

Privacy breaches and cyber incidents can happen

Workforce woes
Last month Medical Forum put a much-needed spotlight on the issues facing general practice.
While the current (and ageing) GP workforce is haemorrhaging at the rate of knots, it’s a double whammy as medical students increasingly shun that career path.
Thank you for your candid responses – we share some of them in this edition. It seems a lot of GPs are worried about the erosion of such an honourable profession, but on a positive, many have expressed how much they still love their work and have no plans to pull the pin.
Nurses are in short supply, and new government mandates are looming which will require aged care homes to have at least one registered nurse onsite at all times.

As we recover from the worst of COVID, it is also no bed of roses for the aged care sector.
We've all heard stories about baristas in Broome earning six figure incomes. Record low unemployment is good for those in the market for a job at the moment but it is very challenging for employers –particularly those in aged care.
Nurses are in short supply, and new government mandates are looming which will require aged care homes to have at least one registered nurse onsite at all times. It is only going to get tougher to recruit workers who are being courted by more generous pay offers from other sectors.
Palliative care is another area that is undergoing significant change and this month we explore how services are evolving and working to educate patients about their end of life options.
Just as voluntary assisted dying is a legitimate path for some, palliative care is a valid choice that has suffered in the past from misconceptions and media coverage suggesting many people linger in pain.
More honest and balanced discussions are needed.
SYNDICATION AND REPRODUCTION
Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.





PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au


EDITORIAL TEAM
Editor
Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production
Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist
Eric Martin 08 9203 5222 eric@mforum.com.au


Clinical
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au









Marketing
Quinn Hampton quinn@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au

ADVERTISING
Advertising
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical

Andrew Bowyer 08 9203 5222 andrew@mforum.com.au

6006
Phone:
9203 5222
08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
Eye hub a game-changer
The Lions Outback Vision Kimberley Eye Hub in Broome has recently expanded, marking significant progress in treating eye disease in the Kimberley and Pilbara.

The hub is aimed at providing greater equity of eye health services in remote, regional and vulnerable Aboriginal communities.
It provides permanent specialised eye health services in Broome and outreach to 20 communities and five regional towns across the Kimberley. It includes a full-service eye clinic with state-of-the-art diagnostic equipment, education and training spaces, a café and facilities for multidisciplinary use by visiting specialists.
Staffing includes three resident doctors and two optometrists.
The McCusker Director of Lions Outback Vision, Associate Professor Angus Turner, said the hub enabled patients to be treated closer to home, which was crucial in dealing with the challenges of remote eye health.

“People in isolated places like the North West have more blindness and complications from eye disease than in other places,” he said. “In particular, Aboriginal and Torres Strait Islander people have more than three times the rates of blindness and 14 times the rates of vision loss from diabetes.”
About 11% of the North-West Aboriginal population are vision-impaired or blind, and 35% of this group have never had an eye examination.
Medical biz is booming
A new report by the Melbourne Institute shows profits of medical businesses are growing faster than businesses in other industries.
Despite rising costs during the COVID pandemic, profits have bounced back, especially for nonGP specialists.
Led by Professor Anthony Scott, the report shows GP and non-GP specialist medical businesses saw profits rise by an average of 2.4% a year for GPs and 5.4% a year for non-GP specialists before the pandemic.
It found that while profits were increasing, so were expenses, which could be leading more medical entities to consolidate. The total number of doctors in solo private practices has fallen between 2013 and 2020, while the number in group private practices has increased.
The report includes new national data from the peak of the pandemic when medical businesses had a sudden increase in costs as
they adapted to COVID settings. Though profits initially fell during the pandemic, they have since increased again because of the pent-up demand, especially for nonGP specialists.
Robotic hernia ops Hollywood Private Hospital upper gastrointestinal surgeon Laurence Webber and his team have performed the first robotic ventral hernia repair in WA, using the DaVinci Xi Robot.

Robotic hernia surgery allows more patients to be treated with a minimally invasive approach, with potential benefits including less pain, shorter length of hospital stay and fewer complications.
The surgery in early October was a significant milestone for Dr Webber’s team, which included
A ventral hernia occurs when abdominal contents protrude through a weak point of the abdominal wall. Symptoms include pain or a lump in the abdomen.
While hernias occur in men and women, they are more common in men. About one man in every 20 will develop a hernia at some point in his life.
Hollywood was the first hospital in WA to purchase the da Vinci Xi Surgical System. The technology offers advanced robotic, computer and optical capabilities that assist a surgeon.
Costly menopause
Menopause comes at a price, and it’s not just physical costs like hot sweats and fatigue, new figures reveal.
Celebrating 40 years of palliative care at home
Since the program began with the State Government and the Cancer Council in August 1982, our service is now nationally and internationally recognised for our outstanding outcomes.
According to the Productivity Commission, approximately 70% of Australians would prefer to die at home but only 15% are able to do so.
Our holistic approach provides a gold standard of care to nearly 3,500 West Australians each year. Almost 60% of clients who died were able to do so in the comfort and safety of their own homes.
As a result Western Australia now has the lowest number of palliative care beds per capita in hospitals nationally.

This year marks the 40th year of Silverchain’s palliative care service that has provided generations of Western Australians with access to quality palliative care in their homes.
Our innovative service is defined by a dedicated team who provide complete care with compassion and unwavering commitment to our clients of all ages, including babies and children.
Due to the quality of our care, we were voted the most trusted home care brand in the state for 2022.
For more information or to refer our services, please call: 1300 300 122
Dr Alex Tang has become the first WA recipient of a Young Investigator Grant from New York’s Brain and Behavior Research Foundation. The Perron Institute and UWA neuroscientist will use $100,000 to look at how magnetic brain stimulation enhances neural plasticity.

WA nutrition expert Associate Professor Christina Pollard has been made a life member of the Public Health Association of Australia. Since 1994, she has advocated for improved food and nutrition, playing a key role in the Go for 2&5 campaign.

Royal Perth Hospital and the WA Museum Boola Bardip have created a photographic exhibition of the staff and patients in the days and months following the 2002 Bali bombings. Remembering the Bali bombings: 20 years on will be open until February 12 next year.
Dr Stephanie Godrich from Edith Cowan University is heading Food Community, a project aimed at giving people better access to healthy food, which is being rolled out across WA after a successful trial.

Curtin University is a big winner in the latest National Health and Medical Research Council and Medical Research Future Fund grants, with $800,000 for a project to increase COVID vaccination rates in Aboriginal women, and almost $3 million to develop online tools that will help predict the effects of mild traumatic brain injuries.

The Australian Institute of Superannuation Trustees estimates menopause costs women more than $17 billion a year in lost earnings in wages and superannuation and has called on the Federal Government to investigate the role it plays in contributing to the superannuation gender gap.
AIST, the peak body for the $1.6 trillion profit-to-member super sector, said recent British studies indicated up to a quarter of menopausal women experienced debilitating symptoms leading to long-term absences from work or forcing them into early retirement.
This aligned with data in Australia showing 26.8% of working women retired under the age of 55.
Women retire with 40% less super than men on average because they earn less and spend more time out of the workforce caring for children and other family members.
AIST said women aged 45 to 54 retired on average at 52, which was earlier than planned (59 years) and earlier than men (59.5 years), with
44.9% of citing “own sickness, injury or disability” for leaving their last job.
It pointed to a health crisis in under 55-year-old women driving retirement well ahead of what was intended.
The average age of menopause is 51, with many women experiencing symptoms for five to 10 years.
Study on skin tears a winner
A study by Silverchain on the effectiveness of a skin tear assessment tool has won the original research article award in the Coloplast Biatain Literary Awards.
The study, published in the Journal of Wound Practice and Research, was undertaken by Dr Robyn Rayner, Professor Keryln Carville, Joanna Smith and Cate Maguire.
It examined healing times and dressing costs for older adults with skin tears using the Skin Tear Audit Research classification that was developed by Silverchain and Curtin University in 2007.
The eyes and ears of research
Scientists at the Lions Eye Institute and Ear Science Institute Australia are moving closer to having personalised therapies for Usher syndrome, the most common form of inherited deaf-blindness, thanks to a Medical Research Future Fund grant.
Lead chief investigator Dr Samuel McLenachan, who runs the ocular tissue engineering laboratory at LEI, said a coordinated approach would allow them to test and develop more treatments for Usher syndrome.
Usher syndrome robs children of their two main senses, hearing and sight. Although some hearing can be restored with a cochlear implant, once a child loses their vision it cannot be restored. There are very few treatments to slow this vision loss, and there is no cure.
“Children diagnosed with Usher syndrome may only have a small window of time before their eyesight starts to deteriorate, and
once vision is lost, it cannot be restored,” Dr McLenachan said.
As part of the project, scientists will create retinal and inner ear organoids, which replicate the eye and ear tissue of a person with Usher syndrome.
They will use these organoids to test a range of drug and gene therapy treatments being developed by leading research groups at the University of WA, and Curtin and Murdoch universities. The pre-clinical testing would help identify safe and effective treatments that could be progressed into human clinical trials.

continued from Page 6
Skin tears are the most common wounds found among older people and are often associated with knocks or falls.
It is the first study to look at the implications of using a skin tear classification tool for determining healing times and dressing costs for treatment. It reviewed more than 2100 skin tears in Silverchain clients aged 65 years and older.
Professor Carville said the study would help make wound care more effective as well as provide greater transparency of healing times and treatment costs.
“The STAR classification has demonstrated to be an effective tool for assessing skin tears and for providing a basis for risk stratification that determines which skin tears are likely to be more costly in terms of healing times and treatments,” she said.
No fall in rate of falls
Falls and their related injuries continue to be a significant public health issue in WA, ranking as the leading cause of injury hospitalisations.
Injury Matters has released its 2022 Western Australian Falls Report, which shows that one person died every 25 hours in 2019, was hospitalised every 17 minutes in 2020 and attended the emergency department every 13 minutes in 2020 due to a falls-related injury.
The 31,708 falls-related hospitalisations in 2020 resulted in 239,669 hospital bed days and cost an estimated $286 million. On average 7.6 days was spent in hospital per falls-related admission in 2020.
On average 84 falls incidents a day – or more than 30,000 cases – required an ambulance attendance in 2020.
LETTER TO THE EDITOR
Dear Editor,
I read with interest your editorial on GPs, our national treasures in the September edition of Medical Forum
I am of the view that many senior doctors with many years of valuable medical expertise are giving up because of the unreasonable requirements of the Medical Board for them to renew registration to continue part-time practice.
The Medical Board requires full medical registration and medical insurance with increasing demands for continuing medical education, including recency of practice
requirements that makes it very difficult for part-timers, so many of my colleagues decide to give up and retire.
The Australian Senior Active Doctors Association (ASADA) has been appealing to the Medical Board to relax some of the onerous requirements but has had little success.
Unless this problem is addressed, the number of doctors retiring will progressively rise and this is likely to be substantial, as I understand at least 30% of doctors are of retiring age.
Dr Kar Chan Wan Consultant Occupational PhysicianThinking outside the box
To solve the crisis in general practice, we need to think like the mining industry, argues a former WA chair of the RACGP, Dr Colin Hughes.

The GP workforce crisis needs some out-of-thebox thinking. As well as the current position of the RACGP regarding capitation and moderate cost-of-living increases, do we need to rethink the quintiles to reward productivity and longer consultations?
We all know that our patients don’t read the text books and come in with just one complaint. Yet the current system rewards six-minute medicine and penalises those GPs
practising holistic care, particularly female GPs seeing female patients.
Our rural colleagues' circumstances also need radical thinking. Shouldn't we reward their sacrifices and try to retain GPs by offering paid holiday study and long service leave?
Some may see this as an ambit claim and maybe it is, but we must be bold and get our GP colleagues behind us.
The definition of insanity is doing the same thing over and over and expecting a different result. It’s time the RACGP polled their members as to these proposals.
Change the quintiles as follows: Level A 0-5 minutes: $20 simple injection, obtaining result with no intervention required.
Level B 6-10: $40 standard consultation requiring single issue examination and treatment, e.g. blood pressure check or immunisation; response to acute problem like colds and flu.
Level C 11-20: $80 more than one complex problem requiring examination and treatment plan and at least one ageappropriate preventive screening question, e.g. are you up to date with immunisation, Pap smear,


Thinking outside the box
cholesterol check, quit smoking, safe sex?
Level D 20-30: $120 for three complex problems or one major complex problem like management of diabetes requiring referral investigation, or mental health review.
The advantages
Firstly, patients are now being charged a gap fee of $40 particularly in areas where there is a GP shortage, e.g. Karratha.
GPs do have access to specific health items like care plans or mental health review, but patients have multiple, complex needs which don’t fit into boxes. GPs need the ability to deal with multiple, unrelated issues at the time of consultation.
Research shows productivity increases and patient visits decrease the longer you spend with patients. (In Norway the standard visit is 20 minutes.)
There is little or no incentive to raise preventive activities, yet research shows simple interventions and health advice is the single most effective intervention reducing morbidity and disease burden.
Easy to check compliance and stop rorting by clinical audits.
Rural GP crisis
We love working in remote and rural general practice. The biggest problem is the constant on-call and quality of life. It is essential that rural and remote GPs get adequate compensation for leave provision and that means fully salaried, with:
• 6 weeks annual leave
• 2 weeks study leave to attend conferences and reskilling every 2 years
• 10 weeks long service leave after 5 years
The advantages
This would both retain current GPs and also attract future GPs. If the mining industry can offer these kinds of conditions for working
Tattoo-free radiation therapy now available at GenesisCare, Wembley
GenesisCare, Wembley offers the latest stereotactic treatments with the implementation of the Versa HD Linac and CRAD (surface-guided RT) technology.
Tattoo-free radiation therapy - eliminating the emotional impact of permanent marks on patients’ skin.

