protect patients from sexual misconduct over the past five years, but there is always scope to improve and do more.”
Ahpra and the National Boards will hold a public review of the criminal history registration standard which applies to all registered health practitioners, and how it is applied to sexual misconduct offences.
Ahpra said it had also presented a wider blueprint for reform to all states and territories to provide a more transparent regulatory system for patients and the public.
A community-based support service by Silverchain and Asthma
WA for people with chronic obstructive pulmonary disease is hoped to reduce re-admissions and associated health care costs.
The service, which is offered to non-oxygen-dependent COPD patients discharged from hospital, is funded by the WA Primary Health
Alliance and made possible through the Australian Government’s Primary Health Network Program.
The joint COPD program was originally offered as a small trial before expanding across the Perth metropolitan region in July 2021. A study of the expanded service showed that clients had less anxiety about their condition and were better able to self-manage it.
COPD is the fifth leading cause of death, the third leading specific cause of total disease burden and the leading cause of potentially preventable hospitalisations for men.
The State Government has awarded four WA cancer specialists a share in $905,000 via the WA Cancer Fellowship program.
In its 10th year, the program supports doctors to develop experience and skills with the goal
continued on Page 6
A renowned WA ophthalmologist who led the development of a revolutionary intervention to treat glaucoma has been awarded an




Professor Anna Nowak, an academic with clinical and research programs in mesothelioma and neuro-oncology, has been appointed Deputy Vice-Chancellor Research at UWA and has relinquished her clinical practice.

One-off Strengthening Medicare General Practice grants of $25,000 to $50,000 will be administered in Western Australia by the WA Primary Health Alliance. Grants can focus on digital health, infection prevention and control, and maintaining RACGP standards.
Yvonne Timson is the new CEO of Community Vision Australia, a not-for-profit which helps West Australians with home care, disability and family day care service programs.

Among the West Australians recognised with recent Australia Day honours were Health Department Director-General Dr David RussellWeisz, who received a Public Service Medal, and long-time Moora GP Dr Bernard Chapman, who received a Medal of the Order of Australia.
Sam Bloom, twice World Para Surfing Champion and inspiration for the movie Penguin Bloom, will be a keynote speaker at this month’s WA Rural Health Conference at the Perth Convention and Exhibition Centre on March 11-12.
continued from Page 6 of improving health outcomes for cancer patients.
Funding for salaries would be covered for one year in the form of two streams – training and research. Fellowships are extended to WA medical practitioners close to completion or who have recently completed a specialist qualification and are practising in a cancerrelated specialty.
Those awarded fellowships for 2023 are:
Dr Andrew Fantoni to improve understanding of lung cancer; Dr Piyush Grover to develop allergooncology; Dr Tulene Kendrick to refine the diagnosis of acute myeloid leukaemia; and Dr Jessica Nash for a project to improve lung cancer care.
Peel-based GPs are being offered incentives to upskill, with the hope it will help retain doctors in one of the fastest-growing regions in WA.
WA Primary Health Alliance and Rural Health West are offering doctors access to the Peel GP Incentive Fund Initiative’s education and training support project. They will have access to activities including the CPD Support Subsidy, the Peel GP Health Forum, a mental health skills training workshop, conferences, procedural forums, upskilling workshops and evening educational sessions.
This initiative is part of a wider focus on developing sustainable GP recruitment and retention strategies to improve patient access to primary health care in the region. WAPHA general manager of strategy and engagement Chris Kane said solutions to the GP recruitment issues facing the region could equally be applied throughout the state.
“There is no one solution to GP recruitment and the Peel GP Incentive Fund Initiative has therefore looked to deliver incentives including training, recruitment assistance and local networking that, together, help to make a place attractive to new and existing GPs,” she said.
Participant dosing in the Phase 1 clinical trial to test the safety of the stroke drug ARG-007 has been completed, with healthy participants showing no serious adverse events.
This neuroprotective peptide drug developed by researchers at the Perron Institute and UWA is a novel therapeutic aimed at reducing brain tissue death after ischaemic stroke.
It is being commercialised by WA biotechnology company Argenica Therapeutics.

Results of the Phase 1 trial at Linear Clinical Research indicate the drug is safe and well tolerated in healthy participants.
Perron’s head of stroke laboratory
Researchers at Perth’s Lion Eye Institute and Monash University have improved understanding of how the immune system is regulated to prevent disease, identifying a previously unknown role of ‘natural killer’ immune cells.
The study identified a group of immune cells – tissue-resident memory natural killer (NKRM) cells – which limit immune responses in tissues and prevent autoimmunity.
While more research is required, the discovery may ultimately be used to treat autoimmune diseases like Sjogren’s Syndrome and possibly chronic inflammatory conditions.
Originally, NK cells were thought to be short-lived cells that circulate in the blood with the sole function of identifying and quickly killing virally infected or damaged cells.
The team’s previous research established that NK cells’ role is far more complex, and the latest study demonstrates for the first time that a subset
At Medical Forum, we love a bit of serendipity.
Dr Chris Gunnell, who heads obstetrics and gynaecology at St John of Hospital in Murdoch, tells us that he graduated from UWA in 1987, in the same year as Dr Genevieve Robbins. They were friends at medical school and have remained so.

Last year, Chris’s son Alex and Genevieve’s daughter Emma graduated as doctors from Notre Dame University. The pair were their year reps and acted as MCs at their graduation ball in December.

To top it off, Emma’s godmother Dr Anita Cvitanovich, who graduated in the same year as Chris and Genevieve and also attended the ball, saw her daughter Kate graduate as a doctor from Notre Dame a few years ago.
Doctors and health industry professionals will be putting in a strong show at this month’s charity cycling event, the Hawaiian Ride for Youth.
Among those doing the ride will be Dr Phil Downing, an inner-city Perth GP who sees many young people and estimates he spends 80% of his day helping people with their mental health.
The WA Primary Health Alliance will be putting in a strong show of support, with CEO Learne Durrington, general manager Rob Salvage and chief digital transformation officer Giles Nunis all getting on their bikes.
research and Argenica chief scientific officer Professor Bruno Meloni said additional clinical studies would test the safety and efficacy of ARG-007 in stroke patients. Plans were underway for a
Phase 2 trial to assess the safety, tolerability and efficacy of the drug in ischaemic stroke patients in Australian hospitals, and phase 1 trial data will be finalised and submitted as part of the ethics approval process.
of NK cells, NKRM, are critical in regulating immune responses in tissues.
Professor Mariapia Degli-Esposti, head of experimental and viral immunology at LEI, said the findings improved understanding of how the immune system was regulated to prevent disease.

“One of the main obstacles in cancer immunotherapy… is the development of immune-related adverse events, which include the development or flare-up of autoimmune complications,” she said. “These events are due to ‘super’ or ‘uncontrolled’ activation of the immune system as a result of the brakes being removed by the therapeutic strategy.
“Furthermore, many therapies cause collateral damage to tissues where tumours are localised. Thus, NKRM may be an adjunct or follow-up therapy to restore immune balance and bring back tissue health.”
From March 21 to 25, the event will see a record 160 riders traverse three traditional pelotons – coastal, inland and Wheatbelt – cycling more than 700 kilometres from Albany to Perth over four-and-a-half days. What began as a small charity event with 24 riders in 2003 has grown in to one of Australia’s most prominent charity cycling events, and the landmark fundraising activity for Youth Focus, which delivers mental health services to young West Australians.
Hawaiian Ride for Youth chair Christina Matthews said the event has become a fundamental platform for highlighting the mental health challenges faced by young people.


Few people would dispute that Medicare is no longer fit for purpose for either patients or doctors, and one of the major casualties is plummeting bulk billing rates, as Cathy O’Leary explains.
One of the first challenges in unpicking dwindling bulk billing rates is getting reliable figures, with a wide variation of estimates across industry and government.
Cleanbill – a website that has collated and published GPs’ fees since 2017 – recently calculated that fewer than half of metropolitan practices still offered universal bulk billing, including fewer than 30% of practices in Perth.
It collated its figures by hiring contractors – in the guise of would-be patients – to call more than 4000 GP practices between August and December 2022, without indicating the information would be published. It subsequently released other survey results which it claimed showed the high and lows of GPs fees, again using contractors who contacted practices directly.
Cleanbill said doctors in one inner-city Sydney suburb were charging an average of $117 for a standard consultation – with an out-of-pocket cost for patients of nearly $77 – while the cheapest postcode was Perth’s Rivervale, with a fee average of $57.
Official health statistics paint a different picture, with data released at the end of last year suggesting bulk billing rates among GPs had fallen to about 83% – the lowest figure since December 2013.
But industry analysts argue the figures do not tell the full story because they are based on services billed rather than the percentage of patients who have all their costs covered.
In the past 12 months, increasing numbers of GP clinics have written to their patients advising they would no longer bulk bill, with competing practices in suburbs even working together to scrap bulk billing from the same date, to prevent patients from jumping ship from one practice to the other in the hope of avoiding a gap fee. And as far as the much-hoped increases to Medicare rebates are concerned, there were no clear indications of what lies ahead from the recently released Strengthening Medicare report.
The Australian Medical Association has been calling for at least a doubling of the rebate, with the peak doctors’ lobby saying general practice needed urgent immediate funding before it could start planning for long-term changes.
While Federal Health Minister Mark Butler agreed more needed to be done to improve access to general practice and primary care – and he did not rule out increases to the Medicare rebate – he added it was “not just about more money” and that would become clear on Budget night.
The Royal Australian College of GPs cautiously welcomed
many measures in the report but said there was “a high level of ambiguity” and “the devil is in the detail”.
RACGP WA chair Dr Ramya Raman told Medical Forum that some of the college’s recommendations to government featured in the report, including voluntary patient enrolment.
“But again, there is little detail on the proposed model and it is critical that we get this right,” she said. “In the United Kingdom, the capitation approach has seen many GPs doing a lot more for less, at the expense of patient care, and that must be avoided at all costs.”
Dr Raman said the decline in bulk billing was deeply concerning because it was making it harder for people to access the care they needed. Healthcare costs were continuing to rise due to the increasing costs of consumables, rent, insurance, new technologies and medicines, and the wages of a skilled labour force.
“Meanwhile Medicare rebates are simply far too low – they were never properly indexed and the freeze ripped $2 billion from general practice patients … and counting,” she said.
“And this is putting pressure on GPs who just want to do the best to care for their patients, and too often end up subsidising
patient care, such as billing a short consult when we’ve spent longer with patients because they need more time to talk through all their concerns.”
Dr Raman said the decline in bulk billing was likely to be particularly challenging for people with complex health needs, as they often required more time with their GP to address their health concerns.
“That’s why we continue to push for increased rebates, particularly for longer consultations, to allow GPs to spend more time with their patients and get to the root of health issues they present with.”
And while there are calls for the rebate to be increased substantially, many industry commentators say it not politically realistic – or appealing – to hand GPs a bucket of extra money for seemingly nothing in return.
And GPs hoping for a substantial increase in Medicare rebates across the board might be disappointed, with political chatter suggesting increases will be targeted.

A report by the Gratton Institute late last year argued that GPs’ work has become much more complex but how general practice was structured and funded had
continued on Page 13
Official health statistics paint a different picture, with data released at the end of last year suggesting bulk billing rates among GPs had fallen to about 83% – the lowest figure since December 2013.



continued from Page 11
not kept up. It advocated making general practice “a team sport” with many clinicians working under the leadership of a GP to provide better care.
To achieve this, the Federal Government would need to dismantle the regulatory and funding barriers that forced GPs to go it alone. To accelerate the change, 1000 more clinicians such as nurses and physiotherapists should be employed in general practices in the communities that needed them most.
The report argued that GPs should be able to choose a new funding model which supported team care and enabled them to spend more time on complex cases such as combining appointment fees with a flexible budget for each patient based on their level of need.
In the meantime, while the current rebate for an item 23 is $39.75, the fee most GPs are now charging for that service is thought to be $85 or more, based on the fee calculated by the AMA, to be reasonable.
Dr Raman said the rebate for item 23 was a clear example of government funding not keeping up with the cost of providing care.
She said the patient rebate for the average GP consult (Level B, less than 20 minutes) increased by a “paltry” 1.6% or 65 cents to $39.75 on July 1, 2022. By comparison, the Consumer Price Index rose 1.9% in the December 2022 quarter and 7.8% annually.
“Band-aid solutions will not solve the crisis Australia is seeing,” she said.” Long-term, we need major health system reform and serious investment in general practice care because this is what keeps people healthy and out of hospital.
“Any long-term health funding reform must build the role of GPs as the stewards of patient care, working hand-in-glove with multidisciplinary health professionals.
“The government also needs urgently to stem the bleeding and provide relief for patients struggling to access care.”
Dr Raman said this required shortterm measures, including improving access to care by tripling bulk billing incentives and increasing Medicare rebates by 20% for longer, complex consultations.
In addition, funding needed to be improved for primary care services for people aged over 65, and those with mental health conditions and disability, while funding was also needed for patients to see their GP after an unplanned hospital visit, she said.
While the bigger picture needed the GP workforce to be boosted by fast-tracking entry for international doctors, reinstating the subsidy for their training, supporting junior doctors to intern in general practice, and introducing payroll tax exemption for independent tenant GPs to prevent more practices closing.
“Band-aid solutions will not solve the crisis Australia is seeing... Long-term, we need major health system reform and serious investment in general practice care because this is what keeps people healthy and out of hospital.”
In the preamble to a recent national webinar for GPs, the case was made that the solution to ambulance ramping and emergency department overcrowding was not in the hands of hospitals themselves, but with general practice.
“For years, GPs have had to deal with the fallout from a broken system that has overburdened practices and left them on their knees,” the webinar’s introduction warned.
“The solution lies in designing our care system and shaping it for what it does well – caring for individuals as part of a team and improving primary care outcomes.”
The event, General practice in a rapidly changing world, was hosted by health commentator Dr Norman Swan and run in association with
the WA Primary Health Alliance and the Perth North, Perth South and Country WA primary health networks.
One of the key speakers needed little backgrounding about the problem at hand. As WA’s chief medical officer and a former Australian Medical Association WA president, Dr Simon Towler knows only too well the see-saw that hovers between primary care and acute health services.
He told the webinar that when it came to the question of whether general practice could salvage the Australian health care system, it was clear that it would require some fundamental shifts in the model that had been in place for 45 years.