With a holistic approach to cancer care, GenesisCare, Wembley offers extensive support services:
Exercise clinic
•
packages
For more information, please contact our team and GenesisCare:
24 Salvado Road, Wembley WA 6014
Tel: (08) 6318 2868 receptiononcologywembley@genesiscare.com
remotely, surely we can offer our rural colleagues similar benefits paid for by increasing royalties on mining exports and a super profits tax on the massive windfall profits made by big gas and coal.
(It’s a lot easier to sell to the community when you tell them it is for providing better GP services to the bush!)
Lastly, the future crisis of GP shortage reminds me of being at Manchester University Department of General Practice. To attract GPs, they offered salaries equivalent to a senior registrar in the hospital system.
HECS fees should be waived for all FRACGP graduates after five years of GP service.
We must think outside the square.
ED: Dr Colin Hughes is former head of Public Health East Perth and a clinical tutor at the Curtin Medical School.
The doctor who called us was stunned. They had been reported to Ahpra and were being investigated for self-prescribing. “It’s my business if I prescribe to myself; and anyway, these were not Schedule 8 medicines!”
And so began a discussion of how the Medical Board views selftreatment by medical practitioners, and how this has changed over the years.
There is broad recognition that our health and wellbeing impacts on our practice, and we are extolled to accept selfcare as a cornerstone of professional life.1,2 However, there are distinct limits to the self-care we can and should provide to ourselves.
Stepping into providing ourselves care that only a registered health practitioner could deliver, likely means we are stepping outside the Medical Board’s Code of Conduct 3 guidelines, with the risk of poor care outcomes or investigation. Every year, there are examples of practitioners who have registration-impacting outcomes at Tribunals resulting from inappropriate self-care and care boundaries.4

Section 11 of the Code, a relatively recent addition, talks about managing one’s own health. This section reflects similar constraints to the provision of care to close friends, family, and those you work with, discussed in section 4 (which was also updated).
Medical practitioners should not be self-prescribing This isn’t just a reference to self-prescribing Schedule 8 drugs (which most jurisdictions restrict or prohibit) or select Schedule 4 drugs, including drugs of dependence. It refers to ALL prescriptions by a practitioner for themselves. In addition, practitioners risk breaching the specific, varying, and complex legislative restrictions on self-prescribing in each jurisdiction – ranging from full self-prescribing prohibition (Victoria) through restrictions on prescribing Schedule 8 drugs and some Schedule 4 medicines (Queensland, ACT, NSW, potentially WA/NT); or restrictions on self-prescribing Schedule 8 drugs. Such breaches may be a criminal offence.
Health practitioners should have their own GP
While I’m sure we all subconsciously self-diagnose at times, the value of independent objective workup, investigation and treatment cannot be overstated. This includes the importance of approaching your treating team for documents like medical certificates, and not issuing these yourself.
Seek advice
There is additional emphasis on the importance of seeking advice in relation to health issues that could impact your work, including stress, burnout and mental health.
Contact the DHAS
If you have troubles locating a GP, the Doctors Health Advisory Service (DHAS) in your jurisdiction may be able to assist in finding GPs who have identified themselves as having an interest in looking after the health of their colleagues. They can also provide confidential telephone callback support in more acute circumstances, such as mental illness, stress, drug and alcohol dependence, and other personal issues.
Mandatory reporting reassurance
Where doctor-patients follow their treating team’s advice on whether their health issue impacts on work and how they should manage this (including modifying their practice), there should be no basis for a mandatory report. Complaints are generally straightforward to deal with if the doctor has sought and followed their treating practitioner’s advice. It is more common for doctors who don’t have a treating team to find themselves in difficulty if a concern about health impairment is made to a health complaints body. Tragically, we are also aware of terrible outcomes arising when doctors attempt to manage their own substance misuse or significant mental health conditions.
Searching for aged care’s many hands

Australia is in the midst of crippling workforce shortages, creating the perfect storm for the aged care sector as it also grapples with new staffing mandates.
Cathy O’Leary reportsIn the lead-up to the last Federal election, the head of WA’s aged care providers’ industry association was asked to list the three key issues for the sector.
For Liz Behjat – a former Member of the Legislative Council during the Barnett Liberal Government – the answer needed little thought – the main concerns were workforce, workforce and workforce.

As WA State manager of the Aged and Community Care Providers Association, Ms Behjat is trying to help the industry negotiate its way through the challenges of acute workforce shortages amid new staffing requirements.
Aged care providers are having to take a deep breath as new minimum standards for staffing and care start to kick in – including having a registered nurse onsite 24 hours a day – after the Royal Commission found that more than half of residents in aged care lived in homes that were significantly understaffed.
Currently the sector has an average 11% job vacancy rate – with staff shortages preventing 341 elderly West Australian people from accessing residential aged care last year.
A national study by the University of Notre Dame Australia and Catholic Health Australia earlier this year estimated there were about 82,000 vacant jobs in the hospital and aged care sectors – 70% of them in aged care. And it is not just a lack of registered nurses, with many aged care facilities scrambling to find cleaners and cooks, as they compete with the hospitality and mining sectors.
Ms Behjat said retaining staff was difficult, with facilities getting staff in and training them, only to see them go elsewhere where they were offered more money. Some organisations had even resorted to offering incentives such as tickets in staff lotteries for their loyal years of service.
Governments were also trying to make it easier for people in Australia on certain categories of visa to be able to work while they waited for permanent residency.
Innovative pilots
Ms Behjat said the State Government was working hard in this space, including ‘job ready’ pilot programs to give people a taste of what it is like working in the aged care and disability sectors.

“Newly built aged care facilities are not your C-class hospital type anymore – and while there are obviously other issues, the biggest challenge is workforce,” she told Medical Forum. “We have to start looking ahead at different models of care, and where the workforce is to come from.
“In WA, we have the added complexity of distance – what do you do in rural and remote areas, where people want to stay and don’t want to move to the city to receive care. How do you get staff and nurses there – and where do the staff live?”
She welcomed moves to have high school students spend time in aged care homes on excursions or as part of community service programs.
“They learn that there’s more to it than wiping old people’s bottoms and it challenges the preconception
that it’s all about old people sitting around in God’s waiting room,” she said. “Many of these kids are surprised to see there are so many activities and therapies like physio and OT, and alternate therapies like art and music therapy.”
Her sentiments are echoed by Clare Grieveson, chief executive officer of Southern Cross Care, one of seven WA aged care providers, representing about 60% of the beds in the State, who are working together in a group known as G7.

Its function is to collaborate with government and industry stakeholders to address issues in the aged care sector, and to ensure the legislative changes for aged care can be practically implemented at the provider level.
“It’s always been a very difficult area, and it’s multi-factorial,” Ms Grieveson said. “The pay for nurses in aged care is lower than in the acute sector, and that’s been the case for some time, so that makes it difficult to attract nurses into the sector.
“The funding from government hasn’t been indexed for many years, so the funding gap has
become wider and wider. Now the sector is at the edge of a financial cliff and for some of the really small providers the gap is at the point where it’s getting too large.”
Ms Grieveson welcomed the introduction of the new Australian National Aged Care Classification funding model and recent moves by the Commonwealth, which has pledged to inject more than $17 billion into aged care.
Wages support
She is fully supportive of the case in the Fair Work Commission looking at a 25% wage increase for nurses in aged care – provided it was fully-funded by government.
The recent data showing 60,000 job vacancies in aged care nationwide was “hugely concerning.”
“It means we can’t fully staff our beds, and existing staff have to work extra shifts, or we need to fill our vacancies with agency staff, which isn’t good for residents because they get to know the existing staff.
“It’s so important to get a workforce to support our residents and provide the staffing levels that are needed in our homes, and while allied health are a core part of the workforce, they’re not recognised
Searching for aged care’s many hands
in the new funding model, which is disappointing.”
Ms Grieveson said it was time to be more creative about how staff were employed, such as looking at the use of migrant workers, and converting overseas qualifications more quickly.
“Expanding skilled migration arrangements for all workers in aged care, not just RNs, but also our kitchen staff, our carers, is crucial, particularly in WA, where we’re competing with the mining sector where pay is so high.
“When we talk about a perfect storm in the sector from COVID, we need to add the mining industry and workforce shortages into that storm in WA.”
Other avenues to grow the workforce included finding ways to fast-track enrolled nurses converting to registered nurses, which currently took 24 months. Reducing that to 12 months and increasing the availability of nursing qualification exams in WA would help, she said.
Another signal of the changing environment goes a step back – to fewer people signing up to nursing places at university. For the first time, Notre Dame University initially struggled to fill its nursing intake quotas this year.
Tom Ristoski, senior director of Industry Partnerships and Pathways at Notre Dame, said that historically its nursing courses had always been significantly overprescribed, but in its mid-year intake this year it struggled.
When the university checked with other higher education institutions, they were seeing the same downward trend in nursing enrolments.
“We ended up filling the places but the fact that it’s gone from consistently high to struggling to fill, something’s happened, and
my best guess is that’s to do with borders being shut, and a big blockage in the visa-processing area of the government,” he said.
“Also playing a role is ‘the great resignation’, as has the significant negative news around health care and how hard it’s been in primary care, but specifically in aged care.
“The headline figure is that the trend is worrying if it continues that way, and it’s absolutely the perfect storm, particularly with the laws passed where from July next year an RN must be present 24 hours at all facilities.”
Action needed
Mr Ristoski said that as a university with strong medical schools and health schools, Notre Dame had been working with industry to look at what could be done, such as accelerating recognition for lapsed and international training and developing career maps.

Another initiative was to accelerate the process of getting nurses into aged care and clinical areas by trialling second-year student nurses doing their practicals and getting paid for it.

“In the past, they wouldn’t have been paid, but now employers are seeing that with such shortages we have to start paying these kids even if they’re not fully qualified. They’ve got some of the minimum qualifications to do very simple work.
“A lot of things being done are bandaid and short-term to deal with the current shortages, but at the end of the day the aged care segment is growing and there is a huge upward trend of baby boomers retiring. Meanwhile the birth rate is declining and so is the immigration rate.
“It’s terrific to raise the wages in aged care, and that will attract more people, but there’s only so many people in the working population, and we really have to look at how we bring in skilled and
unskilled workers, because I don’t think we’ve ever been in a situation that’s so dire.
“When kids look around, they can earn good money driving trucks so there are lots of options out there, and the nursing and aged care workforces are up against that.”
Ms Grieveson reiterated the need for providers to work together to advocate for sector-wide issues – a call to action to get compassionate people who are willing to learn new skills to care for residents and clients.
There was common humanity across the generations – people wanted connection, communication and relationships, and that became more important as people aged.
“We’ve got an ageing population and more people will need aged care. The trend of aged care being provided at home through community care is great, as people can stay at home for longer, but it means that when people do move into aged care they have
Aged care staffing reforms
As a result of the Royal Commission’s recommendations and the Federal Government’s new funding model, new minimum staffing and care requirements for residential aged care are being phased in.

By October 1, 2023: providers must ensure residents receive at least 200 minutes of total care a day from registered nurses, enrolled nurses and personal care workers at least 40 minutes of that care must be provided by an RN an RN must be onsite for morning and afternoon shifts each day (16 hours a day).
By October 1, 2024: providers have to ensure residents receive a minimum of 215 minutes of total care a day at least 44 minutes of that time must be provided by an RN an RN must be onsite 24 hours a day.
The requirements are industry averages, with each home’s requirements adjusted based on the relative complexity of their residents’ care needs. This means providers with a higher than average proportion of high needs residents would need to have additional staff working.
more comorbidities and have more complex care requirements.”
Ms Behjat agreed that more people would be staying in their homes for longer, and when they did go into aged care, they would invariably be older and sicker.
The industry was making sure that the changes could be accommodated by the delivery of services into their homes, or into retirement villages.
Aged care would be very different in the future, and it would not be a one-size-fits-all, she said. Providers would need to be more culturally appropriate, and respect choice and gender diversity.
The industry would also need to be smarter with the resources it had through technology such as telehealth services, particularly to support people in regional areas.
And she added that the elephant in the room was the cost of aged care and the reticence of people to contribute to that.
“During our life we pay our rent or mortgage, but for some reason we all think that at a certain point of life the Government has to look after us. But why do we feel that –that’s a hard conversation to have with people,” she said.
However she said there was still a lot of goodwill and determination in the aged care sector.
And while COVID had been very testing on the industry, with lockdowns and people not being able to visit elderly relatives, some positives could be taken from the experience of WA.
“You know we actually did very well during the height of COVID in WA – we had very few deaths in aged care,” she said. “People can now look back and say ‘we still have mum or dad, we didn’t lose them.’
“That’s a great credit to the aged care industry.”
Surgical audit explores COVID impact
Patients with long COVID who die under the care of a surgeon will be a new focus of WA’s annual audit into surgical-related deaths.
Established as a voluntary audit in 2002, the Western Australian Audit of Surgical Mortality is a peer-reviewed investigation of the care associated with surgery-related deaths to improve patient safety of quality of care.

WAASM is funded by the WA Health Department and has protection under federal legislation. Participation in the audit became a mandatory requirement of the Royal Australasian College of Surgeons in 2010, and since 2013 has been part of the RACS CPD program.
A review of more than 2800 deaths in the past five years, from 2017 to 2021, identified 571 clinical management issues, with 44 involving adverse events that caused death. Of those, 18 were considered preventable.
WAASM’s 2022 report, released in mid-October, recommends an ongoing review of the impact of COVID-19 on deaths under the care of a surgeon, given the increase in COVID cases in WA this year.
WA surgeons are facing the long tail of COVID and tightened rules about how they report deaths, as Cathy O’Leary reports.
This includes a preliminary analysis of reported deaths in elective cases in patients aged 50 years and under or in regional hospitals (where complex cases are predominantly transferred to metropolitan tertiary hospitals) that are considered unexpected. The analysis of low-risk deaths is still in progress and is due to be reported in the 2023 WAASM report.
WAASM is continuing to ask surgeons to identify any patient deaths related to COVID-19. No data was received on this for the years 2020–2021, but audit staff are interested in reviewing this in the future.
Audit clinical director, general and colorectal surgeon
Mr James Aitken said COVID-19 had been the dominant health theme for the past two years.

“Until early 2022, WA had minimal COVID infections and WAASM is not aware of any patient who had died directly or indirectly from COVID-19. This has changed following the widespread development of COVID-19 in WA from early 2022,” he wrote in the report.
Mr Aitken said any increase in deaths was likely to manifest itself directly or indirectly in different ways.
In the acute phase, there was evidence that patients with COVID should not have surgery for at least seven weeks after infection. For those presenting as an emergency, that may not have been possible.
And long COVID was likely to develop in at least 15% of infected patients.
“At the time of writing this report, there is no published data reporting the outcome of surgery in patients suffering from long COVID-19,” Mr Aitken said.
“COVID-19 has an impact on the microvascular circulation and other health conditions that impact on this (such as smoking and diabetes) that can increase complications. So, there is the potential for long COVID-19 to adversely affect surgical outcomes.”
Mr Aitken warned that restrictions on elective surgery during the pandemic had greatly increased
waiting lists. Reducing the increased elective surgery backlog would be a major health priority for the next few years.
“Delaying emergency surgery has long been one safety valve used to prioritise elective lists, so they continue uninterrupted. There is a real risk that prioritising elective cases will delay theatre access for emergency operations. This will compromise emergency surgery outcomes and prolong hospital stay and hence costs.”
More broadly, Mr Aitken said that over the past 20 years there had been a substantial fall in operativerelated mortality, which meant surgery in WA had never been safer.
While some of the improvements were likely to reflect improvements in practice, others reflected the direct impact of WAASM.
One of the trends seen in the first 10 years of the audit was an increase in the number of patients who died under the care of a surgeon but who did not have an operation. RACS believed this suggested a greater recognition of the limitations of surgery and reflected WAASM’s long-term interest in the use of futile surgery.
Mr Aitken said the necessary changes still needed were often systematic, slow to enact and complicated by wide annual variation. The audit cycle often had to be repeated and reinforced if improved care is to be sustained.
The development of clinical quality registries in Australia was many years behind other countries but it was rapidly changing. The key to the integrity of CQR was complete cases and data.
“The availability of more accurate and timely administrative data, coupled with artificial intelligence, is already changing the future,” Mr Aitken said.
“The traditional annual quality assurance ‘data dump’ is already being replaced with near real-time continuous quality improvement data that will increasingly extract and report daily data from administrative datasets. The United Kingdom’s Get It Right First Time program is a glimpse into the future and has already arrived in other Australian states.
“The WA Department of Health is actively engaged in the use of these new techniques. All WA clinicians, and those involved with WAASM, will have to engage with these new demands and at a rapidly accelerating rate.”
Mr Aitken said changes to WAASM would never have commenced without the protection provided by qualified privilege (QP), which was now under Commonwealth legislation.
The QP covering WAASM had recently been adjusted to permit it to identify to the WA Health Department any patient where assessors had identified a Health Roundtable 4 or 5 death.
But only patient identifiers would be provided. All WAASM information such as activities and report would continue to be covered by the same QP protection as previously.
Mr Aitken said this was a small but necessary step to ensure all deaths under a WA surgeon had been appropriately reviewed.
There were also looming changes to the reporting of CPD compliance from the start of 2023, which meant that for most surgeons RACS would become their accredited CPD ‘home’.
Tightening CPD
It was also a requirement of the RACS CPD program that surgeons return WAASM forms within two months – something that had not previously been strictly enforced.
“There is a new focus on encouraging and supporting fellows to comply with the standard to ensure timely completion of the audit requirements,” he said.
“This is an important obligation to comply with.”
Mr Aitken also took a swipe at continued setbacks to the audit being able to access the Coroner’s reports, describing it as a major handicap for those seeking to learn from post mortem reports. “Change to the current legislation is now urgent and long overdue,”
he said.
Second time’s a charm
By Ara JansenWhen you ask Dr Katrina Calvert why she became a doctor, it’s actually a better story to ask her why she became a doctor again.

Thanks to a dad in the air force, Katrina was born in Germany and grew up all over the world. When she decided she wanted to be a GP, she started medical studies at the University of Edinburgh. During her rotations, she fell in love with obstetrics. She loved the happiness and feeling of optimism in the specialty. She’d found her career home.
In 2006, with a year and half to go of her specialist training, she was looking after a patient whom she had grown to know well. The woman delivered a stillborn baby. It broke Katrina’s heart.
“I could not get over it,” Katrina says who was in her early 30s at the time. “I was absolutely devastated. I could not talk to the patient about it, as I could not bring myself to speak to her. The failure of not being able to step out of my own emotions was unbearable to me, alongside not being able to manage my patient.”
“As a result of this event and a growing doubt that I was capable of doing the job anymore, I gave up medicine and walked away from it all.”
Dr Katrina Calvert found her way back to medicine in her 40s and her work now is a love letter to her joys of life – and the mothers and newborn babies she helps.
“I could not talk to the patient about it, as I could not bring myself to speak to her. The failure of not being able to step out of my own emotions was unbearable to me, alongside not being able to manage my patient.”
Katrina had met her husband during her early O&G training. Irishman Dr Paul McGurgan was a year ahead of her. When he was offered a job at King Edward Memorial Hospital, they made the decision to move to Perth. Katrina was pregnant with her third child, joined Cottesloe Playgroup and spent the next 10 years as a stay-athome-mum.
As her children grew and became a little more independent, she started doing some part-time university teaching at UWA with the medical students.

“I really loved teaching and loved the students’ enthusiasm and engagement. I thought that was going to be me – a teacher of medicine.
Hands-on
“One day a student asked a question I didn’t know the answer to and I realised that I had been out of practice for a while. I realised I needed to be practising in order to teach. I applied to AHPRA, decided I would become a GP and got my registration.
“I ended up at King Edward and fell in love with obs and gynae all over again. So, I applied for training and started all over again. I became a resident at King Eddies and completed the program in six years to become a consultant in 2020.”
Despite her age, Katrina returned to being a junior on the delivery teams. A story she remembers fondly was being called the baby singer after manually turning a baby and delivering it, while her team were working with another mother. The team returned and the father told them that Katrina had sung to the baby and it had arrived.
“It's so joyful when you help a woman produce a baby. When you are there in that space, it’s such an incredible feeling. I’m hooked again!”
Now Katrina has the best of both worlds combining her love of teaching and imparting knowledge with practical work. She is director of Post-Graduate Medical Education at KEMH and teaches and advises as well as delivers babies. Her Twitter profile says: obstetrician because there’s no better way to spend the day.
Senior to Katrina for a long while was her husband Paul, who is also
an obstetrician and gynaecologist. The pair have only found themselves in theatre together once. After a number of “loves” and “darlings” came after operating instructions, they figured it was better not to be doing that again.
With two obstetricians in the same house, Katrina jokes that when she’s on overnight call, she often tells people “call me if you need anything. I sleep next to an obstetrician in case you need a second opinion”.
Caring genes
Something of Paul and Katrina’s journeys must have rubbed off on their children as their eldest son is doing medicine and their
daughter is studying psychology with a master’s in education. Their youngest son is still in high school.
“I’m sure we have influenced them,” Katrina says of her children. “It has always been important to us to let them know that they don’t have to do well but they do have to do good. We’ve tried to instill in them a sense of social responsibility.
“They are privileged kids with a lot of good fortune and it’s important they do something to pay that back. It’s also important they pay it back in a way they are passionate about.”
To relax, meditate and decompress, Katrina chases the black line at her local pool and in summer swims to Rottnest once a year. Her team of four have been doing that since 2016. While swimming is great for her physical health because she’s a chronic asthmatic, she says it’s equally important for her mental wellbeing.

The family also have three Irish setters – Rosie, Paddy and Ruadh – who definitely bring plenty of energy to the household and require vigorous daily walks.
Katrina’s biggest hobby is sewing and she makes scrub hats and shirts in material with fun designs. Bright
HBF launches new program to support members living with

–
Eligible
Second time’s a charm
Indigenous and Pride patterns might also be her handiwork if you see them around the hospital. Babies born during NAIDOC week this year received specially patterned beanies as well. Her son in medical school recently went to a local school to help with a teddy bear hospital and Katrina made him scrubs with dinosaurs on them. Of course, the kids were chuffed.
“It’s great for my soul to make these. I wear my own designs and give them away. You have to find ways to put joy into your day.”
Katrina also sits on the board of Helping Little Hands, a notfor-profit which supports and empowers families of premature and sick babies. This allows her to continue supporting babies after delivery.
Not forgotten
While Katrina loves her current work and being back in the medical world, that old wound some days exerts a little power. “It’s a trauma you carry forever. The most I can hope for in my field is not that you won’t have scars but that you are able to recognise and know where your trauma is and its triggers.
“After going back to work in the perinatal field, a very wise midwife helped me see that I don’t have to emotionally distance myself from my patients and that’s what I berated myself for not being able to do.
“It can’t be about you, but it can be that you are affected by an event. You don’t have to be cold and distant. You can be in it, but not in it to the point that it’s about you. I show emotion at work in the teaching and client space and it’s OK to say, ‘I’m having a bad day, but I’m still going to help you’.
“I’ll tell someone ‘this is going to be a sad day but I’ll help you through it’. That allows me to live my core values of helping and being of use and supporting someone going through something without hurting myself.”
In support of her peers and those in training, Katrina started
a cuddle team providing debrief opportunities. She was also largely responsible for adapting a UK emergency multidisciplinary obstetric simulation training course and facilitating it at KEMH.
These were some of the reasons why, at the age of 46, she was awarded the prestigious Dr Camille Michener Legacy Award for Junior Doctor of the Year in 2019, sparking one of her swimming team mates to joke, “What exactly is the definition of ‘junior’ in this junior doctor award?”

Katrina is passionate about doctor education, wellbeing and emotional support. As a result, she is chair of the RANZCOG working group on wellbeing and has a master’s in health professional education from UWA, which looked at outcomes after feedback is given to lecturers.
Outreach
Locally, she is a committee member of the Doctors’ Health Advisory Service WA, a confidential and anonymous advice line and referral system for doctors and medical students seeking assistance with health or personal problems.
The need for the group has been brought into sharp focus with the recent suicide of an obstetrician in Canberra.
“I feel like I have a certain licence that I didn’t have in my 20s, when juniors were often supposed to look and feel strong. I tell them it’s OK to not be OK, and OK to need some space, a cuddle or time off. It’s also OK for others to see that something affects you, or to say you don’t want to see a certain patient because you’re feeling triggered and please can the team help me. I am so lucky to have been able to reach out to my clinical teammates and receive support when I have asked for it. We just need to learn to ask.”
A natural warmth and inclination to teach and help is perhaps no surprise when you discover that Katrina’s mother, grandfather and brother are teachers and her father also taught people to fly.
“It’s in our blood and it’s such a joyful thing to do. It’s so rewarding and I get so much back. It’s cupfilling.
“Being a doctor is a great job and a great thing to do. To be able to make a connection with someone at an important time in their life is a hell of a way to earn a living. You are part of that day and that event. We’re lucky to be able to do that.”
Doing death differently
By Eric MartinPalliative care was cast, thanks largely to sheer juxtaposition, as the ‘choose life’ option for people with a terminal illness, yet research undertaken at St John of God Hospital Subiaco showed that significant numbers of patients who could have benefited from access to these services were not receiving them.
With demand for palliative care expected to increase by 50% over the next decade – and double by 2050 – Medical Forum spoke with the CEO of Palliative Care WA, Lana Glogowski, to discuss the need for doing death differently in Australia.
“Palliative care is actually more about life and living than it is about death and dying – and that is just so important.
Palliative care is much more than symptom control and pain management,” she said.

“Those two things, of course, are critically important, and that's what our palliative care physicians are focused on. But once a person receives a life-limiting diagnosis, palliative care provides a holistic approach to the patient. It's about recognising those many and varied needs in addition to their clinical requirements.
“We need to be able to provide social work support. We might need to provide spiritual support. We might need to connect
these people to a range of social networks so that they have the support they need for the last stage of their lives.”
Ms Glogowski said the research was clear that if people get early access to quality palliative care, they actually live longer because their holistic needs are being met.
“I really emphasise the importance of early access to palliative care, which has been a priority for a long time, but we’re a long way from being able to provide that,” she said. “At this stage, resources are tightly focused on the clinical support, but the social work and allied health supports, and pastoral care really need to kick in straight away.”
New awareness Though the WA Government has expressed its commitment to growing palliative care, Ms Glogowski believes that what emerged from the VAD debate was a growing community awareness about its importance, especially considering the pandemic.

“The real upshot for us is that people are starting to talk about death and dying, which is a real taboo in our community that we need to break down,” she said.
“It's important that people start thinking and talking it. All the debate in the media on voluntary assisted dying legislation has been good for us in terms of opening the lid on those conversations,
and COVID has really encouraged people's recognition of their mortality.
“For many people, this has been their first experience of death and dying. It may not be their immediate family, but it's something that has been very evident across our communities, and that's confronting for many people.”
Ms Glogowski emphasised the importance of those conversations with an unusual example from Palliative Care WA’s upcoming biennial summit, Doing Death Differently, to be held on November 24 at Optus Stadium – ‘death cafes’.
“These are safe spaces where people can talk about death and dying and ask the questions they don't feel comfortable to ask family and friends – environments where people can explore their values and priorities around their dying experience and potentially that will lead to advance care planning,” she explained.
“It's about making that discussion more acceptable for people to come together, to sit around a table with a coffee and a muffin and start talking about these things.”
She said that the biennial event would bring together politicians, palliative care, aged care and community service professionals, researchers, volunteers, policy makers, students, carers and community members to discuss future priorities for quality palliative care in WA.
While community support for voluntary assisted dying may have focused on the right of West Australians to end their own suffering, the debate also shone a spotlight on palliative care – and the need to do more to ensure quality end-of-life.
Growing cohort
The VAD debate, she said, was accompanied by an increasing recognition that the baby boomers were now moving into retirement.
“That’s a big cohort of people, many of them are very well educated, they have been in charge of everything all their lives, and they want to be in charge of their death.
“We are starting to see the kernels of some quite amazing change, with
increased interest in volunteering in the compassionate communities’ approach, and we have phenomenal uptake in our advance care planning workshops, with up to 120 participants recently in Kwinana.
“From our perspective, advance care planning is a critical entry point to palliative care.”

Advance care planning (ACP) is the internationally recognised term for planning for the last stage of a person’s life and Palliative Care WA has been funded by WA Health to run workshops across the State to encourage people to consider the process.
There are no age restrictions on ACP and it is not restricted to people who have a life-limiting diagnosis or were managing chronic disease.
“What we say to people is, you plan for the birth of your children, you plan your engagement, your marriage, your finances, and you plan for retirement. Why don't you plan for the last stage of your life?”
Ms Glogowski said.
“We recognise that people are fearful about death and dying, but what we put to people is that if you engage in the ACP process, it actually takes some of the fear away as you plan in a way that reflects your values and your priorities.
“It takes that responsibility away from your loved ones as well. So rather than putting it on your children, for example, to make those medical decisions that often need to be made in a moment's notice when, perhaps, you’re actively dying –those decisions are made well in advance.”
ACP in WA involves making a will, filling out an enduring power of attorney, an enduring power of guardianship, and an Advanced Health Directive, and Palliative Care WA’s workshops help people to start to consider what their values and priorities are, before using that information to complete the forms.
Workshop value
“The workshops are often most people’s first introduction to palliative care and as part of those discussions, we talk to people about what palliative care really is,” she explained.
“We try and dispel the myths by providing positive information about how palliative care can contribute and try to discourage people from shying away from palliative care because they think it means ‘I'm going to die tomorrow’.”
The discussion also includes VAD,


Doing death differently
though Ms Glogowski explained that as the legislation currently stands, a person must have the capacity to seek and receive voluntary assisted dying, ruling out the use of such an option in the ACP process.
“As the legislation currently stands, people cannot nominate VAD as part of their enduring power of guardianship or their advanced health directive because those two documents come into play if, and when, someone loses capacity,” she said.
“If you have the capacity, right up to the point that you die, you make the decisions about what treatments you receive – when and how. If you lose capacity, then your enduring power of guardianship or your AHD comes into play - that is your voice speaking for you when you don't have capacity.
“However, having said that, we do openly talk about VAD in our workshops. People want to know about it, people want to know whether that's an option for them and we are forthcoming in sharing that information with people.
“We recognise it as an option at end of life and it's important to acknowledge that most people who receive voluntary assisted dying will receive palliative care up to that point, the two are inextricably linked.”
The Advanced Health Directive is a treatment form directed at medical practitioners guiding their treatment of the patient during their end-oflife care and although Palliative Care WA can assist with completion, Ms Glogowski stressed that the person’s GP should be consulted.
“We really encourage people to consult with their treating team, GP or their medical practitioner in regard to finalising that documentation, because medically, they know you better than anybody,” she said.
“However, we recognise that GPs are incredibly busy and often don't have the time to sit down with someone and work through this documentation – which can take hours – and that's the support that
we provide to the system: we have staff who are funded to do that work with people before they have that final conversation with their medical team.
Help at hand
“Our workshops help to inform people about these options and Palliative Care WA has recently unveiled the Advance Care Planning Support Service, where our team members will visit people in their homes to help them complete this process.
“Workforce is, of course, a significant issue for palliative care as well, but there is a growing interest in palliative care volunteer services.”