“I’m an absolute fan of general practice and have been on the board of WAGPET looking at how we improve primary care services in the country,” he said.
“But an entirely medically driven model in general practice, not properly supported by allied health, is not really addressing the chronic disease model. I’m not going to give all the solutions, but if we keep doing what we’re doing it’s not going to address the health care needs of the community we have now.
“What we’re seeing in emergency departments – although there will be many people who will argue that people who go to EDs deserve to be seen – is a lot of people who are there partly because they can’t get a [GP] appointment and partly because they’d rather not pay anything to general practice (when in fact gap payments are coming in almost routinely), but we know that general practice could provide the necessary care.
“In addition, general practice is grossly under-utilised in managing conditions for which they are capable.”
WA’s chief medical officer Dr Simon Towler argues that a complete dependence on the medical model is flawed, and more needs to be done to better use GPs and embrace the role of allied health.
Dr Towler said that in WA if you want to see a neurologist as an outpatient, “you are going to wait for a very long time.”
“The GP model is fundamentally different to hospital care, it is a partnership with the patient over time, exploring diagnosis, early therapies and response to treatments. Hospitals do not provide that.
“What we’re seeing now with longCOVID, the sub-specialty model is not working at all and we’ve seen the introduction of a long-COVID clinic in East Metro Health Service, which is multi-disciplinary, tied back to the GPs, and providing higher quality care.”
Dr Towler said while the current system was clearly not working, the hospital assumption of pushing patients back out into the community because of bed shortages and ED overcrowding was not the solution.
“We’ve seen substantial growth in medical school enrolments and, despite the anxieties currently about the transition in GP training to a college-led program, the
Gratton report found GP numbers are not dropping proportionally.”
(A report by the Gratton Institute late last year found that Australia has plenty of GPs, but they are not always in the right areas. It argued that what was lacking was supporting clinicians to help GPs respond to a growing tide of chronic disease.)
But Dr Towler said he recognised that Australia needed to grow its medical workforce and there were substantial regional shortages.
“COVID over the last few years has reduced the number of international medical graduates coming to Australia and we know that the interest among medical graduates for a career in general practice seems to have also waned.
“So, there is a lot to do in this space and it’s not an easy solution. If you look at WA, being a GP in a small town literally hundreds of kilometres from any other support, is also different to the challenges that might be faced in other jurisdictions.”
Dr Towler said efforts were underway to fill the gaps, such as accelerated pathways, workplacebased assessment programs and close collaboration with ACCRM and RACGP in the training transition.
Needs varied from region to region and there was not a one-size-fits-all solution.
“Where we need to have a practitioner where there isn’t one, we do need to improve the attraction, and some councils and shires in WA offer extraordinary financial support to just get a single doctor to go to a country town.
“We know that when primary care is functioning well, the outcomes for the community are much better, and tertiary and secondary hospital utilisation goes down.”
But Dr Towler said that a complete dependence on the medical component meant there was still going to be difficulties meeting the demand.
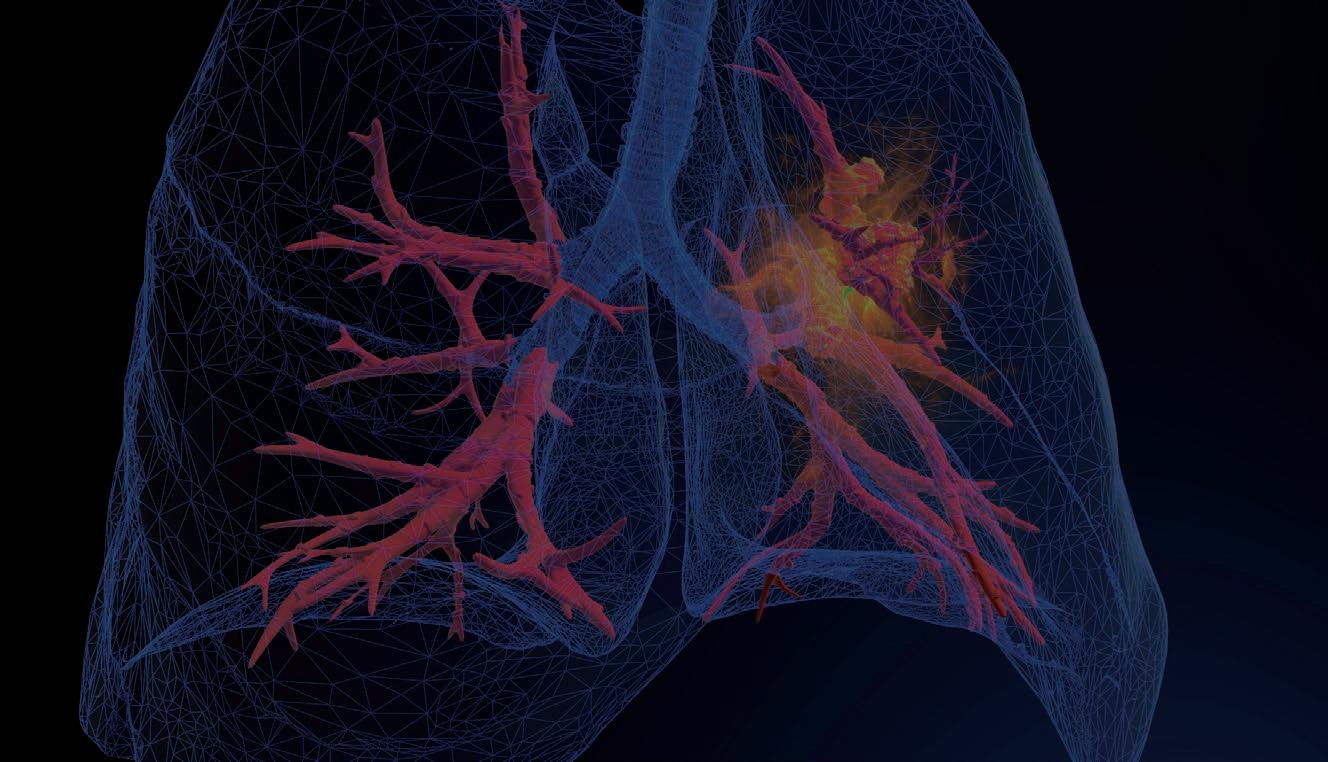
Lung cancer is Australia’s biggest cancer killer, often due to late diagnosis. But a federally funded screening program will offer hope when it comes to survival rates.
 By Suzanne Harrison
By Suzanne Harrison
About five years ago, now 69-year-old Leonie Bamford was told she had lung cancer. Her condition was symptomless, and the fact she had a diagnosis at all was sheer luck.

Not long before, Leonie and her husband, Alan, now 71, had made a routine visit to their GP to check out Alan’s persistent cough. Both being smokers, the GP gave them a leaflet about screening trials then underway at Fiona Stanley Hospital, so they decided to give it a go.
“The trial was just about finished, and they found a lump on my right lung which (over time) had changed form,” says the motherof-three from her Kelmscott home, “so they did a biopsy, and it was cancerous.”
The immediate surgery that followed has saved her life. “If I hadn’t had been in the trial, I’d be dead by now,” said Leonie, now a non-smoker for four years.
Leonie was luckier than many. Lung cancer is the leading cause of cancer death in Australia, according to Cancer Australia, and estimates showed more than 8,600 Australians would die from it in 2022. Lung Foundation Australia says that it’s often diagnosed too late, when treatment options are limited, contributing to an extremely low, 20% five-year survival rate.
But if new screening programs are rolled out – in line with countries such as the UK and to some extent, the US – this could change.
In October last year, the Medical Services Advisory Committee recommended the Federal Government implement a national lung cancer screening program, with the aim of supporting earlier detection of lung cancer.
This welcome announcement resulted from an application from Cancer Australia, following extensive analysis into the feasibility of a national lung cancer screening program.
“The (MSAC) review was conducted independently and concluded with high certainty that the evidence showed the proposed program would reduce lung cancer mortality,” said Cancer Council Australia CEO Professor Tanya Buchanan at the time.
The advice received by MSAC includes a recommendation to implement a new Medicare item for low-dose, computed tomography scans for asymptomatic high-risk Australians (smokers or ex-heavy smokers) to help
detect lung cancer earlier, which would ultimately provide greater treatment options and a higher likelihood of survival.
A study in late 2022 by Australia’s Daffodil Centre, and published in the British Journal of Cancer, strengthened the economic case for a targeted lung cancer screening program in Australia. The study updated costeffectiveness estimates in an Australian context based on the findings of two major international trials of lung cancer screening, the Dutch-Belgian NELSON trial and the US National Lung Screening Trial. It showed that if the results were adapted to the Australian health system, lung cancer screening for Australians with a history of heavy smoking would have a favourable cost-effectiveness ratio given new evidence from the NELSON trial published in 2020.
This study helped inform the supportive recommendation to the government from the MSAC.
“The greatest challenge in cancer screening is ensuring that it delivers more benefit than harm to the population,” said Associate Professor and research fellow at the Daffodil Centre Marianne Weber.
“For most cancers, there are no tests for asymptomatic populations that work without causing significant harms, such as inaccurate results that lead to unnecessary harmful diagnostic tests and treatments, and stress for individuals affected and out-ofpocket costs.
“Governments also consider costeffectiveness as a matter of course. These results, which show targeted lung cancer screening using lowdose computed tomography, could be more cost-effective than previous estimates indicated, strengthening the economic case for such a program.”
In 2019, Dr Weber wrote for Cancer Council NSW that only breast, bowel, and cervical cancers have national cancer screening programs in Australia, and on current evidence, low-dose CT scans for long-term smokers and ex-smokers are the most likely path towards targeted lung cancer screening. As for Leonie, she was involved close to home in the International Lung Screen Trial at Fiona Stanley
Hospital, a lung cancer screening program with the same low-dose chest CT. The ILST began with five centres in Australia and involved international collaborators in Canada, Hong Kong, England and Spain.
West Australian participants were recruited from the community and attended both FSH and Sir Charles Gairdner Hospital, led by FSH respiratory physician Dr Annette McWilliams and project manager Jacqueline Logan.

“Lung cancer kills so many people, but is so treatable when found early,” said Dr McWilliams, who has spent a large part of her career dedicated to lung cancer screening research, both overseas and more recently, in Perth with the ILST.
Dr McWilliams undertook a fellowship in Canada in 2000 on the viability of low-dose CT scans for lung cancer, and as of 2017, comanaged the ILTS trial.
“I’ve been working on lung cancer screening for 20-odd years, and I know that it works,” she said.
The challenge, however, is not whether early detection and government-funded scans reduce deaths, but the protocols of implementation.
“We’re moving from the world of research into clinical practice. We know low-dose CT reduces death rates in an organised program, but you need to have a standardised approach and the infrastructure in place to monitor it all,” she said.
Dr McWilliams said final details – such as the age range and risk assessments of those who qualify –were yet to be released.
“It has to be well thought out and done properly,” she said.
In the UK, mobile pilot programs have been implemented following government approval. The Targeted Lungs Health Check program focuses on those most at risk of lung cancer and will gradually expand.
Lung Foundation Australia’s CEO Mark Brooke said a screening program would bring lung cancer prevention in line with other leading cancers. Bowel, cervical and breast cancers all have a significantly higher five-year survival rate at 70, 74, and 92% respectively.
The screening program proposed by Cancer Australia includes a recommendation for seven mobile screening units, which will bring early detection services to regional and remote areas that currently face significant inequity of access.
Cancer Australia’s report found that not only will the program save over 12,000 lives in the first 10 years, it will also reduce the financial burden to the health system associated with lung cancer in the long term.
At FSH, Leonie was just one of the 21 WA participants in the ILTS study. Yet Dr McWilliams said that in WA alone, there were between 1200 and 1400 cases recorded each year, and with an ageing population, those rates would not be going down.
Leonie did not have to undergo chemotherapy, so believes she was one of the luckier ones. And apart from her breathing being “not as good as it used to be” she does now exercise regularly. Plus, her husband is also off the cigarettes and has been for a year.
“We’re feeling marvellous,” Leonie said, “and I am so grateful.”
With an estimated 800,000 people impacted by adult ADHD nationally, and a price tag of nearly $20 billion a year in social and economic costs, the proliferation of what is often considered a childhood condition has real consequences for society.
By Eric MartinLiterature reviews show that adults with ADHD have a lower life expectancy, are 10 times more likely to visit the doctor and are three times more likely to present at an ED. They are also 42% less likely to be fully employed and on average earn significantly less than their peers.
Considering estimates that up to 75% of children diagnosed with ADHD experience symptoms into adulthood, Medical Forum spoke with Dr Roger Paterson, a psychiatrist with ADHD WA, and Dr Michele Toner, Australia’s first adult ADHD coach and a member of ADHD WA’s Professional Advisory Board, to discuss the latest in diagnosis and treatment.
Dr Paterson said that when he trained in child psychiatry in the late 1980s, he was taught that ADHD existed, but only in children and teenagers, and most, by their mid-teens, had grown out of it.

“Now we know that is not true. People thought that because hyperactive kids became less hyperactive, they appeared to calm down and the hyperactivity seemed to lessen, that their ADHD was gone.
“But no. If they had tested for inattention, that was still there and persisted. The fact the hyperactivity had gone away did not mean that the ADHD had gone. A lot of adults suffer from inattention that could be subtle and harder to pick up.”
continued on Page 20


continued from Page 18
Recent evidence supports the view that children with ADHD do not “outgrow” the disorder, rather, adult ADHD often has a more diverse clinical presentation that exceeds the typical motor symptoms described in children and includes a wider range of emotional dysregulation and functional impairment.
“Adults present for various reasons and some present quite late, but, essentially, adult ADHD is really just childhood ADHD that has been missed for various reasons, such as, for example, they were not the bouncy type,” Dr Paterson said.
“They were less hyperactive and more the inattentive type, which can often be the case in girls, who are normally better behaved than boys, and can mask their symptoms.
“Bright kids or those who have got a good, supportive family or school, can mask their ADHD and may slip through the net. They may start to struggle in Years 11 and 12, and really struggle if they go through to tertiary education.
“Many of them have also got some reading and maths problems and, by Years 11 and 12, start hitting the wall and that is where I start to specialise. I come in around the age of 15 or 16 seeing these kids.”
ADHD has long been associated with educational difficulties and students often require extra help, attend special classes, repeat grades, and have higher rates of academic suspension and dropout. Similarly, university students with ADHD have lower grades on average and are less likely to graduate than their peers.
“The issue with university is that where they may have had good support at home and school to help get them through Year 12, at university they are left to fend for themselves. It is much better than it used to be with mentoring and support, but it is still very much up to them,” Dr Paterson said.