She said New South Wales and Victoria have highly developed palliative care volunteer programs that Palliative Care WA would like to emulate.
“We are working with a network of aged care providers and community organisations who are recognising that we have an ageing society, that we want our members to have a dignified end to their life and that there is a significant role for volunteering,” Ms Glogowski said.
“Which is why the Compassionate Communities approach is so vital – connecting participants with key people in their lives who may have drifted away, who may have become disconnected for a whole lot of reasons.
“It is critically important to try and reconnect people with their networks, be they formal, informal or both, so that people don't feel alone at this vulnerable time in their lives.”
Recently released findings from the Compassionate Connectors
program in the South West by Professor Samar Aoun, (Perron Institute Research Chair in Palliative Care at UWA, Head of Palliative Care Research at Perron Institute, and Adjunct Professor at La Trobe University), showed the initiative had been effective in improving social connectedness, reduced social isolation, increased supportive networks and built the capacity of the community and the palliative care team to work together to deliver quality care.
Research leads
“Professor Samar is part of an international movement [the Compassionate Communities Network, co-founding the South West WA branch in 2018] recognising that we will probably never be funded well enough to provide that holistic support to people from the moment of diagnosis, and that there are community resources, which currently aren't being utilised,” Ms Glogowski said.
“Her Connectors Program is a fascinating example of training volunteers to work with individuals and families to help them connection with both informal and formal supports. They guide the families in finding people in their community who may be willing to make a little contribution, be that walking the dog, mowing the lawn, taking them to their appointments or doing a pharmacy run.
“And that is hugely therapeutic, we shouldn't underestimate the power of a community working with someone who was unwell so that they feel loved, valued and supported.
“Obviously, the clinical services are hugely significant, but we need to do that in balance with activating community support so that people don't feel isolated, that they feel supported by people who value them and who are willing to make a small contribution to a person in the last stage of their lives.”
ED: Doing Death Differently summit is at Optus Stadium, November 24, 7am-3.15pm.
www.palliativecarewa.asn.au
Silverchain commemorates 40 years of palliative care
Many Australians wish to die at home rather than in hospital and one organisation has made that possible for the past 40 years.
Silverchain's Director of Clinical Operations of Palliative Care, Andrew Allsop, and Medical Director of Palliative Care, Dr Fiona
Findlay, explain why its community specialist palliative care service has been a national leader in the area for 40 years.

It’s been four decades since Silverchain started the first inhome palliative care service in Western Australia. It wasn’t possible to choose to die at home rather than in hospital during endof-life care until 1982. The service launched with a governmentfunded pilot program run jointly with Cancer Council WA, before being independently run by Silverchain in 1984.
Now, about 3500 people and their families are supported through end-of-life care each year in WA through Silverchain’s community specialist palliative care service. As Australia’s largest in-home care specialist providing care across Western Australia, South Australia, Victoria, Queensland and New South Wales, Silverchain cares for more than 105,000 people a year. Even though the community health service comprises a range of inhome support, including nursing and allied health services for people at all stages of life, the Silverchain name is synonymous with in-home palliative care.
The palliative care service was acknowledged in 2014 by the
Grattan Institute as the “innovative way palliative care should be provided in Australia”.
“Silverchain’s service has developed a very special place in people’s minds. It’s interesting that when people in the general community talk about Silverchain, one of the services that immediately comes to mind is the palliative care service,”
Mr Allsop says.
“It’s been quite a flagship service built on the work that we do for the people we support. It’s perfectly understandable why that is the case, because it carries so many emotions.”
According to the Productivity Commission, 70% of Australians would prefer to die at home, but only around 15% are able to. However, Silverchain’s palliative care service enables many more West Australians to access end-of-life care at home and, as a result, WA has the lowest number of palliative care hospital beds per capita. Almost 60% of Silverchain clients are able to die in their own homes. Silverchain’s community specialist palliative care service team supports between 570 and 580 people and
their families each day throughout the greater metropolitan area, reaching the far stretches of Peel, Waroona, Two Rocks, Bullsbrook and Serpentine, ensuring that everyone can access quality end-oflife care wherever they are located.
“The quality of your care should not depend on location. You should get the same care no matter which suburb you live in, and you should get good quality palliative care in hospital, in a palliative care unit or in your own home.”
The extensive area is covered by nine interdisciplinary teams made up of specialist palliative care nurses, doctors, social workers, care aides, spiritual care workers, and volunteers, as well as allied health such as occupational therapy and physiotherapy, and the services can be accessed 24/7.
“If an urgent referral comes through out of hours, we have the capacity to respond. We have senior palliative care nurses and doctors who are on-call, and we accept referrals seven days a week,” Mr Allsop says.
Being able to have clinicians in a patient’s home is unique to Silverchain’s service.
“We are able to have different doctors and specialists to visit patients at home, which is uncommon. There is a doctor available by telephone 24 hours a day, seven days a week,” Dr Findlay says.
“A nurse in a patient’s home at 3am can easily contact a palliative care consultant, which is unique and prevents an enormous amount of unnecessary and often unwanted hospital admissions.”
Integrated medical, psychosocial and spiritual care
Forty years on, in the midst of medical and technological advancements in modern health care, Silverchain’s community specialist palliative care service maintains a holistic, person-centred approach that takes into account the intricacies of each condition and circumstance.


“The fundamental ingredients have been there from the start, and it is the true interdisciplinary nature of what we do, while keeping pace with the incredible development and proliferation of other services,” Mr Allsop says.
“Part of what we do is being able to respond to complexity, not just within the last days or weeks of life, but there’s the capacity to respond earlier in a more nuanced approach,” he adds.
The interplay of the physical, psychosocial and spiritual domains of Silverchain’s interdisciplinary approach goes back to the origins of palliative care.
“It’s deeply embedded in what
palliative care is all about – the whole person within their social and support network,” he says. “This is a fundamental aspect of what sets palliative care apart from many other aspects of health care,” he explains.
Fundamental to end-of-life care is patient choice and quality of life. “What we need is for patients and families to have choice and for their choices to get them the best possible interdisciplinary care wherever they are. Keeping the person at the centre and giving them choice is really important,” Dr Findlay says.
“The whole aim is to ensure that the person has the best possible quality of life.”
The importance of being at home with family
For many patients at the final stage of their life, quality of life means being at home in a familiar environment.
“We have the opportunity to make a significant difference at an incredibly vulnerable period in someone’s life. You don’t get the chance to do this twice, so you’ve got to do it right. You only get one chance to be born and you only get one chance to die,” Dr Findlay says.
“The hospital setting can be a frightening place for a lot of people and can be daunting if there are visitor restrictions. The loss of privacy, the loss of choice, and the feeling of loss of control is really
significant, and particularly during COVID, the inability to have visitors.
“What gives people quality and meaning towards the end of their life is family. There’s some evidence that if people become confused or agitated at the end of life, they are much less likely to be agitated if they’re in a familiar environment.”
Dr Findlay said it’s about offering a tailored service unique to the individual and their families. “We simply ask one of my favourite questions: ‘Tell me what’s important to you?’
“If it’s a Muslim family who need burial by sunset, we’ll do everything we can to ensure that they can achieve that. If it’s a family who needs their loved one back on Country, we’ll do everything we can to achieve that. I teach medical students to just ask these simple questions, ‘What can we do? What is important to you?’”
Family and carers
The impact of palliative care is just as important for carers and family members who remain after a loved one dies, with the dying person’s experience having a ripple effect on the family during the experience and long after.
“They’re the ones who are left behind and they’re the ones who have to go on living and live with the decisions,” Dr Findlay explains. “Good palliative care and a good death actually impacts on the way that relatives and those who are left behind face their own illness and death in coming decades, which is powerful.”
Dr Findlay recognises the importance of making death and dying a natural part of life, which helps with the grieving process.
“A hundred years ago, death would have happened in homes. Children would have been exposed to
Staying true through 40 years of service
Many families have been touched by Silverchain’s palliative care service over the four decades and, in some cases, it crosses generations.
“We’ve looked after a husband and then a wife, and we’ve looked after patients who say that we looked after their parents,” Dr Findlay says. “It’s a privilege to recall how many families in the WA community we have had contact with over 40 years of the service.
“Hopefully we have had a positive impact for families at their most difficult time. We are welcomed into homes in crisis situations when families are facing things they haven’t faced before, and I think that’s powerful.
“It genuinely is a privilege to care for people at home at their most vulnerable time, with their families and loved ones around them.”
Silverchain people
Silverchain’s WA workforce comprises more than 3000 people, including nurses, doctors, support care workers, care aides, social workers, and allied healthcare professionals, and its palliative care team in WA is about 180 strong. Some of the staff have been with Silverchain for decades.
Silverchain’s community specialist palliative care service has a strong medical presence, with support from GPs and a training program from doctors and nurses in palliative medicine.
“At any one time we have 10 doctors-in-training placed with us with us. We do a lot of training in palliative medicine, and we train a lot of nursing staff to have them upskilled and able to respond,” Dr Findlay says.
“We need highly trained, highly competent staff with the appropriate structures in place to support quality care.”
Mr Allsop says there is as much complexity in the community health care setting as there is within an acute care environment. It’s different, but it’s still challenging, and people can derive enormous professional satisfaction from working in the community.
“When you’ve got a service such as ours that can offer that level of rigorous supervision and support, it’s a very attractive career option,” he says.
Silverchain’s community specialist palliative care service has integrated a specialist dementia service, a unique service launched in 2020 which won a Palliative Care WA Award in 2021. The expansion of Silverchain’s palliative care services to incorporate the dementia service provides early integration of clients requiring palliative care and adds to the interdisciplinary approach.
grandparents’ deaths and it would have been seen as a normal and a natural part of life,” she says.
“The impact of what happens before the person’s death is significant on the bereavement
experience of the family and friends who are left,” Mr Allsop adds.
Many people associate palliative care with caring for older people at the end of their life, but it also extends to young children and babies.

Dr Findlay says Silverchain works closely with Perth Children’s Hospital, caring for a number of children in their last weeks and months of life, and even babies.

“We care for the whole range of patients in their homes – some who are less than a week old, up to 99 years old and beyond,” she says.
The palliative care service for children and young people includes the management of distressing symptoms, provision of short breaks for planned respite, care at the end-of-life, and bereavement support.
“Palliative care for children and young people is an active and total approach to care, from the point of diagnosis, throughout the child’s life, death and beyond,”
Mr Allsop says. “It embraces physical, emotional, social and spiritual elements and focuses on the enhancement of quality of life for the child or young person and support for the whole family.
“Silverchain’s community specialist palliative care service collaborates closely with the Perth Children’s Hospital to ensure that a seamless level of palliative care is provided to each child and their family as they move between the hospital environment and their home.”
By Kathy Skantzos“Quality of life is fundamental to what palliative care does. It’s really about trying to ensure that the person has the best quality of life for the time that remains, and that may be days or weeks, but it can be months and longer.”
– Andrew Allsop
The new sleep interloper
Covidsomnia and coronasomnia might be the latest buzz words, but for many the situation is real. COVID-19 and its related stressors have greatly affected our sleep and, subsequently, our mental health.
Sleep was an issue well before the pandemic. The Mentally Healthy Workplace Alliance, as part of the National Health Commission, reports that, before the pandemic, one in five Australians were affected by a major sleep disorder.
But enter COVID and the situation has worsened. It’s a universal phenomenon, caused by border closures, financial worries, changes in routine, long work hours combined with home schooling, social isolation and the fear of COVID infection itself, particularly for the vulnerable and essential workers.

COVID has added extra challenges to getting a good night’s sleep, but new tools and greater awareness is helping to tackle insomnia.
Suzanne Harrison explains
A recent review in the journal Brain, Behaviour and Immunity concludes that one of the leading health consequences of the pandemic is the prevalence of sleep-related issues.
“The study's findings summarise that the COVID-19 pandemic has produced ubiquitous mental challenges, including loneliness, anxiety, fear, stress, extreme tiredness, and health concerns,” the review states, adding that the estimated prevalence of ‘covidsomnia’ globally is 36%.
Unsurprisingly, Australian sleep specialists have reported similar findings, including Professor David Hillman, a clinician and researcher at the University of WA’s Centre for Sleep Science.
“There has been anxiety about family – people have been working from home, which can be isolating; routines have changed, and sleep thrives on routine,” he said.
National research by Medibank during the height of the pandemic in 2021 found almost one in four Australians had their sleep affected by COVID-19, equating to an estimated 5 million people. Of those who had their worst year of sleep in 2021, stress was the leading cause, followed closely by financial stress or loss of income and change in work environment.
But from such a seismic shift has come a greater awareness of the importance of sleep, from both within workplaces and the general population.
Respecting sleep
“People have become more aware of mental wellbeing and the need for it,” Professor Hillman said. “And because it’s driving discussions about sleep, it drives its importance home.”
This was the case for Perth-based primary school teacher, Penny*, a classic example of the effects of a huge shift in routine.
“When I had COVID, I obviously needed to rest, so was sleeping during the day, which upset my sleep patterns even more. I was awake at 3am, 4am,” she said.
“But this pattern continued after the illness, so I became more stressed and anxious. I was worried it was Long-COVID and was trying to find ways to manage it.” Initially, she turned to sleeping tablets, but this could not be sustained longterm.
Now, as the pandemic has progressed, getting the message across about solutions to more

people like Penny is paramount.
Moira Junge, from the Melbournebased Sleep Health Foundation, says there’s concern for essential workers doing shift work and vulnerable people (financially and in terms of pre-existing mental and physical health conditions), “because they have been the most negatively affected”.

The Sleep Health Foundation is a not-for-profit charity that aims to raise community awareness about sleep and its common disorders, and to improve public health and safety.
“Burnout rates are high, distress is high, wellbeing is low, staff retention is low and access to healthcare and support is difficult,” Dr Junge said. “Our focus is on the whole society, but right now a priority area is on our essential workers.
Worker health
“Now, more than ever, we need to ensure our sleep health expertise and messages reach those shift workers to improve their sleep and reduce burnout, so we can keep
Be part of WA Health.
WA Health is looking for skilled and experienced health professionals to strengthen its workforce. Be part of the team as we continue to provide world-class public health care for all Western Australians. Be part of WA Health, where you belong.

The new sleep interloper
increasing number of self-guided CBT-I options, such as Sleepio.
in sleep medicine practices, according to Dr Kosky.
workers healthy, as well as get people back into the workforce.”
Public health prevention programs to deal with chronic insomnia and mental health problems have subsequently been cited in various research papers around the world as an important solution.
As such, the Sleep Health Foundation ran the first-ever Sleep Week in September.
The week was kicked off ahead of the start of daylight savings with a focus on fatigue and burnout, the importance of rest, and how to manage life post-COVID. The foundation encouraged workplaces, schools and businesses to set aside an additional 20 minutes during their day to allow students and employees to take a communal break.
The idea was to give people a moment to relax with a cup of tea, step away from electronic devices, or take a short (work from home) power nap. Ideally, an allocated 20 minutes gave them the chance to rest without guilt.
Elsewhere, Alexander Sweetman, research fellow at the Adelaide Institute for Sleep Health at Flinders University and Clinical Sleep Technician at Flinders Medical Centre, SA Health, is a proponent of cognitive behavioural therapy (CBT-I) for treating insomnia and reducing symptoms of anxiety and depression.