“They are told, ‘Here is the lecture theatre, this is when you are going to sit through your exams, and we will see you in six months,’ and they just fall apart.”
He said that while adults with ADHD could be quite impressive, engaging, charismatic and full of ideas, they could become frustrated over work careers that ‘could have been’.
Dr Michele Toner said people with ADHD did not get the same memo as neurotypicals: ‘You do not do this, you do it this way; this is how you get to places on time.
“They do not naturally absorb or learn those skills. The most mundane tasks are often the most challenging,” she said.
“Organisation, time management, prioritisation: they are the things that really interfere with someone with ADHD, and their ability to be successful and thrive, she said.
“There is a huge amount of misunderstanding because of assumptions that someone who is intelligent, and may hold an engineering or a medical degree, should be able to manage their time if they just tried harder.
“People can trivialise those challenges when in fact it is very easy for them to design a bridge or an oil and gas platform out in the ocean, but actually organising themselves to get to work on time is extremely difficult.”
Dr Paterson said people could struggle when they started in the workplace and needed to march to the beat of a boss's drum rather than working at a pace or in a pattern that suited them.
“People with ADHD are notorious for working in bursts, such as doing nothing for a week and then pulling an all-nighter to get something done,” he said. “And you just cannot do that in the workplace.”
However, Dr Toner said people with ADHD could learn skills and turn their lives around when they found out the best way for them to do things.
“ADHD coaching is a bit like being an anthropologist really, it is about finding what is inherent in that person: so, if someone is visually strong and they are able to see things and design them in their mind’s eye, you want to translate their tasks into a visual medium, something that they can see and do,” she said.
Adults with ADHD can also find relationships more challenging, both in the workplace and romantically, according to Dr Paterson.
A recent study showed that in a sample of about 1000 adults, those with ADHD were significantly more likely to have been divorced (28% compared with 15% in the wider population) and were significantly less satisfied with their personal, social, and professional lives.
“People with ADHD can be successful at starting relationships, but often do not have long-lasting relationships,” Dr Paterson said. “They tend to partner with people who are steady, who remain fairly central, and they gravitate around their partner's consistency.”
Dr Toner said a lot of relationship problems came down to communication and a misunderstanding of what was happening for the person with ADHD.
“I often have the person's partner come in for one session. Together, they come to an understanding. By making an adjustment in their communication and their family systems, they can reduce misunderstandings such as forgetting to pay bills or being late for family functions.”
Dr Paterson said that it was common for adults to realise that they may be impacted by the condition when they bring in a relative, often a child, for diagnosis.
“Family history is an extremely common risk for presentation and ADHD can occur at any age. Many of my presentations are from
parents who come along and say, ‘my child has just been diagnosed and when I looked at the symptoms, I realised it was me’,” he said.
“My oldest patient is 91 and lives in a nursing home, but he was incredibly busy looking after his wife for many years and needed his wits about him. I was treating his son and grandson and he said, ‘it sounds like me’.”
Dr Toner’s interest in the condition was sparked because she had family who were diagnosed with ADHD. It became a personal quest to find out as much as she could to support them.
She said one of the greatest sources of contention around the diagnosis of adult ADHD was the high degree of associated co-morbidities that could influence the potential accuracy of assessment strategies, such as the fact that ADHD was often diagnosed later in people with anxiety, who may be less impulsive because of this condition.
Overall, the risk for anxiety disorders is nearly 50% higher for people with ADHD than the general population.

“It is rare to see someone with just straight ADHD. Most of our clients have some anxiety and we often find that we are addressing such issues by helping them to address their ADHD,” Dr Toner said.
“Much of the anxiety that accompanies ADHD is anxiety around everyday things: ‘Am I going to forget something or am I going to say something stupid? Am I going to miss a deadline? Am I going to be late?’
“Often there is this terrible underlying anxiety of waiting for something bad to happen, and as people get more control in their lives, it helps them to manage that anxiety as well.”
She said that while ADHD coaches were not qualified to treat associated psychological conditions, they often worked with other therapists.
Dr Paterson said ADHD was comorbid “with just about everything to a certain degree.”
“If you wake up each day and you have trouble concentrating, well, straight away, you have trouble organising breakfast, getting dressed, or even thinking ‘where am I heading?’,” he said.
“If you can’t concentrate and get organised and productive, you are stressed, and once you are stressed, you are more likely to reveal all sorts of possible co-morbidities.
“Stress might push you down the path of substance abuse to
calm your busy mind, or you have trouble getting on with people, develop a personality disorder, or you could have this low-grade anxiety through your life, impacting every aspect of your thinking.”
Another condition associated with ADHD has been increased criminality, or rates of incarceration at least, with researchers from the US reporting that 47% of patients with ADHD had at least one criminal sentence.
“A lot of young teenagers head down the path of leaving school and becoming delinquent – the prisons in Australia are about one third full of people with ADHD, which is why people are saying places like Banksia Hill should be improved – not nasty prisons, but really five stars in term of great rehabilitation.
“I say, ‘Look, you're only 20 or 30 or 40, and you are only about a third of the way through life, you have many good years ahead. You have some life experiences, let’s use those and your knowledge now and we can start applying it.’
“I want to give them some hope for the future, and we have a gradual acceptance that this is the problem. A lot of people can be full of

Eligible HBF members* can now access this support program which reflects the latest evidence in osteoarthritis research, delivered and supported by trained physiotherapists.
Fully covered for eligible HBF members*
Eligible members can access the program at no additional cost when delivered by a participating Life Ready clinic.
Proven 33% reduction in pain intensity on completion of the program1
3 months after the program, participants experienced an average pain reduction of 33%. There was also an average improvement in joint-related quality of life of 31% for knee participants, with 47% of these participants also reporting a reduction in use of pain relief medication.
Applied to everyday activities – enhancing success
Participants are provided education sessions and given exercises that are suitable and practical for everyday application.
Group sessions delivered by physiotherapists
6 weeks of exercise sessions, education classes and follow up to help patients manage symptoms and develop long term habits.
For more ways HBF can support your patients with a range of health programs visit hbf.com.au/health programs
continued from Page 21
remorse and sometimes blame for parents not taking to them to see someone when they were a child – they are upset about what could have been.
“Especially after they start the medication and suddenly their brains are switched on, they go, ‘Oh, if only my brain had been like this through school and relationships and work, I could have done such and such’.”
Dr Paterson said treating adults was often easier than working with children, because adults had a greater self-awareness and could give good feedback.
“However, with adults, I also make a point of always asking a relative or friend to come along and give some background, and sometimes to keep coming, because some people are not all that aware of how they are going and the impact of the medication,” he said.
“I have even had some patients say, ‘I see absolutely no difference at all,’ but in the background, the spouse or the mother is saying, ‘No, they are fantastic – it is a big change’.”
Dr Paterson said the rate of ADHD was about 5% in children and half that in adults, whereas the rates of taking medication in WA was around 2% in children and close to 1% in adults.
While there was now a range of new, slow-release tablets, the medication had changed little since they were first introduced back in the 1940s and ’50s.
“Dexamphetamine and Ritalin are still exceptionally good drugs and are still being used, though they have now developed long-acting versions of both, which has been the major change,” he said. “They are what we call clean pills: they are good with few side effects; they are not addictive; they are not dangerous, and you can take them forever. Of all the medications prescribed in psychiatry, they are by far the best.”
Psycho-stimulants such as
dexamphetamine sulphate are classified as schedule 8 controlled drugs due to their euphoric effect and ‘likeability’, yet there is limited evidence of psycho-stimulant abuse among ADHD patients.
“Because they are stimulants, they can be abused,” Dr Paterson explained, “but it is low-grade abuse: the bikies are not interested, there is no great street trade in them, but there is a little bit at universities with students that are buying and selling them around exam time.
“Mostly, folk will take them, and they are a bit like a cup of tea or coffee, they have a bit of a lift, but not an enormous difference, whereas someone with ADHD will go, ‘Wow, these are fantastic!’ And some of them will then get accurately diagnosed and treated, and it makes a real difference to them.
“We are only scratching the surface of how the brain works, but as far as we can understand ADHD, it seems to be that parts of the brain are underactive.”
One possible explanation is that ADHD and mood disorders stem from similar neurobiology, with neuroimaging studies revealing differences in volume and activity in the frontal lobe, responsible for attention, behaviour selection and emotion in adults with ADHD and psychiatric disorders.
Studies of neurotransmitters have also pointed to abnormalities in dopamine and norepinephrine signalling, which has been used to support the use of psychostimulants to treat individuals with ADHD due to the dopamine increases.
“When we stimulate with dexamphetamine or Ritalin, the underactive parts of the brain come to life and their executive function works better,” Dr Paterson said.
“The analogy we often use is the underactive parts of the brain are like the conductor and the rest of the brain is the orchestra: ADHD people have their orchestra playing, but no conductor; everybody is off doing their own thing.
“As they take the tablets each day, they wake up the brain, and at the
end of the day, the tablets stop working and you go to sleep. They wear off and each day you start again. You get instant effect and instant wear off at the end of the day.”
In Australia, GPs can investigate but cannot initiate ADHD treatment.
“It is still the province of specialists and probably will remain so for a while yet. We have to be careful about who starts on the medication, how it is controlled and then, once it is stabilised, GPs can get involved with code prescribing,” Dr Paterson said.
“And that is going to increase with the new regulations that are coming in WA to allow more GP involvement with less bureaucratic regulations attached to them, which is a good thing.”
Dr Toner said people with ADHD could also benefit from seeing a coach, particularly if there was a long waitlist to see a specialist. As there was no medical rebate for coaching, people did not need a referral.
“Awareness of ADHD coaching has grown among medical professionals, certainly among the psychiatrists and paediatricians who treat ADHD,” Dr Toner said. Dr Paterson said GPs should have their antenna up for anyone who had mental health problems, to ask more about what their concentration was like in primary school.
“Particularly if they have that lowgrade chronic anxiety or depression and frustration with life, and they have not had much success in relationships or work, you might think, ‘Hang on, what is going on here?’
“Sometimes they are obviously overactive, restless and fidgety and you can tell at the interview that they are a bit all over the shop, but not always – they could be masking their ADHD, especially the inattentive types.”
For Dr Lawrie Beilin, the secret to his career success and happiness has been in choosing to be a clinician, researcher and mentor.
 By Ara Jansen
By Ara Jansen
As a young lad, sitting in a cinema watching Danny Kaye, Lawrie Beilin wanted to be a film star.
Soon after realising he “probably wasn’t up to it”, two incidents subtly shifted the London boy’s thoughts to medicine. Firstly, an anaphylactic reaction to a tetanus shot put him under the care of a doctor whose calm and caring bedside manner was memorable.
Lawrie later found himself in hospital after lopping off the end of a finger in a door. At Middlesex Hospital he was seen by a surgeon, a young man (at least to Lawrie) accompanied by a group of students.
“He was pretty calm and reassuring,” remembers Lawrie, more formally known as Emeritus Professor Lawrie Beilin. “Two things struck me – his attitude and focus, and then his skill, plus his attitude towards his students and teaching. At that moment I felt I wanted to be a doctor.
“I’d always been interested in nature and biology. I thought it was wonderful. How do things grow and develop? How do we become thinking human beings? I can’t really explain it, the interest was suddenly just there and I wanted to do medicine.
“I also have to say that my father was an optician and was disappointed that he didn’t do medicine. I don’t think he ever told me that but, I think they were relieved when I wasn’t going to go for a career on the stage. I was definitely unconsciously driven by those two medical experiences.”
A hard worker with a competitive drive, Lawrie, like all other students at the time applied to all 12 medical schools across London. He failed the first five interviews but wasn’t surprised. Still in high school he was nervous plus he was a state schoolboy who didn’t play rugby, at the time a less than subtle bias in the medical fraternity. Interview number six saw him placed at King’s College Hospital.
“I remember feeling relief and what a privilege it was and that I was going to do the best I could.”
One of the first classes was dissection. There were about 120 students (including about six women) clustered around tables in groups of eight. What Lawrie remembers most is the camaraderie as well as the incredibly hard work of the following study and training years.
“I enjoyed connecting with people and patients and learning from great clinical teachers.”
Of particular influence was Dr Archie Gilpin, a heavy-smoking physician who died of cirrhosis. He showed Lawrie how to listen to and hear patients, as well as giving them the best possible advice. His manner meant people weren’t afraid to ask questions and weren’t frightened to talk to him just because he was a doctor.
Another senior doctor encouraged Lawrie to start teaching other students and share his knowledge as soon as he graduated, something he took to heart and has done all his working life and continues to do.
“I was told that students learn better from people closer in age to them. I could see how important it was to get into that habit of connecting and communicating what you have learnt to help others learn.”
Eighteen months of working at Hammersmith Hospital Royal Postgraduate Medical School taught Lawrie that it was possible to step out of the old conservative ways and combine clinical practice, research and teaching – and experience world-breaking research alongside compassionate and knowledgeable teaching.
Among other adventures, Lawrie, his wife Brenda and year-old first child spent a year working in Los Angeles during the incendiary Watts Riots of 1965 and escaped being drafted to Vietnam because of his green card.
Already with a lot of experience and accolades under his belt, Lawrie arrived in Australia from Oxford at the age of 40 – you can still hear the hint of an accent – when he accepted a job at Royal Perth Hospital as Chair of Medicine in 1977. The hospital wanted someone to reestablish and strengthen their research work as many staff had moved to Charlies.
Lawrie spent a long and respected career working at Royal Perth, with research focusing on hypertension and preventing heart attack and stroke. As his mentors suggested, his work has been a mix of clinical, research and teaching the next generation of doctors.


Lawrie received the 2021 Peter Sleight Excellence Award in Hypertension Clinical Research from the World Hypertension
League, which recognises significant contributions toward advancing hypertension research and treatment.
Now officially retired as a doctor –the 86-year-old let his licence lapse last year – he’s definitely not retired in any other sense of the word.
He’s immediate past Chair of the Royal Perth Hospital Research Foundation and until recently volunteered his time at the Royal Perth Lipid/Hypertension clinic, where he helped patients dealing with complex medical problems. He continues to do research at the foundation as well as mentoring and teaching students.
Throughout his career, he’s “enjoyed working with such fine health care workers from every background” at the hospital and foundation.
Experiencing some of communications’ greatest changes in his lifetime, technology like Zoom now allows Lawrie to collaborate, confer and consult with colleagues world-wide.
As an Honorary Senior Research Fellow at UWA, Lawrie continues to supervise PhD students and collaborates in medical research programs locally and internationally. In recognition of his extraordinary contribution to medical research in WA, the foundation recently named its highest career advancement fellowship in his name.
continued on Page 27


Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.


Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.



continued from Page 25
Once he started digging into his work with blood pressure and cholesterol in his 30s, Lawrie says it started to change his own habits around food and exercise, including feeling somewhat horrified about his medical intern lunch diet of a meat pie and Mars Bar. Apart from getting a pacemaker a few years ago, he remains fit and conscious of keeping in good health. He espouses the mental health benefits of getting up early and having a daily dip in the ocean.
He’s a husband with a “beautiful wife” of nearly 60 years, a dad and an enthusiastic grandfather to six (aged 16-24), as well as a traveler and avid and knowledgeable photographer who tackles the challenges of Photoshop. Lawrie is also a late onset piano learner and enjoys singing in choirs.

Testament to the fact that you’re never too old to learn something new, Lawrie recently completed a Bachelor of Arts, majoring in French, his first non-medical degree since becoming a doctor.
Lawrie says a sense of curiosity and humour plus an enjoyment of family, friends, nature and life in general is what gives him the

passion to get out of bed in the morning.
“All the things I do keep my brain challenged and allow me to be socially active – and they also seem good for marital harmony!
“Having grandchildren is so much more fun than having children. It’s wonderful to hand them back and you don’t have the responsibility to make all the decisions for them. I’ve loved seeing them grow up and evolve.”

My interest in trans, gender diverse, and nonbinary health began in 2008 when, as a medical student, I attended the International AIDS Conference in Mexico City. There, I talked with a trans woman who spoke of the stigma that many TGDNB people face when accessing health care and the impacts that misgendering can have.
TGDNB health was not something we were taught as medical students, but her story stuck with me and was the genesis of my most rewarding work to date.
On graduating from medical school, I specialised in general practice and still did not learn about TGDNB health in my studies. So, when I took on a role as a GP at a sexual health clinic and was told I might see TGDNB patients, I asked the clinic manager for some help.
He introduced me to the then chair of TransFolk of WA, a peer support service for TGDNB people and their loved ones, who taught me the basics of respectful and appropriate language, the use of pronouns and chosen name.
These early encounters gave me the confidence to see TGDNB patients at the practice where I was working. I soon discovered
By Dr Irene Dolan, GP and Health Pathways WA GP Clinical Editor, WA Primary Health Alliance.
that piecing together referral pathways, models of care and the clinical knowledge required was challenging.
At the same time, I was fortunate to be working as a GP Clinical Editor within Health Pathways WA at WA Primary Health Alliance. I took the opportunity to plant the seed about developing a WA-specific
transgender health and gender diversity Health Pathway.
Given the organisation’s commitment to diversity and inclusion and the deficit in information for health professionals on TGDNB health, I got the green light to proceed.
I have been fortunate to work with such a knowledgeable and engaged
As a long-time trans activist and peer supporter, I’ve watched with delight as informed consent models have surged in popularity within gender affirming care.
When I transitioned, very few of us accessed care at all, and those that did required expert knowledge from our peers. I became informed before I ever saw a clinician. Meeting
with a trans friend, I learned how she handled herself, and what preoccupied her. I became an expert through a type of field research, because non-experts were guaranteed to fail the assessments required to access GAC.
It is undoubtedly positive that trans patients no longer need to have an encyclopaedic knowledge of gender
For many doctors, transgender health was not part of their medical training, so they need resources to come up to speed.
A little knowledge goes a long way
group of subject-matter experts on the pathway’s development. This included representatives of the TGDNB community and clinical specialists from Royal Perth Hospital and Perth Children’s Hospital Gender Diversity Services who work with TGDNB people of all ages. GPs with experience in TGDNB health have also been involved in the pathway development.
Their depth of knowledge and insights into the subject matter helped to create a pathway which addresses the complexities faced by TGDNB individuals when accessing health care and some of the challenges faced by GPs when trying to help their patients access gender affirming care.
The pathway steps GPs through the assessment, management and
referral processes to specialised services for TGDNB people of all ages, offers guidance on creating welcoming clinical environments, and provides patient information and information on support organisations for individuals and their families. The pathway also includes links to useful resources and a section on professional support.
The final pathway was informed by consultation undertaken by the WA Department of Health and is a fitting example of collaboration across the depth and breadth of the health system.
The development of the pathway and a forthcoming education series has been shaped by my professional experiences. I share these to show a small amount of knowledge can go a long way and
to demonstrate the importance of lived experience.
I cannot recall another 30-minute conversation I had during medical school or GP training which has influenced my work to the same extent as that conversation in Mexico City.
I hope this work will help to bridge a gap as, equipped with knowledge and confidence, GPs can make an enormous difference to the health of TGDNB people.
ED: Health professionals can access the Transgender Health and Gender Diversity HealthPathway and associated Transgender Specialised Assessment request page, or request access. They can also register for a 2023 education series on trans, gender diverse and non-binary health.
care, for a person just questioning their gender, ‘minimum informed’ might simply be knowing that people with gender incongruence exist. Knowing we exist is one thing, knowing our forms and labels is another, and knowing how to work out if any of these forms fit you is another entirely.

people in your life perceiving you as another gender?” and “if you had a button that could change your external and/or internal gender instantly, would you press it?”
to access GAC, however it leaves us with big shoes to fill if we are to replace those older methods of information transfer. Now that our models have improved, we must be flexible enough to both adequately educate patients, while also not delaying urgent care for others.
If we are to go beyond our minimum requirements for good
Questioning “does my internal gender feel different to my external?” vs “would I feel more comfortable with a different external gender?” may each return strong feelings for a person. It is important for a trans person to understand that each of these are valid trans experiences, even if their answers contradict. Other valuable questions include “can I picture myself growing old as this gender?”, “can you imagine other
When acting on gender incongruence, the ‘minimum informed’ is knowing that hormone replacement therapy exists, understanding its side effects, intended effects and expected time frames, and its reversibility.
For most people this is a tiny piece of their puzzle. Acting on it may mean social transition. It may include dealing with other health issues. Understanding what you can and can’t change about yourself
continued on Page 31







continued from Page 29
starts before hormones and goes far beyond them.
This includes a long process of picking apart which aspects of the self are a cultural gendered expectation, and which parts may be innate or instinctual. Developing a healthy internal narrative of sex and gender is an important part of living a happy life, even for cisgender people.
A trans person who internalises negative gendered stereotypes may attribute these to themselves (from all genders too), and may even intentionally engage in problematic behaviour, having internalised this as a natural part of living as their chosen gender.
As an educator I often find it important to push back on this. I
often joke that just because my gender is valid, doesn’t mean my gender is relevant.
While we may currently lack the perfect informed consent checklist, we need not overcomplicate it. We don’t have to quiz people on gender theory for them to feel safe explaining both what they want and what they think is possible to get from transition.
A questioning person’s needs differ from a confident person who has questioned for years, but each may require urgent care. If someone has an insecurity or stereotype so extreme it may continue to negatively impact them after transition, we should be able to identify that and even challenge it without requiring assessment by a full multidisciplinary team.
All patients should know they can change their mind and should not
be judged for it, but they should also know that regret is extremely rare. Not all trans people medically transition, and some choose to take lower doses of hormones or only take them temporarily for some small changes. Clinicians and patients must also understand that some people regret not accessing HRT sooner, not pursuing a stronger regime, or not transitioning faster or slower.
A transparent, collaborative informed consent process is a massive improvement on older models of GAC, positioning patient and clinician as allies rather than adversary and gatekeeper.
Foster a collaborative environment, gather a good understanding of their personalised goals for transition, aim to reach a mutual agreement to where you each think they are well informed, create a shared agreement for you both to sign, and document it.

Trans people have always been around, evident in culture and history worldwide, including Aboriginal and Torres Strait Islander brotherboys and sistergirls, and Maori whakawā hine and tangata ira t ā ne.
Medical understanding now recognises the spectrum of gender as a normal part of human diversity. Transgender health care is not new: hormonal and surgical treatments were provided in Berlin in 1918, and the treatment of gender-dysphoric adolescents with puberty suppression and hormone treatments commenced in the Netherlands around 1991.
The US Transgender Survey 2015 of 27,715 adults found that 15% first told someone that they were transgender under the age of 15, and 37% between ages 16 and 20 –even before social media, ‘coming
out’ in adolescence was frequent. It is important to understand that some people are trans, and this is OK.
‘Conversion therapy’, or efforts to deliberately change gender identity or sexual orientation, is ineffective, harmful and unethical. Some trans individuals request medical or surgical gender-affirming treatment and experience it as medically essential; some do not want treatment.
These treatment decisions are led by the person's wishes and needs, and the risks are weighed against the risks of withholding treatment.
It is normal for children to have interests and activities that do not conform to cultural ideas of masculine and feminine. This doesn’t need assessment or diagnosis. Some children are
distressed by their sex registered at birth, and make strong statements, wishing to live as their identified gender, at home and school.
Observational evidence indicates that this child-led social transition is associated with positive psychosocial outcomes. This is a family decision, which should be led by the child’s expressed needs.
No medical or surgical treatment is indicated for gender dysphoria before puberty commences. Prepubertal children only need love, support, and listening to. Some become comfortable with their birth-registered sex and gender during late childhood to early puberty, so it is important that children who socially transition are supported to ‘change back’ at any time they wish. Facilitate access
continued on Page 33
Transgender health care across the life span is a core area of clinical skills for all health professionals, writes child and adolescent psychiatrist Dr Julia Moore.
“We have had twelve fit-out contract companies at the St John Of God - Wexford Centre site, and without doubt Medifit Design & Construction stands head & shoulders above the rest for professionalism & quality, I have no problem recommending Medifit for any future works”.
Since 2002, Medifit has helped hundreds of healthcare providers create their dream practices. Our award winning design and construction service will deliver a practice that will enhance your working life and we do it with integrity and transparency from our Perth Head Office.
As Australia’s premier healthcare design and construction provider, we know what it takes to create a beautiful, productive working environment.


If you are considering space at Murdoch, contact Medifit today for a no obligation consultation.

continued from Page 31
to mental health care for common problems including social anxiety, depression, suicidality, autism and ADHD, alongside gender-affirming care.
Puberty suppression with gonadotropin releasing hormone agonists can be indicated when gender dysphoria is exacerbated with distress at the changes of early puberty. Puberty suppression is ideally commenced at Tanner stage 2–3, early enough to provide longterm benefit by preventing breast development or voice deepening and facial masculinisation.
Some young people first experience gender dysphoria peripubertally; puberty suppression may still be appropriate to relieve distress and allow time for clarification of identity. Puberty suppression can be ceased if the patient wishes: its effects are largely reversible. Most people who start puberty suppression remain stable in their gender identity and
decide to commence testosterone or oestrogen gender-affirming treatment in later adolescence or young adulthood.
Oestrogen/anti-androgen or testosterone treatment can be provided to more mature adolescents with long-term stable gender identity, who have developed capacity to give informed consent, including appreciation of the risk of regret. This requires repeated consultations, and specific counselling regarding fertility. Masculinising chest reconstruction is not yet provided in the public health system in WA. Genital surgery is not done under age 18 in Australia. Many trans people do not want genital surgery, but for some it is extremely important.
The treating medical practitioner must obtain the active informed consent of all legal guardians before providing gender-affirming puberty suppression, oestrogen, testosterone, or surgical treatment for a person under age 18,
These programs allow patients to address mental health issues with minimal wait time or disruption to their everyday lives.
Structured, therapeutic group sessions tailored to the specific needs of patients experiencing:
• Depression
• Anxiety
• Bi-polar disorder
• Personality disorder
• Trauma
• Eating disorders
• Substance dependency
ramsaymentalhealth.com.au
For more information visit: ramsaymentalhealth.com.au/hollywood
• Refer directly to Ramsay Clinic Hollywood, no psychiatrist referral necessary
• Cost covered under private health insurance (top cover in psychiatric)
For a GP information pack: please contact Wendy Henson HensonW@ramsayhealth.com.au
regardless of Gillick competence, according to the Family Court of Australia judgement Re: Imogen [2020]
The CAHS Gender Diversity Service is a multidisciplinary team that provides information, support, assessment, and (where requested and appropriate) gender-affirming medical treatment in liaison with the general practitioner.
There is a pressing need to develop more youth trans health care capacity in WA, while maintaining quality and safety of care. Models exist in other states for treatment in primary care with collaboration between GPs and psychologists, with other specialist consultation as appropriate. Peer support through TransFolk of WA, Transcend Australia and PFLAG is very helpful.
ED: Dr Julia Moore is a Consultant Child and Adolescent Psychiatrist with the CAHS Gender Diversity Service. References on request.
More privacy and less visibility at Perth Children’s Hospital have taken some getting used to by nurses, patients and their families, according to Associate Professor Fenella Gill

The design and functionality of workplaces are critical to ensuring employees can complete their jobs to their best ability. Hospitals play a key role in our health system, and it is vital that their design meets the needs of staff, patients and their families.
The Perth Children’s Hospital opened in May 2018 – a state-ofthe-art hospital providing worldclass medical care to WA children in need, and a home to their families who are supporting them.

Any shift into a new work environment can have its challenges, and our team aimed to identify any impacts of the new working environment on PCH stakeholders.
Our research, published in the Journal of Health Services Research & Policy, found that increased privacy for patients and families at the expense of decreased visibility has emerged as the dichotomy of design at PCH.
We were also able to show the design had many positive outcomes including privacy and natural light, but initially challenges reported by nurses working in ward areas were that they experienced feeling exhausted, isolated, and less visible to patients and their families.
At the time of planning this study, the influence of building design with single rooms on patient, family and nurse experience and workflow in a children’s hospital was unquantified, although anticipated challenges were that single patient rooms could increase nurse workload while simultaneously reducing nurse-time spent with patients.
We looked to address the knowledge gap by measuring the effects from a nursing, patient, and family point of view.
The design strategies evaluated
included the predominance of single patient rooms with ensuite bathrooms (from 26% at Princess Margaret Hospital to 75% at PCH) and a 65% larger floor space in ward areas.
To optimise nurse-time with patients, design features included V-shaped wards and decentralised nurses’ stations to increase visibility, as well as automated medication dispensing machines to promote efficient medication management and digital handsfree communication technology to facilitate communication between staff.
PCH architectural features maximised natural light, quietness, and views of nature.
Our research revealed both benefits and challenges. Patients and families liked the new environment, especially how families could all be together in the patient room, yet also recognised how the design resulted in reduced visibility of nurses and a sense of isolation.
After collecting data on the movements of registered nurses, we found they spent the same amount of time at patients’ bedsides, yet they spent double the amount of time walking in the new hospital from an estimated 10 minutes at PMH to about 20 minutes at PCH.
Time spent documenting significantly fell, as did time spent undertaking ward activities and indirect care activities, including supervision of others, while time communicating with other staff increased.
Nurses told us that the new environment resulted in them initially experiencing exhaustion; being less visible to families and other nurses; and decreased capacity to supervise less experienced nurses.
Over time they did adjust to their new working environment and their experiences improved. However,
the experience of increased walking persisted, and similarly, despite the hard data of no change to nurse time spent at patients’ bedsides, the perception and experiences of children, families and nurses were that nurses were less visible and spent less time with patients. Through surveys we collected, nurses reported a decrease in their perceptions of staffing and resource adequacy and in focus groups nurses told us they felt as if there was an insufficient number of nurses.
We identified four key themes that provided further explanation for the perceived decrease in nurse staffing and resource adequacy. These were:
• adapting to ward design and managing workflow in the different environment
• nurse experience of reduced visibility interlinked with how nurses viewed their capacity to take responsibility for patients and provide care, and;
• technology communication.
Reduced visibility of patients has been previously linked to nurses perceiving there are inadequate
resources and experiencing a lack of control over their practice.
The nursing gaze framework describes the process by which nurses assess patient needs against a background of what they consider to be normal in the context of the patient’s condition and the work environment. This gaze guides the setting of work priorities and supporting others.
The challenge of supervising other nurses in single room environments has also been previously reported and includes concern over loss of surveillance of patients.

Despite these initial concerns, a year after moving to PCH, many nurses preferred single rooms, saying they thought that patients and families were happier, noting that “It takes a little bit of work, but you do adjust to the actual working environment … we support each other a little bit more.”
Once they became familiar with using the technology, nurses especially valued the digital handsfree communication technology for working with reduced visibility.
Individual survey item responses
confirmed families’ preferences for the space, privacy, and quiet of single rooms but families also observed at PCH that nurses appeared to be working in a more pressured environment and were less visible to them.
“… you look and there’s often not anyone visible,” one parent commented. “But for some reason that never seemed to happen at the old hospital, the people always seemed to be on the ward.” Yet overall, the experience of care reported by families increased after the move while children’s experiences were unchanged.
The complexities we have identified can be used to assist new hospital design planners to consider potential impacts on nurse, patient and family experience as well as nurse workflow.
ED: The author acknowledges the help of research participants and Channel 7 Telethon Trust for funding the study. A/Prof Fenella Gill holds roles with Curtin University and Perth Children’s Hospital.
Healthy West Australians are being recruited into a clinical trial in a bid to combat rheumatic heart disease in some of the community’s most vulnerable children.
Researchers are seeking volunteers willing to be infected with a bacterium that causes the common sore throat, in the WA-first human challenge study trying to prevent strep throat by using penicillin. While penicillin is already the gold standard treatment for strep throat, the trial will evaluate the dosage required for preventing infections to help develop better forms of the drug.
Telethon Kids Institute and Linear Clinical Research are joining forces with the University of WA and Curtin University for the clinical trial, as a part of the END Rheumatic Heart Disease program, which aims to eradicate RHD in Australia.
TKI Executive Director Professor Jonathan Carapetis said Australia had some of the world’s highest rates of the disease – occurring almost exclusively in Aboriginal and Torres Strait Islander
communities – and it could result in heart failure, disability and premature death.
“This clinical trial is tackling one of the really big health problems of the world today,” Professor Carapetis said.

“About 300,000 people die of RHD every year and more than 40 million people around the world have the disease – and it all begins with a sore throat.
“In a country like Australia, RHD shouldn’t exist yet it does, taking lives and causing disability in some of our most vulnerable. This trial is a really critical step in global health control.”
Linear CEO Jayden Rogers said the trial’s aim was to find out more about the exact dose of penicillin which would protect someone from becoming infected with strep A.
“In this unique study, volunteers will be administered specific, lower-level doses of penicillin before being carefully exposed to a fixed dose of strep A to see if they develop a sore throat in a human challenge study,” Mr Rogers said.
“If people develop symptoms, a standard
treatment course is initiated to effectively treat this condition. The study will then help demonstrate potential dose levels that are protective from strep throat.”
TKI researcher and infectious diseases physician Dr Thel Hla said more than 5000 Aboriginal and Torres Strait Islander people, many being children, are living with RHD.
“Strep A is a type of bacteria that causes sore throats and occasionally skin infections but where there are repeated cases of infection and they are left untreated by antibiotics, the infection can progress to acute rheumatic fever which is associated with damage to kidneys, heart and neurological systems,” she said.
“As a result, heart valves can be damaged, ultimately leading to rheumatic heart disease, particularly in children. By the time they are a young adult or in their 30s or 40s, they can develop intractable heart disease and heart failure which leads to entirely preventable premature death.”
ED: The trial is taking place at the Linear Joondalup Early Phase Centre. Details at https://trials.linear.org.au/trial/sorethroat-challenge-study/
WA researchers are making headway in the battle to eradicate strep A infections and put a halt to rheumatic heart disease.
There are benefits and challenges in an interdisciplinary approach to research, argues Edith Cowan University researcher
Driven by scientific advances and social demands, interdisciplinary research has grown into an important trend in academia. For example, collaborations are growing between the natural and social sciences. Convergence research, which aims to tackle complex issues using interdisciplinary approaches, represents an emerging paradigm.
The merging of the International Council for Science and the International Social Science Council in 2018 to form the International Science Council highlighted the integration of these disciplines.
The blending of tourism and medical science may at first seem an unusual pairing. In truth, however, these fields are related: the mobile nature of travel can spread infectious diseases and aggravate public health crises like the COVID-19 pandemic. These circumstances can in turn threaten the tourism and hospitality industry. At the same time, tourism can help address public health issues such as noncommunicable diseases and healthy ageing by improving people’s quality of life.
Travel medicine, an interdisciplinary branch of medicine, specialises in travellers’ health and safety, which has an initial focus on infectious diseases, but now is enriched with more components such as noncommunicable chronic diseases.
Non-pharmacological interventions can lead to travel experiences that promote health, prevent disease, and relieve illness. These treatment options can also encourage physical movement, social interaction, healthy eating, and positive emotions.
Travel therapy is suitable for multiple groups, including healthy people, those in suboptimal health, and those with conditions such as
intellectual disabilities. Research bridging tourism and the medical sciences can benefit numerous stakeholders – especially given concerns about health, hygiene and safety raised by COVID-19.
For academics, such collaboration provides fresh perspectives to produce a deeper understanding of tourism’s role in public health, while for the general public, particularly vulnerable populations, interdisciplinary studies can prioritise equality in health and tourism by outlining health-related benefits and problems in travel.
These efforts can help health care and tourism practitioners develop targeted products and services as well. Socially, interdisciplinary research may partly mitigate public health challenges to foster sustainable development.
Despite these advantages, studies linking tourism and medical science face barriers. Medical researchers have paid little attention to tourism.

Travel medicine pertains to health and safety during trips. However, it generally revolves around disease to the neglect of possible relationships between tourists’ behaviour and health.
Even less emphasis has been placed on the health benefits of tourism. Several studies have considered the underexplored tourist groups, namely those with health conditions such as dementia, depression, and intellectual disabilities.

But few have demonstrated a solid understanding of medical science. Research findings could be misleading in the absence of clear disease definitions and diagnoses, sample inclusion and exclusion criteria, and ethical considerations. High-quality research blending tourism and medical science is needed to deliver insightful results.
Yet disciplinary obstacles persist. Firstly, health issues are often thought to fall under the purview
continued on Page 39
The Westin, East Perth
Saturday 10th June 2023
Please book a place for the conference at gpurologymasterclass.com.au
RACGP CPD Hours - Approval Pending
Grants available for rural GPs to attend
You may be eligible for funding through the Health Workforce Scholarship Program (HWSP) to attend the GP Urology Masterclass.
To apply for HWSP funding, you must meet the eligibility requirements: ruralhealthwest.com.au/ programs/health-workforce-scholarship-program
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Akhil Hamid
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options.

For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic
Hollywood Clinic | Wexford Clinic
Feel at ease. Expert urological care and surgical management.
Advances in deep brain stimulation are offering a potential step forward for WA patients with Parkinson’s disease, essential tremor and dystonia.
Hollywood Private Hospital neurologist Dr Julian Rodrigues and neurosurgeon A/Prof Steve Lewis are adopting the latest technological innovations such as intraoperative CT, remote brain stimulator programming and directional DBS, now with sensing capability.

DBS requires surgery to implant a neurostimulator that sends electrical signals to areas of the brain responsible for movement.
Hollywood is the only site in WA using remote programming of DBS, which allows Dr Rodrigues to assess patients over live video and adjust their implanted DBS device for better symptom control allowing for treatment for patients living thousands of kilometres away.
In 2017, Hollywood was the first WA hospital to implant a directional DBS lead system which stimulates minute areas of the brain more precisely. The benefits of directional DBS include reduction in side effects from overstimulation
and better symptom control. Directional DBS electrodes capable of recording brain activity were surgically implanted into a patient at Hollywood in June last year in another first for WA.
“It essentially downloads brain signals,” Dr Rodrigues said. “By interpreting these signals, I am hopeful we can predict more specifically where to stimulate, reducing the trial and error aspect.
“The data collecting capabilities of DBS recordings have exciting prospects in terms of analysing abnormal brain rhythms and developing automated treatment algorithms using artificial intelligence.”
continued from Page 37
of medical science whereas tourism belongs to the social sciences. Secondly, academic culture itself can hinder interdisciplinary work: fields feature their own theories, methodologies, concepts, and values, making collaboration complicated.
Scholars need to reach a consensus about interdisciplinary research from several standpoints, spanning research questions, designs, instruments, sample selection, and data analysis. Additionally, medical science stresses objective clinical evidence; tourism, as a soft science, involves subjective judgment.
These differences and associated disciplinary bias can impede interdisciplinary communication. Although such bias is rarely publicly acknowledged, inequitable power relations exist between disciplines and can affect the resolution of collaboration-based disputes.
Thirdly, due to the range of involved research areas, interdisciplinary projects face difficulties in peer review and publication. Traditional single-disciplinary review criteria make it hard to fairly assess these projects’ methods, data, and results.
All that said, the benefits of quality interdisciplinary studies blending tourism and medical science
outweigh the challenges. Highimpact discoveries, such as the potential clinical efficacy of tourism in treating disease, often occur at the intersection of fields. Experts from these two seemingly unrelated disciplines should be called upon to jointly explore solutions to public health problems and promote sustainable societal development.
ED: Fangli Hu is a PhD candidate in the School of Medical and Health Sciences at ECU. Dr Jun Wen (School of Business and Law) and Professor Wei Wang (Centre for Precision Health) at ECU contributed to this article.
Dermatologist-led cosmetic medicine service
Doctor-delivered treatments, for GP-referred patients
EXPERT LASER, INJECTABLES & HAIR LOSS SERVICES:
Laser modalities for Rosacea

Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.

There is an old adage that the more things change the more they stay the same. The bleating (for want of a better word) about Medicare reform reminds me of a quote from then treasurer Paul Keating in 1989.
‘I guarantee if you walk into any pet shop in Australia, what the resident galah will be talking about is microeconomic policy’. Substitute Medicare for microeconomic reform and 34 years later here we are.
Also from the 1980s was the TV series, Yes Minister. Those who haven’t watched the episode about the hospital with no patients should do so. In another episode, Sir Humphrey explains to the Minister that when calling for a report one must first already know the outcome and that the best way to deal with the hardest part is in the title. Thus “Strengthening Medicare’ is the title. Sounds great but what does it actually mean?
Prime Minister Anthony Albanese said health reform was a ‘first priority issue’ for National Cabinet, and that better integration will be a major focus of the planned changes. ‘The key, going forward, is to better integrate the systems,’ he said. In recognition of this importance, a decision was made to consider the matter again in April.
As usual, there is no distinction between “free at point of service” and unaffordable. Why is it assumed that nobody could afford any out of pocket expense. The “average person” sees a GP six times a year. A $30 gap works out to 50c per day.
This month we have articles on aspects of pain management as well as surgical topics. Pain and mental health issues often go together. On a positive note, the decision by the TGA to enable use of MDMA in PTSD and psylocibin in treatment-resistant depression recognises that current treatments do not work for all people and that we need innovation.
Meanwhile, some 14% of medical graduates are now wanting to enter general practice. Speaking from personal experience, it remains enjoyable. However, low remuneration, increasing bureaucratic requirements and regulators which seem to take a shoot first and ask questions later approach does make it less attractive than when I started out.
For those who follow the stars, Pluto enters Aquarius in March and will remain there for over 20 years. The last time this occurred was in the late 18th century coinciding with the French Revolution and American War of Independence. Massive change indeed. Who knows what may happen this time?
As usual, there is no distinction between “free at point of service” and unaffordable. Why is it assumed that nobody could afford any out of pocket expense. The “average person” sees a GP six times a year. A $30 gap works out to 50c per day.
Our surgical capabilities:
• Ophthalmology

• Minor plastic and reconstructive surgery
• Minor gynaecological procedures
• Minor general surgery
• Dental
• IVF
Key benefits for your patients:
• Parking on site
Under new management by Adora Day Surgeries
• Professional and eff icient staff overseeing streamlined admission and recovery processes
• Highly experienced Theatre and Recovery nursing team each with 10+ years’ experience in their field of speciality
• Boutique Day Surgery experience – two theatres supported by 4 x Stage One recovery bay and 6 x Stage Two recovery chairs


 By Dr Ruben Rajan, Colorectal Surgeon, Subiaco
By Dr Ruben Rajan, Colorectal Surgeon, Subiaco