“We recommend CBT-I as the most effective treatment for insomnia,”
Dr Sweetman says, who has been recruiting GPs in Australia for a trial of the app, Sleepio, already available in the UK and US.
Sleepio is an online program that includes six weekly sessions with an animated online character, "The Prof" who delivers CBT-I. This treatment has previously been delivered by trained psychologists/ therapists, but there are now an
“This app is special because it is supported by a large amount of scientific evidence – something that many apps or products in this space don't yet have,” says Dr Sweetman. “This doesn't mean that a self-guided, online approach will be most suitable for everyone, but it is fantastic to have these online options alongside trained therapists and psychologists to increase availability of CBT-I.”
Is it Long-COVID?
For a smaller group of people, there is also the question of whether COVID infection can cause insomnia for a prolonged period as part of Long-COVID. This, however, is complicated by the fact that poor sleep can be intertwined with a host of other Long-COVID problems.
Dr Christopher Kosky, consultant physician in respiratory and sleep medicine at Sir Charles Gairdner Hospital, said sleep disturbances in general had been a common symptom in patients who had COVID infection or suffered from Long-COVID.
“That includes either insomnia (trouble initiating or maintaining sleep) or wanting to sleep a lot of the time (hypersomnia),” Dr Kosky said.
“In addition, there can be a disruption to the natural circadian rhythm. Usually, attention to good sleep habits and sleep retraining with cognitive behavioural therapy for insomnia can help. This is the gold standard treatment for insomnia.
Hypersomnia that is not improving needs assessment by a sleep specialist.”
In another move to tackle sleeplessness, over-the-counter melatonin product Circadian was recently introduced in Australian pharmacies for the over-55s. Melatonin is produced by the brain in response to darkness and regulates our natural circadian rhythms, our sleep patterns and quality.
Another development resulting from the COVID-sleep connection is the rapid uptake of telemedicine
“From sleep retraining for insomnia to the initiation of CPAP for patients with sleep apnoea, we can monitor and alter settings from afar,” he said.
“We had developed this model of care before the pandemic for patients in remote WA and moved it to all patients during COVID. We have done research that shows it is as effective as face-to-face.”
Ancient wonder
As for Penny, she decided to take matters into her own hands after a friend told her about Vedic meditation. This involves undertaking a four-day course of 90 minutes of led meditation a day, followed by two 20-minute solo meditation sessions.
Vedic meditation is done sitting up, so convenient for office workers or when you first wake up. It does not involve an app or any other tools other than utilising a single word or phrase that ultimately allows your brain to clear for as many of those 20 minutes as possible. Ideally, there is no need to concentrate, to focus or to try to stop thoughts.
To some people, this may sound like a lot of time to dedicate to meditation, but if a full night’s sleep without medication is the outcome, then for people like Penny, it’s been worth it.
“I now sleep through the night when before I was turning to sleeping tablets,” Penny says. “It also helps with brain fog and simply to clear your mind.”
It seems the pandemic has triggered a major shift in how we think about, and deal with, sleep.
As Professor Hillman concludes: “People do take sleep for granted. It’s in this area that COVID will have an influence forever.”
ED: The Sleepio trial in Australia is still running. Dr Sweetman is recruiting GPs (who can refer patients to the trial) and has also have developed his own digital CBT-I program, with a trial underway that people with insomnia can access without a GP referral.
Penny* is not her real name



Screening Saves Lives
It’s
To celebrate Pride Month, cancer screening programs in WA are encouraging general practices to order the Screening Saves Lives resources. These tailored resources featuring WA LGBTIQ+ community






promote participation, provide
information, and foster an inclusive, safe service environment.
Resources include posters
and a social media
practice to
To view and download resources visit: www.breastscreen.health.wa.gov.au
To order hard
wacpcn@health.wa.gov.au
Research demonstrates higher rates of certain cancers among the LGBTIQ+ community, including bowel,
however, improve this statistic by inclusive
and providing
Innovation vital to success
While Western Australia boasts one of the best health-care systems globally and readily adopts incoming technology from the outside, it finds it much harder to back local innovators and their technologies.
Clinical research is key to improving human health outcomes, and we know the best standards in healthcare provision come from systems that engage in such activities. Through research and clinical studies, patients can get early access to new therapeutics and treatment methods, be treated by skilled clinicians armed with the latest knowledge in their field and receive the highest standard of care through increased monitoring.
Treating physicians have deep insights into the unmet needs that require new and innovative solutions. So, it should be a given that they are the primary drivers of change, as well as the go-to collaborators for those developing new approaches to tackling illness, right?
WA has produced some leading lights in this space that may lead people to believe that this is indeed the case. We know Fiona Stanley’s work on folate in spina bifida, Barry Marshall’s work on H. pylori and stomach ulcers, and Fiona Wood’s spray-on skin. WA inventions are marketed globally by companies such as Cook Medical, Pajunk, Medela and others.
What is perhaps less widely appreciated is that many of these successes and breakthroughs occurred with limited local support and investment. For every success, there are many more examples of promising ideas and discoveries that never materialised locally because a clinician left the state or country, or the technology was handed over to others to monetise and we now have to spend a lot of money buying the product back.
The thing is, we are good at innovating in WA. Sure, medical school didn’t teach us the commercial piece around how to develop new drugs or how to run a company – that is where we need to partner with others to progress new ideas.
But the barriers to transitioning from a bright idea to a product that improves patient outcomes come in many forms, ranging from lack of leadership support, excessive aversion to engaging with commercial entities for fear of conflict of interest, through to procurement having a preference for overseas providers over local manufacturers.
Luckily, we still have driven individuals who persist in the knowledge that a treating clinician can help one patient at a time, while an innovator has the potential to reach thousands. At OncoRes Medical, I am fortunate to be leading a world-class team based in Perth to develop a solution to the problem of incomplete tumour removal in breast conserving surgery.
For every four women undergoing a lumpectomy procedure, at least one is readmitted for repeat surgery due to positive tumour margins. These avoidable repeat surgeries create a significant cost burden on the system, estimated at over $AU 1b in the US alone every year, not to mention the economic, physical and psychological impacts on patients and families who can survive beyond the ‘all clear’ of cancer.

Through the inspiring work of breast cancer surgeon Professor Christobel Saunders, together with biomedical engineers at UWA led by Associate Professor Brendan Kennedy, OncoRes is developing a handheld device for intraoperative detection of residual tumour at a microscale to ensure that we get all
the cancer where it belongs, in the bucket during the first surgery.
Finding new solutions to unmet medical needs and supporting those innovative ideas to become products to treat patients is what led me to venture capital (VC) and biotech investing.
For the past decade, I have followed this passion through work at Brandon Capital, Australia and New Zealand’s largest life science VC that has supported over 50 medical start-ups to date, of which we helped found over 40.
We are passionate about working with innovators to turn discoveries into products that have potential to change patient outcomes globally. OncoRes is just one of those examples, and after six years we can finally say that our locally grown technology also has the support of some excellent WA based backers, in addition to our national investors.
Many WA clinicians share this passion for innovation and are eager to help drive development of new drugs, devices and diagnostics through entrepreneurship, clinical trials and expert advisory roles. The WA Government is also an increasingly active supporter of the budding life sciences industry through several new funding initiatives.
But to fully harness the creativity of our medical innovators, we need to start removing barriers by rewarding research and trial activities, encouraging multidisciplinary partnerships, championing local innovators and products, while transparently managing conflict through highquality governance. Only then can we truly deliver on the promise of a world-class health service.
ED: Dr Giles is CEO of medtech start-up OncoRes Medical.
Doctors play a vital role in the development of innovative health care, so why are clinician entrepreneurs still the exception, asks Dr Katharine Giles
at

for aged
Hospital treatment and aged care are heavily intertwined areas of health care. Not only do people in aged care tend to require more health services, and more frequently, their ability to recover is often slower, which means more resources are needed to treat them compared with younger people, even for the same condition.
As an allied health practitioner who regularly sees patients in aged care, I’ve observed how often they are cycled through the hospital system only for their condition to deteriorate once they are discharged.
This results in an over-reliance on hospitals as their primary care
system when alternative options carry less risk and are more comfortable for patients.
Hospital in the Home (HITH), also known as Hospital Substitute Treatment, is a model designed to treat patients with illnesses or conditions that need close care and monitoring, but who are not likely to deteriorate rapidly. It offers a familiar environment for patients and minimal disruption during care.

There are several reasons why HITH should be an option for aged care.
Return home sooner
It’s no surprise that patients would
rather be at home than in hospital. One of the key advantages of HITH is being able to offer a suitable amount of health-care support to patients in the comfort of their own home. Once patients are stable, they can return home and continue

to receive regular care. Furthermore, they can also receive care that they may not have been able to access in hospital, for example allied health care, and access structures outside of the medical environment, such as social and community support.
Faster recovery
Returning home sooner also corresponds with faster rehabilitation and reduced readmissions, with one study showing a 19% reduction in mortality and a 23% reduction in re-admission to hospital. In some cases, patients may not need to be admitted to hospital in the first place, which reduces the risk of falls and accidents due to changing environments.
Lower infection risk

One significant risk of entering a hospital environment is cross-infection. Despite the best efforts of hospitals to maintain a sterile environment, the simple fact of being among other sick people means patients are potentially indirectly exposed to more sources of infection. Reducing the amount of time patients are in hospital reduces the exposure they have to infection. Even better if they manage to avoid going to hospital at all.
Lower cost to insurers
Hospital is expensive for insurers and so keeping a patient out of hospital helps to lower costs while still allowing for a suitable amount of care. Being able to achieve better health outcomes at a comparatively lower cost is an exceptional cost benefit.
However, not all insurers support HITH and some only support certain treatments. In 2019, the then Federal Health Minister Greg Hunt outlined a plan to encourage health insurers to cover hospital substitute treatment for a wider range of services. While this has stalled due to COVID-19, the pandemic has simultaneously highlighted the advantages of HITH.
Optimising bed spaces at hospitals
The pandemic has shown what happens when hospitals are overrun. It stands to reason that in a triage system, those who can be treated at home should be treated at home. Moving stable patients who can receive HITH care reduces the burden on the system and keeps beds available for more severe illnesses and conditions. The fact that health outcomes from in-home care are better is a greater incentive.
Better food
Hospital food is rarely better than a home-cooked meal. Opting for in-home care ensures that patients will always have meals that are appetising while meeting their nutritional needs. There’s also something to be said for being able to share a meal with friends and family at home as well.
With the adoption of HITH care, not only could our elderly rehabilitate faster in the comfort of their own homes, but they are less likely to experience re-admission if allowed to recuperate in a familiar environment. Allowing patients to receive quality care while reducing other risks and maintaining their lifestyle is exactly why HITH should be used for aged care.
ED: Jonathon Moody is CEO and cofounder of Physio Inq.
 By Mr Peter Ammon Foot Ankle & Knee Surgery
By Mr Peter Ammon Foot Ankle & Knee Surgery


MR PETER AMMON
St John of God Medical Centre Suite 10, 100 Murdoch Drive Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au

Making moves on Parkinson’s
A recent editorial in The Lancet Neurology calls for an urgent public health response to the burgeoning wave of Parkinson’s disease (PD) across the globe.
The doubling of deaths due to PD between 1990 and 2016 was being described as a pandemic just before the emergence of COVID-19. In fact, in January 2018, JAMA published The Parkinson Pandemic — A call to Action by leading PD researchers Ray Dorsey and Bastiaan Bloem.
They and two other leading colleagues expanded this theme in a book, Ending Parkinson’s Disease: A prescription for action, in 2020. Its publication was delayed because they removed ‘pandemic’ from their original title in view of what was emerging with COVID.
Like COVID, PD poses a major health problem and a significant impact on individual lives. It is reassuring that in June and July this year, the World Health Organization released documents outlining a plan for action, and in July the US Congress passed the National Plan to End Parkinson’s Act, after lobbying from groups such as the MJ Fox and Parkinson’s Foundation. While this is all helpful, those of us living with PD need help and support now, and also need to help ourselves. Information, guidance and inspiration are powerful forces that may potentially shape the course of one’s life with PD.
Locally, Parkinson’s WA is a good place to start with information, seminars and an outstanding team of highly experienced specialist nurses who undertake home visits. The MJF Fox and Davis Phinney websites contain a large amount of high quality, medically verified information.
An excellent book by neurologist Michael Okun, Parkinson’s Treatment: 10 Secrets to a Happier

Life, corrects many common misconceptions about the nature and course of PD, and is an inspirational read.
There is optimism and great hope for research breakthroughs that will discover some specific methods for slowing or curing PD and many different lines of research are being pursued at any given time.
It must not be forgotten that, presently, exercise has a large amount of data supporting its benefit on quality of life in PD, at least short-term improvements in motor function and, most excitingly, the possibility of slowing progression.
Much more needs to be learned about dose, timing, format, and how to adjust according to stage of the disease. If exercise is to be called a ‘medicine’ it has to be used as such with all the details and nuances.
There is tantalising data in animal models about transference of the benefits of exercise by taking serum from exercising animals into sedentary animals. This may have great implications for providing a treatment for those with more advanced disease who cannot exercise, and for other conditions such as stroke.
Exercise needs to be taken seriously, and time needs to be allocated for it almost every day. The American College of Sports Medicine and Parkinson’s Foundation exercise guidelines (2021) are an excellent backbone to create a program, providing guidance for frequency, duration, intensity and form of exercise (aerobic, strength, balance, stretching).
An ideal program involves collaboration between the person with PD, their specialist, their GP, a physiotherapist with neuro or PD expertise, and also an exercise
physiologist with expertise in developing training programs.
Finally, the psychological aspects of PD are enormous; so much of PD is invisible; even if someone seems to be moving well, it is often effortful, awkward and painful.
There may be internal tremor that is not visible. Grossly disrupted sleep, chronic, debilitating fatigue, emotional lability, anxiety, dysphagia, postural dizziness, constipation, anosmia, and many more issues which add substantially to morbidity. It is easy to become depressed, withdrawn and negative, so support through this is crucial.
Support, education and immediate adoption of healthy lifestyle and exercise from the time of diagnosis may be a way of altering the course of PD.
I have previously commented that if a negative, nihilistic image is formed around the time of diagnosis, the self-fulfilling prophecy concept, combined with apathy, could contribute to a lack of engagement in physical therapy which might accelerate progression of PD.
A practical challenge is how best to provide such support within systems of care that have limited resources. I am confident there will be ways to do this, and improve quality of life for those of us who face the struggle of living with PD every day.
ED: Clinical Professor Blacker is medical director of the Perron Institute.
There was a looming pandemic well before COVID and it needs our attention, says clinical neurologist David Blacker.
The heart of the matter

Dr
Dr

Dr
Dr
Professor

Campaign hits the mark
“One drink for you is one drink for your baby.” That’s the message of the powerful Alcohol. Think Again campaign that is making future parents think before they drink.