The advent of robotic surgery is certainly not a new one. With its origins in trauma surgery, being initially developed for deployment in the battlefield and surgeons operating remotely, it was eventually developed for civilian use.
Robotic surgery essentially works as a master-slave manipulator. The operating surgeon works from a console unscrubbed while robotic arms perform his or her movements. Limited artificial intelligence eliminates tremor and fulcrum forces of the endoscopic instruments against the body wall. Articulated robotic arms allow the surgeon to perform fine tasks in limited spaces.
The uptake of robotic surgery in the general surgical space has been met with varying enthusiasm. The presence of advanced skills among the general surgeons means that most tasks achievable with robotic surgery can be achieved, albeit with much difficulty.
While laparoscopic surgery has very much overtaken open surgery in most general surgical fields, the prohibitive cost of robotic surgery has meant that robotic surgery has not followed suit. With several platforms now available in the market, we can expect the transition to be exponential.
The availability of this tool has now meant that surgeons are able to push the limits of minimally invasive surgery and strive for what was previously deemed impossible.
Let’s start with optics. The current generation of robotic endoscopes boast high definition, three dimensional views allowing surgeons to see planes and levels of detail not previously appreciable. The ability of the operating surgeon to be in full control of the operating
Robotic surgery is not actually new, having been developed for military use
Take up in civilian surgery has been slow for a variety of reasons Its advantages, coupled with possible AI will see increasing prevalence in coming years.
camera greatly improves vision and ease of operating.
Some robotic platforms allow for near infra-red vision. This allows surgeons to easily identify ureters, bile ducts, vascularity of tissues with the assistance of indocyanine green.
The combination of better optics and articulating instruments means operating in tight spaces and around corners can be achieved with relative ease. As a colorectal surgeon, this is relevant to me operating in a male, android pelvis, particularly with increasing rates of obesity in our population.
The intuitiveness of the robotic controls allows for unparalleled dexterity, and this becomes immediately apparent when dissecting along vessels for lymphadenectomies during bowel resections.
The ability to control bleeding vessels and the presence of a third operating arm gives the operating surgeon the confidence to perform radical oncological surgery with the ability to mitigate its risks. This
has also allowed us to venture into intracorporeal bowel anastomoses, which can even be handsewn and transanal resection of large polyps. The combination of these factors results in surgery which is less of a physiological insult to the patient and affects post-operative outcomes. Reduced length of stay, length of incisions, post operative pain and the ability to complete procedures in a minimally invasive fashion are just a few advantages these confer. Added to this is the reduced physical toll and increased ergonomics for the operating surgeon.
I see a steep uptake in robotic surgery in the coming years, particularly with the release of multiple new platforms which have now made it a competitive market. This will make robotic surgery more accessible and allow earlier access to surgical trainees.
We may even see an increased presence of artificial intelligence in these platforms, always a polarising topic. We are already seeing an increased use of robotic surgery in colorectal, upper gastrointestinal, hepatobiliary and gynaecological operations. This has also recently been expanded to hernia surgery and emergency general surgery.
The future is bright with robotic surgery, so watch this space.
Author competing interests – nil

Painful diabetic neuropathy is a debilitating chronic condition characterised by burning, tingling or numbness in the feet and/or hands, and can cause extreme discomfort and difficulty in daily activities.
Current first-line therapy includes improving glycaemic control (lifestyle and/or medication).
First-line analgesic options include anti-neuropathic analgesic, tricyclic antidepressants (TCAs), serotoninnoradrenaline reuptake inhibitors (SNRIs) and anticonvulsants.
Although opioids have been used, they are no longer recommended as routine. Atypical opioids (e.g. tramadol, tapentadol,) can be useful in appropriately selected patients.
Other second-line options include topical therapies (e.g. capsaicin cream and lidocaine patches), several natural complex anti-inflammatory/anti-oxidant medications (nutraceuticals) including palmitoylethanolamide (PEA), alpha-lipoic acid (ALA) and benfotiamine (fat soluble Vit B1 prodrug). Despite increasing clinical use, the evidence for cannabinoid analgesics remains limited.
Painful diabetic neuropathy negatively impacts quality of life
Current pharmacological options have limited effect in a significant number of patients
New procedural interventions offer options for significant improvement in pain and quality of life.
Notwithstanding numerous pharmacologic options, a significant number of patients either fail to experience clinically meaningful improvement in pain and quality of life or discontinue treatment due to significant adverse effects. For these patients there are nonpharmacologic procedural options which may improve both pain and nerve function.
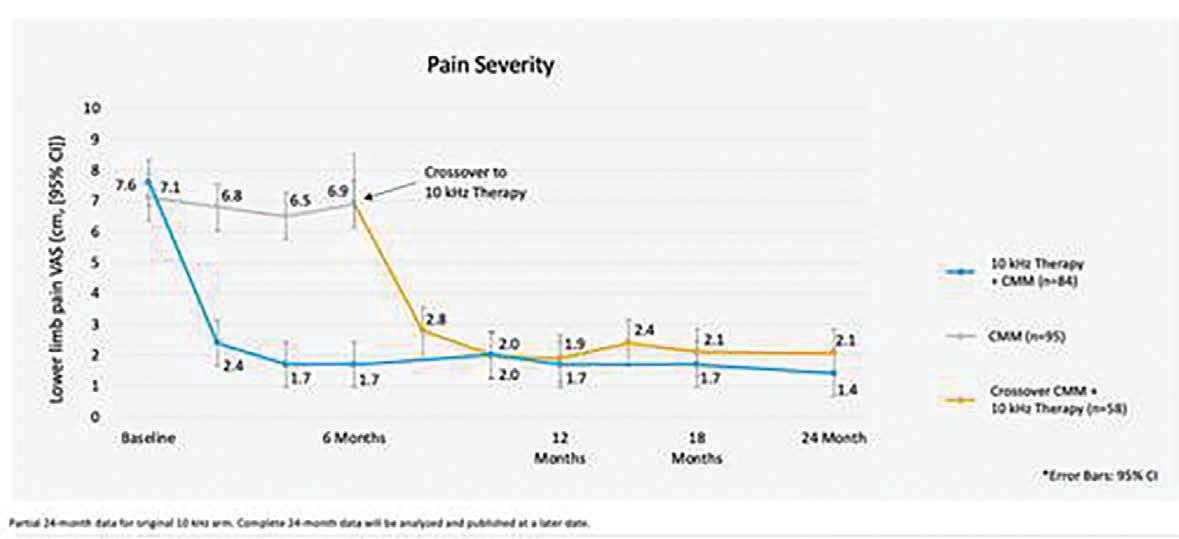
This is a regeneration medicine technique that aims to utilise the growth factors concentrated in platelets to promote proliferation and differentiation of tissue cells, as well as regulate the inflammatory response to accelerate tissue regeneration.
Used for decades in the treatment of musculoskeletal injuries and large joint arthritis, researchers are exploring the potential use of PRP in painful diabetic neuropathy. The theory is that the platelets and growth factors released by PRP can help to reduce inflammation and promote the regeneration of damaged nerves.
Venous blood is collected and centrifuged to remove red (+/white) blood cells and concentrate platelets to 4-5 times. Injecting platelet rich plasma into tissue releases several growth factors in high concentration including PDGF, TGF- ß, VEGF, EGF and IGF-1.
Preclinical evidence has shown PRP-derived growth factors promote differentiation and proliferation of Schwann cells, switching of macrophages from the pro-inflammatory M1 to antiinflammatory M2 phenotypes as well as promoting angiogenesis, improving neuronal survival and reducing susceptibility to ischaemia.
A recent trial randomised 60 patients with painful diabetic peripheral neuropathy confirmed to ultrasound guided injections of platelet rich plasma plus medical
management (glycaemic control, B vitamins, alpha-lipoic acid, SNRIs and pregabalin) or medical management alone.
The platelet rich plasma group showed significant in VAS pain (median 7 to 1) and VAS numbness (median 6.5 to 1) at six months. Medical management alone showed no significant change (6 to 7 and 6 to 7 respectively). Follow-up nerve conduction studies showed significant improvement in motor and sensory nerve conduction velocity.
Although in its infancy, the use of platelet rich plasma offers a lowrisk therapeutic option.
SCS is a neuromodulation technique in which stimulating electrodes are surgically implanted in the epidural space, allowing stimulation of the dorsal column. Preclinical science and use has evolved with several different subparaesthetic stimulation modes that have shown increased efficacy over traditional tonic stimulation. Two randomised controlled studies in painful diabetic neuropathy
have revealed reductions in VAS pain of 42mm at six months, with 60% achieving greater that 50% reduction in VAS. It additionally showed significant improvements in quality of life measures and patient satisfaction.
More recently, a larger randomised controlled trial has studied high frequency (10kHz) subparaesthetic stimulation in comparison to best medical management. These 216 patients with painful diabetic neuropathy were randomised to conventional medical management (CMM) or CMM + 10kHz SCS, with the option of control patients to cross over at six months.
Of the 113 patients randomised to CMM + SCS, 104 underwent a two-week trial of which 90 (86.5%) proceeded to full implantation. At six months, SCS patients showed an average 76.3% reduction in VAS (7.6 to 1.7), with 85% showing >50% reduction in VAS.
The CMM group showed no significant change in VAS (7.0 to 6.9). The SCS group additionally showed significant improvements in quality of life, patient satisfaction, sleep and subjective measures
of neurological function and 62% showed improvements in neurological examination findings (mostly sensory function) as opposed to 6% of the CMM group. At six months, 93% of eligible CM group patients elected to crossover. Follow up has shown similar improvements in pain, sleep, quality of life and neurologic function to the original SCS group.
Ongoing follow up at 12, 18 and 24 (awaiting publication) months shows ongoing efficacy, both in VAS reductions and improvements in sensory function. At 24 months, patients report average of 77% reduction in VAS, with 84% reporting >50% reduction and 61% reporting >80% reduction in comparison to baseline levels.
Safety data showed no stimulation related neurological defects. A small number had infections which resolved with antibiotics.
References available on request
– Author competing interests – the author was provided with unpublished data by Nevro

Australia’s International Women’s Day theme for 2023 is ‘Cracking the Code: Innovations for a gender equal future’.

BreastScreen WA supports innovation and new technologies to improve access and equity in healthcare. BreastScreen WA:
• Has 12 fully digital fixed site clinics in Perth, Bunbury and Albany providing free screening mammograms.
• Deploys a fleet of mobile digital screening units that visit over 100 towns every 2 years across WA.
• Uses rigorous data security measures to ensure the personal information provided by clients is protected.
• Provides daily updates on when appointments are available at screening clinics.
• Delivers a culturally appropriate service, with resources in 32 languages.

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Thyroid nodules commonly present as a neck swelling or as an incidentally detected imaging lesion. While the majority are benign, the risk of malignancy in an adult ranges from 7% to 15%.
A history of childhood head and neck irradiation significantly increases the likelihood of a thyroid nodule being malignant. While the majority of thyroid malignancies are sporadic, a number of familial conditions can predispose to thyroid malignancies. Larger nodules can cause compressive symptoms including dyspnoea, globus and dysphagia. Any symptom suggestive of invasion, including dysphonia or dysphagia, should raise suspicion for an underlying malignancy.
Clinical examination should involve inspection and palpation of the thyroid gland and examination of the cervical lymph nodes.
The presence of a firm, fixed nodule or ipsilateral cervical lymphadenopathy are late features suggestive of malignancy.
The key tests in differentiating a benign from a malignant nodule involve thyroid ultrasound and fine needle aspiration cytology (FNA).
Ultrasound and TSH
Ultrasound is the best imaging modality for thyroid nodules. All patients in whom a nodule has been incidentally detected on another imaging modality should
Thyroid nodules are increasingly encountered due to the widespread use of imaging
Serum TSH, ultrasonography and FNA remain the key initial investigations whilst radionuclide scans are reserved for patients with low TSH
The majority of nodules are benign and may require follow up based on sonographic features. Refer malignant nodules to a high-volume thyroid surgeon.
be referred for an ultrasound of the neck and thyroid.
Numerous ultrasound-based risk stratification systems are in use. The 2015 American Thyroid Association guidelines for thyroid nodules categorised nodules based on the sonographic pattern that provides an estimate of the malignancy risk. Key descriptors that increase the malignancy risk include hypoechogeneity, microcalcification, regular margins and suspicious lymphadenopathy. Notably, the guidelines discourage FNA for thyroid nodules less than 1cm in size. Papillary thyroid carcinoma (the most common type of thyroid carcinoma), less than 1cm in size, is defined as a microcarcinoma.
Many studies have demonstrated that, in the great majority of patients, papillary thyroid microcarcinoma is an indolent disease. Furthermore, inconclusive cytology reports, resulting in patient anxiety and unnecessary interventions, are not infrequent. Therefore, it is considered that at the population level, the morbidity and cost are not in favour of diagnosing thyroid nodules that are <1cm in size.
A thyroid-stimulating hormone (TSH) serum level should be obtained in all patients. While most patients will be euthyroid, a suppressed TSH level might indicate a toxic nodule.
Ultrasound-guided fine needle aspiration should occur for thyroid nodules that satisfy the criteria for biopsy. The table outlines the cytology reporting categories and corresponding risk of malignancy.
The good comprise: Asymptomatic and euthyroid, ultrasonographically benign/ indeterminate, under 3cm nodule, and benign cytology. These patients can be reassured and do not require further investigation or surveillance. Thyroidectomy would be appropriate if there is future development of clinical enlargement or symptoms.
continued from Page 47
The bad comprise: Symptomatic or hyperthyroid, ultra-sonographically suspicious/malignant or >3cm and indeterminate/ follicular cytology. These patients require referral to an endocrinologist or an endocrine/ thyroid surgeon.
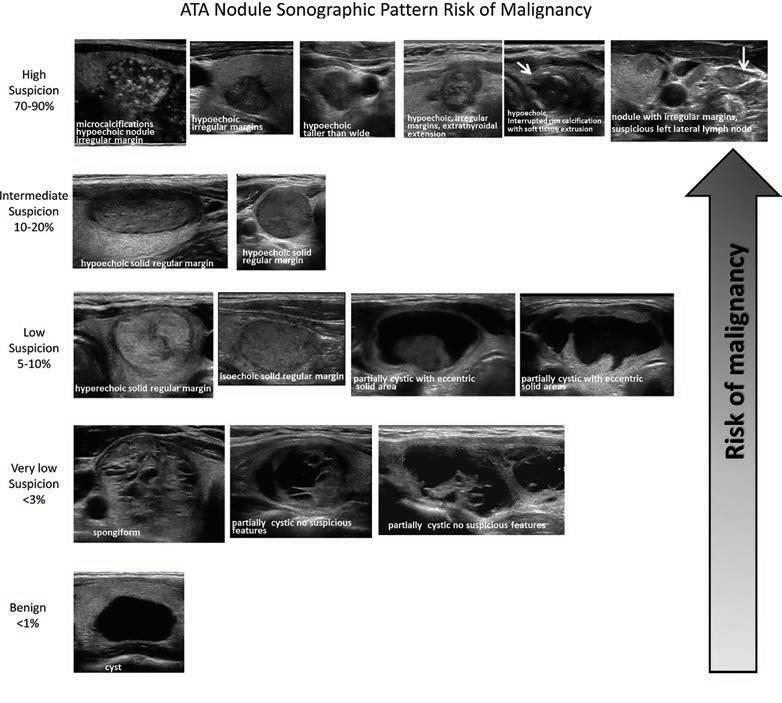
The ugly comprise: Ultrasonographically malignant/ lymphadenopathy and suspicious/ malignant cytology. These patients require referral to an endocrine/ thyroid surgeon. With the exception of benign cytology, all other results should be referred to an endocrinologist or thyroid surgeon for further assessment. A significant proportion of thyroid nodules do not meet FNA criteria, and ultrasound features guide follow-up.
Author competing interests - nil
Our cardiology centres have recently changed their name from GenesisCare Cardiology to Advara HeartCare, following a change of ownership in late 2022.
While things may start to look and sound a little different, our number one priority is continuity of care for your patients.

Our cardiologists, teams and locations remain the same, and this will have no impact on patient care.
For more information: advaraheartcare.com/newname-hcp
Groin hernia are common. Patients will often describe symptoms of swelling and discomfort in the groin, made worse by exercise, straining or coughing, all activities that increase intra-abdominal pressure. There is usually relief on relaxing and lying down and on external pressure to reduce the hernia.
Severe constant pain can develop if the hernia becomes irreducible (incarcerated) or the blood supply of the contents compromised (strangulated).
A thorough clinical examination of the groin and hip joint remain the gold standard in the diagnosis of hernia. An abbreviated differential diagnosis of groin swellings includes lymph nodes, hydrocele, cord or round ligament varix, undescended testis, scrotal pathology, psoas bursa or hip join effusion.
In patients where clinical doubt exists, in suspected recurrent hernias or in obese patients, an ultrasound scan is a highly sensitive and effective way to diagnose hernias.
Patients with groin pain but no obvious swelling or lump present a diagnostic and management dilemma.
Ultrasound scan is very sensitive and potentially overly sensitive, picking up pre-peritoneal fat sliding into the cord. This finding, although labelled as an inguinal hernia is unlikely to be the cause of the patient’s pain. A careful examination is even more prudent to help target further investigations.
Any scars indicating prior surgery should be followed up, as postoperative chronic pain and recurrent hernia should be considered. CT while straining (Valsalva CT) can be very helpful in investigating occult recurrences and other possible post-operative complications. Investigate the scrotum for evidence of orchitis, epididymitis, varices or even neoplasms that can all cause pain. A dedicated scrotal ultrasound may be useful here.
Groin hernias are common
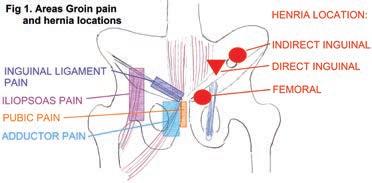
Accurate diagnosis involves history, examination and in select cases imaging Management, depending on hernia and patient factors, ranges from watchful waiting to laparoscopic or open surgery.
Musculoskeletal causes of pain represent another possibility. The history can mimic hernia with pain on exertion, improving with rest.
Examination can reveal focal tenderness on palpation in the adductor, pubic, inguinal or iliopsoas regions. Resistant testing can be performed for the adductor muscles and hip range of motion to assist with diagnosing hip pathology. These tests can lead to further targeted investigation of the cause of pain.
For hip pain, a plain XR may be a useful start. Following this MRI is the imaging of choice. MRI can diagnose adductor tendonitis, pubic osteitis, hip arthrosis, bursitis iliopectinea, among other musculoskeletal conditions that cause groin pain.
This depends on hernia and patient factors. Femoral hernia should be surgically repaired due to the high risks of strangulation caused but the relatively fixed and inflexible boundaries of the femoral ring. Inguinal hernia, if the patient is symptomatic should also be repaired surgically. Asymptomatic inguinal hernia requires a discussion with the patient. Multiple studies
show that watchful waiting is a safe approach to asymptomatic inguinal hernia in men. However, over time about two thirds developed pain and required operative treatment.
The use of hernia belts or truss systems is limited to highly comorbid patients unable to have operative repair. While such systems do exist and can provide some symptom relief, they are often difficult to correctly place, and inappropriate use may cause skin irritation or pressure injury.
No article written by a surgeon would be complete without at least a short paragraph on the actual surgery!
Groin hernia can be repaired with a number of different techniques, which can be undertaken by open incision or laparoscopically by either Total Extra-Peritoneal or Trans Abdominal Pre-Peritoneal approach. Each technique contains advantages and disadvantages beyond the scope of this article. It is important for the surgeon to consider the relevant patient and hernia factors and provide a personalised hernia treatment plan. Regardless of technique used, the use of a lightweight large pore synthetic mesh is recommended by multiple studies and guidelines as it reduces recurrence rate while not increasing complications such as pain, haematoma or seroma.
Most groin hernia in healthy patients can be safely performed as a day case. Only complex and recurrent hernia or frailer patients will usually require an overnight stay. Postoperatively patients are encouraged to mobilise and conduct normal activities. Return to straining and physical labour is personalised but the latest European Hernia Society guidelines suggest a return to full duties in as little as two weeks.
– References available on request
Author competing interests – nil


Chronic or persistent lower back pain is defined as the experience of lower back pain for over three months. Chronic pain can affect an individual’s ability to engage in activities of daily living, meaningful and recreational activities, work, and interpersonal relationships, impacting overall quality of life.
The burden on the health-care system for those suffering with chronic low back pain (CLBPx) is experienced worldwide and is a leading cause of disability. Despite extensive research, the high prevalence of CLBPx suggests the quality of health care accessed and received for these individuals remains suboptimal.
Studies have explored numerous treatment modalities to identify the optimal course of treatment for CLBPx. However, no consensus on treatment has been achieved. Pain education, exercise, manual therapy and Cognitive Behavioural Therapy (CBT) have all been investigated with varying degrees of success.
The 2021 Cochrane review for persistent lower back pain found with moderate-certainty evidence that exercise treatment is more effective for treating chronic low back pain compared with no treatment, usual care, or placebo comparisons for pain outcomes. The systematic review also identified that exercise improved pain (low-certainty evidence) and functional limitation outcomes (moderate-certainty evidence), compared to other conservative treatments. However, these effects were not clinically significant when considering all subgroup analyses together.
Other studies have found exercise therapy to have a more positive effect on pain and function for those suffering with persistent low back pain. One study identified different characteristics of individuals who benefited most from exercise therapy – specifically, those who were not reliant on pain medications, and those who did not

An individualised holistic biopsychosocial approach needs to be adopted to ensure maximal engagement in rehabilitation programs
No exercise modality is superior to another in managing chronic low back pain. Ensuring an individual enjoys their exercise is an important precipitating factor Implementing pacing and developing flare up plans may assist individuals with engaging in exercise therapy and meaningful activities thus improving overall quality of life.
have heavy physical demands of work.
Many questions remain regarding the optimal exercise dosage, modality, safety and efficacy of prescription. An individualised holistic biopsychosocial approach needs to be adopted to ensure maximal engagement in rehabilitation programs.
Once red flags have been ruled out with an individual’s presentation, engagement in a structured supervised rehabilitation program is deemed as safe, though perceptions around importance and confidence to exercise need to be understood. In many instances, a person’s fear avoidance beliefs or catastrophising behaviours towards exercise engagement need to be addressed and explored to overcome these potential barriers to participation.
At present there is no specific exercise modality that is superior to another for management of CLBPx. Ensuring a client engages with exercise they enjoy is likely to have a further positive effect on their psychological wellbeing and overall participation levels.
It is essential that an individual feels well supported with their rehabilitation and that they are progressed towards independent self-management to improve their overall pain self-efficacy and
continued on Page 52

Back problems affect one in six Australians, with pain being the main symptom. Between 70 and 90% of people will experience back pain at some stage in their lives. Chronic back pain is defined as pain that continues for 12 weeks or longer, even after an initial injury or underlying cause of acute back pain has been treated. Approximately 20% of people with acute back pain develop persistent and disabling symptoms.
Treatment of back pain involves a multimodal, biopsychosocial approach with many treatment options available. Treatment modalities involve patient education, manual therapies (massage, physiotherapy, spinal manipulation), exercise therapy, weight loss, analgesia, psychological therapies, interventional pain therapies and surgery.
Radiofrequency ablation (RFA) is an interventional pain therapy that is becoming increasingly used to manage chronic back pain, especially when conservative measures have failed. RFA is also known as a neurotomy, rhizotomy,
Key messages
RFA is a minimally invasive day procedure that can be used for managing different types of back pain.
Different types of RFA exist with the most common being pulsed, thermal and cooled. RFA should be used as part of a multimodal approach.
lesioning or denervation. Shealy first described the use of percutaneous RFA to treat spinal facet pain in 1975. There have been advances made in the safety and technology of RFA since then, but the technology is mostly unchanged.
RFA is often performed as a day procedure in theatre with a sedated patient. Under sterile, aseptic conditions, a RF needle is directed under X-ray guidance to the target nerve. Sensory or motor stimulation can be performed to further confirm correct needle placement. The nerve can then be pulsed (pulsed RFA), heated (thermal RFA), or watercooled (cooled RFA) to reduce
nociceptive transmission. Generally, this takes about 30 minutes to complete.
Pulsed RFA is performed in short pulses to reduce the target temperature, which allows for cooling of tissues. The temperature of the needle tip typically does not exceed 42C as the threshold for damaging neural tissues occurs at 45C. Therefore, the risk of damaging neural structures is greatly reduced with pulsed RFA.
It is theorised that the mechanism of action is by neuromodulation from the radiofrequency electrostatic field. Studies imply that pulsed RFA alters gene expression, cytokine regulation and neuronal membrane function that favourably alters pain signal transmission. The advantage of pulsed RFA compared with thermal RFA is less tissue destruction, less pain, less risk of deafferentation pain and less neuroma formation.
Thermal RFA utilises heat to reduce nociceptive transmission by thermocoagulation and destruction of neural tissue. A wide range of temperatures ranging from 70-90°C
continued from Page 51
develop an intrinsic/internal locus of control.
Establishment of flare-up plans in the early stages of a program can manage an individual’s expectations – teaching them that pain flare-ups are normal and may occur at some stage during recovery. This puts them in the driver’s seat for when one does eventuate.
Utilisation of an individual flareup management plan can help individuals be prepared for fluctuations of their pain symptoms, thereby viewing a flare-up as a
‘speed bump’ in their recovery rather than a setback.
Additionally, a key concept that should be discussed alongside exercise prescription is the term ‘pacing’. Some individuals may present as endurance copers or avoidance copers.
Endurance copers tend to adopt the ‘boom-bust cycle’ or try to ‘beat the pain’ during exercise and participation in daily life activity, while avoidance copers tend to avoid activity due to fear that exercise engagement may lead to exacerbations of their symptoms and pain.
Educating individuals around establishment of safe baselines for activity/exercise participation is an excellent starting point. Taking a ‘time focused’ approach rather than a ‘pain focused’ approach allows engagement in an activity for a certain amount of time – with the activity then being ceased before pain increases above tolerable limits. Breaking up specific daily activities into smaller blocks throughout the day is a form of pacing and may work as a strategy for symptom management.
– References available on request
Author competing interests - nil
are used. Thermal RFA produces heat by current flow, rather than heat through transfer from the tip of the needle.
Similar to pulsed RFA, an electrostatic field is thought to result in neuromodulation to further reduce pain transmission. Thermal RFA usually provides a longer duration of pain relief compared to pulsed RFA. However, the risks are injury to motor nerves with improper needle placement, increased post-procedural pain and risk of deafferentation pain.
Cooled RFA has a history of use in cardiac electrophysiology and tumour ablation, with its application in pain medicine being more recent. It uses a multichannel electrode
that is cooled by the continuous flow of sterile water preventing the electrode from reaching a high tissue temperature, allowing more energy to be delivered to surrounding tissues. A larger spherical lesion is created to provide more extensive denervation and reduces the chance of missing the target nerve.
RFA can be applied in the management of pain along the cervical, thoracic, lumbar, sacral, coccygeal levels of the spine for:
• Facet joint pain by targeting the medial branch
• Radicular pain by targeting the dorsal root ganglion
• Discogenic pain
• Sacroiliac joint pain by targeting the lateral branches
• Coccyx pain by targeting the ganglion impar.
It is important to note that although the lesions created by RFA are relatively small, they do not destroy nociceptive fibres only. Accurate RF needle placement with careful consideration of anatomy and radiological landmarks is essential to minimise injury to surrounding structures. Post-procedural discomfort is the most common complication and is usually transient. Other complications include infection, bleeding and nerve damage due to improper needle placement.
Pain relief with RFA is nonpermanent and repeat procedures may be required in some patients. RFA is just one method for management of back pain. It should not be used as sole treatment, but as part of a multimodal strategy that complements other therapies. The aim of RFA is to provide pain relief to reduce the need for strong opioid analgesia, facilitate rehabilitation, improve function and quality of life.
Author competing interests – nil

Our sleep & respiratory centres have recently changed their name from GenesisCare Sleep to Advara Sleep & Respiratory Care, following a change of ownership in late 2022.
Our sleep & respiratory physicians, teams and locations remain the same, and this will have no impact on patient care.

Our name has changed, but our high-quality patient-focused care remains the same.