The One Drink campaign informs women who are pregnant or planning a pregnancy and those around them that any amount of alcohol a mother drinks, the baby drinks too, and that there is no ‘safe’ level of alcohol use.
The campaign first launched in WA in early 2021 and is guided by the national alcohol guidelines, which recommend that women who are pregnant or planning a pregnancy should not drink alcohol.
Published in the journal Drug and Alcohol Review in time for International FASD Awareness Day, our new study evaluated the impact of the One Drink campaign among West Australians. The George Institute researchers analysed data from 889 WA respondents, about two-thirds female, one-quarter of which were either pregnant or planning a pregnancy. Twothirds of respondents were in the 26 to 45-year-old age group, there was an even spread across socioeconomic status, and onequarter resided in regional or remote areas.
The research showed that in just six months of being aired, the campaign resulted in 71% of respondents recognising the campaign. This was even higher among females who were pregnant or trying to conceive, with 85%.
In addition to being highly visible, the campaign was also well received, with most respondents considering it to be believable, clear, trustworthy, and memorable. Most promising, 78% said it was among the best they had seen.
As a result of the campaign, 85% of all respondents said they are now very concerned about the
potential harms from drinking during pregnancy, 83% of female respondents say they would be much less likely to drink alcohol during pregnancy, and 81% report that they are a lot more likely to support others not to drink alcohol during pregnancy. Interestingly, more than half of those who were pregnant (53%) and trying to conceive (54%) reported that the campaign taught them something new.
Perhaps most importantly, when asked what actions they took as a result of seeing the campaign, 33% of female respondents said they had decided not to use alcohol at all while pregnant. Fourteen per cent also spoke to their partner about the impacts of drinking alcohol during pregnancy and 7% of all respondents said they spoke to a health professional as a result of seeing the campaign.
This research shows that welldesigned campaigns on the effects of alcohol use during pregnancy can influence the drinking behaviour of future parents.
In addition to the One Drink
campaign, a key component of the Mental Health Commission’s FASD prevention program is the delivery of training sessions for health professionals and service providers. Those interested in the training sessions and supporting women to have alcohol-free pregnancies can visit the MHC website.

Alcohol use during pregnancy can result in a wide range of harms, including the risk of miscarriage, stillbirth and low birth weight, as well as FASD. While the prevalence of FASD in Australia or WA is not known, Australia’s first prevalence study of FASD was conducted in Fitzroy Crossing in WA where one in five children born in the region has FASD, one of the highest prevalence rates in the world.
Alcohol use during pregnancy continues to be of concern across Australia. Despite the national guidelines having recommended zero alcohol during pregnancy for over a decade, national surveys show that 35% of pregnant women drank alcohol while pregnant in 2019. This highlights that there is a need to continue to communicate effectively about alcohol use during pregnancy.
The Alcohol. Think Again website has resources for health professionals, including brochures on supporting alcohol-free pregnancies.
NO FASD Australia is another resource. It’s a family-focused organisation linking those with lived experience with researchers and clinicians. Visit www.nofasd.org.au for more.
ED: Danica Keric is acting Alcohol Program Manager at Cancer Council WA, Tahnee McCausland is acting Manager of Public Education and Health Promotion Programs at the Mental Health Commission, and Professor Simone Pettigrew is Head of Food Policy at The George Institute for Global Health.
The ‘glass baby’ works: evaluating the Alcohol. Think Again One Drink campaign shows impressive results, say researchers Danica Keric, Tahnee McCausland and Professor Simone Pettigrew

 Editor
Editor
Ageing gracefully or disgracefully
There is much talk and even more hand-wringing about the ageing population. It is taken as a given that demands for a variety of health and aged care services will increase. This is likely, but is it inevitable? Our belief that age must be accompanied by poor health and an inability to function may be misplaced.
The late Queen was in good health till the last few days of her life and passed away peacefully in her own home. That she had access to the best medical care does not totally explain this. Genetics plays a part, yet her sister died aged 71. The component most overlooked though is how people look after themselves.
Surveys of centenarians consistently show a similar theme. People who live a healthy long life tend to eat sensibly, not be significantly overweight, are physically active and have good social connections. Add to that, not drinking excessive alcohol and not smoking and we have a formula.
Populations in Japan and Sardinia with the longest life expectancies largely adhere to the ‘successful formula’. We also know that a car which is well maintained will be in better condition for longer. The human body is more forgiving than a car, but ultimately the same principal applies.
In September, I saw Kiss on their farewell tour. Founding members Gene Simmons and Paul Stanley are in their 70s. Stanley did a ‘fly over’ the audience and while not as athletic as Pink, did well for a guy with an artificial hip. Mick Jagger and Keith Richards, both 80 next year, are still touring. The latter has not led the most abstemious life.
In medicine, we typically look for a better ambulance at the base of the cliff rather than a better fence at the top of it (the two are not mutually exclusive). We tend to dismiss those who age well as ‘lucky’ rather than express more curiosity as to why they may do so.
Through COVID, nobody sought to ask older people whether they wanted to not hug their family. Nobody asked them about whether quality of life mattered. Nobody asked them what their priorities were. Going forward, if we are genuinely interested in the wellbeing of the older population –their opinions and values must be sought.
Life has no guarantees, and the best fence can be scaled. Ageing rockers and the late Queen enable us to reflect on what is possible and why that may be the case.
In medicine, we typically look for a better ambulance at the base of the cliff rather than a better fence at the top of it (the two are not mutually exclusive).












A geronto-rheumatologist's view of the 'giants of geriatrics'
By Dr Charles Inderjeeth, Geronto Rheumatologist, Nedlands
There is emerging interest and evidence that provides some support that ageing, and more especially pathological ageing, may be immune mediated –‘inflammaging’. Autoimmunity is where the immune system cannot distinguish between pathogens such as bacteria and own cells and attack, causing damage to own cells. This is the pathogenesis of immune-mediated diseases including rheumatoid arthritis.
In novel research, published in Alzheimer's & Dementia, the authors suggest that Alzheimer’s dementia (AD) is a chronic autoimmune disease within the immune system of the brain. Furthermore, cardiovascular disease is the main driver of excess mortality in rheumatoid arthritis (RA) and osteoporosis (OP) and treating both conditions with anti-tumour necrosis factor (TNF) and bisphosphonates, respectively, reduce cardiovascular mortality significantly by up to 30% by three years. An immune target is hypothesised for the improvement.
Colchicine, another immune agent targeting neutrophils, has been demonstrated to improve cardiovascular outcomes and has advocates for its use in cardiovascular protection.
The concurrence of comorbidities in ageing also raises the possibility that there are common pathways in ageing-associated diseases that may have implications for future therapeutic options. Advocates for the neologism of ‘inflammaging’ suggest that ageing like autoimmune disease are due to immune dysfunction.
RA may accelerate ageing resulting in reduced life expectancy (up to 10 years) due to premature onset of comorbidities including cardiovascular mortality. Combining RA with pathological ageing exponentially increases the risk of premature mortality.
Ageing may be due to a chronic subclinical inflammatory status where upregulation of CRP, IL6,
Key messages
Ageing is inevitable but healthy ageing is the goal
Be aware of the ‘geriatric giants’ and proactively screen and manage them
Pathological ageing affects multiple organ systems and addressing common targets may have more universal benefit e.g., inflammation.
TNFα, IL1 β has been described. In healthy (physiological ageing), IL6 is reported to be the best predictor of mortality. In frail (pathological ageing), TNFα is reported to be the best predictor of mortality. These cytokine targets in RA correlate with autoimmune and age-related diseases e.g atherosclerosis, insulin resistance, AD and OP.
Identifying common pathways in pathogenesis will lend itself to identifying common targets for preventative and therapeutic strategies. We have multiple local WA studies looking at crosstalk between bone and brain, two organs significantly vulnerable to the impact of ageing, and the benefit of medications for AD in reducing OP risk. Watch this space.
Table: Targeting the Geriatric Giants
Screening patients for risk factors e.g nutrition, dementia, delirium, depression, falls and fracture risk
Optimisation of medical care and addressing comorbidities e.g autoimmune and endocrine syndromes
Medication monitoring and compliance (use blister packs and medication reminders)
Social/recreational needs (community centres, churches, religious groups)
Assistance with housekeeping, shopping, cooking
Adequate nutrition (Meals-on-Wheels)
Caregiver education and support
Assistance with legal matters
Respite for caregivers
Elder abuse issues
Transportation
Targeting the impact of ageing, especially premature ageing, is a fundamental strategy to improve healthy ageing and reduce the impact of pathological ageing, which has significant impact on patients, carers, health care systems and funding providers with an ageing demographic.
Geriatric giants
This is a term coined by geriatrician Bernard Isaacs in 1965 and refers to the principal chronic disabilities of old age that impact on the physical, mental and social domains of older adults. Many of these conditions, commonly misperceived to be an unavoidable part of old age, can in fact be improved.
These are dementia, delirium, depression, incontinence, orthostatic hypertension, falls and dizziness, osteoporosis, polypharmacy, pain, failure to thrive, frailty and elder abuse. He had foresight in identifying the impact and consequences of ageing. At that time, he named the geriatric giants as immobility, instability, incontinence and impaired intellect/memory.
Our understanding of geriatrics has evolved over the subsequent years. The modern ‘geriatric giants’ have evolved to encompass the four significant new syndromes that overlap and help us understand those described previously i.e., frailty, sarcopenia, the anorexia of ageing, and cognitive impairment. These conditions are the sentinel features in falls, hip fractures, depression, and delirium. Early detection of these syndromes and intervention to correct these early signs of accelerated ageing can reduce disability, hospitalisation, institutionalisation, and mortality.
It is important to make sure patients have appropriate care needs met to prevent them from developing the geriatric giants. These are listed in the table.
Author competing interest – nil
Dr Simon McRae joins Western Haematology and Oncology Clinics
more than 20 years’ experience in both clinical and laboratory haematology and a dedication to providing patient-focused care and education.
Dr Simon McRae has enjoyed an impressive medical journey in Australia and internationally and now takes up the role as senior consultant haematologist with Western Haematology and Oncology Clinics in West Perth.
Dr McRae has special interest in thrombotic and haemostatic disorders and broad experience in the management of malignant haematological conditions. He has been involved in clinical trials as principal investigator and published more than 50 peer reviewed publications and book chapters and acted as a contributing author to consensus international guidelines in his areas of interest.
At Western Haematology and Oncology Clinics, his goal is to offer high quality, best-practice care for his patients, educate and inform, continue his own professional development and expand his knowledge base in a new environment.


“Making care patient-focused and providing education and accurate information in a straightforward, but compassionate manner, has been a consistent and important theme everywhere I have worked,” he says. After completing haematology training in Tasmania, New South Wales and Scotland, Dr McRae undertook a three-year clinical fellowship in venous thrombosis
Australia, including time as Director of Clinical Haematology at both the Royal Adelaide and Launceston General Hospitals.
As a result, he says he now has a clear strategy to empower patients when it comes to his role at Western Haematology and Oncology Clinics.
“All treatment options have benefits and risks, and the balance between the two will be perceived differently by individuals. Presenting all the information that a patient needs to make an informed decision is therefore important. People need to have accurate and realistic information to fully engage with treatment that can be potentially difficult,” he says.
“The decision not to treat or overinvestigate is often as important as the one to proceed with treatment, particularly in a setting where increasingly we are detecting laboratory abnormalities in asymptomatic individuals.”
Like many haematologists, Dr McRae says he was attracted to the balance of both clinical and laboratory disciplines, and the opportunity to take a patient though both the diagnostic and treatment pathways.
During his medical career, Dr McRae has also witnessed and experienced many changes and challenges.
“Underlying molecular pathophysiology of conditions has changed treatment dramatically,” he says. “We no longer have to use broad based shot-gun type therapies for many of the haematological malignancies.
outcomes dramatically, but also increased workload for the broader haematological community.
“The advent of effective oral anticoagulants that do not require monitoring has also been a game changer during my career, as had the availability of effective subcutaneous treatment options for haemophilia A (and soon B).”
Dr McRae is a man of many talents, not only being an accomplished haematologist, but also a musician and keen tennis player.
“I have played regularly in bands for the past 30 years and am currently recording an album with my partner – who sings far better than me –and we hope to have that out in six months.”
The WA general manager of Montserrat Day Hospitals, Brendon Ball, says Dr McRae is an excellent addition to the team and will make an important contribution to haematological medicine in the State.
Patients of Western Haematology and Oncology Clinics are able to receive comprehensive, personalised treatment from a multidisciplinary team under one roof.
Dr McRae has previously served on the executive of the Australian Society of Thrombosis and Haemostasis (ASTH now THANZ) and was chair of the Australian Haemophilia Centre Directors Organisation (AHCDO) for more than six years.

Biochemical changes with ageing: are laboratory cut-offs appropriate?
By Dr Michael Page, Chemical Pathologist, Jandakot
The cut-offs that appear on laboratory reports, intended to flag results that may signify disease, have various origins and purposes.
A minority are diagnostic of particular disorders, based on evidence of clinical outcomes.
For example, an HbA1c result of ≥ 6.5%, found in a large clinical study some years ago to be an inflection point for the development of microvascular complications, became a diagnostic criterion for type 2 diabetes mellitus.
By contrast, most laboratory cutoffs are reference intervals : lower and/or upper limits defining a range of results seen in the majority (often set at 95%) of a population believed to be free of relevant disease. Therefore, a proportion of flagged results will not indicate any disordered physiology and, conversely, patients with non-flagged results may have disease; hence, the more pedantic pathologist’s aversion to terms such as ‘normal’ or ‘abnormal’ results.
Some reference intervals are partitioned to account for expected age- and sex-related differences. Older people are underrepresented in reference interval studies, so data to confidently establish ageappropriate reference intervals for this group are frequently lacking.
Systemic biases in recruitment may partly account for this. Another often-cited factor is the difficulty in finding older people who are free of relevant diseases in whom reference values can be established.
There is debate as to whether a ‘healthy’ population is the best one from which to draw reference values. As an example, cut-offs for cardiac troponins are based on the 99th percentile of a healthy reference population, but many older and unwell inpatients without primary cardiac disease have values above this.
Mariathas et al (2019) found an upper reference limit for older inpatients that was more than 10 times higher than the established 99th percentile. While inpatientand age-specific troponin reference intervals could reduce overinvestigation and inappropriate treatment, the significant complexity they would introduce to result interpretation and clinical protocols is a major barrier.
Even where age-specific reference intervals can be defined using a representative, age-matched population of patients thought to be free of relevant disease, their implementation may not be appropriate.
For example, some studies have found a lower reference limit for serum sodium of 132 mmol/L in older people, compared with 135 mmol/L in younger adults. However, it is also known that even mild hyponatraemia (sodium 130 - 134 mmol/L) is associated with adverse outcomes, including falls and mortality. Therefore, even those thought to be free of significant disease, but with mild hyponatraemia by a young adult standard, could be at increased risk.
On the other hand, some hormones exhibit age-related changes that can be safely incorporated into clinical practice.
For example, mean thyroid stimulating hormone (TSH) concentrations rise with age, but this may not be detrimental. There is some evidence that older people with higher TSH concentrations within the reference interval, or subclinical hypothyroidism with TSH up to 10 mU/L, have lower mortality and, unlike in younger adults, no increased risk of atherosclerosis.
The establishment of age-related TSH reference intervals for older people is complicated by the nonstandardised nature of TSH assays, and disagreement over appropriate upper reference limits for TSH in general. Nonetheless, local and international guidelines support higher TSH treatment targets, for example up to 6 mU/L (compared with approximately 4 mU/L in younger adults), for older adults on thyroid hormone replacement therapy.
Reference intervals are inherently imperfect, but with further research could be improved for older people. In the meantime, the basic principle of interpreting laboratory test results within the overall clinical context applies, supplemented by advice from relevant clinical specialists and pathologists where required.

– References available on request.
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Cerebral amyloid angiopathy: a silent cause of haemorrhagic stroke
By A/Prof Hamid R. Sohrabi, Centre for Healthy Ageing, Murdoch
Approximately 56,000 Australians have at least one stroke annually and over 10,000 individuals die from stroke each year. Stroke in older adults is a major risk factor for dementia, disability and death.
Cerebral amyloid angiopathy (CAA) is a common cause of stroke in older adults and results from the accumulation of β-amyloid protein within the media and adventitia of small to medium-sized arteries and capillaries of the leptomeninges and cerebral cortex.

It is considered a cerebrovascular condition resulting in lobar intracerebral haemorrhage and cognitive impairment and commonly seen in older adults. A high prevalence of CAA has been reported in patients with Alzheimer’s disease (AD), with advanced CAA present in approximately 25% of AD brains.
Similar to other old-age conditions, CAA has young and late onset forms. The former can be seen as familial or sporadic. With ageing, the risk of sporadic CAA increases significantly.
The familial forms of CAA are autosomal dominant and result from genetic mutations in one of several genes. The hereditary cerebral haemorrhage with amyloidosis, Dutch type (HCHWA-D) or Dutch-CAA is the most common form of familial CAA and is seen due to mutation in the amyloid precursor protein (APP) gene located on chromosome 21. Usually, those with Dutch-CAA experience the first haemorrhagic stroke before the age of 65. The Dutch-CAA, like other types of CAA, does not have a disease modifying treatment or medical preventive plan available. Patients and their medical doctors may not become aware of the earliest signs until the first stroke, which can be fatal in about one third of people. So far, there is no specific sign, symptom, imaging or non-imaging biomarkers that can predict the time and brain region of the first
Key messages
Moderate-to-severe CAA affects 48% of the general population and 23% of people with Alzheimer's disease (AD) Although approximately a quarter of people with AD have severe CAA, about half of those with the latter will receive a diagnosis of AD due to signs and symptoms
CAA course of progression is unknown (when and in which part of brain) and no prevention or preclinical screening is available.
haemorrhagic stroke. Hence, the “silent cause of stroke” well describes the progression of this condition.
The diagnosis of CAA in clinics relies on the Modified Boston Criteria with four categories including Definite CAA with post-mortem evidence of CAA, Probable CAA with clinical data and pathologic tissue, Probable CAA with clinical data and imaging evidence, and Possible CAA with clinical data and imaging evidence. The first two require autopsy or biopsy results supporting a CAA diagnosis, while the last two require only brain imaging evidence of
multiple haemorrhages or single haemorrhage, respectively, and age over 55.
Currently, in collaboration with two international research teams based at the Harvard Medical School, USA, and Leiden University Medical Centre, the Netherlands, we are running the first trial run-in study for those with Dutch-CAA to identify the best biomarkers for monitoring response to treatment in upcoming clinical trials. The study will be completed by mid2024 and we are hoping to start the first large-scale clinical trial for Dutch-CAA within two years post the completion of this trial run-in study.
Further, to promote clinical care and research in CAA, we are hosting the 8th International Cerebral Amyloid Angiopathy (ICAA) Conference, Perth, Western Australia (November 3-5, 2022). This is the first time that this conference will be hosted by a country outside of North America and Europe. For more information, please see the website: https://icaaconference.org
– References available on request Author competing interests
Personalised joint replacements
By Dr William Blakeney, Orthopaedic Surgeon, SubiacoWhen joint replacements were first developed in the 1970s and ’80s, the surgeon had many obstacles to overcome. The predominant focus was on survivorship of the implants.
Rudimentary instrumentation meant that standardised, systematic techniques were devised that simplified implantation, making it more reliable in the surgeon’s hands. The longevity of joint replacements in the Australian joint registry is testament to the success of this strategy.

With improved technology, the focus shifted to patient satisfaction and improved function. The ultimate goal of a joint replacement is a pain-free joint that functions like a natural joint – ‘a forgotten joint’.
The standardised, one-size-fitsall approach to joint replacement does not achieve this. Surgeons are moving to personalised joint replacements, where novel technologies have enabled a bespoke approach to each patient’s surgery which involves:
1. Sophisticated pre-operative planning to assess the patient’s anatomy and joint kinematics
2. Advanced technologies for implementing the surgical plan, such as robotics and patientspecific guides
Key messages
New precision technologies allow surgeons to plan and execute joint replacement surgery more accurately



Patients have a better, longer functioning joint, with greater satisfaction
The “holy grail” of joint replacement surgery is a forgotten joint.
3. Custom implants where a standard implant will not fit the patient’s anatomy or pathology.
Total knee arthroplasty
Studies show that up to 20% of patients are not satisfied with their knees following knee replacement surgery.
Gait analysis studies demonstrate that patients with prosthetic knees do not have a normal gait pattern. One reason for this is that surgeons have been altering the patient’s normal anatomy to put in a knee replacement in the same average alignment for all.
We know there is a huge variety in knee anatomy and therefore by putting all knees in the same neutral alignment, we are reproducing <1% of patients’ anatomies. Known as
mechanical alignment strategy, this was introduced when knee replacements were first developed, as instrumentation was rudimentary and errors of alignment frequent.
The problem with this strategy is that it frequently produces imbalances in the native soft tissue envelope, when a new bony alignment is introduced. The surgeon then must compensate for this imbalance by releasing soft tissue and ligaments till the knee feels balanced.
What has then been created is a functional knee, but not surprisingly one that has abnormal kinematics –and may leave a small but significant number of patients unhappy.
More recently there has been a move towards reproducing the patient’s anatomy with kinematic or personalised alignment, made possible by using pre-operative three-dimensional imaging to accurately assess the patient's knee and standing anatomy.
We can then accurately plan our bone cuts to within one degree or 1mm. I use a robot intra-operatively to execute this plan. The robot also allows for intra-operative assessment of soft tissue tension to ensure that the knee will be well balanced prior to performing the bone cuts.
Studies show that knee replacements performed this way have more normal gait patterns and greater patient satisfaction.
Total hip arthroplasty

Hip replacement (one of the most successful operations in history) has high patient satisfaction with generally very good function. The Australian National Joint Replacement registry shows that dislocation is the most common cause of revision in the first five years.
A dislocating hip is a devastating complication for patients. One of the main causes of dislocation is incorrect positioning of the components in a hip replacement, possibly from surgical error or abnormal hip kinematics in the individual patient.
The hip-spine alignment is increasingly understood as a cause
for dislocation. The hip socket or acetabulum, changes position from sitting to standing due to pelvic tilt, and this varies from patient to patient. A standard AP and lateral hip x-ray provide no information about these changes in acetabular position.
Some patients due to spinal stiffness or abnormal alignment may be ‘stuck sitting’ or ‘stuck standing’. The surgeon should alter the position of the cup to compensate for this, or sometimes change to a different prosthesis completely. Advanced technologies using pre-operative CT scans and imaging in functional positions (sitting, stepping up, leaning forward) allows modelling of the patient’s changes in acetabular position and adjustment of implant position accordingly.
Intra-operatively, 3D-printed customised guides with laserassistance allow precise positioning of the prosthesis reducing dislocation risk and accurately reproducing the leg length. In patient’s where this sophisticated pre-operative assessment suggests they are at high risk of dislocation, a specific dual mobility prosthesis (a more forgiving implant with reduced dislocation) risk is used.
New technologies are allowing the surgeon to accurately plan and execute shoulder replacement surgery to maximise patient outcomes.
Total shoulder arthroplasty
Pre-operative CT scanning again allows for accurate positioning and simulation of joint range of motion. Intra-operatively, use of patient specific guides and computer navigation improves the surgeon’s ability to execute the plan. Sometimes, this is not enough, and a patient may have such severe pathology or abnormal anatomy that a custom-made implant is required.
The images show a patient with severe glenoid bone loss due to advanced arthritis with the humeral head wearing away the posterior glenoid due to posterior subluxation of the humeral head. This cannot be corrected satisfactorily using a standard implant. Technologies with 3D-printing to create a customised implant for the patient are used. We need to reconstruct the bone loss, to create a stable and wellfunctioning implant.
Author competing interests – nil

multidimensional,


in the



Extracorporeal Shockwave Therapy for chronic musculoskeletal conditions
By Dr Arjun Rao, Sports Physician, Floreat
Extracorporeal Shockwave Therapy (ESWT) is used to treat a variety of musculoskeletal, primarily chronic, conditions, particularly those affecting medium to large-sized tendons and their insertions on bone.

These include plantar fasciopathy, Achilles tendonopathy, retrocalcaneal bursitis, common extensor tendinopathy (tennis elbow), common flexor tendinopathy (golfer’s elbow), calcific tendinopathy (supraspinatus tendon, etc.), patellar tendinopathy (jumper’s knee), Morton’s neuroma and chronic stress/non-union fractures.
ESWT has been available in Australia since the mid-1990s but has recently been popularised with the advent of low-energy ESWT. It is an intervention that stimulates the body’s natural healing process. Additionally, ESWT has been shown to have a direct effect on local nerve endings resulting in a decrease in pain.
It is important to understand the difference between low energy and high energy ESWT when considering whether or not your patient is an appropriate candidate for ESWT, and which type of ESWT is most likely to yield positive results in the treatment of the condition.
Focal shockwave therapy
High energy ESWT or ‘true’ (focal) shockwaves are classified as short duration (approx. 10 msec) high energy pulses (5-100MPa) that break the sound barrier resulting in a shockwave. High energy shockwave technology allows the shockwave to be focused directly through the affected tissue resulting in several effects:
• The mechanical pressure and tension forces applied to the tissue increases cell membrane permeability, thereby increasing microscopic circulation and metabolism within the treated area, promoting healing and potential dissolution of calcific deposits
• The pressure front creates
Key messages
ESWT produces a regenerative and tissue-repairing effect in musculoskeletal tissues
When comparing radial and focused shockwave therapy, the main considerations are penetration depth and localisation of the treatment
Radial shockwave therapy plays a role mainly in superficial tissue injury.
“cavitation bubbles”. When they collapse, they create a force that has a mechanical impact on the treated tissue, which helps to break down calcific deposits embedded in damaged tissue.
• Focal shockwaves stimulate osteoblasts (cells responsible for bone healing and new bone production) and fibroblasts (cells responsible for healing of connective tissue such as tendons).
• Focal shockwaves diminish pain through hyperstimulation anaesthesia – local nerve endings are overwhelmed with so many stimuli that their activity diminishes resulting in short-term reduction in pain – and are the gate-control mechanism, whereby local nerves are stimulated to recalibrate perception of pain and result in longer-term reduction in pain.
Types of shockwave therapy
There are three different mechanisms for generating shockwaves resulting in three different types of ESWT device. These are electromagnetic – “true” shockwave (focal), piezoelectric and electrohydraulic – low-energy shockwaves (radial).
Low-energy shockwaves are generated by a radial pressure wave and differ from ‘true’ (focal) shockwave technology. Low-energy shockwaves travel at a much slower speed and do not break the sound barrier and hence a true shockwave is not produced.
Low-energy shockwaves are longer, slower and less intense. Radial pressure waves diverge from the source unlike high-energy shockwaves that converge on a target, resulting in less energy applied to the tissue with lowenergy ESWT vs high-energy ESWT.
Due to the reduced cost of lowenergy shockwave machines, many patients may have the wrong impression that they have received focal shockwave therapy but there are certainly differences in effectiveness of high-energy vs lowenergy shockwave therapy.
Generally, the effectiveness of ESWT tends to be generally between 60-80%. Compliance with treatment and rehabilitation recommendations are important factors in achieving optimal results.
In essence radial shockwave therapy plays a role in superficial tissues, 3-4cm in depth, spreads to treat larger areas with a slow impulse and low-energy density. Focal shockwaves have greater accuracy and greater treatment depth (up to 12cm) with a fast impulse and high-energy density. For the above reasons, true’ (focal) shockwave is the treatment of choice for insertional tendinopathy (enthesopathy) i.e., where tissue is close to bone, calcific tendinopathy and fractures where there is either delayed or non-union.
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
The painful forefoot
By Clin/Assoc Professor Gerard Hardisty, Orthopedic Surgeon, Murdoch
Pain in the forefoot is a common clinical problem and has a broad differential diagnosis. Despite careful clinical assessment, the cause of forefoot pain can sometimes remain unexplained, however, x-ray and ultrasound can diagnose most problems. Forefoot pain is essentially metatarsalgia and deformities.
Metatarsalgia
This refers to pain in the ball of the foot. Common causes include Morton’s neuroma, plantar plate instability, stress fracture, sesamoid problems and Freiberg’s disease.
The aetiology of Morton’s neuroma (interdigital neuroma) remains unclear. Repetitive microtrauma may cause the nerve to swell, which initiates the cycle of inflammation and enlargement of the nerve. Patients complain of shooting pain into the toes often made worse with footwear.
Neuromas are commoner in the 3/4th web than the 2/3rd web. Numbness, though clinically evident in the web of the toes is rarely complained of. Ultrasound is usually diagnostic. MRI only if there is any diagnostic confusion. Treatment consists of injections under ultrasound control, if caught early. With increasing length of symptoms, patients often come to surgery, which is curative.
Plantar plate instability is a common cause of metatarsalgia that is often under-diagnosed. It is a tearing of the plantar plate that can be traumatic but is usually degenerative. The exact cause is not known but it is associated with bunion formation.
The plantar plate provides stability to the metatarsophalangeal joint (MTP) but also has elastic fibres that allow movement. The commonest joint affected is the second MTP. Patients complain of “walking on a stone” and often have swelling in the forefoot. It can be difficult to differentiate between plantar plate instability of the second MTP and a 2/3rd web neuroma.
Key messages
Forefoot pain can be challenging to diagnose
X-ray and ultrasound can diagnose most problems
Surgery is indicated for intractable pain.
Clinical examination reveals the toe can be subluxed dorsally reproducing their pain (anterior draw sign). Ultrasound can be diagnostic but if in doubt an MRI is required. Treatment consists of MTP injections and strapping leading to orthotics. With chronicity, surgery is required. This involves a metatarsal osteotomy, debriding the plantar plate and re-inserting into the proximal phalanx using sutures.
The best results are when the plantar plate rupture is caught early.
If left, it can lead to subluxation and clawing of the toe. At worst it can lead to the crossover toe deformity associated with bunions.
Stress fractures are classed as fatigue (from overuse) or insufficiency type (osteoporosis).
Middle and distal thirds of the second and third MT are affected most frequently. There is pain over the metatarsals often associated with swelling in the early stages.
If the x-rays are normal, then a repeat in two weeks will often show the healing callous forming along the metatarsal. Treatment is protective weight-bearing for the first two weeks with a Darco shoe (obtainable from orthotists) and then progressive graduation to normal footwear. If symptoms
are persistent after six weeks, a CT and or bone scan is indicated. Modification of the patients’ activities are sometimes required but occasionally patients need bone grafting and internal fixation.
Sesamoid pain can be a difficult condition to treat. In the younger, more athletic patients, a six-week break from activity often settles symptoms. Occasionally a steroid injection will improve this. Plain x-rays can be normal, but a bipartite sesamoid occasionally has to be differentiated from a fracture.