Rectal cancer surgery as we know it started almost 100 years ago with the Miles operation. This is surprisingly similar to the current extralevator abdominoperineal resection, which is still often used for very low cancers involving or
rectal cancer was managed by permanent stoma rate. Nowadays, increasing numbers of patients under the age of 40 and fit over 80-year-olds wanting aggressive treatment. Today, rectal cancer
trained colorectal surgeons and multidisciplinary team (MDT) input colorectal surgeons, oncologists, histopathologists, colorectal nurses
Rectal cancer treatment has evolved substantially with five year survival in Australia around 70%, close to the highest in the world
Early diagnosis, ideally from screening, still has the greatest impact on outcome in colorectal cancer
Optimising treatment for a wide range of rectal cancers in a diverse patient group is backed by science but is an art requiring an experienced, high volume multidisciplinary team.
be performed by four modes –open, laparoscopic, robotic and transanal (TaTME). Open remains the gold standard. Laparoscopic is technically demanding. Robotic and TaTME are theoretically technically easier but require specialised training and equipment.
specialised pelvic exenteration units.
Early rectal cancers can selectively be managed with local excision per anus utilising TAMIS, TEMS or transanal excision.
Anal cancers are HPV-related and very different to rectal adenocarcinomas. Anal (SCCs) are exquisitely radiosensitive and have been highly successfully managed with chemoradiotherapy for over 30 years. Surgery is occasionally needed only for persistence or regrowth.
patients remains total mesorectal excision (i.e. removal of the rectum clear margins). Work-up requires pelvis, CT chest/abdomen +/- PET scan and review at MDT. Pelvic MRI is extremely accurate at accessing the primary tumour/circumferential reception margin and extramural venous invasion (EMVI) but remains
It is likely robotic will eventually become the preferred approach but, importantly, evidence of improved outcomes of TaTME and robotic surgery is currently lacking. Not all patients and cancers are optimally resected by the same technique, so most colorectal surgeons will choose between two or three of the above four modes depending on their training and experience.
‘Watch and wait’ remains contentious but is becoming a standard option. Like SCCs, rectal adenocarcinomas also respond well to chemo-radiotherapy, but only 20-30% get a complete response. Watch and wait is a good option especially for patients with low rectal cancers wanting to avoid surgery and permanent stoma. It requires intensive surveillance as most patients regrow and end up needing delayed surgery. Some authors have predicted that organ preservation will become the goal of rectal cancer surgery – a concept unfathomable until recently.
preoperatively and most patients
next week versus the traditional chemotherapy (LCCRT) over five weeks then a 6-12 week wait till
Total neoadjuvant therapy (TNT) is Folfox chemotherapy for 3-6 months after long-course standard chemo/radiotherapy. TNT is used for locally advanced, high-risk rectal cancers (e.g. T4, N2, threatened circumferntial resection margin or EMVI). The rationale of TNT is to avoid distant metastases (in the future) and maximally downstage the primary. There is now good evidence (from RAPIDO and PRODIGE trials which impressively showed survival advantages).
Large T4 and recurrent rectal cancers are usually downstaged with TNT and referred on to
Overtreatment, versus undertreatment, remains a consideration. With local recurrence rates now under 5%, avoiding excessive morbidity by limiting surgery or avoiding chemo/ radiotherapy is always considered, especially in the frail/comorbid/ elderly patient
Pelvic MRI is extremely accurate at assessing the primary tumour/ circumferential resection margin and EMVI but remains relatively inaccurate for nodal status.
Author competing interests – nil

 By Clinical A/Prof Jonathan Chan, Dermatologist, Karrinyup
By Clinical A/Prof Jonathan Chan, Dermatologist, Karrinyup

When it comes to pigmented skin lesions, melanoma tends to dominate the discussion and rightly so. However, melanoma accounts for only a tiny fraction of the pigmented lesions we see as clinicians.
So, what about the multitude of other non-melanoma pigmented lesions?
These can be a source of disproportionate distress to patients, particularly when they occur on cosmetically sensitive areas. These lesions become more common with age, and favour areas of greater sun exposure. Benign pigmented skin lesions can be difficult to diagnose, as there is overlap with solar dyschromia (nonuniform colour changes) in sundamaged individuals (Fig 1).

Further, it is essential to choose the most appropriate treatment modality to achieve the best outcome for patients with cosmetically distressing lesions.
Ephelides (freckles)
• Small, light to dark brown spots (never very dark or black)
• Common with lighter skin types (Fitzpatrick 1, 2) and blond or red hair
• Develop around three years of age (earlier with sun-exposure)
• Darker in summer months; fade without sun exposure
• Intense sun exposure (e.g. burn) can cause permanence
Solar dyschromia is common and difficult to diagnose accurately once melanoma is excluded
Darker skin lesions such as lentigines as well as solar and seborrhoeic keratoses exacerbate the appearance of ageing and sun damage
Laser and light technologies are safe and effective management options for solar dyschromia.
• Caused by increased melanocytic activity (rather than increased numbers of melanocytes)
• Treatment is sun protection.
Simple lentigo
• Occur at birth, increase in number during childhood
• More common with darker skin types (Fitzpatrick 3, 4)
• Do not fade with sun protection; may darken over summer
• Small, evenly pigmented light brown to black patches, with irregular edges
• Favour acral areas and genitalia in darker skin types
• Caused by mild hyperplasia of melanocytes in the basal layer, elongation of rete and surrounding melanin hyperpigmentation
• A solitary lentigo can be difficult to differentiate from a small junctional naevus
• Multiple lentigines can indicate genetic syndromes (e.g. PeutzJeghers, Carney complex, LEOPARD syndrome)
• Optimal treatment is laser. Experienced practitioner recommended due to risk of hypo or hyper pigmentation. Prone to recurrence.
Solar lentigo (Fig 2)
• Occur on areas of sun exposure/ sun damage, especially backs of hands and face
• Larger, less uniformly pigmented, and often asymmetrical (versus simple lentigines)
• More common in lighter skin types (Fitzpatrick 1, 2)
• Similar histology to simple lentigo, but with an overlay of solar elastosis and actinic changes in the dermis
• Treatment is laser. Recurrence is common.
Pigmented actinic keratoses
• AKs are traditionally thought of as crusting nonpigmented keratotic lesions
• However, can have light brown irregular pigmentation, resembling lentigines
• Occur on sun damaged areas such as backs of hands, face, shoulders and upper limbs
• Tangential view shows altered skin surface with irregular scale and disrupted skin lines (versus lentigines, where the skin looks normal when viewed tangentially)
• Usual treatment for solitary lesions is cryotherapy.

Flat seborrhoeic keratoses
• Seborrhoeic keratoses co-exist with, and may be indistinguishable from pigmented actinic keratoses and solar lentigines
• Caused by proliferation of small basaloid cells, without significant melanin hyperpigmentation
• Limited response to laser or intense light therapies – generally require destructive therapies (e.g. cryotherapy), leaving hyper and hypo pigmented areas.
Patients do not like pigmented skin lesions, even when melanoma is ruled out. Patients may complain that these benign pigmented lesions make the skin look ‘dirty’ and old. Studies have shown that treatment of pigmentary lesions improves patient perception of skin ageing and skin health.
Lentigines, both simple and solar, especially in fair patients on hands and face respond very well to laser (nano-second Q-switched YAG/pico-second at 532/734/1064nm), broad band intense light (IPL®/ BBL®) as well as fractional laser technologies (Fig3). Patients only require one to two treatments with improvement in colour uniformity. Repeated treatments may also improve skin texture. There is improvement within days, the downtime showing dry, dark-coloured small crusts akin to dried Milo®. Patients have clearance of lesions lasting up to 12-18 months, some patients requiring annual treatments, but some showing longterm, almost permanent, improvement.
Chemical peels (e.g. trichloroacetic acid, glycolic acid) can show similar results but require more treatments and are more difficult to achieve uniform colour.
Liquid nitrogen cryotherapy can be used but requires deft skill and is very likely to result in some level of hyper and hypo-pigmented areas particularly on backs of hands, lips and forehead areas.
Topical retinoids as well as glycolic acids can gradually improve the appearance of sun damaged skin but require years of therapy. These are often used in conjunction with physical treatment such as laser.
Due to the risk of hypopigmentation, caution is recommended when treating benign pigmented lesions on cosmetically sensitive areas. The risk of patient dissatisfaction is greatest for lesions on the face/decolletage, or in patients with darker skin types (Fitzpatrick 3+). Consider referral to an experienced laser specialist if in doubt.
– References available on request
Author competing interests – nil
By Mr Peter Ammon Foot Ankle & Knee Surgery


 By Ara Jansen
By Ara Jansen
Compelled to write, Dr Michelle Johnston also loves the acquisition of knowledge which comes with each book she has written.
“I’m always writing and learning something new,” she says. With her recent novel, Tiny Uncertain Miracles, she did a dive into the world of bacteria, among other investigations.
The book is set in the subterranean realms of a large public hospital where a chaplain, struggling with the loss of his family and faith, meets the hospital’s scientist who believes the bacteria he is working with might be producing gold.
In the meantime, the number of homeless outside the hospital is increasing, almost Christmas and you can’t buy chocolate in the gift shop. It’s a story exploring science, faith and alchemy.
“For a long time, I have been keen to set a story in Royal Perth Hospital,” Michelle says. “It’s a
rabbit warren and has labyrinthine space and dead ends. It has been cobbled together and there are so many unusual doors. In the book, it’s almost a magical place as it explores what makes you believe what you do.
“It was important to me to do some research and keep the veracity of the science and have that be believable, alongside some magical realism. I also found it interesting to explore medical issues through the eyes of a chaplain rather than a doctor.”
Michelle has been a consultant emergency physician since 1999.

“There’s a lot to love about medicine,” she says. “It’s an amazing job – incredibly rewarding, satisfying, challenging and gives me great pleasure. I would not swap it for anything and it feels like a rewarding way to spend one’s life.”
Her first novel, Dustfall, is the story of two doctors at different times
who end up at Wittenoom hospital in a story of crashing consequences and the suffering caused by asbestos mining.
The author says it’s hard to nail down why she loves to write. She considers it a compulsion more than anything.
“I don’t feel complete if I am not writing. That has been the case for most of my life. Writing has helped me understand the craziness of the world and it gives me a perspective on things. I also would not call it a soothing hobby.”
As her children are now grown, Michelle works part time in order to write more and makes it her spare time priority. She’s now in the exploration stage of her third novel.
Tiny Uncertain Miracles was about four years in the writing. Michelle says it took a little while to find the story, with ideas and drafts being written and dumped before it started to reveal itself. She calls the process “joyful difficulty”.
A voracious reader, Michelle has written for most of her life, taking a hiatus during her medical studies and then in her children’s early years.


“My goal is that I just want to be able to keep writing. As long as I have some readers, that’s good too. There’s such a joy in writing, in creating new things. To write a beautiful sentence must be like crack cocaine. Though I don’t know what that’s actually like – cocaine, that is – I do know writing a magical sentence is such a buzz.”
Tiny Uncertain Miracles is available now.

The beauty of the arts is that it can take you anywhere and a WA-made project called The Stars Descend is asking you to take a drive into the south-west of the state.
This ambitious dance project consists of five concerts in different outdoor locations, starting in Margaret River on March 17 and concluding in Kalgoorlie on April 1. It features professional and volunteer dancers and each performance will be unique, performed only once. The concert series involves a number of aspects. Firstly, the events happen within the forests and spaces of the Gondwana Link, a 1000km wildlife corridor that includes the Great Wetlands, the world’s largest temperate woodland. The events feature professional dancers collaborating with volunteers drawn from each location who have been working together in community workshops to create dances which speak locally but have global environmental meaning. Volunteers range in age from 14 to 70 and their occupations include students, retirees, nurses and farmers, drawn from their local region. Together the shows will involve around 75 performers and some 25 arts workers on the production side.
By Ara Jansen“They are people with different experiences of life, who live in the area, care for it and are interested in preserving our major ecological assets,” says award-winning dance producer Annette Carmichael, who is the project director. She has a history of working in regional communities and creating shows which shine a light on local but universal issues. The Stars Descend continues her work on large scale projects.
As you follow the performances and sonic soundscapes through various regional towns, it’s also a chance to explore the community organisations and Indigenous tour businesses who are actively engaged in environmental restoration and cultural experiences.

Because of the ecological link, the performances don’t take place in man-made spaces, but instead happen in nature-created spaces. New music has also been created for the five chapters.
“Because of the project’s focus on climate, we want people to smell the sheoak needles, feel the breeze or note the red dirt of our biodiverse state. We hope all these elements will focus people’s attention on these wonderful
places that need our protection and attention. We also want to create powerful memories so people will be encouraged to care more for the natural world.
“It’s important for the work, if it’s going to say what we need it to say, that it’s performed by many different people as climate action is required by many different people.” For those involved in the project, including the volunteers, Annette says one of the joys of creating such a multi-faceted work has been seeing those with no history in community art or dance projects discovering a resilience and bravery in themselves.
“They are connecting with other people and doing something they never thought possible. I have been seeing moments of real happiness inside this project and that is hugely satisfying – even before we’ve performed a show.”
ED: Follow The Stars Descend for the 16-day odyssey or as stand-alone chapters in single locations.
Tickets and itinerary details from www.heartlandjourneys.com.au/ the-stars-descend
Take a drive in the southern part of WA to explore climate action through a series of newly-created dance works staged outdoors.
It is a pleasure to again review this trail-blazing iconic Margaret River producer, and again the four wines tasted were of the highest quality. Cape Mentelle was central to bringing the Margaret River region to recognition in Australia and subsequently to international appreciation.
Winning consecutive Jimmy Watson Memorial Trophies with their 1982 Cabernet in ’83 and the 1983 Cabernet in ’84 was central to this recognition, this trophy being awarded to the best Australian one or two-year-old dry red wine. And indeed, they have subsequently played a leading role in establishing the definitive Margaret River Cabernet Sauvignon style, which is now sought after world-wide.
Their 145ha of estate vineyards includes all the highly recognised regional varieties and gives them total viticultural control as there is no need to use non-estate fruit.

I was excited to review their Zinfandel for this article. This distinctive variety had its origins in Croatia and is closely related to the Primitivo variety from Italy, and while Californians like to claim it as their own, it did not get planted there till the 1880s. There are very few Australian examples of this variety, and I consider the Cape Mentelle Zin to easily be the best in Australia. It was planted in 1974, with the Californian connection being Cape Mentelle founder David Hohnen.
Cape Mentelle is now part of the international giant LVMH –Louis Vuitton Moet Hennessy.

A big ripe, fruit-driven wine. Since I reviewed this wine last year, it has shown a very slight evolution, now more mellow and integrated, but still with a long life ahead.
Deep red in colour, the meniscus is lighter than last year. Spicy Shiraz aromatics, with cardamon and cinnamon. In the mouth, very full bodied and spicy, especially on the finish.
Redcurrant Spanish black olive and blackberry flavours are concentrated and bring the high alcohol into balance. The tannins are 'punchy', the acid firm, giving structural integrity. A good South-West Shiraz style.
2018 Zinfandel (RRP $65)
If you like big bold flavours, huge tannins and alcohol warmth, then this 'Zin' is for you. I, for one, like these characters and have followed these wines since the early releases. The colour, a youthful deep garnet/ ruby. Aromas of rich fruitcake and bramble berry. On the palate, big flavours of black fruits, dark chocolate, forest floor, and that characteristic briary edge. Tannins are long, fine and drying. A great zesty palate gripping finish.
A shining example of Margaret River Chardonnay. Displays a youthful green-gold colour. Beautiful aromatics, rich and redolent, with peach, orange blossom and oak characters coming through. The palate has a wonderful textural mouth-feel, with flavours of mango and ripe peach, a touch of butterscotch and cashew from the perfectly intertwined oak. A long clean finish by way of balanced acidity. A real beauty with 8-10 years ahead of it.
Cape Mentelle Margaret River
2018 Cabernet Sauvignon (RRP $110)
WOW. The essence of Margaret River. The flagship of Cape Mentelle, and from that great 2018 vintage. Without question it is the top wine of the tasting. Appearance is still so youthful with its bold colour. Aromatics are enticing — cassis, dried herbs and smoky oak. The flavours abound with blackcurrant, blackberry and ripe plum, all with a superimposed gamey earthy character. The tannins fine-grained, firm and persistent. This wine shows power combined with elegance. There is purity of fruit and structural integrity. As much as I love this wine now, it will reward cellaring for another 20 to 30 years. Oh, if only one might still be around to experience that!