A fracture usually has a history of trauma, and a CT will be diagnostic. Avascular necrosis and degenerative arthritis are more difficult to treat. Orthotics should be tried with a sesamoid rest. Sesamoidectomy surgery is a last resort as the results are variable.
Freiberg’s disease is avascular necrosis of the second MT (rarely the third MT) head. Usually seen in teenage girls and younger woman, occasionally in the older patient. The x-ray in the older patient is then usually more dramatic with fragmentation of the second metatarsal head. Aetiology –probably repetitive microtrauma. The x-ray shows sclerosis and flattening and later on, frank osteoarthritis. MRI allows early diagnosis and excludes other causes. Treatment if diagnosed in the early stages is with orthotics and cessation of athletic activities. With established avascular necrosis and fragmentation, joint debridement and metatarsal osteotomy is required.
Common deformities
Hallux valgus (bunions), Hallux rigidus (OA of the first MTP), claw toes, hammer toes, mallet toes and bunionettes (fifth metatarsal bunion) can all cause forefoot pain. Forefoot deformity is common but not always painful. Surgery is indicated for footwear problems, pain experienced daily or cosmetic issues.
Author competing interests – nil
Personal stories heal and celebrate
Volunteer biographers in a Sydney hospital tell the life stories of terminally ill patients and the results offer so much more than just a story for their families.
By Ara JansenA story is a powerful thing. Telling your personal story can be a potent tool to look back on the decisions you’ve made and why.
In the documentary A Friend in Death, the Sacred Heart Biography Service at St Vincent’s Hospital offers people in palliative care the opportunity to work with a trained biography volunteer to tell their life story.
Perth filmmaker Josh Lee was inspired to make A Friend in Death after a close friend was diagnosed with terminal cancer and prompted him to research palliative care.

“It started me thinking about how we make meaning out of our lives,” he said. “As soon as I came across the Sacred Heart Biography Service, I thought I could do something on it.”
One of the biographers is longterm volunteer Kerry Little, an adult educator and business owner in her seventh decade. She cared for both her parents with terminal illnesses and brings both that experience and compassion to her biography work. She usually does about six spoken interviews with each client – if they
are able – and at the end pulls together a book with photos telling their life story. Little has learnt from this work that in telling their stories, terminally ill patients often find for the first time their place in the world and see patterns in their lives they hadn’t otherwise recognised. But one of the most powerful things to come from these stories is the patient truly understanding they matter to those around them and their story (and in turn their life) is worth something.
“Some of them speak about things they have never spoken about before,” says Little. “It’s about letting them tell their story. We’re holding the space, holding a spiritual space and being a witness. We use the biography process to connect with them and be empathetic.”
From research and development through to completion A Friend in Death took about 18 months. Lee says while the subject was heavy, it’s some of the most fun he’s had on a film.
“I loved that this film was inclusive and collaborative with both the biographers and their subjects. People like Colin (one of the
interview subjects) were perfect and he brought such humour to the whole experience.
“This really has helped me contemplate death and what it means. I’m still thinking about it and my view of death has changed to be an important part of life and a meaningful part of life. I now live my life with a strong awareness of how I am living.
“This has shown me the importance of community connection and being part of making meaning in your life. There’s so much you can do with that with the power of storytelling. Stories are so powerful in the way we make sense of the world. I think A Friend in Death is a beautiful insight to that.”
ED: Palliative Care Western Australia offers a similar service through their Lasting Words project. They are also looking for volunteer interviewers. For more details go to: palliativecarewa.asn. au/lasting-words.
A Friend in Death screened on Compass recently and may return to ABC iView.
Palliative care – early conversations make a difference
By Dr Derek Eng, Palliative Care Physician, Subiaco
Palliative care (PC) is a medical specialty of clinicians (doctors, nurses, allied health, pastoral care) who provide support for patients with progressive, lifelimiting illness and their families. We hope to provide whole-person care (incorporating the four pillars of bio-psycho-social-spiritual) in order to enhance function and quality of life in the last few months of a patient’s life.
The reasons are multiple and complex, but the research evidence cannot be denied. Patients are not referred to specialist palliative care as often or as early as they should.
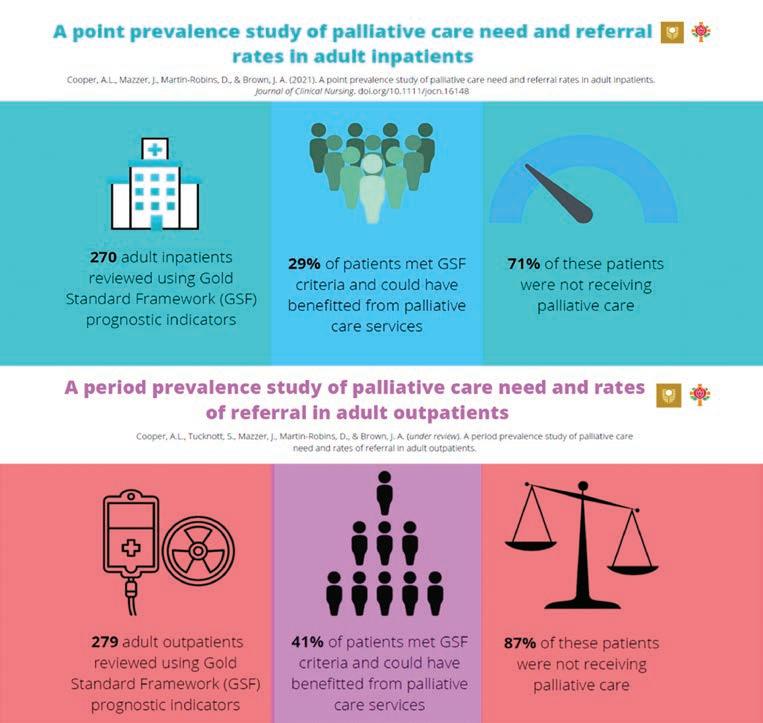
In a study looking at adults using a large WA hospital, an overwhelming 71% of inpatients were not receiving specialist palliative care even though they could have benefited when an internationally validated screening tool, the Gold Standards Framework (GSF), was applied. In another study of nine Australian tertiary hospitals, 1693 patient deaths were reviewed and 41% were referred to specialist PC in the last 2.3 days of their life.
The Supportive & Palliative Care Indicators Tool (SPICT www.spict.org.uk/spict-4all/) and GSF screening tools (www.goldstandardsframework. org.uk/PIG) have been developed to guide GPs and hospital clinicians to refer patients for specialist PC assessment because they could be in the last 12 months of their lives. Both tools are easy to use and although indicators are broad, the intent is to trigger doctor–patient conversation about life choices and health-care preferences in the context of deteriorating function or worsening symptoms.
Developing communication skills to start the “last 12 months of life” dialogue may not come naturally to clinicians. Patients have fears and concerns about death, and they value a doctor who speaks clearly, honestly and compassionately. These initial conversations usually include three key steps: 1. Breaking the (bad) news – that their health is going to deteriorate over the next few months and why.
Key messages
Patients are not referred to palliative care as early or often as they should
Communication skills to start the last 12 months of life discussion may not come naturally Education and support are available.
2. Emotional support – patients may be surprised by this and become emotional. Skills in acknowledging and validating these emotions will help.
3. Map out their health and lifestyle priorities, values, wishes and goals – find out what is most important to them about their health and lifestyle and what functions are essential, that they cannot live without (these functions define their quality of life).
Cancer Council WA run half-day, high-fidelity simulation workshops for clinicians to learn and practise
these conversations (go to www.pasce.com.au/comms).
Once patients have identified these values, wishes and goals, please encourage them to speak to their family and loved ones about this and to document it in an Advance Health Directive (AHD). The new WA version of the AHD was published in August 2022 and is a much more comprehensive document. Patients can be directed to the website by typing “Advanced Health Directive WA” into any search engine.
Should you find these conversations difficult, a referral to a specialist palliative care service (physician, nurse practitioner and a clinical nurse) may help. Most large private hospitals and tertiary public hospitals will have palliative care clinics – email referrals to the central referral service of the hospital within the patient’s catchment area.
– References available on request Author competing interests – nil
Colourful tractors lead the way
The regional town of Gnowangerup has found a way to attract tourists by making old things new again, as Ara Jansen explains.
Over the past few years, residents of the town of Gnowangerup in the Great Southern have been involved in a revitalisation project to attract tourists back to the town.
A group of concerned citizens realised they needed to create reasons for people to visit Gnowangerup. Using a Cars movie reference, local Cassandra Beeck says her town was starting to look a bit like Radiator Springs.
They came up with a number of local business initiatives – which have been highly successful – but by far the most colourful and fun idea is The Horsepower Highway

It’s a trail of 20 vintage and quirky tractors which have been restored in unique and colourful ways. Starting at Broomhill, The Horsepower Highway goes through Gnowangerup and ends in the Stirling Range National Park. Many of the tractors have been donated by local farmers and cleaned up to become interesting and photoworthy opportunities along the drive south. The plan is to continue adding to the collection.
All the tractors have names which either reflect their history or a local story.
Hero is named for SES volunteers, Lizzy is a local icon that originally helped clear a lot of the original properties in the area, and Snowy has skis on the bottom to adapt to the wintery conditions at the Bluff Knoll Ski Club. Mad Max was the one which was too far gone to restore and has become a wild sculpture using found agricultural
equipment. Lucinda is a hot pink tractor situated between two water tanks which have been painted with portraits of local women showing the diversity of contributions they make, including a farmer, an agronomist, volunteers, a sportswoman and Blair Hinkley, fondly known as “the chook lady”.
The tractors are positioned perfectly for stopping and taking photos. It’s also an opportunity to learn about each of the machines,

their history and part in local rural life.
The Dyipni (or the jeepney) is the latest addition to the highway. It was created by 14 local Filipino welders and fitters who call Gnowangerup home and is a homage to the most popular form of transport in the Philippines.

Created as a local answer to the transport scarcity after World War II, the wildly colourful open buses showcase Filipino ingenuity and creativity. This jeepney – which you can sit in – features both the colours and symbols of the Philippines in harmony with plenty of Aussie touches to celebrate both countries.

“The trail really has given us an identity,” says Cassandra, one of the creators of The Horsepower Highway and chairperson of the management committee. She’s also a local primary school teacher and farmer. “Now a lot more people are coming through our town.
“Not only do people get to see the tractors, but they also have a chance to experience the beauty of the landscape here. It’s a stunning drive. That has been great for visitors and also the locals.”
Around 250 locals have been involved in the project – all of them volunteers. There are also volunteers who have adopted each tractor and make sure they remain
in tidy condition and ready them ahead of holidays and add thematic touches for notable dates like Christmas and ANZAC Day. Finding a tin flower at each tractor will also help you Crack the Highway Code competition.
Meet all the tractors and get a map at www.thehorsepowerhighway. com.au

Arlewood celebrates family
Garry Gossati’s entry into the wine business was no doubt influenced by his great grandfather’s position as the boss (capo) of a wine cooperative in Valtellina, a region in Italy’s far north abutting the Swiss border.

Having started Arlewood in Wilyabrup in 1988, Garry seized the opportunity in 2008 to purchase and restore an established but run-down vineyard located just south of Witchcliffe in Forest Grove. It was close planted in 1999 by Xanadu’s then winemaker Jurg Muggli. Garry’s restoration was hands on. His two sons, Jordan and Adrian, are now working the small vineyard of 6.08ha. Cath Oates is the current winemaker.
In 2017, James Halliday nominated Arlewood as the Dark Horse Winery of the Year and in 2020 Gourmet Traveller Wine heralded it as the Best Small Cellar Door. With Witchcliffe being located at the southern part of Margaret River region, it has the cooling influence of the southerlies, resulting in wines with appealing acidity and crispness, the whites especially.
2021 Arlewood Villagio
A blend of 85% Semillon, 10% Sauvignon Blanc and 5% Chardonnay. Fresh attractive flavours of passionfruit and citrus with a touch of mown grass. Crisp and very lively with a long and fruity finish. The preponderance of Semillon makes it a winner. 12% alcohol – $28
2020 Arlewood Cabernet Merlot

A wine comprising 78% Cabernet Sauvignon, 20% Merlot and 2% Cabernet Franc. Stainless-steel fermented and 20% new oak maturation for 24 months Ripe plums and violets with a touch of spice. Soft supple tannins and a clean finish. Here the Merlot expands and softens the Cabernet Sauvignon making for early drinkability 13.5% alcohol – $30
2018 Arlewood Cabernet Sauvignon
From the outstanding 2018 vintage. Crushed/destem to tank, fermented on skins for 3-4 weeks with regular pump over and 24 months’ oak maturation (30% new). Berries and leafy earthy olive aromas abound. Full and supple palate showing elegance finesse with a long lingering finish. It’s a classic Margaret River Cabernet and a wine to savour. 14% alcohol – $40

2021 Arlewood Chardonnay

Lovely white peach and grapefruit mingled with a whiff of toasty oak and a hint of struck match. This may not have quite the voluminous fruit of some its more northerly neighbours but more than makes up for it with a deliciously cool crispy palate structure that shows balance and finesse. Finishes long. Very good wine indeed! 13% alcohol – $40
2017 La Bratta Rosso
50% Cabernet Franc, 43% Merlot and 7% Cabernet Sauvignon with open fermentation and 24 months in 40% new oak. The wine is named after Garry’s mother’s birth village in Valtellina and inspired by his Italian viticultural heritage. Powerful, red fruits, allspice with dried herbs and violets on the bouquet. A full and generous mouth filling palate structure. Ample tannins and a good long finish. Nice to see a good example of Cabernet Franc. 14.5% alcohol – $50.
Leaders in TMS Therapy

You’re invited to explore the ways

Stimulation (TMS) can




during a
with a

to make headway

is utilising
(OCD)
(PTSD).
can also improve the burden of

and has even been
(e.g.
tinnitus.












